Pre psychosis symptoms
Early Psychosis and Psychosis | NAMI: National Alliance on Mental Illness
In this 2-part podcast series, NAMI Chief Medical Officer Dr. Ken Duckworth guides discussions on early psychosis that offer insights from individuals, family members and mental health professionals. Read the transcript.
Note: Content includes discussions on topics such as suicide attempts and may be triggering.
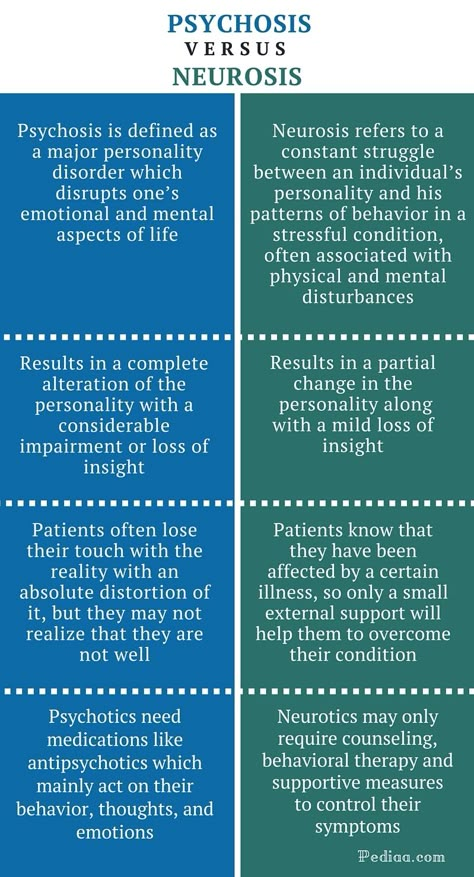
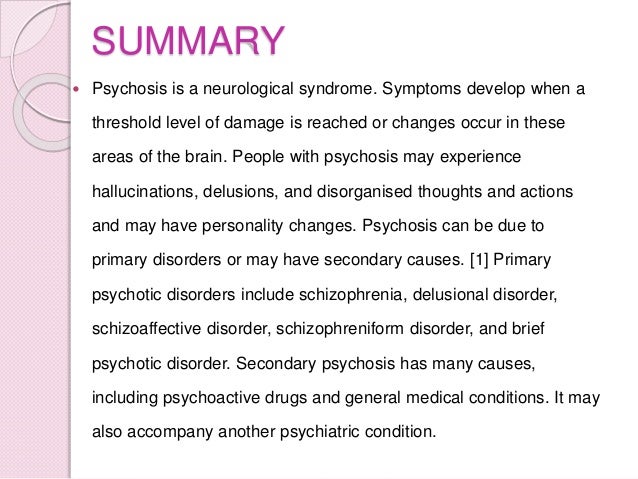
Most people think of psychosis as a break with reality. In a way it is. Psychosis is characterized as disruptions to a person’s thoughts and perceptions that make it difficult for them to recognize what is real and what isn’t. These disruptions are often experienced as seeing, hearing and believing things that aren’t real or having strange, persistent thoughts, behaviors and emotions. While everyone’s experience is different, most people say psychosis is frightening and confusing.
Psychosis is a symptom, not an illness, and it is more common than you may think. In the U.S., approximately 100,000 young people experience psychosis each year. As many as 3 in 100 people will have an episode at some point in their lives.
Early or first-episode psychosis (FEP) refers to when a person first shows signs of beginning to lose contact with reality. Acting quickly to connect a person with the right treatment during early psychosis or FEP can be life-changing and radically alter that person’s future. Don’t wait to take the first step and prepare yourself with information by reviewing these tip sheets:
What is Early and First-Episode Psychosis?
Early Psychosis: What's Going on and What Can You Do?
Encouraging People to Seek Help for Early Psychosis
Early Intervention: Tips for School Staff and Coaches
Symptoms
Early warning signs before psychosis
Early psychosis or FEP rarely comes suddenly. Usually, a person has gradual, non-specific changes in thoughts and perceptions, but doesn't understand what's going on. Early warning signs can be difficult to distinguish from typical teen or young adult behavior. While such signs should not be cause for alarm, they may indicate the need to get an assessment from a doctor.
Early warning signs can be difficult to distinguish from typical teen or young adult behavior. While such signs should not be cause for alarm, they may indicate the need to get an assessment from a doctor.
Encouraging people to seek help for early psychosis is important. Families are often the first to see early signs of psychosis and the first to address the issue of seeking treatment. However, a person's willingness to accept help is often complicated by delusions, fears, stigma and feeling unsettled. In this case, families can find the situation extremely difficult, but there are engagement strategies to help encourage a person to seek help.
It's important to get help quickly since early treatment provides the best hope of recovery by slowing, stopping and possibly reversing the effects of psychosis. Early warning signs include the following:
- A worrisome drop in grades or job performance
- Trouble thinking clearly or concentrating
- Suspiciousness or uneasiness with others
- A decline in self-care or personal hygiene
- Spending a lot more time alone than usual
- Strong, inappropriate emotions or having no feelings at all
Signs of early or first-episode psychosis
Determining exactly when the first episode of psychosis begins can be hard, but these signs and symptoms strongly indicate an episode of psychosis:
- Hearing, seeing, tasting or believing things that others don’t
- Persistent, unusual thoughts or beliefs that can’t be set aside regardless of what others believe
- Strong and inappropriate emotions or no emotions at all
- Withdrawing from family or friends
- A sudden decline in self-care
- Trouble thinking clearly or concentrating
Such warning signs often point to a person’s deteriorating health, and a physical and neurological evaluation can help find the problem.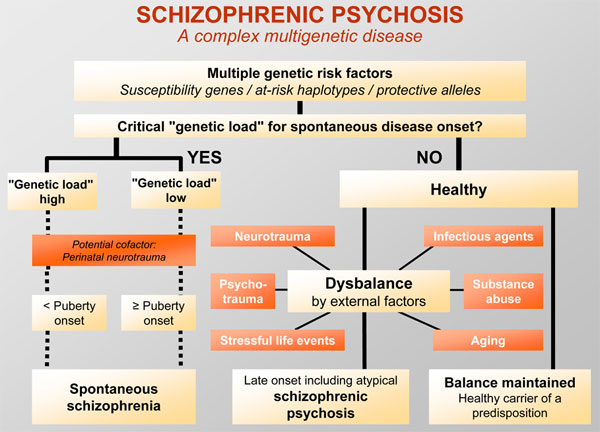 A mental health professional performing a psychological evaluation can determine if a mental health condition is involved and discuss next steps. If the psychosis is a symptom of a mental health condition, early action helps to keep lives on track.
A mental health professional performing a psychological evaluation can determine if a mental health condition is involved and discuss next steps. If the psychosis is a symptom of a mental health condition, early action helps to keep lives on track.
Psychosis
Psychosis includes a range of symptoms but typically involves one of these two major experiences:
Hallucinations are seeing, hearing or feeling things that aren’t there, such as the following:
- Hearing voices (auditory hallucinations)
- Strange sensations or unexplainable feelings
- Seeing glimpses of objects or people that are not there or distortions
Delusions are strong beliefs that are not consistent with the person’s culture, are unlikely to be true and may seem irrational to others, such as the following:
- Believing external forces are controlling thoughts, feelings and behaviors
- Believing that trivial remarks, events or objects have personal meaning or significance
- Thinking you have special powers, are on a special mission or even that you are God.
