Ocd intrusive thoughts help
How to Take the Power Back from Intrusive Thought OCD
03.22.2017
Debra Kissen, PhD, MHSA
Member Since 2010
Dr. Debra Kissen is CEO of Light On Anxiety CBT Treatment Center. Dr. Kissen specializes in Cognitive Behavioral Therapy (CBT) for anxiety and related disorders. Dr. Kissen is the author of the Panic Workbook for Teens, Rewire Your Anxious Brains for Teens: Using CBT, Neuroscience, and Mindfulness to Help You End Anxiety, Panic, and Worry (The Instant Help Solutions Series) and the soon to be released Break Free from Intrusive Thoughts: An Evidence-Based Guide for Managing Fear and Finding Peace. Dr. Kissen also has a special interest in the principles of mindfulness and their application for anxiety disorders. Dr. Kissen has presented her research on CBT and mindfulness-based treatments for anxiety and related disorders at regional and national conferences. Dr. Kissen is the Co-Chair of the Anxiety and Depression Association of America Public Education Committee.
Dr. Kissen was the recipient of the 2020 Gratitude for Giving Spirit Award and the 2018 Anxiety Depression Association of America Member of Distinction Award.
Dr. Kissen often serves as a media psychologist and is available for press inquiries and strives to further the dissemination of empirically supported treatment (EST) information by offering user friendly quotes and simple to understand, practical tips and solutions to help mental health consumers move past stress and anxiety.
Dr. Kissen and ADAA
"I was lucky enough to do my early practicums under the leadership and guidance of Dr. Karen Cassiday who is now president of ADAA. I learned from Dr. Cassiday that time spent with ADAA is one of the best professional investments that I could make. Through continuing education, professional connections and additional contact with mental health consumers, ADAA is truly my professional home. I have always had a passion for enhancing dissemination of empirically supported treatment protocols to mental health consumers.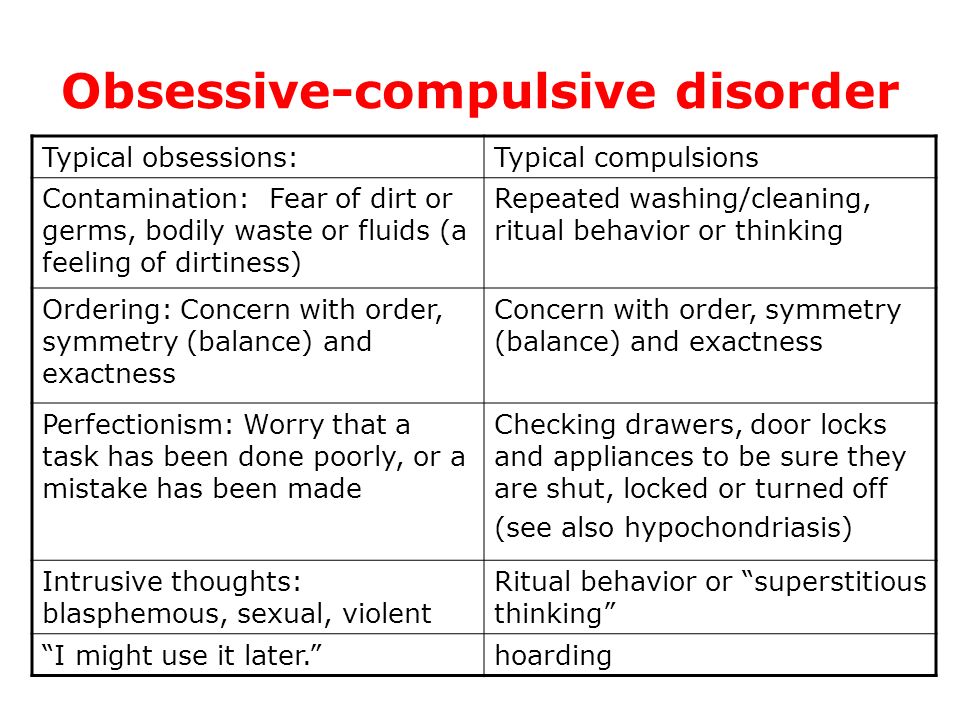 The public education committee offers a wonderful opportunity to create innovative programming to reach mental health consumers where they are, not just in the treatment room. I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
The public education committee offers a wonderful opportunity to create innovative programming to reach mental health consumers where they are, not just in the treatment room. I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
Light on Anxiety CBT Treatment Center
Boost Search Results
On
March 22, 2017
How to Take the Power Back from Intrusive Thought OCD
Step 1: See Through OCD’s Scare Tactics
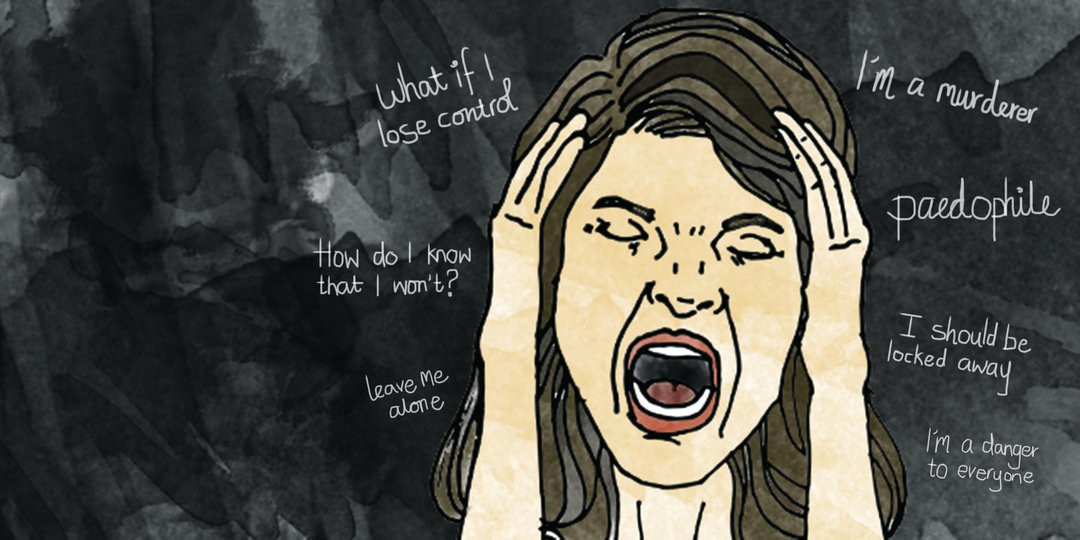
OCD is the fear network of the brain sending a signal that something is wrong and needs to be done about it IMMEDIATELY. OCD only reports on feared consequences that are important to a person. For example, if somebody does not fear spilling water on the floor, OCD will not send the intrusive thought, “Oh no you spilled water. You must clean it up IMMEDIATELY”. On the other hand if someone does care about the safety of her family, OCD might say, “Oh no you left the stove on. You must go back and check IMMEDIATELY or the most important people in your life will die and it will be all your fault.” Similarly, if you care deeply about your family's well-being or your students safety, OCD may inject itself into your awareness with the thought “Oh no. What if I lose control and harm my children or students.”
You must go back and check IMMEDIATELY or the most important people in your life will die and it will be all your fault.” Similarly, if you care deeply about your family's well-being or your students safety, OCD may inject itself into your awareness with the thought “Oh no. What if I lose control and harm my children or students.”
My clients always ask me what it means about them that they could have such “horrible thoughts”. What I tell them is that somewhere within an obsession is the flip side of a core value. If OCD taunts you with images and thoughts about offending god, then religion must be important to you. If OCD reviews all the ways your family could be hurt, then your family is clearly one of your top priorities.
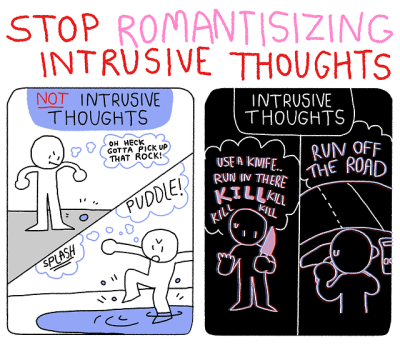
There is checklist of common intrusive thoughts that I find helpful to share with my patients. There are numerous thoughts on this list regarding losing control and acting out violently or sexually. Several research studies found that when this list is shown to a non-clinical sample of people, approximately 90 percent of those surveyed will agree to having experienced some of the intrusive thoughts.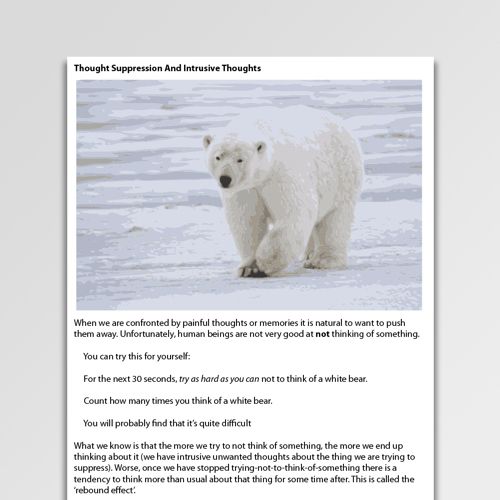
When the non-clinical sample is asked how bothered they are by experiencing these intrusive thoughts, they are most often only mildly bothered by them. In contrast, when this same list is shown to individuals diagnosed with OCD, a similar percentage of the sample will agree to having experienced these intrusive thoughts but the big difference is how much distress these thoughts evoke for the OCD sample. For those meeting criteria for OCD, there will be a much higher level of emotional distress when these same intrusive thoughts surface.
