Fainting from needles
Applied Tension Technique - For People Who Faint at the Sight of Blood or Needles
Most people feel a bit uneasy when they see blood or have to get a needle. However, for some people, seeing blood or needles causes them to faint or to feel like they will faint. It is very rare to actually faint from anxiety, unless you have this problem. If you tend to faint when you get an injection or have blood drawn you can benefit from learning a simple technique that will help you prevent fainting or speed up the recovery time if you do faint.
Why Do Some People Faint at the Sight of Blood or a Needle?
Fainting is caused by a sudden drop in your heart rate or blood pressure. When we are anxious, our heart rate and blood pressure actually go up. This is why it is so rare to faint when you are feeling anxious. However, some people with a fear of blood or needles experience an initial increase and then a sudden drop in their blood pressure, which can result in fainting. This drop in blood pressure is called the vasovagal response.
Only a small minority of people have this response at the sight of blood or needles. The good news is, if you have this problem there is a way to prevent it and keep yourself from fainting.
In most cases, fainting is harmless.The sudden drop in blood pressure that results from the vasovagal response is not dangerous or life-threatening.
However, it is important that you discuss your fainting with a doctor before using this technique or exposing yourself to situations (such as needles or blood) that could cause fainting.
The Applied Tension Technique
The Applied Tension Technique (The Applied Tension Technique was developed by Lars-Göran Öst) is a strategy developed to help prevent fainting or help people recover faster if they do faint. The technique involves tensing the muscles in your body, which then raises your blood pressure. If your blood pressure increases, you are less likely to faint.
How to Do It
Sit in a comfortable chair and tense the muscles in your arms, legs and trunk forabout 10 to 15 seconds. You should hold the tension until you start to feel a warm sensation in the head. Then, relax your body for 20 to 30 seconds. Repeat 5 times.
You should hold the tension until you start to feel a warm sensation in the head. Then, relax your body for 20 to 30 seconds. Repeat 5 times.
TIP: When you relax your muscles after tensing them, the goal is not to become completely relaxed, as this will cause your blood pressure to drop. Rather, the goal is to let you body return to a normal state (not overly tense or completely relaxed).
Practicing
It is important that you practice this strategy several times a day for at least a week.
Using the Applied Tension Technique with Exposure Exercises
After you have practiced this technique for at least a week, you can start using this strategy when doing exposure exercises to blood and needles. See modules on Specific Phobia for more information.
Helpful Tips:
- Speedy Recovery: If you do faint, you can speed up your recovery by lying down and elevating your feet.
- Tense & Relax: If you tense your arm when you are receiving a needle, it can be more painful.
 Try to relax the arm that will be receiving the needle, while tensing the other parts of your body. However, since this can be difficult to do, it’s important to practice before going to get an injection. Alternatively, you can use the tension technique before and after getting a injection but try to release the tension in your body when you actually get the needle.
Try to relax the arm that will be receiving the needle, while tensing the other parts of your body. However, since this can be difficult to do, it’s important to practice before going to get an injection. Alternatively, you can use the tension technique before and after getting a injection but try to release the tension in your body when you actually get the needle. - Warning: If you develop a headache when trying the applied tension technique, try to reduce the level of tension or the frequency of practice sessions.
- Warning Signs: It can be helpful to learn to recognize the early signs of your blood pressure dropping, such as feelings of lightheadedness. Try to use the tension technique as soon as you start to experience these sensations.
- Practice: Even though this strategy sounds simple, it takes practice to be helpful.
Why blood and needles make some people faint
Fainting at the sight of a needle or blood is so common that Sharon Burke, a registered emergency nurse at Thomas Jefferson University Hospital, has a rule for family members who want to stay in the room when she starts an IV line.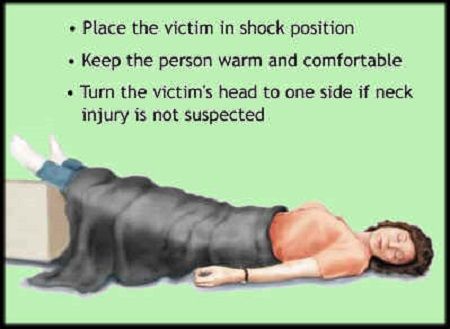
“If they refuse to sit down, we won’t stick the patient,” Burke said. “It’s not a policy, it’s kind of the street rule.”
