What is catatonic state
Definition, Causes, Symptoms & Treatment
Overview
What is catatonia?
Catatonia is a disorder that disrupts how your brain works, disrupting how a person processes and reacts to the world around them. People with catatonia often don’t react to things happening nearby or may react in ways that seem unusual. Impaired communication, unusual movements or lack of movement, and behavior abnormalities are the most striking features of this condition.
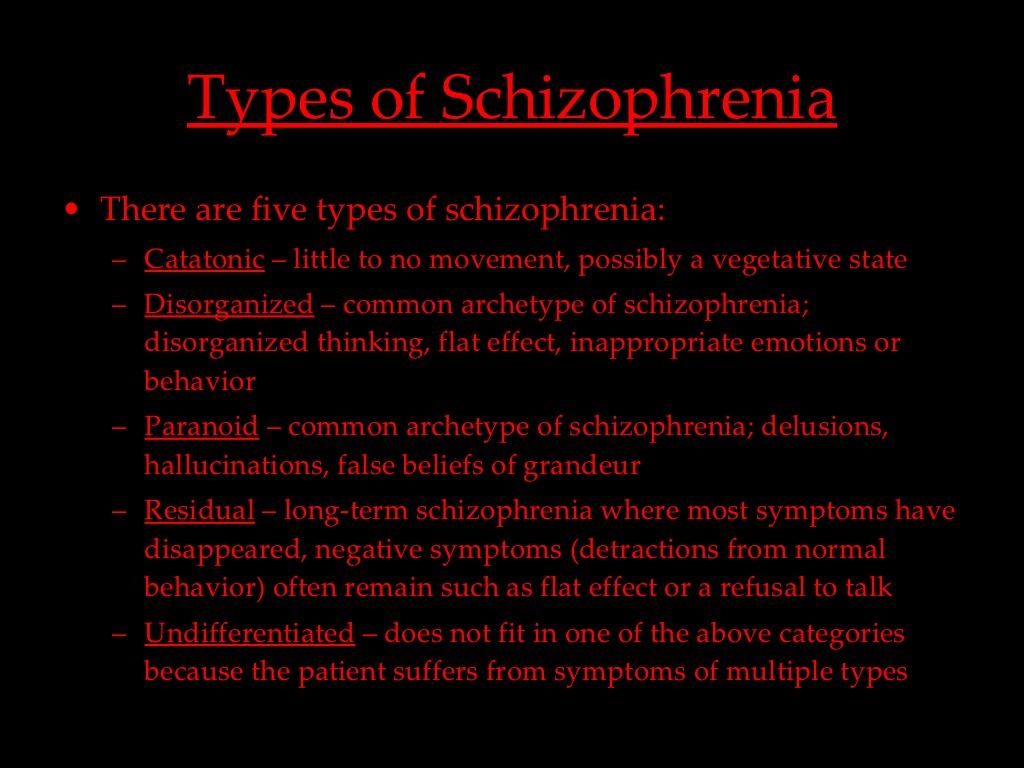
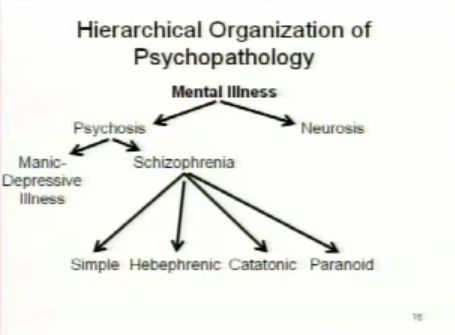
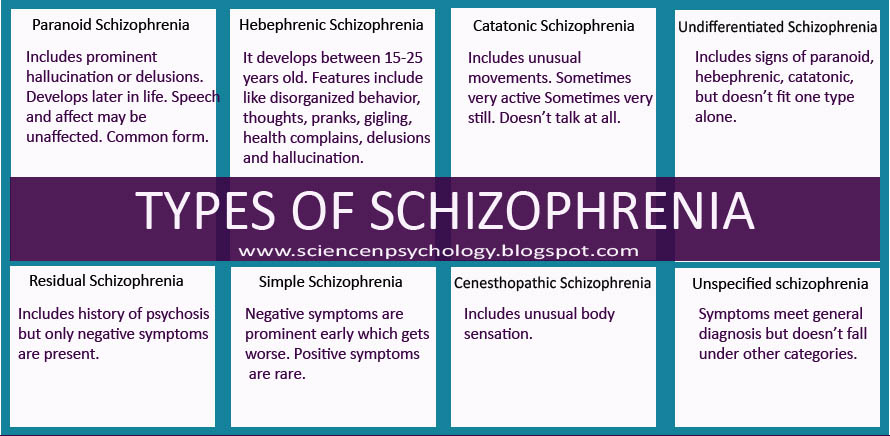
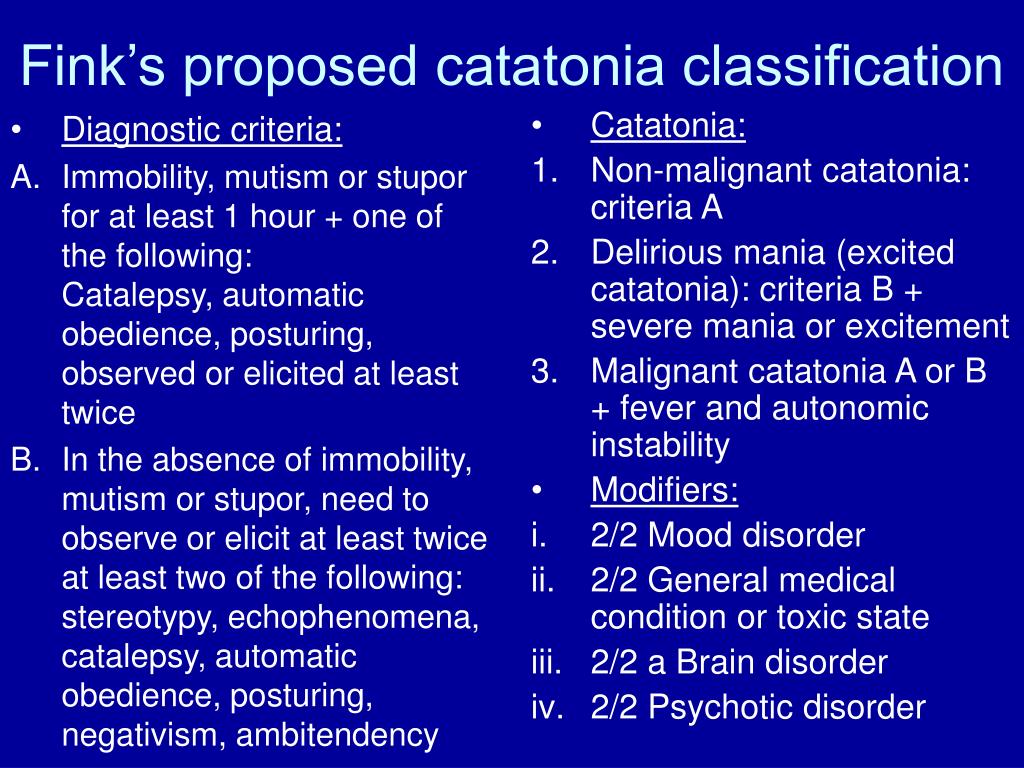
Researchers have studied catatonia since German psychiatrist Karl Kahlbaum named and described it in 1874, but it remains highly underdiagnosed. Part of this is because, until recent decades, catatonia was mistakenly believed to only occur in people with schizophrenia. Further challenges to diagnosis include disagreement within psychiatry on how many criteria and which criteria are required to diagnose catatonia. In addition, some catatonic signs, such as agitation and mutism, overlap with other conditions.
Who does catatonia affect?
Catatonia doesn’t affect any population differently based on race, sex, etc. It’s most common with the following kinds of conditions (more about these conditions is under the Causes and Symptoms section):
- Psychiatric conditions, which specifically affect your mental health.
- Neurological conditions, which specifically affect how your brain works.
- Medical conditions, which affect how one or more systems in your body function.
How common is this condition?
According to available research, catatonia happens in 0.5% to 2.1% of people receiving psychiatric care. That number climbs to around 10% for people who need inpatient mental health treatment.
How does this condition affect my body?
Catatonia disrupts how certain parts of your brain work, causing a person to go into a “catatonic state.” The areas of your brain that are affected are those that control or manage:
- Movement.
- Senses (vision, hearing, smell, touch and taste).
- Memory.
- Thinking and concentration (cognitive) abilities.
- Motivation.
- Emotions.
- Judgment and self-control (executive functions).
Because catatonia can disrupt many different brain areas, it can have many symptoms. That’s one of the reasons that it can happen with so many conditions and why it’s challenging for experts to diagnose.
Symptoms and Causes
What are the symptoms of catatonia?
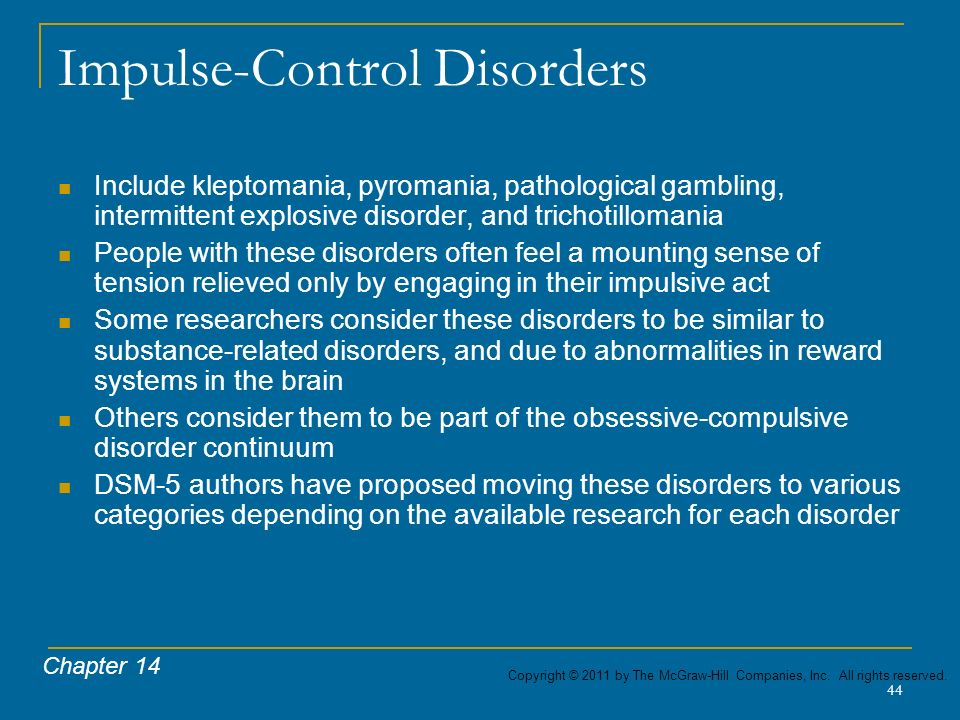
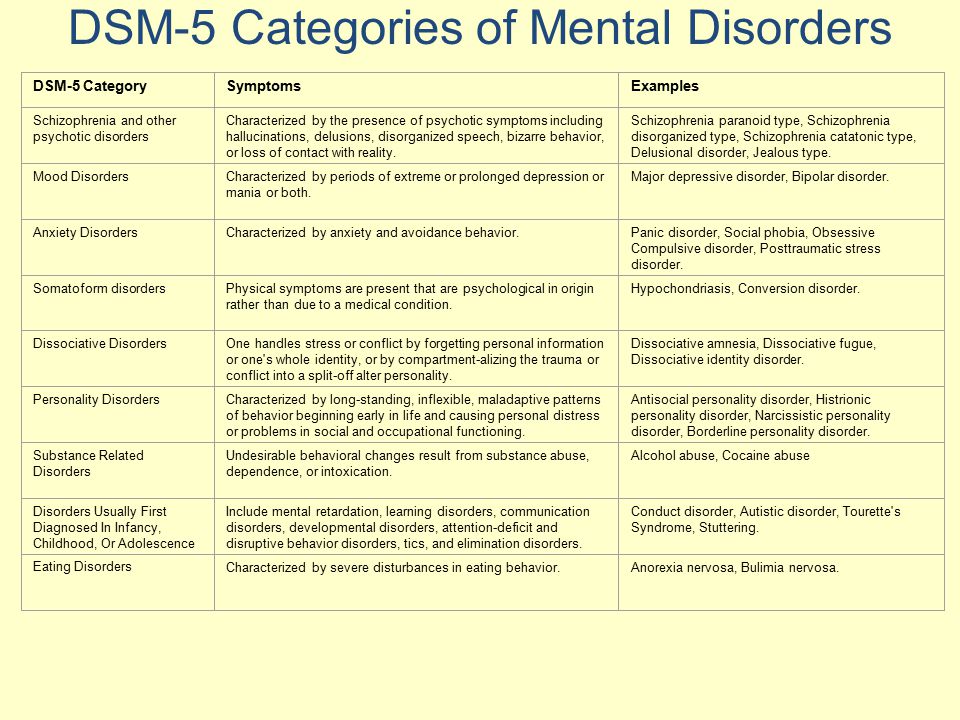
There are 12 officially accepted symptoms of catatonia, according to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Those are:
- Agitation. This means a person acts upset or irritable. It only counts as a symptom of catatonia if it happens and it isn’t a response to something around the person having it.
