Mood disorders defined
Mood Disorders | Johns Hopkins Medicine
A mood disorder is a mental health class that health professionals use to broadly describe all types of depression and bipolar disorders.
Children, teens, and adults can have mood disorders. However, children and teens don’t always have the same symptoms as adults. It’s harder to diagnose mood disorders in children because they aren’t always able to express how they feel.
Therapy, antidepressants, and support and self-care can help treat mood disorders.
What are the different types of mood disorders?
These are the most common types of mood disorders:
-
Major depression. Having less interest in usual activities, feeling sad or hopeless, and other symptoms for at least 2 weeks may indicate depression.
-
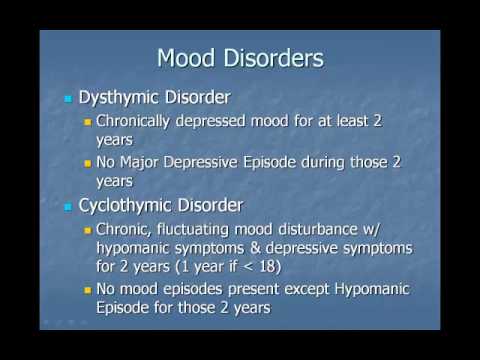
Dysthymia. This is a chronic, low-grade, depressed, or irritable mood that lasts for at least 2 years.
-
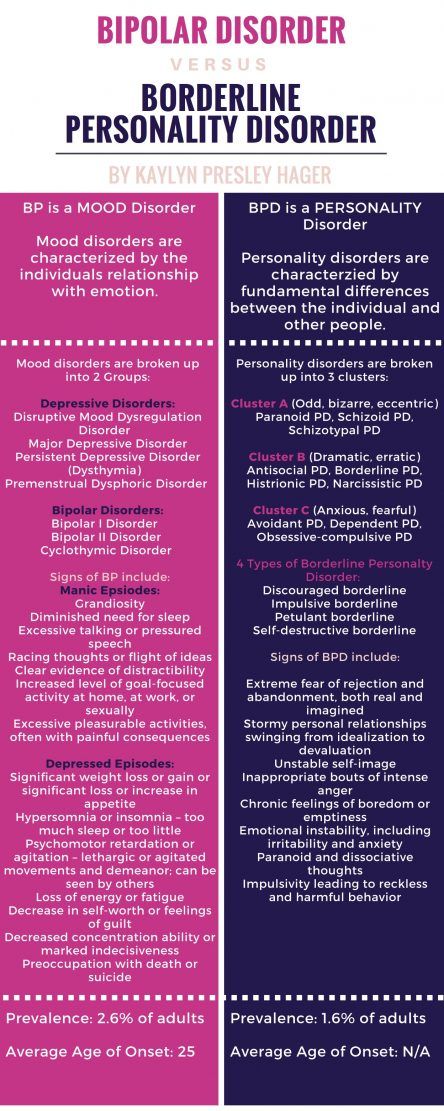
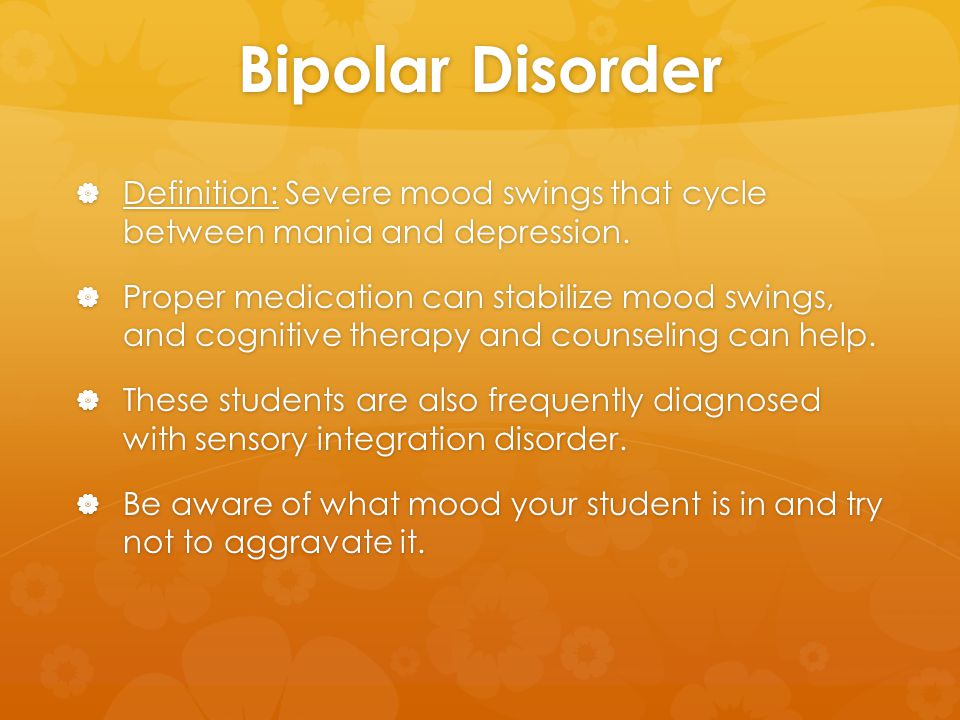
Bipolar disorder.
This is a condition in which a person has periods of depression alternating with periods of mania or elevated mood.
-
Mood disorder related to another health condition. Many medical illnesses (including cancer, injuries, infections, and chronic illnesses) can trigger symptoms of depression.
-
Substance-induced mood disorder. Symptoms of depression that are due to the effects of medicine, drug abuse, alcoholism, exposure to toxins, or other forms of treatment.
What causes mood disorders?
Many factors contribute to mood disorders. They are likely caused by an imbalance of brain chemicals. Life events (such as stressful life changes) may also contribute to a depressed mood. Mood disorders also tend to run in families.
Who is at risk for mood disorders?
Anyone can feel sad or depressed at times. However, mood disorders are more intense and harder to manage than normal feelings of sadness. Children, teens, or adults who have a parent with a mood disorder have a greater chance of also having a mood disorder. However, life events and stress can expose or worsen feelings of sadness or depression. This makes the feelings harder to manage.
Children, teens, or adults who have a parent with a mood disorder have a greater chance of also having a mood disorder. However, life events and stress can expose or worsen feelings of sadness or depression. This makes the feelings harder to manage.
Sometimes, life's problems can trigger depression. Being fired from a job, getting divorced, losing a loved one, death in the family, and financial trouble, to name a few, all can be difficult and coping with the pressure may be troublesome. These life events and stress can bring on feelings of sadness or depression or make a mood disorder harder to manage.
The risk of depression in women is nearly twice as high as it is for men. Once a person in the family has this diagnosis, their brothers, sisters, or children have a higher chance of the same diagnosis. In addition, relatives of people with depression are also at increased risk for bipolar disorder .
Once a person in the family has a diagnosis of bipolar disorder, the chance for their brothers, sisters, or children to have the same diagnosis is increased.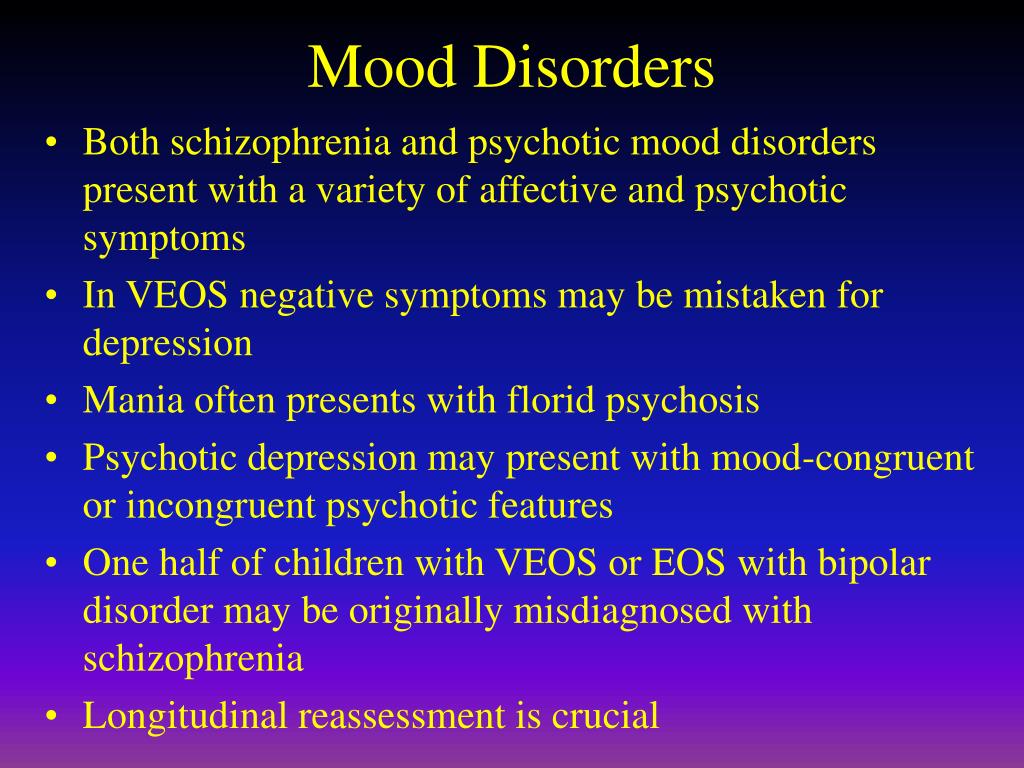 Relatives of people with bipolar are also at increased risk for depression.
Relatives of people with bipolar are also at increased risk for depression.
What are the symptoms of mood disorders?
Depending on age and the type of mood disorder, a person may have different symptoms of depression. The following are the most common symptoms of a mood disorder:
-
Ongoing sad, anxious, or “empty” mood
-
Feeling hopeless or helpless
-
Having low self-esteem
-
Feeling inadequate or worthless
-
Excessive guilt
-
Repeating thoughts of death or suicide, wishing to die, or attempting suicide (Note: People with this symptom should get treatment right away!)
-
Loss of interest in usual activities or activities that were once enjoyed, including sex
-
Relationship problems
-
Trouble sleeping or sleeping too much
-
Changes in appetite and/or weight
-
Decreased energy
-
Trouble concentrating
-
A decrease in the ability to make decisions
-
Frequent physical complaints (for example, headache, stomachache, or tiredness) that don’t get better with treatment
-
Running away or threats of running away from home
-
Very sensitive to failure or rejection
-
Irritability, hostility, or aggression
In mood disorders, these feelings are more intense than what a person may normally feel from time to time.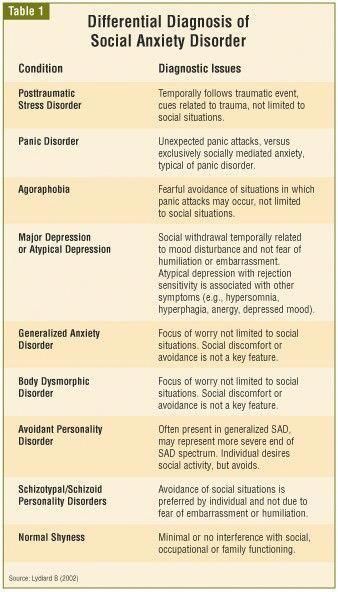 It’s also of concern if these feelings continue over time, or interfere with one's interest in family, friends, community, or work. Any person who expresses thoughts of suicide should get medical help right away.
It’s also of concern if these feelings continue over time, or interfere with one's interest in family, friends, community, or work. Any person who expresses thoughts of suicide should get medical help right away.
The symptoms of mood disorders may look like other conditions or mental health problems. Always talk with a healthcare provider for a diagnosis.
How are mood disorders diagnosed?
Mood disorders are a real medical disorder. A psychiatrist or other mental health professional usually diagnoses mood disorders through a complete medical history and psychiatric evaluation.
How are mood disorders treated?
Mood disorders can often be treated with success. Treatment may include:
-
Antidepressant and mood stabilizing medicines—especially when combined with psychotherapy have shown to work very well in the treatment of depression
-
Psychotherapy—most often cognitive-behavioral and/or interpersonal therapy.
 This therapy is focused on changing the person’s distorted views of himself or herself and the environment around him or her. It also helps to improve interpersonal relationship skills, and identifying stressors in the environment and how to avoid them
This therapy is focused on changing the person’s distorted views of himself or herself and the environment around him or her. It also helps to improve interpersonal relationship skills, and identifying stressors in the environment and how to avoid them -
Family therapy
-
Other therapies, such as electroconvulsive therapy and transcranial stimulation
Families play a vital supportive role in any treatment process.
When correctly diagnosed and treated, people with mood disorders can live, stable, productive, healthy lives.
Can mood disorders be prevented?
At this time, there are no ways to prevent or reduce the incidence of mood disorders. However, early diagnosis and treatment can reduce the severity of symptoms, enhance the person’s normal growth and development, and improve the quality of life of people with mood disorders.
Key points about mood disorders
-
A mood disorder is a mental health class that health professionals use to broadly describe all types of depression and bipolar disorders.
-
The most common types of mood disorders are major depression, dysthymia (dysthymic disorder), bipolar disorder, mood disorder due to a general medical condition, and substance-induced mood disorder.
-
There is no clear cause of mood disorders. Healthcare providers think they are a result of chemical imbalances in the brain. Some types of mood disorders seem to run in families, but no genes have yet been linked to them.
-
In general, nearly everyone with a mood disorder has ongoing feelings of sadness, and may feel helpless, hopeless, and irritable. Without treatment, symptoms can last for weeks, months, or years, and can impact quality of life.
-
Depression is most often treated with medicine, psychotherapy or cognitive behavioral therapy, family therapy, or a combination of medicine and therapy. In some cases, other therapies, such as electroconvulsive therapy and transcranial stimulation may be used.
Bipolar Disorder | Johns Hopkins Medicine
What is bipolar disorder?
