Depression and mental confusion
Depression and Memory Loss: Know the Facts
Depression and Memory Loss: Know the FactsMedically reviewed by Timothy J. Legg, PhD, PsyD — By Annamarya Scaccia — Updated on September 13, 2019
Overview
Depression has been linked to memory problems, such as forgetfulness or confusion. It can also make it difficult to focus on work or other tasks, make decisions, or think clearly. Stress and anxiety can also lead to poor memory.
Depression is associated with short-term memory loss. It doesn’t affect other types of memory, such as long-term memory and procedural memory, which controls motor skills.
Other symptoms of depression include:
- feeling sad, anxious, numb, or hopeless
- a loss of interest in activities or hobbies
- having little energy and feeling fatigued
- feeling restless or irritable
- feeling shame, guilt, worthlessness, or powerlessness
- a loss of appetite and drastic changes in weight
- having trouble sleeping or sleeping too much
- thinking about death or suicide
- having physical problems, such as headaches, stomachaches, and back pain
Researchers in one 2013 study discovered that people with depression couldn’t identify objects on a screen that were identical or similar to an object they had seen previously. According to researchers, this suggests that memory can be diminished as a result of depression. Researchers in a 2015 study came to a similar conclusion. They concluded that depression might cause short-term memory loss.
Other reasons you may experience memory loss can include the following:
- Normal age-related memory loss is common and manageable. One example of this is forgetting where you put your glasses but remembering later in the day.
- Alzheimer’s disease is the most common form of dementia. It can cause progressive, irreparable brain damage and memory loss.
- Mild cognitive impairment can alter thinking skills and eventually progress to Alzheimer’s disease or other forms of dementia.
- Minor head injury or trauma can trigger slight memory problems, even if you didn’t lose consciousness.
- Forgetfulness is a potential side effect of certain medications.
- Brain tumors or brain infections can affect your memory or trigger dementia-like symptoms.

- Vitamin B-12 deficiency can create problems with your memory. This is because you’re not maintaining healthy nerve cells and red blood cells.
- Alcoholism or drug abuse can impair your mental state and abilities. This can also occur when alcohol interacts with medications.
- Hypothyroidism slows your metabolism, which can lead to memory problems and other issues with thinking.
- Brain or nerve damage caused by diseases such as Parkinson’s disease or multiple sclerosis can cause memory problems. A 2013 study found that people with depression have a greater risk of developing Parkinson’s disease.
Electroconvulsive therapy (ECT) can cause memory loss. ECT alters brain chemistry, which can reverse the symptoms of depression and other mental illnesses. If you have ECT, your doctor will perform it while you’re under general anesthesia. During ECT, your doctor sends small electric currents through your brain, triggering a brief seizure. People can experience confusion and short-term memory loss after receiving ECT treatments.
Your doctor will perform a physical exam and ask you questions to help them identify the cause of your memory loss. This can also help them determine the extent of your memory problems. Your doctor may want to know:
- when you started experiencing memory problems and for how long
- if you’ve been feeling depressed, anxious, or sad recently
- if you’re taking prescription or over-the-counter drugs regularly and at what dose
- if you started a new medication
- what tasks are difficult to start or complete
- how you’ve treated your memory issues and if it has worked
- how often and how much alcohol you drink
- if you injured your head or had an accident
- if you were recently ill
- if your daily routine has changed
Your doctor may also evaluate your memory and thinking skills with a short question-and-answer test and perform an electroencephalogram to test your brain activity. They may also run blood tests and imaging tests of your brain, such as an MRI, to help them make a diagnosis.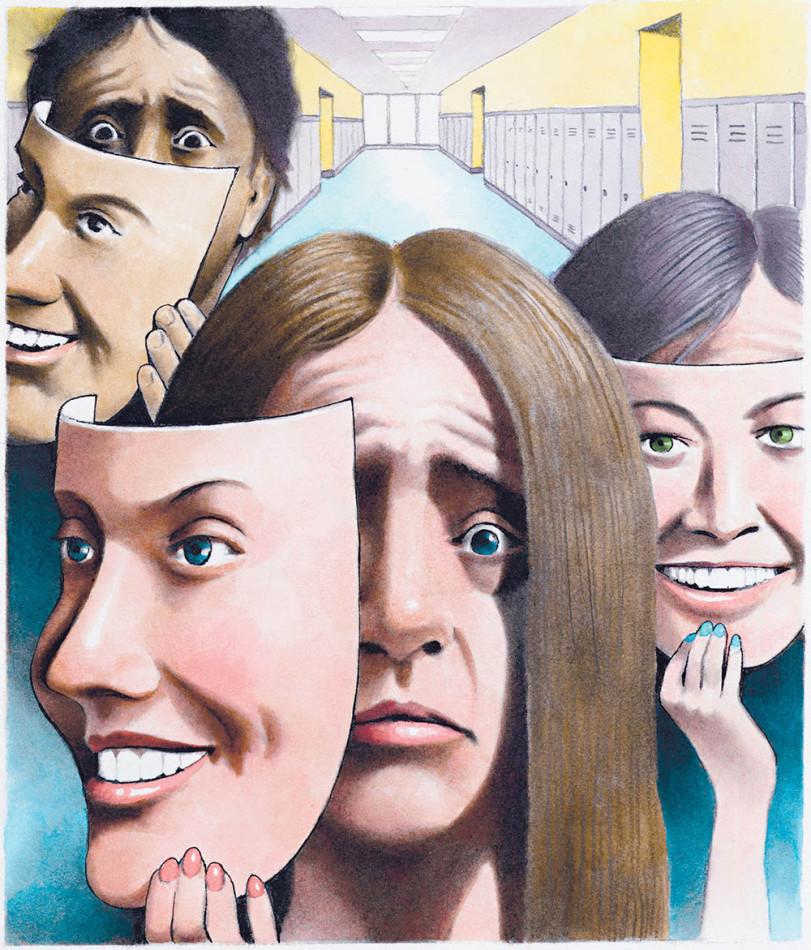 They could also refer you to a specialist, such as a neurologist or a psychiatrist, for diagnosis.