Feeling faint or woozy at the sight of blood or a needle is a common reflex, initially triggered by the same “fight or flight” response that kicks in when people feel threatened or surprised.
“Initially their adrenaline spikes. All of a sudden they get a little bit jittery, their eyes get wider, they become hyper aware of things,” said Dr. Dan Frisch, a cardiologist at Thomas Jefferson University Hospital who specializes in arrhythmias.
This fight or flight response is your sympathetic nervous system kicking into gear.
“The classic example would be the tiger chasing you,” Frisch said. “Perhaps if you’re a cave man, that’ll get your blood pressure up, that’ll get your heart rate going, and you’ll run pretty fast and be hyperaware of your surroundings.”
After the threat has passed, the opposite system, the parasympathetic nervous system, is designed to take over to calm the body down by lowering blood pressure and heart rate. This opposite reaction to the “fight or flight” reaction is commonly called the “rest and digest” response.
This opposite reaction to the “fight or flight” reaction is commonly called the “rest and digest” response.
“Say you’ve captured that tiger and made it into a meal, at the conclusion of your meal, that feeling of being a little bit sedated or drowsy, that’s mediated more by the parasympathetic nervous system,” Frisch said.
These two systems are meant to balance each other out. But in people who feel woozy or faint when they see blood, a needle, or another surprising or upsetting trigger, the parasympathetic response overpowers the initial fight or flight response. Blood pressure and heart rate quickly drop too low and not enough oxygen is delivered to the brain so it starts to shut down. If you have stayed vertical during the initial feelings of wooziness, clammy skin and nausea, you’ll faint.
Unique human physiology leads to a uniquely human problem
This parasympathetic nervous system reaction is called the “vasovagal response” because it triggers a large, wandering nerve called the vagus nerve. Similar responses occur in animals too, but they don’t have the same fainting problem as humans.
Similar responses occur in animals too, but they don’t have the same fainting problem as humans.
The difference can be blamed on our ongoing battle with gravity, said Dr. Behzad Pavri, another Thomas Jefferson University cardiologist and the author of a book on fainting. As bipedal creatures, our heads are far above our hearts. It takes a lot of work to pump blood against gravity to keep our brains filled with oxygen, which predisposes us to fainting.
But that fight with gravity is just part of the story.
“If you’re talking head being above the heart, think of the giraffe,” Pavri said. “It ought to be fainting all the time, but it doesn’t. This is a problem that is unique to the human species.”
It is a unique problem because of our unique physiology. Pavri lists three reasons why:
1) Our enormous brains”We have to push one-fifth of our cardiac output up to our big, oxygen requiring brain,” much larger than our relative, the chimpanzee, Pavri said.
2) Our powerful lower extremitiesOur legs, which can carry us on marathons and ultra-marathons, can hold a lot of blood. When blood vessels all over the body dilate in the parasympathetic system’s “rest and digest” response, blood can pool in the legs and remain there instead of circulating back to the heart.
When blood vessels all over the body dilate in the parasympathetic system’s “rest and digest” response, blood can pool in the legs and remain there instead of circulating back to the heart.
3) We can lock our kneesThis prevents blood from being pumped back up to our hearts.
Fainting was likely a good thing for our ancestors
Because this fainting reaction has endured through hundreds of thousands of years of human evolution, doctors believe it must have been beneficial in some way.
One idea why, said Pavri, is that fainting allows us to play dead very effectively in the face of a predator.
“When [someone faints], they look like they died, they drain of blood from their face, they become completely pale, they are limp and unconscious on the floor, immobile,” Pavri said. “You can imagine how an aggressor may think the person is dead and walk away.”