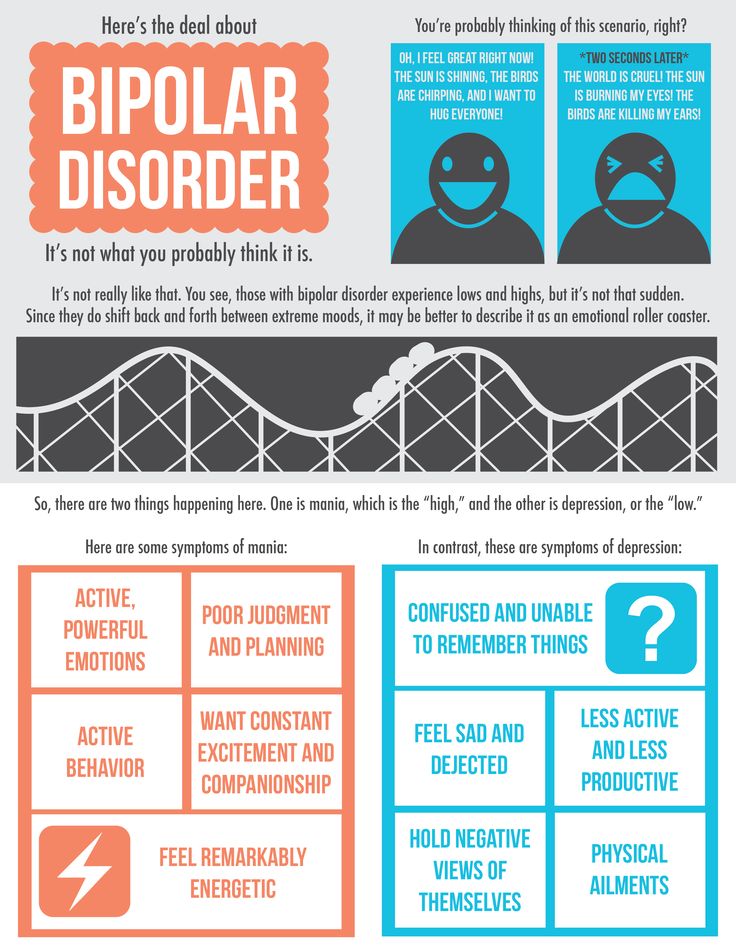
Bipolar disorder is a mood disorder. It causes a person to have cycles of extreme mood changes that go beyond normal ups and downs. A person with this disorder will have periods of feeling joyful, energized, and excited (called mania). These are followed by periods of feeling sad and depressed. For this reason, it’s also called manic depression.
Depression affects your body, mood, and thoughts. It also affects how you eat and sleep, think about things, and feel about yourself. It’s not the same as being unhappy or in a blue mood. It’s not a sign of weakness or a condition that can be willed away. Treatment is often needed and is key to recovery.
Bipolar disorder affects equal numbers of men and women. But women tend to have more symptoms of depression than of mania. This disorder often begins in the teens or early adulthood.
What causes bipolar disorder?
The cause of bipolar disorder is not known.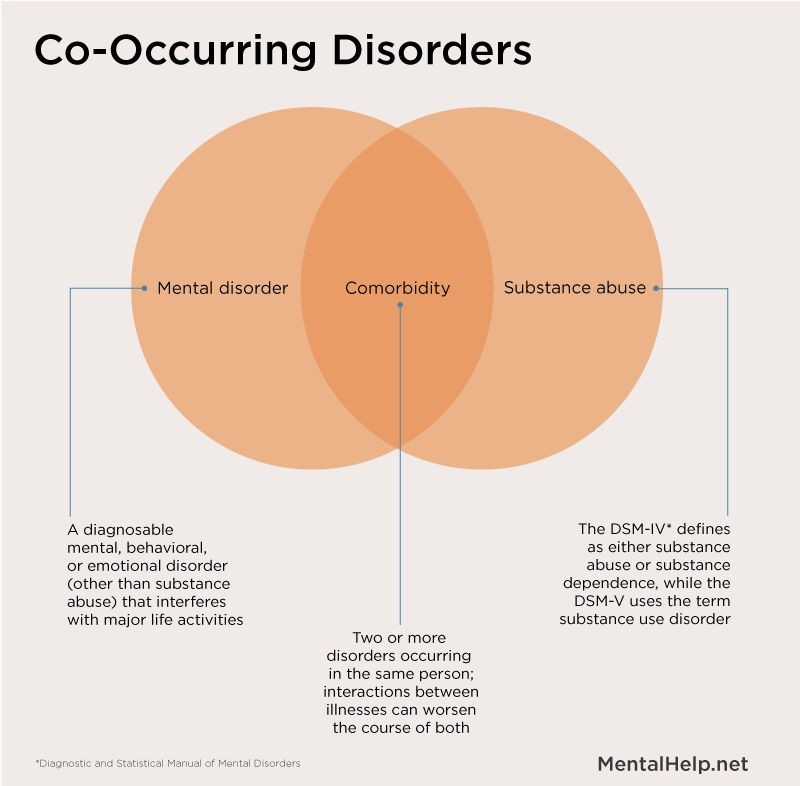 Experts agree many factors seem to play a role. This includes environmental, psychological, and genetic factors.
Experts agree many factors seem to play a role. This includes environmental, psychological, and genetic factors.
Bipolar disorder tends to run in families. Researchers are still trying to find genes that may be linked to it.
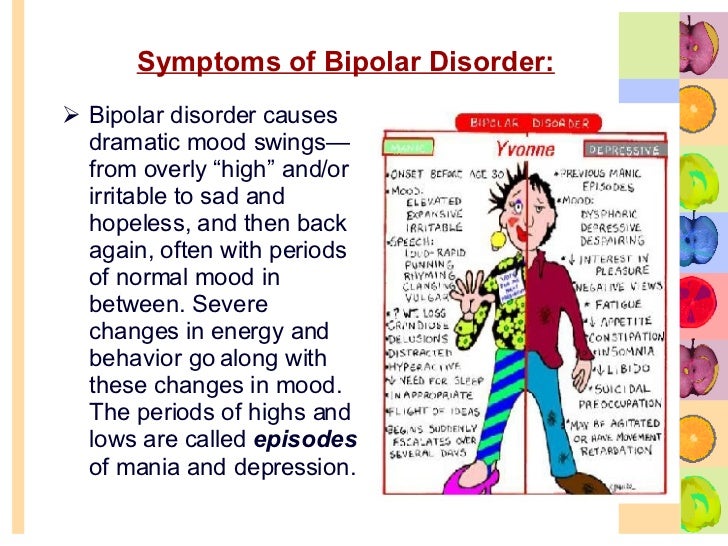
What are the symptoms of bipolar disorder?
Each person may have different symptoms. The following are the most common symptoms:
Depressive symptoms may include:
Constant sad, anxious, or empty mood
Loss of interest in things that you once enjoyed, including sex
Feeling restless or irritable
Inability to focus, think, or make decisions
Low energy, fatigue, being slowed down
Keep having thoughts of death or suicide, wishing to die, or attempting suicide (Note: People with this symptom should get treatment right away)
Feeling worthless or hopeless
Feeling undue guilt
Changes in eating habits, eating too much or not enough
Changes in sleep patterns, such as fitful sleep, inability to sleep, waking up very early, or sleeping too much
Headaches, digestive problems, or chronic pain
Manic symptoms may include:
Inflated self-esteem
Need for less rest and sleep
Easily distracted or irritable
Racing thoughts
Physical agitation
Risky, aggressive, or destructive behavior
Talking a lot and talking fast
Excessive high or euphoric feelings (feeling overly happy)
Increased sex drive
Increased energy
Unusual poor judgment (for instance, buying sprees or sexual indiscretion)
Increased denial
How is bipolar disorder diagnosed?
To diagnose bipolar, your healthcare provider will ask about your symptoms.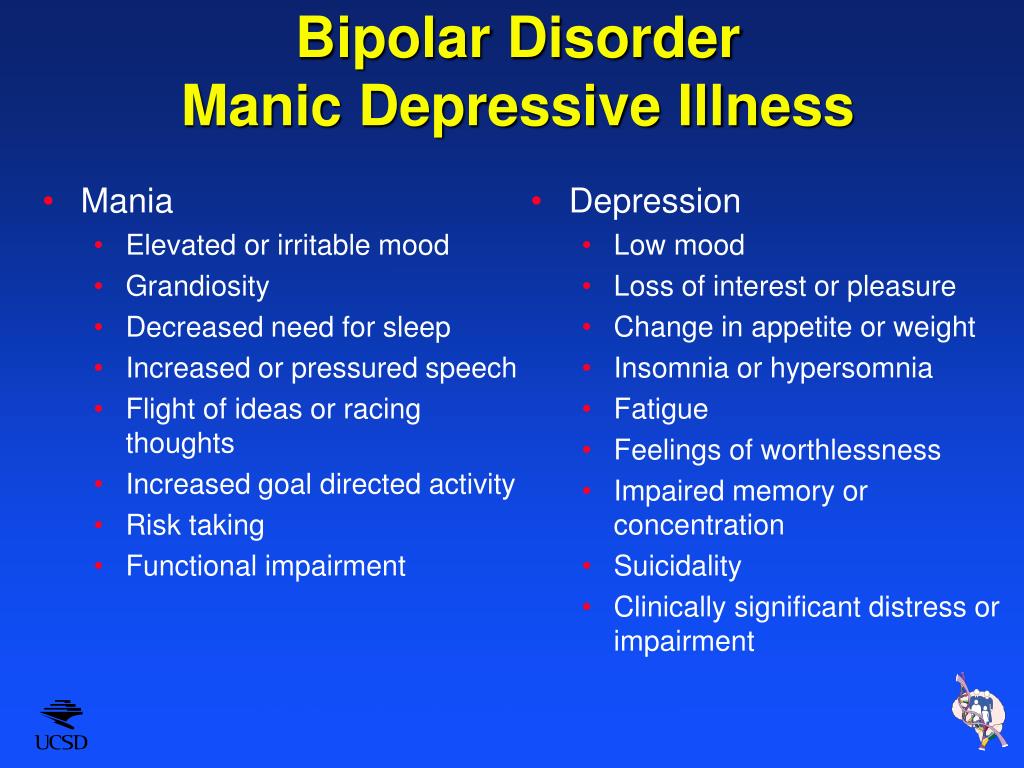 You may have both depressive and manic symptoms to a varying degree. The symptoms of bipolar disorder may look like other mental health conditions.
You may have both depressive and manic symptoms to a varying degree. The symptoms of bipolar disorder may look like other mental health conditions.
Always see a healthcare provider for a diagnosis. A diagnosis is made after a careful psychiatric exam and medical history done by a mental health professional.
How is bipolar disorder treated?
There is no cure for bipolar disorder, but treatment works well for many people. Treatment may include one or a combination of the following:
Medicine. Many different medicines are available for bipolar disorder. But, it often takes 4 to 6 weeks for anti-depressants to have a full effect. So it’s important to keep taking the medicine, even if it doesn’t seem to be working at first. It’s also important to talk to your healthcare provider before stopping. Some people have to switch medicines or add medicines to get results.
Therapy. This is most often cognitive-behavioral or interpersonal therapy.
 It focuses on changing the distorted views you have of yourself and your environment. It works to improve your interpersonal relationship skills. It also helps you identify stressors and learn how to manage them.
It focuses on changing the distorted views you have of yourself and your environment. It works to improve your interpersonal relationship skills. It also helps you identify stressors and learn how to manage them.Electroconvulsive therapy (ECT). This treatment may be used in people with severe, life-threatening depression that has not responded to medicines. A brief electrical current is passed through the brain, triggering a mild seizure. For unknown reasons, this helps restore the normal balance of chemicals in the brain and ease symptoms.
In most cases, consistent, long-term treatment is needed to stabilize the mood swings.
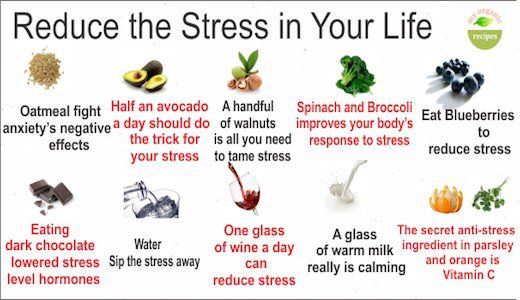
Self care
You can also take steps to help yourself. During periods of depression, consider the following:
Get help. If you think you may be depressed, see a health professional right away.
Set realistic goals and don’t take on too much.
Break large tasks into small ones.
 Set priorities, and do what you can as you can.
Set priorities, and do what you can as you can.Try to be with other people and confide in someone. This is usually better than being alone and secretive.
Do things that make you feel better. Going to a movie, gardening, or taking part in religious, social, or other activities may help. Doing something nice for someone else can also help you feel better.
Get regular exercise.
Expect your mood to get better slowly, not right away. Feeling better takes time.
Eat healthy, well-balanced meals.
Avoid alcohol and drugs. These can make depression worse.
It’s best to postpone big decisions until the depression has lifted. Before making big decisions (changing jobs, getting married or divorced), discuss it with others who know you well and have a more objective view of your situation.
People don’t snap out of a depression. But with treatment they can feel a little better day by day.
Try to be patient and focus on the positives. This may help replace the negative thinking that is part of the depression and the negative thoughts will disappear as your depression responds to treatment.
Let your family and friends help you.
Key points
Bipolar disorder causes cycles of extreme mood changes that go beyond life's regular ups and downs. Treatment is key to recovery.
There is no clear cause of bipolar disorder. Mental health experts think it’s a result of chemical imbalances in the brain. It seems to run in families, but no genes have yet been linked to it.
It causes unusual mood swings. A person will have periods of extreme joy, elevated mood, or irritability (called mania). This switches with periods of depression.
Bipolar disorder may be diagnosed after a careful psychiatric exam and medical history done by a mental health professional.
It is most often treated with medicine, therapy, or a combination of both.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.
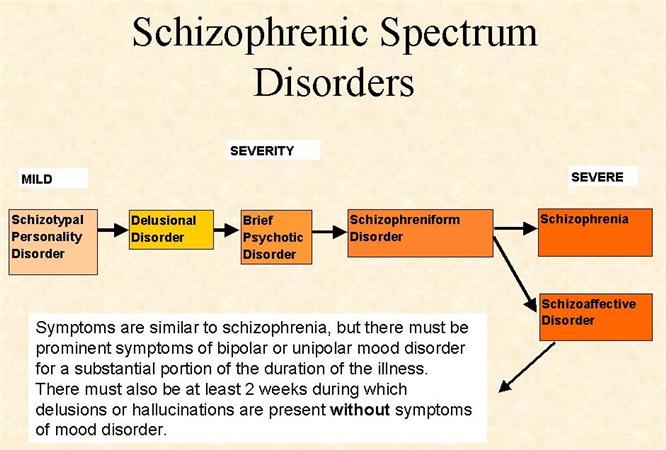
Affective disorders
Emotional disorders are a group of mental illnesses characterized by emotional changes in depression and elevation. Includes various forms of depression and manic psychiatrist manic depression, emotional instability, anxiety and discomfort. Musical disorders were accompanied by a decrease, an increase in the amount of activity of the whole body and autonomic nervous symptoms. Specific diagnostics include interviews, observations, experimental tests, and psychological tests of psychiatrists. Treatment includes drug therapy (antidepressant, anxiolytic, citation) and psychotherapy.
