Strattera vs guanfacine
Which Non-Stimulant ADHD Medication Should I Take?
Navigating the world of ADHD medications can be very confusing, especially when it comes to side effects. Stimulant medications are popular for treating ADHD because they help regulate dopamine levels in the brain, which can improve focus and reduce impulsivity. However, common side effects of these medications include restlessness and anxiety—which are also common symptoms of ADHD.
Fortunately, there are non-stimulant ADHD medications that deliver results while avoiding the side effects that come with stimulant substances. These medications give people with ADHD more treatment options with less risk of increasing their anxiety.
Whether your ADHD is minimally disruptive or affects every aspect of your life, non-stimulant medications can be a gentler alternative to more mainstream forms of treatment. In this article, we’ll outline which non-stimulant ADHD medication you should take.
If you want to get in front of a licensed ADHD specialist within the next 48 hours, schedule an appointment today or take our free self-evaluation.
Stimulant vs. Non-Stimulant ADHD Medication
ADHD medications work by leveling out the brain’s chemical levels to reduce symptoms. These medications come in two forms, stimulant and non-stimulant, each of them with its own benefits and disadvantages. Stimulant drugs are the most researched and prescribed form of ADHD medication, but they may not always manage symptoms effectively. Non-stimulant medications aren’t used as often, but they can be an effective alternative that improves overall concentration and impulse control.
One of the key advantages of non-stimulant ADHD medication is the reduced risk of addiction. Though they’re carefully controlled and monitored, stimulant medications always carry some risk of addiction, especially for those with a history of substance use disorder. Non-stimulants offer symptom regulation without many of the same addictive qualities, ensuring people can get the treatment they need without worrying about how it might lead to a more severe problem.
Below is a detailed list of the most popular non-stimulant medications, including what they are, how they work, and potential risks.
What is Strattera?
Strattera is the brand name for atomoxetine, a medication used to treat ADHD. It’s often used as part of a treatment plan with psychological or social treatments. It’s the first FDA-approved non-stimulant medication for the treatment of ADHD, and it’s recognized as an effective alternative to drugs like Adderall and Ritalin.
It’s available via prescription, and it should only be taken at the discretion of a medical professional to avoid any substance abuse or unpleasant side effects.
How Does Strattera Work?
Strattera is a selective norepinephrine reuptake inhibitor (SNRI), which means it raises norepinephrine activity in the brain. This increase in norepinephrine usage is thought to help improve attention and curb impulsive behavior, two things that people with ADHD often struggle with.
This non-stimulant medication may also raise dopamine levels in the brain, which is another chemical that typically fluctuates in those with ADHD and causes many of the same symptoms.
How Long Does Strattera Last?
Depending on a person’s age, weight, and the severity of their ADHD symptoms, one or two doses of Strattera may be required daily. If a person requires two doses, the first dose is best taken first thing in the morning, and the second dose is best taken in the late afternoon/early evening as the first dose wears off. This ensures that Strattera’s benefits last throughout the day while avoiding any insomnia that could result from taking the medication late at night.
What Are the Side Effects of Strattera?
Strattera has many of the same side effects as other ADHD medications. It is highly unlikely that every person who takes Strattera will experience every side effect, and some people may experience certain side effects differently from others.
Some of the most common side effects of this non-stimulant ADHD medication include:
- Upset stomach
- Nausea
- Vomiting
- Loss of appetite/weight loss
- Dry mouth
- Dizziness
- Trouble sleeping
- Decrease in sexual ability/desire
- High blood pressure
How Much Does Strattera Cost?
The cost of Strattera varies depending on the dosage and the number of capsules purchased. The generic formula, atomoxetine, can be as low as $44 for 7 of the 10 mg capsules and as high as $1,501 for 90 of the 100 mg capsules. Most health insurance companies cover the cost of generic Strattera.
The generic formula, atomoxetine, can be as low as $44 for 7 of the 10 mg capsules and as high as $1,501 for 90 of the 100 mg capsules. Most health insurance companies cover the cost of generic Strattera.
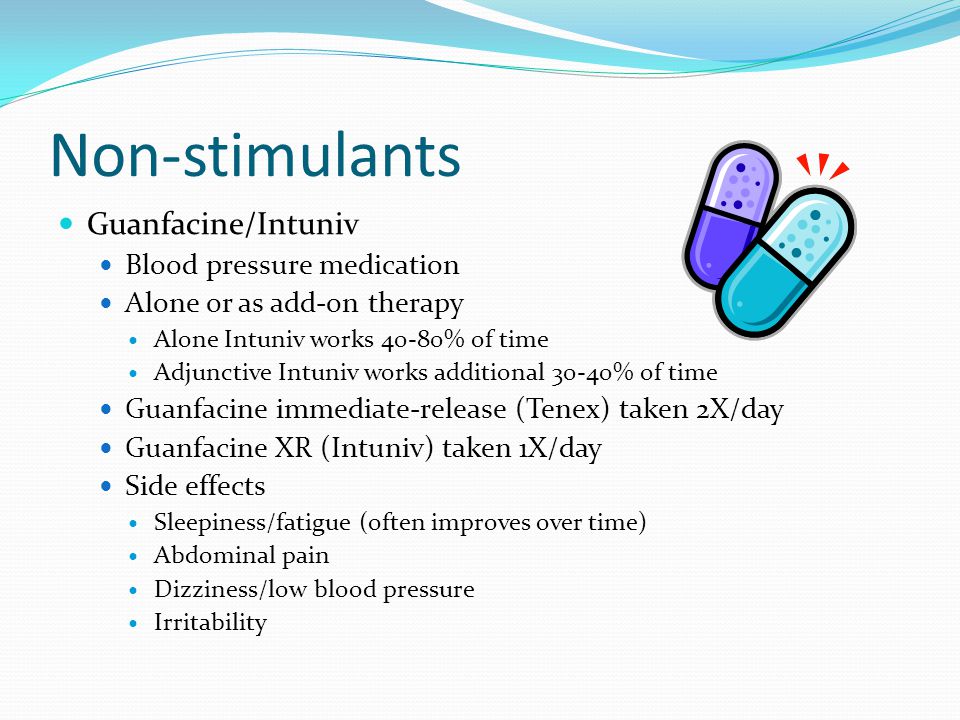
What is Intuniv?
Intuniv is the brand name of guanfacine, an alpha-2 adrenergic agonist medication that can be used to treat ADHD. Similar to Strattera, this non-stimulant medication is often used in conjunction with other psychological, educational, and social treatments. Intuniv is most often prescribed to children and adolescents between ages 6 and 17 who cannot take stimulant-based medications due to medical or personal reasons.
How Does Intuniv Work?
It’s unclear exactly how Intuniv works to lessen ADHD symptoms, but it’s believed to affect receptors in the brain and strengthen memory, reduce distraction, and help with impulse control. While multiple forms of guanfacine are available via prescription, Intuniv is the only formula approved to treat ADHD.
How Long Does Intuniv Last?
Intuniv lasts all day and is taken orally in either the morning or evening. Your dosage may be increased as you become more acclimated to the medication’s effects, but it will still only have to be taken once daily.
What Are the Side Effects of Intuniv?
Intuniv is a non-stimulant ADHD medication with fewer side effects than Strattera and other ADHD medications.
