Reasons for therapy
Do I Need Therapy? Will Therapy Help?
Medically reviewed by Alex Klein, PsyD — By Carly Vandergriendt on November 24, 2020
People seek therapy for a number of reasons, from day-to-day stress to marital troubles to phobias and harmful habits. When it comes to seeking help, no problem is too big or too small.
This list includes an overview of some of the most common reasons why people seek therapy.
Substance use — whether it’s alcohol, tobacco, or drugs — is often a way of coping with an unresolved problem. The same is true of behaviors such as problem gambling and bingeing and purging.
A psychologist can help address both the problem behavior and its root cause, whether it’s stress, depression, or childhood experiences.
Psychologists also provide support for family members dealing with a loved one’s addiction. Individual and group therapy can help family members and caregivers better understand how best to support their loved one’s recovery while also coping with their own feelings.
It’s not unusual to experience stress associated with certain situations, like a performance review, a first date, or a school presentation. A therapist will work with you to identify sources of stress in your life and can help you build healthy coping strategies.
It’s also worth seeking help if you’re having difficulty managing day-to-day anxiety and stress. Chronic stress and anxiety can lead to other problems, such as sleep issues, unhealthy habits, and depression. While anxiety may never completely go away, you can learn ways to manage its symptoms.
In some cases, a therapist acts as a coach, helping you to recognize your full potential, work on communication skills, and find motivation. For many people, talking with a therapist can help them to see their problems more clearly and take action.
It’s not the same as talking with a friend. Psychologists are trained to be careful and unbiased listeners. When appropriate, your therapist might challenge you to recognize thought or relationship patterns that aren’t helping you move forward.
Depression is one of the most common health concerns in the United States, affecting people of all genders, ages, and races. According to the National Institute of Mental Health (NIMH), 17.3 million adults in the United States experienced at least one episode of major depression in 2017.
Depression makes it hard to function on a day-to-day basis. It can affect your work, relationships, sleep, energy levels, and appetite. Often, it causes overpowering feelings of hopelessness, helplessness, and guilt.
Therapy can help you explore the cause of depression and manage your symptoms, which can provide relief.
The death of a spouse, a parent, a child, or a friend can be difficult to deal with on your own. Even when you give yourself the time and the space to mourn, grief doesn’t have a timeline. Denial can cause grief and related problems to linger.
Speaking with a psychologist about what you’re feeling can help you find closure.
And because grief can be the result of other experiences in life outside of death, talking with a therapist can help you understand and work through what is related to your grief.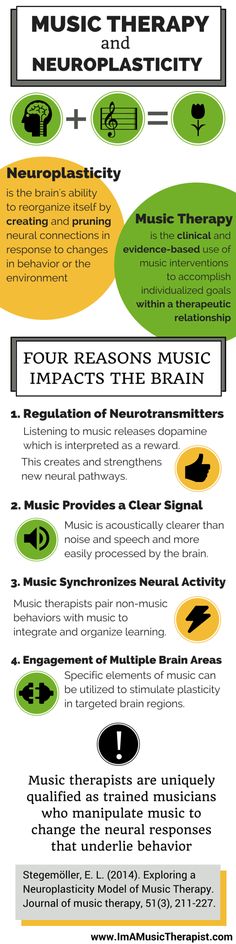
Any serious illness, whether your own or a loved one’s, can be devastating. You might feel a range of emotions, from anger and denial to sadness and regret. Therapy can help you to cope with emotions and symptoms caused by your illness.
The same applies to mental illnesses. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), mental illnesses affect an estimated one in five Americans every year. A mental illness can be a lot to deal with on your own.
Effective, evidence-based psychological treatments are available for most mental health issues.
From the fear of pregnancy and childbirth (tokophobia) to anxiety disorders such as agoraphobia, phobias cause legitimate emotional distress. Most people cope by avoiding what they fear, which can seriously restrict their everyday activities.
Even seemingly small fears, such as the fear of spiders (arachnophobia) or the fear of flowers, can be serious enough to impact everyday functioning.
Psychologists who specialize in treating phobias can help you recognize and tackle your fears using techniques such as exposure therapy and talk therapy.
Relationships can have a significant impact on how you feel. This includes your relationships with your family members, colleagues, romantic partners, and friends.
It’s not uncommon to seek help dealing with a relationship that has become a source of anxiety or distress. Therapy can help you to better understand and nurture the relationships that are important to you.
In addition to working one-on-one with clients, many psychologists also offer therapy for couples, families, and even co-workers.
Insomnia can seriously impact your everyday life, leaving you feeling drowsy in the daytime and wide awake at night.
It often has an underlying cause. While medication can help you sleep better, it won’t help you resolve whatever’s causing your insomnia.
According to the Mayo Clinic, cognitive behavioral therapy (CBT) is an effective non-drug treatment for insomnia.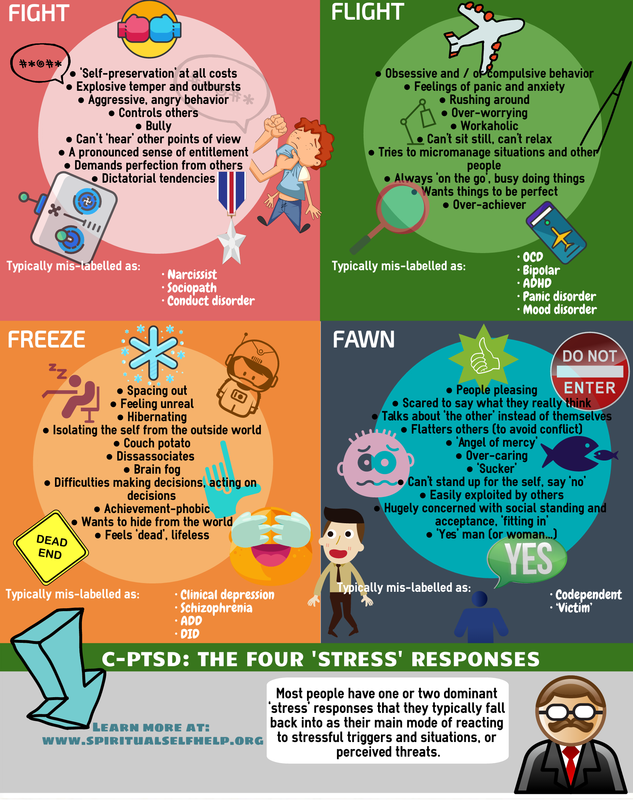 Look for a cognitive behavioral psychologist who specializes in treating insomnia.
Look for a cognitive behavioral psychologist who specializes in treating insomnia.
Life threatening events, such as crimes, accidents, and natural disasters, can stay with you long after they’re over. In time, a traumatic event can lead to post-traumatic stress disorder (PTSD).
PTSD causes symptoms such as flashbacks, avoidance, and emotional distress. It can affect all people, including children.
Psychotherapy is an effective treatment for PTSD. Psychologists use techniques such as cognitive processing therapy (CPT) and stress inoculation training (SIT) to help clients manage PTSD symptoms.
Psychologists aren’t only there to help after a problem becomes overwhelming. They can also help you plan for exciting but challenging life changes, such as moving cities, starting your own business, having a baby, or transitioning.
Taking a proactive approach can help you put your best foot forward, much in the same way that an athlete trains for a sporting event.
There are a variety of healthcare providers available for individual, couple’s, marriage, and family therapy. They typically provide counseling services and are sometimes trained to diagnose mental illnesses or administer diagnostic tests.
