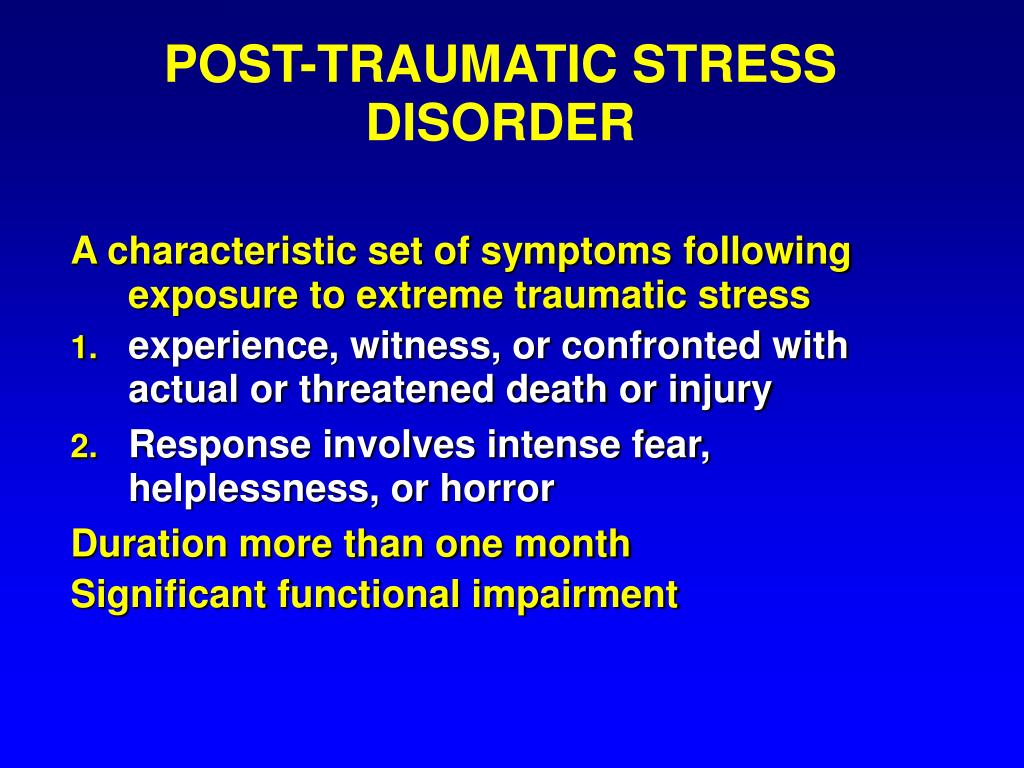
Symptoms of stress disorder
Post-traumatic stress disorder (PTSD) - Symptoms and causes
Overview
Post-traumatic stress disorder (PTSD) is a mental health condition that's triggered by a terrifying event — either experiencing it or witnessing it. Symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.
Most people who go through traumatic events may have temporary difficulty adjusting and coping, but with time and good self-care, they usually get better. If the symptoms get worse, last for months or even years, and interfere with your day-to-day functioning, you may have PTSD.
Getting effective treatment after PTSD symptoms develop can be critical to reduce symptoms and improve function.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Post-traumatic stress disorder symptoms may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. Symptoms can vary over time or vary from person to person.
Intrusive memories
Symptoms of intrusive memories may include:
- Recurrent, unwanted distressing memories of the traumatic event
- Reliving the traumatic event as if it were happening again (flashbacks)
- Upsetting dreams or nightmares about the traumatic event
- Severe emotional distress or physical reactions to something that reminds you of the traumatic event
Avoidance
Symptoms of avoidance may include:
- Trying to avoid thinking or talking about the traumatic event
- Avoiding places, activities or people that remind you of the traumatic event
Negative changes in thinking and mood
Symptoms of negative changes in thinking and mood may include:
- Negative thoughts about yourself, other people or the world
- Hopelessness about the future
- Memory problems, including not remembering important aspects of the traumatic event
- Difficulty maintaining close relationships
- Feeling detached from family and friends
- Lack of interest in activities you once enjoyed
- Difficulty experiencing positive emotions
- Feeling emotionally numb
Changes in physical and emotional reactions
Symptoms of changes in physical and emotional reactions (also called arousal symptoms) may include:
- Being easily startled or frightened
- Always being on guard for danger
- Self-destructive behavior, such as drinking too much or driving too fast
- Trouble sleeping
- Trouble concentrating
- Irritability, angry outbursts or aggressive behavior
- Overwhelming guilt or shame
For children 6 years old and younger, signs and symptoms may also include:
- Re-enacting the traumatic event or aspects of the traumatic event through play
- Frightening dreams that may or may not include aspects of the traumatic event
Intensity of symptoms
PTSD symptoms can vary in intensity over time. You may have more PTSD symptoms when you're stressed in general, or when you come across reminders of what you went through. For example, you may hear a car backfire and relive combat experiences. Or you may see a report on the news about a sexual assault and feel overcome by memories of your own assault.
You may have more PTSD symptoms when you're stressed in general, or when you come across reminders of what you went through. For example, you may hear a car backfire and relive combat experiences. Or you may see a report on the news about a sexual assault and feel overcome by memories of your own assault.
When to see a doctor
If you have disturbing thoughts and feelings about a traumatic event for more than a month, if they're severe, or if you feel you're having trouble getting your life back under control, talk to your doctor or a mental health professional. Getting treatment as soon as possible can help prevent PTSD symptoms from getting worse.
If you have suicidal thoughts
If you or someone you know has suicidal thoughts, get help right away through one or more of these resources:
- Reach out to a close friend or loved one.
- Contact a minister, a spiritual leader or someone in your faith community.
- Call a suicide hotline number — in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to reach a trained counselor.
 Use that same number and press 1 to reach the Veterans Crisis Line.
Use that same number and press 1 to reach the Veterans Crisis Line. - Make an appointment with your doctor or a mental health professional.
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 or your local emergency number immediately.
If you know someone who's in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person to keep him or her safe. Call 911 or your local emergency number immediately. Or, if you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
You can develop post-traumatic stress disorder when you go through, see or learn about an event involving actual or threatened death, serious injury or sexual violation.