Some of the most common Intuniv side effects include:
- Drowsiness
- Dizziness
- Constipation
- Headache
- Dry mouth
- Stomach pain
- Low Blood Pressure
Intuniv is well-tolerated by most patients and doesn’t usually produce serious side effects. However, if you experience severe dizziness, slow heartbeat, fainting, or severe mood changes, contact your healthcare provider immediately.
How Much Does Intuniv Cost?
There is a considerable price disparity between brand-name Intuniv and generic guanfacine, with the generic medication being significantly cheaper. For a 1 mg dosage, 7 tablets of guanfacine cost as little as $24. Conversely, 90 tablets of a 4 mg dosage of Intuniv can cost as much as $905.
For a 1 mg dosage, 7 tablets of guanfacine cost as little as $24. Conversely, 90 tablets of a 4 mg dosage of Intuniv can cost as much as $905.
What is Kapvay?
Kapvay is the brand name for clonidine ER, which is an alpha-2 adrenergic agonist, just like Intuniv. It can be used either alone or as part of a treatment plan. Kapvay is less popular than similar drugs, as it is typically more expensive.
How Does Kapvay Work?
Like Intuniv, it is not clear how Kapvay works to treat ADHD. The medication affects certain receptors in the brain, so it’s believed that these receptors manage the behaviors associated with ADHD symptoms. Its non-stimulant composition makes it favorable for children and adolescents, but it can also be prescribed for adults.
How Long Does Kapvay Last?
Kapvay is an extended-release non-stimulant ADHD medication, so one dosage should last all day, but it can be taken twice daily if needed. Kapvay is prescribed in a very small 0.1 mg dosage and shouldn’t be taken more than twice a day. This will help prevent severe side effects and potential dependence on the drug.
This will help prevent severe side effects and potential dependence on the drug.
What Are the Side Effects of Kapvay?
Kapvay has many of the same side effects as Intuniv, as it falls under the same class of drugs. Allergic reactions to Kapvay are rare, and very few people report experiencing serious side effects.
Some of the most common side effects when taking Kapvay include:
- Lightheadedness
- Dizziness
- Dry mouth
- Constipation
To reduce the risk of lightheadedness and dizziness, get up slowly when rising from a sitting or lying position. If you experience dry mouth from taking Kapvay, suck on sugarless lozenges or ice chips, drink water, or use a saliva substitute.
How Much Does Kapvay Cost?
The brand name Kapvay can be expensive, but the generic clonidine ER is usually a less expensive alternative. The 30 clonidine ER tablets can be as low as $71, while 60 tablets of brand name Kapvay may cost $516. This non-stimulant ADHD medication is covered by a majority of health insurance providers, and it is possible to reduce the price through various coupons and discounts.
What is Qelbree?
Qelbree, the brand name version of viloxazine, is a selective norepinephrine reuptake inhibitor (SNRI) often used as a part of a treatment plan that includes behavioral therapy. Qelbree is only effective in treating children and adolescents ages 6 to 17, so it’s not recommended for adults.
How Does Qelbree Work?
Like Strattera, Qelbree works by adjusting how the brain uses the neurotransmitter norepinephrine, often resulting in increased focus, reduced impulsivity, and regulation of many other ADHD-related symptoms.
How Long Does Qelbree Last?
One capsule of Qelbree lasts all day, and the dosage can be adjusted depending on how you react to the medication. Qelbree’s starting dose is typically 100 mg, but it can be raised to a maximum 400 mg dose if needed. If you have kidney problems, this dosage will have to be carefully managed to prevent any complications.
What Are the Side Effects of Qelbree?
Qelbree has minimal side effects, making it a generally safe non-stimulant ADHD medication compared to some others. That said, the side effects it does have could become more serious and should be carefully monitored. If you have severe side effects like a fast heartbeat or you experience an allergic reaction such as trouble breathing or rash, contact your healthcare provider immediately.
That said, the side effects it does have could become more serious and should be carefully monitored. If you have severe side effects like a fast heartbeat or you experience an allergic reaction such as trouble breathing or rash, contact your healthcare provider immediately.
The most common side effects of Qelbree include:
- Tiredness
- Decreased appetite
- Nausea
- Vomiting
How Much Does Qelbree Cost?
Qelbree doesn’t have a generic alternative available for purchase, making it much less flexible in cost when compared to similar ADHD medications. Prices for Qelbree can be as low as $39 for 3 of the 100 mg capsules, and they can get as high as $1,199 for 90 of the 200 mg capsules.
Which is the Best Non-Stimulant ADHD Medication For You?
Of the non-stimulant ADHD medications listed above, Strattera is the one most often prescribed. It has been found to reduce ADHD symptoms in children who did not respond to stimulant medication, and it has been shown to be helpful in treating all subtypes of ADHD. Strattera is also more effective in treating ADHD in adults than the aforementioned medications, which are usually used to treat childhood ADHD.
Strattera is also more effective in treating ADHD in adults than the aforementioned medications, which are usually used to treat childhood ADHD.
Although Strattera may be more widely useful, it may not be the right medication for everyone. To get the non-stimulant medication that’s right for you, speak to a healthcare provider about your symptoms, medical history, and allergies.
How Klarity Pairs You With the Right ADHD Medication
Klarity can connect you with licensed and certified healthcare providers that specialize in personalized ADHD treatment and non-stimulant ADHD medications.
With an initial online visit, you can receive an evaluation and treatment plan based on your current conditions and medical history. After your healthcare provider determines which medication is best for you, they’ll set you up with a one-month prescription if applicable so you can try it and see how well it works. If the medication works well for you, and without severe side effects, it might be an option for you to receive the direct prescription from your provider on Klarity.
ADHD can be disruptive, but you don’t have to manage your symptoms alone. Schedule an appointment with an ADHD specialist on Klarity today to receive ADHD treatment or diagnosis if applicable.
ADHD Medications: Strattera, Antidepressants & More
There are many drugs other than psychostimulants that can be used to treat ADHD.
Nonstimulant therapy
Strattera® (atomoxetine) is the first nonstimulant medication approved by the Food and Drug Administration (FDA) for the treatment of attention-deficit/hyperactivity disorder (ADHD). Strattera and all the other nonstimulants are generally considered to be less effective than psychostimulants in treating ADHD. The nonstimulants are usually considered second- and third-line medications.
Strattera works on the neurotransmitter (chemical in the brain that transmits nerve impulses) called norepinephrine. Like the stimulant drugs, Strattera is effective in treating and controlling ADHD symptoms. Unlike stimulant drugs, Strattera is not a controlled substance. Therefore, people are less likely to abuse or become dependent on it.
Therefore, people are less likely to abuse or become dependent on it.
In addition, Strattera doesn't cause many of the potential side effects linked to psychostimulants, such as sleeplessness. Strattera can cause very significant abdominal pain, nausea and drowsiness, especially when starting the medication. Strattera tends to offset the effect of the stimulant starting to work and then wearing off. At times, it still should be taken more than once a day.
How does Strattera work?
This medication works by increasing the amount of norepinephrine, an important chemical in the brain. Doing this appears to help ADHD by increasing attention span and reducing impulsive behavior and hyperactivity.
Who should not take Strattera?
There are certain situations in which you shouldn't take Strattera. If you or your child has any of the following conditions, you should inform your healthcare provider before taking Strattera:
- Allergy to Strattera or any of its components.

- Narrow angle glaucoma (a condition that causes increased pressure in the eyes and can lead to blindness).
- Treatment with a type of medication called monoamine oxidase inhibitors (MAOIs), such as Nardil® (phenelzine), Parnate® (tranylcypromine), Marplan® (isocarboxazid) or Emsam® (selegeline transdermal system) within 14 days of starting Strattera.
