Should i take viibryd at night or in the morning
Viibryd side effects and how to avoid them
Common Viibryd side effects include gastrointestinal symptoms and insomnia. Learn how to avoid these and when to seek help for serious side effects.
Common Viibryd side effects | Diarrhea | Nausea & vomiting | Insomnia | Serious side effects | How long do side effects last? | Warnings | Interactions | How to avoid side effects
Viibryd (brand name of vilazodone hydrochloride) is an FDA-approved medication for the treatment of major depressive disorder (MDD). Initially approved by the FDA in 2011, Viibryd can effectively reduce depression symptoms by increasing serotonin activity in the body. Serotonin is an important hormone in the body that stabilizes mood, happiness, and overall well-being. Viibryd is a unique medication because it has both selective serotonin reuptake inhibitor (SSRI) activity and serotonergic (5-HT1A) receptor partial agonist activity. As with most antidepressants, Viibryd has some possible side effects.
The most common Viibryd side effects are diarrhea, nausea, vomiting, and insomnia.
The unique side effect profile of Viibryd can make it preferred over other antidepressants for some patients. This is especially useful if a patient has developed sexual/erectile dysfunction, weight gain, or increased blood pressure on an SSRI or an SNRI (serotonin-norepinephrine reuptake inhibitor). Viibryd is also a more suitable option for those who cannot tolerate an atypical second-generation antipsychotic because of weight gain, sedation, extrapyramidal symptoms, or dyslipidemia. It is important for people with MDD to determine with their doctor the best antidepressant treatment plan. While Viibryd is a great option for some people, it may not be the best fit for others. This article is going to dive into possible side effects, warnings, and interactions for Viibryd.
Common side effects of Viibryd
Here are the most common side effects of vilazodone (Viibryd):
- Diarrhea
- Nausea
- Vomiting
- Insomnia
- Headache
- Dry mouth
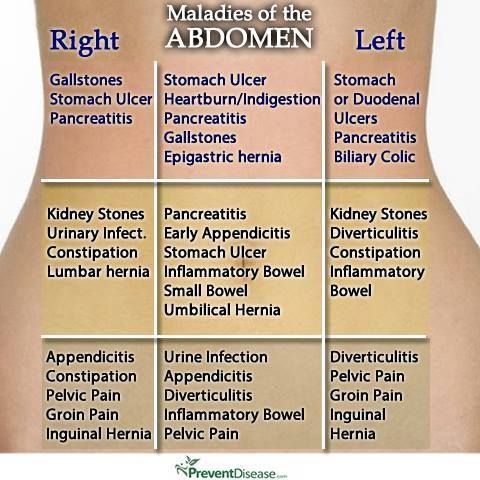
- Stomach pain
- Dizziness
- Blurred vision
- Dry eye
- Sexual dysfunction
- Changes in appetite
Diarrhea
One of the most common side effects of Viibryd is diarrhea and will affect about 28% of people. Most SSRIs and SNRIs can cause gastrointestinal (GI) side effects like diarrhea. Compared to SSRIs and SNRIs, Viibryd has a similar chance of causing GI upset.
Most SSRIs and SNRIs can cause gastrointestinal (GI) side effects like diarrhea. Compared to SSRIs and SNRIs, Viibryd has a similar chance of causing GI upset.
Serotonin is a chemical messenger (neurotransmitter) made in the body that plays a large role in digestion. Medications that work on serotonin receptors in the body can affect the movement of food in the GI tract. As a result, Viibryd can cause diarrhea typically in the first few days or weeks of beginning treatment.
Nausea and vomiting
Other common gastrointestinal side effects of Viibryd include nausea and vomiting. Nausea will happen in about 23% of people, while vomiting is less likely, affecting about 5% of people. Similar to the adverse effect of diarrhea, nausea and vomiting can occur due to the effects serotonin has in the GI tract. Some clinical studies have determined that nausea and vomiting are the most common reasons for discontinuation of antidepressant treatment.