Many animals play dead, but the theory goes that because our human adversaries were so much smarter than other animals, actually being unconscious helped to eliminate any telltale movement that an adversary may notice as signs of life.
Other research suggests that fainting could protect the heart during stressful situations.
Finally, plummeting heart rate and blood pressure could help stop the bleeding from a big cut.
“This reflex kicks in at the sight of blood or with pain [and] I faint, but while my blood pressure’s low it gives the bleeding limb a chance to clot,” Pavri said.
Why we often have this reaction when we see others bleeding or getting stuck with a needle is still an open question.
It could just be that a needle is a needle, no matter where it is aimed.
Or, it could be a sign of a kind of unconscious empathy pre-programmed into all of us humans.
“There’s just something about observing physical symptoms in others that seems to kind of put us in touch with that kind of sensation in ourselves,” said Blaine Ditto, a McGill University psychology professor who has studied how much a fear of blood predisposes donors to passing out.
How to prevent fainting at the sight of blood
Turning away or sitting down when you or someone you know gets a shot is perhaps the easiest way to avoid fainting. Repeated exposure will often lessen symptoms.
Repeated exposure will often lessen symptoms.
When that doesn’t work, try a technique called “applied tension”: squeeze the muscles in your arms, legs and torso before seeing something that is likely to make you woozy. This raises your blood pressure before exposure and can help prevent you from getting woozy.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
SYNCOPAL CONDITIONS OR, SIMPLY SPEAKING, FAINS
Honored Worker of Science of Russia, professor of neuropathology Konstantin Grigoryevich Umansky headed the clinical department of the Institute of Poliomyelitis and Viral Encephalitis of the Russian Academy of Medical Sciences. his articles in Science and Life have always attracted interest, and the popular science book Neuropathology for All was a bestseller. Now Konstantin Grigorievich lives in Denver (USA). With his permission and the permission of the Weekly International West-East, we present to you a new article written just recently.
With his permission and the permission of the Weekly International West-East, we present to you a new article written just recently.
Science and life // Illustrations
Matthias Grunewald (1470-1530). "Mary's Fainting". Fragment of the altar of the Isenheim monastery in Germany.
‹
›
View full size
Fainting, in fact, is not a disease. These are temporary states that a person can fall into for a variety of reasons. That is why in modern medical literature they are referred to as syncope.
This name comes from the Greek word "syncope" (synkope) - in direct translation "chopping". The medical meaning of the term since ancient times means a deep swoon with loss of consciousness. It is interesting that it literally corresponds to the vulgar, often used in life Russian expressions - "passed out" or "passed out" when it comes to a person who suddenly lost consciousness.
Syncope (syncope) is usually called a sudden loss of consciousness, independent of the cause, most often of a short duration. Despite the apparent simplicity of this suffering and the relative, in most cases, ease of flow, its causes are quite complex and diverse.
Despite the apparent simplicity of this suffering and the relative, in most cases, ease of flow, its causes are quite complex and diverse.
...One day a young woman came to see me. Short, skinny. The features of the face are pointed, there are deep shadows under the eyes, the lips are somewhat cyanotic. He fumbles nervously in his purse, looking for directions. Works as a secretary-typist in a construction company. He talks about his illness with excitement, while his face and neck are covered with red spots.
- I have long been advised to consult a neurologist. Previously, she was treated by her district therapist. But he also said that all this was on my nerves.
When she calmed down a little, he asked to tell in more detail what was bothering her.
By nature, I am an easily excitable and impressionable person. I get nervous about every little thing both at home and at work. But that's not what worries me the most. Just do not believe it: just that - I immediately faint. Recently, we underwent medical examination, and they had to take blood from me. As soon as the laboratory assistant took up the needle, I lost consciousness. I can't stand one kind of blood, including someone else's. Recently, my son fell and cut his forehead a little - so here I lost consciousness ...
