Whats multiple personality disorder
Causes, Symptoms, Types & Treatment
Overview
What is delusional disorder?
Delusional disorder is a type of psychotic disorder. Its main symptom is the presence of one or more delusions.
A delusion is an unshakable belief in something that’s untrue. The belief isn’t a part of the person’s culture or subculture, and almost everyone else knows this belief to be false.
People with delusional disorder often experience non-bizarre delusions. Non-bizarre delusions involve situations that could possibly occur in real life, such as being followed, deceived or loved from a distance. These delusions usually involve the misinterpretation of perceptions or experiences. In reality, these situations are either untrue or are highly exaggerated.
Non-bizarre delusions are different from bizarre delusions, which include beliefs that are impossible in our reality, such as believing someone has removed an organ from your body without any physical evidence of the procedure.
People with delusional disorder often continue to socialize and function well, apart from the subject of their delusion. Generally, they don’t behave in an odd or unusual manner. This is unlike people with other psychotic disorders, who might also have delusions as a symptom. In some cases, however, people with delusional disorder might become so preoccupied with their delusions that their lives are disrupted.
What are the types of delusional disorder?
There are different types of delusional disorder, which are determined based on the main theme of the delusions the person experiences. The types of delusional disorder include:
- Erotomanic: People with this type of delusional disorder believe that another person, often someone important or famous, is in love with them. They may attempt to contact the person of the delusion and engage in stalking behavior.
- Grandiose: People with this type of delusional disorder have an overinflated sense of self-worth, power, knowledge or identity.
 They may believe they have a great talent or have made an important discovery.
They may believe they have a great talent or have made an important discovery. - Jealous: People with this type of delusional disorder believe that their spouse or sexual partner is unfaithful without any concrete evidence.
- Persecutory: People with this type of delusional disorder believe someone or something is mistreating, spying on or attempting to harm them (or someone close to them). People with this type of delusional disorder may make repeated complaints to legal authorities.
- Somatic: People with this type of delusional disorder believe that they have a physical issue or medical problem, such as a parasite or a bad odor.
- Mixed: People with this type of delusional disorder have two or more of the types of delusions listed above.
What is the difference between delusional disorder and schizophrenia?
Schizophrenia is a spectrum (or range) of conditions that involve psychotic symptoms, which include:
- Disorganized speech or behavior.
- Negative symptoms (a decrease in emotion in a person’s facial expressions and motivation).
Delusional disorder is different from schizophrenia because there aren’t any other psychotic symptoms other than delusions.
In addition, in contrast to schizophrenia, delusional disorder is relatively rare, and daily functioning isn’t as impaired as it is in schizophrenia.
Who does delusional disorder affect?
Delusional disorder most often occurs in middle to late life, with the average age of onset being 40 years.
The persecutory and jealous types of delusional disorder are more common in people assigned male at birth (AMAB), and the erotomanic type is more common in people assigned female at birth (AFAB).
People who tend to be socially isolated are more likely to develop delusional disorder. These populations include:
- Immigrants who have language barriers.
- People who are deaf.
- People who are visually impaired.
- Elderly people.

How common is delusional disorder?
Although delusions might be a symptom of more common disorders, such as schizophrenia, delusional disorder itself is rather rare. Approximately 0.05% to 0.1% of the adult population has delusional disorder.
What is the most common type of delusional disorder?
The most common type of delusional disorder is the persecutory type — when someone believes others are out to harm them despite evidence to the contrary.
Symptoms and Causes
What are the signs and symptoms of delusional disorder?
The presence of delusions is the most obvious sign of delusional disorder, which vary based on the type.
Another characteristic of this condition is that the person often lacks self-awareness that their delusions are problematic. They’re unable to accept that their delusions are irrational or inaccurate, even if they recognize that other people would describe their delusions this way.
Anger and violent behavior may be present if someone is experiencing persecutory, jealous or erotomanic delusions.
People with delusional disorder may also develop anxiety and/or depression as a result of the delusions.
Early symptoms of delusional disorder may include:
- Feelings of being exploited.
- Preoccupation with the loyalty or trustworthiness of friends.
- A tendency to read threatening meanings into benign remarks or events.
- Persistently holding grudges.
- A readiness to respond and react to perceived slights.
What causes delusional disorder?
As with many other psychotic disorders, researchers don’t yet know the exact cause of delusional disorder. Researchers are, however, looking at the role of various factors that may contribute to the development of the condition, including:
- Genetic factors: The fact that delusional disorder is more common in people who have family members with delusional disorder or schizophrenia suggests there might be a genetic factor involved. Researchers believe that, as with other mental disorders, a tendency to develop delusional disorder might be passed on from parents to their biological children.
- Biological factors: Researchers are studying how abnormalities of certain areas of your brain might be involved in the development of delusional disorder. An imbalance of certain chemicals in your brain, called neurotransmitters, has been linked to the formation of delusional symptoms.
- Environmental and psychological factors: Evidence suggests that delusional disorder can be triggered by stress. Alcohol use disorder and substance use disorder might contribute to the condition. Hypersensitivity and ego defense mechanisms like reaction formation, projection and denial are some psychodynamic theories for the development of delusional disorder. Social isolation, envy, distrust, suspicion and low self-esteem are also some psychological factors that may lead to a person seeking an explanation for these feelings and, thus, forming a delusion as a solution.
Diagnosis and Tests
How is delusional disorder diagnosed?
Healthcare providers — mainly mental health professionals — diagnose delusional disorder when a person has one or more delusions for one month or more that can’t be explained by any other condition. The person must also not have the characteristic symptoms of other psychotic disorders, such as schizophrenia.
The person must also not have the characteristic symptoms of other psychotic disorders, such as schizophrenia.
If someone is experiencing signs and symptoms of delusional disorder, a healthcare provider will perform a complete medical history and physical examination. Although there aren’t any laboratory tests to diagnose delusional disorder, their healthcare provider might use various diagnostic tests — such as imaging tests, a urine drug screen and blood tests — to rule out any physical conditions, medications or substances that could be causing the symptoms.
If their healthcare provider finds no physical reason for the symptoms, a consultation with a psychiatrist or psychologist will likely be made. Psychiatrists and psychologists use specially designed interview and assessment tools to evaluate a person for a psychotic disorder. They’ll ask questions about the delusions and assess the person’s mental status.