They could also refer you to a specialist, such as a neurologist or a psychiatrist, for diagnosis.
Memory loss due to depression is typically managed with regular counseling or therapy and antidepressants. Leading an active lifestyle and getting involved in your community can also elevate your mood.
You can also manage your memory loss by using memory aids. Depending on your needs, this could mean using alarm clocks to keep track of time, color-coding household items, or placing safety notes with instructions on appliances. You may also consider getting a home care provider to help you as needed. You may also consider joining a support group.
Medications that can improve memory and brain function in people with Alzheimer’s disease or other neurological disorders are also available.
If you have depression, chances are you’re experiencing a memory issue. Memory loss due to depression can either improve or worsen depending on your emotional and mental state.
If you notice that you’re having problems with your memory, you should schedule an appointment with your doctor. They can work with you to determine the cause. From there, they can create an effective treatment plan to elevate your depression and improve your memory.
Last medically reviewed on July 5, 2016
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Depression. (2016, May)
nimh.nih.gov/health/topics/depression/index.shtml#part_145397 - Hubbard, N. A., Hutchison J. L., Turner, M., Montroy, J., Bowles, R. P., & Rypma B. (2015, January 6). Depressive thoughts limit working memory capacity in dysphoria
ncbi.nlm.nih.gov/pubmed/25562416?dopt=Abstract - Mayo Clinic Staff.
 (2015, July 22). Depression (major depressive disorder)
(2015, July 22). Depression (major depressive disorder)
mayoclinic.org/diseases-conditions/depression/basics/risk-factors/con-20032977 - Mayo Clinic Staff. (2014, June 5). Memory loss: When to seek help
mayoclinic.org/memory-loss/art-20046326 - Mayo Clinic Staff. (2015, September 19). Test and procedures: Electroconvulsive therapy (ECT)
mayoclinic.org/tests-procedures/electroconvulsive-therapy/basics/definition/prc-20014161 - Medication for memory loss. (n.d.)
alz.org/alzheimers_disease_standard_prescriptions.asp - Shelton, D., & Kirwan, C. B. (2013, August 7). A possible negative influence of depression on the ability to overcome memory interference. Behavioural Brain Research, 256: 20-26
sciencedirect.com/science/article/pii/S0166432813004920 - Shen, C., Tsai, S., Perng, C.-L., Kuo, B. I.-T., & Yang, A. C. (2013, October 2). Risk of Parkinson disease after depression.
 Neurology, 81(17), 1538-1544
Neurology, 81(17), 1538-1544
neurology.org/content/81/17/1538 - Understanding memory loss: What to do when you have trouble remembering. (2015, October 22)
nia.nih.gov/alzheimers/publication/understanding-memory-loss/serious-memory-problems-causes-and-treatments
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Timothy J. Legg, PhD, PsyD — By Annamarya Scaccia — Updated on September 13, 2019
Read this next
Memory Loss
Medically reviewed by Timothy J. Legg, PhD, PsyD
Everyone occasionally experiences forgetfulness. Mild memory loss tends to increase with age and is generally no cause for concern. But progressive…
READ MORE
Depression Can Make Your Brain Age More Quickly
Researchers say depression can increase your risk for dementia.
 Here’s why and some simple steps you can take to reduce the odds.
Here’s why and some simple steps you can take to reduce the odds.READ MORE
Symptoms of Depression
Medically reviewed by George Krucik, MD, MBA
Suffering from depression on a regular basis and for weeks at a time is a sign that you need to seek professional help. Talk to your doctor.
READ MORE
Depression: The Growing American Mental Health Storm
Recent reports show depression is one of the greatest mental health challenges facing Americans today. Here’s how it may affect you or someone you…
READ MORE
What to Know About Ketamine Therapy for Depression
Medically reviewed by Nicole Washington, DO, MPH
Ketamine offers a new, fast-acting approach to relieving treatment-resistant depression. Learn the research-backed benefits and how to try it.

READ MORE
Unipolar Depression Explained — Plus Tips to Get Support
Medically reviewed by Nicole Washington, DO, MPH
Unipolar depression often refers to major depression, also called clinical depression. Learn the signs and how it compares to bipolar disorder.
READ MORE
New Study Debunks Old Theory That Depressed People Are Just More Realistic
New research raises doubts about a decades-old theory that depressed people are more realistic.
READ MORE
Task Force Recommends Depression, Anxiety Screenings for Children
A federal task force is recommending children between the ages of 8 and 18 be screened for anxiety while children 12 to 18 be screened for depression
READ MORE
More People May Experience Seasonal Affective Disorder This Year
Experts theorize that a greater number of people may experience Seasonal Affective Disorder this year.
 Here's how to spot the signs.
Here's how to spot the signs.READ MORE
Why does it happen? Causes and testing
Symptoms of depression include sadness and changes in mood. Depression, though, is a complex diagnosis that affects many aspects of functioning, including memory.
