Lorazepam high blood pressure
Effects of lorazepam on film-induced differentiated emotions in healthy volunteers
Clinical Trial
. 1997;11(5):466-75.
doi: 10.1111/j.1472-8206.1997.tb00210.x.
C Garcia 1 , P Philippot, B Lacarelle, M Valli, B Rimé, B Bruguerolle, O Blin
Affiliations
Affiliation
- 1 Clinical Pharmacology & CPCET, Timone Hospital, Marseille, France.
- PMID: 9342601
- DOI: 10.1111/j.1472-8206.1997.tb00210.x
Clinical Trial
C Garcia et al. Fundam Clin Pharmacol. 1997.
. 1997;11(5):466-75.
doi: 10.1111/j.1472-8206.1997.tb00210.x.
Authors
C Garcia 1 , P Philippot, B Lacarelle, M Valli, B Rimé, B Bruguerolle, O Blin
Affiliation
- 1 Clinical Pharmacology & CPCET, Timone Hospital, Marseille, France.
- PMID: 9342601
- DOI: 10.1111/j.1472-8206.1997.tb00210.x
Abstract
We studied the effects of lorazepam, a benzodiazepine, on differentiated emotions in healthy volunteers.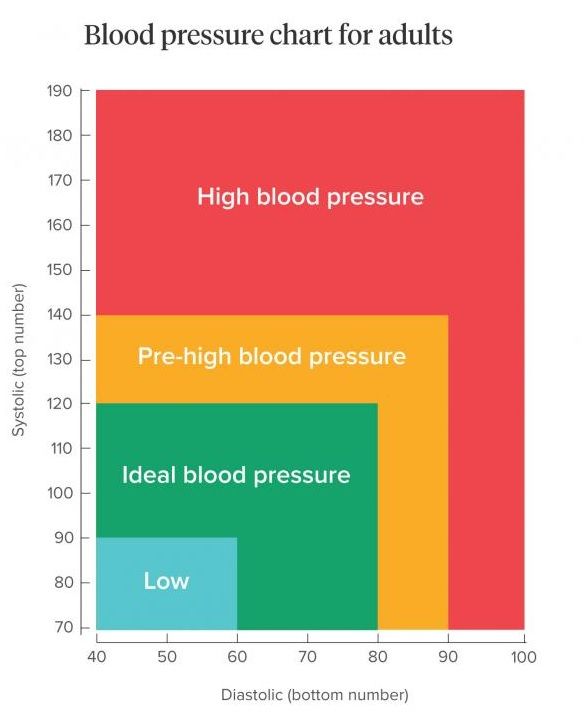 In order to induce differentiated emotions, film excerpts were selected on the basis of the type of emotion they induced (fear, anger and for affective tone neutral film). For 6 days (D1 to D6), ten healthy volunteers received lorazepam (1 mg bid) or placebo in a randomized cross-over double-blind trial. During each treatment period, emotional induction occurred on D4, D5 and D6. One film excerpt (fear, anger or neutral) was presented each morning after relaxation. Evaluation was performed before and after each emotional induction and included questionnaires (Differential Emotions Scale and physical activation visual analog scales), and neurophysiological parameters (systolic and diastolic blood pressure, heart rate and norepinephrine levels). Globally, the film excerpts induced the predicted emotions. An analysis of variance was undertaken and revealed a significant effect of lorazepam versus placebo. On the Differential Emotions Scale and during fear induction, lorazepam induced a significantly higher increase in fear, anxiety and disgust emotions than placebo, whereas no effect was observed after anger induction.
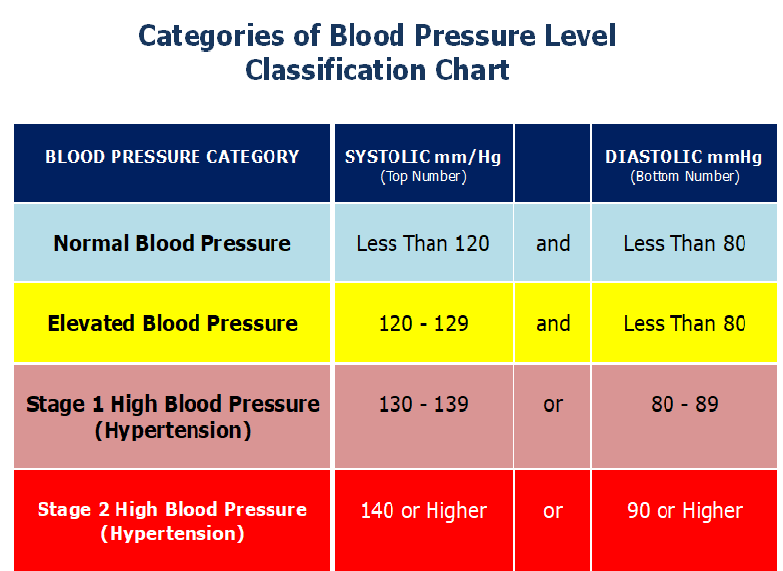
In order to induce differentiated emotions, film excerpts were selected on the basis of the type of emotion they induced (fear, anger and for affective tone neutral film). For 6 days (D1 to D6), ten healthy volunteers received lorazepam (1 mg bid) or placebo in a randomized cross-over double-blind trial. During each treatment period, emotional induction occurred on D4, D5 and D6. One film excerpt (fear, anger or neutral) was presented each morning after relaxation. Evaluation was performed before and after each emotional induction and included questionnaires (Differential Emotions Scale and physical activation visual analog scales), and neurophysiological parameters (systolic and diastolic blood pressure, heart rate and norepinephrine levels). Globally, the film excerpts induced the predicted emotions. An analysis of variance was undertaken and revealed a significant effect of lorazepam versus placebo. On the Differential Emotions Scale and during fear induction, lorazepam induced a significantly higher increase in fear, anxiety and disgust emotions than placebo, whereas no effect was observed after anger induction. Lorazepam also induced a significantly higher increase in diastolic and systolic blood pressure with no change in heart rate, and physical activation items ("tears" and "faster breathing") without no significant change in norepinephrine. In conclusion, our results are consistent with an overall increase in emotional reactivity with lorazepam (1 mg bid) as compared to placebo. The pertinence of film-induced differentiated emotions has to be confirmed for clinical pharmacological use.
