How long do the side effects of prozac last
Do Prozac Side Effects Go Away Over Time? – Even
Prozac, also known by the generic name fluoxetine, was the first selective serotonin reuptake inhibitor (SSRI) approved by the U.S. Food and Drug Administration (FDA) for the treatment of depression. Since its debut in 1988, Prozac has been one of the most commonly prescribed drugs in the United States and continues to rank among the top five prescribed antidepressants.
Although Prozac is a safe and effective medication for many people, the nature of the drug and its long active duration in your body can cause side effects for some people.
So, what are the side effects of Prozac, and do Prozac side effects ever go away?
What are the side effects of Prozac?
Prozac is associated with a number of side effects, some of which can be particularly troubling and intolerable for certain patients.
Common side effects associated with Prozac include:
- Nausea and vomiting
- Diarrhea
- Nervousness and anxiousness
- Insomnia
- Weight gain
- Headache
- Dry mouth
- Dizziness
- Sexual side effects, including erectile dysfunction, loss of libido, and difficulty achieving orgasm
- Tremors
- Suicidal thoughts and behaviors
The most common side effects of Prozac affect the gastrointestinal system and include nausea, vomiting, and diarrhea. It is believed that Prozac affects the digestive tract as a result of its action on its serotonin receptors, which are found not only in the brain but also in the gut. Gastrointestinal symptoms most commonly affect patients early on in their treatment with Prozac.
Other side effects, such as tremors, may develop only after a patient has taken Prozac for an extended period of time and may get worse the longer the medication is used. Doctors and patients should weigh the pros and cons of using Prozac to treat depression.
Do Prozac side effects ever go away?
If you’re one of the people experiencing side effects while using Prozac, it may feel like you’ll never get relief from your symptoms. However, the side effects that most people experience while taking Prozac, including nausea, diarrhea, vomiting, insomnia, and headaches, tend to be short lived and typically will resolve on their own within a few weeks as your body gets used to the medication.
Most patients find that stabilizing their dose resolves some of these initial side effects. However, Prozac also causes other side effects that may remain for the duration of a patient’s use of the medication.
Side effects such as sexual dysfunction (erectile dysfunction, loss of libido, difficulty achieving orgasm, etc), tremors, particularly of the face, weight gain, and suicidal thoughts and behaviors tend to be more persistent and may last for the duration of a patient’s use of Prozac. Some patients may be able to find relief from their symptoms by lowering their dose with the approval and supervision of their doctor or by switching medications.
However, it should be noted that Prozac is generally regarded as one of the antidepressants that causes the fewest side effects. Therefore, switching medications may not cut out side effects completely.
Is there anything I can do to minimize the side effects of Prozac?
As noted above, it may be possible to minimize the side effects caused by Prozac by safely reducing the dose of Prozac under the approval and supervision of a healthcare professional.
However, this will not be an acceptable strategy for all patients because some may need to take higher doses of the medication in order to relieve their depression symptoms.
Patients who do not want to or cannot reduce the dose of their medication may be able to minimize the side effects of antidepressants with a nutritional supplement that helps support healthy brain function, healthy digestion, a healthy metabolism, and overall well-being.
Summary
Mild side effects of Prozac typically go away within a few weeks of starting the medication as your body adjusts, but some side effects, including weight gain, sexual side effects, tremors, and suicidal thoughts and behaviors may continue for the duration of the use of the medication.
Patients who are experiencing side effects from Prozac may benefit from taking a specially formulated nutritional supplement from Even designed to support healthy brain function, healthy digestion, a healthy metabolism, and overall well being.
Sources:
https://www.webmd.com/depression/features/prozac-pro-con#1
https://www.nhs.uk/medicines/fluoxetine-prozac/
https://www.goodrx.com/blog/common-myths-and-misconceptions-about-antidepressants/
https://www.womenshealthmag.com/health/a18930189/prozac-side-effects/
Fluoxetine (Prozac) | NAMI: National Alliance on Mental Illness
Brand names:
- Prozac®
- Capsules: 10 mg, 20 mg, 40 mg
- Prozac Weekly®
- Capsules (delayed-release): 90 mg
- Sarafem®
- Tablets: 10 mg, 20 mg
- Fluoxetine
- Capsules: 10 mg, 20 mg, 40 mg
- Capsules (delayed release): 90 mg
- Liquid: 20 mg/5ml
- Tablets: 10 mg, 20 mg, 60 mg
Generic name: Fluoxetine (floo OKS e teen)
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Fluoxetine And What Does It Treat?
Fluoxetine is an antidepressant medication that works in the brain. It is approved for the treatment of major depressive disorder (MDD), obsessive compulsive disorder (OCD), panic disorder, bulimia nervosa, and premenstrual dysphoric disorder (PMDD).
Symptoms of depression include:
- Depressed mood - feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, and helpless
- Loss of interest or pleasure in your usual activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving and thinking in slow motion)
- Suicidal thoughts or behaviors
Obsessive compulsive disorder (OCD) occurs when a person experiences the following symptoms at the same time:
- Obsessions (unwanted, recurrent, and disturbing thoughts)
- Compulsions (repetitive, ritualized behaviors that the person feels driven to perform in order to lessen the anxiety produced by the obsessions)
Panic disorder occurs when a person experiences unexpected and repeated episodes of intense fear. These episodes have physical symptoms including chest pain, shortness of breath, heart palpitations, sweating, dizziness, and nausea. Fear of future episodes is also part of panic disorder.