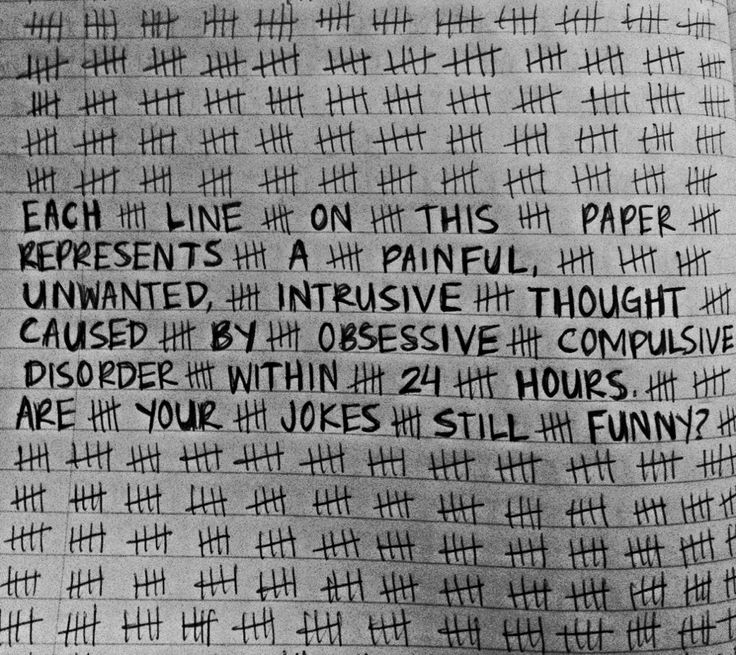
What keeps OCD alive and well is not the experience of intrusive thoughts but actually one’s reaction to them. The more one dislikes experiencing intrusive thoughts and then tries to repress or fight with these thoughts, the greater the frequency of intrusive thoughts one will experience. The very act of trying to “not have” a bothersome thought guarantees its resurfacing. The only way to know if you are having or not having a thought is to think “Am I think about X” or “I better not think about X” which of course causes one to think about X.
So back to the question of why do those meeting criteria for OCD have such disturbing thoughts? Because they are human and to be human means one will experience freaky, odd thoughts. The human mind is constantly spinning around trying to find interesting problems to solve, in order to keep us alive. We don’t have the speed of the jaguar or the strength of a bear but we do have an all too powerful mind that is very good at planning for future challenges but also for tying itself into a knot. Freedom from OCD is not about stopping the mind from offering up strange and occasionally disturbing thoughts but learning how to recognize spam vs. urgent mail.
I must give a disclaimer here that OCD loves taking anything that is reassuring and turning it into a compulsion. So, if you are reading this blog for the hundredth time and desperately trying to figure out if this sounds like you and if your “awful thoughts” are OCD or if in fact you are an awful person, then STOP reading this blog. As I am sure your experience has shown you obtaining short-term anxiety relief through a compulsion comes at a cost in the form of greater overall anxiety. Instead, strive for long-term freedom from OCD by teaching your mind to not take itself so seriously.
As I am sure your experience has shown you obtaining short-term anxiety relief through a compulsion comes at a cost in the form of greater overall anxiety. Instead, strive for long-term freedom from OCD by teaching your mind to not take itself so seriously.
Step 2: Exposure and Response Prevention (ERP)
There is no way past OCD except through it. As described in step one, the more one avoids an intrusive thought, the more one will experience the feared, bothersome, super annoying thought. Therefore, we need to flip the equation on its head and practice bringing on the thought while disengaging from any compulsions that have been utilized to obtain short-term anxiety relief. Common compulsions engaged in, when struggling with intrusive thought OCD are reassurance seeking, information seeking/googling to determine if there is something wrong with self, mental reviewing and avoidance. The best way to organize exposure tasks is by creating an exposure hierarchy that outlines baby steps that you can take to slowly but surely prove to OCD who is in charge (hint…YOU).
Step 3: Get Support
“Support” may sound superfluous but without it your Intrusive Thought OCD fighting plan will most likely be a bust. It is near impossible to do this work alone. It is not that you are not smart enough or determined enough or brave enough to beat OCD. The reason you need external support is because there is nothing more powerful in taking the wind out of OCD’s sails than voicing intrusive thoughts out loud, to a compassionate, informed coach. The same intrusive thoughts that feel so real, all powerful and self-defining when swirling around in your head will disintegrate when said out loud. When your intrusive thoughts are released into the world and your supportive coach looks back at you, and still sees the YOU they believe in and hears your intrusive thought as “blah blah blah” and possibly laughable, your brain will be one step closer to understanding that these thoughts are spam mail and nothing more.
In terms of finding a supportive OCD coach, you can contact a therapist that is well trained in CBT for OCD but if this is price prohibitive or if there is not access in your local community to OCD experts, there are other options. You can purchase a CBT for OCD workbook and go chapter by chapter through it with any licensed therapist in your community. You can schedule an appointment with one of ADAA’s OCD specialists who offer tele-mental health services. And it is perfectly acceptable to purchase a CBT for OCD workbook and go through the material together with a friend or family member.
You can purchase a CBT for OCD workbook and go chapter by chapter through it with any licensed therapist in your community. You can schedule an appointment with one of ADAA’s OCD specialists who offer tele-mental health services. And it is perfectly acceptable to purchase a CBT for OCD workbook and go through the material together with a friend or family member.
So you now know the three basic steps necessary to kick intrusive thought OCD to the curb. And remember, we are all so much more than our thoughts. Our lives are defined by the actions that we choose to take, not by the electrical storm of thoughts that flicker through our minds.
Dr. Kissen and Dr. Ashley D. Kendall, PhD presented a live webinar on this topic on March 12, 2018 at 1:00 pm ET.
This webinar shares tips and tools to:
- Identify if you may be dealing with harm OCD
- Make sense of why harm OCD picks such painful themes and content
- Take the power away from harm OCD
- Re-engage in your life now that you are giving less of your attention and energy to harm OCD
Watch here.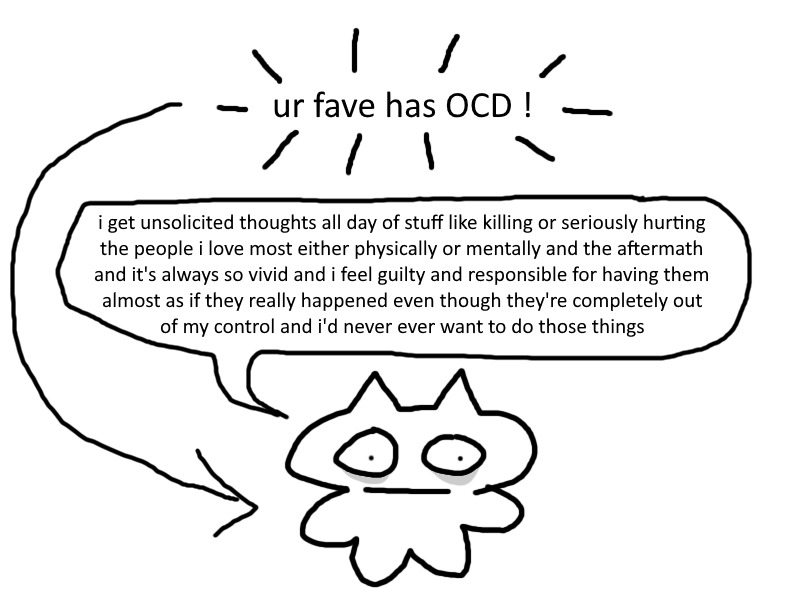
Debra Kissen, PhD, MHSA
Member Since 2010
Dr. Debra Kissen is CEO of Light On Anxiety CBT Treatment Center. Dr. Kissen specializes in Cognitive Behavioral Therapy (CBT) for anxiety and related disorders. Dr. Kissen is the author of the Panic Workbook for Teens, Rewire Your Anxious Brains for Teens: Using CBT, Neuroscience, and Mindfulness to Help You End Anxiety, Panic, and Worry (The Instant Help Solutions Series) and the soon to be released Break Free from Intrusive Thoughts: An Evidence-Based Guide for Managing Fear and Finding Peace. Dr. Kissen also has a special interest in the principles of mindfulness and their application for anxiety disorders. Dr. Kissen has presented her research on CBT and mindfulness-based treatments for anxiety and related disorders at regional and national conferences. Dr. Kissen is the Co-Chair of the Anxiety and Depression Association of America Public Education Committee. Dr. Kissen was the recipient of the 2020 Gratitude for Giving Spirit Award and the 2018 Anxiety Depression Association of America Member of Distinction Award.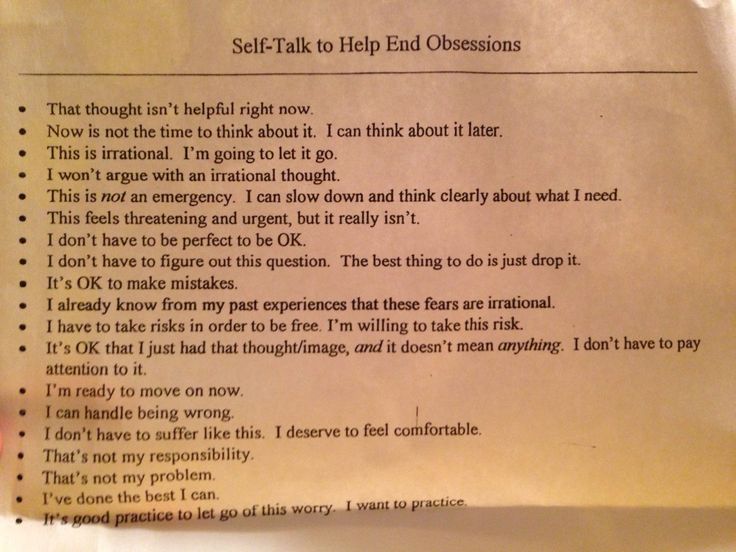
Dr. Kissen often serves as a media psychologist and is available for press inquiries and strives to further the dissemination of empirically supported treatment (EST) information by offering user friendly quotes and simple to understand, practical tips and solutions to help mental health consumers move past stress and anxiety.