Lorazepam also induced a significantly higher increase in diastolic and systolic blood pressure with no change in heart rate, and physical activation items ("tears" and "faster breathing") without no significant change in norepinephrine. In conclusion, our results are consistent with an overall increase in emotional reactivity with lorazepam (1 mg bid) as compared to placebo. The pertinence of film-induced differentiated emotions has to be confirmed for clinical pharmacological use.
Similar articles
-
Effects of lorazepam on emotional reactivity, performance, and vigilance in subjects with high or low anxiety.
Garcia C, Micallef J, Dubreuil D, Philippot P, Jouve E, Blin O. Garcia C, et al. J Clin Psychopharmacol. 2000 Apr;20(2):226-33. doi: 10.1097/00004714-200004000-00016. J Clin Psychopharmacol. 2000. PMID: 10770462 Clinical Trial.

-
Neutral and emotional episodic memory: global impairment after lorazepam or scopolamine.
Kamboj SK, Curran HV. Kamboj SK, et al. Psychopharmacology (Berl). 2006 Nov;188(4):482-8. doi: 10.1007/s00213-006-0552-7. Epub 2006 Sep 19. Psychopharmacology (Berl). 2006. PMID: 17047934 Clinical Trial.
-
Pharmacological manipulations of arousal and memory for emotional material: effects of a single dose of methylphenidate or lorazepam.
Brignell CM, Rosenthal J, Curran HV. Brignell CM, et al. J Psychopharmacol. 2007 Sep;21(7):673-83. doi: 10.1177/0269881107077351. Epub 2007 Jul 2. J Psychopharmacol. 2007. PMID: 17606475 Clinical Trial.
-
The effects of lorazepam on skin conductance responses to aversive stimuli in healthy subjects.

Siepmann M, Heine B, Kluge A, Ziemssen T, Mück-Weymann M, Kirch W. Siepmann M, et al. Clin Auton Res. 2007 Jun;17(3):160-4. doi: 10.1007/s10286-007-0407-2. Epub 2007 Mar 27. Clin Auton Res. 2007. PMID: 17390103 Clinical Trial.
-
A comparative study on the clinical effects of flunitrazepam and lorazepam.
Mansikka M, Kangas L, Kanto J. Mansikka M, et al. Int J Clin Pharmacol Ther Toxicol. 1980 Jul;18(7):320-1. Int J Clin Pharmacol Ther Toxicol. 1980. PMID: 6107279 Clinical Trial.
See all similar articles
Cited by
-
Effect of risperidone versus haloperidol on emotional responding in schizophrenic patients.
Fakra E, Khalfa S, Da Fonseca D, Besnier N, Delaveau P, Azorin JM, Blin O.
 Fakra E, et al. Psychopharmacology (Berl). 2008 Oct;200(2):261-72. doi: 10.1007/s00213-008-1203-y. Epub 2008 Jun 25. Psychopharmacology (Berl). 2008. PMID: 18575849 Clinical Trial.
Fakra E, et al. Psychopharmacology (Berl). 2008 Oct;200(2):261-72. doi: 10.1007/s00213-008-1203-y. Epub 2008 Jun 25. Psychopharmacology (Berl). 2008. PMID: 18575849 Clinical Trial. -
Relations between emotion and conscious recollection of true and false autobiographical memories: an investigation using lorazepam as a pharmacological tool.
Pernot-Marino E, Danion JM, Hedelin G. Pernot-Marino E, et al. Psychopharmacology (Berl). 2004 Aug;175(1):60-7. doi: 10.1007/s00213-004-1776-z. Epub 2004 Mar 9. Psychopharmacology (Berl). 2004. PMID: 15007596
Publication types
MeSH terms
Substances
What Does Ativan Do to Your Heart?
Benzodiazepines or benzos are central nervous system depressants that increase levels of GABA (gamma-aminobutyric acid) in the brain to reduce nerve activity and produce relaxation.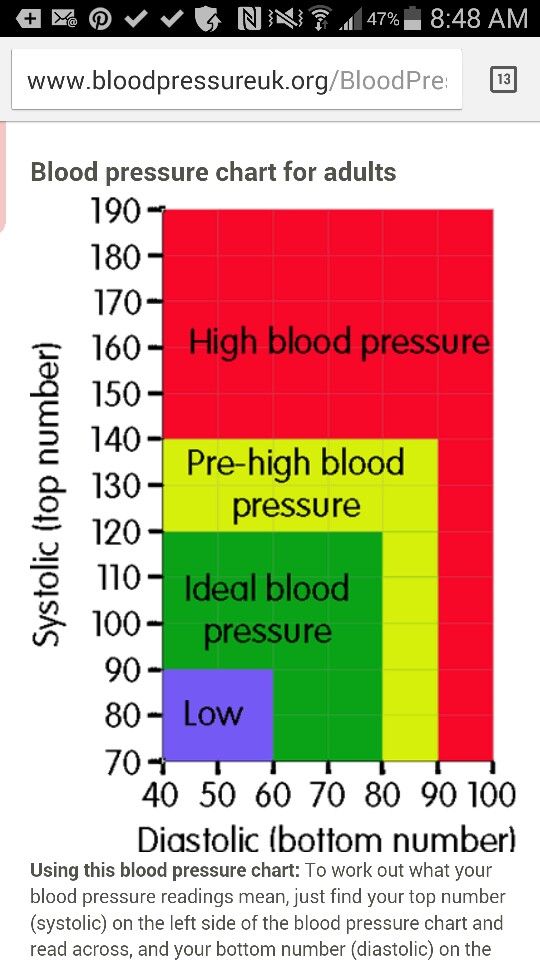 GABA works by blocking brain signals (neurotransmissions), reducing nerve activity, and making drugs like Ativan effective medications for seizures and anxiety disorders. But while it may help treat some conditions, what does Ativan do to your heart? This is a concerning topic for those taking this drug regularly for their conditions.
GABA works by blocking brain signals (neurotransmissions), reducing nerve activity, and making drugs like Ativan effective medications for seizures and anxiety disorders. But while it may help treat some conditions, what does Ativan do to your heart? This is a concerning topic for those taking this drug regularly for their conditions.
How Does Ativan Affect Your Heart?
Despite being a prescription drug, Ativan poses the threat of tolerance and addiction because of its impact on the brain, which is why it’s only recommended for short-term use. However, anxiety disorders, insomnia, and seizures aren’t usually short-term problems. As a result, when this drug is no longer an option for people who once took it for their conditions, they may try to self-medicate by obtaining it illegally or doctor shopping (going to several doctors for a prescription).
