Is propranolol addictive
Propranolol FAQs: 25 Common Questions Answered
Searching for information about propranolol? Approved by the FDA for more than 40 years and prescribed to millions of American adults, propranolol is one of the most common beta blockers used to treat heart conditions, anxiety, headaches and other health issues.
Below, we’ve answered 29 of the most frequently asked questions about propranolol, covering everything from propranolol’s common dosages to primary effects, potential side effects, using propranolol for anxiety and more.
What is Propranolol?
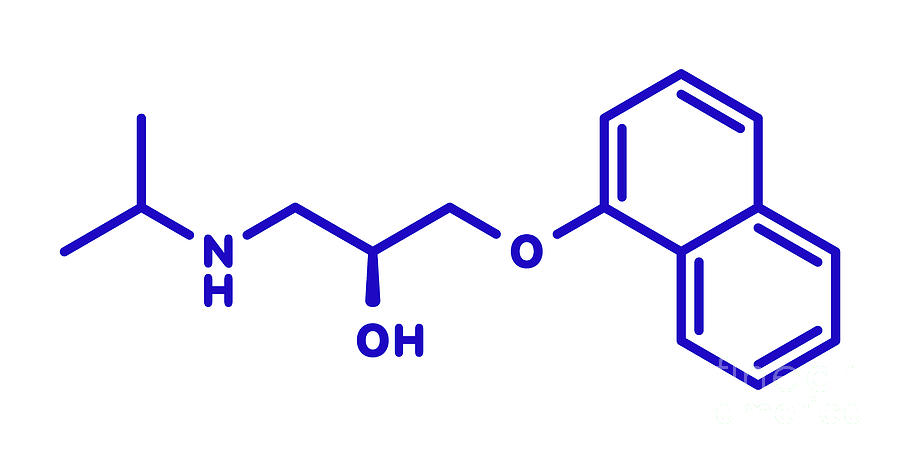
Propranolol is a beta blocker medication. It works by blocking the effects of stress hormones, such as adrenaline (epinephrine) and noradrenaline (norepinephrine) on beta receptors in the heart, lungs and other tissue.
Originally developed in the 1960s, propranolol was initially approved by the FDA in the 1970s and has been on the market for decades as a treatment for several conditions.
Our guide to beta blockers goes into more detail on how propranolol and similar beta blocker medications work.
What is Propranolol Used For?
Propranolol is used to treat several medical conditions, including those that affect the vascular system and heart.
Currently, propranolol is used to treat hypertension (high blood pressure), heart arrhythmia (an irregular heartbeat), hypertrophic subaortic stenosis (heart muscle disease) and angina (a form of chest pain caused by poor blood flow to the heart).
Propranolol is also prescribed to improve general health in people who’ve suffered myocardial infarction, or heart attack.
In some cases, propranolol is used to treat benign essential tremor -- a disorder that can cause uncontrollable shaking in the hands, arms, head, neck and torso -- and restless leg syndrome.
Like many other medications, propranolol is also sometimes prescribed off-label for uses other than those approved by the FDA.
For example, propranolol is often prescribed as an off-label treatment for some forms of anxiety, such as performance anxiety. When used as an anxiety medication, propranolol can reduce the severity of some physical anxiety symptoms, such as sweating and an elevated heart rate.
When used as an anxiety medication, propranolol can reduce the severity of some physical anxiety symptoms, such as sweating and an elevated heart rate.
Our guide to propranolol and performance anxiety goes into more detail about how propranolol can work as an off-label anxiety treatment.
online counseling
the best way to try counseling
Is Propranolol Available Over the Counter?
No. Propranolol is a prescription medication, meaning it can’t be purchased over the counter in a drug store. To purchase propranolol, you’ll need to talk to your primary care provider or take part in an online consultation using our telehealth service.
How Does Propranolol Make You Feel?
Propranolol works by blocking the physical effects of anxiety on your heart. This means that you won’t experience the usual physical symptoms of anxiety, such as sweating, shaking or a faster heart rate when you feel nervous.
Unlike other medications for anxiety, propranolol doesn’t promote mental relaxation or calm your mind. However, by reducing the physical symptoms of anxiety, propranolol might help you to feel calmer, less nervous and more composed.
However, by reducing the physical symptoms of anxiety, propranolol might help you to feel calmer, less nervous and more composed.
Does Propranolol Affect Mental Function?
Some medications used to treat anxiety, such as benzodiazepines and antidepressants, work by “slowing down” certain aspects of your brain and causing you to feel tired.
Propranolol primarily affects your body’s physical response to stress, with few significant effects on your cognitive function.
In a 2000 study, researchers found that people who used propranolol to treat hypertension (high blood pressure) performed almost exactly the same on 11 tests of cognitive function after using their medication for three or 12 months.
It’s worth noting that this study was carried out on people who received a significant propranolol dosage of 80 to 400mg per day. This dosage, which is used to treat hypertension, is higher than the as-needed dose that’s typically used to treat social anxiety and performance anxiety.
How Long Does it Take for Propranolol to Work?
Propranolol typically reaches its peak concentration in one to four hours. It may take 30 to 60 minutes for the physical effects of propranolol, such as reduced shaking or a slower heart rate, to become noticeable.
If you’re prescribed propranolol for performance anxiety, your healthcare provider may suggest a specific time to take your medication before specific events.
Is it Okay to Take Propranolol With Food?
Propranolol can typically be taken with or without food. Taking propranolol with protein-rich food may increase its bioavailability, although this does not seem to make the medication work faster or increase its duration of action.
If you’re prescribed an extended-release form of propranolol, such as Innopran XL® or Inderal XL®, it should be consistently taken either with food or without food every time.
When Should I Take Propranolol?
If you’re prescribed propranolol for a cardiovascular health condition, it’s important to follow your healthcare provider’s instructions and take it as prescribed.
Oral propranolol comes in several forms. The extended-release tablet of propranolol is generally taken one time each day. Your healthcare provider may instruct you to take propranolol before going to bed or during the daytime.
If you’re prescribed a shorter-acting propranolol tablet or solution, you may need to take it two to four times each day. Make sure to closely follow the instructions provided with your medication and ask your healthcare provider if you have any questions about using propranolol.
How Long Does Propranolol Last?
Propranolol has a half-life of three to six hours, meaning approximately half of each dose will be active in your body three to six hours after using the medication. Some long-acting versions of propranolol have a half-life of eight to 11 hours.
Research suggests that propranolol might last for longer in elderly people due to aging-related changes in the body’s oxidation capacity. The effects of propranolol are usually noticeable for several hours after each dose.
How Much Propranolol Should You Take for Anxiety?
Because propranolol is used off-label to treat anxiety, there’s no standard recommended dosage provided by the FDA.
Most research suggests that a propranolol dosage of 40 to 120mg per day is effective at treating several forms of anxiety.
When used for other health conditions, propranolol is prescribed at dosages ranging from 40mg to 640mg per day:
For hypertension, propranolol is prescribed at an initial dosage of 40mg taken two times per day, which may be increased to a maintenance dose of 120 to 240mg per day. The maximum dosage of propranolol for hypertension is 640mg per day.
For atrial fibrillation (irregular, abnormally fast heart rate), propranolol is prescribed at a recommended dose of 10 to 30mg, taken three to four times per day.
To improve heart function after a heart attack, propranolol is prescribed at a dosage of 180 to 240mg per day, taken in divided doses.

For angina pectoris (chest pain), propranolol is typically prescribed at a total daily dose of 80 to 320mg, split into one to four separate doses per day.
For migraine, propranolol is usually prescribed at a range of 80 to 240mg per day, taken in divided doses.
For essential tremor, propranolol is usually prescribed at an initial dosage of 80mg a day, taken in two separate doses. This dosage may be adjusted to a maximum of 320mg per day over time.
As with other medications, there’s no “perfect” dose of propranolol for everyone. Based on your symptoms, bodyweight and response to the medication, your healthcare provider may prescribe propranolol at a moderate or high dosage for use before anxiety-inducing events.
What Happens if You Miss a Dose of Propranolol?
If you’re prescribed propranolol for a cardiovascular health issue, tremor or other condition that requires you to use your medication on a regular schedule, you should take the missed dose as soon as you remember it.
If it’s almost time for your next propranolol dose, you should skip the missed dose of propranolol and continue using your medication as prescribed. Do not double your dose of propranolol after a missed dose.
What Happens if You Take Too Much Propranolol?
It’s possible to overdose on propranolol. Taking too much propranolol may cause a severe drop in blood pressure, reduced heart rate and abnormal heart function. Overdosing on propranolol can potentially cause death.
If you’ve taken too much propranolol, you should contact emergency services on 911 or call the poison control helpline on 1-800-222-1222.
Can Propranolol Be Taken As Needed?
Yes. When used for performance anxiety and social anxiety, propranolol can be taken only when it’s needed. Many people use propranolol as needed before public speaking events, meetings or other stressful, anxiety-inducing situations.