Dr. Kissen and ADAA
"I was lucky enough to do my early practicums under the leadership and guidance of Dr. Karen Cassiday who is now president of ADAA. I learned from Dr. Cassiday that time spent with ADAA is one of the best professional investments that I could make. Through continuing education, professional connections and additional contact with mental health consumers, ADAA is truly my professional home. I have always had a passion for enhancing dissemination of empirically supported treatment protocols to mental health consumers. The public education committee offers a wonderful opportunity to create innovative programming to reach mental health consumers where they are, not just in the treatment room.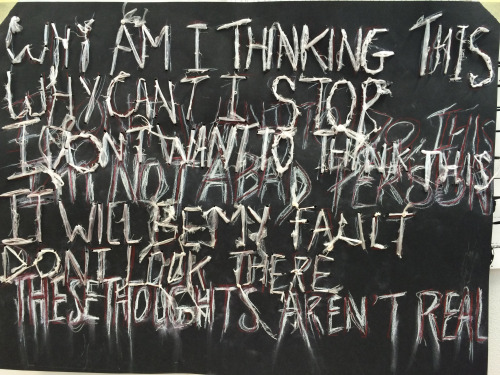 I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
Light on Anxiety CBT Treatment Center
Obsessive-Compulsive Disorder (OCD)
ADAA Blog Content and Blog Comments Policy
ADAA Blog Content and Blog Comments Policy
ADAA provides this Website blogs for the benefit of its members and the public. The content, view and opinions published in Blogs written by our personnel or contributors – or from links or posts on the Website from other sources - belong solely to their respective authors and do not necessarily reflect the views of ADAA, its members, management or employees. Any comments or opinions expressed are those of their respective contributors only. Please remember that the open and real-time nature of the comments posted to these venues makes it is impossible for ADAA to confirm the validity of any content posted, and though we reserve the right to review and edit or delete any such comment, we do not guarantee that we will monitor or review it.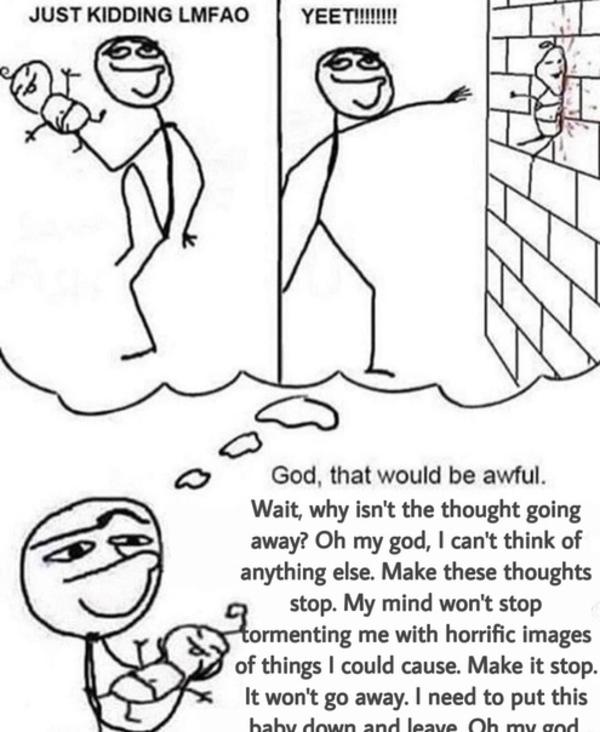 As such, we are not responsible for any messages posted or the consequences of following any advice offered within such posts. If you find any posts in these posts/comments to be offensive, inaccurate or objectionable, please contact us via email at [email protected] and reference the relevant content. If we determine that removal of a post or posts is necessary, we will make reasonable efforts to do so in a timely manner.
As such, we are not responsible for any messages posted or the consequences of following any advice offered within such posts. If you find any posts in these posts/comments to be offensive, inaccurate or objectionable, please contact us via email at [email protected] and reference the relevant content. If we determine that removal of a post or posts is necessary, we will make reasonable efforts to do so in a timely manner.
ADAA expressly disclaims responsibility for and liabilities resulting from, any information or communications from and between users of ADAA’s blog post commenting features. Users acknowledge and agree that they may be individually liable for anything they communicate using ADAA’s blogs, including but not limited to defamatory, discriminatory, false or unauthorized information. Users are cautioned that they are responsible for complying with the requirements of applicable copyright and trademark laws and regulations. By submitting a response, comment or content, you agree that such submission is non-confidential for all purposes. Any submission to this Website will be deemed and remain the property of ADAA.
Any submission to this Website will be deemed and remain the property of ADAA.
The ADAA blogs are forums for individuals to share their opinions, experiences and thoughts related to mental illness. ADAA wants to ensure the integrity of this service and therefore, use of this service is limited to participants who agree to adhere to the following guidelines:
1. Refrain from transmitting any message, information, data, or text that is unlawful, threatening, abusive, harassing, defamatory, vulgar, obscene, that may be invasive of another 's privacy, hateful, or bashing communications - especially those aimed at gender, race, color, sexual orientation, national origin, religious views or disability.
Please note that there is a review process whereby all comments posted to blog posts and webinars are reviewed by ADAA staff to determine appropriateness before comments are posted. ADAA reserves the right to remove or edit a post containing offensive material as defined by ADAA.
ADAA reserves the right to remove or edit posts that contain explicit, obscene, offensive, or vulgar language. Similarly, posts that contain any graphic files will be removed immediately upon notice.
2. Refrain from posting or transmitting any unsolicited, promotional materials, "junk mail," "spam," "chain mail," "pyramid schemes" or any other form of solicitation. ADAA reserves the right to delete these posts immediately upon notice.
3. ADAA invites and encourages a healthy exchange of opinions. If you disagree with a participant 's post or opinion and wish to challenge it, do so with respect. The real objective of the ADAA blog post commenting function is to promote discussion and understanding, not to convince others that your opinion is "right." Name calling, insults, and personal attacks are not appropriate and will not be tolerated. ADAA will remove these posts immediately upon notice.
4. ADAA promotes privacy and encourages participants to keep personal information such as address and telephone number from being posted.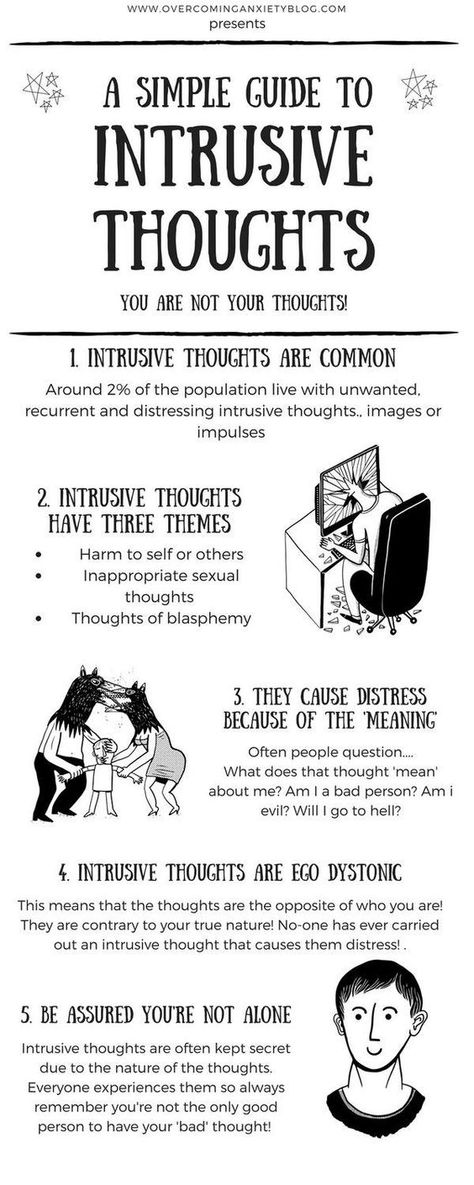 Similarly, do not ask for personal information from other participants. Any comments that ask for telephone, address, e-mail, surveys and research studies will not be approved for posting.
Similarly, do not ask for personal information from other participants. Any comments that ask for telephone, address, e-mail, surveys and research studies will not be approved for posting.
5. Participants should be aware that the opinions, beliefs and statements on blog posts do not necessarily represent the opinions and beliefs of ADAA. Participants also agree that ADAA is not to be held liable for any loss or injury caused, in whole or in part, by sponsorship of blog post commenting. Participants also agree that ADAA reserves the right to report any suspicions of harm to self or others as evidenced by participant posts.
