Which would be an emotional symptom of depression
Emotional Symptoms, Physical Signs, and More
Medically Reviewed by Smitha Bhandari, MD on March 16, 2023
It's natural to feel down sometimes, but if that low mood lingers day after day, it could signal depression. Major depression is an episode of sadness or apathy along with other symptoms that lasts at least two consecutive weeks and is severe enough to interrupt daily activities. Depression is not a sign of weakness or a negative personality. It is a major public health problem and a treatable medical condition.
Shown here are PET scans of the brain showing different activity levels in a person with depression, compared to a person without depression.
The primary symptoms of depression are a sad mood and/or loss of interest in life. Activities that were once pleasurable lose their appeal. Patients may also be haunted by a sense of guilt or worthlessness, lack of hope, and recurring thoughts of death or suicide.
Depression is sometimes linked to physical symptoms. These include:
- Fatigue and decreased energy
- Insomnia, especially early-morning waking
- Excessive sleep
- Persistent aches or pains, headaches, cramps, or digestive problems that do not ease even with treatment
Depression can make other health problems feel worse, particularly chronic pain. Key brain chemicals influence both mood and pain. Treating depression has been shown to improve co-existing illnesses.
Changes in appetite or weight are another hallmark of depression. Some patients develop increased appetite, while others lose their appetite altogether. Depressed people may experience serious weight loss or weight gain.
Without treatment, the physical and emotional turmoil brought on by depression can derail careers, hobbies, and relationships. People with depression often find it difficult to concentrate and make decisions. They turn away from previously enjoyable activities, including sex. In severe cases, depression can become life-threatening.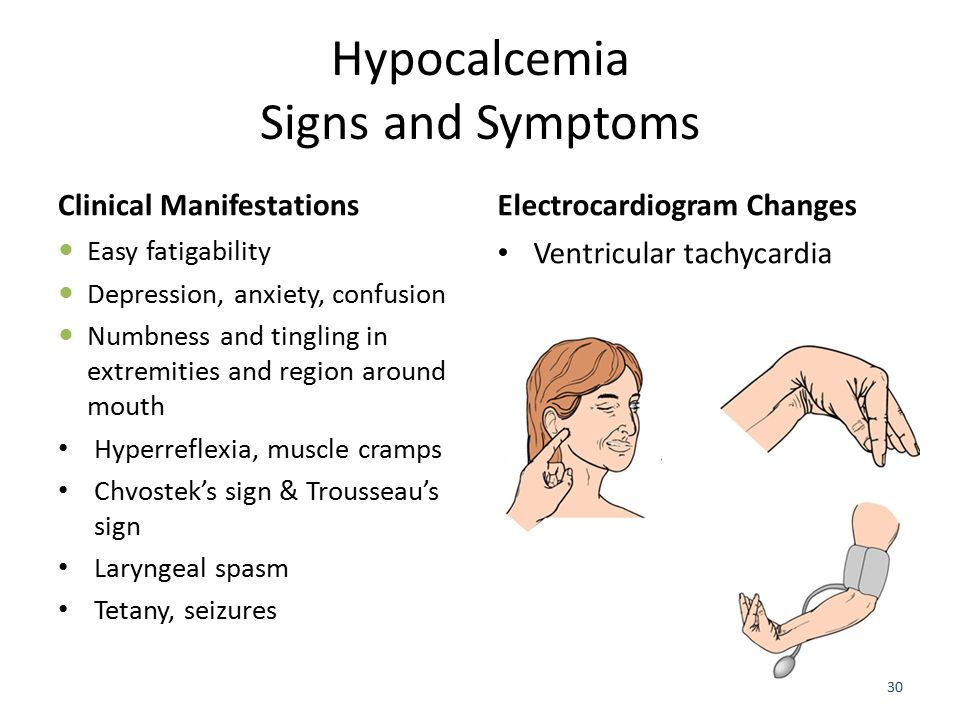
People who are depressed are more likely to attempt suicide. Warning signs include talking about death or suicide, threatening to hurt people, or engaging in aggressive or risky behavior. Anyone who appears suicidal should be taken very seriously. Do not hesitate to call one of the suicide hotlines: 800-SUICIDE (800-784-2433) and 800-273-TALK (800-273-8255). If you have a plan to commit suicide, go to the emergency room for immediate treatment.
Anyone can become depressed, but many experts believe genetics play a role. Having a parent or sibling with depression increases your risk of developing the disorder. Women are twice as likely as men to become depressed.
Doctors aren't sure what causes depression, but a prominent theory is altered brain structure and chemical function. Brain circuits that regulate mood may work less efficiently during depression. Drugs that treat depression are believed to improve communication between nerve cells, making them run more normally. Experts also think that while stress -- such as losing a loved one -- can trigger depression, one must first be biologically prone to develop the disorder. Other triggers could include certain medications, alcohol or substance abuse, hormonal changes, or even the season.
Experts also think that while stress -- such as losing a loved one -- can trigger depression, one must first be biologically prone to develop the disorder. Other triggers could include certain medications, alcohol or substance abuse, hormonal changes, or even the season.
Illustrated here are neurons (nerve cells) in the brain communicating via neurotransmitters.
If your mood matches the season -- sunny in the summer, gloomy in the winter -- you may have a form of depression called seasonal affective disorder (SAD). The onset of SAD usually occurs in the late fall and early winter, as the daylight hours grow shorter. Experts say SAD affects from 3% to 20% of all people, depending upon where they live.
The "baby blues" strikes as many as three out of four new mothers. But nearly 12% develop a more intense dark mood that lingers even as their baby thrives. This is known as postpartum depression, and the symptoms are the same as those of major depression. An important difference is that the baby's well-being is also at stake. A depressed mother may have trouble enjoying and bonding with their infant.
A depressed mother may have trouble enjoying and bonding with their infant.
In the United States, depression affects 2% of grade school kids and about one in 10 teenagers. It interferes with the ability to play, make friends, and complete schoolwork. Symptoms are similar to depression in adults, but some children may appear angry or engage in risky behavior, called "acting out." Depression can be difficult to diagnose in children.
As of yet, there is no lab test for depression. To make an accurate diagnosis, doctors rely on a patient's description of the symptoms. You'll be asked about your medical history and medication use since these may contribute to symptoms of depression. Discussing moods, behaviors, and daily activities can help reveal the severity and type of depression. This is a critical step in determining the most effective treatment.
Studies suggest different types of talk therapy can fight mild to moderate depression. Cognitive behavioral therapy aims to change thoughts and behaviors that contribute to depression. Interpersonal therapy identifies how your relationships impact your mood. Psychodynamic psychotherapy
helps people understand how their behavior and mood are affected by unresolved issues and unconscious feelings. Some patients find a few months of therapy are all they need, while others continue long term.
Interpersonal therapy identifies how your relationships impact your mood. Psychodynamic psychotherapy
helps people understand how their behavior and mood are affected by unresolved issues and unconscious feelings. Some patients find a few months of therapy are all they need, while others continue long term.
Antidepressants affect the levels of brain chemicals, such as serotonin and norepinephrine. There are many options. Give antidepressants a few weeks of use to take effect. Good follow-up with your doctor is important to evaluate their effectiveness and make dosage adjustments. If the first medication tried doesn't help, there's a good chance another will. The combination of talk therapy and medication appears particularly effective.
Research suggests exercise is a potent weapon against mild to moderate depression. Physical activity releases endorphins that can help boost mood. Regular exercise is also linked to higher self-esteem, better sleep, less stress, and more energy. Any type of moderate activity, from swimming to housework, can help. Choose something you enjoy and aim for 20 to 30 minutes four or five times a week.
Any type of moderate activity, from swimming to housework, can help. Choose something you enjoy and aim for 20 to 30 minutes four or five times a week.
Light therapy has shown promise as an effective treatment not only for SAD but for some other types of depression as well. It involves sitting in front of a specially designed light box that provides either a bright or dim light for a prescribed amount of time each day. Light therapy may be used in conjunction with other treatments. Talk to your doctor about getting a light box and the recommended length of time for its use.
St. John's wort is an herbal supplement that has been the subject of extensive debate. There is some evidence that it can fight mild depression, but two large studies have shown it is ineffective against moderately severe major depression. St. John's wort can interact with other medications you may be taking for medical conditions or birth control. Talk to your doctor before taking this or any other supplement.
A playful puppy or wise-mouthed parrot is no substitute for medication or talk therapy. But researchers say pets can ease the symptoms of mild to moderate depression in many people. Pets provide unconditional love, relieve loneliness, and give patients a sense of purpose. Studies have found pet owners have less trouble sleeping and better overall health.
Because loneliness goes hand-in-hand with depression, developing a social support network can be an important part of treatment. This may include joining a support group, finding an online support community, or making a genuine effort to see friends and family more often. Even joining a book club or taking classes at your gym can help you connect with people on a regular basis.
Vagus nerve stimulation (VNS) may help patients with treatment-resistant depression that does not improve with medication. VNS is like a pacemaker for the brain. The surgically implanted device sends electrical pulses to the brain through the vagus nerve in the neck. These pulses are believed to ease depression by affecting mood areas of the brain.
These pulses are believed to ease depression by affecting mood areas of the brain.
Another option for patients with treatment-resistant or severe melancholic depression is electroconvulsive therapy (ECT). This treatment uses electric charges to create a controlled seizure. Patients are not conscious for the procedure. ECT helps 80% to 90% of patients who receive it, giving new hope to those who don't improve with medication.
A newer option for people with stubborn depression is repetitive transcranial magnetic stimulation (rTMS). This treatment aims electromagnetic pulses at the skull. It stimulates a tiny electrical current in a part of the brain linked to depression. rTMS does not cause a seizure and appears to have few side effects. But doctors are still fine-tuning this treatment.
In the midst of major depression, you may feel hopeless and helpless. But the fact is, this condition is highly treatable. More than 80% of people get better with medication, talk therapy, or a combination of the two.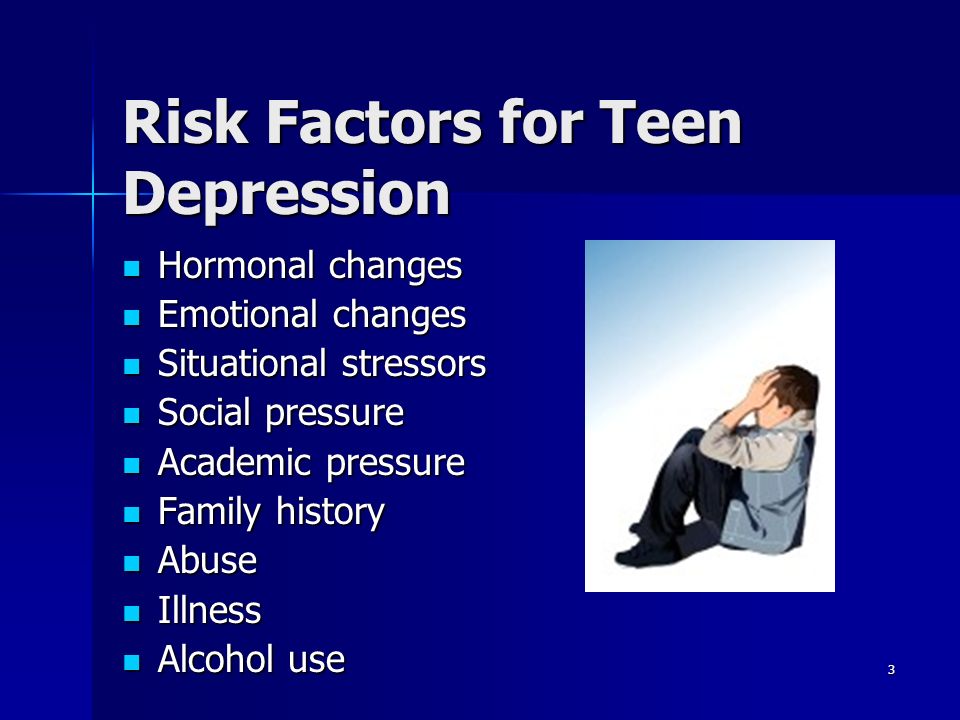 Even when these therapies fail to help, there are cutting-edge treatments that pick up the slack.
