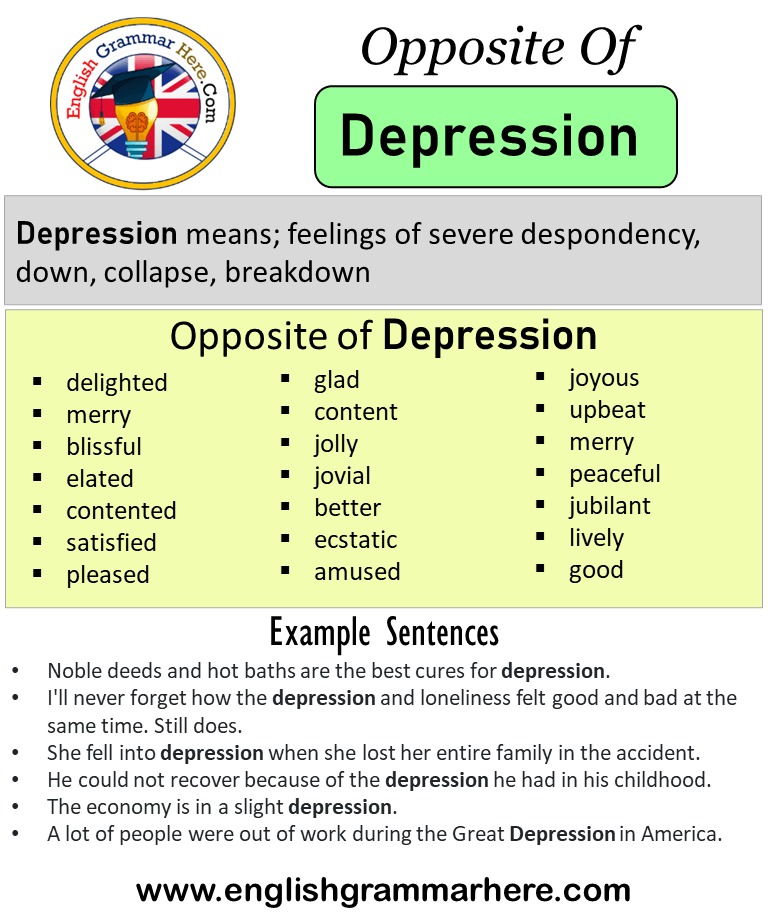
Opposite of postpartum depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.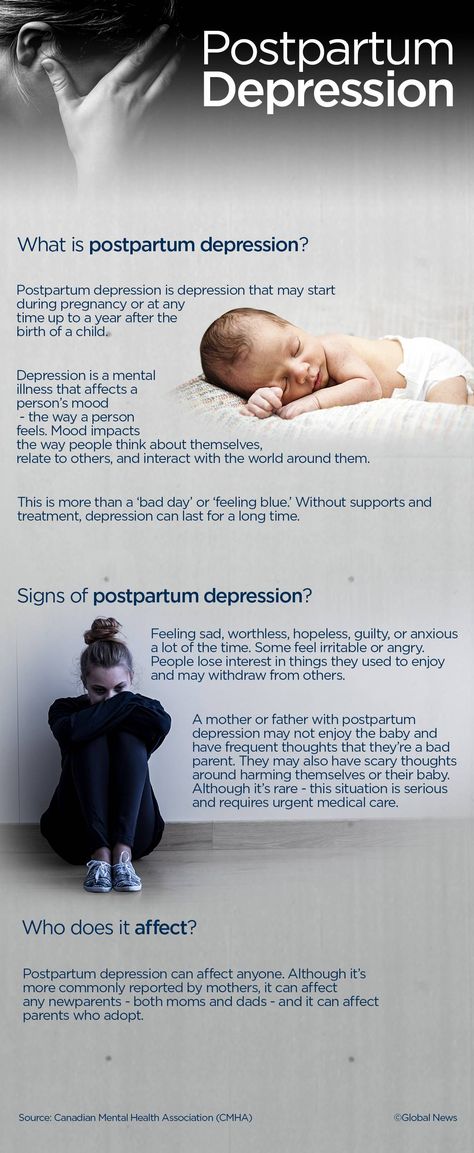 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.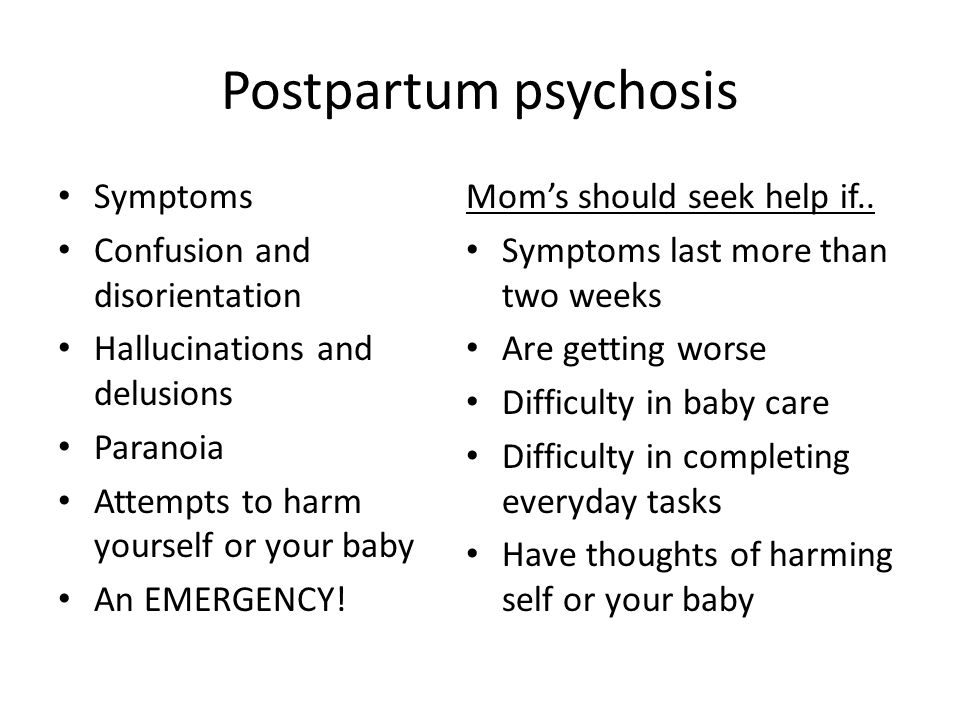
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Error 404 | Regional perinatal center
UPDATED NEWS!
⚡⚡⚡ From February 6 to February 10, the appointment of patients with Guryev DL, Deputy Chief Physician for Medical Affairs, is cancelled.
-00-04 / 41-4516-2022 due to the excess of the epidemiological threshold for acute respiratory viral infections among the population of the Yaroslavl region on the basis of clause 10.5 of the Resolution of the chief state sanitary doctor for the Yaroslavl region dated 05. 12.2022 No. 21 "On the announcement of an epidemiological rise in the incidence of influenza and ARVI among the population of the Yaroslavl region" in order to prevent the nosocomial spread of respiratory viral infections for the period of circulation of influenza viruses and other respiratory viruses of non-influenza etiology, a ban on visits to structural units of stationary-type institutions by visitors was introduced.
12.2022 No. 21 "On the announcement of an epidemiological rise in the incidence of influenza and ARVI among the population of the Yaroslavl region" in order to prevent the nosocomial spread of respiratory viral infections for the period of circulation of influenza viruses and other respiratory viruses of non-influenza etiology, a ban on visits to structural units of stationary-type institutions by visitors was introduced.
Based on the foregoing, the presence of relatives during the delivery of a pregnant woman (partner birth) is equated to visiting patients in structural units of a stationary type.
Removal of restrictions will be possible with the improvement of the epidemiological situation for influenza and SARS in the Yaroslavl region.