RELATED: Nausea medications and remedies
Insomnia
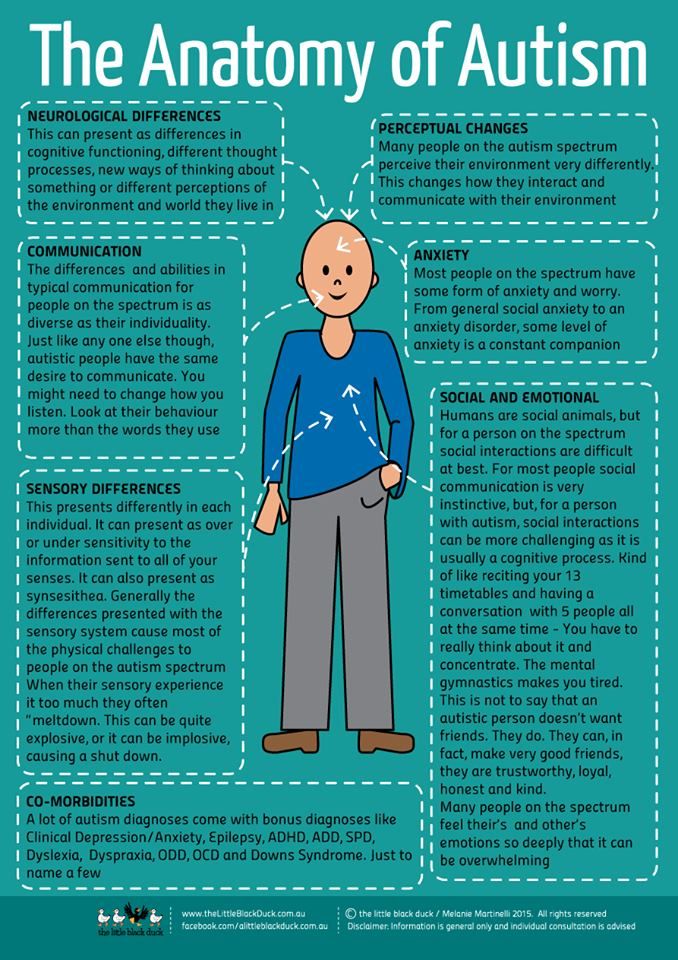
Difficulties falling or staying asleep are possible side effects of Viibryd that affect about 6% of people. On the other hand, sleep disturbances are a main symptom of depression. In the long term, all antidepressants will show improvement in sleep after achieving improvement of mood and daytime activity. However, in the short term, some may impair sleep due to the activating effects the medicine has on the body. The antidepressants with SSRI activity may worsen trouble sleeping due to activation of serotonin receptors.
On the other hand, sleep disturbances are a main symptom of depression. In the long term, all antidepressants will show improvement in sleep after achieving improvement of mood and daytime activity. However, in the short term, some may impair sleep due to the activating effects the medicine has on the body. The antidepressants with SSRI activity may worsen trouble sleeping due to activation of serotonin receptors.
SSRIs have been found to increase REM sleep latency, which measures how long it takes a person to reach their first REM sleep stage after turning the lights out. Additionally, SSRIs were found to reduce the overall time spent in the REM phase while sleeping. These effects on REM sleep are typically within the initial days/weeks of treatment and may return to baseline levels after eight weeks of treatment.
Serious side effects of Viibryd
The following are possible serious side effects of Viibryd:
- Suicidal thoughts and behaviors
- Serotonin syndrome
- Increased risk of bleeding
- Activation of mania or hypomania
- Hyponatremia (abnormally low sodium levels)
- Angle-closure glaucoma
How long do Viibryd side effects last?
Most of the common side effects of Viibryd are temporary while the body adjusts to the new medication. The GI side effects like diarrhea, nausea, and vomiting typically happen within the first few days or weeks of beginning Viibryd. After a few weeks of treatment, GI upset should lessen or resolve. If people experience the side effect of insomnia, they should see improvement after about eight weeks.