Causes
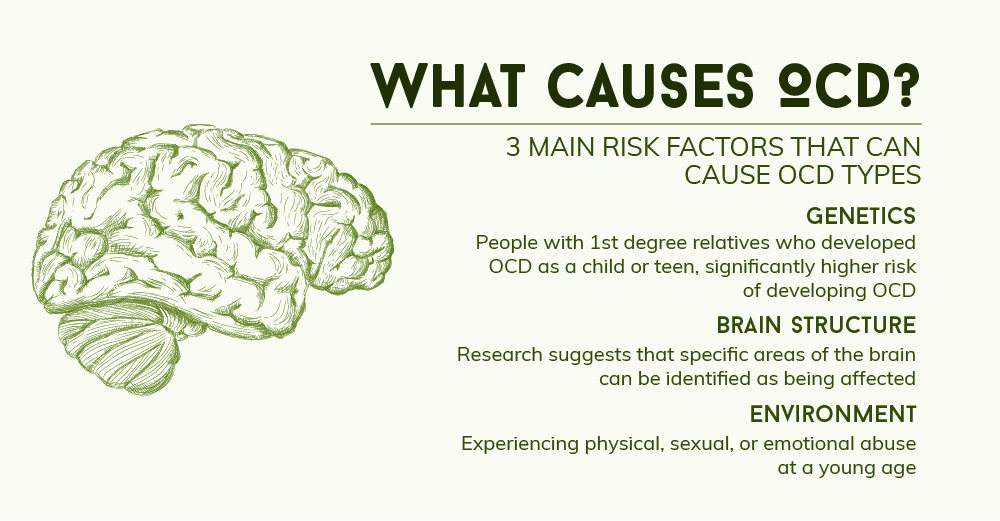
We are still learning about how and why psychosis develops, but several factors are likely involved. We do know that teenagers and young adults are at increased risk of experiencing an episode of psychosis because of hormonal changes in their brain during puberty.
Several factors that can contribute to psychosis:
- Genetics. Many genes can contribute to the development of psychosis, but just because a person has a gene doesn’t mean they will experience psychosis. Ongoing studies will help us better understand which genes play a role in psychosis.
- Trauma. A traumatic event such as a death, war or sexual assault can trigger a psychotic episode. The type of trauma—and a person’s age—affects whether a traumatic event will result in psychosis.
- Substance use. The use of marijuana, LSD, amphetamines and other substances can increase the risk of psychosis in people who are already vulnerable.

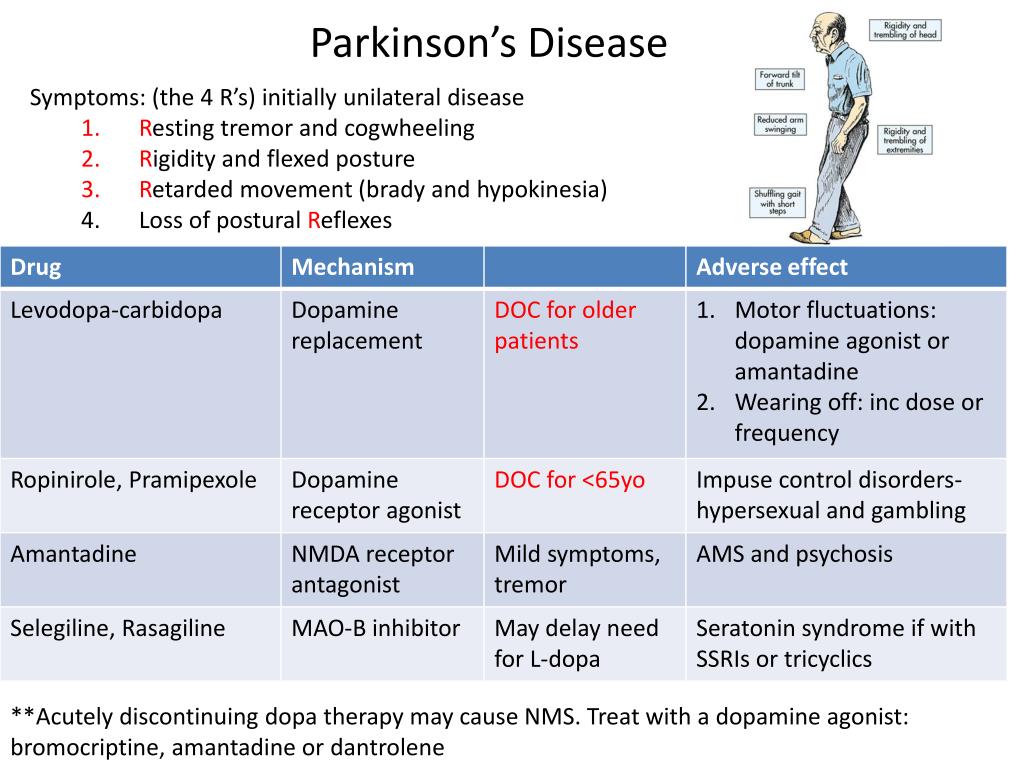
- Physical illness or injury. Traumatic brain injuries, brain tumors, strokes, HIV and some brain diseases such as Parkinson’s, Alzheimer’s and dementia can sometimes cause psychosis.
- Mental health conditions. Sometimes psychosis is a symptom of a condition like schizophrenia, schizoaffective disorder, bipolar disorder or depression.
Diagnosis
A diagnosis identifies an illness; symptoms are components of an illness. Health care providers draw on information from medical and family history and a physical examination to diagnose someone. If causes such as a brain tumor, infection or epilepsy are ruled out, a mental illness might be the reason.
If the cause is related to a mental health condition, early diagnosis and treatment provide the best hope of recovery. Research shows that the earlier people experiencing psychosis receive treatment, the better their long-term quality of life.
Treatment
Early or first-episode psychosis
Early treatment of psychosis, especially during the first episode, leads to the best outcomes.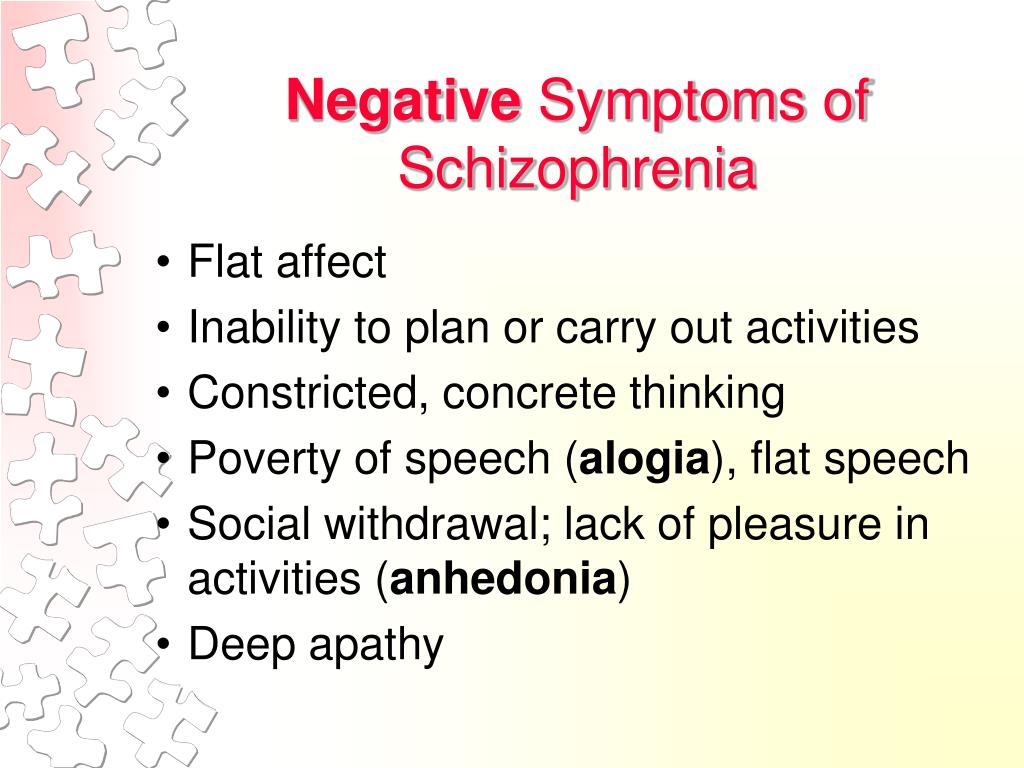
Research has shown significant success using a treatment approach called Coordinated Specialty Care (CSC). CSC uses a team of health professionals and specialists who work with a person to create a personal treatment plan based on life goals while involving family members as much as possible.