⚡⚡⚡
Memo for medical workers on the differential diagnosis of COVID-19 with influenza and SARS, determining the tactics of managing patients, including children, the elderly and pregnant women with the algorithm of actions of medical workers providing medical care on an outpatient basis , including at home, to patients with acute respiratory viral infections and Leaflet for the public (link) on the prevention and treatment of seasonal influenza, COVID-19, RS infection and other acute respiratory viral infections (letter of the Ministry of Health of the Russian Federation of November 28, 2022 No. 30-4 / I / 1-20344)
30-4 / I / 1-20344)
------------------------------------------------ -------------------------------------------------- -------------------------------------------------- ---------
⚡⚡⚡
Given the epidemiological situation, there is currently a restriction on visits to inpatient departments of the Perinatal Center.
⚡⚡⚡ Helpline on reproductive selection and crisis states 8 (4852) 78-81-70- Psychological and Social Service of the GBUZ "Regional Perinatal Center"
Information information for patients with infertility who need ART
In accordance with the order of the Ministry of Health of the Russian Federation dated July 31, 2020 No. 803n “On the procedure for using assisted reproductive technologies, contraindications and restrictions on their use”, which entered into force on January 1, 2021, the presence of indications ART programs are carried out by the attending physician. He also draws up a referral for infertility treatment by IVF.
He also draws up a referral for infertility treatment by IVF.
To get a referral, you need to consult a fertility doctor at the reproductive health department of the Regional Perinatal Center, who decides on referral to the IVF program. Recording by phone registry (4852) 78-81-96.
⚡⚡⚡ Citizens' Instructions for Asymptomatic or Mild Novel Coronavirus Infection and Acute Respiratory Virus Infection (Download full memo, download short memo)
Coping with symptoms of postpartum depression
- Home ::
- What we work with ::
- Postpartum depression
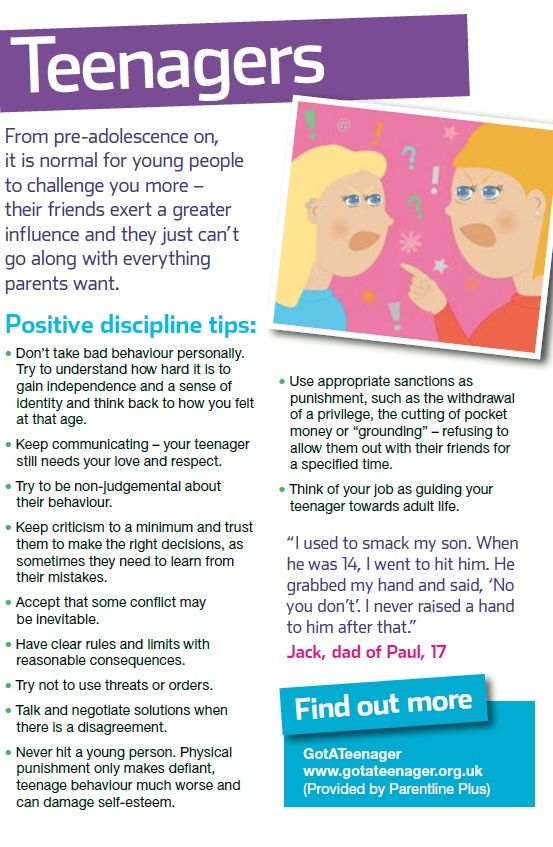
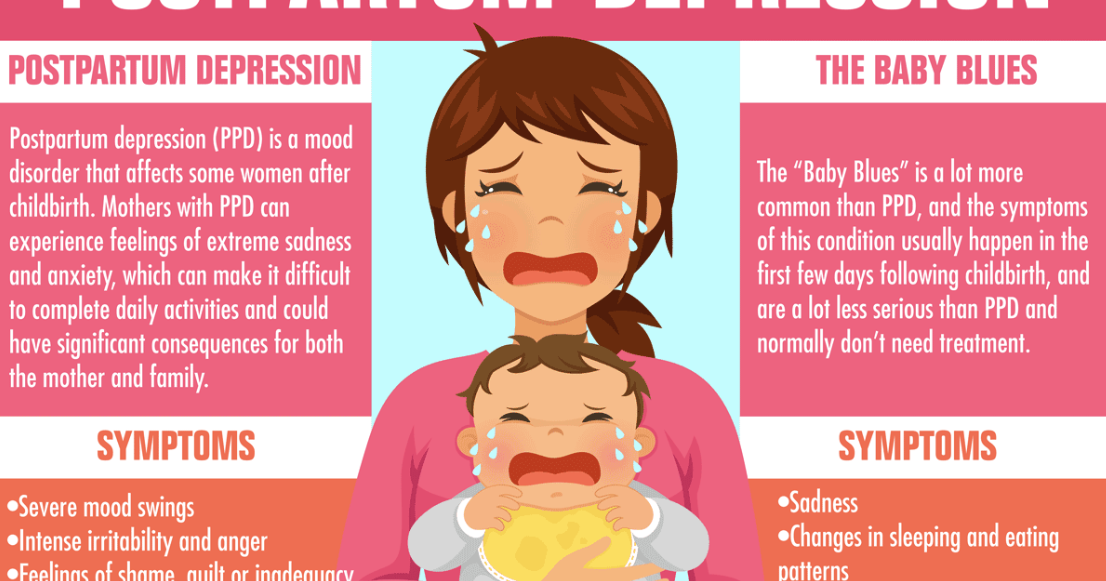
According to various sources, the prevalence of postpartum depression reaches 10-15% and is a serious problem not only for mothers themselves, but also has a huge negative impact on the development of the child, both in the short and long term.
