Complex trauma stress disorder
What Is Complex PTSD? The Symptoms Caused By Chronic Trauma
Written by WebMD Editorial Contributors
Medically Reviewed by Dan Brennan, MD on April 12, 2021
In this Article
- Symptoms of PTSD
- What Is Complex PTSD?
- Risk Factors for Complex PTSD
- Conditions Similar to Complex PTSD
- Treatment for Complex PTSD
You may have heard of post-traumatic stress syndrome or PTSD, but you may not be familiar with complex PTSD, sometimes known as c-PTSD. Complex PTSD is caused by prolonged or chronic trauma. Those with complex PTSD usually have at least some of the symptoms of PTSD, but they could also have other symptoms.
Most people experience at least one traumatic event during their lives, and about a fourth go on to develop PTSD. No one knows how many people have complex PTSD.
Symptoms of PTSD
People who experience trauma may feel its effects for days. If the symptoms last weeks or longer, and if they disrupt your life, you may have PTSD. See a trained mental health professional if you're worried that you might have PTSD.
Symptoms of PTSD usually fall into three categories.
Re-experiencing symptoms. Flashbacks and nightmares are probably the best-known PTSD symptoms. Memories of the trauma may trigger powerful emotions. The person may relive the sights, smells, and sounds of the traumatic event.
Sense-of-threat symptoms. Those with PTSD often feel that they must be on their guard. They may be hypervigilant (over aware of their surroundings), jumpy, and easily startled.
Avoidance symptoms. Those with PTSD spend a lot of energy avoiding triggers — people, places, or situations that remind them of the trauma they experienced. They may self-medicate with drugs or alcohol.
What Is Complex PTSD?
Besides the symptoms of PTSD, those with complex PTSD may also have other symptoms.
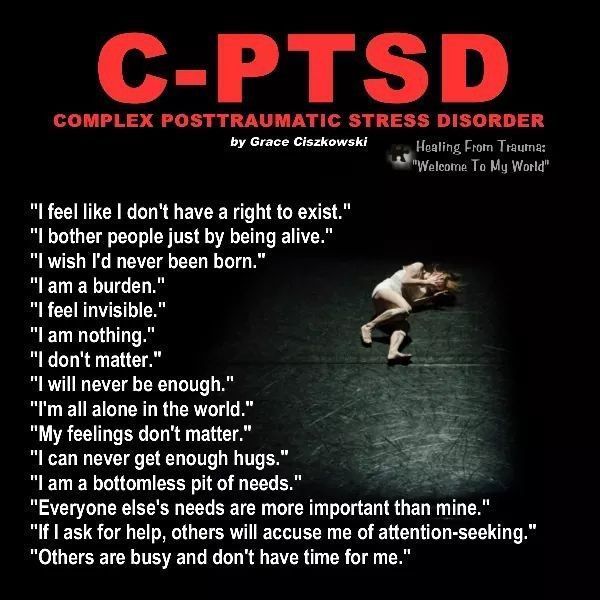
Problems with self-esteem.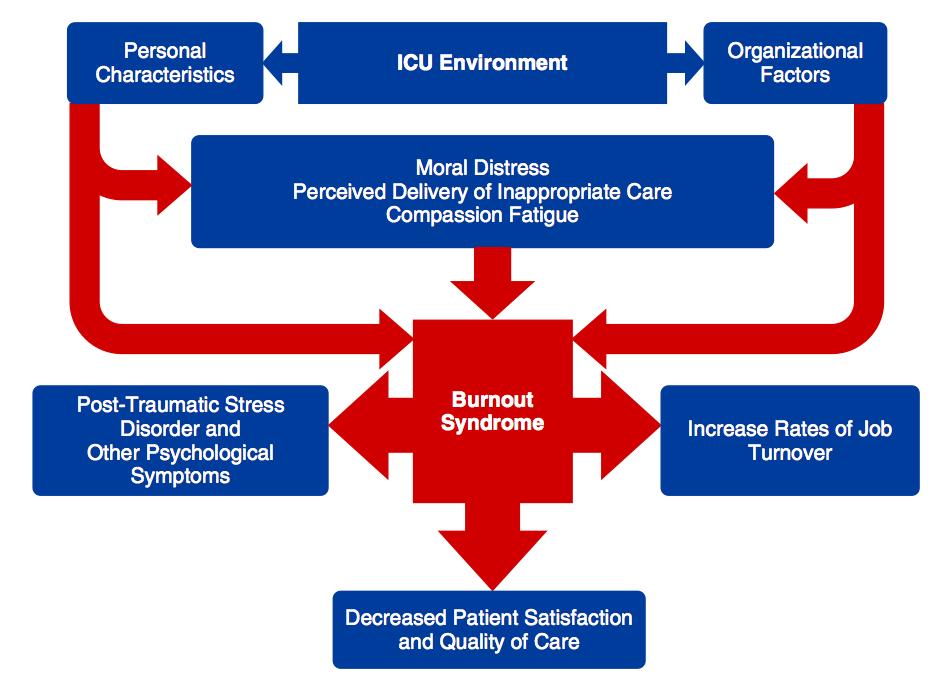 Those with complex PTSD may feel worthless or blame themselves for their trauma. They may believe bad things happen because of something in them.
Those with complex PTSD may feel worthless or blame themselves for their trauma. They may believe bad things happen because of something in them.
Emotional dysfunction. Those with complex PTSD often experience intense emotions, which are sometimes inappropriate. Besides anger and sadness, they may feel like they're living in a dream. They may have trouble feeling happy.
Relationship problems. Complex PTSD can make it difficult to trust others. Some people stay in unhealthy relationships because the situation is familiar. If their trauma involved abuse, their feelings about their abuser may be complicated. Or they may obsess about their abuser or focus on revenge.
Risk Factors for Complex PTSD
Originally used to describe the results of childhood trauma, complex PTSD now includes other kinds of chronic trauma.
- Childhood abuse or neglect
- Long-standing domestic violence
- Trafficked or forced into sex work
- Kidnapped, enslaved, or tortured
- Incarcerated in a prisoner of war camp
- Witnesses to repeated acts of violence
There are also additional risk factors for complex PTSD.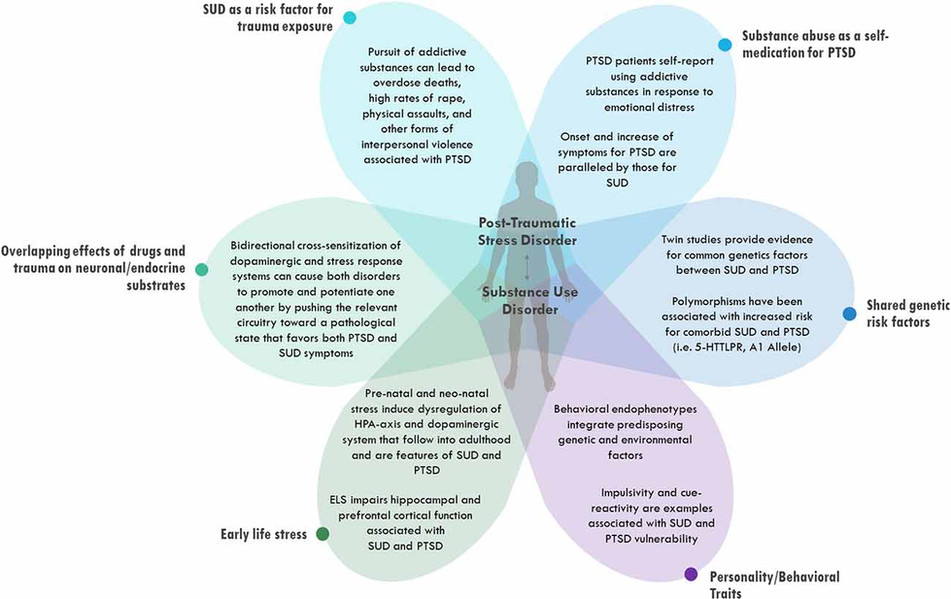
- Multiple traumas
- Trauma from an early age
- Long-term trauma
- Abuse by a close family member or friend
- Not having a hope for change when trapped
Conditions Similar to Complex PTSD
A Harvard researcher coined the term "complex PTSD" in 1988. Mental health professionals today may use other terms.
Enduring Personality Changes After Catastrophic Events (EPCACE). To have a diagnosis of EPCACE, the person needs to have a personality change that lasts for 2 years after trauma. EPCACE is no longer recognized by the World Health Organization, which uses complex PTSD instead. Some mental health professionals prefer EPCACE and still use it.
Disorders of Extreme Stress Not Otherwise Specified (DESNOS). This term sometimes is used to mean the same thing as complex PTSD, especially in the United States. The risk factors and symptoms are very similar.
