Treatment for cptsd
Symptoms, Tests, Treatment, and Finding Support
Complex post-traumatic stress disorder (CPTSD) is closely related to post-traumatic stress disorder (PTSD). However, it usually develops due to repeated trauma over months or years rather than a single event.
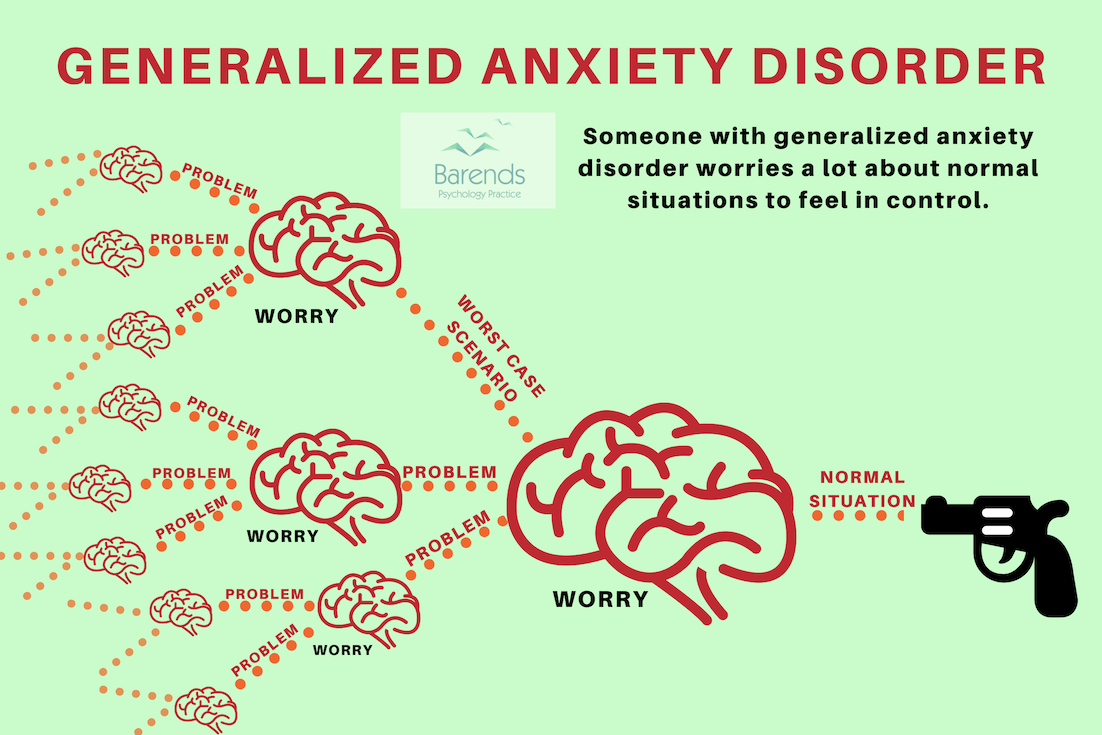
Most people are familiar with PTSD, an anxiety disorder that results from a traumatic event, such as a natural disaster or car accident.
However, a similar condition called CPTSD is becoming more widely recognized by doctors in recent years. Read on to earn more about the symptoms, causes, differences from PTSD, diagnosis, treatment, and more.
The symptoms of CPTSD usually include those of PTSD, plus an additional set of symptoms.
Symptoms of PTSD
Reliving the traumatic experience
This can include having nightmares or flashbacks.
Avoiding certain situations
You might avoid situations or activities, such as large crowds or driving, that remind you of the traumatic event. This also includes keeping yourself preoccupied to avoid thinking about the event.
Changes in beliefs and feelings about yourself and others
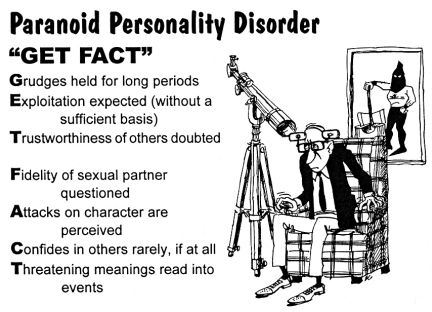
This can include avoiding relationships with other people, not being able to trust others, or believing the world is very dangerous.
