How to work when depressed
SAMHSA’s National Helpline | SAMHSA
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems.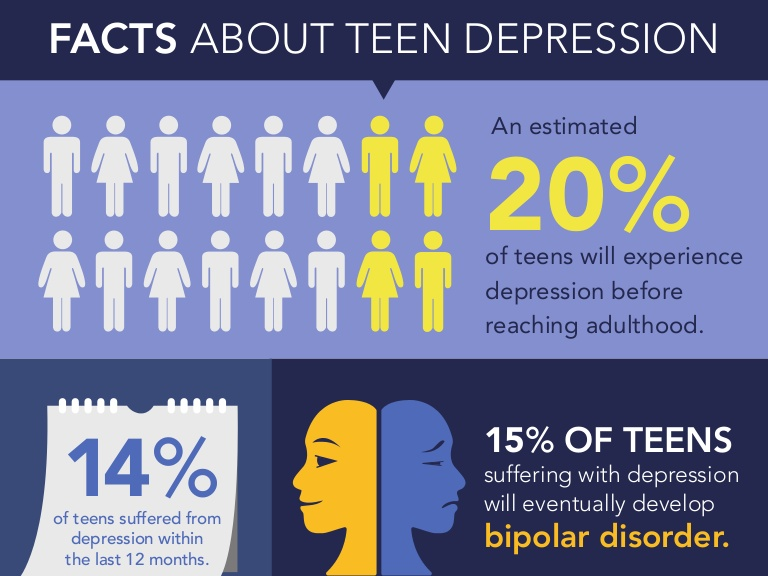 Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated
Last Updated: 03/22/2023
Partial eclipse. How to cope with work in depression
There were 40 minutes left before the planning meeting, when, as in Brodsky's poem, I realized that I simply could not leave the room. Okay, out of the apartment. There was no strength left at all, as if his head was stuffed with cotton wool. A hostile and chaotic world began outside the door, and the prospect of navigating the subway seemed an impossible task. And what useful thing could I squeeze out of myself at a meeting? I sat on the floor in the middle of the kitchen and, looking at the blurry screen, dialed another unconvincing text message to the authorities about a sudden ailment. Just six months before, I had moved to a new job with a dream team, with a promotion and big plans for the future. Around the same time, the doctor prescribed me the first antidepressants.
Just six months before, I had moved to a new job with a dream team, with a promotion and big plans for the future. Around the same time, the doctor prescribed me the first antidepressants.
If we sum up all the man-hours that, according to the World Health Organization, the world's population lost due to the depression in 2012, and convert them into years, we get 75.6 million years. Some patients completely lose their ability to work, others continue to work, but much less efficiently: along with the disorder comes not only a decline in mood, but also increased fatigue, problems with concentration, memory impairment and a general decline in cognitive functions. Solving a problem that used to take an hour can take three, and the inability to switch the language layout on the keyboard the first time can sometimes destroy self-confidence for a whole day. There are problems with building processes and making decisions: a depressed person can get confused and “freeze”, even if he needs to perform a simple sequence of actions, for example, boil a kettle and make a sandwich. The body also experiences stress: sleep “breaks”, appetite deteriorates, immunity is weakened and blood pressure rises. Therefore, the frequent feeling of fatigue is not just a perception distorted by depression, but a very real physical condition.
The body also experiences stress: sleep “breaks”, appetite deteriorates, immunity is weakened and blood pressure rises. Therefore, the frequent feeling of fatigue is not just a perception distorted by depression, but a very real physical condition.
So beloved by narrow-minded well-wishers, the advice “get together, rag!” does not work here: this problem cannot be solved by purely forceful methods, but with a whip it is very easy to drive yourself even further into a dead end. But at the same time, indulging in frustration is also not an option. For people with no ambitions, the “vegetable regimen” quickly ruins self-esteem, which is already vulnerable in depression, and they fall into a vicious circle: “I just do what I’m lying on the couch, so I’m not capable of anything, so I just and it remains that further to lie on the couch. To feel at work, but not to overwork, simple routine operations help: wash the dishes, answer letters, make a couple of calls according to a prepared script, check the text for speech errors, write a formal report. But for creative workers, this is not a solution either: they are expected to be involved and creative.
But for creative workers, this is not a solution either: they are expected to be involved and creative.