Even when these therapies fail to help, there are cutting-edge treatments that pick up the slack.
IMAGES PROVIDED BY:
(1) Science Source / Photo Researchers, Inc.
(2) Glowimages
(3) Bartomeu Amengual / age fotostock
(4) Jutta Klee / Stone
(5) Symphonie / Iconica
(6) Nikolaevich / Photonica
(7) Jetta Productions, Inc / Iconica
(8) 3D4Medical.com
(9) Megan Wyeth / Aurora
(10) Charles Gullung / Photonica
(11) Image Source
(12) Steve McAlister / Riser
(13) Mauro Fermariello / Photo Researchers, Inc.
(14) Mauro Fermariello / Photo Researchers, Inc.
(15) Katzer / Mauritius
(16) Christopher Furlong / Getty Images
(17) Dr. Jeremy Burgess / Photo Researchers, Inc.
(18) Leigh Schindler / Photodisc
(19) Alistair Berg / Digital Vision
(20) David J. Phillip / AP
(21) Will McIntyre / Photo Researchers, Inc.
(22) Universal Images Group / Getty
(23) Frank Gaglione / Riser
SOURCES:
Barkham, M.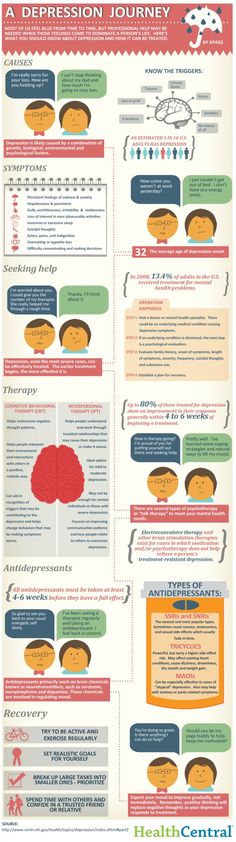 British Medical Bulletin, 2001.
British Medical Bulletin, 2001.
Gjerdinjen, D. Journal of the American Board of Family Medicine, 2007.
Harvard Health Publications: "Exercise and Depression."
Johns Hopkins Health Alerts: "The Many Benefits of Pets."
Johns Hopkins Medicine: "Seasonal Affective Disorder."
Mental Health America: "Co-occuring Disorders and Depression."
National Institute of Mental Health, National Institutes of Health: "How is depression diagnosed and treated?" "What causes depression?" "What are the signs and symptoms of depression?" "What illnesses often co-exist with depression?" "Magnetic Stimulation Scores Modest Success as Antidepressant," "Major Depressive Disorder in Children."
The Merck Manual: "Depression."
© 2023 WebMD, LLC. All rights reserved. View privacy policy and trust info
Emotional And Physical Warning Signs
So...you or someone you care about has been out of sorts for a while. You may not be able to put your finger on the problem. Maybe a “play it safe” physical exam turned up nothing of note. Still, you feel in your gut that something isn’t right.
Maybe a “play it safe” physical exam turned up nothing of note. Still, you feel in your gut that something isn’t right.
It could be any number of issues. But it’s possible that what you or your loved one is dealing with is depression, even if the feelings or behavior you’re noticing don’t quite fit your idea of what the signs and symptoms of depression are.
“People throw the word ‘depressed’ around a lot in everyday conversation, often to describe feeling sad or down. Sadness can definitely be a symptom of depression. But there are many signs and symptoms that contribute to a clinical diagnosis,” says Alexis Menken, PhD, a Montclair, New Jersey-based clinical psychologist and founder of the Conscious Motherhood Experience.
While it’s estimated that 21 million adults in America¹ had at least one major depressive episode in 2020, the unfortunate reality is that about two-thirds² of those struggling with depression don’t receive treatment. Not just because of the stigma still associated with help-seeking for mental illness. But because many are still unaware of what depression can look and feel like. (Lack of access to health care is another issue.)
But because many are still unaware of what depression can look and feel like. (Lack of access to health care is another issue.)
“Depression can wear many disguises,” says Heidi Heimler, PsyD, a psychologist with New Frontiers Psychiatry in Milwaukee, Wisconsin. How it manifests itself can depend on any number of factors including your physiological makeup, culture, age, gender, and mental health history.
Symptoms of depression may also emerge gradually, even subtly, and may therefore not be obvious. “A person with a limp or a hacking cough will likely get concerned or may be urged to see their doctor. But a person who grows more sullen or quiet, who doesn't show up for social functions or misses days of work, is more likely to fly under the radar,” says Heimler.
To make a diagnosis of clinical depression, health care providers generally follow guidelines laid out in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Your doctor may also order lab work and conduct a thorough physical exam to rule out other conditions like thyroid disease, low blood pressure, anemia, and vitamin D deficiency, which can have similar symptoms.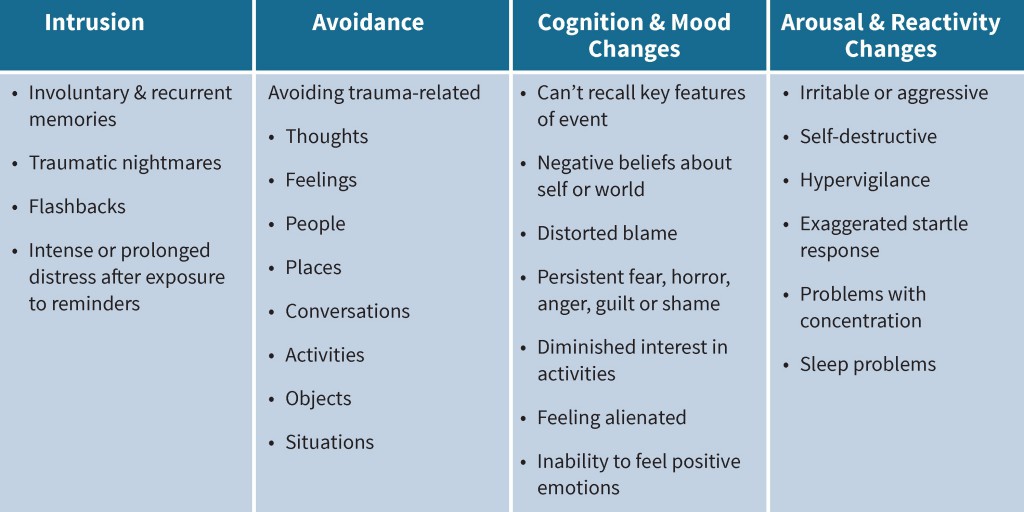
According to the DSM-5³, a patient meets the criteria for major clinical depression if they exhibit at least five out of a list of nine common symptoms on a daily basis for a minimum of two weeks. These symptoms may be a departure from what is usual. And a patient may be experiencing one of two symptoms in particular: sadness/depressed mood and loss of enjoyment of things they once found pleasurable (also sometimes called anhedonia). However, even these two symptoms can manifest in less obvious ways depending on the individual.
Keep in mind that the DSM gives health care providers flexibility when it comes to making their diagnosis. “Sometimes a patient may repress feelings of sadness and instead come off as irritable or disengaged. It’s up to therapists to explore those feelings and make the determination of whether their patient is dealing with depression, something else like anxiety or PTSD, or a combination of issues,” says Brent Metcalf, LCSW, a provider at Tri-Star Counseling in Johnson City, Tennessee.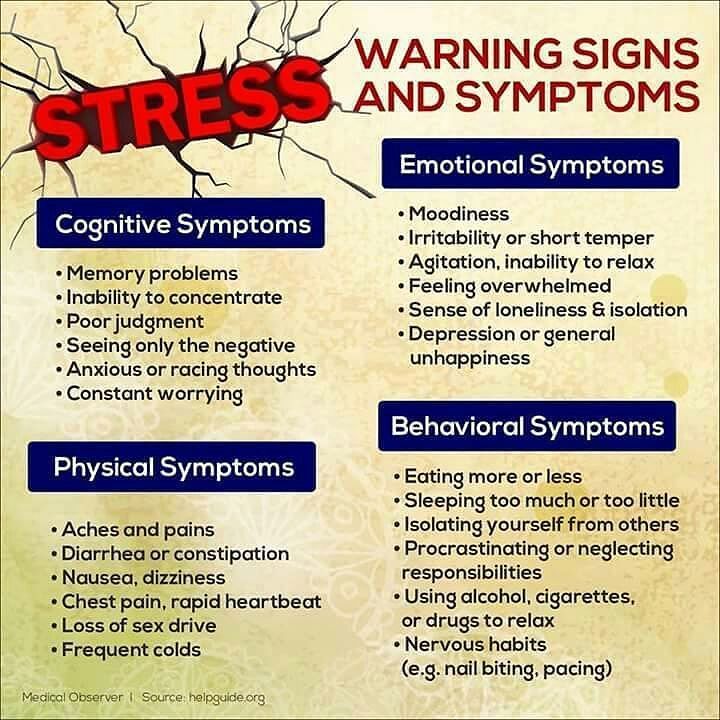
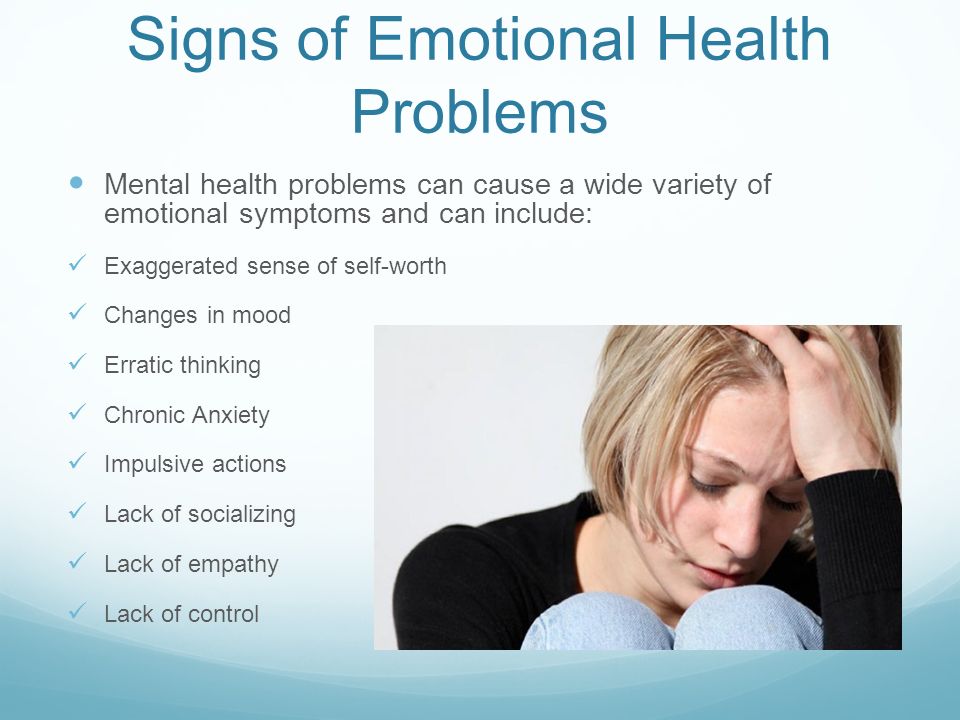
Emotional Symptoms
Following are some emotional symptoms often associated with major depressive disorder, some of which are included as DSM-5 criteria, but also others that can still be common related signs of the condition:
Persistent feelings of sadness and hopelessness. You feel down most of the day, almost every day, and have little or no optimism about life improving.