Hyperarousal
Hyperarousal refers to constantly being on-alert or jittery. For example, you might have a hard time sleeping or concentrating. You might also be unusually startled by loud or unexpected noises.
Somatic symptoms
These refer to physical symptoms that don’t have any underlying medical cause. For example, when something reminds you of the traumatic event, you might feel dizzy or nauseated.
Symptoms of CPTSD
People with CPTSD typically have the above PTSD symptoms along with additional symptoms, including:
Lack of emotional regulation
This refers to having uncontrollable feelings, such as explosive anger or ongoing sadness.
Changes in consciousness
This can include forgetting the traumatic event or feeling detached from your emotions or body, which is also called dissociation.
Negative self-perception
You may feel guilt or shame, to the point that you feel completely different from other people.
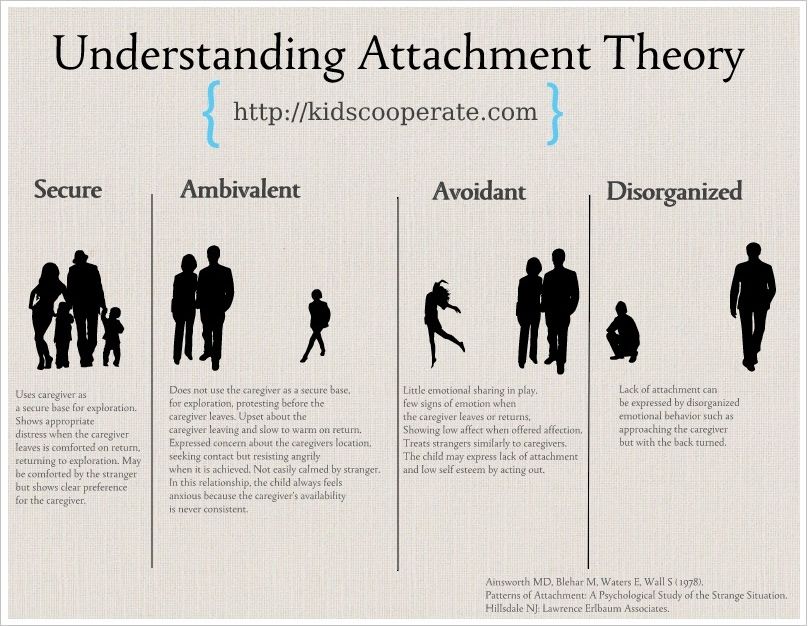
Difficulty with relationships
You might find yourself avoiding relationships with other people out of mistrust or a feeling of not knowing how to interact with others. On the other hand, some might seek relationships with people who harm them because it feels familiar.
Distorted perception of abuser
This includes becoming preoccupied with the relationship between you and your abuser. It can also include preoccupation with revenge or giving your abuser complete power over your life.
Loss of systems of meanings
Systems of meaning refer to your religion or beliefs about the world. For example, you might lose faith in some long-held beliefs you had or develop a strong sense of despair or hopelessness about the world.
It’s important to note that symptoms of both PTSD and CPTSD can vary widely between people, and even within one person over time. For example, you might find yourself avoiding social situations for a period of time, only to start seeking potentially dangerous situations months or years later.
For example, you might find yourself avoiding social situations for a period of time, only to start seeking potentially dangerous situations months or years later.
If you’re close to someone with CPTSD, it’s also important to remember that their thoughts and beliefs might not always match up with their emotions. They might know that, logically, they should avoid their abuser. However, they might also hold onto a sense of affection toward them.
Researchers are still trying to figure out exactly how traumatic stress affects the brain and leads to conditions like CPTSD. However, studies on animals suggest that trauma can have lasting effects on the amygdala, hippocampus, and prefrontal cortex. These areas play a big role in both our memory function and how we respond to stressful situations.
Any type of long-term trauma, over several months or years, can lead to CPTSD. However, it seems to appear frequently in people who’ve been abused by someone who was supposed to be their caregiver or protector. Examples include survivors of human trafficking or ongoing childhood sexual abuse by a relative.
