What is a eating disorder mean
NIMH » Eating Disorders
Overview
There is a commonly held misconception that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that are associated with severe disturbances in people’s eating behaviors and related thoughts and emotions. Preoccupation with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder.
Signs and Symptoms
Anorexia nervosa
Anorexia nervosa is a condition where people avoid food, severely restrict food, or eat very small quantities of only certain foods. They also may weigh themselves repeatedly. Even when dangerously underweight, they may see themselves as overweight.
There are two subtypes of anorexia nervosa: a restrictive subtype and a binge-purge subtype.
Restrictive: People with the restrictive subtype of anorexia nervosa severely limit the amount and type of food they consume.
Binge-Purge: People with the binge-purge subtype of anorexia nervosa also greatly restrict the amount and type of food they consume. In addition, they may have binge-eating and purging episodes—eating large amounts of food in a short time followed by vomiting or using laxatives or diuretics to get rid of what was consumed.
Anorexia nervosa can be fatal. It has an extremely high death (mortality) rate compared with other mental disorders. People with anorexia are at risk of dying from medical complications associated with starvation. Suicide is the second leading cause of death for people diagnosed with anorexia nervosa.
If you or someone you know is in crisis and needs immediate help, call the toll-free National Suicide Prevention Lifeline (NSPL) at 1-800-273-TALK (8255), 24 hours a day, 7 days a week.
Symptoms include:
- Extremely restricted eating
- Extreme thinness (emaciation)
- A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight
- Intense fear of gaining weight
- Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape, or a denial of the seriousness of low body weight
Other symptoms may develop over time, including:
- Thinning of the bones (osteopenia or osteoporosis)
- Mild anemia and muscle wasting and weakness
- Brittle hair and nails
- Dry and yellowish skin
- Growth of fine hair all over the body (lanugo)
- Severe constipation
- Low blood pressure
- Slowed breathing and pulse
- Damage to the structure and function of the heart
- Brain damage
- Multiorgan failure
- Drop in internal body temperature, causing a person to feel cold all the time
- Lethargy, sluggishness, or feeling tired all the time
- Infertility
Bulimia nervosa
Bulimia nervosa is a condition where people have recurrent and frequent episodes of eating unusually large amounts of food and feeling a lack of control over these episodes. This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. People with bulimia nervosa may be slightly underweight, normal weight, or over overweight.
This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. People with bulimia nervosa may be slightly underweight, normal weight, or over overweight.
Symptoms include:
- Chronically inflamed and sore throat
- Swollen salivary glands in the neck and jaw area
- Worn tooth enamel and increasingly sensitive and decaying teeth as a result of exposure to stomach acid
- Acid reflux disorder and other gastrointestinal problems
- Intestinal distress and irritation from laxative abuse
- Severe dehydration from purging of fluids
- Electrolyte imbalance (too low or too high levels of sodium, calcium, potassium, and other minerals) which can lead to stroke or heart attack
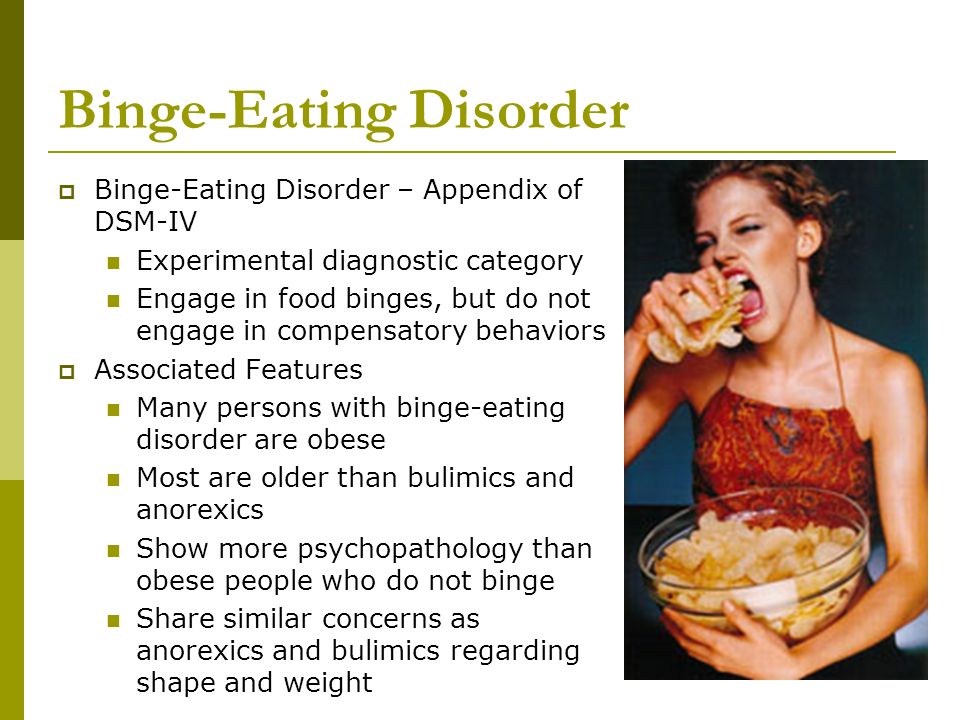
Binge-eating disorder
Binge-eating disorder is a condition where people lose control over their eating and have reoccurring episodes of eating unusually large amounts of food.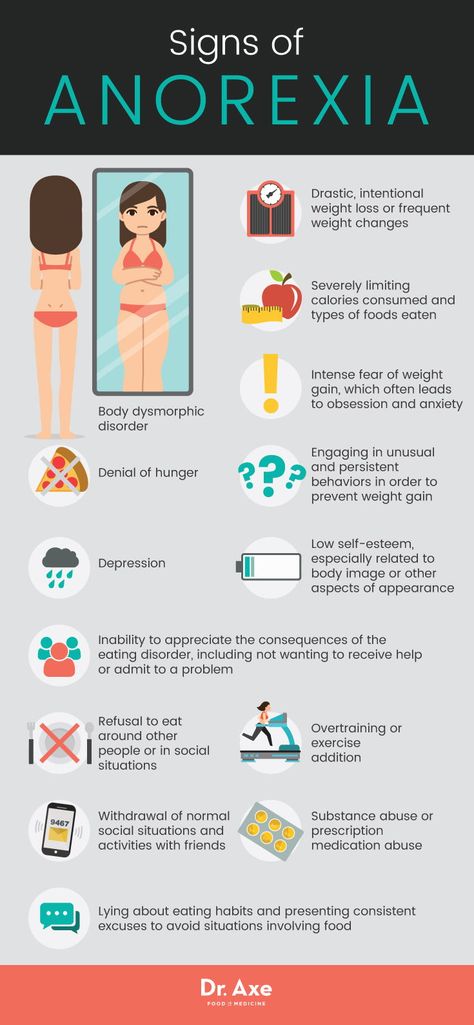 Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. As a result, people with binge-eating disorder often are overweight or obese. Binge-eating disorder is the most common eating disorder in the U.S.
Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. As a result, people with binge-eating disorder often are overweight or obese. Binge-eating disorder is the most common eating disorder in the U.S.
Symptoms include:
- Eating unusually large amounts of food in a specific amount of time, such as a 2-hour period
- Eating even when you're full or not hungry
- Eating fast during binge episodes
- Eating until you're uncomfortably full
- Eating alone or in secret to avoid embarrassment
- Feeling distressed, ashamed, or guilty about your eating
- Frequently dieting, possibly without weight loss
Avoidant restrictive food intake disorder
Avoidant restrictive food intake disorder (ARFID), previously known as selective eating disorder, is a condition where people limit the amount or type of food eaten. Unlike anorexia nervosa, people with ARFID do not have a distorted body image or extreme fear of gaining weight. ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
Symptoms include:
- Dramatic restriction of types or amount of food eaten
- Lack of appetite or interest in food
- Dramatic weight loss
- Upset stomach, abdominal pain, or other gastrointestinal issues with no other known cause
- Limited range of preferred foods that becomes even more limited (“picky eating” that gets progressively worse)
Risk Factors
Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Eating disorders frequently appear during the teen years or young adulthood but may also develop during childhood or later in life.
Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, behavioral, psychological, and social factors. Researchers are using the latest technology and science to better understand eating disorders.
Researchers are using the latest technology and science to better understand eating disorders.
One approach involves the study of human genes. Eating disorders run in families. Researchers are working to identify DNA variations that are linked to the increased risk of developing eating disorders.
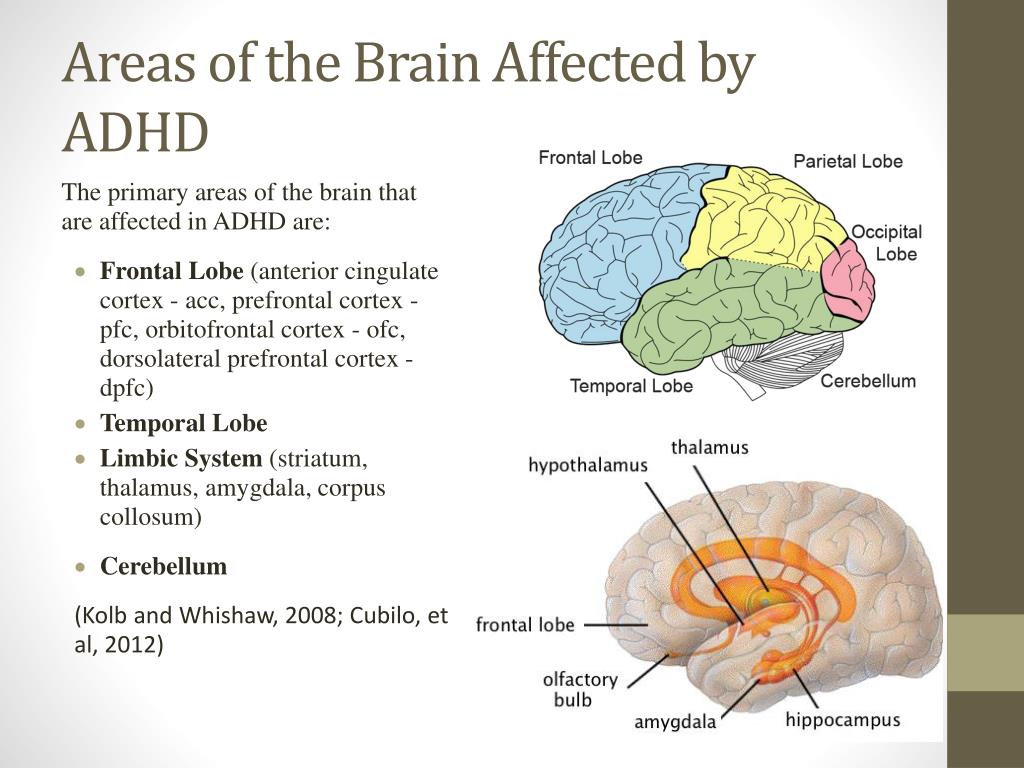
Brain imaging studies are also providing a better understanding of eating disorders. For example, researchers have found differences in patterns of brain activity in women with eating disorders in comparison with healthy women. This kind of research can help guide the development of new means of diagnosis and treatment of eating disorders.