The GI side effects like diarrhea, nausea, and vomiting typically happen within the first few days or weeks of beginning Viibryd. After a few weeks of treatment, GI upset should lessen or resolve. If people experience the side effect of insomnia, they should see improvement after about eight weeks.
If any of these common side effects continue after several weeks, are bothersome, or worsen over time, patients should contact their healthcare provider to discuss their treatment. If an allergic reaction is suspected, a healthcare professional should be contacted immediately.
Viibryd contraindications and warnings
Black box warning
Viibryd has a serious warning called a black box warning. As an antidepressant, it has an increased risk of suicidal thinking and behavior in children, adolescents, and young adults for MDD and other psychiatric disorders. The black box warning for Viibryd states that people of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior.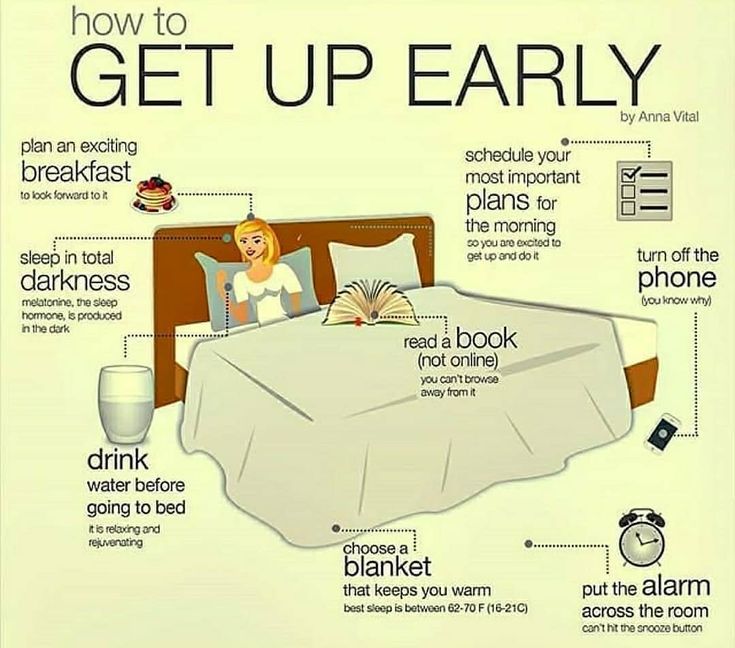 Families and caregivers should be advised of the need for close observation and communication with the healthcare team.
Families and caregivers should be advised of the need for close observation and communication with the healthcare team.
Withdrawal
When a person stops taking Viibryd, there is a chance of discontinuation syndrome. This means there are symptoms that occur when the body withdrawals from the medication. The symptoms of discontinuation syndrome for Viibryd include irritability, agitation, anxiety, and confusion. These withdrawal symptoms could be avoided by slowly reducing the dose to discontinuation rather than an abrupt stop.
Overdose
Clinical trials of Viibryd identified doses of 200 to 280 mg with dangerous adverse reactions including serotonin syndrome, lethargy, restlessness, hallucinations, and disorientation. If an overdose is suspected, people should call 911 or visit an emergency medical facility.
Restrictions
- Viibryd is not approved in pediatric patients.
- For women who are pregnant or breastfeeding, Viibryd should only be used if the potential benefits outweigh the potential risks due to limited data.
- Use caution in patients with a history of seizure disorder.
- Use caution in patients with bipolar disorder.
- Avoid use in patients with angle-closure glaucoma or anatomically narrow angles of the eyes as Viibryd use could trigger an angle-closure attack and cause severe eye pain.
Viibryd interactions
Viibryd has several drug interactions that should be avoided to prevent dangerous side effects. The following are medications and medication classes that should be avoided:
- MAOIs: Viibryd cannot be used at the same time as a class of drug called MAOI (monoamine oxidase inhibitors) or within 14 days of stopping or starting an MAOI. Examples of MAOIs are phenelzine (Nardil), selegiline (Zelapar), tranylcypromine (Parnate), and isocarboxazid (Marplan). This interaction is serious and potentially life-threatening as it can cause dangerously high levels of serotonin, known as serotonin syndrome.