Unfortunately, because of benzos’ effects on the brain, long-term abuse often leads to addiction. With an Ativan addiction comes a variety of health issues, such as heart problems. Ativan affects the heart by slowing your heart rate and lowering your blood pressure. This drug depresses the central nervous system, and physiological functions like breathing, heart rate, blood pressure, and circulation are reduced, contributing to relaxation.
Ativan affects the heart by slowing your heart rate and lowering your blood pressure. This drug depresses the central nervous system, and physiological functions like breathing, heart rate, blood pressure, and circulation are reduced, contributing to relaxation.
Bradycardia (Slow Heart Rate)
Although these side effects are common in people who take Ativan, they can become dangerous when the drug is abused; this includes taking a higher dose than directed and mixing it with other drugs or alcohol. Otherwise known as bradycardia, having a slower than normal heart rate can have a huge impact as, usually, adults have a resting heartbeat of between 60 and 100 times a minute.
Although these side effects are common in people who take Ativan, they can become dangerous when the drug is abused; this includes taking a higher dose than directed and mixing it with other drugs or alcohol. Otherwise known as bradycardia, having a slower than normal heart rate can have a huge impact as, usually, adults have a resting heartbeat of between 60 and 100 times a minute.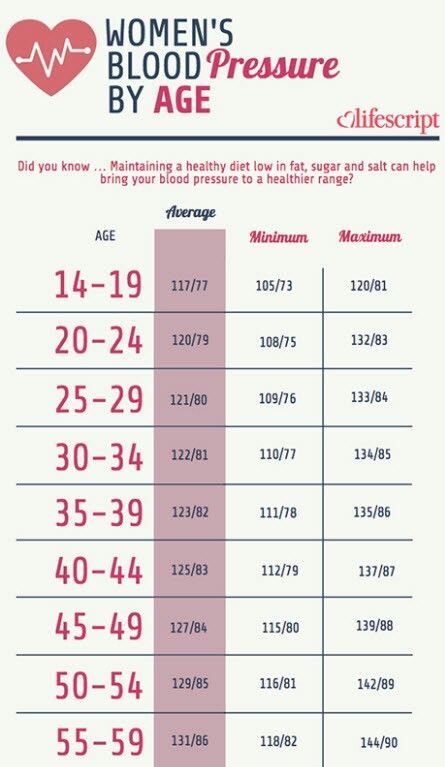
While it’s normal for Ativan to reduce your heart rate slightly when taking it as prescribed, if abused or mixed with other depressants like alcohol, it can potentially lead to heart attack and sudden heart failure.
Hypotension (Low Blood Pressure)
Additionally, not only does Ativan lower heart rate, but it can also lower your blood pressure, which can also take a toll on the heart. Blood pressure is the pressure of blood in your arteries, which carry your blood from your heart to the rest of your body. You need a certain amount of pressure to get the blood to your body.
Also known as hypotension, low blood pressure causes your heart rate to increase, and the blood vessels in other parts of your body constrict or narrow to help maintain blood pressure. If your heart rate doesn’t increase enough, or your blood vessels don’t constrict enough, your blood pressure drops.
Although rare, severe hypotension can lead to shock, which can be fatal. More commonly, however, hypotension makes the heart work harder to maintain blood pressure and also prevents the heart from getting blood to other areas of the body. Hypotension can also cause injuries related to fainting and falling.
Hypotension can also cause injuries related to fainting and falling.
Long-Term Effects of Ativan on the Heart
So, what does Ativan do to your heart over time? Because Ativan is usually prescribed for short-term use, those who take it for longer than a few weeks usually obtain it illegally and abuse it. When taken in larger doses than recommended, lorazepam’s side effects can become worse, increasing the individual’s potential for heart, liver, and kidney problems as well as overdose. Taking benzos like Ativan with alcohol can also intensify the effects of lorazepam on the heart.
The effects of Ativan long-term use on the heart include:
- Hypotension
- Changes in heart rate
- Heart rhythm problems
- Circulatory problems
- Cardiac arrest
Ativan can also cause heart problems if the person stops taking it suddenly, which can result in heart arrhythmia or even heart attack. Withdrawal symptoms are common in people who are physically dependent on drugs of abuse when they suddenly reduce or stop taking them. These withdrawal symptoms can become complicated, which is why a medically monitored detox is recommended for people who want to quit a particular drug or alcohol.
These withdrawal symptoms can become complicated, which is why a medically monitored detox is recommended for people who want to quit a particular drug or alcohol.
Finding Lorazepam Addiction Treatment
Long-term Ativan abuse can lead to a multitude of problems in addition to low blood pressure and changes in heart rhythm. A common side effect of chronic lorazepam use is addiction, a chronic disease characterized by uncontrollable substance abuse. If you’re addicted to this drug, the good news is that you aren’t alone.
Once patients at our Delaware drug rehab have completed their medical detox programs, they can then move on to one of our substance-specific programs. In addition to detox, we also offer benzo addiction treatment on a residential level of care for those who are addicted to drugs like Ativan, Valium, and Xanax. During their treatment, patients may also receive drug therapy – such as cognitive or dialectical behavior therapy – to learn how to regain control over their thoughts and actions.
Our Milford treatment center is dedicated to the safety and well-being of our patients. For more information regarding Ativan (lorazepam) addiction and treatment options available at our inpatient drug rehab, call Banyan Treatment Centers Delaware today at 888-280-4763.
Related Readings:
- Benzos and Weight Gain
- Benzodiazepines and Breastfeeding: Is It Safe?
- How Long Benzos Stay in Your System
Arpimed
Tell your doctor if you are taking, have recently taken or might take any other medicines. It is especially important to note the following drugs:
If necessary, your doctor will reduce the dose of these drugs before you use lorazepam.
Avoid alcohol while taking lorazepam as this may increase the sedative properties of the drug.
Tell your doctor or pharmacist if you are taking Lorazepam before using any other medicines or when you are hospitalized.
Some elderly patients may experience dizziness and fainting after taking Lorazepam.
When taking Lorazepam, there is a risk of developing addiction, which can lead to a gradual decrease in effectiveness after several weeks of taking Lorazepam.
Lorazepam has the potential to develop dependence, particularly in patients with a history of alcohol and/or recreational drug abuse.
