Clonazepam dosage for depression
Clonazepam as a therapeutic adjunct to improve the management of depression: a brief review
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Wiley
Full text links
Review
. 2009 Apr;24(3):191-8.
doi: 10.1002/hup.1015.
Shigeru Morishita 1
Affiliations
Affiliation
- 1 Depression Prevention Medical Center, Kyoto Jujo Rehabilitation Hospital, Minami-ku, Kyoto, Japan. [email protected]
- PMID: 19330803
- DOI: 10.1002/hup.1015
Review
Shigeru Morishita. Hum Psychopharmacol. 2009 Apr.
. 2009 Apr;24(3):191-8.
doi: 10.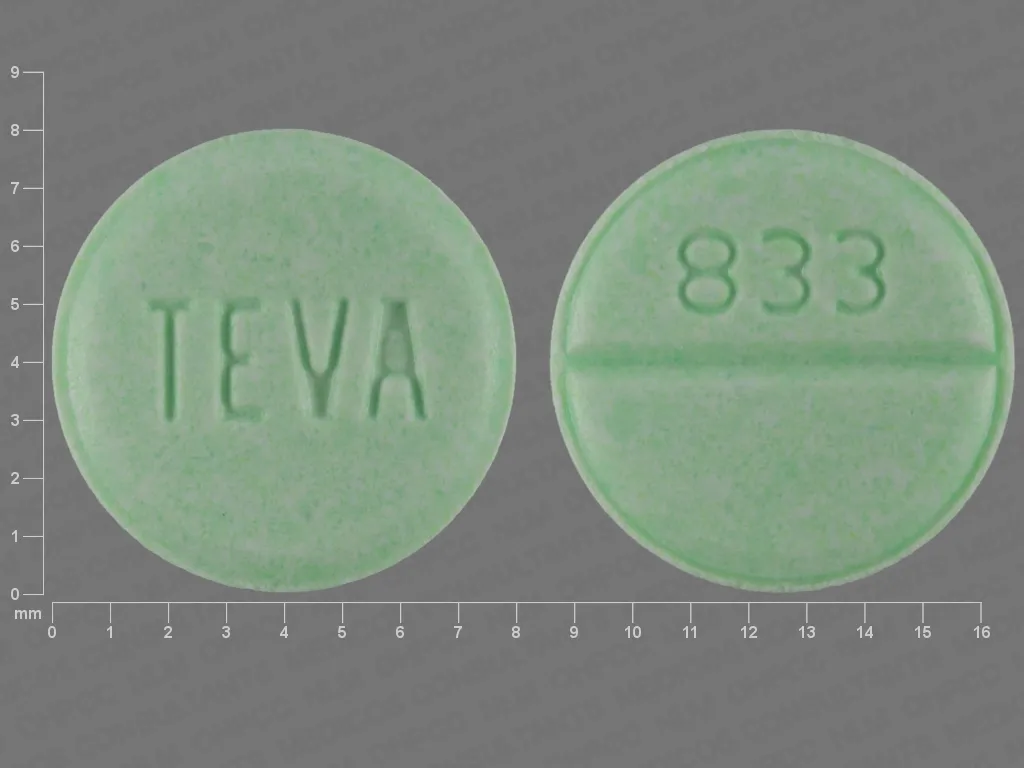 1002/hup.1015.
1002/hup.1015.
Author
Shigeru Morishita 1
Affiliation
- 1 Depression Prevention Medical Center, Kyoto Jujo Rehabilitation Hospital, Minami-ku, Kyoto, Japan. [email protected]
- PMID: 19330803
- DOI: 10.1002/hup.1015
Abstract
Clonazepam, first used for seizure disorders, is now increasingly used to treat affective disorders. We summarize the use of clonazepam to improve the management of depression. Clonazepam is useful for treatment-resistant and/or protracted depression, as well as for acceleration of response to conventional antidepressants. Clonazepam is at this time recommended for use in combination with SSRIs (fluoxetine, fluvoxamine, sertraline) as an antidepressant, and should be used at a dosage of 2.5-6.0 mg/day. If clonazepam is effective, a response should be observed within 2-4 weeks. It is significantly more effective for unipolar than for bipolar depression. Low-dose, long-term treatment with clonazepam exhibits a prophylactic effect against recurrence of depression. Although the mechanism of action of clonazepam has not yet been established, some investigators have been suggested that it involves enhancement of anti-anxiety effects, anticonvulsant effects on subclinical epilepsy, increase in 5-HT/monoamine synthesis or decrease in 5-HT receptor sensitivity mediated through the GABA system, and regulate in GABA activity.
Clonazepam is at this time recommended for use in combination with SSRIs (fluoxetine, fluvoxamine, sertraline) as an antidepressant, and should be used at a dosage of 2.5-6.0 mg/day. If clonazepam is effective, a response should be observed within 2-4 weeks. It is significantly more effective for unipolar than for bipolar depression. Low-dose, long-term treatment with clonazepam exhibits a prophylactic effect against recurrence of depression. Although the mechanism of action of clonazepam has not yet been established, some investigators have been suggested that it involves enhancement of anti-anxiety effects, anticonvulsant effects on subclinical epilepsy, increase in 5-HT/monoamine synthesis or decrease in 5-HT receptor sensitivity mediated through the GABA system, and regulate in GABA activity.
Similar articles
-
[Clonazepam as a therapeutic adjunct to improve the management of depression].
Morishita S. Morishita S. Nihon Shinkei Seishin Yakurigaku Zasshi. 2004 Apr;24(2):75-8. Nihon Shinkei Seishin Yakurigaku Zasshi. 2004. PMID: 15164614 Review. Japanese.
-
[Clonazepam in the treatment of protracted depression: a hundred-case report].
Morishita S. Morishita S. Nihon Shinkei Seishin Yakurigaku Zasshi. 2002 Jun;22(3):97-101. Nihon Shinkei Seishin Yakurigaku Zasshi. 2002. PMID: 12166090 Japanese.
-
Possible predictors of response to clonazepam augmentation therapy in patients with protracted depression.
Morishita S, Arita S. Morishita S, et al. Hum Psychopharmacol. 2007 Jan;22(1):27-31. doi: 10.1002/hup.818. Hum Psychopharmacol. 2007. PMID: 17191267
-
Theory of active antidepressants: a nonsynaptic approach to the treatment of depression.

Kiss JP. Kiss JP. Neurochem Int. 2008 Jan;52(1-2):34-9. doi: 10.1016/j.neuint.2007.04.006. Epub 2007 Apr 19. Neurochem Int. 2008. PMID: 17507113 Review.
-
[A trial of clonazepam treatment for manic-depressive psychoses].
Morishita S, Aoki S. Morishita S, et al. Nihon Shinkei Seishin Yakurigaku Zasshi. 1999 Oct;19(4):127-32. Nihon Shinkei Seishin Yakurigaku Zasshi. 1999. PMID: 10681156 Review. Japanese.
See all similar articles
Cited by
-
The role of cytochromes P450 in the metabolism of selected antidepressants and anxiolytics under psychological stress.
Zemanova N, Anzenbacher P, Anzenbacherova E. Zemanova N, et al.
 Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2022 May;166(2):140-149. doi: 10.5507/bp.2022.019. Epub 2022 Apr 12. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2022. PMID: 35438085 Review.
Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2022 May;166(2):140-149. doi: 10.5507/bp.2022.019. Epub 2022 Apr 12. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2022. PMID: 35438085 Review. -
Proteomics Study Reveals the Anti-Depressive Mechanisms and the Compatibility Advantage of Chaihu-Shugan-San in a Rat Model of Chronic Unpredictable Mild Stress.
Zhu X, Li T, Hu E, Duan L, Zhang C, Wang Y, Tang T, Yang Z, Fan R. Zhu X, et al. Front Pharmacol. 2022 Jan 17;12:791097. doi: 10.3389/fphar.2021.791097. eCollection 2021. Front Pharmacol. 2022. PMID: 35111057 Free PMC article.
-
Sleep Disorders in Stroke: An Update on Management.
Cai H, Wang XP, Yang GY. Cai H, et al. Aging Dis. 2021 Apr 1;12(2):570-585.
 doi: 10.14336/AD.2020.0707. eCollection 2021 Apr. Aging Dis. 2021. PMID: 33815883 Free PMC article. Review.
doi: 10.14336/AD.2020.0707. eCollection 2021 Apr. Aging Dis. 2021. PMID: 33815883 Free PMC article. Review. -
Somatostatin-Positive Gamma-Aminobutyric Acid Interneuron Deficits in Depression: Cortical Microcircuit and Therapeutic Perspectives.
Fee C, Banasr M, Sibille E. Fee C, et al. Biol Psychiatry. 2017 Oct 15;82(8):549-559. doi: 10.1016/j.biopsych.2017.05.024. Epub 2017 Jun 8. Biol Psychiatry. 2017. PMID: 28697889 Free PMC article. Review.
-
Impaired GABA synthesis, uptake and release are associated with depression-like behaviors induced by chronic mild stress.
Ma K, Xu A, Cui S, Sun MR, Xue YC, Wang JH. Ma K, et al. Transl Psychiatry. 2016 Oct 4;6(10):e910. doi: 10.1038/tp.2016.181. Transl Psychiatry.
 2016. PMID: 27701406 Free PMC article.
2016. PMID: 27701406 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Full text links
Wiley
Cite
Format: AMA APA MLA NLM
Send To
Side effects, dosage, uses, and more
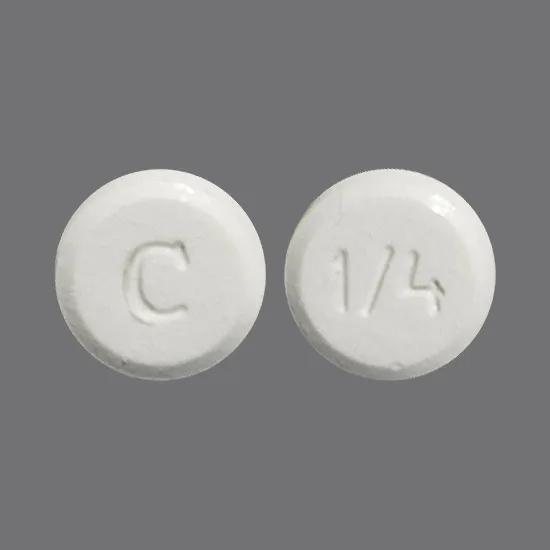
- Clonazepam oral tablet is available as a generic drug and a brand-name drug, Klonopin.
- Clonazepam comes as both an oral tablet and an oral disintegrating (dissolving) tablet.
- Clonazepam is used to treat panic disorder and seizures.
Clonazepam oral tablet is a prescription drug that’s available as the brand-name drug Klonopin. It’s also available as a generic drug. Generic drugs usually cost less. In some cases, they may not be available in every strength or form as the brand-name version.
It’s also available as a generic drug. Generic drugs usually cost less. In some cases, they may not be available in every strength or form as the brand-name version.
Clonazepam comes as both an oral tablet and an oral disintegrating (dissolving) tablet.
Clonazepam is a controlled substance.
Why it’s used
Clonazepam is used to treat panic disorder. It’s also used to stop seizures.
Clonazepam may be used as part of a combination therapy. This means a person may need to take it with other medications.
How it works
Clonazepam belongs to a class of drugs called benzodiazepines. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Clonazepam works by increasing the activity of gamma aminobutyric acid (GABA). This is a chemical that sends signals throughout a person’s nervous system. If a person does not have enough GABA, their body may be in an excited state. This may cause them to have panic attacks or seizures. When a person takes this drug, they will have more GABA in their body. This will help them have fewer panic attacks and seizures.
When a person takes this drug, they will have more GABA in their body. This will help them have fewer panic attacks and seizures.
Clonazepam can cause mild or serious side effects. The following list contains some of the key side effects that may occur while taking clonazepam. This list does not include all possible side effects.
For more information on the possible side effects of clonazepam, or tips on how to deal with a troubling side effect, a person should talk with their doctor or pharmacist.
Common side effects
The more common side effects of clonazepam oral tablet can include:
- drowsiness
- problems with walking and coordination
- dizziness
- depression
- fatigue
- problems with memory
If these effects are mild, they may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, a person should talk to their doctor or pharmacist.
Serious side effects
A person should call their doctor right away if they have serious side effects. They should call 911 if their symptoms feel life-threatening or if they think they are having a medical emergency. Serious side effects and their symptoms can include the following:
They should call 911 if their symptoms feel life-threatening or if they think they are having a medical emergency. Serious side effects and their symptoms can include the following:
- depressed mood or thoughts of suicide (harming themself)
- seizures (these are more likely to happen if a person stops taking this drug too quickly, or if they already have a seizure disorder)
The clonazepam dosage a doctor prescribes will depend on several factors. These include:
- the type and severity of the condition the person is using clonazepam to treat
- the person’s age
- the form of clonazepam they take
- other medical conditions they may have
Typically, a doctor will start a person on a low dosage and adjust it over time to reach the dosage that’s right for them. They’ll ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, a person should be sure to take the dosage the doctor prescribes for them.
However, a person should be sure to take the dosage the doctor prescribes for them.
A doctor will determine the best dosage to suit a person’s needs.
Forms and strengths
Generic: Clonazepam
- Form: oral tablet
- Strengths: 0.5 mg, 1 mg, 2 mg
- Form: oral disintegrating tablet
- Strengths: 0.125 mg, 0.25, 0.5 mg, 1 mg, 2 mg
Brand: Klonopin
- Form: oral tablet
- Strengths: 0.5 mg, 1 mg, 2 mg
Dosage for panic disorder
Adult dosage (ages 18 to 64 years)
- Typical starting dose: 0.25 mg taken twice per day
- Dose increases: A doctor may increase the dose to 0.5 mg taken two times per day after three days.
- Maximum dose: 4 mg per day.
- Dose reduction: A doctor should decrease a person’s dose slowly when stopping treatment with this drug.
 They should decrease the dose by no more than 0.125 mg every three days. For example, if the person was taking 2 mg two times per day, their doctor would start by decreasing the dose to 1.875 mg, taken two times per day.