During my three years of treatment for depression, I tried different ways to engage in creative tasks and keep up my work pace no matter what. As a result, I managed to do without capital fakups, participate in several interesting media projects and write a book. Below I offer a list of tricks that ended up being the most useful. Of course, depression can occur differently in different people (some do not lose their ability to work at all, and the disease manifests itself only through psychosomatics - this is called masked depression), so my advice may not be suitable for everyone. Nevertheless, they help to build a life schedule in general and are good at counteracting popular symptoms of the disorder.
Time management and organization
Estimate how long it will take you to deliver the project if nothing interferes with you, and multiply it by one and a half. This is the minimum that should be called to the customer.
This is the minimum that should be called to the customer.
The method “First try to do the job at least somehow, even if it's bad, and then bring it to the standard” reduces the level of anxiety and perfectionism. If you start doing at least something, there is a high probability of “warming up” in the process. It's the same with brainstorming: if you come up with and write down 10–20 idiotic ideas without self-criticism, things usually get off the ground.
For those who have problems with structuring, a flipchart may be helpful. It is convenient to draw umbrella schemes on it: place the topic / main idea in the center, and subheads, theses or associations associated with it at the ends of the rays.
It is useful to make a list of simple, routine, not requiring much creativity in advance in case you sit down at the computer and realize that the brain has turned into a pumpkin. And keep it on your desktop or in your browser bookmarks. Since depression makes it difficult to make decisions, ready-made algorithms bring relief. They can be planned in advance with the help of someone close to you.
They can be planned in advance with the help of someone close to you.
Most depressed people feel overwhelmed in the morning and improve in the evening. If your emotional schedule does not differ from the typical case, it makes sense to plan things for the afternoon.
Evaluation of results
If during work you feel that the project is failing catastrophically, try to be as specific as possible: what exactly is wrong? Don't be satisfied with the inner critic's vague answers like "it's just complete shit." Furious design? Bored and incomprehensible? Are you obviously too stupid not to screw up in such a complex topic? All this can and should be tested on people who can objectively evaluate these parameters.
If you are feeling depressed or anxious, it is important to temporarily stop trying to objectively assess the quality of your work. Now you are not capable of it. It is good to have at hand rationally thinking people whom you trust and who will point out logical inconsistencies in your catastrophic picture of the world in time. Important! Precisely on logical inconsistencies. Not “everything will be fine”, not “you are great and I believe in you”, but “your text cannot be too boring and too frivolous at the same time”.
Important! Precisely on logical inconsistencies. Not “everything will be fine”, not “you are great and I believe in you”, but “your text cannot be too boring and too frivolous at the same time”.
It's also good to have verifiable and adequate success rates and resist the temptation to discount them as you go along. For example, the approval of people whom you yourself consider cool specialists. And if they approved - believe it.
It doesn't matter how much you beat yourself up if it doesn't help your productivity. If you didn’t do anything today, it really doesn’t matter if you shamelessly stuck on a new series or sobbed over the file all day and tried to collect yourself. If you start to track the uselessness of your own guilt, it helps to abolish it as a non-working tool.
Motivation
It is important to learn to separate abilities and skills, and if something does not work out, ask yourself: “Maybe the point is not that I lack brains / talent / will, but that I don't have the required skill? And if so, how to master it?
Discussing the topic of the project with those who are interested in it helps to cope with anxious thoughts about “nobody will need it”. No need to retell all your ambitious plans - just tell a funny detail and see someone else's animation.
No need to retell all your ambitious plans - just tell a funny detail and see someone else's animation.
One of the most unpleasant thoughts in depression is "it will never end." Here you need to constantly keep in mind that the current situation is temporary, even if now it seems hopeless. Your uplifting reading is about the stories of bright people who successfully overcame depression and, having recovered, created something beautiful and useful.