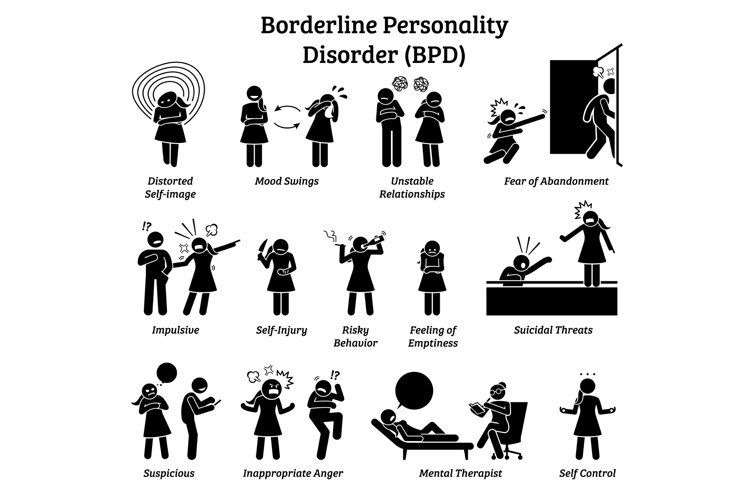
Borderline Personality Disorder (BPD).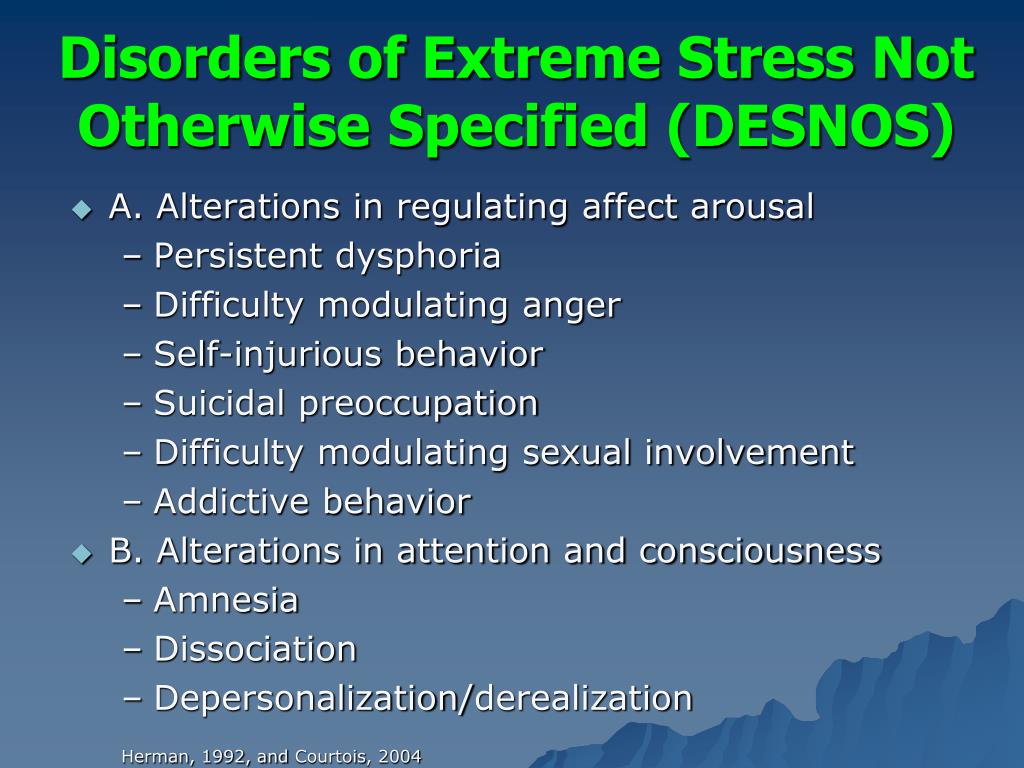 The symptoms of complex PTSD and BPD are similar, but BPD does not require a history of trauma. Some researchers believe that genetics or brain function could be at the root of BPD. Some authorities consider complex PTSD a subtype of BPD, but others believe they're two separate conditions.
The symptoms of complex PTSD and BPD are similar, but BPD does not require a history of trauma. Some researchers believe that genetics or brain function could be at the root of BPD. Some authorities consider complex PTSD a subtype of BPD, but others believe they're two separate conditions.
Treatment for Complex PTSD
Because complex PTSD is a relatively new diagnosis, mental health professionals are still working on treatment options. There are still some options that may help.
- Talk therapy to help process the trauma
- Medication such as antidepressants and anti-anxiety medications
- Exposure therapy in which subjects face their memories in a safe space
- Cognitive Behavior Therapy (CBT), which addresses thought patterns
Some therapists use a relatively new therapy called eye movement desensitization and reprocessing (EMDR). It may be helpful for complex PTSD too. In EMDR, the subject remembers a trauma while following a bilateral stimulus (one that switches from one side of the body to the other) that leads to a back-and-forth eye movement. The stimulus could be one they see such as a finger moving back and forth or a sound. EMDR is effective for PTSD, but experts debate if the bilateral stimulation is really important or if the process could happen without it.
The stimulus could be one they see such as a finger moving back and forth or a sound. EMDR is effective for PTSD, but experts debate if the bilateral stimulation is really important or if the process could happen without it.
What is Complex Post-Traumatic Stress Disorder, (CPTSD)?
Complex Post-Traumatic Stress Disorder (CPTSD, C-PTSD, Complex PTSD) describes the results of ongoing, inescapable, relational trauma. Unlike Post-Traumatic Stress Disorder (PTSD), Complex PTSD typically involves being hurt by another person. These hurts are ongoing, repeated, and often involving a betrayal and loss of safety.
PTSD (Post-Traumatic Stress Disorder) is often associated with a one-time experience or a single-incident trauma.
It is estimated that 70% of adults or 223.4 million people in the United States have experienced at least one form of trauma in their lifetime, as reported by the National Council for Behavioral Health (NCBH) in 2013. In addition, 90% of childhood sexual abuse victims, 33% of children exposed to community violence, and 77% of children exposed to school shootings develop Post Traumatic Stress Disorder (NCBH).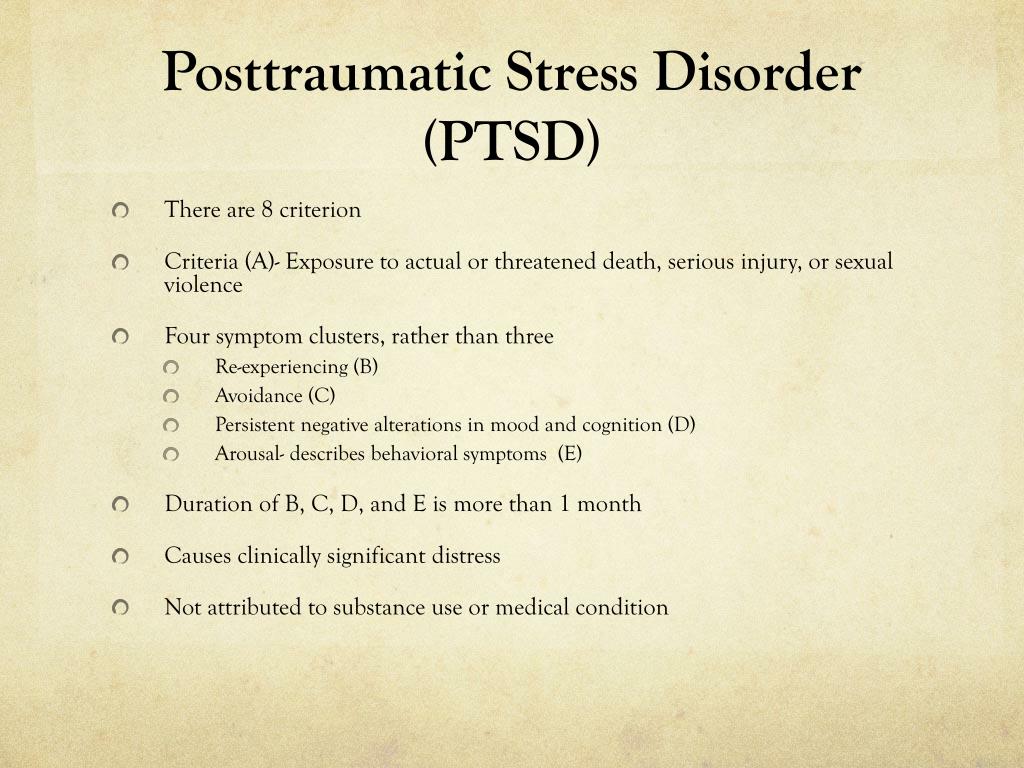
Humans require safe people, safe places, and safe things during childhood and adolescence in order for healthy brain development to take place. Many adult survivors of complex trauma, having experienced this loss of safety, had no agency over themselves or their environment during critical times in brain development for extended periods of time. This loss of agency during their early years stunted their growth, depriving them of the opportunity to create the lives they deserved, and has ultimately left many stripped of their sense of worth and sense of self. Without the ability to understand what has happened, young survivors grow up to be adults who live in the same constant state of hypervigilance and suffering, even after escaping physical danger.
Adult survivors of complex trauma often experience amnesia, alienation, chronic mistrust, chronic physical pain, re-victimization, debilitating flashbacks, nightmares, body memories, anxiety, dissociation, trouble with regulating volatile emotions, severe depression, toxic shame, auto-immune disease, along with other deeply distressing and potentially life-altering symptoms.
In addition to the mental and emotional effects of CPTSD, the Adverse Childhood Experiences study shows that individuals who experience higher levels of childhood trauma have increased risks for additional health problems. These include Coronary Heart Disease (13%) and COPD (27%), as well as increased risk for health risk behaviors such as smoking (33%) and heavy drinking (24%).
The severe impact of these aftereffects causes many adult survivors to isolate as a means of coping with their overwhelming feelings of unsafety. The isolation meant to keep them safe often leads to despair and suicidality, which increases the possibility of inadvertently modeling these dangerous behaviors and coping strategies for their own children, thereby creating intergenerational cycles of trauma.
Healing CPTSD requires creating some new daily habits. These new daily habits afford adult survivors the profoundly empowering opportunity to reclaim their sense of agency, and sense of self worth. Once equipped, they can day-by-day create their new lives, and look forward to their future, ultimately resulting in the prevention of complex relational trauma, leaving a legacy of healing for future generations.
Once equipped, they can day-by-day create their new lives, and look forward to their future, ultimately resulting in the prevention of complex relational trauma, leaving a legacy of healing for future generations.
Here, at CPTSD Foundation, we are helping to end the cycles of complex relational trauma by providing the safety, life skills, relational education, and reparative experiences needed to create new daily habits, improving every area of life.
Key Differences between PTSD and CPTSD – written by friend of our organization, respected clinician, and guest on the annual We Are Healing Trauma Virtual Summit – Robyn Brickel, MA, LMFT.
Post-traumatic stress disorder (PTSD) | English translation
However, most people realize what happened after a few weeks, sometimes a little longer, and then their symptoms will begin to disappear.
Research shows that certain groups of people are at increased risk of developing post-traumatic stress disorder. The risk of developing PTSD is reduced when a person has:
The risk of developing PTSD is reduced when a person has:
Any traumatic event can cause PTSD, although the more severe the shock, the more likely it is to develop PTSD. For example, PTSD is more likely to develop if the event:
- is a sudden and unexpected
- lasts a long time
- , it happens when you get into a trap from which
- could not get out of
- deaths
- leads to injuries
- include children
if you are still stressed and in an uncertain state, this will make it difficult to get rid of the symptoms of PTSD.
How do I know that I have overcome a traumatic experience?
You may have already gotten over the traumatic event if you can:
- think about it without worrying
- not feel like you are under constant threat
- not think about it all the time
Why is PTSD not always diagnosed?
There are a number of reasons why a person with PTSD may not be diagnosed.
Stigma and misunderstanding
People with PTSD often avoid talking about their feelings to avoid thinking about the traumatic event.
Some people believe that the symptoms they are experiencing (such as avoidance or emotional numbness) help them cope and do not realize that they are caused by PTSD.