The psychiatrist or psychologist may also interview family members and friends so they can provide further details about the person’s delusions and a timeline of the symptoms.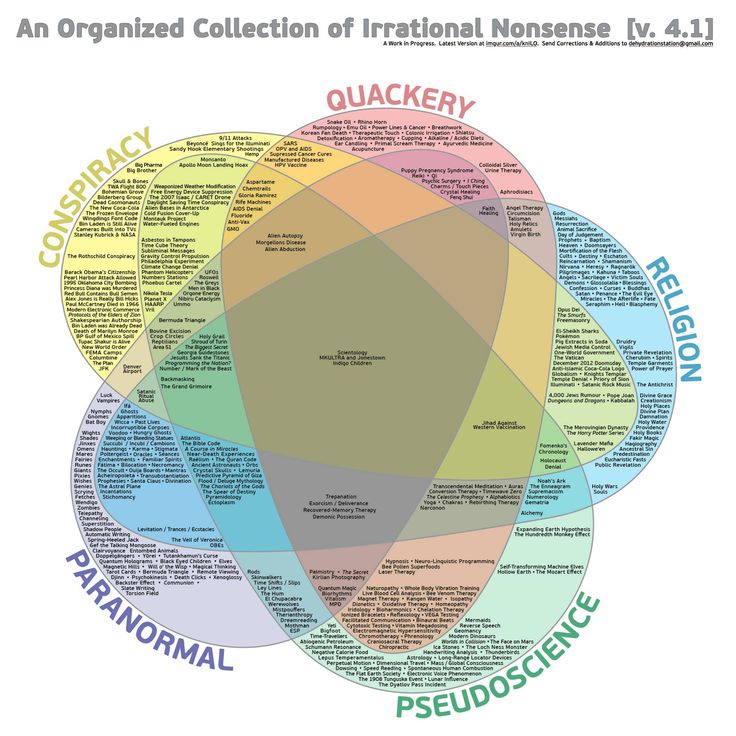
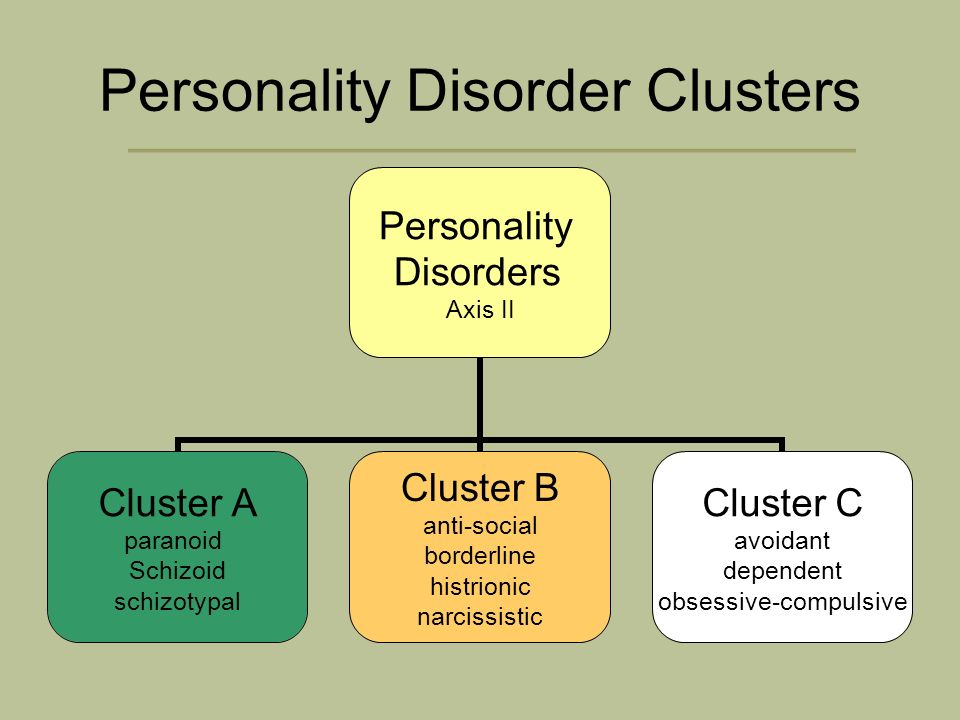
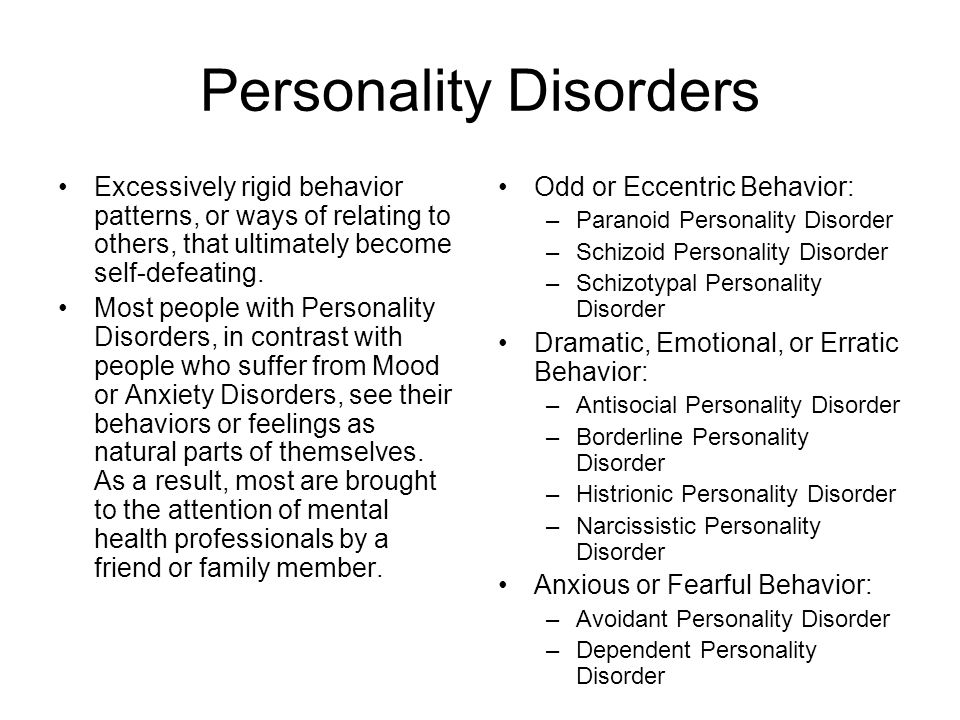
As other mental health conditions can cause delusions, mental health professionals carefully assess the person for other symptoms. Delusional disorder can be misdiagnosed as any of the following conditions:
- Obsessive-compulsive disorder.
- Schizophrenia.
- Delirium/major neurocognitive disorder.
- Bipolar disorder.
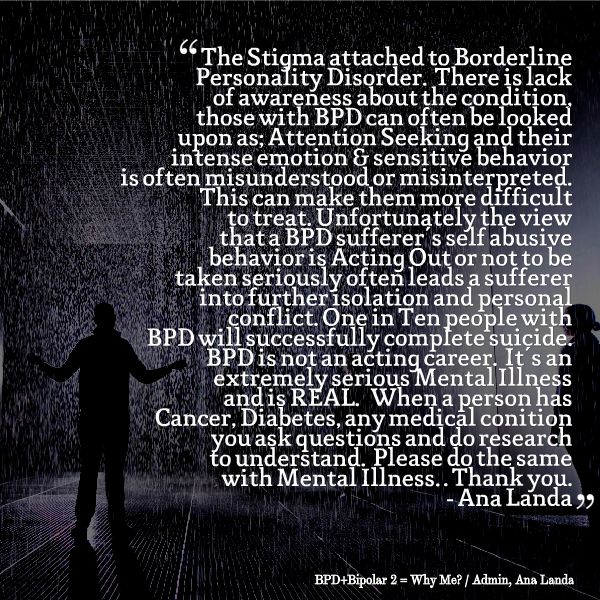
- Personality disorders, especially borderline personality disorder and paranoid personality disorder.
Management and Treatment
How is delusional disorder treated?
Treatment for delusional disorder most often includes psychotherapy (talk therapy) and medication, but delusional disorder is highly resistant to treatment with medication alone.
People with delusional disorder often don’t seek treatment for the condition on their own because most people with delusional disorder don’t realize their delusions are problematic or incorrect. It’s more likely they’ll seek help due to other mental health conditions such as depression or anxiety.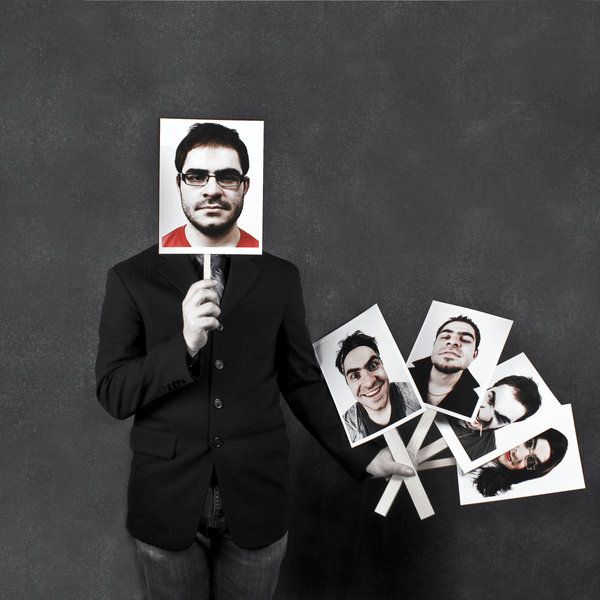
People with severe symptoms or who are at risk of hurting themselves or others might need to be admitted to the hospital until the condition is stabilized.