These episodes have physical symptoms including chest pain, shortness of breath, heart palpitations, sweating, dizziness, and nausea. Fear of future episodes is also part of panic disorder.
Bulimia is a condition where a person binges on food, then uses various methods to purge (e.g., use of laxatives, vomiting) in order to prevent weight gain.
Premenstrual dysphoric disorder (PMDD) is a condition where a woman experiences depression, tension, and irritability for a few days prior to menstruation that end when menstruation begins. These symptoms are more severe than those of premenstrual syndrome (PMS).
Fluoxetine may also be helpful when prescribed “off-label” for body dysmorphic disorder, binge eating disorder, generalized anxiety disorder (GAD), social phobia (also known as social anxiety disorder), dysthymia, or posttraumatic stress disorder (PTSD). “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment.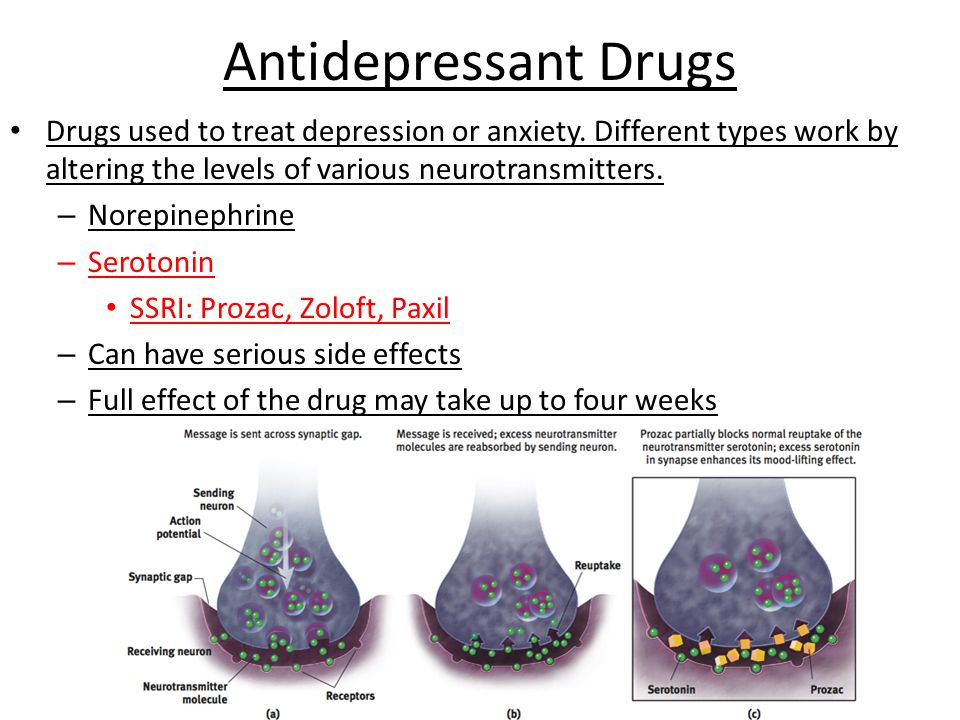 They should be clear about the limits of the research around that medication and if there are any other options.
They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Fluoxetine?
Do not stop taking fluoxetine, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medicine.
Missing doses of fluoxetine may increase your risk for relapse in your symptoms.
Stopping fluoxetine abruptly may result in one or more of the following withdrawal symptoms: irritability, nausea, dizziness, vomiting, nightmares, headache, and/or paresthesias (prickling, tingling sensation on the skin).
Depression is also a part of bipolar illness. People with bipolar disorder who take antidepressants may be at risk for "switching" from depression into mania. Symptoms of mania include "high" or irritable mood, very high self-esteem, decreased need for sleep, pressure to keep talking, racing thoughts, being easily distracted, frequently involved in activities with a large risk for bad consequences (for example, excessive buying sprees).
Medical attention should be sought if serotonin syndrome is suspected. Please refer to serious side effects for signs/symptoms.
Are There Specific Concerns About Fluoxetine And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with MDD who wish to become pregnant face important decisions. Untreated MDD has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers. For women who take antidepressant medications during weeks 13 through the end of their pregnancy (second and third trimesters), there is a risk that the baby can be born before it is fully developed (before 37 weeks).