CSC has the following key components:
- Case management
- Family support and education
- Psychotherapy
- Medication management
- Supported education and employment
- Peer support
SAMHSA maintains an Early Serious Mental Illness (ESMI) Treatment Locator as a source of information for family members who are seeking CSC programs in the US. Portions of their website are available in Spanish.
Psychosis treatment
Traditional treatment for psychosis involves psychotherapy and medication. Several types of therapy have successfully helped individuals learn to manage their condition. In addition, medication targets symptoms and helps reduce their impact.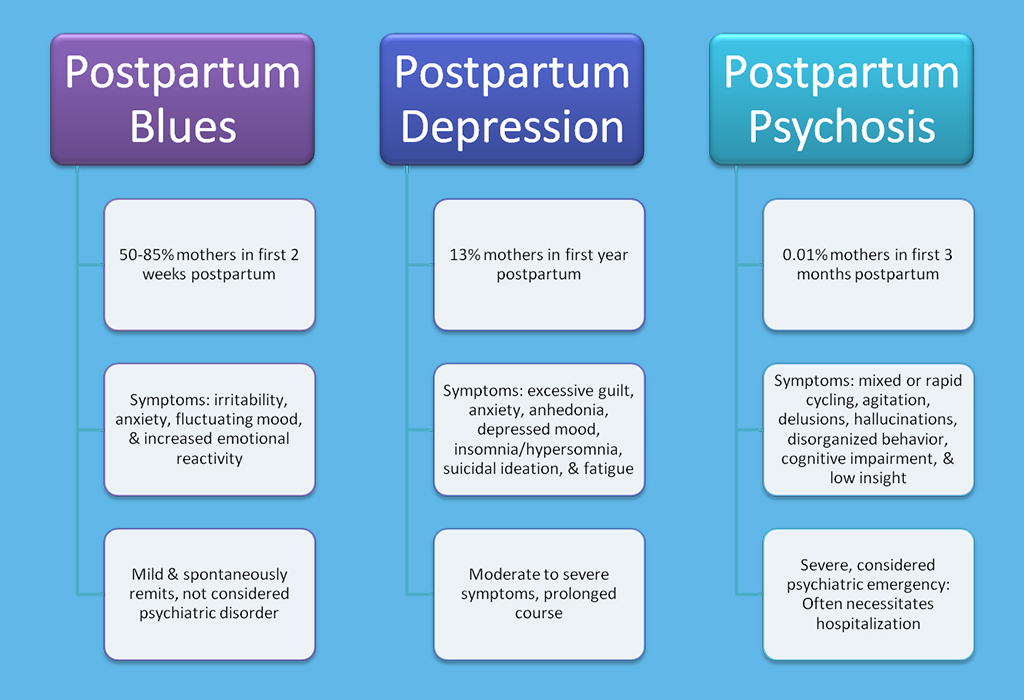
Related Conditions
Psychosis can be related to several mental health conditions:
- Bipolar Disorder
- Schizoaffective Disorder
- Schizophrenia
- Substance use disorders / Dual Diagnosis
Early Psychosis Intervention - CMHA Toronto
In the “What is Psychosis?” section, we go into more detail about the causes and treatment of psychosis. In this section, we concentrate on the importance of identifying the early warning signs of a developing psychoses, getting an assessment and initiating treatment to reduce the impact of the episode.
Let’s begin with a brief overview of psychosis.
What is Psychosis?
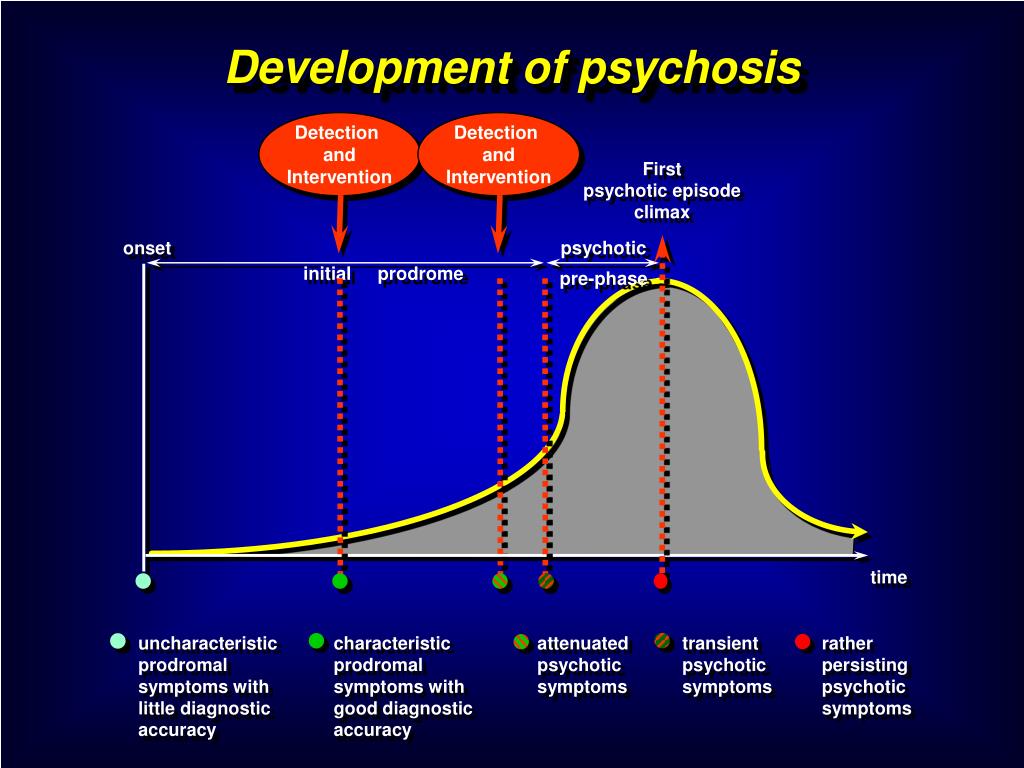
Psychosis describes a treatable medical condition that affects the mind and can result in some loss of contact with reality. People who suffer from psychosis often have prodromal and acute phases to their illness.
Prodromal Stage
The early stage prior to a full-blown episode of psychosis is known as the prodromal stage.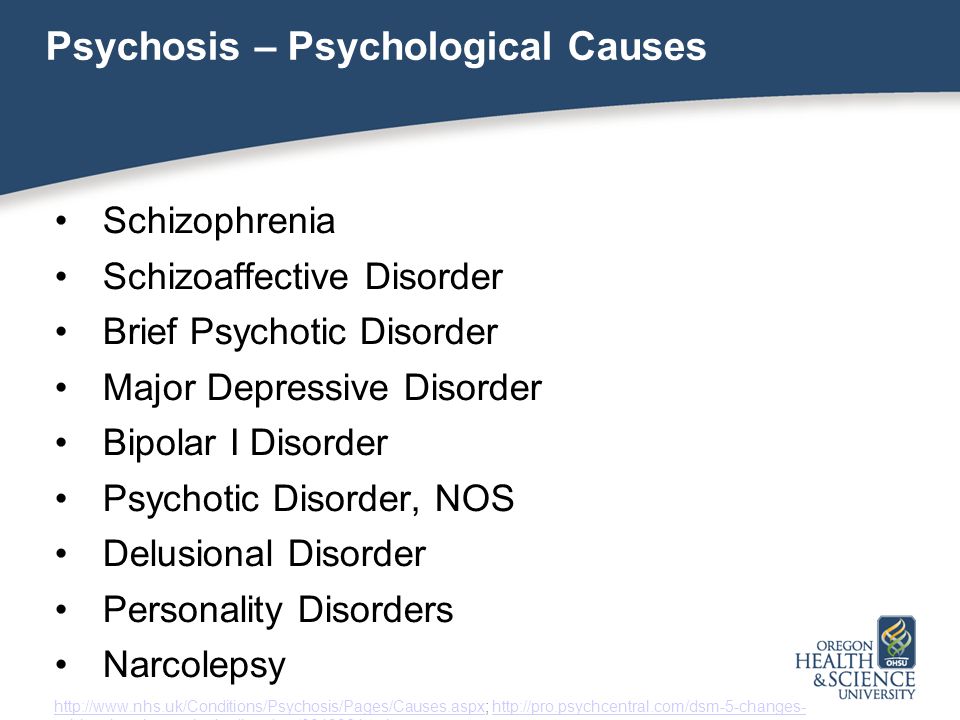 Symptoms of this phase are often subtle; they develop gradually and can be mistaken as “normal” behaviour, particularly in adolescents.
Symptoms of this phase are often subtle; they develop gradually and can be mistaken as “normal” behaviour, particularly in adolescents.
The duration of the prodromal stage can vary from person to person, however it commonly lasts for several months.
Prodromal symptoms can include:
- Withdrawal from friends and family
- Depression
- Tiredness
- Sleep disturbances
- Anxiety and/or suspiciousness
- Mood swings (extreme happiness to anger)
- Reduced ability to focus and feelings of disorientation
- A dislike to being touched by anyone
- An extreme sensitivity to noise, light, colours, textures
Acute Episode
If the prodromal stage is not recognized (or in some cases, does not occur) and treatment is not initiated, an individual’s condition will develop into an acute episode of psychosis. In this phase, a person will exhibit symptoms that are severe enough to impair day to day function.
They may include symptoms such as:
- Increased confusion – The person feels like their thoughts are racing around, speeding up or slowing down uncontrollably;
- Delusions – Otherwise called false beliefs, delusions range from paranoia to feelings of grandeur.
 For example, an individual believes he is being followed, his thoughts are being manipulated, or that he is able to control other peoples’ minds;
For example, an individual believes he is being followed, his thoughts are being manipulated, or that he is able to control other peoples’ minds; - Hallucinations – The individual sees, hears, smells or tastes things that are not present;
- Altered emotions – A person experiences greatly enhanced mood swings, “flat” mood or feelings of being disengaged;
- Behavioural changes – The individual acts differently than usual, exhibiting bouts of high and low energy, inappropriate laughter and sudden, unexpected bouts of anger.
An acute episode of psychosis is frightening for both the person suffering from the condition and for the people around them. It is a confusing, disruptive and potentially devastating time, particularly for young people who are just developing their self-image, their relationships and their view of a positive, productive future.
In most cases, psychosis will not go away on its own – detection and treatment are required before recovery can occur.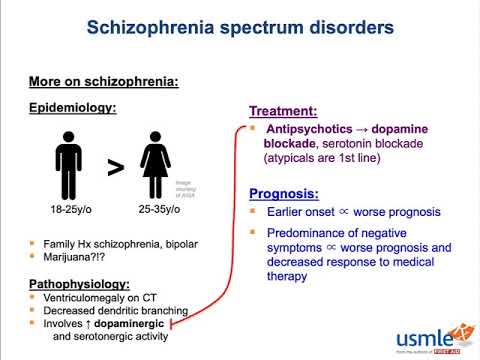
What is Early Psychosis Intervention?
We talk about treatment approaches in our pamphlet “What is Psychosis?” so we won’t repeat them here. However, we do want to talk about the critical importance of assessment and treatments as early as possible when a psychotic episode is developing.
Research has discovered that the sooner an intervention begins (in other words, the earlier identification, assessment and treatment start), the better the results. Once a psychotic episode is identified, the professionals who make up a treatment team can organize medications, education and support for the individual, as well as friends and family.
We refer to this as early psychosis intervention or EPI. EPI has been found to be so effective that the seriousness of a psychotic episode can be greatly reduced, and possibly even avoided, if treatment is started quickly and appropriately.
EPI reduces the impact of psychosis on a person’s activities, relationships and self-esteem.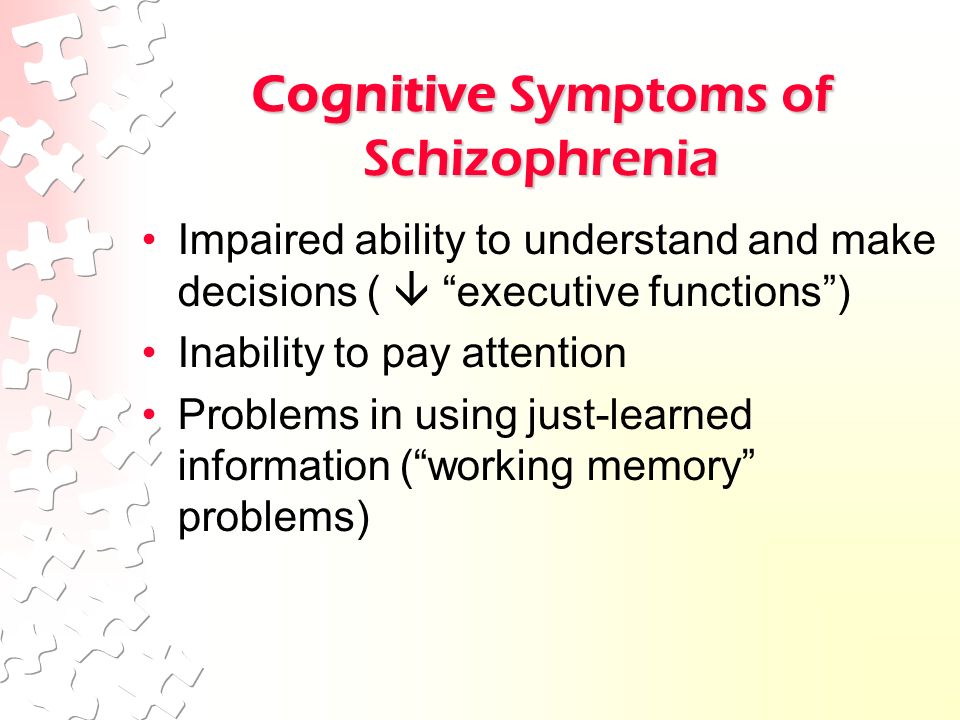 It reduces the risk of depression, suicide, substance use problems, hospitalization and relapses as well as helps with a faster, more complete recovery. All in all, EPI assists individuals in maintaining the life they have planned for themselves and reducing the effects of the illness.
It reduces the risk of depression, suicide, substance use problems, hospitalization and relapses as well as helps with a faster, more complete recovery. All in all, EPI assists individuals in maintaining the life they have planned for themselves and reducing the effects of the illness.
Obstacles to EPI
With all the benefits of EPI, why isn’t it used all the time? Early detection is the key; if early identification is not made, then treatment is delayed and the benefits of EPI are decreased.
The prodromal symptoms of psychosis are often not recognized as early warning signs. Sometimes people – including the person afflicted, family friends, and even the support professionals – do not identify behavioural changes as red flags to an impending psychotic episode. The individual who is undergoing the episode may feel “different”, but without the necessary awareness of prodromal symptoms, he may not understand the significance. Indeed, there may not be any significance to these feelings however if they continue, a medical assessment is required to rule out psychosis.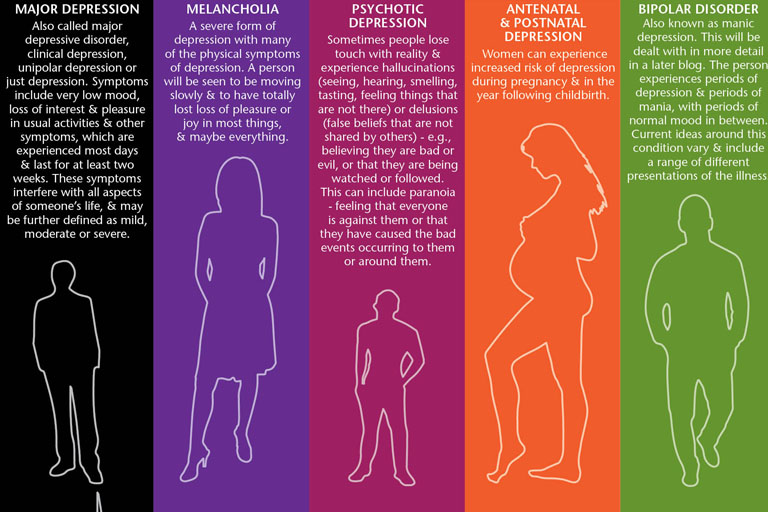
Even if an individual, or their loved ones, recognize that “something is wrong”, the prejudice and discrimination associated with mental illness can discourage people from seeking help. The misguided hope of a “wait and see” attitude leads people to delay treatment and in the process, only serves to prolong the disease process.
Don’t Delay – Act Today
If you, or someone you care about, suffer from psychosis, what can you do?
First, learn all that you can about psychosis, including the signs and symptoms of both the prodromal and acute stages. It is particularly helpful if you increase your knowledge about the subtle changes that occur in the early stages of a psychotic episode; learn to recognize them and act without delay. In the initial stages, it may only be the person with psychosis who actually notices small changes in the way they feel, and it is not until the psychosis develops that family and friends see the more obvious signs.
If you are part of the support network for a person with psychosis, be sure to encourage them to seek help if you see signs developing in their behaviour.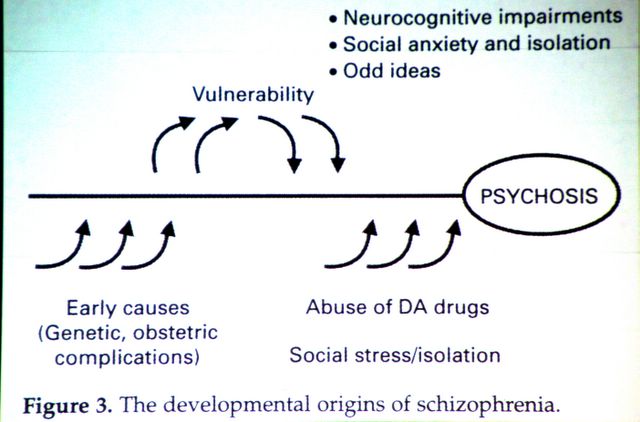 Help them to see their family doctor or mental health professional for an assessment. Ensure that the professionals they see are experienced in early psychosis, identification and treatment.
Help them to see their family doctor or mental health professional for an assessment. Ensure that the professionals they see are experienced in early psychosis, identification and treatment.
Finally, do all you can to shatter the stigmaaround mental illness. Our society tends to discriminate against those with any disease of the mind at the same time as we try to help those with physical ailments. Why? Fear and ignorance play a big role; dispel them by learning the facts and sharing that knowledge.
Put the Brakes on Psychosis.
Early psychosis intervention has been proven to be effective in reducing – even preventing – the symptoms of a psychotic episode. The sooner assessment and treatment are begun, the better the results of medication, counseling and support in helping a person cope with a psychotic episode.
If left unchecked, the symptoms of a psychotic episode will gather speed and a train wreck of tangled relationships, disrupted work or school activities and damaged self-esteem can result.
Learn all you can about early psychotic intervention and put the brakes on psychosis. Remember – psychosis is treatable.
Click Here to Download an Information Pamphlet
Psychosis - American Medical Clinic
Psychosis - a pronounced violation of the mental state, when the perception of a person contradicts the real situation. In this regard, there is a disorder in the perception of the real world and disorganization of behavior.
People who suffer from psychosis often become isolated and do not make contact. However, it is early diagnosis that contributes to the return to a normal lifestyle. As psychosis develops, the patient's behavior becomes less and less adequate, and consequences that are irreversible for the psyche arise.
Many of the symptoms of psychosis appear in a mild form before the onset of an exacerbation. However, it is very difficult to recognize them. However, if you do this and seek help in a timely manner, you will avoid serious consequences.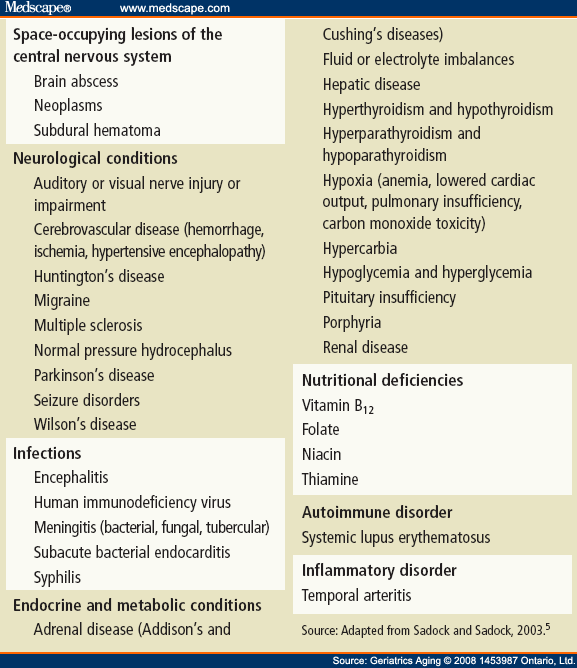
Early symptoms of psychosis
Do you feel a sudden change in your mental state? You should be concerned if you experience the following symptoms:
-
Character changes:
- irritability, nervousness, anxiety;
- hypersensitivity;
- lack of energy, interest, lack of initiative.
-
Changes in sensation:
- fears;
- depression.
-
Decreased performance
-
Changes in communication with people:
- self-closure;
- suspiciousness, incredulity;
- rupture of contacts with friends and acquaintances.
-
Change of interest:
- lack of interest in the former increase;
- unexpected interest in what was previously indifferent.
-
Changes in perception:
- feeling of extraneous influence, surveillance;
- changes in the perception of noise, color and smells.
Often these signs are attributed to transitional age, hormonal disruptions, etc. Do not listen to anyone, trust your feelings! If you are experiencing these symptoms, see your doctor. This will prevent the further development of mental illness at an early stage.
However, if the moment is missed, then psychosis can have extremely negative manifestations.
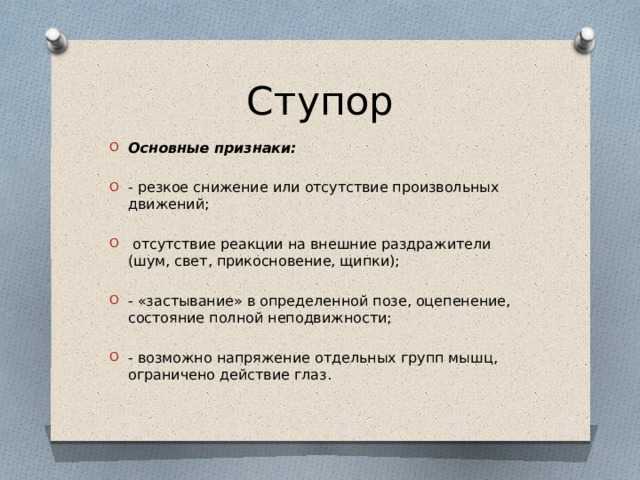
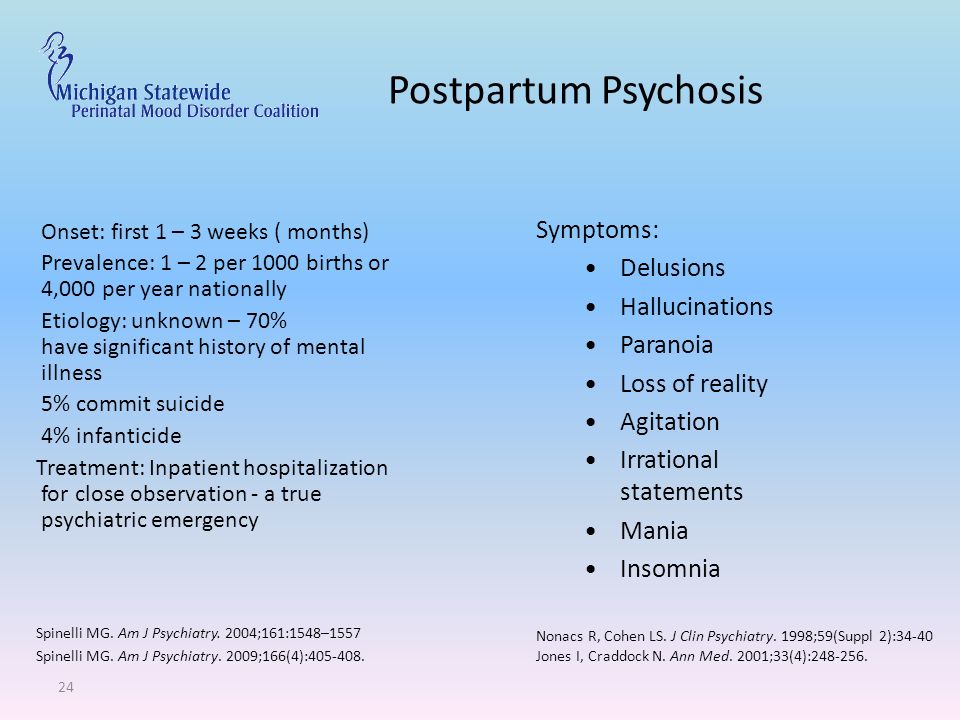
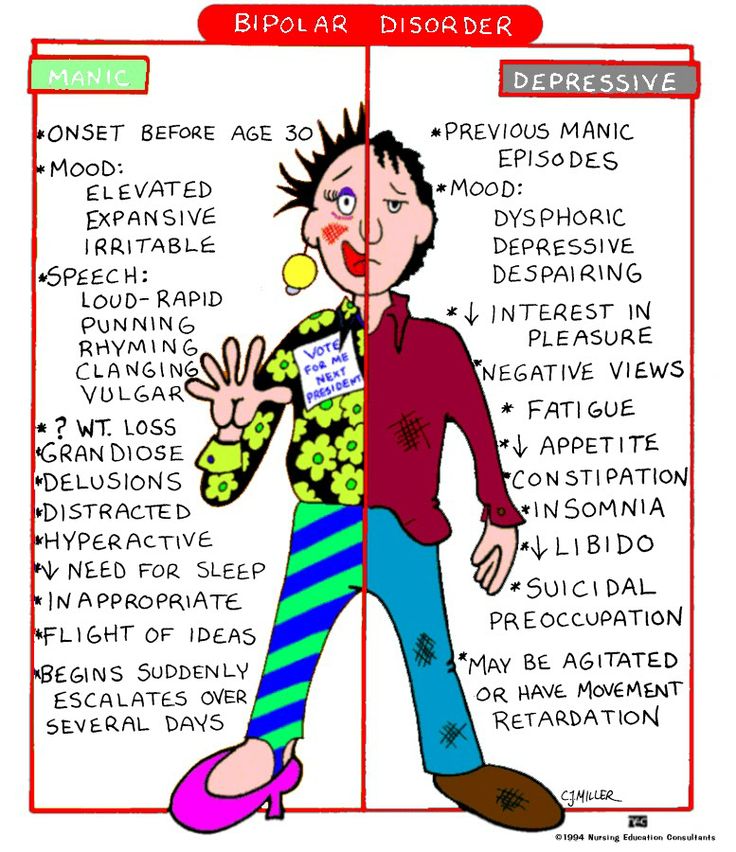
Manic-depressive psychosis
Manic-depressive psychosis is one of the most common forms of the disease. It is characterized by the alternation of manic and depressive phases with healthy periods. The duration of one phase is from three months to two years, the healthy period is usually longer and takes an average of 3.5 years.
Symptoms of depressive psychosis:
- sad mood;
- stiffness of movements;
- inhibition of thought processes.
With depressive psychosis, the patient is indifferent to everything and extremely depressed.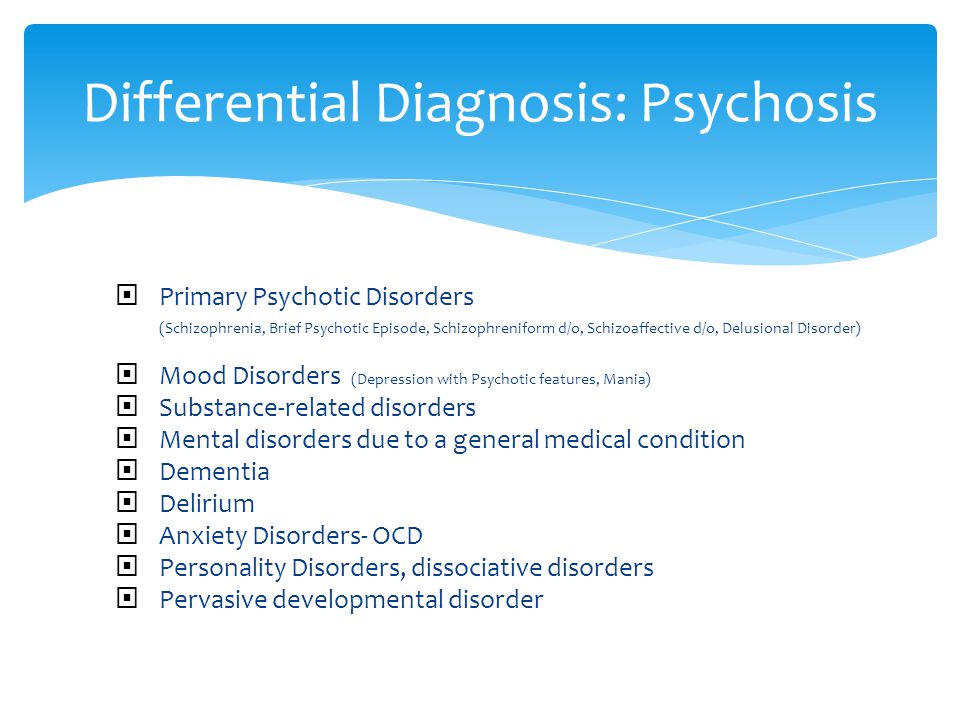 He answers all questions in monosyllables, with a delay. Can spend a long time in one position, almost without movement - lying or sitting on the bed.
He answers all questions in monosyllables, with a delay. Can spend a long time in one position, almost without movement - lying or sitting on the bed.
The depressive phase is characterized by a rapid increase in the disease to a certain peak. At this time, a feeling of worthlessness and meaninglessness of life can push the patient to suicide. After a short period, the disease gradually fades away.
Symptoms of manic psychosis:
- elevated mood;
- acceleration of thought processes;
- psychomotor agitation.
With manic psychosis, a person has everything around him that pleases him. The patient laughs a lot, communicates with people, actively gesticulates during dialogues. He often overestimates his strength, nominates himself for candidates that he does not match. Sleeps little and eats a lot.
The manic phase is usually shorter than the depressive phase and lasts from several days to several months.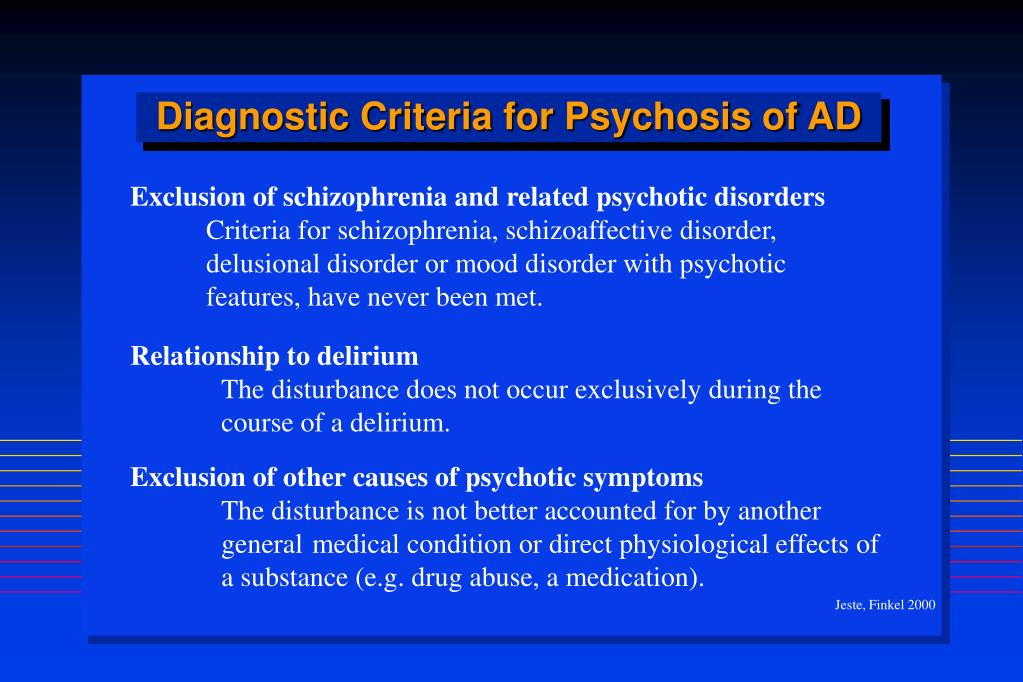 A seasonal course of the disease is characteristic - more often patients fall into a depressive phase in the fall, and into a manic phase in the spring.
A seasonal course of the disease is characteristic - more often patients fall into a depressive phase in the fall, and into a manic phase in the spring.
The “positive” side of manic-depressive psychosis is the absence of progressive personality changes, even with a long course of the disease. However, not all types of the disease are like this.
Alcoholic psychosis
Alcoholic psychosis is the general name for mental illness that occurs due to alcohol abuse. They are characterized by specific changes in the central nervous system and internal organs.
The most common type of alcoholic psychosis is delirium tremens. It occurs when there is a sharp reduction in alcohol consumption due to illness or injury.
She is characterized by the following symptoms:
- sleep disorders;
- causeless anxiety;
- excessive sweating;
- changeable mood;
- depressed state;
- trembling of hands and feet;
- increased heart rate.
During the day, the patient's condition is satisfactory, and at night there is delirium, auditory, visual and tactile hallucinations. It seems to a person that insects are crawling on him, he sees dead relatives, he hears reproaches from various voices.
If left untreated, alcoholic psychosis causes serious complications - a person becomes stupid, dumb and forgets a lot of information known to him. In addition, irreparable damage to internal organs is caused. Perhaps the development of cirrhosis of the liver, coronary heart disease, stomach ulcers, etc.
Treatment of psychosis
Psychosis, as a rule, requires hospitalization so that the patient cannot harm himself or those around him.
The rehabilitation course includes drug therapy along with psychological help. In addition, physiotherapy is used, which relieves emotional stress and training programs that develop a positive outlook on the world in a person.
Remember that the timely start of treatment for psychosis of any kind is the key to a speedy return to your usual way of life and the prevention of irreversible mental abnormalities.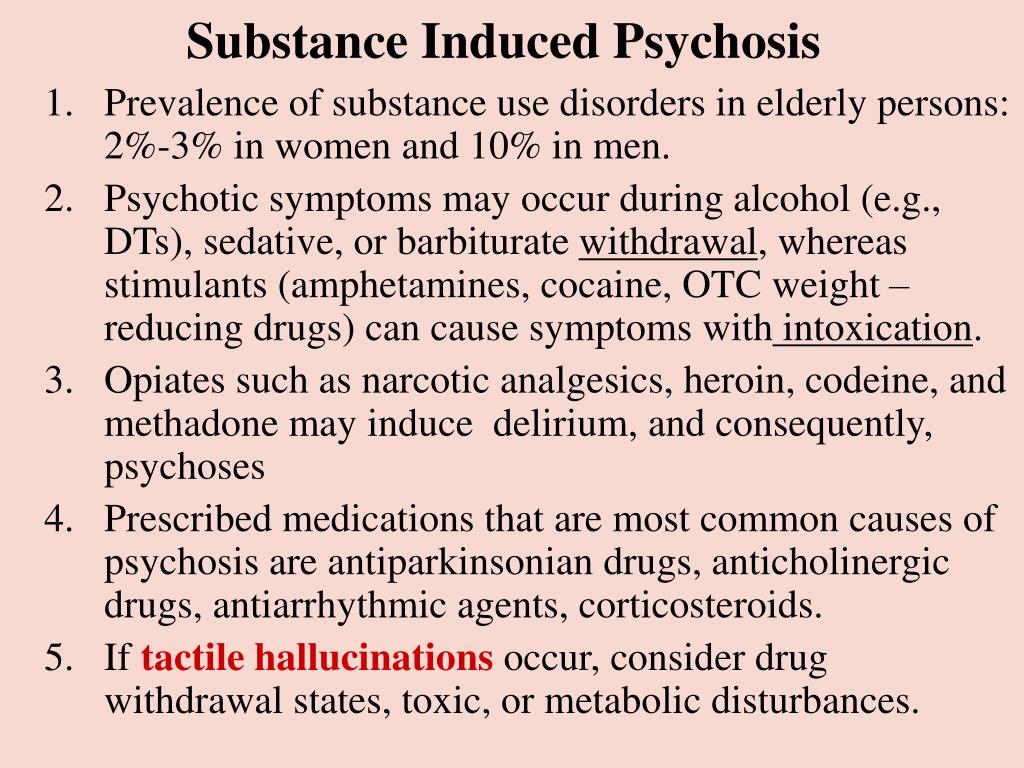
Psychosis - Hadassah Medical Moscow
Psychosis is a mental illness. Under it, a person cannot adequately behave, he does not perceive the world around him and does not react to it. At the initial stages, psychosis can be recognized by changes in behavior, atypical reactions appear in a person, and the emotional background is disturbed. He can't handle his
feelings, expresses emotions inappropriate to situations. If you or your loved ones experience these symptoms, you should immediately consult a doctor. The appearance of psychosis may indicate the development of schizophrenia, delirium tremens, senile dementia and other serious diseases.
Full text
Symptoms of psychosis
Psychosis is a group of psychotic disorders. Their manifestations depend on the specific type of violation. However, all of them are characterized by a gradual increase in signs, a change in behavior. You can recognize the symptoms of psychosis by the following manifestations:
- Hallucinations - can be auditory, visual, gustatory, tactile, olfactory;
- Crazy ideas - there are obsessive thoughts and judgments that do not correspond to reality.
 A person may feel that he is being watched;
A person may feel that he is being watched; - Movement disorders - periods of excitement are replaced by a sharp stupor;
- Mood disorders - apathy, melancholy, indifference to everything;
- Manic disorders - excessive aggressiveness, building unrealistic plans, a sharp addiction to alcohol, promiscuity;
- Emotional disorders - a person cannot express his feelings, he does not relate his feelings to what is happening.
Make an appointment
Leave your number, our operator will answer all your questions in detail
for problems in the work of neurons. Due to the violation of bonds in the molecules, they do not receive nutrition, they experience a lack of oxygen. This leads to the fact that neurons cannot transmit nerve impulses - multiple disorders occur in the central nervous system. The type of psychosis that occurs depends on which part of the brain suffered from a hunger strike. The causes of this disease are of 3 types:
- Endogenous, associated with internal processes.
 These can be endocrine, neurological disorders, bronchial asthma, vitamin B deficiency, conditions accompanied by acute pain (ulcer, heart attack, sarcoidosis), electrolyte imbalance, systemic diseases, genetic predisposition, age;
These can be endocrine, neurological disorders, bronchial asthma, vitamin B deficiency, conditions accompanied by acute pain (ulcer, heart attack, sarcoidosis), electrolyte imbalance, systemic diseases, genetic predisposition, age; - Exogenous, or external: stress, intoxication with alcohol, drugs, drugs, consequences of infectious processes, mental trauma;
- Organic, when changes in the brain become the cause of psychosis: tumors, injuries, hemorrhages.
Psychosis diagnostic methods
Psychologist diagnoses psychosis. At the first appointment, he conducts a pathopsychological examination: he studies human behavior, asks questions to determine the process and course of thinking. It is necessary to understand how the patient reacts to the world around him. Relatives of a sick person are also involved in the diagnosis of psychosis - they will help to collect a complete clinical picture. Further diagnostics include
X-ray of the brain
MRI of the brain
Electroencephalogram
Blood test for hormones
Urinalysis for drugs and alcohol
Methods of treating psychosis
Psychosis is usually treated in a hospital setting.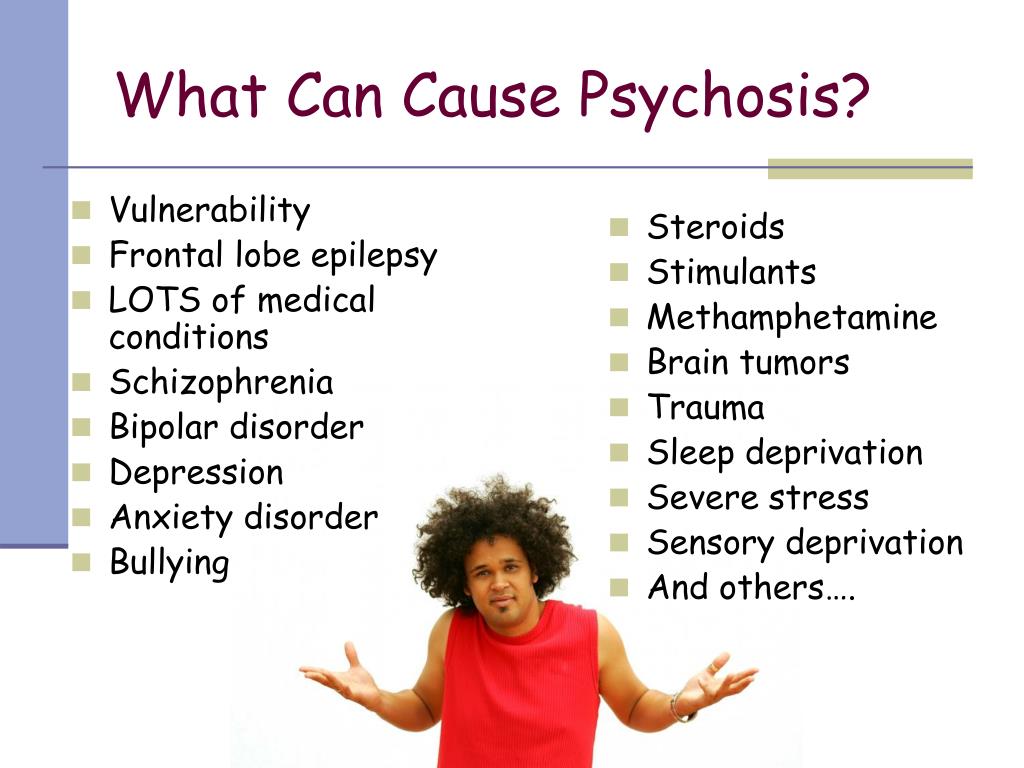 Such patients require hospitalization, as they cannot control their actions, they can harm themselves and others. The basis of therapy is taking medications, including:
Such patients require hospitalization, as they cannot control their actions, they can harm themselves and others. The basis of therapy is taking medications, including:
- Antipsychotics - stop psychosis, relieve delirium and hallucinations;
- Atypical antipsychotics - restore neurochemical connections;
- Nootropics - restore brain function, improve mental activity;
- Normotimics - prevent the development of depressive and manic tendencies;
- Antidepressants - relieve symptoms of depression.
Treatment of psychosis necessarily includes psychotherapy. The patient will have to work with a psychologist for a long time in order to successfully return to society. In some forms of the disease, an electroconstrictive effect is shown, in which the current restores the metabolic processes of the nervous system in the brain. A good effect in the treatment gives physiotherapy: acupuncture, exercise therapy, reflexology.
Prevention and treatment programs for psychosis at the Hadassah Clinic
Psychosis is a relapsing disease.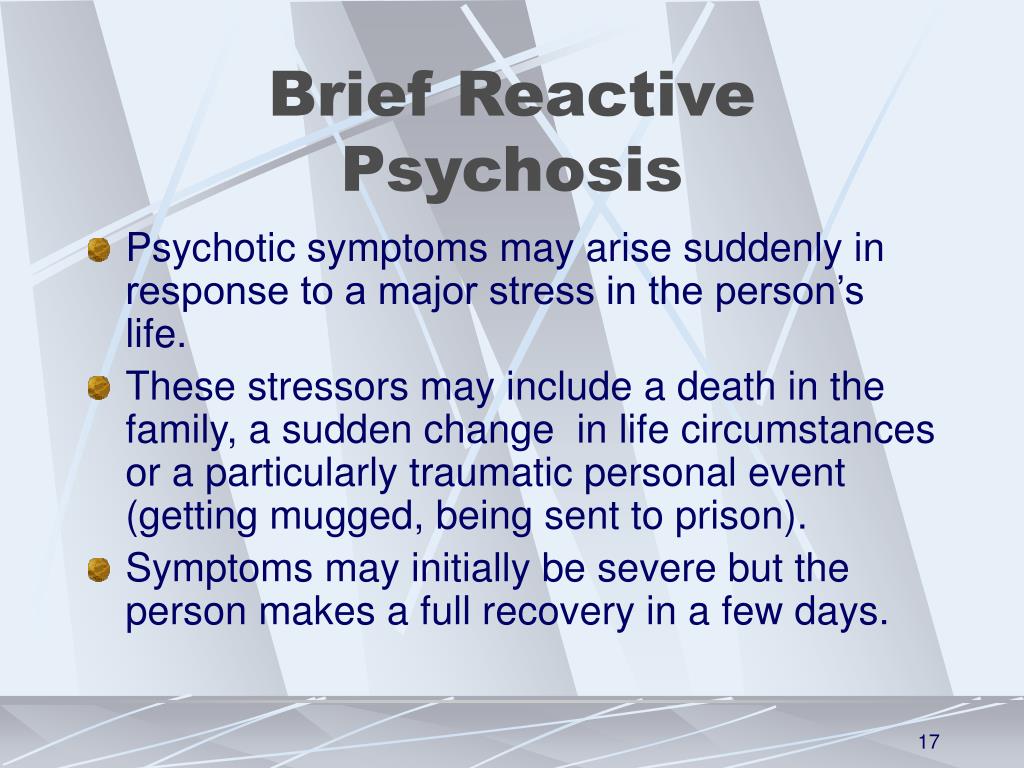 With timely and comprehensive treatment, the prognosis will be favorable. However, the patient will have to undergo preventive examinations for several more years. If the patient follows all the recommendations of the doctor, the likelihood of exacerbations in the future will be minimal. To prevent the development of psychosis, you need to monitor your physical and mental health. For this:
With timely and comprehensive treatment, the prognosis will be favorable. However, the patient will have to undergo preventive examinations for several more years. If the patient follows all the recommendations of the doctor, the likelihood of exacerbations in the future will be minimal. To prevent the development of psychosis, you need to monitor your physical and mental health. For this:
- Eat a healthy and balanced diet;
- Give up bad habits, especially the use of alcohol and drugs;
- Avoid stressful situations;
- Avoid physical and psycho-emotional overload;
- Seek medical attention for all head injuries;
- See a therapist if necessary;
- Observe the daily routine;
- Communicate more.
Psychosis is an insidious and dangerous problem. And it is very important to notice it in time and start treating it. If you see signs of approaching psychosis in yourself or loved ones, you should immediately consult a doctor.