RESOURCES AND NEWS
Evidence-based Tips & Strategies from our Member Experts
RELATED ARTICLES
Block reference
TAKING ACTION
BabyGirl's Enduring Impact: Helping Those with Anxiety and Depression
BabyGirl was a miniature (puddin) Jack Russell who was 8 years old and only 6 pounds. She was…
Read More
Load More
Managing intrusive thoughts - Harvard Health
Disturbing thoughts that pop into your mind unbidden may make you feel uneasy, but they are common — and there are strategies you can use to manage them.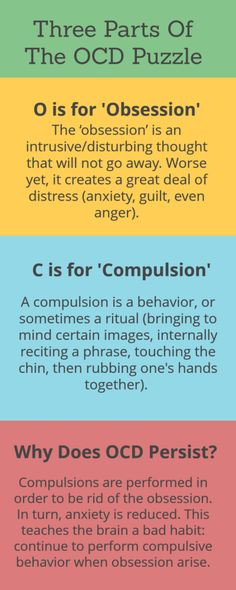
It seems to come out of nowhere — a strange, disturbing thought or a troubling image that pops into your mind. It might be violent or sexual, or a recurring fear that you’ll do something inappropriate or embarrassing. Whatever the content, it’s often unsettling and may bring on feelings of worry or shame. The more you try to push the thought from your mind, the more it persists.
Intrusive thoughts, as these are called, are thought to affect some six million Americans, according to the Anxiety and Depression Association of America.
Sometimes intrusive thoughts are associated with a mental health disorder, such as obsessive-compulsive disorder, where thoughts become so bothersome that they prompt repetitive behaviors or compulsions to try to prevent them from occurring. They are also common in post-traumatic stress disorder, which can be triggered by a life-threatening or extremely stressful event, such as an accident or violent attack. But many people who experience these thoughts don’t have a mental health disorder, says Dr. Kerry-Ann Williams, a lecturer in psychiatry at Harvard Medical School.
Kerry-Ann Williams, a lecturer in psychiatry at Harvard Medical School.
Intrusive thoughts are often triggered by stress or anxiety. They may also be a short-term problem brought on by biological factors, such as hormone shifts. For example, a woman might experience an uptick in intrusive thoughts after the birth of a child.
"Any life stressor, if big enough, can increase your risk of having intrusive thoughts," says Dr. Williams.
Periods of stress and isolation
These days many women have experienced significant stress from the isolation caused by the pandemic, says Dr. Olivera Bogunovic, an assistant professor of psychiatry at Harvard Medical School. Anxiety symptoms may also commonly occur as women transition to a different stage of their life. They may become more isolated, or develop a fear of aging or of developing physical ailments, she says. This can lead to an uptick in anxiety, and in some instances, obsessive thinking.
While intrusive thoughts may be disturbing, they aren’t harmful or a sign that you have a secret desire to do the things that popped into your mind.
People are often too embarrassed or ashamed to talk about it, says Dr. Williams. "A lot of times when patients bring it up to me, they might preface it with something like, ‘I’m not crazy, but this weird thought comes into my mind,’" she says. "They might think about hurting a family member, such as a baby. When the thought happens, they’re horrified—‘I can’t even believe that came into my mind. I shouldn’t tell anyone; they might think something is wrong with me.’"
Identifying intrusive thoughts
So, how can you tell if you are experiencing intrusive thoughts? There are some signs to look for.
The thought is unusual for you. An intrusive thought is usually very different from your typical thoughts. "For example, it might be uncharacteristically violent," says Dr. Williams.
The thought is bothersome. If a thought is disturbing and it’s something you want to push out of your mind, it might be an intrusive thought.
The thought feels hard to control.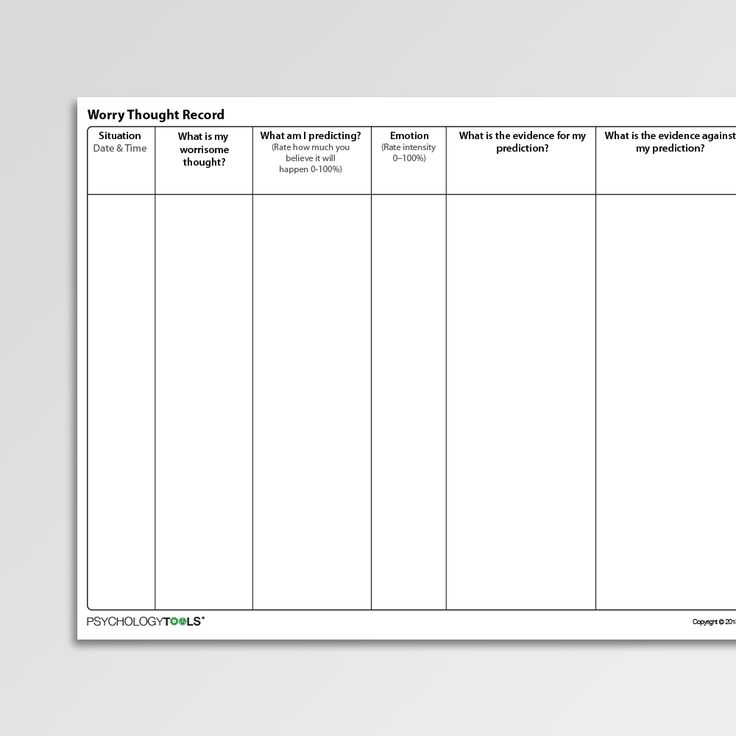 Intrusive thoughts are often repetitive and won’t go away.
Intrusive thoughts are often repetitive and won’t go away.
"The more you think about it, the more anxious you get and the worse the thoughts get," says Dr. Williams. Instead of fighting intrusive thoughts, it’s better to learn to live with them. When these thoughts emerge, try taking the following steps:
1. Identify the thought as intrusive. "Think to yourself, ‘that’s just an intrusive thought; it’s not how I think, it’s not what I believe, and it’s not what I want to do,’" says Dr. Williams.
2. Don’t fight with it. When you have an intrusive thought, just accept it. "Don’t try to make it go away."
3. Don’t judge yourself. Know that having a strange or disturbing thought doesn’t indicate that something is wrong with you.
When to seek help
See a mental health professional if unwanted thoughts are starting to disrupt your daily life, particularly if they’re impairing your ability to work or to do things you enjoy.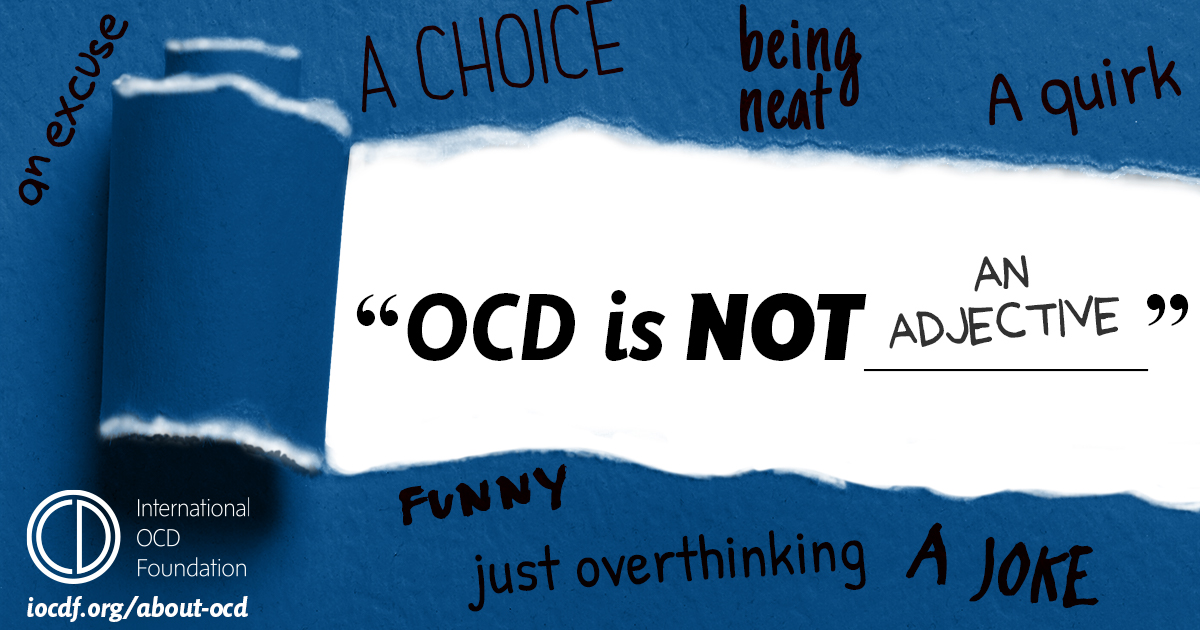 However, even if intrusive thoughts aren’t affecting your life in a significant way, you can still see someone to get help.
However, even if intrusive thoughts aren’t affecting your life in a significant way, you can still see someone to get help.
Cognitive behavioral therapy is one strategy that is often successful in helping people manage intrusive thoughts. The process may help you to shift some of your general thought patterns, which can enable you to better manage these thoughts when they do occur and might lessen their frequency.