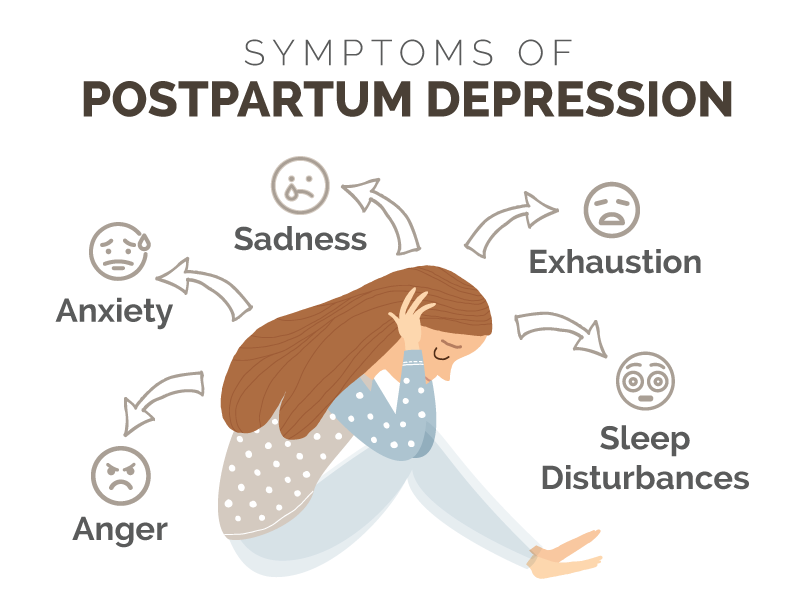
Symptoms of postpartum depression
Signs of postpartum depression include complete unwillingness and inability to communicate with the child, apathy and similar symptoms, as well as the opposite state of constant anxiety about the child, his condition, the inability to leave the child even for a minute, the impossibility entrust it to someone for the shortest possible time and the almost complete exclusion of all kinds of social contacts.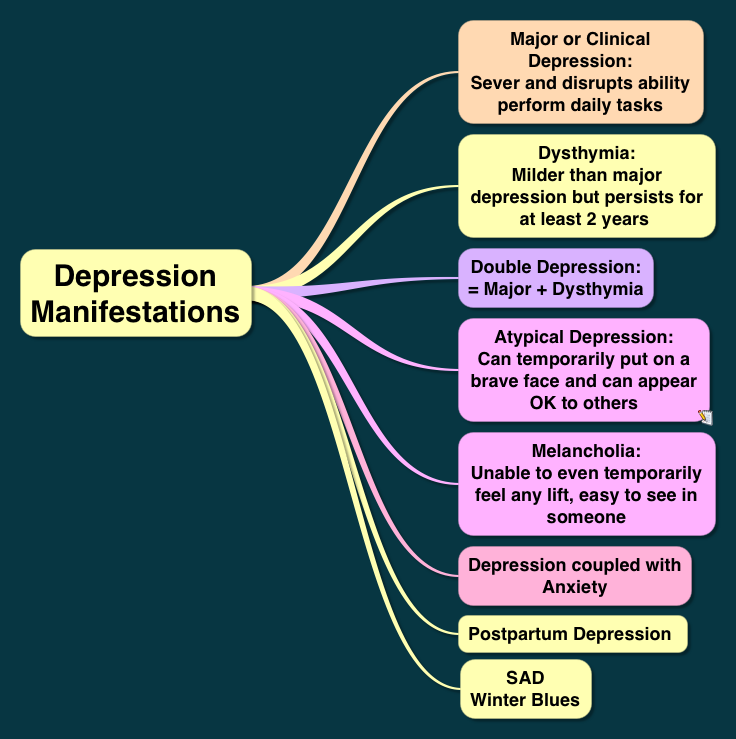
- Anhedonia - a symptom characteristic of depression in general - in the case of postpartum depression, it manifests itself in the absence of a sense of joy from life. Things and activities that were previously pleasant and loved are no longer perceived as such, not because they lack the strength or time, but precisely because of the loss of the ability to enjoy. An example is the loss of sexual desire and pleasure from having sex.
