Depression and depersonalization
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Recovery and Recovery Support | SAMHSA
Recovery and Resilience
Resilience refers to an individual’s ability to cope with change and adversity. Resilience develops over time and gives an individual the capacity not only to cope with life’s challenges but also to be better prepared for the next stressful situation. Psychological resilience, the ability to cope with adversity and to adapt to stressful life events, varies widely from person to person and depends on environmental as well as personal factors. It refers to positive adaptation, or the ability to maintain mental and physical health despite participating in stressful situations. Resilience is playing up those protective factors so they can outweigh the risk factors. Optimism and the ability to remain hopeful are essential to resilience and the process of recovery.
Because recovery is a highly individualized process, recovery services and supports must be age appropriate and offered over the life course and flexible enough to ensure cultural relevancy.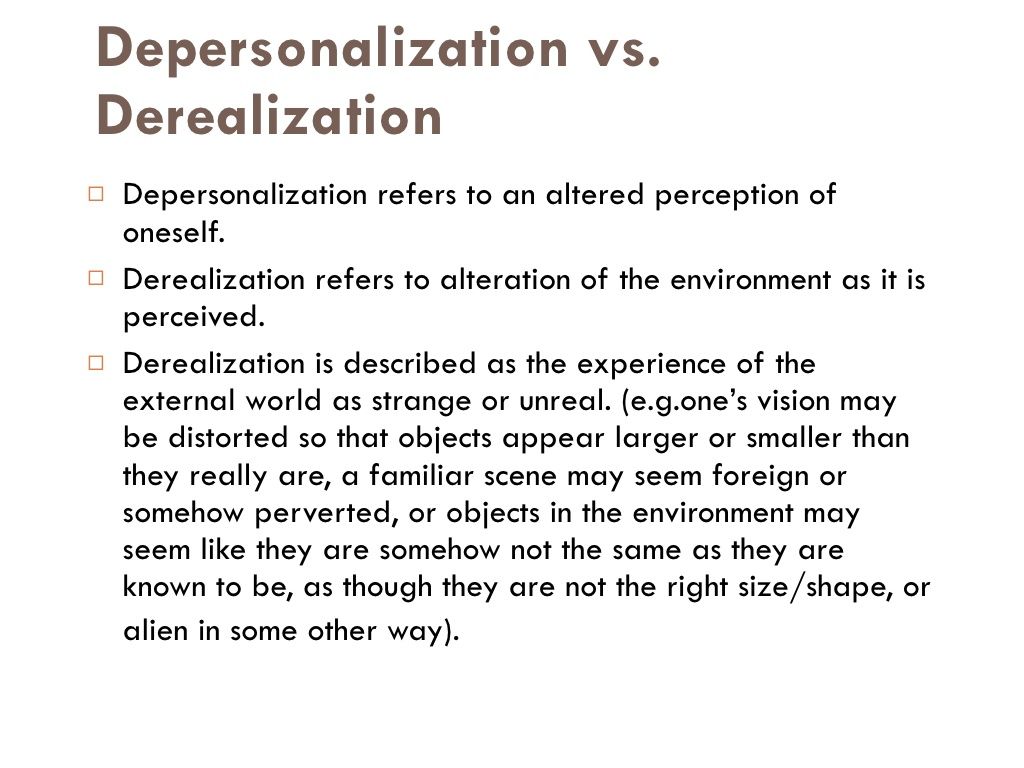 What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
Recovery and Relationships
The process of recovery is supported through relationships and social networks. This often involves family members who become the champions of their loved one’s recovery. They provide essential support to their family member’s journey of recovery and similarly experience the moments of positive healing as well as the difficult challenges. Families of people in recovery may experience adversities in their social, occupational, and financial lives, as well as in their overall quality of family life.
These experiences can lead to increased family stress, guilt, shame, anger, fear, anxiety, loss, grief, and isolation. The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
Peer support assists individuals to engage or stay connected to the recovery process through a shared understanding, respect, and mutual empowerment. Peer support extends beyond the reach of clinical treatment into the everyday environment providing non-clinical, strengths-based support. This relationship can help lay the foundation for SAMHSA’s four dimensions of recovery.
Recovery Support
SAMHSA advanced recovery support systems to promote partnering with people in recovery from mental and substance use disorders and their family members to guide the behavioral health system and promote individual, program, and system-level approaches that foster health and resilience; increase housing to support recovery; reduce barriers to employment, education, and other life goals; and secure necessary social supports in their chosen community.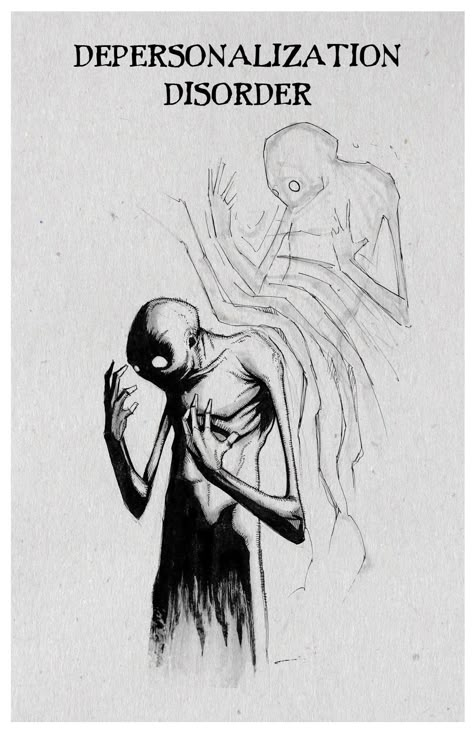
Recovery support is provided in various settings. Recovery support services help people enter into and navigate systems of care, remove barriers to recovery, stay engaged in the recovery process, and live full lives in communities of their choice.
Recovery support services include culturally and linguistically appropriate services that assist individuals and families working toward recovery from mental and/or substance use problems. They incorporate a full range of social, legal, and other services (PDF | 409 KB). that facilitate recovery, wellness, and linkage to and coordination among service providers, and other supports shown to improve quality of life for people (and their families) in and seeking recovery.
Recovery support services may be provided before, during, or after clinical treatment, or may be provided to individuals who are not in treatment but seek support services.
These services, provided by professionals and peers, are delivered through a variety of community and faith-based groups, treatment providers, schools, and other specialized services.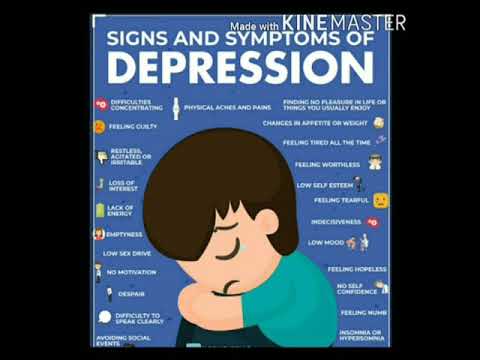 The broad range of service delivery options ensures the life experiences of all people are valued and represented.
The broad range of service delivery options ensures the life experiences of all people are valued and represented.
For example, in the United States there are 34 recovery high schools that help reduce the risk in high school environments for youth with substance use disorders. These schools typically have high retention rates and low rates of students returning to substance use.
Additionally, SAMHSA's Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS) advances effective recovery supports and services for people with mental or substance use disorders and their families.
Find more Publications and Resources on Recovery and Recovery Support.