They should decrease the dose by no more than 0.125 mg every three days. For example, if the person was taking 2 mg two times per day, their doctor would start by decreasing the dose to 1.875 mg, taken two times per day.
Child dosage (ages 0 to 17 years)
It hasn’t been confirmed that clonazepam is safe and effective for use in people younger than 18 years for this condition.
Senior dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause their body to process drugs more slowly. As a result, more of a drug stays in their body for a longer time. This raises their risk of side effects. Their doctor may start them on a lowered dose or a different dosing schedule. This can help keep levels of this drug from building up too much in their body.
Dosage for seizures
Adult dosage (ages 18 to 64 years)
- Typical starting dose: 0.5 mg taken three times per day
- Dose increases: A doctor may increase a person’s dose by 0.
 5 to 1 mg every three days until their seizures are controlled.
5 to 1 mg every three days until their seizures are controlled. - Maximum dose: 20 mg per day, taken in divided doses.
Child dosage (ages 11 to 17 years)
- Typical starting dose: 0.5 mg taken three times per day
- Dose increases: A doctor may increase a child’s dose by 0.5 to 1 mg every three days until their seizures are controlled.
- Maximum dose: 20 mg per day, taken in divided doses.
Child dosage (ages 0 to 10 years or children who weigh 66 lbs. [30 kg] or less)
- Typical starting dose: 0.01 to 0.03 mg/kg of body weight per day. The dose shouldn’t be more than 0.05 mg/kg per day given in two to three divided doses.
- Dose increases: A doctor may increase a child’s dose by 0.25 to 0.5 mg every three days until their seizures are controlled.
- Maximum dose: 0.1–0.2 mg/kg per day taken in divided doses.
Senior dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause their body to process drugs more slowly. As a result, more of a drug stays in their body for a longer time. This raises their risk of side effects. Their doctor may start them on a lowered dose or a different dosing schedule. This can help keep levels of this drug from building up too much in their body.
This can cause their body to process drugs more slowly. As a result, more of a drug stays in their body for a longer time. This raises their risk of side effects. Their doctor may start them on a lowered dose or a different dosing schedule. This can help keep levels of this drug from building up too much in their body.
Clonazepam oral tablet is used for short-term treatment. It comes with risks if a person does not take it as prescribed.
If a person stops taking the drug suddenly or doesn’t take it at all: If a person does not take this drug, their panic disorder or seizures won’t get better and may get worse. If they stop taking it suddenly, they may have symptoms of withdrawal. These include irritability, trouble sleeping, and anxiety.
If a person misses doses or doesn’t take the drug on schedule: They may have withdrawal symptoms if they don’t take the drug on schedule.
If a person takes too much: They could have dangerous levels of the drug in their body. Symptoms of an overdose of this drug can include:
Symptoms of an overdose of this drug can include:
- sleepiness or drowsiness
- confusion
- trouble with coordination or slow reflexes
- coma (being unconscious for a long time)
If a person thinks they have taken too much of this drug, they should call their doctor or local poison control center. If their symptoms are severe, they should call 911 or go to the nearest emergency room right away.
What to do if a person misses a dose: A person usually should take a missed dose as soon as they remember. But if they remember just a few hours before their next scheduled dose, take only one dose. They should never try to catch up by taking two doses at once. This could result in dangerous side effects.
How to tell if the drug is working: A person should have fewer panic attacks or seizures.
This drug comes with several warnings.
FDA warnings
- This drug has a black box warning.
 This is the most serious warning from the Food and Drug Administration (FDA). A black box warning alerts doctors and patients about drug effects that may be dangerous.
This is the most serious warning from the Food and Drug Administration (FDA). A black box warning alerts doctors and patients about drug effects that may be dangerous. - Using clonazepam with opioid drugs can cause dangerous effects. These can include severe drowsiness, slowed breathing, coma, and death. If your doctor prescribes clonazepam with an opioid, they will monitor you closely. Examples of opioids include hydrocodone, codeine, and tramadol.
- Risk of dependence: Using Clonazepam, even as prescribed, can lead to physical dependence and withdrawal if you stop taking the drug suddenly. Withdrawal can be life threatening. Taking this drug can also lead to misuse and addiction. Misuse of Clonazepam increases your risk of overdose and death.
- Follow the prescription: Only take this drug as your doctor prescribes. Talk with your healthcare provider if you have any concerns about safely taking this drug.
Clonazepam is a central nervous system (CNS) depressant. This type of drug can slow down the brain’s activity and interfere with a person’s judgment, thinking, and reaction time. A person should not drink alcohol or use other drugs that can also slow down their brain’s activity while they are taking this medication. They also shouldn’t drive, use machinery, or do other activities that require alertness until they know how this drug affects them.
This type of drug can slow down the brain’s activity and interfere with a person’s judgment, thinking, and reaction time. A person should not drink alcohol or use other drugs that can also slow down their brain’s activity while they are taking this medication. They also shouldn’t drive, use machinery, or do other activities that require alertness until they know how this drug affects them.
Suicidal thoughts and behavior
Clonazepam can increase the risk of suicidal thoughts or behavior (thoughts or actions of harming oneself). A person should tell their doctor if they have worsening depression, suicidal thoughts or behavior, or any unusual changes in mood or behavior.
Alcohol interaction
The use of drinks that contain alcohol can increase a person’s risk of sedative effects from clonazepam. A person may have slowed reflexes, poor judgment, and sleepiness. This can be dangerous. If a person drinks alcohol, they should talk to their doctor.
Allergy warning
Clonazepam can cause a severe allergic reaction. Symptoms can include:
Symptoms can include:
- trouble breathing
- swelling of the throat or tongue
If a person has an allergic reaction, they should call their doctor or local poison control center right away. If their symptoms are severe, call 911 or go to the nearest emergency room. A person should not take this drug again they have ever had an allergic reaction to it. Taking it again could be fatal (cause death).
Warnings for people with certain health conditions
For people with depression: A person’s depression might get worse while they are taking this drug. If a person has worsening symptoms of depression or any suicidal thoughts (thoughts of harming themself), call the doctor right away.
For people with acute narrow angle glaucoma: A person should not take this drug if they have acute narrow angle glaucoma. It can make the condition worse.
For people with liver disease: If a person has liver problems, their body may not be able to clear this drug well. This can cause the drug to build up in the body. This puts them at a higher risk for side effects.
This can cause the drug to build up in the body. This puts them at a higher risk for side effects.
Warnings for other groups
For pregnant women: Clonazepam is a category D pregnancy drug. That means two things:
- Studies show a risk of adverse effects to the fetus when the mother takes the drug.
- This drug should only be used during pregnancy in serious cases where it’s needed to treat a dangerous condition in the mother.
A person should talk to their doctor if they are pregnant or planning to become pregnant. This drug should be used only if the potential benefit justifies the potential risk to the fetus. A person should call their doctor right away if they become pregnant while taking this drug.
For women who are breastfeeding: Clonazepam passes into breast milk and causes side effects in a child who is breastfed. A person should talk to their doctor if they breastfeed their child. They may need to decide whether to stop breastfeeding or stop taking this medication.
