What types of eating disorders are there
Types, Causes, Treatment, and Recovery
Although the term “eating” is in the name, eating disorders are about more than food. They’re complex mental health conditions that often require the intervention of medical and psychological experts to alter their course.
These disorders are described in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) (1).
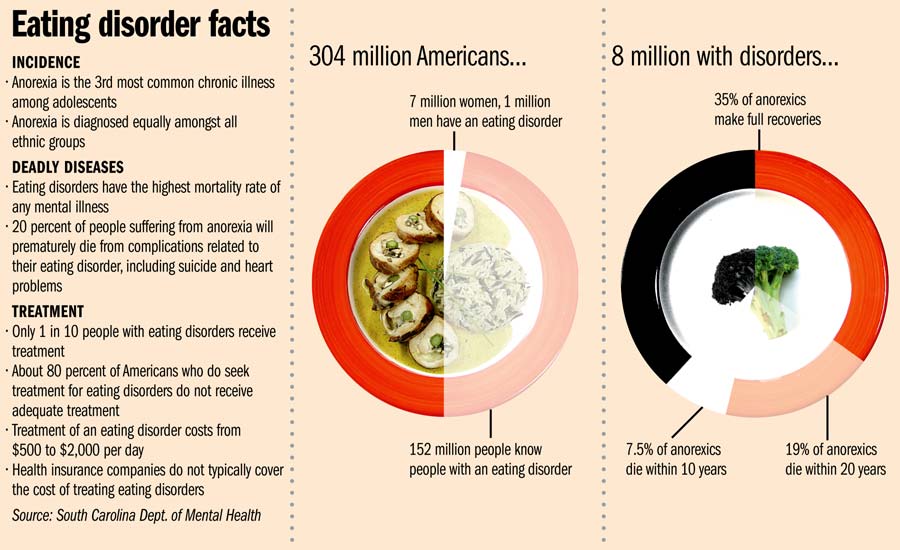
In the United States alone, an estimated 28 million Americans have or have had an eating disorder at some point in their life (2).
This article describes six of the most common types of eating disorders and their symptoms.
Eating disorders are a range of psychological conditions that cause unhealthy eating habits to develop. They might start with an obsession with food, body weight, or body shape (3).
In severe cases, eating disorders can cause serious health consequences and may even result in death if left untreated. In fact, eating disorders are among the deadliest mental illnesses, second to opioid overdose (4).
People with eating disorders can have a variety of symptoms. Common symptoms include severe restriction of food, food binges, and purging behaviors like vomiting or overexercising.
Although eating disorders can affect people of any gender at any life stage, they’re increasingly common in men and gender nonconforming people. These populations often seek treatment at lower rates or may not report their eating disorder symptoms at all (5, 6).
Different types of eating disorders have different symptoms, but each condition involves an extreme focus on issues related to food and eating, and some involve an extreme focus on weight.
This preoccupation with food and weight may make it hard to focus on other aspects of life (3).
Mental and behavioral signs may include (7):
- dramatic weight loss
- concern about eating in public
- preoccupation with weight, food, calories, fat grams, or dieting
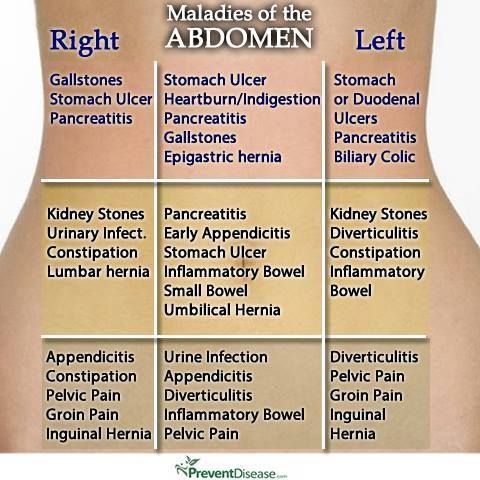
- complaints of constipation, cold intolerance, abdominal pain, lethargy, or excess energy
- excuses to avoid mealtime
- intense fear of weight gain or being “fat”
- dressing in layers to hide weight loss or stay warm
- severely limiting and restricting the amount and types of food consumed
- refusing to eat certain foods
- denying feeling hungry
- expressing a need to “burn off” calories
- repeatedly weighing oneself
- patterns of binge eating and purging
- developing rituals around food
- excessively exercising
- cooking meals for others without eating
- missing menstrual periods (in people who would typically menstruate)
Physical signs may include (7):
- stomach cramps and other gastrointestinal symptoms
- difficulty concentrating
- atypical lab test results (anemia, low thyroid levels, low hormone levels, low potassium, low blood cell counts, slow heart rate)
- dizziness
- fainting
- feeling cold all the time
- sleep irregularities
- menstrual irregularities
- calluses across the tops of the finger joints (a sign of inducing vomiting)
- dry skin
- dry, thin nails
- thinning hair
- muscle weakness
- poor wound healing
- poor immune system function
Experts believe that a variety of factors may contribute to eating disorders.
One of these is genetics. People who have a sibling or parent with an eating disorder seem to be at an increased risk of developing one (3).
Personality traits are another factor. In particular, neuroticism, perfectionism, and impulsivity are three personality traits often linked to a higher risk of developing an eating disorder, according to a 2015 research review (8).
Other potential causes include perceived pressures to be thin, cultural preferences for thinness, and exposure to media promoting these ideals (8).
More recently, experts have proposed that differences in brain structure and biology may also play a role in the development of eating disorders. In particular, levels of the brain messaging chemicals serotonin and dopamine may be factors (9).
However, more studies are needed before strong conclusions can be made.
Eating disorders are a group of related conditions involving extreme food and weight issues, but each disorder has unique symptoms and diagnosis criteria.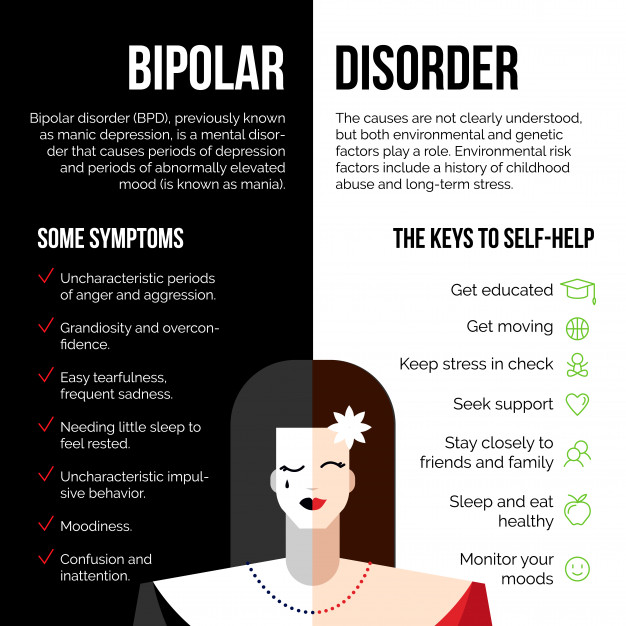 Here are six of the most common eating disorders and their symptoms.
Here are six of the most common eating disorders and their symptoms.
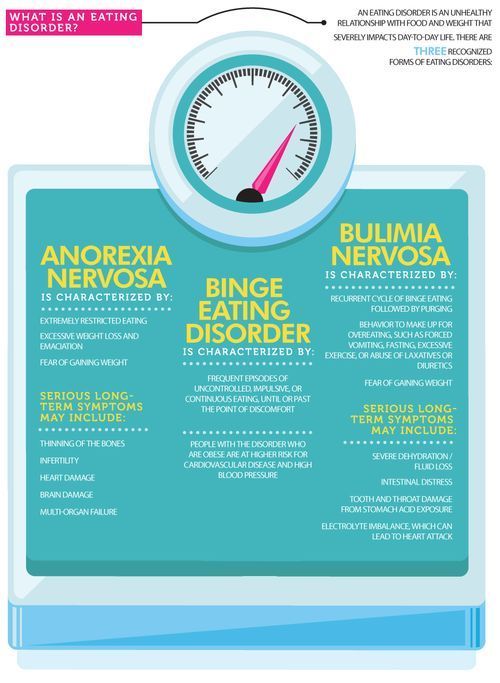
Anorexia nervosa is likely the most well-known eating disorder.
It generally develops during adolescence or young adulthood and tends to affect more women than men (10).
People with anorexia generally view themselves as overweight, even if they’re dangerously underweight. They tend to constantly monitor their weight, avoid eating certain types of foods, and severely restrict their calorie intake.