Psychotherapy for delusional disorder
Psychotherapy is a term for a variety of treatment techniques that aim to help people identify and change troubling emotions, thoughts and behaviors. Working with a mental health professional, such as a psychologist or psychiatrist, can provide support, education and guidance to the person and their family.
Through therapy, people with delusional disorder can learn to manage their symptoms, identify early warning signs of relapse and develop relapse prevention plans. Types of psychotherapy include:
- Individual psychotherapy: This type of therapy can help a person recognize and correct the underlying thinking that has become distorted.
- Cognitive behavioral therapy (CBT): This is a structured, goal-oriented type of therapy.
 A mental health professional helps people take a close look at their thoughts and emotions. They’ll come to understand how their thoughts affect their actions. Through CBT, they can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits.
A mental health professional helps people take a close look at their thoughts and emotions. They’ll come to understand how their thoughts affect their actions. Through CBT, they can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits. - Family-focused therapy: This therapy can help people with delusional disorder and their families. This treatment involves psychoeducation regarding delusional disorder, communication improvement training and problem-solving skills training.
Medications for delusional disorder
The primary medications used to help treat delusional disorder are called antipsychotics (neuroleptics). Medications include the following:
- First-generation (“typical”) antipsychotics: Healthcare providers have used these medications to treat mental health conditions since the mid-1950s. These medicines work by blocking dopamine receptors in your brain. Dopamine is a neurotransmitter believed to be involved in the development of delusions.
 First-generation antipsychotics include chlorpromazine (Thorazine®), fluphenazine (Prolixin®), haloperidol (Haldol®), thiothixene (Navane®), trifluoperazine (Stelazine®), perphenazine (Trilafon®) and thioridazine (Mellaril®).
First-generation antipsychotics include chlorpromazine (Thorazine®), fluphenazine (Prolixin®), haloperidol (Haldol®), thiothixene (Navane®), trifluoperazine (Stelazine®), perphenazine (Trilafon®) and thioridazine (Mellaril®). - Second-generation (“atypical”) antipsychotics: These newer antipsychotics are also effective in treating the symptoms of delusional disorder. They work by blocking dopamine and serotonin receptors in your brain. These drugs include risperidone (Risperdal®), clozapine (Clozaril®), quetiapine (Seroquel®), ziprasidone (Geodon®) and olanzapine (Zyprexa®). These medications are usually better tolerated than first-generation antipsychotics.
Other medications that healthcare providers might prescribe to treat delusional disorder include anxiolytics and antidepressants. Anxiolytics might help if the person has a very high level of anxiety and/or problems sleeping. Antidepressants can help treat depression, which often occurs in people with delusional disorder.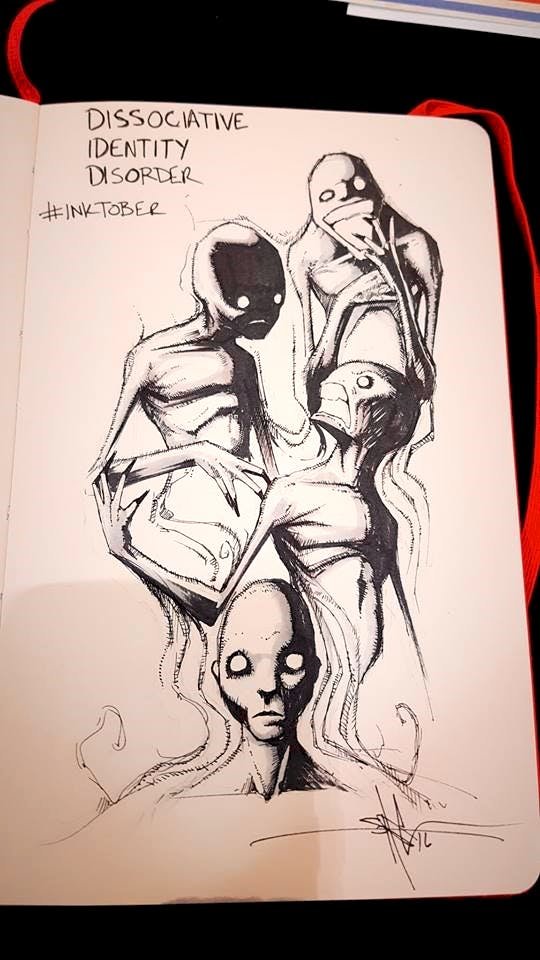
Prevention
Can delusional disorder be prevented?
There’s no known way to prevent delusional disorder. However, early diagnosis and treatment can help decrease the disruption to the person’s life, family and friendships.
Outlook / Prognosis
What is the prognosis (outlook) for delusional disorder?
The prognosis (outlook) for people with delusional disorder varies depending on a few factors, including:
- The type of delusional disorder.
- The severity of the delusions.
- The person’s life circumstances, including the availability of support and a willingness to stick with treatment.
Delusional disorder doesn’t usually significantly affect a person’s daily functioning, but the severity of the delusion may gradually get worse. Most people with delusional disorder can remain employed as long as their work doesn’t involve things related to their delusions.
The prognosis of delusional disorder is better if the person sticks to their treatment plan.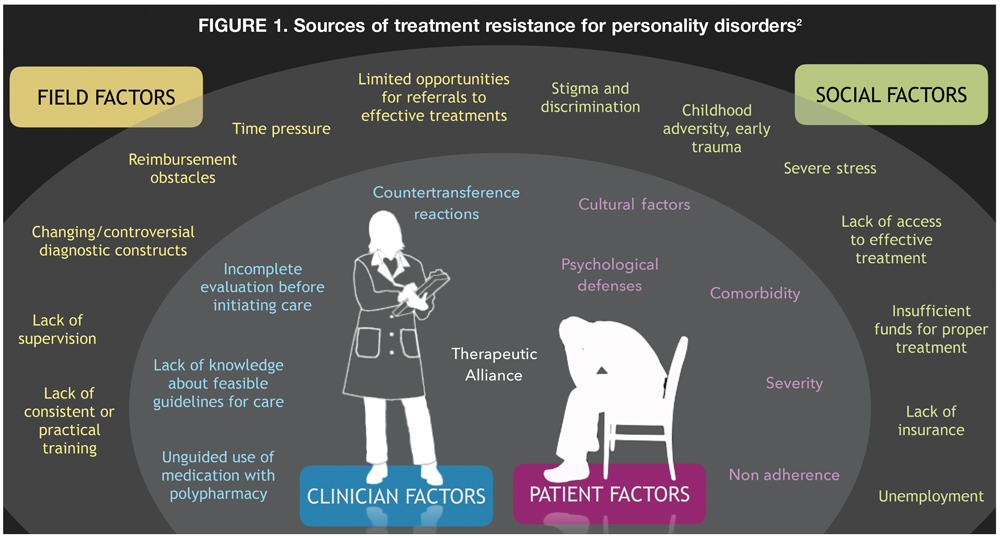 Almost 50% of people have a full recovery, more than 20% of people report a decrease in symptoms and less than 20% of people report minimal to no change in symptoms.
Almost 50% of people have a full recovery, more than 20% of people report a decrease in symptoms and less than 20% of people report minimal to no change in symptoms.
Unfortunately, many people with this condition don’t seek help. It’s often difficult for people with mental health conditions to recognize they’re not well. They also might be too embarrassed or afraid to seek treatment. Without treatment, delusional disorder can be a life-long condition.
What are the possible complications of delusional disorder?
If left untreated, delusional disorder might lead to:
- Depression, often as a consequence of difficulties associated with the delusions.
- Social isolation.
- Legal issues — for example, stalking or harassing the person involved with the delusion could lead to arrest.