- An adrenal problem called pheochromocytoma or a history of this condition.
- Severe heart disease.
What are the side effects of Strattera?
The most common side effects in children and adolescents are:
- Upset stomach (e.g., nausea, vomiting).
- Decreased appetite, which may cause weight loss.
- Nausea.
- Dizziness.
- Headache.
- Mood swings.
- Insomnia.
- Drowsiness.
- Abdominal pain.
The most common side effects in adults are:
- Constipation.
- Dry mouth.
- Insomnia.
- Erectile dysfunction.

- Urinary tract abnormalities (e.g., trouble passing urine, pain with urination).
- Painful menstruation.
- Hot flashes.
These side effects can be significant and may require stopping the medication.
However in most cases, these side effects are generally not severe. Only a very small percentage of patients needed to stop Strattera due to side effects experienced during clinical trials.
Allergic reactions to Strattera are rare but do occur, usually as swelling or hives. Tell your provider right away if you or your family member taking Strattera develops a skin rash, swelling, hives or other allergic symptoms.
There have been reports of slightly decreased growth in children and teens taking Strattera. It's recommended that children and adolescents be observed, measured and weighed periodically while on Strattera.
Strattera should be stopped if you have signs of jaundice — yellowing of the skin or whites of the eyes. Jaundice is a sign of liver damage. Itching, right upper belly pain, dark urine and unexplained flu-like symptoms may also be signs of liver injury. If blood tests show evidence of liver damage, stop taking Strattera.
Itching, right upper belly pain, dark urine and unexplained flu-like symptoms may also be signs of liver injury. If blood tests show evidence of liver damage, stop taking Strattera.
Strattera can increase suicidal thinking in teens who take the drug. Patients should be monitored for suicidal thoughts and actions while taking Strattera®.
Strattera can cause serious heart-related complications (e.g., heart attack, stroke), high blood pressure and increased heart rate especially if you have a history of heart and/or vessel disease and/or irregular heart rate. Therefore, patients should be evaluated for heart disease prior to starting Strattera and be monitored for changes in blood pressure and heart rate during therapy.
Strattera should be discontinued if symptoms of psychosis (such as hearing voices, believing things that are not true, being suspicious) or mania occur.
Aggressive or hostile behavior may occur. Therefore, monitoring for this type of behavior during Strattera therapy is recommended.
This is not a complete list of all side effects. If you have questions about side effects, please contact your healthcare provider.
Be sure to tell your healthcare provider:
- If you are nursing, pregnant or plan to become pregnant.
- If you are taking or plan to take any prescription drugs (especially antidepressants or other psychiatric medicines, blood pressure medicines, linezolid or methylene blue), dietary supplements, herbal medicines or nonprescription medications (especially cough and cold medicines that contain decongestants or nonsteroidal anti-inflammatory medicines like ibuprofen or naproxen).
- If you have any past or present medical problems, including high blood pressure, seizures, heart disease, glaucoma or liver or kidney disease.
- If you have a history of drug or alcohol abuse or dependency or if you have had mental health problems, including depression, manic depression or psychosis.
- If you have had any liver problems or jaundice in the past.

- If you become agitated or irritable or if you develop ideas of hurting yourself.
Take Strattera exactly as prescribed by your healthcare provider. It's usually taken once or twice a day and may be taken with or without food. Your physician may adjust the dose until it's correct for you or your child. No specific laboratory testing is required while taking Strattera. It may be used for extended or long-term treatment as long as there are periodic evaluations with your healthcare provider.
Is antidepressant therapy used to treat ADHD?
Several types of antidepressant drugs can be used to treat ADHD. Antidepressant therapy for ADHD is sometimes used as the treatment of choice for children or adults who have ADHD and depression.
Antidepressants, however, are generally not as effective as stimulants or Strattera at improving attention span and concentration.
Antidepressants used for treating ADHD include the following:
- Tricyclic antidepressants, such as Pamelor™ (nortriptyline), Tofranil® (imipramine) and Norpramin® (desipramine) have been shown to be helpful in children and adults with ADHD, but they can cause some unpleasant side effects, such as dry mouth, constipation or urinary problems.
 They are also relatively inexpensive.
They are also relatively inexpensive. - Wellbutrin® (bupropion), a different type of antidepressant, has been found to be effective in treating ADHD in adults and children. It's generally well-tolerated, but it also has some side effects that may be a problem for some people who have anxiety, headaches or seizures.
- Effexor® (venlafaxine) and Effexor XR® (venlafaxine extended-release) are newer antidepressants that increase the levels of norepinephrine and serotonin in the brain. The drugs are effective at improving mood and concentration in adults as well as children and teens. They are occasionally used to treat ADHD.
- Monoamine oxidase inhibitors (MAOIs) are a group of antidepressants that can treat ADHD with some benefit, but are rarely used because they have significant and sometimes serious side effects and can dangerously interact with certain foods and other medications. They may be of benefit in situations when other medications have failed. Examples include Nardil (phenelzine), Parnate (tranylcypromine), Marplan (isocarboxazid) or Emsam (selegeline transdermal system).
 Monoamine oxidase inhibitors are generally not prescribed for children or teens.
Monoamine oxidase inhibitors are generally not prescribed for children or teens.
Note: The FDA has determined that antidepressant medications increase the risk of suicidal thinking and behavior in children and adolescents with depression and other psychiatric disorders. If you have questions or concerns, please discuss them with your healthcare provider.
How do antidepressants work?
Since most antidepressants work by increasing the levels of brain messenger chemicals (neurotransmitters), such as norepinephrine, serotonin and dopamine, it makes sense that they might have effects similar to other ADHD stimulant and nonstimulant treatments that appear to work by similar mechanisms.
Antidepressant treatment can have a small effect on attention span as well as impulse control, hyperactivity and aggressiveness. Children and adolescents treated with antidepressants are often more willing to take direction and may be less disruptive.
Antidepressants have the advantage of a low potential for abuse and there is no evidence that they suppress growth or contribute to significant weight loss.
Who should not take antidepressants?
Antidepressants should not be used in the following situations:
- If you have a history or tendency toward manic behavior or manic depression (bipolar disorder).
- Wellbutrin (bupropion) should not be taken if you have any history of seizures or epilepsy.
- Treatment with antidepressants should not be initiated if you have taken a MAO inhibitor antidepressant, such as Nardil, Parnate. Marplan or Emsam within the last 14 days.
Each type of antidepressant has its own contraindications and usage warnings; you should discuss these with your healthcare provider.
The most common side effects experienced with tricyclic antidepressants include:
- Stomach upset.
- Constipation.
- Dry mouth.
- Blurred vision.
- Drowsiness.
- Dizziness.
- Low blood pressure.
- Weight gain.
- Tremor.
- Sweating.
- Difficulty urinating.
Some tricyclic antidepressants are more likely to cause particular side effects than others.
Tricyclic antidepressants are potentially lethal in the event of an overdose of medication.
Tricyclic antidepressants also have the potential to cause serious heart conduction defects. Periodic electrocardiogram (EKG) monitoring is recommended during tricyclic antidepressant therapy to look for these heart problems.
Wellbutrin sometimes causes stomach upset, anxiety, headaches and rashes.
Effexor and Effexor XR can cause nausea, anxiety, sleep problems, tremor, dry mouth and sexual problems in adults.
