Feeling sad before period
Why It Happens, Treatments, and Finding Support
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Is it PMS?
Premenstrual syndrome (PMS) is a collection of physical and emotional symptoms that start a week or so before your period. It makes some people feel more emotional than usual and others bloated and achy.
PMS can also make people feel depressed in the weeks leading up to their period. This may make you feel:
- sad
- irritable
- anxious
- tired
- angry
- teary
- forgetful
- absentminded
- uninterested in sex
- like sleeping too much or too little
- like eating too much or too little
Other reasons you might feel depressed before your period include:
- Premenstrual dysphoric disorder (PMDD). PMDD is very similar to PMS, but its symptoms are more severe.
Many people with PMDD report feeling very depressed before their period, some to the point of thinking about suicide. While recent research estimates about 75 percent of women have PMS during their reproductive years, only 3 to 8 percent have PMDD.
- Premenstrual exacerbation. This refers to when symptoms of an existing condition, including depression, become worse in the weeks or days leading up to your period. Depression is one of the most common conditions that coexists with PMS. About half of all women who get treated for PMS also have either depression or anxiety.
Read on to learn more about the connection between PMS and depression.
Experts aren’t sure about the exact cause of PMS, but it’s likely linked to hormonal fluctuations that happen during the second half of the menstrual cycle.
Ovulation happens about halfway through your cycle. During this time, your body releases an egg, causing estrogen and progesterone levels to drop. A shift in these hormones can cause both physical and emotional symptoms.
A shift in these hormones can cause both physical and emotional symptoms.
Changes in estrogen and progesterone levels also influence serotonin levels. This is a neurotransmitter that helps regulate your mood, sleep cycle, and appetite. Low levels of serotonin are linked to feelings of sadness and irritability, in addition to trouble sleeping and unusual food cravings — all common PMS symptoms.
Your symptoms should improve when estrogen and progesterone levels rise again. This usually happens a few days after you get your period.
There’s no standard treatment for depression during PMS. But several lifestyle changes and a few medications may help relieve your emotional symptoms.
Track your symptoms
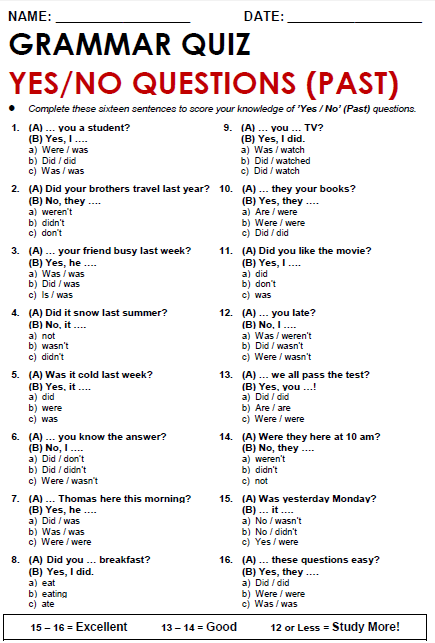
If you don’t already, start keeping track of your menstrual cycle and your emotions throughout its different stages. This will help you confirm that your depression symptoms are indeed linked to your cycle. Knowing that there’s a reason you’re feeling down can also help keep things in perspective and offer some validation.
Having a detailed log of your last few cycles is also handy if you want to bring up your symptoms with your doctor. There’s still some stigma around PMS, and having documentation of your symptoms might help you feel more confident about bringing them up. It can also help your doctor get a better idea of what’s going on.
You can track your cycle and symptoms using period-tracking app on your phone. Look for one that allows you to add your own symptoms.
You can also print out a chart or make your own. Across the top, write the day of the month (1 through 31). List your symptoms down the left side of the page. Put an X in the box next to the symptoms you experience each day. Note whether each symptom is mild, moderate, or severe.
To track depression, make sure to note when you experience any of these symptoms:
- sadness
- anxiety
- crying spells
- irritability
- food cravings or appetite loss
- poor sleep or too much sleep
- trouble concentrating
- lack of interest in your daily activities
- tiredness, lack of energy
Hormonal birth control
Hormonal birth control methods, such as the pill or patch, can help with bloating, tender breasts, and other physical PMS symptoms. For some people, they can also help with emotional symptoms, including depression.