FGBNU NTsPZ. ‹‹Depression and depersonalization››
The data given in the previous chapter show that depersonalization in MDP significantly worsens the course of the disease and sharply reduces the therapeutic sensitivity of affective attacks. Great difficulties arise in the treatment of other mental disorders if depersonalization plays a significant role in their psychopathological picture.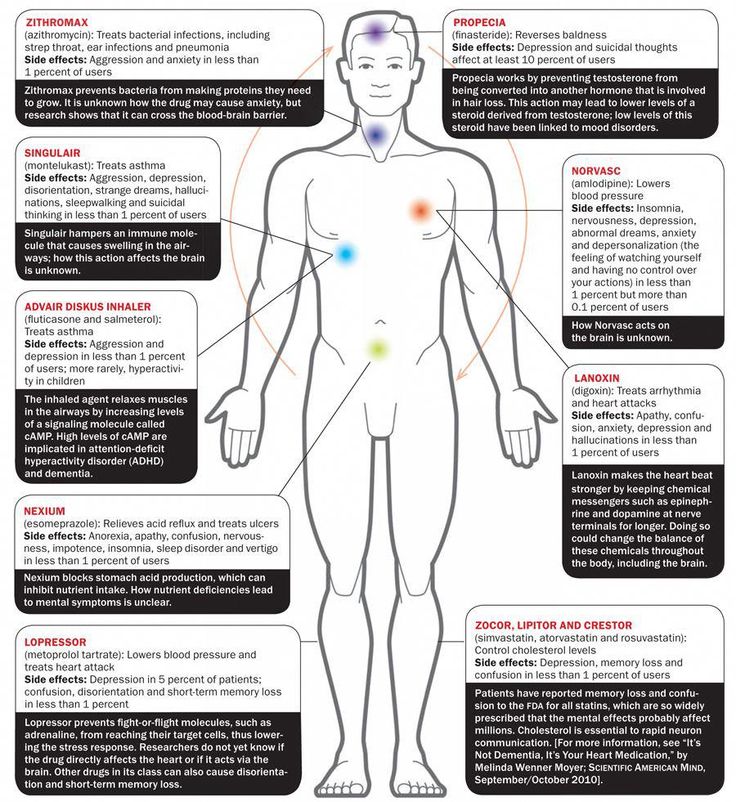 However, despite the importance of this problem, very little special research has been devoted to depersonalization, and it remains one of the least studied psychopathological phenomena. nine0003
However, despite the importance of this problem, very little special research has been devoted to depersonalization, and it remains one of the least studied psychopathological phenomena. nine0003
First of all, this is confirmed by extremely vague terminology, since almost every school gives the term "depersonalization" different meanings. This is partly due to the failure of the word itself: it is often understood literally (i.e., "depersonalization", loss of one's "I") and numerous disorders are attributed to depersonalization: a split personality, the phenomenon of "made", etc. Depersonalization also often includes violations of the body schema, gross derealization, opto-vestibular disorders, etc. However, it should be remembered that Degas, who introduced this term, emphasized that depersonalization is not a loss of the sense of "I", but a feeling (feeling) of loss of his "I", which is one of the many manifestations of the mental disorder denoted by this term. There are other terms that denote it: “a sense of alienation”, which, according to L.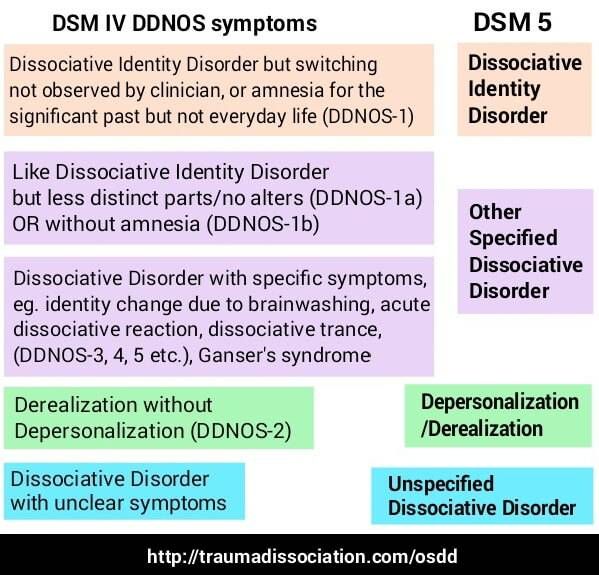 L. Megrabyan (1962), is more adequate, “psychic anesthesia”, “feeling of unreality”, “hypopathy”, etc. However, the word “depersonalization” has firmly entered the literature, and its replacement seems currently inappropriate, despite its obvious failure.
L. Megrabyan (1962), is more adequate, “psychic anesthesia”, “feeling of unreality”, “hypopathy”, etc. However, the word “depersonalization” has firmly entered the literature, and its replacement seems currently inappropriate, despite its obvious failure.
Most of the works devoted to depersonalization are either purely descriptive or interpret this phenomenon from psychological and philosophical positions, in foreign literature - most often from the point of view of psychoanalysis. nine0003
When studying this or that psychopathological phenomenon, a number of questions arise:
1) in what diseases it occurs and what is its diagnostic value;
2) whether there is a predisposition to it and in response to what influences and harmfulness it arises;
3) with what other symptoms it correlates;
4) whether it can cause or participate in the formation of other psychopathological disorders; nine0003
5) how it affects the course of the disease.
The accumulation of such data, obviously, should contribute to the solution of the final task: the disclosure of pathogenetic mechanisms and the discovery of effective methods of treatment and prevention of the disorder under study.
As you know, depersonalization disorders are observed in almost all mental illnesses, epilepsy, in borderline conditions, as well as in a mild and short-term form in mentally healthy people with emotional stress, somatic diseases, after childbirth. nine0003
The manifestation of depersonalization is characterized by the loss of the emotional component of mental processes. This applies not only to the classic symptoms of mental anesthesia: loss of feelings for loved ones, lack of emotional perception of the environment, nature, works of art, etc., but also to the depersonalization of thinking, memory, somatopsychic depersonalization. In such patients, thoughts pass without leaving a trace; there is no feeling of their ending, as they go without emotional accompaniment, they are faceless; memory is disturbed, but there is no feeling of recognition; previous experiences, images, thoughts are dull, as if erased, so it seems that there is nothing in the memory.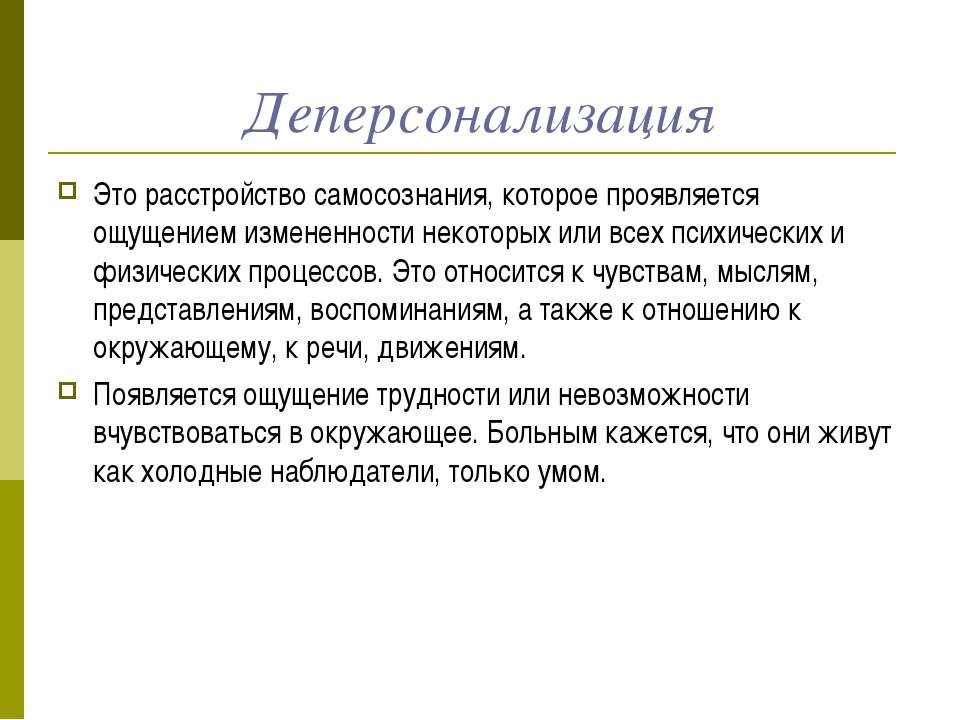 nine0003
nine0003