- Catalepsy (pronounced “cat-ah-lep-see”). This is when a person holds a position in which someone places them (you can still move them around to make them take on a new pose).
- Echolalia (pronounced “eck-oh-la-lee-ah”). This is when a person echoes sounds that someone else makes.
- Echopraxia (pronounced “eck-oh-prax-ee-ah”). This is when a person mimics or mirrors someone else’s movements.
- Grimacing. This is holding the same facial expression, usually with stiff or tense facial muscles. Sometimes, it can take the form of smiling in inappropriate contexts.
- Mannerism. This is when a person acts out motions or movements that could be normal but does them in an unusual or exaggerated way.
- Mutism (pronounced “mew-tizm”). This is when a person is either very or totally quiet (this is only a symptom if the person doesn’t have another condition, such as aphasia, to explain why they aren’t speaking).
- Negativism (pronounced “neg-uh-tiv-ism”). This means a person doesn’t react to something happening around them or actively resists what’s happening around them for no rational reason.

- Posturing. This is when a person holds a specific position, which would often be uncomfortable to people who aren’t catatonic. In contrast to catalepsy, this doesn’t involve being placed in the position by another person.
- Stereotypy (pronounced “stair-ee-oh-type-ee”). These are repetitive movements that don’t seem to have a purpose. They can include finger-play and patting/rubbing one’s body.
- Stupor (pronounced “stoop-er”). This is when a person is awake but doesn’t respond to what’s happening around them. People with catatonia often don’t respond to painful stimuli, such as being pinched.
- Waxy flexibility. This is when a person puts up some slight even push-back or resistance to any attempt to change their position. Then their muscles slowly release and their limbs bend like a warm candle.
Catatonia activity levels
While most people think of catatonia as a disorder that involves moving very little or not at all, that’s not always the case.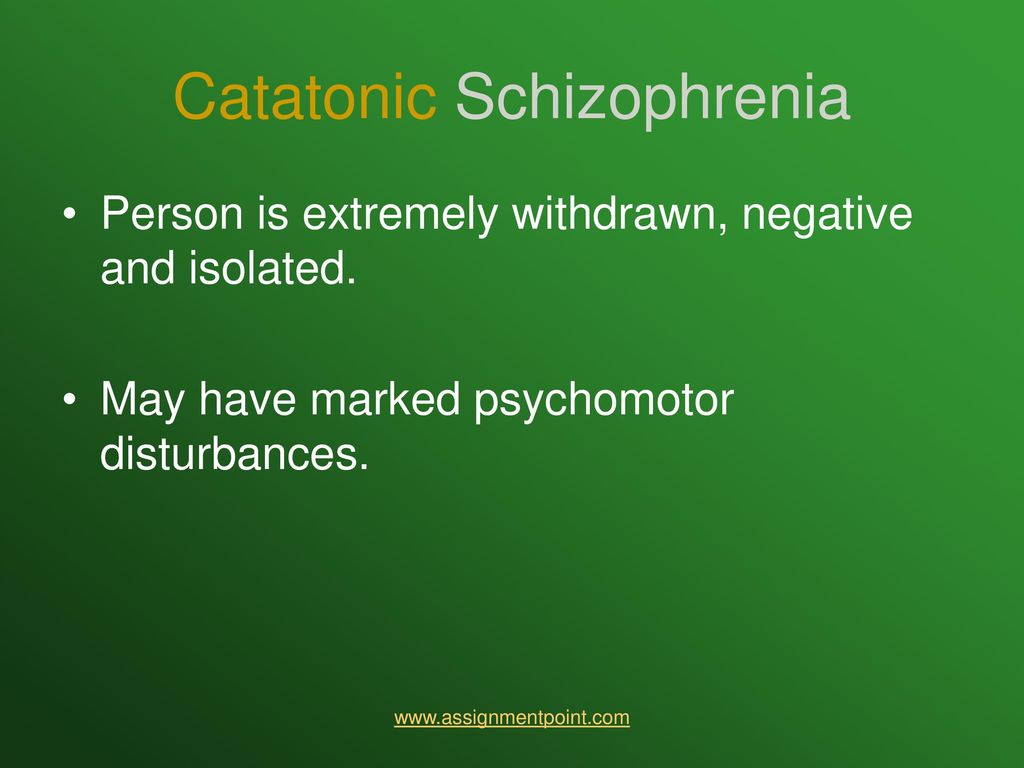 Catatonia can also involve sudden and unpredictable behavior changes, including excessive or even constant movement. The activity levels of catatonia are as follows:
Catatonia can also involve sudden and unpredictable behavior changes, including excessive or even constant movement. The activity levels of catatonia are as follows:
- Excited/hyperkinetic. This form usually involves behavior changes, such as pacing, agitation, aggression and violent behavior without any situations causing the behavior change. It can also include acting or speaking strangely, mimicking how others nearby move or talk or even acts of self-harm.
- Withdrawn/hypokinetic. This form of catatonia is often what people think of when they talk or think about this disorder. People with this form are awake but don’t react to what’s happening around them, as if they just aren’t aware of their surroundings. They’re usually silent and have little or no facial expressions. They also might hold themselves in an unusual posture or position and may even resist attempts to move them. They often don’t eat or drink and may have incontinence.
- Mixed. This form combines features of hyperkinetic and hypokinetic catatonia. A person with catatonia can quickly switch between hyperkinetic and hypokinetic behaviors without warning.
Malignant catatonia
In some cases, catatonia can have deadly complications. When this happens, it’s known as malignant catatonia. This condition causes dysautonomia, which is when your autonomic nervous system doesn’t work as it should. Your autonomic nervous system is what controls the automatic body processes you don’t need to think about, such as heartbeat, blood pressure, etc.
The symptoms of malignant catatonia are:
- Dangerously high body temperature and fever (hyperthermia).
- Fast heart rate (tachycardia).
- Sweating (diaphoresis).
- Unstable blood pressure.
- Cyanosis (this is low blood oxygen that causes areas of your skin, especially around your lips and fingernails, to turn blue).
Because malignant catatonia disrupts how your brain runs your body’s automatic processes, it has the potential to cause death. That means it’s a problem that needs immediate medical care.
That means it’s a problem that needs immediate medical care.
What causes catatonia?
Despite almost 150 years of study, experts still don’t know exactly why catatonia happens. However, there are several possible explanations, ranging from chemical imbalances in the brain to genetic causes passed from generation to generation.
Without a specific cause, experts can only point to other conditions that may involve catatonia. The mental health conditions that most commonly involve catatonia are:
- Bipolar disorder.
- Schizophrenia.
- Schizoaffective disorder.
- Major depressive disorder.
The neurological and medical conditions that most commonly involve catatonia are:
- Autism spectrum disorder.
- Autoimmune diseases (such as lupus or multiple sclerosis).
- Degenerative brain diseases (such as dementia and Parkinson’s disease).
- Down syndrome.
- Drug-related conditions (this includes prescription and recreational drugs).
- Encephalitis, including anti-NMDA receptor encephalitis.
- Electrolyte imbalance conditions.
- Epilepsy.
- Intellectual disability.
- Normal-pressure hydrocephalus.
- Stroke.
- Tourette syndrome.
Is it contagious?
Catatonia isn’t contagious, and you can’t spread it to or catch it from others.
Diagnosis and Tests
How is catatonia diagnosed?
Your healthcare provider will diagnose catatonia using a combination of methods. This usually starts with a neurological examination. During that exam, your provider will test your reflexes, reactions and how they respond (or don’t respond) to the world around you.
Your provider will then use a standardized assessment tool, usually the Bush Francis Catatonia Rating Scale, to rate the presence or absence of catatonia and the degree of severity. Once catatonia is identified, healthcare providers must then identify the cause of catatonia, as catatonia is always associated with another psychiatric or medical condition.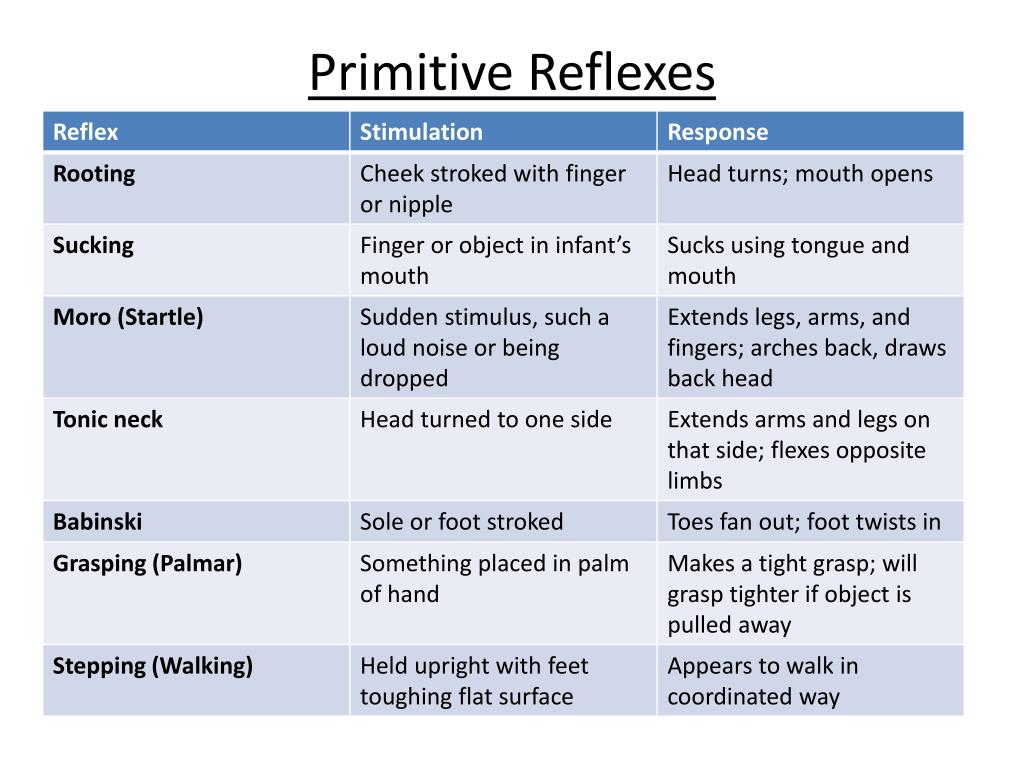 As catatonia can occur alongside serious or even deadly conditions, ruling out more severe underlying conditions is a priority.
As catatonia can occur alongside serious or even deadly conditions, ruling out more severe underlying conditions is a priority.
What tests will be done to diagnose this condition?
Diagnosing catatonia and identifying the underlying condition usually involves lab, diagnostic and imaging tests.
- Imaging tests. These can include computerized tomography (CT) scans, magnetic resonance imaging (MRI) scans and other imaging tests.
- Blood, urine and cerebrospinal fluid (spinal tap) tests. These tests look for chemical changes in bodily fluids, infections and more.
- Brain activity testing. An electroencephalogram (EEG) analyzes and records the electrical activity in your brain, which can rule out seizures or epilepsy.
Management and Treatment
How is catatonia treated, and is there a cure?
The treatment for catatonia usually depends on the condition(s) with which it happens. If it happens with a medical or a neurological condition, treating that condition — if possible— will often reverse the effects of catatonia. Other treatment approaches have the best chances of success when it happens along with mental health conditions.
If it happens with a medical or a neurological condition, treating that condition — if possible— will often reverse the effects of catatonia. Other treatment approaches have the best chances of success when it happens along with mental health conditions.
What medications or treatments are used?