With the usual regimen of lorazepam, the development of dependence is unlikely, but the risk increases with increasing dose and duration of treatment, as well as in patients with a history of alcohol and / or recreational drug abuse, or in patients with a personality disorder. Therefore, lorazepam should be avoided in patients with a history of alcohol and/or recreational drug abuse.
Dependence can lead to the development of a withdrawal syndrome, especially when treatment is stopped abruptly. Therefore, it is necessary to cancel the drug gradually.
When taking lorazepam for more than 4 weeks, your doctor should conduct a study of the peripheral blood picture, as well as a biochemical blood test for liver markers, since drugs in this group can lead to impaired liver function.
Long-term use of Lorazepam may lead to the development of drug dependence. Therefore, Lorazepam is usually prescribed in short courses lasting from several days to 4 weeks, including a period of dose reduction and drug withdrawal. This reduces the risk of developing drug dependence or adverse side effects observed when the drug is discontinued. (See section "Cancellation of Lorazepam").
The dose of Lorazepam should be increased gradually to avoid side effects.
How to take Lorazepam
Lorazepam should be taken exactly as directed by your doctor. If you have any doubts, then you should consult with your doctor.
When Lorazepam is used to treat anxiety and insomnia, treatment usually lasts from a few days to 4 weeks, including a period of dose reduction and drug withdrawal.
The physician should prescribe the lowest effective dose, calculated for the shortest possible period of taking the drug.
Lorazepam tablets should be swallowed with water.
Adults and children over 13 years of age
For anxiety, the daily dose of Lorazepam is 1-4 mg taken in divided doses. Your healthcare provider will determine how often you should take Lorazepam. It is not recommended to take Lorazepam to children under 12 years of age with anxiety.
For sleep disturbances, 1-2 mg Lorazepam at bedtime is prescribed. Before taking the drug, you must be sure that you can sleep for 7-8 hours.
Lorazepam 2-3 mg is given the night before surgery and 2-4 mg 1-2 hours before surgery.
Children 5 to 13 years old
For surgery, the dose is usually 0.5-2.5 mg (depending on your child's weight) taken one hour before the procedure.
Lorazepam is not recommended for use in children 5 to 13 years of age for the treatment of anxiety and sleep disorders, and in children under 5 years of age.
Elderly
The physician should prescribe lorazepam to elderly or malnourished patients at low doses.
The drug may be effective at half or even less than the recommended dose in elderly patients, but if necessary, the dose should be adjusted.
Patients with renal and hepatic insufficiency
In case of impaired renal function or mild to moderate hepatic insufficiency, Lorazepam is allowed to be taken only in low doses.
Lorazepam is contraindicated in patients with severe hepatic impairment.
If you forget to take Lorazepam
If you forget to take Lorazepam to treat anxiety and if less than 3 hours have passed from your scheduled appointment time, you should take it as soon as you remember. If more than 3 hours have passed from the appointed time, do not worry, take the next dose at the appointed time. Do not take a double dose to make up for a missed one.
If you forget to take Lorazepam to treat a sleep disorder, take it if you are sure you can sleep for 7-8 hours after taking the drug.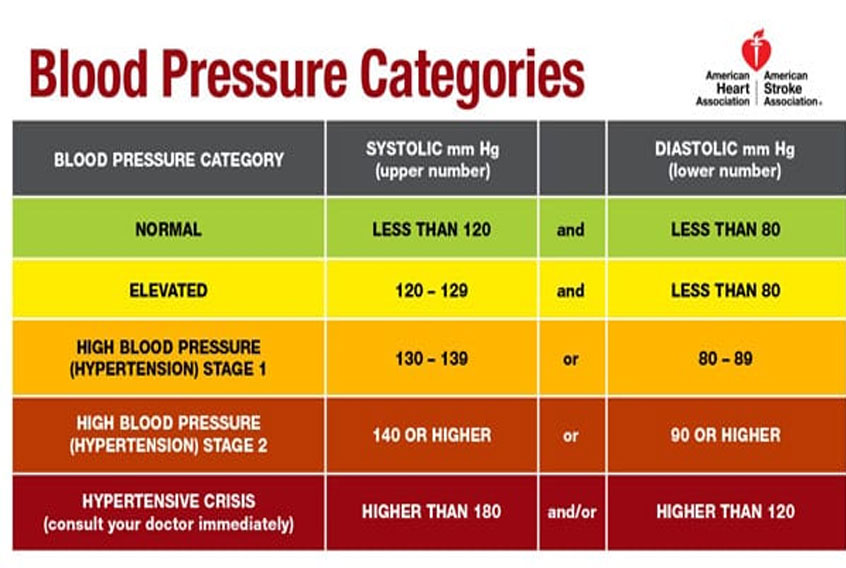
If you have taken more Lorazepam than recommended
If you have taken more Lorazepam than prescribed by your doctor, get medical help right away, call your doctor or go to the nearest hospital. Take the medicine package with you, even if there are no pills left.
Stopping Lorazepam
After completing the prescribed course of treatment, your doctor will decide whether to continue further treatment.
The dose and frequency of lorazepam should be reduced gradually until the drug is discontinued. This allows your body to adjust to the absence of Lorazepam and reduce the risk of adverse effects when the drug is discontinued. Your doctor will explain to you how to do this.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Withdrawal
Abrupt discontinuation of Lorazepam may result in withdrawal symptoms such as headaches, muscle pain, anxiety, tension, depression, restlessness, dizziness, nausea, diarrhea, loss of appetite, irritability, confusion, confusion agitation, tremors, abdominal pain, heart rhythm disturbances, short-term memory loss, fever, and sweating. Possible relapse of insomnia. If you have any of these symptoms, contact your doctor.
Possible relapse of insomnia. If you have any of these symptoms, contact your doctor.
Do not stop taking Lorazepam suddenly. This can lead to more severe withdrawal symptoms such as loss of sense of reality, feelings of unreality or detachment from everyday life, loss of the ability to feel emotions.
Some patients experience numbness or tingling of the hands or feet, vomiting, ringing in the ears, muscle twitches, hallucinations, seizures, and hypersensitivity to light, sound, and touch. If you have any of these symptoms, contact your doctor immediately.
Treatment of hypertension complicated by anxiety uMEDp
Psychosomatic disorders include somatogenic disorders, psychogenic disorders in somatic diseases (due to iatrogeny), somatized mental disorders, as well as various somatic diseases, in the origin of which stress factors matter, somatic complications some mental illnesses.