Intrusive thoughts can also be managed by addressing the underlying problem, such as anxiety, stress, or a personal history of trauma. While it may be helpful to share the particular thoughts you are having, keep in mind that even if you aren’t comfortable talking about them in detail, a therapist can still help. Women should also know that intrusive thoughts typically respond well to therapy, says Dr. Bogunovic.
"Keep in mind that you might not need help forever," says Dr. Williams. "It may be a very short-term thing."
Image: © Aleutie/Getty Images
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.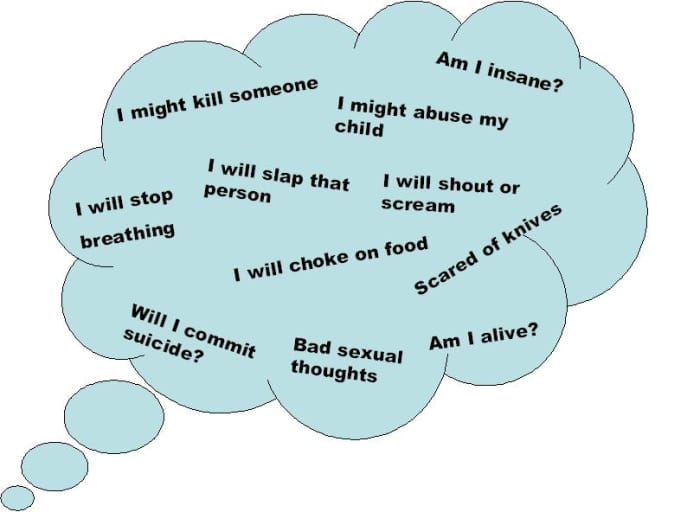
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
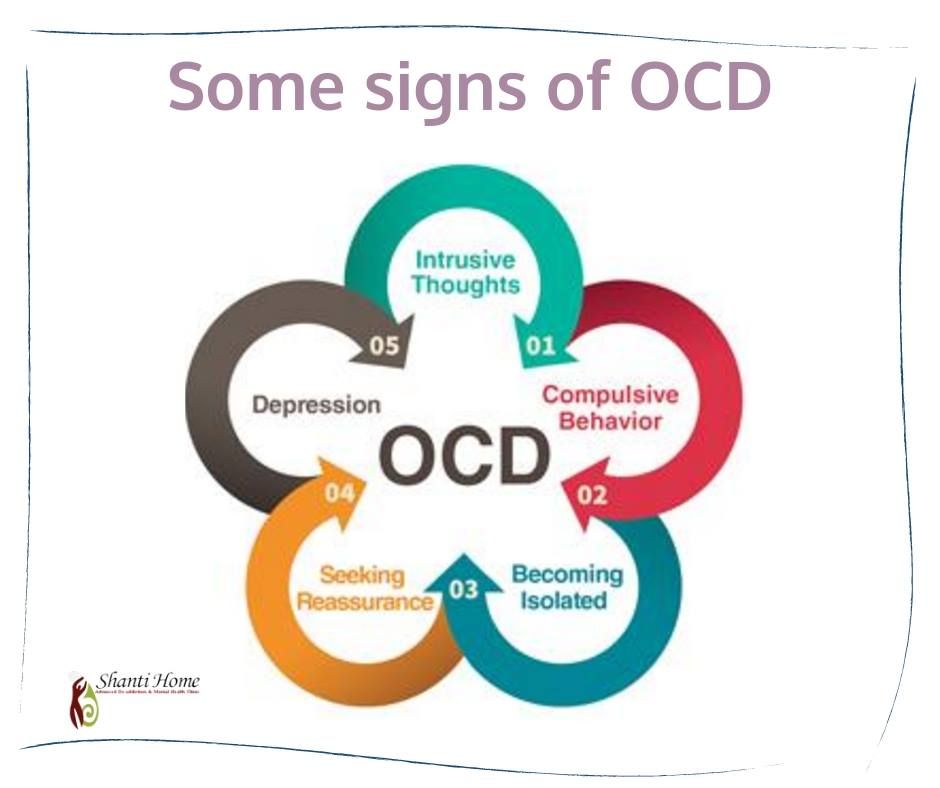
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts.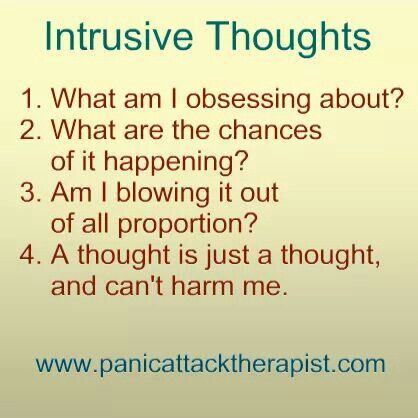 Compulsions are difficult to resist: the anxiety will grow until the person gives up.
Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life.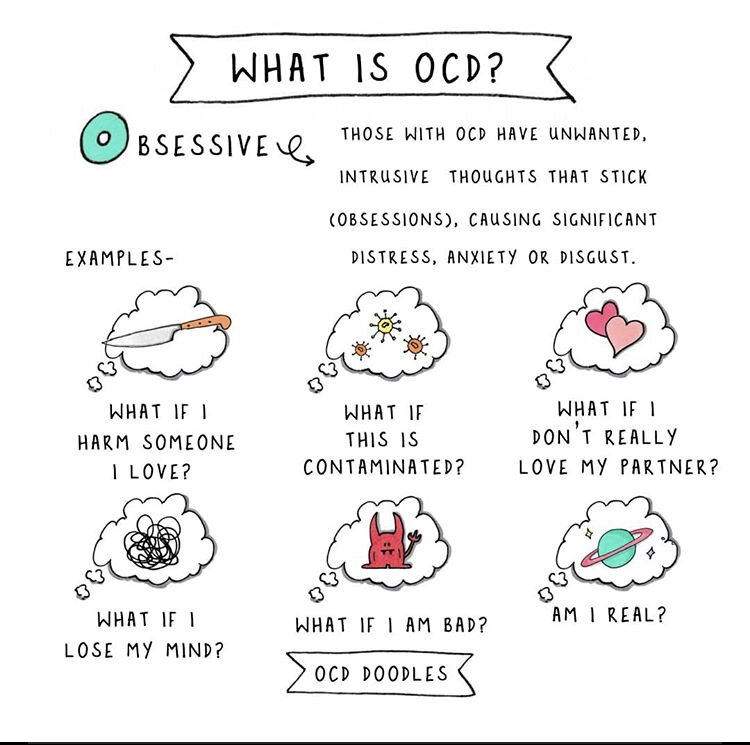 If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasurable. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
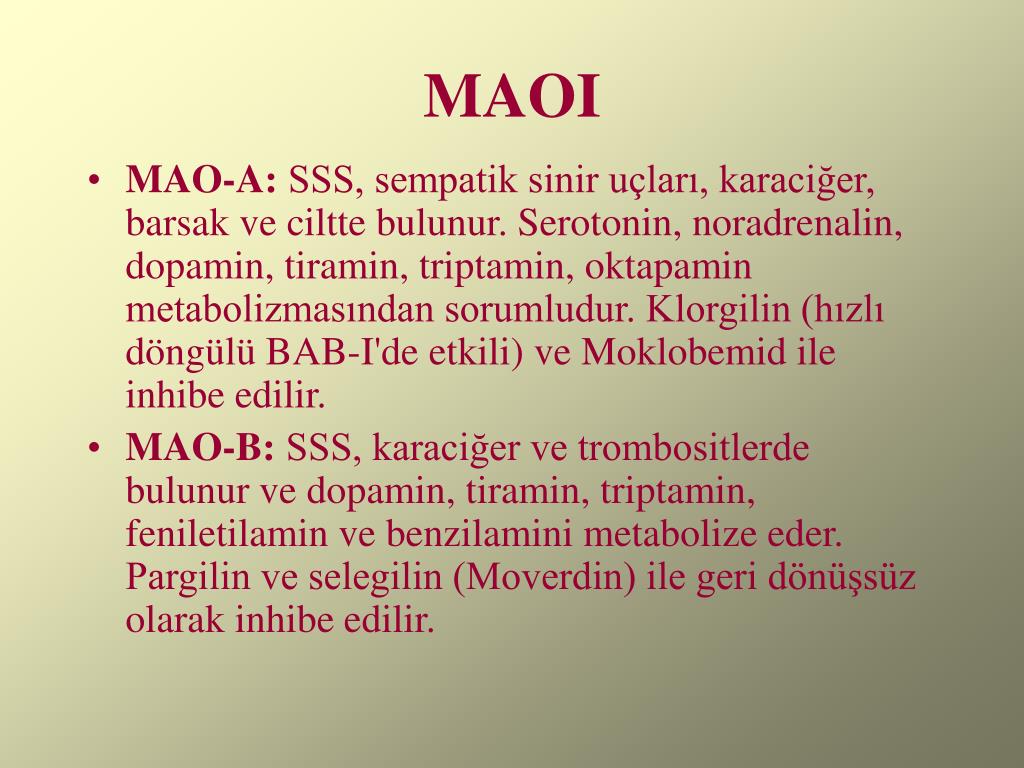
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group.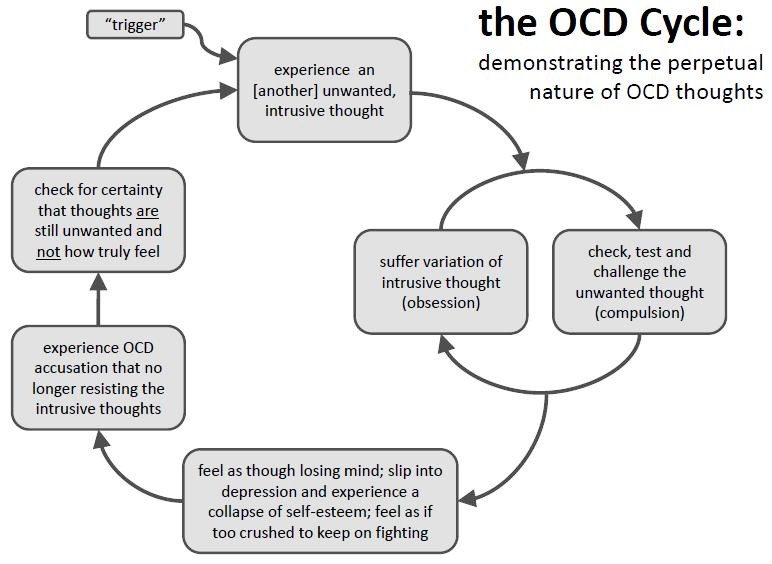 They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn.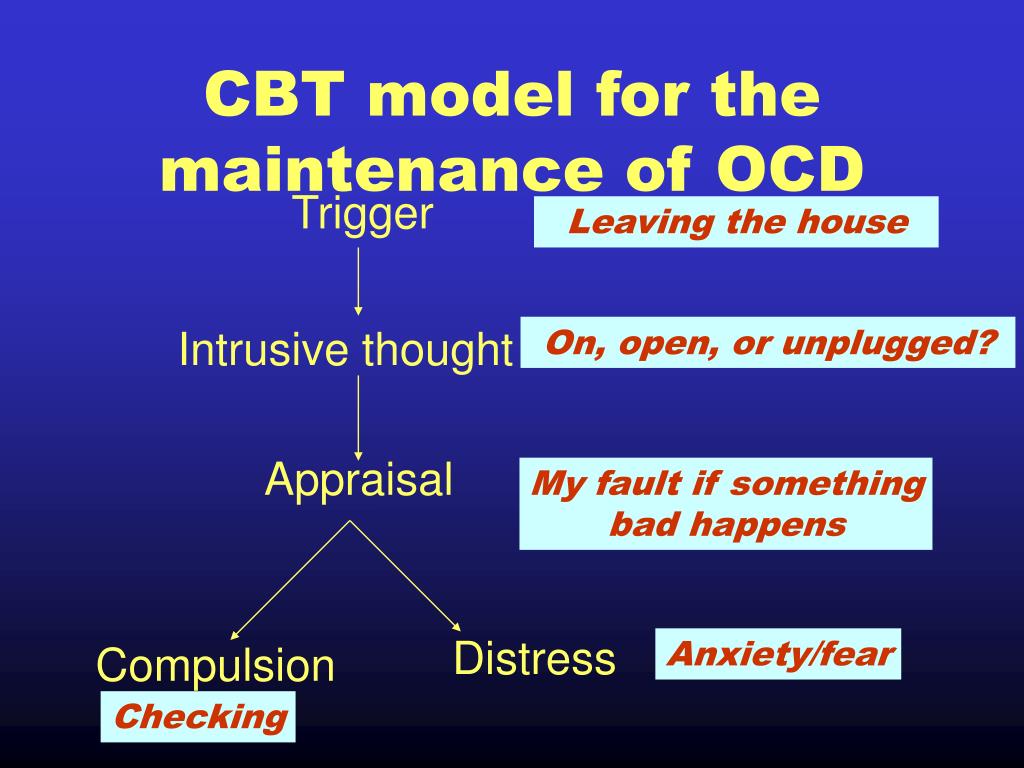 I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalization My condition worsened, I tried to ignore obsessive thoughts.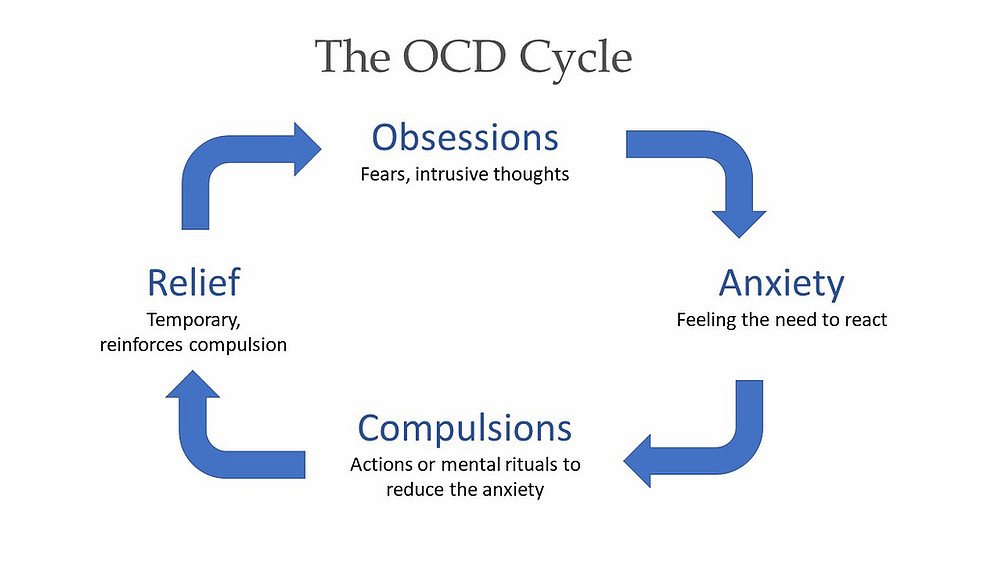 But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
But there was no strength to argue with the psychiatrist.
The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them.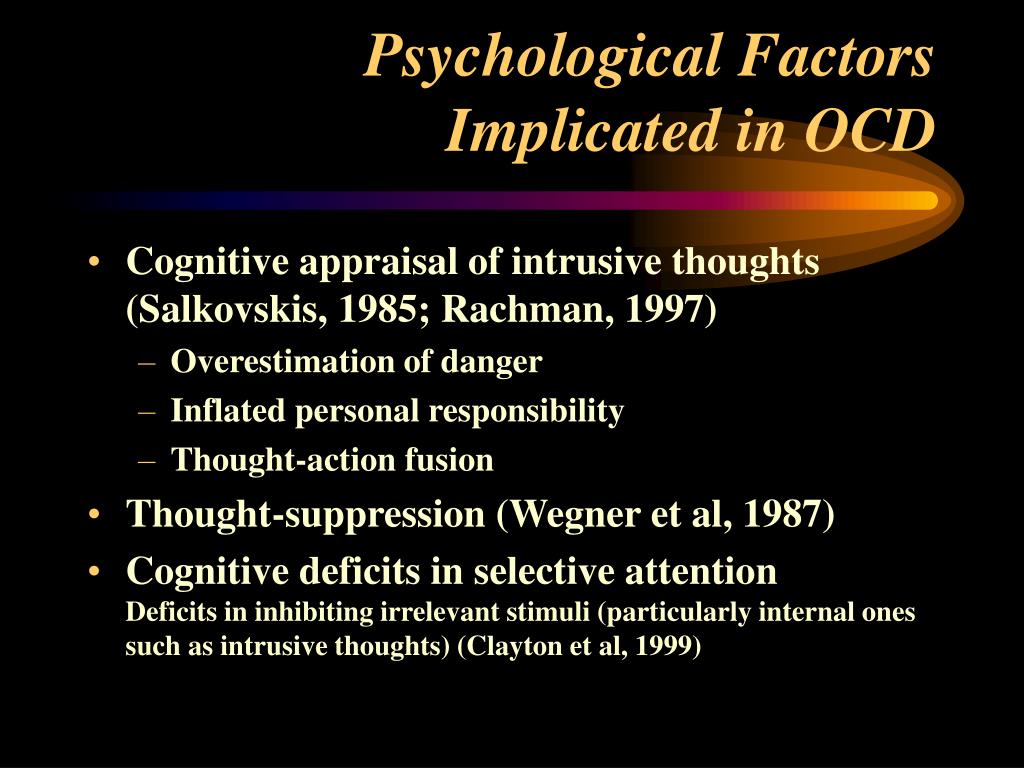 Usually the registrar complied with my request.
Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant.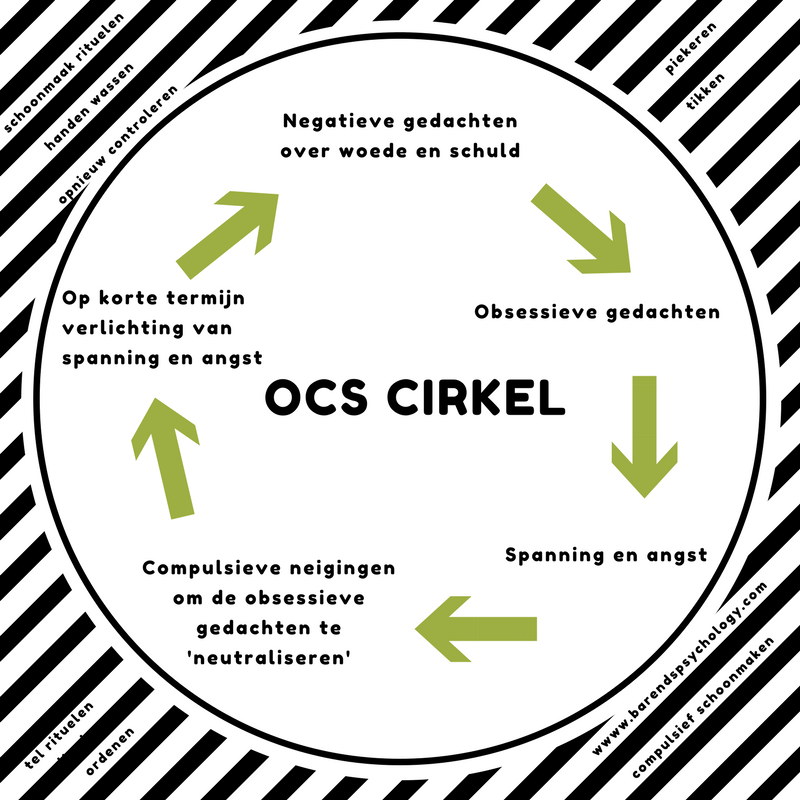 When I wanted to buy one more to have a supply, the pharmacist refused
When I wanted to buy one more to have a supply, the pharmacist refused Treatment
Second hospitalization and psychotherapyAfter six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions.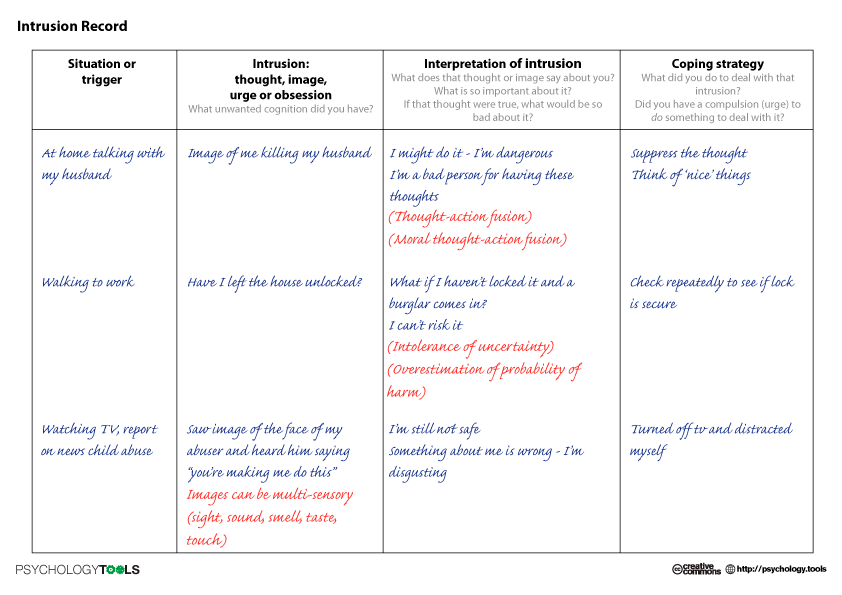 Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.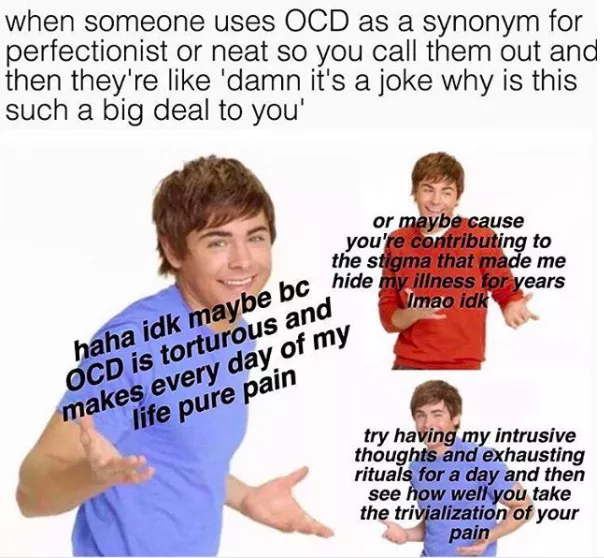
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
- A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job.
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Share
Obsessive Compulsive Disorder (OCD): what it is, symptoms, treatment, doctor's advice
Updated August 08, 2022, 15:45
Shutterstock
Both men and women are affected by OCD, regardless of age. Some people develop symptoms during adolescence, although they are usually diagnosed in adults.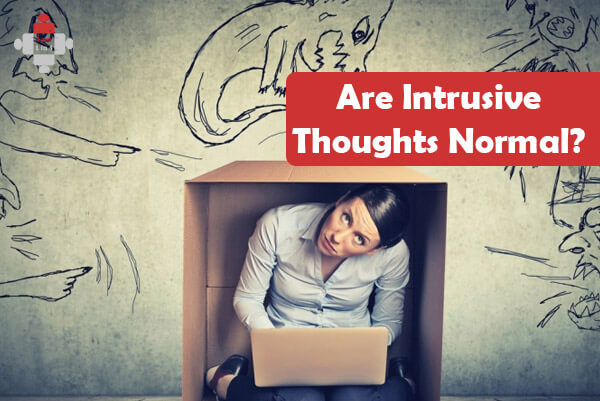 Obsessive-compulsive disorder can significantly interfere with a fulfilling life, but treatment can help keep it under control.
Obsessive-compulsive disorder can significantly interfere with a fulfilling life, but treatment can help keep it under control.
Let's figure out together with experts what are the causes of OCD, what therapeutic and drug methods are used by doctors, and how to behave relatives of a person who has been diagnosed with this disorder.
Contents
- What it is
- Signs and symptoms
- Causes
- Diagnosis
- How to treat
- Advice for relatives 9004 Forums and support groups
- obsessions - persistent thoughts or impulses, intrusive and unacceptable, causing anxiety;
- compulsions are rituals that are built into the thoughts of a person, he considers it necessary to perform them in response to an obsession.
- present daily;
- are uncontrollable;
- are not enjoyable;
- affect work and social life.
- Checks if the door is locked, if the iron and oven are switched off.
- Unreasonably suspects undiagnosed health conditions such as pregnancy or schizophrenia.
- Afraid of germs, things that can be dirty, constantly cleaning.
- Strives for excessive symmetry and order, feels the need to arrange things in a certain way: by size, colors or alphabet.
- Cannot drive obsessive thoughts and ideas away from himself. Some of them can be violent or disturbing.
- Genetics. If you have OCD in your next of kin—father, mother, brother, and sister—the chances are high that you have it too.
- The structure and functioning of the brain. In the brain of OCD sufferers, increased activity is recorded in the region of the cortico-striatal-thalamo-cortical loop [5].
- Environment. High levels of stress, increased anxiety can also be a trigger for the development of obsessive-compulsive disorder.
- Concomitant diseases. OCD is often diagnosed in parallel with eating disorders and depression [6].
- Traumatic events. The disorder can be the result of difficult circumstances experienced: psychological and sexual abuse, physical trauma, loss of loved ones.
- Infections. Occasionally, OCD is found in children who have had a streptococcal infection.
 This is called pediatric autoimmune neuropsychiatric disorders.
This is called pediatric autoimmune neuropsychiatric disorders. - Do you experience obsessive thoughts about possible tragic events, death, serious illnesses, fires, accidents?
- Are you worried about the possibility of contamination with germs and chemicals?
- Do you unnecessarily re-read emails or text messages before or after sending them?
- Are you obsessed with keeping everything in order (cataloging books, perfect stacks of clothes in the closet, pencils arranged by size on the table)?
- Do you repeat routines such as opening a door, putting on your shoes, or getting into bed over and over again until you feel like you've done it "right"?
- Do you have recurring inappropriate thoughts (often of a religious, violent, or sexual nature) that seem intrusive and out of control?
- Do you feel the need to constantly seek confirmation of what you have said or done?
- Do you follow ritualized washing, cleaning or personal grooming habits (eg washing your hands five times in a row)?
- Do you avoid certain colors or numbers because you consider them "unlucky"?
- Do you check your trash before you throw it away to make sure it's clean?
- Do you worry about doing something out of a senseless urge, like pushing a stranger or hitting a loved one?
- Do you check oven handles, door locks and car brakes over and over again in a short period of time?
- Anxiety and Depression Association of America (ADAA) - mental health resources, including conferences of the International OCD Foundation.
 There are online support groups for those with the disorder.
There are online support groups for those with the disorder. - OCD Peers - Virtual support groups (6-10 members) using a HIPAA compliant platform. Video conferences with group mentor, open discussions and agenda. All groups are paid.
- 7 cups - on the platform you can find a volunteer who will be in touch and ready to listen to the problem. This is not a qualified professional, but sometimes speaking out to an attentive listener is just as important as working through a problem with a licensed psychotherapist.
- Support Groups - A free resource with several hundred support groups on a variety of topics, including those for OCD sufferers. Groups are moderated to avoid bullying and inappropriate user reactions.
- HealthUnlocked - literally "health unlocked" - a resource with forums to support people with various diseases. The ROC topic is moderated not only by the portal administrators, but also by representatives of the International ROC Foundation.
Learn more
What is obsessive-compulsive disorder?
Unsplash
Obsessive-compulsive disorder is a common chronic and long-term condition in which a person has uncontrollable repetitive, obsessive thoughts (ideas) and/or actions (behaviors) [1]. OCD is diagnosed in 1.3% of the world's population [2].