- Extreme irritability . Outbursts of anger and anger, followed by feelings of guilt, are also a common symptom of postpartum depression. Often, irritation is replaced by periods of feeling helpless patience and doom, through which, after a while, irritation breaks out again.
- The feeling of guilt experienced by mothers is often a serious obstacle in treatment, because it is precisely this feeling that most mothers do not seek professional help.
- Remorse related to the performance of maternal duties.

- Feeling of isolation , loneliness, misunderstanding on the part of loved ones.
- Postpartum depression often accompanies sleep and appetite disorders .
Duration of postpartum depression
Postpartum depression may last from several weeks to several years. It is a great regret that the majority of women suffering from this disorder do not receive the necessary help and the problems of their condition are not diagnosed, despite the fact that the supervision of the mother and child is carried out by a large number of specialists.
Love, hate and ambivalence towards a child
Achieving an ambivalent attitude towards a child – the ability to feel love for a child and at the same time strong negative feelings towards him – represents the achievement of a mature attitude towards a child. Ambivalence acts here as the opposite of a conflict relationship, when love and hatred for the child are incompatible. Therefore, both of these feelings cannot coexist together, but are experienced alternately: either as excessive, grotesque concern for the child, or as uncontrollable outbursts of anger. Awareness of this internal conflict, feelings of anger, rage and hatred for the child is accompanied by a deep sense of guilt and inferiority, so negative feelings are repressed.
Therefore, both of these feelings cannot coexist together, but are experienced alternately: either as excessive, grotesque concern for the child, or as uncontrollable outbursts of anger. Awareness of this internal conflict, feelings of anger, rage and hatred for the child is accompanied by a deep sense of guilt and inferiority, so negative feelings are repressed.
Hatred for a child, which does not exclude warm feelings, love and tenderness, but rather is an integral part of them, the reverse side - turns out to be a forbidden feeling. Displaced into the area of the unconscious, these feelings become the cause of increased anxiety. The mother's own aggression, being repressed and, as a result, poorly controlled, poses a danger to the child. Being incapable of experiencing these feelings as phenomena of her inner world, the mother perceives her own aggression as an external danger, and anxiety takes the place of hatred. When asked about worries about the child, such mothers often talk about fantasies filled with violence and aggression against the child, but the source of danger is either other people or some impersonal factors (diseases, viruses, fires, sharp objects, etc.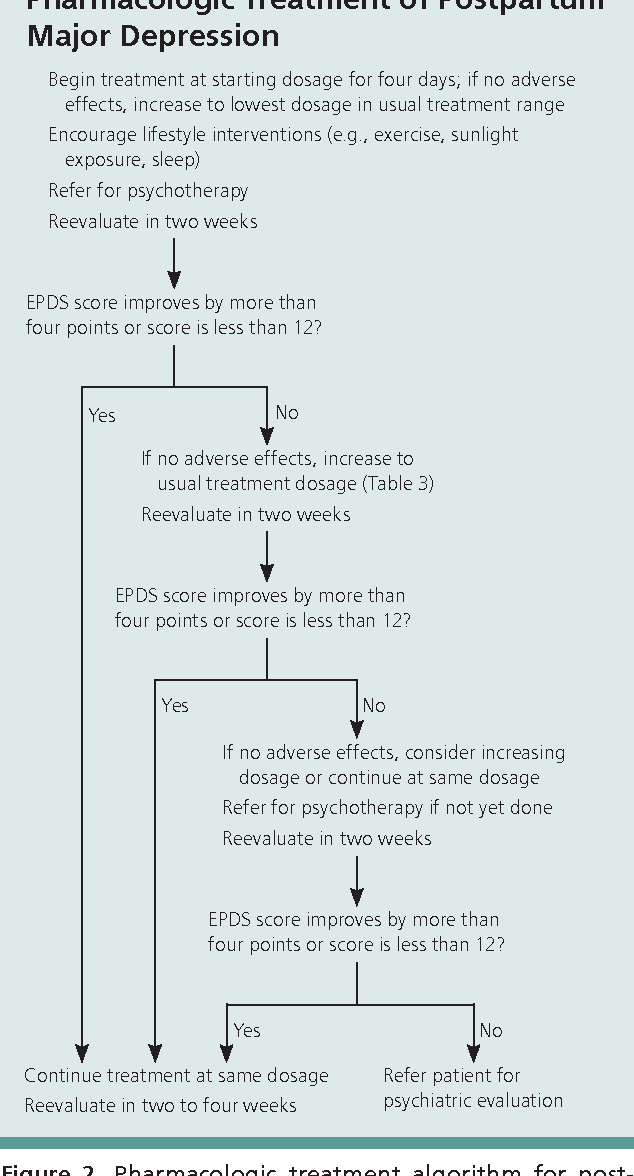 ) . Erupting into consciousness in the form of outbursts of irritability and anger, aggressive feelings cause a strong sense of guilt and shame, which only increases the feeling of depression, failure and alienation. The return of their own aggressive feelings, the opportunity to find expression for them without destructiveness and feelings of guilt - often brings such mothers great relief.