For mothers who have taken SSRIs during their pregnancy, there appears to be less than a 1% chance of infants developing persistent pulmonary hypertension. This is a potentially fatal condition that is associated with use of the antidepressant in the second half of pregnancy.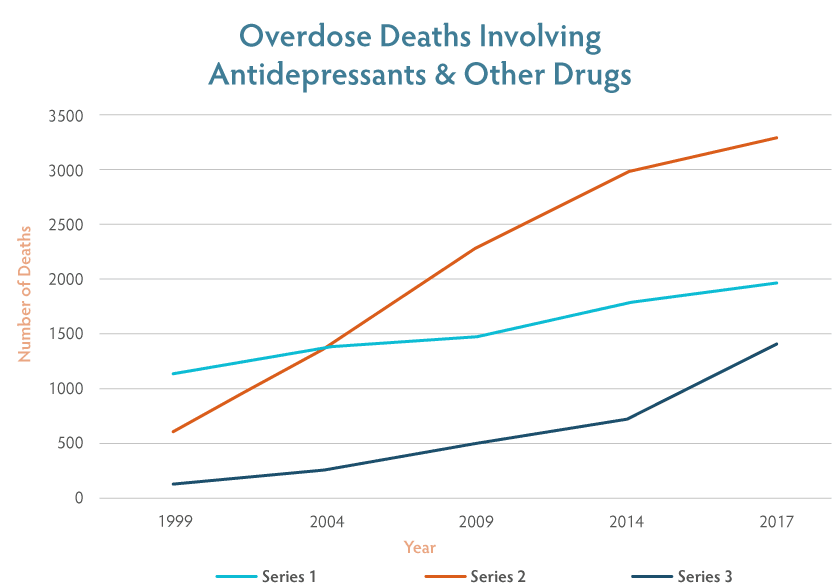 However, women who discontinued antidepressant therapy were five times more likely to have a depression relapse than those who continued their antidepressant. If you are pregnant, please discuss the risks and benefits of antidepressant use with your health care provider.
However, women who discontinued antidepressant therapy were five times more likely to have a depression relapse than those who continued their antidepressant. If you are pregnant, please discuss the risks and benefits of antidepressant use with your health care provider.
Caution is advised with breastfeeding since fluoxetine does pass into breast milk.
What Should I Discuss With My Health Care Provider Before Taking Fluoxetine?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your provider. Some side effects may pass with time, but others may require changes in the medication.
- Any other psychiatric or medical problems you have, including a history of bipolar disorder
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment.
 Your provider can explain how these different treatments work with the medication.
Your provider can explain how these different treatments work with the medication. - If you are pregnant, plan to become pregnant, or are breastfeeding
- If you drink alcohol or use drugs
How Should I Take Fluoxetine?
Fluoxetine is usually taken one time per day with or without food.
Typically patients begin at a low dose of medicine and the dose is increased slowly over several weeks.
The dose usually ranges from 20 mg to 80 mg when taken once daily or 90 mg taken once weekly. Only your health care provider can determine the correct dose for you.
If you are taking fluoxetine for PMDD, it can be taken once daily (everyday) or intermittently (usually starting 14 days prior to menstruation through the first full day of menses of each cycle). Discuss this with your prescriber.
The liquid should be measured with a dosing spoon or oral syringe which you can get from your pharmacy.
The delayed release form should be swallowed whole. It should not be chewed, crushed, or broken.
It should not be chewed, crushed, or broken.
Consider using a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Fluoxetine?
If you miss a dose of fluoxetine that you take daily, take it as soon as you remember, unless it is closer to the time of your next dose. If you take fluoxetine once weekly, take it as soon as possible, then go back to your regular schedule the next week. Discuss this with your health care provider. Do not double your next dose or take more than what is prescribed.
What Should I Avoid While Taking Fluoxetine?
Avoid drinking alcohol or using illegal drugs while you are taking antidepressant medications. They may decrease the benefits (e.g., worsen your condition) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Fluoxetine?
If an overdose occurs, call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of fluoxetine does not exist.
What Are The Possible Side Effects Of Fluoxetine?
Common side effects
Headache, nausea, diarrhea, dry mouth, increased sweating, feeling nervous, restless, fatigue, or having trouble sleeping (insomnia). These will often improve over the first week or two as you continue to take the medication.
Sexual side effects, such as problems with orgasm or ejaculatory delay often do not diminish over time.
Rare/serious side effects
Low sodium blood levels (symptoms of low sodium levels may include headache, weakness, difficulty concentrating and remembering), teeth grinding, angle closure glaucoma (symptoms of angle closure glaucoma may include eye pain, changes in vision, swelling or redness in or around eye), serotonin syndrome (symptoms may include shivering, diarrhea, confusion, severe muscle tightness, fever, seizures, and death), seizure, QT prolongation and ventricular arrhythmia including Torsades de Pointes (changes in the electrical activity of your heart; symptoms may include fast, slow or irregular heartbeat, shortness of breath, and dizziness or fainting)
SSRI antidepressants including fluoxetine may increase the risk of bleeding events. Combined use of aspirin, nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen), warfarin, and other anti-coagulants may increase this risk. This may include symptoms such as gums that bleed more easily, nose bleed, or gastrointestinal bleeding. Some cases have been life threatening.
Combined use of aspirin, nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen), warfarin, and other anti-coagulants may increase this risk. This may include symptoms such as gums that bleed more easily, nose bleed, or gastrointestinal bleeding. Some cases have been life threatening.
Are There Any Risks For Taking Fluoxetine For Long Periods Of Time?
To date, there are no known problems associated with long term use of fluoxetine. It is a safe and effective medication when used as directed.
What Other Medications May Interact With Fluoxetine?