Common symptoms of anorexia nervosa include (1):
- very restricted eating patterns
- intense fear of gaining weight or persistent behaviors to avoid gaining weight, despite being underweight
- a relentless pursuit of thinness and unwillingness to maintain a healthy weight
- a heavy influence of body weight or perceived body shape on self-esteem
- a distorted body image, including denial of being seriously underweight
However, it’s important to note that weight should not be the major focus of diagnosing someone with anorexia.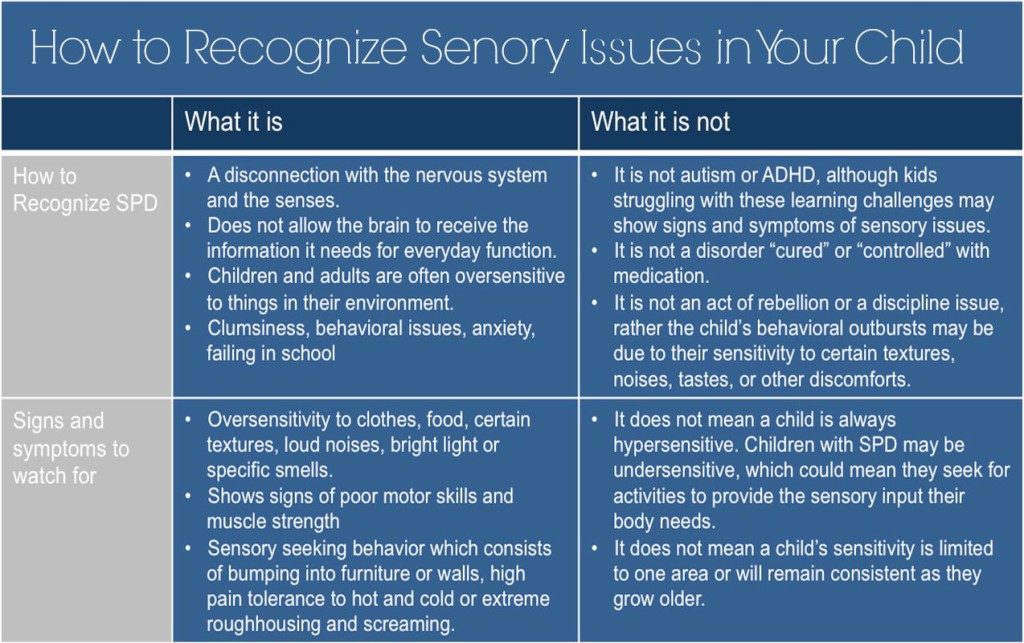
Using body mass index as a factor in diagnosis is outdated because people who are categorized as “normal” or “overweight” can have the same risks.
In atypical anorexia, for example, a person may meet the criteria for anorexia but not be underweight despite significant weight loss (7).
Obsessive-compulsive symptoms are also often present. For instance, many people with anorexia are preoccupied with constant thoughts about food, and some may obsessively collect recipes or hoard food.
They may also have difficulty eating in public and exhibit a strong desire to control their environment, limiting their ability to be spontaneous (3).
Anorexia is officially categorized into two subtypes — the restricting type and the binge eating and purging type (1).
Individuals with the restricting type lose weight solely through dieting, fasting, or excessive exercise.
Individuals with the binge eating and purging type may binge on large amounts of food or eat very little.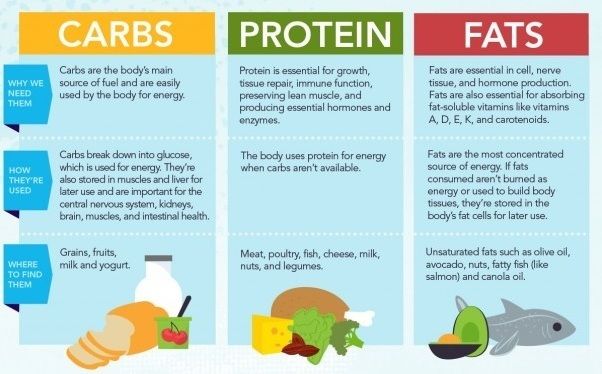 In both cases, after they eat, they purge using activities such as vomiting, taking laxatives or diuretics, or exercising excessively.
In both cases, after they eat, they purge using activities such as vomiting, taking laxatives or diuretics, or exercising excessively.
Anorexia can be very damaging to the body. Over time, individuals living with it may experience thinning of their bones, infertility, and brittle hair and nails.
In severe cases, anorexia can result in heart, brain, or multi-organ failure and death.
Bulimia nervosa is another well-known eating disorder.
Like anorexia, bulimia tends to develop during adolescence and early adulthood and appears to be less common among men than women (10).
People with bulimia frequently eat unusually large amounts of food in a specific period of time.
Each binge eating episode usually continues until the person becomes painfully full. During a binge, the person usually feels that they cannot stop eating or control how much they are eating.
Binges can happen with any type of food but most commonly occur with foods the individual would usually avoid.
Individuals with bulimia then attempt to purge to compensate for the calories consumed and to relieve gut discomfort.
Common purging behaviors include forced vomiting, fasting, laxatives, diuretics, enemas, and excessive exercise.
Symptoms may appear very similar to those of the binge eating or purging subtypes of anorexia nervosa. However, individuals with bulimia usually maintain a relatively typical weight rather than losing a large amount of weight.
Common symptoms of bulimia nervosa include (1):
- recurrent episodes of binge eating with a feeling of lack of control
- recurrent episodes of inappropriate purging behaviors to prevent weight gain
- self-esteem overly influenced by body shape and weight
- a fear of gaining weight, despite having a typical weight
Side effects of bulimia may include an inflamed and sore throat, swollen salivary glands, worn tooth enamel, tooth decay, acid reflux, irritation of the gut, severe dehydration, and hormonal disturbances (11).
In severe cases, bulimia can also create an imbalance in levels of electrolytes, such as sodium, potassium, and calcium. This can cause a stroke or heart attack.
Binge eating disorder is the most prevalent form of eating disorder and one of the most common chronic illnesses among adolescents (12).
It typically begins during adolescence and early adulthood, although it can develop later on.
Individuals with this disorder have symptoms similar to those of bulimia or the binge eating subtype of anorexia.
For instance, they typically eat unusually large amounts of food in relatively short periods of time and feel a lack of control during binges.
People with binge eating disorder do not restrict calories or use purging behaviors, such as vomiting or excessive exercise, to compensate for their binges (12).
Common symptoms of binge eating disorder include (11):
- eating large amounts of food rapidly, in secret, and until uncomfortably full, despite not feeling hungry
- feeling a lack of control during episodes of binge eating
- feelings of distress, such as shame, disgust, or guilt, when thinking about the binge eating behavior
- no use of purging behaviors, such as calorie restriction, vomiting, excessive exercise, or laxative or diuretic use, to compensate for the binge eating
People with binge eating disorder often consume an excessive amount of food and may not make nutritious food choices. This may increase their risk of medical complications such as heart disease, stroke, and type 2 diabetes (13).
This may increase their risk of medical complications such as heart disease, stroke, and type 2 diabetes (13).
Pica is an eating disorder that involves eating things that are not considered food and that do not provide nutritional value (14).
Individuals with pica crave non-food substances such as ice, dirt, soil, chalk, soap, paper, hair, cloth, wool, pebbles, laundry detergent, or cornstarch (11).
Pica can occur in adults, children, and adolescents.
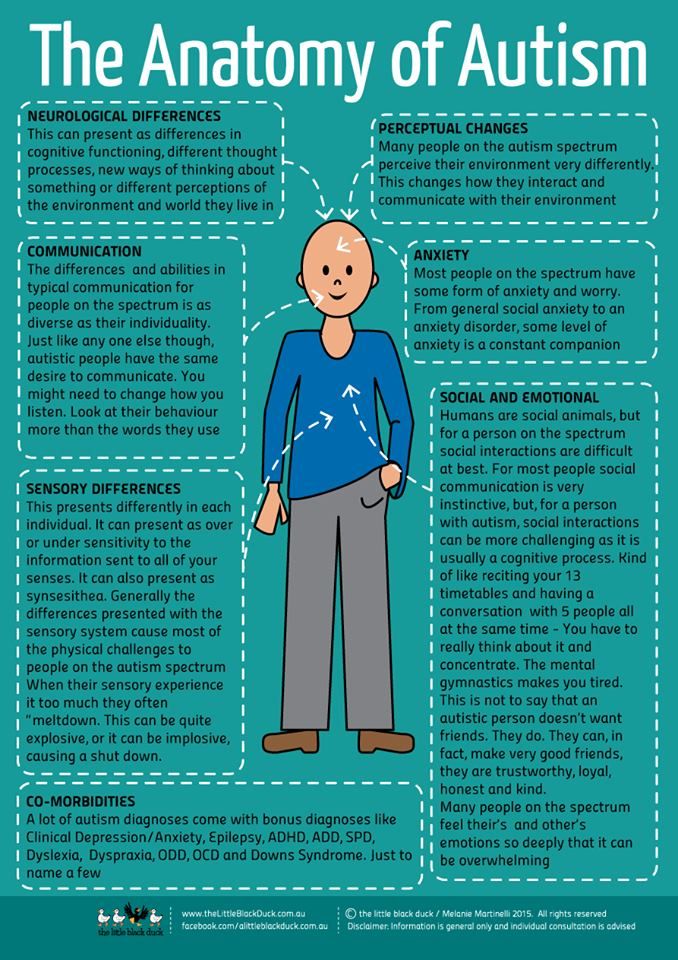
It is most frequently seen in individuals with conditions that affect daily functioning, including intellectual disabilities, developmental conditions such as autism spectrum disorder, and mental health conditions such as schizophrenia (14).