- Self-harm or harm to others. This is more common in the jealous and persecutory types.
Living With
How can I help someone with delusional disorder?
If you know someone with delusional disorder, you can help by providing support and encouragement for them to seek help and treatment.
People with delusional disorder who feel pressured or repeatedly criticized by others will likely experience stress, which may worsen their symptoms. Because of this, a positive approach may be more helpful and effective.
The friends and family members of people with delusional disorder often experience stress, depression, grief and isolation. It’s important to take care of your mental health and seek help if you’re experiencing these symptoms.
A note from Cleveland Clinic
It’s important to remember that delusional disorder is a mental health condition. As with all mental health conditions, seeking help as soon as symptoms appear can help decrease the disruptions to life. Mental health professionals can offer treatment plans that can help manage thoughts and behaviors.
Substance Use Disorder (SUD): Symptoms & Treatment
Overview
What is substance use disorder?
Substance use disorder (SUD) is a mental health condition in which a person has a problematic pattern of substance use that causes distress and/or impairs their life.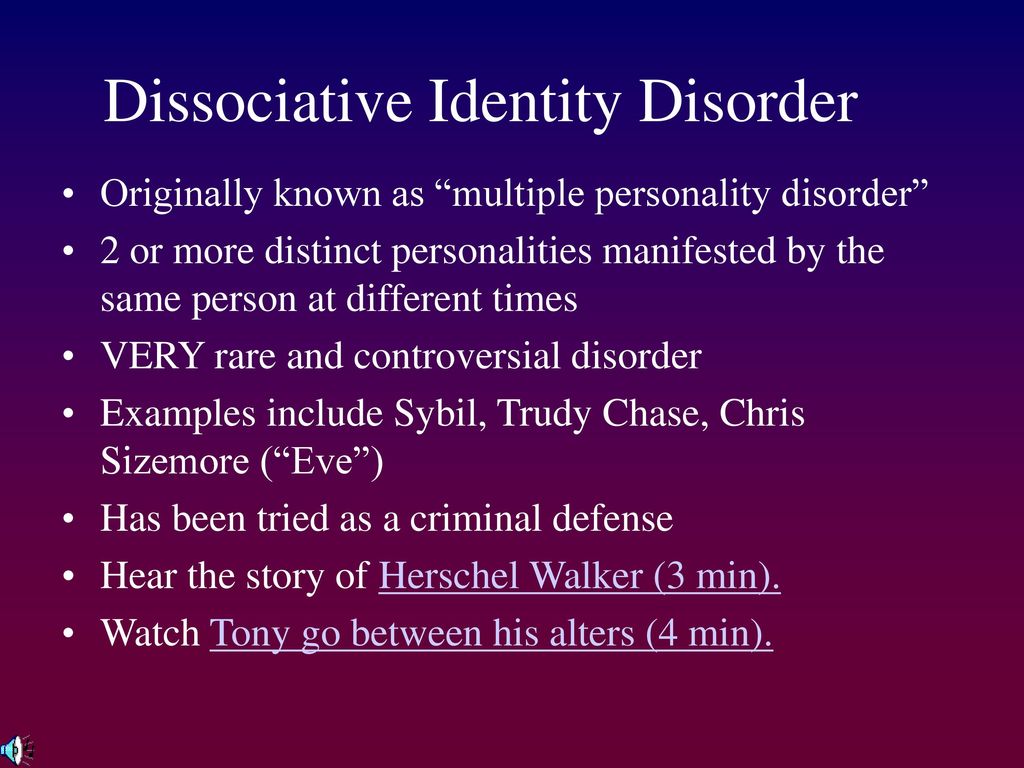
SUD exists on a spectrum and may be mild, moderate or severe. It typically involves an overpowering desire to use the substance, increased tolerance to the substance and/or withdrawal symptoms when you stop taking the substance.
A person can have more than one substance use disorder at a time, such as alcohol use disorder and cocaine use disorder.
Substance use disorder can significantly impact your health, relationships and overall quality of life. It can also be life-threatening. It’s crucial to seek help as soon as you develop signs of SUD.
What are substances?
Substances are drugs that have addiction potential. They can be prescription drugs or non-medical drugs and include:
- Alcohol.
- Caffeine.
- Cannabis (marijuana).
- Hallucinogens, such as PCP and LSD.
- Hypnotics, sedatives and anxiolytics (anti-anxiety drugs), such as sleeping pills, benzodiazepines and barbiturates.
- Inhalants, such as paint thinners, aerosol sprays, gases and nitrites (poppers).

- Prescription and non-prescription opioids, such as codeine, oxycodone and heroin.
- Prescription and non-prescription stimulants, such as Adderall®, cocaine and methamphetamine.
- Tobacco/nicotine, such as smoking cigarettes and electronic cigarettes (e-cigarettes or vaping).
While these substances are very different from each other, they all strongly activate the reward center of your brain and produce feelings of pleasure.
These substances vary in how likely they are to lead to SUD. The likelihood is called “addiction liability,” and it depends on multiple factors, including:
- How you take the substance (such as orally, by injection or by inhaling).
- The rate at which the substance crosses the blood-brain barrier and triggers the reward pathway in your brain.
- The time it takes to feel the effect of the substance.
- The substance’s ability to induce tolerance and/or withdrawal symptoms.
What’s the difference between substance use/misuse and substance use disorder?
Substance use/misuse refers to occasional episodes of substance use rather than chronic, habitual or patterned use.
People can use substances occasionally without developing SUD, but even a few episodes of taking certain substances can lead to tolerance and dependence. Tobacco, heroin, cocaine, alcohol, cannabis and benzodiazepines are all substances that you can develop tolerance and dependence to.
What is the difference between substance use disorder and addiction?
Substance use disorder can be mild, moderate or severe. Addiction is the most severe form of SUD. It involves continued substance use despite negative consequences. Addiction to substances happens when the reward system in your brain “takes over” and amplifies compulsive substance-seeking.
Both involve the development of physical dependence and psychological dependence.
People are psychologically dependent when a drug is so central to their thoughts, emotions and activities that the need to continue its use becomes a craving or compulsion despite negative consequences.
With physical dependence, your body has adapted to the presence of the substance, and withdrawal symptoms happen if you suddenly stop taking the drug or you take a reduced dosage.
In the past, healthcare providers, organizations and members of the public often used the terms “addiction/addict,” “abuse/abuser” and “dependence” when referring to substance use.
Mental health condition classification systems, including the Diagnostic and Statistical Manual of Mental Disorders (DSM), have become more sophisticated over time. The term “substance use disorder” allows for more clarity in diagnosis. SUD also recognizes a spectrum of problematic substance use, not just physiologic addiction.
In addition, there’s a lot of stigma and negativity associated with the terms “addiction/addict” and “abuse/abuser.” Similarly, people often use the terms “addiction” and “addict” casually to describe an affinity for a thing, place or hobby. This downplays the seriousness and complexity of true addiction and substance use disorder.
Who does substance use disorder affect?
Substance use disorder affects people of all ages, races, genders and socioeconomic levels.
In general, people assigned male at birth (AMAB) are more likely to develop SUD. Substance use/misuse is highest among people aged 18 to 25.
How common is substance use disorder?
Substance use disorder is common. Over 20 million people in the United States have at least one SUD.
About 20% of people in the U.S. who have depression or an anxiety disorder also have a substance use disorder.
Of the over 20 million people in the U.S. who have SUD:
- 38% have a drug substance use disorder.
- 73% have alcohol use disorder.
- 12% have both a drug SUD and alcohol use disorder.
What is the most common substance use disorder?
Tobacco use disorder is the most common substance use disorder worldwide and in the United States.
Symptoms and Causes
What are the signs and symptoms of substance use disorder?
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, the signs of substance use disorder include:
- Taking the substance in larger amounts and for a longer amount of time than you’re meant to if it’s a prescription.
- Having a strong desire or urge to use the substance.
- Having unsuccessful efforts to cut down on or control substance use.