Examples include survivors of human trafficking or ongoing childhood sexual abuse by a relative.
Other examples of long-term trauma include:
- ongoing physical, emotional, or sexual abuse
- being a prisoner of war
- living in an area of war for long periods of time
- ongoing childhood neglect
While anyone can develop CPTSD, some people may be more likely to develop it than others. Aside from having past traumatic experiences, risk factors include:
- underlying mental illness, such as anxiety or depression, or a family history of it
- inherited personality traits, which is often referred to as temperament
- how your brain regulates hormones and neurochemicals, especially in response to stress
- lifestyle factors, such as not having a strong support system or having a dangerous job
CPTSD is still a relatively new condition, so some doctors aren’t aware of it. This can make it hard to get an official diagnosis, and you might be diagnosed with PTSD instead of CPTSD. There’s no specific test for determining whether you have CPTSD, but keeping a detailed log of your symptoms can help your doctor make a more accurate diagnosis. Try to keep track of when your symptoms started as well as any changes in them over time.
There’s no specific test for determining whether you have CPTSD, but keeping a detailed log of your symptoms can help your doctor make a more accurate diagnosis. Try to keep track of when your symptoms started as well as any changes in them over time.
Once you find a doctor, they’ll start by asking about your symptoms, as well as any traumatic events in your past. For the initial diagnosis, you likely won’t need to go into too much detail if it makes you uncomfortable.
Next, they may ask about any family history of mental illness or other risk factors. Make sure to tell them about any medications or supplements you take, as well as any recreational drugs you use. Try to be as honest as you can with them so they can make the best recommendations for you.
If you’ve had symptoms of post-traumatic stress for at least a month and they interfere with your daily life, your doctor will likely start with a diagnosis of PTSD. Depending on the traumatic event and whether you have additional symptoms, such as ongoing relationship problems or trouble controlling your emotions, they may diagnose you with CPTSD.
Keep in mind that you may need to see a few doctors before you find someone you feel comfortable with. This is very normal, especially for people dealing with post-traumatic stress.
There are several treatment options for CPTSD that can both reduce your symptoms and help you better manage them.
Psychotherapy
Psychotherapy involves talking with a therapist either alone or in a group. It also includes the use of cognitive behavioral therapy (CBT). This type of treatment helps you identify negative thought patterns and gives you tools to replace them with more healthy, positive thoughts.
Your doctor might also recommend dialectical behavioral therapy, a type of CBT that helps you better respond to stress and build stronger relationships with others.
Eye movement desensitization and reprocessing (EMDR)
EMDR is commonly used to treat PTSD, and it can be helpful for CPTSD as well. You’ll be asked to briefly think about a traumatic moment while moving your eyes from side to side. Other techniques include having someone tap on your hands instead of moving your eyes. Over time, this process may help to desensitize you to traumatic memories and thoughts.
Other techniques include having someone tap on your hands instead of moving your eyes. Over time, this process may help to desensitize you to traumatic memories and thoughts.
While there’s some debate within the medical community over its use, the American Psychological Association conditionally recommends it for PTSD. This means that they recommend it but additional information is still needed due to insufficient evidence.
Medication
Medications traditionally used to treat depression can also help with symptoms of CPTSD. They tend to work best when combined with another form of treatment, such as CBT. Common antidepressants used for CPTSD may include:
- sertraline (Zoloft)
- paroxetine (Paxil)
- fluoxetine (Prozac)
While some people benefit from using these medications long term, you may only need to take them for a short period of time while you learn new coping strategies.
Having an under-recognized condition like CPTSD can be isolating. If you feel like you need some extra support, the National Center for PTSD has several resources, including a PTSD coaching app for your phone. While many of these resources are geared toward people with PTSD, you may still find them helpful for many of your symptoms.
If you feel like you need some extra support, the National Center for PTSD has several resources, including a PTSD coaching app for your phone. While many of these resources are geared toward people with PTSD, you may still find them helpful for many of your symptoms.
The nonprofit organization Out of the Storm also has many online resources, including a forum, information sheets, and book recommendations, specifically for CPTSD.