) . Erupting into consciousness in the form of outbursts of irritability and anger, aggressive feelings cause a strong sense of guilt and shame, which only increases the feeling of depression, failure and alienation. The return of their own aggressive feelings, the opportunity to find expression for them without destructiveness and feelings of guilt - often brings such mothers great relief.
Another way to deal with one's own aggressive impulses towards the child is to transfer one's own feelings to the child's father. This is not about telepathy or other similar paranormal phenomena, but about situations that are quite common in families, when the source of restrictions, demands, discontent towards the child is exclusively the father, while the mother is the complete opposite. Psychotherapeutic work allows spouses to feel like a couple that has and maintains common requirements for the child, common and agreed ideas about the development of the child, etc.
Factors affecting the development of postpartum depression
- Factors that increase the risk of developing postpartum depression include a history of depression in the mother .
- Severe pregnancy and complicated delivery also increase the risk of developing emotional disorders in the postpartum period.
- The presence or absence of social support (especially from the more experienced woman and, more importantly, from the spouse) will influence the emotional state of the mother and the interaction in the mother-child dyad.
- With regard to demographic data, such as education level, income level, the statistics speak in favor of the fact that less socially protected segments of the population are more prone to developing depression including in the postpartum period. There is also a higher percentage of development of postpartum depression among underage mothers compared with nulliparous peers. The second age-related rise in the incidence of postpartum depression occurs after 40 years.
- An unfavorable factor is separation of mother and child immediately after childbirth , including separation for medical reasons.
The appearance of a child, especially in the early postnatal period, when the mother-child bond is so strong, aggravates the woman's own internal conflicts , including those associated with her own mother.
Many mothers suffering from postpartum depression tend to expect during pregnancy that with the birth of a child, love for him will appear, which will solve all the difficulties and problems that have appeared with the child. However, it often turns out that love for a child is not always born with him, but is the result of a longer and laborious period of adaptation of the mother to the child and vice versa. Deep disappointment and the accompanying guilt that a woman does not experience a long-awaited tender feeling often accompanies postpartum depression.