Fluoxetine should not be taken with or within 6 weeks of taking monoamine oxidase inhibitors (MAOIs). These include phenelzine (Nardil®), tranylcypromine (Parnate®), isocarboxazid (Marplan®), rasagiline (Azilect®), and selegiline (Emsam®).
Although rare, there is an increased risk of serotonin syndrome when fluoxetine is used with other medications that increase serotonin, such as other antidepressants, migraine medications called “triptans” (e. g., Imitrex®), some pain medications (e.g., tramadol (Ultram®), amphetamines, and the antibiotic linezolid (Zyvox®).
g., Imitrex®), some pain medications (e.g., tramadol (Ultram®), amphetamines, and the antibiotic linezolid (Zyvox®).
Fluoxetine may increase the levels and effects of:
- Certain anticonvulsants, such as phenytoin (Dilantin®), carbamazepine (Tegretol®, Equetro®)
- Certain antipsychotics, such as haloperidol (Haldol®), aripiprazole (Abilify®)
- Benzodiazepines, such as alprazolam (Xanax®), diazepam (Valium®)
- Atomoxetine (Straterra®)
- Warfarin (Coumadin®)
- Metoclopramide (Reglan®)
- Tricyclic antidepressants, such as imipramine (Tofranil®), desipramine (Norpramin®)
- Beta blockers, such as metoprolol (Toprol XL®, Lopressor®) and propranolol (Inderal®)
Fluoxetine may decrease the effects of tamoxifen (Nolvadex®) and codeine.
Fluoxetine may increase the effects of other medications that can cause bleeding (e.g., ibuprofen (Advil®, Motrin®), warfarin (Coumadin®), and aspirin).
How Long Does It Take For Fluoxetine To Work?
Sleep, energy, or appetite may show some improvement within the first 1-2 weeks. Improvement in these physical symptoms can be an important early signal that the medication is working. Depressed mood and lack of interest in activities may need up to 6-8 weeks to fully improve.
Summary Of FDA Black Box Warnings
Suicidal thoughts or actions in children and adults
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications. This risk may persist until significant remission occurs.
In short-term studies, antidepressants increased the risk of suicidality in children, adolescents, and young adults when compared to placebo. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24. Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24. Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Provided by
(December 2020)
©2020 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4. 0 International License. Last Updated: January 2016.
0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
What they treat us with: Prozac. From depression to bulimia
Medicine
16:00, December 14, 2017
Analysis of one of the popular antidepressants how it is customary to treat them and whether the antidepressant Prozac works, read in the new material of the heading “How we are treated”.
Prozac is on the list of the most important, safest and most effective (including from an economic point of view) drugs according to the World Health Organization. However, as we remember after the article with the analysis of Tamiflu, this does not guarantee its effectiveness.
Prozac is prescribed for the treatment of depression, obsessive-compulsive disorders, bulimia nervosa. If you know very well what it is, you can immediately skip to the “from what, from what” part.
When life is not nice
Depression is called depression, loss of interest in what used to make the patient happy. According to the international classification of diseases ICD-10, the main criteria by which such a diagnosis can be made include depressed mood for more than two weeks, loss of strength and consistently high fatigue (more than a month) and anhedonia (the inability to enjoy what used to bring joy). Doctors consider additional criteria for depression to be pessimism, low self-esteem, thoughts of death and suicide, appetite disturbances (weight loss or overeating), sleep problems, constant fears and anxieties, feelings of worthlessness and guilt, inability to concentrate, and a constant sweet taste in the mouth. These symptoms are unlikely to occur simultaneously (for example, fatigue and apathy may predominate in some cases, while anxiety and guilt may prevail in others), therefore, in order to diagnose depression, the patient's condition must meet at least two main criteria and three additional ones. At the same time, according to the definition of the US National Institute of Mental Health, such a state should last quite a long time (more than two weeks).
These symptoms are unlikely to occur simultaneously (for example, fatigue and apathy may predominate in some cases, while anxiety and guilt may prevail in others), therefore, in order to diagnose depression, the patient's condition must meet at least two main criteria and three additional ones. At the same time, according to the definition of the US National Institute of Mental Health, such a state should last quite a long time (more than two weeks).
Severe depression (clinical) includes a complex set of symptoms called major depressive disorder and may sometimes not be accompanied by low mood at all. However, because of her, the patient is physically unable to live and work normally, and the comments of those around him in the spirit of “he just can’t pull himself together” or “enough to turn sour that he spread snot” sound like a mockery. Such phrases stigmatize depression, blaming a person for his condition, while he himself will not be able to cope and needs treatment. To diagnose major depressive disorder, there is a whole questionnaire of major depression compiled by the World Health Organization. Also, depressive disorders include other conditions accompanied by depression, such as dysthymia (daily low mood and mild symptoms of depression for two years or more).
Also, depressive disorders include other conditions accompanied by depression, such as dysthymia (daily low mood and mild symptoms of depression for two years or more).