Suggested reads
- “The Body Keeps Score” is considered a must-read for anyone recovering from trauma.
- “The Complex PTSD Workbook” contains exercises and examples designed to empower you to take control of your physical and mental health.
- “Complex PTSD: From Surviving to Thriving” is a great resource for breaking down complex psychological concepts related to trauma. Plus, the author is a licensed psychotherapist who happens to have CPTSD.
Was this helpful?
CPTSD is a serious mental health condition that can take some time to treat, and for many people, it’s a lifelong condition. However, a combination of therapy and medication can help you manage your symptoms and significantly improve your quality of life.
However, a combination of therapy and medication can help you manage your symptoms and significantly improve your quality of life.
If starting treatment sounds overwhelming, consider joining a support group — either in person or online, first. Sharing your experience with people in similar situations is often the first step toward recovery.
Symptoms, Tests, Treatment, and Finding Support
Complex post-traumatic stress disorder (CPTSD) is closely related to post-traumatic stress disorder (PTSD). However, it usually develops due to repeated trauma over months or years rather than a single event.
Most people are familiar with PTSD, an anxiety disorder that results from a traumatic event, such as a natural disaster or car accident.
However, a similar condition called CPTSD is becoming more widely recognized by doctors in recent years. Read on to earn more about the symptoms, causes, differences from PTSD, diagnosis, treatment, and more.
The symptoms of CPTSD usually include those of PTSD, plus an additional set of symptoms.
Symptoms of PTSD
Reliving the traumatic experience
This can include having nightmares or flashbacks.
Avoiding certain situations
You might avoid situations or activities, such as large crowds or driving, that remind you of the traumatic event. This also includes keeping yourself preoccupied to avoid thinking about the event.
Changes in beliefs and feelings about yourself and others
This can include avoiding relationships with other people, not being able to trust others, or believing the world is very dangerous.
Hyperarousal
Hyperarousal refers to constantly being on-alert or jittery. For example, you might have a hard time sleeping or concentrating. You might also be unusually startled by loud or unexpected noises.
Somatic symptoms
These refer to physical symptoms that don’t have any underlying medical cause. For example, when something reminds you of the traumatic event, you might feel dizzy or nauseated.
Symptoms of CPTSD
People with CPTSD typically have the above PTSD symptoms along with additional symptoms, including:
Lack of emotional regulation
This refers to having uncontrollable feelings, such as explosive anger or ongoing sadness.
Changes in consciousness
This can include forgetting the traumatic event or feeling detached from your emotions or body, which is also called dissociation.
Negative self-perception
You may feel guilt or shame, to the point that you feel completely different from other people.
Difficulty with relationships
You might find yourself avoiding relationships with other people out of mistrust or a feeling of not knowing how to interact with others. On the other hand, some might seek relationships with people who harm them because it feels familiar.
Distorted perception of abuser
This includes becoming preoccupied with the relationship between you and your abuser. It can also include preoccupation with revenge or giving your abuser complete power over your life.
Loss of systems of meanings
Systems of meaning refer to your religion or beliefs about the world. For example, you might lose faith in some long-held beliefs you had or develop a strong sense of despair or hopelessness about the world.
It’s important to note that symptoms of both PTSD and CPTSD can vary widely between people, and even within one person over time. For example, you might find yourself avoiding social situations for a period of time, only to start seeking potentially dangerous situations months or years later.
If you’re close to someone with CPTSD, it’s also important to remember that their thoughts and beliefs might not always match up with their emotions. They might know that, logically, they should avoid their abuser. However, they might also hold onto a sense of affection toward them.
Researchers are still trying to figure out exactly how traumatic stress affects the brain and leads to conditions like CPTSD. However, studies on animals suggest that trauma can have lasting effects on the amygdala, hippocampus, and prefrontal cortex. These areas play a big role in both our memory function and how we respond to stressful situations.
Any type of long-term trauma, over several months or years, can lead to CPTSD. However, it seems to appear frequently in people who’ve been abused by someone who was supposed to be their caregiver or protector. Examples include survivors of human trafficking or ongoing childhood sexual abuse by a relative.