For some people, they can also help with emotional symptoms, including depression.
But for others, hormonal birth control can make depression symptoms worse. If you go this route, you might have to try out different types of birth control before you find a method that works for you. If you’re interested in the pill, opt for a continuous one that doesn’t have a week of placebo pills. Continuous birth control pills can eliminate your period, which sometimes helps eliminate PMS, too.
Natural remedies
A couple of vitamins may help relieve PMS-related symptoms of depression.
A clinical trial found that a calcium supplement helped with PMS-related depression, appetite changes, and tiredness.
Many foods are good sources of calcium, including:
- milk
- yogurt
- cheese
- leafy green vegetables
- fortified orange juice and cereal
You can also take a daily supplement containing 1,200 milligrams of calcium, which you can find on Amazon.
Don’t be discouraged if you don’t see results right away. It can take about three menstrual cycles to see any symptom improvement while taking calcium.
Vitamin B-6 might also help with PMS symptoms.
You can find it in the following foods:
- fish
- chicken and turkey
- fruit
- fortified cereals
Vitamin B-6 also comes in supplement form, which you can find on Amazon. Just don’t take more than 100 milligrams a day.
Learn about other supplements that can help with PMS symptoms.
Lifestyle changes
Several lifestyle factors also seem to play a role in PMS symptoms:
- Exercise. Try to be active for at least 30 minutes more days of the week than not. Even a daily walk through your neighborhood can improve symptoms of depression, fatigue, and trouble concentrating.
- Nutrition. Try to resist the junk food cravings that can come with PMS. Large amounts of sugar, fat, and salt can all wreak havoc on your mood.
 You don’t have to cut them out completely, but try to balance out these foods with fruits, vegetables, and whole grains. This will help keep you full throughout the day.
You don’t have to cut them out completely, but try to balance out these foods with fruits, vegetables, and whole grains. This will help keep you full throughout the day. - Sleep. Not getting enough sleep can kill your mood if you’re weeks away from your period. Try to get at least seven to eight hours of sleep a night, especially in the week or two leading up to your period. See how not getting enough sleep affects your mind and body.
- Stress. Unmanaged stress can worsen depression symptoms. Use deep breathing exercises, meditation, or yoga to calm both your mind and body, especially when you feel PMS symptoms coming on.
Medication
If other treatment options aren’t helping, taking an antidepressant may help. Selective serotonin reuptake inhibitors (SSRIs) are the most common type of antidepressant used to treat PMS-related depression.
SSRIs block the absorption of serotonin, which increases the amount of serotonin in your brain. Examples of SSRIs include:
Examples of SSRIs include:
- citalopram (Celexa)
- fluoxetine (Prozac and Sarafem)
- paroxetine (Paxil)
- sertraline (Zoloft)
Other antidepressants that work on serotonin might also help treat PMS depression. These include:
- duloxetine (Cymbalta)
- venlafaxine (Effexor)
Work with your doctor to come up with a dosage plan. They might suggest you only take an antidepressant during the two weeks before your symptoms tend to start. In other cases, they might recommend taking them every day.
Your gynecologist might be the first person you turn to for help when PMS depression becomes overwhelming. It’s important that your doctor is someone you trust and who takes your symptoms seriously. If your doctor doesn’t listen to you, search for another provider.
You can also turn to the International Association for Premenstrual Disorders. It offers blogs, online communities, and local resources that can help you find a doctor familiar with PMS and PMDD.
If you or someone you know is having suicidal thoughts — related to PMS depression or not — get help from a crisis or suicide prevention hotline. Try the National Suicide Prevention Lifeline at 800-273-8255.
If you think someone is at immediate risk of self-harm or hurting another person:
- Call 911 or your local emergency number.
- Stay with the person until help arrives.
- Remove any guns, knives, medications, or other things that may cause harm.
- Listen, but don’t judge, argue, threaten, or yell.
Why It Happens, Treatments, and Finding Support
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Is it PMS?
Premenstrual syndrome (PMS) is a collection of physical and emotional symptoms that start a week or so before your period. It makes some people feel more emotional than usual and others bloated and achy.