They typically provide counseling services and are sometimes trained to diagnose mental illnesses or administer diagnostic tests.
These providers include:
- Psychiatrists. Psychiatrists are medical doctors that specialize in diagnosing and treating psychiatric disorders. They can prescribe medication, but they don’t typically offer counseling services.
- Psychologists. Psychologists also diagnose and treat psychiatric conditions. They typically offer counseling services and other forms of therapy. Psychologists are typically not licensed to prescribe medication as part of their work. They often work closely with other healthcare providers who can.
- Psychiatric nurse practitioners. These professionals offer counseling, education, and can prescribe medication in some states.
- Counselors. Counselors include licensed professional counselors (LPCs), mental health counselors, alcohol and drug use counselors, veterans counselors, and pastoral counselors, among other types.
 They offer counseling targeted towards their area of specialization. Some are able to diagnose and treat certain conditions, but they can’t prescribe medication.
They offer counseling targeted towards their area of specialization. Some are able to diagnose and treat certain conditions, but they can’t prescribe medication. - Clinical social workers. These professionals hold a master’s degree in social work. They can provide individual and group counseling but can’t prescribe medication.
It isn’t always evident which professional you should choose. It will depend not only on your needs, access to health insurance, and budget, but also on factors beyond your control, such as specialists in your area. Keep in mind that online therapy is also available.
Looking for ways to support your mental health and well-being? Try Healthline’s FindCare tool to connect with mental health professionals nearby or virtually so you can get the care you need.
- Start with a healthcare provider. One step to finding help is to contact your family doctor to discuss your options.
 A general physician such as a family doctor can give you an overview of what’s available and possibly provide you with a referral.
A general physician such as a family doctor can give you an overview of what’s available and possibly provide you with a referral. - Ask friends, family, classmates, or colleagues. Friends and family may also be able to refer you to a therapist.
- Check with your insurance provider. If you have health insurance, you’ll want to contact your provider to find out more about what’s covered. Your provider should be able to give you contact information for therapists in your area.
- Look for a therapist online. Use a reliable database, such as the Psychologist Locator from the American Psychological Association (APA) or SAMHSA’s Behavioral Health Treatment Services Locator.
Scheduling an appointment is a great start. Finding the right therapist for you will likely mean meeting with more than one provider over time. If it’s your first time ever meeting with a therapist, keep in mind that just because things don’t click with them doesn’t mean therapy doesn’t work for you. Talk with a different therapist.
Talk with a different therapist.
If you feel discouraged, keep in mind that it’s worth it to put in the time to find someone who can support you over the long term. With the right therapist, you should be able to build trust.
Read this article in Spanish.
10 Reasons to See a Therapist
Seeking therapy, unfortunately, has long been the subject of ridicule and jest. Pursuing professional counsel for mental health concerns has been stigmatized and labeled as something that “only those with mental disorders need.”
Many have been amused by the antics of the neurotic, self-described, obsessive-compulsive Bob Wiley in the blockbuster “What About Bob.” Some may have also found humor in his complete reliance on therapy and his therapist’s prescribed “baby steps” to get through the day.
The same can be said for Adrian Monk, the obsessive-compulsive, former detective portrayed in the television series “Monk.” You may remember seeing Mr. Monk carefully sitting in his therapist’s office engaging in thoughtful talk therapy to effectively function in his germ-filled world.
Whether these and many other fictional characters portrayed their mental health conditions accurately is the subject of another article. The point is seeking therapy has too often been used in pop culture and our society as a punchline.
But effective therapy can be extremely worthwhile for many—and critically necessary for some. The brain, after all, is an organ and, like other organs, requires some qualified medical attention. Therapy can help you manage life’s varied challenges and live a more fulfilled life. It can help you understand what you’re feeling, why and how to cope. Just like visiting your doctor for regular wellness exams, or your dentist for checkups, meeting with a therapist can help keep your mental health in order. Indeed, therapy can be beneficial “just because.”
Therapy can also provide you with the needed tools to manage your emotions. Learning the art of mindfulness-based meditation can even help you take care of your own mental health and wellbeing. And couples counseling can help people work through relationship troubles and live a happier life together.
Learning the art of mindfulness-based meditation can even help you take care of your own mental health and wellbeing. And couples counseling can help people work through relationship troubles and live a happier life together.
In other words, therapy can be an important aspect in improving your overall wellness. There is, however, one caveat: therapy may not be the best option for those in crisis. For anyone having suicidal thoughts, it’s best to forego therapy in lieu of immediate crisis support to help curb any suicide ideation. The National Suicide Prevention Lifeline provides 24/7, free and confidential support for those in a crisis. And for those who may not feel comfortable talking, messaging the Crisis Text Line can immediately connect them to trained Crisis Counselors.
The same can be said for couples counseling: therapy can help, but it may not the best choice for those living in abusive relationships. Those in abusive relationships should strongly consider contacting the National Domestic Violence Hotline immediately. Therapy can then help those involved fully recover and live a happy post-crisis life, free of unhealthy relationships.
Therapy can then help those involved fully recover and live a happy post-crisis life, free of unhealthy relationships.
You’re Feeling Overwhelmingly Sad or Helpless
These feelings can actually be a sign of major depression.
You’ve Run Out of Advice from Friends and Family
However well intentioned, advice from friends and family on coping with life’s challenges may not be enough.
You’re Using Alcohol, Drugs, Porn or Other Unhealthy Coping Mechanisms
Managing painful or difficult emotions with alcohol, drugs, porn or other addictive means commonly leads to larger problems.
You or a Loved One are Living with a Chronic Health Condition
The uncertainty of serious illnesses can bring on stress, anxiety and depression. Therapists can help you see through the troubled waters to a bright horizon.
You’re Undergoing a Big Change
From a major career shift to a change in marital status or relocating to a new state, big changes can lead to emotional distress.
You’ve Recently Lost a Loved One or Close Friend
Grieving is normal and healthy. But if time passes and you’re still feeling a heavy burden from the loss of a family member, trusted friend or pet, therapy can help.
You Suspect You Have a Serious Mental Health Condition
Some of the most common mental health disorders are effectively treated with a combination of medication and therapy.
You Feel Like You’ve Lost Control
Therapy can help calm the waters of rampant substance abuse, rage, anger or other runaway emotions.
You’re Having Family Issues
Couples and family therapy can help improve communication, work through challenges and resolve conflicts. However, as mentioned earlier, couples therapy is not recommended for those in abusive relationships.
You Feel Like You Need to Talk to Someone
It’s as simple as it sounds—trust yourself. If you feel like you need help, seek it. Don’t be ashamed or embarrassed for taking action to improve your mental health, no matter the reason.
Davis Behavioral Health is here to help with life’s challenges. We have compassionate, caring and experienced mental health professionals that help our clients understand and manage their mental wellbeing. Whether it’s because you’ve recently lost a loved one, you’re feeling overwhelmed with life or just need to talk to someone, we’re here to help you improve your mental health.
The main causes of stress and the impact of art therapy on it
What is stress?
Stress is a state of mental stress that occurs in a person in the course of his activity, mainly in extremely difficult conditions. This term comes from the English word stress.
First studies.
In 1936, Hans Selye conducted numerous experiments and found that different diseases caused by different causes have the same type of body reaction. This reaction of the body, according to his observations, consists in loss of appetite, muscle weakness, increased blood pressure, loss of motivation for movements. Selye called this state the term stress.
Selye called this state the term stress.
The biggest one is school stress.