Individuals with pica may be at an increased risk of poisoning, infections, gut injuries, and nutritional deficiencies. Depending on the substances ingested, pica may be fatal.
However, for the condition to be considered pica, the eating of non-food substances must not be a typical part of someone’s culture or religion. In addition, it must not be considered a socially acceptable practice by a person’s peers.
In addition, it must not be considered a socially acceptable practice by a person’s peers.
Rumination disorder is another newly recognized eating disorder.
It describes a condition in which a person regurgitates food they have previously chewed and swallowed, re-chews it, and then either re-swallows it or spits it out (15).
This rumination typically occurs within the first 30 minutes after a meal (16).
This disorder can develop during infancy, childhood, or adulthood. In infants, it tends to develop between 3 and 12 months of age and often disappears on its own. Children and adults with the condition usually require therapy to resolve it.
If not resolved in infants, rumination disorder can result in weight loss and severe malnutrition that can be fatal.
Adults with this disorder may restrict the amount of food they eat, especially in public. This may lead them to lose weight and become underweight (16).
Avoidant/restrictive food intake disorder (ARFID) is a new name for an old disorder.
The term has replaced the term “feeding disorder of infancy and early childhood,” a diagnosis previously reserved for children under age 7 (17).
Individuals with this disorder experience disturbed eating due to either a lack of interest in eating or a distaste for certain smells, tastes, colors, textures, or temperatures.
Common symptoms of ARFID include (11):
- avoidance or restriction of food intake that prevents the person from eating enough calories or nutrients
- eating habits that interfere with typical social functions, such as eating with others
- weight loss or poor development for age and height
- nutrient deficiencies or dependence on supplements or tube feeding
It’s important to note that ARFID goes beyond common behaviors such as picky eating in toddlers or lower food intake in older adults.
Moreover, it does not include the avoidance or restriction of foods due to lack of availability or religious or cultural practices.:max_bytes(150000):strip_icc()/what-can-i-eat-if-i-have-a-peptic-ulcer-1742154-01-ec37a34d14c44195999f8d44372f820b.png?resize=1060%2C707&ssl=1)
In addition to the six eating disorders above, other less known or less common eating disorders also exist.
These include (18):
- Purging disorder. Individuals with purging disorder often use purging behaviors, such as vomiting, laxatives, diuretics, or excessive exercising, to control their weight or shape. However, they do not binge.
- Night eating syndrome. Individuals with this syndrome frequently eat excessively at night, often after awakening from sleep.
- Other specified feeding or eating disorder (OSFED). While it is not found in the DSM-5, this category includes any other conditions that have symptoms similar to those of an eating disorder but don’t fit any of the disorders above.
One disorder that may currently fall under OSFED is orthorexia. Although orthorexia is increasingly mentioned in the media and in scientific studies, the DSM does not yet recognize it as a separate eating disorder (19).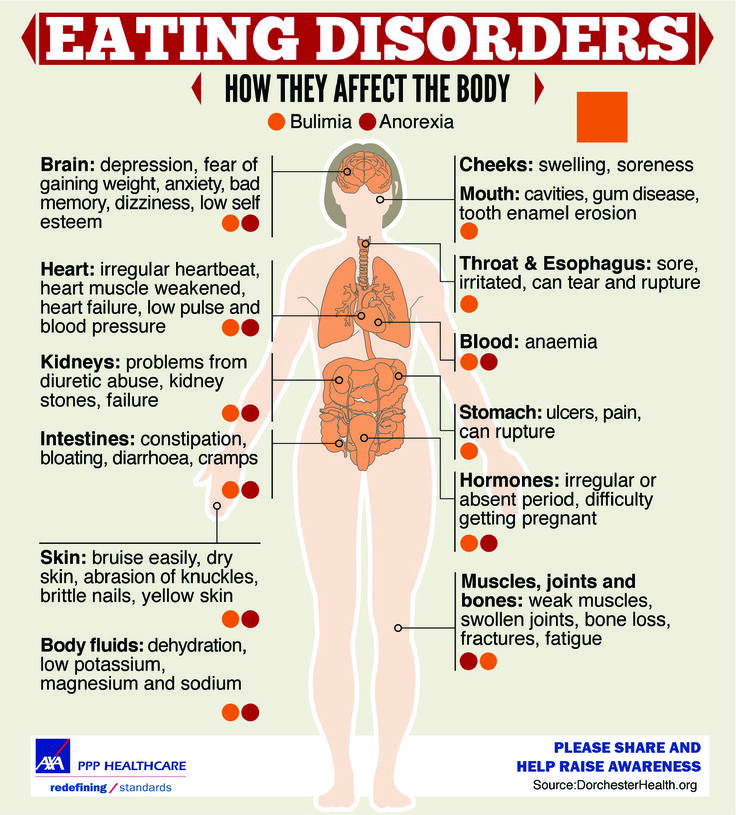
Individuals with orthorexia tend to have an obsessive focus on healthy eating to an extent that disrupts their daily lives. They may compulsively check ingredient lists and nutritional labels and obsessively follow “healthy lifestyle” accounts on social media.
Someone with this condition may eliminate entire food groups, fearing that they’re unhealthy. This can lead to malnutrition, severe weight loss, difficulty eating outside the home, and emotional distress.
Individuals with orthorexia are rarely focused on losing weight. Instead, their self-worth, identity, or satisfaction is dependent on how well they comply with their self-imposed diet rules (19).
If you have an eating disorder, identifying the condition and seeking treatment sooner will improve your chances of recovering. Being aware of the warning signs and symptoms can help you decide whether you need to seek help.
Not everyone will have every sign or symptom at once, but certain behaviors may signal a problem, such as (20):
- behaviors and attitudes that indicate that weight loss, dieting, and control over food are becoming primary concerns
- preoccupation with weight, food, calories, fats, grams, and dieting
- refusal to eat certain foods
- discomfort with eating around others
- food rituals (not allowing foods to touch, eating only particular food groups)
- skipping meals or eating only small portions
- frequent dieting or fad diets
- extreme concern with body size, shape, and appearance
- frequently checking in the mirror for perceived flaws in appearance
- extreme mood swings
If these symptoms resonate with you and you think you may have an eating disorder, it’s important to reach out to a medical professional for help.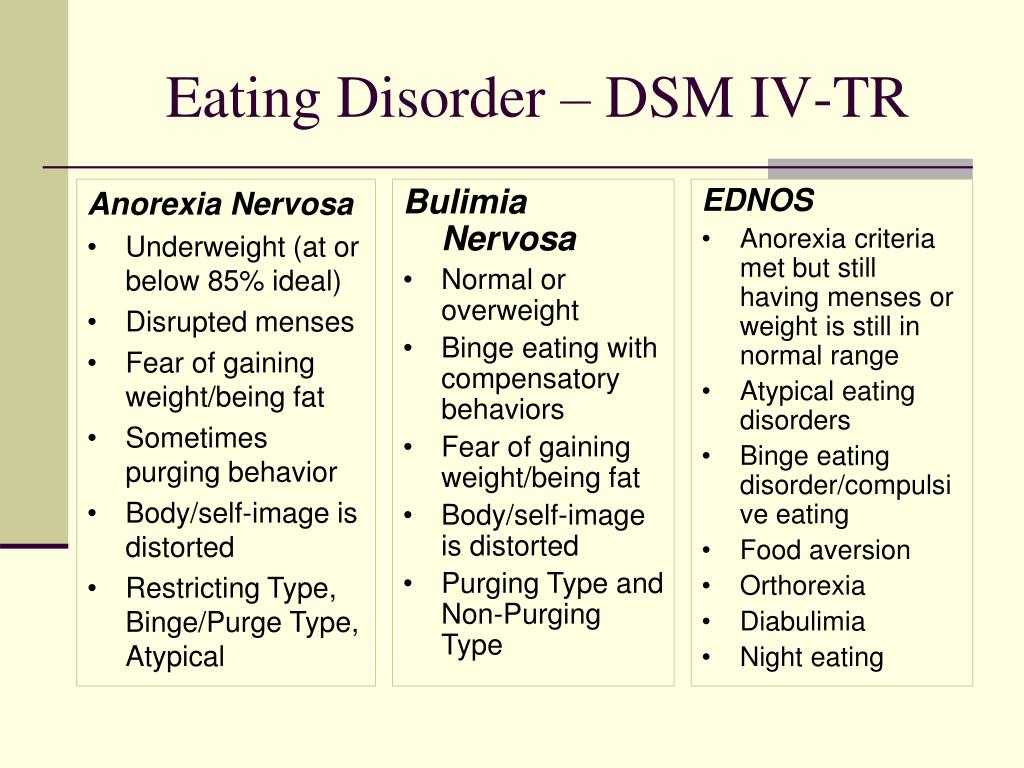
Making the decision to start eating disorder recovery might feel scary or overwhelming, but seeking help from medical professionals, eating disorder recovery support groups, and your community can make recovery easier.