A woman's life during pregnancy has a significant impact on the likelihood of developing postpartum depression. The more negative events a mother has experienced during pregnancy, the higher the likelihood of developing postpartum depression.
An important factor influencing the development of postpartum depression is relationship with a spouse . Relationships in a married couple are changing, which requires the spouses to restructure relationships, adapt the family system to the new state of affairs.
Types of postpartum depression
According to the level of psychopathology, one can speak of neurotic and psychotic depression. In some cases, these are conditions that are treatable on an outpatient basis, while in others hospitalization may be necessary. The main criterion for hospitalization should be the presence of a threat to the life and health of the mother and child, as well as danger to others.
According to the type of course, one can speak of short-term depressive episodes, periodic depressive states and prolonged depression.
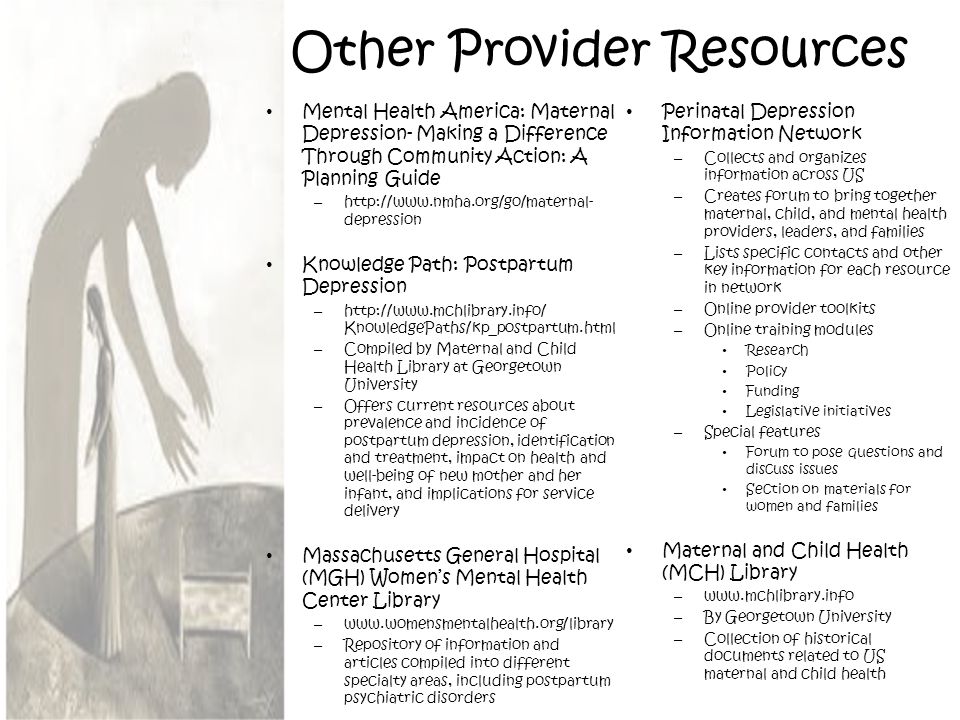
Treatment of postpartum depression
Among the methods of treatment we can highlight:
- Drug treatment;
- Individual psychotherapy and counseling;
- Family psychotherapy;
- Psychotherapy of interaction in the mother-child dyad.
In cases of severe symptoms, the presence of psychotic components (eg, delusions), as well as a prolonged course of the disorder, medical treatment of depression is resorted to. In some cases, in a hospital setting.
Individual psychotherapy and psychological counseling allow patients to better understand and regulate their emotional attitude to the child, to themselves, to their spouse, help resolve internal conflicts and learn new ways of relationships.
Family psychotherapy involves a greater involvement in the treatment process of the whole family, mobilizing the possibilities of social support and facilitating the adaptation of all family members to a new state of affairs, new roles, to each other.
A separate place in the treatment of postpartum mental and behavioral disorders, including postpartum depression, is occupied by the therapy of dyadic relations between mother and child. The specialist, having the opportunity to observe the interaction of mother and child (directly or watching a video), discusses with the mother her own behavioral and emotional reactions to the child and the child's reactions to her.