For seniors: The kidneys of older adults may not work as well as they used to. This can cause their body to process drugs more slowly. As a result, more of a drug stays in their body for a longer time. This raises their risk of side effects.
For children: This medication hasn’t been studied in children with panic disorders. It shouldn’t be used for the treatment of this condition in people younger than 18 years.
Clonazepam can interact with several other medications. Different interactions can cause different effects. For instance, some can interfere with how well a drug works, while others can cause increased side effects.
Below is a list of medications that can interact with Clonazepam. This list does not contain all drugs that may interact with Clonazepam.
Before taking Clonazepam, a person should be sure to tell their doctor and pharmacist about all prescription, over-the-counter, and other drugs they take. They should also tell them about any vitamins, herbs, and supplements they use. Sharing this information can help avoid potential interactions.
Sharing this information can help avoid potential interactions.
If a person has questions about drug interactions that may affect them, they should ask their doctor or pharmacist.
Drugs that increase the risk of side effects
Taking clonazepam with certain other medications may cause more side effects. Examples of these drugs include:
- Benzodiazepines, such as lorazepam, clonazepam, triazolam, and midazolam. A person may feel more sedated and drowsy.
- Opioids, such as codeine and hydrocodone. Taking these drugs with clonazepam puts a person at serious risk of severe drowsiness, slowed breathing, coma, or death.
- Barbiturate and nonbarbiturate sleep drugs, such as amobarbital, butabarbital, eszopiclone, pentobarbital, zaleplon, and zolpidem. A person may feel more sedated and drowsy.

- Other drugs used to treat anxiety, such as buspirone and hydroxyzine. A person may feel more sedated and drowsy.
- Tricyclic antidepressants, such as amitriptyline and nortriptyline. A person may feel more sedated and drowsy.
- Other drugs used to treat seizures, such as gabapentin and pregabalin. A person may feel more sedated and drowsy.
Keep these considerations in mind if a doctor prescribes clonazepam oral tablet.
General
- A person can take clonazepam with or without food.
- They should take this drug at the times recommended by a doctor.
- A person can cut or crush the tablet.
- Not every pharmacy stocks this drug. When filling a prescription, be sure to call ahead.
Storage
- Store clonazepam between 59°F and 86°F (15°C and 30°C).
- Don’t store this medication in moist or damp areas, such as bathrooms.

Refills
A prescription for this medication is refillable. However, clonazepam is a schedule IV controlled substance. Therefore, a prescription for this drug may be refilled no more than five times. Also, a person can only get refills for six months after the date their doctor wrote the original prescription. After that time, they will need a new prescription.
Travel
When traveling with medication, a person should:
- Always carry their medication with them. When flying, they should never put it into a checked bag and instead keep it in a carry-on bag.
- Not worry about airport X-ray machines. They can’t hurt the medication.
- Always carry the original prescription-labeled box, as they may need to show airport staff the pharmacy label for their medication.
- Not put this medication in a car’s glove compartment or leave it in the car. They should be especially sure to avoid doing this when the weather is very hot or very cold.
Clinical monitoring
A person and their doctor should monitor certain health issues. This can help make sure they stay safe while they take this drug. These issues include:
This can help make sure they stay safe while they take this drug. These issues include:
- Kidney function. A doctor may do blood tests to check how well a person’s kidneys are working. If their kidneys aren’t working well, the doctor may lower the person’s dose.
- Mental health and behavioral problems. A person and their doctor should watch for any unusual changes in their behavior and mood. This drug can cause new mental health and behavior problems. It can also make problems a person already has worse.
- Seizures. If a person is taking this drug for seizures, they and their doctor should monitor the number of seizures they have.
Insurance
Many insurance companies require a prior authorization for this drug. This means a doctor will need to get approval from a person’s insurance company before the insurance company will pay for the prescription.
There are other drugs available to treat a person’s condition. Some may be better suited for that person than others. A person should talk to their doctor about other drug options that may work for them.
Some may be better suited for that person than others. A person should talk to their doctor about other drug options that may work for them.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.
Arpimed
What Clonazepam is and what it is used for
Clonazepam is the active ingredient in Clonazepam.
Clonazepam belongs to a group of medicines called benzodiazepines.
Clonazepam is used to treat epilepsy in infants and older children and adults.
Clonazepam reduces the frequency of seizures.
Clonazepam reduces the severity of epileptic seizures.
What you need to know before you use Clonazepam
Do not take Clonazepam,
- If you are allergic (hypersensitive) to clonazepam or any of the other ingredients of this medicine.
- If you are allergic (hypersensitive) to other benzodiazepines, including diazepam, flurazepam, temazepam.
If you have any of these conditions, check with your doctor before using clonazepam.
Do not take Clonazepam,
- If you have breathing problems or lung disease.
- If you have severe liver failure.
- If you have myasthenia gravis (muscle weakness and increased muscle fatigue).

- If you have obstructive sleep apnea (stopping breathing during sleep)
- If you abuse alcohol or take prescription or recreational drugs.
If you have any of these conditions, check with your doctor before using clonazepam.
Warnings and precautions
While being treated with antiepileptic drugs like clonazepam, some people have thoughts of harming themselves or committing suicide. If you experience any of these, tell your doctor immediately.
Talk to your doctor or pharmacist before taking clonazepam if:
- If you have liver or kidney problems or impaired lung function.
- Have you ever been depressed.
- If you have ever had suicidal thoughts.
- If you have recently lost a loved one.
- If you regularly use alcohol or recreational drugs or have abused alcohol or recreational drugs in the past.
- You suffer from spinal or cerebellar ataxia (movements become inaccurate, balance is disturbed when standing, slurred speech and rapid eye movement sleep develop).

- You have a rare genetic blood disorder called porphyria.
- If you are an elderly or malnourished patient, your doctor may need to adjust your dose of clonazepam.
If you have any of these conditions, check with your doctor before using clonazepam.
Drug interactions
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including OTC and herbal remedies. Clonazepam may interfere with the effects of certain drugs. Some drugs may also affect the effects of clonazepam.
The following drugs are especially important to note:
- Other epilepsy drugs such as carbamazepine, hydantoins, phenobarbital, phenytoin, primidone, or sodium valproate.
- Cimetidine (used to treat stomach problems and heartburn).
- Rifampicin (an antibiotic used to treat infections).
- Sleeping drugs.
- Medicines used to relieve anxiety (tranquilizers).

- Painkillers (analgesics) and drugs that reduce muscle tone (muscle relaxants).
Surgery
Tell your doctor or dentist that you are taking clonazepam if you are having surgery or dental work that requires pain relief. clonazepam and alcohol
Pregnancy and breast-feeding
It is not recommended to take clonazepam if you are pregnant, think you might be pregnant, or are breastfeeding, unless your doctor has told you to. Clonazepam has an adverse effect on fetal development during pregnancy.