When people are very ill, it is difficult for them to believe that they are able to feel the way they did before the traumatic event. This may discourage them from getting help.
There is also a common misconception that only military personnel suffer from PTSD. In fact, PTSD can happen to anyone, and any experience of PTSD is real.
Misdiagnosis
Some people with PTSD may be misdiagnosed with conditions such as anxiety or depression. Some people have other mental and physical health problems that make PTSD go unnoticed.
They may also experience medically unexplained symptoms such as:
- gastrointestinal disorders
- pain syndromes
- headaches
These symptoms may mean that their PTSD goes unnoticed.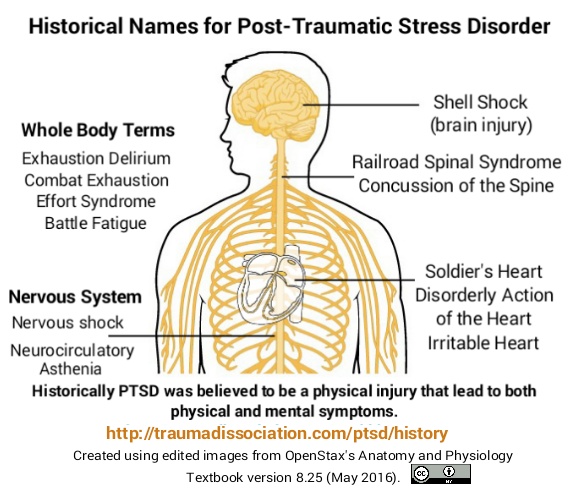
Other difficulties
Some people with PTSD may also have other problems, such as difficulties in human relationships or addiction to alcohol and drugs. They may be caused by post-traumatic stress disorder, but these problems will manifest themselves more clearly than PTSD itself.
Can children develop PTSD?
PTSD can develop at any age. In addition to the symptoms of PTSD common to adults, children may also experience:
- Nightmares - In children, these dreams may or may not reflect an actual traumatic event.
- Repetitive play - some children act out a traumatic event during play. For example, a child who has been in a serious traffic accident may recreate the accident with toy cars.
- Physical symptoms - they may complain of abdominal pain and headaches.
- Fear of imminent death - they may find it hard to believe that they will live long enough to become adults.
What treatments are available for PTSD?
There are a number of different treatments for PTSD, including trauma-focused cognitive behavioral therapy (TF-CBT), eye movement desensitization and processing (EMDR), and medications.
Psychotherapy
Psychotherapy for PTSD will focus on the traumatic experience, not your past life. They will help you:
- Acceptance - learn to accept the fact that although you cannot change what happened, you can think differently about the event, the world around you and your life.
- Memory of the event - remembering what happened, you will not feel fear or anxiety. You will be able to think about what happened when you yourself want it, and not through obsessive thoughts or memories.
- Explaining your experiences in words - by saying out loud what happened, your mind can push the memories away and do other things.
- Finding a sense of security - helps you to better control your feelings. This will make you feel more secure and eliminate the need to avoid memories.
All psychotherapy must be administered by a properly trained and accredited professional. Sessions are usually conducted by the same therapist at least once a week, with a total duration of at least 8-12 weeks.
Sessions usually last about an hour, sometimes they can last up to 90 minutes.
Therapy for PTSD includes:
Trauma-focused Cognitive Behavioral Therapy
A form of talking therapy that can help you change the way you think. Over time, this can help you feel better and behave differently. It is usually done individually, although there is evidence that CBT for trauma can also be done in groups.
Eye Movement Desensitization and Reprocessing (EMDR)
A technique that uses eye movements to help the brain process traumatic memories.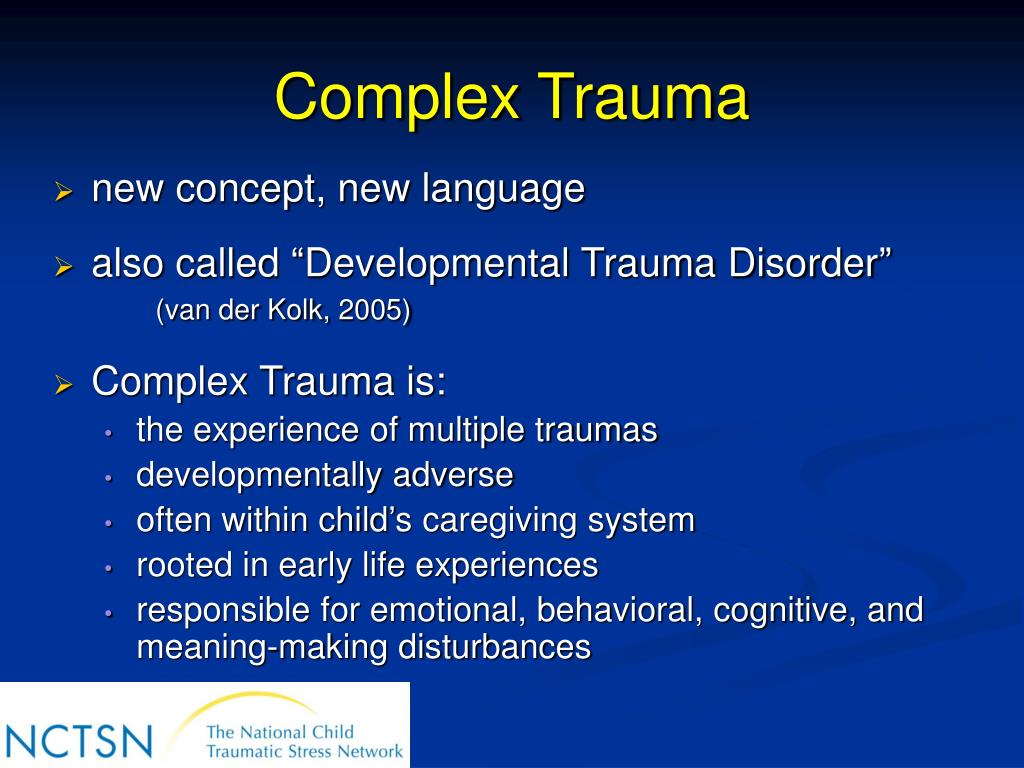
You will be asked to remember the traumatic event and what it made you think and feel. While you do this, you will be prompted to move your eyes or receive other "two-way stimulation" such as tapping your hand. It turns out that this reduces the emotional burden experienced in connection with the traumatic memory and helps to cope with the trauma.
The GERD must be carried out by a qualified person. EPDH usually requires 8-12 sessions, lasting from 60 to 90 minutes.
Some other forms of talking therapy may be useful for treating certain symptoms (eg, poor sleep) in people for whom EMRT or CBT have not been effective for trauma.
Medications
If you have tried various treatments for PTSD and find that they do not work for you, your doctor may prescribe antidepressants for you.
Selective serotonin reuptake inhibitors (SSRIs) are antidepressants that can help reduce symptoms of post-traumatic stress disorder. They can also help you if you are suffering from depression.
If SSRIs are not working for you, you may be offered other drugs, but this should usually be done on the advice of a mental health professional.
Which treatment is more effective?
There is evidence that Cognitive Behavioral Therapy for Trauma and Eye Movement Desensitization and Reprocessing are the best first line treatments. Medication can help those who refuse talking therapy or cannot easily access it.
Which treatment should I take first?
Trauma-focused psychological therapy (TF-CBT or EMBT) should be offered prior to medication, to the extent possible. This is in line with the UK National Institute for Health and Clinical Excellence (NICE) guidelines.
How can I help myself?
There are some things you can do to help you get better if you develop PTSD. Your therapist will help with this and make sure you apply them in a timely manner:
Stick to your daily routine - As far as possible, try to return to or maintain your normal daily routine.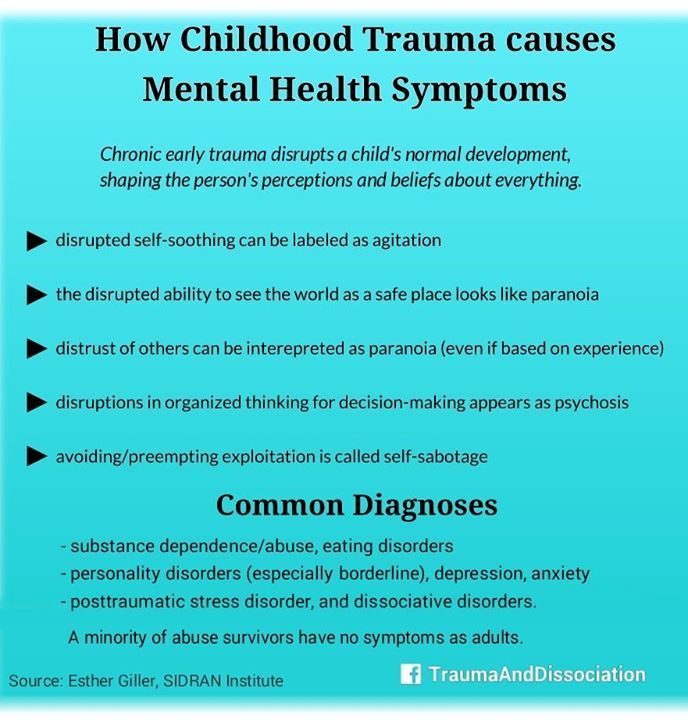 By continuing to lead a life as normal as possible, you can gain a sense of support.
By continuing to lead a life as normal as possible, you can gain a sense of support.
Talk to someone you trust - Although you shouldn't feel like you need to talk to everyone about what happened, talking to someone you trust can help you sort out your feelings in a safe environment. It can also help to talk to someone who has gone through the same thing as you, or someone who has gone through something similar before, as long as it doesn't hurt you.
Try relaxation exercises - Try self-meditation and other relaxation exercises. Relaxing with PTSD can be challenging, so talk to your therapist about exercises or activities that can help you.