The causes of depression can be very different: somatic (due to diseases of the body), psychological (after strong dramatic experiences, such as the death of a relative) and iatrogenic (as a side effect of certain drugs). As strange as it would be to provide first aid to a victim of an electric shock without removing the wire from him, it is difficult to cure the symptoms of depression without eliminating its cause or changing the lifestyle that led the patient to such a state. If the patient lacks some essential substances (for example, tryptophan), it is important to make up for their lack, and not just fight the depressed mood with drugs. If he has some kind of psychological trauma, the help of a psychotherapist will be required. And for a person whose depression is provoked by hormonal disorders, neurological diseases, heart disease, diabetes, or even cancer (and this happens), it is more important to cure the disease itself, and symptomatic treatment of depression will be a secondary goal.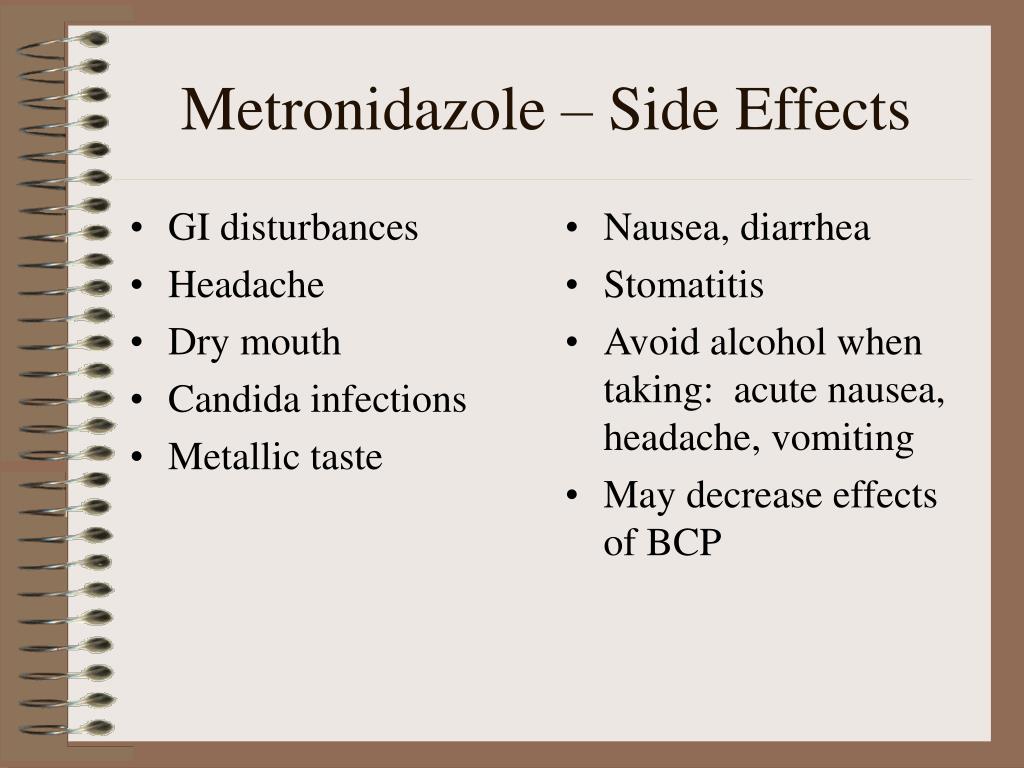
When you can't stop
Obsessive-compulsive disorder, or OCD (also called obsessive-compulsive disorder), consists of two mandatory components: obsessions (obsessive anxious or frightening thoughts) and compulsions (compulsive actions). A classic example is cleanliness-related OCD, where a person is afraid of contamination or contamination by microorganisms. Such thoughts and fears are called obsessions. In order to protect themselves from them, a person will worry too much about cleanliness, such as constantly washing their hands. Any contact with a non-sterile, according to the patient, object, plunges such a person into horror. And if you can’t wash your hands again, he will experience real suffering.
You can learn how to deal with medications on your own in the author's online course "How we are treated" by the editor of Indicator.Ru Ekaterina Mishchenko: https://clck.ru/Pnmtk
Such "protective" behavior is called compulsion. The desire for cleanliness can be understood if a person is in conditions of complete unsanitary conditions or, on the contrary, wants to maintain sterile conditions somewhere in the operating room. But if the action loses its true meaning and becomes a mandatory ritual, it becomes a compulsion.
But if the action loses its true meaning and becomes a mandatory ritual, it becomes a compulsion.
However, OCD can manifest itself not only as a fear of pollution, but also as excessive superstition, fear of losing a necessary object, sexual or religious obsessive thoughts and related actions. Their reasons may lie in several areas: biological and psychological. The first includes diseases and features of the nervous system, lack of neurotransmitters (biologically active substances that ensure the transmission of a nerve impulse from one neuron to another, for example, dopamine or serotonin), genetic predisposition (mutations in the hSERT gene encoding the serotonin carrier protein and located on 17 -th chromosome).
There is also an infectious theory of the development of OCD, associated with the fact that in children it sometimes occurs after infection with streptococcus. This theory is called PANDAS - an abbreviation for the English Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections, which translates as "Children's autoimmune neuropsychiatric disorders associated with streptococcal infections. " The cause of this syndrome may be an attack of its own antibodies produced against streptococcus on the patient's nerve cells. However, this theory has not yet been confirmed.
" The cause of this syndrome may be an attack of its own antibodies produced against streptococcus on the patient's nerve cells. However, this theory has not yet been confirmed.