Loss of interest in activities you have usually enjoyed. You start to avoid or dread many of the pursuits that made life pleasurable, from hanging out with friends to having sex to exercising to eating. You may lose motivation, even to get up out of bed each morning.
Irritability and frustration. Your fuse is short. Everything seems to rub you the wrong way. “For some, it may be easier to lash out at others instead of sitting with what they are feeling. Often, though, under that anger is a lot of sadness. Think back to the bullies in school,” says Menken.
Anxiety. Almost half⁴ of those diagnosed with depression also struggle with intense and persistent anxiety (which can be diagnosed as a disorder unto itself). You may worry incessantly, fixate on certain issues, feel nervous, restless, and even have panic attacks.
Trouble with concentration and other cognitive functions. You just can’t seem to organize your thoughts and take action. Tasks are piling up, you can’t make decisions, the house is a mess, and you're forgetting details and commitments more than usual.
Feelings of guilt and worthlessness. You question your value as a human being. You blame yourself or feel overwhelming guilt about any number of things, from the burden you think you are to your spouse to your perceived failure to fulfill the dreams your parents held out for you.
Suicidal thoughts and ideations. You may or may not have a plan to carry out an attempt (see below for more on this topic).
 If you or someone you know needs help now, contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255). Or, simply call or text 988 to reach the crisis lifeline.
If you or someone you know needs help now, contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255). Or, simply call or text 988 to reach the crisis lifeline.
Physical Symptoms
Depression often goes undiagnosed because a significant percentage⁵ of depressed patients are aware of only physical symptoms (which can get genuinely exacerbated by mental distress: the mind and body are often linked). Also, people (particularly some in certain cultures and/or who feel uncomfortable discussing their mental health) can tend to express emotional upset as physical or bodily issues and seek help from primary care or other non-mental health providers first.
And far too often, these health care providers who are consulted fail to delve beneath the surface.⁶
Here are some common physical symptoms of depression:
Unexplained aches and pains. Achy joints and muscles. Headaches. Back pain. You notice that things just hurt more these days.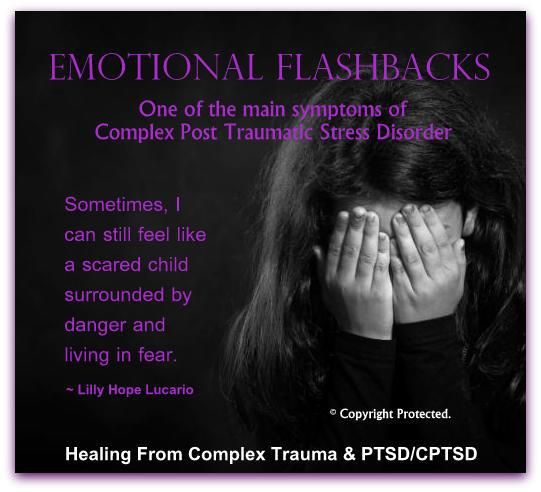 One possible reason: How we experience pain is regulated by serotonin and norepinephrine, two neurotransmitters that also regulate mood.⁷ In a sense, pain and mood share a pathway in the brain. And when one is affected, the other may be, as well.
One possible reason: How we experience pain is regulated by serotonin and norepinephrine, two neurotransmitters that also regulate mood.⁷ In a sense, pain and mood share a pathway in the brain. And when one is affected, the other may be, as well.
Digestive issues. Often called the second brain, the gut is where we process a lot of our emotions and is also rich in serotonin receptors. That’s why when we’re worried or scared, we can literally feel “sick to our stomach.” When you’re depressed, the impact can be ongoing, plaguing you with gastrointestinal miseries like indigestion, nausea, cramps, constipation, and diarrhea.
Changes in sleep patterns. You may be up all night. Or fall asleep, only to wake up in the wee hours, your mind buzzing with worry about anything and everything. “On the other hand, you may find that sleep is the only thing you can do, the only way you can get relief. So you may sleep excessively,” says Heimler.
Fatigue and consistent low energy.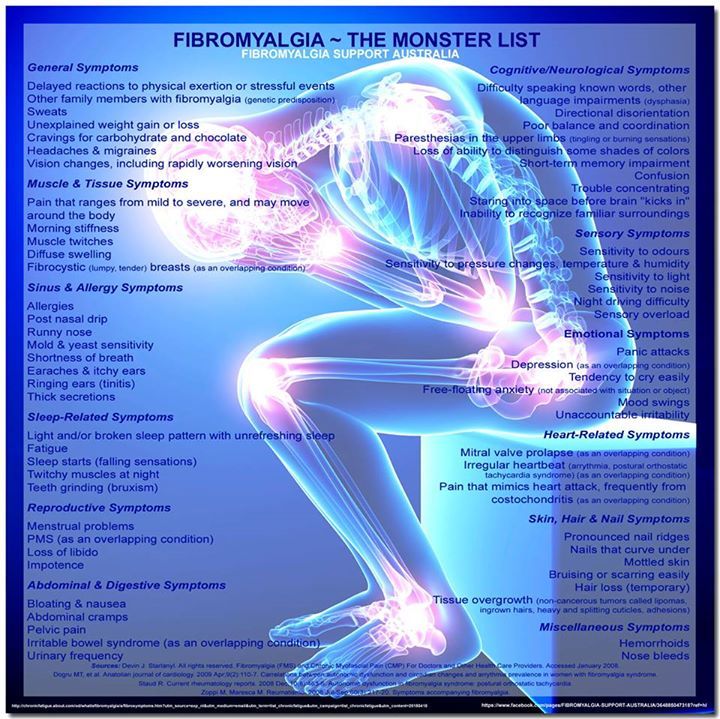 Even if you do sleep at night, you are exhausted all the time. Your limbs feel like lead. You can barely—or just plain can’t-- muster the energy to care for yourself or your family.
Even if you do sleep at night, you are exhausted all the time. Your limbs feel like lead. You can barely—or just plain can’t-- muster the energy to care for yourself or your family.
Appetite or weight changes. You don’t have much or any interest in eating and may be losing weight. “Or you may find that you're really hungry, eating without hunger, without pleasure, or joy,” Heimler says.
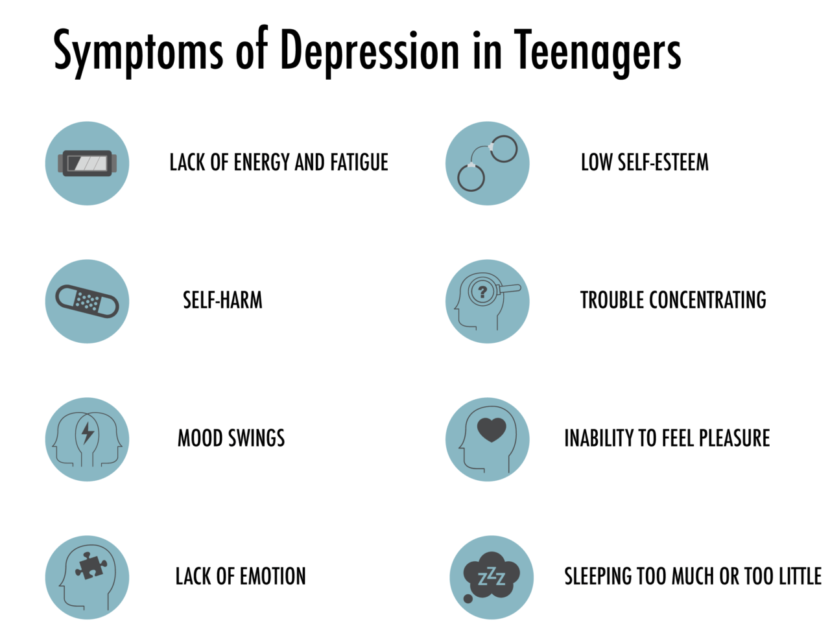
Signs of Depression in Teens, Young Adults, and Children
Young people have many of the same symptoms of depression that adults do, including persistent sadness, anxiety, low energy, unexplained aches and pains like headaches and stomach aches, and changes in appetite.
That said, younger children often are not yet capable of expressing their feelings. So, they may be more likely to show or complain about physical symptoms. Behaviorally, kids may also be more prone to tantrums and crying, crankiness, and may act out in school, at home, and in public.
Teens may behave erratically, crying, lashing out, and angering with little or no trigger.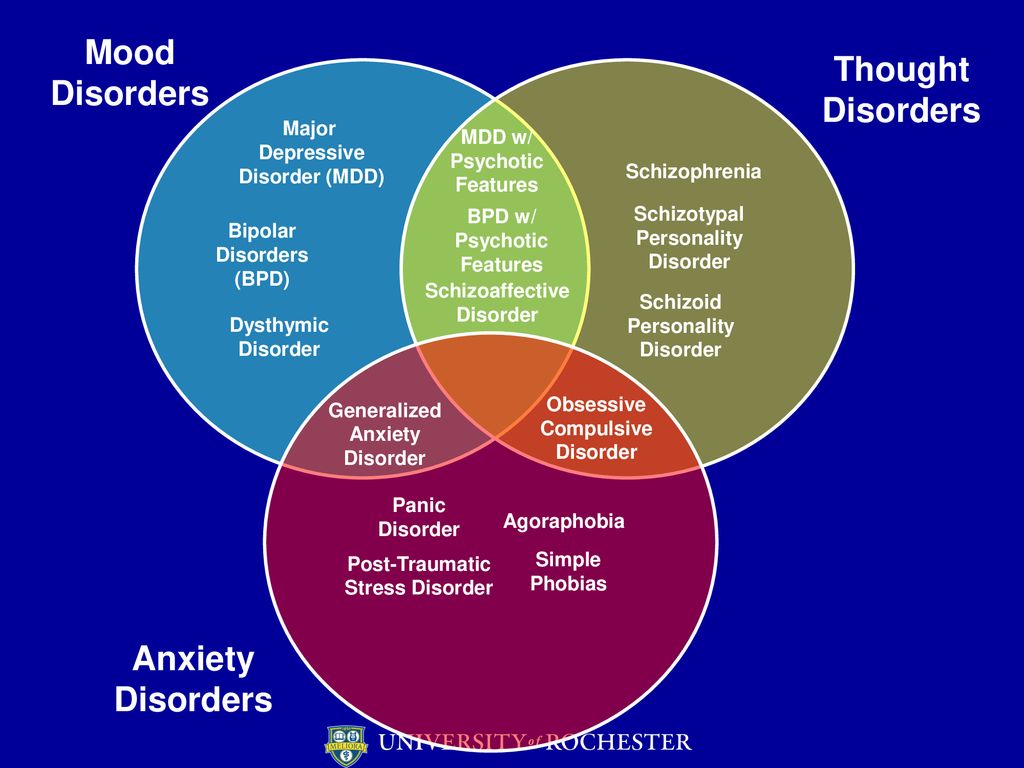 They may stop going out with friends, make frequent visits to the school nurse with vague complaints, tank in their classes, or constantly seek reassurance from parents and loved ones. It’s also not uncommon for depressed teens to self-medicate with drugs or alcohol and engage in self-harm, such as cutting and burning or getting excessive piercings or tattoos.
