How common is narcolepsy
Narcolepsy Fact Sheet | National Institute of Neurological Disorders and Stroke
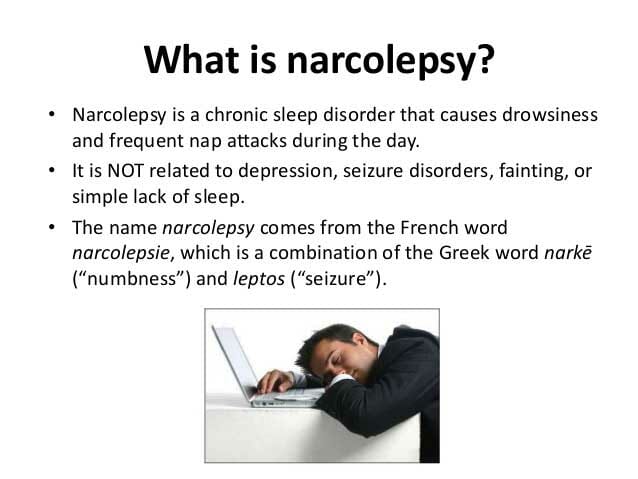
What is narcolepsy?
Who gets narcolepsy?
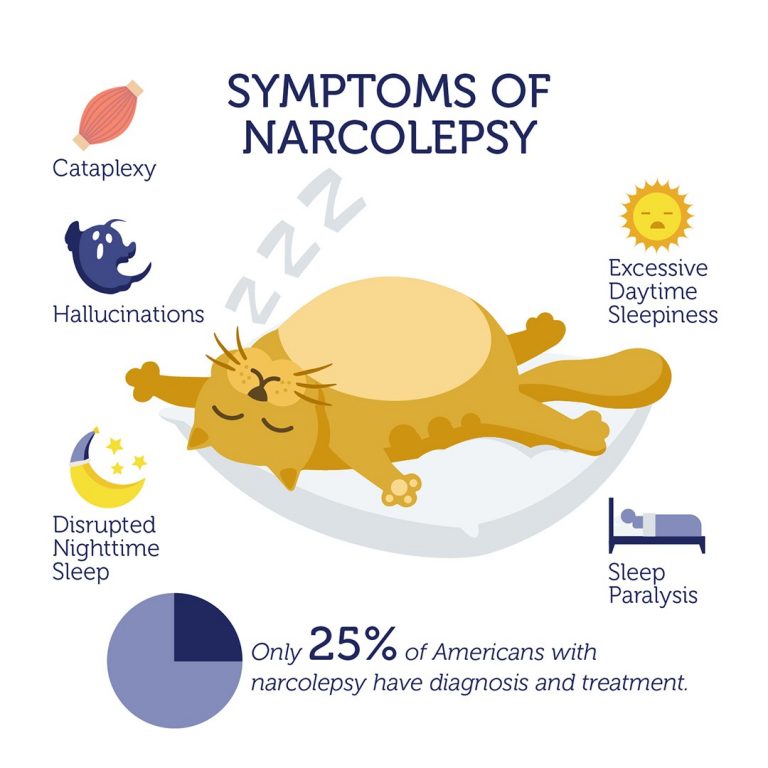
What are the symptoms?
What are the types of narcolepsy?
What causes narcolepsy?
How is narcolepsy diagnosed?
What treatments are available?
What behavioral strategies help people cope with symptoms?
What is the state of the science involving narcolepsy?
What research is being done?
How can I help research?
Where can I get more information?
What is narcolepsy?
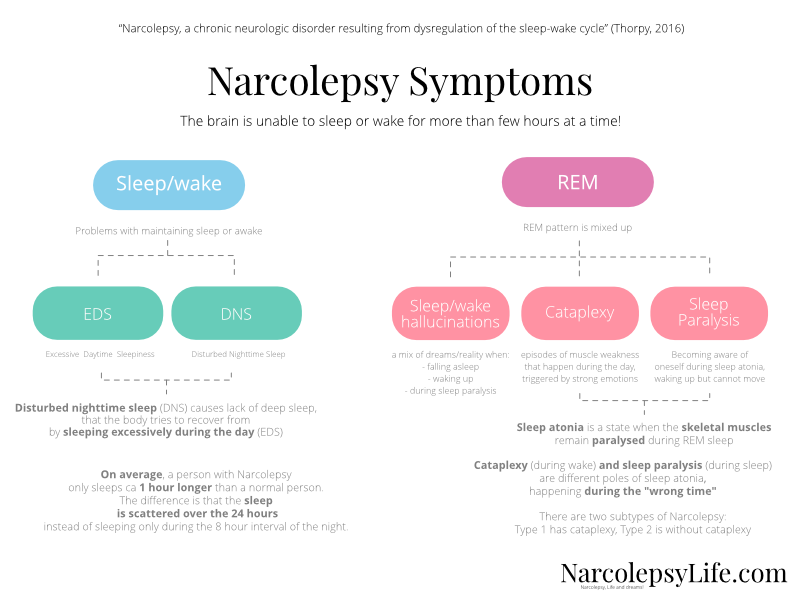
Narcolepsy is a chronic neurological disorder that affects the brain’s ability to control sleep-wake cycles. People with narcolepsy may feel rested after waking, but then feel very sleepy throughout much of the day. Many individuals with narcolepsy also experience uneven and interrupted sleep that can involve waking up frequently during the night.
Narcolepsy can greatly affect daily activities. People may unwillingly fall asleep even if they are in the middle of an activity like driving, eating, or talking. Other symptoms may include sudden muscle weakness while awake that makes a person go limp or unable to move (cataplexy), vivid dream-like images or hallucinations, and total paralysis just before falling asleep or just after waking up (sleep paralysis).
In a normal sleep cycle, a person enters rapid eye movement (REM) sleep after about 60 to 90 minutes. Dreams occur during REM sleep, and the brain keeps muscles limp during this sleep stage, which prevents people from acting out their dreams. People with narcolepsy frequently enter REM sleep rapidly, within 15 minutes of falling asleep. Also, the muscle weakness or dream activity of REM sleep can occur during wakefulness or be absent during sleep. This helps explain some symptoms of narcolepsy.
If left undiagnosed or untreated, narcolepsy can interfere with psychological, social, and cognitive function and development and can inhibit academic, work, and social activities.
Who gets narcolepsy?
Narcolepsy affects both males and females equally.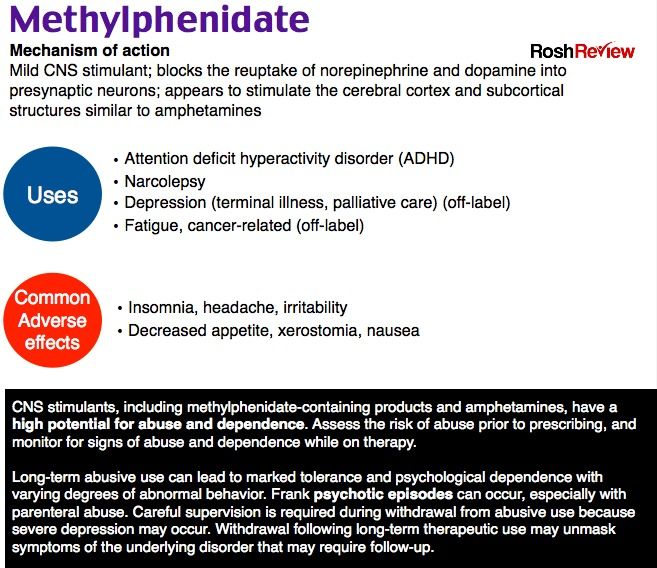 Symptoms often start in childhood, adolescence, or young adulthood (ages 7 to 25), but can occur at any time in life. It is estimated that anywhere from 135,000 to 200,000 people in the United States have narcolepsy. However, since this condition often goes undiagnosed, the number may be higher. Since people with narcolepsy are often misdiagnosed with other conditions, such as psychiatric disorders or emotional problems, it can take years for someone to get the proper diagnosis.
Symptoms often start in childhood, adolescence, or young adulthood (ages 7 to 25), but can occur at any time in life. It is estimated that anywhere from 135,000 to 200,000 people in the United States have narcolepsy. However, since this condition often goes undiagnosed, the number may be higher. Since people with narcolepsy are often misdiagnosed with other conditions, such as psychiatric disorders or emotional problems, it can take years for someone to get the proper diagnosis.
What are the symptoms?
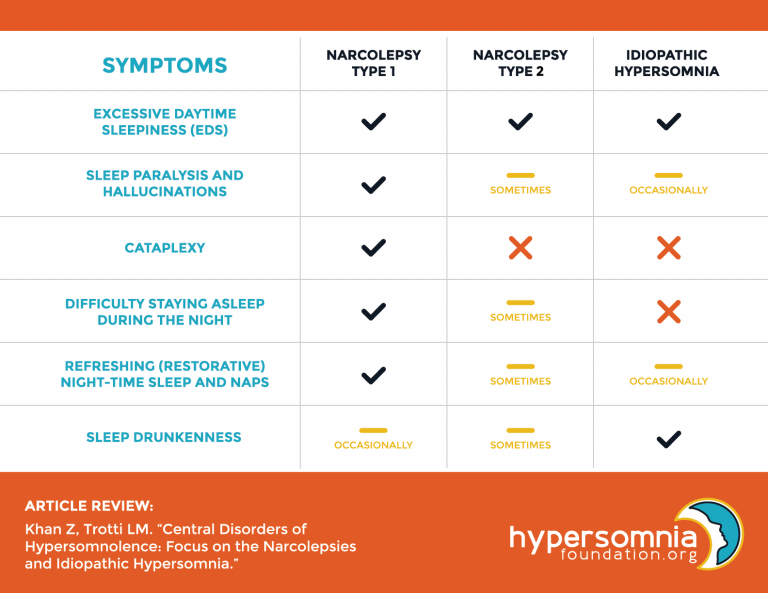
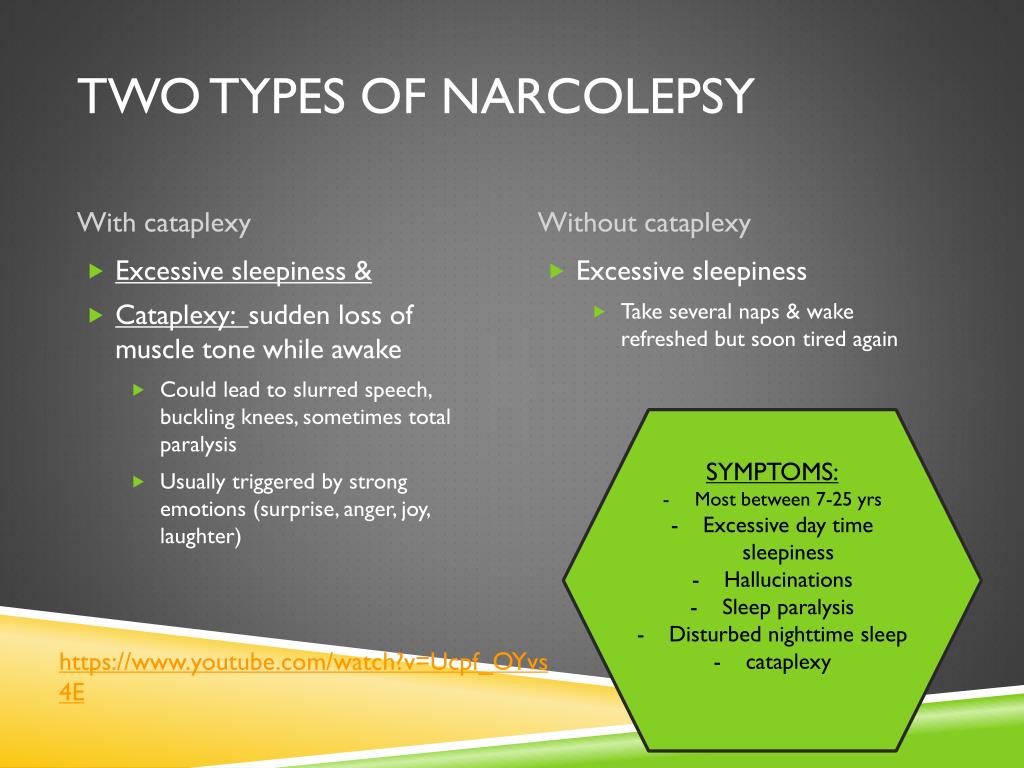
Narcolepsy is a lifelong problem, but it does not usually worsen as the person ages. Symptoms can partially improve over time, but they will never disappear completely. The most typical symptoms are excessive daytime sleepiness, cataplexy, sleep paralysis, and hallucinations. Though all have excessive daytime sleepiness, only 10 to 25 percent of affected individuals will experience all of the other symptoms during the course of their illness.