Patients with AH are characterized by personal characteristics of patients, expressed by anxious suspiciousness, mental rigidity, a tendency to fixate on negative experiences along with high activity, desire for leadership, and high self-control of behavior.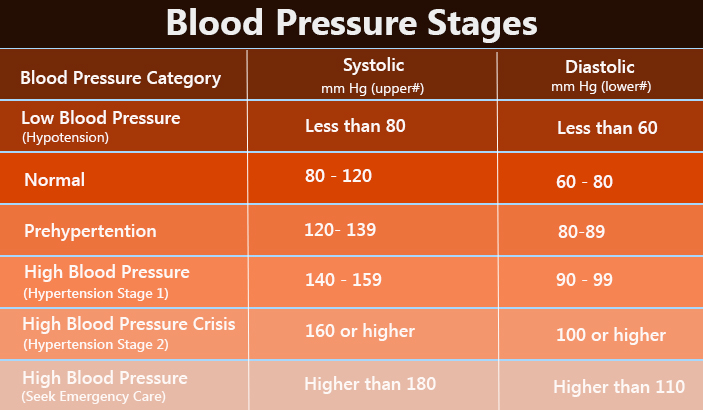 Patients with hypertension are characterized by a special sensitivity, uncontrolled anxiety reactions, which are expressed in the rise in blood pressure (BP) when it is measured (the so-called white coat hypertension). In patients with hypertension, more frequent occurrence of mental adaptation disorders with anxiety-depressive symptoms is noted, the influence of anxiety-phobic and panic disorders on the course of hypertension has been established [3, 4]. Finally, at the remote stages of AH, psychoorganic disorders of various structure and depth are formed - from emotionally labile, cerebrosthenic, anxiety-depressive organic syndromes to manifestations of dementia due to dyscirculatory encephalopathy.
Patients with hypertension are characterized by a special sensitivity, uncontrolled anxiety reactions, which are expressed in the rise in blood pressure (BP) when it is measured (the so-called white coat hypertension). In patients with hypertension, more frequent occurrence of mental adaptation disorders with anxiety-depressive symptoms is noted, the influence of anxiety-phobic and panic disorders on the course of hypertension has been established [3, 4]. Finally, at the remote stages of AH, psychoorganic disorders of various structure and depth are formed - from emotionally labile, cerebrosthenic, anxiety-depressive organic syndromes to manifestations of dementia due to dyscirculatory encephalopathy.
Thus, in the clinical picture of hypertension at various stages of its course, certain mental disorders are detected with predominant anxiety symptoms in the structure of various disorders. It is known that anxiolytic agents have long been used in the complex therapy of hypertension [2].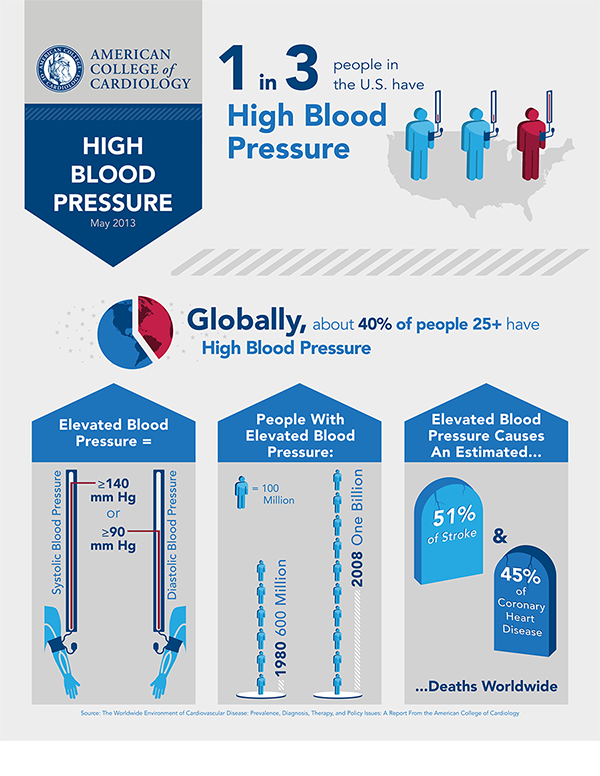 In 1950 G.F. Lang wrote that overexcitation of the hypothalamic pressor centers, caused by overexcitation of the emotional sphere, plays a decisive role in the origin of hypertension, so he recommended including sedatives and hypnotics, in particular barbiturates, in the therapy complex. Large prospective studies have shown that anxiety and depression are independent risk factors for both the development of hypertension and the survival of patients with cardiovascular pathology [5].
In 1950 G.F. Lang wrote that overexcitation of the hypothalamic pressor centers, caused by overexcitation of the emotional sphere, plays a decisive role in the origin of hypertension, so he recommended including sedatives and hypnotics, in particular barbiturates, in the therapy complex. Large prospective studies have shown that anxiety and depression are independent risk factors for both the development of hypertension and the survival of patients with cardiovascular pathology [5].
Anxiety-depressive disorders complement the clinical picture of the disease not only with painful subjective experiences, but also with somatovegetative disorders - cardialgia, tachycardia, shortness of breath, increased blood pressure during a panic attack, sleep disturbances, and an increase in crisis states [6].
In the works of cardiologists, neurologists, a positive effect of tranquilizers, antidepressants of various structures in the complex therapy of AH has been convincingly shown. The COORDINATE study completed to date has confirmed the negative impact of anxiety-depressive disorders in cardiovascular diseases, the effectiveness of the use of the antidepressant tianeptine in the treatment of hypertension. A number of studies indicate the effectiveness of antidepressants from the SSRI group in these cases [7, 8, etc.].
The COORDINATE study completed to date has confirmed the negative impact of anxiety-depressive disorders in cardiovascular diseases, the effectiveness of the use of the antidepressant tianeptine in the treatment of hypertension. A number of studies indicate the effectiveness of antidepressants from the SSRI group in these cases [7, 8, etc.].
However, most often in the complex therapy of hypertension complicated by anxiety disorders, tranquilizers of various structures are used. In the treatment of hypertension, labile arterial hypertension in the elderly, the positive effect of the tranquilizer clonazepam in small therapeutic doses, which stabilizes psychovegetative disorders, has been convincingly shown [9]. The effect of alprazolam in the treatment of anxiety and anxiety-depressive disorders in hypertension was studied. It was shown that in the structure of the depressive syndrome in patients with mild hypertension, the affect of anxiety dominates; the inclusion of alprazolam in the complex treatment of patients with AH crisis course with anxiety and depressive disorders can effectively reduce the frequency of hypertensive crises [3].