- Spending a lot of time obtaining or using the substance or recovering from its effects.
- Having issues fulfilling responsibilities at work, school or home due to substance use.
- Continuing to use the substance, even when it causes problems in relationships.
- Giving up social, occupational or recreational activities because of substance use.
- Using substances again and again, even when it puts you in danger.
- Continuing substance use despite an ongoing physical or psychological problem that’s likely caused or worsened by the substance.
- Developing tolerance (need for increased amounts to get the same effect).
- Experiencing withdrawal symptoms, which can be relieved by taking more of the substance.
Seeking medical care as soon as you have signs of substance use disorder is essential.
Other symptoms and behaviors of substance use may include:
- Confusion.
- Neglecting to eat.
- Withdrawing from friends and family.
- Sudden changes in mood and behavior.
- Engaging in risky behaviors.
- Hostility or denial when you’re confronted about substance use.
- Not caring about your physical appearance as much as you used to.
- Secretive behavior to hide substance use.
- Using substances even when you’re alone.
How does substance use disorder develop?
The progression to a substance use disorder often follows this pattern:
- Experimental use (or prescription use).
- Occasional use (or using prescriptions not as directed).
- Heavy use.
- Substance use disorder.
This progression is complex, and several complex factors contribute to the development of substance use disorder, including:
- The substance’s effect on your brain chemistry.
- Genetics.
- Mental health conditions.
- Access and exposure to the substance.
- Adverse childhood experiences (ACEs).
Brain chemistry
Substances affect your brain, especially the reward center of your brain.
Humans are biologically motivated to seek rewards. Often, these rewards come from healthy behaviors. When you spend time with a loved one or eat a delicious meal, your body releases a chemical called dopamine, which makes you feel pleasure. It becomes a cycle; you seek out these experiences because they reward you with good feelings.
Substances send massive surges of dopamine through your brain, too. But instead of feeling motivated to do the things you need to survive (eat, work and spend time with loved ones), such massive dopamine levels can lead to damaging changes that affect your thoughts, feelings and behavior.
This can create an unhealthy drive to seek more pleasure from the substance and less from more healthy experiences.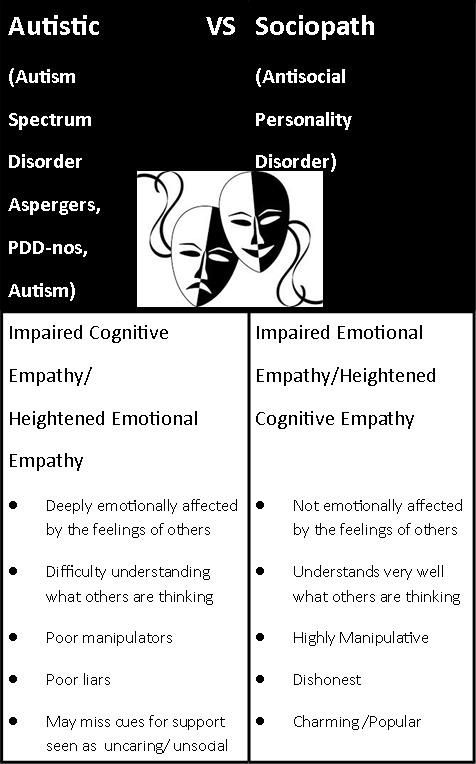
Over time, the substances change your brain chemistry, and you become desensitized to their effects. You then need more to produce the same effect.
For some substances, such as opioids, the withdrawal symptoms are so severe that they create significant motivation to continue using them.
Genetics
Studies show that genetic factors are responsible for 40% to 60% of the vulnerability to any substance use disorder. If you have a first-degree relative (biological sibling or parent) with SUD, you’re more likely to develop it.
Scientists are working to locate specific genes that may contribute to this vulnerability. For example, they’ve found that a change in the CHRNA2 gene on chromosome 8 is associated with cannabis use disorder, including diagnosis at an earlier age.
Mental health conditions
About half of people who experience a mental health condition will also experience a substance use disorder and vice versa. This is known as a dual diagnosis.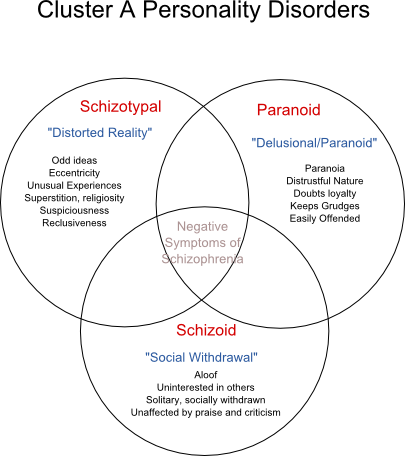 In 2020, 17 million U.S. adults had a co-occurring mental health disorder and SUD.
In 2020, 17 million U.S. adults had a co-occurring mental health disorder and SUD.
SUDs and other mental health conditions are caused by overlapping factors such as genetic vulnerabilities, issues with similar areas of your brain and environmental influences.
Research shows that mental illness may contribute to SUD, and SUD can contribute to the development of mental illness.
Having any of the following mental health conditions can contribute to the development of SUD:
- Attention-deficit/hyperactivity disorder (ADHD).
- Bipolar disorder.
- Borderline personality disorder.
- Depression.
- Generalized anxiety disorder.
- Panic disorder.
- Post-traumatic stress disorder (PTSD).
Access and exposure
Access to substances is a particularly significant environmental risk factor. Factors that increase the extent of exposure and the opportunity for substance use include:
- Use of substances by a member of your household.
- Use of substances by your peers.
- Being prescribed a drug that can be misused, such as opioids or stimulants.
Adolescents are especially at risk for developing SUD due to exposure. Adolescents who start using substances early are more likely to develop an SUD. About 70% percent of people who began using at age 13 have an SUD compared to 27% who started at age 17.
In addition, it’s more likely that someone will use substances that are legally and/or readily available (like alcohol and tobacco). This increases the risk of progression to problematic use. Opioids are another example of this — the availability and volume of prescription opioids make them easier to access.
Adverse childhood experiences (ACEs)
Adverse childhood experiences (ACEs) are stressful or traumatic events during childhood. They can include:
- Childhood abuse and neglect.
- Household dysfunction.
- Witnessing domestic violence.
- Having family members who have SUD.
- Parental incarceration.
ACEs are strongly related to the development of a wide range of health problems throughout a person’s lifespan, including SUD. The more ACEs a child experiences, the more at risk they are for developing SUD at some point in their life.
Diagnosis and Tests
How is substance use disorder diagnosed?
A single test can’t diagnose substance use disorder. Instead, healthcare providers rely on a thorough evaluation of your medical history and behaviors surrounding substance use. They may order drug tests and evaluate prescription drug monitoring program reports.
A provider will also ask about your mental health history, as it’s common to have an SUD and a mental health condition.
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a person must have at least two signs in the symptoms section over 12 months to be diagnosed with substance use disorder.
It’s important to remember that SUD exists on a spectrum of severity:
- Two to three signs indicate a mild substance use disorder.
- Four or five signs indicate a moderate substance use disorder.
- Six or more symptoms indicate a severe substance use disorder.
Management and Treatment
What is the treatment for substance use disorder?
Effective treatments are available for substance use disorder. Treatment is highly individualized — one person may need different types of treatment at different times.
Treatment for SUD often requires continuing care to be effective, as SUD is a chronic condition with the potential for both recovery and relapse.
As people with SUD often have co-occurring mental health conditions, treating them together rather than separately is generally better.
The three main forms of treatment include:
- Detoxification.
- Cognitive and behavioral therapies.
- Medication-assisted therapies.
There are also several different types of treatment settings, including:
- Outpatient counseling.
- Intensive outpatient treatment.
- Inpatient treatment.
- Long-term therapeutic communities, such as sober living communities.