- Excessive daytime sleepiness (EDS).
 All individuals with narcolepsy have EDS, and it is often the most obvious symptom. EDS is characterized by persistent sleepiness, regardless of how much sleep an individual gets at night. However, sleepiness in narcolepsy is more like a “sleep attack”, where an overwhelming sense of sleepiness comes on quickly. In between sleep attacks, individuals have normal levels of alertness, particularly if doing activities that keep their attention.
All individuals with narcolepsy have EDS, and it is often the most obvious symptom. EDS is characterized by persistent sleepiness, regardless of how much sleep an individual gets at night. However, sleepiness in narcolepsy is more like a “sleep attack”, where an overwhelming sense of sleepiness comes on quickly. In between sleep attacks, individuals have normal levels of alertness, particularly if doing activities that keep their attention. - Cataplexy. This sudden loss of muscle tone while a person is awake leads to weakness and a loss of voluntary muscle control. It is often triggered by sudden, strong emotions such as laughter, fear, anger, stress, or excitement. The symptoms of cataplexy may appear weeks or even years after the onset of EDS. Some people may only have one or two attacks in a lifetime, while others may experience many attacks a day. In about 10 percent of cases of narcolepsy, cataplexy is the first symptom to appear and can be misdiagnosed as a seizure disorder.
 Attacks may be mild and involve only a momentary sense of minor weakness in a limited number of muscles, such as a slight drooping of the eyelids. The most severe attacks result in a total body collapse during which individuals are unable to move, speak, or keep their eyes open. But even during the most severe episodes, people remain fully conscious, a characteristic that distinguishes cataplexy from fainting or seizure disorders. The loss of muscle tone during cataplexy resembles paralysis of muscle activity that naturally occurs during REM sleep. Episodes last a few minutes at most and resolve almost instantly on their own. While scary, the episodes are not dangerous as long as the individual finds a safe place in which to collapse.
Attacks may be mild and involve only a momentary sense of minor weakness in a limited number of muscles, such as a slight drooping of the eyelids. The most severe attacks result in a total body collapse during which individuals are unable to move, speak, or keep their eyes open. But even during the most severe episodes, people remain fully conscious, a characteristic that distinguishes cataplexy from fainting or seizure disorders. The loss of muscle tone during cataplexy resembles paralysis of muscle activity that naturally occurs during REM sleep. Episodes last a few minutes at most and resolve almost instantly on their own. While scary, the episodes are not dangerous as long as the individual finds a safe place in which to collapse.
- Sleep paralysis. The temporary inability to move or speak while falling asleep or waking up usually lasts only a few seconds or minutes and is similar to REM-induced inhibitions of voluntary muscle activity. Sleep paralysis resembles cataplexy except it occurs at the edges of sleep.
 As with cataplexy, people remain fully conscious. Even when severe, cataplexy and sleep paralysis do not result in permanent dysfunction—after episodes end, people rapidly recover their full capacity to move and speak.
As with cataplexy, people remain fully conscious. Even when severe, cataplexy and sleep paralysis do not result in permanent dysfunction—after episodes end, people rapidly recover their full capacity to move and speak. - Hallucinations. Very vivid and sometimes frightening images can accompany sleep paralysis and usually occur when people are falling asleep or waking up. Most often the content is primarily visual, but any of the other senses can be involved.
Additional symptoms of narcolepsy include:
- Fragmented sleep and insomnia. While individuals with narcolepsy are very sleepy during the day, they usually also experience difficulties staying asleep at night. Sleep may be disrupted by insomnia, vivid dreaming, sleep apnea, acting out while dreaming, and periodic leg movements.
- Automatic behaviors. Individuals with narcolepsy may experience temporary sleep episodes that can be very brief, lasting no more than seconds at a time.
 A person falls asleep during an activity (e.g., eating, talking) and automatically continues the activity for a few seconds or minutes without conscious awareness of what they are doing. This happens most often while people are engaged in habitual activities such as typing or driving. They cannot recall their actions, and their performance is almost always impaired. Their handwriting may, for example, degenerate into an illegible scrawl, or they may store items in bizarre locations and then forget where they placed them. If an episode occurs while driving, individuals may get lost or have an accident. People tend to awaken from these episodes feeling refreshed, finding that their drowsiness and fatigue has temporarily subsided.
A person falls asleep during an activity (e.g., eating, talking) and automatically continues the activity for a few seconds or minutes without conscious awareness of what they are doing. This happens most often while people are engaged in habitual activities such as typing or driving. They cannot recall their actions, and their performance is almost always impaired. Their handwriting may, for example, degenerate into an illegible scrawl, or they may store items in bizarre locations and then forget where they placed them. If an episode occurs while driving, individuals may get lost or have an accident. People tend to awaken from these episodes feeling refreshed, finding that their drowsiness and fatigue has temporarily subsided.
What are the types of narcolepsy?
There are two major types of narcolepsy:
- Type 1 narcolepsy (previously termed narcolepsy with cataplexy). This diagnosis is based on the individual either having low levels of a brain hormone (hypocretin) or reporting cataplexy and having excessive daytime sleepiness on a special nap test.

- Type 2 narcolepsy (previously termed narcolepsy without cataplexy). People with this condition experience excessive daytime sleepiness but usually do not have muscle weakness triggered by emotions. They usually also have less severe symptoms and have normal levels of the brain hormone hypocretin.
A condition known as secondary narcolepsy can result from an injury to the hypothalamus, a region deep in the brain that helps regulate sleep. In addition to experiencing the typical symptoms of narcolepsy, individuals may also have severe neurological problems and sleep for long periods (more than 10 hours) each night.
What causes narcolepsy?
Narcolepsy may have several causes. Nearly all people with narcolepsy who have cataplexy have extremely low levels of the naturally occurring chemical hypocretin, which promotes wakefulness and regulates REM sleep. Hypocretin levels are usually normal in people who have narcolepsy without cataplexy.
Although the cause of narcolepsy is not completely understood, current research suggests that narcolepsy may be the result of a combination of factors working together to cause a lack of hypocretin. These factors include:
- Autoimmune disorders. When cataplexy is present, the cause is most often the loss of brain cells that produce hypocretin. Although the reason for this cell loss is unknown, it appears to be linked to abnormalities in the immune system. Autoimmune disorders occur when the body's immune system turns against itself and mistakenly attacks healthy cells or tissue. Researchers believe that in individuals with narcolepsy, the body’s immune system selectively attacks the hypocretin-containing brain cells because of a combination of genetic and environmental factors.
- Family history. Most cases of narcolepsy are sporadic, meaning the disorder occurs in individuals with no known family history. However, clusters in families sometimes occur—up to 10 percent of individuals diagnosed with narcolepsy with cataplexy report having a close relative with similar symptoms.
- Brain injuries. Rarely, narcolepsy results from traumatic injury to parts of the brain that regulate wakefulness and REM sleep or from tumors and other diseases in the same regions.
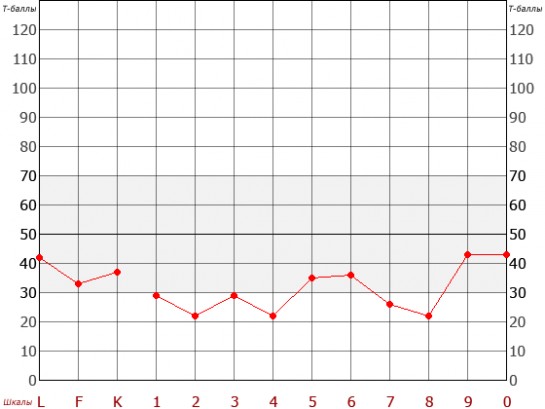
How is narcolepsy diagnosed?
A clinical examination and detailed medical history are essential for diagnosis and treatment of narcolepsy. Individuals may be asked by their doctor to keep a sleep journal noting the times of sleep and symptoms over a one- to two-week period. Although none of the major symptoms are exclusive to narcolepsy, cataplexy is the most specific symptom and occurs in almost no other diseases.
A physical exam can rule out or identify other neurological conditions that may be causing the symptoms. Two specialized tests, which can be performed in a sleep disorders clinic, are required to establish a diagnosis of narcolepsy:
- Polysomnogram (PSG or sleep study). The PSG is an overnight recording of brain and muscle activity, breathing, and eye movements.
 A PSG can help reveal whether REM sleep occurs early in the sleep cycle and if an individual's symptoms result from another condition such as sleep apnea.
A PSG can help reveal whether REM sleep occurs early in the sleep cycle and if an individual's symptoms result from another condition such as sleep apnea. - Multiple sleep latency test (MSLT). The MSLT assesses daytime sleepiness by measuring how quickly a person falls asleep and whether they enter REM sleep. On the day after the PSG, an individual is asked to take five short naps separated by two hours over the course of a day. If an individual falls asleep in less than 8 minutes on average over the five naps, this indicates excessive daytime sleepiness. However, individuals with narcolepsy also have REM sleep start abnormally quickly. If REM sleep happens within 15 minutes at least two times out of the five naps and the sleep study the night before, this is likely an abnormality caused by narcolepsy.
Occasionally, it may be helpful to measure the level of hypocretin in the fluid that surrounds the brain and spinal cord. To perform this test, a doctor will withdraw a sample of the cerebrospinal fluid using a lumbar puncture (also called a spinal tap) and measure the level of hypocretin-1.
 In the absence of other serious medical conditions, low hypocretin-1 levels almost certainly indicate type 1 narcolepsy.
In the absence of other serious medical conditions, low hypocretin-1 levels almost certainly indicate type 1 narcolepsy.
What treatments are available?