Treatments and Therapies
It is important to seek treatment early for eating disorders. People with eating disorders are at higher risk for suicide and medical complications. People with eating disorders can often have other mental disorders (such as depression or anxiety) or problems with substance use. Complete recovery is possible.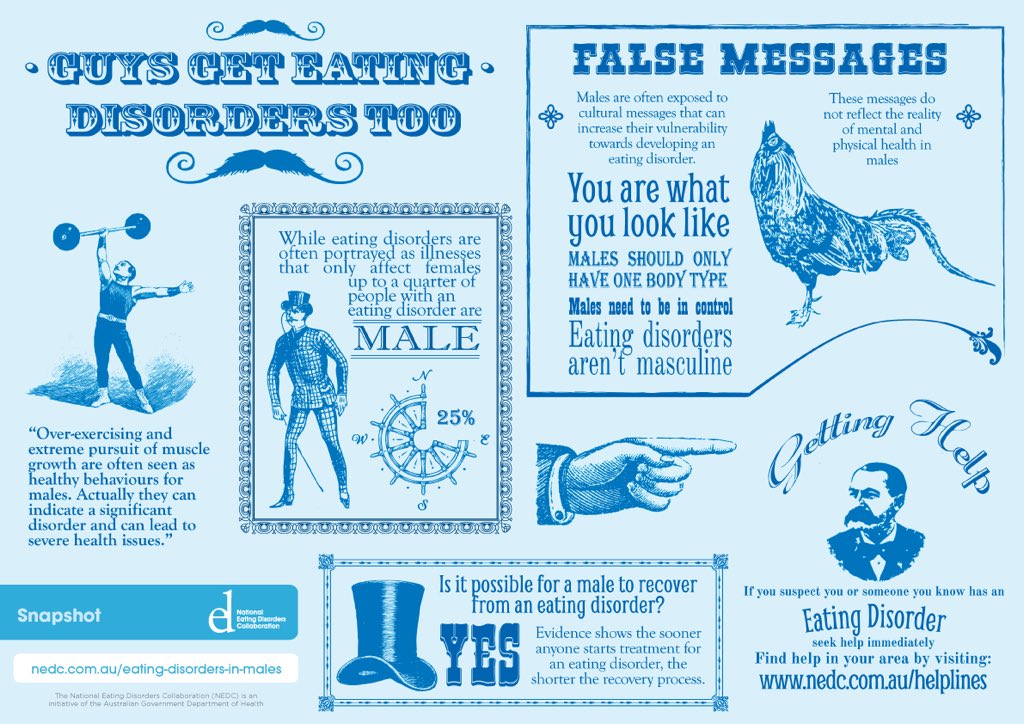
Treatment plans are tailored to individual needs and may include one or more of the following:
- Individual, group, and/or family psychotherapy
- Medical care and monitoring
- Nutritional counseling
- Medications
Psychotherapies
Family-based therapy, a type of psychotherapy where parents of adolescents with anorexia nervosa assume responsibility for feeding their child, appears to be very effective in helping people gain weight and improve eating habits and moods.
To reduce or eliminate binge-eating and purging behaviors, people may undergo cognitive behavioral therapy (CBT), which is another type of psychotherapy that helps a person learn how to identify distorted or unhelpful thinking patterns and recognize and change inaccurate beliefs.
Medications
Evidence also suggests that medications such as antidepressants, antipsychotics, or mood stabilizers may also be helpful for treating eating disorders and other co-occurring illnesses such as anxiety or depression. The Food and Drug Administration’s (FDA) website has the latest information on medication approvals, warnings, and patient information guides.
The Food and Drug Administration’s (FDA) website has the latest information on medication approvals, warnings, and patient information guides.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.
 gov: Current Studies on Eating Disorders: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
gov: Current Studies on Eating Disorders: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Learn More
Free Brochures and Shareable Resources
- Eating Disorders: About More Than Food: A brochure about the common eating disorders anorexia nervosa, bulimia nervosa, and binge-eating disorder, and various approaches to treatment. Also available en español.
- Let’s Talk About Eating Disorders: An infographic with facts that can help shape conversations around eating disorders. Also available in en español.
- Shareable Resources on Eating Disorders: Help support eating disorders awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about eating disorders.
Research and Statistics
- NIMH Eating Disorders Research Program: This program supports research on the etiology, core features, longitudinal course, and assessment of eating disorders.
- Journal Articles: References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Eating Disorders
Multimedia
- Mental Health Minute: Eating Disorders: Take a mental health minute to watch this video on eating disorders.
- Let’s Talk About Eating Disorders with NIMH Grantee Dr. Cynthia Bulik: Learn about the signs, symptoms, treatments, and the latest research on eating disorders.
Last Reviewed: December 2021
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
What is an Eating Disorder?
Eating disorders are serious mental illnesses; they are not a lifestyle choice or a diet gone ‘too far’.
The facts
Eating disorders are serious, complex and potentially life-threatening mental illnesses. They are characterised by disturbances in behaviours, thoughts and attitudes to food, eating, and body weight or shape. Eating disorders have detrimental impacts upon a person’s life and result in serious medical, psychiatric and psychosocial consequences.
Eating disorders are common and increasing in prevalence. There is a lifetime estimated prevalence of 8.4% for women and 2.2% for men.1
Eating disorders do not discriminate and can occur in people of any age, weight, size, shape, gender identity, sexuality, cultural background or socioeconomic group.
