Ptsd brain damage
How PTSD Affects The Brain
Share this page Facebook Twitter Email Print
If you’re experiencing post-traumatic stress disorder (PTSD), it’s important to understand how the different parts of your brain function. Post-traumatic stress is a normal response to traumatic events. However, PTSD is a more serious condition that impacts brain function, and it often results from traumas experienced during combat, disasters, or violence.
Your brain is equipped with an alarm system that normally helps ensure your survival. With PTSD, this system becomes overly sensitive and triggers easily. In turn, the parts of your brain responsible for thinking and memory stop functioning properly. When this occurs, it’s hard to separate safe events happening now from dangerous events that happened in the past.
Over the past 40 years, scientific methods of “neuroimaging” have enabled scientists to see that PTSD causes distinct biological changes in your brain. Not everybody with PTSD has exactly the same symptoms or the same brain changes, but there are observable patterns that can be understood and treated.
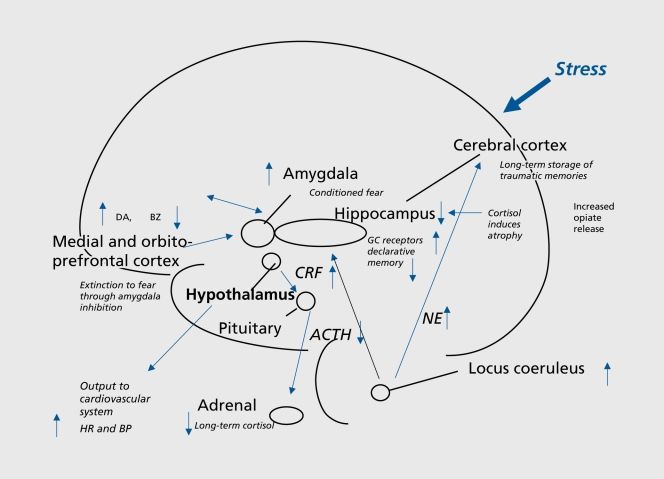
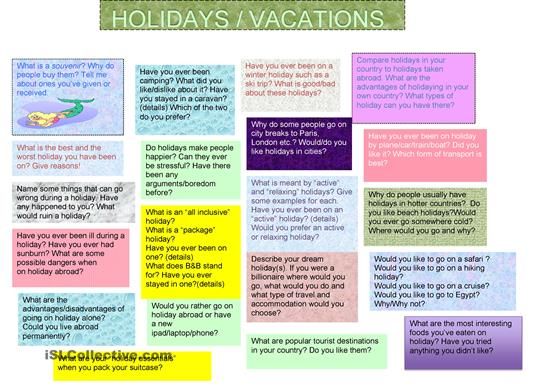
The diagram shows a cross-section of the brain parts discussed here.
Your alarm system
Your amygdala triggers your natural alarm system. When you experience a disturbing event, it sends a signal that causes a fear response. This makes sense when your alarm bells buzz at the right time and for the right reason: to keep you safe. Those with PTSD tend to have an overactive response, so something as harmless as a car backfiring could instantly trigger panic. Your amygdala is a primitive, animalistic part of your brain that’s wired to ensure survival. So when it’s overactive, it’s hard to think rationally.
Your brake system
Your prefrontal cortex (the front-most part of your neocortex) helps you think through decisions, observe how you’re thinking, and put on the “brakes” when you realize something you first feared isn’t actually a threat after all. Your prefrontal cortex helps regulate emotional responses triggered by the amygdala.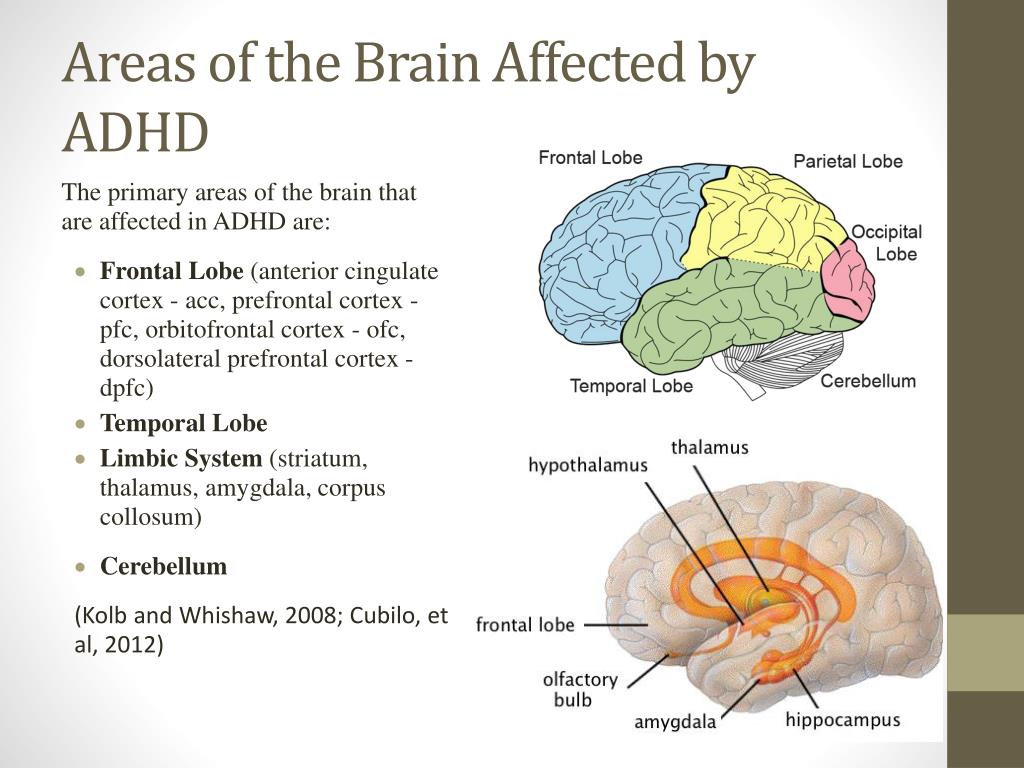 In service members with PTSD, the prefrontal cortex doesn’t always manage to do its job when needed.
In service members with PTSD, the prefrontal cortex doesn’t always manage to do its job when needed.
A bad combination
An overactive amygdala combined with an underactive prefrontal cortex creates a perfect storm. It’s like stomping on your car’s accelerator, even when you don’t need to, only to discover the brakes don’t work. This might help you understand why someone with PTSD might: (1) feel anxious around anything even slightly related to the original trauma that led to the PTSD; (2) have strong physical reactions to situations that shouldn’t provoke a fear reaction; and (3) avoid situations that might trigger those intense emotions and reactions.
System recall errors
Other common PTSD experiences—such as unwanted feelings that pop up out of nowhere or always being on the lookout for threats that could lead to more trauma—seem to be related to the hippocampus, or memory center of your brain. Your hippocampus is a lot like your computer’s memory that writes files to its hard drive.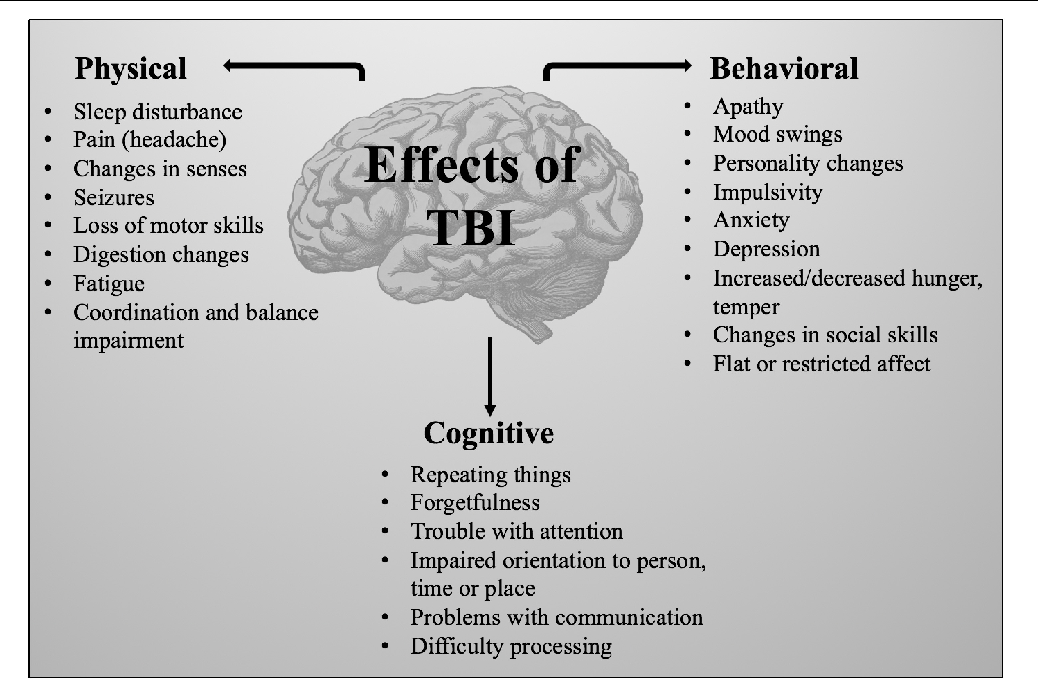 After a trauma, your hippocampus works to remember the event accurately and make sense of it. But because a trauma is typically overwhelming, all the information doesn't get coded correctly. This means that you might have trouble remembering important details of the event, or you might find yourself thinking a lot about what happened because your hippocampus is working so hard to try to make sense of things.
After a trauma, your hippocampus works to remember the event accurately and make sense of it. But because a trauma is typically overwhelming, all the information doesn't get coded correctly. This means that you might have trouble remembering important details of the event, or you might find yourself thinking a lot about what happened because your hippocampus is working so hard to try to make sense of things.
Debrief/Bottom line
Your amygdala, prefrontal cortex, and hippocampus all contribute to the feelings and actions associated with fear, clear thinking, decision-making, and memory. Understanding how they work also might explain why some therapies can help you work through PTSD. For a visual guide to these and other parts of your brain, and more information about them, explore the Center of Excellence for Medical Multimedia’s “Interactive Brain.
Posted on BrainLine May 6, 2019.
How PTSD affects brain “circuitry”. USU | CHAMP, Human Performance Resource Center, 30 May 2017.
Traumatic Brain Injury and PTSD
Available en Español
Traumatic brain injury (TBI) occurs from a sudden blow or jolt to the head. Brain injury often results from a trauma, like an accident, blast or fall. Learn about the overlap in PTSD and TBI symptoms and how to cope.
Reading time: minutes
TBI occurs from a sudden blow or jolt to the head. Brain injury often occurs during some type of trauma, such as an accident, blast, or a fall. Often when people refer to TBI, they are mistakenly talking about the symptoms that occur following a TBI. Actually, a TBI is the injury, not the symptoms.
How Serious Is My Injury?
A TBI is basically the same thing as a concussion. A TBI can be mild, moderate, or severe. These terms tell you the nature of the injury itself. They do not tell you what symptoms you may have or how severe the symptoms will be.