To take into account the dynamics and quantitative assessment of depersonalization symptoms, we used a graded rating scale developed jointly with E. L. Genkina, which includes the following manifestations: various degrees of decrease or change in attitudes towards loved ones, perception of the environment, nature, art, as well as depersonalization of thinking, depersonalization of memory , violation of the sense of familiarity, the presence or absence of emotional reactions (resentment, anger, compassion, joy, etc.), contact with others and a sense of empathy, alienation of one's own "I", depersonalization of ideas, somatopsychic depersonalization (absence or dulling of pain, tactile , temperature sensitivity, taste, hunger, satiety, feeling of sleep, etc.) disturbance of the sense of time, a feeling of mental pain associated with the absence of feelings, as well as symptoms such as anxiety, longing, feeling of incompleteness, derealization, somatic symptoms. Each of the main symptoms was divided into 4-5 gradations.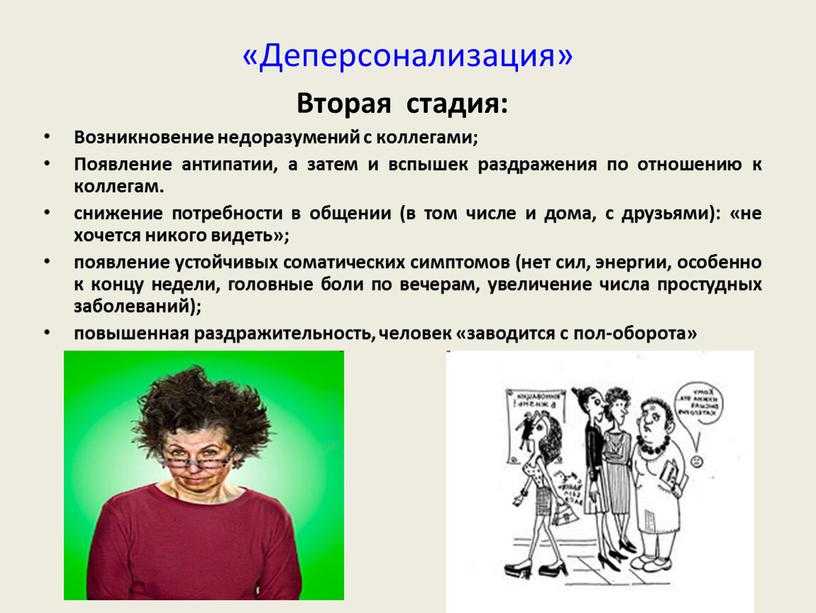 nine0003
nine0003
As a reference, we studied a group of patients (6 men and 12 women), whose psychopathological symptoms were limited to massive or total depersonalization, as well as affective disorders (anxiety, tension, depressive mood). In some patients of this group, depersonalization did not reach the degree of totality, and some of its manifestations were absent: more often there was no complete analgesia (observed in 3 patients), “time stop” (only in 2 patients), not in all cases depersonalization of thinking and memory was noted. Patients in this group were most often diagnosed with organic brain diseases with mental disorders, atypical MDP, and sometimes schizophrenia. nine0003
All these patients had common features in premorbidity: they were hyperemotional personalities, anxious, impressionable, vulnerable, touchy. In childhood, many of them constantly feared the death of their parents. They were extremely painfully worried not only about leponex (clozepine), a neuroleptic with a powerful anti-anxiety effect.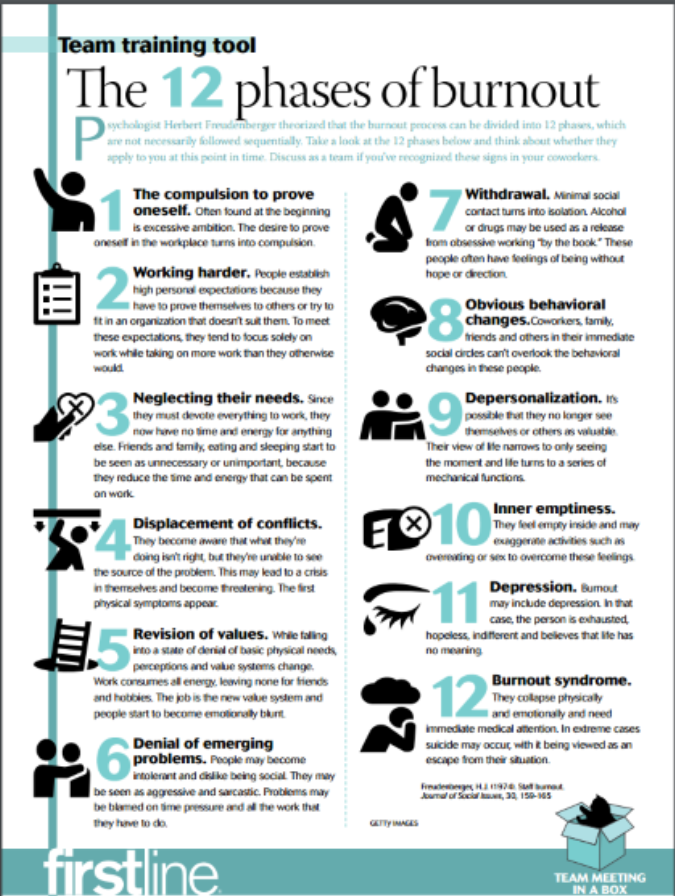 Leponex was administered orally or intramuscularly at doses ranging from 150 to 600 mg per day. In 9 patients, treatment was started in the first months after the development of the depersonalization syndrome, which was characterized, in addition to autopsychic depersonalization, by massive somatic depersonalization, anxiety, tension, and depression. All have 9patients noted either the complete disappearance of psychotic symptoms, or such a significant mitigation that the patients could be discharged from the hospital.
Leponex was administered orally or intramuscularly at doses ranging from 150 to 600 mg per day. In 9 patients, treatment was started in the first months after the development of the depersonalization syndrome, which was characterized, in addition to autopsychic depersonalization, by massive somatic depersonalization, anxiety, tension, and depression. All have 9patients noted either the complete disappearance of psychotic symptoms, or such a significant mitigation that the patients could be discharged from the hospital.
Interestingly, the sequence of regression of symptoms during treatment with Leponex coincided with the order of its occurrence: first anxiety disappeared, then depression, then symptoms of somatic depersonalization, and, most slowly, autopsychic depersonalization. They smoothed out gradually, only on the 4-6th week of treatment with Leponex, hiding most often the improvement began with short periods of "enlightenment", "return of feelings", after which "insensibility" returned again.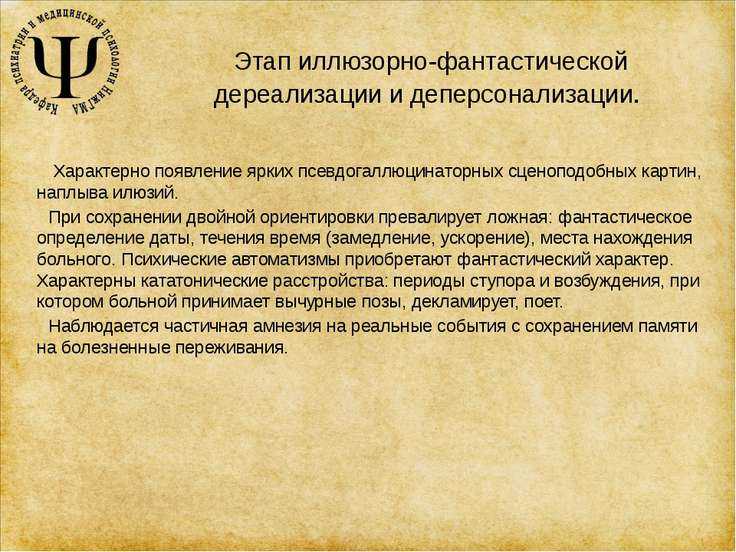 The first to return was the feeling of contact with the interlocutor, affection and warmth for children, other close people, the last to restore the emotional perception of nature, works of art. nine0003
The first to return was the feeling of contact with the interlocutor, affection and warmth for children, other close people, the last to restore the emotional perception of nature, works of art. nine0003
In 3 patients, with a rapid increase in doses of Leponex, the symptoms disappeared critically, following the onset of a state of a kind of confusion, disorientation.
In 6 patients with a long-term course of the disease, the prevalence of autopsychic depersonalization phenomena and the complete absence or presence of only slight anxiety, Leponex treatment turned out to be ineffective or caused only a partial improvement. These data confirm the role of anxiety in the pathogenesis of depersonalization. nine0003
The fact that the positive therapeutic effect of Leponex is associated precisely with its anti-anxiety effect is confirmed by the good results obtained in the treatment of depersonalization states with phenazepam.