Many people confuse OCD with nail biting or negative thinking. Both can be a sign of the disease, but other diagnostic criteria must be taken into account.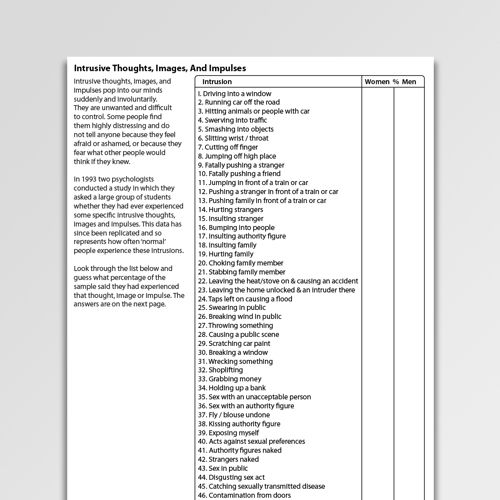 The obsession is often that a person considers certain numbers or colors to be "good" or "bad". It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3].
The obsession is often that a person considers certain numbers or colors to be "good" or "bad". It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3].
Vladimir BelovMedical psychologist, child psychologist, consultant suicidologist, leading specialist of the Semeynaya clinic network
“Obsessive Compulsive Disorder is a neuropsychological disorder that always includes two components:
The most common connection between these components is that compulsions are actions whose purpose is to neutralize or reduce the distress caused by obsessions. Rituals include such processes as endless washing of hands, double-checking one's own actions or the state of some objects. For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
Rituals include such processes as endless washing of hands, double-checking one's own actions or the state of some objects. For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
Signs and symptoms of obsessive-compulsive disorder
Unsplash
Obsessions - involuntary thoughts and ideas: "I shook hands with a person and now I can get infected with something." This rumination in itself is perfectly normal, but the person with OCD will wash their hands again and again, unable to get rid of it. This is already a compulsion - an obsessive behavior, an individual unstoppable ritual. In the short term, it reduces anxiety, but the thought returns and the action must be repeated. A person feels that he must do it, while he cannot stop. Everyone has recurring habits or thoughts that recur frequently. But in the case of OCD they are:
It's not unusual to wonder if the curling iron has been unplugged. It’s worth worrying if this thought haunts you every day, makes you return home halfway from work and check (more than once, even if you just made sure that the device is not turned on). Obsessive-compulsive disorder comes in many forms, but most cases fall into at least one of the four main categories. The symptoms of OCD are rooted in the person's obsessive behavior. For example, he:
Anastasia AfanasyevaPsychiatrist, psychotherapist, clinical director of the psychological platform Alter
“Intrusive thoughts can occur as part of a variety of disorders, from psychosis to anxiety. To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD.
To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD.
People without disorders can also have obsessive thoughts, but normally we quickly cope with them and they do not disturb life, forcing us to rebuild it for ourselves: the thought appeared - the person brushed it off and moved on.
Causes of OCD
Unsplash
Doctors do not give a specific explanation of the causes of the onset and development of OCD. It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
There is a hypothesis that disturbing deviations developed and persisted in the course of evolution [7]. When people did not have access to modern advances in medicine and hygiene, those who had less contact with a possible source of infection and were constantly on the alert, assessing possible risks and double-checking the safety of food and housing, survived.
Obsessive Compulsive Disorder Diagnostics
Unsplash
All people from time to time find themselves in stressful situations, many people find it helpful to put things in order at home or in the closet, everyone at least once caught himself thinking that he had not turned off the coffee maker in a hurry to a meeting. It doesn't mean you have OCD. Only a doctor can make an accurate diagnosis. Contact a specialist if the above symptoms directly affect your relationship with yourself and others, steal time, do not allow you to relax and enjoy life.
In society, the attitude towards OCD is often superficial and not serious. It is often perceived as a funny feature of a person. But the worsening symptoms cannot be controlled by willpower alone. OCD can be expressed in varying degrees of obsession, and for many it really does not interfere (and may help maintain cleanliness and keep processes under control), but for others it poses a real threat to normal life [8].
There are specialized tests for obsessive-compulsive disorder. Try to answer several questions in the format "often", "rarely", "never", "always":
If most of the described thoughts and situations appear suspiciously often in your daily life, you should consult a general practitioner. He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
How to treat obsessive-compulsive disorder
Shutterstock
There is no specific drug that can completely eliminate the symptoms of OCD. But medication support and additional psychological techniques for working on oneself help to work through this problem and keep it under control.
Psychotherapy
Cognitive Behavioral Therapy allows you to change your thinking patterns. Anastasia Afanasyeva believes that one of the most important techniques when working with OCD is distancing, exposing and challenging thoughts: “Distancing is a group of techniques in which we teach a person with OCD to notice intrusive thoughts, realize their ineffectiveness and switch from thinking about them to current ones. affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to.
affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to.
Exposure is the conscious exposure to uncomfortable situations in order to gradually learn to endure stress and stop using rituals that reduce anxiety in the moment, such as double-checking, washing hands, avoiding sharp objects.
Challenging and checking the reality of thoughts helps to understand that often a thought is just a thought and not every thought that comes to mind is worth believing. To assess how true this idea is, you can write it down on a piece of paper and give facts for and against its correctness.
Relaxation
Anxiety and obsessive thoughts are inevitably associated with tension in the body. Available meditation techniques, as well as massage and yoga classes, help to consciously look at the circumstances and cope with stress.
Anastasia Afanasyeva:
“In general, working with anxiety disorders always involves homework, as people learn to cope with their anxiety not only in the psychologist's office, but also in situations that arise in everyday life. Mostly it's working with thoughts and changing behavioral strategies that support OCD or reduce anxiety for only a short time.
The most common treatment for OCD involves individual sessions with a psychotherapist. There are practically no therapy protocols with proven efficacy for groups.”
Medicines
When taking drugs, you can achieve a stable remission. The timing of drug treatment will be determined by the attending physician. Do not stop taking antidepressants at the first sign of improvement.
Vladimir Belov:
“First of all, we need both a psychiatrist and a medical psychologist/psychotherapist. Because, on the one hand, cognitive-behavioral therapy is used, which is quite effective and has a lot of scientific evidence: exposure and prevention of reactions and rituals. This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is.
This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is.
What to do for relatives of a patient with OCD
Unsplash
People who live near a person with OCD often find themselves in difficult conditions. They want to help by interrupting the compulsive manifestations of a loved one, which can create an even more stressful situation for him. But it is also not worth closing your eyes to the disease. Psychologists advise updating it, pronouncing the problem. Develop the emotional intelligence of a loved one: let's understand that he can safely talk to you about any of his feelings. Emphasize that you are always ready to listen and help: “I am with you, we will deal with this problem together.”
Anastasia Afanasyeva:
“If someone in your family suffers from OCD, then one of the important tasks that you face is not to be included in the anxiety maintenance cycle.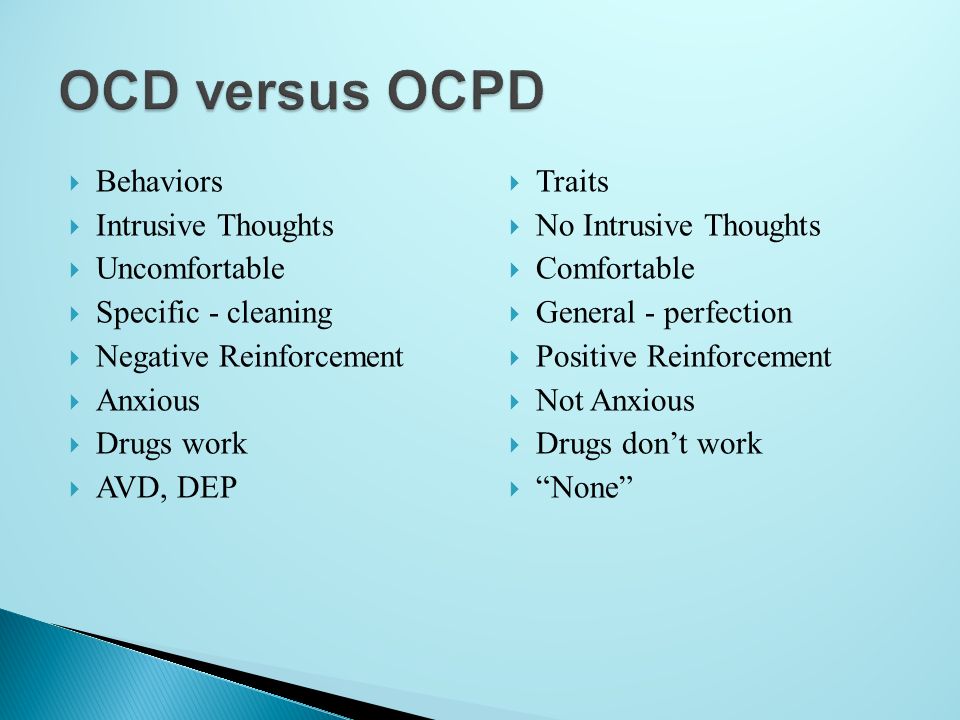 For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified.
For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified.
Forums, support groups for people with OCD
Unsplash
The best option is to contact a trusted doctor and treat according to his recommendations. In addition to medicines and work with a specialist, the fulfillment of independent tasks plays an important role. It is important for people with OCD to talk about the problem and see the support of others. Like-minded forums often help. You can join thematic groups on social networks or contact volunteers: