Ocd vitamin d
Investıgation of vitamin D levels in obsessive-compulsive disorder
Indian J Psychiatry. 2022 Jul-Aug; 64(4): 349–353.
Published online 2022 Jul 13. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_26_22
Author information Article notes Copyright and License information Disclaimer
Background:
The impact of vitamin D on obsessive-compulsive disorder (OCD) remains unknown.
Aim:
Studies suggest that vitamin D deficiency may be associated with neuropsychiatric diseases. The purpose of this study is to investigate vitamin D levels in those diagnosed with OCD. In addition, the relation between OCD symptom severity and serum vitamin D level is investigated.
Methods:
About 174 patients newly diagnosed with OCD and 170 healthy volunteers were included in the study. Yale–Brown Obsessive Compulsive Scale (YBOCS) was used to assess the severity of OCD symptoms. Serum vitamin D levels of the two groups were compared.
Results:
The serum vitamin D levels of the OCD group were found to be significantly lower than the control group. Serum vitamin D levels were negatively correlated with the obsession, compulsion, and total scale scores measured in YBOCS but there was no correlation between the serum vitamin D levels and illness duration of OCD patients.
Conclusions:
To the best of our knowledge, this is one of the first studies to investigate vitamin D levels in newly diagnosed adult OCD patients without comorbidities. Although our findings suggest that vitamin D may play a role in the pathophysiology of OCD, further studies are needed to support our findings.
Keywords: Biomarkers, central nervous system, obsessive-compulsive disorder, vitamin D
Obsessive-compulsive disorder (OCD) is a psychiatric disorder characterized by obsessions (intrusive thoughts, images, and urges) and/or compulsions (repetitive actions performed to reduce obsessional distress) and the lifetime prevalence of OCD in the adult population is 1.6–2.3%.[1,2] OCD usually begins in childhood or adolescence and it is often found in such additional psychiatric disorders as anxiety disorder, major depression, somatoform disorder, and bipolar disorder in OCD patients.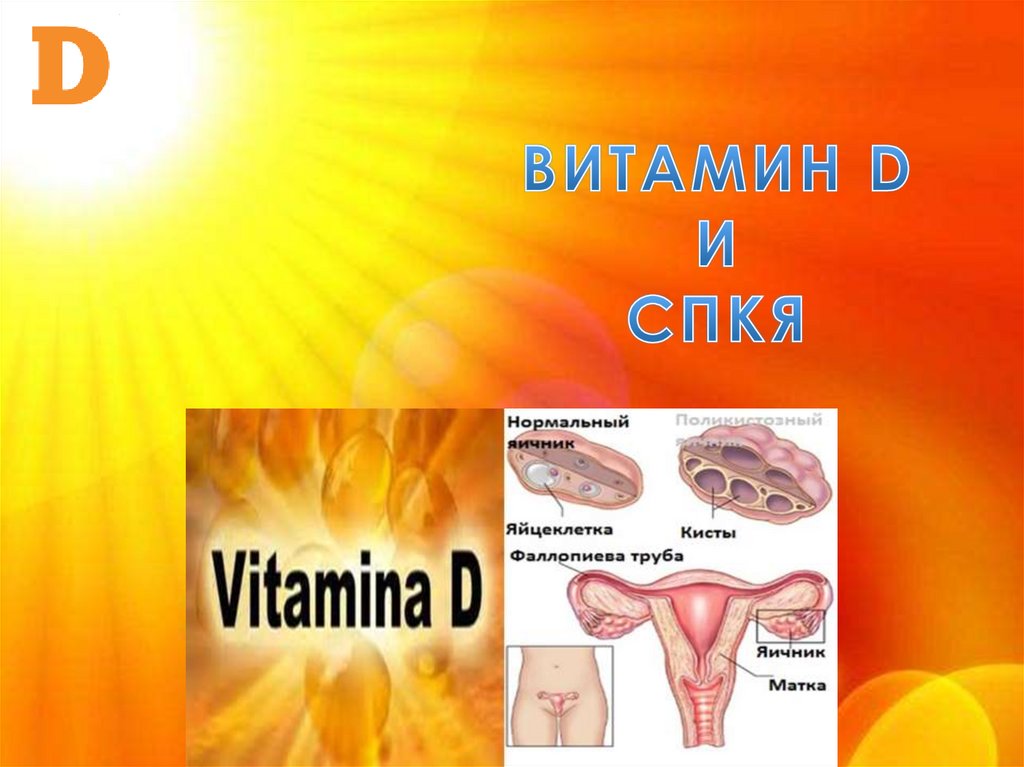 [3]
[3]
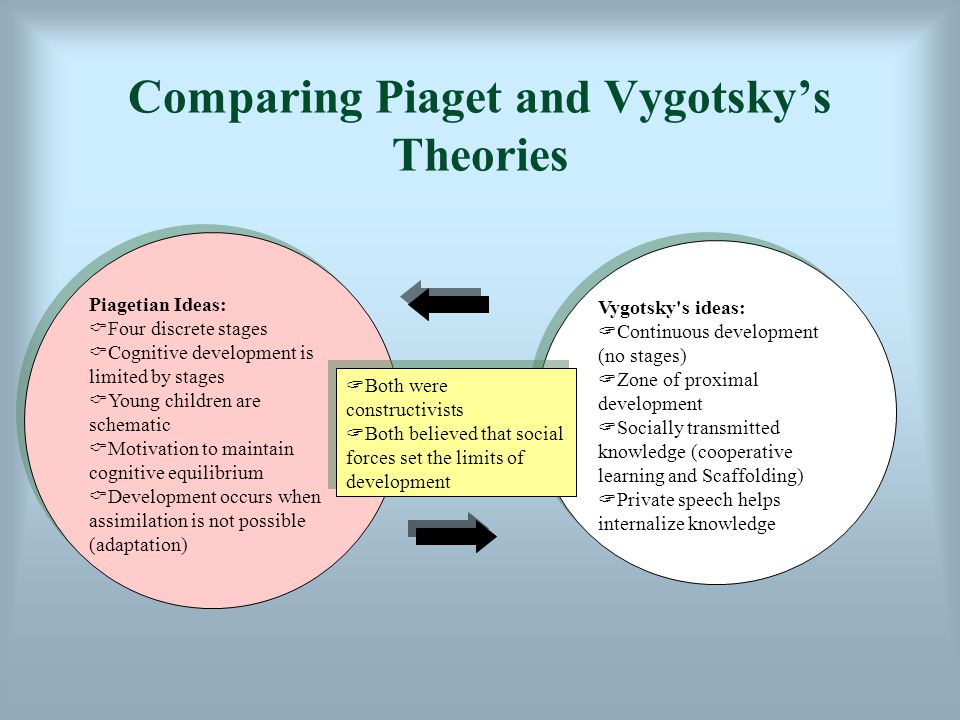
Neurochemical, genetic, immunological, and structural factors are thought to play a role in the etiology of OCD.[4] Some studies report neurotransmitters such as serotonin, dopamine, and glutamate play a role in the etiology of OCD.[5,6,7] Use of selective serotonin reuptake inhibitors (SSRIs) as the first option for psychopharmacological treatment of OCD, and the addition of typical/atypical antipsychotics, clomipramine, and glutamatergic agents to treat treatment-resistant patients supports these studies.[8,9,10]
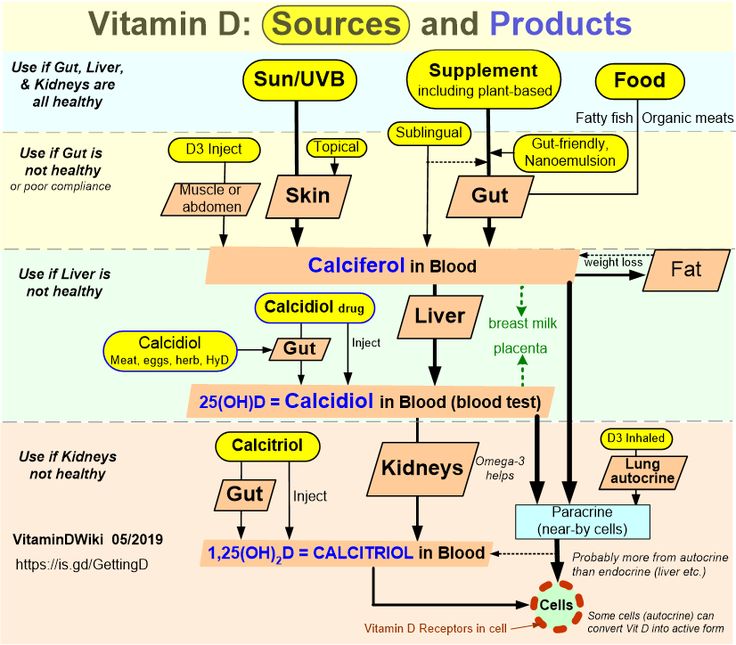
Vitamin D is synthesized in the epidermis as vitamin D3 (cholecalciferol) and converted to 25-OH D3 by hydroxylation in the liver. 25-OH D3 is hydroxylated again in the kidneys and the active form, 1,25 dihydroxy vitamin D3, is formed.[11] Vitamin D is an important molecule that plays a role in the regulation of calcium and phosphorus balance in the body, as well as in immunity, inflammatory response, and antioxidant processes.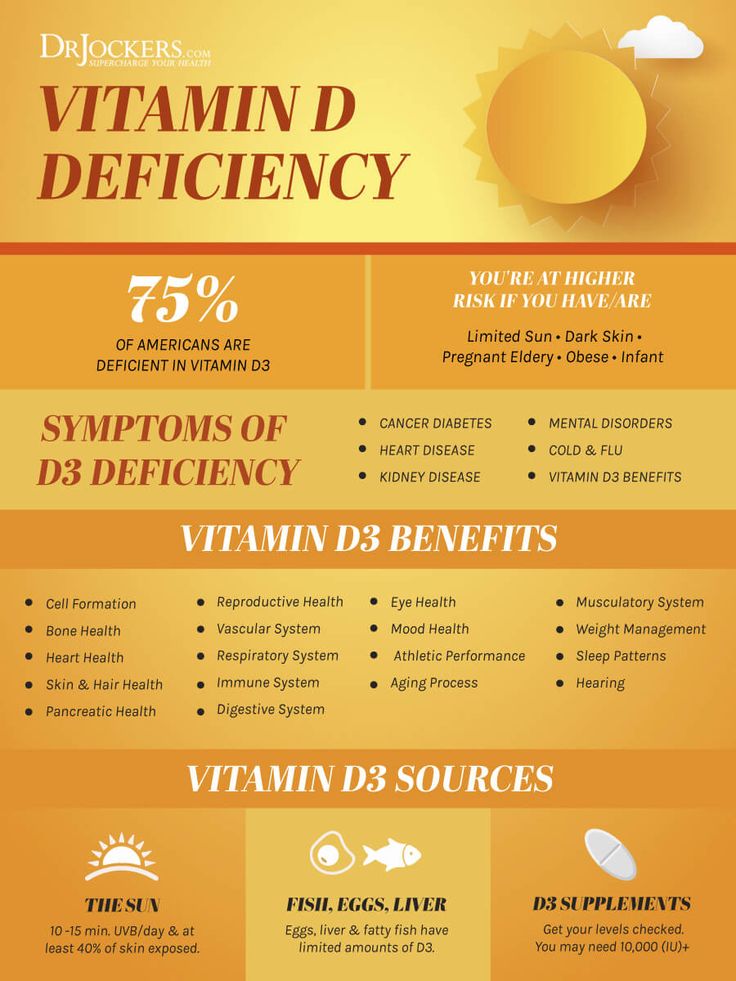 [12] Vitamin D is essential for brain development and maintenance of normal brain function.[13] It also plays an important role in cell proliferation and differentiation in the central nervous system (CNS).[14,15] There are studies reporting that vitamin D deficiency may be associated with neuropsychiatric diseases such as major depression, schizophrenia, attention deficit hyperactivity disorder (ADHD), and autism.[16,17,18,19]
[12] Vitamin D is essential for brain development and maintenance of normal brain function.[13] It also plays an important role in cell proliferation and differentiation in the central nervous system (CNS).[14,15] There are studies reporting that vitamin D deficiency may be associated with neuropsychiatric diseases such as major depression, schizophrenia, attention deficit hyperactivity disorder (ADHD), and autism.[16,17,18,19]
Levels of tryptophan hydroxylase, a speed-limiting enzyme in serotonin synthesis, and tyrosine hydroxylase, a speed-limiting enzyme in dopamine, epinephrine, and norepinephrine synthesis, are regulated by 1,25 dihydroxy vitamin D3. Therefore, vitamin D deficiency can be effective in the etiology of OCD by disrupting the synthesis of serotonin and catecholamine.[20,21] However, vitamin D protects cells against neurotoxicity by inhibiting inducible nitrite oxide synthetase (iNOS), the enzyme responsible for the synthesis of nitrite oxide. Vitamin D deficiency can contribute to OCD development by causing decreased neuroprotectivity. Studies that reported increased levels of nitrite oxide in OCD support this view.[22,23,24]
Studies that reported increased levels of nitrite oxide in OCD support this view.[22,23,24]
Currently, in the adult population, vitamin D insufficiency is defined as serum 25 (OH) D3 levels between 20 and 30 ng/mL; vitamin D deficiency is defined as serum 25 (OH) D3 levels of <20 ng/mL; and sufficient levels of serum 25 (OH) D3 are 30 ng/mL and above.[25]
There are a limited number of studies investigating the relation between OCD and vitamin D, and only one of these studies was conducted in a small sample of adult OCD patients.[26,27,28,29] For these reasons, we believe that this issue is worth investigating. What was aimed in this study is to investigate vitamin D levels and related parameters such as calcium, phosphorus, alkaline phosphatase, thyroid-stimulating hormone (TSH), and parathyroid hormone (PTH) levels in adult OCD patients and to compare them with healthy controls. We also intended to determine the relation between vitamin D levels and the severity of OCD symptoms and the duration of the illness.
Study Design
This study was conducted at the Ministry of Health, Kayseri City Hospital. The study was approved by the Ethical Committee of Kayseri City Hospital and written informed consent was obtained from all the participants.
Participants
About 307 patients between the age of 18 and 45 who were admitted to Kayseri City Education and Research Hospital Psychiatry Outpatient Clinic between July 15 and September 15 in 2021 and newly diagnosed with OCD according to Diagnostic and Statistical Manual for Mental Disorders, fifth edition (DSM-V) criteria were included in the study.[1] The healthy control group was selected among hospital staff or healthy volunteers with consideration of age and gender distribution of the OCD group. Exclusion criteria of the study: The patients with comorbid psychiatric diseases other than OCD, those diagnosed with mental retardation, those using calcium or vitamin D supplement in the past 6 months, those using corticosteroid drugs for any reason in the past 3 months, those having a history of alcohol or substance use, those having a chronic systemic disease such as hypothyroidism, hyperthyroidism, hypoparathyroidism, hyperparathyroidism, and diabetes, those having a clinically active infection, those with pathology detected in routine biochemical tests, and those who were pregnant or breastfeeding. Diagnoses were confirmed by applying The Structured Clinical Interview for DSM-V (SCID-V) to the patients.[30] Thirty-eight patients with comorbid depression, 19 patients with comorbid generalized anxiety disorder, 12 patients with comorbid panic disorder, 3 patients with comorbid social anxiety disorder, 5 patients with comorbid bipolar disorder, 9 patients using calcium or vitamin D supplements in the last 6 months, 6 patients using corticosteroid medication for any reason in the last month, 7 patients with a history of alcohol or substance use in the last 6 months, 6 patients with hypothyroidism, 3 patients with hyperthyroidism, 4 patients with diabetes, 14 patients with pathology in routine biochemical tests (leukocytosis was found in 7 patients, anemia in 5 patients, and thrombocytopenia in 2 patients), 2 breastfeeding patients, and 2 pregnant patients were excluded from the study. Three patients did not want to participate in the study. A total of 174°CD and 170 healthy subjects were included in the study.
Diagnoses were confirmed by applying The Structured Clinical Interview for DSM-V (SCID-V) to the patients.[30] Thirty-eight patients with comorbid depression, 19 patients with comorbid generalized anxiety disorder, 12 patients with comorbid panic disorder, 3 patients with comorbid social anxiety disorder, 5 patients with comorbid bipolar disorder, 9 patients using calcium or vitamin D supplements in the last 6 months, 6 patients using corticosteroid medication for any reason in the last month, 7 patients with a history of alcohol or substance use in the last 6 months, 6 patients with hypothyroidism, 3 patients with hyperthyroidism, 4 patients with diabetes, 14 patients with pathology in routine biochemical tests (leukocytosis was found in 7 patients, anemia in 5 patients, and thrombocytopenia in 2 patients), 2 breastfeeding patients, and 2 pregnant patients were excluded from the study. Three patients did not want to participate in the study. A total of 174°CD and 170 healthy subjects were included in the study.