Long-term impacts
Eating disorders are associated with serious medical and psychological complications.
A person with an eating disorder may experience long-term impairment to social and functional roles, and the impact may include psychiatric and behavioural problems, medical complications, social isolation, disability and an increased risk of death as a result of medical complications or suicide. Suicide is a major cause of mortality for people with eating disorders. Suicide is up to 31 times more likely to occur for someone with anorexia nervosa and 7.5 times higher for someone with bulimia nervosa than the general population.2
Suicide is a major cause of mortality for people with eating disorders. Suicide is up to 31 times more likely to occur for someone with anorexia nervosa and 7.5 times higher for someone with bulimia nervosa than the general population.2
The impact of an eating disorder is not only felt by the individual, but often by that person’s entire family or circle of support. The impact may lead to caregiver stress, loss of family income, disruption to family relationships and a high suicide risk.
Mortality
The mortality rate for people with eating disorders is up to six times higher than that for people without eating disorders. The increased risk of premature death exists for all types of eating disorders, however people living with anorexia nervosa have the highest mortality rate of all psychiatric conditions due to both psychological and physiological complications.3
Classification of eating disorders
Eating disorders are classified into different types, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Fifth Edition. Classifications are made based on the presenting symptoms and how often these occur, and include:
Classifications are made based on the presenting symptoms and how often these occur, and include:
- Binge eating disorder (BED)
- Other specified feeding or eating disorders (OSFED)
- Bulimia nervosa
- Anorexia nervosa
- Avoidant/restrictive food intake disorder (ARFID)
- Unspecified feeding or eating disorder (UFED)
- Pica
- Rumination disorder
1.Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402-13.
2. Preti A, Rocchi MBL, Sisti D, Camboni M, Miotto P. A comprehensive meta‐analysis of the risk of suicide in eating disorders. Acta Psychiatr Scand. 2011;124(1):6-17.
3. Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724-31.
Eating disorders | Tervisliku toitumise informatsioon
Eating disorders are psychiatric illnesses that damage a person's physical and mental health and impair their overall quality of life - relationships, work and personal development suffer.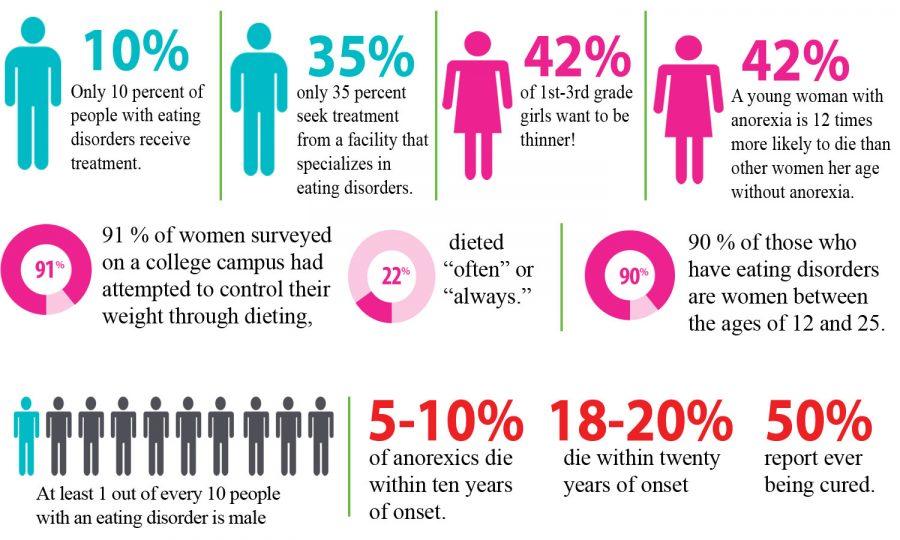
Eating disorders disrupt the connection with one's own body, resulting in highly problematic eating behavior. Weight and body shape are overemphasized, underweight is idealized, and various methods are used to lose weight or prevent weight gain.
Approximately 8% of women and 2% of men will develop an eating disorder during their lifetime. Eating disorders occur in any population, regardless of gender, age, ethnicity, or socioeconomic status. However, they are most common in girls and young women.
Eating disorders are a group of diseases that are distributed differently in different classifications. The most common eating disorders are anorexia ( anorexia nervosa ), bulimia ( bulimia nervosa ) and compulsive overeating ( binge-eating disorder ).