Another group of explanations for the development of OCD is psychological. They go back to the theories of the beginning of the last century (from Freud to Pavlov). Mayakovsky's father died of blood poisoning after being injected with a binder, so it is believed that the poet also showed a pathological love for cleanliness. But you don't have to be a futurist poet to experience the full benefits of OCD: even dogs and cats suffer from it. Only in them this is expressed in the endless licking of wool and attempts to catch their tail.
The Yale-Brown scale is used to diagnose obsessive-compulsive disorder. In the fight against OCD, the method of psychological persuasion can be useful: patients are patiently explained that if they skip the “ritual” once, nothing terrible will happen. But drugs are also used in treatment.
When you are how you eat
Bulimia nervosa (third indication for Prozac) is a binge eating disorder. The main signs of bulimia are uncontrolled eating in large quantities, obsession with excess weight (calorie counting, attempts to induce vomiting after eating, fasting, use of laxatives), low self-esteem, low blood pressure. Other symptoms are sudden changes in body weight, kidney problems and dehydration, enlarged salivary glands, heartburn after eating, and inflammation of the esophagus. Due to provoking vomiting, hydrochloric acid from the stomach constantly enters the oral cavity of patients, which can lead to grinding of tooth enamel and ulcers on the mucous membrane. According to the DSM-5 classification of diseases, uncontrolled consumption of large amounts of food and the simultaneous use of various drastic measures for weight loss is the main criterion for diagnosing bulimia nervosa.
Video about bulimia on the educational medical resource Open Osmosis (USA)
The causes of bulimia can be either biological (incorrect levels of hormones or neurotransmitters, including serotonin) or social. The importance of the latter is highlighted, for example, in a high-profile study among teenage girls in Fiji, which showed a sharp increase in cases of intentional bowel cleansing for weight loss in just three years (from 1995 to 1998) after television appeared in the province. Perhaps the desire to be like models from the screens and covers really pushes for such behavior.
Bulimia can often be associated with other psychiatric disorders (depression, anxiety disorders, sleep disorders). According to a study by the New York State Psychiatric Institute and Columbia University, 70% of people with bulimia have ever experienced depression, compared with just over 25% in the general population.
Bulimia itself is not very common, and it can be more difficult to diagnose than the same anorexia, because changes in body weight in bulimia are less sharp and noticeable.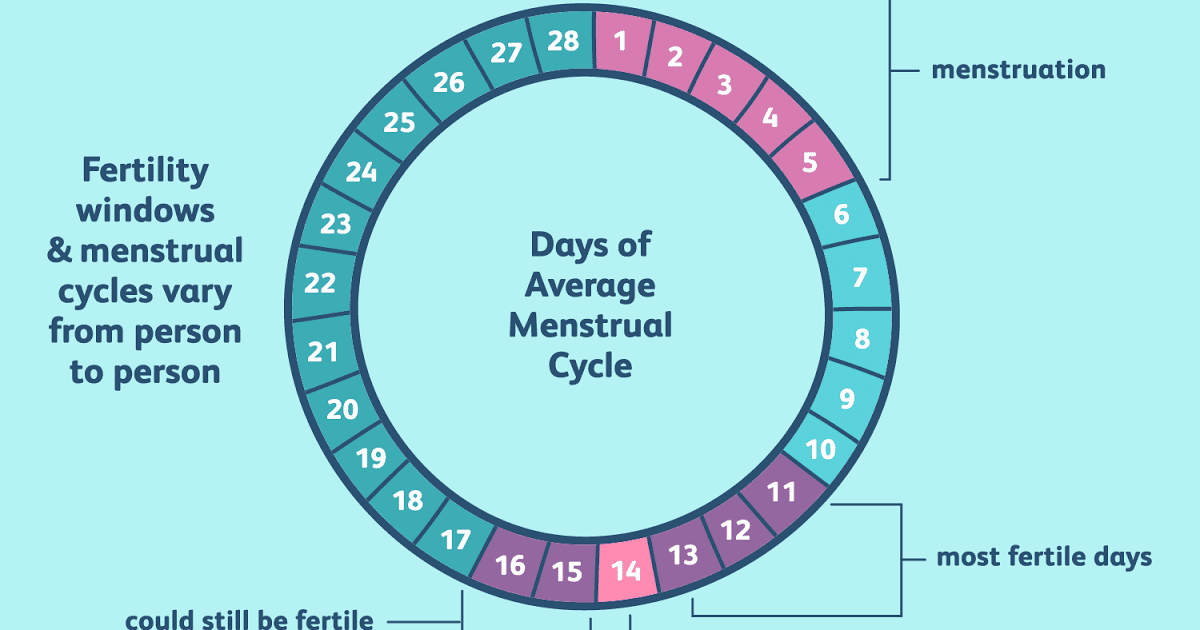 For diagnosis, the food attitude test, developed by the Clark Institute of Psychiatry at the University of Toronto, and other tests based on it, are used. But (as with the tests for OCD and depression above), its result only indicates the likelihood that the patient has developed a disorder, but does not allow for a definitive diagnosis, especially for oneself.
For diagnosis, the food attitude test, developed by the Clark Institute of Psychiatry at the University of Toronto, and other tests based on it, are used. But (as with the tests for OCD and depression above), its result only indicates the likelihood that the patient has developed a disorder, but does not allow for a definitive diagnosis, especially for oneself.