In total, 42 people with severe depersonalization symptoms, which were the leading component of the syndrome, were treated with phenazepam.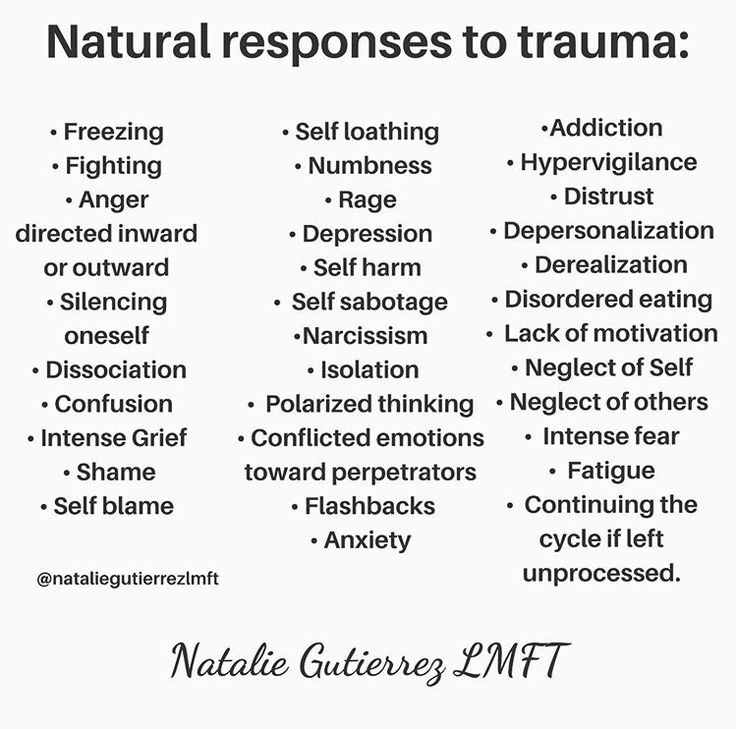 All those treated had phenomena of auto- and somatopsychic depersonalization, in most of them they were accompanied by a feeling of mental pain. As mentioned above, formally, patients were diagnosed with "sluggish schizophrenia", "atypical MDP", "organic brain disease with mental disorders", etc. Most of the patients were women (34 people). Phenazepam was used in daily doses of 3-6 mg, although in some patients the dose reached 20 and even 30 mg. In general, in the treatment of any drugs in patients with depersonalization, larger doses were usually required than in similar diseases, but occurring without it. nine0003
All those treated had phenomena of auto- and somatopsychic depersonalization, in most of them they were accompanied by a feeling of mental pain. As mentioned above, formally, patients were diagnosed with "sluggish schizophrenia", "atypical MDP", "organic brain disease with mental disorders", etc. Most of the patients were women (34 people). Phenazepam was used in daily doses of 3-6 mg, although in some patients the dose reached 20 and even 30 mg. In general, in the treatment of any drugs in patients with depersonalization, larger doses were usually required than in similar diseases, but occurring without it. nine0003
Of the 42 patients, in 13 psychopathological symptoms disappeared completely, in 12 they significantly decreased, in 9 there was a moderate improvement, and in 8 there was no positive effect. Thus, positive results were noted in 25 out of 42 patients, which, given the therapeutic resistance of such patients, should be regarded as a significant success.
Patients who developed depersonalization recently, accompanied by a feeling of mental pain, combined with anxiety, tension, and senestopathies, responded better.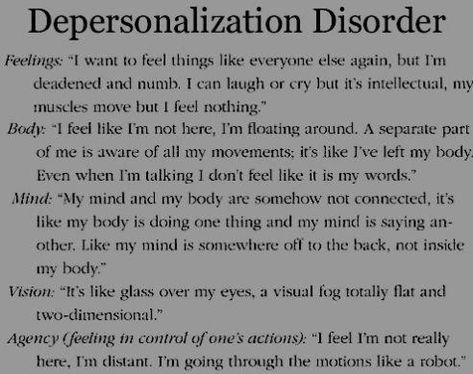 The action of phenazepam was primarily manifested in the mitigation of internal tension and anxiety, then the phenomena of somatopsychic depersonalization began to decrease, and then autopsychic, although the differences in the rate of regression between auto- and somatopsychic depersonalization were sometimes difficult to establish. nine0003
The action of phenazepam was primarily manifested in the mitigation of internal tension and anxiety, then the phenomena of somatopsychic depersonalization began to decrease, and then autopsychic, although the differences in the rate of regression between auto- and somatopsychic depersonalization were sometimes difficult to establish. nine0003
With good effect; usually at the onset of the disease, the complete disappearance of psychopathological symptoms was observed in the first days, and its regression occurred simultaneously.
With prolonged, many months and many years of depersonalization states, the results of treatment with phenazepam were worse, but in a number of cases, when depersonalization was combined with anxiety and the characteristic somatic complaints described above, the effect turned out to be quite good. In general, the impression was made that depersonalization occurs more often and more acutely in women, and to a greater extent it is combined with mental and somatic manifestations of anxiety (stress), but the results of treatment are better for them. nine0003
nine0003
In a significant proportion of patients, after achieving a therapeutic effect, long-term (sometimes several years) maintenance therapy with phenazepam was required.
As mentioned earlier, many patients with manic-depressive psychosis in the classic melancholic syndrome have anaesthesia psychica dolorosa and somatic depersonalization. Depressive phases are less commonly observed, characterized by a pronounced depressive-depersonalization syndrome, in which depersonalization occupies a leading place in the structure of the syndrome. Depersonalization occurred either at the height of a severe melancholic syndrome, with extremely intense vital anguish, or in patients with an acute onset of anxious depression, i.e. and in these cases, depersonalization appeared following the onset of a tense, intense affect of anxiety or vital anguish. For the depressive phases of MDP, occurring with a depressive-depersonalization syndrome, there was a characteristic tendency to a protracted course.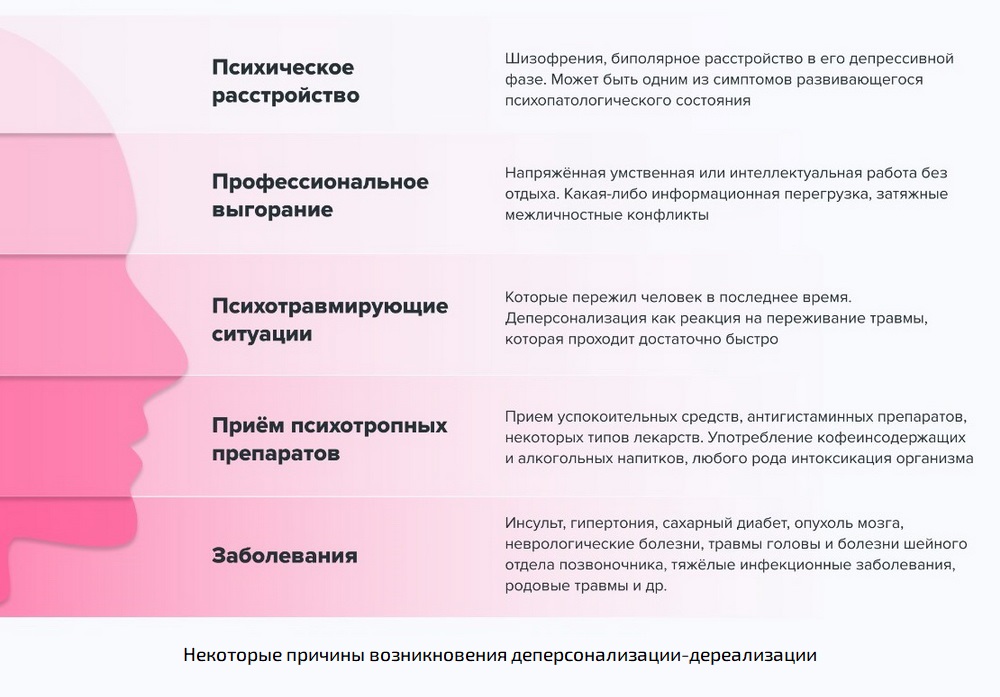 In some cases, depersonalization after several depressive phases gradually begins to spread to the interphase interval, and in 3 patients with a bipolar course of psychosis, depersonalization remained during the period of manic states (see observation 4) .
In some cases, depersonalization after several depressive phases gradually begins to spread to the interphase interval, and in 3 patients with a bipolar course of psychosis, depersonalization remained during the period of manic states (see observation 4) .