Detoxification
In detoxification, you stop taking the substance(s), allowing them to leave your body. Depending on the severity of the SUD, the substance or an alternative may be tapered off to lessen the effects of withdrawal. It’s the first major step of treatment for SUD. You can go through detoxification in both inpatient and outpatient settings.
Cognitive and behavioral therapies
Psychotherapy (talk therapy) can help treat SUD and any other co-occurring mental health conditions. Therapy also teaches healthy coping mechanisms.
Healthcare providers may recommend cognitive and behavioral therapies alone or in combination with medications.
Some examples of effective therapies for adults with SUDs include the following:
- Cognitive behavioral therapy (CBT): CBT is a structured, goal-oriented type of psychotherapy.
 A mental health professional helps you look closely at your thoughts and emotions during CBT. You’ll come to understand how your thoughts affect your actions. You can unlearn negative thoughts and behaviors through CBT and learn to adopt healthier thinking patterns and habits. For SUD, CBT also involves encouraging motivation to change and education about treatment and preventing relapse.
A mental health professional helps you look closely at your thoughts and emotions during CBT. You’ll come to understand how your thoughts affect your actions. You can unlearn negative thoughts and behaviors through CBT and learn to adopt healthier thinking patterns and habits. For SUD, CBT also involves encouraging motivation to change and education about treatment and preventing relapse. - Dialectical behavior therapy (DBT): DBT is especially effective for people who have difficulty managing and regulating their emotions. DBT has proven to be effective for treating and managing various mental health conditions, including SUD.
- Assertive community treatment (ACT): ACT provides mental health services in a community setting rather than a residential or hospital setting. ACT is highly individualized. Your treatment plan will focus on your strengths, needs and goals for the future.
- Therapeutic communities (TCs): A TC is a long-term residential treatment that focuses on helping people with SUD develop new and healthier values and behaviors related to substance use and other co-occurring mental health conditions.

- Contingency management (CM): CM encourages healthy behaviors by offering rewards for desired behaviors. Most commonly, the treatment provides something of monetary value to people with SUD to incentivize them not to use substances. For instance, upon a negative drug test result, you earn a chance to receive a prize or gift card.
Participating in self-help programs, like Narcotics Anonymous, can also play a significant role in SUD treatment.
These programs support behavioral modification through self-help and peer support. The underlying principle of these programs is that people with SUD must understand that they have a chronic condition that will never go away. Group therapy supports people with SUD in maintaining self-control and restraint.
Medication
Medication may be part of your treatment plan. Medications can help modify your brain chemistry to help treat certain SUDs. They can also relieve cravings and withdrawal symptoms.
Medication-assisted treatments are available for:
- Opioids: Methadone, buprenorphine and naltrexone are FDA-approved for the treatment of opioid use disorder.
- Alcohol: Three FDA-approved drugs include naltrexone, acamprosate and disulfiram.
- Tobacco: A nicotine patch, spray, gum or lozenge can help. Or your provider might prescribe bupropion or varenicline.
Prevention
How can I prevent substance use disorder?
Preventing substance use and SUD starts with education. Education in schools, communities and families helps prevent using a substance or misusing a prescription medication for the first time. Other ways to prevent SUD include:
- Following instructions for prescription medications. Don’t ever take more than instructed. Opioid use disorder, for instance, can start after just five days of misuse.
- Never sharing your prescription medication with someone else or selling your medication.
 Always store it in a safe place away from children.
Always store it in a safe place away from children. - If you have leftover prescription medications (such as opioids) at the end of your treatment, find a community drug take-back program or pharmacy mail-back program to safely dispose of them.
The risk of substance use increases greatly during times of stress and change. For an adult, a divorce, loss of a job or death of a loved one may increase the risk of substance use. For a teenager, moving, family divorce or changing schools can increase their risk.
It’s important to turn to healthy coping mechanisms during these times of change, such as exercising, meditating or learning a new hobby. Consider seeing a mental health professional if you’re having issues managing your stress.
Outlook / Prognosis
What is the prognosis for substance use disorder?
The prognosis (outlook) for substance use disorder varies based on several factors, including:
- The type and severity of the SUD.
- The degree of dependence and withdrawal.

- The level of commitment to abstinence.
- Treatment time frame.
- Genetics.
- How you cope during stressful situations.
Substance use disorder is a lifelong disease. But people can recover from it and lead full lives. Getting help is essential to recovery. Different tools work for different people, but ongoing therapy and self-help groups such as Narcotics Anonymous help many.
SUD is a relapsing disease. People who are in recovery have a higher chance of using substances again. Recurrence can happen even years after you last took the substance.
Because of the possibility of relapse, you need ongoing treatment. Your healthcare provider should review your treatment plan with you and change it based on your changing needs.
What are the possible complications of substance use disorder?
The complications of substance use disorder are broad and may depend on the type of substance use.
Substance use disorder can impact multiple systems of your body, including your:
- Nervous system, including psychiatric impacts.
- Cardiovascular system.
- Endocrine system.
- Immune system.
- Hepatic (liver) system.
Specific chronic and acute complications can include:
- Memory loss and overall cognitive issues.
- Personality changes and mood dysregulation.
- Loss of nerve function.
- Stroke.
- Seizures.
- Heart failure.
- Nasal septal perforation.
- Respiratory depression.
- Liver failure.
- Certain cancers. For example, alcohol use disorder is associated with cancers of the mouth, throat, esophagus, liver, colon and breast.
- Blood-borne virus infections, such as hepatitis B (HBV), hepatitis C (HCV) and the human immunodeficiency virus (HIV) from using shared injection equipment.
- Overdose.
- Coma.
- Death.
Living With
How can I help a loved one with substance use disorder?
It can be very challenging and stressful to learn that someone you love may have substance use disorder. Here are some tips to help your loved one and yourself:
Here are some tips to help your loved one and yourself:
- Speak up sooner rather than later: The earlier a person with SUD receives treatment, the better. Address your concerns and help them find treatment as soon as possible. Suggest calling a helpline, talking to a healthcare provider or mental health professional, entering a treatment program or going to a 12-step program. Offer your help and support without being judgmental.
- Practice empathy: Even when you don’t agree with your loved one, listen thoughtfully to them. The more your loved one feels heard, the more they’ll see you as someone they can trust.
- Be patient: Don’t expect a single conversation or action to fix your loved one’s substance use. SUD is a complex chronic condition, and there’s no quick fix to overcoming it.
- Take care of yourself: The friends and family members of people with SUD often experience stress, depression, grief and isolation.
 It’s important to take care of your mental health and seek help if you’re experiencing these symptoms. Consider joining a support group or organization in your community.
It’s important to take care of your mental health and seek help if you’re experiencing these symptoms. Consider joining a support group or organization in your community.
When should I see my healthcare provider?
If you’re currently taking a prescription drug and are concerned you may be developing a dependence, talk to your healthcare provider immediately.
If you think your child may be using substances, get them help as soon as possible.
A note from Cleveland Clinic
Substance use disorder is a complex mental health and brain condition. Substances — such as alcohol, stimulants and opioids — affect your brain, including your decision-making ability. These changes make it hard to stop taking the substance, even if you want to. If you or a loved one has substance use disorder, talk to a healthcare provider as soon as possible. A trained provider can help guide you to the treatment you need.