If you’re prescribed propranolol for a heart condition or other reason, it’s important to follow your healthcare provider’s exact instructions and only use your medication as prescribed.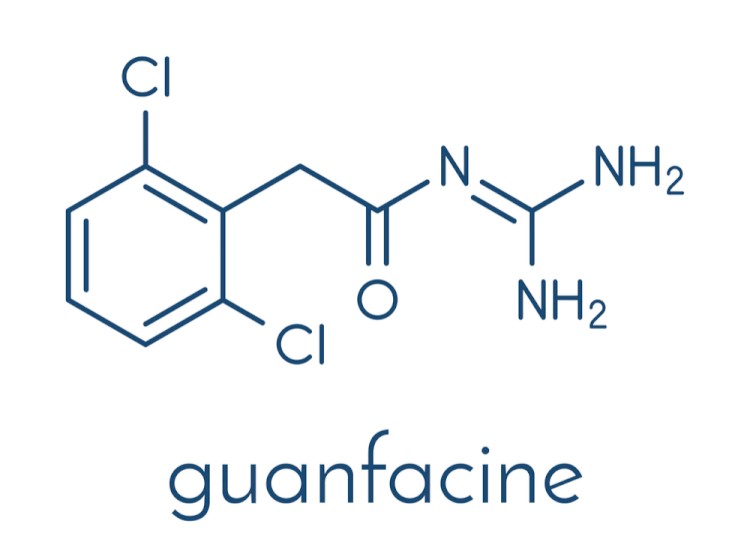
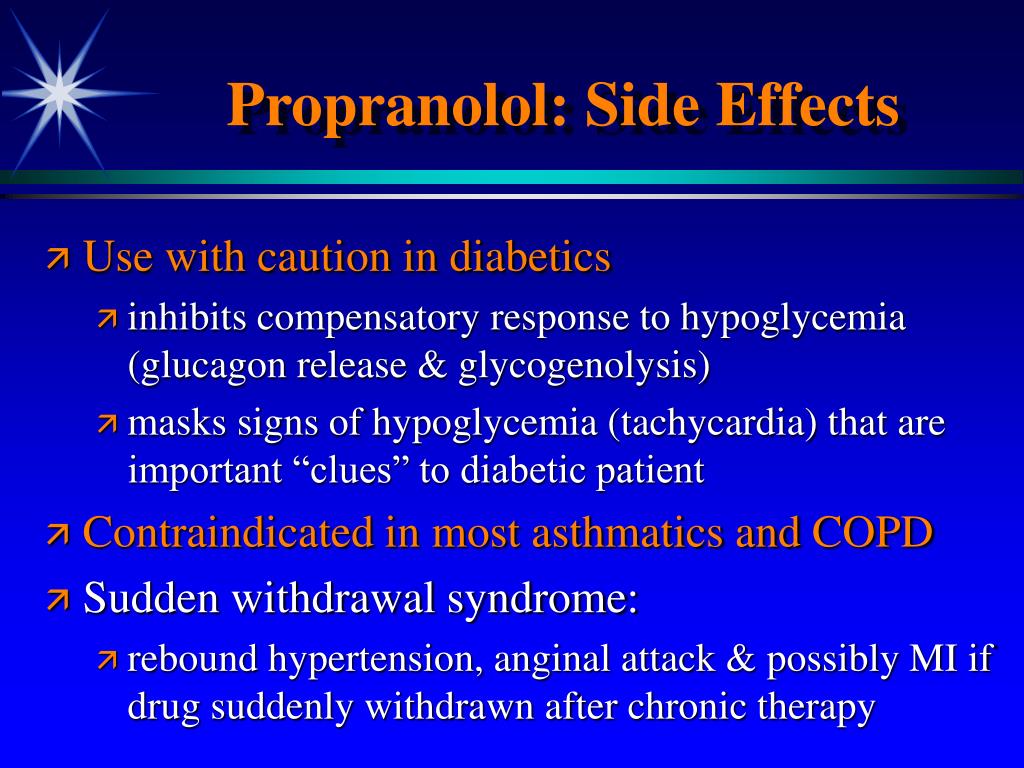
What Are Propranolol Side Effects?
Like other medications used to treat cardiovascular health issues and anxiety, propranolol can potentially cause side effects.
Propranolol can cause several potential side effects. Most side effects of propranolol are minor, with dizziness, lightheadedness, tiredness, diarrhea and constipation some of the most common adverse effects.
If these symptoms are severe or persistent, it’s best to tell your healthcare provider. They might suggest adjusting your dosage of propranolol or making other changes to the way you use your medication.
Propranolol can also cause more severe side effects, including the following:
Rash
Blistering or peeling of the skin
Itching
Hives
Swelling that affects the throat, lips, tongue and/or face
Difficulty breathing and/or swallowing
Faintness
Irregular heartbeat
Weight gain
It’s important to contact your healthcare provider or seek medical treatment if you develop any severe side effects from propranolol or other beta blockers.
Is Propranolol Safe?
Used as prescribed, propranolol is a safe medication with a low risk of side effects. It’s been in use since the 1960s and is prescribed to millions of people of all ages and backgrounds in the United States alone, with a long and reliable safety record.
Like all medications, propranolol needs to be used responsibly. If you use propranolol at doses above those directed by your healthcare provider or more frequently than prescribed, you may have an increased risk of experiencing side effects.
Does Propranolol Cause Weight Gain?
Like other medications, propranolol may cause or contribute to weight gain. In a study published in the BMJ, researchers found that people who used propranolol over the long term put on more weight than those given a non-therapeutic placebo.
It’s worth noting that most research on beta blockers and weight gain involves medications used to treat hypertension and other cardiovascular health issues, not performance anxiety.
If you notice your weight increasing after you begin treatment with propranolol, it’s best to talk to your healthcare provider.
Can Propranolol Make it Harder to Fall Asleep?
Propranolol may cause sleep issues, including difficulty falling asleep or staying asleep. In one study published in the journal International Clinical Psychopharmacology, experts found that a typical dose of propranolol increased insomnia in people prone to difficulty sleeping.
However, research also suggests over-the-counter supplements containing melatonin may help to curb this side effect. Melatonin is an active ingredient in our Sleep Gummy Vitamins.
How Much Does Propranolol Lower Blood Pressure?
Propranolol can cause a significant decrease in blood pressure, especially when used at a high dosage.
In a study published in the Journal of Clinical Hypertension, researchers tested propranolol on a group of more than 400 patients with mild to moderate hypertension. They found that the use of propranolol was associated with a 10. 1 to 11 mmHg reduction in diastolic blood pressure.
1 to 11 mmHg reduction in diastolic blood pressure.
The researchers also found that the decrease in blood pressure was significant in all propranolol doses after eight weeks of treatment.
Symptoms of low blood pressure include dizziness, lightheadedness, nausea, dehydration and unusual thirst, fatigue, difficulty concentrating, blurred vision, rapid breathing, chilled, pale skin, depression and an increase in sweating.
It’s important to inform your healthcare provider if you start to feel any symptoms of low blood pressure after using propranolol.
Does Propranolol Have any Effects on Exercise?
Because propranolol and other beta blockers reduce your heart rate and blood pressure, they may reduce your maximal and submaximal exercise capacity.
While taking propranolol, you may notice that your heart rate is lower while running, cycling or during other forms of cardiovascular exercise.
If you typically train for a target heart rate (for example, by monitoring your heart rate while you work out in order to improve your heart function or burn a certain number of calories), you may need to modify your target heart rate range while using beta blockers.
Is Propranolol Addictive?
Propranolol is not a physically addictive, habit-forming medication. However, when propranolol is used to treat anxiety, it’s possible to become used to the feeling of relaxation that it provides, especially if you often experience performance or social anxiety.
If you feel like you’re overusing propranolol or relying on it unnecessarily, it’s important to inform your healthcare provider.
Is Propranolol a Benzodiazepine?
No. Although propranolol is used to treat certain types of anxiety, it is not a benzodiazepine like alprazolam (Xanax®), diazepam (Valium®) and other anti-anxiety medications.
Is it Safe to Drink Alcohol While Taking Propranolol?
You should not drink alcohol while taking propranolol. Drinking alcohol may increase the amount of propranolol in your body. This may increase your risk of experiencing side effects.
Is Propranolol a Selective or Nonselective Beta Blocker?
Propranolol is a nonselective beta blocker, meaning it can block the effects of stress hormones on beta-1, beta-2 and beta-3 receptors.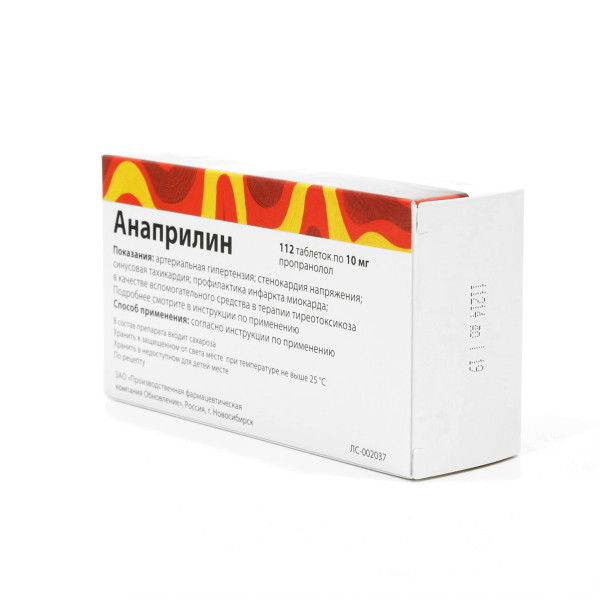 Because of this lack of receptor selectivity, the effects of propranolol may also target tissues outside the heart.
Because of this lack of receptor selectivity, the effects of propranolol may also target tissues outside the heart.
Is it Safe for People With Diabetes to Use Propranolol?
Propranolol may not be suitable for people with diabetes. As a type of nonselective beta blocker, it’s possible for propranolol to prevent the appearance of certain symptoms of hypoglycemia and potentially contribute to hypoglycemia during fasting.
If you have diabetes, it’s important to tell your healthcare provider before considering any type of beta blocker or other medication for anxiety.
Is it Safe to Use Propranolol for Public Speaking?
Yes. Many people experience performance anxiety before giving speeches or performing in front of others. Propranolol is widely used as a performance anxiety treatment by people who perform in public, from event presenters to musicians.
What Else Should You Know Before Using Propranolol?
When it’s used as prescribed, propranolol is generally a safe and effective medication. However, like with any medication, it’s important to avoid using propranolol in a way that could affect your health and wellbeing.
However, like with any medication, it’s important to avoid using propranolol in a way that could affect your health and wellbeing.
Before using propranolol, it’s important to inform your healthcare provider if:
You have any preexisting health conditions, including asthma, heart disease, diabetes, liver disease, thyroid issues, severe allergies or any other medical condition.
You use any other medications or supplements, including prescription medications or drugs available over-the-counter.
You have heart failure, or have previously experienced a cardiovascular event such as a heart attack or stroke.
You smoke cigarettes or use other products that contain tobacco and/or nicotine.
Can Propranolol Interact With Other Medications?
Yes. Propranolol can interact with a range of medications, including medications used to treat heart disease, depression, migraines, anxiety, ulcers and other conditions. These medications may increase or reduce the effects of propranolol, or contribute to dangerous side effects.
If you use other over-the-counter or prescription medications, it’s important to fully inform your healthcare provider before considering propranolol or any other beta blockers.
What Brand Names is Propranolol Sold Under?
Since propranolol is no longer under patent protection, it’s mostly sold as a generic medication without a specific brand name.
It’s also been sold under the brand names Inderal® (the first name for propranolol), Deralin®, Inderalici®, Dociton®, Avlocardyl®, InnoPran XL®, Sumial® and others.
What Forms of Propranolol are Available?
Propranolol is available as a tablet, an extended-release capsule and as a liquid solution. Each form of propranolol comes in several strengths. Make sure to check the type of propranolol you have before using this medication.
In clinical settings, propranolol may be used intravenously to treat atrial fibrillation. This form of propranolol is not typically prescribed for use at home.
online psychiatrist prescriptions
talk to a psychiatry provider.
 it’s never been easier
it’s never been easierLearn More About Treating Anxiety
As a beta blocker, propranolol can help you to deal with the symptoms of performance anxiety and feel more comfortable on stage or in front of others.
We offer propranolol for anxiety online, following a consultation with a healthcare provider who will determine if a prescription is appropriate.
You can also take action to overcome your anxiety and improve your mental wellbeing with our range of online mental health services, including psychiatry and individual therapy.