A TBI can occur even when there is no direct contact to the head. For example, when a person suffers whiplash, the brain may be shaken within the skull.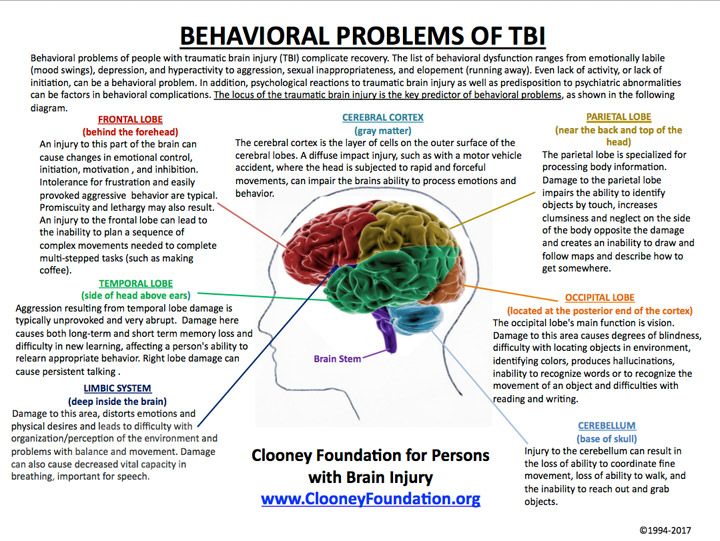 This damage can cause bleeding between the brain and skull. Bruises can form where the brain hits the skull. Like bruises on other parts of the body, for mild injuries these will heal with time.
This damage can cause bleeding between the brain and skull. Bruises can form where the brain hits the skull. Like bruises on other parts of the body, for mild injuries these will heal with time.
About 80% of all TBI's in civilians are mild (mTBI). Most people who have a mTBI will be back to normal by three months without any special treatment. Even patients with moderate or severe TBI can make remarkable recoveries.
The length of time that a person is unconscious (knocked out) is one way to measure how severe the injury was. If you weren't knocked out at all or if you were out for less than 30 minutes, your TBI was most likely minor or mild. If you were knocked out for more than 30 minutes but less than six hours, your TBI was most likely moderate.
What Are the Common Symptoms Following a TBI?
Symptoms that result from TBI are known as post-concussion syndrome (PCS). Few people will have all of the symptoms, but even one or two of the symptoms can be unpleasant. PCS makes it hard to work, get along at home, or relax. In the days, weeks, and months following a TBI the most common symptoms are:
PCS makes it hard to work, get along at home, or relax. In the days, weeks, and months following a TBI the most common symptoms are:
Physical
- Headache
- Feeling dizzy
- Being tired
- Trouble sleeping
- Vision problems
- Feeling bothered by noise and light
Cognitive (Mental)
- Memory problems
- Trouble staying focused
- Poor judgment and acting without thinking
- Being slowed down
- Trouble putting thoughts into words
Emotional (Feelings)
- Depression
- Anger outbursts and quick to anger
- Anxiety (fear, worry, or feeling nervous)
- Personality changes
These symptoms are part of the normal process of getting better. They are not signs of lasting brain damage. These symptoms are to be expected and are not a cause for concern or worry. More serious symptoms include severe forms of those listed above, decreased response to standard treatments, and seizures.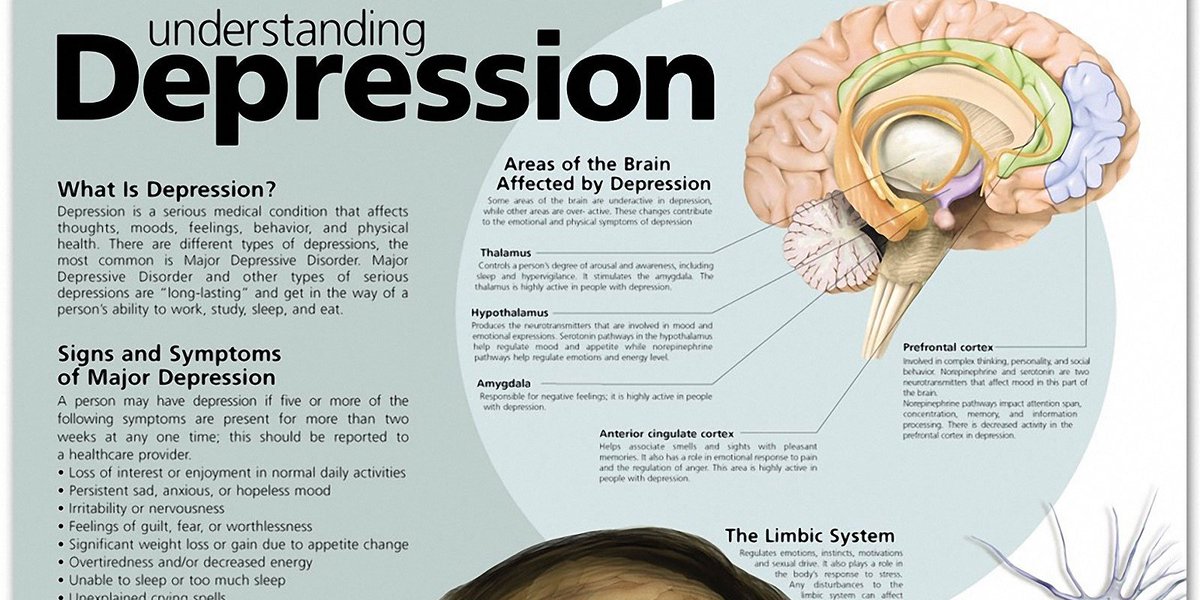
Do I Have the Symptoms that Follow a TBI or PTSD - or Both?
You may notice that many of the symptoms that follow a TBI overlap with the common reactions after trauma (en Español). Because TBI is caused by trauma and there is symptom overlap, it can be hard to tell what the underlying problem is. In addition, many people who get a TBI also develop PTSD.
It is important to be assessed because:
- People with TBI should not use some medications.
- No matter how mild or severe the injury itself was, the effects could be serious.
Although TBI screens are used, a screen is not used to diagnose TBI. Even if your TBI screen is positive, that does not mean that you have a TBI. It means that you should be assessed further.
Diagnosing a TBI is hard because there may not be any physical signs of injury. Details of the trauma may be hard to pin down. Sometimes right after the injury the effects are so brief that they are not noticed. You may go to the doctor some time later when details of the injury are not as clear.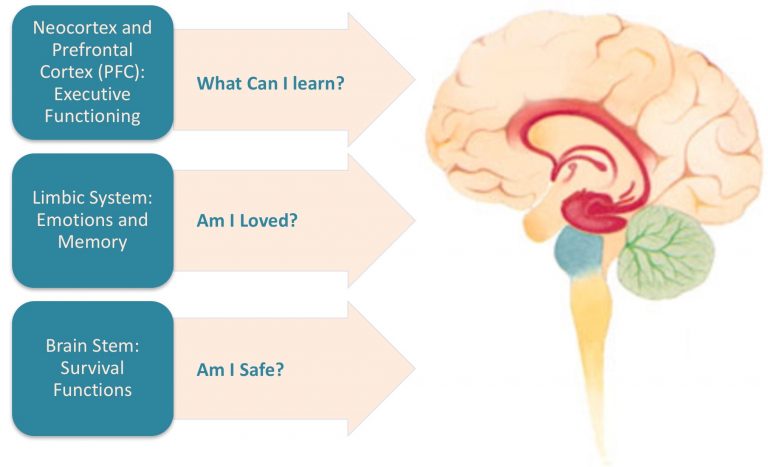 TBI can occur in confused times of crisis, such as combat. In the heat of events the injury may be ignored. Many of the symptoms that can result from a TBI are the same as the symptoms of PTSD. For these reasons, the best way to diagnose a TBI is an interview by a skilled clinician.
TBI can occur in confused times of crisis, such as combat. In the heat of events the injury may be ignored. Many of the symptoms that can result from a TBI are the same as the symptoms of PTSD. For these reasons, the best way to diagnose a TBI is an interview by a skilled clinician.
Are There Effective Treatments?
Many people recover from TBI without any formal treatment. Problems that linger may clear up in a few weeks. You may notice some problems more as you return to your normal routine. For example, you may not realize that you get tired more quickly until you return to your regular chores, work, or school. Even so, people usually get better after a head injury, not worse. Professional treatment for the symptoms that follow TBI usually involves rehabilitation to improve functioning.
The good news is that effective treatments for PTSD also work well for those who have suffered mTBI. This includes two forms of therapy: Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE).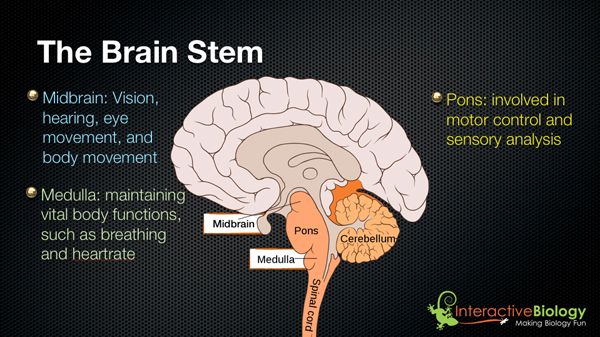 Learn more about Treatment Basics for PTSD.
Learn more about Treatment Basics for PTSD.
What Can I Do to Cope?
The best way to deal with symptoms following TBI is to go back slowly to your normal routine, a little at a time. How much time you spend at work, with family, with others, or exercising depends on what feels comfortable. Pace yourself, and be sure to get all the rest you need. Avoiding alcohol and not taking any unnecessary medications is a good idea, to help allow the brain to heal.
If your symptoms get worse, or if you notice new PCS symptoms, this is a sign that you are pushing yourself too hard. Ignoring your symptoms and trying to "tough it out" often make the symptoms worse. Symptoms are your body's way of giving you information. A broken bone or a torn muscle hurts so that you won't use it and it has time to heal. PCS symptoms are your brain's way of telling you that you need to rest it.
Research suggests that one week of relaxing at home and then a week of slowly doing more after leaving the hospital is best for most patients.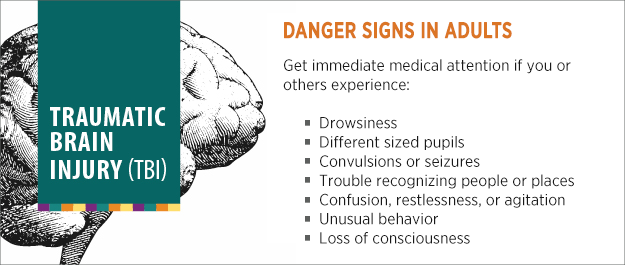 Most patients who took this advice were back to normal at work or school in 3 to 4 weeks. Most patients who weren't told what to do took 5 to 12 weeks to get back to their normal routine. They also had more PCS symptoms than patients who returned slowly to their routines.
Most patients who took this advice were back to normal at work or school in 3 to 4 weeks. Most patients who weren't told what to do took 5 to 12 weeks to get back to their normal routine. They also had more PCS symptoms than patients who returned slowly to their routines.