PMS can also make people feel depressed in the weeks leading up to their period. This may make you feel:
This may make you feel:
- sad
- irritable
- anxious
- tired
- angry
- teary
- forgetful
- absentminded
- uninterested in sex
- like sleeping too much or too little
- like eating too much or too little
Other reasons you might feel depressed before your period include:
- Premenstrual dysphoric disorder (PMDD). PMDD is very similar to PMS, but its symptoms are more severe. Many people with PMDD report feeling very depressed before their period, some to the point of thinking about suicide. While recent research estimates about 75 percent of women have PMS during their reproductive years, only 3 to 8 percent have PMDD.
- Premenstrual exacerbation. This refers to when symptoms of an existing condition, including depression, become worse in the weeks or days leading up to your period. Depression is one of the most common conditions that coexists with PMS. About half of all women who get treated for PMS also have either depression or anxiety.
Read on to learn more about the connection between PMS and depression.
Experts aren’t sure about the exact cause of PMS, but it’s likely linked to hormonal fluctuations that happen during the second half of the menstrual cycle.
Ovulation happens about halfway through your cycle. During this time, your body releases an egg, causing estrogen and progesterone levels to drop. A shift in these hormones can cause both physical and emotional symptoms.
Changes in estrogen and progesterone levels also influence serotonin levels. This is a neurotransmitter that helps regulate your mood, sleep cycle, and appetite. Low levels of serotonin are linked to feelings of sadness and irritability, in addition to trouble sleeping and unusual food cravings — all common PMS symptoms.
Your symptoms should improve when estrogen and progesterone levels rise again. This usually happens a few days after you get your period.
There’s no standard treatment for depression during PMS. But several lifestyle changes and a few medications may help relieve your emotional symptoms.
But several lifestyle changes and a few medications may help relieve your emotional symptoms.
Track your symptoms
If you don’t already, start keeping track of your menstrual cycle and your emotions throughout its different stages. This will help you confirm that your depression symptoms are indeed linked to your cycle. Knowing that there’s a reason you’re feeling down can also help keep things in perspective and offer some validation.
Having a detailed log of your last few cycles is also handy if you want to bring up your symptoms with your doctor. There’s still some stigma around PMS, and having documentation of your symptoms might help you feel more confident about bringing them up. It can also help your doctor get a better idea of what’s going on.
You can track your cycle and symptoms using period-tracking app on your phone. Look for one that allows you to add your own symptoms.
You can also print out a chart or make your own. Across the top, write the day of the month (1 through 31). List your symptoms down the left side of the page. Put an X in the box next to the symptoms you experience each day. Note whether each symptom is mild, moderate, or severe.
List your symptoms down the left side of the page. Put an X in the box next to the symptoms you experience each day. Note whether each symptom is mild, moderate, or severe.
To track depression, make sure to note when you experience any of these symptoms:
- sadness
- anxiety
- crying spells
- irritability
- food cravings or appetite loss
- poor sleep or too much sleep
- trouble concentrating
- lack of interest in your daily activities
- tiredness, lack of energy
Hormonal birth control
Hormonal birth control methods, such as the pill or patch, can help with bloating, tender breasts, and other physical PMS symptoms. For some people, they can also help with emotional symptoms, including depression.
But for others, hormonal birth control can make depression symptoms worse. If you go this route, you might have to try out different types of birth control before you find a method that works for you. If you’re interested in the pill, opt for a continuous one that doesn’t have a week of placebo pills. Continuous birth control pills can eliminate your period, which sometimes helps eliminate PMS, too.
Continuous birth control pills can eliminate your period, which sometimes helps eliminate PMS, too.
Natural remedies
A couple of vitamins may help relieve PMS-related symptoms of depression.
A clinical trial found that a calcium supplement helped with PMS-related depression, appetite changes, and tiredness.
Many foods are good sources of calcium, including:
- milk
- yogurt
- cheese
- leafy green vegetables
- fortified orange juice and cereal
You can also take a daily supplement containing 1,200 milligrams of calcium, which you can find on Amazon.
Don’t be discouraged if you don’t see results right away. It can take about three menstrual cycles to see any symptom improvement while taking calcium.
