Psychotically depressed meaning
Psychotic depression - NHS
Some people who have severe clinical depression will also experience hallucinations and delusional thinking, the symptoms of psychosis.
Depression with psychosis is known as psychotic depression.
Symptoms of severe depression
Someone with severe clinical depression feels sad and hopeless for most of the day, practically every day, and has no interest in anything. Getting through the day feels almost impossible.
Other typical symptoms of severe depression are:
- fatigue (exhaustion)
- loss of pleasure in things
- disturbed sleep
- changes in appetite
- feeling worthless and guilty
- being unable to concentrate or being indecisive
- thoughts of death or suicide
Read more about the psychological, physical and social symptoms of clinical depression
Symptoms of psychosis
Having moments of psychosis (psychotic episodes) means experiencing:
- delusions – thoughts or beliefs that are unlikely to be true
- hallucinations – hearing and, in some cases, feeling, smelling, seeing or tasting things that are not there; hearing voices is a common hallucination
The delusions and hallucinations almost always reflect the person's deeply depressed mood – for example, they may become convinced they're to blame for something, or that they've committed a crime.
"Psychomotor agitation" is also common. This means not being able to relax or sit still, and constantly fidgeting.
At the other extreme, a person with psychotic depression may have "psychomotor retardation", where both their thoughts and physical movements slow down.
People with psychotic depression have an increased risk of thinking about suicide.
What causes psychotic depression?
The cause of psychotic depression is not fully understood. It's known that there's no single cause of depression and it has many different triggers.
For some, stressful life events such as bereavement, divorce, serious illness or financial worries can be the cause.
Genes probably play a part, as severe depression can run in families, although it's not known why some people also develop psychosis.
Many people with psychotic depression will have experienced adversity in childhood, such as a traumatic event.
Read more about the causes of clinical depression
Treating psychotic depression
Treatment for psychotic depression involves:
- medicine – a combination of antipsychotics and antidepressants can help relieve the symptoms of psychosis
- psychological therapies – the 1-to-1 talking therapy cognitive behavioural therapy (CBT) has proved effective in helping some people with psychosis
- social support – support with social needs, such as education, employment or accommodation
The person may need to stay in hospital for a short period of time while they're receiving treatment.
Electroconvulsive therapy (ECT) may sometimes be recommended if the person has severe depression and other treatments, including antidepressants, have not worked.
Treatment is usually effective, but follow-up appointments so that the person can be closely monitored are usually required.
Getting help for others
People with psychosis are often unaware that they're thinking and acting strangely.
As a result of this lack of insight, it's often down to the person's friends, relatives or carers to seek help for them.
If you're concerned about someone and think they may have psychosis, you could contact their social worker or community mental health nurse if they've previously been diagnosed with a mental health condition.
Contact the person's GP if this is the first time they've shown symptoms of psychosis.
If you think the person's symptoms are placing them or others at possible risk of harm you can:
- take them to your nearest accident and emergency (A&E) department, if they agree
- call a GP or local out-of-hours GP
- call 999 to ask for an ambulance
Further information
The following websites provide further information and support:
- SANE
- Mind: psychotic experiences
Driving
If you've been diagnosed with psychotic depression, it's your legal obligation to tell the Driver & Vehicle Licensing Agency (DVLA). It could affect your ability to drive.
It could affect your ability to drive.
Visit GOV.UK for more information about medical conditions, disabilities and driving
Page last reviewed: 10 December 2019
Next review due: 10 December 2022
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Types of depression - iFightDepression [EN]
There are different types of depression, which are different.
Signs and symptoms vary in number, time, severity and frequency, but are generally very similar. Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Neurotic, reactive (minor) depression is treated with psychotherapy.
Somatic and psychotic - medication. These terms are used by psychiatrists.
Studies have shown that depression has a phasic course. Periods of normal mood alternate with depressive episodes. Sometimes, instead of a depressive phase,
there may be a manic phase, which is manifested by irritability and high mood. If so, then it is not depression, but bipolar disorder (a more serious illness).