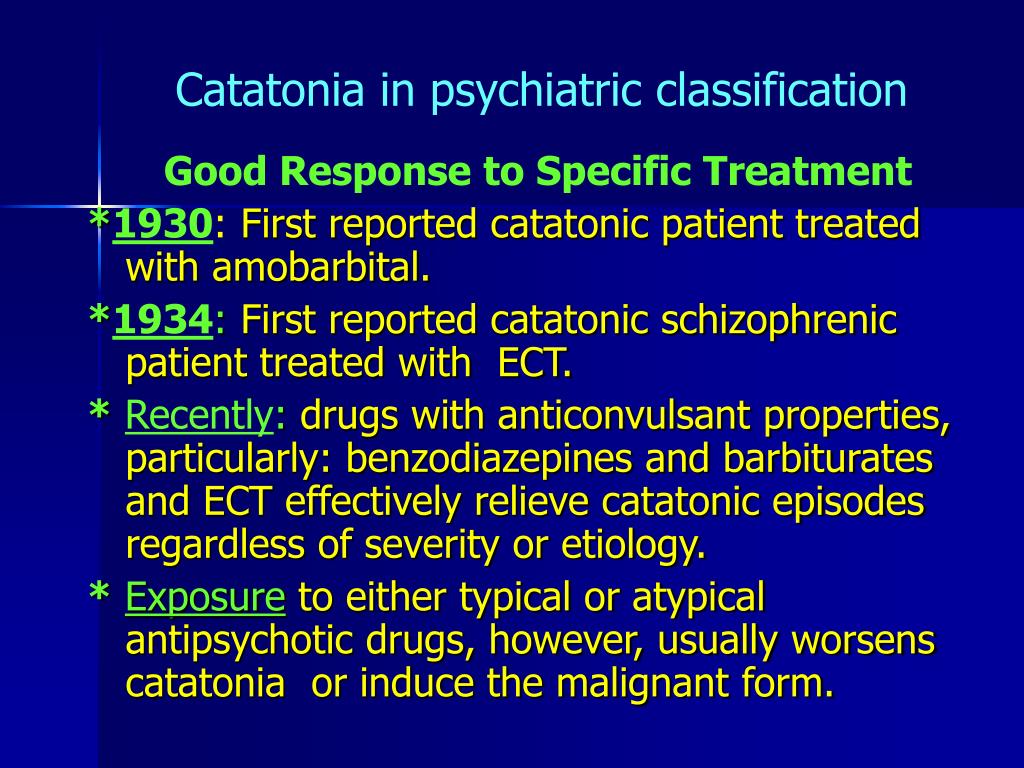
There are two main ways to treat catatonia: medications and electroconvulsive therapy. There are other possible treatments like transcranial magnetic stimulation, but more research is necessary to understand if these are effective enough for widespread use.
Medications
Benzodiazepines are the primary medication for treating catatonia because they’re safe and very effective. Between 60% and 90% of people with catatonia will improve if treated with benzodiazepines. Lorazepam is the medication of choice, but others like clonazepam, diazepam and zolpidem are also effective. Healthcare providers can give these medications as an infusion through intravenous (IV) lines, an injection or in pill form depending on the particular medication.
Other medications (such as mood stabilizers or antipsychotic drugs) may also help but usually aren’t first-line treatments. These are most helpful for treating other symptoms after the initial catatonia symptoms improve, especially because antipsychotic medications can cause catatonia to become malignant catatonia or neuroleptic malignant syndrome.
Electroconvulsive therapy
Electroconvulsive therapy (ECT) is a treatment that involves running a very mild electrical current through an area of your brain to cause a short seizure. People who undergo ECT do so under general anesthesia, which means they’re in a deep sleep so they don’t feel pain from this treatment.
ECT is also very effective, helping nearly all people with catatonia who receive it. It’s the main treatment for people who have malignant catatonia and is often a life-saving treatment in those cases. It’s also helpful for people whose catatonia isn’t responding to medications.
Complications/side effects of the treatment
The possible complications and side effects of treatments for catatonia can vary depending on which treatment — or combination of treatments — a person receives. A healthcare provider is the best person to explain the side effects or complications that are possible or likely.
A healthcare provider is the best person to explain the side effects or complications that are possible or likely.
How do I take care of myself or manage symptoms?
Catatonia is a difficult condition to diagnose even for trained, experienced healthcare providers. It also can happen because of life-threatening conditions that need immediate medical care. Because of both those factors, you shouldn’t try to self-diagnose or treat it.
How soon after treatment will I feel better, and how long does it take to recover?
With conditions like catatonia, every case is different. Your healthcare provider is the best source of information on the timeline for recovery. That’s because they can consider all the factors that affect a specific case, including the related conditions, a person’s medical history and more.
Benzodiazepines are usually effective quickly. When given intravenously, many people start to improve within 10 to 15 minutes. When a person can take medications by mouth in pills, it can take as little as 20 to 30 minutes for medications to work.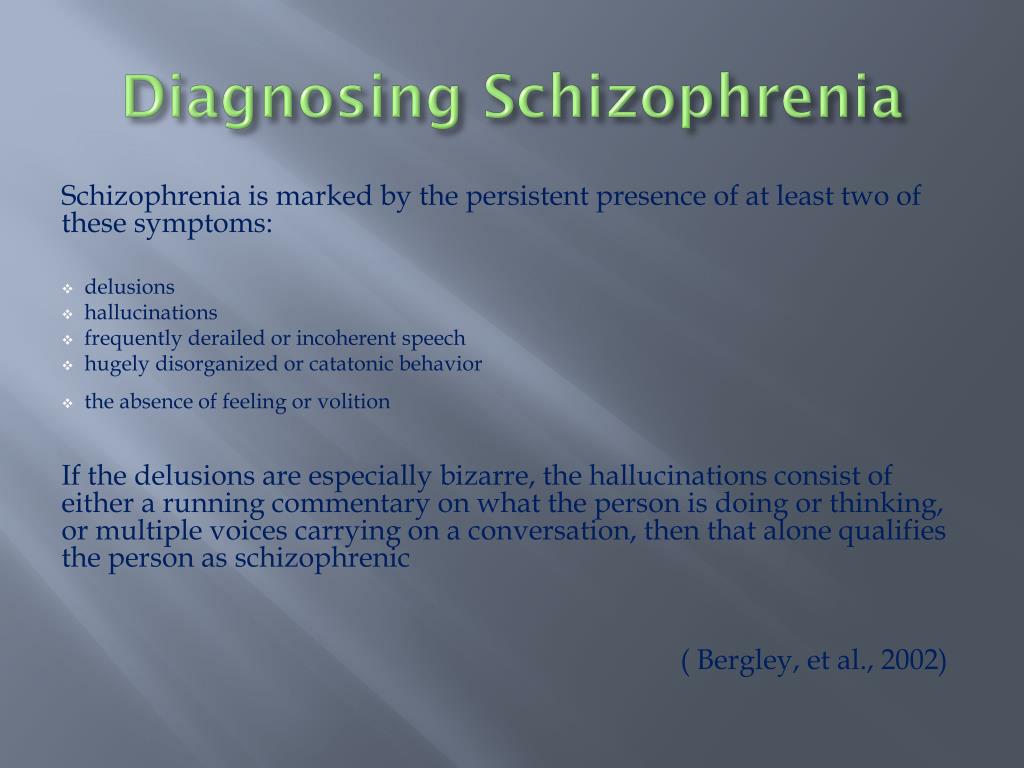 However, it can take time to find the right dose, so some people may need several days of treatment before their catatonia improves.
However, it can take time to find the right dose, so some people may need several days of treatment before their catatonia improves.
ECT can also be effective quickly. Some people can start to show some improvement within minutes or hours of treatment, while others may need multiple treatments before responding. Most people will receive ECT a few times a week for a few weeks, but some may need daily treatments until symptoms improve.
Prevention
How can I reduce my risk or prevent this?
Catatonia happens unpredictably and for reasons that experts still don’t fully understand, so it isn’t possible to prevent it or reduce your risk of it happening.
If you have a mental health condition for which you’re prescribed medication, your risk of catatonia may increase if you stop taking your medications.
Outlook / Prognosis
What can I expect if I have this condition?
Most people who have catatonia are at least somewhat aware of the world around them. They simply can’t react to what’s happening around them as they would normally. It’s also common for people with catatonia to remember some of what happened to them even though they seemed unaware.
They simply can’t react to what’s happening around them as they would normally. It’s also common for people with catatonia to remember some of what happened to them even though they seemed unaware.
Because of how catatonia affects a person’s awareness of the world around them, it’s common that people who have it can’t speak for themselves or make decisions about their medical care. In those cases, healthcare providers will usually talk to a family member or loved one and ask them to make choices about care.
How long does catatonia last?
How long catatonia lasts depends partly on the conditions that it happens along with and the treatments received. Timely treatment is important because the longer that catatonia lasts, the less likely it’ll respond to treatment. Your healthcare provider is the best person to explain how long catatonia will last and what to expect.
What’s the outlook for this condition?
Catatonia usually isn’t life-threatening by itself (except for malignant catatonia, which is deadly without quick treatment).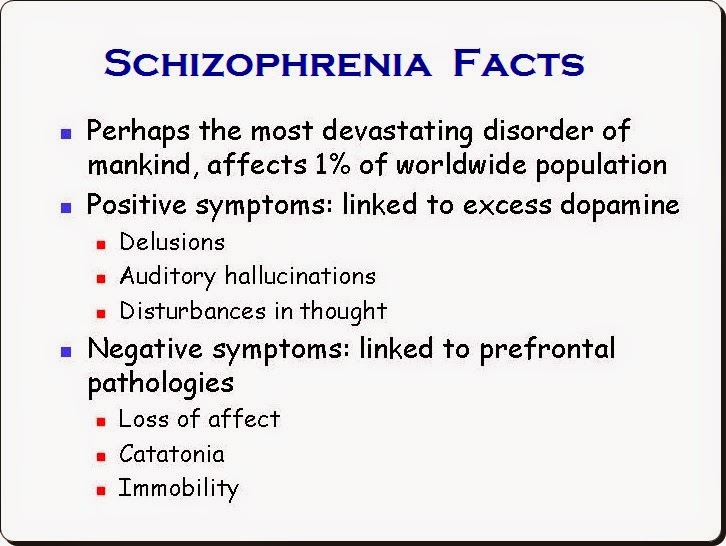 However, it’s associated with an increased risk of death from conditions that happen from not moving much, such as pulmonary embolism and pneumonia. Catatonia is also harder to treat when it lasts longer or when a person has it more than once. Fortunately, benzodiazepines and ECT have very high success rates for this condition, which means it’s very treatable.
However, it’s associated with an increased risk of death from conditions that happen from not moving much, such as pulmonary embolism and pneumonia. Catatonia is also harder to treat when it lasts longer or when a person has it more than once. Fortunately, benzodiazepines and ECT have very high success rates for this condition, which means it’s very treatable.
People with mood disorders, such as bipolar disorder and major depressive disorder, tend to respond better to treatment than people with schizophrenia. However, this can still vary, and no two cases are alike. Your healthcare provider is the best person to explain the outlook for this condition because they can provide information that’s most relevant and accurate for your situation.
Living With
How do I take care of myself?
People with severe catatonia can’t take care of themselves and need care from trained medical professionals. That’s because catatonia increases the risk of complications that happen when a person can’t move or react to the world around them.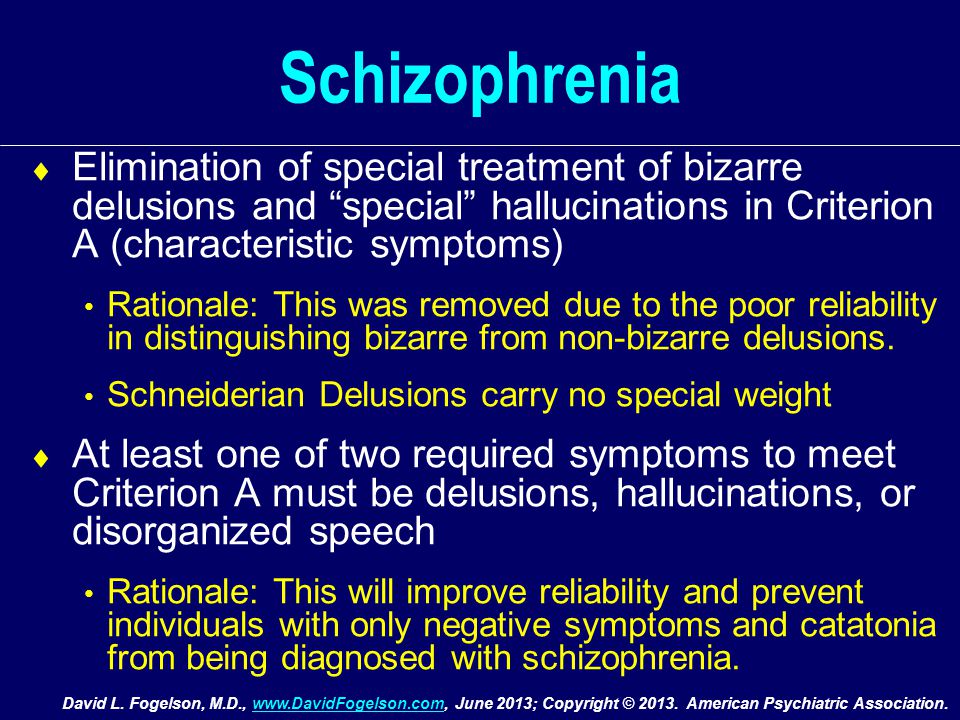 That means they can’t eat or drink, leading to problems like dehydration and malnutrition. Lack of movement can also lead to pneumonia. They can also have blood clots, which puts them at risk of a stroke or a pulmonary embolism. They’re also at risk for behavior that may cause them to harm themselves or others.