From what, from what
What is a medicine that is prescribed for three types of disorders at once? The active ingredient in Prozac is fluoxetine. The patent for Prozac expired back in 2001, so many generics are available in pharmacies - cheaper copies that use the same active ingredient, but are not as well studied and may differ slightly from the original. These drugs include Fluoxetine, Prodel, Profluzak, Fluval.
Fluoxetine, discovered and marketed by Eli Lilly and Company, belongs to a group of antidepressants called selective serotonin reuptake inhibitors. This group is considered third-generation antidepressants, fairly well tolerated and without significant side effects.
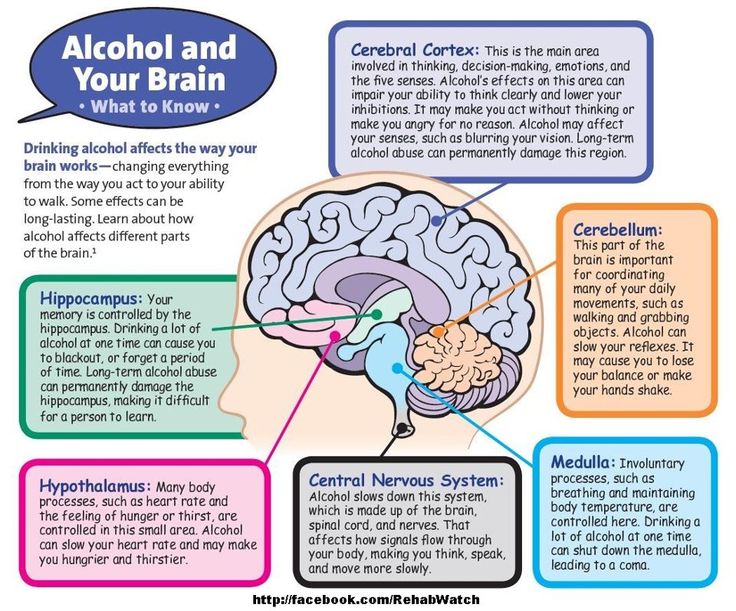
Fluoxetine is readily absorbed into the blood, can bind to plasma proteins and accumulate in body tissues. It also penetrates the blood-brain barrier, which protects the nervous system and brain from many substances circulating in the blood. There, in the nervous system, it works in the synaptic cleft we have already mentioned, preventing the excess serotonin ejected from the synapse from returning to the neurotransmitter. Because of this, serotonin is longer present in the synaptic cleft and can bind to receptors. How exactly fluoxetine achieves this effect is not clear even to manufacturers, but it is known that it has little effect on the work of other neurotransmitters. However, at high doses, fluoxetine increases adrenaline and dopamine levels, as studies in rat brain tissue show.
Fluoxetine and its metabolite, norfluoxetine, can interfere with each other's actions. Because of this, according to scientists from the Institute of Research Medicine in Barcelona, a constant concentration of fluoxetine in the blood is achieved only after four weeks of taking the drug.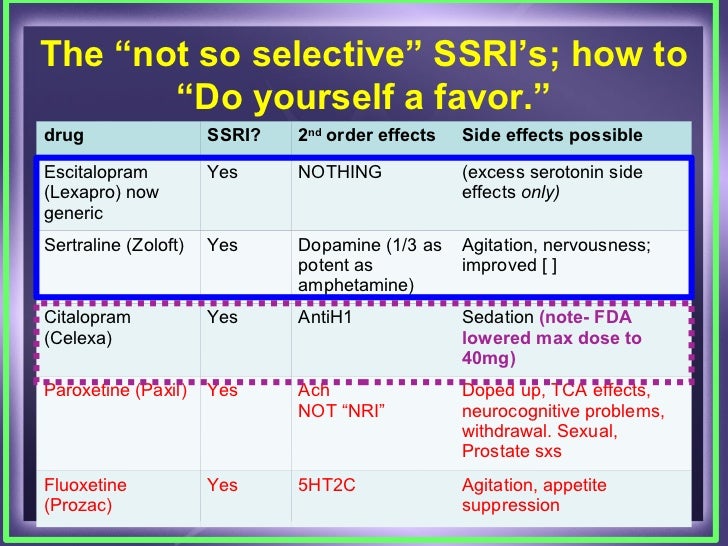 Similarly, the effects of taking the medicine do not disappear immediately. Associated with this is the difficulty in selecting the required dose for a particular patient.
Similarly, the effects of taking the medicine do not disappear immediately. Associated with this is the difficulty in selecting the required dose for a particular patient.
Serotonin itself, which is absolutely incorrectly called the “happiness hormone” (hormones are produced in one organ of the body, but perform their function in another, serotonin in this context simply conducts nerve impulses in the brain regions responsible for good mood, and is produced there well), in fact, it performs much more functions. Yes, it affects mood, sleep, and appetite, so some cases of depression, bulimia nervosa, and OCD may be caused by insufficient production of this neurotransmitter and corrected with serotonin reuptake inhibitors. But in addition, platelets can actively capture it and affect blood clotting. Serotonin is also involved in the processes of memorization and learning. At the same time, not only vertebrate animals can produce it: according to a study by Chinese and American scientists, the pain from an insect bite is largely due to the presence of serotonin in the poison, and the dysentery amoeba, according to an article in Science, can cause diarrhea by releasing serotonin in our intestines.