Tranquilizers of the benzodiazepine series have a wide spectrum of activity - anxiolytic, sedative, muscle relaxant, anticonvulsant, hypnotic, vegetostabilizing effect, which is important in stopping various symptoms of mental maladaptation. Another advantage of tranquilizers is their safety, high efficiency, and rapid achievement of a therapeutic effect [10, 11].
However, benzodiazepine tranquilizers are known to have significant side effects - excessive sedation, symptoms of mental disinhibition, agitation, cognitive impairment with long-term use. In addition, all benzodiazepine derivatives can, to one degree or another, cause withdrawal syndrome, which is manifested by autonomic disorders (hyperhidrosis, digestive disorders, tachycardia), sleep disorders, dizziness, and emotional lability. In the clinic of the withdrawal syndrome, acute psychotic states, depression, choreoathetosis and, finally, states of dependence are also described.
These two circumstances - the high demand for tranquilizers in the treatment of mental adaptation disorders and the likelihood of adverse events in the long-term administration of benzodiazepine tranquilizers - necessitated the creation of other (effective, but safe) tranquilizers. These drugs include the anxiolytic etifoxine (Stresam), a tranquilizer of a non-benzodiazepine structure (Biocodex, France).
These drugs include the anxiolytic etifoxine (Stresam), a tranquilizer of a non-benzodiazepine structure (Biocodex, France).
The first data on the drug as a potential psychotropic compound refer to 1970s [12]. For the period from 1995 to 2007. etifoxine has been used to treat more than 11.3 million patients. The drug etifoxine is registered in more than 40 countries of the world, in 2008 - in the Russian Federation under the trade name Stresam.
Analysis of the results of special studies of the drug etifoxine, conducted in various French clinics (psycho-neurological and cardiological departments) indicates its proven high anxiolytic efficacy and safety [13, 14].
The results of another later study also testify to the high therapeutic efficacy of etifoxine [15]. The purpose of this double-blind, randomized, parallel-group trial is to compare the efficacy of etifoxine, a nonbenzodiazepine anxiolytic drug, and lorazepam, a benzodiazepine, in the treatment of outpatients with adjustment disorders for anxiety disorders seen in general practitioners. According to the authors, such cases account for almost 10% of psychologically motivated consultations in primary care settings.
According to the authors, such cases account for almost 10% of psychologically motivated consultations in primary care settings.
The anxiolytic effect of etifoxine was not lower than the effect of lorazepam (decrease on the HAM-A scale 54.6% and 52.3%, respectively, p = 0.0006). These drugs showed the same effectiveness on the 28th day. However, response to treatment was higher in patients treated with etifoxine; a significant therapeutic effect without adverse events was also reported in a larger number of patients taking etifoxine (p = 0.04). In addition, fewer patients treated with etifoxine experienced recurrence of symptoms of anxiety disorders 1 week after discontinuation of therapy compared with patients treated with lorazepam.
In a review on the possibilities of using the anxiolytic Stresam [16], the results of various studies performed in the last three years are presented - comparative studies of the effectiveness of etifoxine and other anxiolytics, evaluation of its effectiveness in the treatment of various patient populations, in particular with somatoform and psychosomatic disorders. In accordance with these data, etifoxine significantly reduced the severity of anxiety disorders, the frequency of panic paroxysms, and manifestations of cardiovascular and respiratory dysregulation [17], in addition, it significantly improved mood in patients with mild depressive manifestations [18, 19].
In accordance with these data, etifoxine significantly reduced the severity of anxiety disorders, the frequency of panic paroxysms, and manifestations of cardiovascular and respiratory dysregulation [17], in addition, it significantly improved mood in patients with mild depressive manifestations [18, 19].
Due to the reduction of excessive activation of the sympathetic part of the autonomic nervous system and the increased anxiety associated with it pathogenetically, the drug has a pronounced vegetative stabilizing effect in the treatment of vegetovascular dystonia [20]. The use of the drug contributed to the reduction and disappearance of sympathalgia, reducing the frequency of panic attacks. The drug also had a positive effect on sleep disorders, anxiety, weather dependence, neuromuscular excitability and tension headache.
Empirically, it was found [21] that while taking etifoxine, the frequency of heartbeats, discomfort in the chest, attacks of shortness of breath and "shortness of breath" decreased, vegetative manifestations in the form of dry mouth, sweating practically disappeared, sleep normalized, general working capacity, lability of pulse and arterial pressure was less often noted. Patients noted the disappearance of fear of the possible development of an attack.
Patients noted the disappearance of fear of the possible development of an attack.
Studies in gastroenterological practice also testify to the high efficiency of etifoxine in the complex treatment of somatic pathology against the background of severe neurotic disorders [22, 23], where etifoxine can be considered the drug of choice. When using the drug, it has been reliably established that it weakens the increased motility of the gastrointestinal tract and the feeling of discomfort in the abdomen, stabilizes blood pressure, which is just not typical for benzodiazepine drugs. Etifoxine can be considered as an integral component of combination therapy for chronic pain syndrome, in particular in patients with chronic pain syndrome due to rheumatoid arthritis [24].
The general point of view of researchers is that the anxiolytic etifoxine is effective in a very wide range of anxiety and neurotic disorders and psychosomatic pathology, sleep disorders, vegetovascular dystonia, etc. It does not adversely affect psychomotor and cognitive functions, muscle tone; dependence, tolerance is not formed to it, and also there is no withdrawal syndrome. Thanks to this, the drug opens up great opportunities for the effective treatment of various disorders in psychiatric, narcological, neurological and general somatic practice.
It does not adversely affect psychomotor and cognitive functions, muscle tone; dependence, tolerance is not formed to it, and also there is no withdrawal syndrome. Thanks to this, the drug opens up great opportunities for the effective treatment of various disorders in psychiatric, narcological, neurological and general somatic practice.