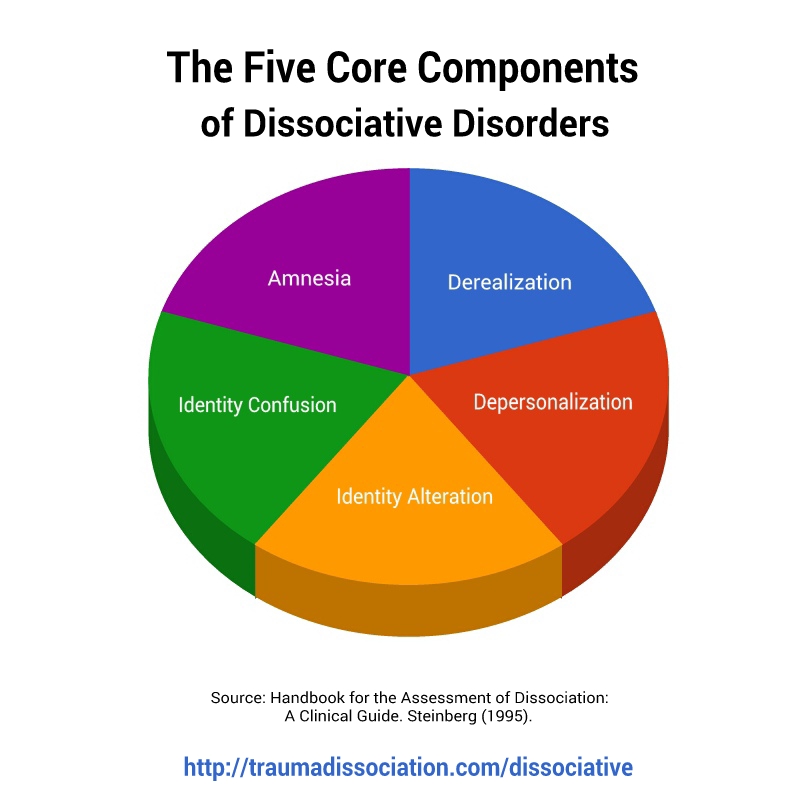
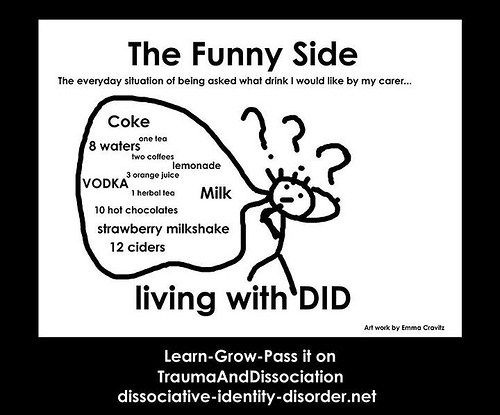
What is Dissociative Identity Disorder?
Dissociative Identity Disorder is a mental disorder characterized by either having two or more personalities, or a state of disconnection from the outside world, one's identity, and an inability to recall certain daily life events and important personal information. This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
Types of dissociative personality disorder
There are several types of dissociative disorders, which are characterized by different symptoms and manifestations. One of them is dissociative fugue, a disorder in which a person can find himself in a completely unfamiliar place and not remember how he got there. In this case, a person may forget some important information about himself and not even remember his name. At the same time, memory for some information, such as literature, science, and other things, can be preserved. In a state of fugue, a person assumes a different personality and identity with a different character, mannerisms and behavior. While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
A person who has a dissociative disorder is actually suffering a lot from their condition.
Another type of dissociative disorder is the presence of several personalities in which a person finds himself in turn or simultaneously. At such moments, he disconnects from himself and stops feeling his own body, and also cannot see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and behave in completely different ways. Often these personalities can even have different physiological manifestations. For example, while in one personality, a person can see poorly and wear glasses, and in another, have excellent vision and walk without glasses or lenses (or think that he sees perfectly and does without glasses). Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Manifestations of dissociative identity disorder
This disease affects both children (adolescents) and adults and presents with similar symptoms. However, dissociative disorder with multiple personalities in adolescents is quite rare. In old age, dissociation practically does not develop. When a specialist suspects a person of dissociative identity disorder, he usually asks if it happened that the person suddenly found himself in some place and did not understand how he got there. Also, the patient may suddenly speak in a completely different voice, he may have a different handwriting. For example, a person who has one of his personalities as a child may suddenly begin to write in a child's handwriting. Such phenomenal manifestations can be evoked in a patient suffering from dissociative personality disorder, and in a state of hypnosis. That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
See also
Myths about hypnosis
A person who has a dissociative disorder is, in fact, suffering greatly from his condition. He sees the negative or dismissive attitude of those around him: they look at him strangely, they reject him, no one finds a common language with him, because of him the family can collapse, and so on. At the moment of a dissociative state, a person does not have the opportunity to critically look at himself and his own behavior. That is, in a situation where one of the alternative personalities appears, he is in an inadequate state.
The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence.
Dissociation is one of three conditions in which the patient is exempt from criminal liability, along with psychosis and mental retardation. There were cases when people in a dissociative state committed murder and rape. In such situations, even taking into account the severity of the crimes, patients are not sent to prison, but are sent to a psychiatric hospital or, in extreme cases, to a special ward of the psychiatric department of the prison.
Causes of dissociative identity disorder
Scientists have not yet found the genetic causes of dissociative identity disorder. The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence. However, even this theory does not explain all 100% of cases of dissociative states. There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
Diagnosis of dissociative identity disorder
Diagnosis of dissociative identity disorder is made through clinical interviews with several specialists. Sometimes the diagnosis requires not one, but several meetings with psychologists and psychiatrists, so that they have the opportunity to identify different aspects of the disorder, look at the patient's condition from several points of view and assemble a consultation. However, the specialist who identifies this disorder must have a great deal of experience and qualifications, since this disease can often be confused with others.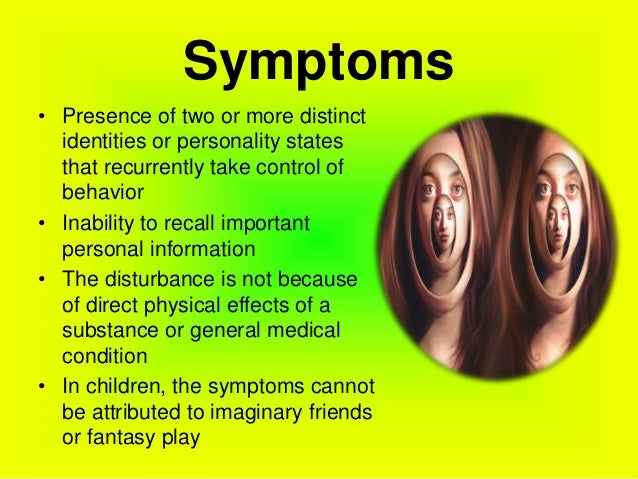 In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
Medications do not cure dissociative identity disorder, but only relieve some of the symptoms.
See also
Mental norm and pathology
A separate task for a specialist in the process of diagnosing dissociation in a child is to distinguish diseases from the presence of imaginary friends in a child, which very often appear in perfectly healthy children at a certain age. To do this, a specialist must be highly qualified in the field of developmental psychology and clearly be able to recognize a dissociative disorder not only in adults, but also in children.
Treatment of dissociative identity disorder
The main treatment for dissociative personality disorder is hypnosis. Sometimes specialists connect methods of psychoanalysis or cognitive-behavioral psychotherapy to treatment. Also, in some cases, medication is used to relieve symptoms. Drugs are prescribed if the disorder is accompanied by depression, panic attacks, drug or alcohol addiction. Medications do not cure dissociative identity disorder, but only relieve some of the symptoms. If a child suffers from this disease, then specialists carry out separate work with his parents, provide them with methods of proper communication with the child to improve the results of his treatment.
Sometimes specialists connect methods of psychoanalysis or cognitive-behavioral psychotherapy to treatment. Also, in some cases, medication is used to relieve symptoms. Drugs are prescribed if the disorder is accompanied by depression, panic attacks, drug or alcohol addiction. Medications do not cure dissociative identity disorder, but only relieve some of the symptoms. If a child suffers from this disease, then specialists carry out separate work with his parents, provide them with methods of proper communication with the child to improve the results of his treatment.
If you do not treat dissociative personality disorder, but let the disease take its course, then in the case of multiple personalities, a person in an inadequate state can commit some extremely negative actions in relation to others, for example, violent ones. In the case of a dissociative fugue, a person may get lost and never return home - it will simply be impossible to find him.