Biochemical measurements
Since plasma vitamin D concentrations have seasonal biologic variance, the blood of all the participants was only collected between July 15 and September 15. 10 mL of fasting venous blood was collected in the morning between the hours of 08.00 and 10.00 AM into K2-EDTA-containing serum separator tubes. Serum and plasma were centrifuged for 30 min after collection. Plasma total 25 (OH) D3 concentrations were measured by using liquid chromatography (Shimadzu, HPLC Prominence LC-20A, Japan) coupled with tandem mass spectrometry (LC MS/MS) (AB Sciex Q TRAP 4500, Toronto, Canada), using an Immuchrom 25 OH Vitamin D3/D2 kit (Immuchrom GmbH, Germany). Serum calcium (Ca) and phosphorus (P) were measured by photometric methods, alkaline phosphatase (ALP) by colorimetric method, and thyroid-stimulating hormone (TSH) and parathyroid hormone (PTH) by sandwich immunoassay methods on, Roche Cobas c501 and 601 (Roche Diagnostics GmbH, Mannheim, Germany) autoanalyzers.
Data collection instruments
SCID-V Disorders, Clinician Version (SCID-V-CV): It is a clinical interview scale developed and structured to investigate DSM-V diagnoses.[30] Validity and reliability tests of the Turkish version were performed by Elbir et al.[31]
The Yale–Brown Obsessive Compulsive Scale (YBOCS): This scale was developed by Goodman et al.[32] to evaluate the severity of obsession and compulsion symptoms. The scale consists of 19 items and 10 items are scored (5 obsessions and 5 compulsive items). Three different evaluation scores can be calculated from the scale: obsession, compulsion, and total. The total score of the scale changes between 0 and 40. Higher total scores indicate higher severity of OCD symptoms. Validity and reliability tests of the Turkish version were performed by Karamustafalıoğlu et al.[33]
Statistical analyses
The data were evaluated in the statistical package program of IBM SPSS Statistics Standard Concurrent User V 26 (IBM Corp. , Armonk, New York, USA). Categorical measurements were summarized as numbers and percentages, and continuous measurements as mean and standard deviation (median and minimum-maximum where appropriate). Shapiro–Wilk test was used to determine whether the parameters in the study showed normal distribution. The Chi-square test was used in the analysis of categorical expressions. Mann–Whitney U test was used for binary variables for parameters that did not show normal distribution. Spearman correlation analysis was used to determine the relationship between continuous measurements. The statistical significance level was taken as 0.05 in all tests.
, Armonk, New York, USA). Categorical measurements were summarized as numbers and percentages, and continuous measurements as mean and standard deviation (median and minimum-maximum where appropriate). Shapiro–Wilk test was used to determine whether the parameters in the study showed normal distribution. The Chi-square test was used in the analysis of categorical expressions. Mann–Whitney U test was used for binary variables for parameters that did not show normal distribution. Spearman correlation analysis was used to determine the relationship between continuous measurements. The statistical significance level was taken as 0.05 in all tests.
The sociodemographic characteristics of the control group and the OCD group are presented in . There was no significant difference between the groups in terms of sociodemographic characteristics such as age, gender, marital status, profession, and educational status (p > 0,05).
Table 1
Sociodemographic data of control group and OCD group
| Control Group n=170 | OCD Group n=174 | P | |
|---|---|---|---|
| Age (years) | 28 (CI: 24-30) | 29 (CI: 27-32) | 0,135a |
| Gender n (%) | |||
| Female | 92 (54,1) | 88 (50,6) | 0,642b |
| Male | 78 (45,9) | 86 (49,4) | |
| Education (years) | 13 (CI: 11-13) | 13 (CI: 12-13) | 0,251a |
| Marital status | |||
| n (%) | 68 (40) | 60 (34. 5) 5) | 0,339b |
| Single | 94 (55.3) | 96 (55.2) | |
| Married | 8 (4.7) | 18 (10.3) | |
| Divorced | |||
| Profession n (%) | |||
| Not working | 70 (41,2) | 62 (35,6) | 0.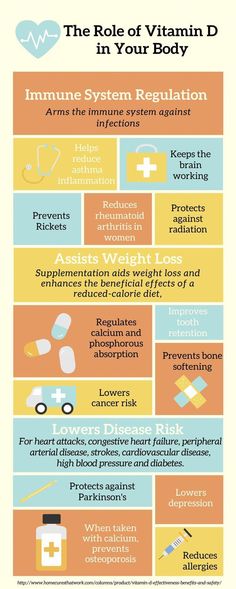 455b 455b |
| Working | 100 (58,8) | 112 (64,4) |
Open in a separate window
OCD: Obsessive-compulsive disorder; aMann–Whitney U test; bChi-square test
Biochemical data of the control group and the OCD group are presented in . The serum 25OH-D3 levels of the OCD group were found to be significantly lower than the control group (p < 0.001), but there was no significant difference between the two groups in terms of serum calcium, serum phosphate, ALP, PTH, and TSH levels (p > 0,05). The number of participants with vitamin D insufficient (20–30 ng/mL) and vitamin D deficiency (< 20 ng/mL) in the OCD group was statistically significantly higher than the control group (p < 0,001) and also the number of participants whose vitamin D levels were in the normal range (> 30 ng/mL) in the OCD group was statistically significantly lower than the control group (p < 0,001).
Table 2
Biochemical data of the control group and OCD group
| Control Group n=170 | OCD Group n=174 | P | |
|---|---|---|---|
| 25OH-D3 (ng/mL) | 27,8 (CI: 25,8-29,1) | 19,4 (CI: 18,3-20,9) | <0,001a |
| Min-max (ng/mL) | 9.4-37.3 | 13.6-43.8 | |
| Sufficient (>30 ng/mL) | 50 (29. 4%) 4%) | 21 (12.1%) | <0,001 b |
| Insufficient (20-30 ng/mL) | 102 (60%) | 55 (31.6%) | <0,001 b |
| Deficiency (<20 ng/mL) | 18 (10.6%) | 98 (56.3%) | <0,001b |
| Phosphor (mg/dL) | 3,73 (CI: 3,64-3,95) | 3,76 (CI: 3,65-3,89) | 0.870a |
| TSH (mU/L) | 2,68 (CI: 2,45-3,12) | 2,64 (CI: 2,45-3,23) | 0,814a |
| PTH (pg/mL) | 34,4 (CI: 30,8-36,4) | 34,9 (CI: 30,2-37,8) | 0. 575a 575a |
| ALP (IU/L) | 65 (CI: 58-72) | 64 (CI: 58-72) | 0.879a |
Open in a separate window
TSH: Thyroid-stimulating hormone; PTH: Parathyroid hormone; ALP: Alkaline phosphatase; aMann–Whitney U test; bChi-square test
In the OCD group, the YBOCS obsession score is 12 (CI: 11-13), the YBOCS compulsion score is 13 (CI: 12-14), and the YBOCS total score is 26 (CI: 24.5-27). The illness duration of OCD patients is 12 months.
Serum 25OH-D3 levels were negatively correlated with the obsession (r = -0,693, P < 0.001), compulsion (r = -0,633, P < 0.001), and total scale scores measured in YBOCS (r = -0,705, P < 0.001). No correlation was found between the serum 25OH-D3 levels and illness duration of OCD patients (p > 0,05).
In this study, we purposed to investigate vitamin D levels and related parameters such as calcium, phosphorus, ALP, TSH, and PTH levels in OCD patients and to compare them with healthy controls. We also investigated the relation of vitamin D levels with the severity of OCD symptoms and the duration of the illness. The results of the study showed that OCD may be associated with vitamin D deficiency and there is a moderately negative correlation between serum vitamin D levels and OCD symptom severity. According to this, as vitamin D levels decrease, YBOCS scores increase. The idea that vitamin D deficiency may play a role in various psychiatric disorders is getting stronger day by day. In recent studies, it has been shown that vitamin D levels in patients with depression and anxiety disorders are lower than in healthy controls.[34,35,36] Depression and anxiety disorders have a similar etiology to OCD and serotonin plays an important role in this etiology.[37] Low levels of vitamin D can increase the severity of OCD symptoms as they decrease the amount of serotonin by decreasing tryptophan hydroxylase synthesis. We found that there was no significant correlation between disease duration and serum vitamin D levels. This may be because vitamin D levels fluctuate seasonally as it is affected by sunlight.
We found that there was no significant correlation between disease duration and serum vitamin D levels. This may be because vitamin D levels fluctuate seasonally as it is affected by sunlight.
As far as we know, there are only four studies that investigate the association between OCD and vitamin D. In addition, three of these studies were conducted on pediatric and adolescent OCD patients.[26,27,28] There is only one study conducted on adult OCD patients.[29] Our study is the first to investigate vitamin D levels and related parameters such as calcium, phosphorus, ALP, TSH, and PTH levels in adult OCD patients without comorbid psychiatric conditions.