Recently, we underwent medical examination, and they had to take blood from me. As soon as the laboratory assistant took up the needle, I lost consciousness. I can't stand one kind of blood, including someone else's. Recently, my son fell and cut his forehead a little - so here I lost consciousness ...
These are quite typical complaints, they often have to be heard, as well as to observe the fainting spells themselves.
The main cause of such neurogenic syncope is constitutional, that is, congenital, features of the easily excitable nervous and autonomic systems, against the background of which sudden oxygen deficiency plays a decisive role.
As you know, all the activity of the body is regulated by the homeostasis system, which ensures the normal supply of all organs and systems of the body with the necessary products, primarily oxygen. This system constantly monitors and maintains all the basic parameters of the body's vital activity at the required level.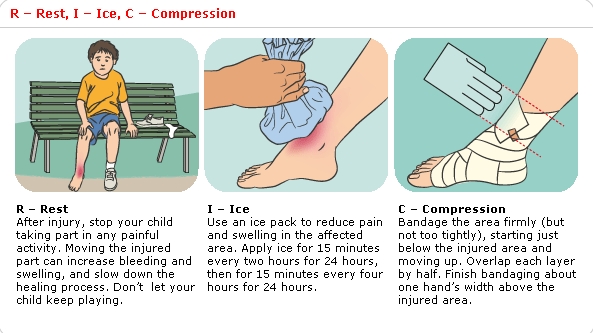 But sometimes, in extreme conditions, for various reasons, this system fails, and it cannot provide the central nervous system with oxygen in the right amount. Then there are fainting spells. This is usually characteristic of people suffering from vegetovascular dystonia (dysfunction of the autonomic nervous system). And it can be congenital, as in our patient, and then it is difficult to cope with it, especially when there is a hysterical mood of the nervous system, although it is usually possible to mitigate its manifestations. But such dystonia can also be the result of injuries, infections, intoxications, dysfunction of the endocrine system, neurosis. In these and many other cases, treatment is more effective. Syncope is also not uncommon in people with heart disease.
But sometimes, in extreme conditions, for various reasons, this system fails, and it cannot provide the central nervous system with oxygen in the right amount. Then there are fainting spells. This is usually characteristic of people suffering from vegetovascular dystonia (dysfunction of the autonomic nervous system). And it can be congenital, as in our patient, and then it is difficult to cope with it, especially when there is a hysterical mood of the nervous system, although it is usually possible to mitigate its manifestations. But such dystonia can also be the result of injuries, infections, intoxications, dysfunction of the endocrine system, neurosis. In these and many other cases, treatment is more effective. Syncope is also not uncommon in people with heart disease.
The nervous mood of the nervous system, as they said earlier, or more simply - a tendency to hysterical reactions, in some cases can be combined with the so-called Freudian complexes. In this case, the causal mechanism of fainting is the same as described above.
I don’t know if the founder of psychoanalysis, Sigmund Freud, and the famous Russian writer Viktor Viktorovich Smidovich, who is better known to all of us under the pseudonym Veresaev, knew each other, who lived at the same time, but both seemed to observe the same patient. It is described by Veresaev in the Notes of a Doctor.
This woman of Balzac's age very often, from girlhood, saw almost real passionate erotic dreams, in which nude men were not inactive. In real life, at the sight of a naked man, she suddenly fainted. Later, fainting set in even at the sight of only one men's underpants. Neither psychoanalysis nor the famous doctor Smidovich helped. She remained an old maid, although in dreams, as in constant erotic fantasies, everything remained the same.
The immediate cause for any neurogenic syncope can be stress, excitement, overheating, being in a stuffy room, fright, etc. In people suffering from various kinds of neurosis, fainting most often occurs reflexively - in response to such “starting” moments, such as, for example, the sight of blood, or as a reaction to even small painful stimuli or their foreseeing - just the sight of a medical needle is enough.