If you’re not sure where to start, you can contact the National Eating Disorders Association helpline for support, resources, and treatment options for yourself or someone you know.
To contact, call: (800) 931-2237
Monday–Thursday 11 a.m.–9 p.m. ET
Friday 11 a.m.–5 p.m. ET
Text: (800) 931-2237
Monday–Thursday 3 p.m.–6 p.m. ET
Friday 1 p.m.–5 p.m. ET
Eating disorder treatment plans are specifically tailored to each person and may include a combination of multiple therapies.
Treatment will usually involve talk therapy, as well as regular health checks with a physician (21).
It’s important to seek treatment early for eating disorders, as the risk of medical complications and suicide is high (11).
Treatment options include:
- Individual, group, or family psychotherapy. A type of psychotherapy called cognitive behavioral therapy (CBT) may be recommended to help reduce or eliminate disordered behavior such as binge eating, purging, and restricting. CBT involves learning how to recognize and change distorted or unhelpful thought patterns (11).
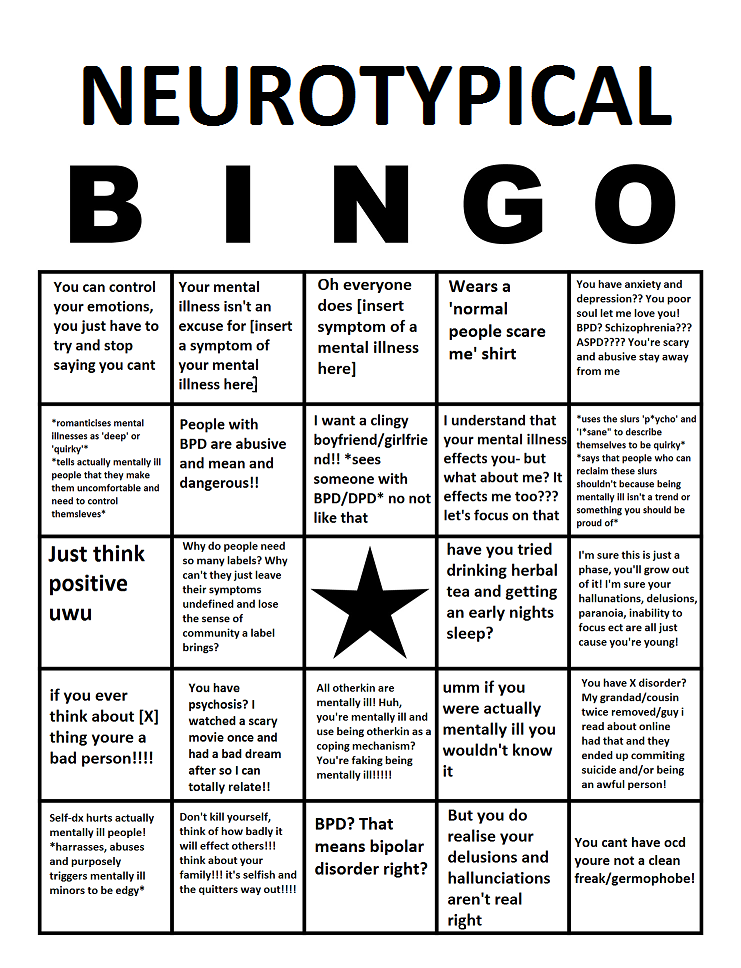
- Medications. A doctor may recommend treatment with medications such as antidepressants, antipsychotics, or mood stabilizers to help treat an eating disorder or other conditions that may occur at the same time, such as depression or anxiety (11).
- Nutritional counseling. This involves working with a dietitian to learn proper nutrition and eating habits and may also involve restoring or managing a person’s weight if they have experienced significant weight changes. Studies suggest that combining nutritional therapy with cognitive therapy may significantly improve treatment outcomes (22).
If you think someone in your life has an eating disorder, your best bet is to support and encourage them to seek help from a healthcare professional.
This can be extremely difficult for someone living with an eating disorder, but supporting them in other ways will help them feel cared for and encouraged in their recovery.
Recovering from an eating disorder can take a long time, and this person may have periods of relapsing into old behaviors, especially during times of stress. If you’re close to this person, it’s important to be there for them, and be patient, throughout their recovery (21).
Ways to support someone with an eating disorder include (21):
- Listening to them. Taking time to listen to their thoughts can help them feel heard, respected, and supported. Even if you don’t agree with what they say, it’s important that they know you’re there for them and that they have someone to confide in.
- Including them in activities.
 You can reach out and invite them to activities and social events or ask if they want to hang out one-on-one. Even if they do not want to be social, it’s important to check in and invite them to help them feel valued and less alone.
You can reach out and invite them to activities and social events or ask if they want to hang out one-on-one. Even if they do not want to be social, it’s important to check in and invite them to help them feel valued and less alone. - Trying to build their self-esteem. Make sure they know that they are valued and appreciated, especially for nonphysical reasons. Remind them why you are their friend and why they are valued.
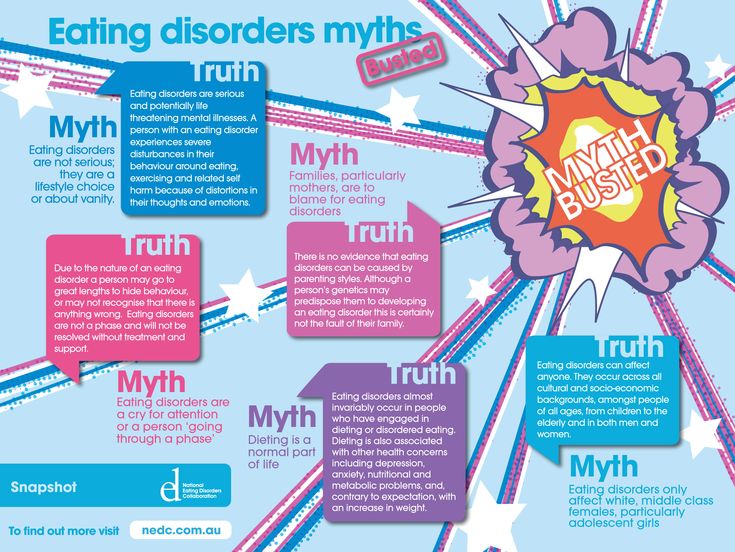
The categories above are meant to provide a better understanding of the most common eating disorders and dispel myths about them.
Eating disorders are mental health conditions that usually require treatment. They can also be damaging to the body if left untreated.
If you have an eating disorder or know someone who might have one, you can seek help from a healthcare professional who specializes in eating disorders.
You can book an appointment with an eating disorder specialist in your area using our Healthline FindCare tool.
Read this article in Spanish.
12 Types of Eating Disorders [Updated List]
Eating is a complicated part of life. It’s affected by all sorts of things like our genes, the way we were raised, our mental health, imagery in the media, biological changes, and injuries even. This is why we see so many different types of eating disorders!
There are 5 types of eating disorders recognized as medical diagnoses in the ICD and DSM (these are two manuals medical doctors and psychologists use to officially keep track of valid diagnoses). We’ve also included an additional 8 types of eating disorders that mental health scientists recognize.
Eating Disorders: An Overview
The term eating disorder covers a range of unique mental illnesses. Their main characteristic as a group is that they cause some type of harmful food centered behavior. Behaviors vary but most often include food-restriction or excessive eating. Eating disorders can lead to harmful physical effects and even death.