Thus, it seems that depersonalization, triggered by the affects of anxiety and, probably, vital anguish, at first closely associated with them, later acquires an autonomous existence, regardless of the affective background. In the debut, depersonalization is more dependent on affect. This is confirmed by the data of the "diazepam test". As shown in Chap. 4 , intravenously administered seduxen caused a reduction in depersonalization symptoms in a significant proportion of patients. Processing by factor analysis of these data showed that depersonalization turned out to be a core symptom of two factors, and in one it was associated with psychopathological manifestations of anxiety, in the other it was not. nine0003
Of interest is the reaction to the introduction of seduxen in a patient admitted in a state of stupor that arose at the height of the affect of fear.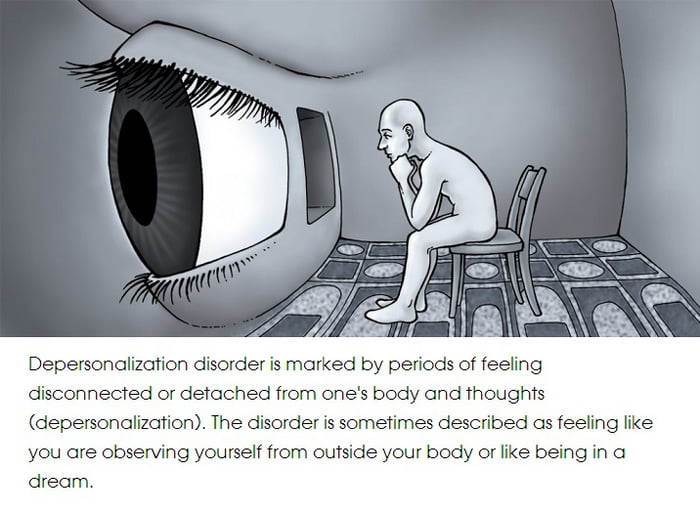 Prior to this, the patient had been taking the contraceptive drug infecundin for many years, after the cancellation of which an anxiety-depressive state developed, and anxiety and fear quickly increased, they were joined by massive depersonalization symptoms, reaching the degree of total depersonalization. After the introduction of Seduxen and a period of sleep, instead of the previous insensibility, the patient felt an acute vital anguish, which gradually, within 2 hours, disappeared. It seems that in this case, depersonalization, as it were, blocked the affect of melancholy, and after its removal, melancholy "broke out". nine0003
Prior to this, the patient had been taking the contraceptive drug infecundin for many years, after the cancellation of which an anxiety-depressive state developed, and anxiety and fear quickly increased, they were joined by massive depersonalization symptoms, reaching the degree of total depersonalization. After the introduction of Seduxen and a period of sleep, instead of the previous insensibility, the patient felt an acute vital anguish, which gradually, within 2 hours, disappeared. It seems that in this case, depersonalization, as it were, blocked the affect of melancholy, and after its removal, melancholy "broke out". nine0003
The ability of depersonalization to block productive symptoms and stabilize the course of the process is indicated by two cases of removal of massive depersonalization in patients with schizophrenia. At the age of 18, one patient developed an anxiety-depressive state, which was replaced by depersonalization, which lasted more than 5 years. Medical therapy was ineffective. After severe stress (a car accident that happened through the fault of the patient), depersonalization completely disappeared, but a month later the patient had ideas of persecution, relationships, influence, hallucinations, Kandinsky-Clerambault syndrome. Another patient from the age of 24 had periodic stuporous states, accompanied by fear, an influx of thoughts. A catatonic form of schizophrenia was diagnosed, the patient received treatment with various antipsychotics, ECT without a significant effect. Later, in the interprison periods, depersonalization developed, combined with anxious tension. At 1976 (pa 18th year of illness) as a result of treatment with phenazepam, depersonalization disappeared for the first time, and the patient was discharged home. However, soon after a month, paranoid symptoms developed acutely against the background of a pronounced affect of fear.
After severe stress (a car accident that happened through the fault of the patient), depersonalization completely disappeared, but a month later the patient had ideas of persecution, relationships, influence, hallucinations, Kandinsky-Clerambault syndrome. Another patient from the age of 24 had periodic stuporous states, accompanied by fear, an influx of thoughts. A catatonic form of schizophrenia was diagnosed, the patient received treatment with various antipsychotics, ECT without a significant effect. Later, in the interprison periods, depersonalization developed, combined with anxious tension. At 1976 (pa 18th year of illness) as a result of treatment with phenazepam, depersonalization disappeared for the first time, and the patient was discharged home. However, soon after a month, paranoid symptoms developed acutely against the background of a pronounced affect of fear.
These observations are isolated, and it is difficult to draw any conclusions on their basis, however, it seems that in both patients, depersonalization stabilized the disease process, preventing the development of productive symptoms, since after the disappearance of depersonalization and short-term remission (up to a month), there was an acute hallucinatory-paranoid syndrome.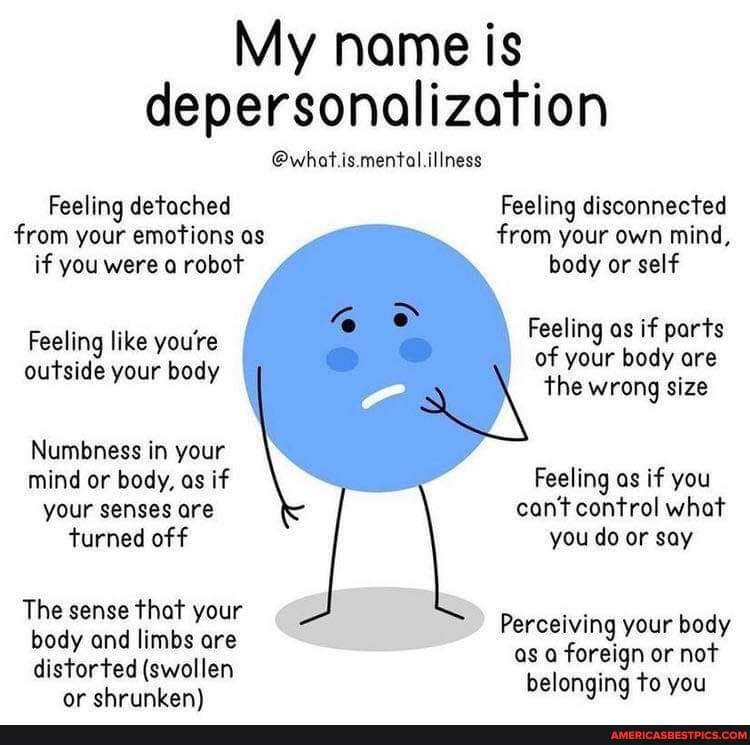 nine0003
nine0003
Our few observations concerning the occurrence of depersonalization in the clinic of borderline conditions and in mentally healthy individuals coincide with the literature data. In all these cases, depersonalization arose after a severe stress reaction caused by severe and acute psychotrauma. So, long-term and massive depersonalization symptoms arose in a young woman whose 4-year-old daughter was lost in the taiga. In another case, a man experienced depersonalization after he drowned and was barely rescued. We also observed long-term autopsychic depersonalization (more than 10 years) in former prisoners of fascist concentration camps. There are literary data about the occurrence of depersonalization in the Nazi death camps (Bluhm H., 1948).
Usually in these cases, depersonalization is not recognized as a disease and is discovered by chance when meeting with a psychiatrist or neuropsychiatrist due to other reasons. These individuals are characterized by certain behavioral features: in essence they are lonely, they strive to fill life with a chain of formal tasks and rules (for example, daily walks along the same route, which, however, do not bring any pleasure, attending popular lectures “as if by duty”, concerts, meetings, etc. , a petty schedule of the day by the hour, although there is no particular shortage of time, etc.). They try to act “as it should be”, “as is customary”, although they do not have an internal incentive for certain actions . Remembering the period of time after the onset of depersonalization, they hardly mark individual milestones; “Despite the fact that each day stretches terribly long, the past years flashed by quite imperceptibly, leaving almost no trace in the memory.”
All the patients of this group observed by us in the past also showed increased impressionability and anxiety, a tendency to strong emotional reactions.