In addition to the neurogenic syncope described above, there are often those that have, so to speak, somatogenic origin. That is, due to any violations of the internal environment of the body and its reactivity due to certain diseases.
In the fiction of the nineteenth century, among many classics, as well as in the medical literature of that time, you can very often find descriptions of fainting, which then occurred much more often than in our time. Mostly in the "noble environment", more in young girls, starting from puberty. Both in medical literature and in fiction, they were considered a manifestation of "chlorosis". Obviously, by the pale greenish skin tone that distinguishes them. "Chlorosis" is a Greek word (chloros), in direct translation - "greenish". Only by the end of the 19th - beginning of the 20th century, when they began to study the biochemistry of blood, it turned out that chlorosis is a manifestation of iron deficiency anemia. And then ... Maybe it was then that the original Russian expression appeared - "pale sickness."
Maybe it was then that the original Russian expression appeared - "pale sickness."
At that time, “wasp” waists were in fashion, to achieve which a strict diet was required (at that time, almost hungry). And to use a waist simulator - a corset, a not too full figure was also needed. In addition, you don’t really eat in it.
By the way, often some modern “fashionable” amateur diets, among them many published ones, can just as well lead to similar consequences, and sometimes to much worse ones.
Of course, anemia was only a background against which the physiological disturbances common to all fainting states developed extremely easily.
Such fainting is often observed in people with cardiovascular and respiratory failure, with a sharp decrease in blood sugar in diabetics, and in the presence of many other reasons.
It is not uncommon for heavy smokers to faint when they already have chronic lung diseases that lead to constant venous congestion and easily appearing oxygen deficiency during coughing - at this moment a sudden loss of consciousness can occur.
In some people, fainting may occur when moving from a horizontal to a vertical position too quickly, when throwing the head back sharply (for example, in a barber's chair).
There are also extreme syncope due to profound metabolic disorders (metabolic processes) of the brain. They arise as a result of extraordinary external influences that exceed the physiological possibilities of adaptation to them. The decisive factor in their occurrence belongs to a significant lack of oxygen in the inhaled air. For example, with high-altitude, or, as it is also called, mountain, illness in climbers. Similar conditions can also occur with the neurotoxic effect of certain poisons, side effects of drugs, etc. There are also multifactorial syncope, in the occurrence of which several factors can be blamed at once.
Fainting does not always occur unexpectedly. Much more often it is preceded by rapidly growing unpleasant sensations in the form of nausea, nausea, flashing before the eyes, ringing in the ears. All this is accompanied by general weakness, sometimes yawning. Often the skin acquires a pale shade, sweating may appear. Then, at some point, muscle relaxation occurs, the legs give way, and the patient falls, losing consciousness. During fainting, the patient's body is motionless, contact with it is impossible, the muscles are relaxed, the pulse is usually rare (rarely rapid), of weak filling. Blood pressure drops, breathing becomes shallow. The pupils are often narrowed, but in some cases they can be dilated. In this state, a person almost does not respond to injections. With prolonged fainting and, therefore, prolonged oxygen deficiency, convulsions may even begin, somewhat similar in some cases to epileptic ones. Syncope almost always develops in people who are sitting, standing, or walking. As a rule, this does not happen with those lying down.
All this is accompanied by general weakness, sometimes yawning. Often the skin acquires a pale shade, sweating may appear. Then, at some point, muscle relaxation occurs, the legs give way, and the patient falls, losing consciousness. During fainting, the patient's body is motionless, contact with it is impossible, the muscles are relaxed, the pulse is usually rare (rarely rapid), of weak filling. Blood pressure drops, breathing becomes shallow. The pupils are often narrowed, but in some cases they can be dilated. In this state, a person almost does not respond to injections. With prolonged fainting and, therefore, prolonged oxygen deficiency, convulsions may even begin, somewhat similar in some cases to epileptic ones. Syncope almost always develops in people who are sitting, standing, or walking. As a rule, this does not happen with those lying down.