A 2018 analysis of earlier studies into the effects of depression and memory found that people with at least one symptom of depression self-reported memory complaints and other symptoms of depression. This suggests that memory loss could be a symptom of depression.
Some older people may mistake symptoms of depression as dementia. According to an older article, depression may cause a person to perform worse on brain function tests over time.
An article in the British Journal of Psychiatry indicates that some affective disorders, including depression, may increase the risk of dementia, especially if a person does not seek treatment.
Share on PinterestStudies suggest that there is a link between memory loss and depression.
People who have depression report struggling to recall particular memories. This suggests that depression can affect different types of memory, including declarative and autobiographical memories.
In a 2013 study, a group of young adults scored poorly in pattern separation. This is the method the brain uses to encode memories of similar events and other stimuli.
If pattern separation is impaired, people may become confused when thinking about where they have been, particularly if they have visited several similar places.
These findings support the idea that depression could reduce the performance of declarative memory, which involves the memory of facts and events.
The authors of the study hypothesize that depression may slow down the creation of nerve cells. This could make it difficult to form or access new memories.
One 2018 study published in Psychological Medicine found people with depression may also struggle to remember specific elements of their autobiographical memories — memories that focus on a person’s life history.
Researchers observed that people living with depression can over-generalize their autobiographical memories and recall little detail.
Researchers have also identified a link between depression and different types of memory loss, including impaired short-term memories and memory loss associated with dementia. According to the International Neuropsychiatric Disease Journal, some depression medications could also affect memory.
Short-term memory loss
Depression may cause short-term memory loss. A 2018 study on people with depression found that memory complaints had correlations with more severe symptoms of depression.
A 2014 meta-analysis of previous research found a clear association between depression and cognitive performance. People with depression had trouble with attention and memory.
They also struggled with executive function. Executive function is responsible for skills that help people focus on tasks, pay attention, and self-monitor their behavior.
Another 2014 study found that the effects of depression may affect memory even after treatment. This study found that people with a prior history of depression were more likely to remember negative adjectives from a list than people who had never experienced depression.
Dementia
There may also be a link between depression and dementia, but scientists have found untangling this link challenging.
Sometimes caregivers and even doctors may mistake symptoms of depression, including memory loss, as dementia in older people. However, a 2010 analysis indicates that this may not be a mistake.
In many cases, the cognitive impairments that some older people experience with depression could be an early warning sign of dementia.
The researchers state that depression could be an early symptom of an underlying neurodegenerative condition.
Other research has found that people with depression may have a lower volume of gray matter. For instance, a 2013 paper details gray matter changes in people with depression. Gray matter volume declined in areas of the brain associated with emotion and working memory.
Gray matter volume declined in areas of the brain associated with emotion and working memory.
People with dementia may also have decreased levels of gray matter. This suggests that depression and dementia might have similar structural effects on the brain, potentially causing some of the same symptoms.
Long-term studies
A 2019 study looked at data from the National Child Development Study, a long-term study of children into adulthood. It found that people who had symptoms of depression in their twenties were more likely to have poorer immediate memory and delayed memory when they reached 50.
This correlation does not mean depression causes memory loss later in life, as other factors, such as individual differences, could explain this phenomenon. Scientists must do more research to understand the link between depression and dementia.
Antidepressants
Researchers have also identified a link between antidepressants and memory loss.
Tricyclic antidepressants may increase the risk of memory problems in some people. Similarly, a 2016 analysis found that people taking selective serotonin reuptake inhibitors (SSRIs) also experienced a decline in memory function within 8 weeks of starting treatment.
Similarly, a 2016 analysis found that people taking selective serotonin reuptake inhibitors (SSRIs) also experienced a decline in memory function within 8 weeks of starting treatment.
More research might clarify whether this decline continues or improves after the body adjusts to the medication.
Very little research has evaluated strategies for treating memory loss in people with depression. For some people, treating depression may ease memory loss. A healthcare provider can help a person compare treatment options and track changes over time.
Other strategies may also help. Those include:
- creating reminders for upcoming events
- slowing down to commit information to memory
- working in a distraction-free environment where possible
- focusing on one thing at a time
- using digital calendars for automatic notifications
Learn more about 8 techniques that can improve memory here.
A person who has depression and memory loss should not assume that depression is the cause, particularly if the memory issues interfere with daily functioning. Dementia, head injuries, infections, and other causes may also damage memory.
Dementia, head injuries, infections, and other causes may also damage memory.
If a doctor thinks memory loss is a problem, they may recommend a person takes some memory tests. A doctor might also recommend additional testing, such as a brain magnetic resonance imaging (MRI) scan to check for brain injuries or blood work to assess for signs of infection.
A person should always see a doctor for memory loss because even subtle memory loss may signal a more serious problem.
If a doctor thinks that depression is the culprit, consider asking about strategies to improve memory and referral for psychiatric treatment. Follow up with the doctor if memory loss gets worse or interferes with day-to-day life.
The outlook for memory loss and depression depends on the cause. Some people find that their memory loss improves with treatment, or when switching to a different antidepressant. However, when depression is the cause, memory loss does not typically get worse.
When a neurodegenerative condition causes memory loss, symptoms may steadily worsen, eventually causing other cognitive problems.
When a person experiences memory loss, they may feel scared and avoid seeking treatment. However, it is essential to speak to a doctor who can ease a person’s worries, determine why they have memory loss, and offer a range of treatment options.
Depression
Russian Academy of Medical Sciences
SCIENTIFIC CENTER FOR MENTAL HEALTH
DEPRESSION (from hope to certainty).