Monoamine oxidase inhibitors can cause a wide variety of side effects, including dangerously increased blood pressure when combined with certain foods or medications. Prior to starting MAOI therapy, please consult a healthcare professional concerning potential food and drug interactions.
This is not a complete list of all side effects for antidepressants. If you have questions about side effects, please contact your healthcare provider.
When taking antidepressants for ADHD, be sure to tell your healthcare provider:
- If you are nursing, pregnant or plan to become pregnant.

- If you are taking or plan to take any prescription drugs, dietary supplements, herbal medicines or nonprescription medications.
- If you have any past or present medical problems, including high blood pressure, seizures, heart disease and urinary problems.
- If you have a history of drug or alcohol abuse or dependency or if you have had mental health problems, including depression, manic depression or psychosis.
- If you develop any depressive symptoms or feelings that you might harm yourself.
- If you develop irregular heartbeats (heart palpitations) or fainting spells.
The following are useful guidelines to keep in mind when taking antidepressants or giving them to your child for ADHD:
- Always give the medication exactly as prescribed. If there are any problems or questions, call your healthcare provider.
- Consult your physician prior to discontinuing antidepressant therapy.
- Antidepressants usually take 2-4 weeks before the full effects are apparent.
 Be patient and don’t give up before giving them a chance to work.
Be patient and don’t give up before giving them a chance to work. - Your provider will probably want to start your medication at a low dose and increase gradually until symptoms are controlled.
- It's better not to miss doses of antidepressants. Most are given once or twice a day. If you miss a day or two of Effexor, it can cause an unpleasant withdrawal syndrome.
- Taking bulk laxatives (fiber) and drinking lots of water is a good idea with tricyclic antidepressants, as they tend to cause constipation and hard stools.
- Tell your provider if you notice any new or unusual side effects.
What other nonstimulant therapies are used to treat ADHD?
Two drugs, Kapvay® (extended-release clonidine) and Intuniv® (extended-release guanfacine), have been approved by the FDA for use alone or with stimulant drugs for the treatment of ADHD. These drugs can improve mental functioning as well as behavior in people with ADHD. However, they are usually reserved for those who respond poorly to and cannot tolerate stimulants or Strattera.
Clonidine is also available as a short-acting tablet and as a transdermal patch. Guanfacine is also available as a short-acting tablet. These dosage forms have also been used to treat ADHD, however they are not specifically approved by the FDA for this indication.
How do these drugs treat ADHD?
How these drugs work in treating ADHD is not yet known, but it is clear that they have a calming effect on certain areas of the brain.
Who should not take these drugs?
Kapvay should not be used in patients who are allergic to clonidine (e.g., Catapres®). Intuniv should not be used in patients who are allergic to guanfacine (e.g., Tenex®).
What are the side effects of these drugs?
The most common side effects include:
For Kapvay:
- Drowsiness.
- Headache.
- Irritability.
- Insomnia.
- Nightmares.
- Change in mood.
- Dry mouth.
For Intuniv:
- Drowsiness.
- Headache.

- Nausea.
- Weakness.
- Stomach pain.
- Dizziness.
These drugs can rarely cause irregular heartbeats. They can lower blood pressure and slow heart rate.
Careful screening for heart rhythm irregularities and regular monitoring of blood pressure and EKGs is recommended.
Both drugs can cause significant drowsiness; use caution when operating dangerous equipment or driving until you know how these drugs affect you.
This is not a complete list of side effects. If you experience a potential side effect while taking these drugs, please consult a healthcare professional.
Are there tips and precautions for nonstimulant medications in ADHD treatment?
When taking one of these drugs for ADHD, be sure to tell your healthcare provider:
- If you are nursing, pregnant or plan to become pregnant.
- Consult your provider before discontinuing therapy; Kapvay and Intuniv should not be abruptly discontinued.
- If you are taking or plan to take any prescription drugs, dietary supplements, herbal medicines or nonprescription medications.

- If you have any past or present medical problems, including low blood pressure, seizures, heart rhythm disturbances and urinary problems.
- If you develop irregular heartbeats (heart palpitations) or fainting spells.
The following are useful guidelines to keep in mind when taking clonidine or guanfacine or giving them to your child for ADHD:
- Always take or give the medication exactly as prescribed. If there are any problems or questions, call your provider. It is best not to miss doses as this may cause the blood pressure to rise quickly, which may cause headaches and other symptoms.
- Your health care provider will probably want to start the medication at a low dose and increase gradually until symptoms are controlled.
- For very young children, clonidine short-acting tablets can be formulated into a liquid by a compounding pharmacy to make it easier to give the medication. Short-acting clonidine tablets can be crushed and mixed with food if necessary.
 However, Kapvay which is a long-acting clonidine tablet should not be chewed, crushed or broken.
However, Kapvay which is a long-acting clonidine tablet should not be chewed, crushed or broken. - Intuniv, which is a long-acting guanfacine, should not be chewed, crushed or broken.
- Do not stop clonidine therapy, including Kapvay or guanfacine, including Intuniv, suddenly since this can cause a rebound increase in blood pressure. These medications must be tapered.
Drug load is a problem for people with autism
06/09/17
Many children and adults with autism take many drugs at the same time, which can lead to serious side effects and may not even be effective
Source: Spectrum News
Connor was diagnosed with autism early at the age of 18 months. Even at that age, his condition was obvious. “He would arrange things in rows, turn lights on and off non-stop,” says his mom, Melissa. He was bright, but did not speak until he was 3 years old and quickly lost his temper. When he went to school, he couldn't sit at his desk, shouted out answers without raising his hand, and freaked out when he didn't understand something in math or couldn't write by hand at the same speed as everyone else. “One day he wrapped himself in a carpet like a roll and refused to come out until I arrived at school,” recalls Melissa.
When he went to school, he couldn't sit at his desk, shouted out answers without raising his hand, and freaked out when he didn't understand something in math or couldn't write by hand at the same speed as everyone else. “One day he wrapped himself in a carpet like a roll and refused to come out until I arrived at school,” recalls Melissa.
Connor was prescribed his first psychiatric drug, methylphenidrate (Ritalin), when he was 6 years old. The drug did not last long, but at the age of 7, the parents tried again. The psychiatrist suggested a low dose of dextroamphetamine (Adderall), a psychostimulant used to treat attention deficit hyperactivity disorder (ADHD). The drug markedly improved his behavior at school: now he could sit at his desk longer and follow what the teachers were saying. His handwriting "like a chicken's paw" became legible. Then his handwriting became neat. Then perfect. And then he became the subject of Connor's obsession.
“We were told that there would always be pros and cons. The drug helped him get through a day of school and we thought it was worth it,” says Melissa. And he was worth it. For some time.
The drug helped him get through a day of school and we thought it was worth it,” says Melissa. And he was worth it. For some time.
But when Adderall's action ended at the end of the day, Connor felt worse than ever. During the day he wept and refused to do anything. Because of the psychostimulant, it became difficult for him to fall asleep in the evening. So after a month or two, the psychiatrist added a second drug, guanfacine (Intuniv), to treat ADHD, anxiety, and hypertension, which can also reduce insomnia. The psychiatrist hoped this would ease Connor's daytime and help him sleep.