They may stop going out with friends, make frequent visits to the school nurse with vague complaints, tank in their classes, or constantly seek reassurance from parents and loved ones. It’s also not uncommon for depressed teens to self-medicate with drugs or alcohol and engage in self-harm, such as cutting and burning or getting excessive piercings or tattoos.
Depression can look different in women. Most research confirms that depression is about twice as common⁸ in women than in men. Fluctuations in estrogen levels throughout the reproductive cycle likely play a role, as do genetics. So do socioeconomic factors, such as women’s increased risk of living in poverty and experiencing emotional and sexual abuse.⁹
Women, in general, tend to be more in touch with their emotions than men and may be more inclined to seek help. Men on the other hand (thanks to social stereotypes about what it “means to be a man”) may consider mental illness and help-seeking as signs of weakness. Uncomfortable with and embarrassed about feelings of sadness and despair, they may withdraw from others and mask their symptoms.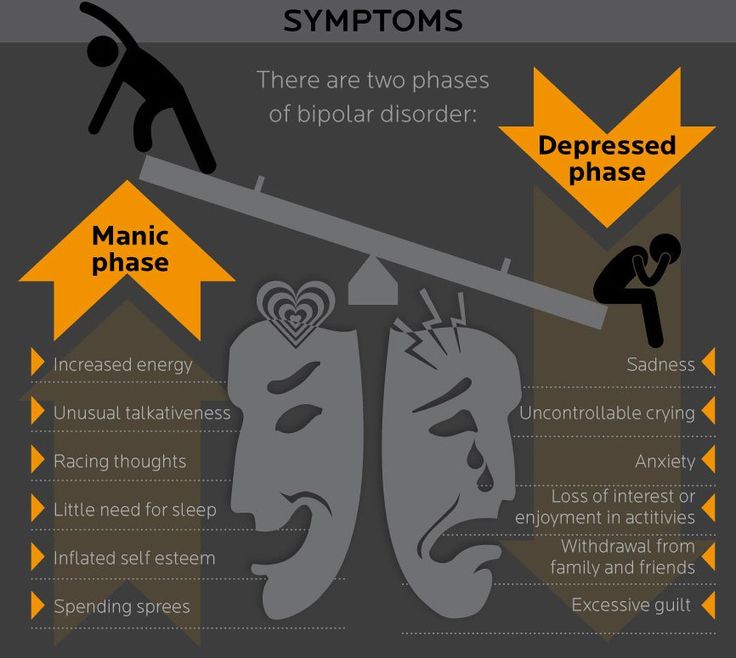 They can also be less talkative about their emotions.
They can also be less talkative about their emotions.
“People often just think men are angry because they're men and full of testosterone or have a temper. Really, this can be a symptom of depression,” says Metcalf. To cope, men may avoid family and friends by spending much of their time at work or playing sports; drink too much or develop a drug habit; exhibit risky behaviors, like aggressive driving; or become violent, controlling, or abusive.
Symptoms of Depression in Older People
Depression is often missed¹⁰ in elderly people because symptoms–such as social withdrawal, memory loss, and cognitive impairment–are chalked up to aging or attributed to age-related illnesses, like Alzheimer’s, Parkinson’s, or vascular disease. Sometimes these conditions may also co-occur or exacerbate one another. Complaints about physical aches and pains are common in elderly depression. Older people may also begin to neglect their personal hygiene, fixate on death, and seem to lose their will to live.
Men 85 and older have the highest suicide rate of any group in the U.S., according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
What To Do if You Think You Have Symptoms of Depression
If you suspect you’re depressed, you might first want to reach out to your primary care provider. They can screen you for depression and rule out any physical issues that might be causing your symptoms. Make sure you share with your doctor exactly what you’re feeling and tell them outright that you believe you may be depressed. Otherwise, they may miss the diagnosis, which is common.¹¹
If your primary care provider suspects depression, they can refer you to a therapist, and, if needed, a psychiatrist who can prescribe medication. If access to mental health specialists is limited (a problem that’s been exacerbated by the pandemic) your primary care provider can prescribe medication for depression. However, the best outcomes for major clinical depression are generally associated with a combination of talk therapy and medication. ¹²
¹²
“Some people absolutely do not want their primary care provider to know anything about their mental health. If that’s the case with you or if you don’t have a primary care provider, you can reach out to a therapist directly,” says Metcalf. And, of course, if you or someone you care about might be in danger of harming themselves, go to an ER or call the police for a welfare check. You can also contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or 988.
Suicidal Thoughts And Ideations
People with depression (and those with substance abuse issues) are at increased risk of suicide and suicidal ideation. What is suicidal ideation? Simply put, suicidal ideation involves thoughts about taking your own life. Some people in distress wish they could stop living but they don't actually have an organized plan to make that happen. Others put together an actual plan to end their life. Both are forms of suicidal ideation.
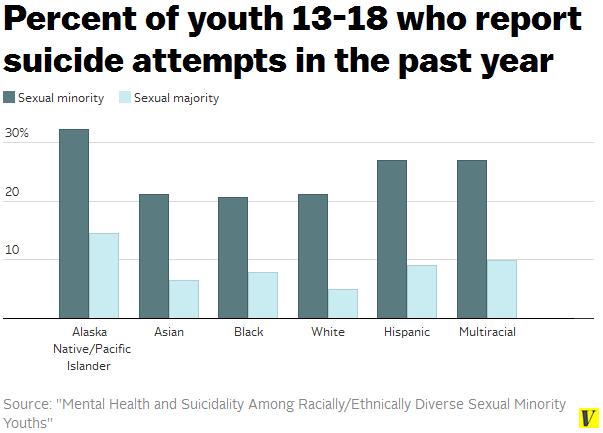
Suicide is the 10th leading cause of death in the United States and the second leading cause of death for young people (ages 10 to 34).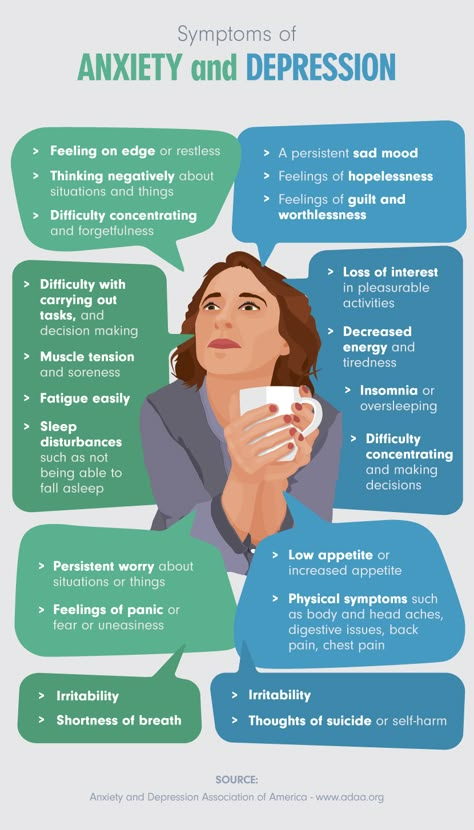 Although women attempt suicide more often than men, men are three to four times more successful, according to data from the National Institute of Mental Health (NIMH).
Although women attempt suicide more often than men, men are three to four times more successful, according to data from the National Institute of Mental Health (NIMH).
Suicide risk factors include a previous suicide attempt, depression, social isolation, struggling financially, having impulsive behavior, job loss or problems with crime, issues around substance use, legal problems, and having a serious illness.
Pay close attention to subtle behavior changes as they can be warning signs that someone is contemplating suicide. Be on the lookout for these indications:
Talking about death and suicide
Seeking access or researching the topic
Threatening to kill oneself
Withdrawing from family and friends
Expressing hopelessness by telling friends or family members they'd be "better off without me."
Drinking more alcohol or using more drugs
Giving away possessions
Saying goodbye
Mood changes—from dark to light—can also be a major red flag. It seems counterintuitive but once a person makes the decision (or formulates a plan) to end their life, they may feel relieved. Don't be fooled into thinking they are doing better, especially if other risk factors are present or you'd noticed the behaviors mentioned above.
It seems counterintuitive but once a person makes the decision (or formulates a plan) to end their life, they may feel relieved. Don't be fooled into thinking they are doing better, especially if other risk factors are present or you'd noticed the behaviors mentioned above.
One common misconception is that asking a person if they are thinking about suicide gives them the idea to do it. This is not the case. Many people struggling with depression don't feel comfortable talking about it and may be grateful for your concern. Having the courage to ask what's going on could quite literally save a life.
If you or someone you know needs help now, contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or 988.
Frequently Asked Questions About Depression
What is the number one sign of depression?
How depression manifests itself can depend on any number of factors including your physiological makeup, culture, age, gender, and mental health history. Sometimes, the only thing people are aware of are physical issues like unexplained aches and pains. That said, the two hallmark symptoms of depression–and the ones an official diagnosis generally hinges on–are sadness/depressed mood and the loss of enjoyment of things that a person once found pleasurable.
Sometimes, the only thing people are aware of are physical issues like unexplained aches and pains. That said, the two hallmark symptoms of depression–and the ones an official diagnosis generally hinges on–are sadness/depressed mood and the loss of enjoyment of things that a person once found pleasurable.
What would be an emotional symptom of depression?
Depression takes a heavy emotional toll. Among the ways it can show up are persistent feelings of sadness and hopelessness, loss of interest in activities you have usually enjoyed, irritability and frustration, anxiety, and feelings of guilt and worthlessness.
Can depression make you mean?
Irritability, hostility, and frustration are common symptoms of depression. “For some, it may be easier to lash out at others instead of sitting with what they are feeling. Often, though, under that anger is a lot of sadness. Think back to the bullies in school,” says Menken. Men, in particular, tend to mask feelings they are having and can become controlling and abusive.
How long do symptoms of depression last?
That can depend on many factors including the nature and severity of your depression, your mental health history, and whether you are receiving treatment. However, the mean duration of a depressive episode appears to range anywhere from three to 10 months, according to research.¹³ Importantly, many people experience more than one bout of depression in their lifetime. Treatment can reduce the risk of recurrence and help lessen the severity and duration of depressive episodes.
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. (2021) https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf. Accessed March 28, 2022.
- Williams SZ, Chung GS, Muennig PA. Undiagnosed depression: A community diagnosis. SSM - Population Health.
 2017;3:633-638. Accessed March 28, 2022.
2017;3:633-638. Accessed March 28, 2022. - Tolentino JC, Schmidt SL. Dsm-5 criteria and depression severity: implications for clinical practice. Front Psychiatry. 2018;9:450. Accessed March 28, 2022.