Effects on ability to drive and use machines
Talk to your doctor about driving and using machines before using clonazepam, because clonazepam slows down your response rate, especially when you start taking it. If you have any doubts about your ability to perform certain activities, contact your doctor. Clonazepam affects the ability to drive vehicles, as the drug can cause drowsiness and dizziness.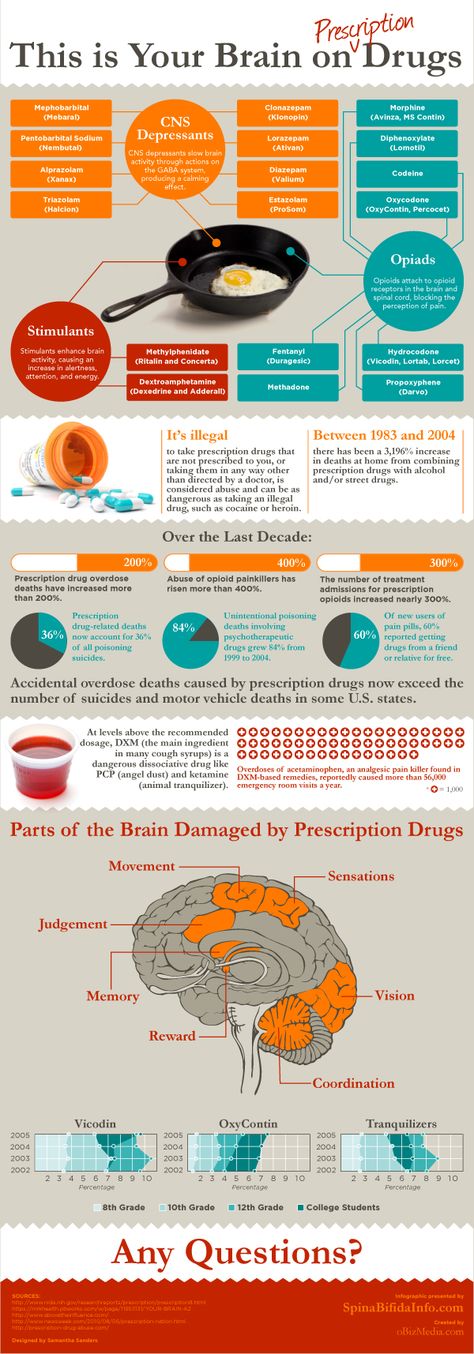
- Do not drive while taking this drug until you know how it affects you.
- If you know that this drug affects your ability to drive, driving while taking the drug is a legal violation.
- You will not be held liable if:
- Clonazepam has been prescribed for medical and dental problems and,
- You have taken clonazepam as prescribed by your doctor or as described in this package insert and, Clonazepam
- does not affect the ability to drive safely.
- If you have any doubts about your ability to drive safely while taking clonazepam, talk to your doctor.
Development of dependence
When taking clonazepam, there is a risk of dependence, which increases with increasing dose and duration of treatment, in patients with a history of alcohol and / or drug abuse.
Important information about the ingredients of Clonazepam
Clonazepam tablets contain lactose.
If you have been told by your doctor that you have an intolerance to some sugars, check with your doctor before taking clonazepam.
How to take Clonazepam
Clonazepam should be taken exactly as directed by your doctor. If you have any doubts, then you should consult with your doctor.
- Clonazepam should be started at a low dose and increased gradually over 2-4 weeks until the optimal maintenance dose is found to meet the patient's needs.
- Usually, on the recommendation of a physician, the daily dose is divided into 3 doses per day in equal doses for each dose with an equal interval of time between doses.
- If the daily dose cannot be evenly divided into several doses, take the largest dose at bedtime.
- After reaching an effective maintenance dose, the drug can be taken in a single daily dose at bedtime.
Adults and children over 12 years old
- The usual starting dose is 1 mg or less per day.

- Then the dose is gradually increased (usually up to 4-8 mg per day). The maximum daily dose should not exceed 20 mg.
Old age
- The usual starting dose is 0.5 mg or less per day.
- Then the dose is gradually increased (usually up to 4-8 mg per day). The maximum daily dose should not exceed 20 mg.
Children under 1 year
- The usual starting dose is 0.25 mg or less per day.
- Then the dose is gradually increased (usually up to 0.5-1 mg per day).
Children 1 to 5 years
- The usual starting dose is 0.25 mg or less per day.
- Then the dose is gradually increased (usually up to 1-3 mg per day).
Children 5 to 12 years old
- The usual starting dose is 0.5 mg or less per day.
- Then the dose is gradually increased (usually up to 3-6 mg per day).

If you have taken more Clonazepam than recommended
- If you have taken more clonazepam than recommended, contact your doctor or nearest hospital immediately. Take a pack of medicines with you.
- If you have taken a large amount of clonazepam, you may experience lethargy, drowsiness, dizziness, incoordination and decreased body reaction.
If you forget to take Clonazepam
- If you forget to take Clonazepam, skip the missed dose and take your next dose at the scheduled time.
- Do not take a double dose to make up for a missed one.
Stopping Clonazepam
If you take clonazepam for a long time, you may develop addiction and withdrawal symptoms if you stop taking it.
- You should talk to your doctor before you stop taking clonazepam, because if you suddenly stop taking the drug, you may have a recurrence of epileptic seizures and the development of a withdrawal syndrome.
 (see Possible Side Effects).
(see Possible Side Effects). - If you need to reduce the dose or stop taking the drug, you need to do it gradually. Your doctor will tell you how to do this.
If someone else has taken clonazepam by mistake, they should contact their doctor or the nearest hospital immediately.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Possible side effects
Like all medicines, clonazepam can cause side effects, although not everyone gets them.
Important side effects :
Allergic reactions .
If you develop an allergic reaction, call your doctor immediately.
Allergic reactions may manifest as the following symptoms:
- Sudden swelling of the larynx, face, lips and mouth. These symptoms can lead to difficulty breathing or swallowing.
- Sudden swelling of hands, feet and ankles.
- Skin rash or itching.

Cardiovascular adverse reactions
If you have any of these symptoms, you should contact your doctor immediately.
These symptoms include:
- Shortness of breath, swelling of the ankles, cough, fatigue and palpitations.
- Pain in the chest area, which can radiate to the neck, shoulder and left arm.
Nervous system side effects
If you have any of these symptoms, you should talk to your doctor.
These symptoms include:
- Feelings of aggression, agitation, irritability, nervousness, agitation, anxiety and hostility.
- Sleep disturbance, nightmares and vivid dreams.
- Hallucinations, manias and speech impairment.
- Development of new types of seizures not previously observed
Children and infants
- Special care should be taken when taking clonazepam in children and infants, since clonazepam may lead to the development of respiratory dysfunction, coughing and a feeling of suffocation.
 This may be caused by excessive salivation.
This may be caused by excessive salivation. - Early puberty possible. After the abolition of clonazepam, this process stops.
Other possible side effects
Taking clonazepam may cause the following symptoms:
- Drowsiness and fatigue
- Dizziness and fatigue.
- Muscle weakness or flexibility, jerky movements (poor coordination)
- Walking instability
Tell your doctor if you have any of these symptoms. Your healthcare provider will prescribe you a low dose, if necessary, by gradually increasing the dose of clonazepam.