The term "eating disorder" is often erroneously used as a synonym for selective eating disorder, as both are associated with eating disorders. However, the reasons for them are different: an eating disorder is caused by a desire to control weight, while in a selective eating disorder, eating certain foods causes anxiety or fear.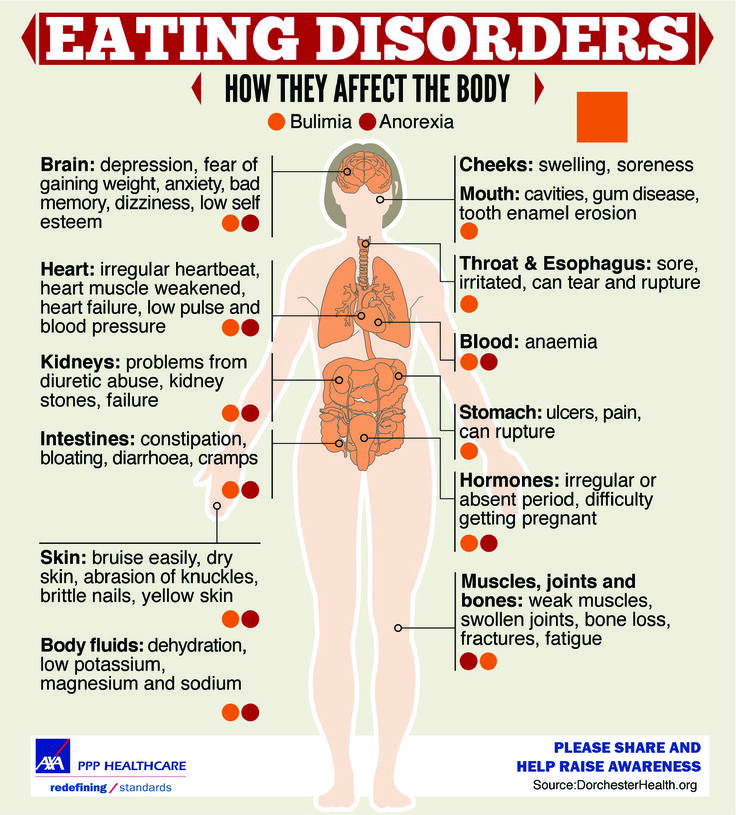
Other eating disorders
Anorexia, bulimia and binge eating disorders are the three most common and well-known eating disorders. However, often not all of the symptoms of a person with an eating disorder correspond to one specific disorder. In such cases, these disorders are referred to as "atypical" or "other eating disorders". A common myth is that in such cases the course of the disease is milder and treatment is treated more lightly. However, this is erroneous, since the name of the disease indicates only its diagnostic criteria, and not the severity or course.
All eating disorders, no matter how they are called or classified, are dangerous conditions that impair quality of life and require treatment.
Causes of Eating Disorders
There is never one single cause of an eating disorder. These are complex diseases, in the development of which a combination of many factors plays an important role. Genetic, biological and environmental factors always play a role.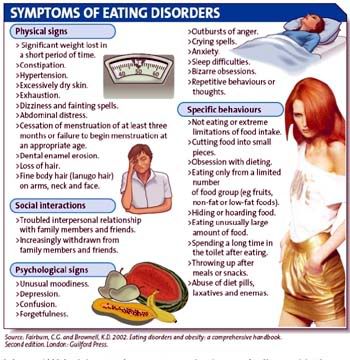 Modern social representations, including the culture of diets and the cult of slimness, contribute to the development of psychological vulnerability, which can become a fertile environment for the formation of eating disorders. Probably for the same reasons, a higher incidence of eating disorders is observed in sports in which weight is of great importance, and among representatives of professions focused on appearance. However, it should be emphasized that browsing social networks or playing a certain sport does not contribute to the development of the disease. There are many factors involved in the development of the disease that are usually beyond the control of the individual. However, it is often more practical and even more important to identify the factors that support the disease, since changing them is associated with better treatment outcomes.
Modern social representations, including the culture of diets and the cult of slimness, contribute to the development of psychological vulnerability, which can become a fertile environment for the formation of eating disorders. Probably for the same reasons, a higher incidence of eating disorders is observed in sports in which weight is of great importance, and among representatives of professions focused on appearance. However, it should be emphasized that browsing social networks or playing a certain sport does not contribute to the development of the disease. There are many factors involved in the development of the disease that are usually beyond the control of the individual. However, it is often more practical and even more important to identify the factors that support the disease, since changing them is associated with better treatment outcomes.
Treatment Options for Eating Disorders
Eating disorders can be life-threatening illnesses with a long and chronic course; they have one of the highest mortality rates of any psychiatric illness.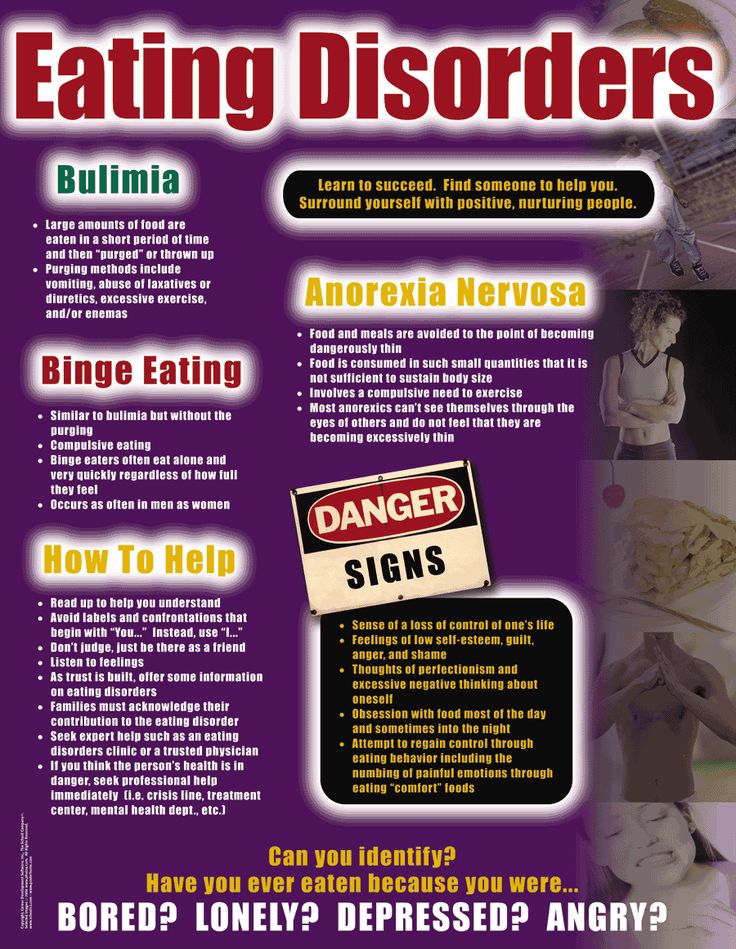 Treating eating disorders is often a lengthy and complex process. However, early intervention is paramount to achieve a good treatment outcome.