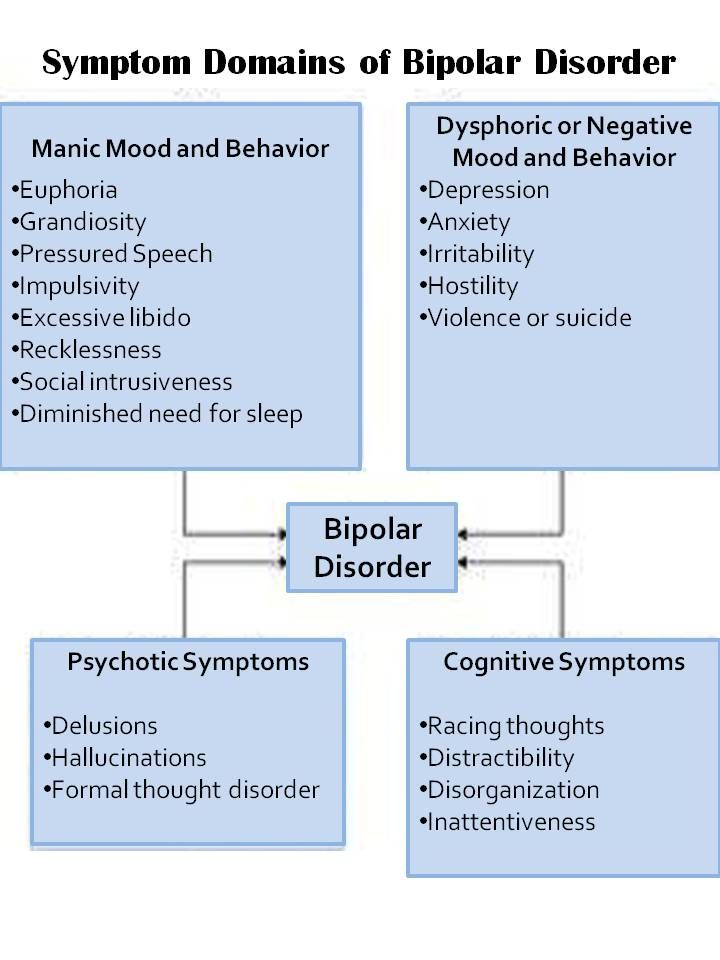
Renowned psychiatrist and researcher of depression and bipolar disorder, Kay Redfield Jamison, believes that periods of depression are conducive to deep reflection and, in a sense, can be productive for creativity and mental work. Those patients whose cognitive functions are less dull during periods of mood decline (but still lack the strength to work intensively) can devote this time to analyzing what has already been done or planning future steps.
Relations with people
In the eyes of the customer/employer, it is important to remain, if not super efficient, but at least the most predictable and consistent person. If something goes wrong, it's more profitable to report it in advance and prevent an even bigger disaster than to sit in a stupor or hope that desperation will give strength three hours before the deadline.
If something goes wrong, it's more profitable to report it in advance and prevent an even bigger disaster than to sit in a stupor or hope that desperation will give strength three hours before the deadline.
If you are obviously not going to be useful at the workplace today, it is better to plead unhealthy and take a day off (and this will not even be a hoax!). But it would be good to invest the freed time in something useful: for example, take a walk in the park, do light exercises or do yoga, and then try to solve the simplest of the current work tasks or write down all the upcoming tasks in the organizer.
It's better to answer calls and letters right away - at least something, let people see that you are alive and you care. At worst, you can come up with a universal phrase like "Hello, of course, I remember about this task, now I'm in time trouble, I'll write the details soon."
Don't try to do everything on your own if you can't seem to do it. Many depressive patients have impostor syndrome (a persistent feeling that you have achieved success undeservedly and this is about to be revealed): it often seems that when you ask for advice or help from colleagues, you give yourself away completely and you will be exposed as a miserable and incompetent layman, but in fact, this is a common working situation.
People who have gone a long way from beating themselves up about their worthlessness to accepting the very fact of their disorder may be tempted to build a new identity around their struggle with depression. But it is strange to think that depression defines your personality more than, for example, gastritis or scoliosis. This is a completely prosaic breakdown in the functioning of the brain, unpleasant, but common. With this approach, it will be easier for those around you to treat the situation with understanding: at least they will no longer suspect you of trying to wrap yourself in a Byronic cloak.
It is worth considering carefully with whom to share feelings associated with depression and how to avoid overdosing. If you just want to “handle”, you can ask a loved one to hug you without a detailed description of fresh symptoms. If there is a problem that is bothering you, you can reformulate it into a task: requests for practical advice are usually better received than complaints. This does not mean that you need to completely abandon frankness, but it is important to ensure that no one is too tired of it (except for the psychotherapist - he is used to it).