Accept and deal with the stress of the injury
Be aware that having a head injury adds more stress to your life, not just bumps and bruises to your head. The trauma itself, being in the hospital, and going back to work or school and normal routines are all things that add stress to most patients' lives. You may have some trouble with work or school at first, and even though it is normal, this may be stressful and frustrating.
Another main cause of stress after a TBI is worry about the symptoms you have. Thinking and worrying about your symptoms can make them seem worse. Doctors who treat TBI agree that the single most important factor in recovery is that you know what to expect and what to do about the symptoms. You should remember that the symptoms are a normal part of getting better. They will likely go away on their own.
You should remember that the symptoms are a normal part of getting better. They will likely go away on their own.
Involve Family
Any level of TBI can disrupt families. Roles and responsibilities change when a family member is hurt. From the start, families needs to be involved and informed about TBI. By supporting the family, patient outcomes can be improved and burnout prevented.
Return to school or work slowly
Returning to school or work is often the biggest challenge after TBI. This is because PCS symptoms can get in the way of meeting your work and school demands. For example, trouble focusing and memory problems may make it harder to learn new things in school. Or fatigue may limit your being able to handle work demands. Keep in mind when trying to return to work or school that the process will be slow. Don't expect yourself to perform right away as you did before your TBI. Instead, you should slowly resume responsibilities as you are able. Slowly increase your workload and hours.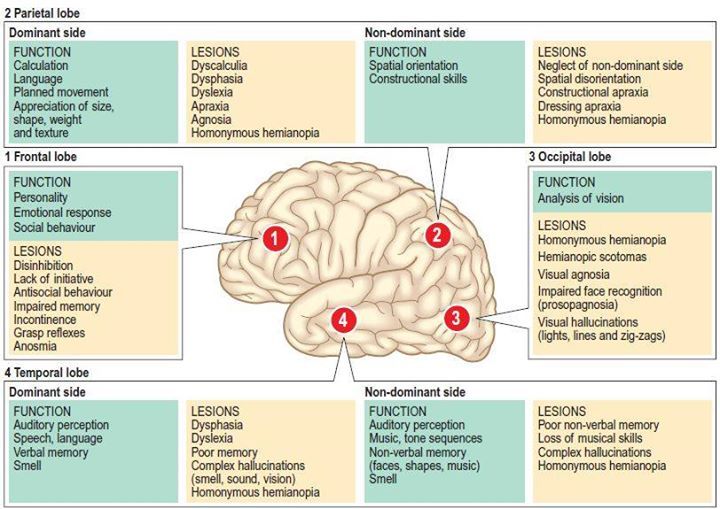 Only increase them when you feel fully ready.
Only increase them when you feel fully ready.
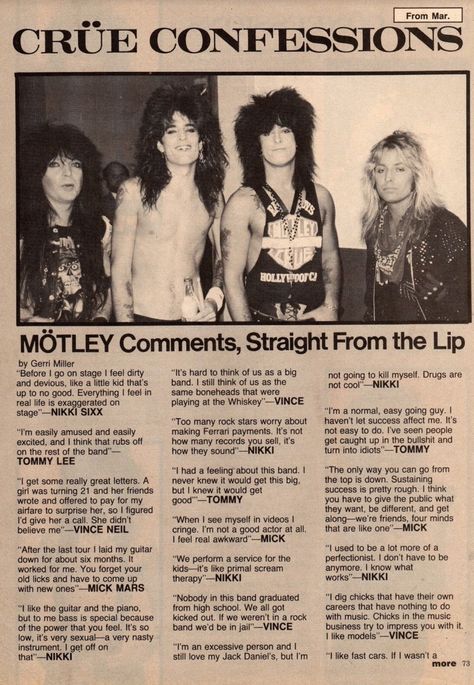
TBI and Veterans
The conflicts in Afghanistan and Iraq (OEF/OIF) have resulted in increased numbers of Veterans who have TBI. The main causes of TBI in OEF/OIF Veterans are blasts, motor vehicle accidents, and gunshot wounds. The Department of Defense and the Defense and Veteran's Brain Injury Center estimate that 22% of all OEF/OIF combat wounds are brain injuries. This is compared to TBI in 12% of combat wounds that occurred in Vietnam.
Veterans seem to have symptoms for longer than civilians. Some studies show most will still have symptoms 18-24 months after the TBI. Also, many Veterans have more than one medical problem, including: PTSD, chronic pain, or substance abuse. From 60-80% of Service members who are hurt in other ways by a blast may have a TBI. These other problems make it harder to get better from any single problem. Veterans should remember, though, that their TBI symptoms are likely to last only a limited time. With proper treatment and healthy behaviors, they are likely to improve.
With proper treatment and healthy behaviors, they are likely to improve.
VA is working to make sure that TBI care is easy to access. VA is using a TBI screening tool to begin the assessment process. VA has put in place the Polytrauma System of Care to treat Veterans with TBI who also have other injuries. Veterans with the most severe wounds are being treated at one of the 4 Polytrauma Rehabilitation Centers or one of the 21 Polytrauma Network Sites. Patients with less severe wounds may get treatment at local VA Medical Centers. No matter where a Veteran goes first, there is no "wrong door" for treatment.
Sources
Traumatic brain injury: A guide for patients. (n.d.). CogSMART, VA San Diego Healthcare System. Accessed at: http://www.mentalhealth.va.gov/docs/tbi.pdf.
Go To Provider Version
Traumatic brain injury: neurological and psychopathological aspects
Traumatic brain injury 1 is among the leading causes of preventable death, serious health problems and disability in individuals younger than 40 years [1].
Cerebral injury is most often associated with falls, road accidents (including motorcycle accidents), which account for over ½ of all traumatic cases. Due to a blow to the head or other causes, the brain rapidly shifts within the cranium [2]. At the same time, along with the primary brain damage associated with direct physical impact, secondary damage caused by a violation of cerebral blood flow or an increase in intracranial pressure is isolated.
Traumatic brain injury (traumatic brain injury) - TBI - as a result of physical effects on the brain substance must be distinguished from post-traumatic stress disorder .
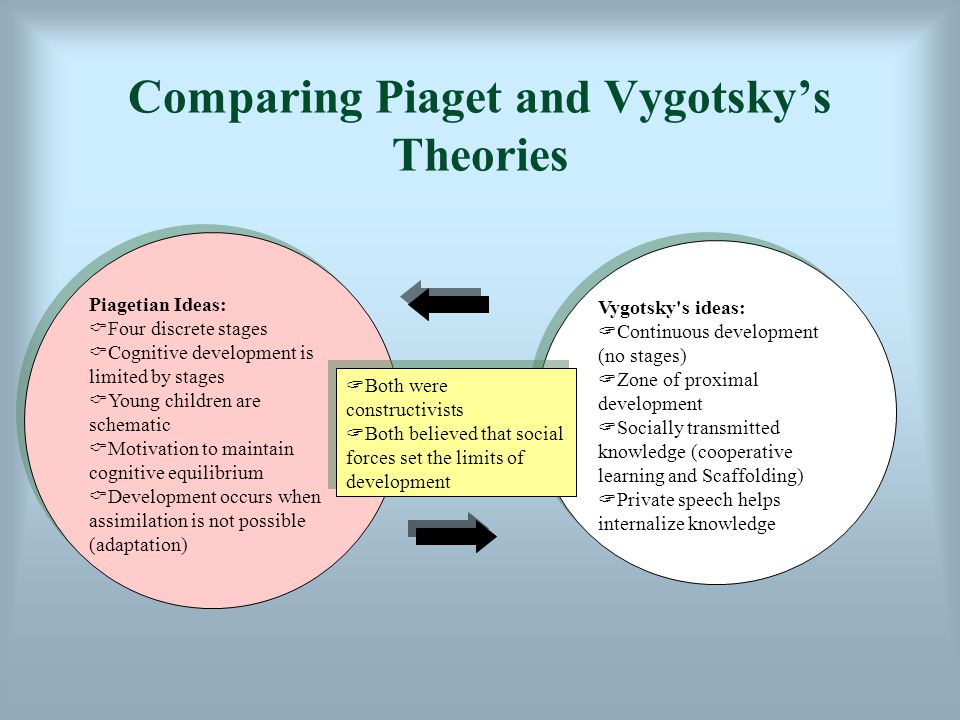
Terminological difficulties that arise when the concepts of TBI and PTSD are confused are exacerbated by the fact that these conditions often accompany each other [2]. Moreover, despite the psychogenic mechanisms of PTSD development, which make it possible to attribute it to the so-called functional states, the psychopathological symptoms of this disorder are usually accompanied by structural changes in the brain, primarily hippocampal atrophy [3, 4].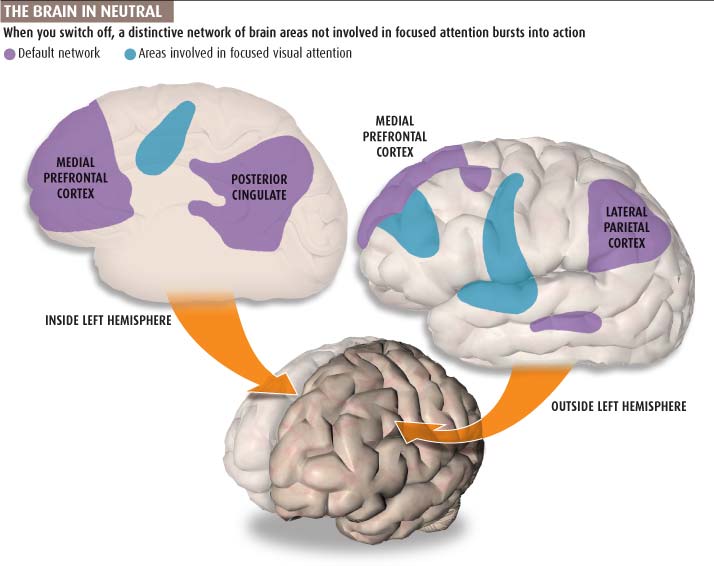
In this article, the rest of the discussion will focus mainly on TPM.
Epidemiology
The prevalence of the consequences of brain injury in the US is close to 2%; higher rates distinguish developing countries [5]. TBI is significantly more common in children, adolescents, and young adults than in adults. Its frequency in men is approximately 3 times higher than in women [6].
From 150 to 200 million new cases of severe disability due to head trauma are registered annually in the world [1].