If so, then it is not depression, but bipolar disorder (a more serious illness).
1. Depressive episode
The most common and typical form of depression is the depressive episode. An episode lasts from a few weeks to a year, but is always longer than 2 weeks. A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime. However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
2. Intermittent (recurrent) depressive disorder
When a depressive episode recurs, it is recurrent depressive disorder or major depressive disorder, which usually begins in adolescence or early adulthood. With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
3. Dysthymia
Dysthymia presents with milder and less severe symptoms than a depressive episode or recurrent depression. However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression". This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
4. Bipolar depression, type I
This is the type of depression in bipolar disorder, formerly called manic-depressive illness, and is less common than unipolar depression. It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
Manic phases are characterized by excessively high mood associated with hyperactivity, anxiety, and decreased need for sleep.
Mania affects thinking, judgment and social behavior causing serious problems and difficulties. When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.
The best way to describe these "emotional upheavals" is "to be on top of the world and fall into the depths of despair".
Symptoms of the phases of depression in bipolar disorder are sometimes difficult to distinguish from unipolar depression.
5. Bipolar depression type II
More like recurrent depressive disorder than bipolar disorder. In this disorder, multiple depressive phases alternate with phases of mania, but with less pronounced euphoria. During these phases, family and loved ones may even mistakenly assume that the person is doing well.
6. Mixed anxiety-depressive disorder
In anxiety-depressive disorder, the clinical picture is very similar to depression, however, in depression, depressive syndromes always come first. In this case, both anxious and depressive symptoms are evenly combined.
In this case, both anxious and depressive symptoms are evenly combined.
7. Depressive psychotic episode
A special form of depressive episode is psychotic or delusional depression. Psychosis is a condition in which people see or hear things that do not exist (hallucinations) and/or have false ideas or beliefs (delusions). There are various types of delusions such as self-accusation for no reason (delusion of guilt), financial ruin (delusions of poverty), feeling of an incomprehensible illness (hypochondriac delusions). People with delusional depression almost always require inpatient psychiatric treatment. Psychotic episodes can be either unipolar or bipolar.
8. Atypical depression
This type of depression is characterized by hypersensitivity and mood swings, overeating and drowsiness, panic attacks. This type of depression is mild and can be bipolar.
9. Seasonal depressive disorder
This type of depression is similar to atypical depression and comes on seasonally with climate change, usually in autumn or winter. Usually, when the season ends, people return to normal functioning again.
Usually, when the season ends, people return to normal functioning again.
10. Brief depressive disorder
This is a milder variant of depression that more often affects young people and is characterized by short depressive episodes lasting less than 2 weeks.
Regional State Budgetary Institution "Shumyachskaya Central District Hospital"
World Health Day is celebrated annually on April 7 in honor of the WHO Foundation Day.
2017 is dedicated to the fight against depression. Depression affects people of all ages, from all walks of life, in all countries. It causes mental anguish and affects people's ability to perform daily tasks. At its worst, depression can lead to suicide, the second leading cause of death for people aged 15–29years, according to the WHO. “Beginning October 10, 2016, the overall goal of World Mental Health Day is that all people suffering from depression in all countries can seek and receive help. More specifically, we want to educate the general public about depression, its causes and possible consequences, including suicide, and the types of help available to prevent and treat depression. We want people with depression not to be afraid to seek help, so that their family members, friends and colleagues can support them,” the WHO website says.
More specifically, we want to educate the general public about depression, its causes and possible consequences, including suicide, and the types of help available to prevent and treat depression. We want people with depression not to be afraid to seek help, so that their family members, friends and colleagues can support them,” the WHO website says.
WHO has decided to focus on three groups that are at particular risk: adolescents and young adults, women of childbearing age (especially after childbirth) and the elderly (over 60 years of age).