That means they can’t eat or drink, leading to problems like dehydration and malnutrition. Lack of movement can also lead to pneumonia. They can also have blood clots, which puts them at risk of a stroke or a pulmonary embolism. They’re also at risk for behavior that may cause them to harm themselves or others.
When should I see my healthcare provider, or when should I seek care?
People who show signs of catatonia need medical attention as soon as possible. That’s because the symptoms of this condition are also possible with dangerous conditions that are emergencies and need immediate care. If a loved one shows signs of catatonia, you may need to take them to the hospital or even call 911 (or your local emergency services number).
When should I go to the ER?
People who have catatonia, especially with conditions like schizophrenia, have an increased risk of self-harm and suicide. You should go to the ER or call 911 (or your local emergency services number) if you have thoughts about harming yourself, including thoughts of suicide, or about harming others.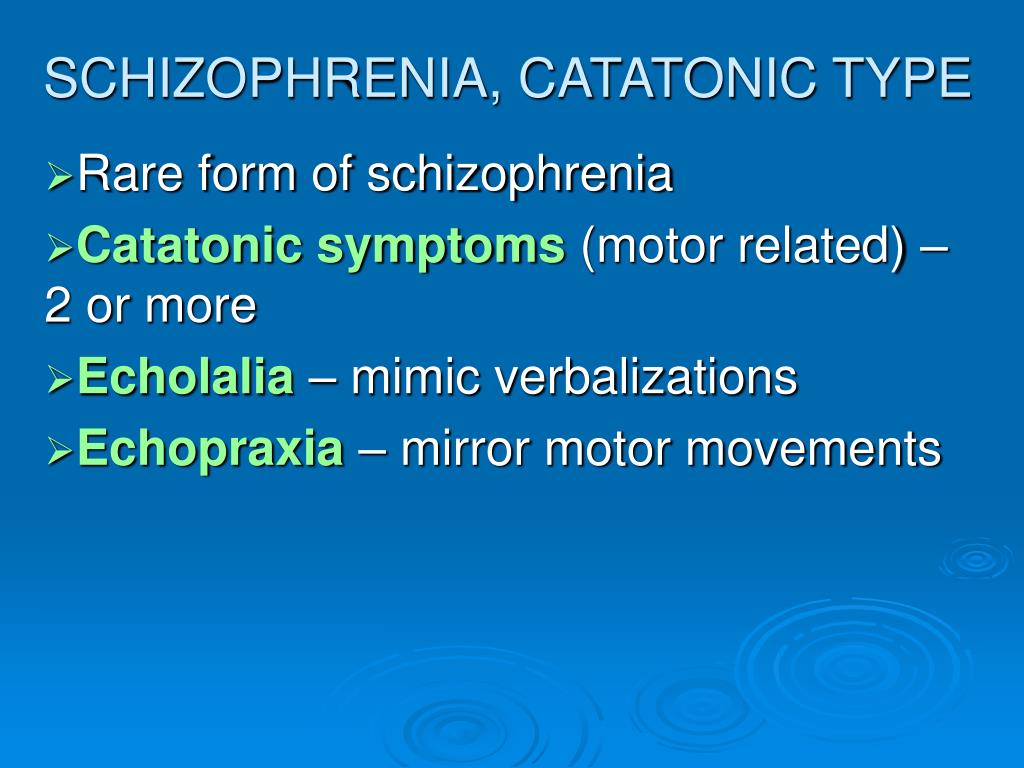 If you have thoughts like this, you can call any of the following:
If you have thoughts like this, you can call any of the following:
- National Suicide Prevention Lifeline (United States). To call this line, dial 988.
- Local crisis lines. Mental health organizations and centers in your area may offer resources and help through crisis lines.
- 911 (or your local emergency services number): You should call 911 (or the local emergency services number) if you feel like you’re in immediate danger of harming yourself. Operators and dispatchers for 911 lines can often help people in immediate danger because of a severe mental crisis and send first responders to assist.
A note from Cleveland Clinic
Catatonia is a disorder that can disrupt how a person’s brain works, affecting how they respond to the world around them. People with catatonia sometimes respond very little or not at all to what’s happening around them. Others may behave in ways that are unpredictable or dangerous to themselves or others. Catatonia can happen with many conditions, ranging from mental health disorders to medical conditions. It’s usually not acutely life-threatening, though there’s potential for serious complications and progression to malignant catatonia, which is a life-threatening emergency.
Catatonia can happen with many conditions, ranging from mental health disorders to medical conditions. It’s usually not acutely life-threatening, though there’s potential for serious complications and progression to malignant catatonia, which is a life-threatening emergency.
People with this disorder also often can’t care for themselves, which means they need medical care from trained healthcare personnel. Fortunately, catatonia is very treatable, and most people respond to medication. Those who don’t respond to medication usually respond to electroconvulsive therapy. With timely, effective treatment, the effects of catatonia are often reversible, offering the chance for the treatment of or recovery from underlying conditions associated with catatonia.
Definition, Causes, Symptoms & Treatment
Overview
What is catatonia?
Catatonia is a disorder that disrupts how your brain works, disrupting how a person processes and reacts to the world around them. People with catatonia often don’t react to things happening nearby or may react in ways that seem unusual. Impaired communication, unusual movements or lack of movement, and behavior abnormalities are the most striking features of this condition.
People with catatonia often don’t react to things happening nearby or may react in ways that seem unusual. Impaired communication, unusual movements or lack of movement, and behavior abnormalities are the most striking features of this condition.
Researchers have studied catatonia since German psychiatrist Karl Kahlbaum named and described it in 1874, but it remains highly underdiagnosed. Part of this is because, until recent decades, catatonia was mistakenly believed to only occur in people with schizophrenia. Further challenges to diagnosis include disagreement within psychiatry on how many criteria and which criteria are required to diagnose catatonia. In addition, some catatonic signs, such as agitation and mutism, overlap with other conditions.
Who does catatonia affect?
Catatonia doesn’t affect any population differently based on race, sex, etc. It’s most common with the following kinds of conditions (more about these conditions is under the Causes and Symptoms section):
- Psychiatric conditions, which specifically affect your mental health.

- Neurological conditions, which specifically affect how your brain works.
- Medical conditions, which affect how one or more systems in your body function.
How common is this condition?
According to available research, catatonia happens in 0.5% to 2.1% of people receiving psychiatric care. That number climbs to around 10% for people who need inpatient mental health treatment.
How does this condition affect my body?
Catatonia disrupts how certain parts of your brain work, causing a person to go into a “catatonic state.” The areas of your brain that are affected are those that control or manage:
- Movement.
- Senses (vision, hearing, smell, touch and taste).
- Memory.
- Thinking and concentration (cognitive) abilities.
- Motivation.
- Emotions.
- Judgment and self-control (executive functions).
Because catatonia can disrupt many different brain areas, it can have many symptoms.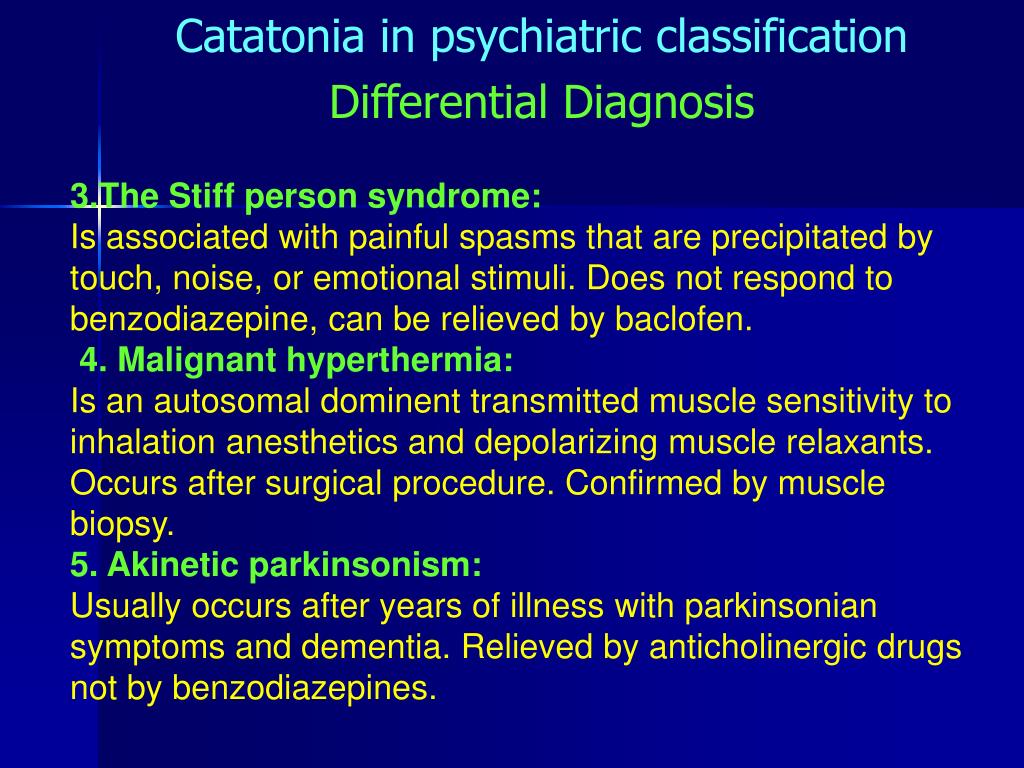 That’s one of the reasons that it can happen with so many conditions and why it’s challenging for experts to diagnose.
That’s one of the reasons that it can happen with so many conditions and why it’s challenging for experts to diagnose.
Symptoms and Causes
What are the symptoms of catatonia?
There are 12 officially accepted symptoms of catatonia, according to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Those are:
- Agitation. This means a person acts upset or irritable. It only counts as a symptom of catatonia if it happens and it isn’t a response to something around the person having it.
- Catalepsy (pronounced “cat-ah-lep-see”). This is when a person holds a position in which someone places them (you can still move them around to make them take on a new pose).
- Echolalia (pronounced “eck-oh-la-lee-ah”). This is when a person echoes sounds that someone else makes.
- Echopraxia (pronounced “eck-oh-prax-ee-ah”).
 This is when a person mimics or mirrors someone else’s movements.
This is when a person mimics or mirrors someone else’s movements. - Grimacing. This is holding the same facial expression, usually with stiff or tense facial muscles. Sometimes, it can take the form of smiling in inappropriate contexts.
- Mannerism. This is when a person acts out motions or movements that could be normal but does them in an unusual or exaggerated way.
- Mutism (pronounced “mew-tizm”). This is when a person is either very or totally quiet (this is only a symptom if the person doesn’t have another condition, such as aphasia, to explain why they aren’t speaking).
- Negativism (pronounced “neg-uh-tiv-ism”). This means a person doesn’t react to something happening around them or actively resists what’s happening around them for no rational reason.
- Posturing. This is when a person holds a specific position, which would often be uncomfortable to people who aren’t catatonic.
 In contrast to catalepsy, this doesn’t involve being placed in the position by another person.
In contrast to catalepsy, this doesn’t involve being placed in the position by another person. - Stereotypy (pronounced “stair-ee-oh-type-ee”). These are repetitive movements that don’t seem to have a purpose. They can include finger-play and patting/rubbing one’s body.
- Stupor (pronounced “stoop-er”). This is when a person is awake but doesn’t respond to what’s happening around them. People with catatonia often don’t respond to painful stimuli, such as being pinched.
- Waxy flexibility. This is when a person puts up some slight even push-back or resistance to any attempt to change their position. Then their muscles slowly release and their limbs bend like a warm candle.
Catatonia activity levels
While most people think of catatonia as a disorder that involves moving very little or not at all, that’s not always the case. Catatonia can also involve sudden and unpredictable behavior changes, including excessive or even constant movement. The activity levels of catatonia are as follows:
The activity levels of catatonia are as follows:
- Excited/hyperkinetic. This form usually involves behavior changes, such as pacing, agitation, aggression and violent behavior without any situations causing the behavior change. It can also include acting or speaking strangely, mimicking how others nearby move or talk or even acts of self-harm.
- Withdrawn/hypokinetic. This form of catatonia is often what people think of when they talk or think about this disorder. People with this form are awake but don’t react to what’s happening around them, as if they just aren’t aware of their surroundings. They’re usually silent and have little or no facial expressions. They also might hold themselves in an unusual posture or position and may even resist attempts to move them. They often don’t eat or drink and may have incontinence.
- Mixed. This form combines features of hyperkinetic and hypokinetic catatonia. A person with catatonia can quickly switch between hyperkinetic and hypokinetic behaviors without warning.
Malignant catatonia
In some cases, catatonia can have deadly complications. When this happens, it’s known as malignant catatonia. This condition causes dysautonomia, which is when your autonomic nervous system doesn’t work as it should. Your autonomic nervous system is what controls the automatic body processes you don’t need to think about, such as heartbeat, blood pressure, etc.
The symptoms of malignant catatonia are:
- Dangerously high body temperature and fever (hyperthermia).
- Fast heart rate (tachycardia).