- Anxiety and Depression Association of America, Understanding Depression and Anxiety. (September 19, 2021) Available at https://adaa.org/understanding-anxiety/facts-statistics. Accessed March 28. 2022.
- Anxiety and Depression Association of America, Understanding Depression and Anxiety. (September 19, 2021) Available at https://adaa.org/understanding-anxiety/facts-statistics. Accessed March 28. 2022.
- Olver JS, Hopwood MJ. Depression and physical illness. Medical Journal of Australia. 2013;199(S6). Accessed March 28, 2022.
- Sheng J, Liu S, Wang Y, Cui R, Zhang X. The link between depression and chronic pain: neural mechanisms in the brain. Neural Plasticity. 2017;2017:1-10. Accessed March 28, 2022.
- Kuehner C. Why is depression more common among women than among men? The Lancet Psychiatry.
 2017;4(2):146-158. Accessed March 28, 2022.
2017;4(2):146-158. Accessed March 28, 2022. - Albert PR. Why is depression more prevalent in women? jpn. 2015;40(4):219-221. Accessed March 28, 2022.
- Allan CE, Valkanova V, Ebmeier KP. Depression in older people is underdiagnosed. Practitioner. 2014;258(1771):19-22, 2-3. Accessed March 28, 2022.
- Olver JS, Hopwood MJ. Depression and physical illness. Medical Journal of Australia. 2013;199(S6). Accessed March 28, 2022.
- Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry. 2014;13(1):56-67. Accessed March 28, 2022.
Notes: This article was originally published April 1, 2022 and most recently updated April 11, 2022.
Depression - is it genes or events?
In this article, we will talk about one of the most mysterious and controversial mental disorders. Until now, there are the most original and incredible explanations of how and why depression occurs.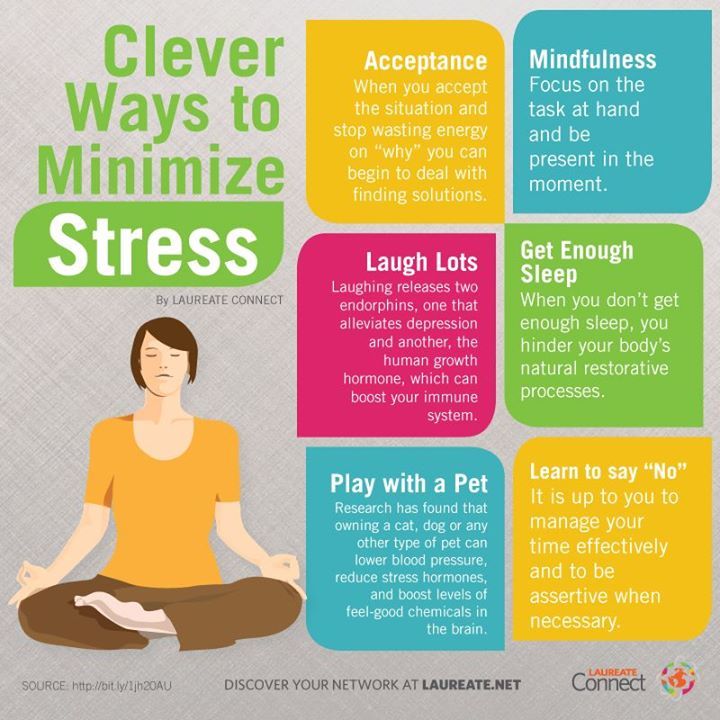 In fact, the disease is often disguised and takes surprising forms: sometimes it looks like ordinary insomnia, sometimes it looks like chronic fatigue with back pain. Arranging everything in different boxes, sticking beautiful and understandable labels, will definitely not work here.
In fact, the disease is often disguised and takes surprising forms: sometimes it looks like ordinary insomnia, sometimes it looks like chronic fatigue with back pain. Arranging everything in different boxes, sticking beautiful and understandable labels, will definitely not work here.
Although we struggle to come up with an exhaustive definition that would suit everyone, one thing is for sure: depression is not just sadness due to some kind of difficulty or failure.
It is a change in how we feel, think, and experience everyday emotions that keeps us from going to work and university, connecting with friends, and enjoying life.
Causes
Today, brain scientists do not single out any one specific cause of depression. There is a consensus that it is caused by a combination of a number of factors: biological, psychological and social , and each will have its own set. One will find relatives who had depression, and the other, it turns out, has always been prone to introspection, and recently also lost his job.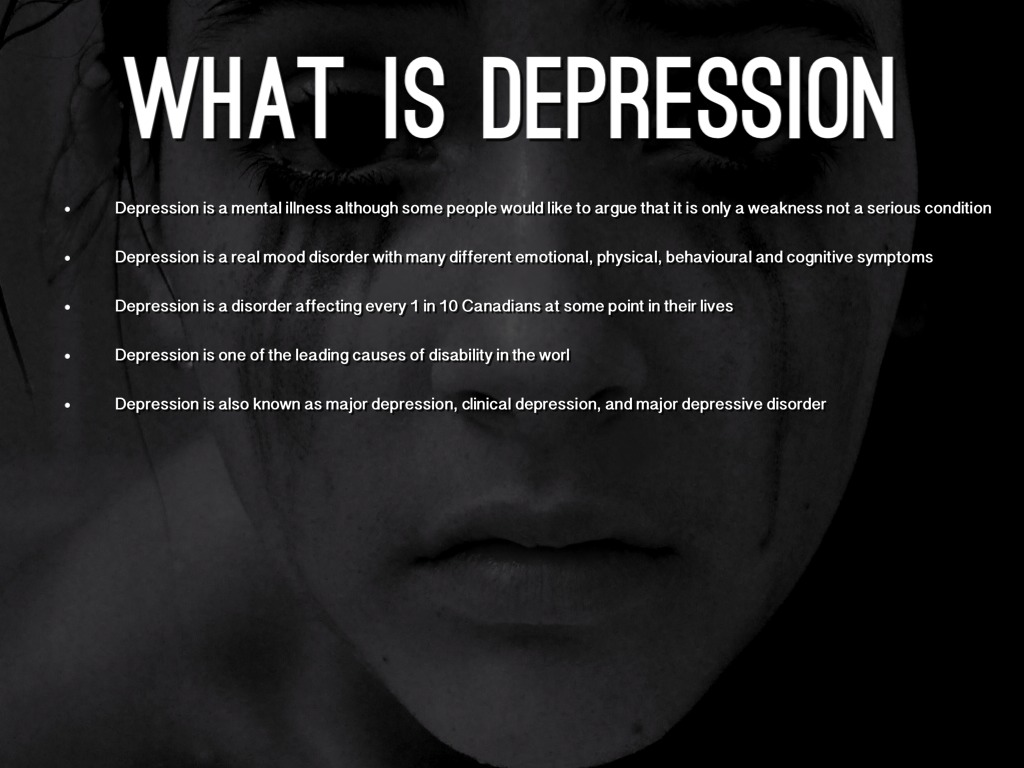
Of course, the factors always work together. For example, N. got divorced some time ago, while he already has a hereditary predisposition. Then these events can provoke a binge, and this, in turn, will change the biochemistry of the brain of N. Well, social consequences, such as losing relationships with friends, which often happens with alcohol abuse, will only aggravate the course. And this, as you understand, is just one scenario out of countless possible ones.
When talking about the most common causes, among them, as a rule, they note [1]:
- Hormonal problems , inflammatory processes, immunity decline, brain tissue pathologies, etc.
- Injuries and chronic diseases accompanied by pain syndrome .
- Taking barbiturates, corticosteroids, benzodiazepines, and certain birth control pills.
- History of anxiety . These diseases go hand in hand: about half of those who struggle with depression also suffer from increased anxiety.

- Stressful experiences , family and financial difficulties. This also includes perfectionism, the inability to move up the career ladder or otherwise be realized, as well as disorder in personal life.
- Drug and alcohol addiction . Psychoactive substances don't just cause powerful cravings. They create problems at the biochemical level, changing the quality of transmission of nerve impulses, which provokes chronic anxiety and low mood.
Is it possible to argue that some people are predisposed to this disease more than others? Apparently, yes.
Biological risk factors include a family history, as well as prior post-traumatic stress disorder, bulimia, and anorexia. Of course, there is no single gene. Therefore, if your parents suffered from this disease, it is not at all a fact that you will develop it. On the other hand, if you have been diagnosed with depression, your children have every chance of living a happy life without ever having a problem.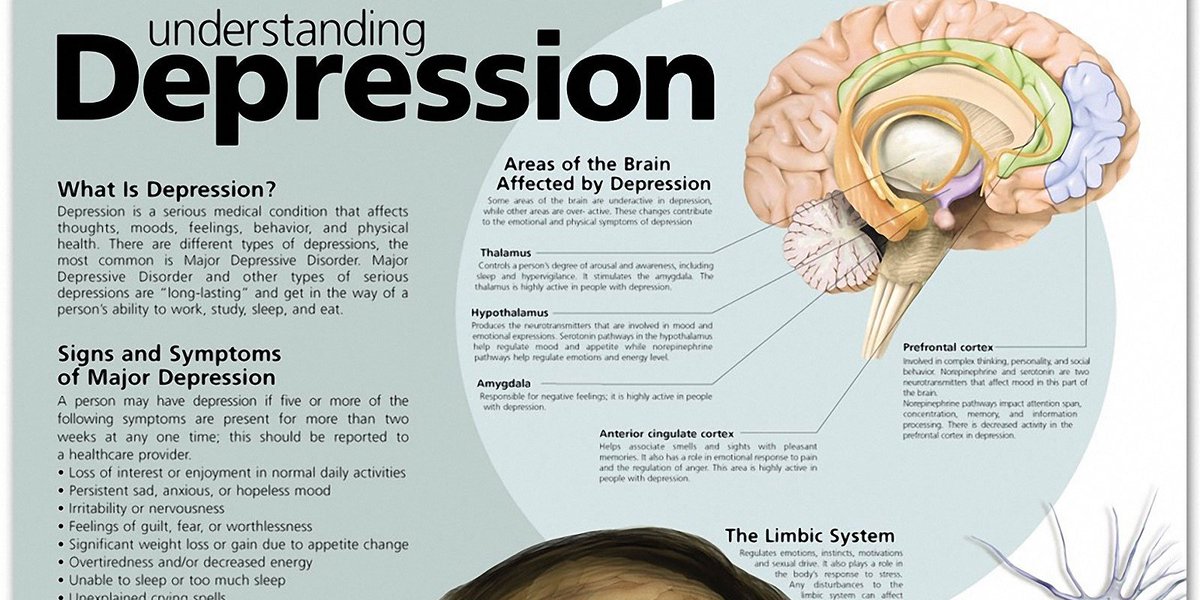 However, this is another reason to be vigilant and attentive to yourself and loved ones.
However, this is another reason to be vigilant and attentive to yourself and loved ones.
As for psychosocial risk factors, they invariably include increased self-criticism, early childhood trauma, including violence, and loneliness.
Sometimes it happens that a person who is already over thirty, looking back, realizes that he never made friends. Or found yourself in circumstances where loved ones are far away. Under these conditions, when there is no support around, getting out of depression may be somewhat more difficult.