In almost all cases, the onset of syncope has a fairly general clinical picture. True, sometimes fainting can come suddenly, as if without visible precursors.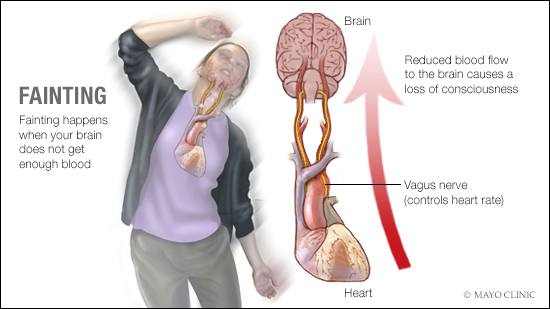 The outcome of fainting, as well as the way out of this state, proceed in different ways, depending on the cause of the occurrence.
The outcome of fainting, as well as the way out of this state, proceed in different ways, depending on the cause of the occurrence.
However, not every sudden loss of consciousness that occurs with the same signs is a true syncope. A person gets into the same state, for example, with hypoglycemia - a significant decrease in blood sugar levels. Then the patient needs the immediate help of medical specialists. Therefore, to any person who suddenly lost consciousness, it is necessary to urgently call a doctor, except, obviously, in those cases when it is reliably (from the doctor) known that we are talking about fainting. For example, when similar conditions are repeated in the same person.
Well, if in your presence a person fainted, then how to help him until the doctor arrived?
First, you must immediately lay it down so that the head is located below the body, the legs are raised - this will improve the blood supply to the brain. Open windows in the room immediately. Relax everything that tightens the neck, chest, stomach. If there is ammonia, give it a sniff, but only so that it does not get on the mucous membranes of the nose, lips, eyes, otherwise you can cause a burn. Spray your face with cold water. Rub the skin of the temples and chest with a dry towel or moistened with cologne, you can also cool water. Apply heating pads to the limbs. In one of the old manuals, I read the following recommendation: cut the onion in half, rub the whiskey in places of the cut and let it smell. Obviously, this can also give a good effect. But always, in all cases, if the patient does not regain consciousness within a few minutes, you must immediately call an ambulance.
Relax everything that tightens the neck, chest, stomach. If there is ammonia, give it a sniff, but only so that it does not get on the mucous membranes of the nose, lips, eyes, otherwise you can cause a burn. Spray your face with cold water. Rub the skin of the temples and chest with a dry towel or moistened with cologne, you can also cool water. Apply heating pads to the limbs. In one of the old manuals, I read the following recommendation: cut the onion in half, rub the whiskey in places of the cut and let it smell. Obviously, this can also give a good effect. But always, in all cases, if the patient does not regain consciousness within a few minutes, you must immediately call an ambulance.
It should be remembered that fainting is most often a sign of trouble in the body, a consequence of some disease from which the nervous system also suffers. However, despite the many prerequisites that may contribute to the onset of fainting, one should
to say that most people are not at all predisposed to fainting. This largely depends on the type of nervous system, stability and stability of internal processes, even in the presence of any chronic diseases.
This largely depends on the type of nervous system, stability and stability of internal processes, even in the presence of any chronic diseases.
Needlephobia. How to overcome fear?
After a few months of practicing blood sampling, every health worker will encounter a patient who, at the sight of a needle, will have a paralyzing fear. According to Dr. James Hamilton, a family physician in Durham, North Carolina, who is the world's leading specialist in needle phobia, 20% of the population is affected by this fear. It is believed that there is a genetic predisposition to needle phobia. Experts have calculated that 80% of needlephobes have a close relative (parent, child, or sibling) with needlephobia. Most of them avoid medical institutions.
