Acute anxiety stress disorder
Acute Stress Disorder - Mental Health Disorders
By
John W. Barnhill
, MD, New York-Presbyterian Hospital
Last full review/revision Apr 2020| Content last modified Sep 2022
CLICK HERE FOR THE PROFESSIONAL VERSION
Acute stress disorder is an intense, unpleasant, and dysfunctional reaction beginning shortly after an overwhelming traumatic event and lasting less than a month. If symptoms persist longer than a month, people are diagnosed as having posttraumatic stress disorder Posttraumatic Stress Disorder (PTSD) Posttraumatic stress disorder (PTSD) involves intense, unpleasant, and dysfunctional reactions beginning after an overwhelming traumatic event. Events that threaten death or serious injury can... read more (PTSD).
(See also Overview of Trauma- and Stress-Related Disorders Overview of Trauma- and Stress-Related Disorders Trauma- and stress-related disorders result from exposure to a traumatic or stressful event. Specific disorders include acute stress disorder and posttraumatic stress disorder. These disorders... read more .)
People with acute stress disorder have been exposed to a terrifying event. They may experience it directly or indirectly. For example, direct exposure may involve experiencing serious injury, violence, or the threat of death. Indirect exposure may involve witnessing events happening to others or learning of events that occurred to close family members or friends. People mentally re-experience the traumatic event, avoid things that remind them of it, and have increased anxiety.
People with this disorder may have dissociative symptoms Overview of Dissociative Disorders Occasionally everyone has minor problems integrating their memories, perceptions, identity, and consciousness. For example, people may drive somewhere and then realize that they do not remember... read more . For example, they may feel emotionally numb or disconnected from themselves. They may feel that they are not real.
They may feel that they are not real.
The number of people with acute stress disorder is unknown. The likelihood of developing acute stress disorder is greater when traumatic events are severe or recurrent.
Acute stress disorder is diagnosed when people have been
In addition, they also must have had at least 9 of the following symptoms for 3 days up to 1 month:
Recurring, uncontrollable, and intrusive distressing memories of the event
Recurring distressing dreams of the event
Feelings that the traumatic event is recurring—for example, in flashbacks
Intense psychologic or physical distress when reminded of the event (for example, by entering a similar location, or by sounds similar to those heard during the event)
A persistent inability to experience positive emotions (such as happiness, satisfaction, or loving feelings)
An altered sense of reality (for example, feeling in a daze or as if time has slowed)
Memory loss for an important part of the traumatic event
Efforts to avoid distressing memories, thoughts, or feelings associated with the event
Efforts to avoid external reminders (people, places, conversations, activities, objects, and situations) associated with the event
Disturbed sleep
Irritability or angry outbursts
Excessive attention to the possibility of danger (hypervigilance)
Difficulty concentrating
An exaggerated response to loud noises, sudden movements, or other stimuli (startle response)
In addition, symptoms must cause significant distress or significantly impair functioning.
Doctors also check to see whether symptoms could result from use of a drug or another disorder.
- Self-care
Supportive measures
Many people recover from acute stress disorder once they are removed from the traumatic situation and given appropriate support in the form of understanding, empathy for their distress, and an opportunity to describe what happened and their reaction to it. Some people benefit from describing their experience several times. Friends and loved ones can often provide this support. Otherwise, doctors or other health care professionals are helpful.
Sometimes doctors temporarily give drugs to relieve anxiety or help people sleep, but other drugs (such as antidepressants) are usually not given.
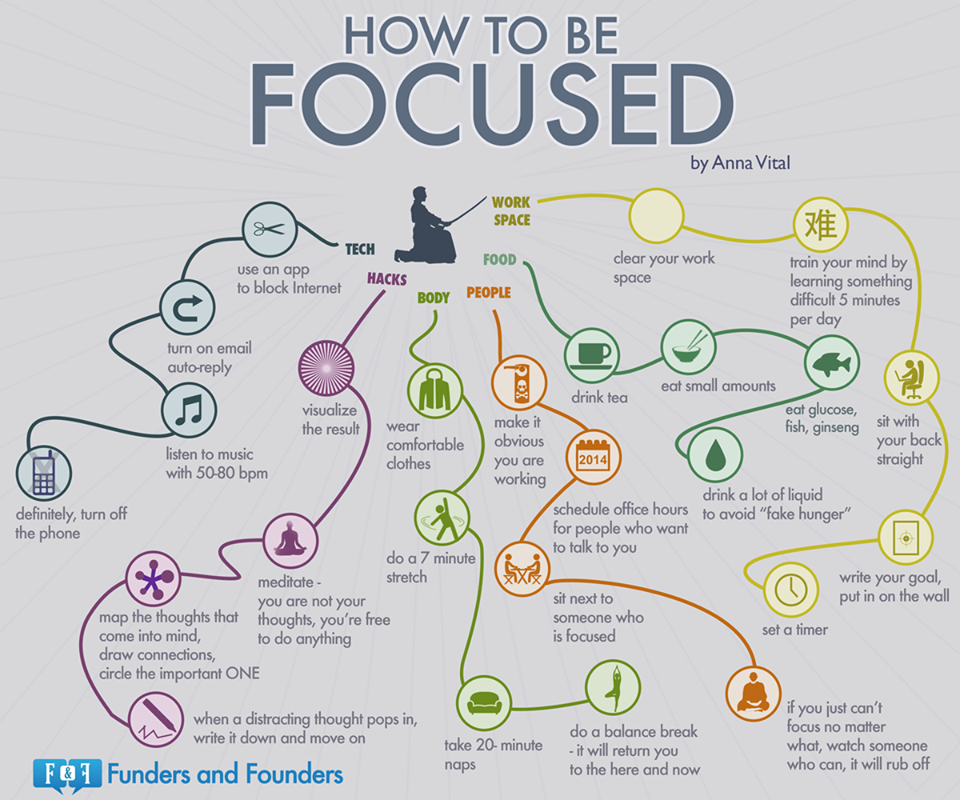
Self-care is crucial during and after a crisis or trauma. Self-care can be divided into 3 components:
Personal safety
Physical health
Mindfulness
Personal safety is fundamental.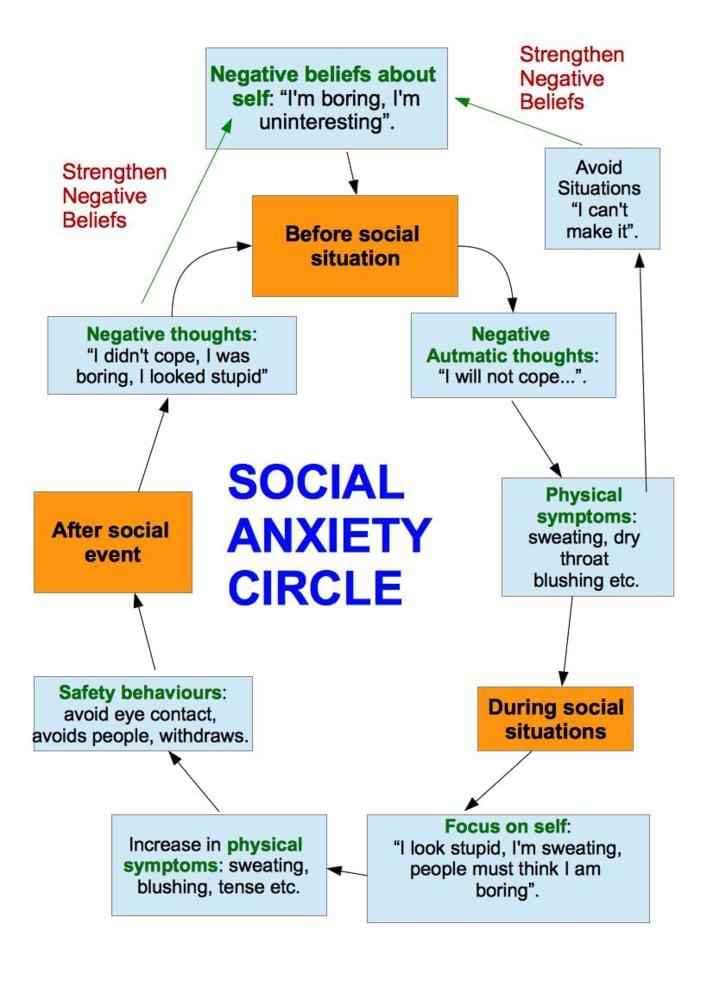 After a single traumatic episode, people are better able to process the experience when they know that they and their loved ones are safe. It can be difficult, however, to gain complete safety during ongoing crises such as domestic abuse, war, or an infectious pandemic. During such ongoing difficulties, people should seek the guidance of experts on how they and their loved ones can be as safe as possible.