Treating eating disorders is often a lengthy and complex process. However, early intervention is paramount to achieve a good treatment outcome.
Diagnosis and treatment of an eating disorder usually begins with the family doctor. Family sisters can provide advice on healthy eating. Psychiatrists are specialists in the diagnosis and treatment of eating disorders as a psychiatric illness. The participation of a clinical psychologist or psychotherapist is also important.
There are two centers in Estonia that specialize in the treatment of eating disorders: the Department of Eating Disorders of the Mental Health Center of the Tallinn Children's Hospital treats children and adolescents, and the Department of Eating Disorders of the Psychiatric Clinic of the Tartu University Hospital treats adolescents and adults.
For more information about eating disorders and advice on what to do if you suspect a loved one has an eating disorder, visit peaasi.ee.
Eating problems
Eating behavior is the totality of our eating habits - our taste preferences, eating habits, diet, etc. Eating behavior depends on many factors - cultural, ethnic, family traditions and values, the characteristics of the upbringing and behavior of family members and the biological characteristics of the body, the standards and standards of norm and beauty that have developed in this society. These habits can change—and often change over time—but not all of these changes will be considered a painful eating disorder. The most obvious unhealthy eating behaviors include anorexia nervosa and bulimia .
Eating behavior depends on many factors - cultural, ethnic, family traditions and values, the characteristics of the upbringing and behavior of family members and the biological characteristics of the body, the standards and standards of norm and beauty that have developed in this society. These habits can change—and often change over time—but not all of these changes will be considered a painful eating disorder. The most obvious unhealthy eating behaviors include anorexia nervosa and bulimia .
Anorexia nervosa (lat. anorexia neurosa) (from other Greek ἀν- - “without-”, “non-” and ὄρεξις - “urge to eat, appetite”) - eating disorder , characterized by deliberate weight loss, caused and / or supported by the patient, in order to lose weight or to prevent weight gain. In anorexia, there is a pathological desire to lose weight, accompanied by a strong fear of obesity. The patient has a distorted perception of their physical form and there is a concern about weight gain, even if this is not actually observed. The overall prevalence of anorexia nervosa is 1.2% among women and 0.29% among men. About 90% of patients with anorexia are girls aged 12-24 years. The remaining 10% includes men and women of more mature age up to menopause.
The causes of anorexia and bulimia are divided into biological, psychological (family influence and internal conflicts), and social (environmental influence: expectations, standards and standards of beauty, social stereotypes, diets). Biological factors - overweight and early onset of the first menstruation. In addition, the cause of the disease may lie in the dysfunction of neurotransmitters regulating eating behavior, such as serotonin, dopamine, norepinephrine. Family factors - More likely to develop an eating disorder in those who have relatives or loved ones suffering from anorexia nervosa, bulimia nervosa or obesity. Having a family member or relative with depression, alcohol or drug abuse or addiction, also increases the risk of an eating disorder. Personality factors - Psychological risk factors include perfectionism and obsessive personality, especially for the restrictive type of anorexia nervosa. Low self-esteem and frustration tolerance, feelings of inferiority, insecurity and inadequacy are risk factors. Cultural factors - these include: living in an industrialized country and an emphasis on harmony (thinness) as an important and significant sign of female beauty. Stressful events, such as the death of a close relative or friend, or sexual or physical abuse, can also be risk factors for developing an eating disorder. The self-esteem of an anorexic patient depends on the figure and weight, and the weight is not assessed objectively, the perception of the norm is reduced inadequately. Losing weight is regarded as an achievement, weight gain is regarded as insufficient self-control. Such views persist even in the last stage (“my height is 170, weight 39kilogram, I want to weigh 30”).
Stages of anorexia
- Dysmorphomanic — thoughts about one's own inferiority and inferiority predominate, due to imaginary fullness.
 Characterized by a depressed mood, anxiety, prolonged examination of oneself in the mirror. During this period, there are the first attempts to limit oneself in food, the search for the ideal diet.
Characterized by a depressed mood, anxiety, prolonged examination of oneself in the mirror. During this period, there are the first attempts to limit oneself in food, the search for the ideal diet. - Anorectic - occurs against the background of persistent starvation. A weight loss of 20-30% is achieved, which is accompanied by euphoria and a tightening of the diet, "to lose even more weight." At the same time, the patient actively convinces himself and those around him that he has no appetite and exhausts himself with great physical exertion. Due to a distorted perception of his body, the patient underestimates the degree of weight loss. The volume of fluid circulating in the body decreases, which causes hypotension and bradycardia. This condition can be accompanied by chilliness, dry skin, and even alopecia (baldness). Another clinical sign is the cessation of the menstrual cycle in women and a decrease in libido and spermatogenesis in men. Adrenal function is also impaired, up to adrenal insufficiency.
 Due to the active decay of tissues, appetite is additionally suppressed by intoxication of the body.
Due to the active decay of tissues, appetite is additionally suppressed by intoxication of the body. - Cachectic — period of irreversible dystrophy of internal organs. Comes in 1.5-2 years. During this period, weight loss reaches 50 percent or more of its mass. In this case, protein-free edema occurs, the water-electrolyte balance is disturbed, and the level of potassium in the body sharply decreases. This step is usually irreversible. Dystrophic changes lead to irreversible inhibition of the functions of all systems and organs and death.