The following symptoms may occur at any time during treatment with clonazepam
Circulatory, renal and hepatic system Your healthcare provider should perform periodic blood tests if needed. Gastrointestinal tract Organs of vision Respiratory system Skin and hair Sexual system Syndrome Withdrawal When taking benzodiazepines such as clonazepam, addiction to the drug may develop. The following symptoms are less common: Trauma Patients taking benzodiazepines are at an excessive risk of falling or breaking bones, especially the elderly, patients taking sedatives, including alcohol. Reporting side effects insert. How to store Clonazepam Package contents and additional information What Clonazepam contains One tablet contains: active substance - clonazepam - 2 mg; excipients: microcrystalline cellulose, lactose monohydrate, corn starch, povidone, sodium starch glycolate, magnesium stearate, purified talc. What Clonazepam looks like and contents of the pack: White, round, flat tablets scored on one side. Carton containing 24 tablets (1 blister of 24 tablets) with leaflet. Dispensing conditions Dispensed according to prescription Isolation of PR was significant not only according to clinical criteria, but also according to the characteristics of the patients' response to therapy, which include: High efficacy of antidepressants; Insufficient effect of the use of traditional benzodiazepine tranquilizers; Insufficient effectiveness of psychotherapy. Russian psychiatrists still practice the use of traditional benzodiazepines (diazepam, chlordiazepoxide, phenazepam) in PR, less often - small doses of antidepressants (amitriptyline, azaphen) and small antipsychotics (teralen, sonapax), or a combination of these groups of drugs often does not lead to to a lasting and pronounced effect. It is now established that PR responds well to pharmacotherapy. Treatment for panic disorder can be divided into 3 main steps: Stopping PN up to the establishment of remission (4-6 weeks - 2-3 months) Stabilizing (further treatment) therapy to consolidate the results, restore the level of social adaptation, overcome agoraphobic manifestations (anticipation anxiety, avoidant behavior) and early relapses (4-6 months). Prophylactic (long-term) therapy aimed at preventing the development of relapses and maintaining a stable remission (up to 1 year or more) Currently, the following anti-panic (used to block PN) drugs are distinguished: tricyclic antidepressants, selective serotonergic drugs, MAO inhibitors, etc. atypical (or high potency) benzodiazepines (alprazolam and clonazepam). A) Tricyclic antidepressants (TAD). The most commonly used tricyclic antidepressants are clomipramine (anafranil), imipramine (melipramine), demipramine (petilil, pertofran), nortriptyline, and amitriptyline. The effectiveness of the tetracyclic antidepressant maprotiline (Ludiomil) and the atypical TAD tianeptine (Coaxil, Stablon) similar in action to TAD is described. Clomipramine (anafranil) is the most commonly used and most effective TAD in the treatment of PR. TAD treatment is initiated at low doses (12.5–25 mg/day) and then gradually increased to a tolerable level (average 12.5–25 mg over 3–5 days). The average effective daily dose is usually 150-200 mg / day, rarely reaches 300 mg. The anti-panic effect of TAD is also “delayed” like the thymoanaleptic, but comes on somewhat faster - the latent period is usually about two weeks. TAD has an effect in PR mainly due to the effect on the thymic and especially on the phobic component, less affecting the expectation anxiety and somatovegetative manifestations. In the case of a good reaction, a decrease in the frequency of PR occurs rather quickly, anxiety of expectation and phobias are reduced, and mood is evened out. However, in half of the patients, from the first days of TAD use, an increase in anxiety and vegetative symptoms occurs, which increases the occurrence of PP, therefore, with an inadequate increase in dosages, the patient's condition either does not improve at all, or the initial improvement will be lost after a few weeks. B) selective serotonin reuptake inhibitors (SSRIs). In addition to TAD, selective serotonin reuptake inhibitors are effective in the treatment of PR: fluoxetine (Prozac, Portal, Prodep), fluvoxamine (fevarin, floxifral. Luvox), sertraline (Zoloft), paroxetine (Paxil), citalopram (Cipramil). The main disadvantage of this group is the occurrence during the first 2-3 weeks of treatment of hyperstimulation (irritability, insomnia, nervousness) and increased anxiety and panic symptoms (probably due to excessive stimulation of serotonin autoreceptors). The technique of application does not differ from the treatment of depression, but the initial doses are usually minimal (5 mg fluoxetine, 50 mg fluvoxamine, 25 mg sertraline). B) monoamine oxidase inhibitors (MAOIs). In Russia in recent years, only the so-called. reversible MAOIs (moclobemide (Aurorix) and pyrazidol). They are usually used in cases of intolerance to the above drugs - studies on their use are insufficient. In general, they seem to be inferior in effectiveness to the above drugs, but are much better tolerated. Moclobemide is particularly effective in the combination of PP with social phobia. Treatment begins with 25-50 mg / day with a gradual increase in dose of 50 mg / day. The effective daily dose is usually 450-600 mg/day. D) Atypical (high potency) benzodizepines (ABZD). An important group for the treatment of PR are atypical benzodiazepines: alprazolam (Xanax, Cassadan) and clonazepam (Antelepsin, Rivotril). Features of ABZD is their high affinity for benzodiazepine receptors (3 times higher than that of typical BZD). Unlike antidepressants, which reduce PN and agoraphobia, but have little effect on the anxiety of expecting an attack, alprozalam not only suppresses the anticipation and avoidance component (agoraphobic), but also stops the psychopathological and somatovegetative manifestations of the attack itself (panic component) and prevents the development of PN. In addition, it practically does not cause side effects up to a dose of 4-6 mg / day, i.e. it has a very good tolerance. The drug does not cause exacerbation of anxiety like antidepressants, the anti-panic effect develops without a "latent period". In addition, alprazolam has a distinct antidepressant (thymoanaleptic) effect, which develops 2-3 weeks after the start of therapy. The disadvantage is the possibility of developing dependence (substance abuse) and "withdrawal syndrome", as well as the need for 3-4 times a day due to a short half-life (the prolonged form of Xanax retard is free from this disadvantage). Clonazepam (antelepsin, rivotril) also has a pronounced anti-panic effect at a dose of 2-6 mg/day, however, it has more pronounced side effects (drowsiness, lethargy, ataxia, depressogenicity), which limits its use. In long-term treatment with BDD, the safety, efficacy, and indications for therapy should be periodically assessed. It is recommended to answer the following questions at certain intervals (2-4 months): Do existing disorders justify continued therapy? Did the patient feel much better after BZD therapy? Does the duration of use remain within the prescribed range, has the patient avoided other unprescribed medications? Does the patient show signs of intoxication or confusion associated with the use of BZD or their combination with other drugs? Any "no" answer is an indication that treatment should be stopped. Traditional BZD in an isolated form are currently rarely used in PD, prescribed only as "correctors" of antidepressants in the initial phase of treatment or even anticipating the appointment of the latter ("premedication"). E) Criteria for choosing drugs. Therapy with TAD and especially with clomipramine is clearly effective in patients with rapid onset of depression with endogeneity traits, with a high proportion of maniophobia and depersonalization-derealization disorders in the structure of PP. With a stronger representation of the somatovegetative components of the PR (compared to the "mental"), the effectiveness of TAs is less, they are worse tolerated and more often cause exacerbation of the PR. In these cases, it is