Return to work or school - if you feel empowered, it can help you return to work, school or university by giving you a sense of routine. However, you should try to avoid situations in which you may be subjected to further injury or severe stress.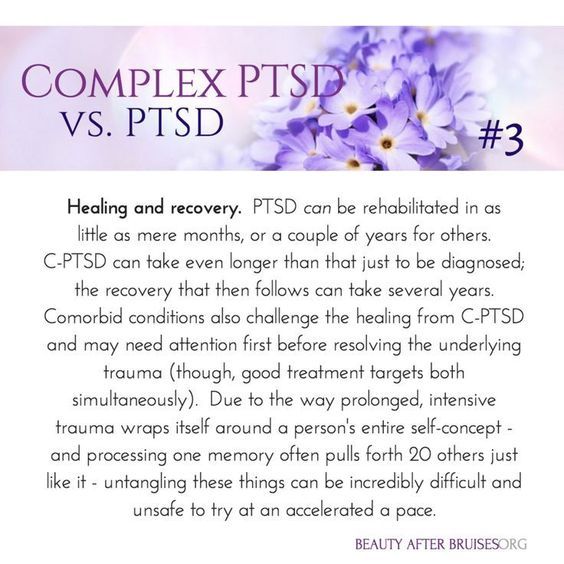 It is usually best to work in a supportive, low-stress environment before starting treatment.
It is usually best to work in a supportive, low-stress environment before starting treatment.
Eat and exercise regularly - Try to eat at regular times, even if you don't feel hungry. If you feel fit, try to exercise regularly. It can also help you feel tired before bed.
Spend time with others - Spending time with the people you care about will help you feel supported.
Expect to get better - Concentrating on thoughts that you will feel better over time will be useful for your recovery. Remember that you should not strain yourself in an attempt to recover faster.
Go back to where the traumatic event happened - If you feel you can do it, you may want to go back to where the traumatic event happened. Talk to your therapist or doctor if you are considering this so they can support you through this step.
There are also some things you should avoid while recovering.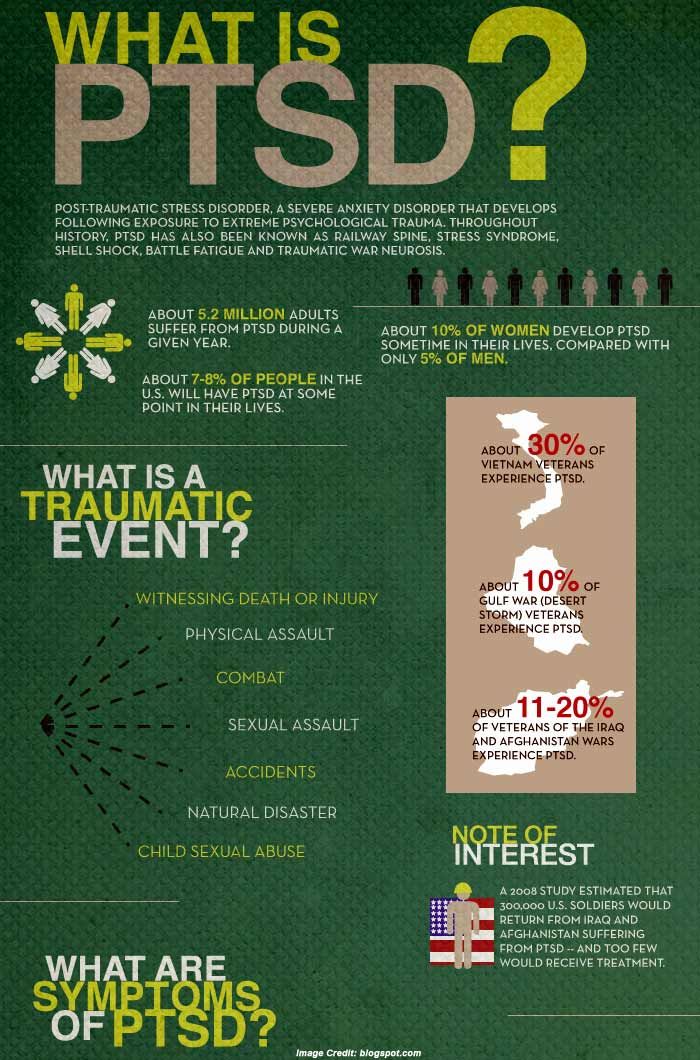 However, doing the "right things" can be very difficult, and you shouldn't feel guilty if you find yourself doing any of the following:
However, doing the "right things" can be very difficult, and you shouldn't feel guilty if you find yourself doing any of the following:
Self-criticism - PTSD symptoms are not a sign of weakness. This is a normal reaction to violent experiences.
Keep your feelings to yourself. If you have PTSD, don't feel guilty about sharing your thoughts and feelings with others. Talking about how you are feeling can help your recovery.
Expect things to get back to normal quickly - PTSD can take some time to heal. Try not to demand too much of yourself in a short amount of time.
Stay away from other people. Spending a lot of time alone can increase your sense of isolation and make you feel less well.
Drink alcohol or smoke. While alcohol can help you relax, and coffee and nicotine can act as stimulants, they can make you feel worse over time if you're experiencing symptoms associated with post-traumatic stress disorder.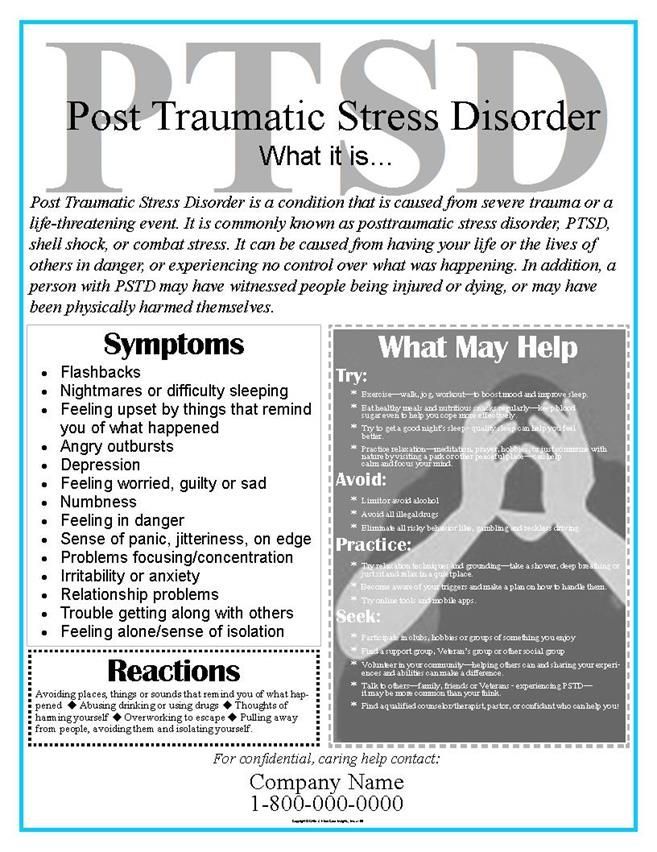
Overwork. Post-traumatic stress disorder can make it difficult to sleep, but as much as possible, try to stick to your regular sleep schedule and stay up late, as this can make you feel worse. You can learn more about good sleep in our resource.
Finally, you should be careful while driving. After a traumatic episode, people may have more accidents.
What is complex PTSD?
Some people develop complex post-traumatic stress disorder, caused by an experience or series of events that is extremely threatening or terrifying. These events can occur in childhood or adulthood.
Often such events are difficult or impossible to avoid. For example:
- torture
- slavery
- genocide
- living in war zones
- prolonged domestic violence
- repeated sexual and physical abuse
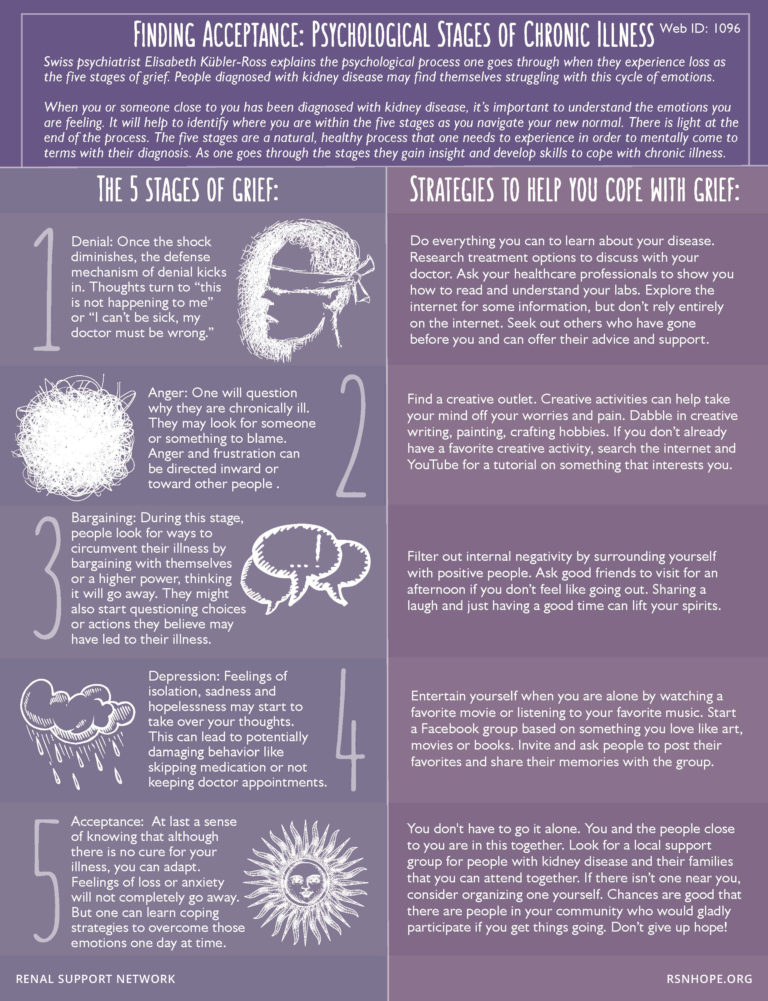
In addition to symptoms of post-traumatic stress disorder, people with complex post-traumatic stress disorder may also:
- emotions and emotional reactions
- have difficulty maintaining relationships and feelings of closeness with other people
How do I recover from complex PTSD?