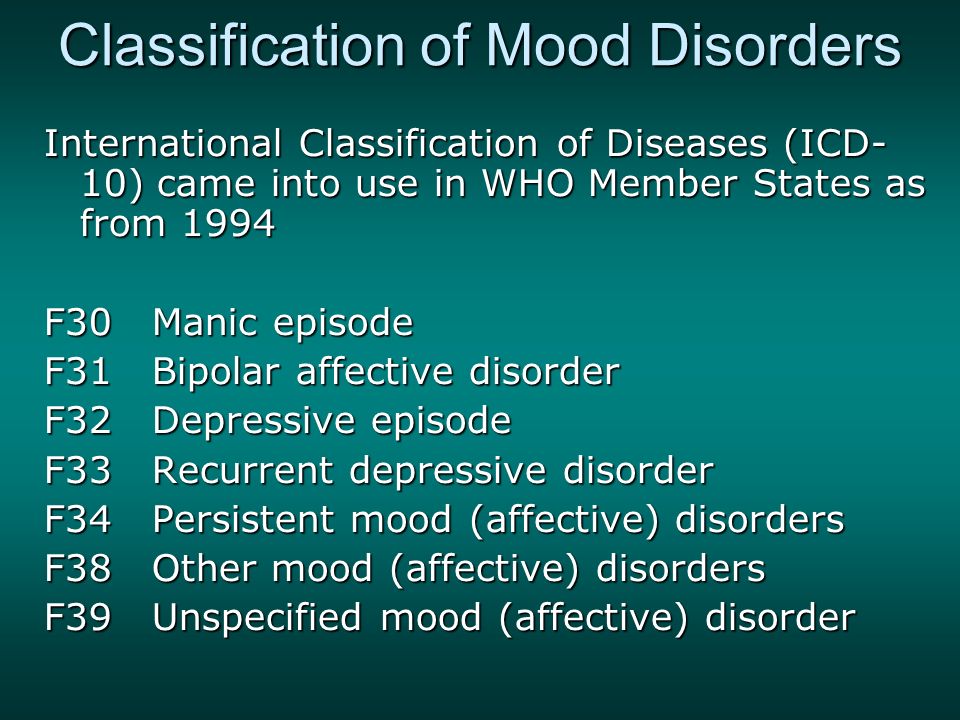
ICD-10
General information
Synonyms for emotional disorders are emotional disorders and mood disorders. Not only as an independent mental illness, but also as a complication of neurological illnesses and other physical illnesses, his illness is significant. This has led to the difficulty of diagnosis. People view depression, anxiety, and frustration as a temporary symptom according to the situation. According to statistics, 25% of the population experienced various mental disorders, but only one of them was eligible. Depending on the type of depression, it is seasonal, and in many cases the illness worsens in the winter.
This has led to the difficulty of diagnosis. People view depression, anxiety, and frustration as a temporary symptom according to the situation. According to statistics, 25% of the population experienced various mental disorders, but only one of them was eligible. Depending on the type of depression, it is seasonal, and in many cases the illness worsens in the winter.
Causes
Emotional disorders are caused by external and internal causes. There are neuropathy, endogenous and symptoms. In each case, there is a certain fact that leads to the formation of emotional disorders, such as unbalanced anxiety disease and divisional pathological personality of the central nervous system. Determination of the onset and progress of this disease is classified into several groups.
- Psychogenic harmful factors. Emotional disorders can be caused by psychological trauma or prolonged stress. The most common causes are the death of loved ones (spouses, parents, children), quarrels, domestic violence, divorce, and financial stability.
- Constitutional disease. Complications of other diseases can cause emotional distress. Dysfunction of the internal divisional gland, which produces the nervous system, hormones, and neurotransmitters, is the direct cause. In addition, mood worsens for reasons such as severe symptoms (pain, weakness) and poor disease prognosis (more likely to die).
- Genetic priority. Anomalies in emotional responses may be related to genetic physiological causes, specificity of brain structure, rate of neurotransugography, and goal-directed consciousness. For example, Bipolar Emotional Disorder.
- Natural hormones have unstable endocrine effects on pregnancy, childbirth, adolescence and menopause. Hormonal imbalance affects the function of the emotional response of the brain.
Pathogenesis
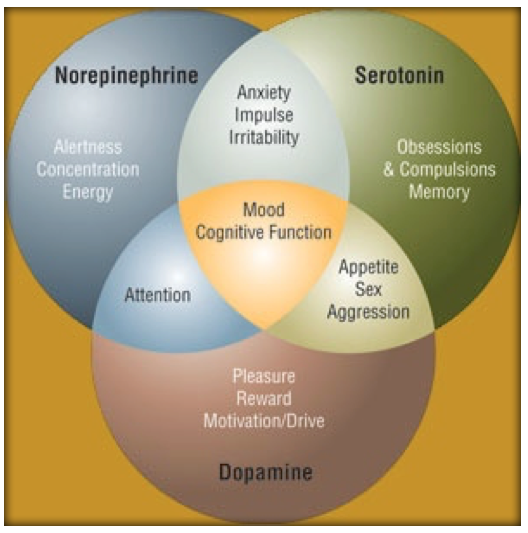
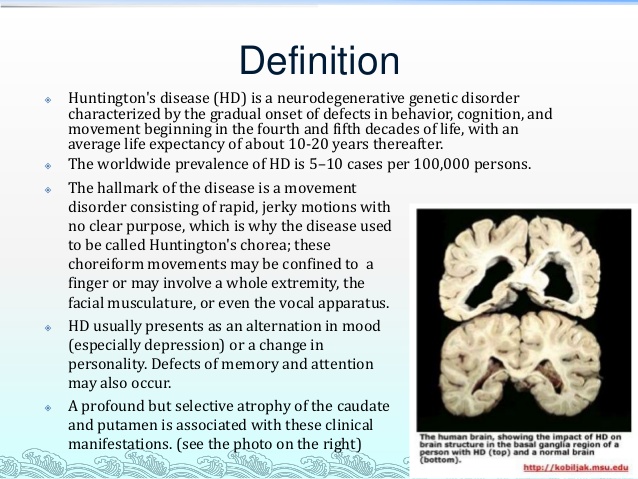
The pathological basis of most emotional disorders is a disorder of the bone edge, sides and hypophagosis, hypophagosis, and the synthesis of the synthesis of serotonin, norepinephrine and dopamine, a neurorotransmitter.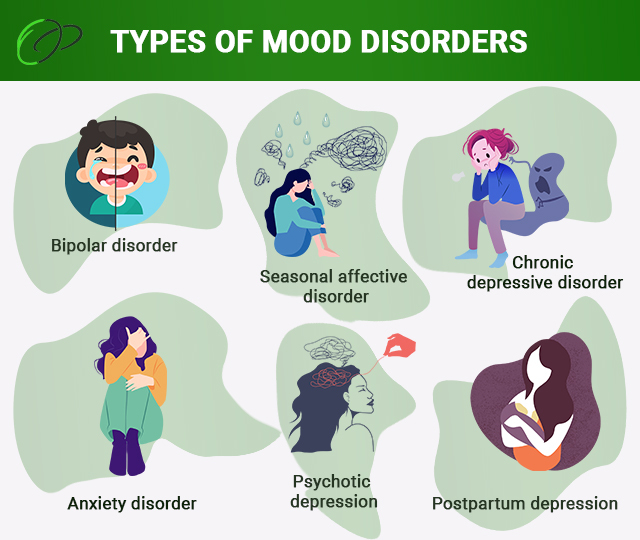 Serotonin allows the body to effectively deal with stress and reduce anxiety. If the production of serotonin is insufficient or the sensitivity of a certain receptor is reduced, depression becomes depressed. Noruepinephrine supports the level of awakening and cognitive activity of the body, helping to cope with exposure, stress and danger. The absence of this catecholamine causes lack of concentration, anxiety, increased mental motor agitation, and sleep disturbances.
Serotonin allows the body to effectively deal with stress and reduce anxiety. If the production of serotonin is insufficient or the sensitivity of a certain receptor is reduced, depression becomes depressed. Noruepinephrine supports the level of awakening and cognitive activity of the body, helping to cope with exposure, stress and danger. The absence of this catecholamine causes lack of concentration, anxiety, increased mental motor agitation, and sleep disturbances.
If dopamine works enough, you will be able to switch attention and emotions, and you will be able to correct muscle movements. Absence becomes lethargic and indifferent, as well as excessive mental stress and excitement. When neurotransmitter balance is lost, it affects the brain structure that controls emotions. Emotional disorders can be caused by external factors such as stress, internal factors such as disease, and inherited biochemical processes.
Classification
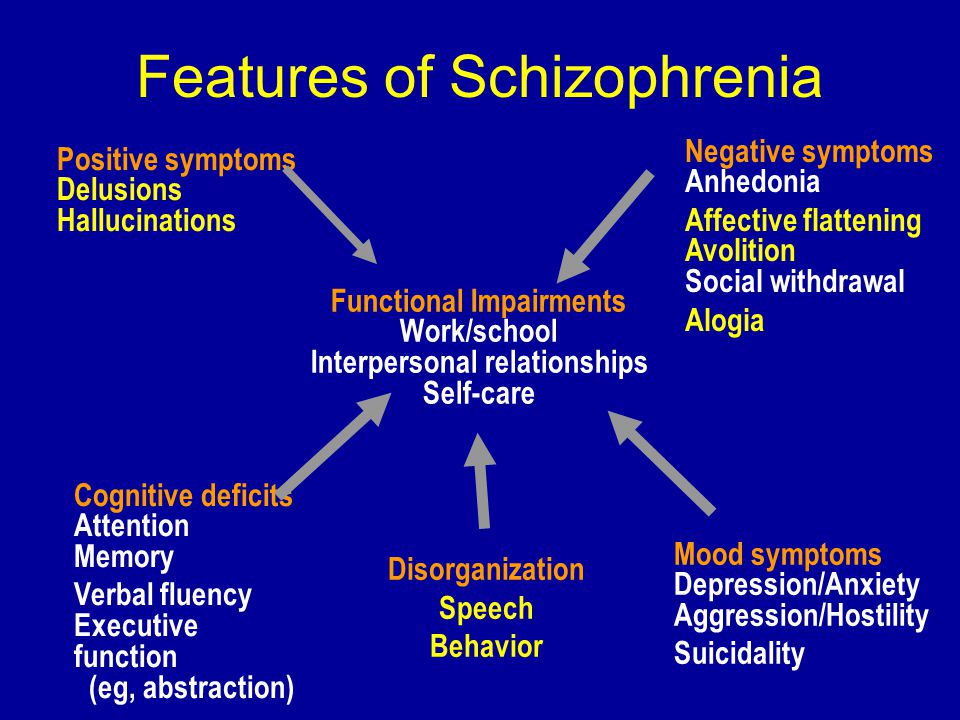
Psychiatric treatment is widely used to classify emotional disorders from clinical symptoms.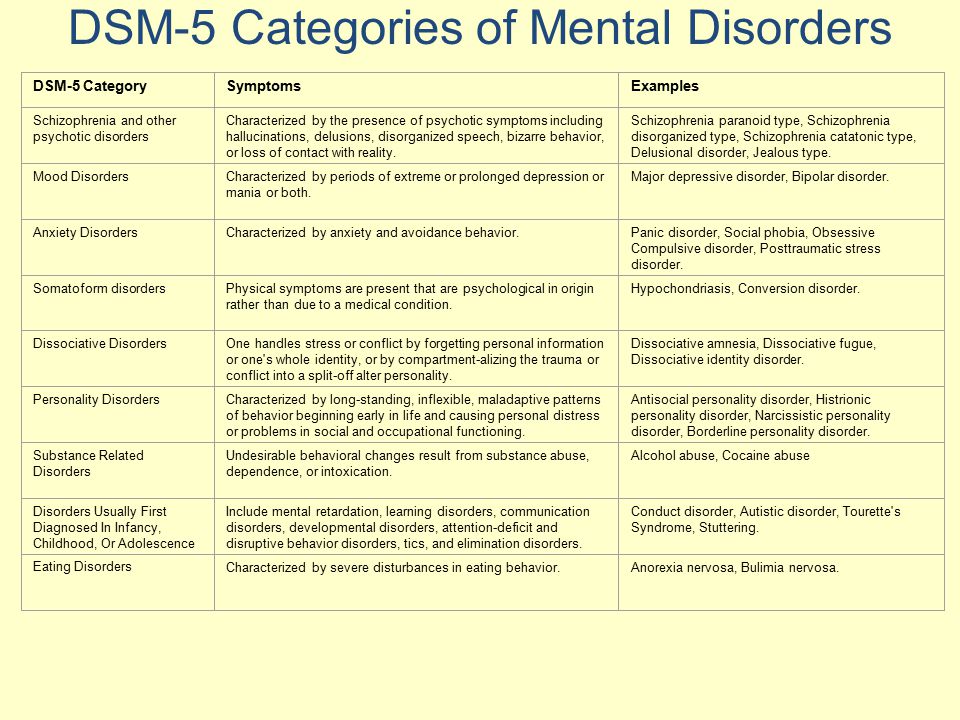 This is different from depression disorder, manic disorder, anxiety disorder, and bipolar disorder. The main classification is based on aspects of various emotional reactions. This is different from.
This is different from depression disorder, manic disorder, anxiety disorder, and bipolar disorder. The main classification is based on aspects of various emotional reactions. This is different from.
- Those who are too disturbed in emotional expression are called emotional hypersensitivity, weakness. This group includes sensitivity, emotional coldness, emotional poverty and lethargy.
- Emotional suitable obstacle. In a dual built simultaneously in different directions, there is another direction, so normal reactions can be made to surrounding events. Unsupported is characterized by a discrepancy between the quality (direction) of the strike and the stimulus that influences it. Example: I feel laughter and joy at tragic news.
- Emotional stability disorder. Emotional unstable indicates an increase in emotional arousal with unreasonable fluctuations, outburst, anger and aggression. In bearish fluctuating emotions such as tears, sentimental, freaky and irritable.
Symptoms of affective disorders
The clinical image of this disease is determined by this form. The main symptoms of depression are "depression", which has a long-term sadness and depressing mood, and "an indifferent state", which is not interested in others. Patients experience despair, meaninglessness, their own incompetence and uselessness. Mild depression is characterized by decreased work ability, fatigue, tears, anorexia, and sleep disturbances.
Moderate depression is characterized by an inability to perform adequate work and household chores, increased feelings of fatigue and lethargy. They spend more time at home, prefer loneliness to communication, avoid physical and mental activity, often cry. Suicidal thoughts may occur, causing excessive drowsiness and insomnia, loss of appetite. Severe depression causes people to spend most of their time in bed, uninterested in events and unable to make any effort to eat and take care of their hygiene.