16 Sources
Hims & Hers has strict sourcing guidelines to ensure our content is accurate and current. We rely on peer-reviewed studies, academic research institutions, and medical associations. We strive to use primary sources and refrain from using tertiary references.
- Drugs@FDA: FDA-Approved Drugs. (n.d.). Retrieved from https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.
 process&ApplNo=016762
process&ApplNo=016762 - Propranolol (Cardiovascular). (2017, August 15). Retrieved from https://medlineplus.gov/druginfo/meds/a682607.html
- Shahrokhi, M. & Gupta, V. (2021, May 7). Propranolol. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557801/
- Bounds, C.G. & Nelson, V.L. (2020, November 22). Benzodiazepines. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470159/
- Pérez-Stable, E.J., et al. (2000, April 1). The effects of propranolol on cognitive function and quality of life: a randomized trial among patients with diastolic hypertension. The American Journal of Medicine. 108 (5), 359-65. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10759091/
- Inderal® (propranolol hydrochloride) Tablets. (2010, November). Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/016418s080,016762s017,017683s008lbl.pdf
- Srinivasan, A.
 V. (2019, January-March). Propranolol: A 50-Year Historical Perspective. Annals of Indian Academy of Neurology. 22 (1), 21–26. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6327687/
V. (2019, January-March). Propranolol: A 50-Year Historical Perspective. Annals of Indian Academy of Neurology. 22 (1), 21–26. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6327687/ - Steenen, S.A., et al. (2016, February). Propranolol for the treatment of anxiety disorders: Systematic review and meta-analysis. Journal of Psychopharmacology. 30 (2), 128–139. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4724794/
- Amundson, D.E. & Brodine, S.K. (1988, October). A fatal case of propranolol poisoning. Drug Intelligence & Clinical Pharmacy. 22 (10), 781-2. Retrieved from https://pubmed.ncbi.nlm.nih.gov/3229344/
- Rössner, S., Taylor, C.L., Byington, R.P. & Furberg, C.D. (1990, April 7). Long term propranolol treatment and changes in body weight after myocardial infarction. BMJ. 300 (6729), 902-3. Retrieved from https://pubmed.ncbi.nlm.nih.gov/2186832/
- Danjou, P., Puech, A., Warot, D.
 & Benoit, J.F. (1987, April). Lack of sleep-inducing properties of propranolol (80 mg) in chronic insomniacs previously treated by common hypnotic medications. International Clinical Psychopharmacology. 2 (2), 135-40. Retrieved from https://pubmed.ncbi.nlm.nih.gov/3298418/
& Benoit, J.F. (1987, April). Lack of sleep-inducing properties of propranolol (80 mg) in chronic insomniacs previously treated by common hypnotic medications. International Clinical Psychopharmacology. 2 (2), 135-40. Retrieved from https://pubmed.ncbi.nlm.nih.gov/3298418/ - Fares, A. (2011, July-September). Night-time exogenous melatonin administration may be a beneficial treatment for sleeping disorders in beta blocker patients. Journal of Cardiovascular Disease Research. 2 (3), 153–155. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3195193/
- Sica, D.A., Neutel, J.M., Weber, M.A. & Manowitz, N. (2004, May). The antihypertensive efficacy and safety of a chronotherapeutic formulation of propranolol in patients with hypertension. Journal of Clinical Hypertension. 6 (5), 231-41. Retrieved from https://pubmed.ncbi.nlm.nih.gov/15133405/
- Low Blood Pressure - When Blood Pressure Is Too Low. (2016, October 31). Retrieved from https://www.
 heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/low-blood-pressure-when-blood-pressure-is-too-low
heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/low-blood-pressure-when-blood-pressure-is-too-low - Tučková, D., et al. (2016). Effectiveness of β-blockers in physically active patients with hypertension: protocol of a systematic review. BMJ Open. 6 (6), e010534. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4916615/
- How do beta blocker drugs affect exercise?(2017, August 31). Retrieved from https://www.heart.org/en/health-topics/consumer-healthcare/medication-information/how-do-beta-blocker-drugs-affect-exercise
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Uses, Side Effects & Is It Addictive?
What is Propranolol (Zovirax)?
Propranolol is an FDA-approved, nonselective beta-blocker. Beta-blockers subvert beta receptors, which are tiny proteins, while they latch onto the chemical messengers from the central nervous system (CNS).
Beta-blockers subvert beta receptors, which are tiny proteins, while they latch onto the chemical messengers from the central nervous system (CNS).
They prevent those receptors and messengers from binding together. This:
- slows your heart rate
- lowers your blood pressure
- relaxes your blood vessels
Propranolol calms you down, improves your blood flow, and regularizes your cardiac rhythm.
Propranolol comes in tablet form, as an extended-release oral capsule, and as a solution. All forms of propranolol are generally safe to take, but you should consult your doctor before taking propranolol.
If you’re allergic to propranolol, you have a severe heart condition, or you have an abnormally slow heart rate, you should talk to your doctor about whether or not propranolol is safe for you.
If you’re a smoker or suffer from asthma or another medical condition that gives you trouble breathing, you should also consult your doctor.
Propranolol is considered safe for breastfeeding women, as there are low levels of propranolol in breast milk.
Some brand names for propranolol include:
- Inderal
- Inderal LA
- InnoPran XL
- Hemangeol
Other beta-blockers for heart conditions include metoprolol and atenolol.
Don't Know Where to Start?
Get confidential help 24/7. A specialist can help:
- Answer questions about treatment
- Provide financial assistance options
- Give you valuable guidance and resources
Call now (928) 723-1202Who answers?
Propranolol Uses
Propranolol is used to treat many conditions, including:
- Anxiety disorders
- Migraines
- High blood pressure
- Irregular heartbeat, such as atrial fibrillation
- Angina (a type of chest pain caused by reduced blood flow to the heart)
- Tremors (shaking)
- Hypertension (when the force of the blood against the artery walls is too high). Treatment for this condition may include taking propranolol along with weight control techniques, exercise, and diet
- Other heart conditions
What is the Dosage for Propranolol?
Talk to your doctor about the propranolol dosage that’s appropriate for you. Only take this medicine as directed by your doctor, and note that your dose may need to be adjusted a few times to determine what amount and frequency work best for you.
Only take this medicine as directed by your doctor, and note that your dose may need to be adjusted a few times to determine what amount and frequency work best for you.
If you have missed a propranolol dose, you should take it as soon as possible unless it’s almost time for your next dose. If this is the case, you should skip it and resume your regular dosing schedule. In other words, do not double your dosage.
Before taking propranolol, let your doctor know if you have any of the following:
- Low blood sugar or diabetes
- Slow heart rhythm
- Low blood pressure
- Thyroid issues
- Congestive heart failure
- Liver disease
- Kidney disease
- Adrenal gland tumor (pheochromocytoma)
- Circulation problems, such as Raynaud's syndrome
- A muscle disorder
- Breathing disorders, such as emphysema or bronchitis
- Depression
Questions About Insurance?
Addiction specialists are available 24/7 to help you navigate costs, insurance, and payment options
Learn MoreWho answers?
How Should I Take Propranolol?
You may swallow an oral dose of propranolol or take it via injection. The medication comes in tablet form, an extended-release capsule, or a solution. Depending on your need and dosage, your doctor will let you know the best way to take propranolol, whether it's an oral solution or an injection.
The medication comes in tablet form, an extended-release capsule, or a solution. Depending on your need and dosage, your doctor will let you know the best way to take propranolol, whether it's an oral solution or an injection.
Do not take propranolol any more or less than your doctor directs. Likewise, do not exceed your treatment plan. Store your propranolol medication at room temperature.
What are the Side Effects of Propranolol?
Taking propranolol may cause some side effects in some people.
While these common side effects are not necessarily serious, they can be uncomfortable:
- Fatigue or drowsiness
- Weight gain
- Shortness of breath or difficulty breathing
- Chest pain
- Tingling sensation
- Coldness in hands or feet
- Lightheadedness or dizziness
- Migraine headaches
- Insomnia
- Unusual dreams
- Nausea
- Constipation or diarrhea
- Depression
- Low libido
- Skin rash
You may not experience any side effects from taking propranolol. That said, most people who take beta-blockers will experience at least one. It may take time to get adjusted to propranolol, as with other beta-blockers. That’s why about one in five users end up switching to another beta-blocker or drug.
That said, most people who take beta-blockers will experience at least one. It may take time to get adjusted to propranolol, as with other beta-blockers. That’s why about one in five users end up switching to another beta-blocker or drug.
If you experience an allergic reaction to propranolol, consult your doctor right away.
Get Personalized Care
The best treatment is one that works for YOU. An addiction specialist can answer your questions and guide you through your options. Get the help YOU need today.
Learn MoreWho answers?
What Medications Should Not Be Taken With Propranolol?
Some over-the-counter and prescription drugs may interact with propranolol, such as other drugs to treat high blood pressure and other heart conditions. Propranolol does not, however, have any known severe drug interactions with other medications.
To be proactive, inform your doctor of any other medications for heart conditions (like amiodarone, quinidine, or propafenone) that you are taking before starting propranolol.
Is Propranolol Addictive?
Beta-blockers, including propranolol, are considered a non-addictive medication, unlike some other treatments for anxiety. You may begin to get used to the calming effect that propranolol can provide. When you’re feeling anxious, you may feel inclined to take propranolol to soothe your symptoms.
If you are worried about becoming dependent on your medication or experiencing adverse effects, talk to your doctor about alternatives that may better suit you.
Propranolol FAQs
Is propranolol good for anxiety?
Propranolol can help treat anxiety. This is because the beta-blocker works by slowing your heart rate and lowering your blood pressure, which both increase with anxiety. Propranolol is one treatment option to help ease stress, though it may not be for everyone.
How does propranolol make you feel?
Propranolol can make you feel at ease. This is because it blocks the physical symptoms of anxiety by lowering your heart rate and decreasing your blood pressure. You may experience a feeling of calm while taking propranolol and, hence, better manage any stressors in your life. This is why treating anxiety is one of the many possible uses for propranolol.
You may experience a feeling of calm while taking propranolol and, hence, better manage any stressors in your life. This is why treating anxiety is one of the many possible uses for propranolol.
Some people may experience uncomfortable side effects when taking propranolol. While these side effects are not life-threatening, they can be enough to make you choose to switch to another medication.
Can propranolol cause weight gain?
Weight gain is one of the potential side effects of taking propranolol. While it is possible, not everyone who takes propranolol will experience weight gain. If you do experience weight gain, consult your healthcare provider for medical advice.
What is propranolol used for?
Propranolol is used to treat many heart problems and other conditions such as high blood pressure, an irregular heartbeat or heart rhythm, an essential tremor, hyperthyroidism, and hypertrophic subaortic stenosis (a heart disease of the muscle).