It should be noted the positive experience of using new generation anxiolytics (Stresam and Atarax) in the treatment of anxiety disorders within adjustment disorders and generalized anxiety disorder [25]. New data on the spectrum of anxiolytic effects of Stresam have been obtained. The drug can be used in the treatment of anxiety neurotic conditions with manifestations of reactively provoked and generalized anxiety. The reduction of a number of manifestations of mental anxiety (anxious mood, internal tension, emotional lability) in combination with the effect of the drug on the somatic equivalents of anxiety confirms that Stresam is an effective tool for the course treatment of mild to moderate anxiety disorders. Stresam has an anxiolytic effect, not accompanied by behavioral toxicity, hypnosedative and muscle relaxant effects, destabilization of cognitive functions in the absence of the risk of drug dependence and withdrawal syndrome.
Stresam has an anxiolytic effect, not accompanied by behavioral toxicity, hypnosedative and muscle relaxant effects, destabilization of cognitive functions in the absence of the risk of drug dependence and withdrawal syndrome.
In 2008-2009 for the first time in Russia, an open randomized controlled trial of the effectiveness of etifoxine compared with phenazepam in the treatment of patients with adjustment disorders was conducted [26]. For this study, 90 patients were selected in three psychiatric centers in Moscow and St. Petersburg. Patients were randomized into two groups receiving oral phenazepam at a dose of 0.5 mg twice a day (morning and evening) or etifoxine at a dose of 150 mg per day (50 mg in the morning and 100 mg in the evening). Treatment was carried out for 6 weeks. Efficacy and safety were evaluated on days 7 and 42 of course therapy. Withdrawal syndrome was assessed after 1 week. after the end of the study (49th day). The level of anxiety was recorded in accordance with the Hamilton anxiety scale at baseline, on days 7 and 42.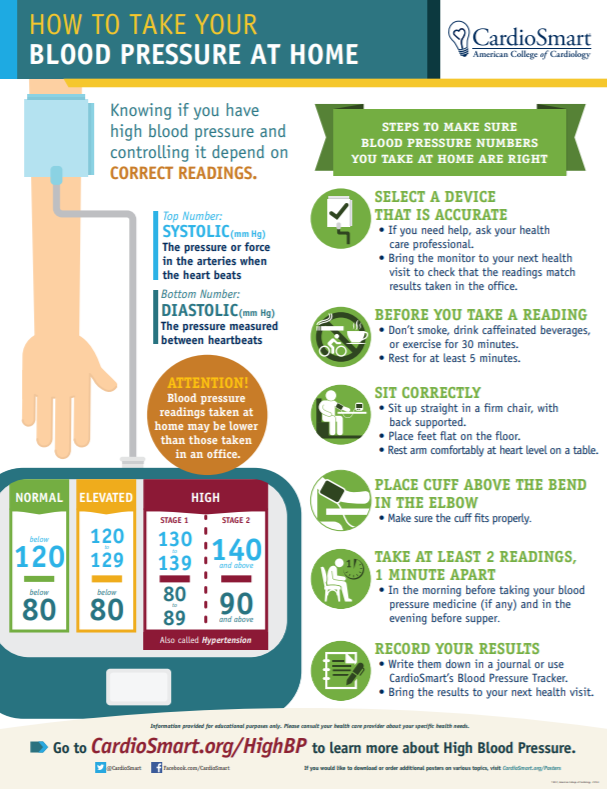 Overall disease progression was assessed using the CGI (Global Clinical Impression Scale): global clinical improvement at days 7 and 42, disease severity at baseline at days 7 and 42, and therapeutic index at days 7 and 42. days. Side effects diagnosed independently or during observation were recorded throughout the study. The withdrawal syndrome after the end of therapy was estimated at 49day on the HAM-A and CGI scales and was defined as the difference between the results of the 49th and 42nd days. A randomization list was created for each center before the start of the study in determining its design.
Overall disease progression was assessed using the CGI (Global Clinical Impression Scale): global clinical improvement at days 7 and 42, disease severity at baseline at days 7 and 42, and therapeutic index at days 7 and 42. days. Side effects diagnosed independently or during observation were recorded throughout the study. The withdrawal syndrome after the end of therapy was estimated at 49day on the HAM-A and CGI scales and was defined as the difference between the results of the 49th and 42nd days. A randomization list was created for each center before the start of the study in determining its design.
The results of the study show that etifoxine is effective in the treatment of adjustment disorders. Thus, anxiety scores on the HAM-A scale decreased on the 7th day and subsequently decreased steadily until the 42nd day of treatment. These indicators were compared with the data on the anxiolytic effect of phenazepam in patients of the comparison group.
The revealed high efficacy of etifoxine in the treatment of adjustment disorders, which is not inferior to phenazepam, and its practical absence of side effects suggests that an anxiolytic agent has appeared in clinical practice, equal in action to the most powerful tranquilizers from the benzodiazepine group.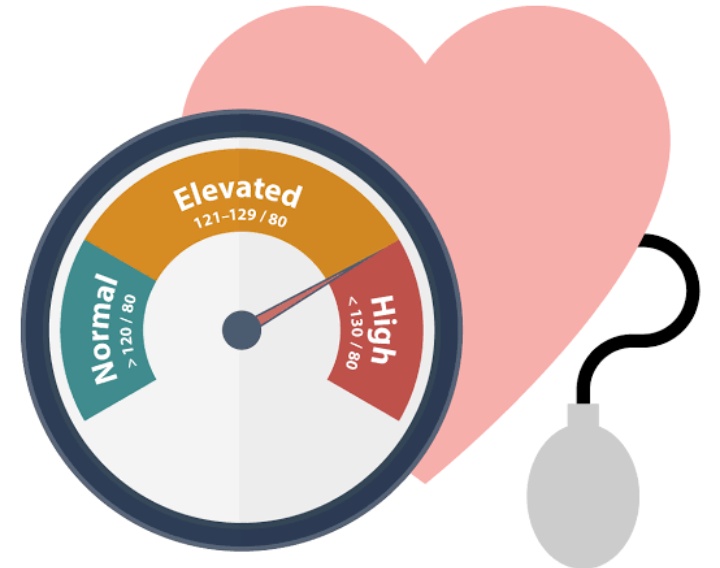 According to the study, etifoxine is better tolerated than phenazepam (1 side effect in the etifoxine group versus 21 in the phenazepam group), which indicates the possibility of its use in the daytime.
According to the study, etifoxine is better tolerated than phenazepam (1 side effect in the etifoxine group versus 21 in the phenazepam group), which indicates the possibility of its use in the daytime.