After a single traumatic episode, people are better able to process the experience when they know that they and their loved ones are safe. It can be difficult, however, to gain complete safety during ongoing crises such as domestic abuse, war, or an infectious pandemic. During such ongoing difficulties, people should seek the guidance of experts on how they and their loved ones can be as safe as possible.
Physical health can be put at risk during and after traumatic experiences. Everyone should try to maintain a healthy schedule of eating, sleeping, and exercise. Drugs that sedate and intoxicate (for example, alcohol) should be used sparingly, if at all.
A mindful approach to self-care aims to reduce the feelings of stress, boredom, anger, sadness, and isolation that traumatized people normally experience. If circumstances allow, at-risk individuals should make and follow a daily normal daily schedule, for example, get up, shower, get dressed, go outside and take a walk, and prepare and eat regular meals.
It is useful to practice familiar hobbies as well as activities that sound fun and distracting: draw a picture, watch a movie, or cook.
Community involvement can be crucial, even if it is difficult to maintain human connection during a crisis.
Stretching and exercise are terrific, but it can be equally helpful to sit still and count one's own breaths or listen carefully for surrounding sounds. People can become preoccupied with the trauma or crisis, and so it is useful to choose to think of other things: read a novel or get engaged with a puzzle. Unpleasant emotions may typically feel "frozen" during and after a trauma, and it can be a relief to find activities that shift the feeling state: laugh, watch a fun movie, do something silly, or draw with crayons. Under stress, people can become short-tempered, even with people they care about.
Spontaneous kindness can be a win/win solution for everyone: sending a nice note, making someone cookies, and offering up a smile may not only be a nice surprise for the recipient, but they can reduce the hopelessness and passivity that tends to be part of the sender's experience of trauma.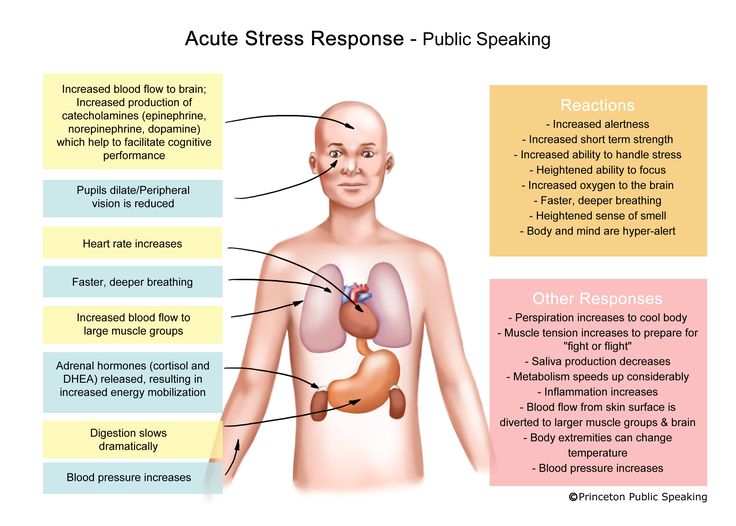
CLICK HERE FOR THE PROFESSIONAL VERSION
Copyright © 2022 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Acute Stress Disorder: Causes, Symptoms, and Diagnosis
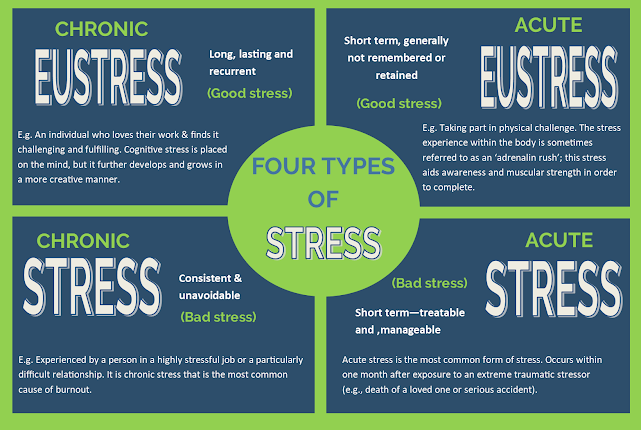
Acute stress disorder (ASD) typically occurs within one month of a traumatic event. Symptoms are similar to those seen in post traumatic stress disorder (PTSD), however this disorder is temporary, lasing from a few days to a month. Some people with this disorder can go on to develop PTSD.
What’s acute stress disorder?
In the weeks after a traumatic event, you may develop an anxiety disorder called acute stress disorder (ASD).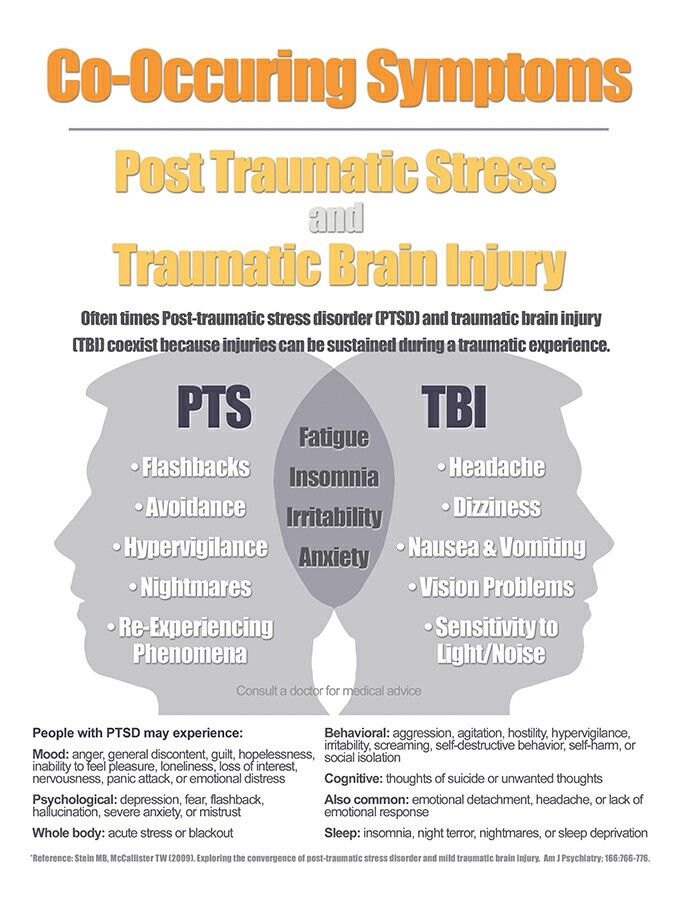 ASD typically occurs within one month of a traumatic event. It lasts at least three days and can persist for up to one month. People with ASD have symptoms similar to those seen in post-traumatic stress disorder (PTSD).
ASD typically occurs within one month of a traumatic event. It lasts at least three days and can persist for up to one month. People with ASD have symptoms similar to those seen in post-traumatic stress disorder (PTSD).
Experiencing, witnessing, or being confronted with one or more traumatic events can cause ASD. The events create intense fear, horror, or helplessness. Traumatic events that can cause ASD include a:
- death
- threat of death to oneself or others
- threat of serious injury to oneself or others
- threat to the physical integrity of oneself or others
Approximately 6 to 33 percent of people who experience a traumatic event develop ASD, according to the U.S. Department of Veterans Affairs. This rate varies based on the nature of the traumatic situation.