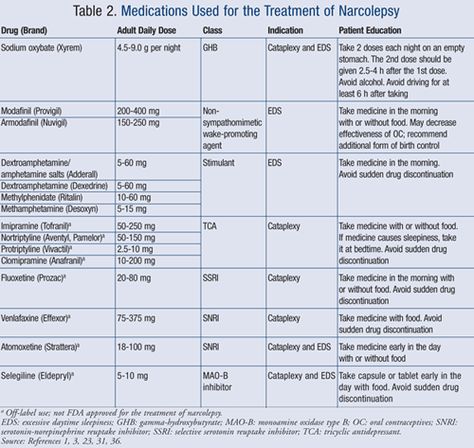
Although there is no cure for narcolepsy, some of the symptoms can be treated with medicines and lifestyle changes. When cataplexy is present, the loss of hypocretin is believed to be irreversible and lifelong. Excessive daytime sleepiness and cataplexy can be controlled in most individuals with medications.
Medications
- Modafinil. The initial line of treatment is usually a central nervous system stimulant such as modafinil. Modafinil is usually prescribed first because it is less addictive and has fewer side effects than older stimulants. For most people these drugs are generally effective at reducing daytime drowsiness and improving alertness.
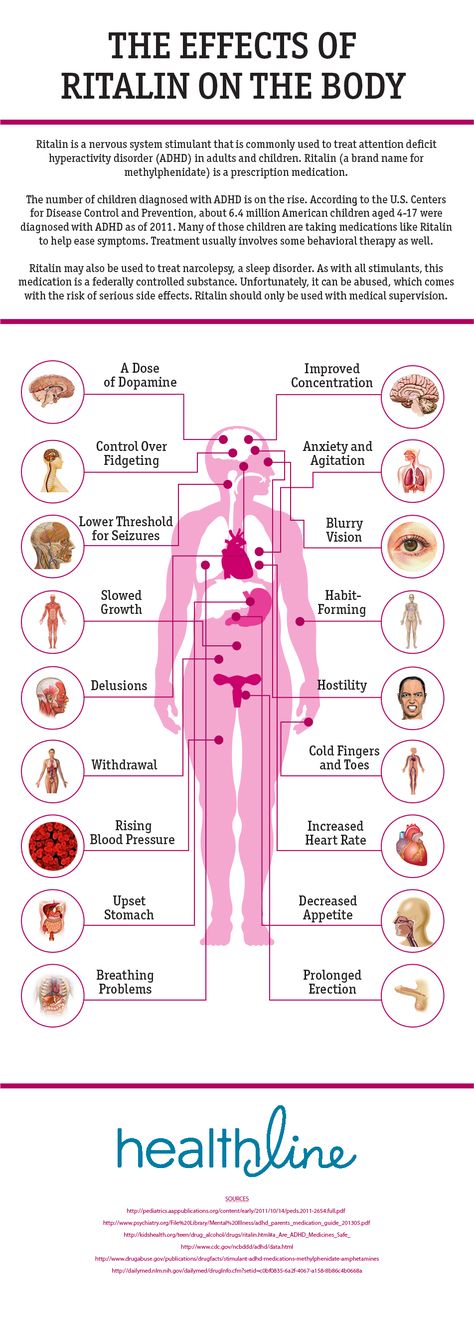
- Amphetamine-like stimulants. In cases where modafinil is not effective, doctors may prescribe amphetamine-like stimulants such as methylphenidate to alleviate EDS.
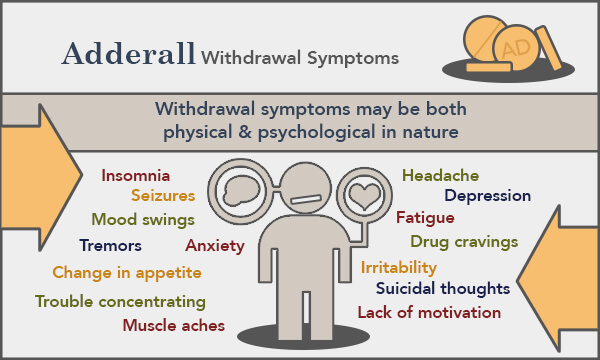
 However, these medications must be carefully monitored because they can have such side effects as irritability and nervousness, shakiness, disturbances in heart rhythm, and nighttime sleep disruption. In addition, health care professionals should be careful when prescribing these drugs and people should be careful using them because the potential for abuse is high with any amphetamine.
However, these medications must be carefully monitored because they can have such side effects as irritability and nervousness, shakiness, disturbances in heart rhythm, and nighttime sleep disruption. In addition, health care professionals should be careful when prescribing these drugs and people should be careful using them because the potential for abuse is high with any amphetamine. - Antidepressants. Two classes of antidepressant drugs have proven effective in controlling cataplexy in many individuals: tricyclics (including imipramine, desipramine, clomipramine, and protriptyline) and selective serotonin and noradrenergic reuptake inhibitors (including venlafaxine, fluoxetine, and atomoxetine). In general, antidepressants produce fewer adverse effects than amphetamines. However, troublesome side effects still occur in some individuals, including impotence, high blood pressure, and heart rhythm irregularities.
- Sodium oxybate. Sodium oxybate (also known as gamma hydroxybutyrate or GHB) has been approved by the U.
 S. Food and Drug Administration to treat cataplexy and excessive daytime sleepiness in individuals with narcolepsy. It is a strong sedative that must be taken twice a night. Due to safety concerns associated with the use of this drug, the distribution of sodium oxybate is tightly restricted.
S. Food and Drug Administration to treat cataplexy and excessive daytime sleepiness in individuals with narcolepsy. It is a strong sedative that must be taken twice a night. Due to safety concerns associated with the use of this drug, the distribution of sodium oxybate is tightly restricted. - Histamine 3 receptor antagonist/inverse agonist: Pitolisant was recently approved by FDA as the only non-scheduled product for the treatment of excessive daytime sleepiness or cataplexy in adult patients with narcolepsy. Pitolisant is thought to increase histamine levels in the brain. Pitolisant is administered orally, once daily after waking up in the morning. It has been commercially available in the U.S. since 2019. The most common adverse reactions to Pitolisant, occurring in 5 percent of adults or more, were insomnia, nausea, and anxiety.
Lifestyle changes
Not everyone with narcolepsy can consistently maintain a fully normal state of alertness using currently available medications. Drug therapy should accompany various lifestyle changes. The following strategies may be helpful:
Drug therapy should accompany various lifestyle changes. The following strategies may be helpful:
- Take short naps. Many individuals take short, regularly scheduled naps at times when they tend to feel sleepiest.
- Maintain a regular sleep schedule. Going to bed and waking up at the same time every day, even on the weekends, can help people sleep better.
- Avoid caffeine or alcohol before bed. Individuals should avoid alcohol and caffeine for several hours before bedtime.
- Avoid smoking, especially at night.
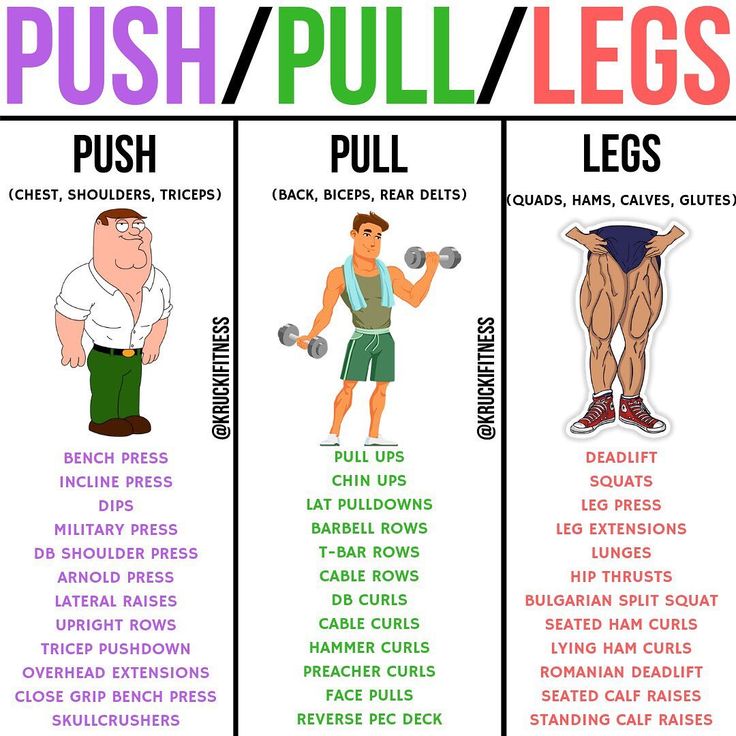
- Exercise daily. Exercising for at least 20 minutes per day at least 4 or 5 hours before bedtime also improves sleep quality and can help people with narcolepsy avoid gaining excess weight.
- Avoid large, heavy meals right before bedtime. Eating very close to bedtime can make it harder to sleep.
- Relax before bed.
 Relaxing activities such as a warm bath before bedtime can help promote sleepiness. Also make sure the sleep space is cool and comfortable.
Relaxing activities such as a warm bath before bedtime can help promote sleepiness. Also make sure the sleep space is cool and comfortable. - Safety precautions, particularly when driving, are important for everyone with narcolepsy. People with untreated symptoms are more likely to be involved in automobile accidents although the risk is lower among individuals who are taking appropriate medication. EDS and cataplexy can lead to serious injury or death if left uncontrolled. Suddenly falling asleep or losing muscle control can transform actions that are ordinarily safe, such as walking down a long flight of stairs, into hazards.
-
The Americans with Disabilities Act requires employers to provide reasonable accommodations for all employees with disabilities. Adults with narcolepsy can often negotiate with employers to modify their work schedules so they can take naps when necessary and perform their most demanding tasks when they are most alert. Similarly, children and adolescents with narcolepsy may be able to work with school administrators to accommodate special needs, like taking medications during the school day, modifying class schedules to fit in a nap, and other strategies.

Additionally, support groups can be extremely beneficial for people with narcolepsy who want to develop better coping strategies or feel socially isolated due to embarrassment about their symptoms. Support groups also provide individuals with a network of social contacts who can offer practical help and emotional support.
What is the state of the science involving narcolepsy?
In the past few decades, scientists have made considerable progress in understanding narcolepsy and identifying genes strongly associated with the disorder.