necessary to decide whether to replace the TAD with an ABSA or an MAOI. The ideal target for ABZD are predominantly somatovegetative PP without distinct agoraphobia; with severe phobic symptoms, their use does not lead to a clear effect, stopping only the anxiety of expectation and PP. Thus, if we proceed from traditional nosological ideas about the place of PD as a syndrome in the structure of a particular disease, then when choosing therapy, the following should be taken into account: psychopathological phenomena (fear of going crazy, depression, depersonalization, anxiety,) “large” TADs (clomipramine, impramine, amitriptyline) are most effective. Their significance will increase even more as the PR picture approaches the melancholic raptus. Clomipramine, SSRIs, MAOIs are also the drug of choice for severe agoraphobia or the presence of other concomitant phobias or obsessions that may not be thematically related to agoraphobia, i.e. with a large proportion of ideational obsessions within the framework of sluggish schizophrenia, cyclothymia. TIR. In case of PR within the framework of neurosis, the value of clomipramine and SSRIs is high in case of obsessive-compulsive disorder, but decreases in asthenic neurosis and hysteria, where ABZD or MAOI are more effective. It should be noted that in the treatment of patients with PD, it is often necessary to combine basic "anti-panic" drugs with drugs that allow influencing psychopathic (most often hysterical) and overvalued (hypochondriac) disorders. In such situations, drugs from the group of neuroleptics are added to the basic drugs: thioridazine (sonapax), alimemazine (teralen), periciazine (neuleptil), sulpiride (eglonil), chrolprothixen. In addition, when diagnosing a schizophrenic process, it is necessary to add antipsychotics to the “syndromal” therapy, which have an anti-negative effect and affect the overall progression of the disease (trifluoperazine (triftazin, stelazin), clozapine (azaleptin, leponex), risperidone (rispolept), etc.). E) PR psychotherapy. Effective treatment of PD requires (especially in cases complicated by agoraphobia) the use of psychotherapeutic techniques. The latter usually begin to be used at the stage of stabilizing (further treatment) psychopharmacotherapy and continue for some time after stopping the medication (largely facilitating the latter). Behavioral and, more rarely, cognitive psychotherapy are most effective in PR. They allow you to reduce the level of anxiety in phobic situations and reduce the fear of waiting for an attack. Cognitive psychotherapy is aimed at correcting fixed erroneous ideas of patients, according to which they give exaggerated reactions to non-life-threatening somatic sensations. Systematic desensitization is the leading method of behavioral therapy (BT). immersion in a phobia situation (imaginary or real). The patient and therapist make a scale of scenes associated with the onset of symptoms, ranking them in ascending order from least to most distressing. Applying the techniques of progressive muscle relaxation, the patient learns to relax, imagining more and more painful scenes. Then the sessions are transferred from the office to a real life setting, to situations that cause anxiety. In other behavioral techniques, the patient is directly immersed in an anxiety-provoking situation: after several weeks, during which the patient is no longer disturbed by PP, the doctor encourages him to deliberately encounter phobic stimuli.
 Symptoms include feeling tired, bruising from minor concussions, shortness of breath, and nosebleeds.
Symptoms include feeling tired, bruising from minor concussions, shortness of breath, and nosebleeds.
 Therefore, with a sudden discontinuation or dose reduction of clonazepam, a withdrawal syndrome may develop. Withdrawal syndrome can lead to the development of the following symptoms:
Therefore, with a sudden discontinuation or dose reduction of clonazepam, a withdrawal syndrome may develop. Withdrawal syndrome can lead to the development of the following symptoms:
 You can also report side effects to Arpimed LLC by going to the website www.arpimed.com and filling out the appropriate form “Report a side effect or ineffectiveness of a drug” and to the Scientific Center for Expertise of Drugs and Medical Technologies named after. Academician E.Gabrielyan, by going to the website www.pharm.am in the section “Report a side effect of a drug” and fill out the form “Map of reporting a side effect of a drug”. Scientific center hotline: +37410237665; +37498773368 By reporting side effects, you help provide more information about the safety of this drug.
You can also report side effects to Arpimed LLC by going to the website www.arpimed.com and filling out the appropriate form “Report a side effect or ineffectiveness of a drug” and to the Scientific Center for Expertise of Drugs and Medical Technologies named after. Academician E.Gabrielyan, by going to the website www.pharm.am in the section “Report a side effect of a drug” and fill out the form “Map of reporting a side effect of a drug”. Scientific center hotline: +37410237665; +37498773368 By reporting side effects, you help provide more information about the safety of this drug.
 Ask your doctor or pharmacist how to dispose of medicines you no longer need. Keep the medicine with you if your doctor has instructed you to do so.
Ask your doctor or pharmacist how to dispose of medicines you no longer need. Keep the medicine with you if your doctor has instructed you to do so. FGBNU NTSPZ.
 ‹‹Panic disorder (clinic, diagnosis, therapy)››
‹‹Panic disorder (clinic, diagnosis, therapy)››
 At this stage, it is necessary to conduct adequate psychotherapy.
At this stage, it is necessary to conduct adequate psychotherapy. 
 Patients may reach a “tolerance plateau” two or three times before the final dose is selected. To avoid premature discontinuation of the drug, any benzodiazepine drugs (diazepam 5-10 mg / day, phenazepam 0.5-1 mg / day), as well as α-blockers (anaprilin 20-40 mg / day), can be added to TAD, which allows to reduce the severity of exacerbation of PR and wait for a somewhat delayed effect of the antidepressant. TAD treatment is continued for 4-6 months, and if the condition is stable, a gradual reduction in dose levels is started, which usually lasts 1-2 months. In the future, decide on a longer prophylactic therapy. Thus, the main disadvantages of TAD are the delayed effect and pronounced side effects, especially those associated with hyperstimulation of the autonomic nervous system: palpitations, tremor, hyperhidrosis, dizziness, anticholinergic effects, paradoxical increase in blood pressure, sexual dysfunction, weight gain. These effects are especially pronounced in amitriptyline, which significantly limits its use in this group of patients.
Patients may reach a “tolerance plateau” two or three times before the final dose is selected. To avoid premature discontinuation of the drug, any benzodiazepine drugs (diazepam 5-10 mg / day, phenazepam 0.5-1 mg / day), as well as α-blockers (anaprilin 20-40 mg / day), can be added to TAD, which allows to reduce the severity of exacerbation of PR and wait for a somewhat delayed effect of the antidepressant. TAD treatment is continued for 4-6 months, and if the condition is stable, a gradual reduction in dose levels is started, which usually lasts 1-2 months. In the future, decide on a longer prophylactic therapy. Thus, the main disadvantages of TAD are the delayed effect and pronounced side effects, especially those associated with hyperstimulation of the autonomic nervous system: palpitations, tremor, hyperhidrosis, dizziness, anticholinergic effects, paradoxical increase in blood pressure, sexual dysfunction, weight gain. These effects are especially pronounced in amitriptyline, which significantly limits its use in this group of patients. Efficacy was noted in some patients with PR of the atypical TAD tianeptine (coaxil) at a dose of 37.5 mg/day. Decrease or blockade of PP, reduction or decrease in the intensity of agoraphobia are observed by 5-6 weeks of treatment. A good effect is noted in patients with "atypical" PP and signs of "secondary" depression, comorbid PD.