(INFORMATION FOR PATIENTS AND THEIR FAMILIES)
MOSCOW
2008
Oleichik I.V. - Candidate of Medical Sciences, Leading Researcher of the Department for the Study of Endogenous Mental Disorders and Affective States
© 2008, Oleichik I.V.
© 2008, NTsPZ RAMS
The vast experience accumulated by mankind and reflected in many literary works convincingly shows that sadness (sadness, spleen) has always gone side by side with people, being one of the natural human emotions. None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
A depressive state (from the Latin word depressio - suppression, oppression) is a disease that concerns not only an individual specific sick person, but is also a significant burden of modern society, since it is spreading more and more widely in the world, causing enormous damage to the health of the population and the state. economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help, because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help, because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
In the most general sense, a depressive state is one of the possible forms of a person's response to the impact of stress factors. In some cases, depression can be triggered by external negative influences, for example, mental trauma, excessive educational or work overload, infection or other serious somatic disease, traumatic brain injury, changes in the hormonal background, which is especially important for the female body, regular certain medications, such as hormones, blood pressure medications, alcohol or other drug abuse. In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression. Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression. Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Manifestations of depression
Manifestations of depression can be very different. Depressive states can be manifested by a violation of almost all aspects of mental life: mood, memory, will, activity, which is expressed in the appearance of sadness, sadness, mental and muscle retardation, lasting at least 2 weeks. Depressed mood during depression can manifest itself as mild sadness, sadness, and boundless despair. Often it is accompanied by a feeling of melancholy, unbearable heaviness in the soul, with excruciating pain behind the sternum, a feeling of hopelessness, deep depression, hopelessness, helplessness, despair and uncertainty. At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
The picture of depression is complemented by the disappearance of desires, interests, a pessimistic assessment of everything around, ideas of one's own low value and self-blame. Deficiency of vital impulses is manifested in patients with a variety of symptoms - from lethargy, physical weakness to a state of weakness, loss of energy and complete impotence. Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems.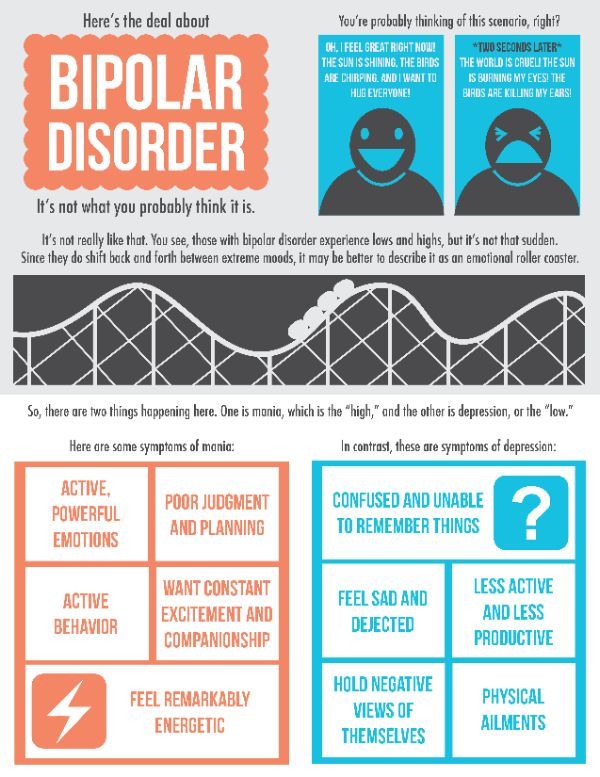 At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
People suffering from depression often feel "stupid", "mentally retarded", "feeble-minded". Thinking in depression becomes viscous, painful, requires special efforts, one mental image is hardly forced out by the next. The sick person is oppressed by the feeling of his own intellectual insolvency, professional collapse. Depressed patients can hardly describe their painful experiences to the doctor. Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Typical story
Aleksey, 18 years old, 1st year student of a technical university, describes his condition during depression as follows:
“From childhood, I was fond of technology and modeling, I could read special literature for hours, won school and regional olympiads in mathematics and physics. After graduating from school, my dream came true - I brilliantly passed the exams to a prestigious university. Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Depression can also be accompanied by real setbacks: for example, a decrease in academic performance, the quality of work, family conflicts, sexual disorders and their consequences for personal relationships. As a rule, the significance of these failures is exaggerated and as a result there is a false sense of the irreparability of what happened, "the collapse of all hopes. "
"
Another generally recognized danger of depression is the possibility of suicidal thoughts, which often lead to suicide attempts. The condition of a person suffering from depression can suddenly deteriorate sharply, which happens either without clear external causes, or under the influence of traumatic situations, unpleasant news. It is during these hours, and sometimes even minutes, that a fatal decision is made. Factors that increase the risk of suicide in depression are past suicide attempts, the severity and duration of the depressive state, the presence of anxiety in its structure, prolonged insomnia, loneliness or alienation in the family, alcohol and drug abuse, loss of work and a sharp change in lifestyle, as well as relatives commit suicide.
Typical story
Eugene E., 35 years old, leading manager of the company.
Almost all my life, my career went “on the ascending”, the goals set were clear, clear and achievable. The marriage was extremely harmonious, two beloved children grew up. He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc." I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car.
He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc." I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared.