Comparison of the above observations and literature data makes it possible to answer a number of the questions posed above. nine0003
1. Depersonalization is a nosologically specific reaction that occurs in various psychoses, as well as in patients with borderline conditions and in mentally healthy individuals under conditions of strong emotional stress (meaning negative emotions and affects: anxiety, fear, melancholy).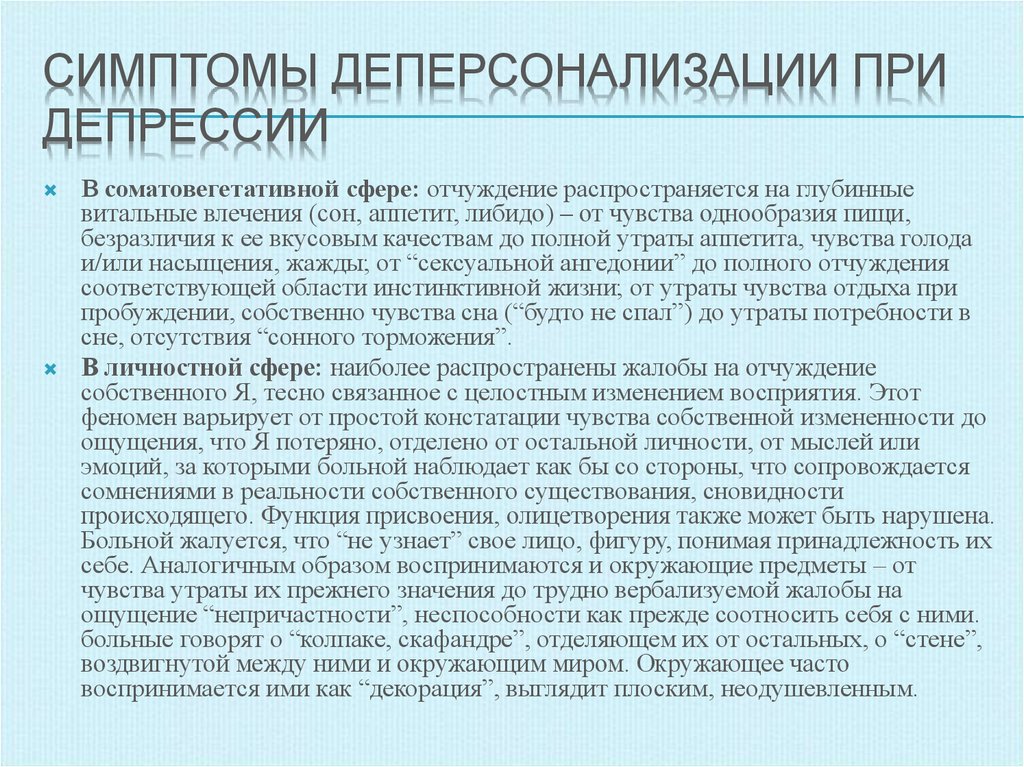
2. Depersonalization, as a rule, occurs in persons who in premorbid can be characterized as "anxious impressionable", hyperemotional.
In a significant part of these patients, in the years preceding the appearance of depersonalization, there was an increase in somatic and mental manifestations of anxiety (increased muscle tone, spastic phenomena and their consequences, vegetative disorders, periods of insomnia, obsessions, more often phobias, etc.). nine0003
3. Depersonalization, as a rule, occurs after intense stress, psychopathologically manifested by the affects of anxiety and fear. Often the stress reaction is caused by a severe psychotraumatic situation, less often it is somatogenic. In endogenous psychoses, depersonalization appears at the height of psychotic anxiety, fear, and, probably, severe vital anguish. The relationship of depersonalization with anxiety is confirmed by the effectiveness of anti-anxiety drugs (leponex, phenazepam, large doses of intravenously administered seduxen) in the treatment of depersonalization at the onset of the disease, stopping anxiety, they lead to a reduction in depersonalization symptoms.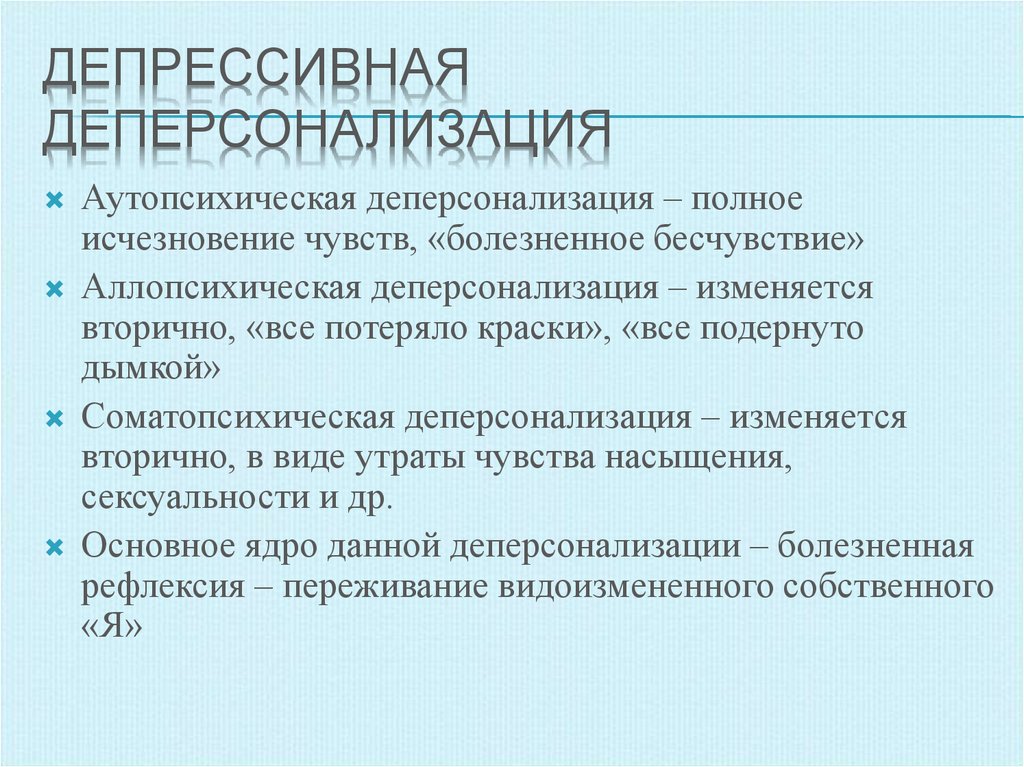 nine0003
nine0003
4. In the debut, depersonalization is usually combined with affective disorders (anxiety, melancholy) and various mental and somatic manifestations of anxiety: phobias, autonomic and muscle (spastic) disorders, which are usually classified as senestopathies.
5. Depersonalization often underlies hypochondriacal fixation and hypochondriacal delusions.
6. In affective psychoses, massive depersonalization leads to prolonged turning of depressive phases and causes their resistance to antidepressant therapy. In schizophrenia, depersonalization in some cases stabilizes the course of psychosis. nine0003
An analysis of the data presented and, in particular, the results of treatment of depersonalization with anti-anxiety drugs shows that two stages are clearly distinguished in the development of depersonalization: the first, initial, is characterized by a close relationship between depersonalization and affect, since it is during this period that anti-anxiety drugs lead to reduction of depersonalization after the removal of anxiety.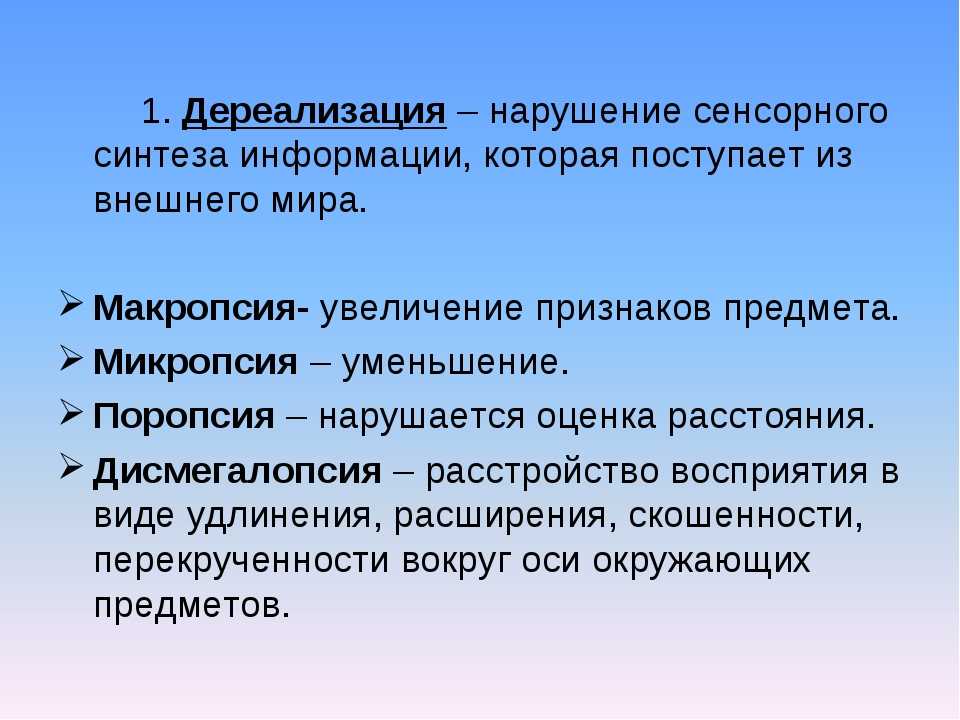 In the clinical picture, somatopsychic depersonalization is expressed, autopsychic depersonalization is accompanied by "mental pain", affective disorders are clearly manifested - anxiety, melancholy, as well as characteristic somatic complaints. nine0003