Bulimia nervosa (from other Greek βοῦς, bus - "bull" and other Greek λῑμός, limos - "hunger") (literally bullish hunger, kinorexia) - an eating disorder characterized by a sharp increase in appetite (wolfish appetite), usually coming in the form of an attack and accompanied by a feeling of excruciating hunger, general weakness, sometimes pain in the epigastric region. This violation of eating behavior is manifested mainly by recurring bouts of gluttony, food "spree". To avoid obesity, most patients with bulimia at the end of the "revelry" resort to one or another method of cleansing the stomach and intestines, artificially inducing vomiting in themselves or taking laxatives and diuretics. Others use excessive exercise or intermittent fasting. Like those with anorexia nervosa, most bulimics are young women, usually in their late teens and early 30s. Bulimics often look normal and healthy on the outside, but are usually overly demanding of themselves and others, prone to loneliness and depression. They tend to raise standards and lower self-esteem. Their life is almost entirely focused on food, their own figure and the need to hide their "mania" from others. Even when working or attending school, they usually shun society. Bulimia can be indicated by depression, poor sleep, talk of suicide, excessive fear of gaining weight, and frantic grocery shopping. Typically, bulimics have "bouts" about 11 times a week, but the frequency of such attacks varies from 1-2 per week to 4-5 per day.
To avoid obesity, most patients with bulimia at the end of the "revelry" resort to one or another method of cleansing the stomach and intestines, artificially inducing vomiting in themselves or taking laxatives and diuretics. Others use excessive exercise or intermittent fasting. Like those with anorexia nervosa, most bulimics are young women, usually in their late teens and early 30s. Bulimics often look normal and healthy on the outside, but are usually overly demanding of themselves and others, prone to loneliness and depression. They tend to raise standards and lower self-esteem. Their life is almost entirely focused on food, their own figure and the need to hide their "mania" from others. Even when working or attending school, they usually shun society. Bulimia can be indicated by depression, poor sleep, talk of suicide, excessive fear of gaining weight, and frantic grocery shopping. Typically, bulimics have "bouts" about 11 times a week, but the frequency of such attacks varies from 1-2 per week to 4-5 per day. Bulimia can have severe health consequences. Frequent vomiting causes irritation of the pharynx and esophagus, as well as destruction of tooth enamel by acid from the stomach. Sometimes there is a cessation of menstruation. The most serious effects are associated with dehydration and loss of electrolytes (sodium and potassium) due to vomiting and diarrhea caused by laxatives.
Bulimia can have severe health consequences. Frequent vomiting causes irritation of the pharynx and esophagus, as well as destruction of tooth enamel by acid from the stomach. Sometimes there is a cessation of menstruation. The most serious effects are associated with dehydration and loss of electrolytes (sodium and potassium) due to vomiting and diarrhea caused by laxatives.
The treatment of anorexia and bulimia requires the combined efforts of doctors from different specialties. Integral components of treatment are alimentary rehabilitation and measures aimed at restoring body weight. Nutritional rehabilitation programs typically use emotional care and support, as well as a variety of behavioral psychotherapy techniques that involve a combination of reinforcing stimuli that combines exercise, a strict exercise regimen and rest, in addition, prioritizing target body weight, desirable behaviors and informative feedback. The nutritional management of patients with anorexia nervosa is an important part of their treatment. In chronic starvation, the need for energy is reduced. Therefore, weight gain can be promoted by initially providing a relatively low caloric intake and then gradually increasing it. There are several schemes for increasing nutrition, the observance of which guarantees the absence of side effects and complications in the form of edema, impaired mineral metabolism, and damage to the digestive organs. Supportive psychotropic drugs are often used in the treatment of anorexia and bulimia, in particular antidepressants and atypical antipsychotics . Plays an important role, individual psychotherapy ; it should be carried out by a specialist who inspires confidence in the patient. We all come from childhood. In people with eating problems, the upbringing and family situation is often quite typical. Lack of parental attention and approval, or a “contrast shower” due to sudden changes in parental mood, love and affection, forms a “complex” and attitude in the child: I must earn love! Serving her, the child becomes a perfectionist, demanding first of all to himself: everything must be perfect, from grades at school to appearance, figures .