It is also used to treat pheochromocytoma, which is a tumor on a small gland near the kidneys, to prevent angina (chest pain), and to improve survival after a heart attack. Because propranolol alleviates physical symptoms of anxiety, such as high blood pressure and an increased heart rate, it can also be used to treat anxiety and migraine headaches.
Because propranolol alleviates physical symptoms of anxiety, such as high blood pressure and an increased heart rate, it can also be used to treat anxiety and migraine headaches.
Propranolol has not been adequately tested in heart failure.
How quickly does propranolol work for anxiety?
Do propranolol side effects go away?
Propranolol side effects can last a few days to weeks, depending on the patient and dosage.
Call to find out how much your insurance will cover
Call now (928) 723-1202Who answers?
Propranolol prolongs life and protects against cancer
In animal studies, lipophilic metoprolol given daily from 12 months of age extended median lifespan in long-lived male mice by 10%. A 2017 meta-analysis concludes that lipophilic beta-blockers (metoprolol and propranolol) are significantly better at reducing the risk of cardiovascular death in people than hydrophilic ones. Propranolol significantly and more than other beta-blockers reduce platelet aggregation, reduces mortality within 2-3 years after myocardial infarction by 23-26%. Propranolol is on the list of first line drugs to reduce the frequency of migraine attacks, the only drug approved by the US FDA for the treatment of essential tremors, used to treat anxiety disorders, hyperthyroidism. Proparnolol is associated with a 71% reduction in breast cancer mortality over a 10-year survival period, is associated with an increase in life expectancy compared to selective beta-blockers in women with epithelial ovarian cancer, with improved survival and a reduced risk of melanoma progression, and is able to stop angiosarcoma. Treatment with propranolol is associated with a high statistically significant reduction in the incidence of hepatocellular carcinoma (liver cancer) in patients with cirrhosis of the liver.
Propranolol significantly and more than other beta-blockers reduce platelet aggregation, reduces mortality within 2-3 years after myocardial infarction by 23-26%. Propranolol is on the list of first line drugs to reduce the frequency of migraine attacks, the only drug approved by the US FDA for the treatment of essential tremors, used to treat anxiety disorders, hyperthyroidism. Proparnolol is associated with a 71% reduction in breast cancer mortality over a 10-year survival period, is associated with an increase in life expectancy compared to selective beta-blockers in women with epithelial ovarian cancer, with improved survival and a reduced risk of melanoma progression, and is able to stop angiosarcoma. Treatment with propranolol is associated with a high statistically significant reduction in the incidence of hepatocellular carcinoma (liver cancer) in patients with cirrhosis of the liver.
Medicines can be life-threatening. They can only be used with a doctor's prescription! The material in this article is for illustrative and educational purposes only and is not warranted for any medical use.
 For more information, please contact your doctor.
For more information, please contact your doctor. What are beta-adrenergic blockers and how propranolol differs from selective adrenoblockers
Beta-blockers block the sensitivity of β-adrenergic receptors to adrenaline and norepinephrine. But if selective andenoblockers do not block all types of β-adrenergic receptors, but only one type, then propranolol, as a non-selective beta-adrenergic blocker, blocks all β-adrenergic receptors (β1, β2 and β3):
- β1-adrenergic receptors are located mainly in the heart and kidneys
- β2-adrenergic receptors are found mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle.
- β3-adrenergic receptors are found in fat cells.
Link to source:
- https://en.m.wikipedia.org/wiki/Beta_blocker
Propranolol, as a non-selective beta-blocker, blocks all β-adrenergic receptors (β1, β2 and β3). Selective beta-blockers (eg, bisoprolol/concor) do not affect β2 receptors and are therefore ineffective in delaying the progression of cancers whose growth is delayed or prevented by propranolol. Propranolol is a blocker of both β2 and β3 receptors that play a large role in the progression of cancer growth . This is especially true of breast cancer and brain metastases. The use of propranolol reduced breast cancer mortality by 71% over a 10-year survival period.
Selective beta-blockers (eg, bisoprolol/concor) do not affect β2 receptors and are therefore ineffective in delaying the progression of cancers whose growth is delayed or prevented by propranolol. Propranolol is a blocker of both β2 and β3 receptors that play a large role in the progression of cancer growth . This is especially true of breast cancer and brain metastases. The use of propranolol reduced breast cancer mortality by 71% over a 10-year survival period.
Research links:
- www.ncbi.nlm.nih.gov/pubmed/21632503
- www.ncbi.nlm.nih.gov/pubmed/27035124
- www.ncbi.nlm.nih.gov/pubmed/21317458
The use of propranolol in early-stage breast cancer patients may result in reduced tumor proliferation (www.ncbi.nlm.nih.gov/pubmed/28031536). In triple-negative breast cancer, the combination of propranolol with metformin at clinically available concentrations reduced tumor cell proliferation, their mitochondrial activity, migration, invasion, and also reduced tumor growth rates in vitro and in vivo, which provides a good basis for testing this combination in clinical trials (www. .ncbi.nlm.nih.gov/pubmed/27926515).
.ncbi.nlm.nih.gov/pubmed/27926515).
In addition, propranolol, unlike most beta-blockers, is able to cross the blood-brain barrier (protective barrier of the brain) and affect the central nervous system in addition to peripheral activity
Research links:
- http://jop .sagepub.com/content/30/2/128
- www.ncbi.nlm.nih.gov/pubmed/21180298
- www.ncbi.nlm.nih.gov/pubmed/2865152
Commonly used therapeutics for anxiety disorders are selective serotonin reuptake inhibitors, tricyclic antidepressants and benzodiazepines, and probably also propranolol (www.ncbi.nlm.nih.gov/pubmed/8679756) (www.ncbi.nlm.nih.gov/pubmed/8679756). Although a 2016 meta-analysis concludes that the quality of evidence for the efficacy of propranolol is currently insufficient for its routine use in the treatment of anxiety disorders (www.ncbi.nlm.nih.gov/pubmed/26487439).
Therefore, non-selective beta-blockers are used to prevent many types of cancer.
Propranolol prevents and treats some types of malignant and benign tumors
Over the past 10 years, it has become obvious that the prevention of cancerous tumors will allow you to push (delay) the moment of the disease to a later age. Thanks to such prevention, people can live longer for many years. In recent decades, mortality from cardiovascular diseases has sharply decreased due to the chemoprevention of diseases of the heart and blood vessels. If this trend continues, then people will soon die mainly not from cardiovascular diseases, but from cancer. One of the candidates for cancer prevention is considered propranolol. It is well studied as it has been used since 1965 years old.
In 2015, a study in women with epithelial ovarian cancer showed that propranolol was associated with increased life expectancy compared to selective beta-blockers.
Study Link:
- www.ncbi.nlm.nih.gov/pubmed/26301456
Propranolol was demonstrated in 2014 in human clinical trials to stop angiosarcoma with a very poor initial prognosis, one of the most aggressive malignant tumors that kill even with treatment 91% of patients.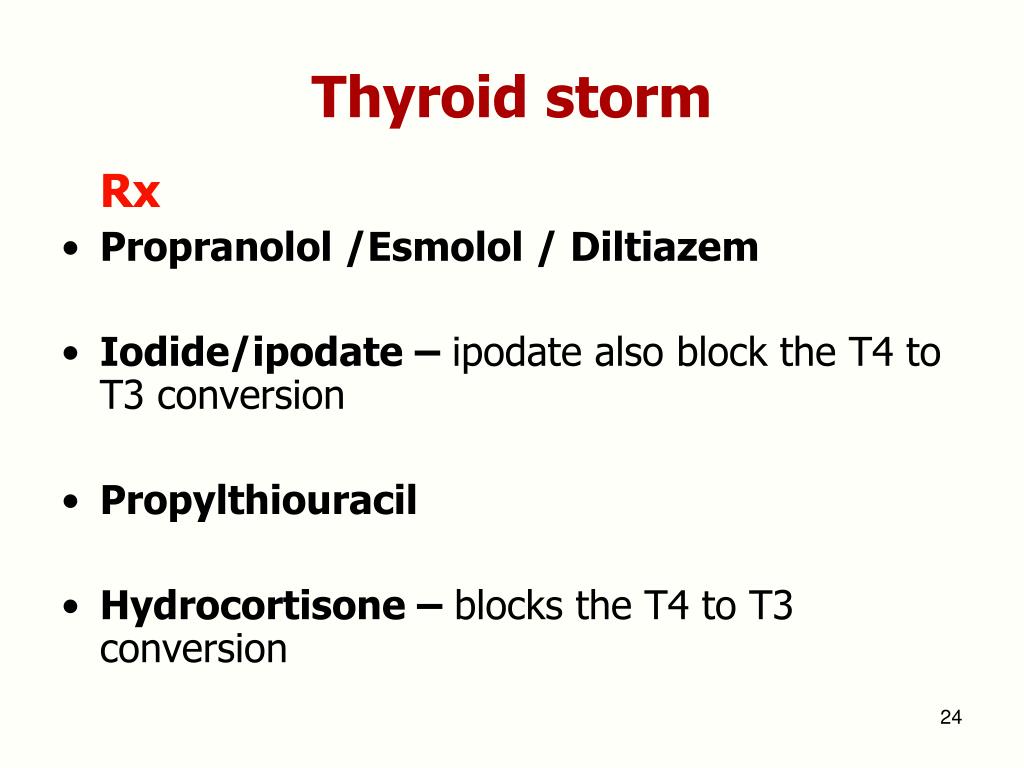 It is interesting that already a week after the start of taking propranolol (40 mg 2 times a day), angiosarcoma stops growing, and when chemotherapy is added, in some patients it completely regresses, dramatically increasing the overall survival of study participants. Propranolol costs "penny". For comparison, the previously ineffective treatment of angiosarcoma cost patients about $10,000.
It is interesting that already a week after the start of taking propranolol (40 mg 2 times a day), angiosarcoma stops growing, and when chemotherapy is added, in some patients it completely regresses, dramatically increasing the overall survival of study participants. Propranolol costs "penny". For comparison, the previously ineffective treatment of angiosarcoma cost patients about $10,000.
Study links:
- www.ncbi.nlm.nih.gov/pubmed/27211551
- http://archderm.jamanetwork.com/article.aspx?articleid=2436318
- www.newswise.com/articles/conventional-heart-drug-stops-the-progression-of-cancer
Human clinical trials of stage II propranolol began today after good results in animals to test its ability to slow the growth of breast cancer .
Research links:
- www.newswise.com/articles/conventional-heart-drug-stops-the-progression-of-cancer
- www.ncbi.nlm.nih.
 gov/pubmed/19442150
gov/pubmed/19442150 - www.ncbi.nlm.nih.gov/pmc/articles/PMC3248157
- www.ncbi.nlm.nih.gov/pubmed/21632501
- www.ncbi.nlm.nih.gov/pubmed/21317458
Studies show that treatment with propranolol is associated with a high statistically significant reduction in the incidence of hepatocellular carcinoma (liver cancer) in patients with cirrhosis of the liver and associated esophageal varices. This amazing finding needs confirmation, but the result is biologically plausible.