- Diseases and disorders
Share:
how multiple personality arises - T&P
Multiple personality disorder is a bright but rather controversial disease that still causes heated discussions among doctors and scientists.
 Someone doubts whether it exists at all, someone doubts whether this state should be considered a deviation from the norm. "Theories and Practices" remembered how the research of this psychiatric phenomenon began and why one should not rush to evaluate it.
Someone doubts whether it exists at all, someone doubts whether this state should be considered a deviation from the norm. "Theories and Practices" remembered how the research of this psychiatric phenomenon began and why one should not rush to evaluate it. Dissociative identity disorder is a condition in which, in addition to the main personality, the patient has at least one (and often more) subpersonality that periodically “takes control” of the body and acts in accordance with their own ideas about life. These ideas can be very different from the habits and philosophy of the real owner of the body.
Despite the fact that some experts consider this disease iatrogenic - that is, provoked by the careless words of doctors or watching a "scientific" TV show - there is a number of evidence indicating the opposite. One of the most impressive is the history of the disease. Cases of dissociative disorder were also recorded when neither psychotherapists nor TV shows were in sight. However, psychiatry itself did not exist.
However, psychiatry itself did not exist.
One of the first described cases of dissociative personality disorder occurred at the end of the 18th century in the German city of Stuttgart. A revolution had just taken place in France, and the aristocrats, saving their lives, fled from their native country to neighboring states, including Germany. A young resident of Stuttgart took their misfortunes too close to her heart. She suddenly had a second personality - a Frenchwoman. She not only spoke her “native language” perfectly, but also coped noticeably worse with German, she had a noticeable accent. The Frenchwoman who appeared was of aristocratic blood, and her manners and habits fully corresponded to her status. It is noteworthy that the German girl did not remember what the "Frenchwoman" was doing, and she did not know anything about the legal mistress of the body.
The young German woman was not the only person with this disease in her century, but nevertheless her illness turned out to be extremely rare - in total, 76 cases of dissociative identity disorder were documented up to the middle of the 20th century. Interestingly, in recent decades, much more of them have been described - today more than 40 thousand people with this diagnosis live in the world. However, this does not mean the beginning of an "epidemic" - psychiatry, with all its arsenal of medicines, appeared only in the middle of the last century, and, accordingly, control over the incidence of such disorders began not much earlier.
Interestingly, in recent decades, much more of them have been described - today more than 40 thousand people with this diagnosis live in the world. However, this does not mean the beginning of an "epidemic" - psychiatry, with all its arsenal of medicines, appeared only in the middle of the last century, and, accordingly, control over the incidence of such disorders began not much earlier.
To date, quite a lot of books and articles have been written about multiple personality disorder, both popular and academic. The most interesting thing about it is, perhaps, the moment of the onset of the disease in childhood. No one is born a “ready-made”, whole person. Growing up, the child experiences many emotions and experiences that are loosely related to each other. Over time, they integrate together, forming one common identity. However, the development of a child does not always go smoothly. In cases where children at an early age (about 2 years) are separated from their mother when they experience abuse or some traumatic experience, childhood experiences can remain segregated and lead to the formation of two or more personalities. Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Dissociative identity disorder often begins in childhood, but may appear later. Over the years, patients, as a rule, have an increasing number of "tenants". Since individuals, as a rule, perform certain functions, help to cope with certain life situations, with the emergence of new tasks and problems, new residents appear who are able to cope with them. Each of the subpersonalities has its own worldview, its own habits, gestures and facial expressions, even age and intelligence. At certain moments, by the good will of the "owner" or against it, some of the personalities gain control over the body, and everything done by it during use, as a rule, is not controlled and is not remembered by the patient himself.
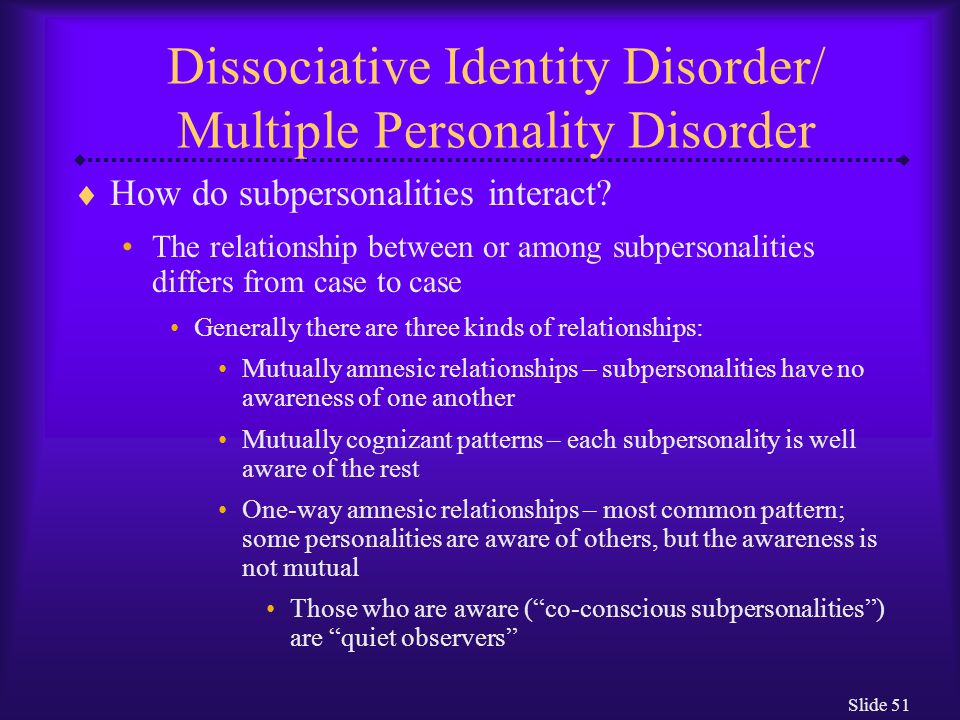
A key issue in the lives of patients with dissociative personality disorder is the relationship that has developed in the “team”. Sub-personalities may or may not be aware of each other's existence, be aggressive or silently roam museums at their own time, negotiate rental schedules with the owner of the body, or regularly stage power grabs. The treatment strategy also depends on these factors - it is based on psychotherapy, and although its ultimate goal is to come to the integration of personalities into one, an important task in the process is the "neutralization" of dangerous tenants, and the organization of harmonious relations between all subpersonalities.
Sub-personalities may or may not be aware of each other's existence, be aggressive or silently roam museums at their own time, negotiate rental schedules with the owner of the body, or regularly stage power grabs. The treatment strategy also depends on these factors - it is based on psychotherapy, and although its ultimate goal is to come to the integration of personalities into one, an important task in the process is the "neutralization" of dangerous tenants, and the organization of harmonious relations between all subpersonalities.
More than one person in one body is unfortunately not the only symptom of dissociative identity disorder. It is often accompanied by depression, anxiety disorders, phobias, sleep and eating disorders, even hallucinations. Dissociative disorder is sometimes confused with schizophrenia, but these diseases can be distinguished - in schizophrenia, as a rule, the symptoms are perceived as enemy actions of aliens, the KGB or members of the Masonic lodge, which is not the case with dissociative disorder. In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not only separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not only separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
Treatment of patients diagnosed with multiple personality disorder is usually long, difficult and emotionally costly. However, not everyone agrees that it should be treated at all. The American psychologist James Hillman, the founder of the school of archetypal psychology, is convinced that the position that multiple personality syndrome is considered a disorder is nothing more than a stereotype that can and should be fought, advocating the right of people with this diagnosis to be considered no less normal than others. The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
Flora Schreiber
A serious and very detailed book written by a doctor about his own patient who is trying to get along with her sixteen subpersonalities.
Daniel Keyes
Incredible biography of the most famous criminal diagnosed with multiple personality disorder. 24 personalities coexisted in the body of Billy Milligan, including a Yugoslav communist, a lesbian poet, and a three-year-old girl.