This does not mean that you need to completely abandon frankness, but it is important to ensure that no one is too tired of it (except for the psychotherapist - he is used to it).
These tips, based on personal experience, will help you better cope with internal chaos, but they will not replace a visit to a psychotherapist, and even less treatment with antidepressants.
how to deal with a sick employee / Sudo Null IT News
"I'm sorry, I think I should have said this earlier - I'm dealing with depression." I received such a letter in the morning from one of the employees, who for a couple of days could not close a simple ticket.
Context: I work as a team leader in a large corporation, subordinate to a remote team of 50 people (territorial spread - from New York to Tokyo). The employee who faced depression is my age (+- 30 years old), has been working at this place for 5 years. One of the best members of the team, consistently showing excellent results, there were no problems with motivation before.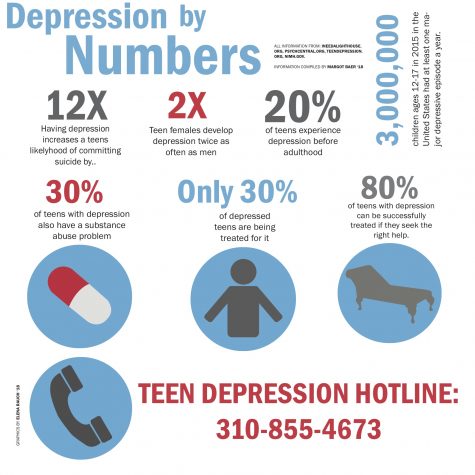 The working day is irregular: sometimes thick, sometimes empty.
The working day is irregular: sometimes thick, sometimes empty.
No, this is not professional burnout. His work has always driven him, he doesn’t want to change anything in it (neither the location, nor the team). "I'm looking for a therapist."
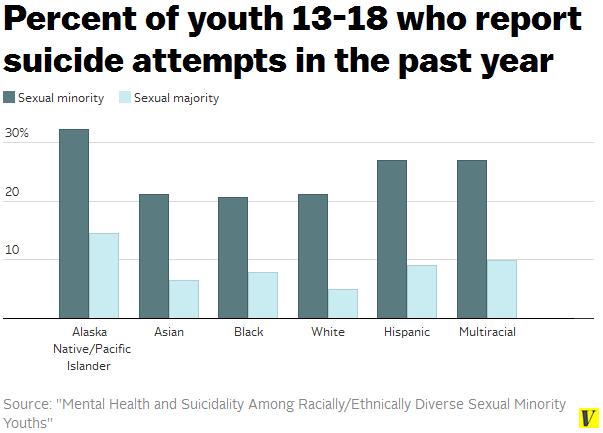
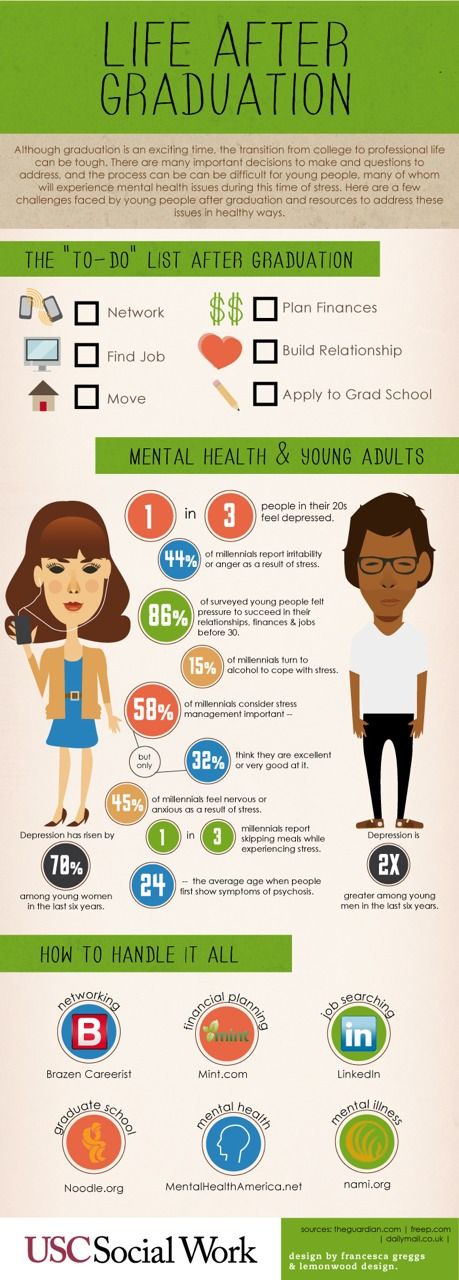
Some dry statistics . According to the World Health Organization, 264 million people worldwide suffer from depression. In severe cases, the disease can lead to suicide: 800,000 people die every year as a result of suicide. Depression and anxiety disorders cost the global economy $1 trillion a year.