The 12 Types of Eating Disorders
Those included in the ICD and DSM:
1. Anorexia Nervosa
Experts consider anorexia nervosa to be the most deadly of all mental illnesses because it has the highest mortality rate. For this reason, we can consider it to be the most severe of the 12 types of eating disorders. This condition involves severe food-restriction and sometimes extreme exercising and other purging behaviors. The individual will typically show these signs and symptoms:
- Intense fear of gaining weight, even small amounts are intolerable.
- Losing weight rapidly and consistently staying underweight. Their skinny appearance can be alarming for friends and family.
- Refusal to acknowledge that such a low body weight can have harmful health consequences.

- Amenorrhea: this is a term for when women stop menstruating due to low-fat content.
- Heart damage: anorexia stresses the cardiovascular system and can lead to a variety of life-threatening heart conditions.
2. Bulimia Nervosa
This condition, bulimia nervosa, occurs when someone is repeatedly binging on large amounts of food and then purging it. Purging behaviors include forcing oneself to throw up, over-exercising, and using diet pills and laxatives. Both binging and purging behaviors are dangerous, and together they can quickly lead to dangerous physical symptoms.
3. Muscle Dysmorphia
Unlike most types of eating disorders, muscle dysmorphia tends to affect more men than women. The disorder is characterized by a disruptive obsession with musculature and physique. The individual will fixate on obtaining the ‘perfect’ form of musculature.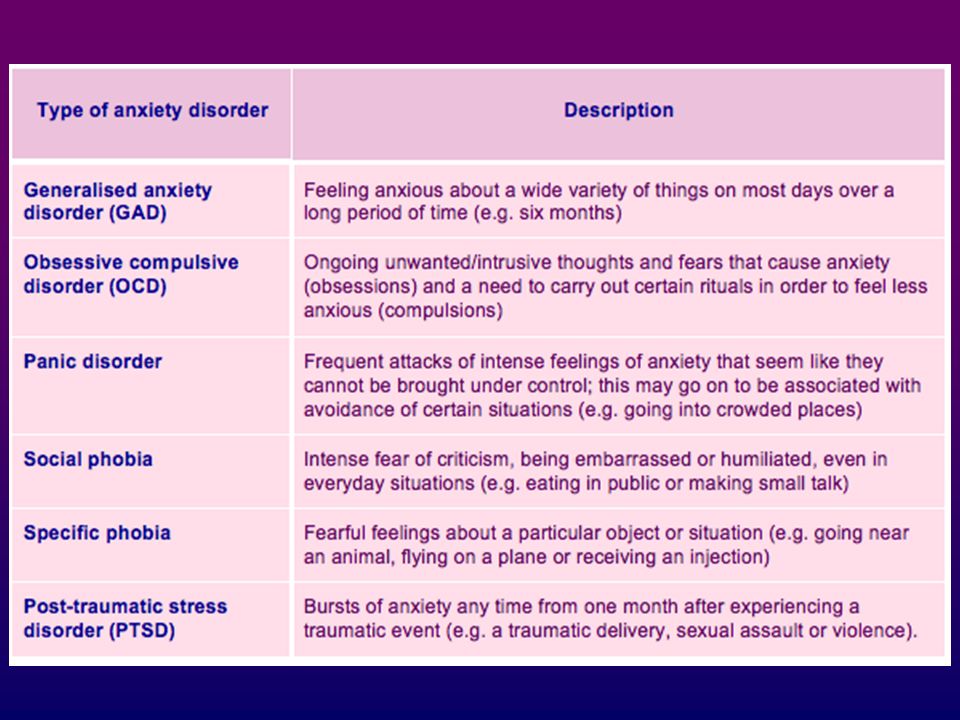
4. Binge Eating Disorder (BED)
BED is characterized by episodes of binging on large amounts of food. A binge describes when someone consumes an excessive amount of food within a period of two hours. Binges are accompanied by a trance-like state, feeling guilty and ashamed afterward, and weight gain. Unlike bulimia, BED does not usually include any purging behaviors. Typically, those affected by BED are overweight or obese because of the binging.
If you believe that you or someone you love is suffering from an eating disorder, do not hesitate to ask for help. Our experienced staff is here to help you find the appropriate treatment.
Click below to call us now and get the help you need. We are here 24/7.
(800) 929-5904
5. Other Specified Feeding or Eating Disorder (OSFED)
OSFED is a “catch-all” for types of eating disorders that don’t fit into the above categories. Doctors and psychologists will often diagnose those with atypical anorexia or bulimia, as well as the following 7 unofficial diagnoses, with OSFED.
“Unofficial” Eating Disorder Diagnoses
These disorders are not included in any diagnostic manual, but doctors and psychologists still use these terms. Practitioners often group people with these conditions into OSFED, other specified feeding or eating disorder, as the official diagnosis. However, these terms are more specific and can help us communicate more clearly.
6. Compulsive Over Eating (COE)
This disorder is similar to binge eating disorder. What makes COE unique is that the individual doesn’t binge in spurts, but rather eats large amounts of food all day long.
7. Prader Willi Syndrome
This syndrome, which leads to compulsive eating and obesity, is caused by an inherited genetic disease. It begins with weak muscles, poor feeding, and slow development in babies. Then, in childhood, the disease causes insatiable hunger. Children with Prader Willi Syndrome often develop diabetes and struggle to adapt to a normal lifestyle.
8. Diabulimia
This occurs when someone who is diabetic uses their prescription insulin to try to induce weight loss.
9. Orthorexia Nervosa (a term coined by the writer and medical doctor, Steven Bratman)
We are all under pressure to eat healthier for various reasons. In the case of orthorexia nervosa, someone becomes so obsessed with planning a perfect diet that it disrupts their life.
10. Selective Eating Disorder
This eating disorder is a bit like picky eating, but at an extreme, debilitating level. An individual is so selective about their food, usually sticking to a one or two meals, that they become sick.
11. Drunkorexia
With a slightly crass sounding name, this term describes an eating disorder that is accompanied by alcoholism as well. The drunkorexic individual restricts food and purges in order to “save calories” for drinking alcohol. Severe malnutrition can develop when drunkorexia goes untreated.
12. Pregorexia
Since it is fairly common knowledge that pregnancy leads to weight gain and other bodily changes, so most women go into pregnancy with a weight loss plan.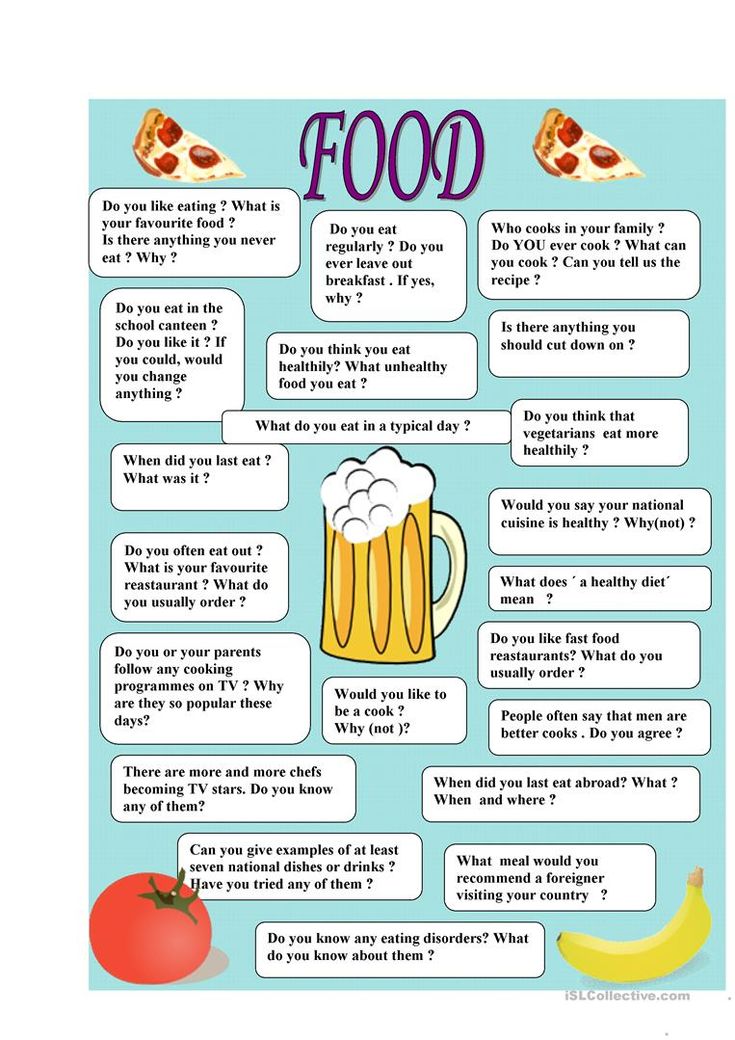 Sometimes, the weight loss plan can be too extreme and can endanger both mom and baby. Pregorexia can lead to low birth weight, coronary heart disease, type 2 diabetes, stroke, hypertension, cardiovascular disease risk, and depression.