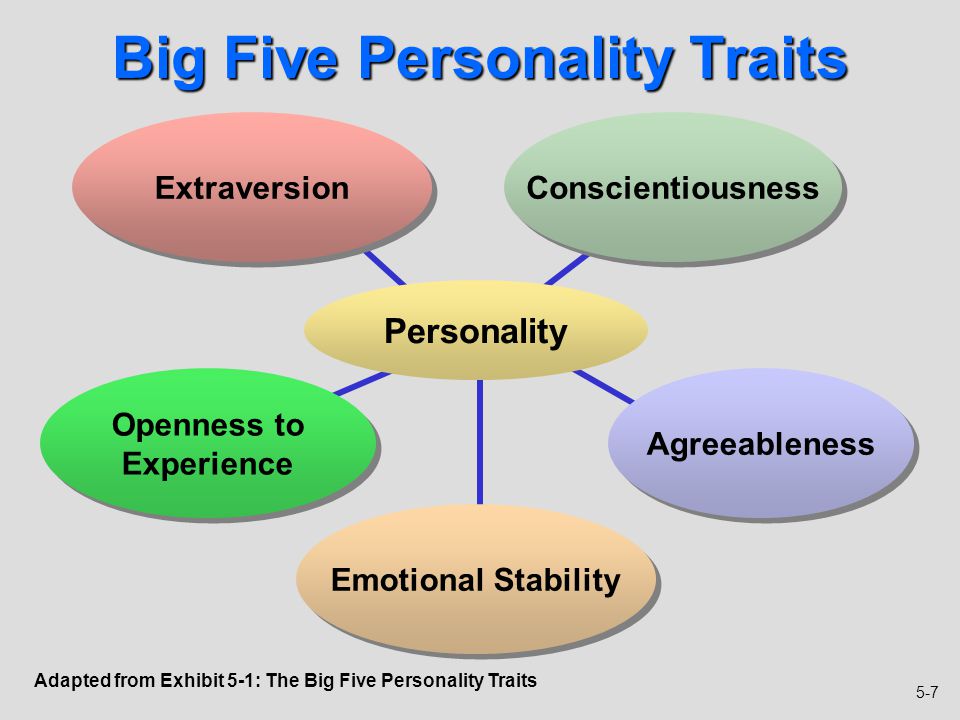
Doctors aren't sure why some people get PTSD. As with most mental health problems, PTSD is probably caused by a complex mix of:
- Stressful experiences, including the amount and severity of trauma you've gone through in your life
- Inherited mental health risks, such as a family history of anxiety and depression
- Inherited features of your personality — often called your temperament
- The way your brain regulates the chemicals and hormones your body releases in response to stress
Risk factors
People of all ages can have post-traumatic stress disorder. However, some factors may make you more likely to develop PTSD after a traumatic event, such as:
However, some factors may make you more likely to develop PTSD after a traumatic event, such as:
- Experiencing intense or long-lasting trauma
- Having experienced other trauma earlier in life, such as childhood abuse
- Having a job that increases your risk of being exposed to traumatic events, such as military personnel and first responders
- Having other mental health problems, such as anxiety or depression
- Having problems with substance misuse, such as excess drinking or drug use
- Lacking a good support system of family and friends
- Having blood relatives with mental health problems, including anxiety or depression
Kinds of traumatic events
The most common events leading to the development of PTSD include:
- Combat exposure
- Childhood physical abuse
- Sexual violence
- Physical assault
- Being threatened with a weapon
- An accident
Many other traumatic events also can lead to PTSD, such as fire, natural disaster, mugging, robbery, plane crash, torture, kidnapping, life-threatening medical diagnosis, terrorist attack, and other extreme or life-threatening events.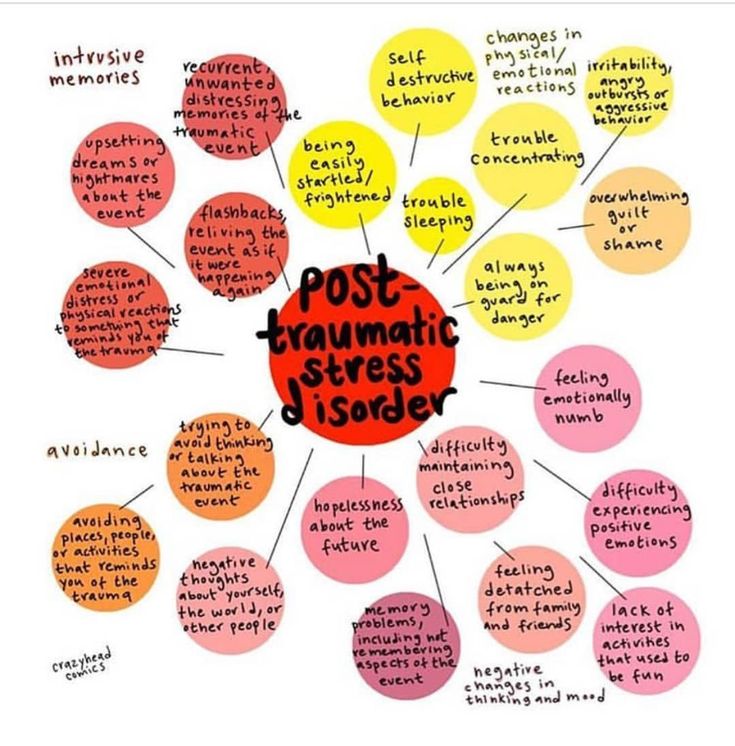
Complications
Post-traumatic stress disorder can disrupt your whole life ― your job, your relationships, your health and your enjoyment of everyday activities.
Having PTSD may also increase your risk of other mental health problems, such as:
- Depression and anxiety
- Issues with drugs or alcohol use
- Eating disorders
- Suicidal thoughts and actions
Prevention
After surviving a traumatic event, many people have PTSD-like symptoms at first, such as being unable to stop thinking about what's happened. Fear, anxiety, anger, depression, guilt — all are common reactions to trauma. However, the majority of people exposed to trauma do not develop long-term post-traumatic stress disorder.