However, it seems to appear frequently in people who’ve been abused by someone who was supposed to be their caregiver or protector. Examples include survivors of human trafficking or ongoing childhood sexual abuse by a relative.
Other examples of long-term trauma include:
- ongoing physical, emotional, or sexual abuse
- being a prisoner of war
- living in an area of war for long periods of time
- ongoing childhood neglect
While anyone can develop CPTSD, some people may be more likely to develop it than others. Aside from having past traumatic experiences, risk factors include:
- underlying mental illness, such as anxiety or depression, or a family history of it
- inherited personality traits, which is often referred to as temperament
- how your brain regulates hormones and neurochemicals, especially in response to stress
- lifestyle factors, such as not having a strong support system or having a dangerous job
CPTSD is still a relatively new condition, so some doctors aren’t aware of it. This can make it hard to get an official diagnosis, and you might be diagnosed with PTSD instead of CPTSD. There’s no specific test for determining whether you have CPTSD, but keeping a detailed log of your symptoms can help your doctor make a more accurate diagnosis. Try to keep track of when your symptoms started as well as any changes in them over time.
This can make it hard to get an official diagnosis, and you might be diagnosed with PTSD instead of CPTSD. There’s no specific test for determining whether you have CPTSD, but keeping a detailed log of your symptoms can help your doctor make a more accurate diagnosis. Try to keep track of when your symptoms started as well as any changes in them over time.
Once you find a doctor, they’ll start by asking about your symptoms, as well as any traumatic events in your past. For the initial diagnosis, you likely won’t need to go into too much detail if it makes you uncomfortable.
Next, they may ask about any family history of mental illness or other risk factors. Make sure to tell them about any medications or supplements you take, as well as any recreational drugs you use. Try to be as honest as you can with them so they can make the best recommendations for you.
If you’ve had symptoms of post-traumatic stress for at least a month and they interfere with your daily life, your doctor will likely start with a diagnosis of PTSD. Depending on the traumatic event and whether you have additional symptoms, such as ongoing relationship problems or trouble controlling your emotions, they may diagnose you with CPTSD.
Depending on the traumatic event and whether you have additional symptoms, such as ongoing relationship problems or trouble controlling your emotions, they may diagnose you with CPTSD.
Keep in mind that you may need to see a few doctors before you find someone you feel comfortable with. This is very normal, especially for people dealing with post-traumatic stress.
There are several treatment options for CPTSD that can both reduce your symptoms and help you better manage them.
Psychotherapy
Psychotherapy involves talking with a therapist either alone or in a group. It also includes the use of cognitive behavioral therapy (CBT). This type of treatment helps you identify negative thought patterns and gives you tools to replace them with more healthy, positive thoughts.
Your doctor might also recommend dialectical behavioral therapy, a type of CBT that helps you better respond to stress and build stronger relationships with others.
Eye movement desensitization and reprocessing (EMDR)
EMDR is commonly used to treat PTSD, and it can be helpful for CPTSD as well. You’ll be asked to briefly think about a traumatic moment while moving your eyes from side to side. Other techniques include having someone tap on your hands instead of moving your eyes. Over time, this process may help to desensitize you to traumatic memories and thoughts.
You’ll be asked to briefly think about a traumatic moment while moving your eyes from side to side. Other techniques include having someone tap on your hands instead of moving your eyes. Over time, this process may help to desensitize you to traumatic memories and thoughts.
While there’s some debate within the medical community over its use, the American Psychological Association conditionally recommends it for PTSD. This means that they recommend it but additional information is still needed due to insufficient evidence.
Medication
Medications traditionally used to treat depression can also help with symptoms of CPTSD. They tend to work best when combined with another form of treatment, such as CBT. Common antidepressants used for CPTSD may include:
- sertraline (Zoloft)
- paroxetine (Paxil)
- fluoxetine (Prozac)
While some people benefit from using these medications long term, you may only need to take them for a short period of time while you learn new coping strategies.
Having an under-recognized condition like CPTSD can be isolating. If you feel like you need some extra support, the National Center for PTSD has several resources, including a PTSD coaching app for your phone. While many of these resources are geared toward people with PTSD, you may still find them helpful for many of your symptoms.