- Sweating (diaphoresis).
- Unstable blood pressure.
- Cyanosis (this is low blood oxygen that causes areas of your skin, especially around your lips and fingernails, to turn blue).
Because malignant catatonia disrupts how your brain runs your body’s automatic processes, it has the potential to cause death. That means it’s a problem that needs immediate medical care.
What causes catatonia?
Despite almost 150 years of study, experts still don’t know exactly why catatonia happens.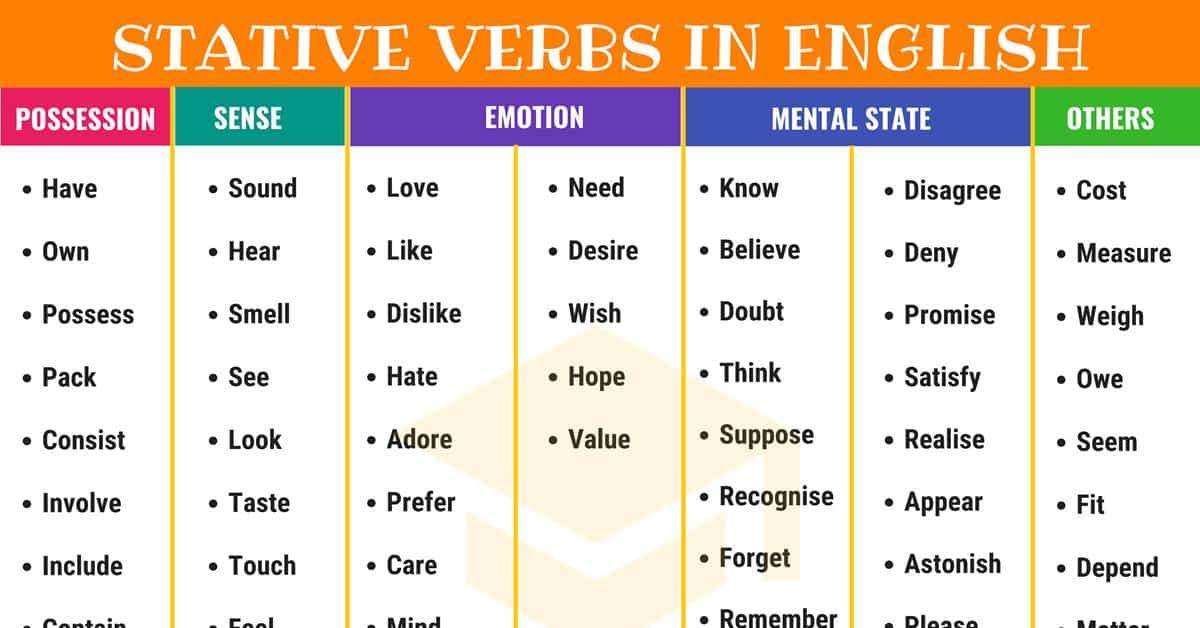 However, there are several possible explanations, ranging from chemical imbalances in the brain to genetic causes passed from generation to generation.
However, there are several possible explanations, ranging from chemical imbalances in the brain to genetic causes passed from generation to generation.
Without a specific cause, experts can only point to other conditions that may involve catatonia. The mental health conditions that most commonly involve catatonia are:
- Bipolar disorder.
- Schizophrenia.
- Schizoaffective disorder.
- Major depressive disorder.
The neurological and medical conditions that most commonly involve catatonia are:
- Autism spectrum disorder.
- Autoimmune diseases (such as lupus or multiple sclerosis).
- Degenerative brain diseases (such as dementia and Parkinson’s disease).
- Down syndrome.
- Drug-related conditions (this includes prescription and recreational drugs).
- Encephalitis, including anti-NMDA receptor encephalitis.
- Electrolyte imbalance conditions.
- Epilepsy.
- Intellectual disability.
- Normal-pressure hydrocephalus.
- Stroke.
- Tourette syndrome.
Is it contagious?
Catatonia isn’t contagious, and you can’t spread it to or catch it from others.
Diagnosis and Tests
How is catatonia diagnosed?
Your healthcare provider will diagnose catatonia using a combination of methods. This usually starts with a neurological examination. During that exam, your provider will test your reflexes, reactions and how they respond (or don’t respond) to the world around you.
Your provider will then use a standardized assessment tool, usually the Bush Francis Catatonia Rating Scale, to rate the presence or absence of catatonia and the degree of severity. Once catatonia is identified, healthcare providers must then identify the cause of catatonia, as catatonia is always associated with another psychiatric or medical condition. As catatonia can occur alongside serious or even deadly conditions, ruling out more severe underlying conditions is a priority.
What tests will be done to diagnose this condition?
Diagnosing catatonia and identifying the underlying condition usually involves lab, diagnostic and imaging tests.
- Imaging tests. These can include computerized tomography (CT) scans, magnetic resonance imaging (MRI) scans and other imaging tests.
- Blood, urine and cerebrospinal fluid (spinal tap) tests. These tests look for chemical changes in bodily fluids, infections and more.
- Brain activity testing. An electroencephalogram (EEG) analyzes and records the electrical activity in your brain, which can rule out seizures or epilepsy.
Management and Treatment
How is catatonia treated, and is there a cure?
The treatment for catatonia usually depends on the condition(s) with which it happens. If it happens with a medical or a neurological condition, treating that condition — if possible— will often reverse the effects of catatonia.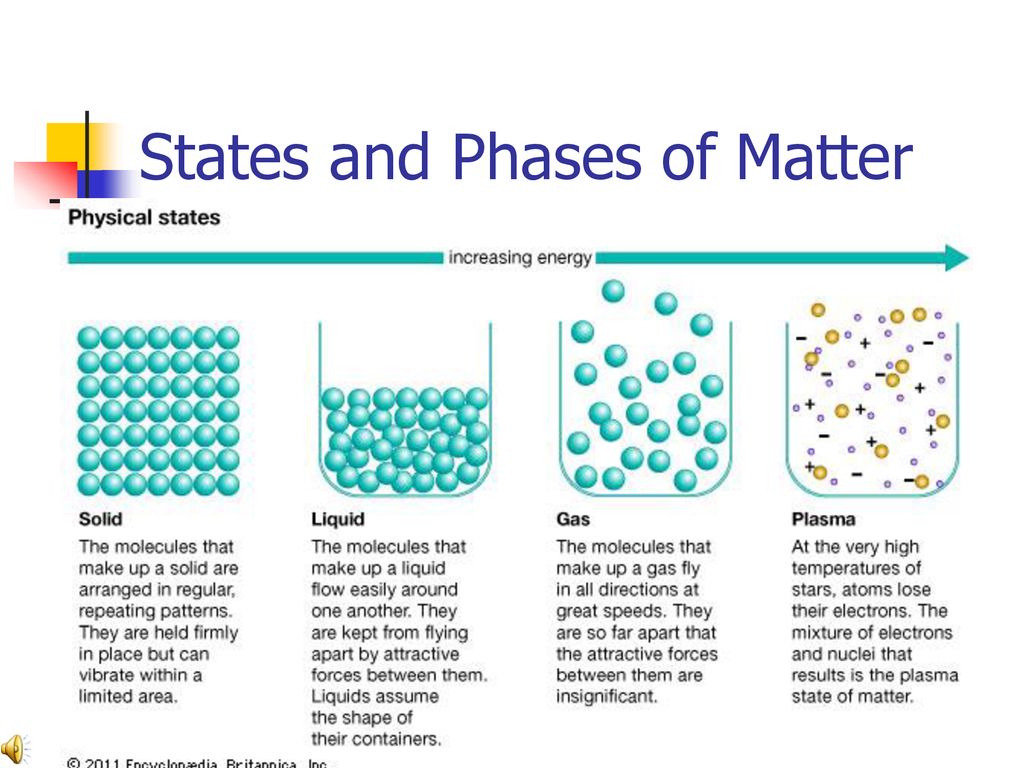 Other treatment approaches have the best chances of success when it happens along with mental health conditions.
Other treatment approaches have the best chances of success when it happens along with mental health conditions.
What medications or treatments are used?
There are two main ways to treat catatonia: medications and electroconvulsive therapy. There are other possible treatments like transcranial magnetic stimulation, but more research is necessary to understand if these are effective enough for widespread use.
Medications
Benzodiazepines are the primary medication for treating catatonia because they’re safe and very effective. Between 60% and 90% of people with catatonia will improve if treated with benzodiazepines. Lorazepam is the medication of choice, but others like clonazepam, diazepam and zolpidem are also effective. Healthcare providers can give these medications as an infusion through intravenous (IV) lines, an injection or in pill form depending on the particular medication.
Other medications (such as mood stabilizers or antipsychotic drugs) may also help but usually aren’t first-line treatments.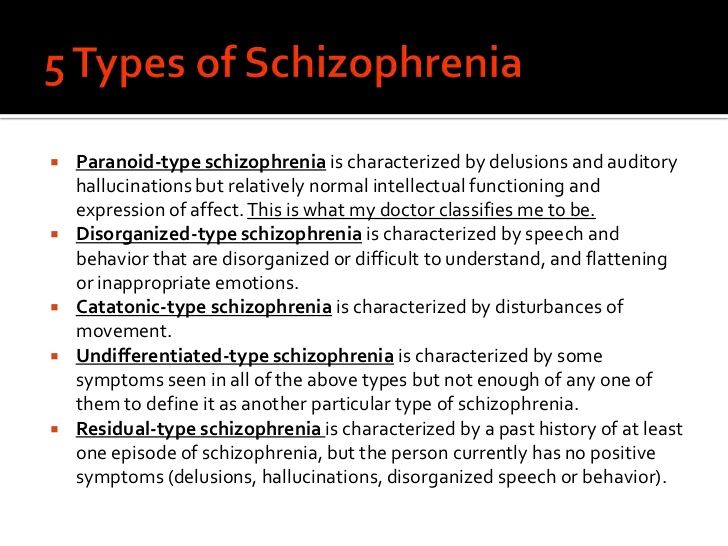 These are most helpful for treating other symptoms after the initial catatonia symptoms improve, especially because antipsychotic medications can cause catatonia to become malignant catatonia or neuroleptic malignant syndrome.
These are most helpful for treating other symptoms after the initial catatonia symptoms improve, especially because antipsychotic medications can cause catatonia to become malignant catatonia or neuroleptic malignant syndrome.
Electroconvulsive therapy
Electroconvulsive therapy (ECT) is a treatment that involves running a very mild electrical current through an area of your brain to cause a short seizure. People who undergo ECT do so under general anesthesia, which means they’re in a deep sleep so they don’t feel pain from this treatment.
ECT is also very effective, helping nearly all people with catatonia who receive it. It’s the main treatment for people who have malignant catatonia and is often a life-saving treatment in those cases. It’s also helpful for people whose catatonia isn’t responding to medications.
Complications/side effects of the treatment
The possible complications and side effects of treatments for catatonia can vary depending on which treatment — or combination of treatments — a person receives. A healthcare provider is the best person to explain the side effects or complications that are possible or likely.
A healthcare provider is the best person to explain the side effects or complications that are possible or likely.
How do I take care of myself or manage symptoms?
Catatonia is a difficult condition to diagnose even for trained, experienced healthcare providers. It also can happen because of life-threatening conditions that need immediate medical care. Because of both those factors, you shouldn’t try to self-diagnose or treat it.
How soon after treatment will I feel better, and how long does it take to recover?
With conditions like catatonia, every case is different. Your healthcare provider is the best source of information on the timeline for recovery. That’s because they can consider all the factors that affect a specific case, including the related conditions, a person’s medical history and more.
Benzodiazepines are usually effective quickly. When given intravenously, many people start to improve within 10 to 15 minutes. When a person can take medications by mouth in pills, it can take as little as 20 to 30 minutes for medications to work. However, it can take time to find the right dose, so some people may need several days of treatment before their catatonia improves.
However, it can take time to find the right dose, so some people may need several days of treatment before their catatonia improves.
ECT can also be effective quickly. Some people can start to show some improvement within minutes or hours of treatment, while others may need multiple treatments before responding. Most people will receive ECT a few times a week for a few weeks, but some may need daily treatments until symptoms improve.
Prevention
How can I reduce my risk or prevent this?
Catatonia happens unpredictably and for reasons that experts still don’t fully understand, so it isn’t possible to prevent it or reduce your risk of it happening.
If you have a mental health condition for which you’re prescribed medication, your risk of catatonia may increase if you stop taking your medications.
Outlook / Prognosis
What can I expect if I have this condition?