Another clinical form is masked depression.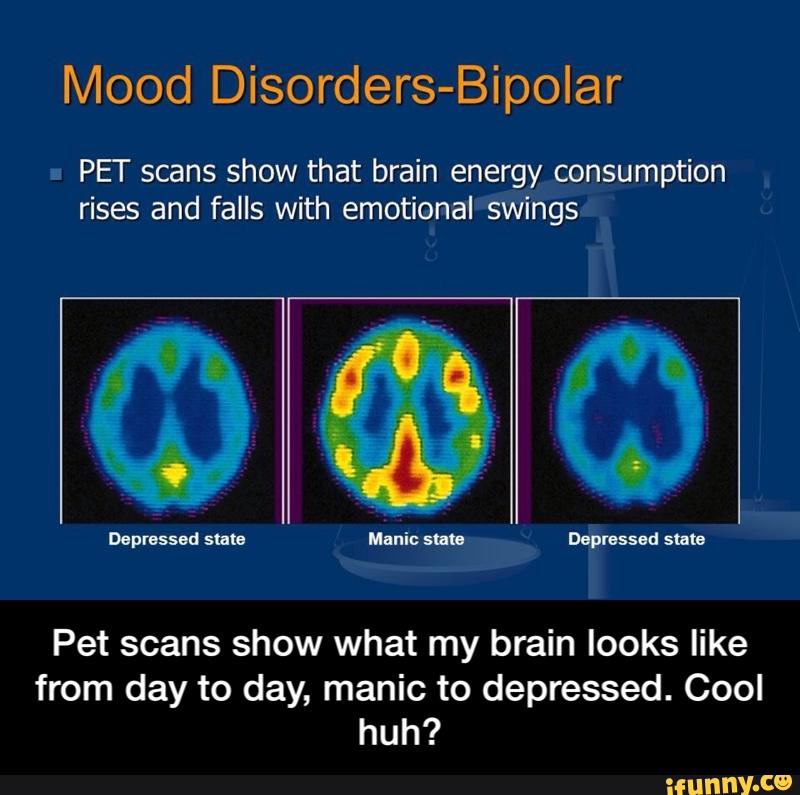 It is characterized by the denial of pain and depression and the absence of external signs of emotional distress. At the same time, somatic symptoms develop, such as headache, arthralgia, muscle pain, weakness, dizziness, nausea, shortness of breath, fluctuations in blood pressure, tachycardia, and digestive disorders. In many cases, the disease is not detected, even if the doctor checks the improvement of the constitution, and the medicine does not work. Depression is diagnosed at a later stage than classical depression. At this point, the patient begins to experience a vague feeling of restlessness, restlessness and restlessness, losing interest in favorite activities.
It is characterized by the denial of pain and depression and the absence of external signs of emotional distress. At the same time, somatic symptoms develop, such as headache, arthralgia, muscle pain, weakness, dizziness, nausea, shortness of breath, fluctuations in blood pressure, tachycardia, and digestive disorders. In many cases, the disease is not detected, even if the doctor checks the improvement of the constitution, and the medicine does not work. Depression is diagnosed at a later stage than classical depression. At this point, the patient begins to experience a vague feeling of restlessness, restlessness and restlessness, losing interest in favorite activities.
In mania, the mood is unnaturally elevated, the pace of thought and speech is fast, the behavior is irritable, facial expressions reflect joy or excitement. Patients are optimistic, always joking, witty, downplay problems and cannot carry on serious conversations. Energetic gestures, frequent change of position, standing up.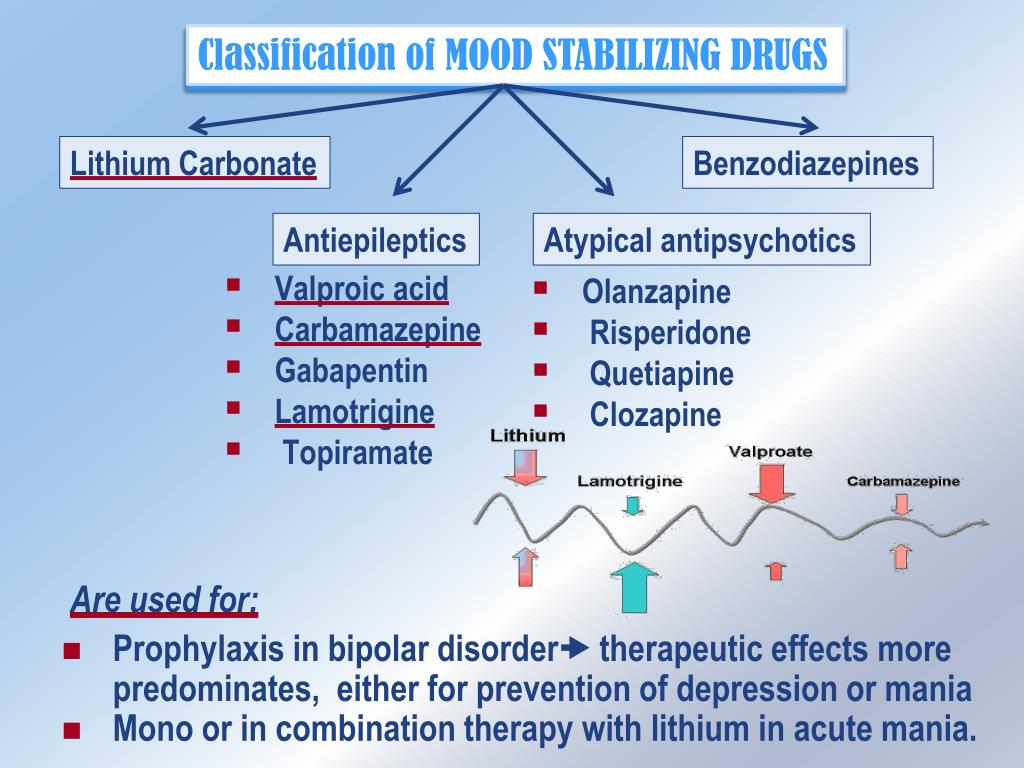 Poor mental concentration: Patients often become distracted, ask questions, and abandon activities they have just begun, replacing them with more interesting ones. Fear subsides, vigilance weakens, strength and courage appear. All difficulties seem trivial, problems seem solvable. Increased libido and appetite, reduced need for sleep. As the disorder worsens, irritability increases, unmotivated aggression, delusions and hallucinations may occur. Bipolar affective disorder is characterized by cyclic episodes of alternating mania and depression. When the symptoms are mild, it is called cyclothymia.
Poor mental concentration: Patients often become distracted, ask questions, and abandon activities they have just begun, replacing them with more interesting ones. Fear subsides, vigilance weakens, strength and courage appear. All difficulties seem trivial, problems seem solvable. Increased libido and appetite, reduced need for sleep. As the disorder worsens, irritability increases, unmotivated aggression, delusions and hallucinations may occur. Bipolar affective disorder is characterized by cyclic episodes of alternating mania and depression. When the symptoms are mild, it is called cyclothymia.
Anxiety disorders are characterized by persistent feelings of unease, tension and fear. Patients anticipate a negative event, but its probability is usually very small. In severe cases, anxiety develops into agitation, manifested by psychomotor agitation in the form of restlessness, hand tremors and walking around the room. The patient tries to find a comfortable position or a quiet place, but in vain.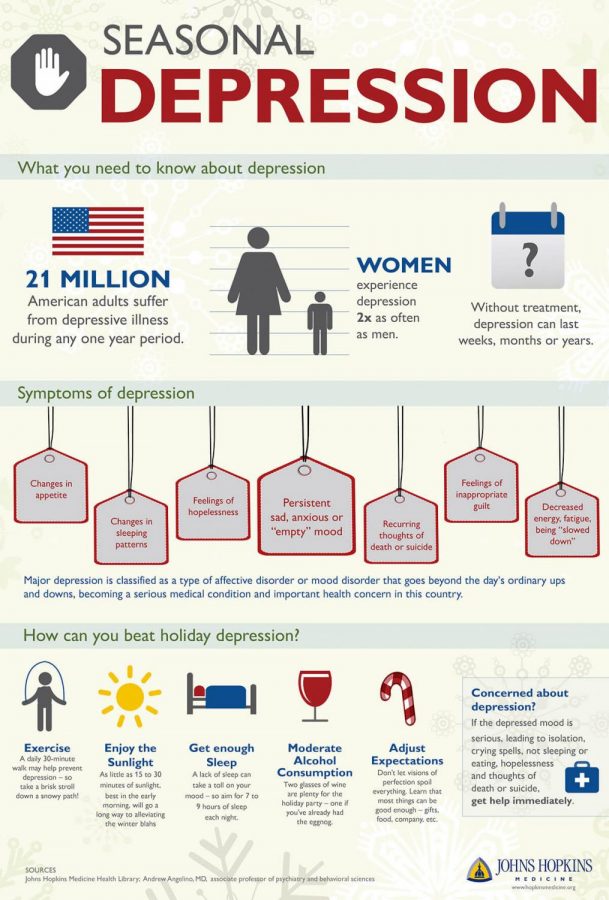 Increased anxiety is accompanied by panic attacks with autonomic symptoms such as shortness of breath, dizziness, dyspnoea, and nausea. Frightening thoughts appear, appetite and sleep are disturbed.
Increased anxiety is accompanied by panic attacks with autonomic symptoms such as shortness of breath, dizziness, dyspnoea, and nausea. Frightening thoughts appear, appetite and sleep are disturbed.
Complications
Prolonged emotional disturbance without appropriate treatment significantly reduces the patient's quality of life. Mild emotional illnesses inhibit occupational functions—depressions reduce the amount of work done, and manic and anxiety disorders reduce the quality of work. Avoid communication with colleagues and clients, causing conflicts with increased irritability, and control is ineffective. In severe depression, there is a risk of suicide with a suicide attempt. Such patients should be constantly monitored by relatives and medical personnel.
Diagnostics
Psychiatrists examine the patient's medical history and mental illness. To clarify the exact nature of symptoms, onset and relationship between mental trauma and stress status, clinical interviews with patients can provide more complete and objective information (patients have their own). You may be unresolved or stunned by the state). If there is no remarkable psychogenic factor in the progression of the pathology, a neurologist, endocrine department or general practitioner will be appointed to investigate the true cause. The specific survey method is as follows.
You may be unresolved or stunned by the state). If there is no remarkable psychogenic factor in the progression of the pathology, a neurologist, endocrine department or general practitioner will be appointed to investigate the true cause. The specific survey method is as follows.
- Status of clinical interviews. In talking to the patient, the psychiatrist knows the symptoms of anxiety and identifies a way of speaking to show emotional disturbances. In the case of depression, the patient speaks slowly, inaccurately and answers the question in one way. In the case of mania, she becomes talkative and uses flashy derogatory names and humor to quickly change the subject. Anxiety is characterized by embarrassed performance, irregular pace, and decreased concentration.
- I'm watching. Observation of emotions and behavioral expressions is often done naturally. Physicians evaluate the patient's facial expression, gesture characteristics, motor skill activity and purpose, and plant symptoms.
 Standard facial expression patterns include a quick (detailed analysis of the express facial test). As a result, signs of depression - drop in the corner of the mouth and outer corner of the eye, accompanying wrinkles, painful expression, rigidity of movement, a sign of mania - increased muscle tension, external muscles and facial muscle tension.。
Standard facial expression patterns include a quick (detailed analysis of the express facial test). As a result, signs of depression - drop in the corner of the mouth and outer corner of the eye, accompanying wrinkles, painful expression, rigidity of movement, a sign of mania - increased muscle tension, external muscles and facial muscle tension.。 - Psychological and physiological tests are implemented to assess mental and physiological tension, expression and stability of emotions, direction and quality. A.M. Checking the COLOR OF RESPONSIBILITY ETIKIND, I. G. Weseskark "Difference in meaning", A.R.'s conjugate motion operation was used. Luria. In this test, mental and emotional disorders are confirmed by an intolerable system of accepting color, language and associations. The result is interpreted individually.
- projection method. These methods are aimed at studying emotions through the prism of unconscious personality characteristics, personality characteristics and social relationships.
 The specific theme recognition test, the Rosenzwicke frustration test, the Shirch roll test, the "draw a person" test, and the "draw a person in the rain" test are applied. As a result, depression, manic, anxiety, aggressive tendencies, impulsiveness, antisocial and frustration were confirmed, causing emotional deviation.
The specific theme recognition test, the Rosenzwicke frustration test, the Shirch roll test, the "draw a person" test, and the "draw a person in the rain" test are applied. As a result, depression, manic, anxiety, aggressive tendencies, impulsiveness, antisocial and frustration were confirmed, causing emotional deviation. - Post questionnaire. The method is based on the ability of self-reports, that is, the patient to evaluate their emotions, personality characteristics, health status and interpersonal characteristics. Typically using a narrow sensory test (Beck Depression Questionnaire, Depression Questionnaire) and complex emotional methods (Derogatis, MMPI (SMIL), Eysenck test) to diagnose depression and anxiety.
Treatment of Mood Disorders
Physicians are selected individually for the treatment of emotional disorders, depending on the pathology, clinical symptoms and nature of the disease. Common treatments include psychotherapy and social work to treat acute symptoms, removing the cause (when possible), and improving adaptability. An integrated approach includes the following fields:
An integrated approach includes the following fields:
- Patients with pharmacotherapy are given antidepressants, which are medications that improve mood and performance. SECONDARY can be used for anxiety symptoms. The drug in this group relieves tension, promotes relaxation and reduces anxiety and fear. Normohics have an anti-operanic effect, releasing the next emotional heaviness and preventing it from occurring. Antimicant diseases eliminate mental and motor excitement and mental illness (delusions, hallucinations). In parallel with psychiatric therapy, endocrine diseases and neurological diseases are treated.
- Psychotherapy. The direction of psychotherapy is determined by the characteristics of the disability. If the element of depression is strong, it is advisable to gradually participate in a personal session of cognitive therapy, cognitive-behavioral therapy and group sessions (Gestalt therapy, psycho-drama). Non-sick patients must learn coping and relaxation techniques and deal with misperceptions that inhibit stress.
- Strive to return to society. The relationship of the patient and close relatives plays an important role in the recovery of the patient. Psychologists and psychotherapists hold a family meeting to discuss the need for rational care, exercise, adequate nutrition, gradual participation in daily life, walking together, and the need for sports activities. Sometimes there is a pathological interpersonal relationship with the family that supports the disability. In this case, a session is needed to solve the problems of psychotherapy.
Prognosis and prevention
Emotional disorders show a relatively good transformation in both psychogenic and symptomatic and contribute to disability recovery through early and comprehensive treatment. Since hereditary emotional disorders tend to resolve chronically, patients need regular treatment to maintain their health and prevent relapse. To prevent, it is important to avoid bad habits, maintain intimate trust in relatives, have enough sleep, work and rest to provide time for hobbies and leisure.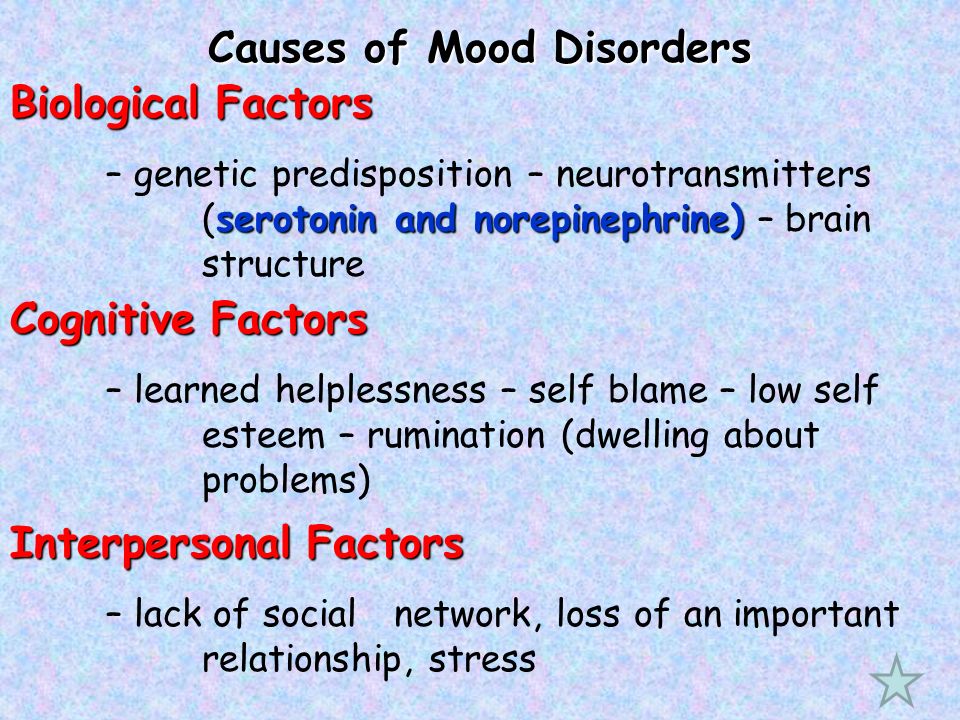 If there is a risk factor, such as a genetic factor, a regular psychiatric examination is required.