The nonprofit organization Out of the Storm also has many online resources, including a forum, information sheets, and book recommendations, specifically for CPTSD.
Suggested reads
- “The Body Keeps Score” is considered a must-read for anyone recovering from trauma.
- “The Complex PTSD Workbook” contains exercises and examples designed to empower you to take control of your physical and mental health.
- “Complex PTSD: From Surviving to Thriving” is a great resource for breaking down complex psychological concepts related to trauma. Plus, the author is a licensed psychotherapist who happens to have CPTSD.
Was this helpful?
CPTSD is a serious mental health condition that can take some time to treat, and for many people, it’s a lifelong condition. However, a combination of therapy and medication can help you manage your symptoms and significantly improve your quality of life.
However, a combination of therapy and medication can help you manage your symptoms and significantly improve your quality of life.
If starting treatment sounds overwhelming, consider joining a support group — either in person or online, first. Sharing your experience with people in similar situations is often the first step toward recovery.
How to work with Hyde. Assholes under control
If you suspect that you have a Mr. Hyde at work and want to help him, be frank and considerate. Be open about your suspicions. The best time to talk is right after a substance abuse incident. As was the case with Miles. You will most likely hear apologies and evasive responses. But this does not mean that you should not find out from a colleague what happened. Let him express his point of view. It is likely that Hyde will not agree with the claims, but he may later turn to you for help if the comments were made in a polite manner. Denying his guilt, Hyde feels deep shame. He often needs the advice of someone who will not condemn him. Even if the conversation upset him, after a while this method can give results. Even the most sincere sympathy can be perceived with hostility at first. But remember that Hyde's changes, like any other person, depend on how much he is interested in them.
Even if the conversation upset him, after a while this method can give results. Even the most sincere sympathy can be perceived with hostility at first. But remember that Hyde's changes, like any other person, depend on how much he is interested in them.
It's great if you can get the employee involved in a conversation about drug use in order to explain to him the need to change the situation 109 . However, in the workplace, such conversations should primarily concern the performance of official duties, and not the fact of addiction itself. It is important to emphasize how Hyde's habit is reflected in the performance. Be persistent and use comparisons to previous successes to emphasize the need for treatment. In the hands of a leader, this is a particularly effective technique. While the drugs do tremendous damage to Mr. Hyde and ruin his life, this may not seem as obvious to him as it is to you. Try to convince him that he needs to correct his behavior. And don't forget to say that you are ready to help. Tell me how to find the right treatment, the right rehabilitation program, a consultation, or just sincerely support and inspire the employee. Do not miss the opportunity to involve Hyde himself in the support process.
Tell me how to find the right treatment, the right rehabilitation program, a consultation, or just sincerely support and inspire the employee. Do not miss the opportunity to involve Hyde himself in the support process.
Some companies have a strong anti-drug policy that identifies signs of abuse. In such cases, according to the contract, control tests for the content of alcohol and drugs are allowed. Employees are required to participate in rehabilitation programs or sign a bilateral agreement that allows unscheduled tests. This is one of the conditions for maintaining a job. The contract also spells out the consequences that will arise in case of repeated use. Of course, such a policy should not go against the law and must be agreed with the personnel department.
Be prepared that you are unlikely to be able to remain calm, because on the part of Hyde you will find pretense, lies and distortion of facts. Remember: his ability to mislead is so effective that he even convinces himself that there are no problems. He will deal with you too. Hyde is possessed by a strong desire to continue using or return to it. And it's not his own choice. You will have to be persistent, set boundaries and explain all the consequences. Record conversations and don't forget to make sure they are clear to the employee. Hyde needs strict agreements about not using drugs, but also about visits, lateness and late departures from work. Sometimes the limits must be stricter than for the rest of the employees. Contractual obligations regarding alcohol and drug testing, as opposed to spontaneous measures, will help to avoid lies and manipulation during treatment.
He will deal with you too. Hyde is possessed by a strong desire to continue using or return to it. And it's not his own choice. You will have to be persistent, set boundaries and explain all the consequences. Record conversations and don't forget to make sure they are clear to the employee. Hyde needs strict agreements about not using drugs, but also about visits, lateness and late departures from work. Sometimes the limits must be stricter than for the rest of the employees. Contractual obligations regarding alcohol and drug testing, as opposed to spontaneous measures, will help to avoid lies and manipulation during treatment.