Getting timely help and support may prevent normal stress reactions from getting worse and developing into PTSD. This may mean turning to family and friends who will listen and offer comfort. It may mean seeking out a mental health professional for a brief course of therapy.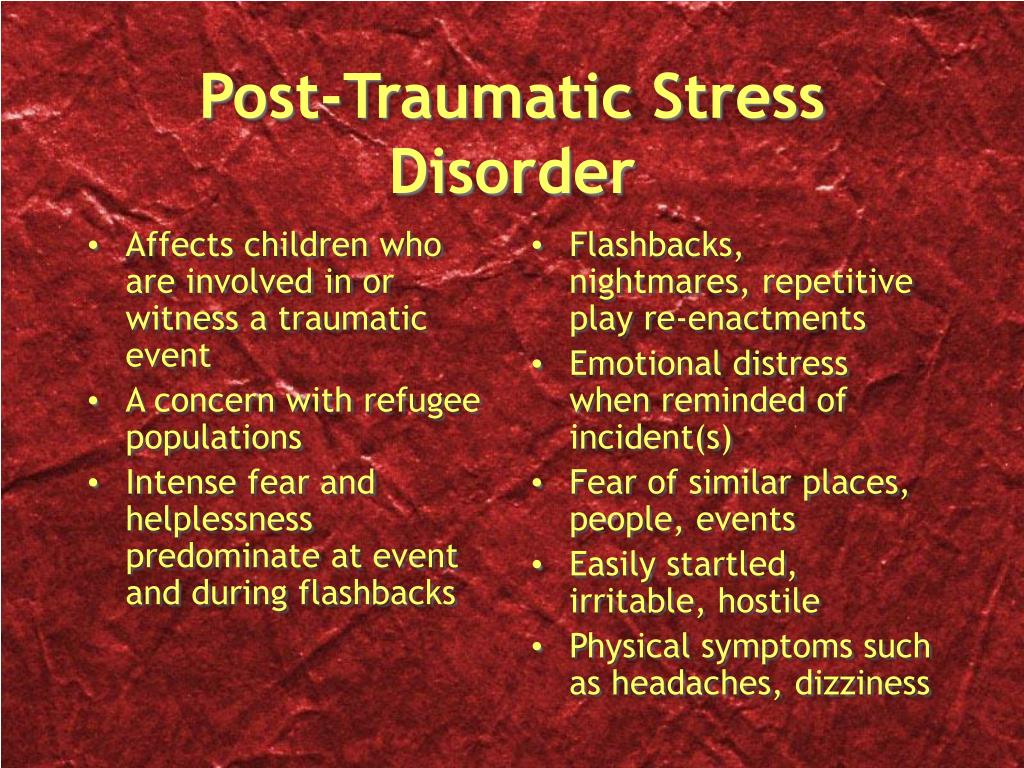 Some people may also find it helpful to turn to their faith community.
Some people may also find it helpful to turn to their faith community.
Support from others also may help prevent you from turning to unhealthy coping methods, such as misuse of alcohol or drugs.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Acute Stress Disorder: Causes, Symptoms, and Diagnosis
Acute stress disorder (ASD) typically occurs within one month of a traumatic event. Symptoms are similar to those seen in post traumatic stress disorder (PTSD), however this disorder is temporary, lasing from a few days to a month. Some people with this disorder can go on to develop PTSD.
What’s acute stress disorder?
In the weeks after a traumatic event, you may develop an anxiety disorder called acute stress disorder (ASD). ASD typically occurs within one month of a traumatic event. It lasts at least three days and can persist for up to one month. People with ASD have symptoms similar to those seen in post-traumatic stress disorder (PTSD).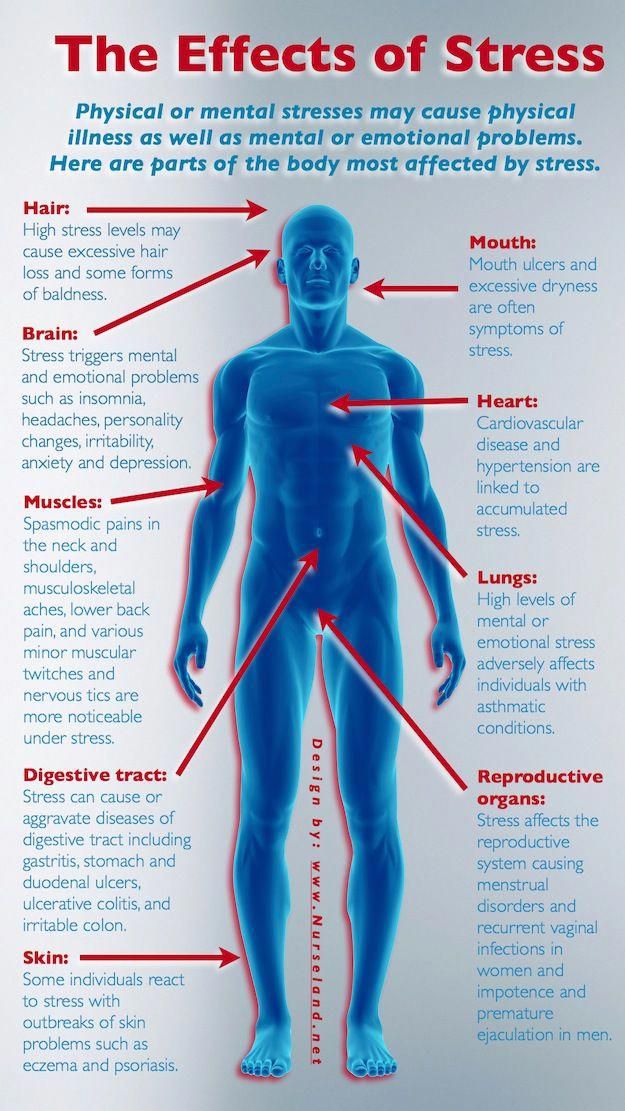
Experiencing, witnessing, or being confronted with one or more traumatic events can cause ASD. The events create intense fear, horror, or helplessness. Traumatic events that can cause ASD include a:
- death
- threat of death to oneself or others
- threat of serious injury to oneself or others
- threat to the physical integrity of oneself or others
Approximately 6 to 33 percent of people who experience a traumatic event develop ASD, according to the U.S. Department of Veterans Affairs. This rate varies based on the nature of the traumatic situation.