Efficacy was noted in some patients with PR of the atypical TAD tianeptine (coaxil) at a dose of 37.5 mg/day. Decrease or blockade of PP, reduction or decrease in the intensity of agoraphobia are observed by 5-6 weeks of treatment. A good effect is noted in patients with "atypical" PP and signs of "secondary" depression, comorbid PD.  Within 2 weeks, the dose is brought to an average, and then, if necessary, it is increased or remains the same. Subsequently, even with prolonged therapy, the dose does not change. For long-term (maintenance) treatment, drugs are much more convenient than TAD due to the lack of anticholinergic and adrenergic effects and possible single dose during the day.
Within 2 weeks, the dose is brought to an average, and then, if necessary, it is increased or remains the same. Subsequently, even with prolonged therapy, the dose does not change. For long-term (maintenance) treatment, drugs are much more convenient than TAD due to the lack of anticholinergic and adrenergic effects and possible single dose during the day. 
 Rarely, compared with other BZD, weakness, lethargy, drowsiness, fatigue, ataxia are noted. The likelihood of developing dependence limits the possibility of long-term (more than 4-6 weeks) taking the drug, however, if antidepressants are intolerant, alprazolam must be prescribed for a long time, followed by an extremely slow dose reduction. Initial doses of alprazolam 0.25-0.5 mg/day with an increase of 0.25-0.5 mg every 3 days until complete blockade of the occurrence of PP. Preservation of PP, their recurrence indicates an insufficient dose of the drug, and side effects (sedation, lethargy, drowsiness) indicate the need to reduce the dose. Average doses are 4-6 mg/day, treatment is continued for 4-6 months after which, with good adaptation of patients, the dose is reduced at an average rate of 0.5 mg per week in order to avoid withdrawal syndrome.
Rarely, compared with other BZD, weakness, lethargy, drowsiness, fatigue, ataxia are noted. The likelihood of developing dependence limits the possibility of long-term (more than 4-6 weeks) taking the drug, however, if antidepressants are intolerant, alprazolam must be prescribed for a long time, followed by an extremely slow dose reduction. Initial doses of alprazolam 0.25-0.5 mg/day with an increase of 0.25-0.5 mg every 3 days until complete blockade of the occurrence of PP. Preservation of PP, their recurrence indicates an insufficient dose of the drug, and side effects (sedation, lethargy, drowsiness) indicate the need to reduce the dose. Average doses are 4-6 mg/day, treatment is continued for 4-6 months after which, with good adaptation of patients, the dose is reduced at an average rate of 0.5 mg per week in order to avoid withdrawal syndrome.  At the same time, due to the longer half-life, a milder “withdrawal syndrome” is noted, there is no need for a three-time mandatory appointment, and it is easier to reduce the dose. The initial dose is usually 0.5 mg 2 times a day, with a gradual increase to 2-6 mg / day.
At the same time, due to the longer half-life, a milder “withdrawal syndrome” is noted, there is no need for a three-time mandatory appointment, and it is easier to reduce the dose. The initial dose is usually 0.5 mg 2 times a day, with a gradual increase to 2-6 mg / day.
 Attempts to gradually reduce the dose are recommended every 4 months. In some patients, the drug can be completely canceled, in others an exacerbation occurs, requiring the resumption of treatment. Intermittent breaks in treatment may help to identify patients with persistent anxiety but good BZD effect: they are especially indicated for long-term therapy. The FDA Commission (USA) in its recommendations indicates that the use of BZD for more than 4 months has not been studied. In addition, patients with personality disorders and substance abuse (including alcohol abuse) should not be treated long-term with BDD, even if they have a history.
Attempts to gradually reduce the dose are recommended every 4 months. In some patients, the drug can be completely canceled, in others an exacerbation occurs, requiring the resumption of treatment. Intermittent breaks in treatment may help to identify patients with persistent anxiety but good BZD effect: they are especially indicated for long-term therapy. The FDA Commission (USA) in its recommendations indicates that the use of BZD for more than 4 months has not been studied. In addition, patients with personality disorders and substance abuse (including alcohol abuse) should not be treated long-term with BDD, even if they have a history.  In patients with late addition of depression to PR, its atypical, erased character, high proportion of pseudosomatic (somatovegetative) and conversion disorders, rare agoraphobia, the effectiveness of TAD is usually low. This subtype of PR is closer to the diagnosis of hypochondriacal development or "somatoform disorder" according to ICD-10. Thus, the more pronounced the mental component of anxiety and the more phobic experiences are presented, the greater the effect of TAD can be expected and the less exacerbation of PR during treatment.
In patients with late addition of depression to PR, its atypical, erased character, high proportion of pseudosomatic (somatovegetative) and conversion disorders, rare agoraphobia, the effectiveness of TAD is usually low. This subtype of PR is closer to the diagnosis of hypochondriacal development or "somatoform disorder" according to ICD-10. Thus, the more pronounced the mental component of anxiety and the more phobic experiences are presented, the greater the effect of TAD can be expected and the less exacerbation of PR during treatment.  A high incidence of PP and alexithymia (i.e., the inability of patients to adequately express their experiences or talk about them) are also predictors of the low effectiveness of ABZD.
A high incidence of PP and alexithymia (i.e., the inability of patients to adequately express their experiences or talk about them) are also predictors of the low effectiveness of ABZD. 

 After a little training, many patients begin to feel free in previously avoided situations. A more formal PT may, however, be needed for prolonged and severe phobias. There are many techniques for their treatment, the common thing for which is a collision with a phobic stimulus in real life. Most important for therapeutic success is the duration of exposure: sessions lasting 2-3 hours are preferable to those lasting less than an hour. Another important condition is the frequent repetition of sessions, the prevention of the execution of the usual avoidance reaction for the patient and, if possible, the reproduction in sessions of circumstances close to real life. The effect of PT is significantly increased when it is carried out in groups, when patients, after training with imaginary situations, first, accompanied by a therapist, make joint trips, finding themselves in real phobogenic situations. An important modification of the method is the involvement of an instructed relative of the patient as a behavioral co-therapist.
After a little training, many patients begin to feel free in previously avoided situations. A more formal PT may, however, be needed for prolonged and severe phobias. There are many techniques for their treatment, the common thing for which is a collision with a phobic stimulus in real life. Most important for therapeutic success is the duration of exposure: sessions lasting 2-3 hours are preferable to those lasting less than an hour. Another important condition is the frequent repetition of sessions, the prevention of the execution of the usual avoidance reaction for the patient and, if possible, the reproduction in sessions of circumstances close to real life. The effect of PT is significantly increased when it is carried out in groups, when patients, after training with imaginary situations, first, accompanied by a therapist, make joint trips, finding themselves in real phobogenic situations. An important modification of the method is the involvement of an instructed relative of the patient as a behavioral co-therapist.