Sometimes, the weight loss plan can be too extreme and can endanger both mom and baby. Pregorexia can lead to low birth weight, coronary heart disease, type 2 diabetes, stroke, hypertension, cardiovascular disease risk, and depression.
Types of Treatment for Eating Disorders:
"I wake up. I feel my thighs and my pelvic bones to see if they rise above my stomach slightly, but they don’t - not enough. I’m already disappointed in myself. Getting on the scale this morning will set my mood for the day. The number on the scale is a direct reflection of my happiness. It will determine everything that follows in my relationship with food and how I feel about myself."
It can be difficult to find the right type of treatment for eating disorders. It is important that the eating disorder treatment program has a full staff dedicated to eating disorder treatment that would include a medical doctor, eating disorder therapists, eating disorder registered dietitians, and support staff that understand and support the eating disorder program and most importantly the client.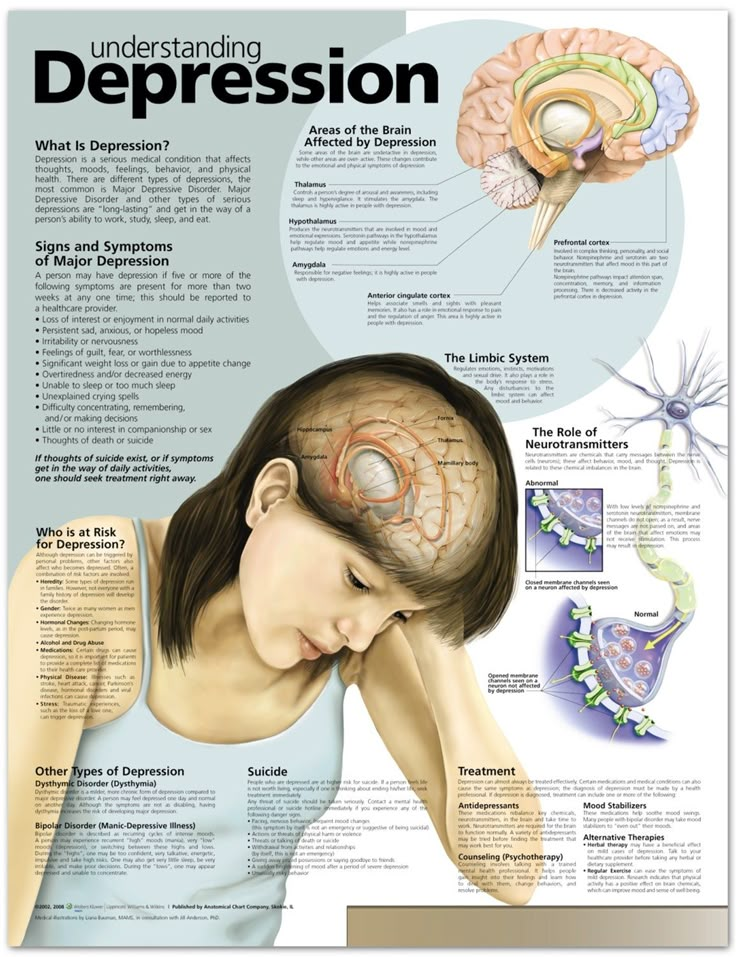
Each type of treatment for eating disorders requires the program to consider what the client is struggling with in their relationship with food, weight and body image, in addition to the potential medical consequences that can accompany the specific type of eating disorder. This way the entire team can support each client’s individual recovery with optimum care.
Breathe Life Healing Centers addresses the types of treatment for eating disorders from this perspective. No one person is the same. Our treatment for eating disorders focuses on supporting and understand each person’s clinical, emotional, and medical needs. Our Medical Director is a regarded expert in treating eating disorders, as well as our eating disorder dietitians, eating disorder therapists and staff.
Call now (800) 929-5904 for an assessment with our admissions department to see what type of eating disorder treatment can support your recovery. You can be free!
Get Help at Breathe’s Eating Disorder Treatment Center
If you or someone you love seems to be struggling with one of these eating disorders, reach out for help. Here at Breathe Life Healing Centers, we have a world-renowned eating disorder treatment program to help you heal your mind, body, and soul.
Here at Breathe Life Healing Centers, we have a world-renowned eating disorder treatment program to help you heal your mind, body, and soul.
(800) 929-5904
Eating disorders | Tervisliku toitumise informatsioon
Eating disorders are psychiatric illnesses that damage a person's physical and mental health and impair their overall quality of life - relationships, work and personal development suffer.
Eating disorders disrupt the connection with one's own body, resulting in highly problematic eating behavior. Weight and body shape are overemphasized, underweight is idealized, and various methods are used to lose weight or prevent weight gain.
Approximately 8% of women and 2% of men will develop an eating disorder during their lifetime. Eating disorders occur in any population, regardless of gender, age, ethnicity, or socioeconomic status. However, they are most common in girls and young women.
Eating disorders are a group of diseases that are distributed differently in different classifications. The most common eating disorders are anorexia ( anorexia nervosa ), bulimia ( bulimia nervosa ) and compulsive overeating ( binge-eating disorder ).
The term "eating disorder" is often erroneously used as a synonym for selective eating disorder, as both are associated with eating disorders. However, the reasons for them are different: an eating disorder is caused by a desire to control weight, while in a selective eating disorder, eating certain foods causes anxiety or fear.
Other eating disorders
Anorexia, bulimia and binge eating disorders are the three most common and well-known eating disorders. However, often not all of the symptoms of a person with an eating disorder correspond to one specific disorder. In such cases, these disorders are referred to as "atypical" or "other eating disorders".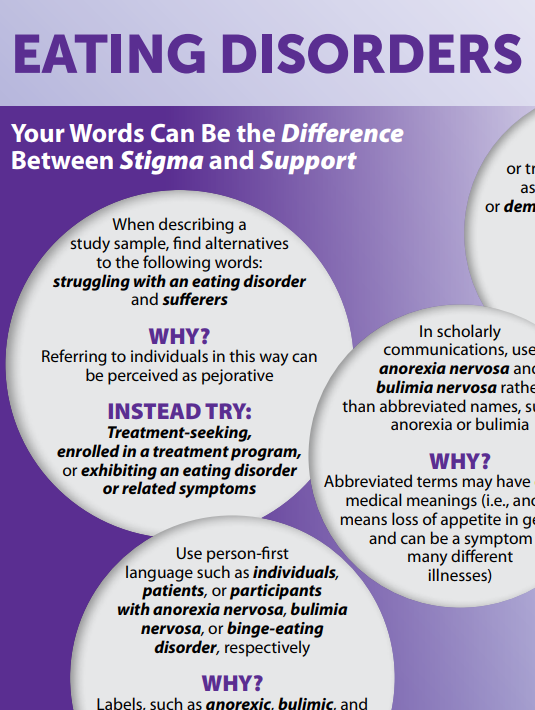 A common myth is that in such cases the course of the disease is milder and treatment is treated more lightly. However, this is erroneous, since the name of the disease indicates only its diagnostic criteria, and not the severity or course.
A common myth is that in such cases the course of the disease is milder and treatment is treated more lightly. However, this is erroneous, since the name of the disease indicates only its diagnostic criteria, and not the severity or course.
All eating disorders, no matter how they are called or classified, are dangerous conditions that impair quality of life and require treatment.
Causes of Eating Disorders
There is never one single cause of an eating disorder. These are complex diseases, in the development of which a combination of many factors plays an important role. Genetic, biological and environmental factors always play a role. Modern social representations, including the culture of diets and the cult of slimness, contribute to the development of psychological vulnerability, which can become a fertile environment for the formation of eating disorders. Probably for the same reasons, a higher incidence of eating disorders is observed in sports in which weight is of great importance, and among representatives of professions focused on appearance. However, it should be emphasized that browsing social networks or playing a certain sport does not contribute to the development of the disease. There are many factors involved in the development of the disease that are usually beyond the control of the individual. However, it is often more practical and even more important to identify the factors that support the disease, since changing them is associated with better treatment outcomes.
However, it should be emphasized that browsing social networks or playing a certain sport does not contribute to the development of the disease. There are many factors involved in the development of the disease that are usually beyond the control of the individual. However, it is often more practical and even more important to identify the factors that support the disease, since changing them is associated with better treatment outcomes.
Treatment Options for Eating Disorders
Eating disorders can be life-threatening illnesses with a long and chronic course; they have one of the highest mortality rates of any psychiatric illness. Treating eating disorders is often a lengthy and complex process. However, early intervention is paramount to achieve a good treatment outcome.