Needlephobia experts urge health care providers who draw blood to recognize signs of paranoia about needles and conduct the procedure in a manner that minimizes trauma from the procedure. Such patients are usually extremely wary of venipuncture and other needle procedures. Children who are afraid of needles resist physically, crying, screaming and doing everything they can to avoid the procedure. When a patient appears with a particularly pronounced anxiety, the health worker must realize that he is facing a person with acupuncture and take measures so that this fear does not become lifelong. These measures include:
Children who are afraid of needles resist physically, crying, screaming and doing everything they can to avoid the procedure. When a patient appears with a particularly pronounced anxiety, the health worker must realize that he is facing a person with acupuncture and take measures so that this fear does not become lifelong. These measures include:
Applying an ice pack to the puncture site to prevent the patient from developing a shock reaction.
The use of iontophoresis.
The use of sedatives.
Use of local anesthesia.
· Demonstration of the deepest complicity, patience and understanding towards the patient.
Rejection of physical restraints as a substitute for a compassionate patient approach.
Symptoms of a shock reaction that occurs in patients with acupuncture during needle procedures include fainting, lightheadedness, dizziness at the sight of the needle, pallor, profuse sweating, and nausea. Patients with needle phobia often go into shock during or immediately after the procedure and develop arrhythmia and even cardiac arrest. At least 23 deaths due to needle phobia have been described.
At least 23 deaths due to needle phobia have been described.
According to Dr. Hamilton, the easiest and fastest way to prevent a shock reaction is to lay the patient down with their legs up and place an ice pack or ice cubes wrapped in a wet diaper on the arm 10 to 15 minutes before the venipuncture. In this case, the hand becomes numb, and the shock reaction does not start. Some patients with needle phobia prefer to take sedatives or sedatives about half an hour before donating blood. You can also apply a special cream, a local anesthetic, to the puncture site. However, it has a limited penetration depth and must be applied at least 1 hour before the procedure. The use of drugs should be documented and the results should be noted as such.
One of the most promising treatments for needle phobia is iontophoresis. Iontophoresis involves the application of a cotton pad soaked in lidocaine and passing a weak electric current through it for 10-15 minutes. Lidocaine completely anesthetizes the venipuncture site down to the bone tissue for at least 1 hour.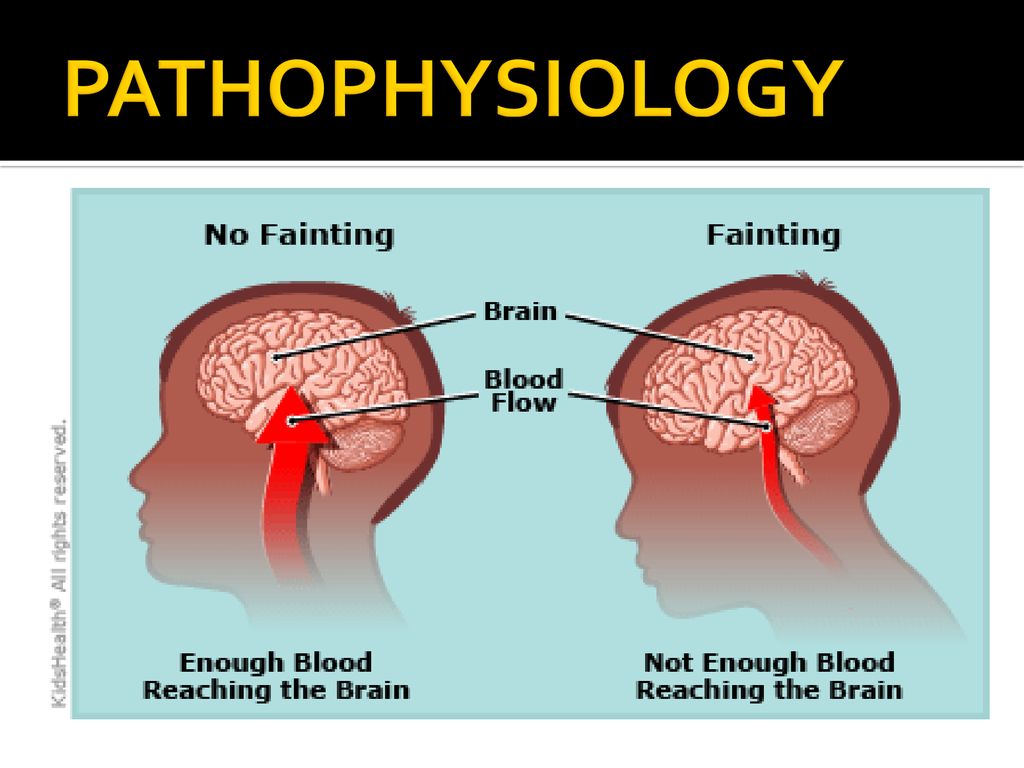
Needlephobia experts agree that healthcare professionals should approach patients with signs of fear of needles with compassion and empathy. They advise asking a few simple questions. Instead of asking bluntly, “Are you scared of needles?” ask questions like:
1. Have you ever donated blood? Did you have injections? Did you have any problems with this?
2. Would you like me to hide the needle or have everything visible and I explain to you what I'm going to do before I do it?
3. How can I make you feel comfortable during the procedure?
Taking steps to minimize the stress of venipuncture is the key to healing a patient from a lifelong fear of needles and avoidance of medical attention.
Avoiding a shock reaction during invasive procedures in those who are predisposed to them, allows the right approach. Recognizing these people and taking steps to minimize the stress of venipuncture is the key to healing a patient from a lifelong fear of needles and avoiding medical attention. A health worker who recognizes needlephobes, takes preventive action, and shows empathy personally contributes not only to alleviating pain and anxiety during venipuncture, but also to prolonging the life of the patient.
A health worker who recognizes needlephobes, takes preventive action, and shows empathy personally contributes not only to alleviating pain and anxiety during venipuncture, but also to prolonging the life of the patient.
Here are some tips that can help health care providers prevent their patients from developing needlephobia:
Make it a rule to identify those children who are undergoing an invasive procedure for the first time. Suggest that physicians, especially pediatricians, ask their patients if this is their first time donating blood and notify the lab before the patient arrives.
Find out if the family history of needle phobia in the parents is not aggravated.
Ask the parents if the child has a pronounced reaction to pain stimuli.
Find out if the child has ever fainted from fright or for some unknown reason.
· If during the first contact with the needle/blood a vegetovascular reaction is suspected or stated, all subsequent procedures with needles should be performed with the deepest sympathy and understanding, using preventive measures.
· Those who are predisposed to acupuncture and come to the first procedure in their life should gain a painless experience. In such a situation, the prophylactic use of local anesthesia or iontophoresis with lidocaine is justified. When deciding whether to withdraw anesthesia and when to do so, be guided by the patient's reactions.
· The provider should not practice negative emotional restraint, ridicule, or punishment for resisting a fearful and painful procedure. Treat the cause of the resistance, not the resistance itself.
· A child should not be physically restrained or otherwise forced to undergo any procedure involving needles, such as drawing blood, unless it is necessary to save a life, limb or health in the future. Even mandatory procedures should not be forced to be performed on children, with the possible exception of mentally ill or too young children who are not actually aware of what is happening. When the procedure is required for a very small or mentally unwell patient, the use of drugs (pharmacological limitation) may be the best approach.
The health worker must be completely honest with parents and patients. There is no room for untruth, even if the intentions are the best. Painful procedures should not be described as painless. If the patient experiences pain after being told that it will not hurt, he feels confused, loses self-confidence, and eventually becomes angry and distrustful. Many needlephobes relate their lifelong distrust of health care workers to their betrayal of trust in childhood. Even expressions such as "you may feel a little pressure" should be avoided. Pressure and pain are two different things, don't confuse them. In not wanting to add to the discomfort, remember that it is much easier to hurt a child with half-truths or untruths than by being honest about the procedure.
· If the child is too young to understand, make an effort to make the invasive procedure as painless and calm as possible until the child is old enough to be aware of what is happening. The path of emotional support is long.