- Linezolid: This is an antibiotic that can lead to toxic levels of serotonin if taken with Viibryd.
- Methylene blue injection: This treatment for methemoglobinemia can lead to toxic levels of serotonin if taken with Viibryd.
- NSAIDs and anticoagulants: Viibryd may increase the risk of bleeding if taken with NSAIDs (nonsteroidal anti-inflammatory drugs) such as ibuprofen or naproxen, aspirin, and other medications that affect blood clotting.
How to avoid Viibryd side effects
When starting a new medication, it’s important to read the drug information provided with the prescription and talk with a pharmacist for medical advice about potential side effects.
1. Take Viibryd as directed
The typical dose of Viibryd is a 40 mg tablet taken by mouth once daily. When this medicine is started, people will usually work their way up to the treatment dose of 40 mg daily. The typical starting dose is 10 mg daily for seven days, followed by 20 mg once daily for an additional seven days, and then increase to 40 mg once daily. Viibryd is available as a Starter Kit that includes the 10 mg, 20 mg, and 40 mg doses for starting therapy. Starting on a lower dose and gradually increasing the dose can help to lessen side effects.
Viibryd is available as a Starter Kit that includes the 10 mg, 20 mg, and 40 mg doses for starting therapy. Starting on a lower dose and gradually increasing the dose can help to lessen side effects.
If a dose is missed, it’s important to take the missed dose as soon as it’s remembered. However, if the time is close to the next dose, skip the missed dose and return to the normal dosing time. Do not take two doses at the same time or extra doses.
2. Take Viibryd with food
Some medications, like Viibryd, must be taken with food to make sure the medicine works properly. Taking Viibryd with food can help make sure the dose is effective.
3. Read the black box warning
It’s important for people and their family members or close friends to understand the black box warning associated with Viibryd. People should be aware of and closely monitor for warning signs of suicidal thoughts and behaviors. The National Suicide Prevention Lifeline is available 24/7 via a toll-free hotline: 1-800-273-8255.
4. Tell the doctor about all medications being taken
Some medications, like MAOIs, can cause dangerous drug interactions if taken with Viibryd. MAOIs should not be used with Viibryd or within 14 days of stopping or starting an MAOI. Viibryd may increase the risk of bleeding if taken with NSAIDs (like ibuprofen or naproxen), aspirin, warfarin, and other medications that affect blood clotting. It’s important that a healthcare professional is aware of all medications, including over-the-counter medications and supplements, being taken by patients starting new medications.
5. Do not abruptly stop taking Viibryd
If patients want to stop taking Viibryd because of side effects or they think the medication is not helping their depression, their healthcare providers should be consulted. Abruptly stopping Viibryd can lead to discontinuation syndrome. Symptoms include irritability, agitation, anxiety, and confusion. If Viibryd needs to be stopped, patients should work with their healthcare providers to slowly reduce the dose to discontinuation.
RELATED: What to know before switching antidepressants
6. Tell the doctor about all medical conditions
To avoid potentially serious side effects with Viibryd, tell the prescribing healthcare provider about all medical conditions. This is especially important for patients with a history of seizures, bipolar disorder, or abnormal bleeding. It’s important that a healthcare professional is aware of all medical conditions a patient has before starting new medications.
7. Keep all doctor appointments after starting Viibryd
Like most antidepressants, Viibryd takes several weeks to work in the body. Most people will notice improvements in their depression symptoms after two to six weeks, while the maximum benefit may take six to 12 weeks. Over the initial few weeks of starting Viibryd, people may have gradual dose increases to the treatment dose so it’s important that people are aware of the dose they should be taking. Communication with the healthcare team is also important to discuss any ongoing side effects, the patient’s mental health, and determine if the medication is effective for the patient.