If you are an employer, you can use leverage to help Hyde recognize the need to seek help 147 . Make it clear that there is a risk of losing your job. Approximately 50% of those seeking psychological help are addicted to drugs or alcohol 139 . However, many of them want to overcome anxiety or depression rather than get rid of addiction. It is precisely because of the refusal to acknowledge its negative consequences that it is difficult to convince Hyde of the need to fight it. There are many effective methods. And the best time to start using them is when the addiction becomes known at work. The desire to save a place is a great motivation 90 .
It is precisely because of the refusal to acknowledge its negative consequences that it is difficult to convince Hyde of the need to fight it. There are many effective methods. And the best time to start using them is when the addiction becomes known at work. The desire to save a place is a great motivation 90 .
There are many programs and treatments available: drug therapy, the Twelve Step Program, Alcoholics Anonymous communities, special programs for working addicts, individual or group therapy, and inpatient care. Everything depends on the specific case. Some people benefit from various relaxation techniques, acupuncture or hypnosis. It is important to remember that it is not always possible to quickly overcome addiction without medical intervention. Addicts experience withdrawal symptoms or even die from withdrawal symptoms in cases of alcohol or an anti-anxiety drug called Xanax. Drugs such as methadone and suboxone help to cope with drug addiction and keep working capacity. In some cases, even people who take them without much enthusiasm, there are significant improvements, but subject to reasonable use under the supervision of a physician.
In some cases, even people who take them without much enthusiasm, there are significant improvements, but subject to reasonable use under the supervision of a physician.
Many people experience relapses during drug withdrawal. During such periods, people try to avoid negative emotions and experience increased social pressure. Usually breakdowns are associated with holidays, vacations, travel or difficult experiences: the loss of a loved one, divorce, dismissal 109 . Another reason a relapse may occur is the removal of barriers, such as close supervision at work 130 . Even a fleeting breakdown can quickly return Mister Hyde to a state of addiction. Realizing what they have done, such people, as a rule, plunge into depression.
In conclusion, I want to say something important about preventing such situations. It is very useful to have a clearly defined anti-alcohol and anti-drug policy in the company that is consistent with the environment in the team and local legislation. Drug and alcohol testing does not necessarily lead to reduced use or increased productivity 46, 105 . It may be more beneficial to reduce stress levels in the office through educational courses, psychological support, and peer-to-peer programs. Also pay special attention to the health of employees and try to prevent cases of harassment and violence.
Drug and alcohol testing does not necessarily lead to reduced use or increased productivity 46, 105 . It may be more beneficial to reduce stress levels in the office through educational courses, psychological support, and peer-to-peer programs. Also pay special attention to the health of employees and try to prevent cases of harassment and violence.
The healing power of plants
How many women suffer from PMS?
Just yesterday you were cheerful and friendly, but today, instead of a friendly young lady, Mr. Hyde in a skirt looked out of the mirror. Who doesn't happen to? It happens to many, and quite regularly: once a month. You just have premenstrual syndrome (PMS).
Recent studies indicate a high prevalence of premenstrual syndrome. According to scientists, it is observed in almost 90% women. The first sign of PMS is sudden mood swings. At this time, for no apparent reason, some women begin to be overcome by panic horror, someone cannot concentrate on anything, it becomes extremely difficult for others to control their emotions - be it anger or tears.
At this time, for no apparent reason, some women begin to be overcome by panic horror, someone cannot concentrate on anything, it becomes extremely difficult for others to control their emotions - be it anger or tears.
Who gets PMS more often?
Physiological symptoms during PMS include headaches, swelling, pain in muscles, joints and chest, tachycardia, lethargy and apathy, weight gain, general weakness and an increased need for sweets.
An interesting fact - according to American scientists, overweight women suffer from PMS first of all - they often eat foods high in sugar and starch. Women who quickly gain or lose more than 10 kg are also at risk of PMS, and, oddly enough, women who are constantly dieting.