People with complex post-traumatic stress disorder are characterized by a lack of trust in other people and in the world at large.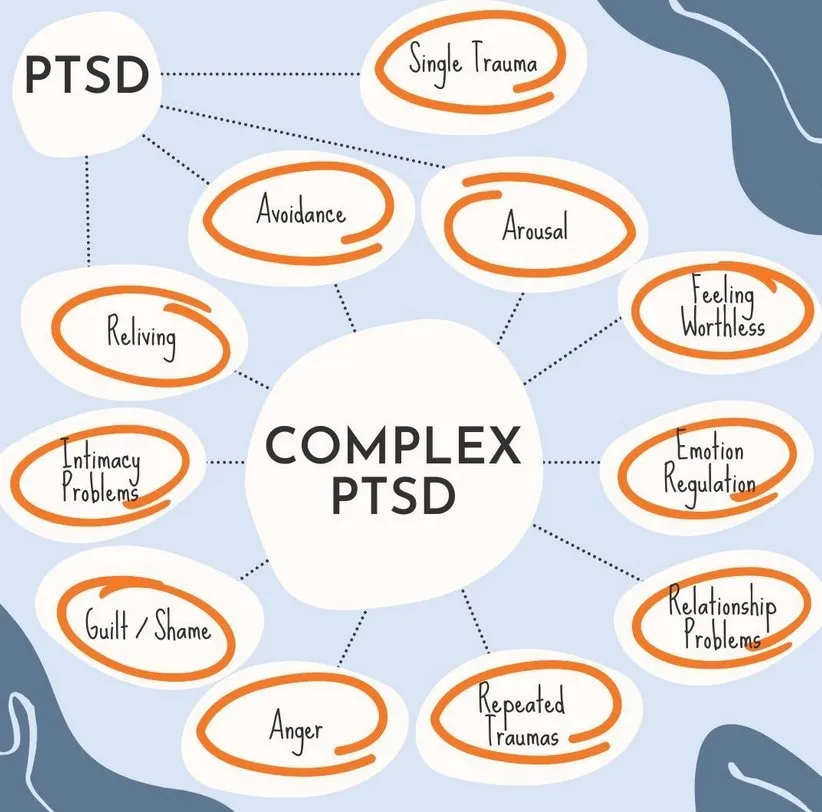
Emotional stabilization
During the stabilization phase, you will learn to trust your therapist and to understand and manage feelings of distress and alienation.
As part of stabilization, you can familiarize yourself with the work with supports - "grounding techniques". This can help you focus on familiar physical sensations and remind you that you are living in the present, not the past.
Stabilization can help you "unplug" your feelings of fear and anxiety from the memories and the emotions they evoke, helping to make those memories less frightening.
The goal of stabilization is so that you can eventually live your life free from anxiety or memories.
Sometimes stabilization may be the only help needed.
Trauma Focused Therapy
Trauma Focused Therapy, including EMDR (Eye Movement Desensitization and Processing) or Trauma Focused Cognitive Behavioral Therapy, can help you deal with traumatic experiences.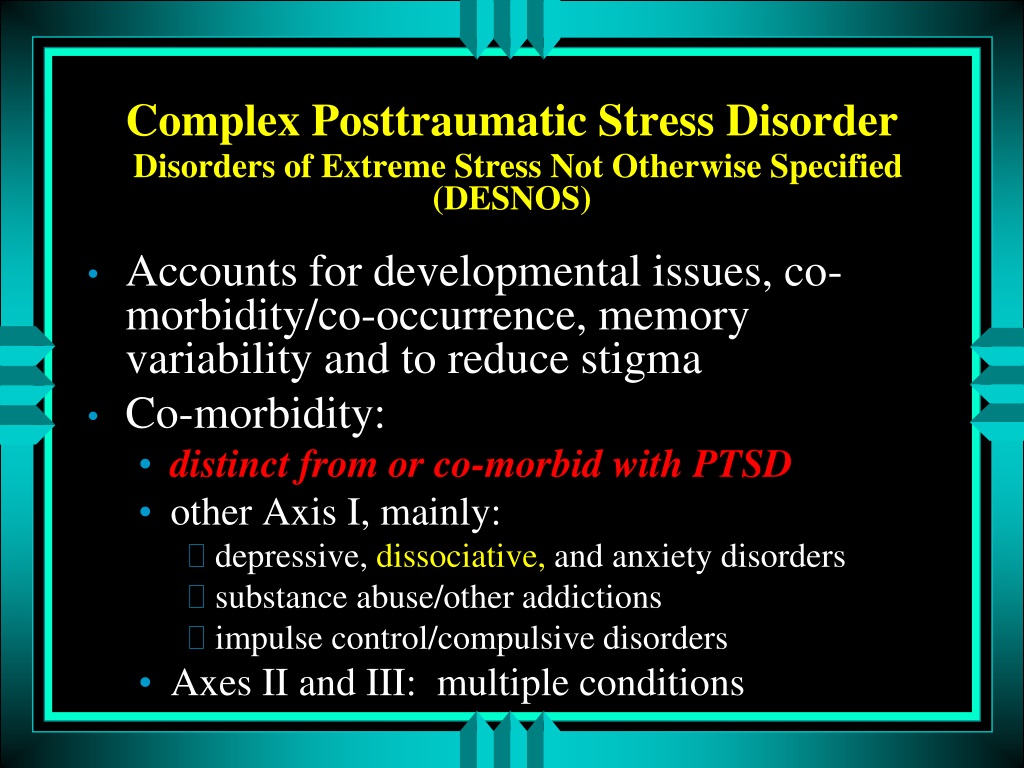 Other types of psychotherapy, including psychodynamic psychotherapy, may also be helpful. For complex post-traumatic stress disorder, care must be taken as these treatments can make things worse if not used properly.
Other types of psychotherapy, including psychodynamic psychotherapy, may also be helpful. For complex post-traumatic stress disorder, care must be taken as these treatments can make things worse if not used properly.
Reintegration and recovery
Reintegration into normal life can help you adjust to the real world at a time when you have emerged from the dangerous situation you were in before. This can help you begin to see yourself as a person with a choice.
Reintegration can help you:
- be compassionate towards yourself and others
- restore trust in yourself and others
- renew friendships, intimate relationships, and activities that promote your health and well-being
Medications
As with PTSD, antidepressants or other medications may be used along with psychotherapy. Medication may also be used if psychotherapy does not help or is not available to you. It would also be helpful to have a mental health professional help you oversee your medication.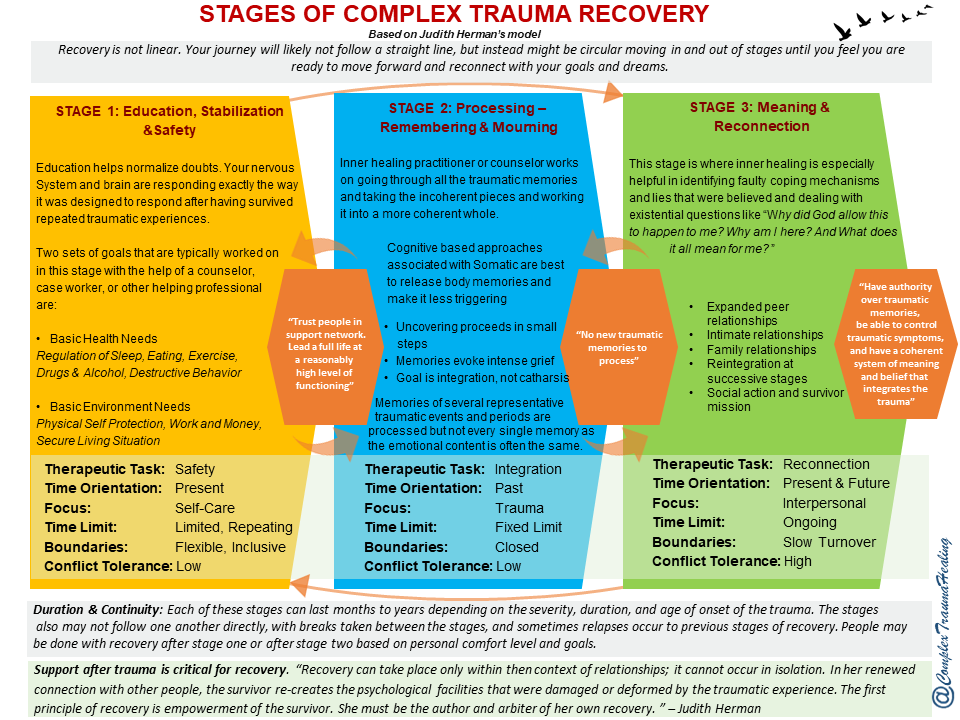
Self Help
If you develop complex PTSD, it may be helpful to try to do ordinary things that have nothing to do with your past traumatic experience. 9Ol000 . However, this can take time, and there is no need to be ashamed that at first these things will seem difficult to you or you will not be able to do them right away.
How do you know if someone has PTSD?
If you know someone who has just experienced a traumatic event, there are a few things you should be aware of. These moments can be signs that a person is not coping:
- Changes in behavior - low productivity at work, lateness, sick leave, minor accidents.
- Changes in emotions - anger, irritability, depression, lack of interest and lack of concentration.
- Changes in thought - preoccupation with threats or fears, negative outlook on the future
- Unexpected physical symptoms such as shortness of breath, nervousness or abdominal pain.
If you think a person may be showing signs of PTSD, you can suggest that they talk to their doctor. If you don't feel close enough to him for such a recommendation, talk to someone in his family or friends who could do it for you.
They may also find it helpful to refer to information about PTSD, such as this resource, to help identify the difficulties they face.
How can I help someone who has experienced a traumatic event?
For those who have experienced a traumatic event, the following actions may help:
- Be there - invite people to be with them. If they refuse, you can reassure them that you will be with them if they change their mind. Should not be imposed, but try to convince them to accept your help.
- Listen - try not to pressure people if they don't want something. If they want to talk, try to listen without interrupting or trying to share your own experience with them.
- Ask general questions - When you ask questions, try to keep them general and non-judgmental. For example, you might ask, "Have you talked about this with anyone else?" or “Can I help you find more help?”
- Offer real (practical) help - Some people may have difficulty taking care of themselves or doing daily activities. Offer help, such as cleaning the house or preparing meals;
Try not to tell people:
- That you know how they feel - even if you have experienced something like this, people experience situations differently. Comparing your experience with that of others is not always helpful;
- How lucky they are to be alive - people who have experienced traumatic events often don't think they are "lucky". Often they feel guilty about the fact that they survived while others died;
- Belittling the significance and seriousness of the experience - try not to tell people that things could be much worse, even if you do it out of good intentions and thereby try to help them.
 Such statements can make people feel that their experiences are not being taken seriously by others;
Such statements can make people feel that their experiences are not being taken seriously by others; - Giving inappropriate advice - Try not to give advice or suggestions, even if it has helped you in the past. All people are different and often they have already tried what you offer.
References:
This information was prepared by the Public Engagement Editorial Board of the Royal College of Psychiatrists (PEEB). It reflects the best available evidence at the time of writing.
Special thanks to PTSD UK for kindly providing feedback on this resource.