8. Lessen gastrointestinal side effects
Viibryd may cause diarrhea, nausea, and/or vomiting side effects. If these side effects happen, they will most likely happen in the first few days or weeks. Viibryd should be taken with food to help with absorption—and taking the dose with food can also help to prevent stomach upset. Additionally, the dose can be taken as close to bedtime as possible. This way people can rest in bed and fall asleep before any nausea develops.
9. Manage the side effect of insomnia
Viibryd may cause trouble sleeping when it is first started. This can lead to daytime tiredness and some reports of abnormal dreams. Typically, insomnia will resolve, and sleep should improve in patients after several weeks. In the meantime, people can practice good sleep hygiene habits. Some good sleep hygiene practices include setting a sleep schedule with a fixed wake-up time, following a nightly routine, and ensuring a healthy lifestyle (some examples include cutting down on afternoon/evening caffeine, being physically active, reducing alcohol consumption, and not eating dinner late).
Vilazodone (Viibryd) | NAMI: National Alliance on Mental Illness
Brand name: Viibryd®
- Tablets: 10 mg, 20 mg, 40 mg
Generic name: vilazodone (vil AZ oh done)
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Vilazodone And What Does It Treat?
Vilazodone is an antidepressant medication that works in the brain. It is approved for the treatment of major depressive disorder (MDD).
Symptoms of depression include:
- Depressed mood - feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, and helpless
- Loss of interest or pleasure in your usual activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving and thinking in slow motion)
- Suicidal thoughts or behaviors
What Is The Most Important Information I Should Know About Vilazodone?
Do not stop taking vilazodone, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medicine.
With input from you, your health care provider will assess how long you will need to take the medicine.
Missing doses of vilazodone may increase your risk for relapse in your symptoms.
Stopping vilazodone abruptly may result in one or more of the following withdrawal symptoms: irritability, nausea, feeling dizzy, vomiting, nightmares, headache, and/or paresthesias (prickling, tingling sensation on the skin).
Depression is also a part of bipolar illness. People with bipolar disorder who take antidepressants may be at risk for "switching" from depression into mania. Symptoms of mania include "high" or irritable mood, very high self-esteem, decreased need for sleep, pressure to keep talking, racing thoughts, being easily distracted, frequently involved in activities with a large risk for bad consequences (for example, excessive buying sprees).
Medical attention should be sought if serotonin syndrome is suspected. Please refer to serious side effects for signs/symptoms.
Are There Specific Concerns About Vilazodone And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with MDD who wish to become pregnant face important decisions. Untreated MDD has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
Caution is advised with breastfeeding since vilazodone does pass into breast milk.
What Should I Discuss With My Health Care Provider Before Taking Vilazodone?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your provider. Some side effects may pass with time, but others may require changes in the medication.
- Any other psychiatric or medical problems you have, including a history of bipolar disorder
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment. Your provider can explain how these different treatments work with the medication.
- If you are pregnant, plan to become pregnant, or are breastfeeding
- If you drink alcohol or use drugs
How Should I Take Vilazodone?
Vilazodone is usually taken one time per day with food or milk.
Typically patients begin at a low dose of medicine and the dose is increased slowly over several weeks.
The dose usually ranges from 20 mg to 40 mg. Only your health care provider can determine the correct dose for you.
Consider using a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Vilazodone?
If you miss a dose of vilazodone, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your health care provider. Do not double your next dose or take more than what is prescribed.
What Should I Avoid While Taking Vilazodone?
Avoid drinking alcohol or using illegal drugs while you are taking antidepressant medications. They may decrease the benefits (e.g., worsen your condition) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Vilazodone?
If an overdose occurs, call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of vilazodone does not exist.
What Are The Possible Side Effects Of Vilazodone?