Symptoms
The most common manifestations include:
- feelings of helplessness and hopelessness
- indifference to hobbies and leisure
- change in appetite and weight
- insomnia or drowsiness
- anger
- lethargy
- negative attitude towards oneself
- reckless behavior (reckless spending, extreme sports, dangerous driving, substance use)
It is important for those around you to understand that their loved one or colleague not only has no desire to go about their usual life, although it really may not be. But also there is no strength to continue to live as before. In other words, 90,015 people in a state of depression can neither be persuaded, nor encouraged, nor weakly taken.
But also there is no strength to continue to live as before. In other words, 90,015 people in a state of depression can neither be persuaded, nor encouraged, nor weakly taken.
Let's consider separately what changes in sleep take place. Many would probably assume that these people are constantly sleeping, because they have no strength for anything. This happens, but often the opposite happens - and all because of the disturbing component that we already mentioned. Anxiety prevents sleep, makes sleep intermittent, and due to the increased level of cortisol that is produced during stress, some patients complain of waking up early, around 4-6 in the morning.
According to the American Academy of Child and Adolescent Psychiatry, younger students are less likely to meet criteria in the DSM-5 Diagnostic and Statistical Manual of Mental Disorders. At the same time, among the specific features, irritability and anger are noted primarily. The fact is that it is difficult for children to explain what they feel, so they express their emotional pain in simple emotional reactions.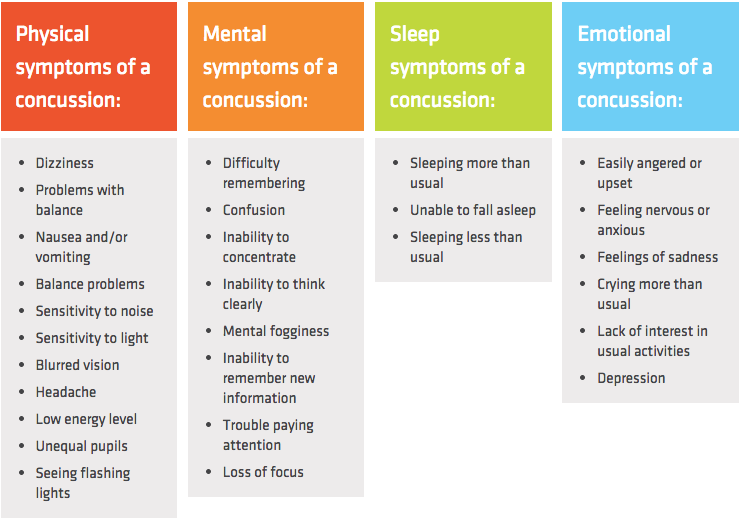 And although anxiety disorders are more often found in children of primary school age, in adolescents we already see more or less distinct manifestations of depression. In addition to irritability and tearfulness, specific symptoms of depression also include:
And although anxiety disorders are more often found in children of primary school age, in adolescents we already see more or less distinct manifestations of depression. In addition to irritability and tearfulness, specific symptoms of depression also include:
- unwillingness to spend time with peers
- low concentration
- decline in academic performance
- psychomotor agitation or retardation
- somatic pain (in the abdomen, headaches, etc.) [2]
I recall a case when a boy of thirteen after the holidays and against the background of a difficult relationship between his parents developed apathy and a breakdown. All tests were normal, including MRI and ultrasound. It was difficult for the child to talk, while he spoke very quietly, always looked at the floor, it was difficult for him to remember something. It was felt that he absolutely did not care about anything around: the boy could not name his favorite lessons, did not know what kind of wallpaper he would like in his bedroom, which was then being renovated.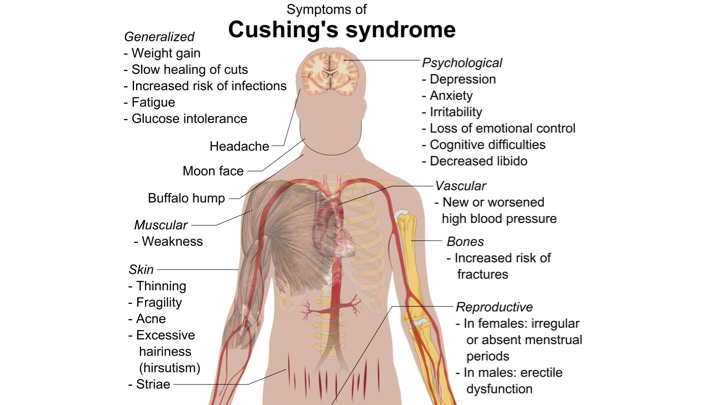 Of course, problems began at school, bad grades rained down one after another. And only against the background of taking SSRIs (they will be discussed later in the article) was it possible to restore eye contact, the child was no longer afraid to look into his eyes, he began to enthusiastically talk about his favorite games. Fortunately, he made friends again and his studies returned to normal.
Of course, problems began at school, bad grades rained down one after another. And only against the background of taking SSRIs (they will be discussed later in the article) was it possible to restore eye contact, the child was no longer afraid to look into his eyes, he began to enthusiastically talk about his favorite games. Fortunately, he made friends again and his studies returned to normal.
Pathogenesis
Although it is already 2023, scientists are still in no hurry to give a definite answer to the question of what and where breaks down in the body during depression. There are, however, several popular theories, one of which links the development of the disease with neurotransmitters - chemicals that ensure the conduction of nerve impulses. If you have already read our previous articles, then you know that from a chemical point of view, some of them are monoamines. Therefore, this concept is also known as monoamine.
Her idea is as follows. Our neurons are connected by tiny structures called synapses.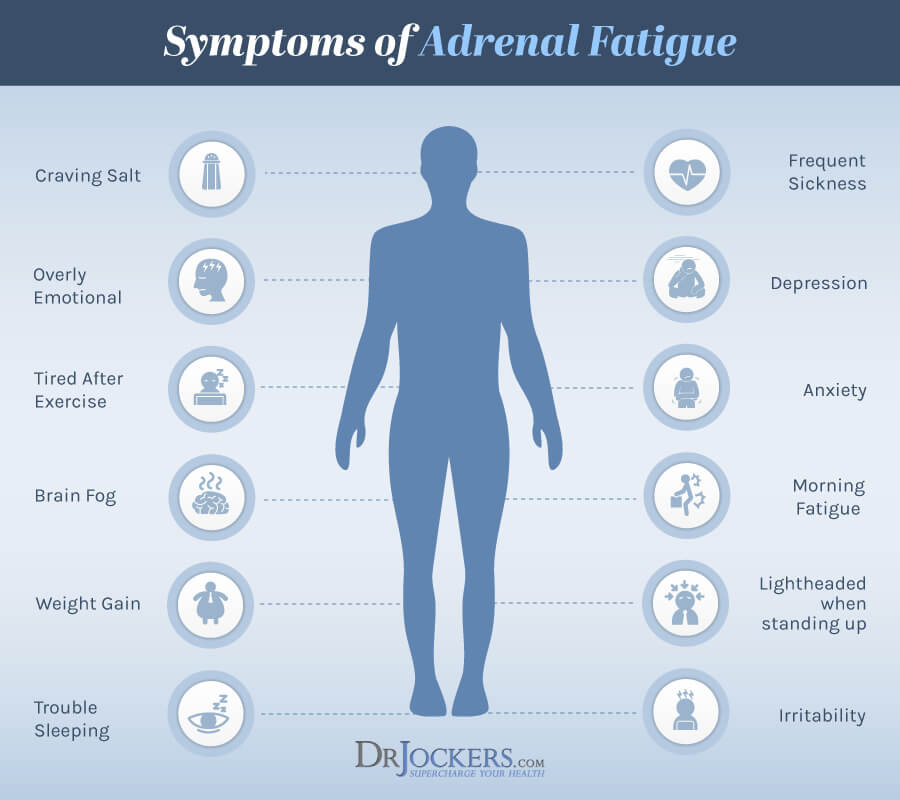 Such connections are somewhat similar to a joint. When excited, a certain amount of neurotransmitter is released into the synaptic space. It is logical that with a decrease in the level of neurotransmitters, the propagation of impulses will be difficult. And it is precisely here that the supporters of the monoamine hypothesis see the whole root of evil. It has been noticed that a lack of serotonin gives lethargy, depression and poor sleep, when it is difficult to fall asleep, and waking up, a person does not feel cheerful. With a deficiency of norepinephrine, a chronic pain syndrome is formed, and a lack of dopamine, in turn, provokes a decrease in motivation, when we not only do not want to conquer new heights, but even refuse what used to please and fascinate. It would seem that a harmonious concept that sorts out the emotional, behavioral and even bodily aspects. However, oddly enough, there are some questions to it in scientific circles [3].
Such connections are somewhat similar to a joint. When excited, a certain amount of neurotransmitter is released into the synaptic space. It is logical that with a decrease in the level of neurotransmitters, the propagation of impulses will be difficult. And it is precisely here that the supporters of the monoamine hypothesis see the whole root of evil. It has been noticed that a lack of serotonin gives lethargy, depression and poor sleep, when it is difficult to fall asleep, and waking up, a person does not feel cheerful. With a deficiency of norepinephrine, a chronic pain syndrome is formed, and a lack of dopamine, in turn, provokes a decrease in motivation, when we not only do not want to conquer new heights, but even refuse what used to please and fascinate. It would seem that a harmonious concept that sorts out the emotional, behavioral and even bodily aspects. However, oddly enough, there are some questions to it in scientific circles [3].
Consider another hypothesis, already quite fresh. We rarely think about how much progress has been made in the field of neuroimaging over the past decade. Namely, this method allowed a group of scientists from the ENIGMA project to study in detail the structural and functional changes in the brain during depression. Doctors and neurophysiologists from all over the world presented their observations in 2020 in the journal Translational Psychiatry [4].
We rarely think about how much progress has been made in the field of neuroimaging over the past decade. Namely, this method allowed a group of scientists from the ENIGMA project to study in detail the structural and functional changes in the brain during depression. Doctors and neurophysiologists from all over the world presented their observations in 2020 in the journal Translational Psychiatry [4].
They found that the size of the hippocampus (a subcortical structure responsible for storing information and reactions based on previous experience) in those suffering from this disease is, on average, smaller than in healthy controls. This difference was especially noticeable when the disease had a recurring course. Curiously, in patients taking antidepressants, the hippocampus eventually returned to normal size.
It is also interesting that adolescents also showed a reduction in the surface area of the cerebral cortex, which was not observed in adults. Probably, this symptom should be considered a marker of an early onset disorder.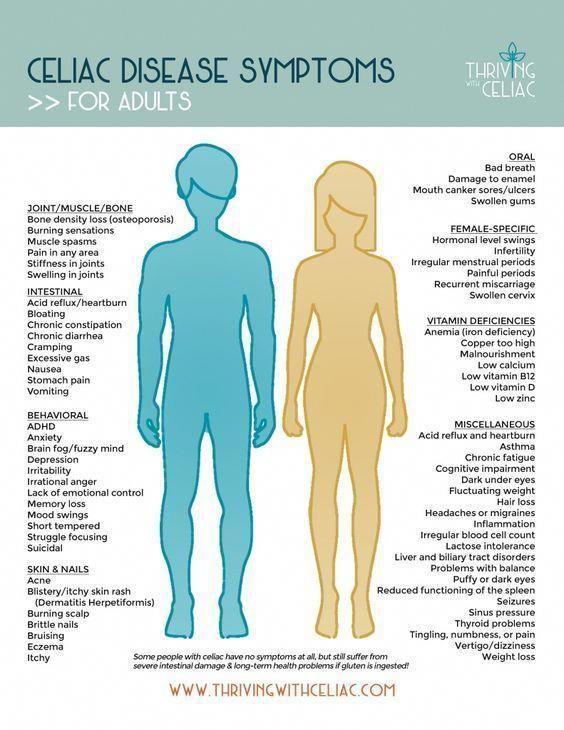
Classification
According to the degree of severity , the following types of depression are distinguished:
- light
- moderate
- large
By flow type differ:
- single episode
- recurrent (recurring)
- dysthymia or persistent depressive disorder
To understand what dysthymia is, imagine a relapsing condition where a person experiences sadness and related symptoms for most of the year. At the same time, its difference from major depression is that the latter, no matter how expressed its manifestations, is still a single, that is, continuous, episode.