Study Link:
- www.ncbi.nlm.nih.gov/pubmed/22869451
Multiple myeloma is a malignant tumor with predominant localization of the process in the bone marrow. Multiple myeloma is still considered a disease that is not curable, but well controlled, in which a long-term remission is possible. A potential cure can only be discussed in cases of successful donor bone marrow transplantation. However, studies show that propranolol can be a good and very cheap way to treat multiple myeloma. 2017, Mayo Clinic, USA. A preclinical study demonstrated the antiproliferative and apoptotic effects of propranolol on multiple myeloma cells. A retrospective analysis has shown that the use of beta-adrenergic locators is associated with improved survival in patients with multiple myeloma.
2017, Mayo Clinic, USA. A preclinical study demonstrated the antiproliferative and apoptotic effects of propranolol on multiple myeloma cells. A retrospective analysis has shown that the use of beta-adrenergic locators is associated with improved survival in patients with multiple myeloma.
Study link:
- www.ncbi.nlm.nih.gov/pubmed/23080133
- www.ncbi.nlm.nih.gov/pubmed/27733010
2011 University of Florence, Italy. Preclinical data show that β-adrenergic antagonists (β-blockers) inhibit tumor progression and metastasis in animal models of melanoma. A pilot clinical study in the adjunctive treatment of melanoma with propranolol for a year showed a reduction in the percentage of disease progression and mortality www.ncbi.nlm.nih.gov/pubmed/21518948. 2011 Ohio State University, USA . Experimental evidence suggests that catecholamine hormones may be involved in stimulating the aggressiveness of malignant melanoma. 4179patients diagnosed with malignant melanoma in Denmark were followed up for an average of 4.9 years. About 372 were treated with β-blockers and their survival time was extended www.ncbi.nlm.nih.gov/pubmed/21933972 www.ncbi.nlm.nih.gov/pubmed/22322621
4179patients diagnosed with malignant melanoma in Denmark were followed up for an average of 4.9 years. About 372 were treated with β-blockers and their survival time was extended www.ncbi.nlm.nih.gov/pubmed/21933972 www.ncbi.nlm.nih.gov/pubmed/22322621
Propranolol may help treat colon cancer according to preclinical studies. 2014, Department of Clinical Epidemiology and Aging Research, German Center for Cancer Research, Germany. The use of beta-blockers may be associated with longer survival in patients with stage IV colorectal cancer.0004
It is amazing how propranolol (at a dosage of 2-3 mg per kg of body weight per day) in a few months (on average 6 months) easily completely and without a trace removes huge hemangiomas (benign tumors) , which are most often found in babies), even if they occupied the entire face or half of the head. But provided that they are treated in infants, then too late.
Research links:
- www.
 ncbi.nlm.nih.gov/pubmed/19467330
ncbi.nlm.nih.gov/pubmed/19467330 - www.ncbi.nlm.nih.gov/pubmed/25693013
Propranolol treats benign liver tumors (haemangiomas) in infants
Research links:
- www.ncbi.nlm.nih.gov/pubmed/212601702
- www.ncbi.nlm.nih.gov/pubmed/20488455
- www.ncbi.nlm.nih.gov/pubmed/25558685
Propranolol blocks anxiety, allows you to forget bad memories, blocks panic phobias
Today, there are almost no safe drugs available for the treatment of post-traumatic syndrome. Propranolol is being investigated as a potential drug for the treatment of Post Traumatic Trauma Syndrome. Propranolol inhibits the action of norepinephrine, which contributes to the consolidation of memory of bad events in life. Propranolol can also reduce emotional distress from already formed negative memories. For this reason, it is also being studied in the treatment of specific phobias. For example, fear of spiders, fears of visiting the dentist, social phobias. As experiments have shown, if people are given propranolol before showing spiders, then all the symptoms of fright disappear. Moreover, they do not return even after the volunteers go through the repeated stage of the attempt to "form fear of spiders." In addition, propranolol improves cognitive functions (memory, thinking, etc.) in post-traumatic syndrome
As experiments have shown, if people are given propranolol before showing spiders, then all the symptoms of fright disappear. Moreover, they do not return even after the volunteers go through the repeated stage of the attempt to "form fear of spiders." In addition, propranolol improves cognitive functions (memory, thinking, etc.) in post-traumatic syndrome
Research links:
- www.ncbi.nlm.nih.gov/pubmed/23182304
- www.nbcnews.com/id/10806799/
- www.ncbi.nlm.nih.gov/pubmed/17588604
- www.biologicalpsychiatryjournal.com/article/S0006-3223(03)00412-8/abstract
- http://jop.sagepub.com/content/30/2/128
- www.ncbi.nlm.nih.gov/pubmed/27014009
- www.ncbi.nlm.nih.gov/pubmed/26808441
- www.ncbi.nlm.nih.gov/pubmed/26942318
- www.ncbi.nlm.nih.gov/pubmed/26707354
- www.ncbi.nlm.nih.gov/pubmed/26487439
- www.ncbi.nlm.nih.gov/pubmed/17200914
Commonly used therapeutics for anxiety disorders are selective serotonin reuptake inhibitors, tricyclic antidepressants and benzodiazepines, as well as propranolol www. ncbi.nlm.nih.gov/pubmed/8679756 www.ncbi.nlm.nih.gov/pubmed /8679756 Although a 2016 meta-analysis concludes that the quality of evidence for the efficacy of propranolol is currently insufficient for its routine use in the treatment of anxiety disorders. www.ncbi.nlm.nih.gov/pubmed/26487439
ncbi.nlm.nih.gov/pubmed/8679756 www.ncbi.nlm.nih.gov/pubmed /8679756 Although a 2016 meta-analysis concludes that the quality of evidence for the efficacy of propranolol is currently insufficient for its routine use in the treatment of anxiety disorders. www.ncbi.nlm.nih.gov/pubmed/26487439
A controlled human trial showed that propranolol at 80 mg one hour before a dentist visit and 40 mg immediately after a visit reduced anxiety before going to the dentist for a tooth extraction this time and the next.
Research links:
- www.ncbi.nlm.nih.gov/pubmed/26607848
Musicians, public speakers, actors and professional dancers in many Western countries use propranolol to block their anxiety before public speaking.
Research links:
- https://en.m.wikipedia.org/wiki/Beta_blocker
Propranolol improves social communication skills in people with autism disorder
Research links:
- www.ncbi.nlm.nih.gov/pubmed/7
- 8
Theranostics of Aging evaluates the diagnostic parameters of your body and informs about the existing ways to increase your life expectancy.
After diagnosing the parameters of your body (https://nestarenie.ru/novaya-teranostika-stareniya-1-5.html) at the medical center, make an appointment for an appointment with a doctor .
Follow your doctor's advice to help you live longer. See you in the 22nd century .
Propranolol slightly inhibits platelet aggregation
A decrease in platelet aggregation, which increases with age, is a good prevention of deadly blood clots. Propranolol significantly and more than other beta-blockers reduces platelet aggregation, which has advantages in reducing the risk of death due to blood clots.
Study Link:
- www.ncbi.nlm.nih.gov/pubmed/24730697
Propranolol helps improve athletic performance in shooting accuracy
Propranolol lowers heart rate and reduces tremors. Therefore, propranolol and other beta-blockers are used in some sports where high accuracy is important: archery, billiards, golf, pistol shooting, etc. But today, beta blockers are banned by the International Olympic Committee. The last high-profile crime occurred in 2008 at the Summer Olympics. Shooting bronze medalist Kim Yong-Soo was stripped of his bronze medal due to the use of beta blockers. For the same reasons, beta blockers are used by neurosurgeons.
But today, beta blockers are banned by the International Olympic Committee. The last high-profile crime occurred in 2008 at the Summer Olympics. Shooting bronze medalist Kim Yong-Soo was stripped of his bronze medal due to the use of beta blockers. For the same reasons, beta blockers are used by neurosurgeons.
Research links:
- https://en.m.wikipedia.org/wiki/World_Anti-Doping_Agency
- www.ncbi.nlm.nih.gov/pubmed/10360293
- www.ncbi.nlm.nih.gov/pmc/articles/PMC1298399
Essential tremor is the most common movement disorder and its cause is unknown. Usually involves tremors in the arms, hands, or fingers, but sometimes the head, vocal cords, or other parts of the body are involved during intentional movements such as eating or writing. It is a separate disease from Parkinson's disease and is often misdiagnosed as some features are common to both conditions. Propranolol is the only drug approved by the US Food and Drug Administration (FDA) for the treatment of essential tremors.
Research links:
- www.ncbi.nlm.nih.gov/pubmed/24385718
- www.ncbi.nlm.nih.gov/pubmed/22013182
Propranolol prevents migraine
Migraine (headache, nausea, etc.) is a common, severe disease affecting up to 15% of the population. Propranolol has been proven to significantly reduce the frequency of migraines. Of all the beta-blockers, the ability to prevent migraine attacks has been proven only for propranolol and timolol.
Research links:
- http://brain.oxfordjournals.org/content/128/1/86.full
- www.worldcat.org/title/biochemistry-of-migraine/oclc/11726870
Migraine is one of the most common causes of headaches. It is a debilitating disease characterized by episodes of unilateral throbbing headache associated with symptoms such as nausea, vomiting, photophobia, and phonophobia. Propranolol is on the list of first-line drugs to reduce the frequency of migraine attacks (www. ncbi.nlm.nih.gov/pubmed/22529202). Propranolol is safe and effective for the treatment of migraine (www.ncbi.nlm.nih.gov/pubmed/15106196 www.ncbi.nlm.nih.gov/pubmed/1830566). Propranolol has also been shown to be better tolerated, most effective, and the most preferred treatment for migraine than other drugs (www.ncbi.nlm.nih.gov/pubmed/28220376 www.ncbi.nlm.nih.gov/pubmed/28220376) . Although a 2019 meta-analysis concludes that more research is needed (www.ncbi.nlm.nih.gov/pubmed/30893319).
ncbi.nlm.nih.gov/pubmed/22529202). Propranolol is safe and effective for the treatment of migraine (www.ncbi.nlm.nih.gov/pubmed/15106196 www.ncbi.nlm.nih.gov/pubmed/1830566). Propranolol has also been shown to be better tolerated, most effective, and the most preferred treatment for migraine than other drugs (www.ncbi.nlm.nih.gov/pubmed/28220376 www.ncbi.nlm.nih.gov/pubmed/28220376) . Although a 2019 meta-analysis concludes that more research is needed (www.ncbi.nlm.nih.gov/pubmed/30893319).