Potential sources of stress in children include school and social problems, including:
separation from close friends;
family relocation;
peer pressure;
abrupt changes in daily routine;
beginning and end of the academic year;
preparation and passing of examinations, interviews;
Excessive interest in computer games, especially aggressive ones.
Symptoms of stress in schoolchildren.
There are a number of signs of stress in children:
Mood swings;
sleep disorders;
Bedwetting;
physical discomfort, including abdominal pain and headaches;
problems concentrating, which dramatically reduces academic performance;
The child becomes withdrawn or spends a lot of time alone, avoids contact with both peers and with their loved ones, including parents.
Methods of stress relief, some of them can improve your well-being and mood.
Outdoor activities.
Vitamin therapy.
Eating foods that improve mood.
Aromatherapy.
Sports
Art Therapy
"Art Therapy"
The term "A pm-therapy " - art therapy, coined by Adrian Hill in 1938. This is a specialized form of psychotherapy based on art, primarily visual and creative activities.
...enjoy the process, unleash your creativity.
Goals of art therapy.
1. From the point of view of art - to enjoy the process, to reveal creative potential.
2. From the position of psychology - to have a therapeutic effect on the patient, to solve internal psychological problems, conflicts.
Art therapy has a number of directions, which are based on different types of creative activity.
Art therapy plays one of the leading roles in stress management. Techniques for working with stress can be divided into two groups:
1. Resource techniques where you express yourself creatively and relax.
2. Techniques for working with negative emotions, during which the negative comes out on paper, plasticine, clay.
Art therapy has a number of directions, which are based on different types of creative activity.
Music therapy - "treatment" with music.
Color Therapy.
Drawing therapy (isotherapy).
Phototherapy.
Library therapy (fairy tale therapy).
Play therapy.
Everyone can choose the listed methods of art therapy at their own discretion. All of them are great help and do not require significant material costs. If your mood has worsened, you are not able to overcome aggression, anger, despondency, fear, then turning to art, art therapy is a simple and wonderful way to solve these problems.
MAIN CAUSES AND CURRENT METHODS FOR CORRECTION OF LOW ADHERENCE TO ANTIRETROVIRAL THERAPY IN DIFFICULT PATIENTS | Musatov
1. Joint United Nations Program (UNAIDS). Global HIV statistics. Geneva, 2017, 6 p. URL: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf (June 26, 2018).
2. Consolidated guidelines on the use of antiretroviral drugs for the treatment and prevention of HIV infection. 2nd ed. Copenhagen: World Health Organization, Regional Office for Europe, 2016. 480 pp. [Consolidated guidance on the use of antiretroviral drugs for the treatment and prevention of HIV infection. 2nd ed. Copenhagen: World Health Organization, Regional Office fior Europe, 2016, 480 p. (In Russ.)].
3. Human Immunodeficiency Virus — Medicine: A Guide for Physicians / Ed. N.A. Belyakova, A.G. Rakhmanova. 2nd ed. St. Petersburg: Baltic Medical Educational Center, 2011. 656 p. [The human immunodeficiency virus — medicine: Guide for doctors. Ed. N.A.Belyakov, A.G.Rakhmanova. 2nd ed. Saint-Petersburg: Baltic medical educational center, 2011, 656 p. (In Russ.)].
N.A.Belyakov, A.G.Rakhmanova. 2nd ed. Saint-Petersburg: Baltic medical educational center, 2011, 656 p. (In Russ.)].
4. Rodger A., Cambiano V., Bruun T. Risk of HIV transmission through condomless sex in MSM couples with suppressive ART. Proceedings of the 22nd International AIDS Conference, Amsterdam, 2018, abstract WEAX0104LB.
5. Samji H., Cescon A., Hogg R.S., Modur S.P., Althoff K.N., Buchacz K. et al. Closing the gap: increases in life expectancy among treated HIVpositive individuals in the United States and Canada. PLOS One, 2014, Vol. 8, no. 12, pp. e81355.
6. HIV/AIDS surveillance in Europe. Copenhagen: World Health Organization, Regional Office for Europe, 2017, 95 p. URL: www.euro.who.int/__data/assets/pdf_file/0007/355570/20171127-Annual_HIV_Report.pdf?ua=1 (June 26, 2018).
7. On the state of sanitary and epidemiological well-being of the population in the Russian Federation in 2017: State report / Ed. A.Yu.Popova. M.: Federal Service for Supervision of Consumer Rights Protection and Human Welfare, 2017. 268 p. [State report on the state of sanitary and epidemiological welfare of the population of the Russian Federation in 2017. Moscow: Federal service for supervision of consumer rights protection and human welfare, 2017, 268 p. (In Russ.)].
268 p. [State report on the state of sanitary and epidemiological welfare of the population of the Russian Federation in 2017. Moscow: Federal service for supervision of consumer rights protection and human welfare, 2017, 268 p. (In Russ.)].
8. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization, 2003, 110 p. URL: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1 (June 26, 2018).
9. World Health Organization, Regional Office fior Europe. HIV treatment and care for children. Copenhagen: World Health Organization, Regional Office fior Europe, 2011, 50 p.
10. Belyaeva V.V., Kuimova U.A., Efremova O.S., Kozhevnikova G.M. An integrated approach to the treatment of patients with comorbidities: HIV infection and chronic hepatitis C // Medical Alphabet. 2011. Vol. 2, No. 10. P. 14–17. [Belyaeva V.V., Kuimova U.A., Efremova O.S., Kozhevnikova G.M. Complex approach to treatment of patients with combined diseases: HIV infection and chronic hepatitis C. Medical Alphabet, 2011, Vol. 2, no. 10, pp. 14–17 (In Russ.)].
Medical Alphabet, 2011, Vol. 2, no. 10, pp. 14–17 (In Russ.)].
11. Selected lectures on HIV infection / Ed. V.V. Pokrovsky. M.: GEOTAR-Media, 2015. 512 p. [Selected lectures on HIV. Ed. V.V. Pokrovsky. Moscow: GEOTAR-Media, 2015, 512 p. (In Russ.)].
12. Pokrovsky V.V., Yurin O.G., Kravchenko A.V., Belyaeva V.V., Ermak T.N., Kanestri V.G. National recommendations for dispensary observation and treatment of patients with HIV infection // Epidemiology and infectious diseases. Topical issues. 2016. No. 6. P. 1–72. [Pokrovsky V.V., Yurin O.G., Kravchenko A.V., Belyaeva V.V., Ermak T.N., Kanestri V.G. et al. National recommendations for dispensary observation and treatment of HIV patients. Epidemiology and Infectious Diseases. Topical Issue, 2016, No. 6, pp. 1–72 (In Russ.)].
13. Belyakov N.A., Levina O.S., Rybnikov V.Yu. Formation of adherence to treatment in patients with HIV infection // HIV infection and immunosuppression. 2013. V. 5, No. 1. S. 7–33. [Belyakov N. A., Levina O.S., Rybnikov V.Yu. Formation of adherence to treatment in patients with HIV infection. HIV Infection and Immunosuppressive Disorders, 2013, Vol. 5, no. 1, pp. 7–33 (In Russ.)].
A., Levina O.S., Rybnikov V.Yu. Formation of adherence to treatment in patients with HIV infection. HIV Infection and Immunosuppressive Disorders, 2013, Vol. 5, no. 1, pp. 7–33 (In Russ.)].