Anyone can develop ASD after a traumatic event. You may have an increased risk of developing ASD if you have:
- experienced, witnessed, or been confronted with a traumatic event in the past
- a history of ASD or PTSD
- a history of certain types of mental problems
- a history of dissociative symptoms during traumatic events
The symptoms of ASD include:
Dissociative symptoms
You’ll have three or more of the following dissociative symptoms if you have ASD:
- feeling numb, detached, or being emotionally unresponsive
- a reduced awareness of your surroundings
- derealization, which occurs when your environment seems strange or unreal to you
- depersonalization, which occurs when your thoughts or emotions don’t seem real or don’t seem like they belong to you
- dissociative amnesia, which occurs when you cannot remember one or more important aspects of the traumatic event
Reexperiencing the traumatic event
You’ll persistently re-experience the traumatic event in one or more of the following ways if you have ASD:
- having recurring images, thoughts, nightmares, illusions, or flashback episodes of the traumatic event
- feeling like you’re reliving the traumatic event
- feeling distressed when something reminds you of the traumatic event
Avoidance
You may avoid stimuli that cause you to remember or re-experience the traumatic event, such as:
- people
- conversations
- places
- objects
- activities
- thoughts
- feelings
Anxiety or increased arousal
The symptoms of ASD may include anxiety and increased arousal. The symptoms of anxiety and increased arousal include:
The symptoms of anxiety and increased arousal include:
- having trouble sleeping
- being irritable
- having difficulty concentrating
- being unable to stop moving or sit still
- being constantly tense or on guard
- becoming startled too easily or at inappropriate times
Distress
The symptoms of ASD may cause you distress or disrupt important aspects of your life, such as your social or work settings. You may have an inability to start or complete necessary tasks, or an inability to tell others about the traumatic event.
Your primary doctor or mental healthcare provider will diagnose ASD by asking you questions about the traumatic event and your symptoms. It’s also important to rule out other causes such as:
- drug abuse
- side effects of medications
- health problems
- other psychiatric disorders
If you don’t already have a primary care doctor or a mental healthcare professional, you can browse doctors in your area through the Healthline FindCare tool.
Your doctor may use one or more of the following methods to treat ASD:
- a psychiatric evaluation to determine your specific needs
- hospitalization if you’re at risk of suicide or harming others
- assistance in obtaining shelter, food, clothing, and locating family, if necessary
- psychiatric education to teach you about your disorder
- medication to relieve symptoms of ASD, such as antianxiety medications, selective serotonin reuptake inhibitors (SSRIs), and antidepressants
- cognitive behavioral therapy (CBT), which may increase recovery speed and prevent ASD from turning into PTSD
- exposure-based therapies
- hypnotherapy
Online therapy options
Read our review of the best online therapy options to find the right fit for you.
Many people with ASD are later diagnosed with PTSD. A diagnosis of PTSD is made if your symptoms persist for more than a month and cause a significant amount of stress and difficulty functioning.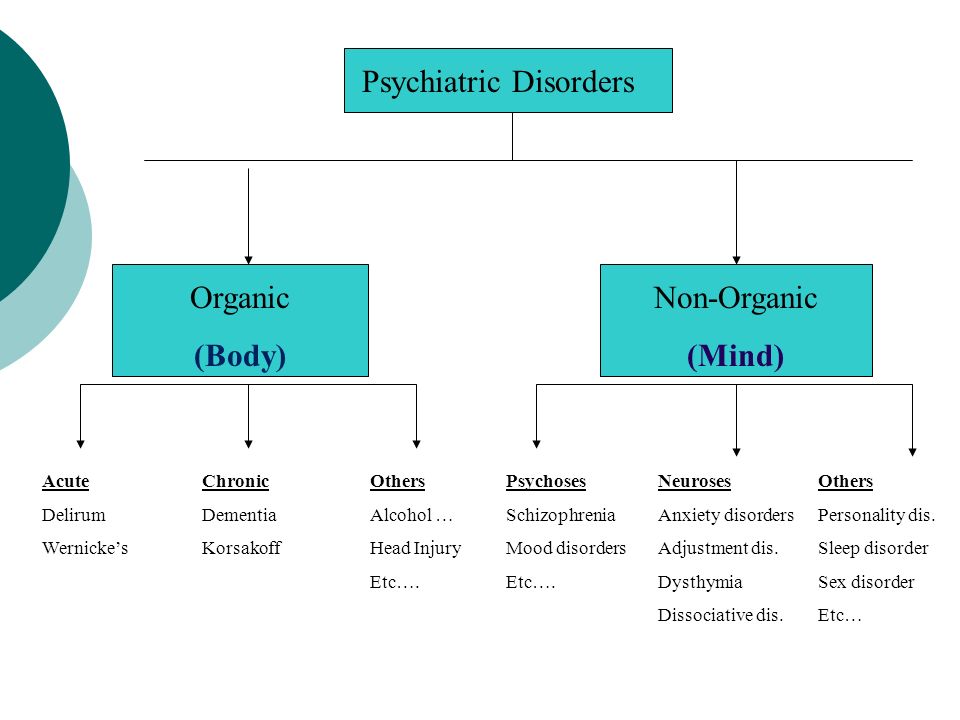
Treatment may reduce your chances of developing PTSD. Approximately 50 percent of PTSD cases resolve within six months, whereas others may persist for years.
Because there’s no way to ensure that you never experience a traumatic situation, there’s no way to prevent ASD. However, there are things that can be done to reduce your likelihood of developing ASD.
Getting medical treatment within a few hours of experiencing a traumatic event may reduce the likelihood that you’ll develop ASD. People who work in jobs that carry a high risk for traumatic events, such as military personnel, may benefit from preparation training and counseling to reduce their risk of developing ASD or PSTD if a traumatic event does occur. Preparation training and counseling may involve fake enactments of traumatic events and counseling to strengthen coping mechanisms.
Anxiety Disorder - American Medical Clinic
US
Medical Clinic
St. Petersburg, embankment of the river Moika, 78.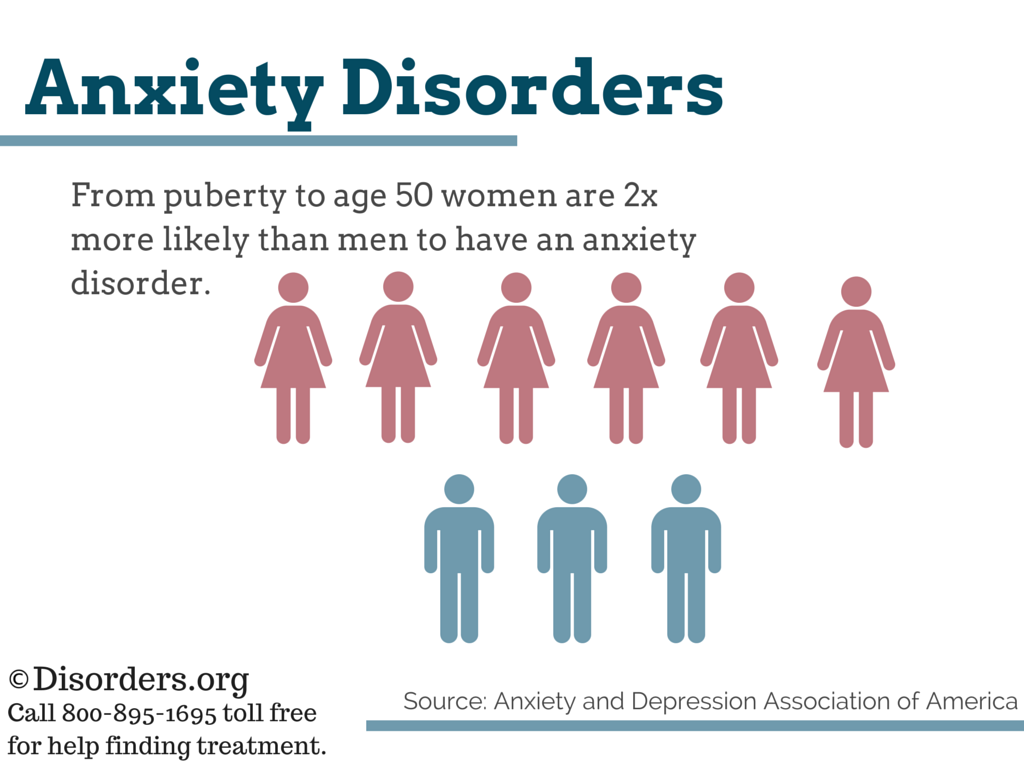
+7 (812) 740-20-90
Content:
Anxiety disorder is a mental disorder characterized by a state of generalized persistent anxiety. Unlike ordinary short-term stress, which, for example, is associated with public speaking, the disease lasts for a long time - for several months or more.