Common side effects
Diarrhea, nausea, vomiting, dry mouth, dizziness, insomnia
Rare/serious side effects
Night sweats, decreased appetite, migraine headaches, sleepiness, tremor, blurry vision, dry eyes, abnormal dreams, agitation, restlessness, increased urination, sexual dysfunction, angle closure glaucoma (symptoms of angle closure glaucoma may include eye pain, changes in vision, swelling or redness in or around eye), Serotonin syndrome (symptoms may include shivering, diarrhea, confusion, severe muscle tightness, fever, seizures, and death), palpitations, irregular heartbeat
Vilazodone may increase the risk of bleeding events. Combined use of aspirin, nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen), warfarin, and other anti-coagulants may increase this risk. This may include gums that bleed more easily, nose bleed, or gastrointestinal bleeding. Some cases have been life threatening.
Combined use of aspirin, nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen), warfarin, and other anti-coagulants may increase this risk. This may include gums that bleed more easily, nose bleed, or gastrointestinal bleeding. Some cases have been life threatening.
Are There Any Risks For Taking Vilazodone For Long Periods Of Time?
To date, there are no known problems associated with long term use of vilazodone. It is a safe and effective medication when used as directed.
What Other Medications May Interact With Vilazodone?
Vilazodone should not be taken with or within 2 weeks of taking monoamine oxidase inhibitors (MAOIs). These include phenelzine (Nardil®), tranylcypromine (Parnate®), isocarboxazid (Marplan®), rasagiline (Azalect®) and selegiline (Emsam®).
Although rare, there is an increased risk of serotonin syndrome when vilazodone is used with other medications that increase serotonin, such as other antidepressants, migraine medications called “triptans” (e. g., Imitrex®), some pain medications (e.g., tramadol (Ultram®), and the antibiotic linezolid (Zyvox®).
g., Imitrex®), some pain medications (e.g., tramadol (Ultram®), and the antibiotic linezolid (Zyvox®).
The following medications may increase the levels and effects of vilazodone requiring decreased dose of vilazodone:
- Antibiotics, such as clarithromycin (Biaxin®), erythromycin (Ery-Tab®), and telithromycin (Ketek®)
- Antifungals, such as fluconazole (Diflucan®), ketoconazole (Nizoral®), and itraconazole (Sporanox®)
- Blood pressure medications, such as verapamil (Calan®, Covera-HS®, Isoptin SR®) and diltiazem (Cardizem®, Tiazac®)
- HIV medications such as protease inhibitors: indinavir (Crixivan®), ritonavir (Norvir®), saquinavir (Fortovase®, Invirase®), and lopinavir/ritonavir (Kaletra®)
- Nefazodone
The following medications may decrease the levels and effects of vilazodone requiring increased dose of vilazodone: carbamazepine (Tegretol®), oxcarbazepine (Trileptal®), rifampin (Rifadin®), phenytoin (Dilantin®), and phenobarbital
How Long Does It Take For Vilazodone To Work?
Sleep, energy, or appetite may show some improvement within the first 1-2 weeks. Improvement in these physical symptoms can be an important early signal that the medication is working. Depressed mood and lack of interest in activities may need up to 6-8 weeks to fully improve.
Improvement in these physical symptoms can be an important early signal that the medication is working. Depressed mood and lack of interest in activities may need up to 6-8 weeks to fully improve.
Summary of FDA Black Box Warnings
Suicidal thoughts or actions in children and adults
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications. This risk may persist until significant remission occurs.
risk may persist until significant remission occurs.