Expert Editor: Prof. Neil Greenberg
Full links to this resource are available upon request.
Translated by Elena Fage, senior intern psychiatrist
Translated by Elena Fage, Specialty doctor in CAMHS
PTSD - post-traumatic stress disorder
Initially, the term "post-traumatic stress disorder" appeared as a diagnosis in the military.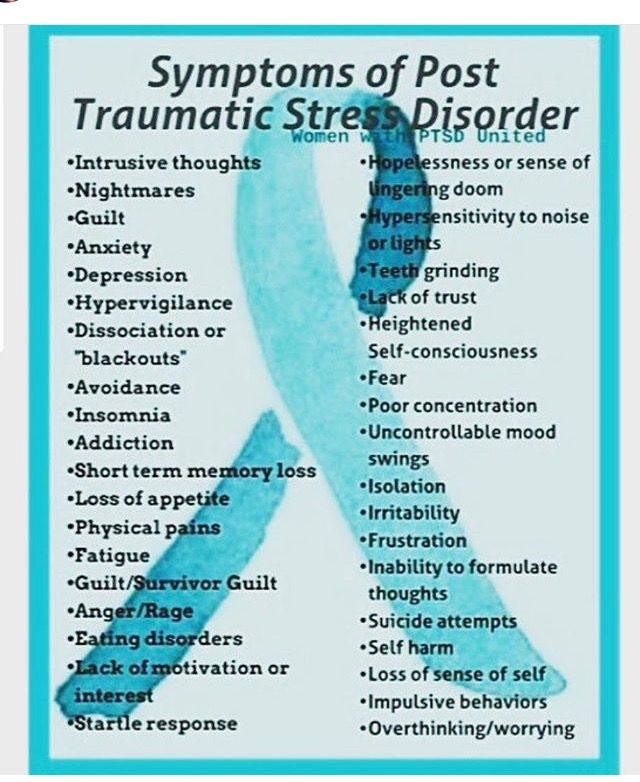 It happened during the Vietnam War. Then he firmly established himself in medical circles, and already at 1968 entered the ICD. But the disorder is actually very ancient - they learned to define it back in ancient Rome.
It happened during the Vietnam War. Then he firmly established himself in medical circles, and already at 1968 entered the ICD. But the disorder is actually very ancient - they learned to define it back in ancient Rome.
PTSD - what is it?
Complex post-traumatic stress disorder is a mental disorder that occurs in a person after some kind of traumatic impact. It was not for nothing that the violation was first diagnosed in the military - it was the military operations that caused PTSD. After the disease became generally accepted, the reasons for its appearance became more "domestic". And the range of causes that cause it has become more extensive. But, as before, the largest part of patients with this disorder are those who did military service.
Post-traumatic stress disorder, in simple words, is a disorder that appears after trauma of a very different nature. For example, after violence, disaster, death of a loved one. Any threat to life can lead to PTSD. Often the diagnosis is misused and applied to people whose symptoms are completely different from those confirmed by psychiatric researchers. Therefore, in recent years, the term has somewhat depreciated. But it is important to understand that the cause has always been and remains strong stress.
Therefore, in recent years, the term has somewhat depreciated. But it is important to understand that the cause has always been and remains strong stress.
According to the ICD, post-traumatic stress disorder always appears as an abandoned and prolonged reaction of the psyche to a stressful event. In this case, the event necessarily has the character of a threat or catastrophe. Here it is necessary to introduce the concept of distress, which is used as a counterweight to eustress - positive stress that does not bring the psyche out of balance. Distress, on the other hand, is always negative, destructive, and it is this that is applied to PTSD. It brings the nervous system out of a stable state, from which the whole organism suffers. The stronger the stress factor, the more likely it is that eustress will turn into distress.
It must always be remembered that PTSD, if not treated in time, can change the patient's personality and destroy his life, leaving an imprint on every area of it.
According to statistics, post-traumatic stress personality disorder is most common among women. Since the most common cause of violation is rape. In percentage terms, the data are as follows: PTSD affects 1.2% of women and 0.5% of men. But not always a stressful event can lead to PTSD. Firstly, not all people are susceptible to it, and secondly, in many cases it can be prevented.
Post-traumatic stress disorder in the ICD-10 is in the group "Neurotic, stress-related and somatoform disorders". Due to the unstable psyche, the disorder is most often diagnosed in the elderly and in children. Resistance to stress in these groups is much lower, and in older people it is also accompanied by a gradual loss of mental adaptation. Plus, the rigidity of mental processes increases.
PTSD needs to be examined comprehensively, so the observation is usually carried out by more than one specialized specialist. Among the areas of medicine that deal with the treatment of patients with post-traumatic stress disorder are psychiatry, psychotherapy and clinical psychology. Often the disorder is accompanied by depression, but it is also not uncommon for the patient to seek a way out of it with the help of chemical addictions. The disorder has relatively recently been recognized by the psychiatric community as a diagnosis in its own right. Therefore, the methods of treatment are still at the research stage. Experts often choose experimental methods, but it is still unclear whether they have high efficiency.
Often the disorder is accompanied by depression, but it is also not uncommon for the patient to seek a way out of it with the help of chemical addictions. The disorder has relatively recently been recognized by the psychiatric community as a diagnosis in its own right. Therefore, the methods of treatment are still at the research stage. Experts often choose experimental methods, but it is still unclear whether they have high efficiency.
PTSD (Post-Traumatic Stress Disorder) is a disorder that provokes instantaneous reactions of the psyche under the influence of a negative event. In patients without PTSD, a self-preservation reaction occurs during stressful moments, but a person with a disorder feels in danger even at a time when nothing threatens his life. And there is no natural fight-or-flight response to a threat. There is no guarantee that the disorder will not occur, even if the person is mentally stable. After all, it is not known what event can bring a person out of balance and how he will react to this or that stress.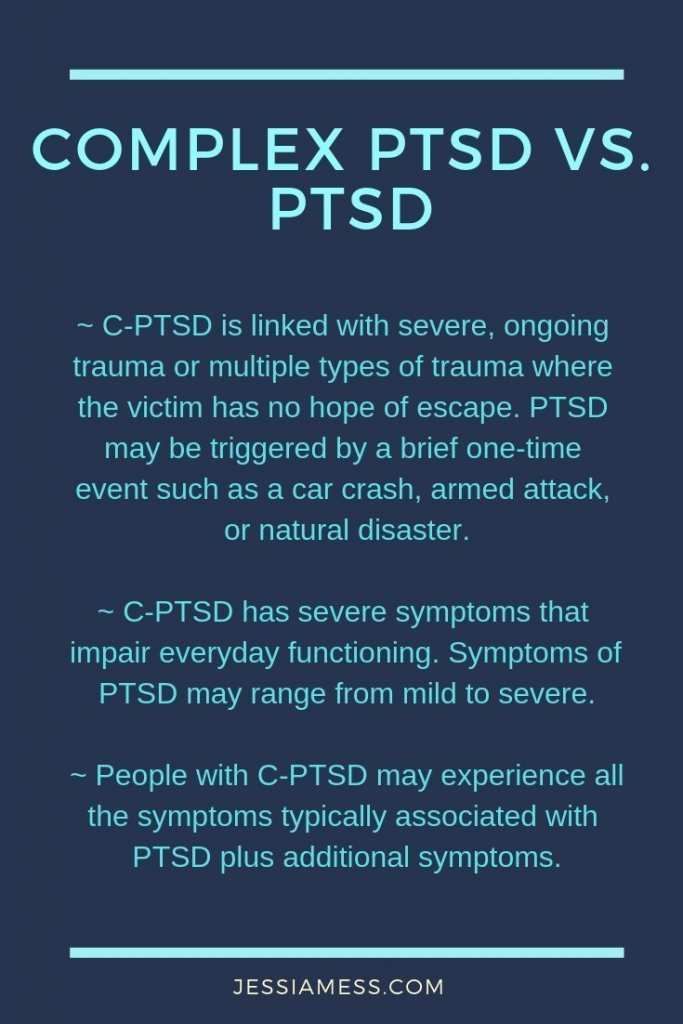
Like any mental disorder, post-traumatic disorder syndrome should be detected in a timely manner, and treatment should be carried out under the strict supervision of a specialist. In this, close people who recognize PTSD by the first signs can play a key role. We cannot close our eyes to the changed state of a person and his inappropriate behavior. The statistics in this disease are disappointing - 8 people out of 100 at least once experienced the condition of this disorder.
Mentally stable people are more at risk of developing this disease under the influence of traumatic circumstances, from calm to go into a state of post-traumatic stress disorder. At the same time, it can also be due to a genetic predisposition and manifest itself during minor shocks. Interestingly, people diagnosed with this condition rarely experience a single stressful shock. Most often, the violation is manifested due to several shocks. They can occur with a significant temporary break or go one after another. The presence of a diagnosis significantly reduces the patient's quality of life, and the disorder itself can take on a more advanced form and become complex - it is more complicated and requires a more thorough approach to treatment.
The presence of a diagnosis significantly reduces the patient's quality of life, and the disorder itself can take on a more advanced form and become complex - it is more complicated and requires a more thorough approach to treatment.
Why PTSD occurs
The causes of the disease are various and very extensive. Not always the disorder can be acquired, heredity also often plays a decisive role in the appearance of signs of PTSD.
The main causes of post-traumatic stress disorder are:
- Military events, military service, participation in hostilities.
- Act of terrorism.
- Cultural and ethnic conflicts.
- Assault causing bodily harm, threat of death.
- Death of loved ones, protracted illnesses that threaten death.

- Psychological or physical abuse.
- Political prerequisites are revolutions, genocide, forced migration, repressions.
- Man-made or natural disasters.
- Epidemics and pandemics.
The number of people with PTSD has increased significantly over the past two years. Because post-traumatic stress disorder usually occurs in a stressful situation, and general panic only exacerbates the situation. This is demonstrated by the situation in the world, which is faced with a coronavirus infection. This suggests that the list of reasons is very dynamic and can expand in connection with the changing situation in society.
In general, the factors that provoke PTSD are past events that led to psychological trauma. They are called acquired. But they can also be congenital - when post-traumatic stress disorder occurs due to heredity. It has been proven that there is a strong connection between a woman and a child. If the first suffered physical abuse during pregnancy, then it is likely that the baby will be predisposed to a mental disorder.