Excessive anxiety, tension and fear that patients with anxiety disorders experience can be accompanied by both psychological and physical ailments. In order to avoid dangerous complications such as paranoia, nervousness, etc. it is necessary to recognize the signs of the disease as early as possible and consult a doctor.
Symptoms of anxiety disorder
Main symptoms of anxiety disorder:
-
Psychological:
- excessive anxiety and tension in connection with current affairs or for no particular reason;
- unreasonable fear for your life and the lives of loved ones;
- stress, inability to relax;
- decreased performance, difficulty concentrating;
- irritability.
-
Physical:
- constant feeling of fatigue and weakness;
- muscle tension;
- pain in the head and abdomen;
- trembling, chills;
- sleep disorders;
- increased sweating;
- shortness of breath up to a feeling of suffocation;
- nausea and vomiting;
- stool disorders.
The degree of manifestation of symptoms or their combinations depends on the form of anxiety disorder and the degree of neglect of the disease.
Forms of anxiety disorder
The following forms of anxiety disorder are distinguished:
- Adaptive Anxiety Disorder Excessive anxiety and other emotional responses are due to difficulties in adapting to a particular stressful situation.
- Generalized Anxiety Disorder (aka anxiety-depressive disorder) - excessive anxiety persists constantly and is associated with a large number of life circumstances - the patient regularly experiences unreasonable fear for his life, work, family, etc.

- Anxiety-phobic disorder - causes panic attacks that cause extreme fear and a sense of impending death; fear of people and their large crowds; fear of some serious illness.
All these obsessive thoughts are unpleasant and alien to patients, often they themselves are not aware of the cause of their occurrence. Seeing a doctor as soon as possible will solve this problem and return the person to a normal life.
Anxiety treatment
Treatment of anxiety disorder is carried out in a complex, in several directions. It includes:
-
Drug therapy - based on the characteristics of the patient's body and the disease, the doctor will prescribe a set of medications to eliminate symptoms:
- benzodiazepines - help relieve physical stress;
- buspirone, alprazolam - reduce anxiety;
- antidepressants - tune in to positive thinking and keep disturbing thoughts under control.

Remember that drug therapy for anxiety disorders is carried out under the strict supervision of a physician. The above drugs, if used incorrectly, cause changes in the patient's behavior. Among them are suicidal thoughts, etc.
-
Psychological therapy - with the help of various psychological methods, the doctor helps the patient overcome his anxiety and anxiety:
- cognitive-behavioral therapy - with the help of rational persuasion, the doctor changes the general way of thinking of the patient in a positive direction;
- behavioral therapy - the doctor teaches the patient relaxation techniques - muscle relaxation, deep breathing, visualization, etc.
The degree of application of certain methods of therapy and the duration of treatment depend on the form of the disease and the degree of its neglect. Remember that it is the timely visit to the doctor that guarantees the absence of severe mental complications.

See also
- Operations in gynecology
- Colonoscopy in St. Petersburg under anesthesia
their systematics, diagnostics and pharmacotherapy
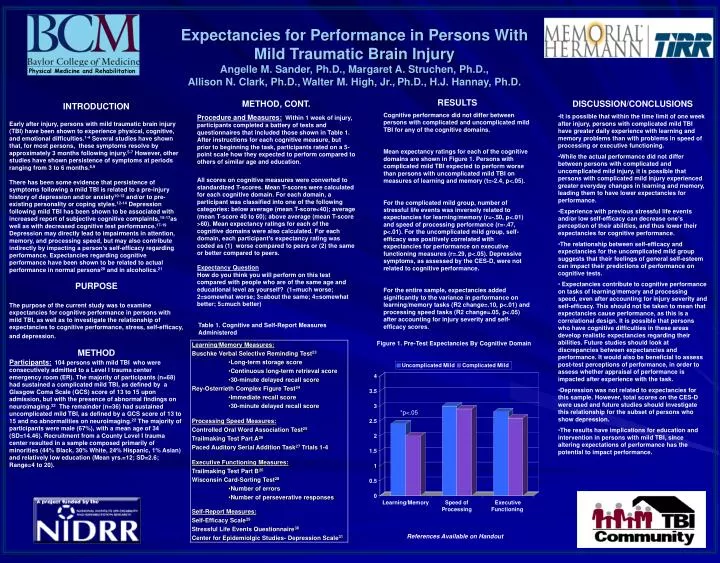
Over the past decade, there has been a significant increase in interest in psychopathological conditions, the clinical picture of which is determined by anxiety. In our country, these states have traditionally been considered within the framework of affective disorders, neuroses and psychogenic reactions. However, the scientific data accumulated during the 1970s and 1980s indicate the need to revise the traditional nosological views and single out anxiety disorders as a separate diagnostic category [1,2]. It usually includes panic disorder, various types of phobias, generalized anxiety disorder, obsessive-compulsive disorder, and mental stress disorders. An extensive group of superficial mental disorders, characterized by the so-called subsyndromal anxiety, adjoins this category.
Epidemiological studies show that anxiety disorders are the second most common group of mental disorders after mood disorders. Their prevalence in the population ranges from 6% to 13.6%. [3]. At the same time, they have a huge impact on disability and quality of life [4].
Since anxiety is a universal psychophysiological phenomenon associated with adaptation to stress, it is important to distinguish between normal (adaptive) and pathological anxiety [5, 6].
Normal anxiety can be defined as a feeling of emotional discomfort due to uncertain prospects. It is associated with a threatening situation, increases with an increase in its subjective significance, increases in conditions of lack of time and information. Adaptive anxiety, as a rule, is short-lived and does not reach excessive strength that interferes with activity (Table 1).
Anxiety is a universal psychophysiological phenomenon associated with adaptation to stress.
Pathological anxiety can also be provoked by external circumstances, but its occurrence is more determined by internal causes.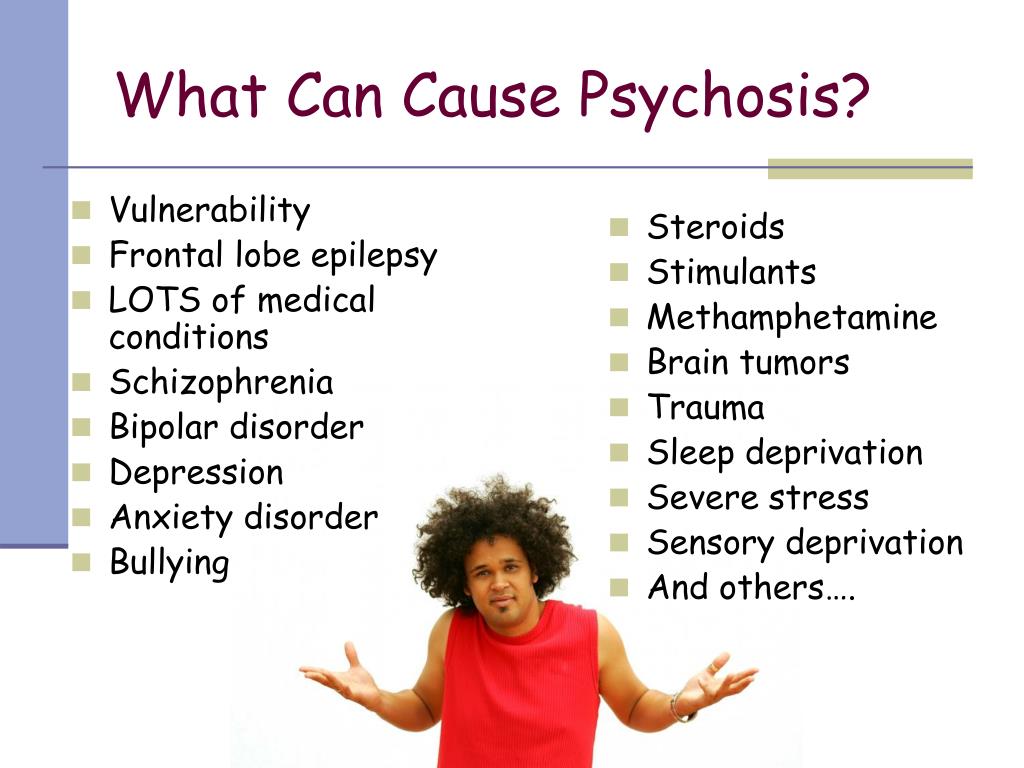 Pathological anxiety is not associated with a real threat and is inadequate to the significance of the situation.