PMS symptoms
PMS symptoms appear 7-14 days before menstruation and continue until the onset of bleeding. In the same woman, the symptoms change little from year to year. And that's not all: if PMS is left unattended (regular pain medication does not count), then over the years, the discomfort before menstruation will only increase. Therefore, in order to meet the upcoming hormonal changes fully armed and cope with them unnoticed by others, without turning their lives into hell, you can prepare in advance for PMS. It's much better to manage the "bad" days than just trying to forget about them.
Therefore, in order to meet the upcoming hormonal changes fully armed and cope with them unnoticed by others, without turning their lives into hell, you can prepare in advance for PMS. It's much better to manage the "bad" days than just trying to forget about them.
Mastodinon
In fact, any woman can cope with this problem, especially if you listen to nature and use its gifts. Since ancient times, people have used the power of medicinal plants to treat various diseases. And nowadays it is absolutely not necessary to swallow a handful of pills for premenstrual ailments - it is enough to take the natural non-hormonal drug Mastodinon. It is produced by a German pharmaceutical company that develops and manufactures the latest generation of highly effective herbal medicines.
Ingredients of Mastodinon
Mastodinon contains six medicinal plants, each of which has its own beneficial effect on the female body. This innovative drug gently restores the natural balance of hormones, eliminates pain, prevents the development of pathological processes in the mammary glands and reduces the irritability and anxiety associated with PMS. "Mastodinon" does not allow unpleasant symptoms to spoil a woman's five years of life - that's how much time, according to statistics, each of us spends in a state of PMS. So your health and good mood are in your hands!
"Mastodinon" does not allow unpleasant symptoms to spoil a woman's five years of life - that's how much time, according to statistics, each of us spends in a state of PMS. So your health and good mood are in your hands!
References
- Muniandy K., Gothai S., Arulselvan P., Kumar SS., Norhaizan ME., Umamaheswari A., Fakurazi S. Mini Review: Wound healing potential of edible plants. // Pak J Pharm Sci - 2019 - Vol32 - N2 - p.703-707; PMID:31081786
- Jin C., Liu D., Shao A., Zhao X., Yang L., Fan F., Yu K., Lin R., Huang J., Ding C. Study on healing technique for weak interlayer and related mechanical properties based on microbially-induced calcium carbonate precipitation. // PLoS One - 2018 - Vol13 - N9- p.e0203834; PMID:30212556
- Tironi M. Hypo-interventions: Intimate activism in toxic environments. // Soc Stud Sci - 2018 - Vol48 - N3 - p.438-455; PMID:29963978
- Haque M., Chowdhury ABMA., Shahjahan M., Harun MGD. Traditional healing practices in rural Bangladesh: a qualitative investigation.
 // BMC Complement Altern Med - 2018 - Vol18 - N1 - p.62; PMID:29448941
// BMC Complement Altern Med - 2018 - Vol18 - N1 - p.62; PMID:29448941 - Sharmila S., Kalaichelvi K., Dhivya SM., Premamalini P., Abirami P., Jayanthi G. Pharmacognostic Assesment of the Endemic and Vulnerable Medicinal Climber-Cayratia pedata (Lam.) Gagnep. var. glabra Gamble and Its Antibacterial Activity. // Pharmacognosy Res - 2017 - Vol9- NSuppl 1 - p.S27-S33; PMID:29333039
- Wubetu M., Abula T., Dejenu G. Ethnopharmacologic survey of medicinal plants used to treat human diseases by traditional medical practitioners in Dega Damot district, Amhara, Northwestern Ethiopia. // BMC Res Notes - 2017 - Vol10 - N1 - p.157; PMID:28420410
- Moalla Rekik D., Ben Khedir S., Ksouda Moalla K., Kammoun NG., Rebai T., Sahnoun Z. Evaluation of Wound Healing Properties of Grape Seed, Sesame, and Fenugreek Oils. // Evid Based Complement Alternat Med - 2016 - Vol2016 - NNULL - p.7965689; PMID:27990170
- Ramzan S., Soelberg J., Jäger AK., Cantarero-Arévalo L. Traditional medicine among people of Pakistani descent in the capital region of Copenhagen.