According to a World Health Organization (WHO) report, depression and anxiety disorders cost the world $1 trillion annually. At the same time, every dollar invested in the fight against these diseases will bring to any economy $ 4 due to improved health and working capacity of the population, according to a WHO study.
Depression is an illness characterized by a persistent state of despondency and loss of interest in activities that would normally bring satisfaction, as well as an inability to do daily activities for at least two weeks. In addition, people with depression usually have some of the following symptoms: lack of energy, decreased appetite, drowsiness or insomnia, anxiety, decreased concentration, indecision, restlessness, feelings of worthlessness, guilt or despair, and thoughts of hurting themselves or suicide.
In addition, people with depression usually have some of the following symptoms: lack of energy, decreased appetite, drowsiness or insomnia, anxiety, decreased concentration, indecision, restlessness, feelings of worthlessness, guilt or despair, and thoughts of hurting themselves or suicide.
Depression (from lat. deprimo - “crush”, “suppress”) - a mental disorder characterized by a “depressive triad”: a decrease in mood and a loss of the ability to experience joy (anhedonia), impaired thinking (negative judgments, a pessimistic view of what is happening, and so on ), motor retardation. With depression, self-esteem is reduced, there is a loss of interest in life and habitual activities. In some cases, a person suffering from it may begin to abuse alcohol or other psychotropic substances.
It is a type of affective disorders (mood disorders). Depression is treatable, but depression is currently the most common mental disorder. It affects one in ten over the age of 40, two-thirds of them are women.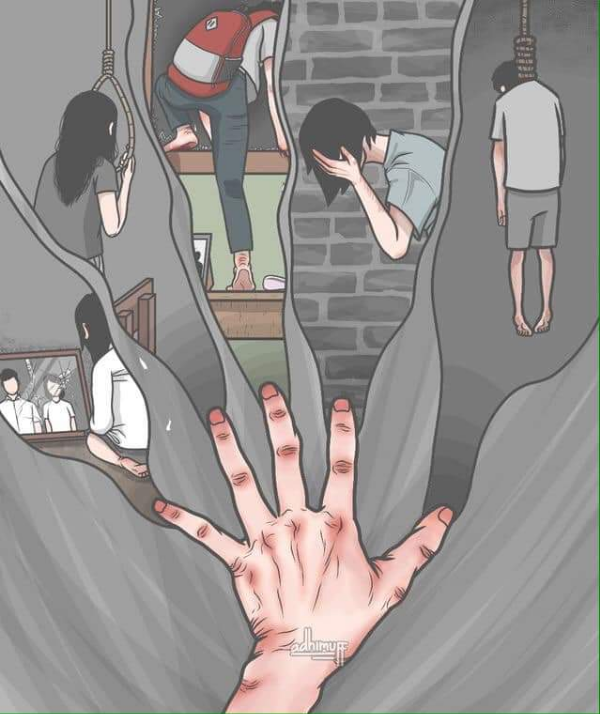 Depression is three times more common among people over 65 years of age. Also, about 5% of children and adolescents aged 10-16 years are affected by depression and depressive states. According to the World Health Organization, depression is the leading cause of adolescent illness and disability. The overall prevalence of depression (of all varieties) in adolescence ranges from 15 to 40%. Many studies emphasize that the greater prevalence of affective disorders at this age corresponds to a higher frequency of suicides.
Depression is three times more common among people over 65 years of age. Also, about 5% of children and adolescents aged 10-16 years are affected by depression and depressive states. According to the World Health Organization, depression is the leading cause of adolescent illness and disability. The overall prevalence of depression (of all varieties) in adolescence ranges from 15 to 40%. Many studies emphasize that the greater prevalence of affective disorders at this age corresponds to a higher frequency of suicides.