Pathological anxiety is not associated with a real threat and is inadequate to the significance of the situation.
An important difference between pathological anxiety is its strong severity. Therefore, painful anxiety causes severe subjective experiences, leads to a decrease in productive activity, and often takes over consciousness. In addition, pathological anxiety usually manifests itself in the form of specific psychopathological syndromes.
Table 1. Differences between adaptive and pathological anxiety
| Normal (adaptation) alarm | Pathological anxiety |
|---|---|
| Driven by a real external threat | Caused by internal causes, but can be provoked by external circumstances |
| Increases in terms of the importance of choice | Not adequate to the real significance of the situation |
| Increases with lack of information | Does not depend on objective information |
| Increases when there is a lack of time, helps to speed up decision making | Blocks constructive decision making |
| Can be controlled and suppressed by the subject himself | Does not give in to subjective control, takes possession of consciousness |
| Subjectively experienced as a natural reaction to the situation | Subjectively experienced as excessive and inadequate, has specific clinical manifestations |
Detailed psychopathological qualification of these syndromes is often difficult and requires the involvement of psychiatrists.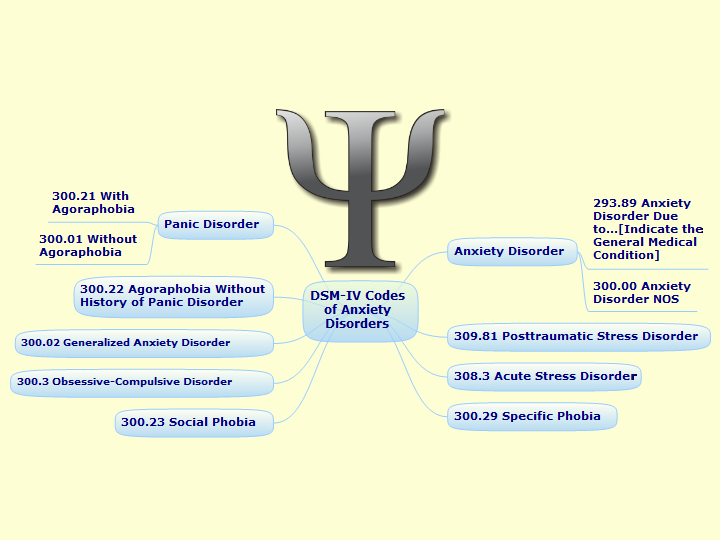 However, in most cases, to determine the medical tactics, it is sufficient to establish only the type of pathological anxiety. There are two such types: paroxysmal and constant [1]. Each of these types can be divided into several subtypes that correspond to the main nosographic groups of anxiety disorders.
However, in most cases, to determine the medical tactics, it is sufficient to establish only the type of pathological anxiety. There are two such types: paroxysmal and constant [1]. Each of these types can be divided into several subtypes that correspond to the main nosographic groups of anxiety disorders.
The main distinguishing features of paroxysmal anxiety are episodic occurrence and intensity. A typical attack is characterized by rapidly increasing anxiety, which turns into fear, accompanied by a large number of autonomic disorders and unpleasant bodily sensations. [6,7]. Paroxysmal anxiety is usually experienced as a feeling of immediate threat to the existence of the individual or the integrity of his "I". Patients experiencing such anxiety complain of inexplicable fear, a sense of impending death, or a sense of loss of reason. Their behavior at the time of the attack is characterized by lethargy or uncoordinated and limited excitement - panic.
The physiological mechanisms of paroxysmal anxiety are associated with pathological activation of the hypothalamus and autonomic centers of the brain stem, which determines polymorphic autonomic symptoms, as well as unpleasant bodily sensations, which the doctor pays attention to first of all when contacting such a patient. However, it should be borne in mind that the overlying structures of the brain, such as the limbic system, hypothalamus, amygdala, septum, hippocampus, prefrontal cortex, and others, also play an important role in the genesis of paroxysmal anxiety [8].
However, it should be borne in mind that the overlying structures of the brain, such as the limbic system, hypothalamus, amygdala, septum, hippocampus, prefrontal cortex, and others, also play an important role in the genesis of paroxysmal anxiety [8].
With social phobia, fear is associated with situations of interpersonal contact. The main experience is the fear of being in a humiliating or awkward position.
Anxiety disorders include panic disorder, agoraphobia, social phobia, and specific phobia. All of these disorders are characterized by anxiety attacks that may occur spontaneously (as in panic disorder) or in response to some stimulus. Depending on the irritant that provokes an anxiety attack, there are various variants of phobias. In agoraphobia, anxiety is provoked by situations in which the patient feels alone and cannot receive the necessary help in case of illness. Usually this feeling occurs in confined spaces, when moving away from home, in a crowd, when it is necessary to remain alone. Agoraphobia tends to develop in people who already have a panic disorder or who have experienced isolated panic attacks in the past.
Agoraphobia tends to develop in people who already have a panic disorder or who have experienced isolated panic attacks in the past.
With social phobia, anxiety attacks are associated with situations of interpersonal contact, or the need to act in the presence of other people (so-called performance phobias). The main experience that takes place in such patients is the fear of being in a humiliating or awkward position.
With a specific phobia, anxiety attacks occur upon contact with some objects or situations specific to each patient. The most common irritants are animals or insects (dogs, spiders, etc.), natural phenomena (thunderstorm, hurricane, etc.), the sight of blood, injections, and certain circumstances (airplane flight, elevator ride, etc.). ).
The most important signs of phobias, in addition to the connection of paroxysmal anxiety with a specific stimulus, also include the avoidance of this irritant by the patient. This phenomenon is usually referred to as avoidant or restrictive behavior.![]()
Anxiety disorders are very common. Table 2 shows the indicators of their prevalence throughout life [1]. The medical significance of these disorders is primarily due to the difficulties of differential diagnosis. Compliance issues are also of great importance, especially in cases where patients, due to anxiety, avoid visiting a doctor, do not adhere to a regimen or do not take medications.
Table 2. Lifetime prevalence in the population of disorders accompanied by paroxysmal anxiety
| Disorders | Intravital frequency (%) |
|---|---|
| panic disorder | 1.7 - 2.9 |
| Agoraphobia | 0.7 - 1.1 |
| social phobia | 3.5 - 6.7 |
| specific phobia | 7.2 - 11.3 |
Permanent alarm
A distinctive feature of this type of anxiety is its constant presence for a long time.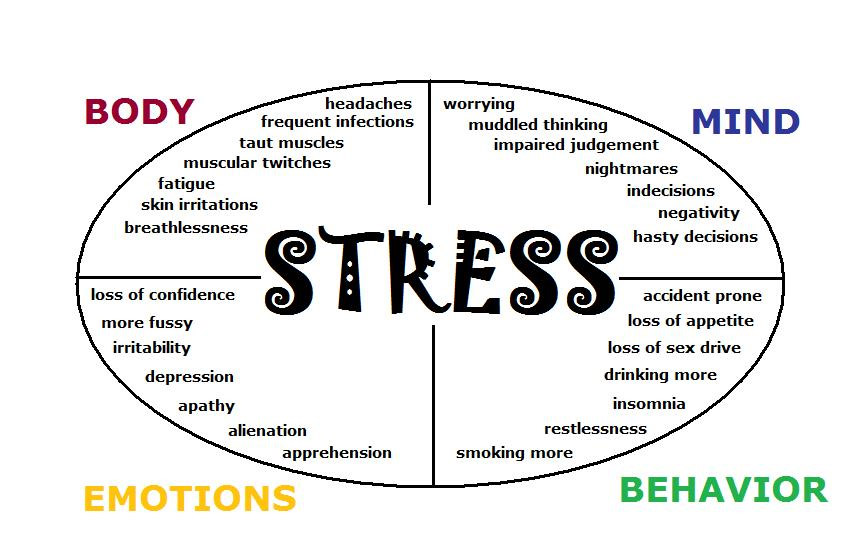 [9, 10, 11]. Constant anxiety, like paroxysmal anxiety, is closely related to autonomic arousal, but this relationship is not expressed to the same extent. Therefore, autonomic symptoms do not necessarily take a large place in the clinical picture. Persistent anxiety is usually experienced as excitement or worry about upcoming events or their consequences. This type of anxiety in different disorders has its own clinical features, which are discussed below.