In a sense, the effect was the opposite. During the day he began to feel better, but Connor developed very severe mood swings and was so irritated every evening that he was very difficult to deal with. And now, instead of just tossing and turning in bed, he began to categorically refuse to go to bed. “He didn’t go to bed because he was always angry about something,” says Melissa. “He worked himself up and couldn’t stop, every night he got upset and started crying. ”
”
Seven months later, the parents said that it was simply impossible to continue taking this combination. They replaced guanfacine with over-the-counter melatonin, which helped Connor sleep better without any visible side effects. However, a year later, he developed a tolerance for Adderall. Connor's psychiatrist increased the dosage, and this, in turn, led to the development of tics: Connor began to jerk his head and sniffle. During a medical examination at the age of 9, the doctor noticed that over the past two years he had hardly grown. His weight had not changed at all since the age of 7, and now he was much lower than normal.
This is where the drug experiments stopped. The parents removed the child from all prescription drugs, and today, at almost 13 years old, Connor still does not take any medication. His tics are almost gone. Although he still struggles to concentrate in class, his mom thinks the risks outweigh the benefits, and she's against new drugs. “If we can somehow manage without drugs, then we will manage without them.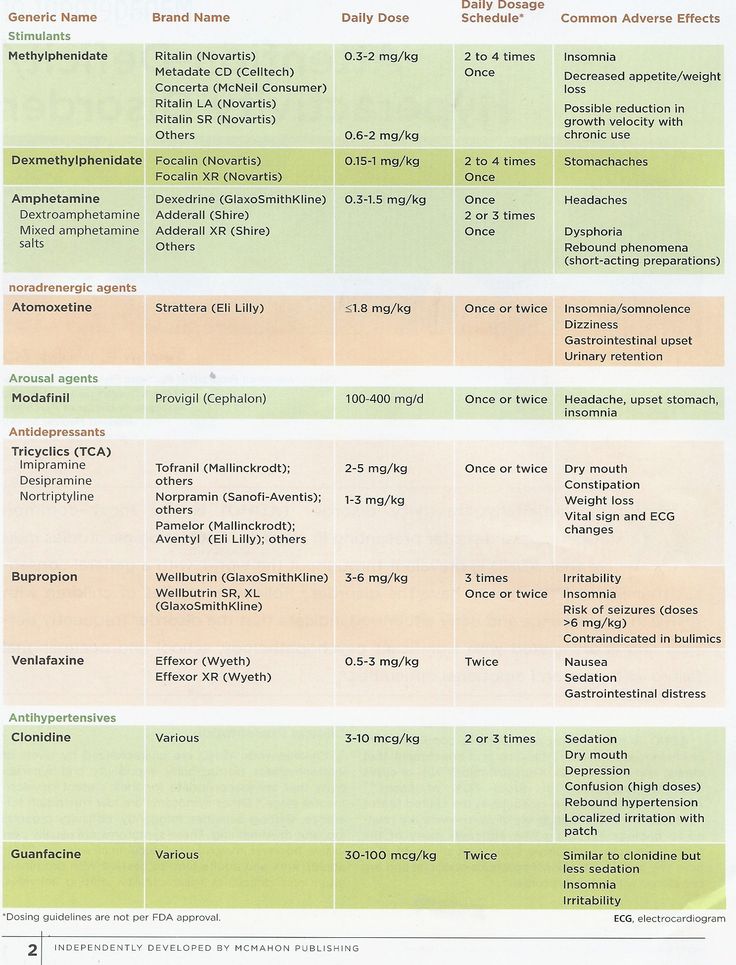 ”
”
Connor is just one of many, many children with autism who are being prescribed multiple drugs at the same time. Phoenix started taking risperidone (Risperdal) at just 4 years old. This drug has been approved for the treatment of irritability in autism. He is now 15 years old and has experience with over ten different psychiatric medications. Ben is 34 and has autism but has been misdiagnosed with other disorders in the past. He was in middle school when his mother insisted that he start taking drugs for depression and behavioral problems. The doctor tried one antidepressant after another, but nothing worked. In high school, at age 15, he was misdiagnosed as having bipolar affective disorder and was prescribed an anticonvulsant drug and an antidepressant.
It is not uncommon for children with autism to take two, three, or even four drugs at the same time. The same is true for many adults with autism. There are not enough statistics on this subject, but the limited information currently available suggests that adults with autism are even more likely to be prescribed multiple drugs than children.
Specialists are particularly concerned about prescribing psychiatric drugs to children because such drugs can have unwanted effects on brain development and are rarely tested on children.
In general, polypharmacy—taking more than one drug at the same time—is very common among people with autism. One study found that among 33,000 people with autism under the age of 21, at least 35% were taking two psychotropic drugs at the same time, and 15% were taking three drugs.
“Psychotropic drugs are so commonly prescribed for people with autism because there are few treatment options,” says Lisa Kroen, director of the Autism Research Program at Kaiser Permanente in California. - Is such a drug load bad? This question is difficult to answer. We just don't know - no research has been done."
Sometimes, as in Connor's case, a second drug is given to treat side effects of the first. Most often, doctors prescribe drugs for each individual symptom - a psychostimulant for concentration, a selective serotonin reuptake inhibitor (SSRI) for depression, an antipsychotic for aggression, and so on. (Children with autism who also have epilepsy take anticonvulsant drugs. But since such drugs are effective and available, they are usually not considered part of the polypharmacy problem.)
(Children with autism who also have epilepsy take anticonvulsant drugs. But since such drugs are effective and available, they are usually not considered part of the polypharmacy problem.)
“Kids come to me on Zoloft, Depakota and risperidone,” says Matthew Siegel, professor of psychiatry and pediatrics at Tufts University in Medford, Massachusetts. Zoloft is an antidepressant, Depakot is a mood stabilizer, and risperidone is an antipsychotic. Three psychotropic drugs per patient.”
In other cases, due to moves, changes in insurance, or dissatisfaction with treatment, people on the spectrum end up with many different doctors, each with their own opinion, who may add a new drug but not remove the old one.
Why is there such confusion? Because there is no single drug for the treatment of autism itself.
There are so-called key characteristics of autism - repetitive behaviors, difficulties with social interaction and impaired communication. Behavioral therapy can help with these three characteristics, but no drug can change them. Those drugs that are prescribed to people with autism are the treatment of peripheral problems that greatly complicate life - ADHD, irritability, anxiety, aggression, self-aggression.
Those drugs that are prescribed to people with autism are the treatment of peripheral problems that greatly complicate life - ADHD, irritability, anxiety, aggression, self-aggression.
The current practice that leads people to take cocktails of psychotropic drugs can be ineffective and harmful. Each doctor decides for himself what will be effective and safe, because there are simply no studies. “We have so few single drug studies, so few studies comparing different drugs alone,” says Brian King, professor of child and adolescent psychiatry at the University of California, San Francisco. “We still have a lot to learn before we even get to research into different combinations of drugs.”
Datura drug
The US Food and Drug Administration has approved only two drugs for children and adolescents with autism: risperidone and aripiprazole. Both are atypical antipsychotics and are prescribed to treat behavioral problems associated with increased irritability, for example, if a child has aggression, tantrums, and self-aggression. These drugs relieve such problems in about 30-50% of cases - they do not help the rest.
These drugs relieve such problems in about 30-50% of cases - they do not help the rest.
This is a huge gap: psychiatric problems are common in children with autism. A 2010 study found that 80% of children with autism who presented to a mental health center also had ADHD, 61% had at least two anxiety disorders, and 56% had clinical depression.