In a study conducted in 2016, vitamin D levels were found to be lower in patients diagnosed with OCD and pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) compared to healthy controls but it was not statistically significant.[26] In this study, increased oxidative stress due to autoimmune disease may have affected vitamin D levels in patients. Therefore, it is not clear whether low vitamin D levels are due to OCD or autoimmune processes. In our study, the participants did not have acute or chronic systemic diseases that may affect vitamin D levels, such as hypothyroidism, hyperthyroidism, hypoparathyroidism, hyperparathyroidism, diabetes, and clinically active infection.
Therefore, it is not clear whether low vitamin D levels are due to OCD or autoimmune processes. In our study, the participants did not have acute or chronic systemic diseases that may affect vitamin D levels, such as hypothyroidism, hyperthyroidism, hypoparathyroidism, hyperparathyroidism, diabetes, and clinically active infection.
A study published in 2017 by Esnafoğlu and Yaman reported lower vitamin D levels in children and adolescents with OCD compared to healthy controls.[27] There are some important differences between Esnafoğlu and Yaman’s study and ours in terms of methodology and limitations: First, vitamin D deficiency is known to be associated with depression or anxiety disorder.[38] Since the patients in this study had depression and other anxiety disorders comorbid with OCD, it is unclear whether low vitamin D levels in the OCD group are associated with comorbidities of depression or anxiety disorder. Secondly, the authors did not provide information about the previous or current use of psychotropic drugs by the patients.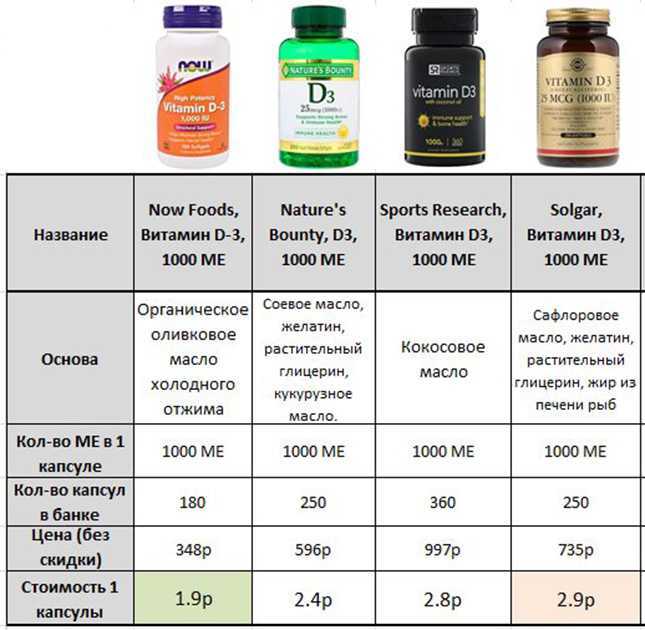 In our study, the patients did not have any comorbid psychiatric disease other than OCD and patients had not been using any drug for at least 3 months. Thirdly, since vitamin D levels are affected by sunlight, blood samples must all be collected during the same season. For this reason in our study, blood was only collected between July 15 and September 15 but it is not clearly stated what time of year the blood collection occurred in the study of Esnafoglu and Yaman.
In our study, the patients did not have any comorbid psychiatric disease other than OCD and patients had not been using any drug for at least 3 months. Thirdly, since vitamin D levels are affected by sunlight, blood samples must all be collected during the same season. For this reason in our study, blood was only collected between July 15 and September 15 but it is not clearly stated what time of year the blood collection occurred in the study of Esnafoglu and Yaman.
In the study of Yazıcı et al.,[28] serum vitamin D levels were found to be lower in children and adolescent OCD patients compared to healthy controls, but this finding was not statistically significant. These findings support our findings.
Finally, Marazziti et al.[29] in their study reported that serum vitamin D levels in 50 adult OCD patients were statistically significantly lower than in the control group. Although this study was conducted in adult OCD patients, it has some important methodological differences from our study.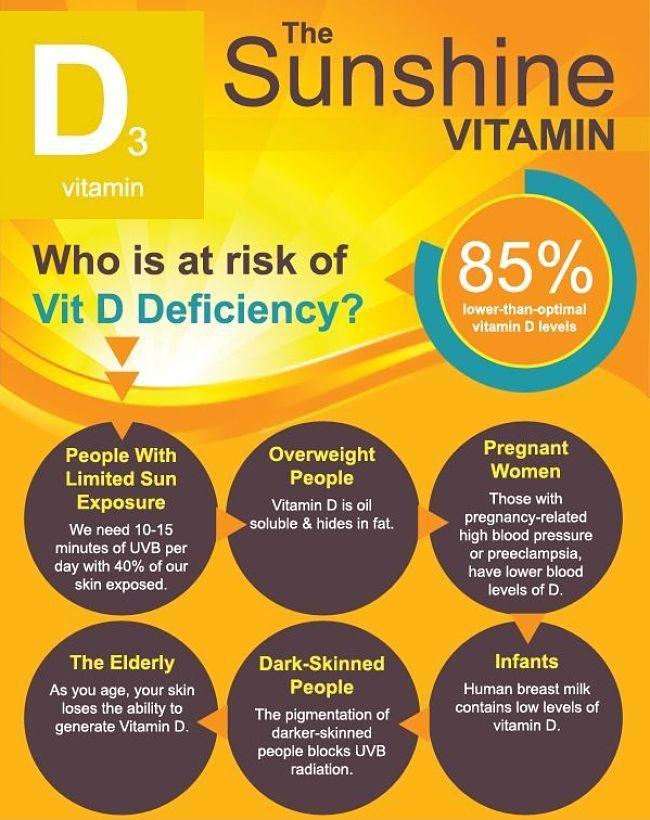 First, the comorbidity with different psychiatric disorders was quite common. Thirty-eight of 50 patients had at least one psychiatric disorder comorbid with OCD. Therefore, low vitamin D levels in OCD patients may be affected by comorbidity. Secondly, 34 of 50 patients were taking at least one or more psychotropic drugs such as antidepressants, mood stabilizers, antipsychotics, and benzodiazepines. Psychotropic drugs can affect both OCD severity and vitamin D levels. It may also mask other psychiatric disorders in patients. Therefore, the OCD group in our study consisted of patients who did not use any psychotropic drugs for at least 3 months. Thirdly, vitamin D-related parameters such as calcium, phosphorus, ALP, TSH, and PTH levels have not been investigated. Lastly, since their sample is relatively small, it may not represent all patients diagnosed with OCD in the community, and there was no control group in the study, a comparison of vitamin D was made between patients and normative values.
First, the comorbidity with different psychiatric disorders was quite common. Thirty-eight of 50 patients had at least one psychiatric disorder comorbid with OCD. Therefore, low vitamin D levels in OCD patients may be affected by comorbidity. Secondly, 34 of 50 patients were taking at least one or more psychotropic drugs such as antidepressants, mood stabilizers, antipsychotics, and benzodiazepines. Psychotropic drugs can affect both OCD severity and vitamin D levels. It may also mask other psychiatric disorders in patients. Therefore, the OCD group in our study consisted of patients who did not use any psychotropic drugs for at least 3 months. Thirdly, vitamin D-related parameters such as calcium, phosphorus, ALP, TSH, and PTH levels have not been investigated. Lastly, since their sample is relatively small, it may not represent all patients diagnosed with OCD in the community, and there was no control group in the study, a comparison of vitamin D was made between patients and normative values.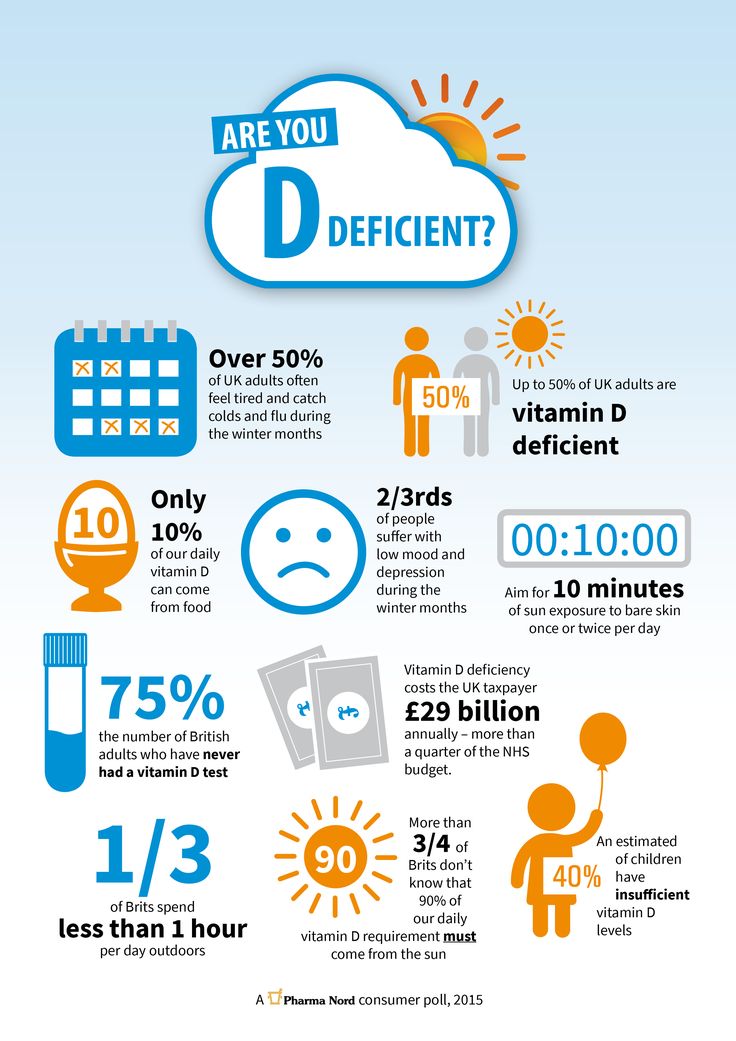
Limitations of the study
This study must be considered with its limitations. We collected blood samples between July 15 and September 15, when sunlight is the most intense in our country. This may have influenced vitamin D levels in both groups. Also, no data were collected regarding the duration of sunlight exposure. OCD patients have great tendency to spend their time in the home due to their obssesions. Therefore, they may be less exposed to sunlight. It may have affected vitamin D levels in the OCD group.