[9, 10, 11]. Constant anxiety, like paroxysmal anxiety, is closely related to autonomic arousal, but this relationship is not expressed to the same extent. Therefore, autonomic symptoms do not necessarily take a large place in the clinical picture. Persistent anxiety is usually experienced as excitement or worry about upcoming events or their consequences. This type of anxiety in different disorders has its own clinical features, which are discussed below.
The mechanisms of constant anxiety as well as paroxysmal anxiety are associated with the limbic system, amygdala, septum, and hippocampus. However, in its genesis, apparently, the prefrontal cortex and brain systems responsible for the perception of exteroreceptor stimuli (thalamus, somatosensory, auditory, and visual cortex) play a greater role [12, 13]. There is evidence of a close relationship between constant anxiety and cognitive impairment, which is especially noticeable in the initial subclinical stages of dementia.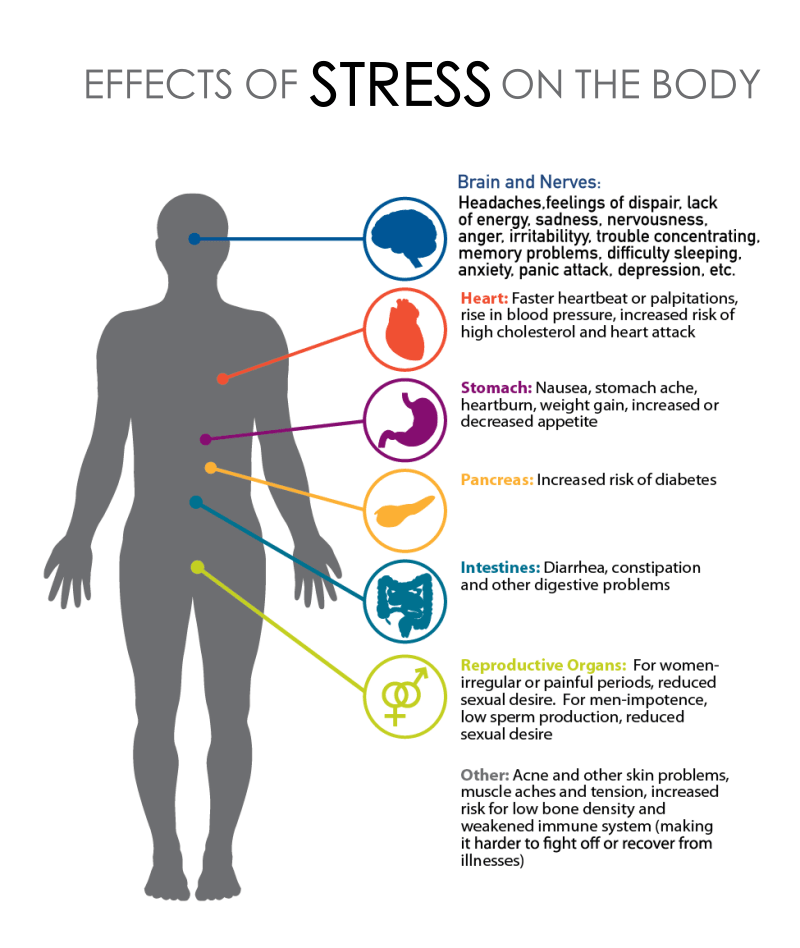
Persistent anxiety occurs in generalized anxiety disorder, adjustment disorders, stress disorders, and a variety of other conditions encountered in medical practice.
Patients with generalized anxiety often show signs of increased autonomic arousal, which is expressed in tachycardia, sweating, dry mucous membranes, difficulty breathing, nausea, chills, gastrointestinal and other somatic symptoms.
The main symptom of generalized anxiety disorder is excessive chronic anxiety, which is supported by constantly arising anxious expectations and anxiety. These concerns arise from various unrelated issues (for example, due to family, economic status, work, health status, etc.). These occasions are of a worldly nature, often replace each other or coexist. At the same time, the readiness for the emergence of anxiety remains even when the events that disturbed the patient are safely resolved. Patients with generalized anxiety disorder are usually aware of the excessiveness of their anxiety, as well as the inability to cope with it on their own. At the same time, they believe that these unrest have real grounds.
At the same time, they believe that these unrest have real grounds.
In addition to anxious expectations, with generalized anxiety, there are violations of the sleep-wake cycle, as well as an increase in general excitability. Patients with generalized anxiety disorder note a feeling of internal tension, combined with increased fatigue, irritability, impaired concentration, and sleep disorders. Generalized anxiety disorder is also accompanied by psychomotor symptoms. Patients experience fussiness and restlessness, an inability to physically relax, and increased muscle tone. Against this background, tension headaches, back pain, a symptom of "restless" legs, tremors and other manifestations close to them can be observed.
Patients with generalized anxiety often show signs of increased autonomic arousal, which is expressed in tachycardia, sweating, dry mucous membranes, difficulty breathing, nausea, chills, gastrointestinal and other somatic symptoms. However, these signs are currently not considered by most specialists as necessary for the diagnosis of generalized anxiety disorder.
Constant anxiety is often noted in disorders caused by the effects of mental stress. The most common variant of these conditions are adjustment disorders. Mental disorders in these cases develop after significant or subjectively significant changes in a person's life (moving, changing marital status, industrial or academic failures, the onset of a disease, etc.). These disorders are usually short-lived, but sometimes they can drag on for months or even years. For many patients, constant anxiety comes to the fore. It manifests itself in doubts, hesitations, fears of the future, as well as in prolonged psychophysical stress. Sleep and appetite disturbances, increased fatigue are typical, explosiveness, capriciousness, suspiciousness or alertness are sometimes noted. These conditions are often accompanied by autonomic disorders in the form of arterial hypertension or digestive disorders. Headaches and other somatic symptoms may be noted.
Stress disorders constitute a special subgroup of conditions accompanied by constant anxiety. These disorders occur when exposed to extreme psychic trauma, i.e. in situations involving the threat of death or serious physical injury to the subject himself or to other people. Currently, it is customary to distinguish between acute stress disorder and post-traumatic stress disorder. Usually, acute stress disorder refers to psychopathological conditions that developed during or immediately after exposure to a mental trauma and lasted from 2 days to 4 weeks [2]. If the stress disorder lasts more than 1 month, then we should talk about the formation of post-traumatic stress disorder (PTSD). And if it lasts more than 3 months, then the indicated disorder passes into the chronic phase. It is important to note that PTSD can occur long after exposure to stress.
These disorders occur when exposed to extreme psychic trauma, i.e. in situations involving the threat of death or serious physical injury to the subject himself or to other people. Currently, it is customary to distinguish between acute stress disorder and post-traumatic stress disorder. Usually, acute stress disorder refers to psychopathological conditions that developed during or immediately after exposure to a mental trauma and lasted from 2 days to 4 weeks [2]. If the stress disorder lasts more than 1 month, then we should talk about the formation of post-traumatic stress disorder (PTSD). And if it lasts more than 3 months, then the indicated disorder passes into the chronic phase. It is important to note that PTSD can occur long after exposure to stress.