If there is a risk factor, such as a genetic factor, a regular psychiatric examination is required.
Manic depression (bipolar emotional disorder) is a mental illness that also appears due to significant emotional disturbances. Depression and manic (or hypomic illnesses) may alternate, or depression alone or many may occur intermittently, causing a mixture or an intermediate state. The cause is not decisive, but genetic primaries and characteristics are important. Diagnosis is based on history, special tests, patients and their relatives. Treatment is drug therapy (antidepressant, Quotaimics, low frequency but antipsychotics).
General
Manic depression (MDP) is a variety of depression and manic state in which depression and manic state intermittently, only depression or manic state, depression and manic symptoms at the same time. This is a mental illness in which a mixed state appears. The disease was first independently described by Bayarger and Falert in France in 1854, but after Krapelin wrote the subject, MDD was not officially recognized as another disease until 1896 years. 。
。
Until 1993, this was called manic depression. Following the approval of the ICD-10, the legal name was changed to "bipolar emotional disorder". The reason is that the old name was incompatible with clinical symptoms (MDD is not necessarily accompanied by a psychiatric illness), and the word "psychiatric" has a prejudice, a "print" type. It was stigmatization. Treatment for TIDP is performed by a mental health professional.
Causes of development and prevalence of manic-depressive psychosis
Although the cause of TIDP has not been fully elucidated, it is assumed that both internal factors (inheritance) and environmental factors (environment) have an effect, and it is the genetic factor that plays more important roles. It has not yet been established whether TID is transmitted by a single or multiple gene or disruption of expression type processes. There is evidence that supports both monetary and polygenomies. There may be a type that is infected with one gene and a type that infects several genes.
Danger factors include melancholic type (strong sensitivity, modest expression of emotional expression, increased fatigue), Statchimi type (pedanic, strong responsibility, increased structural desires), sizoid type (emotional monotonous (emotional monotone). There are people with rational tendencies and Lonely actions), people who are emotional instability, anxiety and sensitive personality.
There are various data on the relationship between manic depression and gender. Previously, females were thought to be 1.5 times larger than males, but current research says that the single-part sex type is more common in females, and double-parts are more common. Women are said to be more likely to develop during hormonal changes (menstruation, postpartum, menopause). It is also said that those who have experienced some mental illness after giving birth will increase their risk of onset.
There is also some ambiguous information about MDD in the general population because investigators use different scoring criteria.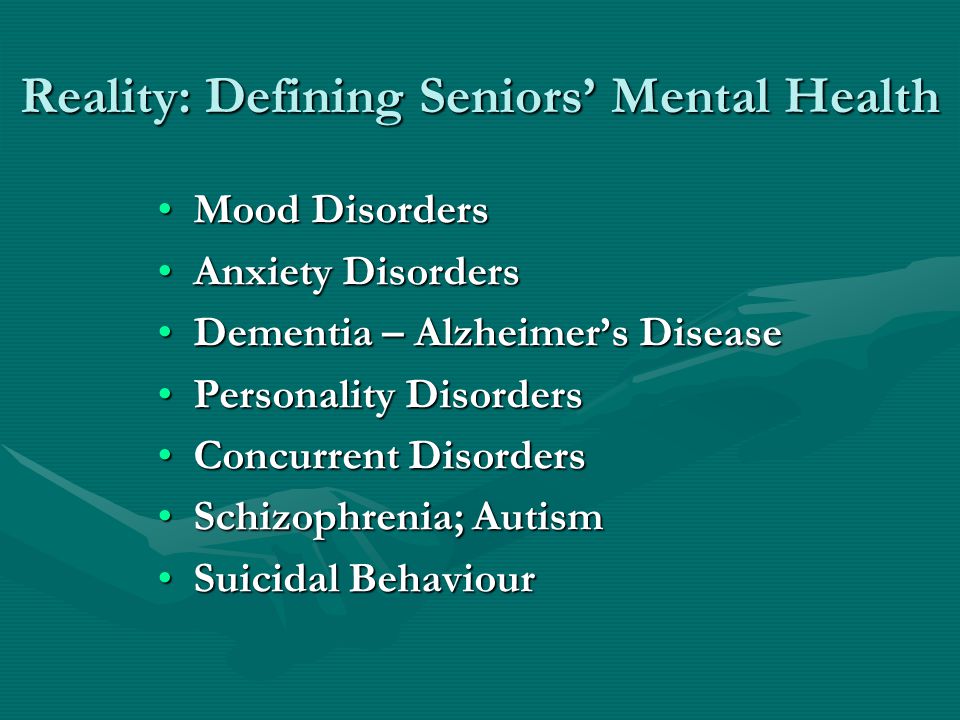 At the end of the 20th century, foreign statistics claimed that 0.5-0.8% of the population had manic depression. Russian experts mentioned the slightly lower figure of 0.45% of the population, saying that only one-third of patients are diagnosed with severe mental illness. In recent years, data on the rate of manic depression have been reviewed, and the latest study found symptoms of TID in up to 1% of the world's population.
At the end of the 20th century, foreign statistics claimed that 0.5-0.8% of the population had manic depression. Russian experts mentioned the slightly lower figure of 0.45% of the population, saying that only one-third of patients are diagnosed with severe mental illness. In recent years, data on the rate of manic depression have been reviewed, and the latest study found symptoms of TID in up to 1% of the world's population.
Because it is difficult to use standard diagnostic criteria, there is no evidence that children may develop MDD. However, it is believed that this disease is often not diagnosed among experts in the first place in childhood or adolescence. For half of the patients, the first clinical symptoms of TID appear between the ages of 25 and 44, and the pole type dominates in young people, as well as in people with middle and old age. Approximately 20% of patients are 50 years of age or older, and the number of phases of depression increases significantly.
Classification of manic-depressive psychosis
In clinical settings, specific emotional disorders (depression or manic) are commonly used in MDD based on alternating episodes of manic and depression. If there is only one type of mood disorder, it is said to be bipolar manic depression if both are both. Single MDDs include intermittent depression and intermittent mania. The bipolar type is different from the four courses.
If there is only one type of mood disorder, it is said to be bipolar manic depression if both are both. Single MDDs include intermittent depression and intermittent mania. The bipolar type is different from the four courses.
- Regular intermittent depression and mania appear alternately, and emotional episodes are separated by clear intervals.
- Irregular intermittent depression and manic erratic substitution (two or more episodes of depression or manic episodes may be continuous) and emotional episodes are separated by slight gaps.
- Twice after depression he develops a manic (or manic due to depression) and has a clear empty void after two emotional episodes.
- Circular p-depression and mania appear alternately, and there are no bright gaps.
The number of steps may vary depending on the patient. Some patients develop only once in a lifetime, while others have several dozen times. One episode period varies from one week to two years, averaging several months.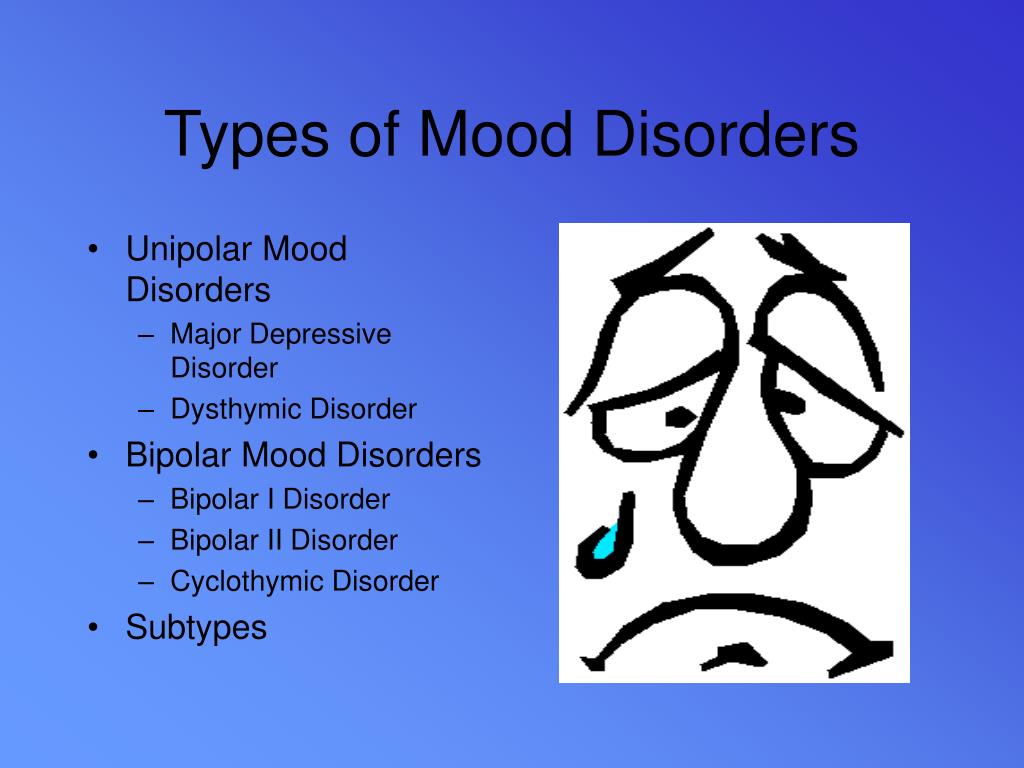 Episodes of depression are more common than manic episodes, and depression is three times longer than manic episodes. Some patients have depressive and manic symptoms at the same time, and may develop mixed episodes that quickly lead to depression and mania. The average period of clarity is 3-7 years.
Episodes of depression are more common than manic episodes, and depression is three times longer than manic episodes. Some patients have depressive and manic symptoms at the same time, and may develop mixed episodes that quickly lead to depression and mania. The average period of clarity is 3-7 years.
Manic-depressive symptoms
The main symptoms of mania are exercise, uplifting mood, and quickening of the mind. The degree of manic is divided into three. Soft things (iponia) are characterized by improving mood and improving social performance, mental and physical productivity. Patients become energetic, alert, chattering and slightly distracted. Sexual desires increase and sleep desires decrease. Instead of euphoria, discomfort (hostility and irritation) may occur. The period of the episode does not exceed a few days.
In moderate analysis (mania without mental symptoms), there is a sudden rise in mood and a significant increase in activity. The need for sleep has almost disappeared. It ranges from joy and excitement to aggression, depression and irritation. Social contact is difficult, the patient is distracted and always distracted. A great concept is born. The period of the episode is 7 days or more, and this episode is accompanied by loss of work and social exchange abilities.
It ranges from joy and excitement to aggression, depression and irritation. Social contact is difficult, the patient is distracted and always distracted. A great concept is born. The period of the episode is 7 days or more, and this episode is accompanied by loss of work and social exchange abilities.
In severe mania (mania with psychiatric symptoms) there is an excitement of remarkable mobility. Some patients have a violent tendency. Thinking is incoherent, but thoughts fly. There are delusions and hallucinations that are different from schizophrenia. Productive symptoms may not match the patient's mood. Extended delusions and exaggerated delusions are termed successive productive symptoms, while neutral and mild emotional delusions and hallucinations are termed inconsistencies.
Depression causes the opposite of manic, i.e. delays in motor function, marked mood and slow thinking. Anorexia and weight loss progress. In women, menstruation stops, and both men and women do not experience sexual desire. In case of mild illness, there is a change per day. The weight of symptoms is maximum in the morning and subsides in the evenings. As you get older, depression gradually becomes disturbed.
In case of mild illness, there is a change per day. The weight of symptoms is maximum in the morning and subsides in the evenings. As you get older, depression gradually becomes disturbed.
Manic depression can cause five types of depression, simple, heart, delusion, excitement, and anesthesia. In simple depression, there are no remarkable symptoms, and the three signs of depression are confirmed. In mental depression, I am delusional that I have a serious illness (the doctor does not know or may be a shameful illness). With depression swinging, there is no delay in motor function. In the depression of anesthesia, painful sensations appear on the anterior part with pain. Patients believe that all emotions so far have become empty, and their emptiness causes severe pain.
Diagnosis and treatment of manic-depressive psychosis
Technically, a diagnosis of MDD requires more than two or more mood disorders, and at least one is a manic or mixed episode. In fact, psychiatrists consider more factors, such as considering life history and listening to relatives.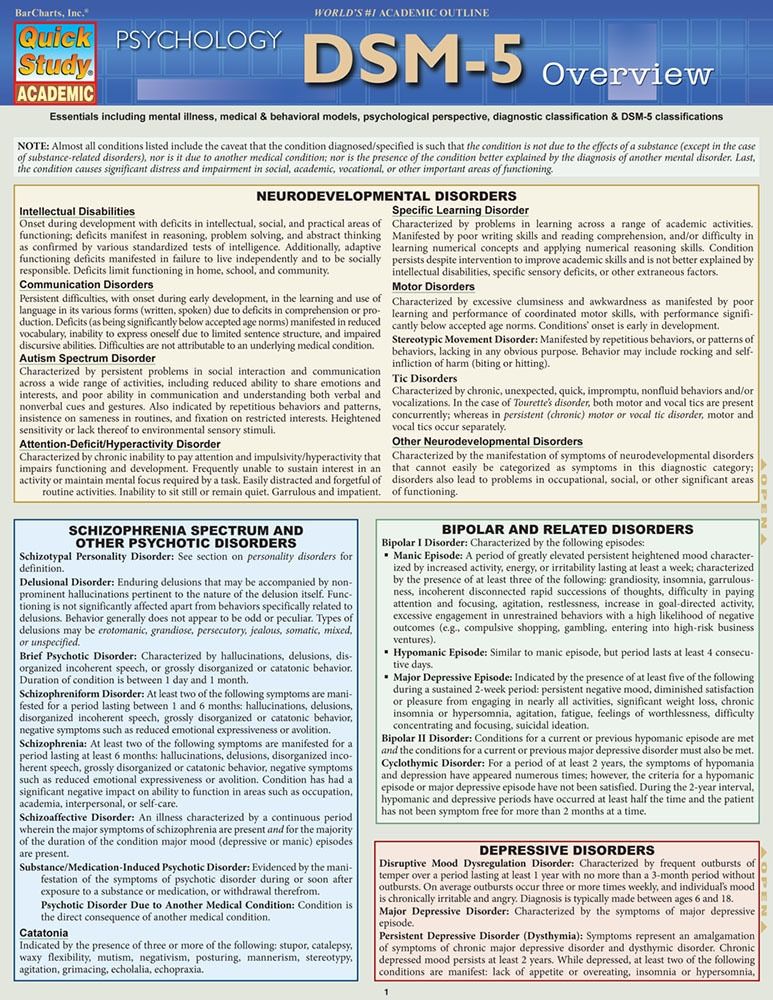 A special scale is used to determine the severity of depression and mania. MDD depression is different from psychogenic depression, and hypomic illnesses are frustrated by both lack of sleep and material use. The differential diagnosis also excludes schizophrenia, neurosis, mental illness, other mental illness, nervous illness, and physical disorders.