The study demonstrated that newly diagnosed OCD patients have lower vitamin D levels than healthy controls. Vitamin D may play a role in the pathophysiology of OCD and may be related to the severity of the disorder. Since vitamin D is affected by sunlight, further studies are needed in different seasons in different parts of the world to support or disprove our findings.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
1. American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V) Washington DC: American Psychiatric Association; 2013. [Google Scholar]
2. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63. [PMC free article] [PubMed] [Google Scholar]
3. Adam Y, Meinlschmidt G, Gloster AT, Lieb R. Obsessive–compulsive disorder in the community:12-month prevalence, comorbidity and impairment.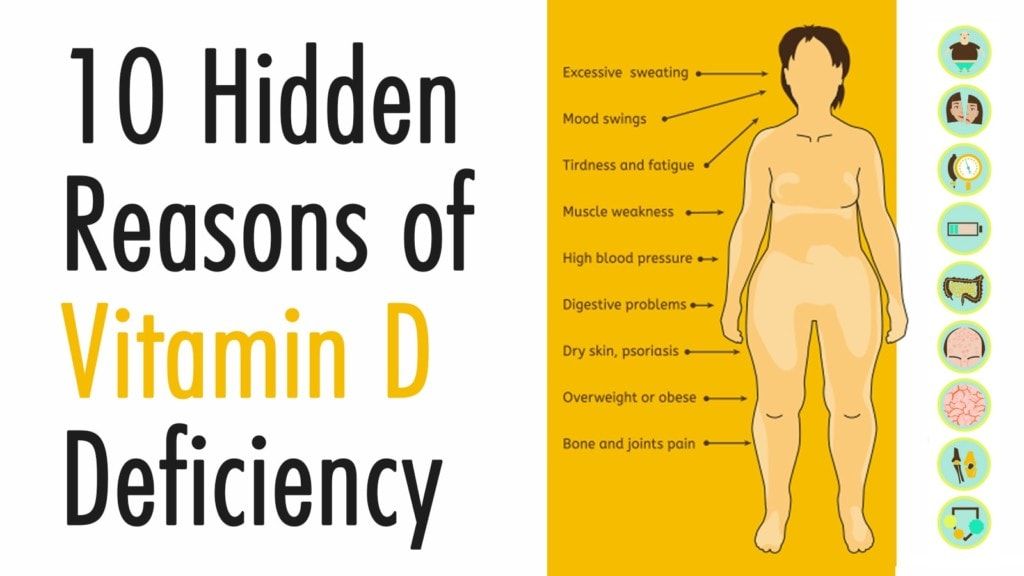 Soc Psychiatry Psychiatr Epidemiol. 2012;47:339–49. [PubMed] [Google Scholar]
Soc Psychiatry Psychiatr Epidemiol. 2012;47:339–49. [PubMed] [Google Scholar]
4. Boileau B. A review of obsessive-compulsive disorder in children and adolescents. Dialogues Clin Neurosci. 2011;13:401–11. [PMC free article] [PubMed] [Google Scholar]
5. Westenberg HG, Fineberg NA, Denys D. Neurobiology of obsessive-compulsive disorder:Serotonin and beyond. CNS Spectr. 2007;12:14–27. [Google Scholar]
6. Koo MS, Kim EJ, Roh D, Kim CH. Role of dopamine in the pathophysiology and treatment of obsessive-compulsive disorder. Expert Rev Neurother. 2010;10:275–90. [PubMed] [Google Scholar]
7. Kariuki–Nyuthe C, Gomez–Mancilla B, Stein DJ. Obsessive compulsive disorder and the glutamatergic system. Curr Opin Psychiatry. 2014;27:32–7. [PubMed] [Google Scholar]
8. Dell'Osso B, Nestadt G, Allen A, Hollander E. Serotonin-Norepinephrine reuptake inhibitors in the treatment of obsessive-compulsive disorder. J Clin Psychiatry. 2006;67:600–10. [PubMed] [Google Scholar]
9. Bloch MH, Landeros-Weisenberger A, Kelmendi B, Coric V, Bracken MB, Leckman JF. A systematic review:Antipsychotic augmentation with treatment refractory obsessive-compulsive disorder. Mol Psychiatry. 2006;11:622–32. [PubMed] [Google Scholar]
Bloch MH, Landeros-Weisenberger A, Kelmendi B, Coric V, Bracken MB, Leckman JF. A systematic review:Antipsychotic augmentation with treatment refractory obsessive-compulsive disorder. Mol Psychiatry. 2006;11:622–32. [PubMed] [Google Scholar]
10. Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2012;51:98113. [PubMed] [Google Scholar]
11. Eyles DW, Burne TH, McGrath JJ. Vitamin D, Effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013;34:47–64. [PubMed] [Google Scholar]
12. DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80:1689S–96S. [PubMed] [Google Scholar]
13. McCann JC, Ames BN. Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction? Faseb J. 2008;22:982–1001. [PubMed] [Google Scholar]
14. Brown J, Bianco JI, McGrath JJ. Eyles DW 1,25-dihydroxyvitamin D3 induces nerve growth factor, promotes neurite outgrowth and inhibits mitosis in embryonic rat hippocampal neurons. Neurosci Lett. 2003;343:139–43. [PubMed] [Google Scholar]
15. Holick MF. Vitamin D and brain health:The need for vitamin D supplementation and sensible sun exposure. J Intern Med. 2015;277:90–93. [PubMed] [Google Scholar]
16. Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affect Disord. 2017;208:56–61. [PubMed] [Google Scholar]
17. Chiang M, Natarajan R, Fan X. Vitamin D in schizophrenia:A clinical review. Evid Based Ment Health. 2016;19:6–9. [PubMed] [Google Scholar]
18. Goksugur SB, Tufan AE, Semiz M, Gunes C, Bekdas M, Tosun M, et al. Vitamin D status in children with attention-deficit-hyperactivity disorder. Pediatr Int. 2014;56:515–9. [PubMed] [Google Scholar]
19. Wang T, Shan L, Du L, Feng J, Xu Z, Staal WG, et al. Serum concentration of 25-hydroxyvitamin D in autism spectrum disorder:A systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2016;25:341–50. [PubMed] [Google Scholar]
20. Cui X, Pertile R, Liu P, Eyles DW. Vitamin D regulates tyrosine hydroxylase expression:N-cadherin a possible mediator. Neuroscience. 2015;304:90–100. [PubMed] [Google Scholar]
21. Kaneko I, Sabir MS, Dussik CM, Whitfield GK, Karrys A, Hsieh JC, et al. 1,25-Dihydroxyvitamin D regulates expression of the tryptophan hydroxylase 2 and leptin genes:Implication for behavioral influences of vitamin D. FASEB J. 2015;29:4023–35. [PubMed] [Google Scholar]
22. Garcion E, Sindji L, Montero-Menei C, Andre C, Brachet P, Darcy F, et al. Expression of inducible nitric oxide synthase during rat brain inflammation:Regulation by 1,25-dihydroxyvitamin D3. Glia. 1998;22:282–94. [PubMed] [Google Scholar]
23. Atmaca M, Tezcan E, Kuloglu M, Ustundag B. Plasma nitrate values in patients with obsessive-compulsive disorder. Psychiatry Clin Neurosci. 2005;59:621–3. [PubMed] [Google Scholar]
24. Behl A, Swami G, Sircar SS, Bhatia MS, Banerjee BD. Relationship of possible stress-related biochemical markers to Oxidative/Antioxidative status in obsessive-compulsive disorder. Neuropsychobiology. 2010;61:210–4. [PubMed] [Google Scholar]
25. Ritu G, Gupta A. Vitamin D deficiency in India:Prevalence, causalities and interventions. Nutrients. 2014;6:729–75. [PMC free article] [PubMed] [Google Scholar]
26. Celik G, Tas D, Tahiroglu A, Avci A, Yüksel B, Çam P. Vitamin D deficiency in obsessive- compulsive disorder patients with Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections:A case control study. Arch Neuropsychiatr. 2016;53:33–7. [PMC free article] [PubMed] [Google Scholar]
27. Esnafoglu E, Yaman E. Vitamin B12, folic acid, homocysteine and vitamin D levels in children and adolescents with obsessive compulsive disorder. Psychiatry Res. 2017;254:232–7. [PubMed] [Google Scholar]
28. Yazıcı KU, Yazıc PI, Üstündağ B. Vitamin D levels in children and adolescents with obsessive compulsive disorder. Nord J Psychiatry. 2018;72:173–8. [PubMed] [Google Scholar]
29. Marazziti D, Barberi FM, Fontenelle L, Buccianelli B, Carbone MG, Parra E, et al. Decreased Vitamin D levels in OCD patients. CNS Spectr. 2021:1–24. doi:10.1017/S1092852921000821. [PubMed] [Google Scholar]
30. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-5-CV) Artmed, Porto Alegre. 2017 [Google Scholar]
31. Elbir M, Alp TopbaşÖ, Bayad S, Kocabaş T, Topak OZ, Çetin Ş, et al. Adaptation and reliability of the structured clinical interview for DSM-5-disorders, clinician version (SCID-5/CV) to the Turkish language. Turk Psikiyatr Derg. 2019;30:51–6. [PubMed] [Google Scholar]
32. Goodman W, Price L, Rasmussen S, Mazure C, Fleischmann R, Hill C, et al. Yale-Brown Obsessive Compulsive Scale (Y-BOCS) Arch Gen Psychiatry. 1989;46:1006–11. [PubMed] [Google Scholar]