Many people believe that depression is a disease that has spread and acquired such great social significance only in our time and was not known before. But this is not so: depression has been known to doctors since antiquity. Even the famous ancient Greek physician Hippocrates described in detail under the name "melancholy" conditions that are very reminiscent of our current definition of depression, and even recommended treatment within the capabilities of ancient medicine.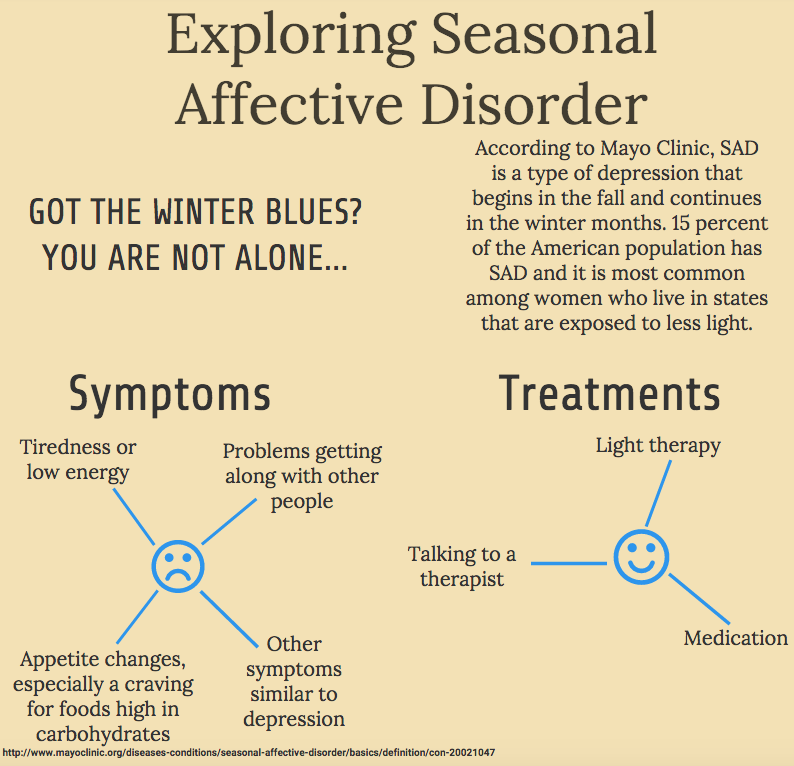
The treatment of depression according to Hippocrates consisted in the appointment of opium tincture, warm cleansing enemas (Hippocrates drew attention to the fact that severe depressions are often accompanied by constipation, and attached great importance to this), psychological support (it was recommended to “encourage and amuse” the patient), long warm baths, massages and drinking mineral water from one of the well-known sources in Crete (as it turned out later, this water contained a large amount of bromine, magnesium and lithium ions - that is, it really could help with depression)
Hippocrates also drew attention to the dependence of the condition of many depressive patients on the weather and season, to the seasonal frequency of depression in many patients, to the improvement in the condition of some patients after a sleepless night. Thus, he was close to discovering the therapeutic effect of sleep deprivation and sunlight (phototherapy), although he did not make this discovery.
The Ebers Papyrus, one of the most important medical treatises of ancient Egypt, also contains a short description of depression. Although the information on the papyrus is full of ritual rites and intricate recipes for expelling disease-causing demons and other evil spirits, it also testifies to long empirical practice and observation.
Causes of depression
Depression can be the result of dramatic experiences, such as loss of a loved one, job, social status. In such cases, we are talking about reactive depression. It develops as a reaction to some external event, situation. According to some theories, depression sometimes occurs when the brain is overworked as a result of stress, which can be based on both physiological and psychosocial factors.
A risk factor for the development of depression in adults may also be severe experiences in childhood: for example, child abuse may be a prerequisite for their future depression.