In short-term studies, antidepressants increased the risk of suicidality in children, adolescents, and young adults when compared to placebo. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24. Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Provided by
(December 2020)
©2020 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Ministry of Health
Almost all of us in our lives are taking any medications. The range of medicines is significant and is constantly expanding. Medications require special attention when using them. Many medicines should only be used as directed by a doctor, who will give you advice on how to use them. But there are general rules drugs, to name some of them.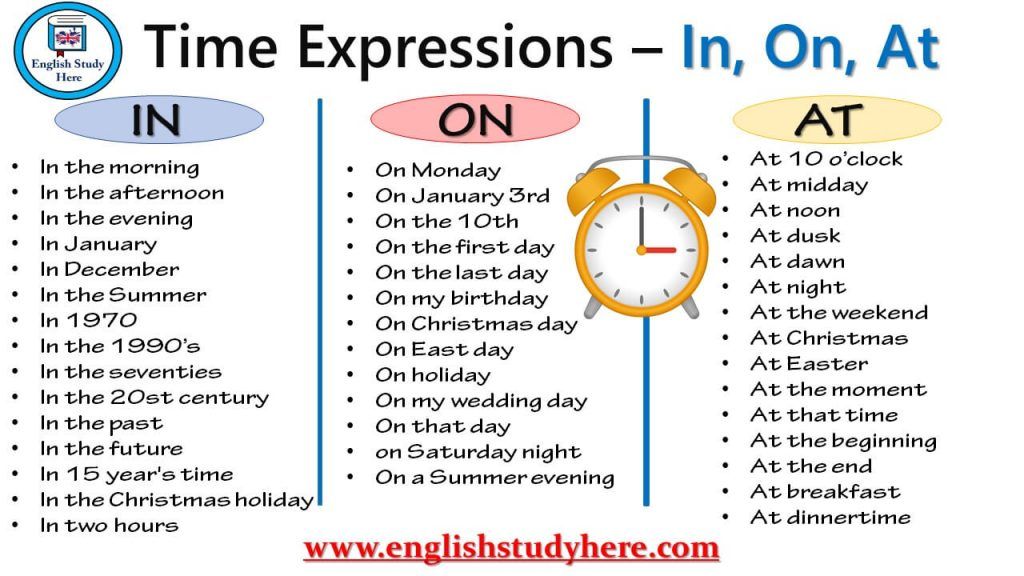
If medicinal drugs prescribed to be taken several times a day, then calculate the interval between doses you need based on 24 hours:
- if medicine is needed take 2 times a day, then the interval between doses will be 12 hours (for example, at 8 am and 8 pm),
- if 3 times - then 8 hours (for example, at 7 o'clock morning, 3 pm and 11 pm)
- if 4 times - interval will be 6 hours (for example, 6 am, 12 noon, 6 pm and 24 nights).
- if an appointment is scheduled medicines 1 time per day, then you need to take the drug every day at the same time time.
Assortment of medicines varied and in some cases it is possible to use the same drug 1, 2 or 3 times a day, but it is important to observe the daily dosage. Therefore, at the appointment with the doctor, tell him how it is more convenient for you and / or your child. take medicine: 1, 2 or 3 times a day.
Any medicine needed taken correctly: on an empty stomach, before, after or with meals, as indicated in instructions.
Taking with food means taking medicine while eating,
on an empty stomach - this is about half an hour before breakfast,
before meals - this is at least 30 - 40 minutes before meals,
after eating is 1.5 - 2 hours after eating.
If you are treating your throat with aerosols/gargles and / or absorbable tablets, then within 1-2 hours after the procedure (or as indicated in the instructions) it is advisable not to drink or eat.
Wash down the majority drugs need clean non-carbonated water in a volume of at least 100 ml, that is half a glass. In some cases, the volume of water can be at least 200-250 ml (glass).
It is forbidden drink tablets/capsules with tea, coffee, Coca-Cola, Pepsi-Cola, sweet juices, soda, alcoholic drinks.
If a the instructions do not indicate when to take the drug and how to take it drink, it means that the reception is allowed at any time, but it would be more correct done with water at room temperature.
If the tablet needs to be sucked, then it can not be chewed, if it is indicated that you need to chew, then the pill is not worth it to swallow. Most often you can't to divide the coated tablet and dragee, because the shell protects the medicine from the action of the acidic environment of the stomach and / or protects the stomach from the action of the drug. If a there is no dividing strip on the tablet, then, most likely, it cannot be break apart.
Undesirable take several different pills at once. If it's necessary, then take your medicine with a break from 30 minutes to 1 hour.
At taking enterosorbents (for example, activated charcoal) and any other tablets the interval between their adoption should be at least 2 hours.