33. Karamustafalıoğlu K, Üçışık A, Ulusoy M, Erkmen H. Validity and Reliability of the Turkish Version of the Yale-brown obsessive compulsive scale. Bursa: SavaşOfset; 1993. p. 86. [Google Scholar]
34. Armstrong DJ, Meenagh GK, Bickle I, Lee AS, Curran ES, Finch MB. Vitamin D deficiency is associated with anxiety and depression in fibromyalgia. Clin Rheumatol. 2007;26:551–4. [PubMed] [Google Scholar]
35. Józefowicz O, Rabe-Jabłońska J, Woźniacka A, Strzelecki D. Analysis of vitamin D status in majör depression. J Psychiatr Pract. 2014;20:329–37. [PubMed] [Google Scholar]
36. Terock J, Hannemann A, Van der Auwera S, Janowitz D, Spitzer C, Bonk S, et al. Posttraumatic stress disorder is associated with reduced vitamin D levels and functional polymorphisms of the vitamin D binding-protein in a population-based sample. Prog Neuropsychopharmacol Biol Psychiatry. 2020;96:109760. [PubMed] [Google Scholar]
37. Westenberg HG, Fineberg NA, Denys D. Neurobiology of obsessive-compulsive disorder:Serotonin and beyond. CNS Spectr. 2007;12:14–27. [Google Scholar]
38. Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affect Disord. 2017;208:56–61. [PubMed] [Google Scholar]
Vitamin D Deficiency and Mental Health: What's the Link?
Vitamin D deficiency is very common in people with mental health and neurological disorders.
Vitamin D is a vital nutrient and hormone best known for its role in bone development.
But did you know that a lack of vitamin D may also play a role in the development of various mental health disorders, such as obsessive-compulsive disorder (OCD) and depression?
Vitamin D insufficiency and deficiency are quite common in the general population. For instance, as many as 40% of adults are vitamin D insufficient and around 6% are deficient.
And while the fortification of milk with vitamin D in the 1930s improved the situation — and even helped eradicate rickets — deficiency in this important nutrient is still a public health issue.
In particular, low levels of Vitamin D appear in several mental health disorders, including:
- obsessive-compulsive disorder (OCD)
- Attention deficit hyperactivity disorder (ADHD)
- schizophrenia
- autism
- depression and anxiety
Obsessive-compulsive disorder (OCD) is a psychiatric disorder in which a person gets caught in an often debilitating cycle of obsessions and compulsions.
Research suggests that a high number of people with OCD have vitamin D deficiency.
A 2017 study found that children and teens with OCD tend to have significantly lower levels of vitamins D and B12 and higher levels of the amino acid homocysteine (an indicator of vitamin deficiency).
These low levels also coincided with symptom severity.
In a 2016 study, researchers compared the vitamin D levels of children with PANDAS-related OCD to those without the condition.
PANDAS is short for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections. Children may be diagnosed with PANDAS when OCD symptoms suddenly occur after a strep infection.
The study findings show that vitamin D deficiency was much more frequent in the OCD group than in the control group (48.5% vs. 20%).
In addition, children with OCD and low levels of vitamin D also had higher rates of co-occurring ADHD than those without the deficiency (87.5% vs. 52.6%).
As mentioned above, vitamin D deficiency may be linked to attention deficit hyperactivity disorder (ADHD). However, research is mixed.
Some evidence suggests that children with ADHD have significantly lower vitamin D levels than those without ADHD, while another study didn’t find a significant difference between the two groups.
Still, researchers say that treating vitamin D deficiency in this population is important.
It’s long been observed that a higher number of people with schizophrenia are born in winter and spring. This led to the hypothesis that low levels of vitamin D may play a role in its development.
A 2018 study supports this idea, as vitamin D deficiency in infants was linked to an increased risk for schizophrenia in later life.
In addition, vitamin D deficiency is quite high in people with schizophrenia. It’s estimated that 65–70% of those with schizophrenia have low vitamin D levels, and more than half of this population has osteoporosis.
At the same time, people with schizophrenia often have poorer diets and health in general, are less active, and often have other medical conditions — all factors which can affect vitamin D levels.
It’s somewhat unclear whether vitamin D supplementation works in adults with schizophrenia.
Some recent evidence suggests that 12 months of supplementation was linked to fewer symptoms of depression and anxiety in people with schizophrenia. But other research showed no noticeable effects, so the findings are mixed.
A growing body of research suggests that vitamin D deficiency during pregnancy and early childhood is linked to some cases of autism, a neurological and developmental disorder.
Children who have autism — or are likely to develop it — have lower levels of vitamin D at 3 months in utero, at birth, and at age 8 compared to their siblings without autism.
A small 2017 study found that vitamin D supplementation during pregnancy, infancy, and early childhood significantly reduced the expected incidence of autism in children of mothers who already had one child with the disorder. The risk ultimately dropped from 20% to 5%.
Vitamin D supplementation may help in childhood too. Two trials found that high doses of vitamin D improved the core symptoms of autism in about 75% of children with the condition.
There are many individual antidotes of vitamin D helping with symptoms of depression and anxiety. Research also confirms a link in some cases, but the exact mechanism remains unclear.
A 2020 study revealed that vitamin D may play a role in restoring balance between the neurotransmitters GABA (calming) and glutamate (excitatory).
A 2020 review of 61 research papers showed an association between vitamin D and major depression disorder, but whether the deficiency caused the depression or vice versa seems to require further research.
Another 2020 study looked at the effects of giving vitamin D supplements to depressed participants over a 6-month period. The findings show that vitamin D supplements improved anxiety symptoms — but not depressive symptoms — in participants with previously low vitamin D levels.
Vitamin D deficiency is surprisingly common. Research from 2021 suggests that 1 billion people around the world have a deficiency.
Symptoms of low vitamin D may be hard to spot and are often similar to symptoms of other deficiencies or disorders. As mentioned above, low levels of D may also play a role in mental health disorders and other diseases. A 2020 review suggests a deficiency may lead to symptoms of depression.