Propranolol prolongs life and reduces mortality from recurrent heart attack and stroke
Beta-blockers (preferably non-selective - propranolol or carvedilol) indirect inhibitors of mTOR. Substances capable of inhibiting mTOR are candidates for anti-aging drugs. It is the mTOR gene that plays one of the leading roles, thanks to which a reduction in calorie intake can prolong life.
In addition, propranolol, through the blockade of receptors for stress hormones, suppresses stress. Stress greatly shortens our lives and accelerates aging, creates wrinkles, raises blood pressure, damages the heart and blood vessels, shortens telomeres, reduces the level of longevity protein Klotho.
Stress greatly shortens our lives and accelerates aging, creates wrinkles, raises blood pressure, damages the heart and blood vessels, shortens telomeres, reduces the level of longevity protein Klotho.
The fact that emotional stress raises blood pressure and causes heart disease is clearly shown in the work of J. Kaplan. Kaplan, using the example of primates, showed that if you collect a group of male primates, then within a few days the monkeys will have a social hierarchy. The worst place in such a hierarchy is at the bottom. Male primates in a subordinate position show a range of indicators of chronic stress. Often such primates develop atherosclerosis. But if scientists gave male primates at the bottom of the social hierarchy (risk group) beta-blockers that suppress the activity of the sympathetic nervous system, then they did not develop atherosclerosis of the vessels. This showed how the sympathetic nervous system, due to stress, negatively affects the development of atherosclerosis and is involved in problems with the heart and blood vessels. The truth is that emotional stress manifests itself through the sympathetic (adrenergic) autonomic nervous system, which links the control centers of our brain and internal organs. Including - with immune, bone marrow, etc. And atherosclerosis is the main factor that leads to the largest number of deaths in developed countries from heart attack and brain stroke.
The truth is that emotional stress manifests itself through the sympathetic (adrenergic) autonomic nervous system, which links the control centers of our brain and internal organs. Including - with immune, bone marrow, etc. And atherosclerosis is the main factor that leads to the largest number of deaths in developed countries from heart attack and brain stroke.
Study link:
- www.ncbi.nlm.nih.gov/pubmed/2899392
Human clinical trials show that propranolol reduces cardiovascular mortality (#1 cause of death in the world),
Link to study:
- www.ncbi.nlm.nih.gov/pubmed/6342840
A 3-year follow-up of patients aged 60-69 who had myocardial infarction showed that propranolol reduced overall mortality in these patients by 23-37%. In addition, propranolol caused a reduction in signs of heart disease and aging (a significantly greater increase in left ventricular ejection fraction and a significantly greater decrease in left ventricular myocardial mass.
Study links:
- www.ncbi.nlm.nih.gov/pubmed/9230162
- www.ncbi.nlm.nih.gov/pubmed/6342843
- http://pda.rlsnet.ru/mnn_index_id_370.htm
- www.ncbi.nlm.nih.gov/pubmed/6342840
- www.ncbi.nlm.nih.gov/pubmed/3 6
- www.ncbi.nlm.nih.gov/pubmed/10381708
In animal studies, lipophilic metaprolol given daily from 12 months of age extended median lifespan in long-lived male mice by 10% (www.ncbi.nlm.nih.gov/pubmed/23314750). Meta-analysis 2017 with analysis 90 935 patients conclude that lipophilic beta-blockers (metoprolol, propranolol and oxyprenolol) reduce the risk of CVD mortality significantly better than hydrophilic ones (atenolol and others) (www.ncbi.nlm.nih.gov/pubmed/28760243) . Atenolol (a hydrophilic beta-blocker) is associated with an increased risk of stroke in the elderly, while lipophilic beta-blockers, mainly metoprolol and propranolol (with moderate to high lipophilicity), do not increase the risk of stroke in this population. In addition, highly lipophilic drugs may more readily penetrate the brain and cell membrane, which may help prevent stroke and cardiac death, indicating that moderate to high lipophilic beta-blockers may have a greater impact on clinical outcomes than hydrophilic ones. beta-adrenergic blockers.
In addition, highly lipophilic drugs may more readily penetrate the brain and cell membrane, which may help prevent stroke and cardiac death, indicating that moderate to high lipophilic beta-blockers may have a greater impact on clinical outcomes than hydrophilic ones. beta-adrenergic blockers.
Currently, propranolol is being considered for the treatment of resistant hypertension, along with other antihypertensive drugs, when other drugs are not sufficient to control blood pressure.
Study link:
- www.ncbi.nlm.nih.gov/pubmed/28292320
Propranolol is used to treat hyperthyroidism, an overactive thyroid gland.
In hyperthyroidism, there is an increased level of thyroid hormones in the circulation, resulting in tachycardia, palpitations, tremors and anxiety. Propranolol has been widely used to treat such symptoms of hyperthyroidism. In addition, propranolol reduces the conversion of thyroid hormone T4 to the more active T3
Study link:
- www.
 ncbi.nlm.nih.gov/pubmed/1688102
ncbi.nlm.nih.gov/pubmed/1688102
Who should not use propranolol
Propranolol is a drug that is well tolerated by healthy people, but can be dangerous in certain health conditions. Therefore, propranolol should not be used without a doctor's prescription!!!
- Propranolol is contraindicated and dangerous for patients with diseases of the lungs and respiratory tract: chronic obstructive pulmonary disease, bronchial asthma, etc.
- Dangerous for patients diagnosed with bradycardia (pulse below 55 beats per minute), sick sinus syndrome (diagnosed by ECG of the heart)
- Deadly in case of blockade of the AV node of the heart (2nd and 3rd degree) (diagnosed by ECG of the heart)
- Dangerous at low pressure as it also reduces pressure.
- Propranolol is fatal when combined with the calcium channel blocker verapamil due to possible excessive blockade of the AV node of the heart and cardiac arrest.
- Propranolol should not be used in renal failure.
- Propranolol is best not used in type 2 diabetes mellitus without special need
- Propranolol should not be used in hepatic impairment, although low doses have been shown to be useful in some studies in liver cirrhosis.
- Propranolol should not be used in psoriasis and in the elderly without special need.
- Propranolol is dangerous in overdose. Therefore, the dose for treatment should be selected, gradually increasing, and coordinating it with the attending physician.
Study Link:
- https://en.m.wikipedia.org/wiki/Propranolol
Caution:
During treatment with propranolol, you should:
- reduce your caloric intake, as it slows down the overall metabolism in the body.
- if possible, do not drive a car (dulls the sense of danger)
- Avoid drinking alcohol (though not dangerous in small doses).
- stop treatment with propranolol gradually over 2 weeks
- use with caution in peripheral vascular disease, "intermittent claudication", etc.

Research links:
- www.cvpharmacology.com/cardioinhibitory/beta-blockers
- www.ncbi.nlm.nih.gov/pubmed/16809680
Due to its high penetration through the blood-brain barrier of the brain, propranolol can cause sleep disturbance and nightmares in some people. Although I personally drink it and sleep very well.
Study link:
- www.ncbi.nlm.nih.gov/pubmed/21180298
Conclusions:
- In animal studies, lipophilic metoprolol administered daily from 12 months of age extended median lifespan in long-lived male mice by 10%. A 2017 meta-analysis concludes that lipophilic beta-blockers (metoprolol and propranolol) are significantly better at reducing the risk of cardiovascular death in people than hydrophilic ones. Propranolol significantly and more than other beta-blockers reduce platelet aggregation, reduces mortality within 2-3 years after myocardial infarction by 23-26%. Propranolol is on the list of first line drugs to reduce the frequency of migraine attacks, the only drug approved by the US FDA for the treatment of essential tremors, used to treat anxiety disorders, hyperthyroidism.
 Proparnolol is associated with a 71% reduction in breast cancer mortality over a 10-year survival period, is associated with an increase in life expectancy compared to selective beta-blockers in women with epithelial ovarian cancer, with improved survival and a reduced risk of melanoma progression, and is able to stop angiosarcoma. Treatment with propranolol is associated with a high statistically significant reduction in the incidence of hepatocellular carcinoma (liver cancer) in patients with cirrhosis of the liver.
Proparnolol is associated with a 71% reduction in breast cancer mortality over a 10-year survival period, is associated with an increase in life expectancy compared to selective beta-blockers in women with epithelial ovarian cancer, with improved survival and a reduced risk of melanoma progression, and is able to stop angiosarcoma. Treatment with propranolol is associated with a high statistically significant reduction in the incidence of hepatocellular carcinoma (liver cancer) in patients with cirrhosis of the liver. - Self-administration of propranolol without a doctor's prescription is deadly.
Attention. The information in this article cannot be used for self-medication, as the drug has a dangerous incompatibility with some other drugs and is unsafe for use in certain heart conditions. Its use is possible only after the permission of the doctor.
We invite you to subscribe by mail to the latest and most relevant news that appear in science, as well as the news of our science and communication group, so as not to miss anything. Be sure to leave your comments below the article you are subtracting. It is very important for us.
Be sure to leave your comments below the article you are subtracting. It is very important for us.
Your name
Some error text
Some error text
Dear readers of the resource www.nestarenie.ru. If you think that the articles of this resource are useful for you, and you want other people to use this information for many years, then you have the opportunity to help develop this site by spending about 2 minutes of your time on it. To do this, click on this link.
We also recommend reading the following articles:
- Metformin is the most studied drug that can prolong life if prescribed by a doctor according to indications.
- A detailed program to extend life in scientifically based ways.
- Vitamin K2 (MK-7) reduces mortality
- Vitamin B6 + magnesium reduces mortality by 34%
- Glucosamine Sulfate effectively prolongs life and protects against many types of cancer
- Folates to prevent early aging
- How to defeat methylglyoxal - a substance that ages us.

Antianginal drug withdrawal syndrome. Clinical significance and prevention measures | #01/99
Withdrawal syndrome can be experienced by every practitioner. It is typical for a wide variety of drugs - sleeping pills, tranquilizers, corticosteroids, antiepileptic drugs, etc. The drugs used in cardiology are no exception. The withdrawal syndrome of clonidine, beta-blockers and a number of other drugs is well known.
- Manifestations of antianginal drug withdrawal syndrome
In patients with ischemic heart disease (CHD) with stable angina pectoris, discontinuation of an antianginal drug can cause a significant increase in angina attacks and a decrease in exercise tolerance. In rare cases, acute myocardial infarction may develop. Since almost all antianginal drugs reduce blood pressure to one degree or another, stopping them often causes an increase, sometimes quite significant. Recently, data have appeared that in some cases, the abolition of an antianginal drug can cause the appearance of so-called asymptomatic myocardial ischemia [1].
| Withdrawal syndrome is understood as the reaction of the body that occurs in response to the termination of the drug and is expressed in the deterioration of the patient's condition. Often, the withdrawal syndrome is manifested by the appearance of qualitatively new signs of the disease that were absent in the patient before |
The withdrawal syndrome is most typical for drugs that are quickly excreted from the body. The faster the drug is excreted from the body, the more pronounced the withdrawal syndrome can be.