Anyone can develop ASD after a traumatic event. You may have an increased risk of developing ASD if you have:
- experienced, witnessed, or been confronted with a traumatic event in the past
- a history of ASD or PTSD
- a history of certain types of mental problems
- a history of dissociative symptoms during traumatic events
The symptoms of ASD include:
Dissociative symptoms
You’ll have three or more of the following dissociative symptoms if you have ASD:
- feeling numb, detached, or being emotionally unresponsive
- a reduced awareness of your surroundings
- derealization, which occurs when your environment seems strange or unreal to you
- depersonalization, which occurs when your thoughts or emotions don’t seem real or don’t seem like they belong to you
- dissociative amnesia, which occurs when you cannot remember one or more important aspects of the traumatic event
Reexperiencing the traumatic event
You’ll persistently re-experience the traumatic event in one or more of the following ways if you have ASD:
- having recurring images, thoughts, nightmares, illusions, or flashback episodes of the traumatic event
- feeling like you’re reliving the traumatic event
- feeling distressed when something reminds you of the traumatic event
Avoidance
You may avoid stimuli that cause you to remember or re-experience the traumatic event, such as:
- people
- conversations
- places
- objects
- activities
- thoughts
- feelings
Anxiety or increased arousal
The symptoms of ASD may include anxiety and increased arousal. The symptoms of anxiety and increased arousal include:
The symptoms of anxiety and increased arousal include:
- having trouble sleeping
- being irritable
- having difficulty concentrating
- being unable to stop moving or sit still
- being constantly tense or on guard
- becoming startled too easily or at inappropriate times
Distress
The symptoms of ASD may cause you distress or disrupt important aspects of your life, such as your social or work settings. You may have an inability to start or complete necessary tasks, or an inability to tell others about the traumatic event.
Your primary doctor or mental healthcare provider will diagnose ASD by asking you questions about the traumatic event and your symptoms. It’s also important to rule out other causes such as:
- drug abuse
- side effects of medications
- health problems
- other psychiatric disorders
If you don’t already have a primary care doctor or a mental healthcare professional, you can browse doctors in your area through the Healthline FindCare tool.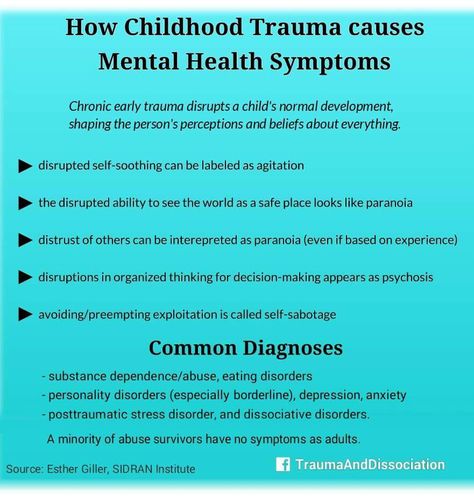
Your doctor may use one or more of the following methods to treat ASD:
- a psychiatric evaluation to determine your specific needs
- hospitalization if you’re at risk of suicide or harming others
- assistance in obtaining shelter, food, clothing, and locating family, if necessary
- psychiatric education to teach you about your disorder
- medication to relieve symptoms of ASD, such as antianxiety medications, selective serotonin reuptake inhibitors (SSRIs), and antidepressants
- cognitive behavioral therapy (CBT), which may increase recovery speed and prevent ASD from turning into PTSD
- exposure-based therapies
- hypnotherapy
Online therapy options
Read our review of the best online therapy options to find the right fit for you.
Many people with ASD are later diagnosed with PTSD. A diagnosis of PTSD is made if your symptoms persist for more than a month and cause a significant amount of stress and difficulty functioning.
Treatment may reduce your chances of developing PTSD. Approximately 50 percent of PTSD cases resolve within six months, whereas others may persist for years.
Because there’s no way to ensure that you never experience a traumatic situation, there’s no way to prevent ASD. However, there are things that can be done to reduce your likelihood of developing ASD.
Getting medical treatment within a few hours of experiencing a traumatic event may reduce the likelihood that you’ll develop ASD. People who work in jobs that carry a high risk for traumatic events, such as military personnel, may benefit from preparation training and counseling to reduce their risk of developing ASD or PSTD if a traumatic event does occur. Preparation training and counseling may involve fake enactments of traumatic events and counseling to strengthen coping mechanisms.
Post Traumatic Stress Disorder - Support and Treatment at EMC
Narrated by Head of Psychiatry and Psychotherapy Clinic,
psychiatrist, psychotherapist Natalya Rivkina
Every person inevitably finds himself in difficult situations during his life.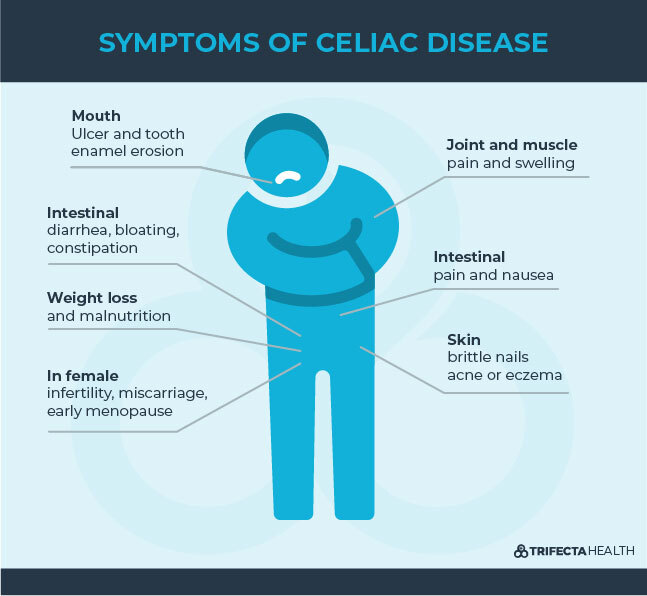 It can be stress at work, illness or loss of a loved one, a car accident. Often people in times of crisis, trying to support loved ones, forget about themselves, trying to cope with difficulties on their own.
It can be stress at work, illness or loss of a loved one, a car accident. Often people in times of crisis, trying to support loved ones, forget about themselves, trying to cope with difficulties on their own.
It is important to understand that the most severe reactions to stress develop not at the time of the traumatic event, but much later, after 3-5 months. For the patient, they may have nothing to do with the difficult events that he experienced. These conditions are called delayed stress responses.
How do delayed reactions to stress manifest themselves?
Symptoms of post-stress disorder are similar to those of depression or anxiety disorder and are characterized by:
-
fatigue,
-
anxiety,
-
panic attacks,
-
depressed mood,
-
sleep disorders,
-
anxiety, irritability,
-
feeling of apathy,
-
loss of the meaning of life, unwillingness to do the usual things.
The person may withdraw, stop communicating with friends and family. Sometimes people leave work, hobbies, break relationships with loved ones, because they do not see the point in them.
The reason is post-stress disorders, which can and should be treated.