14. Belyaeva V.V. Strategies for the formation of adherence to the treatment of HIV infection among users of psychoactive substances // Infectious Diseases. 2013. No. 3. P. 49-54. [Belyaeva V.V. Strategies of formation of adherence to treatment of HIV infection in consumers of psychoactive substances. Infectious Diseases, 2013, no. 3, pp. 49–54 (In Russ.)].
15. Moiseeva M.V., Viktorova I.A., Trukhan D.I., Bagisheva N.V. Prognosis of low adherence to therapy in patients with arterial hypertension at the stage of primary health care // Difficult patient. 2018. No. 3. P. 16–19. [Moiseeva M.V., Viktorova I.A., Trukhan D.I., Bagysheva N.V. Forecast low adherence to therapy in patients with arterial hypertension at the stage of provision of primary health care. Difficult Patient, 2018, no. 3, pp. 16–19(In Russ.)].
3, pp. 16–19(In Russ.)].
16. Key considerations for differentiated antiretroviral therapy delivery for specific populations: children, adolescents, pregnant and breastfeeding women and key populations. Geneva: World Health Organization, 2017, 60 p.
17. Patient evaluation and antiretroviral treatment for adults and adolescents. Copenhagen: World Health Organization, Regional Office fior Europe, 2012, 85 p.
18. Konradi A.O., Polunicheva E.V. Insufficient adherence to the treatment of arterial hypertension: causes and ways of correction // Arterial hypertension. 2004. No. 3. S. 137–143. [Konradi A.O., Polunicheva E.V. Inadequate adherence to treatment of arterial hypertension: causes and ways of correction. Hypertension, 2004, no. 3, pp. 137–143 (In Russ.)].
19. Remien R., Exner T., Morin S., Ehrhardt A.A., Johnson M., Correale J. et al. Medication adherence and sexual risk behavior among HIV-infected adults. AIDS Behav., 2007, Vol. 11, no. 5, pp. 663–675.
20. Joint United Nations Program on HIV/AIDS (UNAIDS). Ending the AIDS epidemic. Progress towards the 90–90–90 targets. Geneva: UN, 2017. 196 p. [The Joint United Nations program on HIV/AIDS (UNAIDS). The end of the AIDS epidemic. Progress towards the 90–90–90 targets. Geneva: United Nations, 2017, 196 p. (In Russ.)].
21. Dolutegravir and the fixed dose combination of tenofovir/lamivudine/dolutegravir. Geneva: World Health Organization, 2018, 10 p. URL: http://www.who.int/hiv/topics/treatment/dtg-tld-briefing-web/en/ (June 26, 2018).
22. Kravchenko A.V., Orlova-Morozova E.A., Shimonova T.E., Kozyrev O.A., Nagimova F.I., Zakharova N.G. Efficacy and safety of a new Russian non-nucleoside reverse transcriptase inhibitor elsulfavirin in the first line treatment of HIV infection in combination with two nucleoside/nucleotide reverse transcriptase inhibitors - a study 96 weeks // Journal of Infectology. 2018. No. 2. S. 76–82. [Kravchenko A.V., Orlova-Morozova E.A., Shimonova T. E., Kozyrev O.A., Nagimova F.I., Zakharova N.G. et al. Efficacy and safety of the new Russian non-nucleoside reverse transcriptase inhibitor elsulfavirin in the first line of HIV treatment in combination with two nucleoside/nucleotide reverse transcriptase inhibitors — a 96-week study. Journal of Infectious Diseases, 2018, no. 2, pp. 76–82 (In Russ.)].
E., Kozyrev O.A., Nagimova F.I., Zakharova N.G. et al. Efficacy and safety of the new Russian non-nucleoside reverse transcriptase inhibitor elsulfavirin in the first line of HIV treatment in combination with two nucleoside/nucleotide reverse transcriptase inhibitors — a 96-week study. Journal of Infectious Diseases, 2018, no. 2, pp. 76–82 (In Russ.)].
23. Kanestri V.G. The contribution of the fixed dose combination of abacavir/lamivudine to improving adherence to treatment in patients with HIV infection // Epidemiology and infectious diseases. Topical issues. 2013. No. 6. P. 66–71. [Kanestri V.G. Contribution of fixed combination of doses of abacavir/lamivudine to improving adherence to treatment of patients with HIV. Epidemiology and Infectious Diseases. Topical Issue, 2013, No. 6, pp. 66–71 (In Russ.)].
24. Margolis D., Gonzalez-Garcia J., Stellbrink H.-J., Eron J., Yazdanpanah Y., Podzamczer D. et al. Long-acting intramuscular cabotegravir and rilpivirine in adults with HIV-1 infection (LATTE-2). Lancet, July 2017, Vol. 390 (10101).
Lancet, July 2017, Vol. 390 (10101).
25. Ostrovsky D.V., Khan G.N., Chaika N.A. Guidelines for multiprofessional teams on building adherence to HAART. St. Petersburg: Return, 2009. 102 p. [Ostrovsky D.V., Khan G.N., Сhaika N.A. Guide for multi-professional teams on adherence to HAART. Saint Petersburg: Return, 2009, 102 p. (In Russ.)].
26. Lennerling A., Forsberg A. Self-reported non-adherence and beliefs about medication in a Swedish kidney transplant population. OpenNurs. J., 2012, Vol. 6, pp. 41–46.
27. Belokolodov V.V. Adherence to treatment in drug addicts // Bulletin of the Chuvash University. 2014. No. 2. C. 195–199. [Belokolodov V.V. Adherence to treatment in drug addicts. Bulletin of the Chuvash University, 2014, no. 2, C. 195–199 (In Russ.)].
28. Belyaeva V.V., Konnov V.V., Kozyrina N.V. Basic definitions of the process of forming adherence to HIV treatment // Infectious Diseases. 2014. No. 2. C. 88–89. [Belyaeva V.V., Konnov V.V., Kozyrina N. V. The base definition of the process of formation of adherence to treatment of HIV infection. Infectious Diseases, 2014, no. 2, pp. 88–89 (In Russ.)].
V. The base definition of the process of formation of adherence to treatment of HIV infection. Infectious Diseases, 2014, no. 2, pp. 88–89 (In Russ.)].
29. Farinha F., Freitas F., Águeda A., Cunha I., Barcelos A. Concerns of patients with systemic lupus erythematosus and adherence to therapy. Patient Pref. Adherence, 2017, Vol. 11, pp. 1213–1219.
30. Kamal S., Nulty P., Bugnon O., Cavassini M., Schneider M. Content analysis of antiretroviral adherence enhancing interview reports. Patient Educ. Couns., 2018, Vol. 101, no. 9, pp. 1676–1682
31. Kelly A., Tong A., Tymms K., March L., Craig J.C., De Vera M. et al. Outcome measures in rheumatology - Interventions for medication adherence. Trials, 2018, Vol. 19, no. 1, pp. 204.
32. Gurevich G.L., Skryagina E.M., Astrovko A.P., Kalechits O.M., Zalutskaya O.M., Dyusmikeeva M.I. Compliance as one of the problems of drug therapy on the example of TB and TB/HIV treatment // Clinical Infectology and Parasitology. 2014. No. 3. C. 86–94. [Gurevich G.L., Skryagina E.M., Astrovko A.P., Kalechits O.M., Zalutskaya O.M., Dyusmikeeva M.I. Compliance as one of the problems of drug therapy on the example of treatment of TB and TB/HIV. Clinical Infectology and Parasitology, 2014, no. 3, pp. 86–94 (In Russ.)].