It is necessary to carry out full course of treatment. Often people, having felt improvement, stop taking drug. This is not true. But if you have any unwanted (side) effect, you should consult your doctor about the possibility of further its application.
Particular attention needs to be paid taking medications children, pregnant and lactating women, people over 65, drivers, athletes.
For children, a wide range is now being produced. assortment with children's dosage forms and dosages.
Recall that it is necessary strictly observe the rules for storing medicines (for example, in a cool place - until 18 degrees, in the refrigerator - from 2 to 8 degrees, some medicines cannot be frozen, many medicines require storage in a dark, dry place) and their expiration dates. Storage conditions and expiration date are indicated on the packaging of the medicinal product.
Before taking medicinal product (and preferably before its purchase) must be carefully read the instructions that came with it.
When is the best time to take blood pressure medication? Scholars Advise
- Michelle Roberts
- BBC News online
Image copyright Getty Images
To get the most benefit from blood pressure medications, take them before bedtime, Spanish scientists advise. This simple advice could save lives, they write in a study published in European Heart Journal .
This simple advice could save lives, they write in a study published in European Heart Journal .
Study says pills protect against strokes and heart attacks better when taken before bed rather than in the morning.
Experts have come to the conclusion that a person's response to drugs is influenced by the "biological clock" and the natural rhythm of our body.
Researchers are finding evidence that many medicines, including those for the heart, work best when taken at certain times of the day.
The study, published in the European Heart Journal, is the largest of its kind to date. It was attended by 19 thousand people taking medication for pressure.
Participants were randomly divided into two groups: one took the pill in the morning, the other before bed. The researchers tracked their condition for the next five years or more.
As a result, they concluded that those participants in the study who took medication in the evening, the risk of death from a heart attack, stroke or heart failure was half as much.
Image copyright, Getty Images
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of story Podcast
Blood pressure should decrease at night when we sleep and our body rests.
If this does not happen and the pressure remains high, then the risk of a heart attack or stroke increases, experts say.
Taking medication in the evening helps control nighttime blood pressure in people with hypertension (high blood pressure), according to a study.
Study participants who took medication before bed had significantly lower mean blood pressure levels both during the day and at night. At night, their blood pressure was lower than those who took the medication in the morning.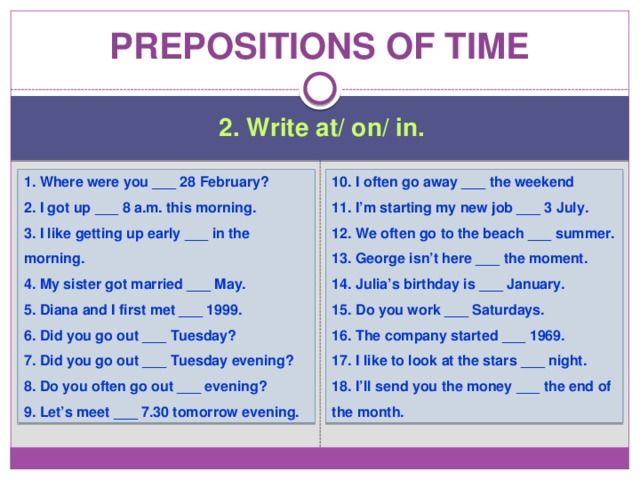
Lead researcher Professor Ramón Hermida of the Spanish University of Vigo said doctors could take this into account and start recommending that their patients take blood pressure medication at night: "It's completely free and could save a lot of lives."
"Current guidelines for the treatment of hypertension do not provide any indication of the best time to take medication. The most common recommendation by doctors is to take pills in the morning with breakfast, but this is based on the erroneous theory that this reduces morning blood pressure," he says.
- What time of day is best not to get treated. And don't get sick
- Will you die in the next 5-10 years? New Blood Test Helps Find The Answer , said the professor.
At the same time, he added that more studies still need to be done among different population groups to check whether his findings with his Spanish colleagues apply to all patients taking different drugs for pressure.