Multiple diagnoses lead to drug cocktails, but there are no clinical trials for drug combinations, so in most cases it is not known how different psychotropic drugs interact with each other. "Each drug has its own side effects, and when you prescribe a mixture of them, you are effectively prescribing a new drug that has not been studied," says King. “And if we are talking about autism, when there can be severe communication disorders, then the risks are even greater, because it is difficult for patients to tell you that they feel bad from your drugs.”
What's more, researchers say these drugs may not work at all for people with autism.
“Many studies have examined the use of drugs to treat ADHD in people with autism. The same is true for drugs to treat obsessive-compulsive disorder and repetitive behaviors, says Daniel Couri, a pediatrician at the National Children's Hospital in Columbus, Ohio. “And virtually all of these studies have shown that these drugs are much less effective for people with autism than for people without autism.”
These studies are relatively rare and were mostly uncontrolled. In 2013, a meta-analysis of existing studies found that most studies of psychiatric drugs for autism are either too small or poorly designed to tell if the drugs are effective. The existing data, the researchers write, “can only be considered speculation that needs to be evaluated in well-controlled studies.”
The symptoms of depression, obsessive-compulsive disorder, ADHD and other psychiatric conditions seem to be the same in people with and without autism. But the causes of autism are very different, which means that the biochemical processes behind them can differ and vary from person to person.
"It's a huge problem with treating autism in general," Siegel says. Autism is caused by so many genetic variations that the condition of each individual can be unique, which means that treatment must be individualized. Even in ideal conditions of clinical trials, the drug can only help 20% of people. The antipsychotics aripiprazole and risperidone stand out because they can be as effective as 50%. “50% is like a record in this area,” Siegel says.
Paradoxically, another reason children and adults with autism may be given different drugs, as in the case of Connor, is that doctors use the second drug to reduce the side effects of the first. Antipsychotics, for example, can lead to weight gain and metabolic disorders, as well as involuntary muscle contractions. Some doctors add metformin for weight gain and benztropine (Cogentin) to relieve involuntary movements.
But every new drug brings its own potential side effects. Metformin can cause muscle pain and, less commonly, anxiety and nervousness. Benztropine can lead to confusion and memory problems. Physicians with little experience in treating patients with autism may mistake side effects for new symptoms and prescribe new drugs in response. In the vast majority of cases, psychotropic drugs are prescribed by doctors with little or no experience with autism, Siegel says. "People just don't know what they're doing, so it's not surprising that kids end up taking multiple drugs."
Benztropine can lead to confusion and memory problems. Physicians with little experience in treating patients with autism may mistake side effects for new symptoms and prescribe new drugs in response. In the vast majority of cases, psychotropic drugs are prescribed by doctors with little or no experience with autism, Siegel says. "People just don't know what they're doing, so it's not surprising that kids end up taking multiple drugs."
Toxic Pills
As a preteen, Ben had problems typical of a child with autism: social anxiety, difficulty communicating with peers, mild depression, violent temper tantrums, inattention, and disruptive behavior in class. When he was 12 years old, school testing revealed he had sensory processing problems and dysgraphia (problems with handwriting), but not autism. At the mother's request, the doctor tried an antidepressant. It didn't help and only led to headaches. A new antidepressant followed, and then another. The side effects weren't worth taking, so Ben got a short break from his medication.
Two years later, when he was 16 years old and his problems at school and at home were getting worse, his mother again insisted on medication. A new doctor prescribed a newly approved SSRI, citalopram (Celexa), recommending that Ben and his mother see a specialist. But for a year, life was too busy to look for a specialist, and Ben just took citalopram.
Over the next year, the situation at the school got worse and worse. Ben was bullied more and more often by his classmates, he increasingly responded to them with aggression, so his mother finally took him to a psychotherapist. He diagnosed Ben with bipolar affective disorder and referred him to a psychiatrist with a recommendation to add valproic acid (Depakote) to his drugs. Ben recalls that the psychiatrist asked him a couple of questions, and then simply gave him a prescription for the two drugs that the therapist asked for. Ben's autism was never diagnosed.
“That's when things really changed,” says Ben. He gained a lot of weight. He couldn't concentrate in class. He made scenes at school and at home, his anxiety reached a new peak. “My behavior has become more aggressive and unpredictable,” he says. In the middle of the night, he would wake up terrified, and then just walk in circles around the room. “I don’t think that such an escalation would have happened without drugs,” he said. He started fighting with his father. “I fell into complete despair, sobbed, I could punch a hole in the wall with my fist.”
He couldn't concentrate in class. He made scenes at school and at home, his anxiety reached a new peak. “My behavior has become more aggressive and unpredictable,” he says. In the middle of the night, he would wake up terrified, and then just walk in circles around the room. “I don’t think that such an escalation would have happened without drugs,” he said. He started fighting with his father. “I fell into complete despair, sobbed, I could punch a hole in the wall with my fist.”
Five drugs and five psychiatrists later, Ben became lethargic, irritable, angry and unable to concentrate on anything.
Finding a combination of drugs is especially difficult if the attending physician changes all the time. In Ben's case, not only was he misdiagnosed, but the family moved twice. In addition, his psychotherapist and psychiatrist did not discuss his diagnosis and treatment with each other. In other cases, people may not have access to doctors who understand autism. Some people change doctors hoping to find an approach they like, or are forced to do so because of insurance changes. The list of drugs is growing due to "the lack of one person responsible for the entire treatment process," says Shafali Jeste, a pediatric neurologist at the University of California, Los Angeles: "In our city, this happens all the time."
The list of drugs is growing due to "the lack of one person responsible for the entire treatment process," says Shafali Jeste, a pediatric neurologist at the University of California, Los Angeles: "In our city, this happens all the time."
The stack of prescriptions may become thicker as the child transitions from adolescence to adulthood.
"People who are prescribed drugs often stay on them for long periods of time and don't even try to determine if they still need them," says David Posey, a psychiatrist in Indianapolis, Indiana. It is usually recommended to review the drug regimen at least once a year, to evaluate the possibility of reducing the dosage, but this is not always possible. "If the drug worked, families might be against trying to take it off."
Jeste says that her clinic is often visited by people with a long list of drugs, but without a well-formed medical record and anamnesis, and it is sometimes impossible for her and her colleagues to understand why a particular drug was ever prescribed and whether it helps. In these cases, she gradually reduces the dosage of one drug after another.
In these cases, she gradually reduces the dosage of one drug after another.
Ben was not lucky enough to find such a specialist. By the end of his last year at school, he fell asleep in class and felt so bad that he dropped out. “Then my parents were getting divorced,” Ben recalls that time. “There was complete chaos around, I was losing all my support, I was losing my usual daily routine, I started sleeping in the car.”
He started smoking marijuana, which he said made him euphoric when combined with antidepressants. But at the same time, she helped him function. “It helped me connect with people better than drugs,” he says. Ben says marijuana helped him better understand how psychiatric drugs work on him, and that they cause the same mood swings, just much more slowly. "I had the idea that maybe the mood cycles I often experience coincide with the drug use."
At the age of 21, he made the decision to get rid of both illegal drugs and prescription drugs. A year later, he was diagnosed with autism. Now he has learned to step aside and take deep breaths every time he feels a fit of anger coming on. No more holes in the wall. He goes for a run six times a week, and physical activity helps him stay calm, clear and focused. Autism may have been responsible for the initial mood swings and aggression, but he says the drugs are a vicious circle.
Now he has learned to step aside and take deep breaths every time he feels a fit of anger coming on. No more holes in the wall. He goes for a run six times a week, and physical activity helps him stay calm, clear and focused. Autism may have been responsible for the initial mood swings and aggression, but he says the drugs are a vicious circle.