A special scale is used to determine the severity of depression and mania. MDD depression is different from psychogenic depression, and hypomic illnesses are frustrated by both lack of sleep and material use. The differential diagnosis also excludes schizophrenia, neurosis, mental illness, other mental illness, nervous illness, and physical disorders.
Severe MDP is being treated in a psychiatric hospital. If it is mild, treatment is possible on an outpatient basis. The main goal is to normalize your mood and mental state and get a stable remission. If an episode of depression occurs, an antidepressant is prescribed. The choice of drugs and the decision of the dose is made taking into account the possibility of a transition from depression to mania. An antidepressant is used in combination with atypical antipsychotics or normotensives. In case of mania, use normotin and in severe cases, use it with antipsychotics.
Mental function may be fully or almost completely restored between attacks, but the prognosis of MDP is generally not good.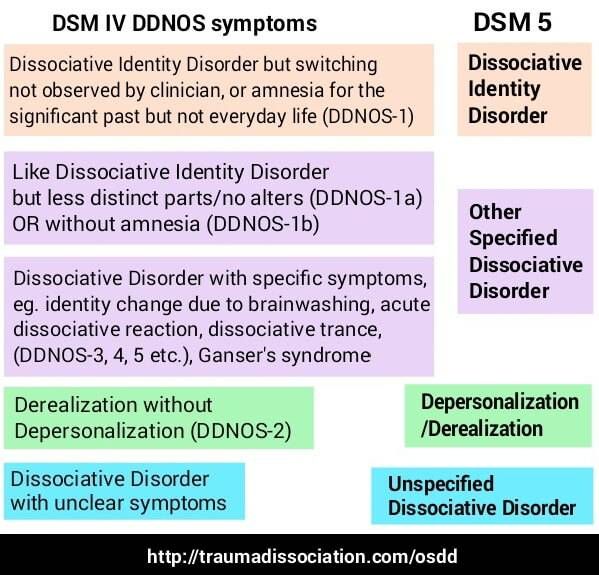 For up to 90% of patients, 35-50% of recurring episodes will complain of ability. 30% of patients continue to experience the mental illness of manic depression and have no clear gaps. The middle often occurs with other mental illnesses. Many patients suffer from alcohol and drug abuse.
For up to 90% of patients, 35-50% of recurring episodes will complain of ability. 30% of patients continue to experience the mental illness of manic depression and have no clear gaps. The middle often occurs with other mental illnesses. Many patients suffer from alcohol and drug abuse.
A complex mental illness that alternates between intense depression and manic states is called manic depression. In the clinical stage, a self-contained manic state and a major depression that interferes with QOL may appear alternately. If the diagnosis is evaluated, you must be introduced to a specialized clinic and receive a reputation.
Diagnosis of manic-depressive psychosis
The disease was first described in 1854 by the French doctor Fellers and Bajarger, but Teed was recognized as another disease in 1896 year. This was prompted by the Criperin study, which was recognized as an independent name for the disease. At this time, the name manic depression appeared. After the introduction of the International Classification ICD-10, it became the diagnostic name of Bipolar Emotional Disorder.
The cause of this condition is not entirely known, but clinical observation may have two causes.
- There is an innate essence.
- A combination of external factors that have worsened due to negative inheritance.
Diagnosis is made through an interview with a psychiatrist. Doctors examine the patient's medical history and lifestyle. If the guess is confirmed, the test will be ordered. The specialist listens to the patient and his environment and explores.
In most cases, the disease develops at a young age. The forecast will be even more negative. If left untreated, the symptoms will worsen. Even if the treatment is carried out and the pathological condition is successful, 90% of patients should be considered by psychiatrists when they relapse.
Psychiatrists use the scale to determine the different stages of the MDP. Mental illness, schizophrenia and psychopaths must be ruled out.
Manic phase of depressive psychosis
As the beginning of the pathology, the manic phase is defined several times as the phase of depression.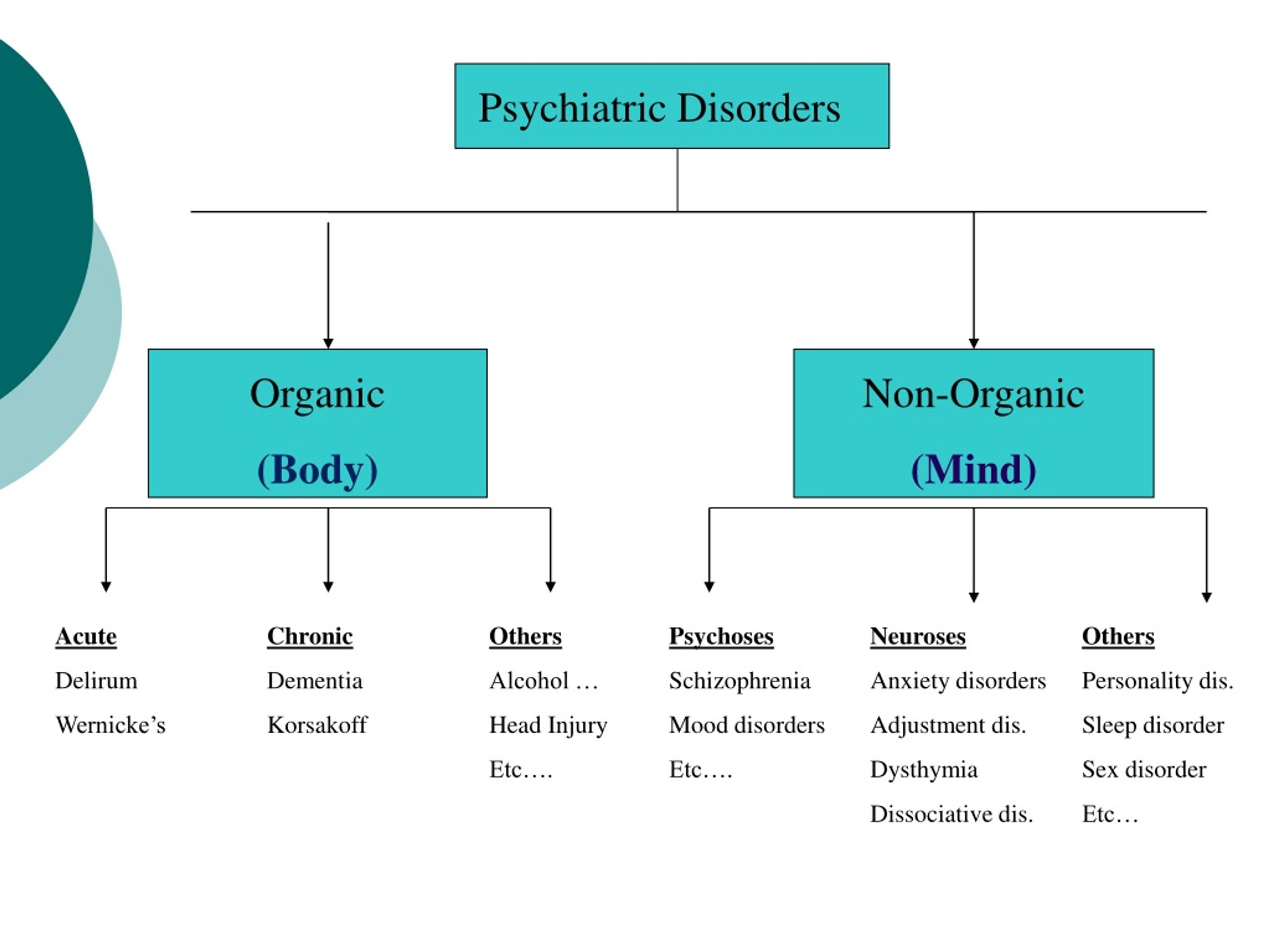 Most patients rarely read such a state for granted, even during the hypomanic period. Patients usually only focus on increasing activity and are quite positive.
Most patients rarely read such a state for granted, even during the hypomanic period. Patients usually only focus on increasing activity and are quite positive.
As a characteristic symptom
- Suppression increased.
- Unhealthy eyes shine
- Redundant.
- At present, the future and the past look like a rainbow color.
- Increasing awareness of your own power and charm.
- I feel unhealthy optimism and endless possibilities.
Patients notice every little thing. He also wants to deal with trivial things. Also, if you're trying to communicate, you tend to address the other side without being appropriate. It is characterized by an overreaction to new acquaintances and dissatisfied surroundings. Patients often demand such people and become bizarre.
To prevent this repression, it often results in reckless behavior, sexual abuse and inadequate monetary spending.
Expression of the baby phase is rarely explained because it is rarer.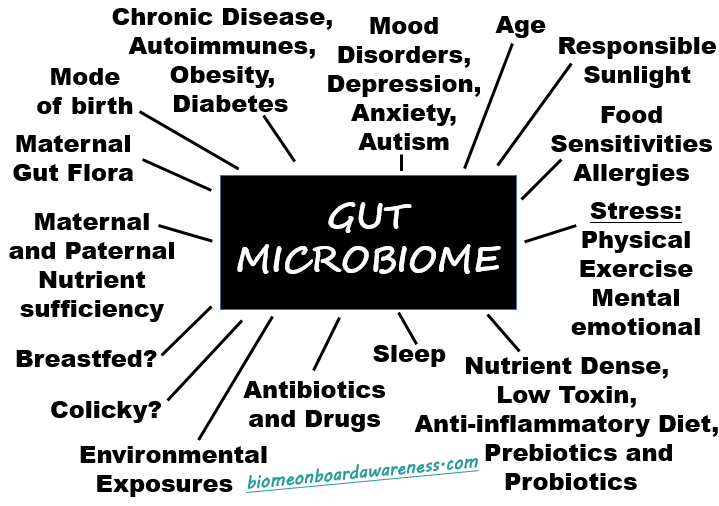 Young patients are hypersensitive, communicating and exciting.
Young patients are hypersensitive, communicating and exciting.
Signs and symptoms of manic-depressive psychosis
Typical symptoms include increased activity, faster thinking and excitement of exercise. The need for sleep decreases, and desires and sexual activity increase. As this state accelerates, it becomes depressing and engulfs the surrounding world with a dark feeling. The period of one menstruation is usually several days. There are phases with a duration of mania and depression.
Alternating in this state, the social function is impaired. In the early days, the neighborhood was surprised by fluctuations in social intent, and then suddenly changed to a negative attitude. The patient's self-awareness is accompanied by disability, and the state is at the level of depression. As the disease progresses, fluctuations in the amount of activity are often encountered and gradually noticed by others.
In severe maniacs violent tendencies can be strongly seen.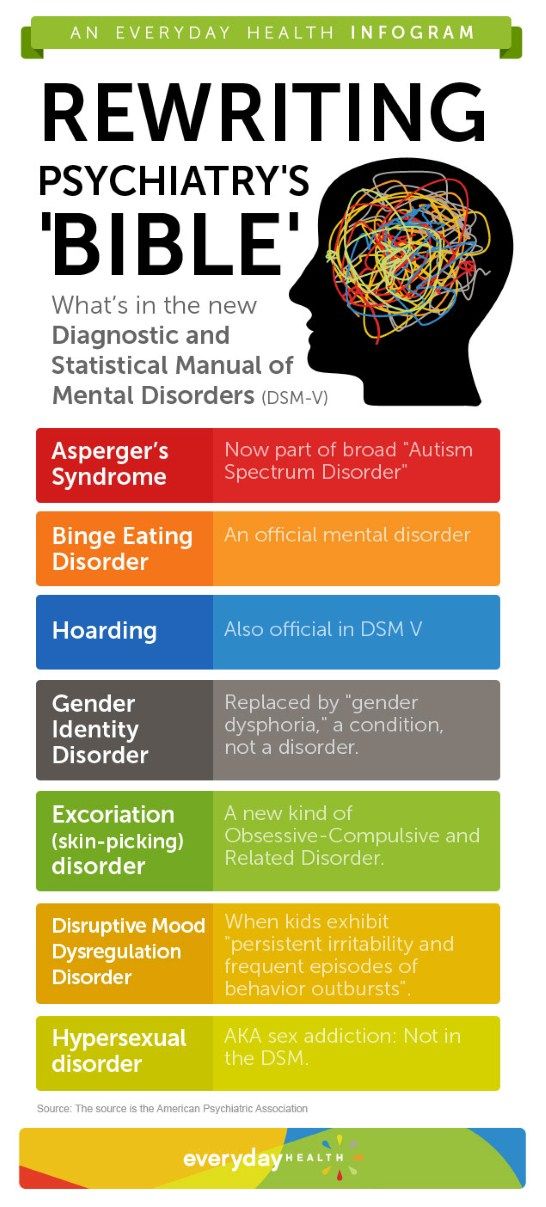 Thinking becomes irregular. A type of hallucination and delusion similar to schizophrenia may occur.
Thinking becomes irregular. A type of hallucination and delusion similar to schizophrenia may occur.
Depression is characteristic and is the opposite of the manic stage. In the Agio type there is an exercise delay. In the case of anesthetic depression, the patient's pathological sensation is ahead. The imagining that occurs instead of each sensation leads to pain. On the other hand, there is no libido at this stage.
Treatment of manic-depressive psychosis
The first step in treatment is the elimination of external factors that are negative triggers. In particular, if long-term drugs and alcohol abuse trigger the onset of pathology, TZD often sets in. You will also need to remove the stressors that become another trauma.