Most people who have catatonia are at least somewhat aware of the world around them.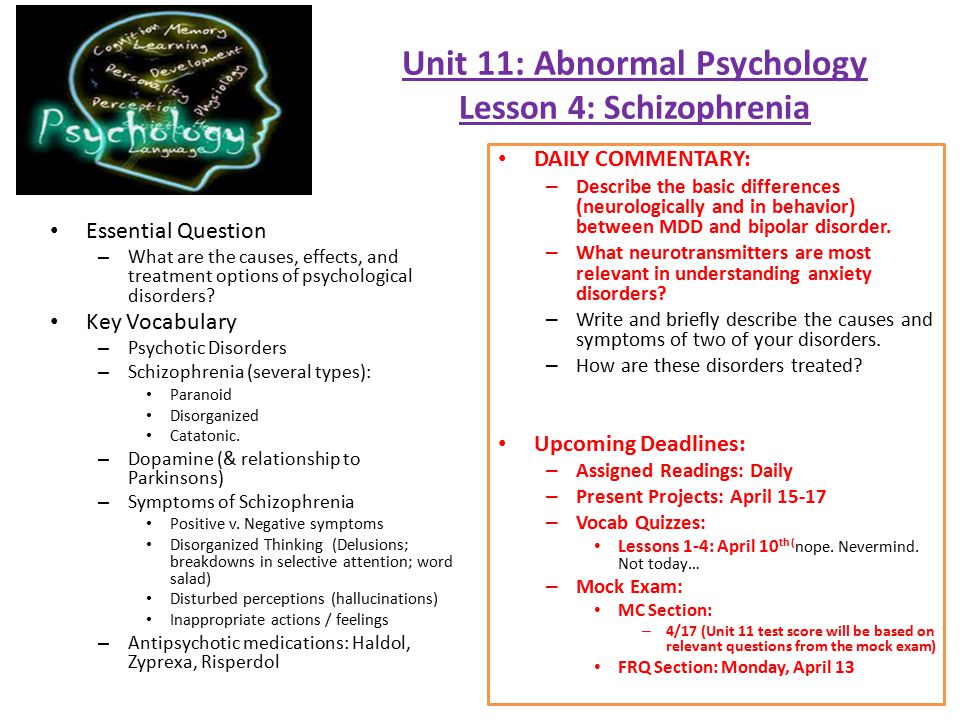 They simply can’t react to what’s happening around them as they would normally. It’s also common for people with catatonia to remember some of what happened to them even though they seemed unaware.
They simply can’t react to what’s happening around them as they would normally. It’s also common for people with catatonia to remember some of what happened to them even though they seemed unaware.
Because of how catatonia affects a person’s awareness of the world around them, it’s common that people who have it can’t speak for themselves or make decisions about their medical care. In those cases, healthcare providers will usually talk to a family member or loved one and ask them to make choices about care.
How long does catatonia last?
How long catatonia lasts depends partly on the conditions that it happens along with and the treatments received. Timely treatment is important because the longer that catatonia lasts, the less likely it’ll respond to treatment. Your healthcare provider is the best person to explain how long catatonia will last and what to expect.
What’s the outlook for this condition?
Catatonia usually isn’t life-threatening by itself (except for malignant catatonia, which is deadly without quick treatment).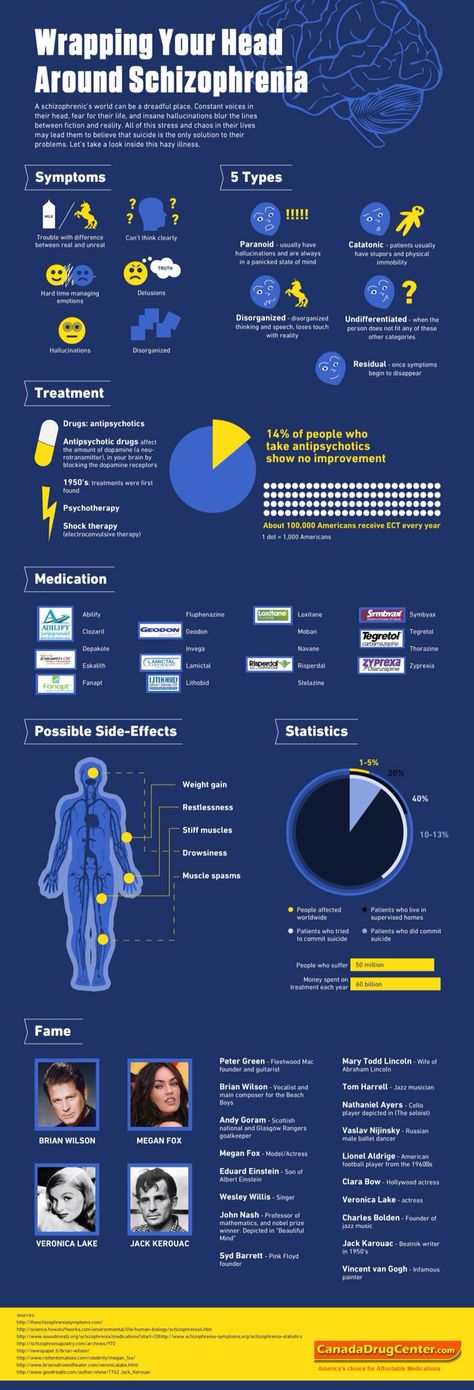 However, it’s associated with an increased risk of death from conditions that happen from not moving much, such as pulmonary embolism and pneumonia. Catatonia is also harder to treat when it lasts longer or when a person has it more than once. Fortunately, benzodiazepines and ECT have very high success rates for this condition, which means it’s very treatable.
However, it’s associated with an increased risk of death from conditions that happen from not moving much, such as pulmonary embolism and pneumonia. Catatonia is also harder to treat when it lasts longer or when a person has it more than once. Fortunately, benzodiazepines and ECT have very high success rates for this condition, which means it’s very treatable.
People with mood disorders, such as bipolar disorder and major depressive disorder, tend to respond better to treatment than people with schizophrenia. However, this can still vary, and no two cases are alike. Your healthcare provider is the best person to explain the outlook for this condition because they can provide information that’s most relevant and accurate for your situation.
Living With
How do I take care of myself?
People with severe catatonia can’t take care of themselves and need care from trained medical professionals. That’s because catatonia increases the risk of complications that happen when a person can’t move or react to the world around them.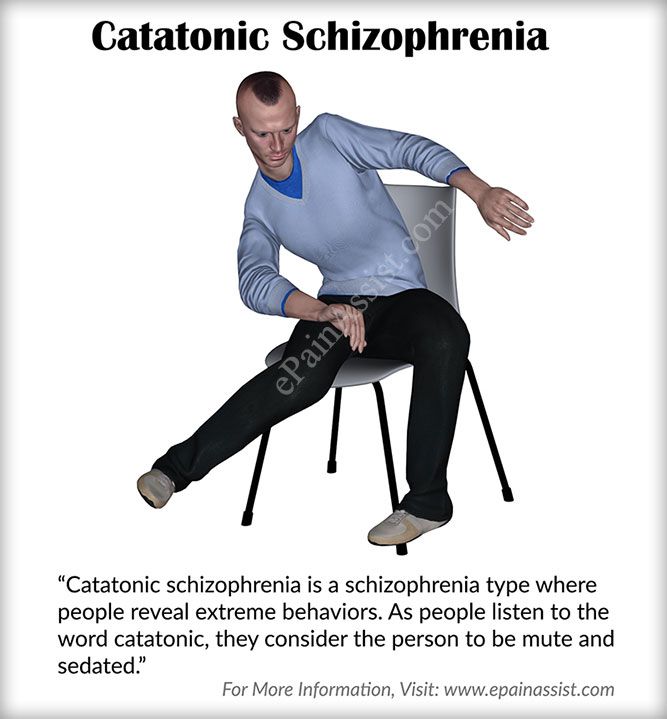 That means they can’t eat or drink, leading to problems like dehydration and malnutrition. Lack of movement can also lead to pneumonia. They can also have blood clots, which puts them at risk of a stroke or a pulmonary embolism. They’re also at risk for behavior that may cause them to harm themselves or others.
That means they can’t eat or drink, leading to problems like dehydration and malnutrition. Lack of movement can also lead to pneumonia. They can also have blood clots, which puts them at risk of a stroke or a pulmonary embolism. They’re also at risk for behavior that may cause them to harm themselves or others.
When should I see my healthcare provider, or when should I seek care?
People who show signs of catatonia need medical attention as soon as possible. That’s because the symptoms of this condition are also possible with dangerous conditions that are emergencies and need immediate care. If a loved one shows signs of catatonia, you may need to take them to the hospital or even call 911 (or your local emergency services number).
When should I go to the ER?
People who have catatonia, especially with conditions like schizophrenia, have an increased risk of self-harm and suicide. You should go to the ER or call 911 (or your local emergency services number) if you have thoughts about harming yourself, including thoughts of suicide, or about harming others.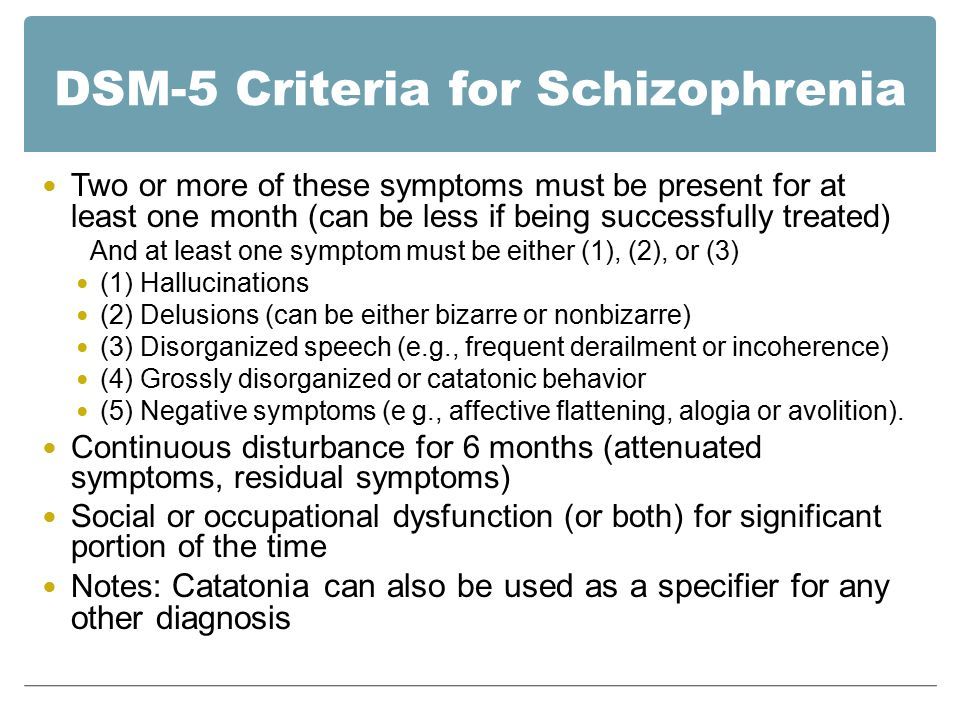 If you have thoughts like this, you can call any of the following:
If you have thoughts like this, you can call any of the following:
- National Suicide Prevention Lifeline (United States). To call this line, dial 988.
- Local crisis lines. Mental health organizations and centers in your area may offer resources and help through crisis lines.
- 911 (or your local emergency services number): You should call 911 (or the local emergency services number) if you feel like you’re in immediate danger of harming yourself. Operators and dispatchers for 911 lines can often help people in immediate danger because of a severe mental crisis and send first responders to assist.
A note from Cleveland Clinic
Catatonia is a disorder that can disrupt how a person’s brain works, affecting how they respond to the world around them. People with catatonia sometimes respond very little or not at all to what’s happening around them. Others may behave in ways that are unpredictable or dangerous to themselves or others. Catatonia can happen with many conditions, ranging from mental health disorders to medical conditions. It’s usually not acutely life-threatening, though there’s potential for serious complications and progression to malignant catatonia, which is a life-threatening emergency.
Catatonia can happen with many conditions, ranging from mental health disorders to medical conditions. It’s usually not acutely life-threatening, though there’s potential for serious complications and progression to malignant catatonia, which is a life-threatening emergency.
People with this disorder also often can’t care for themselves, which means they need medical care from trained healthcare personnel. Fortunately, catatonia is very treatable, and most people respond to medication. Those who don’t respond to medication usually respond to electroconvulsive therapy. With timely, effective treatment, the effects of catatonia are often reversible, offering the chance for the treatment of or recovery from underlying conditions associated with catatonia.
What is catatonia and why is it dangerous
November 7, 2020 Likbez Health
If a person falls into a stupor, speaks badly and adopts a strange posture, he urgently needs the help of a doctor.
What is catatonia
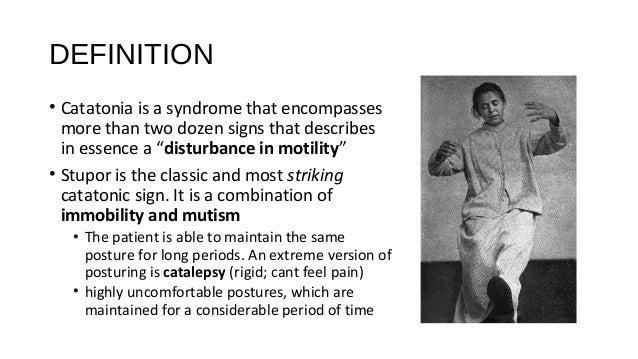
Catatonia, or catatonic syndrome, is a condition in which a person becomes immune to external stimuli and loses the ability to move and speak normally.