What happens to a person at the moment of a traumatic event
In addition to delayed reactions to stress, there are conditions that people experience at the moment of trauma. At the time of difficult events, some people do not experience any feelings and emotions. This is one of the main reasons why they do not seek help. A person is in a state of dissociation, as if watching what is happening from the side, not being a participant in the events. It seems to him that the events are not happening to him. Often patients report that they do not cry, do not experience any emotions, act as if automatically. They feel like they are doing a good job on their own. In fact, the less emotionally a person reacts, the more acute reactions to stress he experiences. If the state of dissociation persists for several weeks, it is very important to consult with specialists in order to rule out pathological reactions to stress.
If the state of dissociation persists for several weeks, it is very important to consult with specialists in order to rule out pathological reactions to stress.
Natural and pathological reactions to stress
There are normal reactions to stress that everyone experiences.
-
The first 2-3 days after bad news or traumatic events, people experience shock, it seems to them that the events are not happening to them.
-
Shock is replaced by anger and anger. People are angry at themselves, at loved ones, at circumstances.
-
When they fully realize what has happened, people feel despair.
-
Then comes the stage of reintegration, when a person begins to build his life further.
Each of these stages has its own duration, but sometimes people can remain in a state of shock for years. Against this background, a person loses the meaning of life, relationships, falls into depression. Life can be ruined simply because the patient did not receive adequate support at the time the traumatic events occurred.
Young children and the elderly are most susceptible to developing pathological or delayed reactions to stress, including post-traumatic stress disorder. Often, in order to protect children or parents, family members withhold information from them. Ignorance makes people even more vulnerable. They may feel the tension associated with the secret, distrust on the part of relatives.
The more time passes from the moment of a severe event to the moment when a person learns about it, the higher the risk of post-traumatic stress disorder. If the family has small children and older people for whom you are concerned, it makes sense to consult a specialist. The doctor will teach you how to report difficult news correctly.
Methods for the treatment of post-stress conditions
The main help is psychotherapy. It is important to contact doctors who specialize in working with traumatic and post-stress conditions, because this is a separate area of \u200b\u200bpsychotherapy that requires special skills.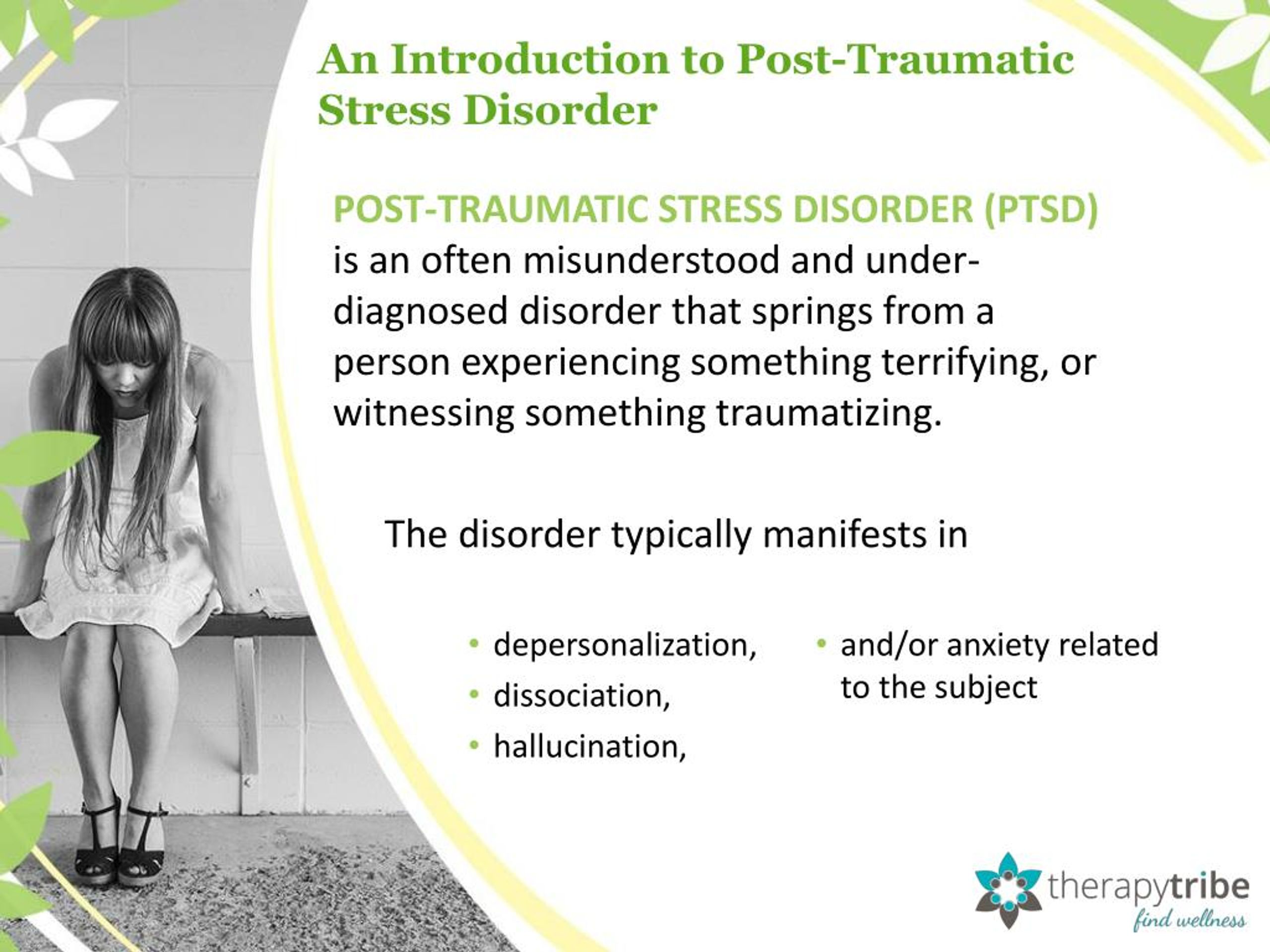 Natalya Rivkina works with post-stress conditions in children and adults at the EMC Clinic of Psychiatry and Psychotherapy in Moscow. She has specialization and extensive experience in this field.
Natalya Rivkina works with post-stress conditions in children and adults at the EMC Clinic of Psychiatry and Psychotherapy in Moscow. She has specialization and extensive experience in this field.