Vitamin B-6 might also help with PMS symptoms.
You can find it in the following foods:
- fish
- chicken and turkey
- fruit
- fortified cereals
Vitamin B-6 also comes in supplement form, which you can find on Amazon. Just don’t take more than 100 milligrams a day.
Just don’t take more than 100 milligrams a day.
Learn about other supplements that can help with PMS symptoms.
Lifestyle changes
Several lifestyle factors also seem to play a role in PMS symptoms:
- Exercise. Try to be active for at least 30 minutes more days of the week than not. Even a daily walk through your neighborhood can improve symptoms of depression, fatigue, and trouble concentrating.
- Nutrition. Try to resist the junk food cravings that can come with PMS. Large amounts of sugar, fat, and salt can all wreak havoc on your mood. You don’t have to cut them out completely, but try to balance out these foods with fruits, vegetables, and whole grains. This will help keep you full throughout the day.
- Sleep. Not getting enough sleep can kill your mood if you’re weeks away from your period. Try to get at least seven to eight hours of sleep a night, especially in the week or two leading up to your period.
 See how not getting enough sleep affects your mind and body.
See how not getting enough sleep affects your mind and body. - Stress. Unmanaged stress can worsen depression symptoms. Use deep breathing exercises, meditation, or yoga to calm both your mind and body, especially when you feel PMS symptoms coming on.
Medication
If other treatment options aren’t helping, taking an antidepressant may help. Selective serotonin reuptake inhibitors (SSRIs) are the most common type of antidepressant used to treat PMS-related depression.
SSRIs block the absorption of serotonin, which increases the amount of serotonin in your brain. Examples of SSRIs include:
- citalopram (Celexa)
- fluoxetine (Prozac and Sarafem)
- paroxetine (Paxil)
- sertraline (Zoloft)
Other antidepressants that work on serotonin might also help treat PMS depression. These include:
- duloxetine (Cymbalta)
- venlafaxine (Effexor)
Work with your doctor to come up with a dosage plan. They might suggest you only take an antidepressant during the two weeks before your symptoms tend to start. In other cases, they might recommend taking them every day.
They might suggest you only take an antidepressant during the two weeks before your symptoms tend to start. In other cases, they might recommend taking them every day.
Your gynecologist might be the first person you turn to for help when PMS depression becomes overwhelming. It’s important that your doctor is someone you trust and who takes your symptoms seriously. If your doctor doesn’t listen to you, search for another provider.
You can also turn to the International Association for Premenstrual Disorders. It offers blogs, online communities, and local resources that can help you find a doctor familiar with PMS and PMDD.
If you or someone you know is having suicidal thoughts — related to PMS depression or not — get help from a crisis or suicide prevention hotline. Try the National Suicide Prevention Lifeline at 800-273-8255.
If you think someone is at immediate risk of self-harm or hurting another person:
- Call 911 or your local emergency number.
- Stay with the person until help arrives.
- Remove any guns, knives, medications, or other things that may cause harm.
- Listen, but don’t judge, argue, threaten, or yell.
PMS, bad mood, menstruation, bad mood in PMS, how PMS is treated In fact, an aggressive and hysterical woman during PMS is a reason to send her to the doctor, and not throw her wallet at her, as in a popular status on social networks.
According to the gynecologist of the medical network "Boris" Oksana Ukrayets, if the family marks the dates of the mother's menstruation in the calendar in order to foresee when she will have mood problems the day before, then this is not the norm. To understand what to do with a bad mood in PMS, it is important to understand a few of its main characteristic points.
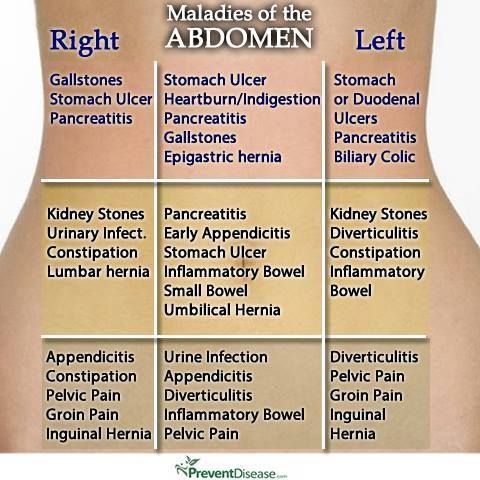
PMS is always a hormonal imbalance. This means that some hormones are produced more than necessary, some less. This leads to the fact that a woman may feel any symptoms. And these symptoms are not limited to just a bad mood. A woman may have a stomach ache or headache a few days before her period, her blood pressure or temperature may rise, she may feel weak and depressed, maybe even depressed. The stronger the imbalance, the more pronounced the symptoms of PMS. If the imbalance is mild, then the woman may not notice its effects.
A woman may have a stomach ache or headache a few days before her period, her blood pressure or temperature may rise, she may feel weak and depressed, maybe even depressed. The stronger the imbalance, the more pronounced the symptoms of PMS. If the imbalance is mild, then the woman may not notice its effects.
PMS depends on age . In different periods of life, a woman tolerates PMS in different ways. The pronounced symptoms of PMS are usually characteristic of adolescence, when the correct production of hormones has not yet been established, and disappear by the age of 20, when a regular cycle is established. Then, at the age of 40-45, the gradual fading of the production of female hormones begins. This process lasts for several years, and during this period the symptoms of PMS become more pronounced.
PMS depends on lifestyle . When we are active, healthy, happy, in love, we usually do not have PMS. Or the symptoms are so minor that we may not notice them. On the contrary, there are factors that exacerbate hormonal imbalance. These are factors that interfere with the normal production of female hormones:
On the contrary, there are factors that exacerbate hormonal imbalance. These are factors that interfere with the normal production of female hormones:
excessive physical activity - if a woman spends too much time in the gym, she begins to produce an excess amount of the male hormone testosterone. In this case, problems with the menstrual cycle may begin;
strict diet – a lack of useful substances that the body experiences with severe food restrictions leads, among other things, to hormonal imbalance;
chronic fatigue syndrome, stress can also be included here.
With severe PMS, it is necessary to eliminate the cause, not the consequences . PMS is not a disease, and the condition does not need to be treated unless it interferes with your life. If your mood or other symptoms of PMS spoil the life of you and your loved ones, you should go to a gynecologist. Depending on the type of PMS, the doctor will prescribe treatment.
What treatment is needed?
If you feel bad during PMS, you know about it, but you just need to cry, read a book, watch a nice movie, chat with a friend or eat a chocolate bar, and your life is getting better, then nothing needs to be done about it. If you are hysterical and throw yourself at everyone or fall into a depressive state, then you should not justify your "nerves" by the fact that you are a woman and you have PMS, but it is better to go to the doctor to identify the cause of your inadequate condition and cope with it, having received doctor's recommendations.
If you are hysterical and throw yourself at everyone or fall into a depressive state, then you should not justify your "nerves" by the fact that you are a woman and you have PMS, but it is better to go to the doctor to identify the cause of your inadequate condition and cope with it, having received doctor's recommendations.
Depending on the symptoms and possible causes that affect the symptoms, there are four types of PMS: edematous, neuropsychic, crisis and cephalgic. Mood changes such as irritability, aggressiveness, depression, loss of energy are characteristic of the neuropsychic form. In addition, sometimes women with this form of PMS may experience auditory and olfactory hallucinations, memory problems, feelings of fear, suicidal thoughts, she may cry or laugh for no reason. There may also be headache, bloating, appetite disorders, breast engorgement.
To confirm the diagnosis of PMS, in addition to the patient's story, you need a blood test to determine the level of hormones progesterone, prolactin and estradiol, which is determined in different phases of the cycle. In the neuropsychic form, as a rule, the level of prolactin increases. Also, the doctor may recommend a consultation with a psychiatrist and a neurologist.
In the neuropsychic form, as a rule, the level of prolactin increases. Also, the doctor may recommend a consultation with a psychiatrist and a neurologist.
To correct the neuropsychic form of PMS, the doctor may prescribe sedative (sedative) drugs, as well as hormonal drugs - analogues of progesterone.
How to avoid anxiety?