The type of treatment varies depending on the stage. For depression, an antidepressant using norms or an antipsychotic drug is recommended. The dose is determined individually for each patient. There is a risk of causing a transition from depression to a manic state, so only doctors are required.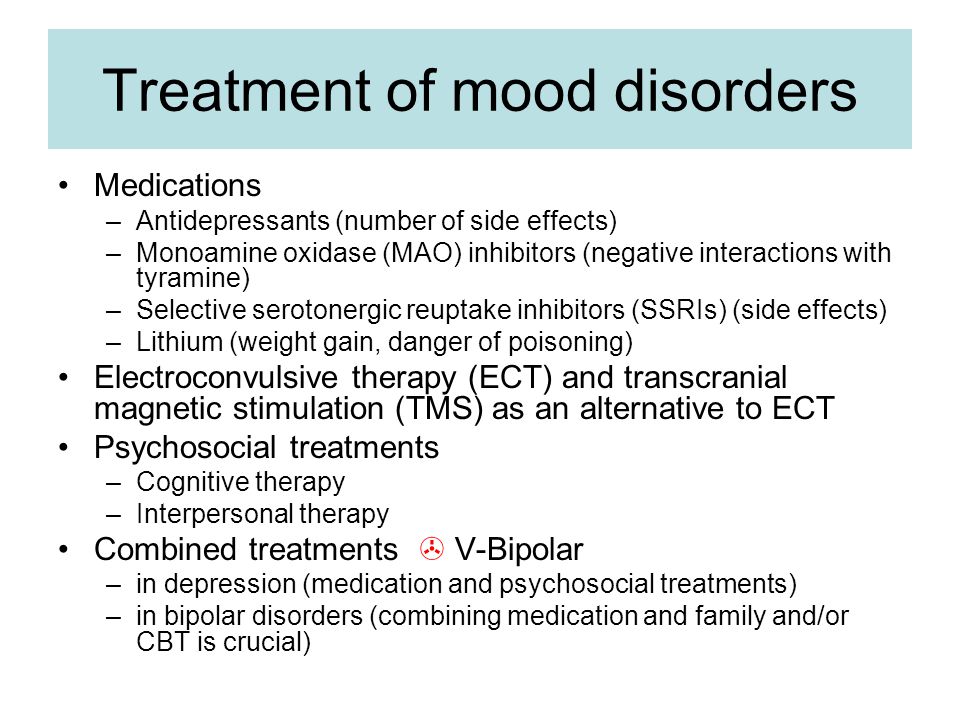
Manic state resolved by prescribing a normotic. For severe illnesses, add an antipsychotic illness.
If you receive appropriate treatment, you will be completely cured, but the period of remission and seizure will alternate, so the prognosis was confirmed to be poor. 90% of patients can return the diagnosis. If you follow a difficult course, treatment will be possible only after hospitalization. If you are in the mild stage, you may be able to handle this outpatient treatment.
About 30% of patients do not go into remission. With such a course of the diagnosis, patients with a background of alcohol or drug addiction often turn. MDD is often accompanied by other psychiatric diagnoses.
Disease manic depressive psychosis
Diagnosis and treatment of MDP is complicated by different types of presentation of the diagnosis.
Affective psychosis, manic-depressive psychosis
Emotional psychosis is a common symptom of MDP. These physical ailments are in addition to many physical and mental illnesses.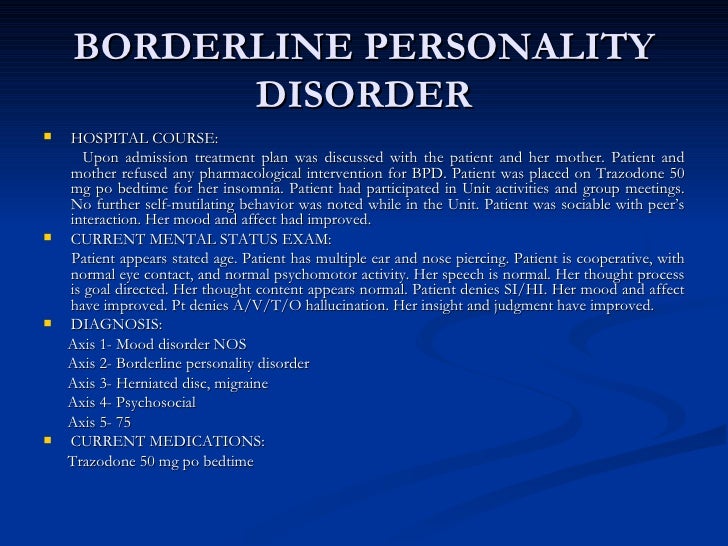 Therefore, it is now included in the MDP. The main symptom is a state of habitual depression.
Therefore, it is now included in the MDP. The main symptom is a state of habitual depression.
Depressed, but not accompanied by depression. The start starts without an explicit trigger. Mental and emotional trauma often leads to bitter melancholy. The condition is often diagnosed as "reactive depression". Genetic factors play an important role in the occurrence. It can also be caused by a serious brain disorder.
bipolar disorder, manic-depressive disorder
MDD in this context manifests itself as a symptom of the manic-depressive disorder described above. Patients fluctuate sharply between high activity and low lethargy.
In a manic state, arousal and libido are increased. Patients often have a flood of unrealistic and impractical ideas. They are hyperactive and need to communicate with others. Mental activity is fragmented, verbal and often intrusive.
Depression makes you completely lethargic. Sexual activity is lost until complete failure. increased drowsiness and lethargy; Patients prefer a stable immobile state, often stay in bed, do not go to work or study, and exclude contact with the outside world.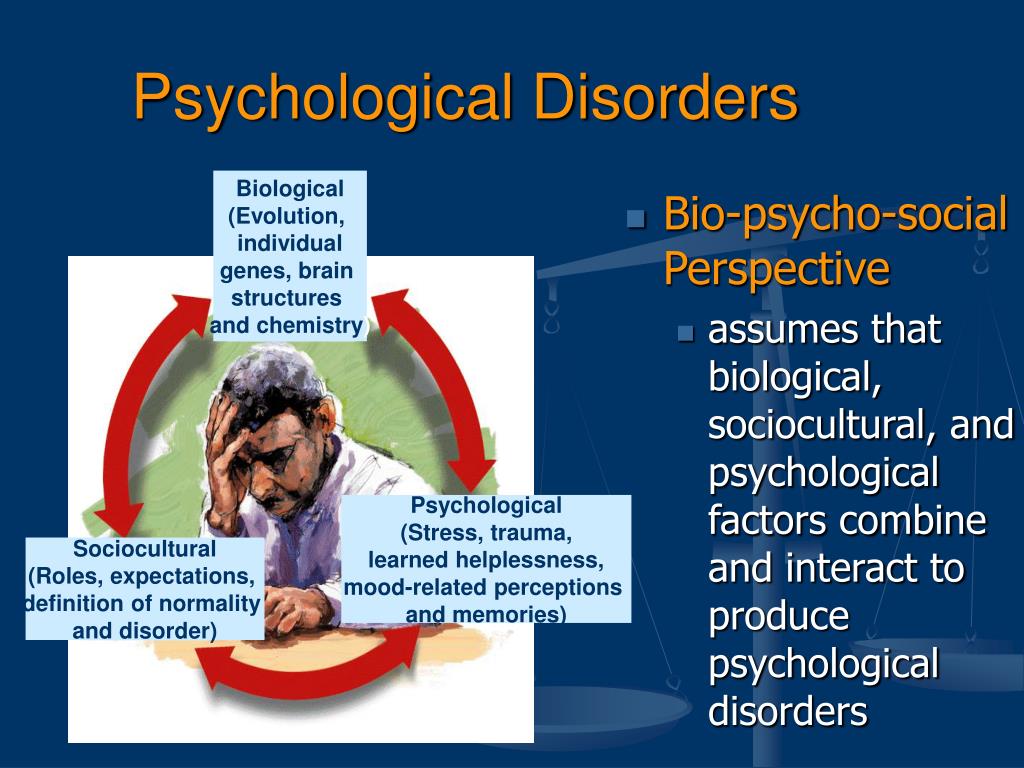 Mindless thoughts and suicide are common.
Mindless thoughts and suicide are common.
bipolar manic depression
This symptom is characterized by worsening of symptoms at the end of each vital function. Patients in the depressed stage present with a complex and often stigmatizing diagnosis. Psychosis involves the transition from activities to the point of wanting to hurt others to a deep depression that nullifies all life's demands and desires.
female depression
This complex mental disorder, inherited in an autosomal dominant manner, is most often diagnosed in the fairer sex. The public perception that women are more prone to depression and hysteria may delay diagnosis. They are reluctant to acknowledge the existence of pathological disorders.
Impulsive fluctuations are often associated with the effects of hormones, but not necessarily the cause of disability. In women, depression tends to be long term and then manic in the short term. There is a time when the zest for life is greatly lost to injure oneself to the point of suicide, and after that the activities become more active and women are indiscriminately bound and they tend to spend unreasonable and unreasonable financial expenses.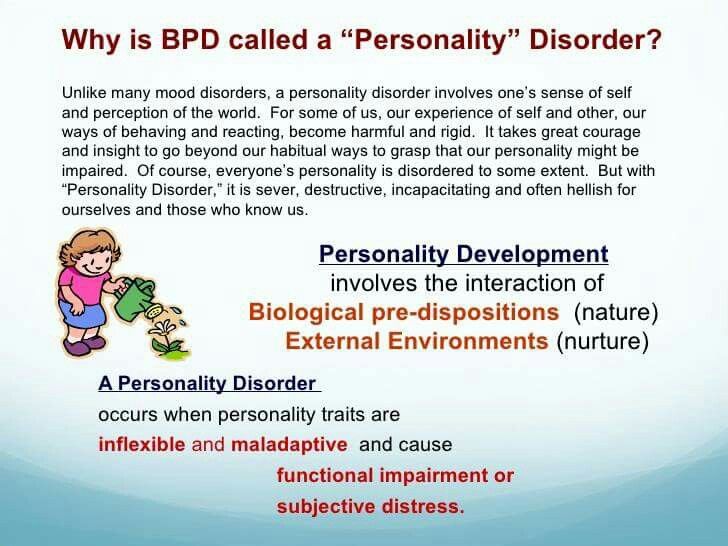 It will. Questionnaire For women, this disease can hide for a long time.
It will. Questionnaire For women, this disease can hide for a long time.
Signs and symptoms of manic depression in women
Manic depression in a woman is accompanied by severe depression. The desire for active and impulsive behavior increased, and then deep depression. The duration of symptoms varies from a few days to a few weeks, and depression is dominant.
Manic depression in men
Men often develop into the manic stage. Society has a positive view of mental and physical activity as an improvement in business sense and productivity at an early stage. And the manic stage can be pushed into an aggressive state.
Men's depression is often more complex and close to tension. Men are more likely to succeed in suicide when they are suffering from MDP.
Signs and symptoms of manic depression in men
Most men are positive and recognize affirmative action when euphoric. Males are very sociable to outsiders, often familiar with non-social elements, and manic turns into aggressive stages more frequently than females.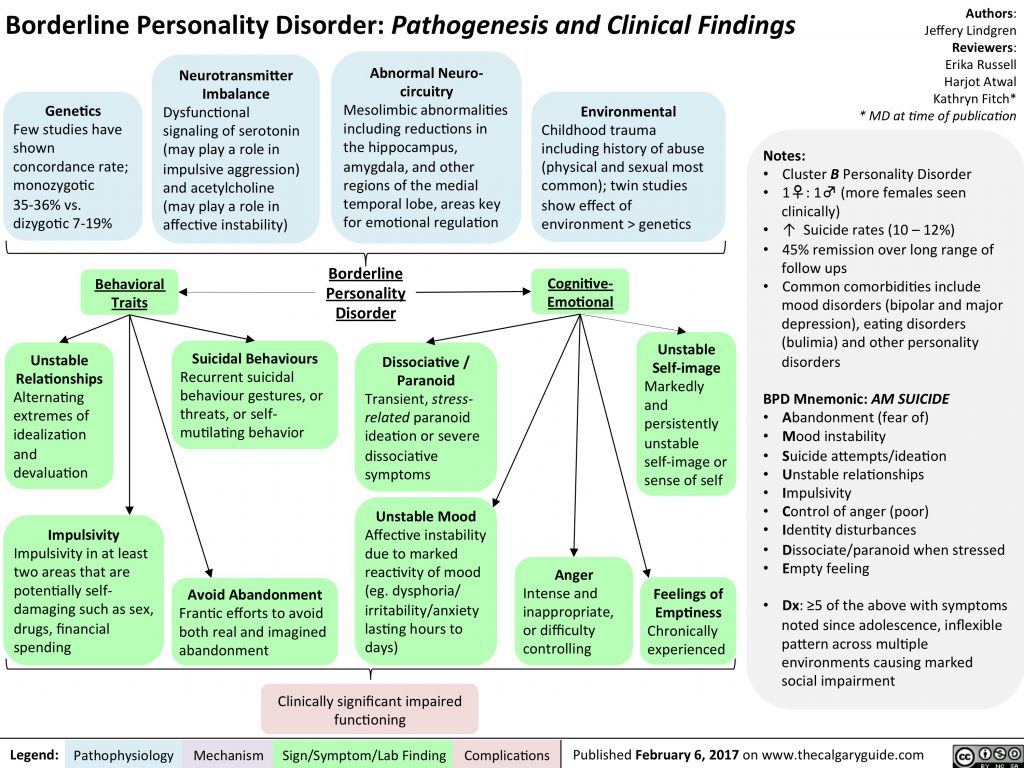
During depression, men are characterized by a lack of purpose in thought and existence, an aggressive aversion to all forms of work, tendencies towards alcoholism, antisocial habits, and suicidal tendencies.。
2 4-hour free consultation
We answer your questions
Rescue clinics have been treating various psychiatric illnesses and disabilities for 19 years. Psychiatry is a complex field in medicine, and physicians require maximum knowledge and skills. Therefore, our employees are all professionals with advanced training, qualifications and experience.
When to consult?
Do you understand that your relatives (grandparents, mother, father, father) cannot remember the basics, forget the date or name, or do not recognize people? This clearly indicates some kind of mental illness or mental illness. Self-carrying in this case is ineffective and even dangerous. The drug, taken by itself without obtaining a doctor's prescription, will temporarily alleviate the patient's physical condition and symptoms. In the worst case, it can harm your health and cause irreparable situations. Folk therapy at home may not give the expected results, and folk remedies are not useful for mental illness. Relying on them is just wasted time for those with mental disorders.
In the worst case, it can harm your health and cause irreparable situations. Folk therapy at home may not give the expected results, and folk remedies are not useful for mental illness. Relying on them is just wasted time for those with mental disorders.
If your relatives have bad memories, complete memory loss, or obviously mental disorders or other signs of serious illness, contact the private psychiatric clinic "rescue".
Why choose us?
Rescue clinics have excelled in the treatment of phobia, phobia, stress, memory disorders and mental illness. We provide cancer care, stroke care, elderly inpatient care, senior care and cancer care. Even at the end of the year, you don't abandon a patient.
Many government agencies are reluctant to see patients aged 50 and 60. We will help everyone who relies on us, even after 50, 60 and 70 years, will provide treatment. There is everything you need for this.
- Leased house
- Nursing home
- Bedside hospice
- Professional Nurse
- Sanatorium.