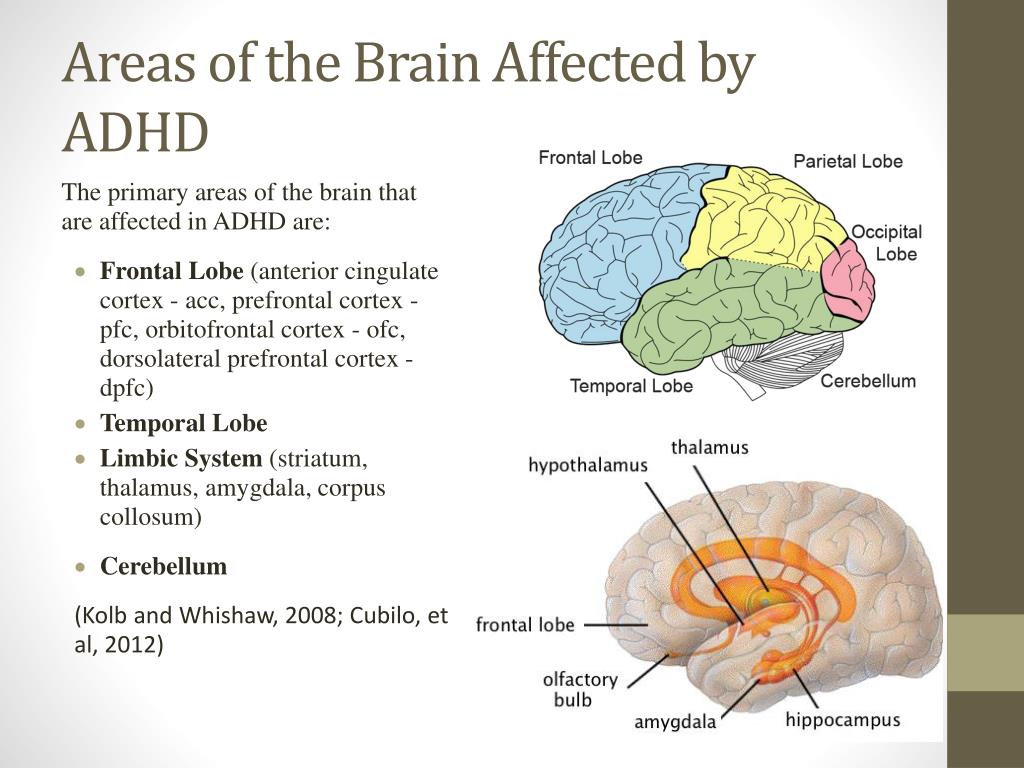
Groups of neurons in several parts of the brain interact to control sleep, and the activity of these neurons is controlled by a large number of genes. The loss of hypocretin-producing neurons in the hypothalamus is the primary cause of type 1 narcolepsy. These neurons are important for stabilizing sleep and wake states. When these neurons are gone, changes between wake, REM sleep, and non-REM sleep can happen spontaneously. This results in the sleep fragmentation and daytime symptoms that people with narcolepsy experience.
This results in the sleep fragmentation and daytime symptoms that people with narcolepsy experience.
It remains unclear exactly why hypocretin neurons die. However, research increasingly points to immune system abnormalities. HLA—human leukocyte antigen—genes play an important role in regulating the immune system. This gene family provides instructions for making a group of related proteins called the HLA complex, which helps the immune system distinguish between good proteins from an individual’s own body and bad ones made by foreign invaders like viruses and bacteria. One of the genes in this family is HLA-DQB1. A variation in this gene, called HLA-DQB1*06:02, increases the chance of developing narcolepsy, particularly the type of narcolepsy with cataplexy and a loss of hypocretins (also known as orexins). HLA-DQB1*06:02 and other HLA gene variations may increase susceptibility to an immune attack on hypocretin neurons, causing these cells to die.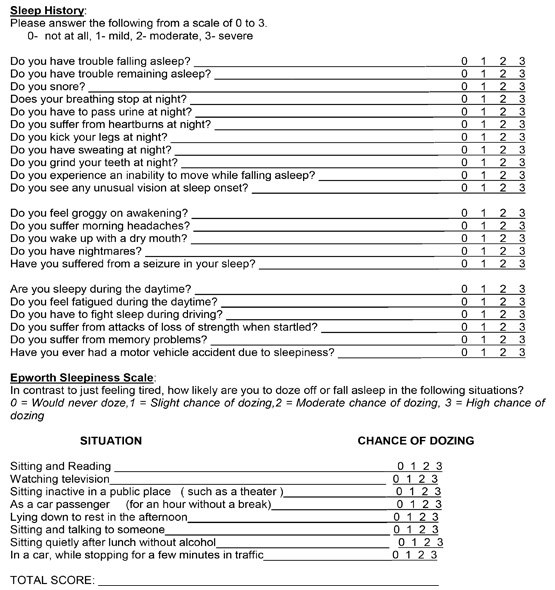 Most people with narcolepsy have this gene variation and may also have specific versions of closely related HLA genes.
Most people with narcolepsy have this gene variation and may also have specific versions of closely related HLA genes.
However, it is important to note that these gene variations are common in the general population and only a small portion of the people with the HLA-DQB1*06:02 variation will develop narcolepsy. This indicates that other genetic and environmental factors are important in determining if an individual will develop the disorder.
Narcolepsy follows a seasonal pattern and is more likely to develop in the spring and early summer after the winter season, a time when people are more likely to get sick. By studying people soon after they develop the disorder, scientists have discovered that individuals with narcolepsy have high levels of anti-streptolysin O antibodies, indicating an immune response to a recent bacterial infection such as strep throat. Also, the h2N1 influenza epidemic in 2009 resulted in a large increase in the number of new cases of narcolepsy. Together, this suggests that individuals with the HLA-DQB1*06:02 variation are at risk for developing narcolepsy after they are exposed to a specific trigger, like certain infections that trick the immune system to attack the body.
Together, this suggests that individuals with the HLA-DQB1*06:02 variation are at risk for developing narcolepsy after they are exposed to a specific trigger, like certain infections that trick the immune system to attack the body.
What research is being done?
The mission of the National Institute of Neurological Disorders and Stroke (NINDS) is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease. The NINDS is a component of the National Institutes of Health (NIH), the leading supporter of biomedical research in the world.
The NINDS, along with several other NIH Institutes and Centers, supports research on narcolepsy and other sleep disorders through grants to medical institutions across the country. Additionally, the NIH’s National Heart, Lung, and Blood Institute manages the National Center on Sleep Disorders Research (NCSDR), which coordinates Federal government sleep research activities, promotes doctoral and postdoctoral training programs, and educates the public and health care professionals about sleep disorders. For more information, visit the NCSDR website at www.nhlbi.nih.gov/about/ncsdr.
For more information, visit the NCSDR website at www.nhlbi.nih.gov/about/ncsdr.
Genetics and biochemicals
NINDS-sponsored researchers are conducting studies devoted to further clarifying the wide range of genetic —both HLA genes and non-HLA genes—and environmental factors that may cause narcolepsy. Other investigators are using animal models to better understand hypocretin and other chemicals such as glutamate that may play a key role in regulating sleep and wakefulness. Researchers are also investigating wake-promoting compounds to widen the range of available therapeutic options and create treatment options that reduce undesired side effects and decrease the potential for abuse. A greater understanding of the complex genetic and biochemical bases of narcolepsy will eventually lead to new therapies to control symptoms and may lead to a cure.
Immune system
Abnormalities in the immune system may play an important role in the development of narcolepsy. NINDS-sponsored scientists have demonstrated the presence of unusual immune system activity in people with narcolepsy. Further, strep throat and certain varieties of influenza are now thought to be triggers in some at-risk individuals. Other NINDS researchers are also working to understand why the immune system destroys hypocretin neurons in narcolepsy in the hopes of finding a way to prevent or cure the disorder.
NINDS-sponsored scientists have demonstrated the presence of unusual immune system activity in people with narcolepsy. Further, strep throat and certain varieties of influenza are now thought to be triggers in some at-risk individuals. Other NINDS researchers are also working to understand why the immune system destroys hypocretin neurons in narcolepsy in the hopes of finding a way to prevent or cure the disorder.
Sleep biology
The NINDS continues to support investigations into the basic biology of sleep, such as examining the brain mechanisms involved in generating and regulating REM sleep and other sleep behaviors. Since sleep and circadian rhythms are controlled by networks of neurons in the brain, NINDS researchers are also examining how neuronal circuits function in the body and contribute to sleep disorders like narcolepsy. A more comprehensive understanding of the complex biology of sleep will give scientists a better understanding of the processes that underlie narcolepsy and other sleep disorders.
How can I help research?
The NINDS supports the NIH NeuroBioBank, a national resource for investigators using human post-mortem brain tissue and related biospecimens for their research to understand conditions of the nervous system. The NeuroBioBank serves as a central point of access to collections that span neurological, neuropsychiatric, and neurodevelopmental diseases and disorders. Tissue from individuals with narcolepsy is needed to enable scientists to study this disorder more intensely. Participating groups include brain and tissue repositories, researchers, NIH program staff, information technology experts, disease advocacy groups, and, most importantly, individuals seeking information about opportunities to donate. More information about NeuroBioBank and opportunities to donate tissue is available at https://neurobiobank.nih.gov/.
Additionally, the NINDS supports genetic and immunological research in narcolepsy at Stanford University.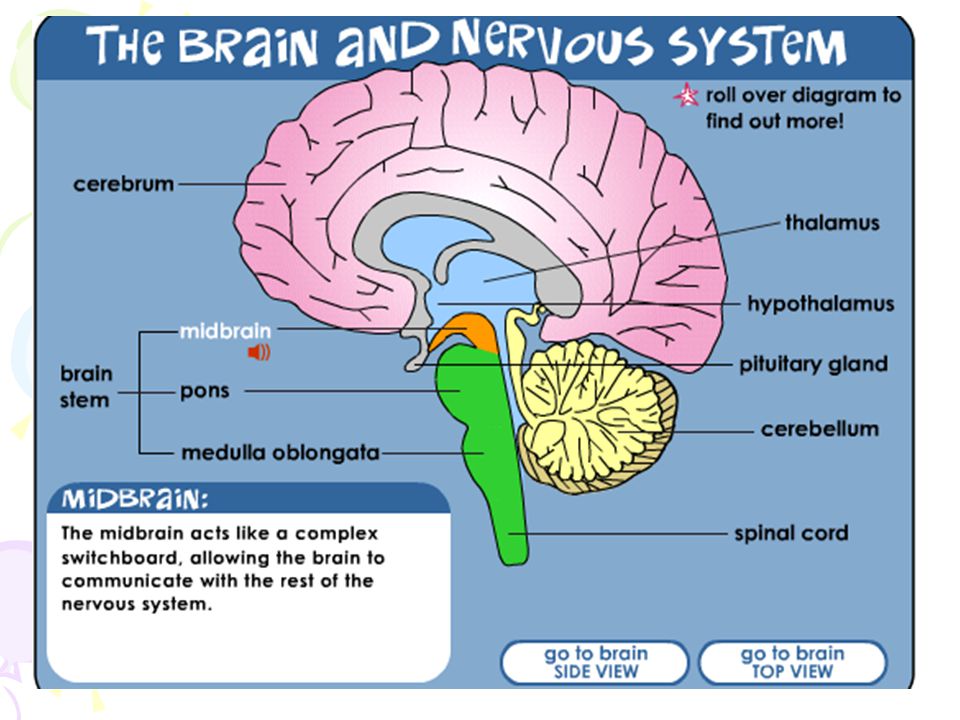 Blood samples from individuals with narcolepsy can be sent by mail and are needed to enable scientists to study this disorder more intensely. Prospective donors may contact:
Blood samples from individuals with narcolepsy can be sent by mail and are needed to enable scientists to study this disorder more intensely. Prospective donors may contact:
Stanford University Center for Narcolepsy
450 Broadway Street
M/C 5704
Redwood City, CA 94063
650-721-7574
https://med.stanford.edu/narcolepsy.html
Where can I get more information?