Remote work creates additional risks for the development of depression. According to a 2017 UN report, 41% of distributed team members reported “high levels of stress.” For comparison, only 25% of workers in traditional offices experienced this condition.
How are they?
In the United States, a person with a disability (depression is on the list of diseases) is protected by the Americans With Disabilities Act (ADA).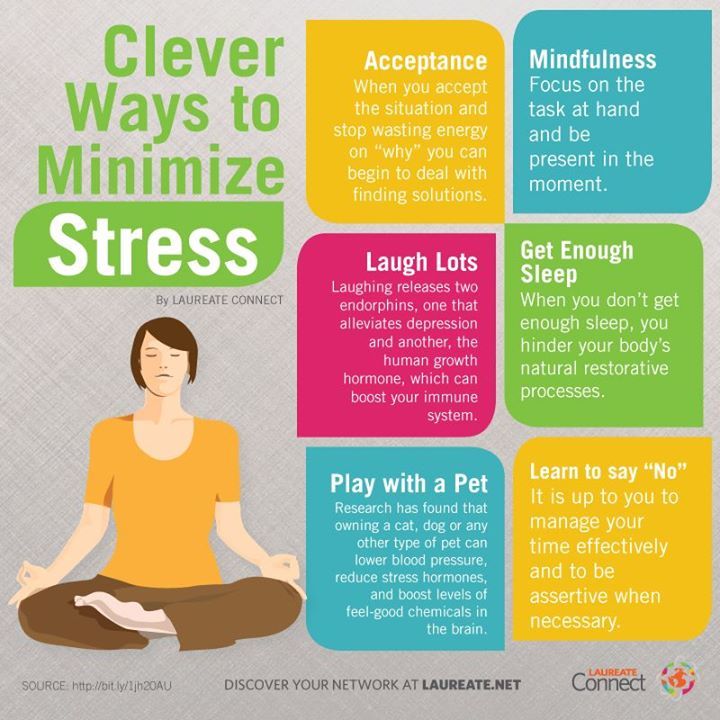 The employer in this case is obliged to provide the employee with “acceptable conditions” for his work in the circumstances. For example, he might offer a depressed person a flexible schedule, the opportunity to be away during work hours to see a doctor or group therapy, a quiet workplace, work from home, and so on.
The employer in this case is obliged to provide the employee with “acceptable conditions” for his work in the circumstances. For example, he might offer a depressed person a flexible schedule, the opportunity to be away during work hours to see a doctor or group therapy, a quiet workplace, work from home, and so on.
The boss may or may not ask the subordinate for a medical certificate with a diagnosis. An employer cannot fire a confessed employee unless he has “objective evidence” that the person cannot do his job or is a danger to others.
At the same time, according to the law, the employer does not have the right to ask the employee if he is sick with something, if he himself did not say. Whether or not to tell your boss about depression is optional. Here is what Ronald Riggio, a professor of psychology at Claremont McKenna College, told me about this topic:0003
“This is a very sensitive issue. In the US, it is illegal to ask about an employee's health status. So the best strategy is to send him to the so-called employee assistance program. Many companies have them (or have a contract with an external agency): within the framework of such a program, a depressed person can receive the help of professional consultants.
So the best strategy is to send him to the so-called employee assistance program. Many companies have them (or have a contract with an external agency): within the framework of such a program, a depressed person can receive the help of professional consultants.
How about us?