Let's talk now about special cases with a repetitive course. Among them, it is worth noting seasonal affective disorder (SAD) . According to statistics, 1-2% of the population suffers from it, mostly young people and girls. This is due to the reduction of daylight in winter and a change in the production of melatonin, a hormone responsible for changing sleep and wake cycles. During the long winter nights, it is produced in excess, and therefore in the mornings some feel drowsy, and during the day - a breakdown. With a genetic predisposition, some people develop a real winter blues.
During the long winter nights, it is produced in excess, and therefore in the mornings some feel drowsy, and during the day - a breakdown. With a genetic predisposition, some people develop a real winter blues.
Interestingly, a special treatment for SAD has been invented, Light Therapy , which is proving to be very effective. The idea is to spend some time, for example at breakfast, in front of a special bright fluorescent lamp. Such devices are much more powerful than conventional lamps and provide illumination up to 10,000 lux, which is several times greater than that of a conventional lamp.
Another case of recurrent depression is called premenstrual dysphoric disorder (PMDD) , which is often an unpleasant addition to the well-known PMS. Some women show irascibility, tearfulness, and experience sleep disturbance. PMDD develops 10-14 days before the menstrual period, and with its onset, everything gradually returns to normal.
Diagnostic methods
The first thing that would come to mind for lovers of self-diagnosis is to take tests for serotonin or cortisol.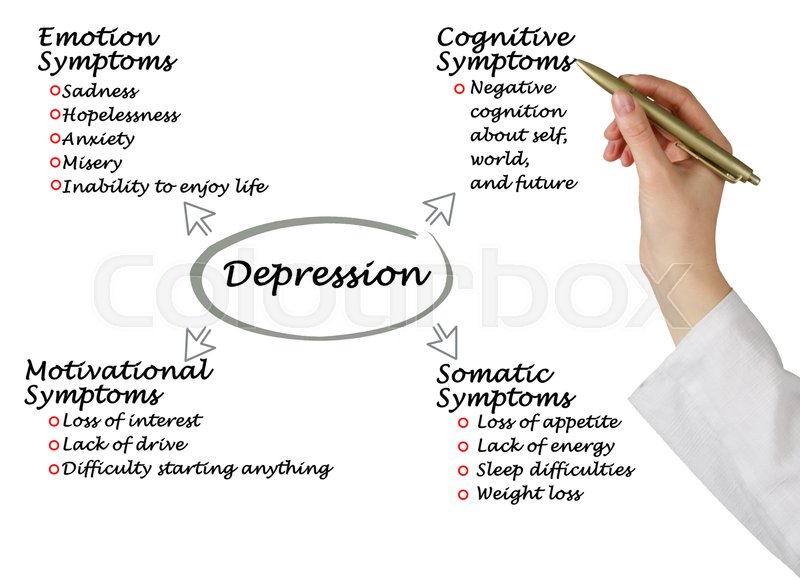 Isn't that logical? Honestly, no. These substances are indeed present in the blood, as they perform other functions in the body. But the thing is that their molecules are too large to penetrate the brain through the blood-brain barrier, which means they do not interact with receptors in the central nervous system in any way. Alas, some laboratories take advantage of the fact that a non-specialist does not know these nuances and offer absolutely uninformative analyzes.
Isn't that logical? Honestly, no. These substances are indeed present in the blood, as they perform other functions in the body. But the thing is that their molecules are too large to penetrate the brain through the blood-brain barrier, which means they do not interact with receptors in the central nervous system in any way. Alas, some laboratories take advantage of the fact that a non-specialist does not know these nuances and offer absolutely uninformative analyzes.
Questionnaires help to understand what is happening. Often used is the Beck scale , as well as the hospital scale HADS .
Although the first questionnaire was created in the sixties of the twentieth century, it continues to be widely used in the diagnosis of depressive states. The Beck Scale has twenty-one questions and four response options. It assesses severity as well as associated cognitive and bodily symptoms.
Hospital scale HADS gives a somewhat less detailed assessment, but allows you to identify an alarming component. The questionnaire consists of 14 questions with four possible answers.
The questionnaire consists of 14 questions with four possible answers.
It is important for a psychiatrist or neurologist to exclude any other causes of mood changes, such as those observed in thyroid pathologies. It is also important to make sure that the patient does not have what is called hypomania, that is, episodes with a surge of energy against the background of disorganized thinking and chaotic activity. If such episodes occur, then, apparently, we are talking about bipolar disorder.
A case comes to mind when a schoolboy was diagnosed with depression. It would seem that everything corresponded to this: the child did not want to go to school, was distracted, did not sleep well. After a month and a half, the treatment still had to be revised, as the boy became aggressive, began to openly be rude at home, although this had not been noted before. After discontinuation of the drug, these behavioral reactions disappeared after a week, but after a couple of months they reappeared, which indicated bipolar disorder.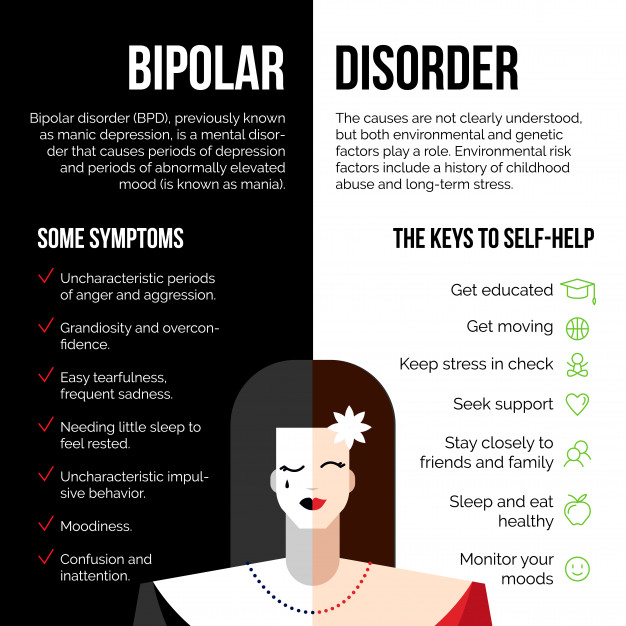 In such cases, psychiatrists prescribe lithium, and antidepressants can be harmful.
In such cases, psychiatrists prescribe lithium, and antidepressants can be harmful.
Methods of treatment
To get rid of depression, you need to contact a psychiatrist or a neurologist . The doctor will examine the patient's condition and, if necessary, prescribe antidepressants - drugs that will slow down the removal of neurotransmitters from the intercellular space. For this, the so-called selective reuptake inhibitors are prescribed, and their specific variety depends on the actual symptomatology. The most common option is selective serotonin reuptake inhibitors (SSRIs). But also, if there is a pain syndrome, those that slow down the excretion of norepinephrine can be prescribed. Or antidepressants with dopamine activity, if there is a loss of "taste for life" and problems with motivation.
Starting therapy, it should be remembered that it will not become easier immediately, but only as the drug accumulates.
Thus, the initial effect will be noticeable not earlier than in one to two months.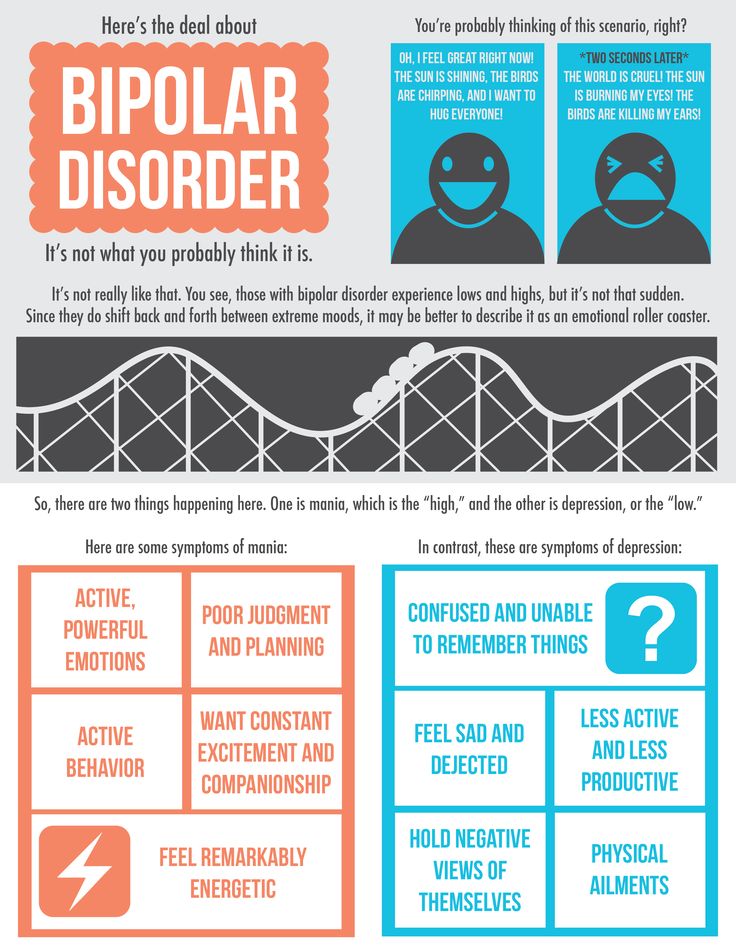 With the initial episode, treatment can take six months, with repeated episodes - at least a year. Accordingly, if the condition recurs, treatment should be longer and more thorough. There is an important nuance here: those same terms are not counted from the start of taking medications, but only from mood stabilization, that is, starting from the moment when the therapy brought the first results. This also applies to trips to a psychotherapist: here, too, you will have to be patient.
With the initial episode, treatment can take six months, with repeated episodes - at least a year. Accordingly, if the condition recurs, treatment should be longer and more thorough. There is an important nuance here: those same terms are not counted from the start of taking medications, but only from mood stabilization, that is, starting from the moment when the therapy brought the first results. This also applies to trips to a psychotherapist: here, too, you will have to be patient.
It is also important to pay attention to comorbidities. Insomnia, for example, requires immediate correction. Only by normalizing sleep, it will be possible to restore working capacity and the overall quality of life, and without this, one cannot speak of a complete recovery.