The nutritional management of patients with anorexia nervosa is an important part of their treatment. In chronic starvation, the need for energy is reduced. Therefore, weight gain can be promoted by initially providing a relatively low caloric intake and then gradually increasing it. There are several schemes for increasing nutrition, the observance of which guarantees the absence of side effects and complications in the form of edema, impaired mineral metabolism, and damage to the digestive organs. Supportive psychotropic drugs are often used in the treatment of anorexia and bulimia, in particular antidepressants and atypical antipsychotics . Plays an important role, individual psychotherapy ; it should be carried out by a specialist who inspires confidence in the patient. We all come from childhood. In people with eating problems, the upbringing and family situation is often quite typical. Lack of parental attention and approval, or a “contrast shower” due to sudden changes in parental mood, love and affection, forms a “complex” and attitude in the child: I must earn love! Serving her, the child becomes a perfectionist, demanding first of all to himself: everything must be perfect, from grades at school to appearance, figures .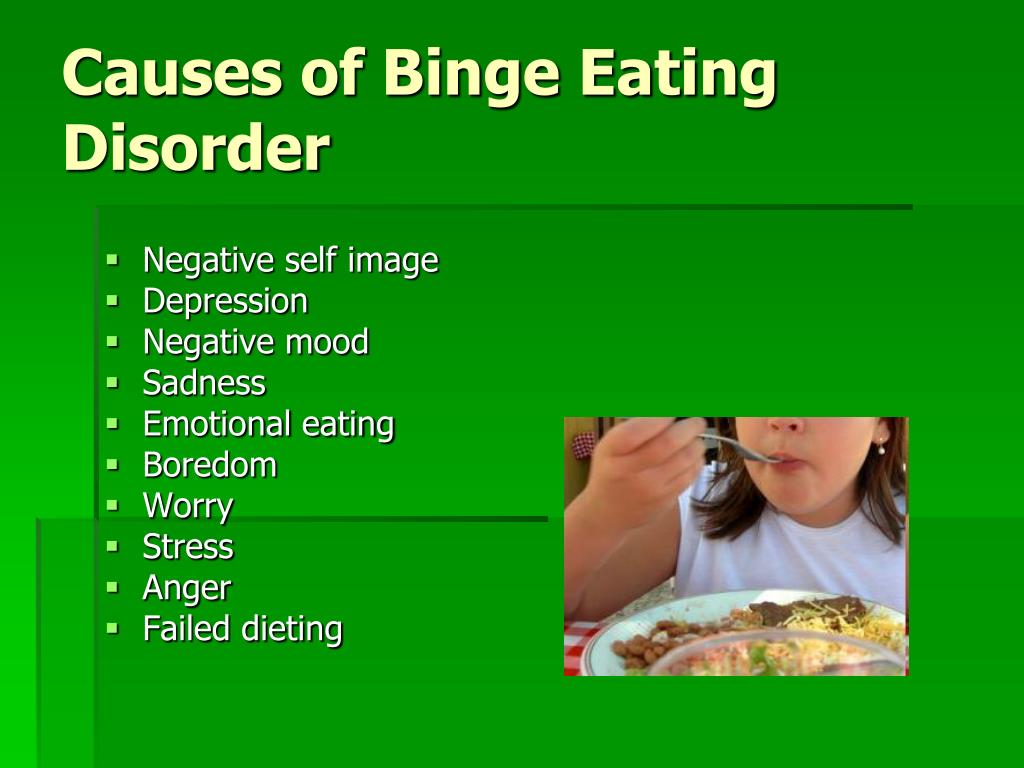 .. Often parents believe that instead of praise it is better to spur their daughter to success by comparisons. "Katya studies better! And Masha is so neat!" the child hears. Mothers, speaking in this way, believe that they come from the best of intentions and will benefit their child by this, they want to give an incentive for great accomplishments and improvement of their child. So, with mother's milk, the stereotype is sown that one should strive to be the first, the very best. The most interesting, smart, beautiful! The most neat, elegant and well-dressed! Unable to distinguish between emotional hunger and physiological hunger, a person easily switches from psychological problems to bodily ones, jams experiences in the literal and figurative sense of the word. Instead of friends, rest and entertainment - the first, second, third and compote. The lack of human communication, love and support is filled with cakes, pastries, favorite dishes and just what turns up under a hot hand and an irritated stomach.
.. Often parents believe that instead of praise it is better to spur their daughter to success by comparisons. "Katya studies better! And Masha is so neat!" the child hears. Mothers, speaking in this way, believe that they come from the best of intentions and will benefit their child by this, they want to give an incentive for great accomplishments and improvement of their child. So, with mother's milk, the stereotype is sown that one should strive to be the first, the very best. The most interesting, smart, beautiful! The most neat, elegant and well-dressed! Unable to distinguish between emotional hunger and physiological hunger, a person easily switches from psychological problems to bodily ones, jams experiences in the literal and figurative sense of the word. Instead of friends, rest and entertainment - the first, second, third and compote. The lack of human communication, love and support is filled with cakes, pastries, favorite dishes and just what turns up under a hot hand and an irritated stomach. Family and friends usually do not understand the essence of the problem and experiences of a person with an eating disorder. They say: "Pull yourself together! Eat like all normal people!". This does not give the desired effect. Moreover, it drives a person with a problem of eating behavior even more into a psychological impasse and nervous tension. Great successes in the treatment of eating disorders are demonstrated by cognitive-behavioral psychotherapy and family therapy. Pharmacotherapy is at best an adjunct to other types of psychotherapy. Psychotherapy is aimed at correcting distorted cognitive formations in the form of perceiving oneself as fat, determining one's own value solely depending on the image of one's own body and a deep sense of inefficiency and inferiority. One of the elements of cognitive therapy is cognitive restructuring . In this approach, patients must find specific negative thoughts, list the evidence for those thoughts and list the evidence that refutes those thoughts, draw a valid conclusion, and use it to guide their own behavior.
Family and friends usually do not understand the essence of the problem and experiences of a person with an eating disorder. They say: "Pull yourself together! Eat like all normal people!". This does not give the desired effect. Moreover, it drives a person with a problem of eating behavior even more into a psychological impasse and nervous tension. Great successes in the treatment of eating disorders are demonstrated by cognitive-behavioral psychotherapy and family therapy. Pharmacotherapy is at best an adjunct to other types of psychotherapy. Psychotherapy is aimed at correcting distorted cognitive formations in the form of perceiving oneself as fat, determining one's own value solely depending on the image of one's own body and a deep sense of inefficiency and inferiority. One of the elements of cognitive therapy is cognitive restructuring . In this approach, patients must find specific negative thoughts, list the evidence for those thoughts and list the evidence that refutes those thoughts, draw a valid conclusion, and use it to guide their own behavior.