To prevent a bad mood during PMS, adjust your work and rest schedule, go in for sports. Eat more foods rich in vitamin B6: walnuts, fish, liver, soy. Do not forget about vegetables and fruits as fiber-rich foods. But limit the use of alcohol, coffee, tea, chocolate in the last phase of the cycle.
Tatyana Koryakina
Psychological problems and PMS. How to understand what is the difference?
Mood swings are one of the common symptoms attributed to PMS.
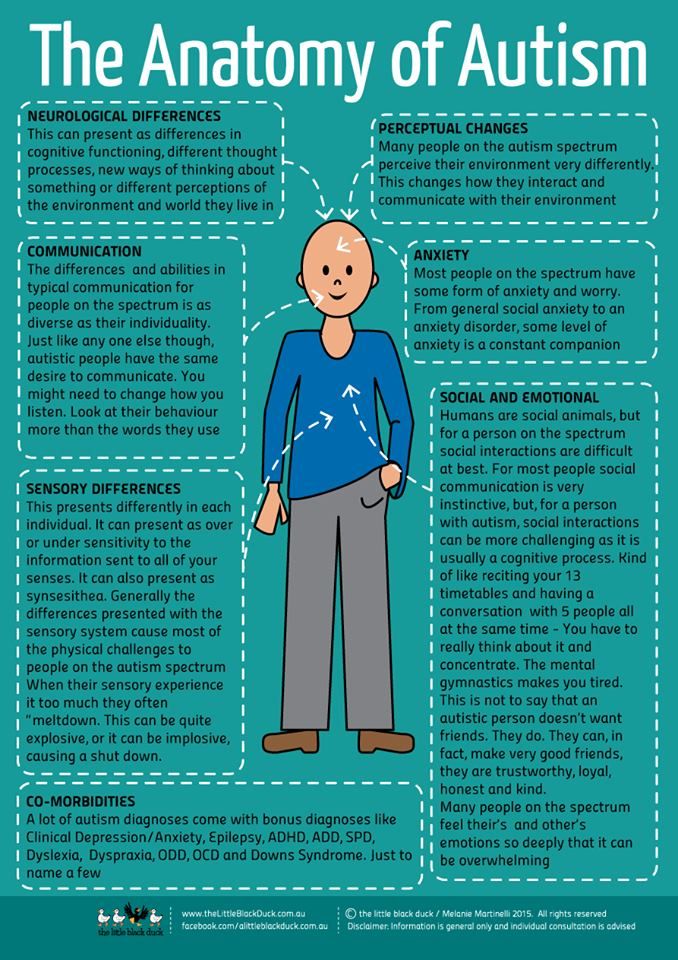
PMS itself is poorly understood and is largely attributed to all women in general, and this is one of the stereotypes that needs to be combated, because it attributes negative emotions to female biology, while in fact, far from all women and far from each cycle experience the psychological symptoms of PMS.
What's more, research suggests that, on average, men and women are equally affected by the same mood swings.
How exactly do hormones affect mental health?
There is no exact answer to this question, but, apparently, the cyclical monthly work of the ovaries plays a key role, producing different amounts of the hormones estradiol and progesterone in each part of the cycle, which, in turn, can affect neurotransmitters, that is, how signals travel through our brains.
Rapidly changing levels of these hormones can affect mood not only before and during menstruation, but also after childbirth and before menopause, leading to a cascade of reactions in the body that cause such hormone-dependent depressive states in predisposed people.
How to distinguish PMS from other psychological problems?