Prevention
If there is a predisposition to depression, it is recommended to work with psychotherapist to correct some stereotypes of perception and thinking and prevent new episodes. It is important for people to know that they are not alone.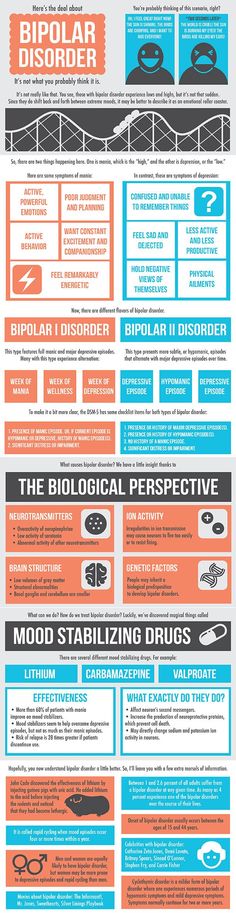 So another good idea is to visit self-help groups, which are usually found in large cities - you can also look for them online.
So another good idea is to visit self-help groups, which are usually found in large cities - you can also look for them online.
What else can be done to prevent relapses? Of course, go in for sports . Physical exercise increases the number of nerve connections and has been proven to increase the level of serotonin and endorphins.
In addition, doctors advise to reduce the amount of "fast" carbohydrates , which lead to mood swings. Their sources include flour and confectionery products , as well as sugar and sugar-sweetened beverages . It is also extremely important to observe the daily routine: getting up and going to bed should be at the same time.
In conclusion, we will also give some recommendations to parents. If you notice that your child often feels sad, avoids peers, sleeps poorly, and finds it difficult to focus on school, you may be dealing with depression. In this case, it is necessary to strictly observe the daily routine and create conditions in which the child will feel love, support and safety. Below are three points that will help maintain a psychologically comfortable atmosphere at home.
Below are three points that will help maintain a psychologically comfortable atmosphere at home.
-
Make sure that your relationship with your spouse does not disturb your son or daughter.
-
Make it so that once a week the child can spend time with each of the parents - without gadgets, without brothers and sisters, just you and him.
-
Practice "round tables" : a kind of meeting, for example once a week or a month, when everyone can tell what is bothering them, in the most confidential atmosphere and without fear of judgment.
Terminals
-
Depression, as you can see, is truly complex, diverse and multifactorial. We believe that for its comprehensive understanding, it is more correct to use a biopsychosocial approach that takes into account physiological, personal and purely external factors. This is the same model that doctors use to treat depression: you take drugs, go to therapy, and along the way, try to change life circumstances where possible.

-
There are many assumptions about the causes of depression and risk factors for their occurrence. Quite likely, but not the only ones, include increased anxiety, addictions, as well as other mental illnesses in history. Most scholars also refer to childhood trauma, some physical illnesses, especially those accompanied by disability or pain, taking certain medications, and stress.
-
Common signs of depression include feelings of helplessness, withdrawal from previous hobbies, sudden weight loss or weight gain, drowsiness or insomnia, negative self-esteem, ignoring danger, and pain of unknown etiology.
-
So far, no evidence has been obtained that the disease is inherited. But it is safe to say that some kind of predisposition still exists. It is believed that the basis is the incorrect conduction of nerve impulses, but it would be wrong to associate everything only with a deficiency of neurotransmitters. Recently, there has been evidence that hippocampal volume reduction also plays a role.
-
Depression is usually classified according to severity (mild, moderate, major) and type of course (recurrent and single episode). At the same time, disorders like dysthymia, SDR and PMDD, which are characterized by a recurring course, are also distinguished.
-
SSRI drugs have proven efficacy and are trusted by doctors. Depending on the symptoms, antidepressants with norepinephrine and dopamine activity, as well as tranquilizers, are sometimes prescribed. In addition to drugs, psychotherapy is also indicated - with timely treatment, this combination can work wonders.
Our Evidence-Based Medicine Clinic Specialists will help you and your loved ones cope with depression.
Sources
1. Depression Types, Causes, and Risk Factors https://www.helpguide.org/depression-types-causes-and-risk-factors.htm
2. American Academy of Child and Adolescent Psychiatry https://www. aacap.org/AACAP/Families_and_Youth/Resource_Centers/Depression_Resource_Center
aacap.org/AACAP/Families_and_Youth/Resource_Centers/Depression_Resource_Center
3. Albert P. R., Benkelfat C., Descarries L. The neurobiology of depression - revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms // Philosophical Transactions of the Royal Society B: Biological Sciences. — 2012; 367 (1601): 2378-2381.
4. ENIGMA project: Seven years of neuroimaging studies of depression https://psyandneuro.ru/stati/enigma/
Depressive disorder (depression)
Depressive disorder (depression)- Health Issues »
- A
- B
- C
- D
- Y
- E
- Y
- F
- 26
- I
- K
- L
- M
- H
- O
- P
- R
- S
- T
- Y
- F
- X
- C
- W S
- b
- S
- b
- E
- Yu
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- D
- D
- E
- Y
- W
- W
- I
- Y
- R
- L
- M
- H
- R
- C
- T
- Y
- F
- X
- C
- H
- W
- W
- b
- Y
- b
- E
- Y 022
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- case studies
- Questions and answers
- Speeches
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Depressive disorder (depression)
Getty Images/1216841763
© Photo
Key Facts
- Depression is a common mental health problem.

- An estimated 5% of the world's adults suffer from depression.
- Depression is more common among women than among men.
- Depression can lead to suicide.
- There are effective treatments for mild, moderate and severe depression.
General Information
Depressive disorder (also called depression) is a common mental health disorder. It is characterized by long periods of depressed mood or loss of interest in or enjoyment of habitual activities.
Depression is different from regular changes in mood and emotions in relation to the realities of everyday life. It can negatively affect all aspects of a person's life, including relationships with family, friends and other people. It can be the result or cause of problems in school and at work.
Depression can affect anyone. People who have experienced violence, bereavement, or other stressful events are more likely to develop depression. Women are more likely to suffer from depression than men.
It is estimated that 3.8% of the population experiences depression, including 5% of adults (4% of men and 6% of women) and 5.7% of people over the age of 60. Around 280 million people worldwide suffer from depression (1) . Among women, the prevalence of depression is about 50% higher than among men. Depression affects more than 10% of pregnant women and women who have just given birth worldwide (2) . More than 700,000 people commit suicide every year. Suicide is the fourth leading cause of death in the 15-29 age group.
Despite the availability of proven and effective treatments for mental disorders, more than 75% of people in low- and middle-income countries receive no treatment (3) . Factors hindering effective treatment include insufficient investment in mental health care, a shortage of trained health workers, and social stigmatization of people with mental disorders.
Symptoms and forms of depression
During a depressive episode, a person experiences a depressed mood (feelings of sadness, irritability, emptiness). He may lose the ability to enjoy or be interested in daily activities.
A depressive episode must be distinguished from regular mood swings. Depressive episodes last most of the day and occur nearly every day for at least two weeks.
Other symptoms of depression are also present, which may include:
- decrease in concentration;
- pathological guilt or low self-esteem;
- lack of faith in the future;
- thoughts of death or suicide;
- sleep disorders;
- changes in appetite or body weight;
- feeling of extreme fatigue or loss of strength.
Depression can make it difficult for a person to function in all areas of life, including socializing with others, at home, at work, and at school.
Depending on the number and severity of symptoms, as well as their impact on a person's daily life, a distinction is made between mild, moderate and severe depressive episodes.
There are several types of depressive episodes:
- a single depressive episode, i.e. the first and only depressive episode in a person's life;
- recurrent depressive disorder, i.e. a history of at least two depressive episodes; and
- bipolar disorder, in which depressive episodes alternate with phases of manic symptoms, including euphoria or irritability, hyperactivity or bursts of energy, and other manifestations such as wordy speech, "jumping ideas", inflated self-esteem, decreased sleep duration, distractibility and impulsive reckless behavior.
Risk factors and prevention
Depression results from a complex interplay of social, psychological and biological factors. An increased risk of developing depression is observed in people who have experienced life shocks (eg, unemployment, loss of a loved one, psychological trauma). Depression, in turn, can lead to increased levels of stress and functional impairment, which only aggravates the life of the patient and, as a result, depression itself.
Depression is closely related to and dependent on physical health. It is known that many of the factors that influence depression (such as lack of physical activity or alcohol abuse) are also risk factors for cardiovascular, oncological and respiratory diseases and diabetes. The difficulties caused by the presence of such diseases can also lead to depression in people suffering from them.
Prevention programs have been shown to reduce the prevalence of depression. Effective forms of preventive work with the population to prevent depression include school programs to develop skills for constructive overcoming of difficulties in children and adolescents. Working with parents of children with behavioral problems can help reduce depressive symptoms in parents and improve the condition of their children. Programs to increase the level of physical activity among older people also contribute to effective prevention of depression.
Diagnosis and treatment
There are a number of effective treatments for depression. These include psychological and medical methods. If you are experiencing symptoms of depression, seek help.
Depression is primarily treated with psychological methods. For moderate to severe depression, they can be combined with antidepressants. Mild depression does not require antidepressants.
Psychological treatments help develop new patterns of thinking, coping and communicating with others. These may include talking therapy, which is carried out by a specialist or lay therapist under the supervision of a specialist. Talk therapy sessions can be done in person or online. Self-help guides, websites and mobile apps can be used to learn psychological treatments.
Effective psychological treatments for depression include:
- behavioral activation;
- cognitive behavioral therapy;
- interpersonal psychotherapy;
- problem-solving therapy.
Antidepressants include selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine.
Health care providers should consider possible adverse side effects of antidepressants, options for psychological or medical treatment (availability of skilled professionals and/or accessibility of therapy to the patient), and individual patient preferences.
Antidepressants should not be used to treat depression in children or considered as first-line therapy in adolescents, in whom antidepressants should be given with extreme caution.
Other drugs and treatments are used to treat bipolar disorder.
Self-help
Self-help often helps to effectively control symptoms of depression and generally improves psychological well-being.
Things you can do yourself:
- try to continue activities that used to be enjoyable;
- stay in touch with friends and relatives;
- maintain regular physical activity, even if only in the form of short walks;
- observe diet and sleep as much as possible;
- give up or cut down on alcohol and not use illicit drugs as this can make depression worse;
- talk about your feelings to people you trust;
- seek medical advice.
If you have suicidal thoughts:
- remember that you are not alone and that many other people who have received help have had similar feelings;
- share your thoughts and feelings with people you trust;
- talk to a healthcare professional such as a doctor or counselor;
- join a support group.
If you feel you are in imminent danger of harming yourself, contact any emergency or crisis line available to you.
WHO action
WHO Mental Health Action Plan 2013–2030 outlines the necessary measures to organize appropriate care for people suffering from mental health disorders, including depression.
Depression, along with self-harm/suicide, is a priority disease in the WHO Mental Health Gap Action Program (mhGAP). The goal of the program is to help countries scale up services for people with mental, neurological and substance use disorders by involving non-psychiatric health professionals in their care.
WHO has developed brief guidelines for the provision of psychosocial support by lay therapists in individual or group therapy. An example is the Handbook Problem Management Plus (PM+), which contains information on techniques such as behavioral activation, stress management, problem management and strengthening social support. In addition, Group Interpersonal Therapy (IPT) for Depression describes how to treat depression in groups. Finally, Healthy Thinking covers the use of cognitive behavioral therapy in the treatment of perinatal depression.
Bibliography
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx) - English (accessed March 4, 2023)
- Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Discord. 2017;219:86–92.
- Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, et al.