However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared.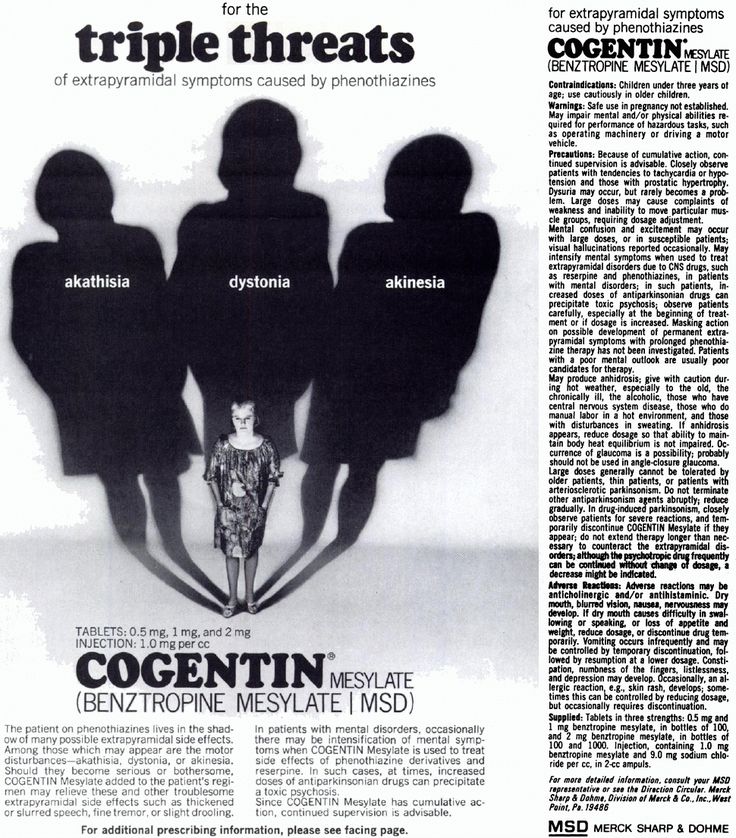 He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
Depression is also characterized by sleep disturbances, occurring in approximately 80% of patients. As a rule, these are early awakenings with the inability to fall asleep, lack of a sense of sleep, difficulty falling asleep. These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
If the depression is not deep, it is sometimes difficult to recognize it. This is due to the fact that people are ashamed to tell others about their problems, to admit to "weaknesses". Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.
Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.
Depressive conditions can occur in shallow forms that are easily treatable, but at least a third of depressions are more severe. Such depressions are characterized by:
- ideas of guilt, sometimes reaching the degree of delirium, i.e. unshakable conviction in their sinfulness, low value (patients consider themselves great sinners, believe that because of them all relatives and Mankind will die, that they are “moral freaks” from birth, supposedly deprived of the foundations of morality and a sense of empathy for other people that they have no place on earth They find in their past numerous "confirmations" of what has been said above, they believe that the doctor and other patients are aware of these transgressions and express contempt and indignation with their facial expressions and gestures, but in the words “they hide, deny the obvious. ” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone.If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone.If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
- mood swings during the day: in typical cases, the patient, waking up, immediately feels longing. Sometimes, even before full awakening, through a dream he experiences a painful premonition of a heavy coming morning. In the evening, the state of health improves somewhat.
- the patient may experience a feeling of unmotivated hostility towards relatives, friends, constant internal discontent and irritation, which makes him unbearable for the family.
- in a number of people suffering from depression, constant doubts, fear for the health and well-being of loved ones, obsessive ones, come to the fore. arising against the will, ideas about the misfortunes and troubles of family members.
arising against the will, ideas about the misfortunes and troubles of family members.
Typical story
Dmitry Petrovich, 58 years old, teacher.
“After minor troubles at work, I began to feel incomprehensible anxiety and agitation. Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered. ”
”
- in many cases, depression is characterized by unpleasant sensations in the body, disturbances in the activity of internal organs in the absence of objective signs of true somatic, i.e. non-mental illness. At the same time, many patients constantly report pain, internal discomfort. Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
- some patients are convinced that they have some rare and difficult to diagnose disease and insist on numerous examinations in general medical institutions. Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
- Patients may experience disturbances in the cardiovascular system, skin itching or lack of appetite. All of these are manifestations of depression.
- the pathological sensations that patients experience during such depressions are quite real, painful, but they are the result of a special mental state, and not an internal disease. It must be remembered that the frequency of latent depressions exceeds the number of explicit ones many times over.
- with such depression, patients, as a rule, also have a changed attitude towards food: they can go without food for a long time and not feel hungry, and sitting down at the table, eat only 1-2 spoons - they have neither strength nor desire for more .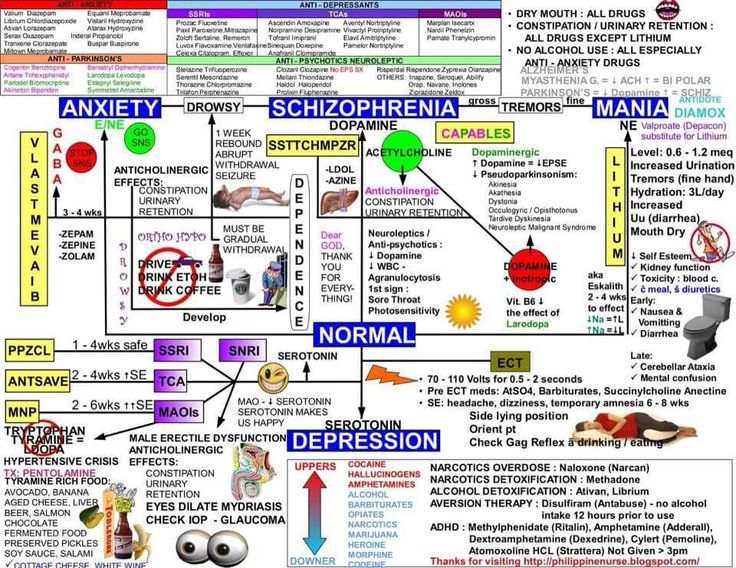
- a sign of depression can serve as a weight loss of more than 5 kg. within a month. In some people, especially women, the appetite for depression, on the contrary, increases, sometimes reaching the level of excruciating hunger, accompanied by severe weakness and pain in the epigastric region. In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
Thus, we see that depression is a disease with many different manifestations that do not go away on their own, requiring special, sometimes long-term, medical intervention. Therefore, when the symptoms described above appear, it is necessary to seek help from a psychiatrist who will prescribe and monitor antidepressant treatment.