Pathogenesis of PTSD
When a traumatic event occurs, there is an instant rush of adrenaline. As a result, a neurological response appears in the brain. For a long time it persists, and provokes various mental reactions in the future in response to similar situations. Each time similar events occur, the activity of the hypothalamus decreases due to the high level of adrenaline. This is what causes the violation.
The pathogenesis of PTSD is also associated with low production of cortisol, increased excretion of corticotropin in the urine. The dexamethasone suppression test in people with PTSD is significantly higher than in those who suffer from clinical depression.
All of these factors indicate an abnormality in the axis of the hypothalamic-pituitary-adrenal axis (HPA). The HRA axis turns on in response to constantly arising fear. Therefore, there is also a connection between the frontal cortex and the limbic system. The axis triggers a hormonal surge, but in turn triggers the LC-noradrenergic system, which is associated with reinforcing bad memories. The subcortical basal nucleus (amygdala) is responsible for emerging threats and natural responses to them.
The subcortical basal nucleus (amygdala) is responsible for emerging threats and natural responses to them.
People with the syndrome have low levels of serotonin, which causes non-standard behavioral symptoms. The patient develops irritability, thoughts of suicide, unreasonable aggression. The secretion of the hormone dopamine is also involved. Its decrease causes apathy, inhibition in actions, and an increased level of dopamine provokes arousal - psychosis, unreasonable anxiety appears.
Symptoms of PTSD
Usually, signs of post-traumatic stress disorder appear within three months after the traumatic event. But there are also patients in whom symptoms do not appear earlier than after 6 months. It is possible at the same time a regular manifestation of a mental state, which allows us to talk about the chronic nature of PTSD.
Symptoms of post-traumatic stress disorder:
- One or more cases of avoiding a traumatic situation.
- One or more recollections of the traumatic situation.

- Two or more cases of violation of an adequate perception of reality, a sharp change in mood.
- Two or more cases of sudden excitability and increased activity.
Characterizing post-traumatic stress disorders, one cannot fail to mention the changing behavior of a person, which leaves an imprint on interaction with people, personal life and career.
- It seems to the patient that he is in a state of nervous breakdown or is about to break loose.
- There are uncontrollable outbursts of anger, sleep disturbance.
- A person enters an anxious state very quickly, instantly passes from a calm state to a frightened one.
The symptoms of this group have a permanent property. If the rest can appear from time to time, then excitability and activity will accompany the patient's behavior throughout the entire period marked by the presence of PTSD.
Characterization of post-traumatic stress disorder necessarily includes the presence of symptoms in the patient.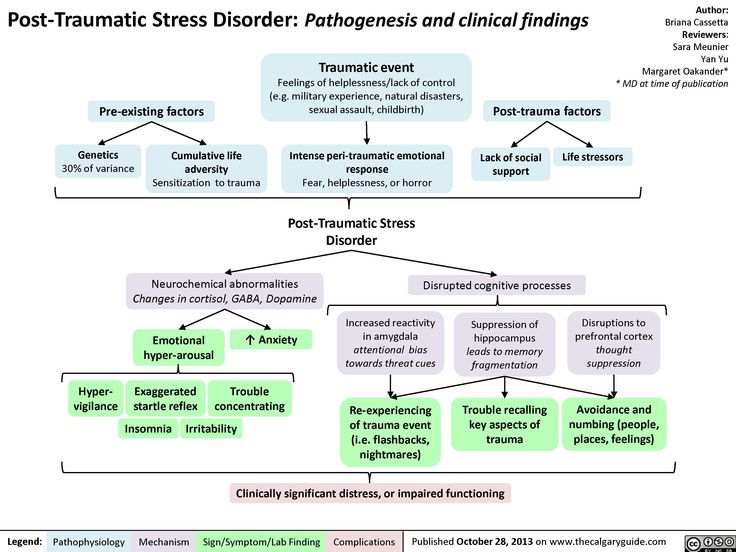 It is important to monitor the patient - these symptoms should be observed for at least a month. Their severity also plays a role - they must have a negative impact on a person's life, his interaction with society.
It is important to monitor the patient - these symptoms should be observed for at least a month. Their severity also plays a role - they must have a negative impact on a person's life, his interaction with society.
How PTSD is classified
The disease can pass into different stages, have a different nature of the course and be characterized by different degrees of severity. All these parameters, as well as signs of post-traumatic stress disorder, allow us to classify the disease.
If we give a general classification of the violation, then experts define it as an anxiety disorder, the accompanying signs of which are unpleasant experiences, behavior unusual for a calm person. Physiological reactions often also occur when contact with a traumatic situation occurs. All of these functions are observed within a month - this is the main distinguishing aspect in comparison with short-term stress.
The disease is divided into 3 forms:
- Sharp. Occurs after 30 days, it is preceded by a strong shock.

- Chronic. The appearance of this form is associated with heredity. Some traumatic event provoked PTSD, but the person had preconditions for this.
- Delayed. When much more than a month passes after the event. Sometimes the event can be repeated, but does not have consequences in the form of PTSD. But the origin of the corresponding biochemical processes provokes the development of the disease.
Post-traumatic stress disorder is also divided into several stages:
- A traumatic situation affects the psyche.
- A person begins to constantly think about it, rethink how it could have been prevented, feels guilty for what happened.
- The subject begins to avoid the place, people and things associated with the situation.
- There are symptoms of arousal, which become permanent.
- Symptoms persist for 30 days or more.
- The symptoms of post-traumatic stress disorder leave an imprint on the patient's habitual life, he has problems in communication and organization of activities.
According to the ICD-10 classification, there are 4 types of PTSD:
- Dysphoric type. The patient is characterized by constant irritability, aggressive behavior, dissatisfaction with the behavior of other people. Such people feel resentment, they can even take revenge, inflict physical damage on others. At the same time, regret about such behavior is not ruled out, but often satisfaction with destructive actions. People with this type of disease try to avoid outside help, refuse to see a doctor.
- Anxious type. He has frequent unmotivated anxiety attacks. It is realized not only mentally, but also manifests itself bodily. Describing post-traumatic stress disorder, specialists note frequent changes in the patient's mood and sleep disturbance in this type. A person strives for communication, as this helps him relieve anxiety.
- somatoform type. Accompanied by massive painful sensations in the body. Most people complain of pain in the heart area, a little less of changes in the gastrointestinal tract, some complain of headaches.
 These symptoms usually appear six months after the event. This type refers to the delayed form of the disease. The patient is constantly fixed on these sensations, which makes him go to the doctor.
These symptoms usually appear six months after the event. This type refers to the delayed form of the disease. The patient is constantly fixed on these sensations, which makes him go to the doctor. - Asthenic type. Characteristics of post-traumatic stress disorders in this case include apathy, lethargy, indifference to everything that happens. This state is depressing. Drowsiness appears, the person does not want to get out of bed. At the same time, dreams do not take the form of nightmares, they may not even appear. This type is most supportive of medical intervention - he willingly responds to the help of loved ones and agrees to appear to a specialist without unnecessary persuasion.
Post-traumatic stress disorder may take up to a month to appear, or it may take much longer. Diagnosis can be complicated by different behavior between types, but one thing unites patients - the indispensable presence in life of a situation that disrupts the usual course of life.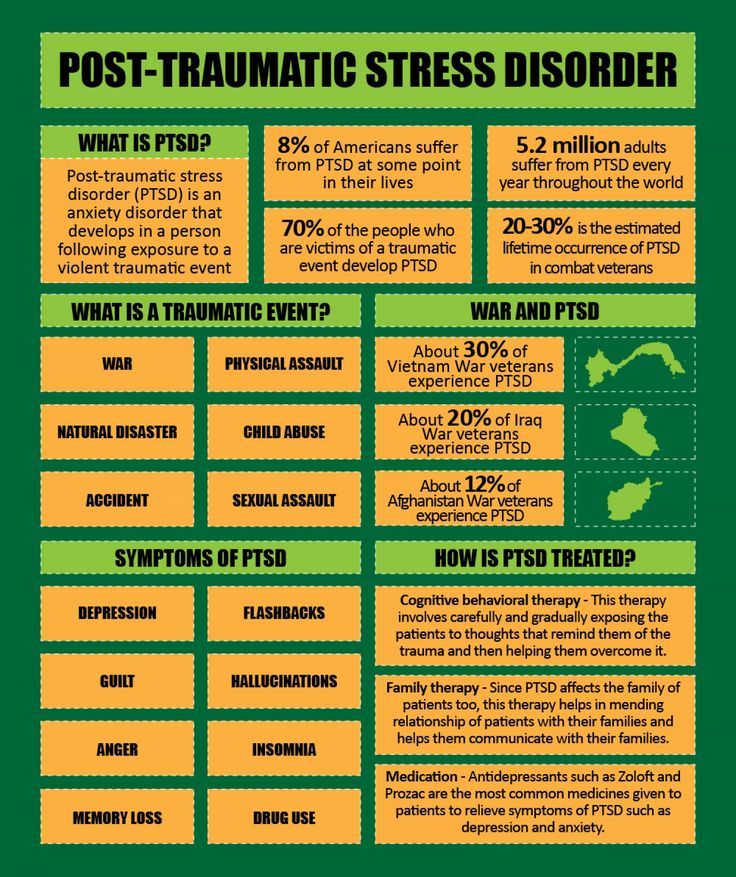
Once diagnosed, PTSD can also be classified as a treatable disorder or a disorder whose symptoms can be completely eliminated. PTSD usually causes disturbances in social, professional and other areas of activity.