In case of acute reactions to stress, we try to avoid drug therapy. But if there are severe sleep disorders, high anxiety, we can prescribe antidepressants.
Important! At the stage of an acute reaction to stress, tranquilizers should not be taken. They can provoke the development of more severe conditions in the future. Unfortunately, most people have tranquilizers at home. If you have questions about the need for emergency medication, it is best to consult a psychiatrist so as not to harm a loved one.
The main goal of psychotherapy is to help the patient get through a difficult time, find resources and support that will help him adapt to current events and build his life on.
If a family loses a loved one, it is necessary to change the structure of the family, and sometimes the way of life.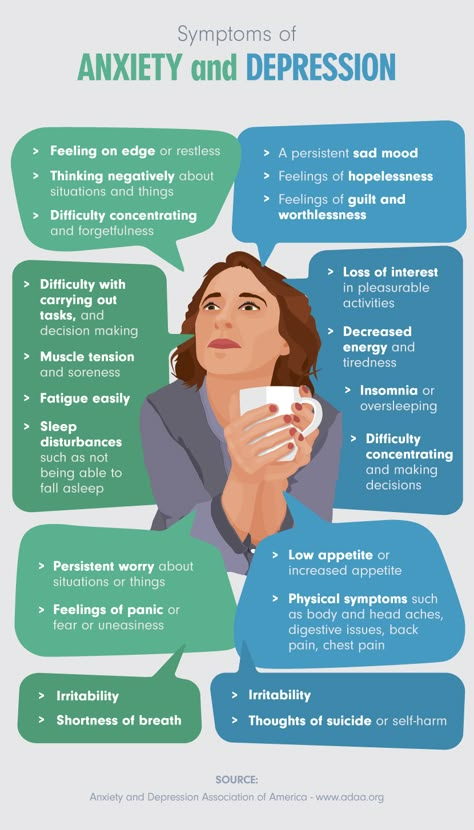 For example, if we are talking about the loss of a person who earned money, or solved the issues of raising children. The whole family has to go through the reorganization of life, and here psychotherapeutic support is very important. Stressful situations are always associated with the loss of the meaning of life, and it is very important that a person finds this meaning, finds a guide and strength to move on.
For example, if we are talking about the loss of a person who earned money, or solved the issues of raising children. The whole family has to go through the reorganization of life, and here psychotherapeutic support is very important. Stressful situations are always associated with the loss of the meaning of life, and it is very important that a person finds this meaning, finds a guide and strength to move on.
The task of psychotherapy is that a person, having experienced traumatic events, could continue to live a full life filled with meaning and joy. Many people who are faced with life-threatening situations are afraid to see a therapist because they fear that they will have to relive painful moments. Modern psychotherapy protects a person from re-experiencing the trauma. A doctor who specializes in working with trauma knows how to conduct the process of psychotherapy in a way that is not painful and traumatic for the patient.
Natalia Rivkina
PTSD: what it is, symptoms, treatment
Psychological trauma can sit inside us for years and decades, undermining strength and from time to time exacerbating pain. A practicing psychologist talks about the nature of post-traumatic stress disorder and explains what might help to cope with it.
A practicing psychologist talks about the nature of post-traumatic stress disorder and explains what might help to cope with it.
Arkady Volkov, psychotherapist, specialist of the service for the selection of psychologists Alter
Advertising on RBC www.adv.rbc.ru
What is PTSD
Each person has many mechanisms and resources at their disposal to help them cope with difficult events, cope with difficulties, endure grief and loss, overcome disappointments and tragedies. Nevertheless, sometimes we are faced with an event that, for one reason or another, we cannot cope with: it does not fit into our personal experience at all and turns out to be an insurmountable shock. Such events, usually associated with a real or perceived risk to life and health, are usually called traumas, and they can cause post-traumatic stress disorder - a mental disorder as a result of encountering a traumatic situation.
Studies show that almost 4% of people suffer from PTSD at least once during their lives.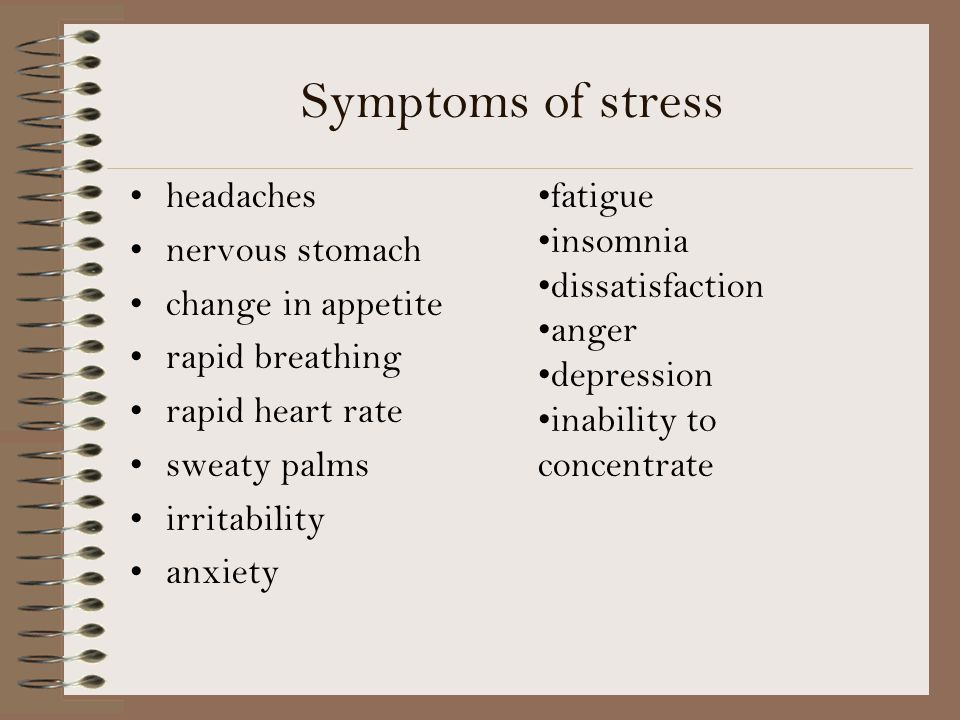 At the same time, statistics in different countries vary significantly: in China, 0.3% of respondents faced the problem, in the Netherlands — 7.4%, in Canada — 9.2% [1], [2].
At the same time, statistics in different countries vary significantly: in China, 0.3% of respondents faced the problem, in the Netherlands — 7.4%, in Canada — 9.2% [1], [2].