In children, vitamin D deficiency may have the following symptoms:
- developmental delay
- lethargy
- irritability
- bone changes
- fractures
People with prolonged and severe vitamin D deficiency may develop a condition called secondary hyperparathyroidism. This causes all of the parathyroid glands to become enlarged and hyperactive.
Symptoms may include:
- bone pain
- joint pain
- muscle pain
- fatigue
- muscle twitching
- weakness
Bone fractures and osteoporosis may also result from chronic vitamin D deficiency.
Between 50–90% of vitamin D is absorbed through the skin via sunlight exposure. To prevent deficiency, researchers suggest 20 minutes of daily sunshine with over 40% of the skin exposed.
Of course, the further away you are from the equator, the harder this becomes.
Diet can provide vitamin D as well. Foods with vitamin D include:
- Fatty fish: salmon, tuna, swordfish, sardines cod liver oil
- Vitamin D-fortified dairy or nut milk products
- Vitamin-D fortified orange juice
- Egg yolk
- Beef liver
- Vitamin D-fortified cereals
Taking regular vitamin D supplements is a good idea for many people.
It’s especially beneficial for those who are older, have darker skin, live in colder climates, or stay mostly indoors, as vitamin D levels are often lower in these groups.
In general, taking regular vitamin D supplements may help reduce cancer cell growth, infection severity, and inflammation (implicated in many mental health disorders). The vitamin is also critical for building strong bones.
For people with mental health disorders, taking vitamin D may help alleviate certain symptoms. It’s likely worth getting your vitamin D levels checked and speaking with your doctor to determine whether vitamin D supplements is a good choice for you.
Vitamin D is a necessary nutrient for promoting brain and bone health. You can get the necessary dose of vitamin D through sunlight, certain foods, or supplements. Although there are many ways to get vitamin D, nearly half of Americans receive an insufficient dosage of vitamin D and billions of people around the world are considered deficient in vitamin D.
Research has revealed that people with mental health disorders are more likely to have vitamin D deficiency or insufficiency. The direct correlation between vitamin D and certain mental health disorders varies.
Some research has found:
- vitamin D deficiency to be more prevalent in people with certain mental health disorders
- vitamin D deficiency to play a role in triggering certain mental health disorders
- vitamin D to help alleviate certain mental health disorder symptoms
Despite there being mixed findings between the relationship between vitamin D and some of the most common mental health and neurological disorders, including OCD, ADHD, schizophrenia, autism, depression, and anxiety, experts agree vitamin D is an essential nutrient that many people are not receiving enough of.
Consider getting your vitamin D checked and speaking with your doctor about ways to get your vitamin D intake to a healthy level. This may be particularly important if you are living with a mental health disorder or have a history of mental illness in your family.
OCD: Supplements to help overcome it
Obsessive Compulsive Disorder (OCD) is exactly what its name suggests.
Basically, it is a mental condition in which a person experiences intrusive, intrusive and disturbing thoughts that cause feelings of discomfort and/or fear, often leading to obsessive-compulsive behavior.
This can manifest itself in a variety of ways, such as (R):
- Body Dysmorphic Disorder (BDD), in which a person cannot stop thinking about one or more perceived defects or flaws in their appearance. For example, "if I had a smaller forehead or if I was 7 centimeters taller, I would be perfect and everyone would love me."
- Storage disorder.
- Trichotillomania, in which hair is pulled out of the scalp, eyebrows and other parts of the body.
- Excoriation (skin picking) disorder.
- Intrusive/repetitive checks, such as whether you locked the door, etc.
- Hand washing and germ phobia.
- Obsessive thoughts and reflections.
- Ritualized eating behavior characteristic of eating disorders.
- Substance or gambling preoccupation, as seen in substance-related disorders and addictions.
- Preoccupation with illness, as in an anxiety disorder of illness.
- Sexual impulses or fantasies, as in paraphilic disorders.
- Impulses seen in disruptive, impulse control and behavioral disorders.
- Reflections of guilt that arise in major depressive disorder.
- Intrusion or delusional preoccupation, as in the schizophrenic spectrum and other psychotic disorders.
- Repetitive behavior patterns that are characteristic of autism spectrum disorders.
- Fears such as fear of infection, fear of aggression/harm, sexual fears, religious fears and the need to do things "right".
Compensatory compulsions for these obsessions include laundry and cleaning, checking, seeking reassurance, repetition, as well as ordering, organizing, etc.
anxiety, depression, autism, fear, etc., so "treatment" can overlap, because what can reduce anxiety, for example, can also reduce OCD.
Let's look at a few mechanisms in the body that potentially contribute to OCD.
HPA axis, glutamate and GABA
HPA (hypothalamus-pituitary-adrenal) axis
The entire stress cascade is elevated in OCD. From the hypothalamus, which secretes the inflammatory corticotropin-releasing hormone (CRH), all the way to the adrenal glands, which secrete cortisol.
Lack of cortisol suppression in the dexamethasone suppression test (DST) is a sign of an abnormal HPA axis in patients with OCD, which may be explained by possible pituitary numbness due to high levels of CRH (CRH) (R). Interestingly, acetylcholine can reduce sensitivity to CRH and lead to increased levels of CRH, ACTH, and cortisol.
Atropine, an anticholinergic drug, activates CRH receptors in the cerebral cortex and shows that excess acetylcholine can contribute to CRH insensitivity and lead to high CRH levels.
High Acetylcholine Syndrome (coming soon)
By taming the HPA axis, we can significantly reduce the symptoms of OCD. And it has been found with many adaptogens such as ashwagandha, valerian, magnesium, etc.
> Learn more about how to lower cortisol levels here (coming soon)
DHEA-S and GABA
OCD patients also have higher plasma levels of dehydroepiandrosterone sulfate (DHEAS), a neuroactive steroid that has an effect opposite to that of allopregnanolone (R). In this study, the effects of allopregnanolone against obsessive-compulsive disorder were comparable to those of fluoxetine, and the benefits were blocked by finasteride (R).
DHEA-S opposes GABA while allopregnanolone is pro-GABA. Too much DHEA-S can leave you in a state of over-activation, such as ADD, ADHD, anxiety, rumination, depression, etc. GABA is needed to inhibit glutamate, which is chronically elevated in OCD.
Another note about acetylcholine:
Decreasing acetylcholine levels by blocking its receptors or by presynaptically activating mAChR M2/M4 (which act as inhibitory autoreceptors) reduces glutamate release. Excess glutamate is associated with depression.
...
glutamatergic hyperactivity is associated with obsessive-compulsive disorder, which may be due to the fact that activation of nicotinic receptors releases glutamate (R).
Glutamate
Some studies have shown that the concentration of glutamate is significantly higher in the cerebrospinal fluid of patients with obsessive-compulsive disorder compared to healthy people. Higher glutamate concentrations are associated with excitotoxicity and oxidative stress (glutamate is excitotoxic and neurotoxic) in patients with obsessive-compulsive disorder, and this appears to be correlated with symptom severity (R).
Glutamate acts on a variety of receptors, one of which is NMDA. Quinolic acid is also an agonist at this receptor and can cause neurotoxicity in large amounts. Quinolic acid is formed in the kynurenine pathway, which is activated by inflammation. Reducing inflammation by reducing intake of polyunsaturated fats, reducing excess iron (and other heavy metals) in the body, lowering parathyroid hormone and aldosterone levels, calming gut inflammation, etc. can help reduce excessive inflammation.
Turmeric, taurine, glycine, carnosine, niacinamide, magnesium, zinc, selenium, cocoa, vitamin C, E, aspirin, vitamin D, and a host of other herbs and supplements can help reduce inflammation.
GABA keeps glutamate (as well as other neurotransmitters) in check, so when GABA is inhibited, neurotransmitters such as glutamate, CRH, serotonin, acetylcholine, etc. can become too high.
GABAergic supplements are very helpful against OCD. Additives such as:
- Progesterone and its 5-alpha-reduced metabolite, 5-alpha-dihydroprogesterone (5a-DHP)
- Niacinamide (many say that niacin and/or niacinamide did a great job with OCD anxiety)
- Taurine
- Valerian root
- Zinc (anxiety and obsessive thoughts (R).
- Baikal skullcap
- Magnolia
- etc.
Another method that has been used for OCD is deep brain stimulation (DBS). The procedure includes drilling holes in your skull and inserting rods into your brain that change the function of various nuclei.It has been shown to suppress the HPA axis and increase thyroid hormone levels, which correlates with improvement in symptoms (R).
This is what 0.01% of people with OCD would do, but it's interesting to note that DBS lowered cortisol levels and increased thyroid levels. Thus, thyroid function is also likely to be suboptimal in people with OCD.