Do your companies have such "programs"? We have a full-time psychologist, but, frankly, there is about as much trust in him as in a corporate therapist (once I came to him with, as it turned out later, advanced sinusitis, and he dripped vasoconstrictors, they say, “there is no temperature, what else sinusitis). Much more useful is the ability to turn to external specialists with whom the company has a contract. Not for one visit (as many are provided for by VMI), but for the entire period of treatment. In Russia, by the way, there are services with which you can agree on the provision of such services to employees, of course, on an anonymous basis. I won't name it here, it's easy to google.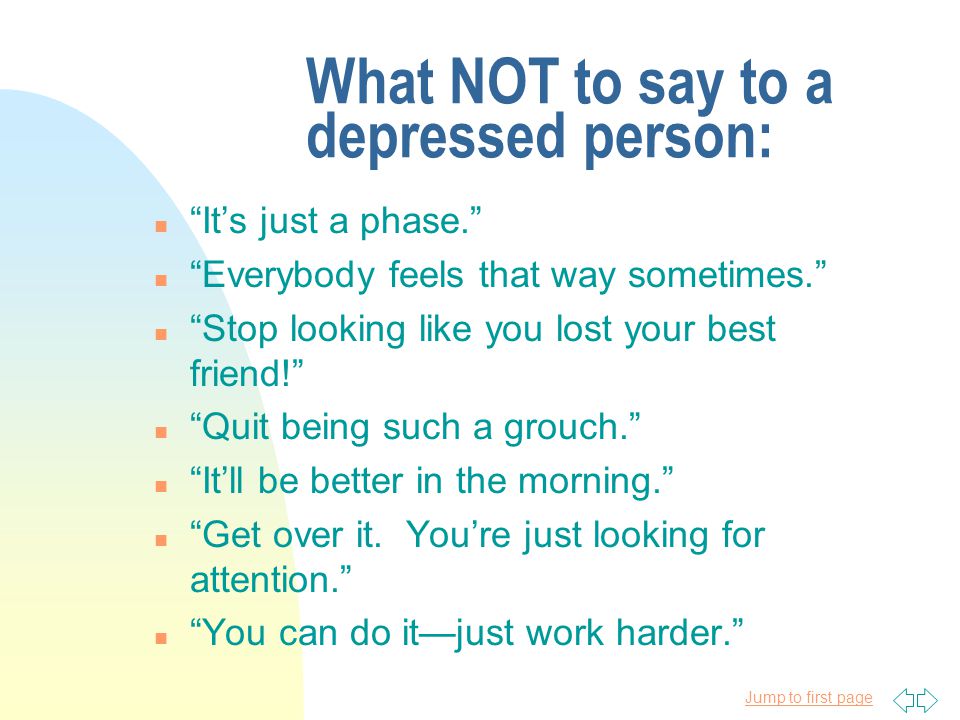
Unfortunately, most people in Russia do not consider depression to be a serious illness, although in severe cases a person is physically unable to get out of bed. How many sick people get sick leave (and this, by the way, is technically possible)? And this despite the fact that in our country about 8 million people suffer from depression - and these are only those who fall into the field of view of doctors. That is, in fact, there are much more sick people. According to statistics, depression is experienced by approximately 8-12% of the world's population.
3 tips for managers:
- Don't discount the problem. Comforters in the spirit of "It will pass!", "Do not hang your nose!" and phrases like “Well, not cancer and thank God!” out of place here
- Offer help. Allow the employee to sometimes work from home (if he is not a remote worker anyway) or change the situation (internship, vacation). If you let an employee go on time off, do not overwhelm him with tasks - let him rest.
 Do not overload with tasks. Ask an employee how else they can help
Do not overload with tasks. Ask an employee how else they can help - Create a trusting environment in the team so that employees are not afraid to share with the manager the problems that affect the work process. Maintain confidentiality - conversation "between us" should not be leaked
Personally, I told my employee the following:
“You are a great fellow for what you said. In our country, this problem is hushed up, many do not take it seriously, they say something like “Get together, rag!”, “Oh, I also have problems”, “You are mad about fat”, etc. With ARVI, people are on sick leave for a week, and for some reason depression is not considered a reason for taking time off. In general, if we, for our part, can help you with something, speak up. We can try to unload you a little and free you from the N project - you always called it routine. We know you love business trips - would you like to go to M for a conference? We can still try to transfer you to another country, if, of course, there is such a desire.