Clinical manifestations
Like many other diseases of the central nervous system, brain injury is manifested by both neurological and psychopathological symptoms, and the distinction between the first and second is not always possible and, moreover, sometimes has no serious practical significance.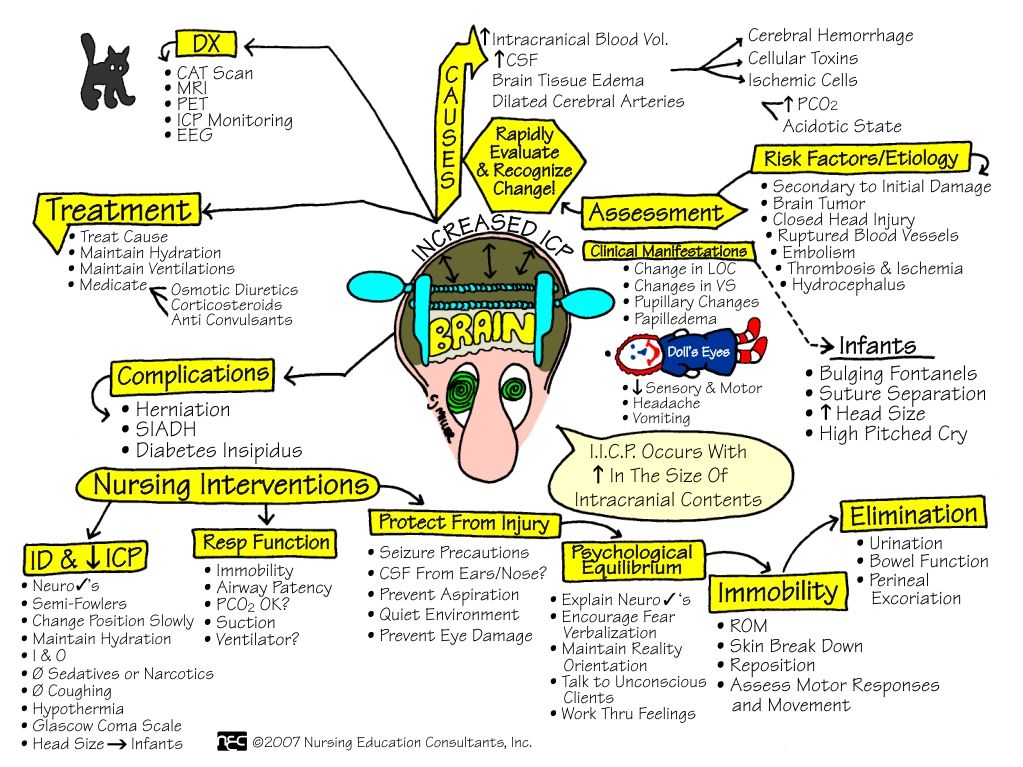
Acute brain injury is defined by the presence of at least one of the following: loss of consciousness, post-traumatic amnesia, disorientation and confusion, and in more severe cases, structural changes determined by neuroimaging, the appearance or increase of paroxysmal disorders, narrowing of visual fields, anosmia, or hemiparesis [2]. Acute and subacute periods of brain injury can be manifested by the so-called post-commotion syndrome, which includes headaches, weakness, fatigue, dizziness, decreased concentration, sleep disturbances, irritability, emotional lability, increased sensitivity to noise and bright light, and other nonspecific symptoms [7].
Chronic TBI is characterized by a wide range of disorders that can persist for many years after injury. Their main manifestation is a neurocognitive deficit, including impairments to memory, attention, executive functions, and learning.
Neurocognitive impairments represent one of the main causes of decline and permanent disability in individuals who have experienced a brain injury.
The predominant type of mental disorders associated with TBI and not related to the cognitive sphere are mood disorders, including irritability, dysphoria, depression, and (much less often) mania. In some cases, there is a combination of depressive and manic disorders. Among the typical psychopathological manifestations of TBI is a combination of symptoms of depression and anxiety as universal and least specific manifestations of cerebral lesions of any etiology. Brain injury significantly increases the risk of suicide [2, 7].
Psychopathological manifestations of brain injury are largely determined by the localization of the lesion (not excluding the influence of premorbid factors). For example, disturbances in emotional regulation, aggression, and a tendency to violence are often associated with damage to the frontal lobes, primarily the orbitofrontal cortex (and, to a certain extent, the cortex of the anterior parietal lobes) [8]. Typical manifestations of the so-called frontal lobe syndrome include impulsivity, irritability, and emotional outbursts [7].
In a number of cases, cerebral injury, especially in the acute period, is complicated by psychosis, proceeding according to organic or endogenous (schizophrenia-like or affective) types; the development of endoform psychoses is usually associated with damage to the orbitofrontal and anterior parietal zones 2 [7].
Like other organic brain diseases, TBI is characterized by reduced tolerance to psychotropic drugs, which must be taken into account when choosing drugs and determining their dosing regimen, which is discussed in more detail below.
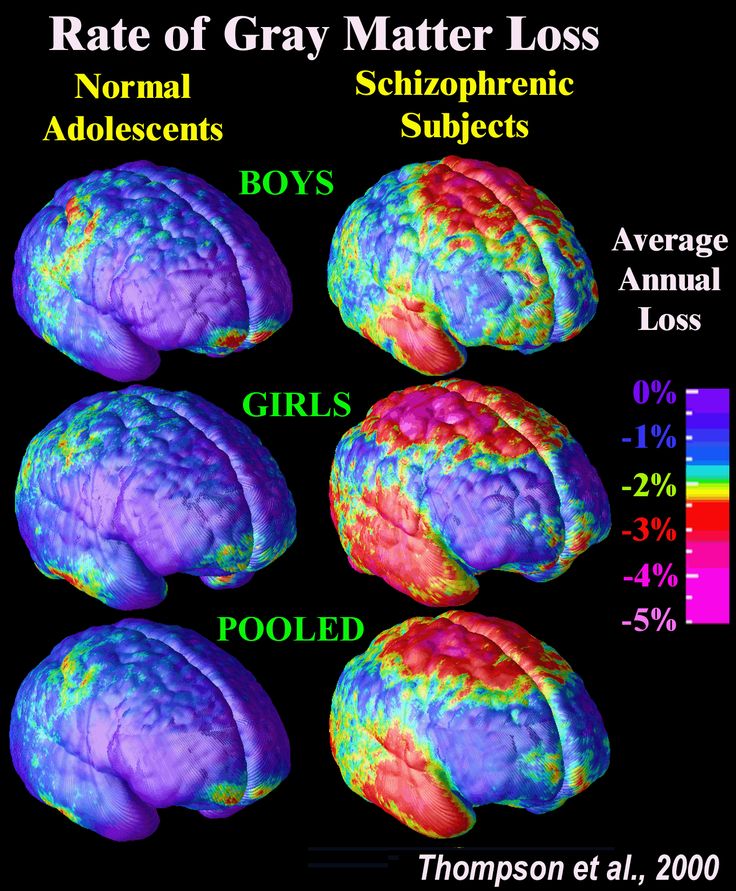
The course and symptoms of traumatic cerebral disorders are characterized by gender differences, and it is assumed that these differences are associated with the influence of sex hormones. However, data have recently appeared that this may be associated with some features of the functioning of cellular brain structures, in particular microglia [6].
As noted above, TBI often occurs in connection with events, a significant part of which is psychological stress (violence, including its domestic forms, war, professional sports, etc.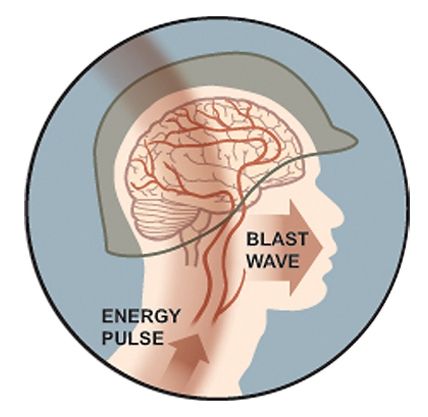 ). Therefore, the differentiation of the origin of individual psychopathological symptoms (for example, anxiety) due to physical or mental trauma or as a result of their combined influence presents significant difficulties.
). Therefore, the differentiation of the origin of individual psychopathological symptoms (for example, anxiety) due to physical or mental trauma or as a result of their combined influence presents significant difficulties.
Diagnosis of TBI is based on history, clinical symptoms, and neuroimaging techniques, primarily computed x-ray and magnetic resonance imaging.
It should be noted that the consequences of brain injury may include not only neurological and mental disorders, but also damage to internal organs caused, in particular, by neuroendocrine factors. So, S. Giuliano et al. [9] report growth hormone deficiency as a manifestation of hypopituitarism in 35–48% of patients with TBI and related visceral obesity and other metabolic disorders.
Course and outcome
The course of TBI and its outcome are characterized by pronounced diversity, which, apparently, is determined by the interaction of various factors, including the severity of the injury, the location of functional and structural changes, individual reactivity, and concomitant circumstances.
It is believed that TBI in children is accompanied by less pronounced mental disorders than in adults, due to the high degree of neuroplasticity of the child's brain. On the other hand, recovery after a childhood brain injury can last up to 5 years, while in adults this period usually does not exceed 2 years [7].
In most cases, the disease is characterized by a favorable course with a gradual restoration of cerebral and mental functions; less often persistent neurocognitive disorders occur, reaching the degree of dementia in some cases.
The so-called fist dementia ( dementia pugilistica ) 3 , which occurs in boxers and is a type of subcortical dementia and is associated with diffuse brain damage, including various parts of the cortex, basal ganglia and cerebellum, is considered as a special form of neurocognitive deficit.
In our opinion, it is necessary to distinguish between traumatic dementia, which develops in direct connection with brain damage, and an increased risk of dementia associated with advanced age, such as Alzheimer's disease (AD). According to some authors [5, 10], moderate and severe forms of TBI increase the risk of developing dementia by 2–4 times. The increased risk of developing AD due to brain injury is partly determined by the fact that traumatic cerebral injury is a trigger for typical structural changes that underlie presenile cerebral atrophy. It was shown [11], in particular, that even a slight repeated traumatic effect on the brain 4 contributes to the development of such typical neuromorphological substrates of Alzheimer's dementia as the formation of β-amyloid and τ-protein.
According to some authors [5, 10], moderate and severe forms of TBI increase the risk of developing dementia by 2–4 times. The increased risk of developing AD due to brain injury is partly determined by the fact that traumatic cerebral injury is a trigger for typical structural changes that underlie presenile cerebral atrophy. It was shown [11], in particular, that even a slight repeated traumatic effect on the brain 4 contributes to the development of such typical neuromorphological substrates of Alzheimer's dementia as the formation of β-amyloid and τ-protein.