This study showed that in patients with OCD, the TSH response to TRH is blunted, meaning they are more likely to have insufficient T4 and T3 with elevated prolactin (TRH increases prolactin) (R).
Melatonin
In patients with obsessive-compulsive disorder, 24-hour melatonin secretion was reduced compared to healthy controls, while its circadian rhythm was preserved (R).
Agomelatine, a melatonin receptor agonist and also a 5-HT2C serotonin receptor antagonist, is useful in obsessive-compulsive disorder (R, R).
Serotonin
Serotonin appears to be involved/disturbed in almost all psychiatric disorders.
Serotonin is created by tryptophan hydroxylase 2 (TPh3) in the brain from the amino acid tryptophan. Serotonin binds to its receptors, 5-HT1 to 5-HT7. (R , R ).
By activating serotonin receptors, 5-HT1A, 1B and 1D have anti-OCD effects, reducing production of serotonin (R, R). Ketamine, a 5-HT1B agonist, has rapid anti-obsessive-compulsive disorder properties in animal models at low doses (R).
mCPP, a potent serotonergic drug, when given to untreated OCD patients increases their anxiety, depression, and dysphoria, and worsens their OCD symptoms (R).
Clomipramine, the gold standard treatment for obsessive-compulsive disorder, inhibits serotonin and norepinephrine reuptake but is a potent α1-adrenergic receptor, histamine h2 receptor, serotonin 5-HT2A, 5-HT2C, 5-HT3, 5-HT6 and 5-HT7 receptors, dopamine D1, D2 and D3 receptors and muscarinic acetylcholine receptors (M1 - M5).
It is clear that the "beneficial" serotonergic drugs work not only by increasing serotonin levels, as shown above, since gold standard serotonergic drugs block most serotonin receptors.
On the other hand, metergoline, which is an antiserotonergic agent, does not improve OCD symptoms because it is a 5-HT1B/D antagonist, meaning that it may increase serotonin levels in certain areas of the brain and may worsen mood in some people .
Antagonism of 5-HT2A and 5-HT2C receptors has an anti-OCD effect since both of these receptors are highly sensitive in OCD (R). Fluoxetine, another serotonergic drug, may be useful in obsessive-compulsive disorder by desensitizing 5-HT2C (R).
Agomelatine inhibits/increases the release of norepinephrine and dopamine, especially in the frontal cortex, by inhibiting the 5-HT2C receptor, making it very useful in OCD (R, R).
Desensitization of serotonin receptors and decreased prolactin levels (associated with less 5-HT2C activation) are associated with improved symptoms (R). This alteration in response to endogenous serotonin may mediate the anti-obsessional effects of clomipramine (R).
Moreover, ondansetron's 5-HT3 antagonism may be useful in obsessive-compulsive disorder (R).
Vitamins and minerals
Vitamin D
Vitamin D levels are negatively correlated with symptom severity in patients with OCD (R).
People with OCD tend to have low vitamin D levels and are more likely to develop ADHD (R).
Vitamin D reduces hair pulling in OCD (trichotillomania) (R).
Vitamin D:
- Increases tyrosine and tryptophan hydroxylase, which can lead to increased levels of dopamine and serotonin.
- Has an antioxidant effect and inhibits inducible nitric oxide synthase, which has neuroprotective properties similar to agmatine.
Zinc, selenium, iron and magnesium
Some people with OCD have been found to have low levels of zinc, selenium, iron and magnesium. In a randomized, placebo-controlled clinical trial, one group received fluoxetine plus zinc and the other group received fluoxetine plus placebo for 8 weeks. This study showed that the zinc group had greater improvement compared to the placebo group (R).
Magnesium and OCD:
The introduction of magnesium reduces anxiety, panic and phobias, improves the state of attention deficit and sleep disorders. We believe that magnesium acts mainly by:
a) reducing the presynaptic release of glutamate;
b) decreased activity of the NMDA receptor due to competition with calcium in calcium channels associated with the NMDA receptor;
c) positive allosteric modulatory action at the level of some metabotropic presynaptic glutamate receptors, reducing presynaptic release of glutamate and stimulating release of GABA;
d) decrease in the release of catecholamines due to the direct presynaptic effect under the influence of some factors, including calcium.
Link
Folic acid and B12
According to this study, patients with OCD tend to be more likely to have low folic acid and B12 levels with elevated homocysteine, which correlates significantly with symptom severity (R).
Nitric Oxide
Nitric Oxide modulates neurotransmitters involved in OCD, and OCD patients have higher plasma nitrate levels, and OCD medications reduce nitric oxide (R) levels. Agmatine is effective in improving compulsive behavior in mice, which appears to be related to brain nitric oxide (R).
> Find out more here about nitric oxide and how to lower it (coming soon)
Healthy Supplements
- Amantadine (100mg) (R).
- Memantine (5-20mg) (R).
- NAC (500mg-2g per day) (R).
- Caffeine (300 mg) (R)
- pro-opioids (which may help reduce anxiety) (R) such as tianeptine (R), selank (R), agmatine (makes other opioids more effective), gluten , dairy products, etc.
- Saffron . "Our results indicate that saffron (30 mg) is as effective as fluvoxamine in treating patients with mild to moderate obsessive-compulsive disorder" (R).
- Minocycline . Minocycline is a fat-soluble antibiotic that can cross the blood-brain barrier. In the brain, it has neuroprotective and neurogenic properties in amyotrophic lateral sclerosis and Parkinson's disease. Minocycline reduces levels of pro-inflammatory agents, including nitric oxide, tumor necrosis factor-α, and interleukin-1β, and reduces glutamate-induced neurotoxicity. Minocycline has a therapeutic effect on neurodegenerative diseases and this can be achieved by blocking glutamate-mediated excitotoxicity (R).
It can be useful not only because it reduces inflammation, but also because it is an antibiotic. Early onset of sudden obsessive-compulsive disorder preceded by streptococcus. The infection was known as PANDAS (Childhood Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections) (R). - Myo-inositol . 18 g/day appears to be helpful in obsessive compulsive disorder (R).
- Glycine (60g, but this dose caused a high dropout rate due to nausea and vomiting (R)).
- Milk Thistle . Results from a single randomized controlled trial (n=35) of milk thistle for the treatment of obsessive-compulsive disorder showed no significant difference in treatment effects between milk thistle (600 mg/day) and fluoxetine . Milk thistle has been shown to have similar effects to fluoxetine in OCD symptoms, and its positive effect begins in the fifth week without serious side effects " (P).
- Valerian extract at 765 mg/day is useful in obsessive-compulsive disorder by activating the GABA (R) system.
- Ashwagandha 120 mg/day (crude extract) (R).
- Curcumin . “ After oral curcumin for 35 days, compulsive checking and ritualistic behaviors were significantly reduced, and quinpyrol-induced aggravations were reversed. These effects of curcumin were comparable to paroxetine " (R).
- Borage extract (500 mg) (R).
- Vitamin B1 . It helps against the anxious part of OCD. Doses of 250 mg/day (thiamine hydrochloride) (R) are commonly used. You can always try sulbutiamine, benfotiamine, or allithiamin, which can be more effective than regular thiamine.
- Psilocybin * (R).
- Uridine . There is no scientific reference to this drug, but there is a lot of anecdotal evidence that it helps with obsessive-compulsive disorder. This is most likely due to the fact that it increases dopamine and increases the number of dopamine receptors, which are reduced in obsessive-compulsive disorder (R, R).
- Kundalini Yoga (R). Not a supplement, but it can be dosed as a supplement if you feel comfortable thinking that way. And this applies not only to kundalini yoga, but also to other styles of yoga or meditation, because it is about calming the mind, deep breathing and reducing overall stress.
Continued discussion of this material on the English-language forum: here
* Psilocycin is on the list of prohibited substances in the Russian Federation.
Categories
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, everything had come to naught, and in my teens I decided that these were just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is obsessive-compulsive disorder - Mayo Clinic
Intrusive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person’s condition does not interfere with himself or others, then everything is in order; if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as their own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasant. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment, remission can be achieved: for a long time to get rid of obsessive thoughts and compulsive actions or reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other medications: tranquilizers, antipsychotics, or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy in which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive Behavioral Therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16.2003 No. 438 "On Psychotherapeutic Care"
OCD in Russia is treated by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease gave a new round. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a psycho-neurological dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalization My condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine at the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 P |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant.Treatment
Second hospitalization and psychotherapyAfter six months of outpatient treatment, the local psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Item of expenditure | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 Р |
Antidepressants
2422 R
Transportation
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Item of expenditure | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 P |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
Learn more