In the clinical picture, somatopsychic depersonalization is expressed, autopsychic depersonalization is accompanied by "mental pain", affective disorders are clearly manifested - anxiety, melancholy, as well as characteristic somatic complaints. nine0003
The second stage is characterized by a long (many months or many years) existence of depersonalization, the predominance and clinical picture of monotonous autopsychic depersonalization without a feeling of peeling pain. Anxiety and melancholy are either absent or appear extremely erased. Anti-anxiety drugs at the atom stage are ineffective, depersonalization is so divorced from affect that, with phasic psychoses, it can exist not only in the interictal intervals, but also during the period of mania. In other words, at the second stage, depersonalization, as it were, breaks away from affective pathology and acquires an independent, autonomous existence. nine0003
What are depersonalization and derealization and how to detect them
Perhaps at least once in your life you felt that your body does not belong to you or that what is happening around you seems to be happening not to you and not really.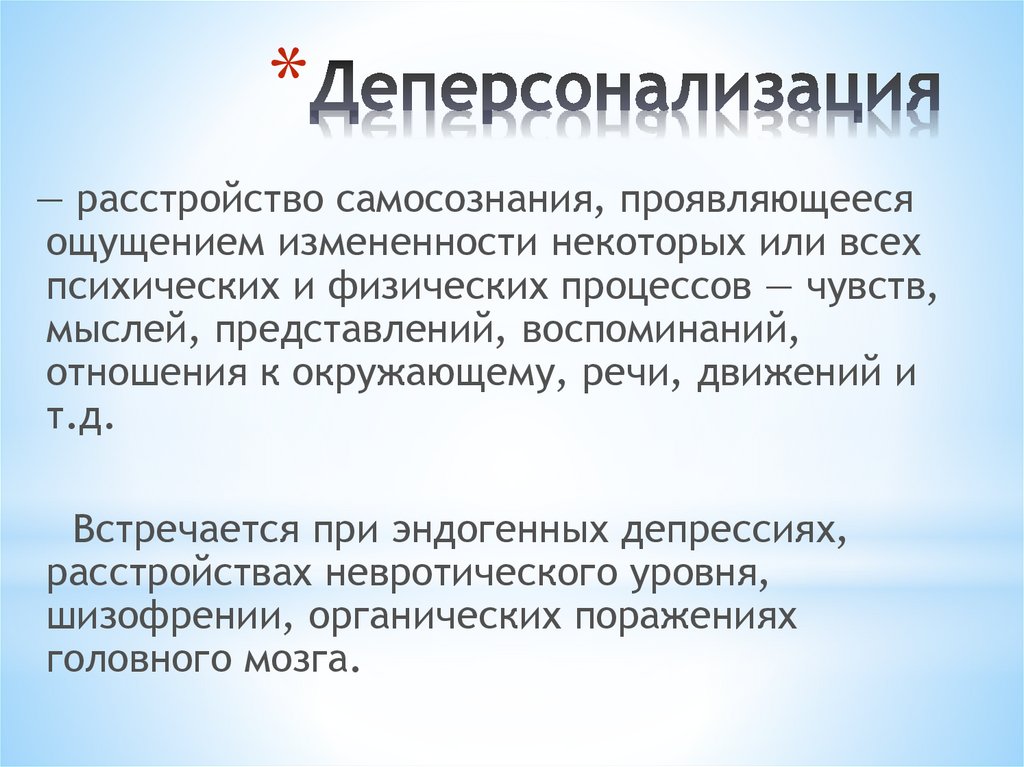 These are quite common in society syndromes of depersonalization and derealization, which can manifest themselves both together and one by one. Due to similarities, the terms are often used together. Zaborona journalist Polina Vernigor figured out what are the signs of these symptoms, when to see a doctor, how to deal with it, and whether it is worth it. nine0097
These are quite common in society syndromes of depersonalization and derealization, which can manifest themselves both together and one by one. Due to similarities, the terms are often used together. Zaborona journalist Polina Vernigor figured out what are the signs of these symptoms, when to see a doctor, how to deal with it, and whether it is worth it. nine0097
What is depersonalization and derealization?
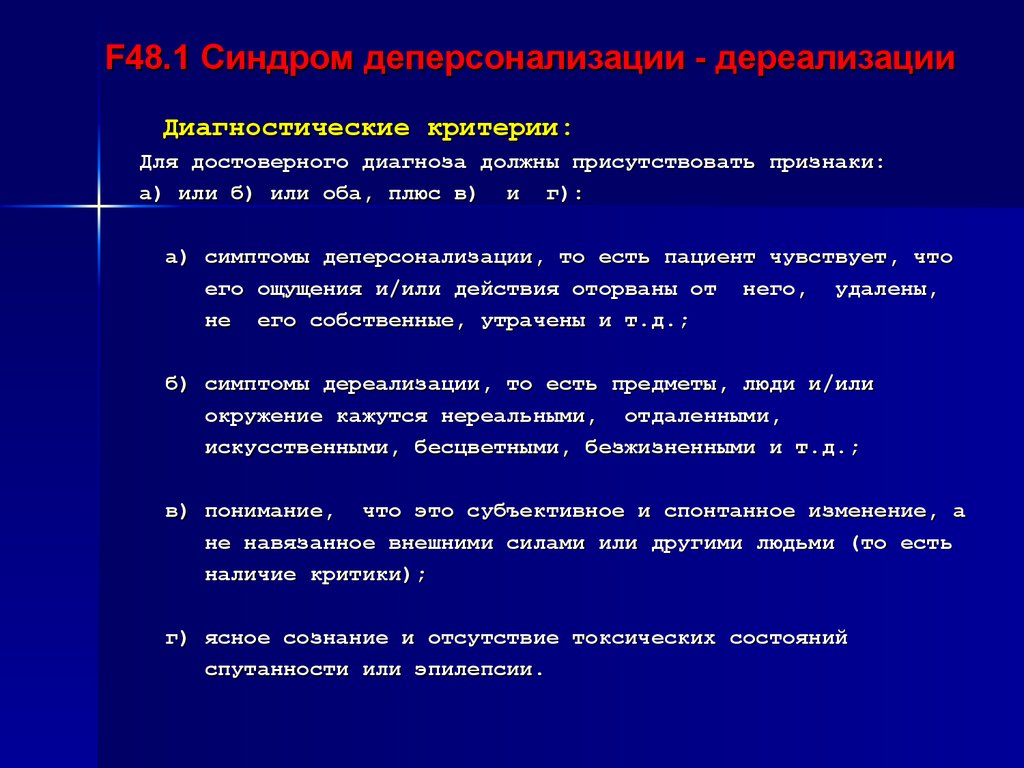
In themselves they are symptoms. Like headache, dizziness or restlessness. But there is a disorder of depersonalization-derealization, which is already a full-fledged psychiatric diagnosis. The disorder itself occurs in only about 2% of the population, but at least 50% of people experience symptoms at least once in their lives.