Until the beginning of the 20th century, it was thought that this only happened in schizophrenia. But then scientists found that more than 50% of cases of catatonia appear in bipolar disorder, about 10-15% are schizophrenia, and 21% are not associated with mental illness at all. nine0003
Catatonia is similar to mental disorders and other illnesses and is therefore difficult to recognize. For example, with it, as with a stroke, a person may respond with incomprehensible phrases or stop talking altogether. Urgent help is needed in both cases, but it will be different.
Catatonia may develop rapidly or gradually over several days. In the first case, the symptoms are usually strong and obvious; jumps in pressure or temperature are added to motor and speech disorders. This can lead, for example, to a stroke.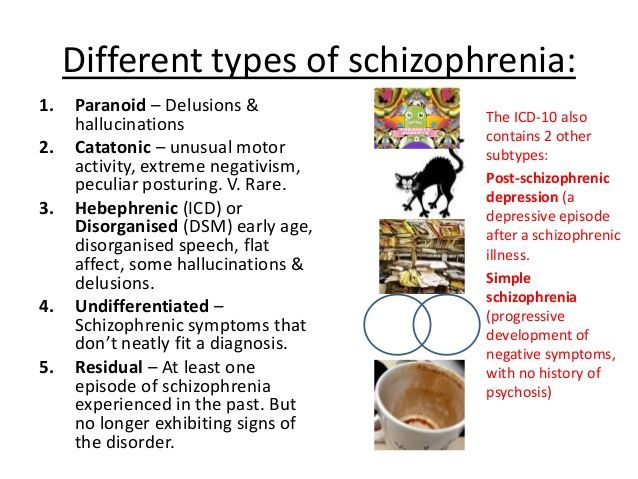 In the second option, the symptoms are hardly noticeable, and this is the most dangerous: complications may appear in 3-4 days or the person will die. nine0003
In the second option, the symptoms are hardly noticeable, and this is the most dangerous: complications may appear in 3-4 days or the person will die. nine0003
Imagine a grandmother with dementia. She often sits on the edge of the bed and looks out the window. But suddenly she spends the whole day like this. Then the grandmother stops talking, reacting to others, but continues to sit. Then she refuses food, water.
The body is exhausted, and 2-3 days after the onset of the first symptoms, blood clots form in the legs from a long immobile posture. At some point, they come off and clog the vessel. The person is dying. But he would have been saved if the dangerous symptoms had been noticed on the first day. nine0003
Why catatonia occurs
Catatonia was first described in detail in 1874, but its causes have not yet been established. Scientists have several theories that roughly explain what changes in the body lead to the onset of catatonic symptoms.
Some researchers believe that the problem lies in the disruption of the transmission of nerve impulses in those areas of the brain that are responsible for muscle contractions.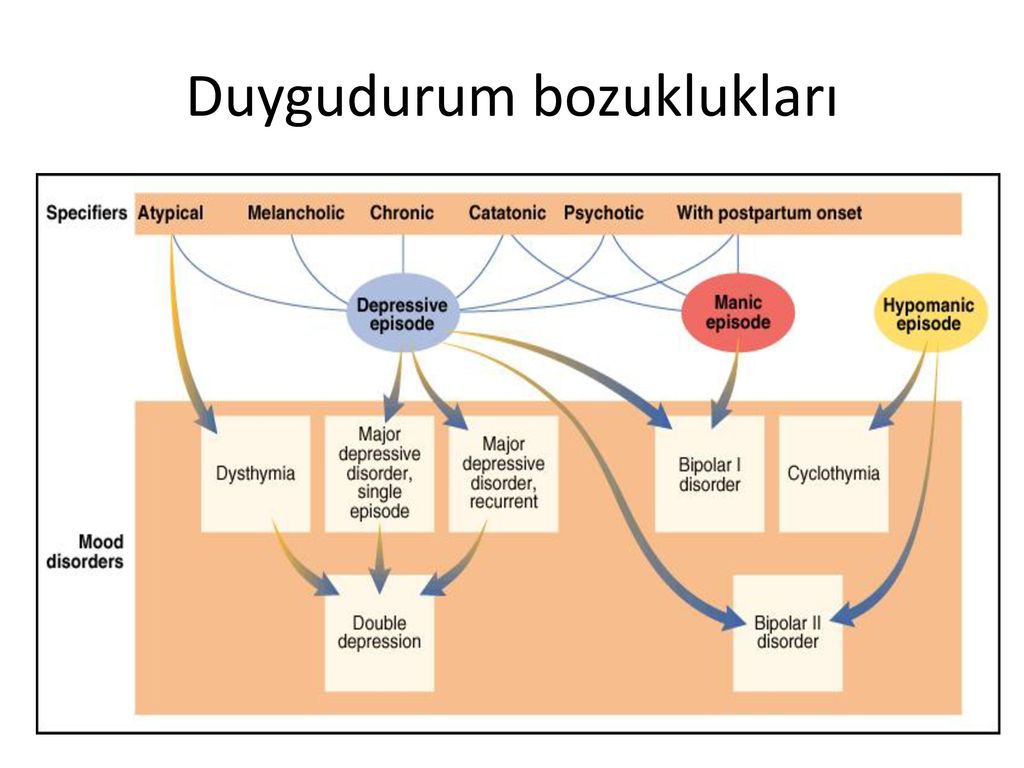 Others associate catatonia with a change in the balance of neurotransmitters - substances that are produced by brain neurons and are involved in the transmission of signals from cell to cell and many biochemical processes. Still others blame the excess or lack of certain hormones of the hypothalamus and pituitary gland, the production of antibodies to brain proteins. nine0003
Others associate catatonia with a change in the balance of neurotransmitters - substances that are produced by brain neurons and are involved in the transmission of signals from cell to cell and many biochemical processes. Still others blame the excess or lack of certain hormones of the hypothalamus and pituitary gland, the production of antibodies to brain proteins. nine0003
Such disturbances in the functioning of the body appear in many diseases:
- psychiatric, such as bipolar disorder, schizophrenia, autism, depression, anorexia nervosa;
- endocrine: Cushing's syndrome, hyperthyroidism, Sheehan's syndrome and others;
- neurological, eg epilepsy, multiple sclerosis, Parkinson's disease, brain tumors, dementia;
- metabolic - this is when the body accumulates substances that have a bad effect on the brain: this happens with Wilson's disease - Konovalov, an increase and decrease in the concentration of sodium in the blood, kidney failure and other diseases; nine0030
- autoimmune, eg systemic lupus erythematosus, antiphospholipid syndrome;
- caused by psychoactive substances: alcohol, antipsychotics, sedatives, drugs;
- infectious: HIV, typhoid fever, tuberculosis, meningoencephalitis, herpes and others;
- vascular, eg thrombosis of the arteries and veins of the brain, stroke, cerebral hemorrhage.
What are the symptoms of catatonia
Catatonia has many symptoms. The DSM-5, used by psychiatrists around the world, identifies 12 main ones. But doctors add other symptoms to them:
- Remaining immobile (stupor).
- Long-term maintenance of the posture that has been given to the body (catalepsy). If a person is planted or placed, he will not move.
- Prolonged silence (mutism). The person does not respond, even if you address him by name. On the contrary, he is likely to turn away.
- Changing the position of the limbs, like a plasticine figurine (wax flexibility). Some patients obey easily and can follow any command, like robots. nine0030
- Passive and strong resistance to any attempt to change the position of the arms and legs (negativism). Sometimes it is physically impossible to bend or straighten the limbs.
- Maintaining an uncomfortable posture (posing). For example, a person can arch on the bed without touching the pillow with his head, as if hanging in the air.
- Pretentiousness of movements (mannership). A catatonic person may gesticulate strangely and inappropriately.
- Repetitive monotonous movement (stereotype). Recall how in horror movies the possessed are constantly swaying, tapping their fingers, or moving their mouths terribly. Most likely, they have an attack of catatonia. nine0030
- Excessive excitement without external stimuli. A person can rush around the room, show aggression, rush at others.
- Involuntary movements of lips, eyebrows. Grimaces that are not built to amuse others.
- Repetition of other people's words (echolalia). Moreover, speech often becomes incoherent, monotonous, words and phrases are spoken continuously, sometimes for a very long time.
- Copying other people's movements (echopraxia).
In addition, there may be symptoms associated with disruption of the autonomic nervous system. With catatonia, the temperature rises, thirst increases, saliva flows, blood pressure rises and the pulse quickens. Often patients refuse water and food. nine0003
Often patients refuse water and food. nine0003
When a doctor makes a diagnosis, he looks for a combination of several symptoms. But medical attention is needed even with the appearance of one symptom. Otherwise, you can miss not only catatonia, but also a stroke, the debut of schizophrenia, a complication of meningitis or another disease.
How catatonia is treated
If a person cannot move, does not respond to an appeal to him, an ambulance should be called. If the symptoms are mild, it is important to go to the therapist as soon as possible.
Based on the words of relatives or by analyzing the medical record, the doctor will determine whether there are mental illnesses, alcohol dependence or other pathologies that can cause catatonia. And if necessary, send to a psychiatrist. nine0003
He will prescribe medication or electroconvulsive therapy as soon as possible.
If there is no danger to the patient's life, examination will help to find the causes of catatonia:
- complete blood count;
- biochemical examination;
- blood electrolyte test;
- liver function tests;
- CT or MRI of the brain.
An electroencephalogram will be done if there is a suspicion of a brain tumor or seizures. nine0003
What medications are prescribed
The psychiatrist uses strong prescription medications to treat catatonia. Taking them on your own is dangerous.
First of all, drugs from the group of second-generation anxiolytics based on benzodiazepine are given. They reduce muscle spasm, soothe, help remove the symptoms of catatonia. Benzodiazepines are effective in 66-100% of patients.
If these drugs do not help, the treatment regimen is changed. Sometimes alternative drugs with sedative, anticonvulsant and muscle relaxant effects give the best effect. For example, lithium preparations will not allow a recurrence of an attack of catatonia. nine0003
Medicines from the group of neuroleptics are rarely prescribed: it is impossible to guess how the patient's body will react. On the one hand, drugs can remove muscle spasm. But at the same time, they can cause neuroleptic malignant syndrome.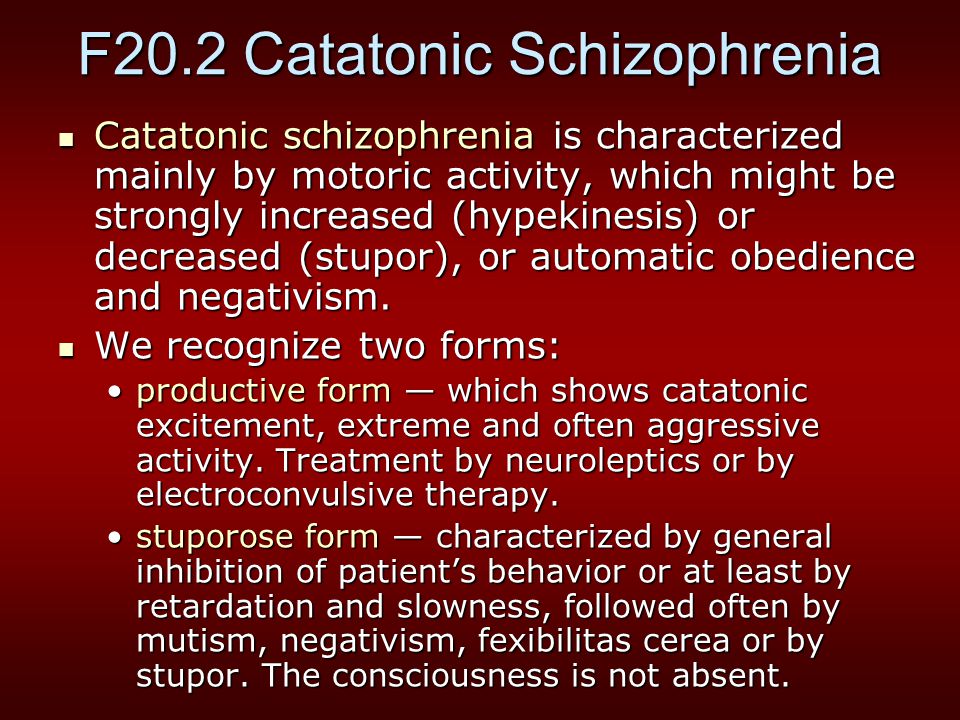 This is a condition when the temperature and pressure rise and the symptoms of catatonia intensify.
This is a condition when the temperature and pressure rise and the symptoms of catatonia intensify.