But if the psychological, iatrogenic or somatic causes of depression are absent or not obvious, such depression is called endogenous, that is, as it were, “occurring from within” (of the body, psyche).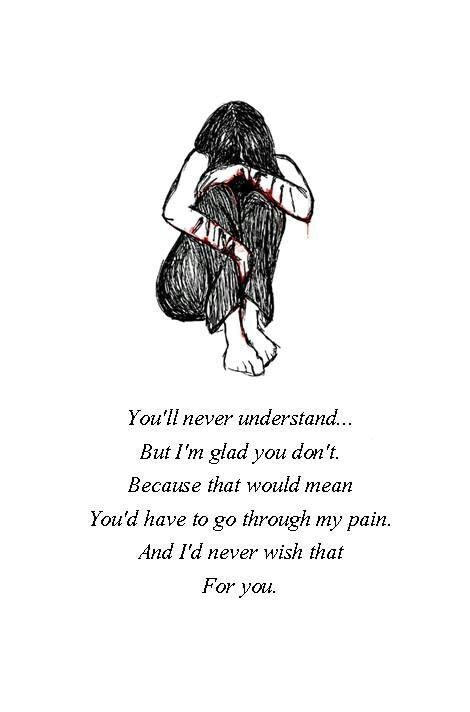 Approximately in one third (about 35%) of cases, overt depression occurs autochthonously, that is, without any external influences. Structurally, such depressions are endogenous from the very beginning.
Approximately in one third (about 35%) of cases, overt depression occurs autochthonously, that is, without any external influences. Structurally, such depressions are endogenous from the very beginning.
The monoamine theory associates the development of depression with a deficiency of biogenic amines, namely serotonin, norepinephrine and dopamine. Some researchers conclude that this theory is not broad enough, as it does not explain the limitations in the effectiveness of antidepressants and the slow development of their therapeutic effect.
Many people in sunless weather or in those who are in darkened rooms, depression can occur due to the lack of bright light. This variety is called seasonal depression or seasonal affective disorder, because it is most often observed in patients in autumn and winter. Treat seasonal depression with sunny walks or light therapy. However, in a study conducted on a large sample (34,294 people), it was not possible to find relationships between depression and the season. Depression was not related to the latitude at which a person lives, nor to the amount of sunlight[13]. But this study has important shortcomings - in particular, the survey of these 34 294 people were conducted by phone, which does not make it possible to diagnose the presence or absence of clinical depression in respondents.
Depression can result from the side effects of many drugs (eg, levodopa, corticosteroids, benzodiazepines)—so-called iatrogenic or pharmacogenic depression.
Most often, this depression resolves quickly on its own or is cured after discontinuation of the corresponding drug.
Antipsychotic depression
(due to the use of neuroleptics) can last from several months to 1.5 years and often have a vital character.
The cause of depression in some cases is the abuse of sedatives or hypnotics, alcohol, cocaine and other opiate psychostimulants.
Depressions can also be somatic or, more precisely, somatogenic,
manifest as a consequence of somatic diseases (for example, Alzheimer's disease, atherosclerosis of the arteries of the brain, traumatic brain injury, or even ordinary influenza).
The main types of depression
There are unipolar depressions, in which the mood remains within one, reduced, "pole", and bipolar depressions, which are an integral part of bipolar affective disorder, which are interspersed with manic, hypomanic or mixed affective episodes. Also, depressive episodes of mild severity can occur with cyclothymia. The following forms of unipolar depressions can be distinguished (according to DSM-IV):
• Major depressive disorder, often referred to as clinical depression.
• A form of major depression is resistant depression, in which two consecutive courses (3-4 weeks each) of antidepressant treatment show no or insufficient clinical effect.
• Minor depression that does not meet all the criteria for clinical depression, but in which at least two of the main diagnostic symptoms have been present for at least two weeks[41].
• Atypical depression is a form of depressive disorder in which, along with the typical symptoms of depression, there are specific signs such as increased appetite, weight gain, increased sleepiness and so-called "emotional reactivity".
• Postnatal depression is a form of depressive disorder that develops immediately after childbirth.
• Recurrent brief depression (RBD), differs from major depressive disorder primarily because of the difference in duration. People with RBD experience depressive episodes about once a month, with individual episodes lasting less than two weeks and usually less than 2–3 days. For RBD to be diagnosed, episodes must have been present for at least one year and, if the patient is female, regardless of the menstrual cycle. People with clinical depression can develop RBD, as well as vice versa].