No. 3. C. 86–94. [Gurevich G.L., Skryagina E.M., Astrovko A.P., Kalechits O.M., Zalutskaya O.M., Dyusmikeeva M.I. Compliance as one of the problems of drug therapy on the example of treatment of TB and TB/HIV. Clinical Infectology and Parasitology, 2014, no. 3, pp. 86–94 (In Russ.)].
33. Normansell R., Kew K., Stovold E. Interventions to improve adherence to inhaled steroids for asthma. Cochrane Database Syst. Rev., 2017, No. 4, pp. CD012226.
34. Dworkin M., Chakraborty A., Zychowski D., Donenberg G., Novak R., Garofalo R. Self-efficacy and ability to read as factors associated with ART adherence in an HIV-infected population. Int. J. STD AIDS, 2018, No. 1. URL: DOI: 10.1177/0956462418776073.
35. Van Loggerenberg F., Grant A.D., Naidoo K., Murrman M., Gengiah S., Gengiah T.N. et al. Individualised motivational counseling to enhance adherence to ART is not superior to didactic counseling in South African patients. AIDS Behav., 2015, Vol. 19, no. 1, pp. 145–156.
36. Johnson M., Neilands T., Dilworth S., Morin S., Remien R., Chesney M. The role of self-efficacy in HIV treatment adherence. J. Behav., Med., 2007, Vol. 30, no. 5, pp. 359–370.
37. Belyaeva V.V., Degtyareva L.Yu., Kozyrina N.V., Degtyarev A.A., Orlova M.O., Konnov V.V. Commitment to maintaining the health of patients infected with HIV // VI International Conference on HIV / AIDS in Eastern Europe and Central Asia: abstracts, April 18–20, 2018 Moscow, 2018. C. 137. [Belyaeva V.V., Degtyareva L.V., Kozyrina N.V. , Degtyaryov A.A., Orlova M.O., Konnov V.V. Commitment to maintaining the health of patients infected with HIV. VI International Conference on HIV/AIDS in Eastern Europe and Central Asia, Abstracts of Papers, April 18–20 2018, Moscow, 2018, pp. 137 (In Russ.)].
38. Sweeney S., Vanable P. The association of HIV-related stigma to HIV medication adherence. AIDS Behav., 2016, Vol. 20, no. 1, pp. 29–50.
39. Ghimire S., Castelino R., Jose M., Zaidi S. Medication adherence perspectives in haemodialysis patients: a qualitative study. BMC Nephrology, 2017, Vol. 18, no. 1, pp. 167.
Medication adherence perspectives in haemodialysis patients: a qualitative study. BMC Nephrology, 2017, Vol. 18, no. 1, pp. 167.
40. Borisov A.S., Bamrah M.S., Njie G.J., Winston C., Burton D., Goldberg S. et al. Update of recommendations for use of once-weekly isoniazidrifapentine regimen to treat latent Mycobacterium tuberculosis infection. Morb. Mortal. Wkly Rep., 2018, Vol. 67, no. 25, pp. 723–726.
41. Nasibov Z. Study of ART adherence rates of people who use drugs // VI International Conference on HIV/AIDS in Eastern Europe and Central Asia: abstracts, April 18–20, 2018 Moscow, 2018. P. 133–134 . [Nasibov Z. Study of the indicators of commitment to the ART of drug abusers. VI International Conference on HIV/AIDS in Eastern Europe and Central Asia, Abstracts of Papers, April 18–20, 2018, Moscow, 2018, pp. 133–134 (In Russ.)].
42. Malta M., Strathdee S., Magnanini M., Bastos F. Adherence to antiretroviral therapy for HIV/AIDS among drug users. Addiction, 2008, Vol. 103, no. 8, pp. 1242–1257.
103, no. 8, pp. 1242–1257.
43. Rassokhin V.V., Bobreshova A.S. New in HIV medicine // HIV infection and immunosuppression. 2015. Vol. 7, No. 4. P. 92–97. [Rassokhin V.V., Bobreshova A.S. New in HIV medicine. HIV Infection and Immunosuppressive Disorders, 2015, Vol. 7, no. 4, pp. 92–97 (In Russ.)].
44. Park H., Seo S., Yoo H., Lee K. Medication adherence and beliefs about medication in elderly patients living alone with chronic diseases. Patient Pref. Adherence, 2018, Vol. 12, pp. 175–181.
45. Cantudo-Cuenca M.R., Jiménez-Galán R., Almeida-Gonzalez C.V., Morillo-Verdugo R. Concurrent use of comedications reduces adherence to ART among HIV-infected patients. J. Manag. care spec. Pharm., 2014, Vol. 20, no. 8, pp. 844–850.
46. Stepanova E.V., Zakharova N.G., Toropov S.E., Minin P.V. Side effects and optimization of HAART based on materials from the St. Petersburg AIDS Center // HIV infection and immunosuppression. 2010. vol. 2, no. 3. pp. 101–108. [Stepanova E. V., Zakharova N.G., Toropov S.E., Minin P.V. Side effects and optimization of baart based on the materials of the St. Petersburg AIDS center. HIV Infection and Immunosuppressive Disorders, 2010, Vol. 2, no. 3, pp. 101–108 (In Russ.)].
V., Zakharova N.G., Toropov S.E., Minin P.V. Side effects and optimization of baart based on the materials of the St. Petersburg AIDS center. HIV Infection and Immunosuppressive Disorders, 2010, Vol. 2, no. 3, pp. 101–108 (In Russ.)].
47. Burnevich E.Z., Tikhonova N.Yu. Ways to improve the adherence of patients with chronic hepatitis to antiviral therapy with telaprevir // Experimental and Clinical Gastroenterology. 2014. No. 3. C. 94–98. [Burnevich E.Z., Tikhonova N.Yu. Ways of increasing adherence of patients with chronic hepatitis to antiviral therapy with teleprevir. Experimental and Clinical Gastroenterology, 2014, no. 3, pp. 94–98 (In Russ.)].
48. Davtyan K., Aghabekyan S., Davtyan A., Margaryan T., Zachariah R., Acosta C. et al. Social support program for tuberculosis patients in Armenia // Panorama Public Health. 2015. No. 3. C. 260–267. [Davtyan K., Aghabekyan S., Davtyan A., Margaryan T., Zachariah R., Acosta C. Program of social support for TB patients in Armenia. Panorama Public Health, 2015, no. 3, pp. 260–267 (In Russ.)].
Panorama Public Health, 2015, no. 3, pp. 260–267 (In Russ.)].
49. McQuaid E.L. Barriers to medication adherence in asthma. Ann. Allergy Asthma Immunol., 2018, Vol. 121, no. 1, pp. 37–42.
50. Adejumo O., Malee K., Ryscavage P., Hunter S., Taiwo B. Contemporary issues on the epidemiology and antiretroviral adherence of HIV-infected adolescents in sub-Saharan Africa. J. Int. AIDS Soc., 2015, Vol. 18, no. 1, pp. 20049.
51. Handbook for the use of digital technologies to support tuberculosis medication adherence. Geneva: World Health Organization, 2017, 56 p.
52. Arnhold M., Quade M., Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation. J. Med. Internet Res., 2014, Vol. 16, no. 4, pp. e104.
53. Santo K., Chow C.K., Thiagalingam A., Rogers K., Chalmers J., Redfern J. MEDication reminder APPs to improve medication adherence in Coronary Heart Disease (MedApp-CHD) Study. Brit. Med. J. Open, 2017, Vol. 7, no. 10, pp. e017540.
7, no. 10, pp. e017540.