Although constant anxiety underlies stress disorders, it does not always come to the fore in the clinical picture. The clinic of these disorders is determined by a wide range of states of altered consciousness and self-awareness (mental numbness or emotional anesthesia, a sense of detachment, depersonalization-derealization phenomena, amnesia).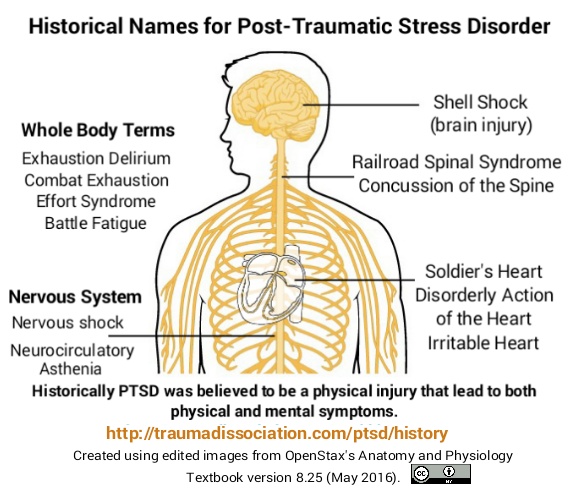 These phenomena are usually combined with intrusive (i.e., invading consciousness) symptoms in the form of repetitive thoughts, images, dreams, illusions, experiences, and mastering ideas. This also includes signs of increased mental sensitivity and avoidance of stimuli reminiscent of the transferred stress. Another sign of a stress disorder is a persistent increase in excitability. This is expressed in difficulty falling asleep and intermittent sleep, fearfulness, irritability, outbursts of anger, impaired concentration, mood swings. For post-traumatic stress disorder, the appearance of persistent vegetative changes and a general change in the reactivity of the body is characteristic.
These phenomena are usually combined with intrusive (i.e., invading consciousness) symptoms in the form of repetitive thoughts, images, dreams, illusions, experiences, and mastering ideas. This also includes signs of increased mental sensitivity and avoidance of stimuli reminiscent of the transferred stress. Another sign of a stress disorder is a persistent increase in excitability. This is expressed in difficulty falling asleep and intermittent sleep, fearfulness, irritability, outbursts of anger, impaired concentration, mood swings. For post-traumatic stress disorder, the appearance of persistent vegetative changes and a general change in the reactivity of the body is characteristic.
Constant anxiety is often observed in other mental disorders, the description of the clinical features of which in this work is impossible due to the limited scope of its scope. However, it should be noted that this type of anxiety, as a rule, accompanies persistent vegetative changes that appear to general practitioners in the form of functional somatic disorders (for example, thermoneurosis, psychogenic dyspnea, “stress” gastritis, irritable bowel syndrome, idiopathic urticaria, etc. ) , as well as eating disorders, sexual disorders and insomnia of an inorganic nature. In many of these cases, we are talking about subsyndromal anxiety, manifested by chronic tension, inability to relax, bad feelings, increased excitability, irritability and fatigue. And, although the unambiguous nosographic qualification of these conditions can be very difficult, therapeutic approaches are in many respects similar to those used for other forms of constant anxiety.
) , as well as eating disorders, sexual disorders and insomnia of an inorganic nature. In many of these cases, we are talking about subsyndromal anxiety, manifested by chronic tension, inability to relax, bad feelings, increased excitability, irritability and fatigue. And, although the unambiguous nosographic qualification of these conditions can be very difficult, therapeutic approaches are in many respects similar to those used for other forms of constant anxiety.
Constant anxiety is quite common [1] (Table 3). Especially often it is detected in patients with somatic diseases. Thus, the frequency of generalized anxiety disorder in coronary heart disease reaches 24% [14], and in diabetes mellitus it ranges from 14% to 40% [15, 16]. 18–40% of trauma patients develop clinically circumscribed PTSD [17, 18], as does a large number of individuals who have undergone heart surgery [19]. At the same time, the symptoms of anxiety can resemble signs of the corresponding diseases, affect the general well-being of the patient and his quality of life.
Table 3. Lifetime prevalence in the population of disorders accompanied by persistent anxiety
| Disorders | Intravital frequency (%) |
|---|---|
| generalized anxiety disorder | 4.2 - 6.6 |
| Post Traumatic Stress Disorder | 7.8 - 9.2 |
Psychopharmacotherapy of pathological anxiety
Pharmacological therapy of anxiety disorders is currently based on the use of two drugs of two classes: anti-anxiety drugs and antidepressants. In turn, among anti-anxiety agents, benzodiazepine tranquilizers (BZD) and hydroxyzine (Atarax) should be pointed out, and among antidepressants, selective serotonin reuptake inhibitors (SSRIs).
Benzodiazepines
The advantages of BZD are their high anti-anxiety activity, good tolerability, as well as the rapid onset of a therapeutic effect. The negative aspects of the action of BZD are associated with the risk of addiction, sedation, impaired cognitive processes and increased tolerance. With the abrupt cancellation of drugs in this group, a recoil syndrome usually occurs, which is expressed in increased mental manifestations of anxiety and its autonomic accompaniment. In the presence of physical dependence, a withdrawal syndrome appears, which is characterized by severe anxiety, sleep disturbance, nausea, headaches, dizziness, increased sensitivity to light and noise, tremors, an increase in body temperature, fluctuations in blood pressure, convulsions and changes in consciousness up to delirium.
The negative aspects of the action of BZD are associated with the risk of addiction, sedation, impaired cognitive processes and increased tolerance. With the abrupt cancellation of drugs in this group, a recoil syndrome usually occurs, which is expressed in increased mental manifestations of anxiety and its autonomic accompaniment. In the presence of physical dependence, a withdrawal syndrome appears, which is characterized by severe anxiety, sleep disturbance, nausea, headaches, dizziness, increased sensitivity to light and noise, tremors, an increase in body temperature, fluctuations in blood pressure, convulsions and changes in consciousness up to delirium.
Constant anxiety is very common and is especially often detected in patients with somatic diseases.
The use of BZD in anxiety disorders should be very limited and, if possible, reduced to only episodic use for paroxysmal anxiety, in particular, for the relief of anxiety attacks.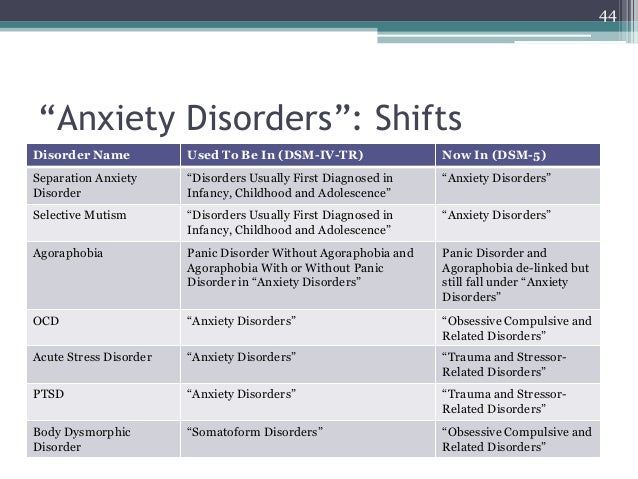 It is advisable (but not indisputable) their short-term use in acute stress anxiety.
It is advisable (but not indisputable) their short-term use in acute stress anxiety.
BZD should not be prescribed to patients with a tendency to abuse psychoactive substances and personality disorders. The use of BZD should be avoided in persistent anxiety, especially in generalized anxiety disorder, adjustment disorders, PTSD, and subsyndromic anxiety. The use of these drugs in these cases leads to unreasonable dose escalation, cognitive impairment, dependence formation, and motor disorders [20].
Hydroxyzine (Atarax)
Hydroxyzine has been actively used to treat anxiety relatively recently. According to its neurochemical properties, it is an h2-histamine receptor antagonist. This drug also has a low anticholinergic activity. Its mechanisms of action remain unexplored. However, the therapeutic effects of hydroxyzine are not limited to an effect on the histamine system, since under experimental conditions this drug exhibits an anti-anxiety effect similar to that of fluoxetine, imipramine, and chlordiazepoxide and does not coincide with the effect of another typical h2-histamine receptor antagonist, chlorpheniramine [21].