Treatment
Multiple medications are not always a bad thing. Some children have very serious problems in their lives, their behavior can pose a serious threat to themselves and others, and in these cases, medication may be the only way out.
Phoenix was one of those children. “He was a little tornado,” his mom says. One day in early 2007, she received a call from the kindergarten asking her to pick him up early because he was being very aggressive, knocking over tables and chairs for no apparent reason. He escaped twice that day - once he jumped out of the car on the way home, then climbed out of the bedroom window. The police found him in the middle of a busy highway. He was only four years old.
Sally, Phoenix's mother, says he has always been a difficult child. But when his mood swings escalated into aggression, he could lash out at people and try to harm his older brother, who also had autism. “He was strong beyond his years,” she says. She knew that at all costs she must help him deal with his anger, for the safety of both boys.
His doctor tried risperidone, then added guanfacine and Adderall. However, this did not affect his aggression. Sally recalls that every morning she and her husband woke up, looked at each other and said: “How is Phoenix now?” After that, "everything inside her froze." It was obvious that drugs needed to be selected, but the family could not cope with him at home. When Phoenix was 6 years old, he was first admitted to the hospital.
By 2009, his clinic had already changed psychiatrists twice. The new psychiatrist replaced Adderall with Vyvans. A blood test then showed that Phoenix had an increased risk of developing breasts, a serious but rare side effect of risperidone called gynecomastia. The psychiatrist changed risperidone to Seroquel. “It was a disaster,” Sally says. Phoenix climbed out of the windows, got up and walked around the classroom, attacked his brother for no reason. None of the drug combinations alleviated the aggression and mood swings. Aude
The psychiatrist changed risperidone to Seroquel. “It was a disaster,” Sally says. Phoenix climbed out of the windows, got up and walked around the classroom, attacked his brother for no reason. None of the drug combinations alleviated the aggression and mood swings. Aude
The case shocked the whole family and ended with a new hospitalization and a new drug combination. The doctors replaced Seroquel with another neuroleptic, Geodon, and also prescribed valproic acid and guanfacine. Since Phoenix's brother, Mack, was greatly helped by Strattera's anti-ADHD drug, the hospital staff replaced Vyvans with Strattera.
Phoenix has been in four different inpatient programs, been hospitalized six times, tried more than a dozen drugs, sometimes four at a time. Hospitalizations helped to take him off certain drugs and gradually introduce others that, at least temporarily, controlled his mood swings. But every time after he was discharged, the drug combinations stopped working and he returned to aggression, mostly against his brother. The first two stationary programs did not help at all. They created stability and structure in his life: every day was the same, the daily routine was very reliable. But the programs could not adjust the drug regimen. And when he returned home, where such a tough regime no longer existed, he began to attack his brother. "We've had holes in our doors from the time Phoenix tried to get to Mac," she says.
The first two stationary programs did not help at all. They created stability and structure in his life: every day was the same, the daily routine was very reliable. But the programs could not adjust the drug regimen. And when he returned home, where such a tough regime no longer existed, he began to attack his brother. "We've had holes in our doors from the time Phoenix tried to get to Mac," she says.
The next two programs focused on children with autism, and they provided the necessary assistance to Phoenix. He was 12 when he entered the third program and began taking an antipsychotic commonly prescribed for bipolar disorder, olanzapine (Zyprexa). And in the fourth inpatient program, when he was 13 years old, doctors found what seemed to be the perfect combination: olanzapine, valproic acid, guanfacine and atomoxetine. He spent weekends at home, but lived at a nearby facility for a week, where he also received behavioral therapy and social adjustment support. “For the first time when he came home, we really enjoyed his company, we were able to see what a real Phoenix is,” says Sally.
But a common side effect of Zyprexa is weight gain, and the drug made Phoenix constantly hungry. “On weekends, he emptied the refrigerator at three in the morning,” she says. The overly thin boy began to suffer from obesity. “He looked like a balloon about to burst,” his mother says. He was sitting and he was short of breath. We had to take it off the Zyprexa."
His doctor took him off Zyprexa and put him on another antipsychotic and then another (Seroquel) until the combination started to work.
Phoenix is now 15 years old, on four drugs and has been stable for over a year. His mood is also stable. “The aggression is gone,” Sally says. He developed a sense of humor and started watching TV with his family and discussing what he saw with them. He also began to develop the capacity for empathy. Now, if he sees that a child at school is behaving the same way as he once did, he says to his brother: "I must apologize to you and mom." According to Sally: “He saw himself from the outside, and it affected him very much. One day, for no reason, he came into the kitchen and said: "You know, mom, I love you." He never said that."
One day, for no reason, he came into the kitchen and said: "You know, mom, I love you." He never said that."
When new symptoms appear, the temptation to change medications can be very strong, especially with a difficult treatment history where parents are used to thinking about the drug approach first. But very often new problems can be solved with simple methods.
This fall, Phoenix began to fall asleep in class during the day. One of the previous drugs had had the same effect on him - he was so sleepy that he could fall asleep even during lunch in a noisy restaurant. Sally was very worried. She was afraid that this meant that the effect of the psychostimulant was ending, or this was some new side effect. She did not want to change the already established treatment regimen.
Before taking him to the doctor, she decided to investigate. She bought a device to restrict and monitor her home Wi-Fi network. It turned out that Phoenix got up at night and spent hours playing on the computer. She started turning off the Internet at night, and Phoenix immediately became alert during the school day.
She started turning off the Internet at night, and Phoenix immediately became alert during the school day.
“It's not uncommon for children to take more than one drug. The question is: do people just try everything in the hope that it will help, or is there some kind of rational justification? says Lawrence Scahill, director of clinical trials at the Marcus Autism Center at Emory University. When treatment decisions are made carefully and with a very clear goal in mind, drug combinations can be very helpful. Under these circumstances, Scahill believes, "we can talk about the so-called rational polypharmacy."
The path of the Phoenix, although very thorny, led him to favorable results. This is an example of how polypharmacy, with care, attention and perseverance, can help people with autism live fulfilling lives.
However, the decision to take drugs always depends on the individual doctor, individual family, individual person. "Every time it's an experiment, but it's not a controlled experiment," Scahill says. Ben, Phoenix and Connor: Each of them faced different problems with no ready-made solutions, because prescribing drugs for autism is still more art than science. There are still no clear rules, and one can only hope that they will nevertheless appear.
Ben, Phoenix and Connor: Each of them faced different problems with no ready-made solutions, because prescribing drugs for autism is still more art than science. There are still no clear rules, and one can only hope that they will nevertheless appear.
See also:
Does a child with autism need to take medication?
Autism treatment - present and future
Autism and mental health
We hope that the information on our website will be useful or interesting for you. You can support people with autism in Russia and contribute to the work of the Foundation by clicking on the "Help" button.
Methods and treatment, Psychiatry
Old man viloxazine for attention deficit hyperactivity disorder
Image: AP.IMPORTANT, CLINICAL TRIALS, NEWSA new non-stimulant ADHD drug is being prepared for launch.