Symptoms of PTSD
Currently, the two main medical diagnostic guidelines (DSM-5, the American Psychiatric Association's guidelines, and ICD-11, the World Health Organization's classification) state the following criteria to conclude that a person is suffering from PTSD:
- Encounter with a life or health threatening situation. At the same time, PTSD can develop in a situation where a person has become a victim of such an event, and if he was a witness to it, or if a similar event happened to his loved ones. This criterion also applies to professionals who, by the nature of their work, are faced with the consequences of traumatic events: doctors, firefighters, crisis psychologists, and so on.
- Presence of at least one of the symptoms of involuntary intrusive and disturbing memories of the event, nightmares, flashbacks, distressing experiences, or a physical reaction in situations that are reminiscent of the event.

- Avoidance of memories and thoughts about the event or anything that might remind of it.
- Disturbances in thinking and emotional state due to the experienced event: inability to remember important aspects of what happened, negative thoughts and beliefs about oneself and the world around, blaming oneself or others that the traumatic event occurred, lowered mood and negative emotions, decreased interest in the world around , feelings of isolation and alienation, reduced ability to experience positive emotions.
- Changes such as irritability and outbursts of anger, aggressive and dangerous behavior to self or others, heightened alertness, startle response to minor stimuli, trouble concentrating and sleeping.
To be diagnosed, the listed symptoms must last more than one month and cause significant distress or social difficulties.
© shutterstock
It is important to note that PTSD is often accompanied by other disorders, primarily depressive ones.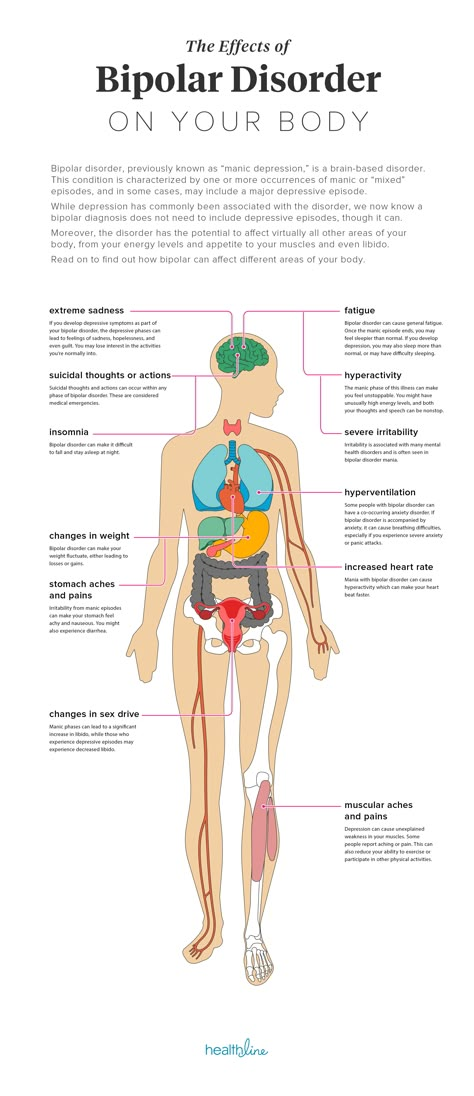
Diagnosis of PTSD, like any other mental disorder, can only be diagnosed by a qualified specialist, but yes to the following questions may be a reason to seek advice and get help (or just be more attentive to yourself or a loved one).
- During your lifetime, have you experienced or witnessed any traumatic event (such as an accident, fire, extreme disaster, physical attack on you or your loved ones)?
During the last month:
- Did you return to this event in your thoughts (not wanting it) or dreams?
- Did you make an effort not to think about this event and avoid being reminded of it?
- Were you more tense than usual?
- Have you ever been frightened for minor reasons?
- Did you feel alienated from your usual activities and loved ones?
- Did you feel guilty or blame yourself or others for the event?
Causes and risk factors
There is still no definite answer to the question of what exactly causes PTSD.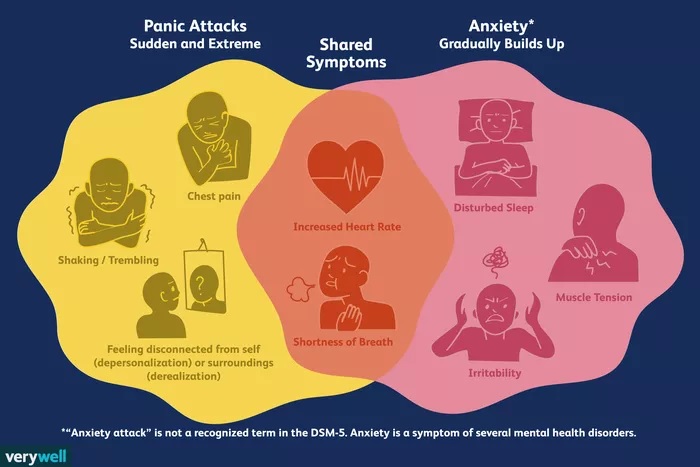 But research has led to some important assumptions.
But research has led to some important assumptions.
At the physiological level, the development of PTSD can be provoked by:
Increased levels of stress hormones
In case of danger, our body produces stress hormones, such as adrenaline, in order to switch into an active mode and somehow escape from the threat (this reaction is often called "fight or flight"). PTSD victims continue to produce large amounts of stress hormones even when the danger is no longer around. This can cause hyperarousal and emotional changes, and can also cause long-term negative health effects, including migraines, pain, and an increased risk of heart, lung, and digestive problems.
Changes in brain function
Trauma-induced stress can damage the hippocampus, the area of the brain involved in the formation of emotions and memory.
Disorders in the hippocampus can interfere with the proper processing of memories and dreams, so the anxiety they cause does not decrease over time. Such changes may explain the increased levels of fear and anxiety, memory and recall problems suffered by PTSD victims.
Such changes may explain the increased levels of fear and anxiety, memory and recall problems suffered by PTSD victims.
© shutterstock
Factors that can increase susceptibility to PTSD:
- Previous traumatic experiences. The stress of a trauma can have a cumulative effect, and a new traumatic experience can exacerbate the negative effects of a previous trauma.
- Experience of violence. People with a history of physical, emotional or sexual abuse tend to be more susceptible to post-traumatic stress.
- PTSD or depression in loved ones.
- Substance use experience.
- Lack of coping skills in traumatic situations.