For more information on neurological disorders or research programs funded by the National Institute of Neurological Disorders and Stroke, contact the Institute's Brain Resources and Information Network (BRAIN) at:
BRAIN
P.O. Box 5801
Bethesda, MD 20824
800-352-9424
Information is also available from the following organizations:
Narcolepsy Network
46 Union Drive #A212
North Kingstown, RI 02852
401-667-2523
888-292-6522
National Sleep Foundation
1010 N. Glebe Road, Suite 420
Arlington, VA 22201
703-243-1697
Wake Up Narcolepsy
P. O. Box 60293
O. Box 60293
Worcester, MA 01606
978-751-3693
National Heart, Lung, and Blood Institute (NHLBI) Health Information Center
National Institutes of Health/DHHS
P.O. Box 30105
Bethesda, MD 20824-0105
301-592-8573
800-575-9355
U.S. National Library of Medicine
National Institutes of Health/DHHS
8600 Rockville Pike
Bethesda, MD 20894
301-594-5983
888-346-3656
"Narcolepsy Fact Sheet", NINDS
NIH Publication No. 17-1637
Back to Narcolepsy Information Page
See a list of all NINDS disorders
Publicaciones en Español
Narcolepsia
Prepared by:
Office of Communications and Public Liaison
National Institute of Neurological Disorders and Stroke
National Institutes of Health
Bethesda, MD 20892
NINDS health-related material is provided for information purposes only and does not necessarily represent endorsement by or an official position of the National Institute of Neurological Disorders and Stroke or any other Federal agency. Advice on the treatment or care of an individual patient should be obtained through consultation with a physician who has examined that patient or is familiar with that patient's medical history.
Advice on the treatment or care of an individual patient should be obtained through consultation with a physician who has examined that patient or is familiar with that patient's medical history.
All NINDS-prepared information is in the public domain and may be freely copied. Credit to the NINDS or the NIH is appreciated.
How Common is Narcolepsy? Prevalence, Symptoms, Causes, More
Narcolepsy is a relatively rare sleep disorder that causes a person to feel sleepy or fall asleep suddenly during the daytime hours.
Between 135,000 and 200,000 people in the United States have narcolepsy. This neurological condition is difficult to diagnose because it shares features with other disorders. Researchers believe narcolepsy may be underdiagnosed.
This article will look at the symptoms you might experience with narcolepsy, what conditions it’s similar to, and how it’s diagnosed and treated.
The true prevalence of narcolepsy isn’t known and may vary from region to region. Researchers suspect the condition is underdiagnosed or sometimes misdiagnosed as other medical conditions.
Researchers suspect the condition is underdiagnosed or sometimes misdiagnosed as other medical conditions.
Conditions that may be either confused or comorbid (occurring together) with narcolepsy include:
- insomnia
- sleep apnea
- depression
- anxiety
- attention deficit hyperactivity disorder (ADHD)
- schizophrenia
- eating disorders
- epilepsy
- head injury
The National Organization for Rare Disorders reports that around 1 in every 2,000 people may have narcolepsy. Other researchers estimate that approximately 20 to 55 per 100,000 people worldwide may live with the condition.
In some countries, this number may be higher or lower. Some researchers point to a “striking” gap in data between reporting of Caucasian and European cases versus those in other populations.
Do you nod off at random points throughout the day? Do you also have trouble sleeping through the night?
If you suspect you have narcolepsy, you may experience the following symptoms:
- Daytime sleepiness.
 Excessive daytime sleepiness (EDS) is the kind of sleepiness that causes someone to fall asleep frequently when they don’t want to — at the wrong time and place. People may also experience sleep attacks.
Excessive daytime sleepiness (EDS) is the kind of sleepiness that causes someone to fall asleep frequently when they don’t want to — at the wrong time and place. People may also experience sleep attacks. - REM sleep changes. REM is a state of sleep during which the eyes move rapidly. People with narcolepsy may quickly slip into REM sleep cycles even during the day.
- Sleep paralysis. As a person awakens from REM sleep, there may be a few seconds to minutes when they’re unable to speak or move their body. Some people with narcolepsy have this symptom frequently, some not at all.
- Hallucinations. Some people may experience vivid and sometimes disturbing dream-like images either when falling asleep or waking up. Usually, hallucinations are visual, but they may also involve touch, smell, and other senses.
- Cataplexy. This symptom, which not all people with narcolepsy experience, involves a sudden loss of muscle tone.
 This may be subtle, with the loss of some of the muscle tone in the the face or hand, or it may affect many muscle groups and result in the person falling to the ground. Unlike sleep paralysis, cataplexy happens when a person is fully awake. It’s often triggered by strong emotions (laughter, anger, fear, excitement, etc.).
This may be subtle, with the loss of some of the muscle tone in the the face or hand, or it may affect many muscle groups and result in the person falling to the ground. Unlike sleep paralysis, cataplexy happens when a person is fully awake. It’s often triggered by strong emotions (laughter, anger, fear, excitement, etc.). - Nighttime sleep disruption. People with narcolepsy may also have trouble falling and staying asleep at night. They may experience vivid dreams, sleep apnea, insomnia, or movements while sleeping, such as acting out and leg movements.
- Automatic behavior. If sleep episodes are very brief, people may continue doing habitual activities, such as brushing teeth or driving. They may also put things in drawers where they don’t belong and write illegibly.
The symptoms of narcolepsy can overlap with other conditions. For example, a person may have excessive daytime sleepiness if they’ve had a head injury or are taking certain medications.
Cataplexy may also sometimes be confused with drop attacks or seizures from epilepsy.
A person can have one of several forms of narcolepsy:
- with cataplexy (narcolepsy type 1)
- without cataplexy (narcolepsy type 2)
- as a result of a brain injury, or lesion in the brain (secondary narcolepsy)
With cataplexy, a person experiences muscle weakness, particularly in response to strong emotions. This means their body or parts of the body may go limp without warning. They may lose control of their muscles or be unable to move during episodes that last anywhere between a few seconds and 2 minutes.
People with cataplexy have low levels of a brain chemical called hypocretin. It’s this marker that can help with diagnosis, as cataplexy is not a feature of similar disorders.
Scientists estimate that somewhere between 25 and 50 in 100,000 people have narcolepsy with cataplexy, according to a 2007 study.
Researchers continue to work on learning the cause of narcolepsy.
Currently, many researchers believe that the following causes are possible:
- Low hypocretin levels. People who have narcolepsy with cataplexy may have very low levels of this chemical. People who have narcolepsy without cataplexy generally have normal levels.
- Autoimmune disorders. If you have an autoimmune disorder, your immune system may attack healthy parts of your body (cells, tissues, etc.). This may affect how much hypocretin your body produces.
- Family history. If other people in your family have narcolepsy, there’s a higher chance you may, too. That said, most cases of narcolepsy are “sporadic” (occurring at random).
- Brain injury or issue. In rare cases, a brain injury may lead to narcolepsy. After an injury, the part of the brain that regulates REM sleep may not function normally. This may also be the case if you have a brain tumor or other issue.
- Other triggers.
 Other possible triggers may include psychological stress and certain infections.
Other possible triggers may include psychological stress and certain infections.
It may take up to 10 years after symptoms appear to get a confirmed diagnosis of narcolepsy.
Researchers suggest that symptoms may start between the ages of 7 and 25 on average. Symptoms may start out mild but become more noticeable with age. Eventually the symptoms are stable over many years.
At your appointment, a doctor will ask about your your sleep symptoms, medical history or family history. From there, you may be asked to do the following:
- Log your symptoms. The doctor may ask you to keep a log of daytime and nighttime sleep. It’s important to note cataplexy because it’s a specific symptom of narcolepsy.
- Have an overnight sleep study. Also called a polysomnography (PSG), a sleep study is usually performed in a lab setting. The doctor will monitor your breathing, brain, and muscle activity as well as your REM sleep patterns to rule out other conditions like sleep apnea or movement disorders.
 People with narcolepsy may enter REM sleep in less than 15 minutes.
People with narcolepsy may enter REM sleep in less than 15 minutes. - Have a multiple sleep latency test (MSLT). An MSLT measures how quickly you can fall asleep during the day and enter a REM cycle. Unlike during a sleep study, where you’re asked to sleep normally through the night, in an MSLT you’re asked to take short naps a couple of hours apart (4 to 5 times) during the day. Falling into REM within 15 minutes in at least two of the five naps is a marker for narcolepsy.
- Try other tests. The doctor can also test your spinal fluid for the presence of hypocretin. The fluid (cerebrospinal fluid or CSF) is obtained through a spinal tap.
Narcolepsy is a lifelong condition. Treatments can help with the symptoms, but there’s currently no cure.
Treatments include:
- Wake-promoting agents. Modafinil or armodafinil promote wakefulness and alertness. Methylphenidate is an amphetamine-like stimulant that also promotes wakefulness, but may have more side effects and addictive properties.
 More recently, pitolisant (Wakix) and solriamfetol (Sunosi) have been introduced.
More recently, pitolisant (Wakix) and solriamfetol (Sunosi) have been introduced. - Antidepressants. Tricyclic antidepressants (TCAs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) may help control episodes of cataplexy.
- Sedatives. Sodium oxybate (gamma hydroxybutyrate or GHB) can be taken at night to help with both cataplexy and daytime sleepiness.
Lifestyle modifications, such as practicing good sleep hygiene habits and taking brief scheduled naps (e.g. after lunch or later in the afternoon), are other options. Exercising each day and avoiding caffeine, alcohol, and nicotine may also make nighttime sleep more restful and help with daytime sleepiness.
You may also ask a doctor about local support groups for people with narcolepsy. Online support is also available at places like the Narcolepsy Network or Rare Connect’s Narcolepsy Community.
While narcolepsy is rare, it’s also difficult to diagnose. The sooner you seek a diagnosis, the sooner you may find help for whatever sleep issue you’re experiencing.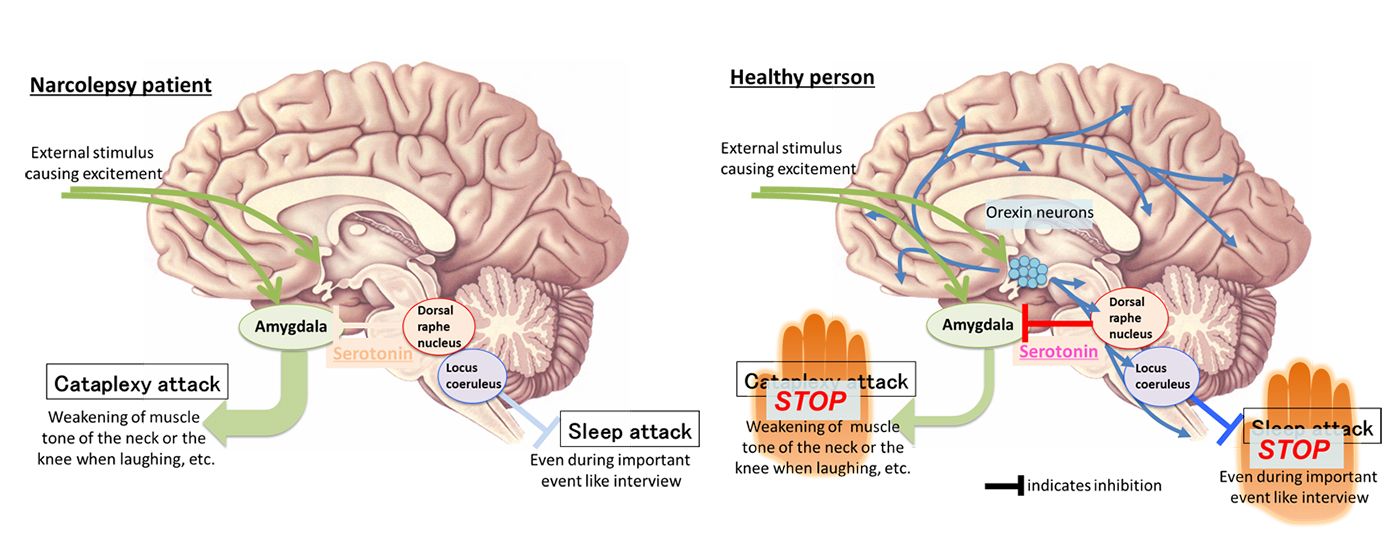
If you do have narcolepsy, a doctor can help you find the appropriate treatments and lifestyle modifications to live your best life.