When electroconvulsive therapy is used
Electroconvulsive therapy is a treatment method in which an electric current is passed through the brain. It suppresses the foci that emit the wrong impulses and helps relieve muscle spasm and cramps. nine0003
Electroconvulsive therapy is used if benzodiazepines have failed or if the patient is at risk of death.
Catatonic attacks sometimes stop completely after electroconvulsive therapy. But there is a risk of side effects: headache, amnesia, confusion.
How successful catatonia is being treated
The sooner catatonia is treated, the better for the patient. Prompt help helps avoid complications and save lives.
But not everyone recovers. According to statistics, 12-40% of patients are successfully cured. Poor prognosis in children and adolescents with schizophrenia, as well as in the elderly.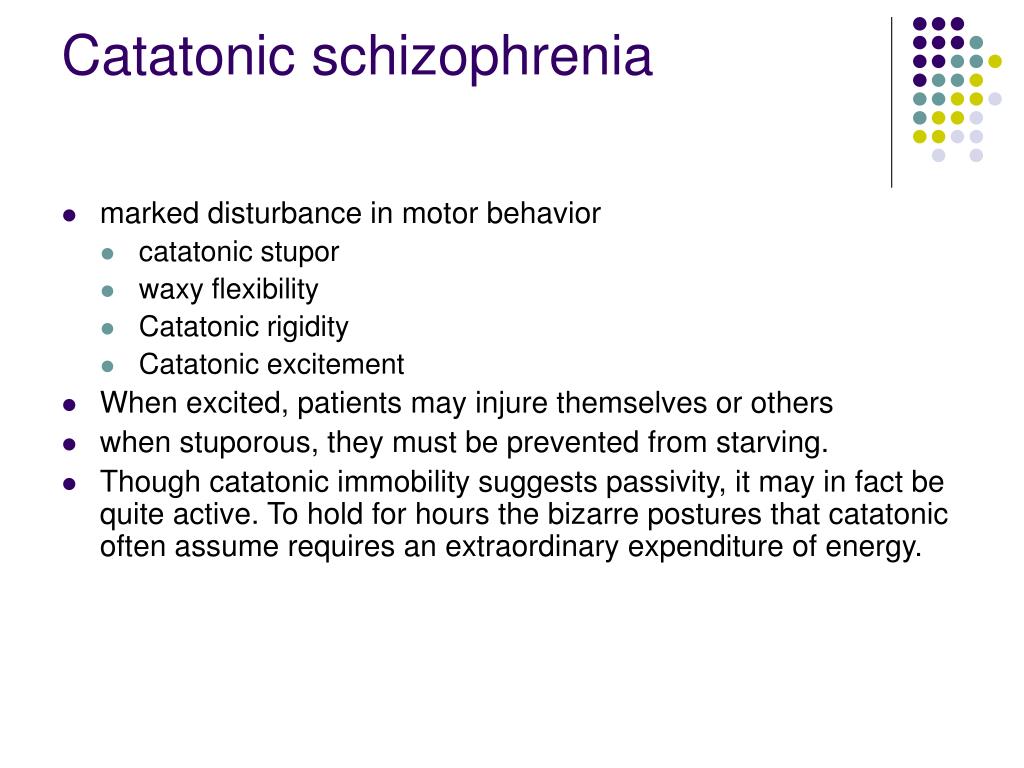 They may need ongoing psychiatric care. nine0003
They may need ongoing psychiatric care. nine0003
If a person has been suffering from kidney failure, alcoholism, Parkinson's disease or other pathology for a long time, then the disturbances in the brain function are already chronic. Therefore, at any time, the catatonic syndrome can recur. In order not to be late with help, you need to remember the dangerous symptoms and follow the doctor's recommendations.
How not to get catatonia
Scientists have not yet learned how to prevent catatonia, like other mental illnesses or brain tumors. But, given the causes of the syndrome, we can advise the following:
- Reduce alcohol consumption and treat addiction symptoms.
- Never use drugs.
- Do not ignore symptoms of depression.
- Do not take hypnotics, sedatives, neuroleptics without a prescription from a specialist.
- Seek medical attention if headaches, dizziness, flies in the eyes.
- Treat kidney and liver diseases in time.
- Avoid casual sex to protect against HIV and syphilis. nine0030
- Watch your weight and avoid stress so as not to worsen the condition of blood vessels.
- Pregnant women should register on time and follow the doctor's recommendations so that the birth goes smoothly.
- Take care not to injure your head.
Read also 💊😨🚑
- How to help your loved one get out of depression
- 8 mental health myths to get out of your head
- How to stop borderline personality disorder from ruining your life
- 12 signs of an anxiety disorder
- How to take care of loved ones with mental disorders
NTSPZ. ‹‹General Psychiatry››
Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
This is a state of mental disorder with a predominance of disorders in the motor sphere, characterized by a picture of lethargy (stupor) or excitation.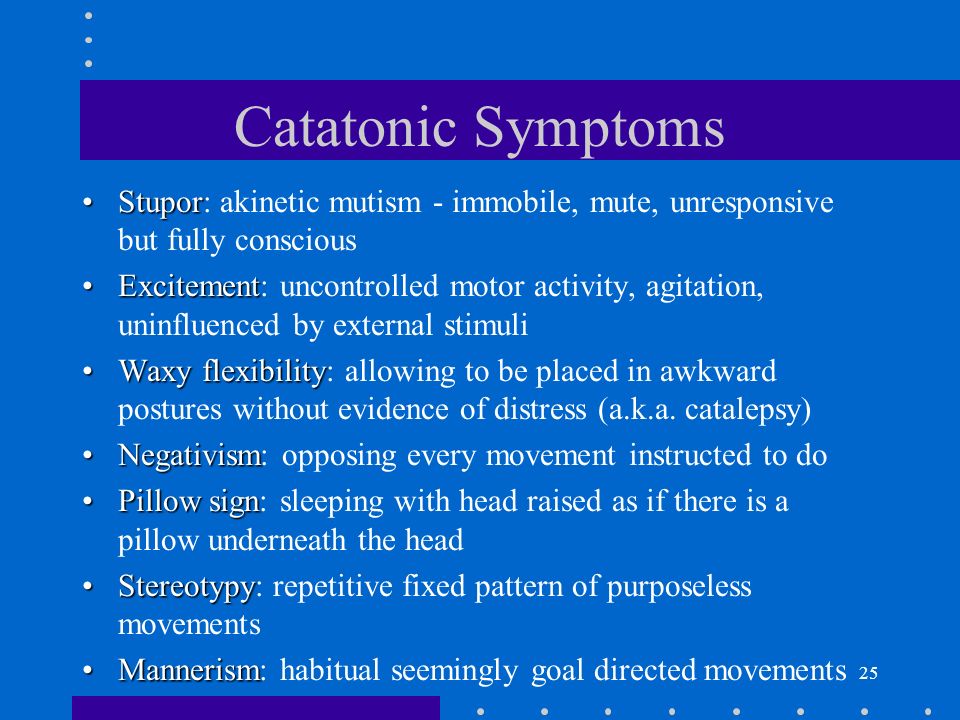
Catatonic stupor is manifested by immobility, increased muscle tone and mutism (refusal of speech). There are stupor with phenomena of wax flexibility, negativistic stupor and stupor with stupor. nine0003
Stupor with phenomena of wax flexibility (catalepsy) - a condition in which any change in the patient's posture persists for a more or less long time. As a rule, the phenomena of wax flexibility occur first in the muscles of the chewing muscles, then successively in the muscles of the neck, upper and lower extremities. The "air cushion symptom" is characteristic, in which the head raised above the pillow retains the position attached to it indefinitely. The disappearance of these phenomena occurs in the reverse order. nine0003
A stupor with wax flexibility can turn into a stupor with negativism. The latter sometimes precedes the onset of stupor with stupor.
Negativistic stupor is manifested by the complete immobility of the patient, and any attempt to change the posture causes a sharp muscle tension with resistance.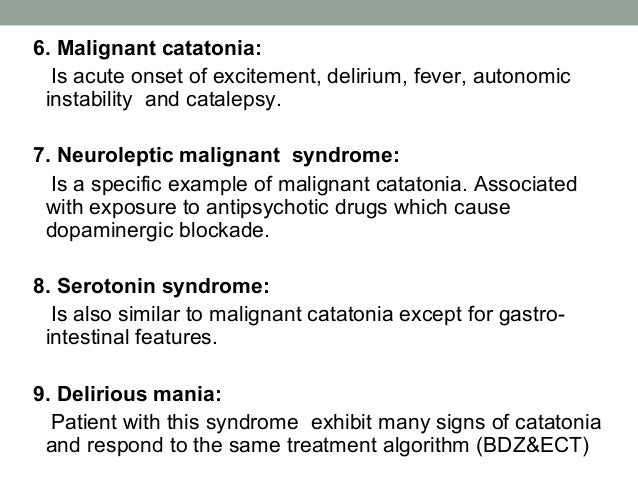 Often there are signs of passive and active negativism. With passive negativism, patients do not follow instructions, and when they try to force them to perform one or another action, they resist, accompanied by an increase in muscle tone. With active negativism, they not only resist the proposed action, but also strive to perform the opposite motor act. nine0003
Often there are signs of passive and active negativism. With passive negativism, patients do not follow instructions, and when they try to force them to perform one or another action, they resist, accompanied by an increase in muscle tone. With active negativism, they not only resist the proposed action, but also strive to perform the opposite motor act. nine0003
Stupor with stupor - a state of extreme muscle tension, in which patients constantly stay in the same position, often in utero: they lie on their side, legs bent at the knee joints and pressed to the stomach, arms crossed on the chest, head pressed to chest, jaw clenched. Often these patients have a symptom of the proboscis: the lips are extended forward with tightly clenched jaws. For stupor with stupor, however, as well as for some other types of catatonic stupor, the phenomena of mutism are characteristic. nine0003
In addition to the listed types of stupor, there are substuporous states with incomplete immobility, mild manifestations of waxy flexibility, and partial mutism.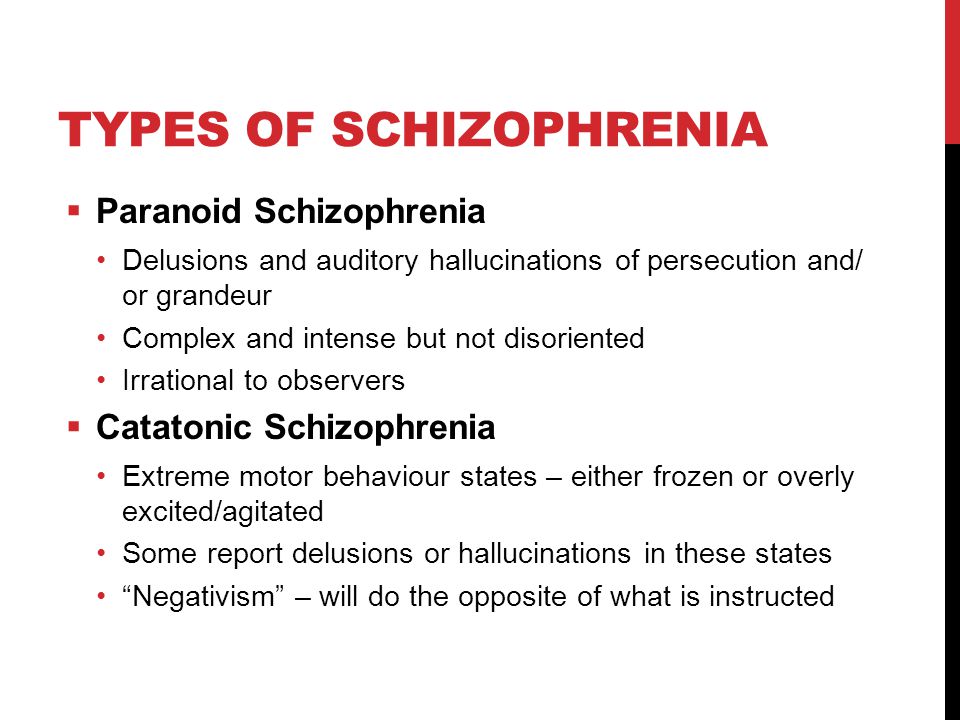
Catatonic excitement can be ecstatic (bewilderedly pathetic), hebephrenic, impulsive and mute (silent).
Ecstatic, or perplexed-pathetic, excitement is manifested by pathos, ecstasy. Patients take theatrical poses, sing, recite poetry, their faces are dominated by an expression of delight, penetration. Spoken, incoherent. Excitation may be interrupted by episodes of stupor or substupor. nine0003
Impulsive excitement is expressed in unexpected, sudden actions. Patients suddenly jump up, run somewhere, try to hit others, fall into a state of violent rage, aggression, freeze for a short time, become excited again. In speech, the repetition of heard words (echolalia) or the repetition of the same words (verbigeration) often predominates.
Hebephrenic excitement is characterized by foolishness, grimacing, ridiculous, senseless laughter. Patients jump, grimacing, dancing, inappropriately flat jokes, suddenly become aggressive.