Briefly
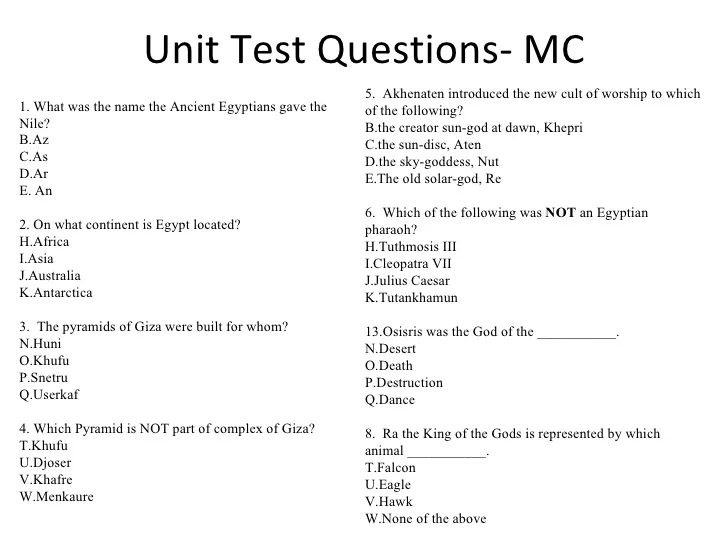
- Supernus Pharmaceuticals successfully conducted two phase III pivotal clinical trials P301 and P303 (multicenter, double-blind, placebo-controlled, parallel group, randomized) of experimental SPN-812, investigating it in non-stimulant treatment of the syndrome attention deficit hyperactivity disorder (ADHD) in children aged 6 to 11 years.

- Results from Phase III clinical trials P302 and P304 testing SPN-812 in adolescents with attention deficit hyperactivity disorder are expected soon. Supernus plans to send the registration dossier to the US Food and Drug Administration (FDA) in the second half of 2019. The appearance on sale is predicted in the second half of 2020. The new product is expected to attract decent interest—peak sales are expected to reach $600 million in 2025—because of the rapid onset of therapeutic effect compared to existing non-stimulant drugs such as Strattera (Strattera, atomoxetine) and Intuniv (Intuniv, guanfacine).
- SPN-812 is a proprietary formulation of viloxazine, a morpholine derivative that is a selective norepinephrine reuptake inhibitor (NRI). Viloxazine, developed by Imperial Chemical Industries and introduced to the European market in 1976, has been widely used as an antidepressant. In 2002, the drug, marketed under the brand names Vivalan, Emovit, Vivarint and Vicilan, was discontinued for commercial reasons.

Details
In rats, viloxazine inhibits the reuptake of norepinephrine in the heart, similar to imipramine, but unlike imipramine and demipramine, does not block the reuptake in the medulla oblongata or hypothalamus. Viloxazine, like demipramine, is a very weak serotonin reuptake inhibitor, but it potentiates serotonin-mediated functions in the brain, similar to amitriptyline (amitriptyline) and imipramine, which are relatively strong serotonin reuptake inhibitors. Viloxazine does not show any anticholinergic effects.
Clinical studies of P301 included 477 patients who received SPN-812 100 or 200 mg daily or placebo for five weeks. The drug groups demonstrated a statistically significant difference with the placebo group in achieving the primary endpoint, as stated by change in total score on the Attention Deficit Hyperactivity Disorder Scale, 5th edition (ADHD-RS-5). There was a change of -16.6 and -17.7 points against -10.9 in the control group (p=0.0004 and p<0. 0001).
0001).
The use of SPN-812 provided a rapid onset of the therapeutic effect: after the first week of treatment, statistically significant changes were recorded (p=0.0004 and p=0.0244). At the end of therapy, there were statistically significant improvements in the ADHD-RS-5 subscales — hyperactivity/impulsivity and inattention (p<0.0001 and p=0.0026).
Clinical trials of P303 included 313 patients who received either 200 or 400 mg SPN-812 daily or placebo for seven weeks. The drug group showed statistically significant improvements on the ADHD-RS-5 scale: −17.6 and −17.5 points versus −11.7 in the placebo group (p=0.0038 and p=0.0063). The therapeutic effect appeared after the first week of treatment, reaching a statistically significant gap with the control group at the fifth week. Similarly to P301, statistically significant positive changes were demonstrated in the ADHD-RS-5 subscales — hyperactivity/impulsivity and inattention (p=0.0020 and p=0.0248).
Forecast of sales of commercialized drugs for the treatment of attention deficit hyperactivity disorder (ADHD).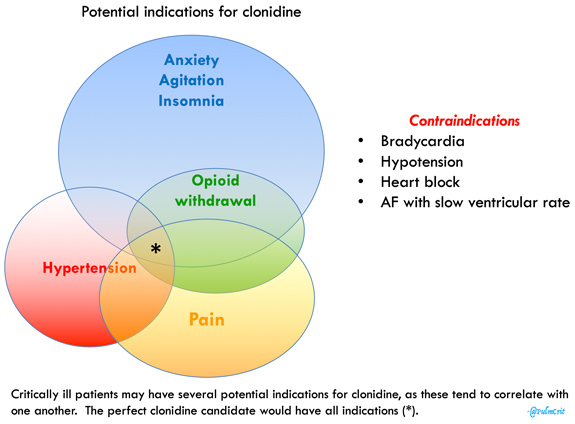 Image: Vantage/EvaluatePharma.
Image: Vantage/EvaluatePharma. The Supernus experimental pipeline also contains: SPN-810 - molindone for the treatment of impulsive aggression in attention deficit hyperactivity disorder, SPN-809 - viloxazine for the treatment of depression, SPN-604 - oxcarbazepine for the treatment of bipolar disorder , SPN-817 is a synthetic form of huperzine A (huperzine A) for the treatment of Dravet's syndrome.
The Supernus portfolio of commercialized medicines includes two sustained release drugs: Oxtellar (Oxtellar, oxcarbazepine) for partial seizures and Trokendi (Trokendi, topiramate) for epilepsy (partial seizures, generalized tonic-clonic seizures, and seizures, caused by Lennox-Gastaut syndrome) and for the prevention of migraine.
Late stage experimental molecules for the treatment of attention deficit hyperactivity disorder (ADHD). Image: Vantage/EvaluatePharma. Other pharmaceutical manufacturers are also involved in the treatment of attention deficit hyperactivity disorder. Thus, dasotralin (dasotralin, SEP-225289), a serotonin, noadrenaline and dopamine reuptake inhibitor (SNDRI), prepared by the Japanese Sumitomo Dainippon Pharma, is awaiting a regulatory verdict. The development of KP415 (methylphenidate in a combined sustained and immediate release formulation) by KemPharm and centanafadine (EB-1020) - SNDRI, which is being developed by Japan's Otsuka Pharmaceutical, is nearing completion.
Thus, dasotralin (dasotralin, SEP-225289), a serotonin, noadrenaline and dopamine reuptake inhibitor (SNDRI), prepared by the Japanese Sumitomo Dainippon Pharma, is awaiting a regulatory verdict. The development of KP415 (methylphenidate in a combined sustained and immediate release formulation) by KemPharm and centanafadine (EB-1020) - SNDRI, which is being developed by Japan's Otsuka Pharmaceutical, is nearing completion.
Important information
Mosmedpreparaty.ru is a specialized research and reference analytical service of the Mosmedpreparaty group of companies, targeted at key events in the global pharmacy, biotechnology, medicine and healthcare industries.
- Nothing on Mosmedpreparaty.ru is an advertisement or promotion of medicines, methods of treatment, medical services.
- Information and publications Mosmedpreparaty.ru are exclusively scientific, educational and informational.
- Medical information broadcast by Mosmedpreparaty.