Diagnosis and treatment of an eating disorder usually begins with the family physician. Family sisters can provide advice on healthy eating. Psychiatrists are specialists in the diagnosis and treatment of eating disorders as a psychiatric illness. The participation of a clinical psychologist or psychotherapist is also important.
The participation of a clinical psychologist or psychotherapist is also important.
There are two centers in Estonia that specialize in the treatment of eating disorders: the Department of Eating Disorders of the Mental Health Center of the Tallinn Children's Hospital treats children and adolescents, and the Department of Eating Disorders of the Psychiatric Clinic of the Tartu University Hospital treats adolescents and adults.
For more information about eating disorders and advice on what to do if you suspect a loved one has an eating disorder, visit peaasi.ee.
6 main types of eating disorders, symptoms and causes
Everyone has heard about the most serious eating disorders - anorexia and bulimia. But there are other disorders that are often considered cute quirks, but they have the strongest impact on health. You cannot leave them unattended.
Mikhail Gavrilov
Source: Unsplash
A person may not have problems with excess weight, but this does not mean that his eating habits can be called healthy.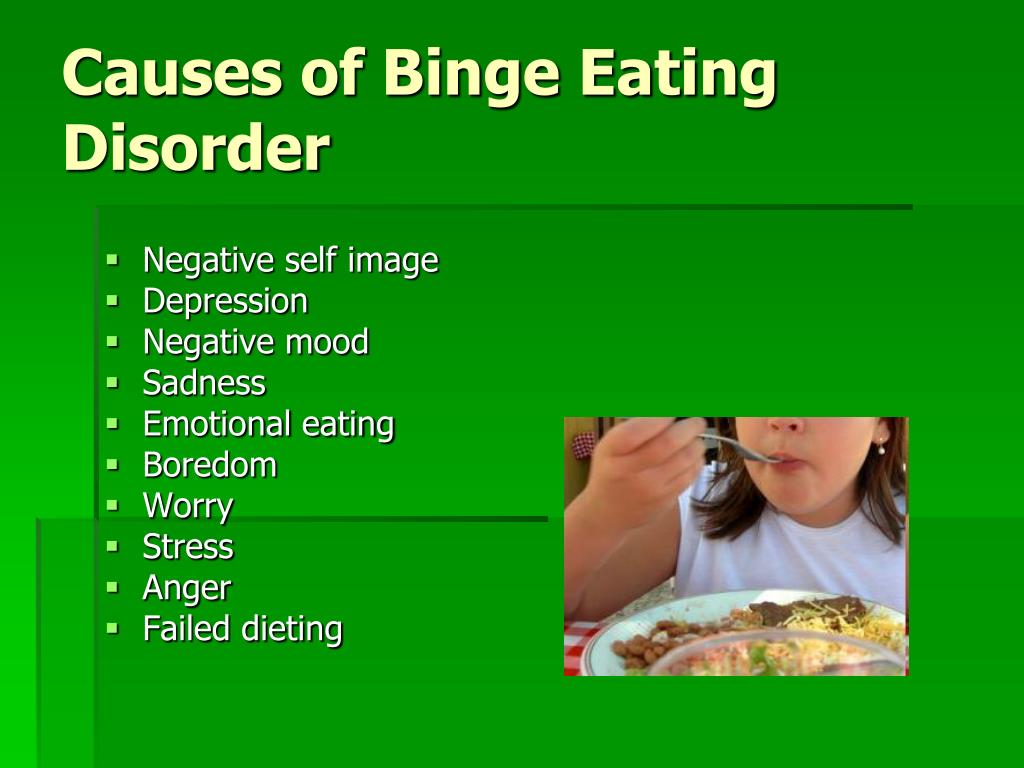 Some eating habits can result in quite serious disorders in the future.
Some eating habits can result in quite serious disorders in the future.
Contents of the article
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
What body signals and eating habits should alert you?
The concept of eating behavior includes everything that is directly related to the choice and preparation of food, eating rituals and emotions that food causes. And all of the above is very closely tied to psychology. It is no coincidence that, if we talk about serious eating disorders, it is usually based on hypochondria, depression, neurosis and other psychotherapeutic disorders.
Do not think that the so-called eating habits are just a cute fad that you can laugh at. For the time being, perhaps it is. But, if this feature enters the system and gradually begins to have a significant impact on mental and physical health, things are bad. This can result in eating disorders such as anorexia, bulimia, orthorexia, and compulsive overeating.
This can result in eating disorders such as anorexia, bulimia, orthorexia, and compulsive overeating.
All of these fairly serious disorders can begin with very minor habits, such as manic calorie counting, fear of eating in public, inability to stop eating even when you are already full, etc.
Of course, each of us has certain peculiarities of eating behavior. But not all of them are disorders. At the same time, some signs of an unhealthy attitude to food are perceived as the norm. These include, for example, malfunctions in your body, lifestyle features, unusual emotional reactions. We will talk about some of the less obvious eating disorders today. Don't leave them unattended!
Gastrointestinal disorders
Various dietary experiences are the real test for your stomach and intestines. At first, you feel pretty good, any restrictive diets, detoxes, cleansing manipulations pass with a bang. But after some time, you increasingly begin to encounter stool disorders, heaviness in the stomach, increased gas formation, and heartburn.
But after some time, you increasingly begin to encounter stool disorders, heaviness in the stomach, increased gas formation, and heartburn.
There are many reasons that may lead to such disorders. These include radical dietary restrictions and an unbalanced diet. All of the above disrupts the production of digestive enzymes, the gastrointestinal mucosa and its functions in general. The speed of digestion processes is significantly reduced, and the body gives you a bunch of unpleasant symptoms.
Puffiness
Another physiological marker of an eating disorder. Excessive fluid retention occurs in response to any imbalance in the body. It can be provoked by severe stress, systemic inflammation, hormonal failure. All of the above quite often becomes the result of long periods of food restrictions, a violation of the drinking regime, the abuse of junk food, and a small amount of protein in the diet. In healthy people, with normalization of nutrition, puffiness disappears.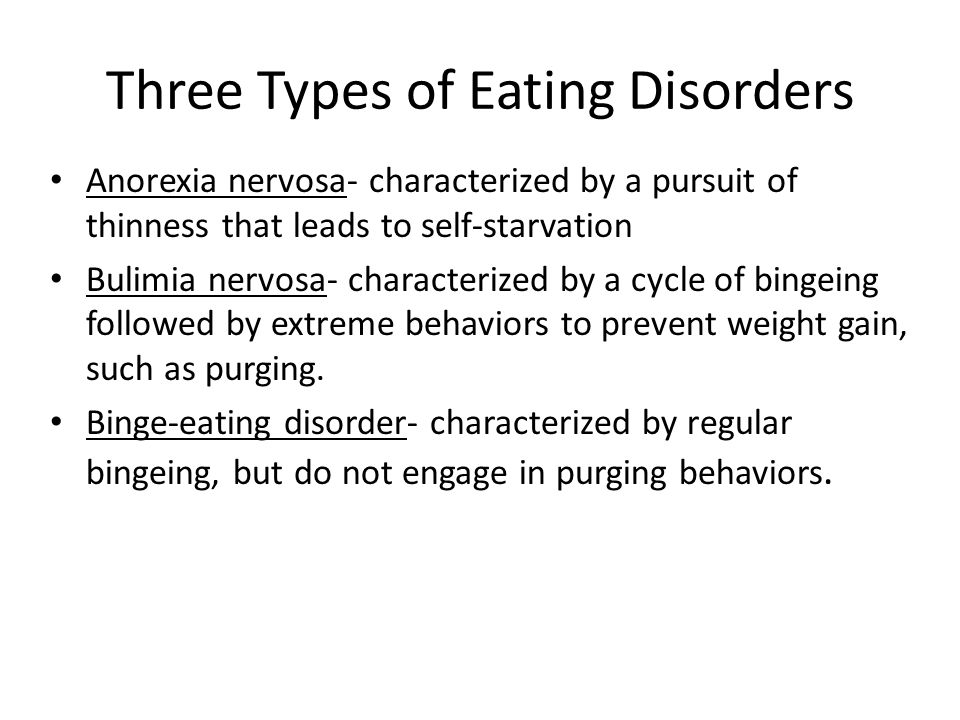 But, if your body is pretty battered due to eating disorders, it will not be easy to remove excess fluid.
But, if your body is pretty battered due to eating disorders, it will not be easy to remove excess fluid.