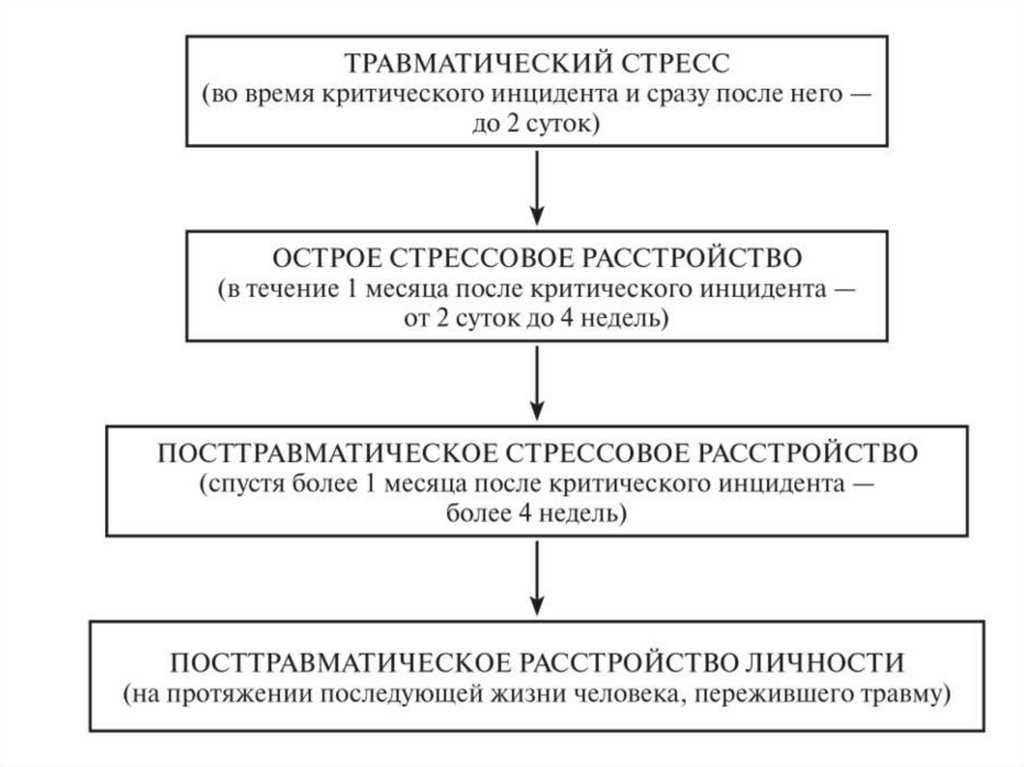
Stages of PTSD
There are several stages of the onset of this disease:
- Traumatic stress. Occurs during a critical incident and immediately after it for 2 days.
- Acute stress disorder. It appears within two days, can last up to 4 weeks.
- Post-traumatic stress disorder. Must have been more than 4 weeks.
- Post-traumatic personality disorder. It can run throughout life.
The last stage is considered incurable, so it is important to recognize the disease in the early stages. Symptoms at all stages are similar, but at each stage the conditions become more and more intrusive, getting rid of them becomes more and more difficult.
The signs themselves depend on the type - at each stage, an asthenic, somatoform, dysphoric or anxious type can manifest itself.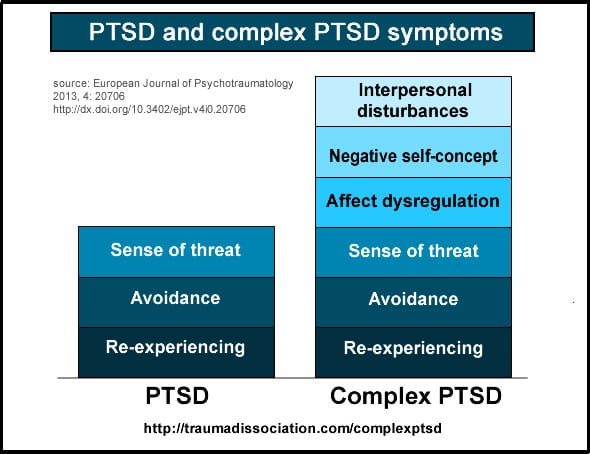 Passing through all the stages, PTSD manifests itself brighter, but the main signs remain the same.
Passing through all the stages, PTSD manifests itself brighter, but the main signs remain the same.
Complications of PTSD
In post-traumatic stress disorder, the consequences can be devastating to a person’s psyche, his physical health, but can also affect other people. This disease greatly increases the risk of problems such as:
- Drug use, alcoholism.
- Constant depression, which is accompanied by medication and the inability to lead a normal life.
- Eating disorder, deterioration of the brain, central nervous system and heart.
When to see a doctor
If a frightening situation has occurred in a person’s life that entails a traumatic experience, then this is already a reason to turn to the text. The patient may notice non-standard behavior behind him or heed the advice of loved ones who have noted changes in his condition.
The presence of symptoms also plays an important role - constantly occurring destructive deviations, disturbing dreams, aggression, or vice versa, an apathetic state. If they appear after a traumatic situation and do not let a person go for 30 days, then you should make an appointment with a psychiatrist or psychotherapist.
If they appear after a traumatic situation and do not let a person go for 30 days, then you should make an appointment with a psychiatrist or psychotherapist.
Only a specialist is able to establish the correct diagnosis and prescribe treatment. It is better to exclude an independent solution to the problem in this disease.
Diagnosis of disorder
Screening is usually used to diagnose PTSD. First of all, this is the PTSD scale, generally accepted in the ranks of researchers of mental disorders. It was developed by the Mississippi Group of Scientists. It is a questionnaire of 35 questions (for the military) or 39(a variation of the test for those suspected of having non-war related PTSD). Answers are ranked on a Likert scale. After the analysis, the final coefficient is derived. The questionnaire form contains inverted values - this prevents the possibility of setting a potential patient. It is also excluded that they are filled in random order.
Diagnostic criteria for post-traumatic stress disorder are established by a psychologist, psychiatrist or psychotherapist - they depend on the stage of the disease, the type and severity of the course.
Before proceeding with the diagnosis, the doctor gets acquainted with the anamnesis and talks with the patient. Often, friends and relatives of the patient are involved and interviewed for diagnosis. A doctor, based on third-party reviews, can create an unbiased and most complete picture of the condition of a potential patient.
Criteria for diagnosing post-traumatic stress disorder always involve the use by a doctor of tests, questionnaires, scales - everything that will help to fully assess the patient's condition. All these tools are used in a conversation not only with the patient himself, but also with his relatives.
The main method of diagnosing the disease is SCID (structured clinical diagnostic interview). It includes blocks of questions that are interconnected and help to smoothly move from one block to another. This technique is convenient in that it can be adjusted depending on specific tasks.
Other methods for diagnosing post-traumatic stress disorder include the Beck questionnaire (used to identify a depressive state), the Keane scale (used to assess the severity of combat experience), the Derogatis scale (assesses the severity of psychopathologies), the scale for assessing the severity of a traumatic event. A significant disadvantage of the listed scales is that they were developed by world scientists and their adaptation into Russian may cause certain difficulties, which will distort the results. At the moment, this problem is a priority in the community of Russian psychiatrists.
Post-traumatic stress disorder, its diagnosis and treatment should be under the strict supervision of a competent specialist.
In general, the diagnosis can be divided into several stages:
- observation.
- Conducting a survey.
- Projective method of personality research.
At this stage, generally accepted tests in psychology are used - Rorschach, Luscher, apperceptive.
- Use of standardized personality questionnaires.
- The use of questionnaires that diagnose the severity of pathopsychological symptoms in accordance with ICD-10.
Treatment of disorder
Depending on the nature of the disease, concomitant factors and the degree of neglect of the patient, the psychotherapist prescribes appropriate treatment. Sometimes medical intervention is required. Treatment for PTSD (post-traumatic stress disorder) often involves a holistic approach.
In the early stages, cognitive behavioral therapy is used. The specialist corrects the behavior model by replacing negative emotions with positive ones. With this approach, the patient can learn to identify depressing thoughts and use various techniques to get rid of them. The goal of therapy is to identify the symptoms of PTSD, monitor stress, behavioral changes, emotional outbursts and understand the nature of their origin. Correction of post-traumatic stress disorder with the help of cognitive therapy is often crowned with success.
Medication is an under-researched method of dealing with PTSD. It is believed that many drugs have a placebo effect - the patient drinks them and through self-hypnosis believes in getting rid of the disease. But the likelihood of relapse is high when prescribing such medications. Today, experts usually prescribe three drugs - paroxetine, venlafaxine and fluoxetine, which have successfully proven their effectiveness.
When authentic, PTSD is best treated with antibiotics. Serotonin-norepinephrine and serotonin reuptake inhibitors are prescribed. Tricyclic antidepressants such as sertraline and venlafaxine have been shown to be effective in some cases. These are second-line drugs for PTSD.
Benzodiazepines are also prescribed as medications. But their effectiveness has not yet been proven and their use is associated with a certain risk. Therefore, many doctors try to refuse these drugs, but some still prescribe them for severe insomnia.
Treatment of PTSD in the early stages of symptoms may include the use of glucocorticoids. The purpose of their appointment is to neutralize neurodegeneration, however, long-term use of them can, on the contrary, enhance it.
Children can also be affected. This is where play therapy helps. Studies have shown that it helps the child connect internal experiences with the outside world.
Psychotherapy for post-traumatic stress disorder, based on repetitive games, involves abstract thinking, helps children experience negative emotions.
As an additional recommendation, the specialist may advise physical activity. It must be moderate. Exercise and sports distract from bad thoughts, can improve self-esteem and control the physiological manifestations of a mental disorder. The main thing is not to overdo it so that the desire to get in shape does not become an obsession.
Therapy for complex post-traumatic stress disorder always includes an individual visit to a psychotherapist - a specialist identifies the causes of the disease, helps to recognize the signs of the condition, and accepts that the patient has a mental disorder.
For the treatment of PTSD, it is better to choose clinics that specialize in the treatment of mental disorders. Doctors with many years of experience work in such institutions, who have been practicing and conducting effective treatment for many years.
Some patients try to cope with the disease on their own. They try to contact other people, seek solace in conversations, recreational activities, hit on religion, practice breathing exercises. But the use of all these methods as a therapy for post-traumatic stress disorder cannot become the basis for its treatment and get rid of it forever.
+7 (495) 121-48-31
Disease prevention
There is no effective prevention for PTSD. A person cannot always predict whether a traumatic event will occur in his life, and what consequences it will lead to.
Some of the research on disorder prevention has focused on learning resilience—the ability to bounce back from tragic events. Such a strategy can be useful for people at risk - military personnel, journalists, members of rapid response teams. But the clinical guidelines for post-traumatic stress disorder don't place much emphasis on the effectiveness of this approach. Such strategies include teaching people how to respond to stressful situations and self-management techniques such as sleep control and mindfulness.
The support of loved ones plays an important role in preventing violations. A person can be helped to adapt to the outside world through conversations, visits to interest groups. It would be useful to contact a psychologist at the slightest symptoms. Prevention of post-traumatic stress disorder is effective only in the early stages. Therefore, contacting a specialist is a prerequisite for its successful treatment.
References:
- Alexandrov, E.O. Stages of clinical dynamics of post-traumatic stress disorder in combatants
- Alexandrov, E. O. Post-traumatic stress disorder: clinic, treatment
- Andryushchenko, A. V. Post-traumatic stress disorder in situations of loss of an object of extraordinary significance
- Voloshin, V.
Learn more