TREATMENT OF DEPRESSIVE DISORDERS
To date, it can be argued that the vast majority of cases of depression respond well to treatment. According to modern views, effective treatment of depression consists of a combination of pharmacotherapy, psychotherapy and, if necessary, other types of treatment. At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
The creation of antidepressants is based on the discovery of scientists that depression develops as a result of a violation of the mechanism of biochemical transmission of nerve impulses in the brain regions responsible for mood, behavior, response to stress, sleep and wakefulness, appetite and some other functions. To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Now antidepressants are used in Russia, which can be conditionally divided into 4 generations according to the time of creation.
The first antidepressants to find wide clinical use were tricyclic drugs: amitriptyline and imipramine. They have a fairly powerful effect on most depressive states by blocking the reuptake of both norepinephrine and serotonin. However, the real clinical effect of these drugs is significantly offset by their undesirable side effects, which drastically reduce the quality of life of patients during treatment. Side effects of tricyclic antidepressants arise due to the nonspecificity of their effect on receptor structures. Acting in addition to the serotonin and norepinephrine system and other neurotransmitters (acetylcholine, histamine, dopamine), these antidepressants cause side effects such as urinary retention, dry mucous membranes, constipation, palpitations, fluctuations in blood pressure, confusion, tremor, sexual dysfunction. functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
The situation was somewhat improved by the introduction into practice of drugs of the second generation - tetracyclic antidepressants, which, along with the ability to block the reuptake of norepinephrine and serotonin, could also affect some other receptors. Being analogues of tricyclic compounds, these drugs have antidepressant activity comparable to them, but unlike their predecessors, they are safer, since they cause unwanted side effects much less often. In addition to the antidepressant, mianserin (lerivon) has a clear sedative, anti-anxiety and hypnotic effect. Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
To date, antidepressants of the 3rd generation, such as fluoxetine (Prozac), fluvoxamine (Fevarin), paroxetine (Paxil), sertraline (Zoloft), citalopram (Cipralex) and some other drugs that selectively (selectively) affect the serotonin metabolism system, have received widespread recognition today. , preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
, preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.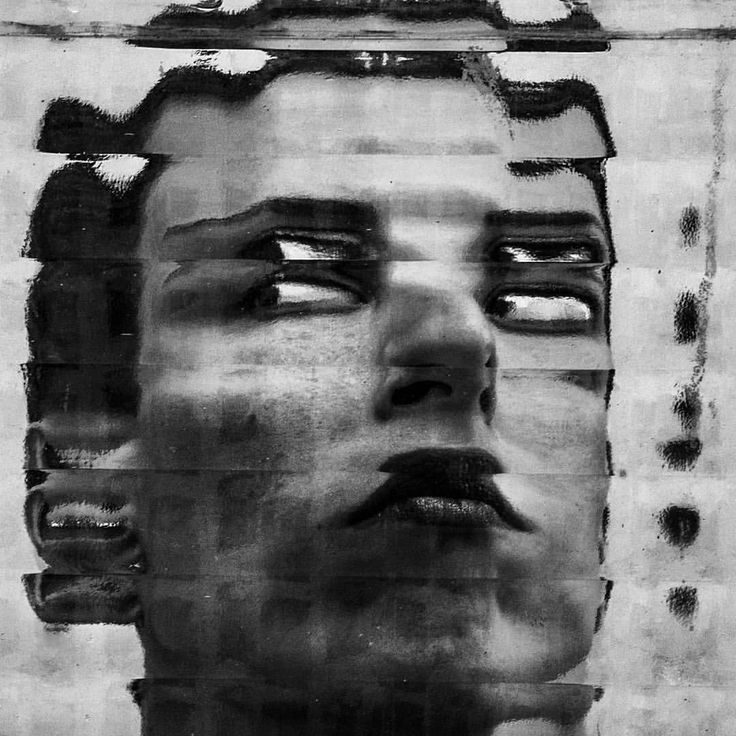
Considering the high frequency of side effects in some of the above drugs and the insufficient antidepressant activity in others, psychopharmacologists have taken the path of developing more effective antidepressants - IV generation drugs that selectively block the reuptake of both serotonin and noradrenaline, without affecting other mediators. system and with minor side effects. Currently, 3 drugs meet these requirements: milnacipran (Ixel), duloxetine (Cymbalta) and venlafaxine (Effexor). Their antidepressant activity in the treatment of patients with severe and moderate depression has been confirmed in a number of specially conducted studies, which at the same time showed that these drugs are well tolerated.
It should be noted that antidepressants of plant origin (negrustin, gelarium hypericum, deprim, etc.) can be effective in mild depressive states, but there are no reliable data guaranteeing their effectiveness. The opinion of a number of doctors that all depression can be treated with herbs or, say, acupuncture, should be recognized as unfounded.