In addition, one third of patients (30 out of 90 examined) with adjustment disorders who were shown to use etifoxine were patients in a cardiological hospital, including those with hypertension. As the results of the study showed, the addition of etifoxine (Stresam) to the complex therapy contributed to the reduction of anxiety disorders and the stabilization of blood pressure.
The results of clinical studies and practice of using etifoxine available to date allow us to determine its main clinical and pharmacological characteristics.
Pharmacological properties of etifoxine: a derivative of benzoxazine, has anxiolytic activity, to a lesser extent - has a sedative effect. Does not cause addiction and withdrawal syndrome. According to one of the hypotheses, the mechanism of action of etifoxine can serve as the reason for the absence of the previously noted effects; its pharmacodynamics. Indeed, a study of the effects of etifoxine has shown that it facilitates GABAergic synaptic transmission in hypothalamic neurons and thus has a dual effect on these neurons: a pronounced positive allosteric modulation of GABA A receptors through a site different from that interacting with benzodiazepines, and an indirect effect in which stimulation may involve peripheral mitochondrial benzodiazepine receptors, which in turn control neurosteroid synthesis.
Indeed, a study of the effects of etifoxine has shown that it facilitates GABAergic synaptic transmission in hypothalamic neurons and thus has a dual effect on these neurons: a pronounced positive allosteric modulation of GABA A receptors through a site different from that interacting with benzodiazepines, and an indirect effect in which stimulation may involve peripheral mitochondrial benzodiazepine receptors, which in turn control neurosteroid synthesis.
Pharmacokinetics: the drug is rapidly absorbed from the gastrointestinal tract, rapidly metabolized in the liver to the formation of several metabolites. One of them (diethyletifoxine) is active and its half-life is about 20 hours. Penetrates through the placental barrier. The time to reach the maximum concentration in the blood is 2-3 hours, the half-life is about 6 hours. It is excreted mainly in the urine in the form of metabolites, in small quantities - unchanged; also excreted in bile.
Indications: used to eliminate anxiety, fear, internal tension, increased irritability, low mood, including against the background of somatic diseases, especially of a cardiovascular nature.
Contraindications: shock conditions, myasthenia gravis, severe liver / kidney dysfunction, hypersensitivity to the drug. It is not recommended to use the drug under the age of 18 years. The use of the drug during breastfeeding and pregnancy is not recommended.
Dosage and administration: inside with a little water. The dose of the drug is determined individually depending on the patient's condition. Usually prescribed 1 capsule (50 mg) 3 times a day or 2 capsules 2 times a day (150-200 mg / day). Duration of treatment - from several days to 4-6 weeks, depending on the patient's condition.
Side effects: slight drowsiness that appears in the first days of admission and usually disappears on its own during treatment; rarely - skin rashes are possible, as well as allergic reactions in the form of urticaria and Quincke's edema.
Overdose: symptoms of lethargy, excessive sleepiness. Treatment - gastric lavage with plenty of water, symptomatic treatment.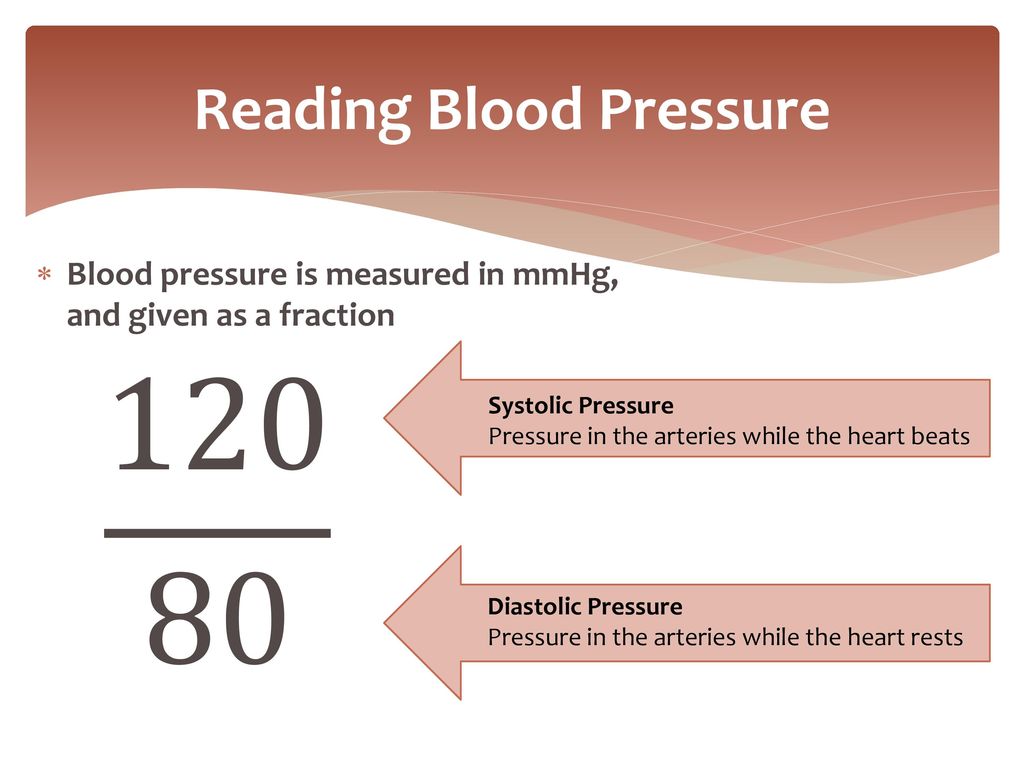 There is no specific antidote.
There is no specific antidote.
Interaction with other drugs: potentiates the effect of drugs that depress the central nervous system, such as opioid analgesics, barbiturates, hypnotics, antihistamines, neuroleptics, etc. It also enhances the effects of alcohol.
Special instructions: due to the presence of lactose in the formulation, the drug should not be used for galactosemia, glucose and galactose malabsorption syndrome, and in case of lactose deficiency. If you miss a dose of the drug, you should not double the dose at the next dose. Due to the risk of drowsiness, driving and activities requiring increased attention should be avoided during treatment. It is not recommended to take the drug together with alcoholic beverages, do not exceed the dose prescribed by the doctor. The drug is dispensed from a pharmacy by prescription.
Thus, the analysis of the available data on the pharmacological activity of etifoxine and the existing experience of its clinical use indicate that this drug has an original mechanism of action, which is characterized by maximum selectivity and physiology in relation to the effect on all links in the development of anxiety.