54. Morrissey E.C., Casey M., Glynn L., Walsh J., Molloy G.J. Smartphone apps for improving medication adherence in hypertension. Patient Pref. Adherence, 2018, Vol. 12, pp. 813–822.
55. Ahmed I., Ahmad N., Ali S., Ali S., George A., Saleem Danish H. et al. Medication adherence apps: review and content analysis. JMIR Mhealth Uhealth, 2018, Vol. 6, no. 3, pp. e62.
56. Amirkhanian Y., Kelly J., Kabakchieva E., Kirsanova A.V., Vassileva S., Takacs J. et al. A randomized social network HIV prevention trial with young MSM in Russia and Bulgaria. AIDS, 2005, Vol. 19, pp. 1897–1905
57. Kelly J.A., Amirkhanian Y.A., Kabakchieva E., Vassileva S., McAuliffe T.L., DiFranceisco W.J. et al. Prevention of HIV and STDs in high risk social networks of young Roma (Gypsy) men in Bulgaria. Brit. Med. J., 2006, Vol. 333, pp. 1098–1101.
58. Latkin C.A. Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep., 1998, Vol. 113, Suppl. 1, pp. 151–159.
Public Health Rep., 1998, Vol. 113, Suppl. 1, pp. 151–159.
59. Amirkhanian Y., Kelly J., Kuznetsova A.V., Tarima S., Musatov V.B., Yakovlev A.A., DiFranceisco W. Social network intervention boosts HIV care uptake among people living with HIV in St. Petersburg. Petersburg, Russia. IAPAC. Proceedings of the 11th International Conference on HIV Treatment and Prevention Adherence, May 2016, Fort Lauderdale, Florida, Poster presentation No. 189.
60. Côté J., Godin G., Ramirez-Garcia P., Rouleau G., Bourbonnais A., Guéhéneuc Y.G. et al. Virtual intervention to support self-management of ART among people living with HIV. J. Med. Internet Res., 2015, Vol. 17, no. 1, pp. e6.
61. Yakovlev A.A., Chaika N.A., Kelly D., Musatov V.B., Amirkhanyan Yu.A. Alcohol abuse and HIV infection // HIV infection and immunosuppression. 2017. V. 9, No. 4. C. 17–32. [Yakovlev A.A., Chaika N.A., Kelly D., Musatov V.B., Amirkhanian Yu.A. Alcohol Abuse and HIV infection. HIV Infection and Immunosuppressive Disorders, 2017, Vol. 9, no. 4, pp. 17–32 (In Russ.)].
9, no. 4, pp. 17–32 (In Russ.)].
62. Kytmanova L.Yu., Degtyarev A.A., Moskvicheva M.G. Work of a multiprofessional team with patients who are dependent on psychoactive substances receiving ART // HIV infection and immunosuppression. 2015. Vol. 7, No. 1. P. 90–96. [Kytmanova L.Yu., Degtyarev A.A., Moskvicheva M.G. Work of a multiprofessional team with patients who are dependent on psychoactive substances receiving ART. HIV Infection and Immunosuppressive Disorders, 2015, Vol. 7, no. 1, pp. 90–96 (In Russ.)].
63. Tsekhanovich A.A. Comprehensive prevention of HIV infection in high-risk groups. Experience of the St. Petersburg Charitable Foundation for Medical and Social Programs "Humanitarian Action". St. Petersburg, 2010, pp. 38–43. [Tsehanovich A.A. Complex prevention of HIV infection in high-risk groups. Experience of the Saint-Petersburg charity Fund of medical and social programs "Humanitarian action". Saint Petersburg, 2010, pp. 38–43 (In Russ.)].
64. V. Yu. Naltrexone as a means of increasing adherence to ARV therapy in HIV-infected patients with concomitant heroin addiction. acad. I.P. Pavlova. 2009. T. 16, No. 2. C. 51–54. [Walgren V.Yu., Krupitsky E.M., Zvartau E.E., Masalov D.V., Burakov A.M., TsoiPogosenin M.V. et al. Naltrexone as a means of improving adherence to antiretroviral therapy in HIV-infected patients with concomitant heroin addiction. Scientific Notes State Medical University named after Akad. I. P. Pavlov, 2009, Vol. 16, no. 2, pp. 51–54 (In Russ.)].
Naltrexone as a means of increasing adherence to ARV therapy in HIV-infected patients with concomitant heroin addiction. acad. I.P. Pavlova. 2009. T. 16, No. 2. C. 51–54. [Walgren V.Yu., Krupitsky E.M., Zvartau E.E., Masalov D.V., Burakov A.M., TsoiPogosenin M.V. et al. Naltrexone as a means of improving adherence to antiretroviral therapy in HIV-infected patients with concomitant heroin addiction. Scientific Notes State Medical University named after Akad. I. P. Pavlov, 2009, Vol. 16, no. 2, pp. 51–54 (In Russ.)].
65. Claborn K., Becker S., Operario D., Safren S., Rich J., Ramsey S. Adherence intervention for HIV-infected persons who use drugs. Addict. sci. Clin. Pract., 2018, Vol. 13, no. 1, pp. 1–11.
66. Madhombiro M., Marimbe-Dube B., Dube M., Kaiyo-Utete M., Paradzai A., Chibanda D. et al. Perceptions of alcohol use in the context of HIV treatment. HIV AIDS (Auckl.), 2018, Vol. 10, pp. 47–55.
67. Probst C., Parry C., Rehm J. HIV/AIDS mortality attributable to alcohol use in South Africa: a comparative risk assessment by socioeconomic status. Brit. Med. J. Open, 2018, Vol. 8, no. 2, pp. e017955.
Brit. Med. J. Open, 2018, Vol. 8, no. 2, pp. e017955.
68. Magidson J.F., Saal W., Nel A., Remmert J.E., Kagee A. Relationship between depressive symptoms, alcohol use, and ART adherence among HIV-infected, clinic-attending patients in South Africa. J. Health Psychol., 2017, Vol. 22, no. 11, pp. 1426–1433
69. Fedyaeva O.N., Yushchuk N.D., Sirota N.A. Prediction of adherence to ART in patients with HIV infection // Kazan Medical Journal. 2014. No. 5. P. 715–721. [Fedyaeva O.N., Yushchuk N.D., Sirota N.A. Prediction of adherence to ART in patients with HIV infection. Kazan Medical Journal, 2014, no. 5, pp. 715–721 (In Russ.)].
70. Li L., Luo S., Lan C.W., Lin C., Tuan L.A., Feng N., Tuan N.A. Alcohol use, HIV treatment adherence, and sexual risk among people with a history of injecting drug use in Vietnam. AIDS Behav., 2017, Vol. 21, Suppl. 2, pp. 167–173.
71. Kim M.H., Mazenga A., Yu X., Ahmed S., Paul M.E., Kazembe P.N., Abrams E.J. High self-reported non-adherence to antiretroviral therapy among adolescents living with HIV in Malawi: barriers and associated factors. J. Int. AIDS Soc., 2017, Vol. 20, no. 1, pp. 21437.
J. Int. AIDS Soc., 2017, Vol. 20, no. 1, pp. 21437.
72. Nkosi S., Rich E.P., Kekwaletswe C.T., Morojele N.K. Experiences of alcohol consumption and taking antiretroviral medication among men living with HIV in Tshwane, South Africa. Afr. J. AIDS Res., 2016, Vol. 15, no. 4, pp. 367–376.