It has been hypothesized [12] that a single moderate-to-severe brain injury contributes to the development of AD, while repeated mild injuries are more likely to lead to the formation of chronic traumatic encephalopathy. There are also sufficient grounds for formulating, on the one hand, the concept of multiple TBI pathology, and, on the other hand, a certain universality of organic brain damage of various origins.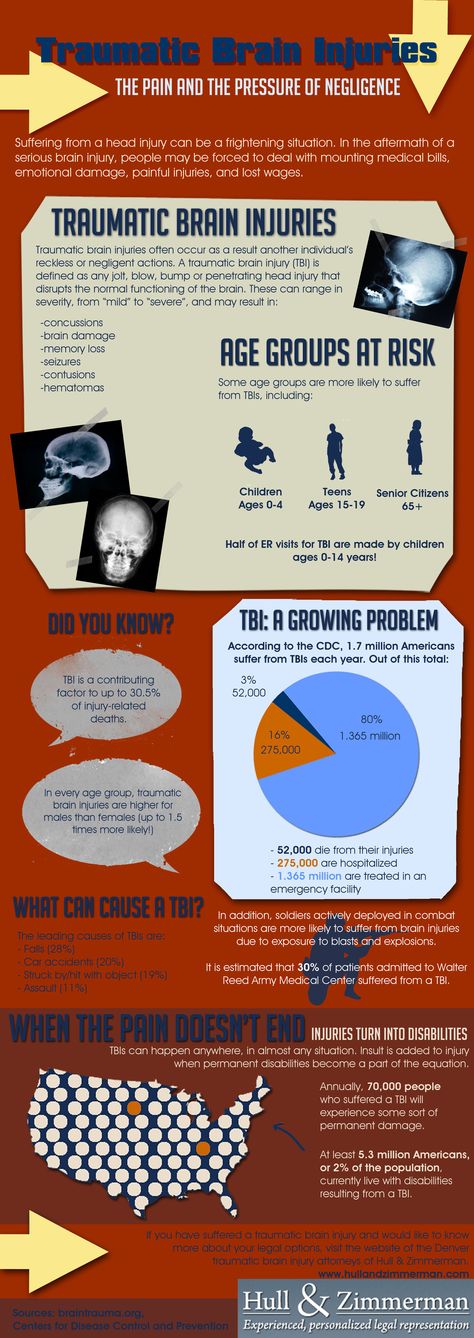 The validity of both one and the other view is confirmed by the presence of such neuromorphological manifestations of cerebral injury as the deposition of β-amyloid, a change in the conformation of the τ-protein, the presence of a pathological form of the TDP-43 protein and Lewy bodies, characteristic of various forms of dementia (BA, frontotemporal dementia, disease with Lewy bodies), previously considered specific for some of them [12].
The validity of both one and the other view is confirmed by the presence of such neuromorphological manifestations of cerebral injury as the deposition of β-amyloid, a change in the conformation of the τ-protein, the presence of a pathological form of the TDP-43 protein and Lewy bodies, characteristic of various forms of dementia (BA, frontotemporal dementia, disease with Lewy bodies), previously considered specific for some of them [12].
Therapy
Therapeutic measures for TBI can be divided into three main areas with some degree of conventionality: 1) correction of cerebral disorders that occur during the acute period of injury; 2) treatment of neurocognitive disorders; 3) treatment of mental disorders.
Treatment of cerebral disorders of the acute period of injury
The main targets of therapy in the acute period of injury are cerebral ischemia, inflammation and imbalance of redox reactions.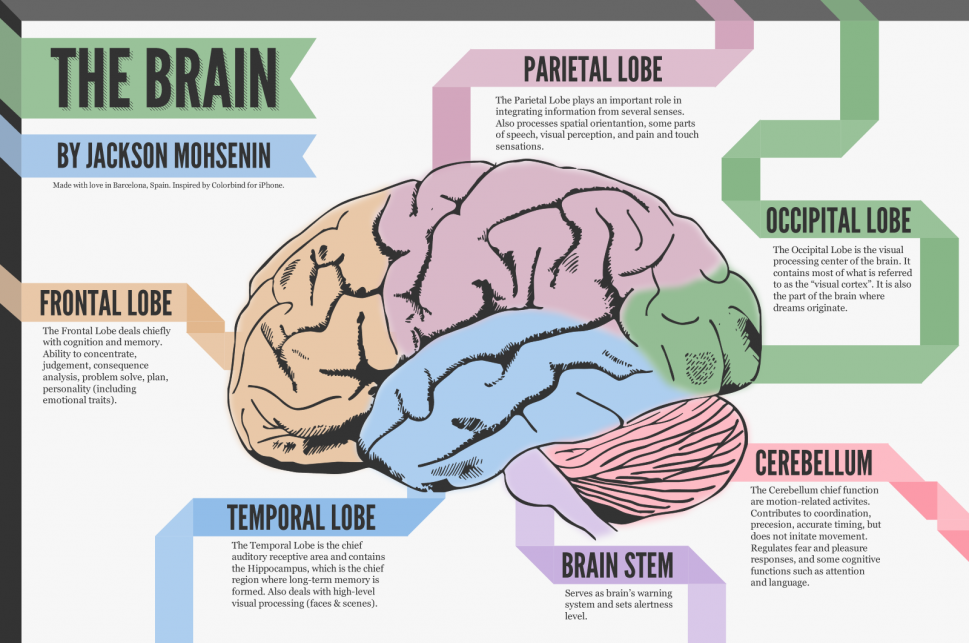
In one of the experimental animal studies [13], the neuroprotective effects of glibenclamide in acute brain injury were noted, mediated by the effect on tight (intercellular) junction proteins, the activity of which is associated with cell apoptosis, blood-brain barrier permeability, tissue water content and hemoglobin.
Experiments with TBI modeling in rats [14] demonstrated the ability of S-nitrosoglutathione to stabilize redox processes and suppress pathological mechanisms of secondary cerebral damage. In comparison with animals of the control group, rats treated with S-nitrosoglutathione had a lower degree of expression of pro-inflammatory proteins, less pronounced activation of macrophages and infiltration of brain tissue by macrophages, a decrease in the number of cell deaths, a smaller area of cerebral damage, and a higher reversibility of general histological changes. Based on the data obtained, the authors suggested possible prospects for the successful use of S-nitrosoglutathione in the treatment of TBI and its consequences in medical practice.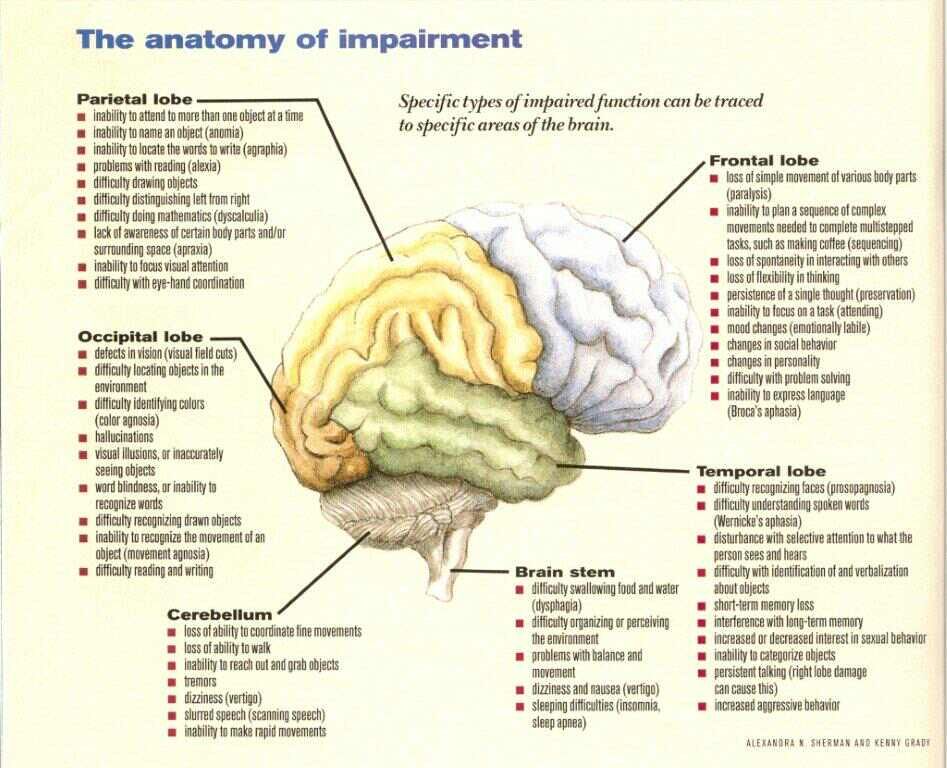
Summarizing the literature data, A. Hadanny and S. Efrati [15] noted the lack of satisfactory effectiveness of pharmacological and non-pharmacological approaches to influence both the clinical symptoms of the acute stage of TBI and the cascade of pathophysiological changes caused by trauma. At the same time, the authors suggested possible therapeutic prospects associated with hyperbaric oxygenation. R. Gultekin et al. came to similar conclusions. [16], who pointed to the lack of evidence for the effectiveness of drugs such as magnesium, monoamine and dopamine agonists, progesterone, aminosteroids, inhibitors of excitatory amino acids, hemostatic and antifibrinolytic agents in the treatment of acute brain injury.
Treatment of neurocognitive disorders
D. Dougall et al. [1] in a systematic Cochrane review, emphasizing the limited number of relevant studies that meet the correct inclusion criteria and the insufficient number of observations excluding the possibility of a meta-analysis, consider the effectiveness of the treatment of chronic neurocognitive disorders associated with TBI with the following drugs: modafinil (51 patients), OSU- 6162 5 (12), atomoxetine (60) and rivastigmine (167).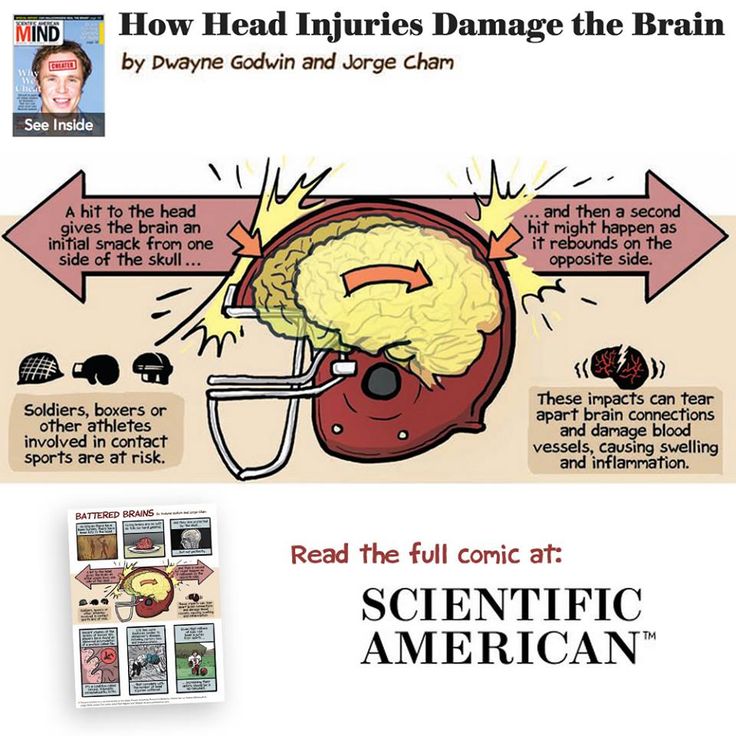 Based on the data obtained, the authors concluded that all substances were tolerable to placebo, with no deaths in all groups, insignificant superiority of rivastigmine and OSU-6162 over placebo in terms of individual efficacy indicators, and the absence of significant differences in the clinical effects of modafinil and atomoxetine from placebo.
Based on the data obtained, the authors concluded that all substances were tolerable to placebo, with no deaths in all groups, insignificant superiority of rivastigmine and OSU-6162 over placebo in terms of individual efficacy indicators, and the absence of significant differences in the clinical effects of modafinil and atomoxetine from placebo.