Even if you are old people, you cannot leave the disease. Comprehensive treatment and rehabilitation gives most patients the best opportunity to restore basic physical and mental functions and significantly improve life prognosis. You can do it.
Our experts use the latest diagnostic and treatment methods, the most effective and safe medicines and hypnosis. If necessary, the doctor will visit the doctor.
- I will have my first consultation.
- Investigated as cause of mental illness.
- Preliminary diagnosis made.
- Acute attacks and hangover relieved.
- If you become seriously ill, you may have to be admitted to a closed rehabilitation center.
Treatment in our hospital is inexpensive. The first consultation is free. All services are fully open and all procedures are included in advance.
Relatives of patients often ask questions: "What is a mental illness?" You can get a thorough consultation in a private clinic "salvation"
We managed to provide real help and treat any mental illness
Bipolar disorder0325 General summary
Bipolar disorder, also known as bipolar affective disorder (BAD) and formerly known as manic-depressive psychosis (PMD). It is a set of mood disorders characterized by marked fluctuations in mood, thinking, behaviour, energy and ability to perform daily activities.
It is a set of mood disorders characterized by marked fluctuations in mood, thinking, behaviour, energy and ability to perform daily activities.
A person suffering from this disorder alternates his state of mind between mania or hypomania - a phase of joy, exaltation, euphoria and grandiosity and depression, with sadness, inhibition and ideas of death.
Four types of bipolar disorder were defined by severity and alternation of moods over time:
- Bipolar I disorder
- Bipolar disorder type II
- Cyclothymia
- Non-specific bipolar disorder
Because bipolar disorder occurs in young people, it has a high social cost. It is the second leading cause of disability worldwide. In addition, those who suffer from it pose a higher risk than the general population of deaths from suicide, homicide, accidents, and natural causes such as cardiovascular disease.
In type 1, the person alternates between depressive episodes with full manic episodes, and in type 2, he alternates between depressive episodes and hypomanic (less severe) episodes.
The symptoms of this disorder are severe, different from the normal highs and lows of mood. These symptoms can lead to relationship problems, work, school, or even suicide.
During the depression phase a person may experience:
- A negative perception of life.
- Inability to feel the pleasure of life.
- No energy
- Self-criticism.
- In extreme cases, suicide.
During a manic phase a person may experience:
- Denial that there is a problem.
- Sudden change of mood.
- Irrational financial decisions.
- Feeling of great enthusiasm
- Don't think about the consequences of your actions.
- Lack of sleep
Although childhood onset occurs, the normal age of onset for type 1 is 18 years and for type 2 is 22 years.
Approximately 10% of bipolar 2 cases develop into type 1.
Although the causes are unclear, genetic and environmental factors (stress, childhood abuse) play a role.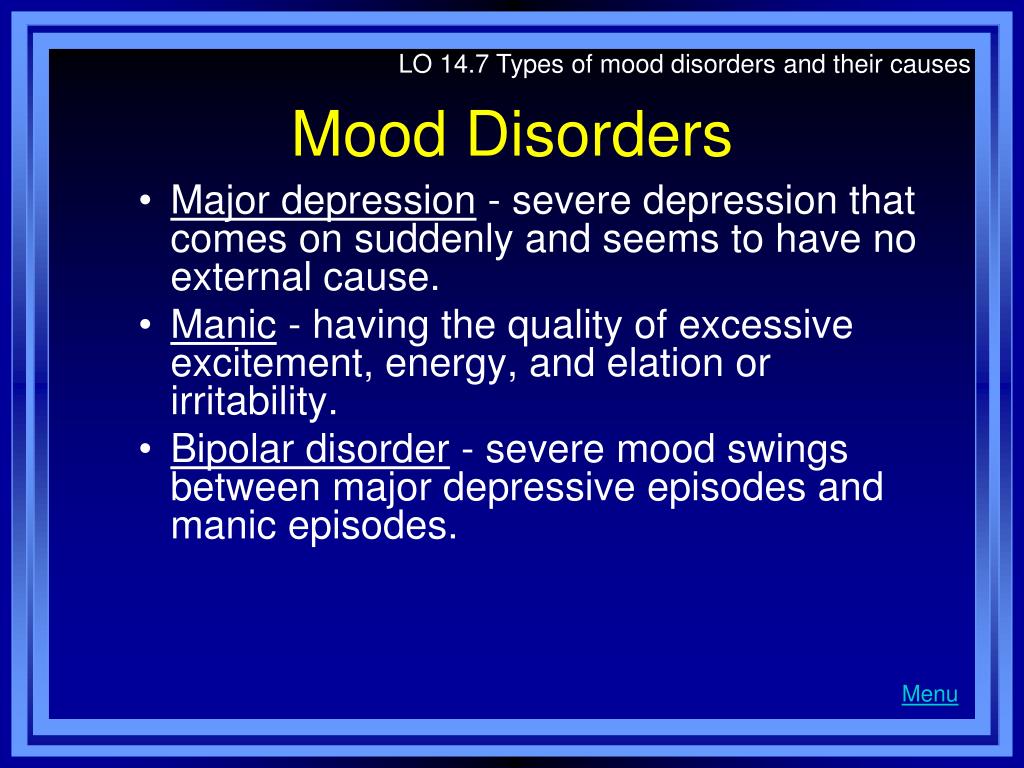
Treatment usually includes psychotherapy, medication, sometimes electroconvulsive therapy may be helpful.
Symptoms
Signs and symptoms of the depressive phase of bipolar disorder include:
- Persistent sadness
- Lack of interest in engaging in pleasurable activities.
- Apathy or indifference.
- Anxiety or social anxiety.
- Chronic pain or irritability.
- Lack of motivation
- Guilt, hopelessness, social isolation.
- Lack of sleep or appetite.
- Suicidal thoughts
- In extreme cases, there may be psychotic symptoms: delusions or hallucinations are usually unpleasant.
Manic symptoms
Mania can occur in different degrees:
Hypomania
This is the least severe degree of mania and lasts at least 4 days. This does not result in a noticeable decrease in a person's ability to work, communicate, or adapt.
He also does not require hospitalization and does not have psychotic characteristics.
In fact, general functioning may improve during a hypomanic episode and is considered a natural anti-depression mechanism.
If the event of hypomania is not accompanied by or precedes depressive episodes, it is not considered a problem if the state of mind is uncontrollable.
Symptoms may last from several weeks to several months.
It is characterized by:
- Great energy and activity.
- Some people may be more creative, while others may be more irritable.
- A person may feel so good that he denies that he is experiencing a state of hypomania.
Mania
Mania is a period of euphoria and high mood for at least 7 days. If left untreated, a manic episode can last 3 to 6 months.
It is characterized by displaying three or more of the following behaviors:
- Talk quickly and smoothly.
- Accelerated thoughts.
- Agitation.
- Light condition.
- Impulsive and risky behavior.
- Excessive cash expenses
- Hypersexuality.
- A person with mania may also experience lack of sleep and inadequate judgment.
- On the other hand, maniacs may have problems with alcohol or other substance abuse.
In extreme cases, they may experience psychosis, so that contact with reality is broken, having a high state of mind.
It is something common that a manic person feels incomparable or indestructible and feels chosen to realize a goal.
Approximately 50% of people with bipolar disorder experience hallucinations or delusions, which can lead to violent behavior or admission to a psychiatric hospital.
Mixed episodes
In bipolar disorder, a mixed episode is a condition in which mania and depression occur simultaneously.
People who experience this condition may have thoughts of grandiosity while having depressive symptoms such as suicidal thoughts or feelings of guilt.
People who are in this state are at high risk of committing suicide because they confuse depressive emotions with mood swings or difficulty controlling impulsivity.
Causes
The exact causes of bipolar disorder are unclear, although they are thought to be largely genetic and environmental.
Genetic factors
It is believed that 60-70% of the risk of developing bipolarity depends on genetic factors.
Several studies have shown that certain genes and chromosomal regions are associated with susceptibility to develop the disorder, with each gene being more or less important.
The risk of bipolar disorder in people with family members with the same diagnosis is 10 times higher than in the general population.
Research indicates heterogeneity, meaning that different genes are involved in different families.
Environmental factors
Research shows that environmental factors play an important role in the development of bipolar disorder, and psychosocial variables may interact with genetic dispositions.
Recent life events and interpersonal relationships contribute to manic and depressive episodes.
30-50% of adults diagnosed with bipolar disorder have been found to report abuse or trauma in childhood, which is associated with an earlier onset of the disorder and more suicide attempts.
Evolutionary factors
From evolutionary theory one might think that the negative effects that bipolar disorder can have on the ability to adapt cause genes not to be selected by natural selection.
However, there is still a high incidence of BD in many populations, so there may be some evolutionary benefit.
Doctors of evolutionary medicine suggest that high rates of BR throughout history suggest that the change between depressive and manic states suggested some evolutionary advantage in ancestral humans.
In highly stressed people, depressed mood can serve as a defense strategy to escape external stress, store energy, and increase sleep hours.
Mania could benefit from her relationship with creativity, confidence, high energy levels and greater productivity.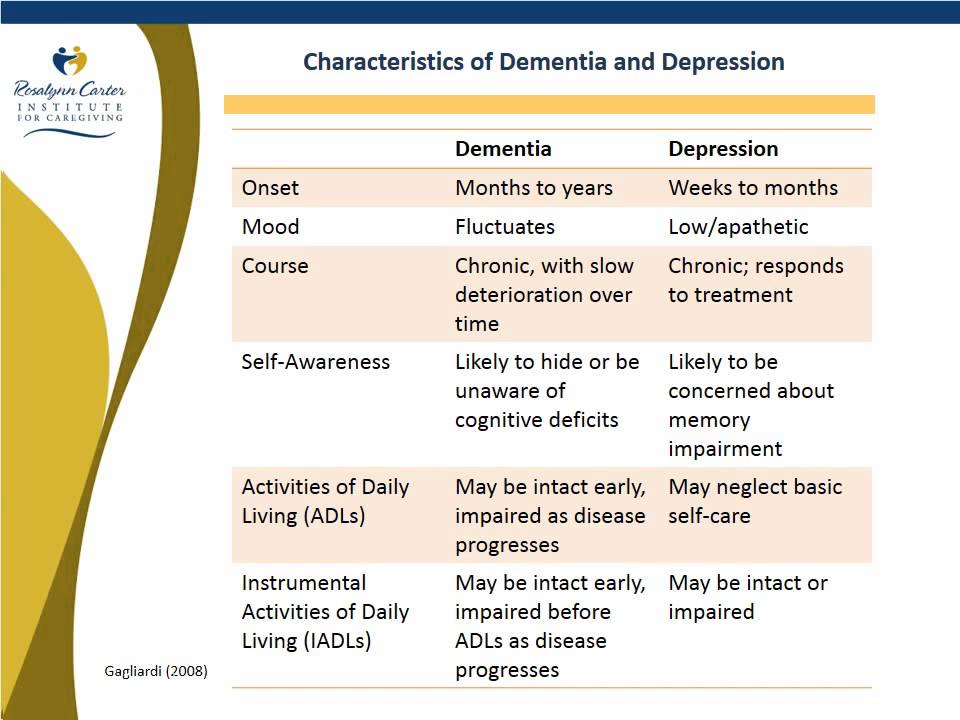
Physiological, neurological and neuroendocrine factors
Brain imaging studies have shown differences in the volume of various brain areas between patients with bipolar disorder and healthy patients.
An increase in the volume of the lateral ventricles and an increase in the rate of white matter hyperintensity were found.
Magnetic resonance studies have shown that there is an abnormal modulation between the abdominal prefrontal region and the limbic regions, especially the amygdala. This will contribute to poor emotional regulation and mood-related symptoms.
On the other hand, there is evidence of an association between early stressful experiences and dysfunction of the hypothalamic-pituitary-adrenal axis, leading to hyperactivation.
A less common bipolar disorder may result from trauma or a neurological condition: brain injury, stroke, HIV, multiple sclerosis, porphyria, and temporal lobe epilepsy.
The neurotransmitter responsible for regulating mood, dopamine, has been found to increase its transmission during the manic phase and decrease during the depressive phase.
Glutamate increases in the left dorsolateral prefrontal cortex during the manic phase.
Diagnosis
A patient must have at least two episodes of affective disorder to be diagnosed with bipolar disorder. At the same time, at least one of them must be either manic or mixed. For the correct diagnosis, the psychiatrist must take into account the characteristics of the patient's history, information received from his relatives. Currently, it is believed that the symptoms of bipolar disorder are characteristic of 1% of people, and in 30% of them the disease becomes a severe psychotic form. Determination of the severity of depression is carried out using special scales. The manic phase of bipolar disorder must be differentiated from arousal caused by the use of psychoactive substances, lack of sleep, or other causes, and the depressive phase from psychogenic depression. Psychopathy, neurosis, schizophrenia, as well as affective disorders and other psychoses due to somatic or nervous diseases should be excluded.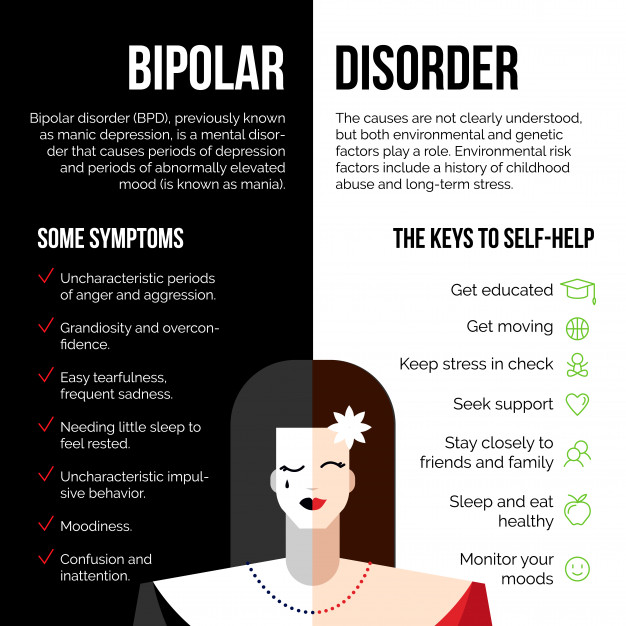
Methods of treatment
The main goal of the treatment of bipolar disorder is to normalize the mental state and mood of the patient, to achieve long-term remission. In severe cases of the disease, patients are hospitalized in the psychiatric department. Mild forms of the disorder can be treated on an outpatient basis. Antidepressants are used to relieve a depressive episode. The choice of a specific drug, its dosage and frequency of administration in each case is determined by a psychiatrist, taking into account the age of the patient, the severity of depression, and the possibility of its transition to mania. If necessary, the appointment of antidepressants is supplemented with mood stabilizers or antipsychotics. Antidepressants help to stop depressive states in bipolar disorder. Drug treatment of bipolar disorder in the stage of mania is carried out by normotimics, and in severe cases of the disease, antipsychotics are additionally prescribed. In the stage of remission, psychotherapy (group, family and individual) is shown.