73. Sileo K., Simbayi L.C., Abrams A., Cloete A., Kiene S.M. The role of alcohol use in antiretroviral adherence among individuals living with HIV in South Africa. Drug Alcohol Depend., 2016, Vol. 167, pp. 103–111.
74. Teixeira C., Dourado M., Santos M.P., Brites C. Impact of use of alcohol and illicit drugs by AIDS patients on adherence to ART in Bahia, Brazil. AIDS Res. Hum. Retroviruses, 2013, Vol. 29, no. 5, pp. 799–804.
75. Tran B.X., Nguyen L., Do C., Nguyen Q., Maher R. Associations between alcohol use disorders and adherence to ART and quality of life among people living with HIV/AIDS. BMC Public Health, 2014, Vol. 14, p. 27.
76. Kredo T., Adeniyi F.B., Bateganya M. , Pienaar E.D. Task shifting from doctors to non-doctors for initiation and maintenance of ART. Cochrane Database Syst. Rev., 2014, Issue 7, Art. no. CD007331.
, Pienaar E.D. Task shifting from doctors to non-doctors for initiation and maintenance of ART. Cochrane Database Syst. Rev., 2014, Issue 7, Art. no. CD007331.
77. Schneider M., Chersich M., Temmerman M., Parry C.D. Addressing the intersection between alcohol consumption and ART: needs assessment and design of interventions for primary healthcare workers. Global Health, 2016, Vol. 12, no. 1, p. 65.
78. Scott-Sheldon L., Carey K.B., Johnson B., Carey M.P. Behavioral interventions targeting alcohol use among people living with HIV/AIDS. AIDS Behav., 2017, Vol. 21, Supp. 2, pp. 126–143.
79. Pellowski J.A., Kalichman S.C., Kalichman M.O., Cherry C. Alcohol-antiretroviral therapy interactive toxicity beliefs and daily medication adherence and alcohol use among people living with HIV. AIDS Care, 2016, Vol. 28, no. 8, pp. 963–970.
80. Krupitsky E.M., Blokhina E.A., Lioznov D.A., Verbitskaya E.V., Yaroslavtseva T.S., Palatkin V.Ya. Efficacy of using implantable naltrexone prolong to improve ART adherence in opioid dependent HIV patients // VI International Conference on HIV/AIDS in Eastern Europe and Central Asia: abstracts, April 18–20, 2018 Moscow, 2018 pp. 138–139. [VI International Conference on HIV/AIDS in Eastern Europe and Central Asia, Abstracts of Papers, April 18–20, 2018, Moscow, 2018, pp. 138–139 (In Russ.)].
138–139. [VI International Conference on HIV/AIDS in Eastern Europe and Central Asia, Abstracts of Papers, April 18–20, 2018, Moscow, 2018, pp. 138–139 (In Russ.)].
81. Piña C., Dange A., Rawat S., Jadhav U., Arnsten J.H., Chhabra R., Patel V.V. Antiretroviral treatment uptake and adherence among MSM and transgender women with HIV in Mumbai. J. Ass. Nurses AIDS Care, 2018, Vol. 29, no. 2, pp. 310–316.
82. Micheni M., Kombo B.K., Secor A., Simoni J.M., Operario D., van der Elst E. et al. Health provider views on improving ART adherence among MSM in Coastal Kenya. AIDS Patient Care STDS, 2017, Vol. 31, no. 3, pp. 113–121.
83. Chakrapani V., Newman P.A., Shunmugam M., Dubrow R. Barriers to free ART access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care, 2011, Vol. 23, no. 12, pp. 1687–1694
84. Skogen V., Berg R., Kazentseva T., Zhukova E., Beloglazov A. Characteristics of taking ART among HIV-infected MSM in Russia // VI International Conference on HIV/AIDS in Eastern Europe and Central Asia: abstracts, April 18–20, 2018 Moscow, 2018. C. 273. [Skogen V., Berg R., Kazentseva T., Zhukova E., Beloglazov A. Characteristics of taking ART among HIV-infected MSM in Russia. VI International Conference on HIV/AIDS in Eastern Europe and Central Asia, Abstracts of Papers, April 18–20, 2018, Moscow, 2018, pp. 273 (In Russ.)].
C. 273. [Skogen V., Berg R., Kazentseva T., Zhukova E., Beloglazov A. Characteristics of taking ART among HIV-infected MSM in Russia. VI International Conference on HIV/AIDS in Eastern Europe and Central Asia, Abstracts of Papers, April 18–20, 2018, Moscow, 2018, pp. 273 (In Russ.)].
85. Lancaster K.E., Cernigliaro D., Zulliger R., Fleming P.F. HIV care and treatment experiences among female sex workers living with HIV in subSaharan Africa. Afr. J. AIDS Res., 2016, Vol. 15, no. 4, pp. 377–386.
86. Denison J., Banda H., Dennis A., Packer C., Nyambe N., Stalter R. et al. "The sky is the limit": adhering to ART and HIV self-management from the perspectives of adolescents living with HIV and their adult caregivers. J. Int. AIDS Soc., 2015, Vol. 18, no. 1, pp. 19358.
87. Kolling A., Madeira de Moura M., Silva Netto J., Brizolara R., Pascom A., Barros Perini F., Benzaken A. Overview of healthcare linkage, retention and adherence in young people living with HIV in Brazil. J. Int. AIDS Soc., 2018, Vol. 21, Suppl. 3, pp. 25–26.
J. Int. AIDS Soc., 2018, Vol. 21, Suppl. 3, pp. 25–26.
88. Ammon N., Mason S., Corkery J. Factors impacting ART adherence among HIV-positive adolescents in Sub-Saharan Africa: a systematic review. Publ. Health, 2018, Vol. 57, pp. 20–31.
89. Erlwanger A., Joseph J., Gotora T., Muzunze B., Orne-Gliemann J., Mukungunugwa S. et al. Patterns of HIV care clinic attendance and adherence to ART among pregnant and breastfeeding women living with HIV in the context of Option B+ in Zimbabwe. J. Acquir. Immune Defic. Syndr., 2017, Vol. 75, Suppl. 2, pp. S198-S206.
90. Kacanek D., Angelidou K., Williams P., Chernoff M., Gadow K., Nachman S. Psychiatric symptoms and antiretroviral nonadherence in US youth with perinatal HIV. AIDS, 2015, Vol. 29, pp. 1227–1237.
91. Vreeman R., Ayaya S., Musick B., Yiannoutsos C., Cohen C.R., Nash D. et al. Adherence to ART in a clinical cohort of HIV-infected children in East Africa. PLoS One, 2018, Vol. 13, no. 2, pp. e0191848.
92. Rakhmanova A.G., Yastrebova E.B., Samarina A.V. Organization and results of medical and social assistance to women and children living with HIV // HIV infection and immunosuppression. 2012. V. 4, No. 1. P. 9-19. [Rakhmanova A.G., Yastrebova E.B., Samarina A.V. Organization and results of medico-social assistance to women and children living with HIV. HIV Infection and Immunosuppressive Disorders, 2012, Vol. 4, no. 1, pp. 9–19 (In Russ.)].
Rakhmanova A.G., Yastrebova E.B., Samarina A.V. Organization and results of medical and social assistance to women and children living with HIV // HIV infection and immunosuppression. 2012. V. 4, No. 1. P. 9-19. [Rakhmanova A.G., Yastrebova E.B., Samarina A.V. Organization and results of medico-social assistance to women and children living with HIV. HIV Infection and Immunosuppressive Disorders, 2012, Vol. 4, no. 1, pp. 9–19 (In Russ.)].