How common is narcolepsy? - Drink-Drink
Narcolepsy is a relatively rare sleep disorder in which a person feels sleepy or suddenly falls asleep during the daytime.
Between 135,000 and 200,000 people in the United States suffer from narcolepsy. This neurological condition is difficult to diagnose because it shares features with other disorders. Researchers believe that narcolepsy may be underestimated.
This article will look at the symptoms that can occur with narcolepsy, what conditions it looks like, and how to diagnose and treat it.
About the prevalence of narcolepsy
The true prevalence of narcolepsy is unknown and may vary from region to region. Researchers suspect that the condition is underdiagnosed or sometimes misdiagnosed as other diseases.
Conditions that may be either confused or comorbid (occurring together) with narcolepsy include:
- insomnia
- sleep apnea
- depression
- anxiety
- attention deficit hyperactivity disorder (ADHD)
- schizophrenia
- eating disorders
- epilepsy
- head injury
The National Organization for Rare Diseases reports that about 1 in every 2,000 people may suffer from drug addiction Other researchers estimate that approximately 20 to 55 people per 100,000 people worldwide may be living with the disease.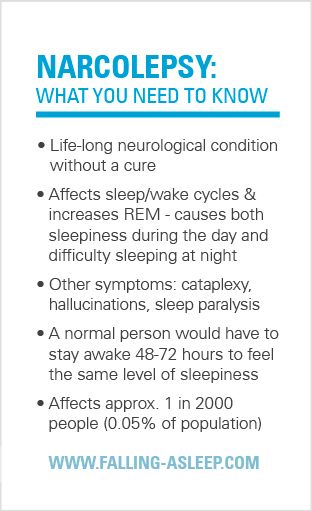
This number may be higher or lower in some countries. Some researchers point to a "striking" data gap between case reports in Caucasians and Europeans compared to other populations.
What are the symptoms of narcolepsy?
Do you fall asleep at random times during the day? Do you also have trouble sleeping at night?
If you suspect you have narcolepsy, you may experience the following symptoms:
- Daytime sleepiness. Excessive daytime sleepiness (EDS) is a type of sleepiness that causes a person to fall asleep frequently when they don't want to - at the wrong time and in the wrong place. People may also experience sleep attacks.
- Changes in REM sleep. REM is a state of sleep during which the eyes move rapidly. People with narcolepsy can quickly enter REM sleep even during the day.
- Sleep paralysis. When a person wakes up from REM sleep, there may be seconds to minutes when they cannot speak or move their body.
 Some people with narcolepsy have this symptom frequently, while others don't have it at all.
Some people with narcolepsy have this symptom frequently, while others don't have it at all. - Hallucinations. Some people may see vivid and sometimes disturbing dream-like images either when falling asleep or when waking up. Usually, hallucinations are visual, but they can also include touch, smell, and other senses.
- Cataplexy. This symptom, which is not experienced by all people with narcolepsy, involves a sudden loss of muscle tone. It may be subtle, with loss of muscle tone in the face or arms, or it may affect multiple muscle groups and cause the person to fall to the ground. Unlike sleep paralysis, cataplexy occurs when a person is fully awake. Often provoked by strong emotions (laughter, anger, fear, excitement, etc.).
- Night sleep disturbance. People with narcolepsy may also have trouble falling asleep and staying asleep at night. They may experience vivid dreams, sleep apnea, insomnia, or movements during sleep such as actions and leg movements.
- Automatic behavior. If sleep episodes are very short, people may continue to do normal activities such as brushing their teeth or driving. They may also put things in drawers where they don't belong and write illegibly.
Symptoms of narcolepsy may overlap with other conditions. For example, a person may have excessive daytime sleepiness if they have had a head injury or are taking certain medications.
Cataplexy can also sometimes be confused with drop attacks or seizures in epilepsy.
What is narcolepsy with cataplexy?
A person may have one of several forms of narcolepsy:
- with cataplexy (type 1 narcolepsy)
- without cataplexy (type 2 narcolepsy)
- as a result of traumatic brain injury or damage to the brain (secondary narcolepsy)
 They may lose control of their muscles or be unable to move during episodes that last from a few seconds to 2 minutes.
They may lose control of their muscles or be unable to move during episodes that last from a few seconds to 2 minutes. People with cataplexy have low levels of a chemical in the brain called hypocretin. It is this marker that can help in the diagnosis, since cataplexy is not a sign of such disorders.
Scientists estimate that somewhere between 25 and 50 per 100,000 According to a 2007 study, people suffer from narcolepsy with cataplexy.
What causes narcolepsy?
Researchers continue to work on the cause of narcolepsy.
Currently, many researchers consider the following possible causes:
- Low level of hypocretin. People suffering from narcolepsy with cataplexy may have very low levels of this chem. People with narcolepsy without cataplexy generally have normal levels.
- Autoimmune disorders. If you have an autoimmune disease, your immune system can attack healthy parts of your body (cells, tissues, etc.
 ). This can affect how much hypocretin your body produces.
). This can affect how much hypocretin your body produces. - Family history. If other members of your family have narcolepsy, chances are high that you can too. However, most cases of narcolepsy are "sporadic" (occurring randomly).
- Traumatic brain injury or problems. In rare cases, traumatic brain injury can lead to narcolepsy. After an injury, the part of the brain that regulates REM sleep may not function normally. This can also be the case if you have a brain tumor or other problem.
- Other triggers. Other possible triggers may include psychological stress and certain infections.
How is narcolepsy diagnosed?
It may take up to 10 years after the onset of symptoms to receive a confirmed diagnosis of narcolepsy.
Researchers suggest that symptoms may begin between the ages of 7 and 25 on average. Symptoms may start out mildly but become more noticeable with age. Eventually the symptoms are stable for many years.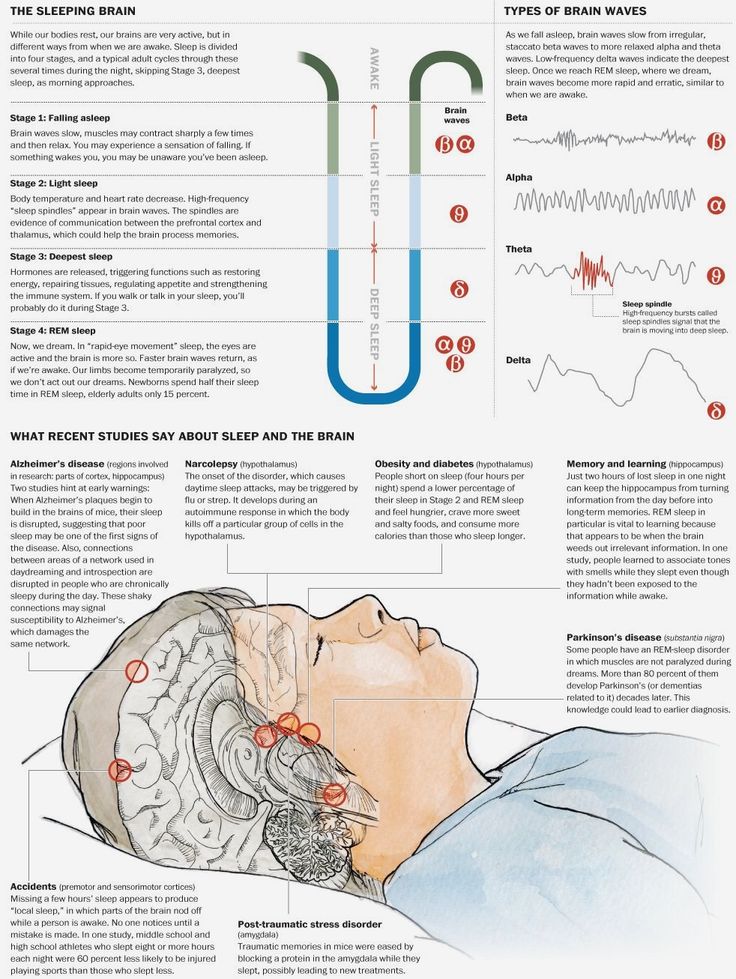
At the appointment, the doctor will ask about sleep symptoms, medical or family history. From there, you may be asked to do the following:
- Write down your symptoms. Your doctor may ask you to keep a log of daytime and nighttime sleep. It is important to note cataplexy because it is a specific symptom of narcolepsy.
- Do a nighttime sleep study. Also called polysomnography (PSG), sleep testing is usually performed in a laboratory setting. Your doctor will monitor your breathing, brain and muscle activity, and your REM sleep patterns to rule out other conditions such as sleep apnea or movement disorders. People with narcolepsy can enter REM sleep in less than 15 minutes.
- Complete the Multiple Sleep Latency Test (MSLT) . MSLT measures how quickly you can fall asleep during the day and enter the REM cycle. Unlike the sleep study, where you are asked to sleep normally throughout the night, in MSLT you are asked to take short naps at intervals of a couple of hours (4 to 5 times) during the day.
 A fall in REM within 15 minutes in at least two out of five naps is a sign of narcolepsy.
A fall in REM within 15 minutes in at least two out of five naps is a sign of narcolepsy. - Try other tests. Your doctor may also test your cerebrospinal fluid for the presence of hypocretin. Fluid (cerebrospinal fluid or CSF) is obtained through a lumbar puncture.
How is narcolepsy treated?
Narcolepsy is a lifelong disease. Treatment may help with symptoms, but there is currently no cure.
Treatments include:
- Wake-promoting agents . Modafinil or armodafinil promotes wakefulness and alertness. Methylphenidate is an amphetamine-like stimulant that also promotes wakefulness, but may have more side effects and addictive properties. More recently, pitolizant (Wakix) and solriamphetol (Sunosi) have been introduced.
- Antidepressants . Tricyclic antidepressants (TCAs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) may help control episodes of cataplexy.
- Sedatives .
 Sodium oxybate (gamma hydroxybutyrate or GHB) can be taken at night to help with both cataplexy and daytime sleepiness.
Sodium oxybate (gamma hydroxybutyrate or GHB) can be taken at night to help with both cataplexy and daytime sleepiness.