Feeling guilty after eating
In fact, this is nothing more than self-punishment for something done, in this case, food eaten, usually high in calories or “forbidden”. Any guilt is based on your own attitudes and beliefs about how you and people in general should be. And if for some reason you don’t act perfectly, go into the category of “losers”. Guilt after eating is associated with the perception of one's body. For example, you may consider yourself not slim enough and every extra bite you eat starts a series of thoughts that you are a person with a weak character.
Compensatory behavior
This point follows directly from the previous one. Compensatory behaviors are those actions with which you punish yourself for disrupting a balanced diet. Any action is in progress.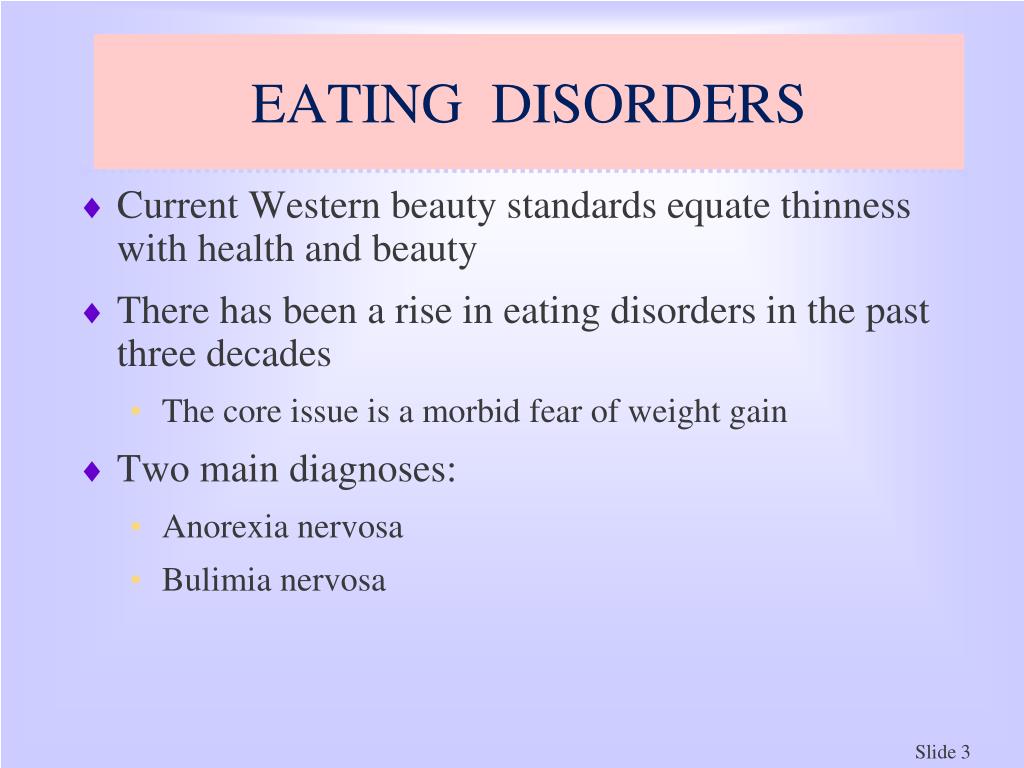 It all usually starts very innocently - a couple of extra workouts in the gym, a few fasting days, a trendy detox. In the future, the method of punishment may become tougher - taking a diuretic or laxative, cleansing enemas ... But all you could do was safely return to vegetable salads and lean meat.
It all usually starts very innocently - a couple of extra workouts in the gym, a few fasting days, a trendy detox. In the future, the method of punishment may become tougher - taking a diuretic or laxative, cleansing enemas ... But all you could do was safely return to vegetable salads and lean meat.
Fear of certain foods or ingredients
There is an incredible amount of information about proper nutrition, the characteristics of certain foods in open sources. Sometimes the danger of certain dishes is greatly exaggerated. People with a fine mental organization react to such information in an extremely straightforward manner, cultivating the rejection of any products. Panic is caused by the very possibility of eating something unhealthy. Such behavior may be typical for those who are overly concerned about a healthy lifestyle, but at the same time have an inadequate idea of what, in fact, is included in this concept.
Eating involves a lot of rituals
And many of them can be quite strange. .. For example, you always separate a set meal into ingredients before you eat it. Or eat only at a table served in a certain way. But if this is not possible, you prefer to stay hungry.... Such, almost manic behavior is often the result of your desire for superiority over others. The special organization of each meal requires remarkable endurance and self-discipline. The application of will causes a feeling of pride in oneself and a condescending attitude towards people who are not capable of such feats.
.. For example, you always separate a set meal into ingredients before you eat it. Or eat only at a table served in a certain way. But if this is not possible, you prefer to stay hungry.... Such, almost manic behavior is often the result of your desire for superiority over others. The special organization of each meal requires remarkable endurance and self-discipline. The application of will causes a feeling of pride in oneself and a condescending attitude towards people who are not capable of such feats.
Body acceptance exercise
An eating disorder often underlies body aversion. Can you love him for who he is? So, deal with nutritional errors. And the technique of working with a mirror will help you with this. It is based on a long study of his reflection in the nude. In the classic version, this needs to be done for a long time - about 2 hours. Too much...
You can practice for 10-15 minutes - until you feel warm feelings towards your reflection, without rejection and negativity.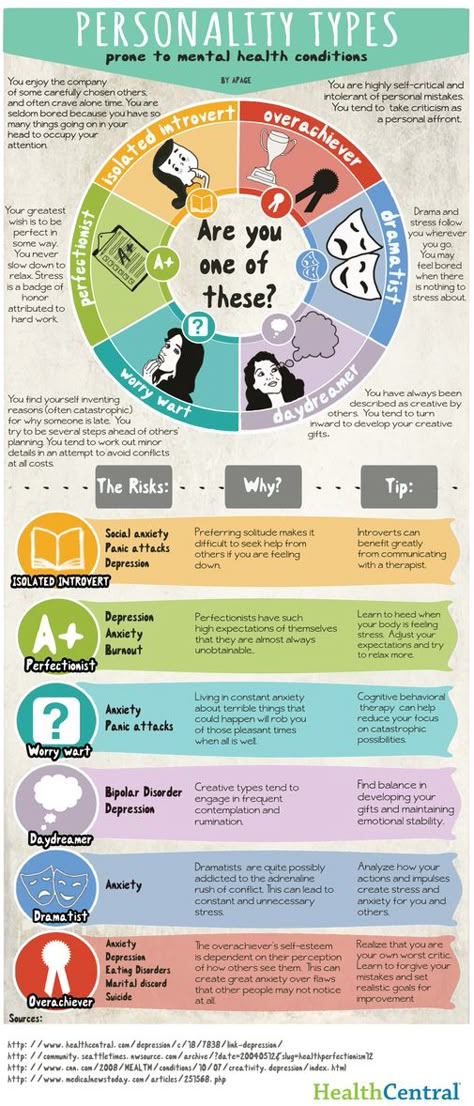 With the seeming simplicity of the exercise, from an emotional point of view, it is difficult to withstand it. Examining your imperfections, you can experience a whole kaleidoscope of unpleasant feelings - from disgust and shame to guilt and anger. But gradually you will get used to what you see. This is a feature of the human psyche.
With the seeming simplicity of the exercise, from an emotional point of view, it is difficult to withstand it. Examining your imperfections, you can experience a whole kaleidoscope of unpleasant feelings - from disgust and shame to guilt and anger. But gradually you will get used to what you see. This is a feature of the human psyche.
On the 2nd or 3rd day of practice, many will already be able to understand that yes, the body is not perfect, but not “horror-horror”. Yes, you have a tummy, deposits on your sides, but you do not feel negative towards them. They just are! It is important to understand that your task is not to learn to be proud of your imperfections (especially if you have the desire and opportunity to correct them), but to develop a neutral attitude towards the features of your body.
Eating disorders treated by a psychotherapist
Have you noticed some oddities in your eating behavior? Eliminate them at the root. Otherwise, they can develop into one of the four unpleasant psychophysiological disorders. And in their treatment, one cannot do without a psychotherapist.
Otherwise, they can develop into one of the four unpleasant psychophysiological disorders. And in their treatment, one cannot do without a psychotherapist.
Anorexia
Expressed in painful thinness. This condition is associated with impaired appetite. Anorexics adhere to a strict calorie restriction of their diet, believing that they are overweight, exhaust themselves with sports loads. The use of diuretics and laxatives. Often such people do not understand that they are sick. Sometimes they have to be treated forcibly in order to simply save their lives.
Bulimia
Characterized by sudden bouts of intense hunger, resulting in everything that is not nailed to the plate being swept away. Food is consumed in huge portions, up to unpleasant sensations in the stomach, physical pain and gag reflex. After that, under the influence of guilt, vomiting is induced, a laxative is taken.