93. Konysheva T.V., Nozhkina N.V., Podymova A.S. Study of the epidemiological features of morbidity and the organization of medical and social support for HIV-infected convicts // Bulletin of the Ural Medical Academic Science. 2012. No. 1. P. 14–18. [Konysheva T.V., Nozhkina N.V., Podymova A.S. Research of epidemiological features of morbidity and organization of medical and social support of HIV-infected convicts. Bulletin of the Ural Medical Academic Science, 2012, no. 1, pp. 14–18 (In Russ.)].
94. Zagdyn Z.M., Danilova T.I., Kovalev N. Yu., Kovelenov A.Yu., Belyakov N.A., Rumman A. et al. Screening for tuberculosis of HIV-positive former and serving sentences prisoners and persons without a fixed place of residence // Journal of Infectology. 2017. No. 1. S. 76–84. [Sagdyn Z.M., Danilova T.I., Kovalev N.Yu., Kovelenov A.Yu., Belyakov N.A. Rumman A. andothers. Screening for TB HIV-positive former and sentenced prisoners and persons without fixed residence. Journal of Infectology, 2017, no. 1, pp. 76–84 (In Russ.)].
Yu., Kovelenov A.Yu., Belyakov N.A., Rumman A. et al. Screening for tuberculosis of HIV-positive former and serving sentences prisoners and persons without a fixed place of residence // Journal of Infectology. 2017. No. 1. S. 76–84. [Sagdyn Z.M., Danilova T.I., Kovalev N.Yu., Kovelenov A.Yu., Belyakov N.A. Rumman A. andothers. Screening for TB HIV-positive former and sentenced prisoners and persons without fixed residence. Journal of Infectology, 2017, no. 1, pp. 76–84 (In Russ.)].
95. Adefolalu A.O. Cognitive-behavioral theories and adherence: Application and relevance in antiretroviral therapy. S. Afr. J. HIV Med., 2018, Vol. 19, no. 1, pp. 762–768.
96. Bucek A., Leu C., Benson S., Warne P., Abrams E., Elkington K. et al. Psychiatric disorders, antiretroviral medication adherence and viremia in a cohort of perinatally HIV-infected adolescents and young adults. Pediatr. Infect. Dis. J., 2018, Vol. 37, no. 7, pp. 673–677.
97. Awori V., Mativo P., Yonga G., Shah R.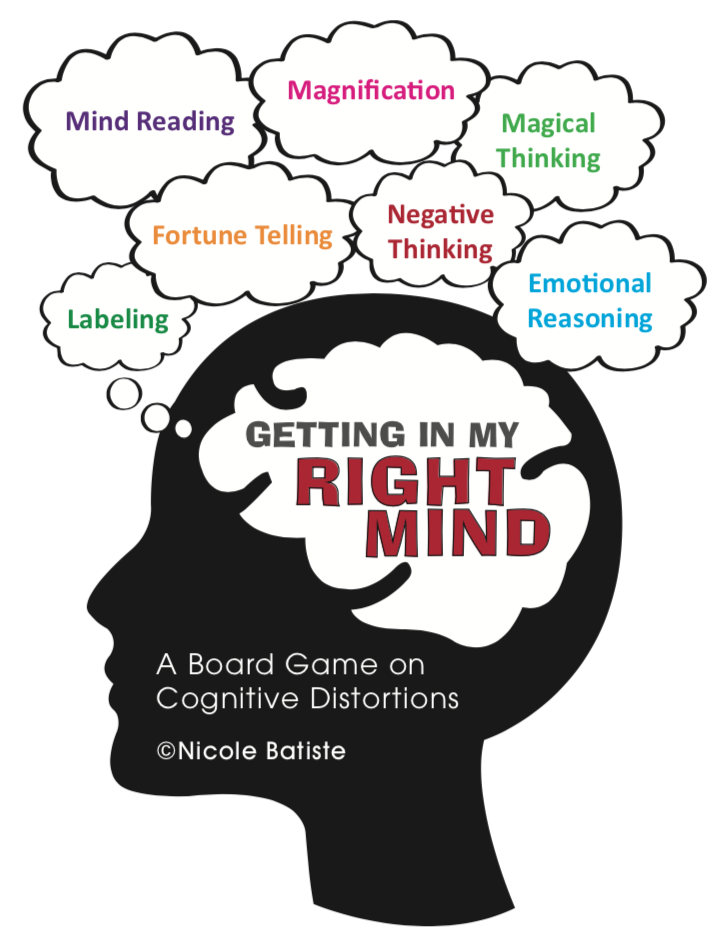 The association between asymptomatic and mild neurocognitive impairment and adherence to ART among people living with HIV. S. Afr. J. HIV Med., 2018, Vol. 19, no. 1, pp. a674.
The association between asymptomatic and mild neurocognitive impairment and adherence to ART among people living with HIV. S. Afr. J. HIV Med., 2018, Vol. 19, no. 1, pp. a674.
98. Pinheiro C.A., Mattos Souza L., Motta J., Kelbert E., Martins C., Souza M.S. et al. Aging, neurocognitive impairment and adherence to ART in HIV-infected individuals. Braz. J. Infect. Dis., 2016, Vol. 20, no. 6, pp. 599–604.
99. Kornilova Z.Kh., Demikhova O.V., Oprishchenko S.A., Polyakov A.A. Medico-social aspects in patients with newly diagnosed tuberculosis in the late stages of HIV infection // Medical Bulletin of Bashkortostan. 2017. No. 5. P. 10–15. [Kornilova Z.Kh., Demikhova O.V., Oprishchenko S.A., Polyakov A.A. Medico-social aspects of patients with newly diagnosed tuberculosis in the late stages of HIV infection. Medical Bulletin of Bashkortostan, 2017, no. 5, pp. 10–15 (In Russ.)].
100. Korzh E.V., Podchos N.A., Izvekova T.S., Malyavko N.A. Antiretroviral therapy in HIV-infected patients with tuberculosis // University Clinic. 2017. T. 4–1, No. 25, pp. 95–100. [Korzh E.V., Podzcas N.A., Izvekova T.S., Malyavko N.A. Antiretroviral therapy in HIV-infected patients with tuberculosis. University Clinic, 2017, Vol. 4–1, no. 25, pp. 95–100 (In Russ.)].
2017. T. 4–1, No. 25, pp. 95–100. [Korzh E.V., Podzcas N.A., Izvekova T.S., Malyavko N.A. Antiretroviral therapy in HIV-infected patients with tuberculosis. University Clinic, 2017, Vol. 4–1, no. 25, pp. 95–100 (In Russ.)].
101. Ryzhkov S.I., Glebova O.A., Shovkun L.A. Factors influencing adherence to treatment of patients with tuberculosis // Chief Doctor of the South of Russia. 2017. No. 2. S. 72–74. [Ryzhkov S.I., Glebova O.A., Shovkun L.A. Factors affecting the adherence to treatment of tuberculosis patients. Chief Physician of the South of Russia, 2017, no. 2, pp. 72–74 (In Russ.)].
102. Yuranova M.A., Ruzanov D.Yu., Buynevich I.V. Analysis of factors influencing the formation of adherence to treatment of patients with tuberculosis // Problems of health and ecology. 2013. No. 1. P. 45–51. [Yuranova M.A., Ruzanov D.Yu. Analysis of factors influencing the formation of adherence to treatment of tuberculosis patients. Problems of Health and Ecology, 2013, no. 1, pp. 45–51 (In Russ.