For extremely severe depressions that do not improve despite the use of the most powerful antidepressants, electroconvulsive therapy (ECT) can be effective, but this situation is extremely rare and requires careful justification by the commission of doctors and the consent of the patient.
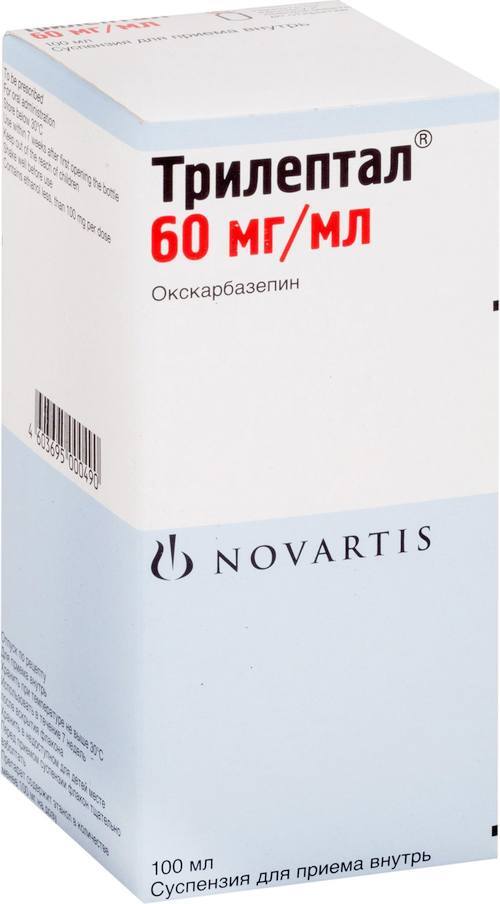
An important additional role in antidepressant therapy, especially with concomitant anxiety, is played by tranquilizers - anti-anxiety drugs, such as Xanax, phenazepam, diazepam, nitrazepam, atarax, etc. Drugs that can, when taken systematically, prevent mood swings in various depressive disorders include so-called mood stabilizers or mood stabilizers - lithium preparations, carbamazepine, valproic acid salts, lamotrigine, topiramate. With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
Antipsychotics play a significant role in the treatment of certain forms of depression. These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
In drug therapy of depressive conditions, an unconventional, strictly individual approach is used, with the obligatory provision of fruitful cooperation between the patient and the doctor. Otherwise, there may be a violation of medical recommendations regarding doses and regimens for taking medications. The patient's faith in the possibility of recovery, the absence of prejudice against the "harm" caused by psychotropic drugs, the systematic observance of the prescriptions prescribed by the doctor largely contribute to the achievement of therapeutic success.
Drug treatment of depression takes time. You should not expect a complete cure already in the first days of taking the drug. It must be remembered that all modern antidepressants begin to act on depressive symptoms no earlier than 1-2 weeks after the start of treatment. Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures. When planning a trip, calculate exactly how many tablets you need for the entire period of absence from home. Breaking therapy is fraught with serious troubles.
Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures. When planning a trip, calculate exactly how many tablets you need for the entire period of absence from home. Breaking therapy is fraught with serious troubles.
Conducted along with drug treatment, psychotherapy of patients with depressive states implies various systems of influence, including individual conversations, family and group therapy, etc. An important element of social rehabilitation is participation in the work of mutual support groups for patients who have experienced depression. This allows other patients to feel help in understanding their problems, to realize that they are not alone in their misfortune, to see the possibilities of personal participation in rehabilitation activities and in social life.
An important element of social rehabilitation is participation in the work of mutual support groups for patients who have experienced depression. This allows other patients to feel help in understanding their problems, to realize that they are not alone in their misfortune, to see the possibilities of personal participation in rehabilitation activities and in social life.
DEPRESSION IS THE MAIN CAUSE OF DISABILITY IN THE WORLD
This diagnosis is often misdiagnosed. Depression is a disease that has many causes and about which we still do not know much.
Sadness, dark thoughts, low self-esteem, loss of interest or inability to enjoy... Depression is not just a blues, but a real illness. It affects all aspects of daily life and is accompanied by an increased risk of suicide. It can lead to the formation of various addictions, as well as heart disease, diabetes or sexual disorders.
Many factors are involved in the development of depression.
Vulnerability factors are at the basis, for example, if a person was a victim of abuse in childhood. The development of depression is usually preceded by the impact of so-called trigger factors. They can be a breakup in a relationship, the death of a loved one, or financial problems.
Apparently, genetic factors also play a certain role, which makes it possible to speak of a hereditary predisposition. Chronic illness, smoking, dependence on alcohol or other psychoactive substances, and even an unbalanced diet can also increase the risk of depression.
322 million
people living with depression in 2017 1
+ 18.4% 2
Less than half of people with depression receive antidepressant medication. 3
A BETTER UNDERSTANDING OF THE CAUSES OF DEPRESSION
DISTURBANCES IN THE OPERATION OF THE SYSTEM OF NEURO-MEDIATORS
In people with depression, the biochemical processes occurring in the brain are disturbed. This disorder can manifest itself as a deficiency or imbalance in the content of one or more types of neurotransmitters - molecules that are released from the terminal part of the neuron (at the synapse) and act as carriers of chemical signals in the brain. Depression disrupts the balance of three neurotransmitters: serotonin, norepinephrine, and dopamine. They are involved in the regulation of mood and behavior, and their function can be restored with the help of antidepressants.