- Lack of social support. Good social and family relationships help mitigate the effects of stress and trauma. Conversely, people who lack supportive relationships and environments tend to be more vulnerable to stress and therefore more at risk for PTSD. Being in a social environment that cultivates shame, guilt, stigma, or self-hatred also contributes to the development of post-traumatic stress disorder.

- High level of stress in everyday life.
Treatment of PTSD
Approaches to the treatment of PTSD can be divided into two groups: medication and psychotherapy. Often methods of both groups are used in different combinations.
There are currently no medications specifically designed to treat PTSD, but there are many medications that work well for other conditions, such as depression and anxiety disorders, and have been shown to be effective in treating the symptoms of PTSD.
When it comes to psychotherapeutic methods, or "healing with a word", there are several approaches that demonstrate the greatest (and research-supported) effectiveness.
Cognitive Process Therapy
In this approach, the therapist invites the client to talk about the traumatic event and its aftermath and describe the experience in detail in a diary, which allows them to better see how the trauma is reflected in thoughts and find new ways to deal with it [3 ].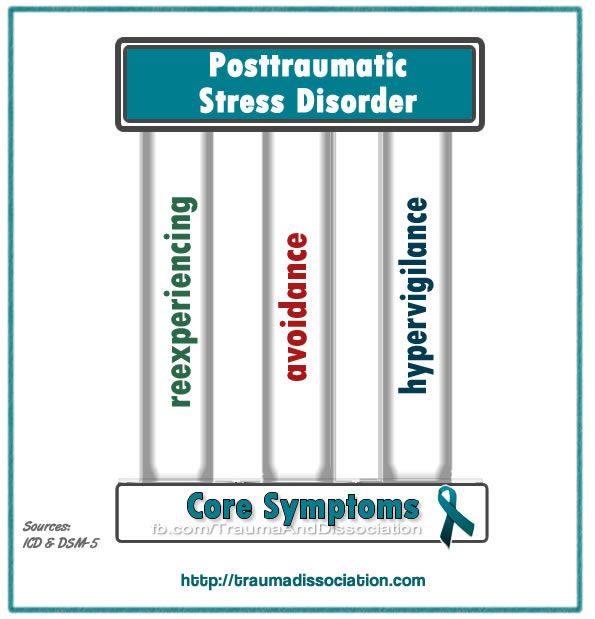
© shutterstock
EMDR - eye movement desensitization and processing
This approach is based on the notion that trauma disrupts the natural coping mechanisms inherent in each person and cannot be built into his experience and memory. The person is asked to focus on an external stimulus (eye movements from side to side directed by the therapist) and in parallel work through complex memories, thoughts and emotions associated with the trauma [4].
Body-oriented and creative approaches
Body Oriented Therapy aims to find resources through attention to bodily sensations, as well as gaining the opportunity to relive the traumatic experience from the position of an active actor, not a victim. Similar goals are set by approaches that use dance and participation in theatrical productions to gain the freedom and spontaneity that PTSD often deprives its victims of [5].
Living with PTSD
Trauma has a huge impact on many areas of our lives, but this does not mean that the problem cannot be solved, even if for one reason or another you do not have access to professional help.
Of particular difficulty in working with PTSD is the very painfulness and severity of the traumatic experience, which often makes it necessary to avoid any reminders of the trauma, excluding the possibility of talking about it, as well as the destructive consequences for the view of oneself and the world around. All this makes it extremely difficult to build close relationships, seek support and help.
What can help you cope with PTSD
The first and most important step is often the recognition of the traumatic experience, which opens up opportunities for conversation and subsequent rethinking. The devastating effect of trauma on the psyche is largely due to the fact that the traumatic event is completely knocked out of the normal course of our life, and it is extremely important to return, build it into our personal history.
Research demonstrates the effectiveness of a simple tool such as writing down your experience: writing down your thoughts and memories of a traumatic event, trying to talk about the impact it had on your life, thinking about the future.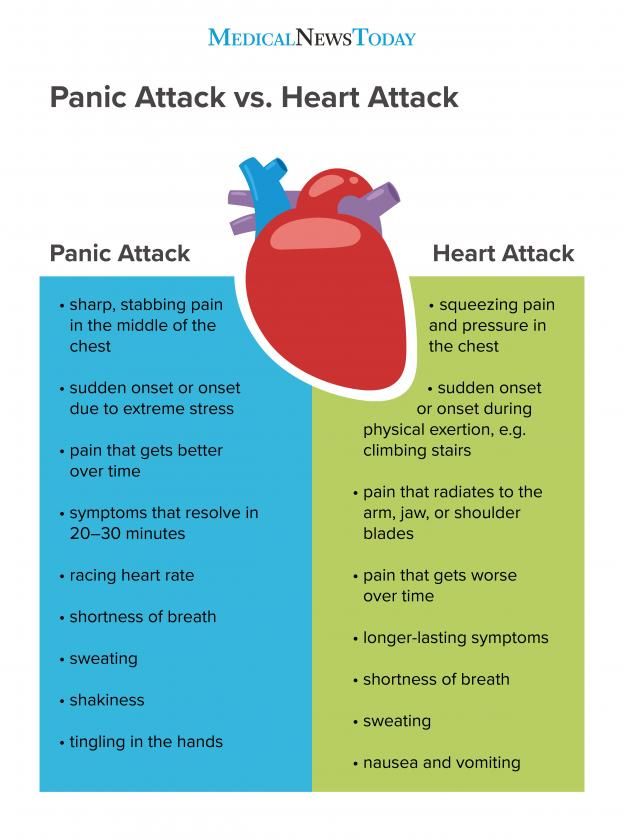
Since trauma affects the body in one way or another, physical exercise, yoga (or regular stretching), meditation, dancing, and even theater classes can be an important help in overcoming its consequences [6].
The support of relatives and friends plays a huge role. It's important to open yourself up and find someone you can talk to about what's bothering you.
However, overcoming PTSD on your own is not easy and can take a long time. Therefore, at the first opportunity, it is worth contacting a psychotherapist.
If your loved one has PTSD
If you notice symptoms of PTSD in a loved one, you can become a support for him and help him. At the same time, it is important to take into account that it can be extremely difficult for him to talk about the trauma and even return to it in his thoughts, so it is important to indicate your willingness to help and be there without exerting any pressure. Your very understanding and supportive presence, your willingness to share activities that bring joy and pleasure, a sense of stability and confidence can be beneficial.