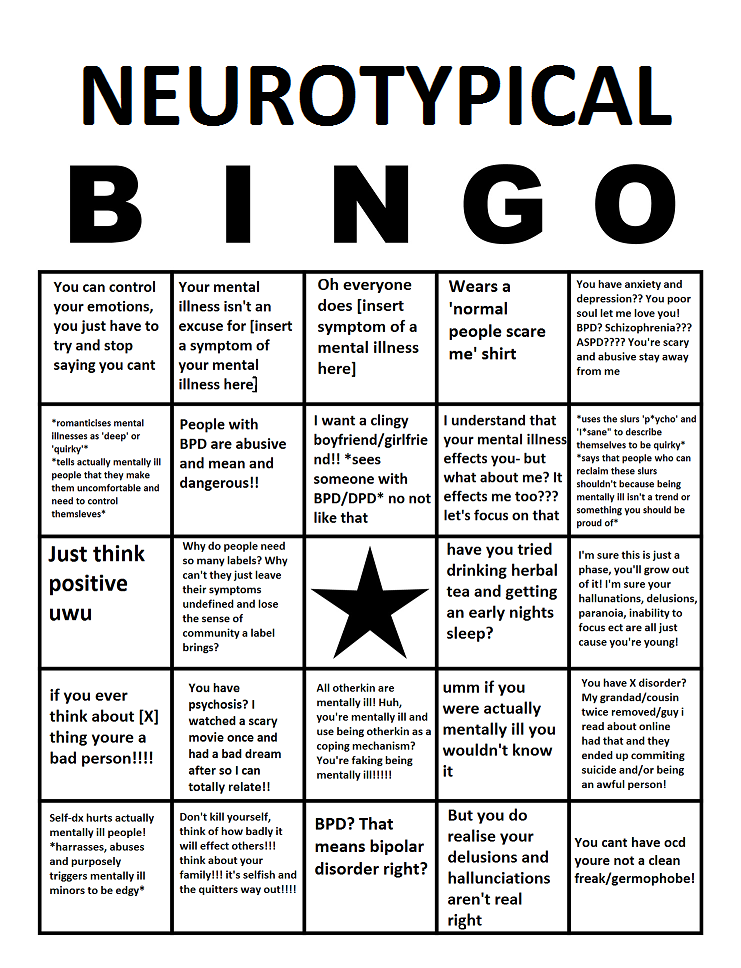
It is important to remember that the stereotypes that surround PMS are similar to those that surround people who have experienced mental health problems, and this stigma needs to be addressed.
From a psychological point of view, it is important to distinguish whether the symptoms are caused specifically by hormonal changes characteristic of PMS or by some other pre-existing mental state. Both women with and without mental health problems can suffer from PMS. Many women are simply afraid to talk about their mood swings and depression just because they believe that they will simply be written off as PMS and supposedly inevitable female biology, they will be called weak and simply devalued.
In rare cases, mood swings and depression can be so severe that they can develop into a serious problem and have a very negative impact on a woman's psychological well-being, which is why it is important to know and be able to recognize the signs that you need qualified help.
PMS and PMDD and their impact on the psychological well-being of women
A severe affective disorder with severe psychological symptoms of PMS is called premenstrual dysphoric disorder. About 3-5% of women suffer from it. PMDD can cause extreme mood swings and intense feelings of hopelessness, deep sadness and depression, and anxiety so severe that it interferes with women's daily lives.
About 3-5% of women suffer from it. PMDD can cause extreme mood swings and intense feelings of hopelessness, deep sadness and depression, and anxiety so severe that it interferes with women's daily lives.
If you're not sure if your symptoms are normal, you can ask other women how they feel during PMS and compare their answers with your own and analyze the differences.
Remember that PMDD is not fiction, but a condition that must be taken seriously and requires medical attention because it interferes with normal life.
How to deal with PMS and its psychological aspects?
It is important to be able to recognize and manage the psychological symptoms of PMS and the additional stress it can put on you.
-
Try to maintain physical mobility and lead an active lifestyle: when moving, endorphins are released, and even a short walk can improve your mood a little.
-
It may seem that a huge chocolate cake or an extra portion of fried potatoes will quickly improve your mood if things are really bad, but in fact it is not, especially if such food has a “forbidden fruit” flavor for you and you will scold yourself later for it . In any health condition, it is better to stick to a balanced diet and not to spread rot on yourself if something did not go as planned.
-
Try to find things that help you relax or calm down. It even makes sense to have a special list of activities and things that make you happy, so that if you are completely sad and at a loss, there is somewhere to look and do something good for yourself. Relaxation helps relieve stress and distract from intrusive thoughts, and the ability to properly rest and recover is one of the most important skills in taking care of yourself.
How do you know if you need help?
Try to mark all symptoms on a special calendar or application to see if they are related to your cycle.