It should not be thought that the withdrawal syndrome develops only after the complete cessation of the drug (Table 1). It has been established that the withdrawal syndrome can also manifest itself during treatment, in the intervals between the action of successive doses of the drug. This is possible, firstly, when the interval between taking two doses of the drug is large enough. For example, the development of a withdrawal syndrome in the morning, before taking the next dose of the drug, when the action of the previous dose has ended, is not excluded. This type of withdrawal syndrome is called the "zero-hour phenomenon" (in English - zero-hour phenomenon) [2].
For example, the development of a withdrawal syndrome in the morning, before taking the next dose of the drug, when the action of the previous dose has ended, is not excluded. This type of withdrawal syndrome is called the "zero-hour phenomenon" (in English - zero-hour phenomenon) [2].
- in response to a very rapid elimination of the drug from the body (for example, the development of the rebound phenomenon at the end of the action of short-acting nifedipine dosage forms) |
Secondly, as already mentioned above, during treatment, a withdrawal syndrome can occur if the drug is very quickly excreted from the body. In such cases, the withdrawal syndrome is often called the rebound phenomenon (in English - rebound effect) or the phenomenon of negative aftereffect. This is possible, in particular, when using certain short-acting dosage forms (for example, short-acting nifedipine) or if a method of administering the drug into the body is chosen that allows you to abruptly stop the drug (for example, when you abruptly stop intravenous administration of the drug or when removing from the skin transdermal dosage form of the drug).
In such cases, the withdrawal syndrome is often called the rebound phenomenon (in English - rebound effect) or the phenomenon of negative aftereffect. This is possible, in particular, when using certain short-acting dosage forms (for example, short-acting nifedipine) or if a method of administering the drug into the body is chosen that allows you to abruptly stop the drug (for example, when you abruptly stop intravenous administration of the drug or when removing from the skin transdermal dosage form of the drug).
All of the above indicates that withdrawal syndrome, firstly, can significantly affect the safety of ongoing therapy with antianginal drugs (in some cases, due to the development of withdrawal syndrome, therapy can even give a paradoxical effect). Second, the onset of withdrawal symptoms is usually quite predictable, and knowledge of the clinical pharmacology of the drugs used can help prevent its occurrence.
Below is information about the possibility of withdrawal syndrome of various groups of antianginal drugs.
- Nitrates
Nitrates were the first antianginal drugs for which a withdrawal syndrome was described. Back in 1898, G. C. Laws reported a deterioration in the health of workers employed in the production of gunpowder on weekends [3]. Subsequently, quite a lot of works appeared containing documented information about cases of sudden death of workers involved in the production of dynamite, which occurred on weekends when contact with nitrates was stopped [4, 5]. The nitrate withdrawal syndrome as such was first described in the mid-twentieth century, when it was shown that some workers involved in the production of dynamite experienced typical non-exercise angina attacks on weekends. Several cases of myocardial infarction and even sudden death have been reported in workers employed in such industries, occurring during the period of cessation of nitrate exposure. A thorough study with coronary angiography did not reveal atherosclerotic changes in the coronary arteries of persons who had myocardial infarction during the period of cessation of contact with nitrates [6]. In addition, it was noted that in workers who experienced retrosternal chest pain on weekends, angina attacks completely disappeared after prolonged isolation from nitrate exposure. The condition that occurred during the period of a sharp cessation of the action of nitrates began to be called the rebound phenomenon [7]. For a long time it was believed that the nitrate withdrawal syndrome described above occurs only when in contact with large doses of them at work, but is not typical for the clinical use of these drugs. However, special studies have shown that nitrate withdrawal syndrome also occurs in clinical practice. In table. 2 shows the main symptoms associated with the manifestation of isosorbide dinitrate withdrawal syndrome in patients with stable exertional angina.
In addition, it was noted that in workers who experienced retrosternal chest pain on weekends, angina attacks completely disappeared after prolonged isolation from nitrate exposure. The condition that occurred during the period of a sharp cessation of the action of nitrates began to be called the rebound phenomenon [7]. For a long time it was believed that the nitrate withdrawal syndrome described above occurs only when in contact with large doses of them at work, but is not typical for the clinical use of these drugs. However, special studies have shown that nitrate withdrawal syndrome also occurs in clinical practice. In table. 2 shows the main symptoms associated with the manifestation of isosorbide dinitrate withdrawal syndrome in patients with stable exertional angina.
| Manifestations | Isosorbide dinitrate | Nifedipine |
| Reduced exercise tolerance (more than 1 minute treadmill test) | 5 | 12 |
| Increase in angina attacks (>25%) | 2 | 8 |
| Occurrence of angina at rest | 0 | 3 |
| BP increase (>20/10 mmHg) | 1 | 2 |
| Changes in the terminal part of the ventricular complex on ECG | 1 | 1 |
| The numbers indicate the number of patients | ||
Interest in the nitrate withdrawal syndrome increased significantly in the late 1980s, when various regimens for intermittent administration of these drugs began to be widely recommended in order to prevent the development of addiction to them. Intermittent administration of nitrates suggests that during the day there should be a period when the body is free from the action of nitrate (nitrate-free period). During this period, the sensitivity to nitrates, which decreased as a result of their previous use, has time to recover [4].
Intermittent administration of nitrates suggests that during the day there should be a period when the body is free from the action of nitrate (nitrate-free period). During this period, the sensitivity to nitrates, which decreased as a result of their previous use, has time to recover [4].
It turned out, however, that against the background of intermittent administration of nitrates, there is a risk of developing a withdrawal syndrome. Thus, it has been shown that after removing stickers of transdermal nitroglycerin from the skin at night, approximately 8% of patients develop rest angina attacks that were absent before [8]. Episodes of asymptomatic myocardial ischemia can also be one of the manifestations of the nitrate withdrawal syndrome in their intermittent administration [1]. All this indicates that the intermittent administration of nitrates, along with undoubted advantages, is fraught with a very real danger.
Studies have shown, however, that the clinical significance of nitrate withdrawal syndrome with intermittent administration is directly dependent on the severity of the patient's condition: in patients with a relatively mild and stable course of the disease, short-term drug withdrawal, as a rule, does not cause negative consequences and is quite safe. In patients with a more severe course of coronary heart disease, in the presence of signs of hemodynamic disturbance, the consequences of the withdrawal syndrome can be much more severe [9]. Therefore, the intermittent administration of nitrates is quite acceptable in patients with a stable and relatively mild course of coronary artery disease (this includes patients with stable angina of the 1-3rd functional class). In patients with more severe CAD (stable angina 4th functional class) or signs of instability (unstable angina, acute myocardial infarction), intermittent administration of nitrates should be avoided [10].
In patients with a more severe course of coronary heart disease, in the presence of signs of hemodynamic disturbance, the consequences of the withdrawal syndrome can be much more severe [9]. Therefore, the intermittent administration of nitrates is quite acceptable in patients with a stable and relatively mild course of coronary artery disease (this includes patients with stable angina of the 1-3rd functional class). In patients with more severe CAD (stable angina 4th functional class) or signs of instability (unstable angina, acute myocardial infarction), intermittent administration of nitrates should be avoided [10].
- Beta blockers
With the possibility of developing a withdrawal syndrome of beta-blockers, clinicians encountered almost immediately, as soon as these drugs began to be used in clinical practice. It has been shown that sudden discontinuation of propranolol can cause a sharp increase in angina attacks, severe arrhythmias, acute myocardial infarction and even sudden death. Subsequently, it turned out that such severe manifestations of the propranolol withdrawal syndrome are observed in no more than 5% of patients, much more often doctors encounter such a manifestation of the propranolol withdrawal syndrome as the occurrence of tachycardia [11].
Subsequently, it turned out that such severe manifestations of the propranolol withdrawal syndrome are observed in no more than 5% of patients, much more often doctors encounter such a manifestation of the propranolol withdrawal syndrome as the occurrence of tachycardia [11].
It also turned out that different beta-blockers have the ability to cause withdrawal syndrome to an unequal degree. Thus, the severity of the withdrawal syndrome of cardioselective beta-blockers, in particular atenolol, was much less than the severity of propranolol withdrawal syndrome [12]. Obviously, it is possible to prevent the occurrence of beta-blocker withdrawal syndrome only by gradually canceling them. Withdrawal regimens for these drugs, however, can vary significantly. Thus, a number of authors recommend canceling propranolol by gradually reducing the dose stepwise over 6-9days. Other authors consider another scheme to be safer: the dose of propranolol is immediately reduced to a small one (30 mg per day), then the drug is taken at this dosage for two weeks, and then completely canceled [13].
- Calcium antagonists
The possibility of a withdrawal syndrome from this group of drugs until recently caused controversy among researchers [14]. At present, it has become obvious that these drugs are quite different from each other in terms of pharmacological properties, respectively, they are capable of causing withdrawal syndrome to varying degrees.
| Figure 1 Comparison of the severity of nifedipine and diltiazem withdrawal symptoms after stopping four weeks of regular use of these drugs (in 24 patients with coronary artery disease with stable exertional angina) |
| The y-axis shows the duration of the test with dosed physical activity on the treadmill until the development of an attack of moderate intensity angina, from K - control period L - treatment with O - drug withdrawal * — significance of differences with the control period (p<0.  005) 005) Arrow indicates signs of nifedipine withdrawal syndrome |
Verapamil. This drug appears to be associated with the least risk of withdrawal of all antianginal drugs. This is primarily due to the ability of verapamil to accumulate in the body with regular use. Accordingly, with the discontinuation of verapamil, the drug is excreted from the body for a sufficiently long time and its effect persists for several days after taking the last dose of the drug.