• Dysthymia is a mild chronic mood disorder in which a person complains of almost daily bad mood for at least two years. Symptoms are not as severe as in clinical depression, although people with dysthymia are also subject to periodic episodes of clinical depression (sometimes called "double depression")].
Other depressive disorders (DD-NOS) under the DSM code 311 include depressive disorders that cause detriment but do not qualify under officially defined diagnoses, that is, "do not meet the criteria for any specified disorder. "
"
In Russian-speaking medicine, the expression vital depression is often used. It means, first of all, the “vital” (“vital”) character of depression, with pronounced melancholy and anxiety, which patients feel on the physical level[45], for example, melancholy can be felt in the form of pain in the solar plexus. It was believed that "vital" depression is caused by a violation of "life processes", develops cyclically, being inaccessible to external influences, and arises for no reason, inexplicable for the patient himself]. This character is often characteristic, in particular, of "bipolar" depression in MDP and endogenous depression in general.
In a narrower sense, vital is primarily called "dreary depression", in which the manifestations of longing and despair are most pronounced, as well as depression with disorders in the "vital sphere" - with disturbances in the need for food, sleep, etc.] Vital depressions are classified as a major depressive episode without psychotic symptoms.
Despite the severity of the condition, such depressions are prognostically favorable, as they respond well to treatment with antidepressants.
In addition, "vital depressions" are sometimes called depressive states in cyclothymia (according to the classification of Schneider, 1959), with blurred manifestations of melancholy, pessimism, despondency, depression, and with a strong dependence of symptoms on the circadian rhythm [50][48]. This terminology is not widely used.
The course of the disease
At first, mild signals are felt in the form of sleep problems, irritability, refusal to perform normal duties. If these symptoms increase within two weeks, then this usually indicates the onset of the disease or its relapse, although it will fully manifest itself after two months] or even later. There are occasional seizures. Left untreated, depression can lead to suicide attempts, alienation from others, failure to perform most life functions, and family breakdown.
Depression can be caused and accompanied by other mental disorders, in particular neurosis.
It has been established that depression is associated with a decrease in the length of telomeres, which is also associated with the aging process of the body.
Also, according to a recent study by scientists, it turned out that depression affects wound healing. In patients with depression, wounds heal more difficult, they are more likely to be rehospitalized. Moreover, the more severe the form of the disorder, the worse the result. Leading researcher Philip Britteon, believes that before the operation, special attention should be paid to the psychological state of the patient, so that the patient recovers as soon as possible.
The average duration of the disease is from 6 to 8 months, but in some patients depression acquires a chronic course. Chronic depression is a depression that lasts more than two years.
Resistant depression is considered to be such a depression in which, during two consecutive courses of adequate and long-term monotherapy with pharmacologically different drugs, there is an absence or insufficiency of a clinical effect (reduction of symptoms according to the Hamilton scale or Montgomery scale - less than 50%).
Not every patient requires hospitalization, treatment is often carried out on an outpatient basis. The main areas of depression therapy are pharmacotherapy, psychotherapy and social therapy. The most important criterion for successful antidepressant therapy is the correct clinical diagnosis: the approach to treating depression should depend on its cause. So, with somatogenic depression, it is necessary first of all to treat a somatic disease and only in the second place - symptomatic psychopharmacotherapy and psychotherapy. With endogenous depression, psychopharmacotherapy is the main method, and psychotherapy is used in addition to it; in psychogenic (neurotic and reactive) depression, psychotherapy is no less important than psychopharmacotherapy.
It should be noted that even in cases where somatic pathology is not the cause of a depressive disorder, the presence of some somatic diseases (for example, subclinical hypothyroidism, Cushing's disease, polycystic ovary syndrome, coronary heart disease, oncological pathology, chronic infections, vitamin or elemental deficiency etc.