S. Gruenbaum et al. [17] in a systematic review and meta-analysis of 25 clinical studies of the effectiveness of neuroprotective therapy concluded that there are no therapeutic agents that undoubtedly improve the neurological outcomes of TBI, and at the same time suggested the possible presence of neuroprotective properties and the ability to improve the course of brain injury in statins, N-acetylcysteine , enzogenol, cerebrolysin and nitric oxide synthase inhibitor. However, according to the authors, a more definite judgment about the effectiveness of these drugs requires further research.
M. Maksimowski and R. Tampi [18] in a systematic review reflecting the results of 18 randomized controlled trials of the effectiveness of psychostimulants (methylphenidate, dextroamphetamine and modafinil 6 ) report a significant reduction in reaction time, a decrease in depressive symptoms, an increase in concentration attention or improvement of short-term (within 30 days) motor memory in patients with TBI, only in separate studies and in general, they state the absence of fundamental differences in the effects of the noted drugs from the effect of placebo.
Data were obtained [19] on the superiority of methylphenidate (in combination with methods of metacognitive rehabilitation) over placebo in the ability to increase attention, improve episodic and working memory, as well as executive functions in individuals with cerebral injury.
Treatment of mental disorders
Mental disorders that develop in acute and chronic periods of brain injury often require the appointment of psychotropic drugs. In these cases, psychopharmacological therapy is symptomatic.
In connection with the above-mentioned predominance of mood disorders in TBI, a special place in the treatment of mental disorders is occupied by normothymic drugs (anticonvulsants-normothymics, lithium preparations). An equally important role belongs to antidepressants as first-line drugs in the treatment of depression and disorders associated with anxiety.
Benzodiazepines and related Z drugs may also be used in the treatment of anxiety and sleep disorders 7 . Buspirone, etifoxine, and pregabalin represent a definite alternative as the newest of these and the most promising treatment for anxiety disorders.
Buspirone, etifoxine, and pregabalin represent a definite alternative as the newest of these and the most promising treatment for anxiety disorders.
Psychotic disorders are, of course, a direct indication for the prescription of antipsychotics (neuroleptics). It is important to note, however, that the use of antipsychotics for the treatment of non-psychotic psychiatric disorders (eg, dysphoria and behavioral disorders) is not only an undesirable but often misguided 8 therapeutic decision.
As noted above, TBI is characterized by a deterioration in the tolerance of psychotropic drugs, therefore one of the leading principles of symptomatic therapy is the administration of drugs in the minimum therapeutic dose, its increase is permissible only if the therapeutic effect is insufficient and there are no noticeable side effects.
When choosing psychotropic drugs for the treatment of TBI, preference should be given to new generations of drugs with an optimal balance of efficacy and tolerability, such as selective serotonin reuptake inhibitors (instead of tricyclic antidepressants and monoamine oxidase inhibitors) and atypical antipsychotics (instead of typical representatives of this class).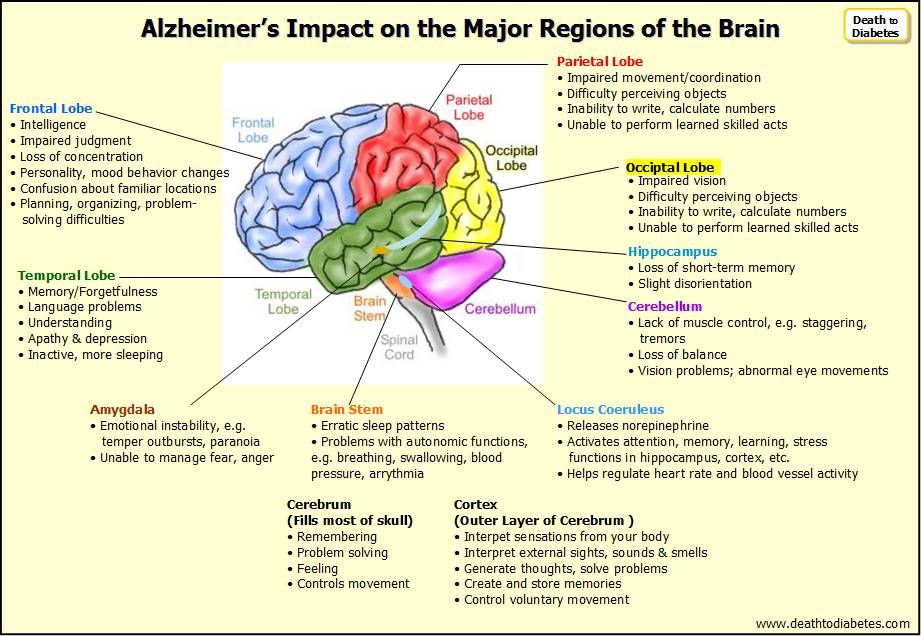
It should also be taken into account that the use of antipsychotics in elderly people with dementia increases the risk of premature death [20, 21], and the relationship between antipsychotics and mortality is dose-dependent [22].
In experiments on rats, the ability of mifepristone, blocking glucocorticoid receptors 9 (but not spironolactone, as a mineralocorticoid receptor antagonist), was noted to prevent the onset of anxiety associated with TBI; researchers suggest that the use of such approaches in acute cerebral injury can prevent anxiety disorders in victims [23].
Behavioral strategies, including cognitive behavioral therapy, which, according to D. Black and N. Andreasen [2], “may be extremely useful” for patients with neurocognitive disorders associated with with cerebral injury.
The authors of one of the Cochrane reviews [24], noting the limited nature of the existing data on cognitive behavioral therapy for TBI (single randomized controlled trials met the inclusion criteria), are very cautious about the effectiveness of such therapy and neurorehabilitation in patients with symptoms of generalized anxiety and acute stress response, indicating the need for further research in this direction.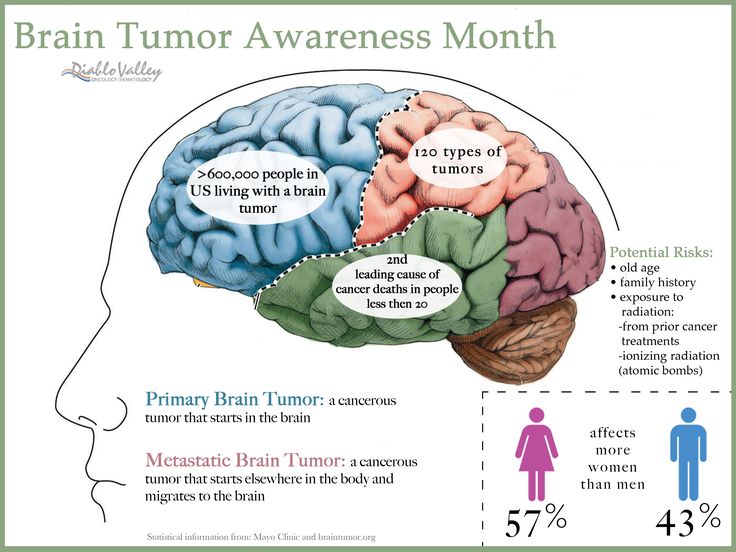
Summarizing the data presented in the article, it can be emphasized that traumatic brain disease manifests itself in a wide range of acute and chronic disorders, the symptoms of which are determined by the severity and duration of the injury, the location of the cerebral lesion, the individual characteristics of the patient's reactivity, and many other factors.
Despite a wide range of modern drugs and non-pharmacological therapeutic approaches, the treatment of both acute and chronic disorders caused by brain injury is still a difficult and far from solved task. Probably, one of the ways to solve the therapeutic problem of TBI is the search for new drugs, although the directions of this search are currently not very clear. Certain therapeutic perspectives are associated with potential effects on neurogenesis.
The data presented in the article also allow us to assess their basis for the assertion that the border between neurology and psychiatry is often conditional and hardly needs precise demarcation.
The authors declare no conflict of interest.
1 Hereinafter in the text we are talking about mild and moderate traumatic brain injuries.
2 An unconditional role, along with the localization of cerebral damage in the development of endoform psychosis of any origin, is played by constitutionally determined features of an individual psychopathological response.
3 One of the slang definitions of this type of traumatic encephalopathy in the English literature is the concept of “punch-drunk syndrome”.
4 Such effects include the above-mentioned systematic brain injuries in athletes, not only boxers, but also, for example, football players.
5 Partial agonist of dopamine D2 receptors and serotonin 5-HT2A receptors, designated as a monoamine stabilizer and exhibiting antipsychotic, antiaddictive and antiparkinsonian properties in animal studies.
6 Strictly speaking, modafinil is regarded as a wakefulness-promoting agent with a different mechanism of pharmacological action from classical psychostimulants (amphetamines); the drug is used to treat narcolepsy, and, according to preliminary data, can improve mood and improve cognitive activity in both healthy and schizophrenic patients and individuals who abuse alcohol.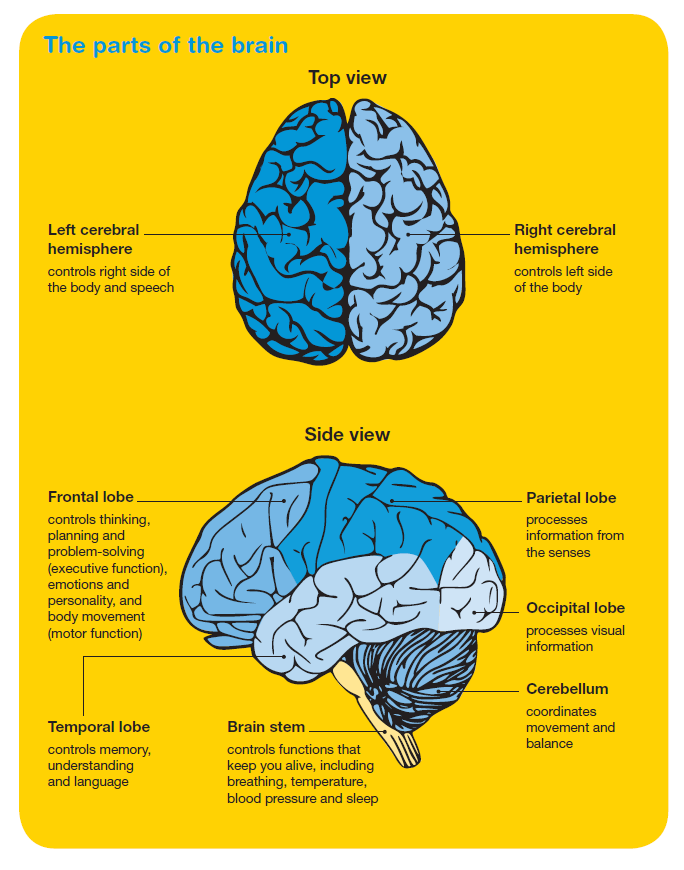
7 Z-drugs include zopiclone, zolpidem, zaleplon, and some other hypnotics.
8 Significantly more effective and safer treatment of dysphoria than neuroleptics are anticonvulsants-normotimics (eg, carbamazepine and valproic acid).
9 Data from experimental studies [23] indicate a certain role of increased glucocorticoid activity in the development of anxiety associated with brain injury.