Other options are lifestyle changes such as good sleep hygiene and short scheduled naps (for example, in the afternoon or late afternoon). Daily exercise and avoiding caffeine, alcohol, and nicotine can also improve nighttime sleep and help with daytime sleepiness.
You can also ask your doctor about local support groups for people with narcolepsy. Online support is also available from places like Narcolepsy Network or Rare Connect's Narcolepsy Community.
Conclusion
While narcolepsy is rare, it is also difficult to diagnose. The sooner you seek a diagnosis, the sooner you can find help for any sleep problem you're experiencing.
If you have narcolepsy, your doctor can help you find the right treatment and make lifestyle changes to help you live better.
NARCOLEPSY: CAUSES, SYMPTOMS, TREATMENT - SLEEP TOPICS
Narcolepsy is a sleep disorder that is often misunderstood. It is characterized by severe and persistent daytime sleepiness, which can cause disruption at school, work, and social media, and increase the risk of serious accidents and injury.
It is characterized by severe and persistent daytime sleepiness, which can cause disruption at school, work, and social media, and increase the risk of serious accidents and injury.
Although rare compared to many other sleep disorders, narcolepsy affects hundreds of thousands of Americans, including children and adults.
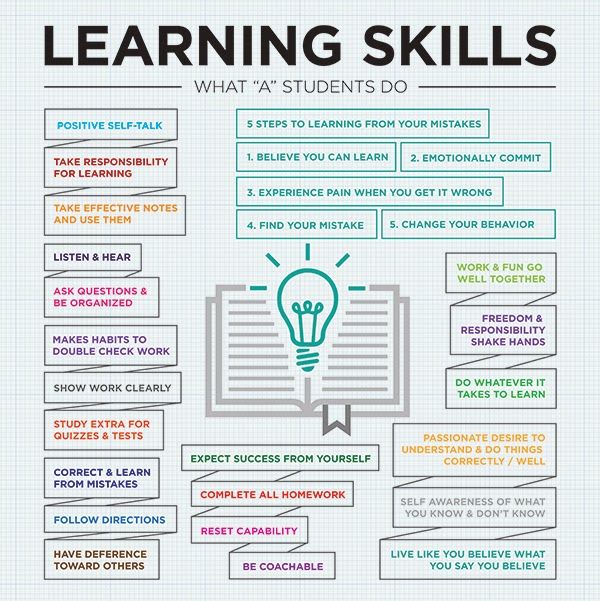
Understanding the types of narcolepsy and their symptoms, causes, diagnosis, and treatment can help patients and their loved ones manage it more effectively.
What is narcolepsy?
Related Reading
Normal sleep goes through a series of stages, with rapid eye movement (REM) sleep occurring in the last stage, usually an hour or more after falling asleep. In narcolepsy, REM sleep is irregular and often begins within minutes of falling asleep.
Haley Jade, Scott Mathers and Eminem
REM occurs quickly in people with narcolepsy due to changes in the brain that interfere with how sleep works. These disruptions also cause daytime sleepiness and other symptoms of narcolepsy.
What are the types of narcolepsy?
According to the International Classification of Sleep Disorders, Third Edition (ICSD-3), there are two types of narcolepsy: narcolepsy type 1 (NT1) and narcolepsy type 2 (NT2).
Narcolepsy type 1
NT1 is associated with the symptom of cataplexy, i.e. a sudden loss of muscle tone. NT1 was formerly called narcolepsy with cataplexy.
Not all patients diagnosed with NT1 experience episodes of cataplexy.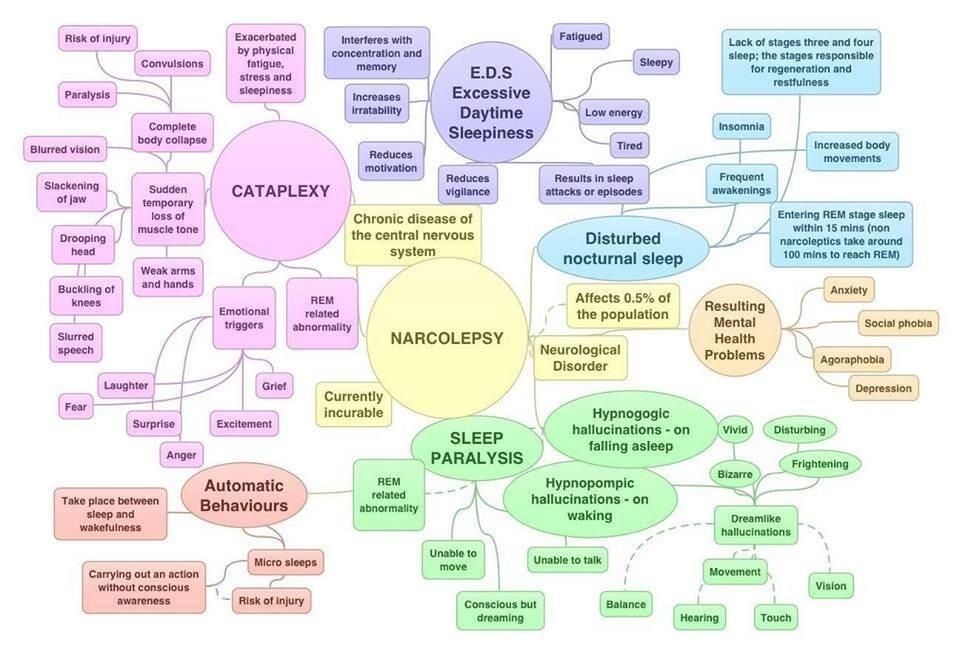 NT1 can also be diagnosed when a person has low levels of hypocretin-1, a chemical in the body that helps control wakefulness.
NT1 can also be diagnosed when a person has low levels of hypocretin-1, a chemical in the body that helps control wakefulness.
Even if not present at diagnosis, cataplexy eventually occurs in a significant number of people with low levels of hypocretin-1.
Narcolepsy type 2
NT2 formerly called narcolepsy without cataplexy. People with NT2 have many of the same symptoms as people with NT1, but they do not have cataplexy or low hypocretin-1 levels.
Tara from my 600 pound life today
If a person with NT2 later develops cataplexy or low levels of hypocretin-1, the diagnosis can be changed to NT1. This change in diagnosis is estimated to occur in about 10% of cases.
How common is narcolepsy?
Narcolepsy is relatively rare. NT1 affects between 20 and 67 people per 100,000 US residents. NT1 is two to three times more common than NT2, which is estimated to affect about 20 people per 100,000 people.
Estimating the prevalence of narcolepsy is difficult due to underdiagnosis and delays in diagnosis.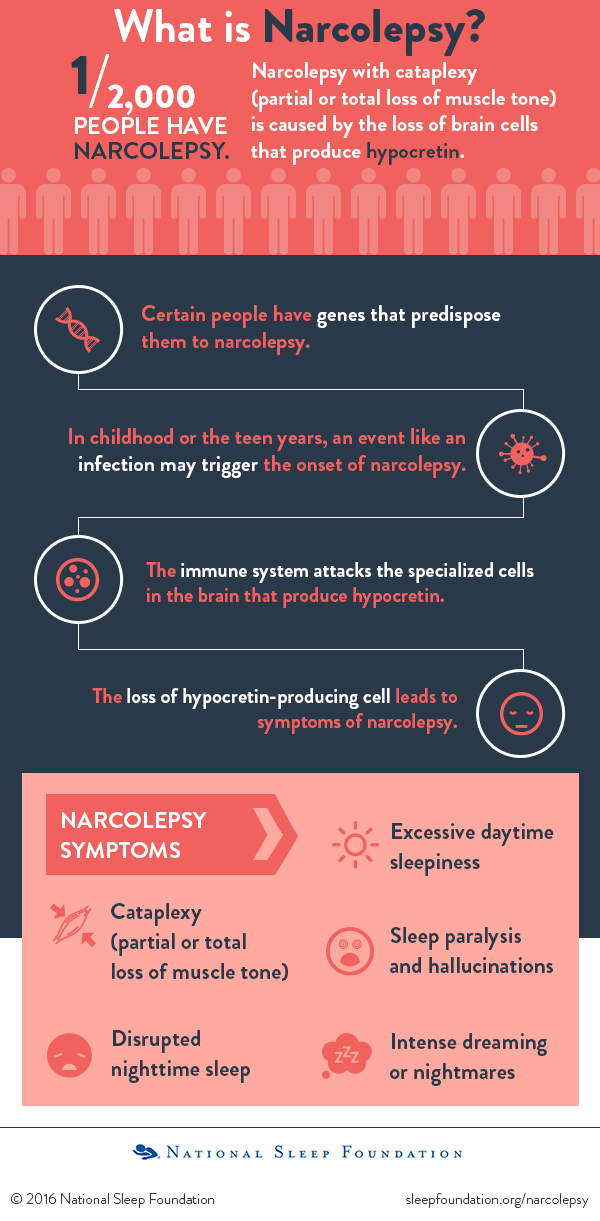 In many patients, narcolepsy is not diagnosed until years after the first symptoms. As a result, according to some estimates, the prevalence of narcolepsy reaches 180 cases per 100,000 people.
In many patients, narcolepsy is not diagnosed until years after the first symptoms. As a result, according to some estimates, the prevalence of narcolepsy reaches 180 cases per 100,000 people.
Narcolepsy occurs in much the same way in men and women and can affect both children and adults. It can happen at any age, but it has been found to peak around age 15 and then around age 35.
What are the symptoms of narcolepsy?
The symptoms of narcolepsy can have noticeable effects both during the day and at night. The most common symptoms include:
- Excessive Daytime Sleepiness (EDS): EDS is the main symptom of narcolepsy and affects all people with this condition. EDS includes an overwhelming desire to sleep, which most often occurs in monotonous situations. Severe drowsiness often causes a decline in attention. Narcolepsy can cause sleep attacks in which you can fall asleep without warning. After a short nap, people with narcolepsy usually feel temporarily rested.
- Automatic behavior: Trying to avoid drowsiness can trigger automatic behavior that occurs when the person is not aware. For example, a student in a class may continue to write, but in reality they are just scribbling lines or gibberish on the page.
- Disturbed night sleep: Sleep fragmentation is common in people with narcolepsy who may wake up several times during the night. Other annoying sleep problems, such as excessive physical movement and sleep apnea, are also more common in narcoleptics.
- Sleep paralysis: People with narcolepsy are more likely to suffer from sleep paralysis, which is the feeling of being unable to move when falling asleep or waking up.
- Sleep-related hallucinations: Vivid images may occur when falling asleep (hypnagogic hallucinations) or upon awakening (hypnopompic hallucinations). This may accompany sleep paralysis, which can be particularly disturbing or frightening.
- Cataplexy: Cataplexy is a sudden loss of muscle control. This only happens in people with NT1, not NT2. An episode of cataplexy often occurs in response to positive emotions such as laughter or joy. Cataplexy usually affects both sides of the body and lasts from a few seconds to several minutes. Some people with NT1 have cataplexy episodes only a few times a year, while others may have a dozen or more episodes a day.
Although all people with narcolepsy have EDS, less than a quarter have all of these symptoms. Also, the symptoms may not occur at the same time. For example, cataplexy often begins several years after a person has EDS.