This disorder can manifest itself as a deficiency or imbalance in the content of one or more types of neurotransmitters - molecules that are released from the terminal part of the neuron (at the synapse) and act as carriers of chemical signals in the brain. Depression disrupts the balance of three neurotransmitters: serotonin, norepinephrine, and dopamine. They are involved in the regulation of mood and behavior, and their function can be restored with the help of antidepressants.
SYMPTOMS
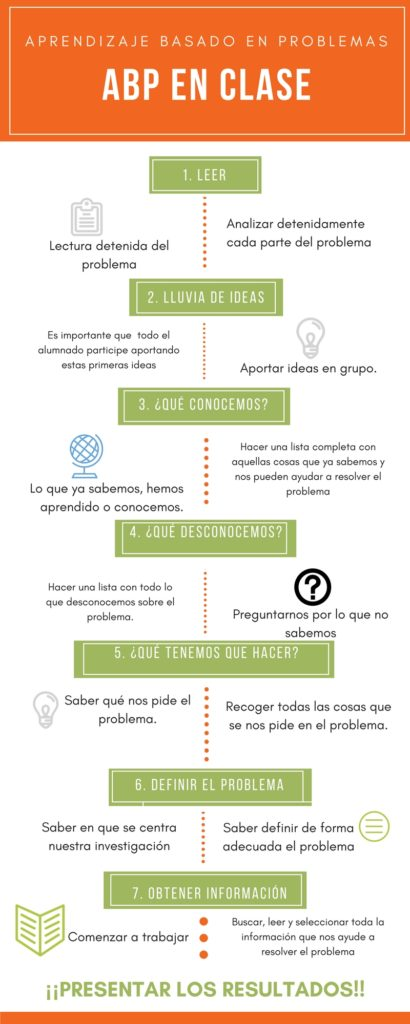
According to guidelines issued by the World Health Organization and republished by the French health authority (Haute Autorité de Santé) in October 2017, “an episode of depression is characterized by the presence of at least two of the following three main symptoms (see infographic) for two consecutive weeks with a certain degree of severity; they must be different from the patient's previous condition and cause significant distress."
Depressive episodes usually resolve after a few weeks or months with treatment or spontaneously. This state is called remission.
This state is called remission.
If subsequent episodes of depression do not recur, recovery is declared, but this rarely happens. In 50–80% of cases, a new episode occurs within the next 5 years. 6 Depression is considered chronic when certain symptoms persist, sometimes less severely, for at least 2 years.
TREATMENTS
Psychotherapy is recommended regardless of the severity of the depression.
Several types of psychotherapy are used, including supportive, cognitive-behavioral, and analytic-based psychotherapies, as well as psychotherapies based on individual, family, and group sessions.
Relatives and friends invariably play a special role in the treatment of the patient. The patient's expression of his suffering and his acceptance of help are of the utmost importance for successful treatment.
In addition to psychotherapy, the use of drugs, in particular antidepressants, is most often useful or even necessary.
Antidepressants are recommended for moderate to severe episodes of depression.
There are several classes of antidepressants. Most of them target nerve cells that release serotonin, norepinephrine, or dopamine. Their action is realized through various mechanisms through which the concentration of neurotransmitters increases or the nerve circuits damaged due to depression are restored.
The physician selects the antidepressant that is most appropriate for the patient, based on their symptoms, medical history, past or current conditions and treatment. The effectiveness of antidepressants usually becomes noticeable only after a few weeks.
TWO PHASES OF TREATMENT (THREE IN THE EVENT OF RECURRENCE):
- The acute phase (6 to 12 weeks) is needed to overcome the current episode of depression.
- The consolidation phase (4 to 6 months) aims to reduce the risk of disease recurrence in the short term.
- Maintenance phase: After three episodes of depression, treatment may be given for several years to prevent relapse.
In most cases, treatment is carried out on an outpatient basis (at the patient's home) under the regular supervision of a healthcare professional. However, sometimes a patient may require emergency care or an episode of depression may be resistant to traditional medications. In this case, hospitalization may be considered.
THE ROLE OF SERVIER
For over 30 years, Servier has provided medical solutions to people who suffer from depression. Recently, the attention of our group has been focused, in particular, on the development of a digital cognitive-behavioral approach.
It combines a cognitive approach, which focuses on correcting the thoughts that keep the patient in a state of emotional decline, and a behavioral approach, which focuses on correcting unacceptable behavior. The goal of therapy is for patients to adopt a new way of thinking and develop optimal behavior.
RECURRENCE PREVENTION MEASURES
- Incorporate regular, moderate-intensity physical activity into your daily routine
Exercise (walking, running, swimming, cycling) at the recommended frequency of 30-40 minutes 5 times a week.
- Eat a balanced diet
A diet rich in fresh fruits and vegetables, fish and seafood, vegetable oils and whole grains. This type of food is high in essential fatty acids, vitamin B12, selenium, zinc, and iron, a lack of which increases the risk of depression. - Discuss your psychological problems without delay
Talking to family, friends or a doctor can help prevent a relapse of depression. In addition, there are communities that provide the necessary assistance to those in need
(1) (2) (3) WHO Report: Depression and other common mental disorders 2017 https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/
(4) http://www.info-depression.fr/spip.php?rubrique16
(5) Léon C, Chan Chee C, du Roscoät E, the Baromètre santé 2017 survey group. La depression en France chez les 18-75 ans: résultats du Baromètre santé 2017. Bulletin épidémiologique hebdomadaire.