Hydroxyzine has proven to be very effective in the treatment of chronic anxiety and, first of all, in the treatment of generalized anxiety disorder. It also has high activity against prolonged adjustment disorders and persistent subsyndromal anxiety. There is evidence that hydroxyzine reduces the number of panic attacks in panic disorder, and may also help normalize sleep. It can be successfully used in various conditions characterized by prolonged psycho-vegetative stress. Useful properties of hydraxizine in the treatment of somatic manifestations of anxiety are its antiemetic effect and antipruritic effect.
The psychopharmacological action of hydroxyzine consists of two phases. In the first phase (within 5-8 days), the general sedative effect, characteristic of many antihistamines, predominates. This period may be accompanied by a number of side effects (drowsiness, lethargy, weakness), apparently due to a direct antihistamine effect. The second phase, usually starting from 6-9 days of therapy, is characterized by a gradual disappearance of the sedation phenomenon and an increase in anti-anxiety and vegetative-stabilizing effects. An important feature of the action of hydroxyzine, which distinguishes it from benzodiazepines, is a positive effect on memory and attention [22, 23].
An important feature of the action of hydroxyzine, which distinguishes it from benzodiazepines, is a positive effect on memory and attention [22, 23].
The advantage of hydroxyzine compared to benzodiazepines is the lack of development of tolerance to its ankisolititic effect even with long-term use. When you stop taking this drug, there is no withdrawal syndrome and no symptoms of rebound. Unlike benzodiazepines, its use does not develop dependence. Hydroxyzine does not have euphoric properties. And after a sharp cessation of taking this drug, a gradual increase in anxiety is noted only after 3-5 days.
Antidepressants
There are several classes of antidepressants, many of which have been successfully used in the treatment of anxiety disorders. However, antidepressants, selective serotonin reuptake inhibitors (SSRIs), remain the drugs of first choice until recently. The drugs of this group are indicated, first of all, for paroxysmal anxiety (panic disorder, agoraphobia, social phobia, some cases of specific phobia). In addition, they have worked well in cases of severe persistent anxiety (post-traumatic stress disorder and generalized anxiety).
In addition, they have worked well in cases of severe persistent anxiety (post-traumatic stress disorder and generalized anxiety).
When prescribing SSRIs, it is necessary to keep in mind the transient increase in anxiety (the so-called initial anxiety), the appearance of gastrointestinal discomfort, sleep disturbances, and the overwhelming effect of these drugs on sexual functions and appetite, which is often noted during their appointment. There is evidence of an increase in body weight under their influence, as well as cases of withdrawal syndrome. In addition, one should take into account possible drug interactions due to the inhibitory effect of SSRIs on the liver enzyme system - cytochrome P450 [24].
Other agents (sedatives, antipsychotics, anticonvulsants) are sometimes used with success in anxiety disorders.
A clinically significant problem is the choice between different drugs in this category. Since various SSRIs are approximately the same in their pharmacological activity, their selection in the treatment of pathological anxiety should be based on the spectrum of side effects, as well as the ratio between stimulating and sedative properties.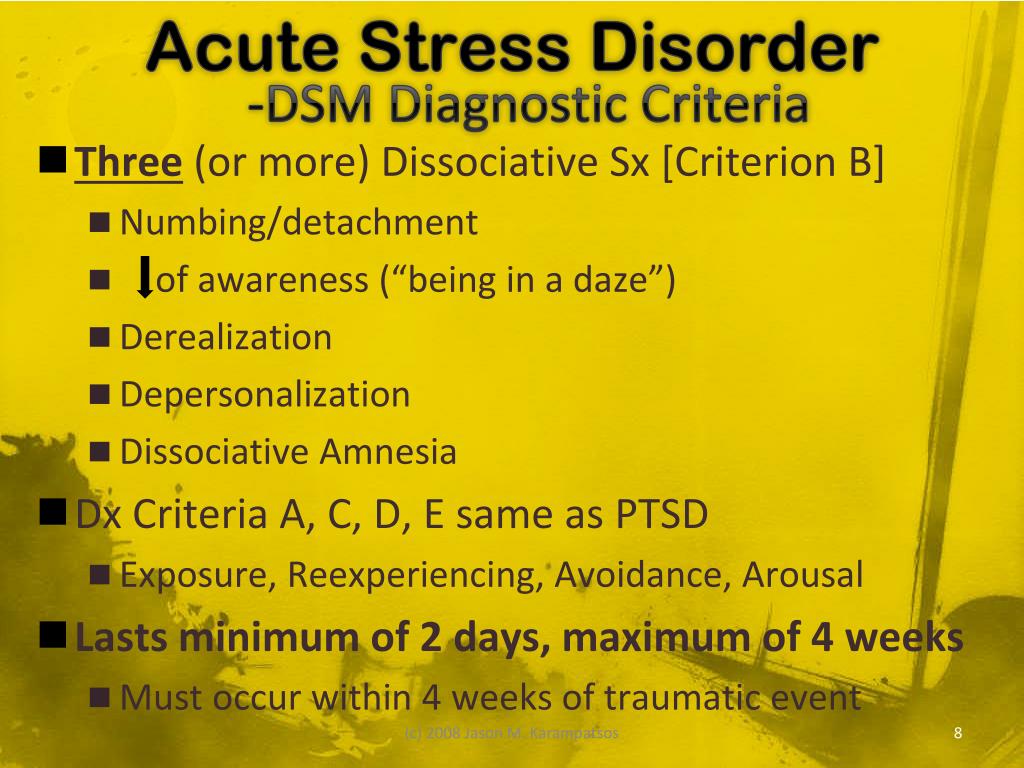 Reliable information on this subject is still scarce. However, based on literature data and clinical experience, some preliminary guidelines can be used.
Reliable information on this subject is still scarce. However, based on literature data and clinical experience, some preliminary guidelines can be used.
So, according to the severity of the sedative effect, SSRIs can be distributed as follows: Fluvoxamine => Paroxetine => Sertraline => Citalopram => Fluoxetine.
According to the ability to provoke initial anxiety: Fluoxetine => Sertraline => Paroxetine => Citalopram => Fluvoxamine.
According to the ability to cause a withdrawal syndrome: Paroxetine => Sertraline => Citalopram => Fluvoxamine => Fluoxetine
By overall frequency of side effects: Fluvoxamine => Fluoxetine => Paroxetine => Sertraline => Citalopram
In terms of side effects, the most common side effects of citalopram are headache, dry mouth, tremors, dizziness, and sweating. Sometimes there is increased drowsiness, with an overdose, a pronounced cardiotoxic effect is possible.
Side effects of fluoxetine include headache, rash, psychomotor agitation, akathisia, sleep disturbances, and appetite suppression. In addition, this drug has the longest half-life, which, on the one hand, reduces the possibility of withdrawal syndrome and allows it to be used in patients with low compliance. On the other hand, with fluoxetine therapy, a longer period is required to establish an equilibrium concentration and the appearance of a therapeutic effect.
In addition, this drug has the longest half-life, which, on the one hand, reduces the possibility of withdrawal syndrome and allows it to be used in patients with low compliance. On the other hand, with fluoxetine therapy, a longer period is required to establish an equilibrium concentration and the appearance of a therapeutic effect.
The most common side effects of fluvoxamine are nausea, diarrhea, dizziness, and tremor. The named drug has a pronounced sedative effect, but it almost does not affect sexual functions and does not lead to an increase in body weight.
Paroxetine is more likely to cause sexual dysfunction, sweating, and weight gain. It has a fairly pronounced sedative effect. It can also cause constipation. And when paroxetine treatment is stopped, a withdrawal syndrome occurs more often than with other SSRIs.
Sertraline has the ability to cause diarrhea, headache, dizziness and tremors, disturb sleep and cause sexual dysfunction. This drug is the only one from this group that does not cause an increase in prolactin.