Are the symptoms of narcolepsy different in children?
The symptoms of narcolepsy in children and adults overlap in many ways, but there are also important differences.
In children, EDS is more likely to present as restlessness or irritability, which can be interpreted as a behavioral problem.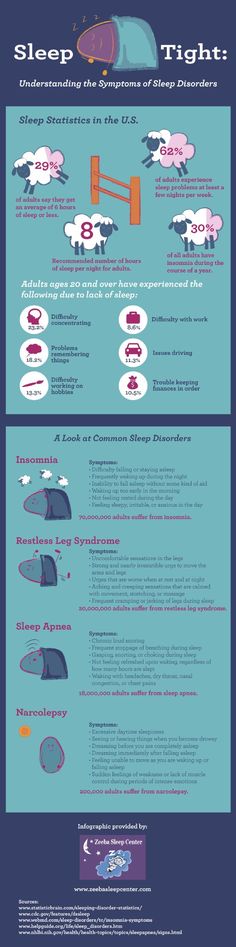 At night, children with narcolepsy may sleep longer and have more active body movements during sleep.
At night, children with narcolepsy may sleep longer and have more active body movements during sleep.
Cataplexy in children is often less noticeable, although it occurs in children. up to 80% of cases. It usually affects the face, not the body, and may be perceived as a facial tic. Cataplexy in children cannot be associated with an emotional reaction. Over time, the symptoms of cataplexy in children take on a more traditional form.
What are the consequences of narcolepsy?
The symptoms of narcolepsy can have serious consequences for the patient's health and well-being. Accidents are a pressing issue as sleep attacks, drowsiness and cataplexy can be life-threatening when driving or in other settings where safety is critical. It is believed that people with narcolepsy are three to four times more likely to be in a car accident.
Khloe Kardashian is pregnant, life and style
Narcolepsy can also interfere with school and work. Drowsiness and attention gaps can impair performance and can be interpreted as behavioral problems, especially in children.
Many patients with narcolepsy feel stigma attached to the condition, which can lead to social isolation. Without proper support, this can contribute to the development of mental disorders and negatively affect school, work and relationships.
People with narcolepsy are at higher risk for other health conditions, including obesity, cardiovascular problems such as high blood pressure, and psychiatric problems such as depression, anxiety, and attention deficit/hyperactivity disorder (ADHD).
What causes narcolepsy?
Research has begun to unravel the biology behind narcolepsy, but more is known about NT1 than NT2. Even with growing knowledge, the exact causes and risk factors for each condition are not fully understood.
NT1
Type 1 narcolepsy is a disease characterized by the loss of neurons in the brain responsible for producing hypocretin, also known as orexin, a chemical that helps regulate wakefulness and sleep. People with NT1 lose 90% or more of the normal number of hypocretin-producing neurons.
Damage to these neurons can occur due to an autoimmune response that occurs in people with a genetic predisposition who are exposed to the environment.
Some evidence suggests that NT1 fluctuates seasonally, which may be related to the influenza virus. There was also an increase in the onset of NT1. after an h2N1 epidemic and with a specific brand of vaccine used against h2N1. Associations with other types of infections have also been found in other cases.
Based on these data, one theory about NT1 is that an external trigger activates the immune system in a way that causes it to attack hypocretin-producing neurons in the brain. However, this autoimmune response does not happen to everyone.
Researchers have found that 98% of people with NT1 carry a gene variant known as DQB1*0602. This gene plays a role in immune function, so this variation may be a genetic predisposition to NT1. While this explanation for NT1 is widely accepted, it has not yet been conclusively proven.
Although researchers know more about NT1 than ever, most individual cases still occur without a clear and direct cause. People with a family history of NT1 have a 1-2% chance of developing the condition. In general, this is a small risk, but it is significantly higher compared to people without a family history.
Rarely, NT1 is due to another disease that causes damage to parts of the brain that contain hypocretin-producing neurons. This may be known as secondary narcolepsy and may result from a brain injury or central nervous system infection.
NT2
Little is known about the biology or risk factors for type 2 narcolepsy. Some experts believe that NT2 is simply a less pronounced loss of hypocretin-producing neurons, but people with NT2 are not usually hypocretin deficient. Others believe that NT2 may be primarily a precursor to NT1, but cataplexy has been seen in only 10% of people who were initially diagnosed with NT2.
In some cases, NT2 has been reported following a viral infection, but in most cases the cause has not been established. Like NT1, NT2 can occur due to other diseases such as head trauma, multiple sclerosis, and other diseases that affect the brain.
Like NT1, NT2 can occur due to other diseases such as head trauma, multiple sclerosis, and other diseases that affect the brain.
More information can be found in our privacy policy.
How is narcolepsy diagnosed?
Diagnosis of narcolepsy requires careful evaluation by a physician familiar with the disease. Because it is rare and symptoms can be mistaken for other causes, narcolepsy can go undetected for years.
The diagnostic process begins with a review of symptoms and medical history. This step helps the clinician understand the patient's sleep pattern and the nature of their EDS. In many cases, especially in the case of children, family members are involved to provide more information about the patient's symptoms.
EDS and sleep tests may be performed. The test, called the Epworth Sleepiness Scale (ESS), is based on a patient's subjective experience of their symptoms. You may need a polysomnography (PSG), a detailed test in which sensors monitor brain and body activity. Such a sleep study is performed at night in a specialized clinic.
You may need a polysomnography (PSG), a detailed test in which sensors monitor brain and body activity. Such a sleep study is performed at night in a specialized clinic.
The day after the PSG test, another test called the Multiple Sleep Latency Test (MSLT) can be used to objectively assess sleepiness. During MSLT, the patient is asked to try to fall asleep at five different intervals while remaining connected to the sensors used in the PSG. People with narcolepsy tend to fall asleep quickly and enter REM sleep quickly during MSLT.
Another test may be used to remove cerebrospinal fluid (CSF) and assess hypocretin levels. This is done through a procedure called a spinal tap or lumbar puncture. A low level of hypocretin indicates NT1 and helps distinguish it from NT2.
Diagnostic criteria for narcolepsy
Physicians follow standardized criteria for diagnosing sleep disorders. Standardization helps ensure accurate diagnosis and differentiate between NT1, NT2, hypersomnia, and other conditions that cause EDS.
Kylie Jenner body plastic surgery
Both criteria for NT1 and NT2 require significant EDS lasting at least three months. For NT1, the patient must have low CSF hypocretin or symptoms of cataplexy plus a short time to fall asleep and enter REM on MSLT. For NT2, the patient should have similar results on MSLT, but cannot have cataplexy or low hypocretin.
how i met your mom blah blah
Other sleep disorders have symptoms similar to those of NT2, making diagnosis difficult. For this reason, the doctor needs to rule out other conditions by carefully analyzing the test results and the patient's symptoms. While this is not sufficient to diagnose NT2, the presence of short refreshing sleep and intermittent nighttime sleep helps distinguish narcolepsy from other hypersomnias.
What are the treatments for narcolepsy?
There is no cure for type 1 or type 2 narcolepsy. The goals of treating narcolepsy are to improve patient safety, reduce symptoms, and improve quality of life.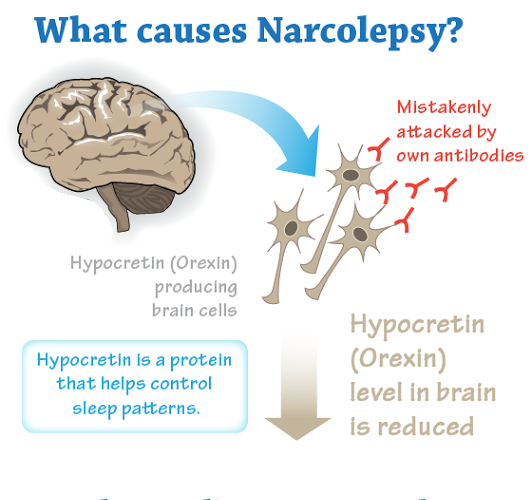
Many people with narcolepsy remain stable over time. In some cases, some symptoms may improve with the age of the patient, and rarely remission of symptoms may occur spontaneously. While experts do not know why the disease proceeds differently in different people.
The treatment of NT1 and NT2 is similar, except that NT2 does not involve the potential use of any medication for cataplexy.
A combination of medical and behavioral approaches can significantly reduce but not eliminate symptoms. Some level of EDS usually persists despite treatment. All treatments should be carried out under the guidance of a physician who can best tailor the treatment plan to the patient's particular situation.
Behavioral approaches to treatment
Behavioral approaches are non-medical forms of therapy and there are several ways they can be incorporated into the daily habits of people with narcolepsy.
- Scheduling naps: Because naps are refreshing for people with narcolepsy, nap time can reduce EDS.
 It may take school or work to find time to sleep.
It may take school or work to find time to sleep. - Maintaining healthy sleep hygiene: To combat poor sleep at night, people with narcolepsy can benefit from good sleep. Good sleep hygiene includes a consistent sleep schedule (before bed and wake up), a sleep environment with minimal distractions and disturbances, and limited use of electronic devices before bed.
- Avoiding alcohol and other sedatives: Any substance that causes drowsiness can aggravate the symptoms of daytime narcolepsy.
- Drive with care: People with narcolepsy should talk to their doctor about safe driving. Taking a nap before driving and avoiding long or repetitive journeys are examples of safety measures.
- Eating a balanced diet: People with narcolepsy have a higher risk of obesity, making proper nutrition an important part of their overall health.
- Implementation: An active lifestyle can help prevent obesity and improve sleep at night.

- Seeking support: Support groups and mental health professionals can promote emotional health and counteract the risks of social withdrawal, depression, and anxiety in people with narcolepsy.
Medications
While behavioral approaches are often helpful, most people with narcolepsy are also treated with medications that help control one or more symptoms.
Drugs for narcolepsy often improve symptoms, but they can also cause side effects. These medicines require a prescription and must be used carefully and as instructed by your doctor and pharmacist.
Some of the most commonly prescribed drugs for narcolepsy include:
- Modafinil and armodafinil: These two wakefulness drugs are chemically similar and are typically the first drug for treating SED.
- Methylphenidate: This is a type of amphetamine that can reduce EDS.
- Solriamphetol: This drug was approved by the FDA in 2019 and has shown comparable effects on EDS as modafinil.
- Sodium oxybate: This medicine may reduce cataplexy, EDS and nighttime sleep disturbances, but it may take weeks for EDS to be affected.
- Pitolysant: FDA-approved in 2019, Pitolysant is a wakefulness drug that also has a positive effect on cataplexy.
Not all medicines work for all patients, and some patients may experience more unpleasant side effects or interactions with other medicines. Working closely with your doctor can help determine the drug and dosage with the best balance of benefits and drawbacks.
Treatment of narcolepsy and children
Treatment of narcolepsy in children is similar to that in adults, but additional precautions may be taken in drug selection and dosage. Cardiovascular screening is recommended by the American Academy of Pediatrics before children start taking stimulant medications.
Treatment of narcolepsy and pregnancy
There is limited safety data for most drugs used to treat narcolepsy in pregnant, trying to conceive, or breastfeeding women.