To date, no studies are known that clearly prove the existence of verapamil withdrawal syndrome. As a result of comparing the effect of discontinuation of propranolol and verapamil, carried out in 20 patients with stable angina pectoris, it was possible to prove that after discontinuation of verapamil, there was a gradual return of the frequency of angina attacks to the initial level, and after discontinuation of propranolol, on the contrary, a sharp increase in angina attacks and a significant decrease exercise tolerance [15].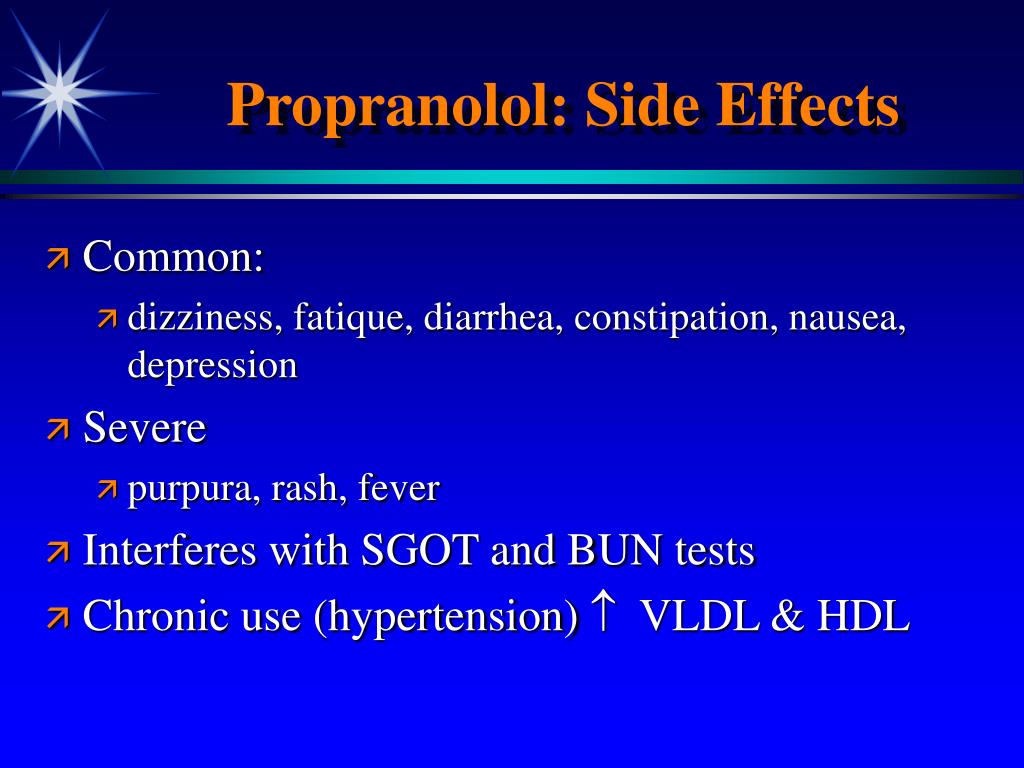 This gives grounds to assert that if it is necessary to stop taking verapamil, it can be canceled immediately, without a gradual dose reduction.
This gives grounds to assert that if it is necessary to stop taking verapamil, it can be canceled immediately, without a gradual dose reduction.
With regular use of verapamil, even in the form of conventional tablets, its effect can be considered fairly uniform, so this drug never causes a rebound phenomenon.
Diltiazem. Works on the study of the possibility of developing diltiazem withdrawal syndrome in patients with stable angina pectoris have not been carried out so far.
We recently conducted a special study, the purpose of which was, in particular, to establish whether a withdrawal syndrome occurs after an abrupt cessation of the regular (four times a day) intake of this drug for four weeks. The reference drug was nifedipine, which was prescribed for the same period and then canceled. The study was conducted using a double-blind, randomized, parallel method.
It was demonstrated that diltiazem withdrawal was associated only with the fact that the number and duration of episodes of myocardial ischemia (as measured by 24-hour ECG monitoring) returned to baseline. Exercise tolerance, according to the treadmill test, simply returned to the values recorded before the start of treatment on the background of discontinuation of diltiazem (see figure). In contrast, on the first day of nifedipine withdrawal, there was a marked increase (compared with the control period) in the number of episodes of myocardial ischemia, while there was a decrease in exercise tolerance below the level recorded before the start of treatment.
Exercise tolerance, according to the treadmill test, simply returned to the values recorded before the start of treatment on the background of discontinuation of diltiazem (see figure). In contrast, on the first day of nifedipine withdrawal, there was a marked increase (compared with the control period) in the number of episodes of myocardial ischemia, while there was a decrease in exercise tolerance below the level recorded before the start of treatment.
Thus, abrupt discontinuation of diltiazem did not cause withdrawal symptoms; abrupt discontinuation of nifedipine, on the contrary, led to an objective deterioration in the condition of patients, which can be considered a manifestation of the withdrawal syndrome of this drug.
Nifedipine. It has been reported above that abrupt discontinuation of regular nifedipine [10] may cause withdrawal symptoms. However, and this seems to be more important, it has been found that nifedipine withdrawal syndrome may occur during therapy with this drug if short-acting dosage forms are used. We have shown that in the morning, before taking the next dose of nifedipine, exercise tolerance was lower than in the control period (this condition is called the zero hour phenomenon). At the same time, in a number of patients, the occurrence of rest angina attacks, which were absent before the appointment of treatment, was noted [16].
We have shown that in the morning, before taking the next dose of nifedipine, exercise tolerance was lower than in the control period (this condition is called the zero hour phenomenon). At the same time, in a number of patients, the occurrence of rest angina attacks, which were absent before the appointment of treatment, was noted [16].
As with nitrates, the effects of nifedipine withdrawal are directly related to the severity of the patient's condition. If in patients with a relatively mild course of the disease, the withdrawal syndrome, even if it manifests itself with obvious symptoms, may not have any serious consequences, then in patients with an unstable course of the disease, the consequences of this syndrome may be much more severe. There is every reason to believe that a number of severe complications, including such as the development of acute myocardial infarction and sudden death, recorded in some studies in which nifedipine was prescribed for unstable angina and acute myocardial infarction in a short-acting dosage form, were explained precisely by the development syndrome of short-term withdrawal of nifedipine (rebound phenomenon) against the background of its use [17, 18].
It must be emphasized that some drugs, in particular beta-blockers, can prevent the occurrence of the rebound phenomenon. Thus, it has been proven that if the use of short-acting nifedipine as monotherapy for unstable angina is associated with an increased risk of complications, then the use of the same drug in combination with beta-blockers is safe and can even improve the prognosis of the disease [17]. It should be noted that the rebound phenomenon is most characteristic of nifedipine, which is produced in the form of so-called fast-disintegrating capsules (in Russia it is known as adalat), which contribute to a rapid increase and an equally rapid decrease in the concentration of the drug in the blood. When prescribing nifedipine in the form of conventional tablets (in Russia they are known under the names Corinfar, Cordafen, etc.), the severity of the rebound syndrome may be less.
Recently, special dosage forms of nifedipine of prolonged action (for example, nifedipine-SR, known in Russia under the name adalat-SL, or nifedipine-GITS, known in Russia under the name osmo-adalat) have been created that help maintain a more or less constant concentration of the drug in the blood. These dosage forms, according to currently available data, do not cause the rebound phenomenon and can be used in patients with unstable CAD.
These dosage forms, according to currently available data, do not cause the rebound phenomenon and can be used in patients with unstable CAD.
The presented data indicate that the withdrawal syndrome in its various forms can significantly affect the efficacy and safety of therapy in patients with coronary artery disease. Situations are quite real when neglecting the risk of developing a withdrawal syndrome leads to a result opposite to the desired one (as happened, for example, when trying to prescribe short-acting nifedipine as monotherapy to patients with unstable angina pectoris). On the contrary, the competent prescription of the drug, taking into account its possible side and undesirable effects, as well as the characteristics of the course of the disease in a particular patient, can significantly improve the result of treatment.
Literature
1. Martsevich S. Yu., Koutishenko N. P. , Metelitsa V. I. Abrupt cessation of short-term continuous treatment with isosorbide dinitrate may cause a rebound increase in silent myocardial ischaemia in patients with stable angina pectoris. Heart 1996; 75:447-450.
, Metelitsa V. I. Abrupt cessation of short-term continuous treatment with isosorbide dinitrate may cause a rebound increase in silent myocardial ischaemia in patients with stable angina pectoris. Heart 1996; 75:447-450.
2. Thadani U. Nitrate tolerance, rebound and their clinical significance in stable angina pectoris, unstable angina, and heart failure // Cardiovasc. Drugs Ther. 1996; 10:735-742.
3. Laws G. C. The effects of nitroglycerin upon those who manufacture it. J.A.M.A. 1898; 31: 793.
4. Carmichael P., Lieben J. Sudden death in explosive workers // Arch. Environ. health. 1963; 7: 50.
5. Lund R. P., Haggendahl J., Johnsson G. Withdrawal symptoms in workers exposed to nitroglycerine // Br. J. Ind. Med. 1968; 25: 136.
6. Lange R. L., Reid M. S., Tresch D. D., Keelan M. H., Bernhard V. M., Coolidge G. Nonatheromatous ischemic heart disease following withdrawal from industrial nitroglycerin exposure. Circuit 1972; 46:666-678.
Circuit 1972; 46:666-678.
7. Abrams J. Nitrate tolerance and dependence // Am. Heart J. 1980; 99:113-123.
8. DeMots H., Glasser S. P., Transdermal-Nitro Trial Study Group. Intermittent transdermal nitroglycerin therapy in the treatment of chronic stable angina // J. Amer. Coll. cardiol. 1989; 13:786-793.
9. Martsevich S. Y., Koutishenko N., Metelitsa V. I. Withdrawal effects of antianginal therapy: comparison of isosorbide dinitrate and nifedipine // Int. J. Cardiol. 1998; 64:137-144.
10. Martsevich S. Yu. Refractoriness to antianginal drugs and development of tolerance to them in patients with ischemic heart disease. Methods of detection, clinical significance, possibility of prevention. Abstract dis. doc. honey. Sciences. M., 1994: 44 p.
11. Shand D. G., Wood A. J. J. Propranolol withdrawal syndrome - why? Circulation 1978; 58:202-203.
12. Walker P. R., Marshall A. J., Farr S., Bauminger B., Walters G., Barritt D. W. Abrupt withdrawal of atenolol in patients with severe angina // Br. Heart J.1985; 53:276-282.
R., Marshall A. J., Farr S., Bauminger B., Walters G., Barritt D. W. Abrupt withdrawal of atenolol in patients with severe angina // Br. Heart J.1985; 53:276-282.
13. Rangno R. E., Nattel S., Lutterodt A. Prevention of propranolol withdrawal mechanism by extended small dose propranolol schedule // Am. J. Cardiol. 1982; 49: 828-833.
14. Lambert C. R., Pepine C. J. Is there a calcium-antagonist withdrawal syndrome? // Practice. cardiol. 1987; 13:190-195.
15. Frishman W. H., Klein N., Strom J., Cohen M. N., Shamoon H., Willens H., Klein P., Roth S., Iorio L., LeJemtel T., Pollack S., Sonnenblick H. Comparative effects of abrupt withdrawal of propranolol and verapamil in angina pectoris. Am. J. Cardiol. 1982; 50:1191-1195.
16. Martsevich S. Yu., Kutishenko N. P., Alimova E. V., Slastnikova I. D., Metelitsa V. I. Calcium antagonists diltiazem and nifedipine: comparison of efficacy in single and long-term use in patients with stable tension angina.