Head Injuries: Causes, Symptoms, Treatment | doc.ua
Causes
Head injury can be closed or open. The closed type is characterized by trauma to the brain through the bones and tissues of the skull, and is sometimes accompanied by a closed fracture of the bones of the skull. In the latter case, it is a closed craniocerebral injury. This also includes damage to the soft tissues of the skull without fracture of the bones. That is, we mean such a craniocerebral injury in which the intracranial cavity remains closed.
Open traumatic brain injury can be non-penetrating and penetrating.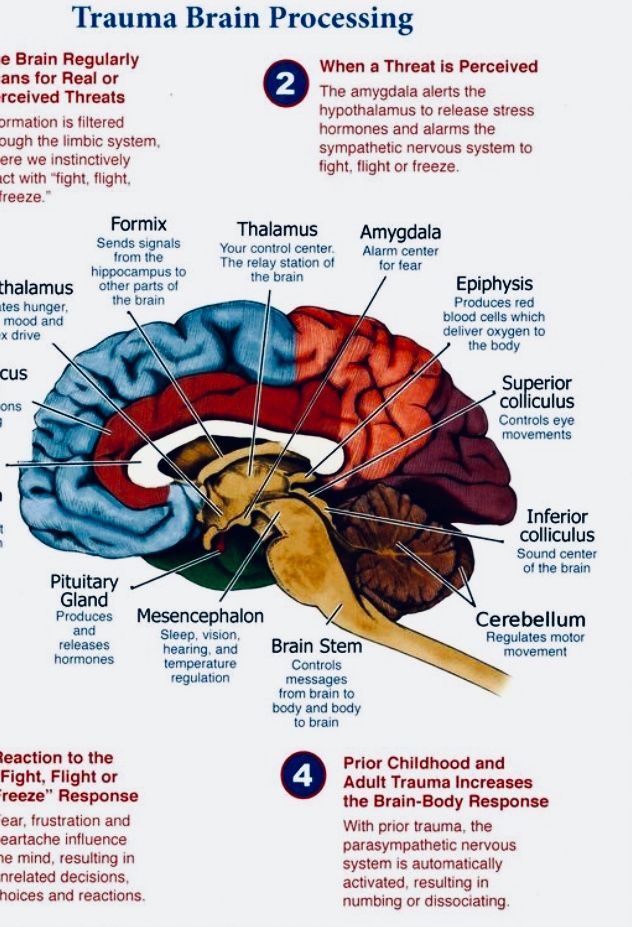 With non-penetrating, the hard shell of the brain remains intact, with penetrating - it is damaged. With a penetrating wound, there is a risk of developing meningoencephalitis, purulent meningitis, and a brain abscess.
With non-penetrating, the hard shell of the brain remains intact, with penetrating - it is damaged. With a penetrating wound, there is a risk of developing meningoencephalitis, purulent meningitis, and a brain abscess.
Consequences of a penetrating trauma of the skull in the brain and its membrane are complex pathological processes that are associated with disorders of both the brain itself and disorders of the liquor and blood circulation, swelling and swelling of the brain, and infection. This complex is called traumatic brain disease. It is divided into five periods:
- acute (initial) - the first three days;
- early reactions and complications - from 3 days to 1 month;
- elimination of early complications and restriction of the infectious focus - from the second month to six months;
- complications - last up to 2-3 years;
- long-term consequences of traumatic brain injury - many years after the injury.
Symptoms
The main feature of injuries is a disorder of consciousness.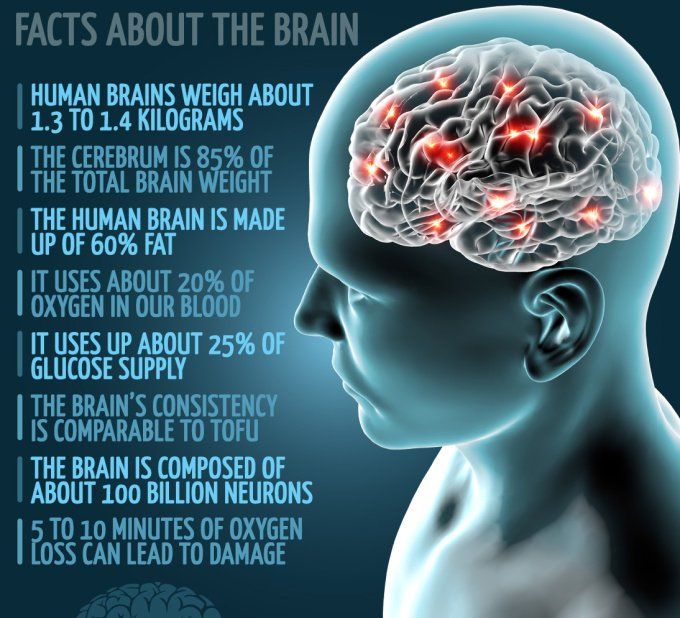 If it continues for a long time, then there is a real threat to the life of the patient. To assess the severity of the patient's condition, the following scheme is used during his first examination:
If it continues for a long time, then there is a real threat to the life of the patient. To assess the severity of the patient's condition, the following scheme is used during his first examination:
- full consciousness after its short-term loss: the victim orients himself in the place of stay, time and situation, he adequately reacts to the environment;
- partial loss of consciousness: lethargy is observed in the behavior of the victim, he is drowsy, but he fulfills insistent demands;
- severe stupor: the victim performs elementary tasks only after insistent demands;
- medium stupor: the victim performs more complex tasks, answers the doctor's questions in monosyllables;
- slight dazedness: the victim is slightly disoriented, responds slowly to questions;
- in the soporous state (hibernation), the victim retained only the main reflexes (corneal, corneal, bronchial and swallowing). The injured person reacts to pain stimuli with a grimace of pain or jerking of the limbs.
 Autonomic reactions to pain persist - rapid breathing and pulse, intermittent pupillary reactions, vasomotor disorders;
Autonomic reactions to pain persist - rapid breathing and pulse, intermittent pupillary reactions, vasomotor disorders; - coma - in this state, the victim does not respond to either external or internal stimuli. Motor activity is completely stopped. With increasing coma, all reflexes disappear, muscle tone decreases, sphincters relax. At the same time, respiratory function is disturbed, heart failure develops. Pupils dilate, pupillary reactions disappear. These symptoms are characteristic of atonic coma.
Often, head injuries associated with loss of consciousness are accompanied by retrograde amnesia: patients do not remember the moment of the injury, they do not know about the loss of consciousness and its duration. The cardiovascular system responds by slowing down the heart rate. In parallel, irritation of the nuclei of the vagus nerve is observed, which then happens in various states. leading to high intracranial pressure. The pulse quickens due to irritation of the sympathetic nuclei of the trunk.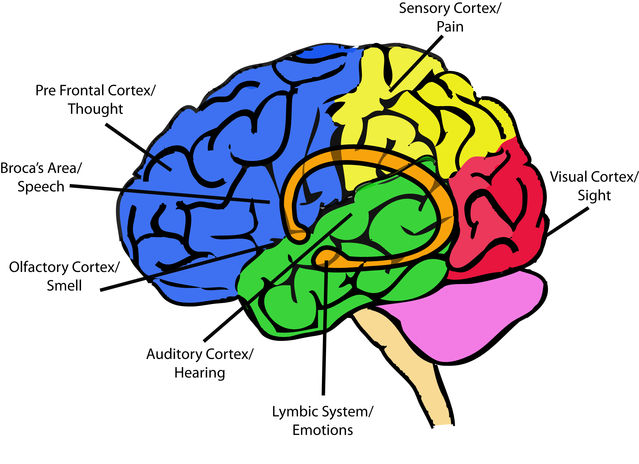 At times, paroxysmal tachycardia joins the symptoms. There is a fluctuation in blood pressure and regional blood flow disorders. Cardiovascular disorders are accompanied by violations of the depth, frequency, rhythm of breathing. This is due to the direct connection of the systems with lesions of the parasympathetic and sympathetic nuclei of the brainstem.
At times, paroxysmal tachycardia joins the symptoms. There is a fluctuation in blood pressure and regional blood flow disorders. Cardiovascular disorders are accompanied by violations of the depth, frequency, rhythm of breathing. This is due to the direct connection of the systems with lesions of the parasympathetic and sympathetic nuclei of the brainstem.
Vomiting is a clear sign of injury. It occurs immediately after the impact. It causes irritation of the IV ventricle, vestibular disorders, irritation of the meninges, as well as high intracranial pressure caused by edema and swelling of the brain. The vestibular apparatus responds with dizziness, a sensation of movement of objects around the injured person, spontaneous nystagmus, a violation of the sense of balance, labyrinthine deceptions that attack paroxysmal, dizziness and loss of consciousness. Often after a blow, a divergent strabismus is diagnosed, as well as a violation of convergence.
Symptoms of moderate and severe craniocerebral trauma make themselves felt with headaches resembling migraines or spasms - the patient complains of pressure in the temples, aching, burning and heaviness of the head, feel a painful pulsation.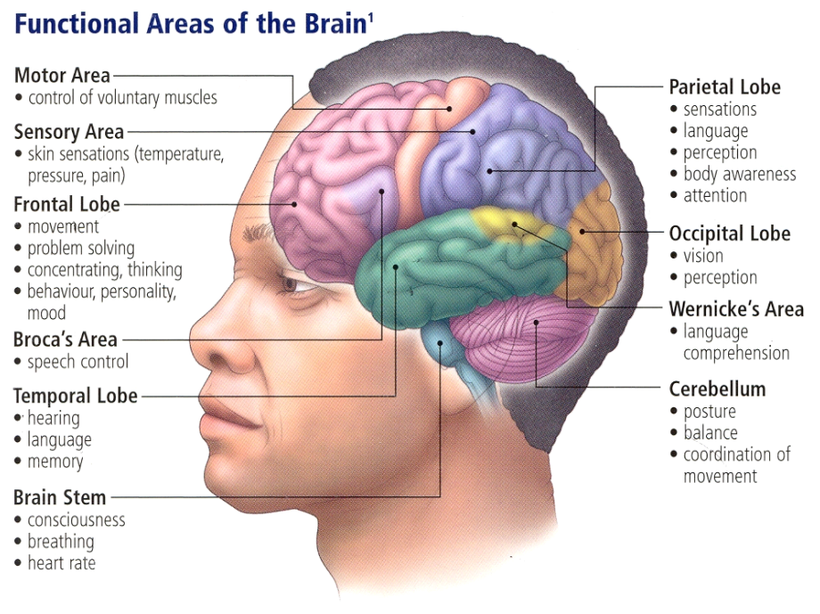 If there is no subarachnoid hemorrhage, then the headache is rarely severe. Pupillary reflexes are sluggish. Focal symptoms are the result of injury to various areas of the brain. Depending on the regular occurrence of the same manifestations or their combination, it is possible to determine which part of the brain is damaged. It does not necessarily coincide with external damage to the tissues of the skull.
If there is no subarachnoid hemorrhage, then the headache is rarely severe. Pupillary reflexes are sluggish. Focal symptoms are the result of injury to various areas of the brain. Depending on the regular occurrence of the same manifestations or their combination, it is possible to determine which part of the brain is damaged. It does not necessarily coincide with external damage to the tissues of the skull.