As symptoms, depersonalization and derealization may indicate mental disorders (panic attack, phobias, post-traumatic stress disorder, depression, schizophrenia, borderline personality disorder, etc.) or neurological (convulsions, brain tumor, post-concussion syndrome, metabolic disorders, migraines, Meniere's disease, etc. ). They can also occur as a reaction to stress or trauma, and are also found in people with alcohol or drug addiction. nine0003
). They can also occur as a reaction to stress or trauma, and are also found in people with alcohol or drug addiction. nine0003
Almost always, these symptoms appear either in late childhood or early adulthood. On average, onset occurs at age 16, and 95% of cases are diagnosed before age 25. The first experience of depersonalization can be scary, as patients fear losing control and separating themselves from the rest of society. Most people with these symptoms misinterpret them as signs of severe psychosis or brain dysfunction. This usually leads to an increase in anxiety and obsessions, which contributes to the worsening of symptoms. nine0003
- Francisco Goya, The Witches Sabbat (1797-98) / Wikimedia
renamed Depersonalization/Derealization Disorder (DPDR).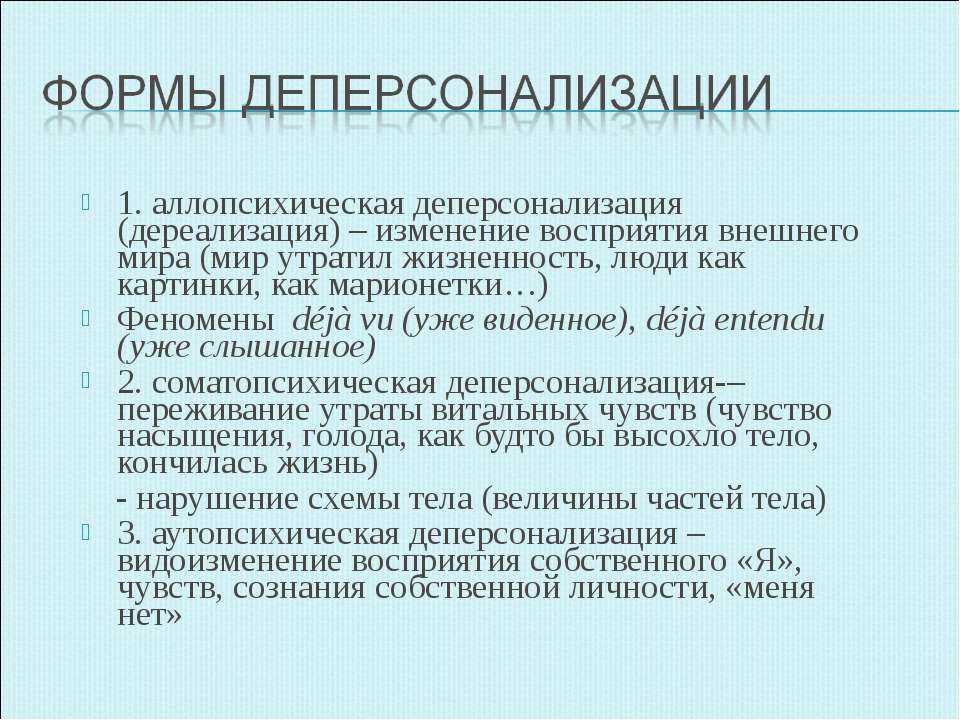 This diagnosis is classified as a dissociative disorder.
This diagnosis is classified as a dissociative disorder.
The latest International Classification of Diseases (ICD-11) reclassified DPDR as a disorder rather than a syndrome as before, and reclassified it as a dissociative disorder from the list of neurotic disorders. The description that is used in ICD-11 is similar to the criteria found in DSM-5. nine0003
How do I know if I have depersonalization or derealization?
You can notice the symptoms yourself, but depersonalization-derealization disorder is a diagnosis that only a doctor can make. No laboratory tests reveal either the symptoms themselves or the disorder. To rule out the physical causes of these conditions, your doctor may order magnetic resonance imaging (MRI), electroencephalography (EEG), x-rays, or a urine test for toxic chemicals. If all these studies turn up nothing, then the cause is most likely mental states. nine0003
Signs of depersonalization:
- a feeling that you are watching your thoughts, feelings, body or parts of it from the outside - for example, as if you are floating in the air above you;
- feels like a robot and/or has no control over your speech and/or movements;
- your body or parts of it seem distorted, deformed, and your head seems to be wrapped in cotton wool;
- emotional or physical numbness of feelings or reactions to the environment;
- your memories lack emotion, and doubts arise whether they are really your memories.
- Henry Fuseli, Nightmare (1781) / Wikimedia
Signs of derealization:
- a feeling of alienation or ignorance of one's surroundings - for example, as if you are living in a movie or in a dream;
- emotional isolation from people close to you, as if a glass wall separates you;
- environment appears distorted, blurry, colorless, two-dimensional or artificial; nine0109
- distortion in the perception of time, for example, recent events are perceived as the distant past;
- curvature of the distance, size and shape of objects.
Depersonalization-derealization disorder can be considered if these symptoms recur frequently and for a long time and are not the result of some other disease or disorder. In any case, if it drains you emotionally or interferes with your life, contact a specialist.
In any case, if it drains you emotionally or interferes with your life, contact a specialist.
What to do about it? nine0100
Very often, both the symptoms and the disorder do not require special treatment and go away on their own. But it depends on their nature and how much they bother you. For many patients, a full recovery is possible, especially if the symptoms are related to another disorder/disease that is being treated, or to stress that is being relieved. In other cases, depersonalization and derealization become more chronic and less noticeable. Even persistent or recurring symptoms can cause only minimal disturbance if you learn to perceive them correctly - for example, to focus on other thoughts or actions. nine0003
- Mikhail Vrubel, "Demon Defeated" (1901-02) / Wikimedia
If we still talk about the treatment of depersonalization-derealization disorder, then psychotherapy helps here.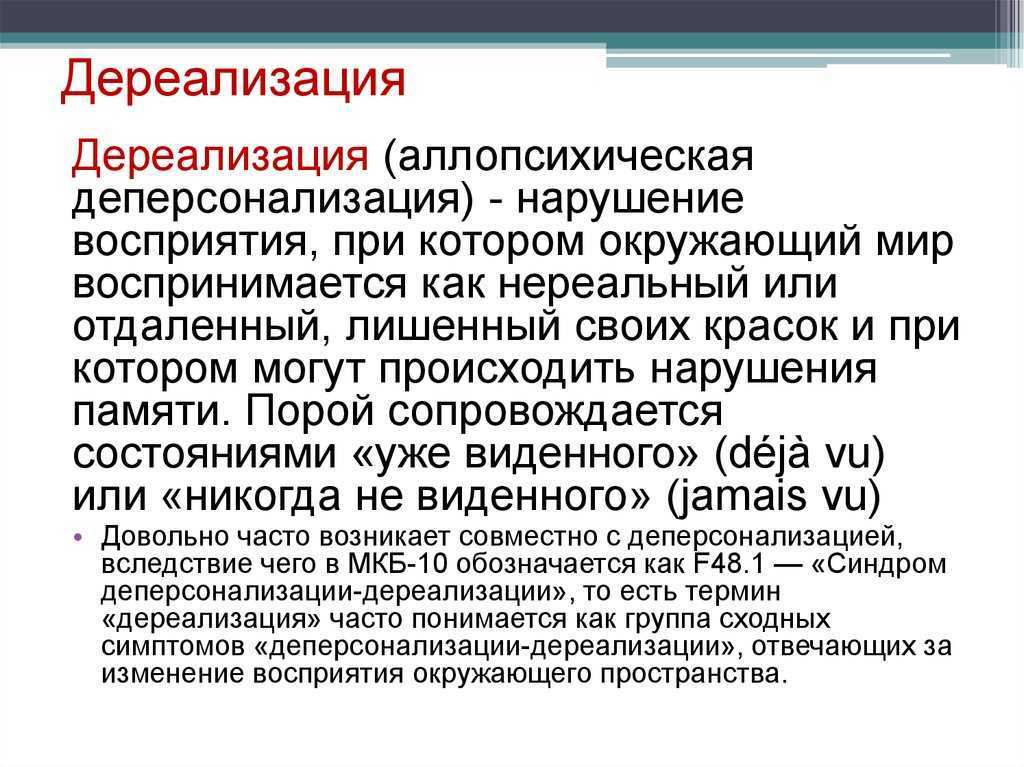 Treatment should take into account all the stresses associated with the onset of the disorder, as well as earlier traumas (eg, childhood abuse or neglect, physical, psychological or sexual abuse, etc.) that may cause patients to have a late onset of depersonalization and/or derealization. . nine0003
Treatment should take into account all the stresses associated with the onset of the disorder, as well as earlier traumas (eg, childhood abuse or neglect, physical, psychological or sexual abuse, etc.) that may cause patients to have a late onset of depersonalization and/or derealization. . nine0003
Different psychotherapeutic methods are successful for different patients. Cognitive techniques can help block intrusive thoughts about an unreal state of being. Behavioral techniques can help patients perform tasks that distract them from depersonalization and derealization. Grounding Techniques uses various senses (such as playing loud music or holding a block of ice) to help patients feel more real in the moment and more connected to the body and surroundings. nine0164 Psychodynamic Therapy helps patients cope with negative feelings, hidden conflicts or experiences that, due to accumulation, provoke symptoms.
Various preparations are also used, but none of them has been clearly proven to be effective.