Thus, paralysis, Jackson-type seizures and paresis are characteristic of the blockade of the functions of the motor center, compressed as a result of a fracture. Increasing paresis indicates the formation of a hematoma, arterial thrombosis, or the spread of phlebothrombosis. An equally important symptom is a speech disorder. The consequences of traumatic brain injury may include: post-traumatic arachnoiditis, brain atrophy, pachymeningitis, liquor fistula, chronic hematoma, etc.
In the presence of any alarming symptoms, it is important to consult a traumatologist or a surgeon in a timely manner.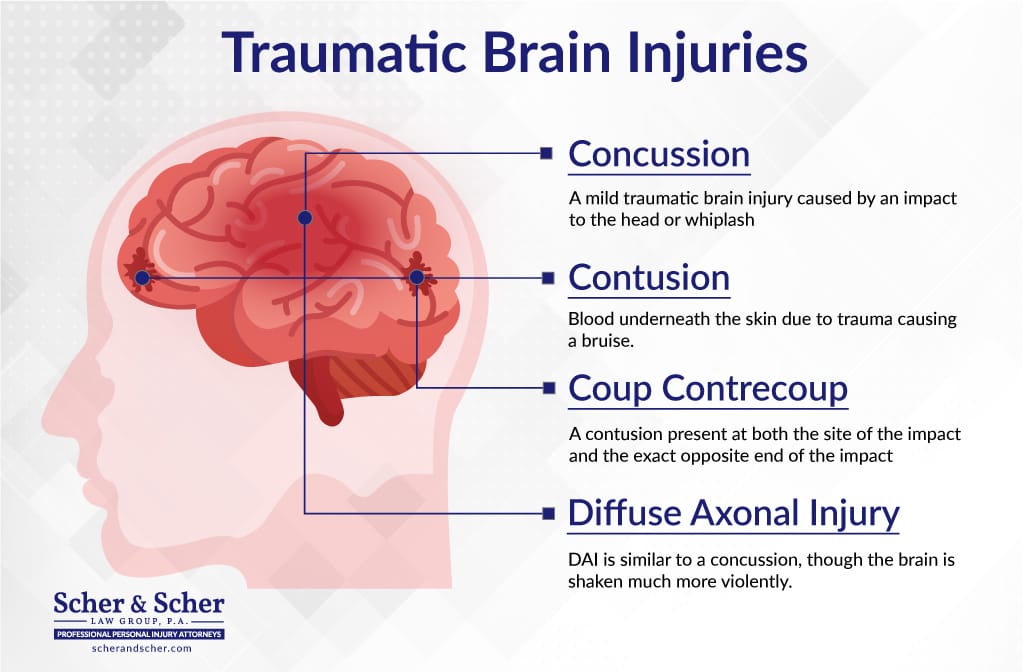 You can choose the right specialist in the list of doctors from the catalog of our website.
You can choose the right specialist in the list of doctors from the catalog of our website.
Cerebral concussion
Cerebral concussion is a complex of symptoms that occurs after a skull injury and develops as functional disorders. First of all, we are talking about vegetative disorders. This is the simplest form of injury of this kind. From the point of view of physiology, this is a syndrome of sudden paralysis or paresis of vasomotor, respiratory, reflex, and other brain activities resulting from injury against the background of loss of consciousness. Such a symptom complex is not accompanied by morphological changes in the membrane and tissues of the brain; this does not apply to other injuries of the skull. Signs of a concussion are:
- impairment of consciousness ranging from stupor to stupor, which can be measured in seconds or minutes;
- retrograde amnesia, which covers events immediately before the injury, as well as anterograde amnesia, which covers a narrow period of time after the injury;
- after regaining consciousness, the victim complains of headaches, dizziness, weakness, noise and ringing in the ears.
 Hot flushes to the face, sleep disturbance, sweating and a number of other vegetative manifestations are observed. There are also pains in the region of the eyeballs and forehead during the movement of the open eyes, vestibular hyperesthesia develops, an oculostatic phenomenon, divergence of the eyeballs during reading;
Hot flushes to the face, sleep disturbance, sweating and a number of other vegetative manifestations are observed. There are also pains in the region of the eyeballs and forehead during the movement of the open eyes, vestibular hyperesthesia develops, an oculostatic phenomenon, divergence of the eyeballs during reading; - breathing becomes shallow, its frequency changes, but without arrhythmia, then it quickly returns to normal;
- the pulse corresponds to the physiological norm, but immediately after the injury it speeds up or slows down a little;
- single vomiting possible immediately after impact;
- the face may turn pale, after which its hyperemia is observed;
- in some cases, concussion is accompanied by asymmetry of the mimic muscles of the face, tendon and skin reflexes. They disappear on the third day after the injury;
- CSF pressure is sometimes lowered.
These patients usually recover within a week of injury, provided adequate concussion treatment is provided .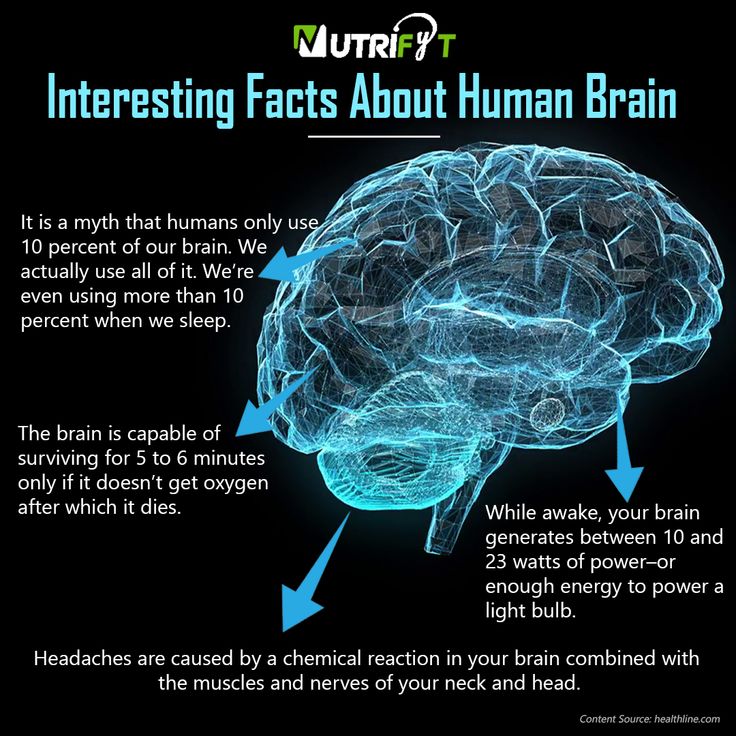
Brain contusion
This type of injury is characterized by focal symptoms. An absolute sign of a bruise of any degree is a fracture of the base and calvaria or the presence of impurities in the cerebrospinal fluid.
Brain contusion may be accompanied by mild or severe anisocoria. Severe anisocoria cannot be confused with Horner's syndrome - it manifests itself in the form of miosis, enophthalmos or ptosis, which is sometimes regarded as mydriasis on the opposite side. These forms of pupillary disorders must be distinguished, since Horner's syndrome is caused by damage to the synaptic plexus, in particular, the stellate ganglion. An increasingly pronounced pupil dilation in some cases indicates direct compression of the optic nerve. This should cause concern, since intracranial hematoma may compress the homolateral hemisphere. Mild contusion: symptoms are characterized by reflex asymmetry.
For a moderate contusion, more pronounced focal symptoms of CNS damage are characteristic - hemiplegia or hemiparesis, aphasia, hypoesthesia, damage to the cranial nerves (trigeminal, auditory, facial, oculomotor).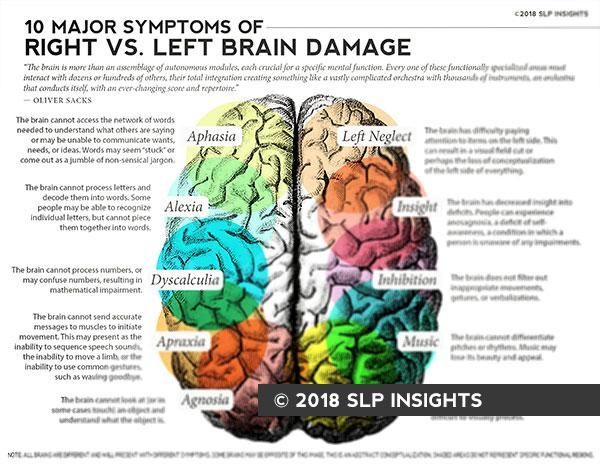 In the acute period, the symptoms resemble cerebral ones, but after the restoration of consciousness, the first ones are more expressive.
In the acute period, the symptoms resemble cerebral ones, but after the restoration of consciousness, the first ones are more expressive.
Severe contusion includes trauma to the base of the brain, mediobasal regions, diencephalic region. This condition can be fatal. It is characterized by a long-term soporous-coma state, especially with a primary lesion of the brain stem, often accompanied by a disorder of vital functions, gross neurological disorders - both cerebral and local, profound disorders of metabolism, blood flow, etc. If intracranial pressure rises, congestive optic discs are present. After coming out of a coma, patients remain in a state of stupor or stupor for a long time, disorientation is noted.
Diagnosis
Diagnosis includes a series of examinations of the patient's brain disease. In particular, they include lumbar puncture to study pressure, transparency and composition of cerebrospinal fluid, angiography of cerebral vessels, encephalography. Angiography allows you to determine the topic and nature of the damage.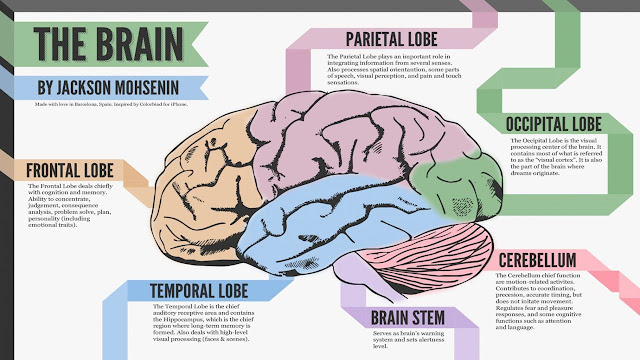 Trial trepanation of the skull is widespread. Such a study allows you to get the most accurate information about the injury and the cranial cavity.
Trial trepanation of the skull is widespread. Such a study allows you to get the most accurate information about the injury and the cranial cavity.
You can deliver the patient to the clinic using the "Honey Taxi" service.
Treatment
Treatment of traumatic brain injury involves a complex of measures. Upon admission of a patient with a severe skull injury, a number of resuscitation measures are carried out - they restore cardiopulmonary activity, brain activity. With a closed injury, accompanied by a depressed fracture of the cranial vault, surgical treatment of the wound is performed. It consists in the removal of bone fragments, the imposition of a blind suture on soft tissues. At the same time, if the patient feels satisfactory, primary cranioplasty can be performed. If the patient is in serious condition, the procedure is postponed.
In case of open head injuries, surgical treatment of the wound is performed - excision of soft tissues, removal of bone fragments, blood clots and brain debris, suturing.