The lists (not) included
But all these are just mechanisms, and besides, they have not been studied to the smallest detail. To understand how this works in real people and how often it helps, let's turn to clinical trials. However, anyone who enters the combination “fluoxetine depression double blind randomized controlled” into the PubMed scientific article database and filters clinical trial (clinical trial) will see more than 558 articles, up to work comparing the effectiveness of Prozac and homeopathy.
Double-blind, randomized, placebo-controlled method is a method of clinical drug research in which the subjects are not privy to important details of the study being conducted. “Double-blind” means that neither the subjects nor the experimenters know who is being treated with what, “randomized” means that the distribution into groups is random, and placebo is used to show that the effect of the drug is not based on autosuggestion and that this medicine helps better than a tablet without active substance. This method prevents subjective distortion of the results. Sometimes the control group is given another drug with already proven efficacy, rather than a placebo, to show that the drug not only treats better than nothing, but also outperforms analogues.
This method prevents subjective distortion of the results. Sometimes the control group is given another drug with already proven efficacy, rather than a placebo, to show that the drug not only treats better than nothing, but also outperforms analogues.
Indicator.Ru
Help
No living person can analyze them within an adequate period of time. And even Cochrane reviews can be found as many as 36 (that's really a lot), although not all of them consider the action of fluoxetine for its direct indications (depression, bulimia and obsessive-compulsive disorder).
The Cochrane Library is a database of the Cochrane Collaboration, an international non-profit organization involved in the development of World Health Organization guidelines. The name of the organization comes from the name of its founder, the 20th-century Scottish medical scientist Archibald Cochrane, who championed the need for evidence-based medicine and the conduct of competent clinical trials and wrote the book Efficiency and Efficiency: Random Reflections on Public Health.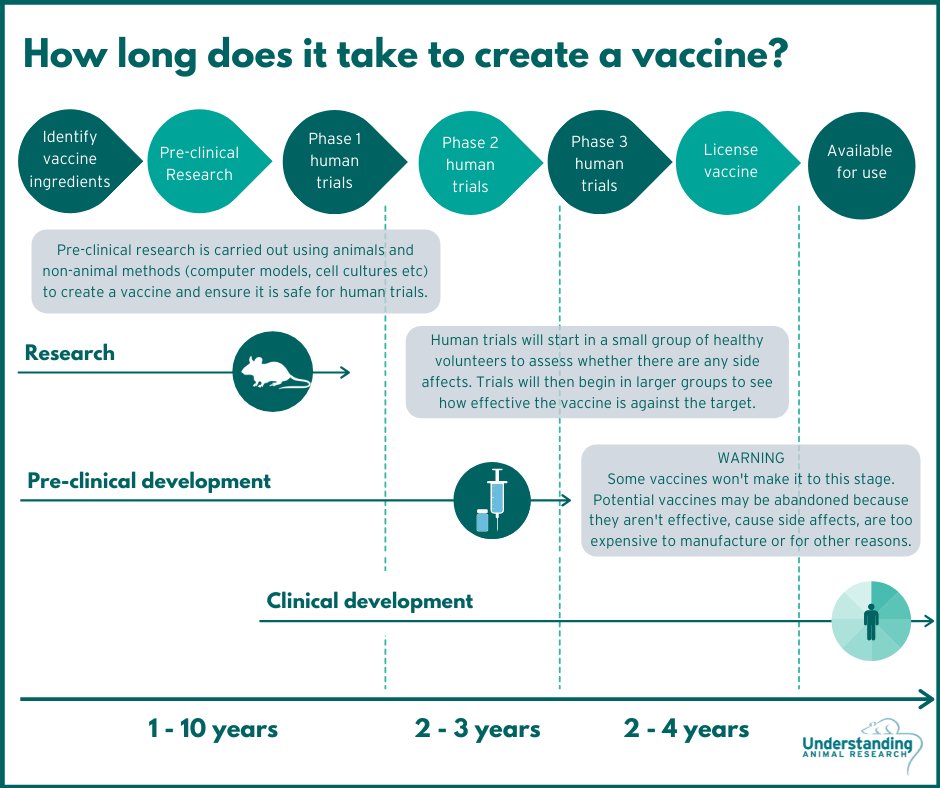 Medical scientists and pharmacists consider the Cochrane Database one of the most authoritative sources of such information: the publications included in it have been selected according to the standards of evidence-based medicine and report the results of randomized, double-blind, placebo-controlled clinical trials.
Medical scientists and pharmacists consider the Cochrane Database one of the most authoritative sources of such information: the publications included in it have been selected according to the standards of evidence-based medicine and report the results of randomized, double-blind, placebo-controlled clinical trials.
Indicator.Ru
Help
One of them is dedicated to antidepressants used against bulimia nervosa. Although in general the authors note that there is little data on this topic, fluoxetine (for which there were only five randomized double-blind controlled trials in 2003) is recognized as a leader in this direction. However, the authors refuse to recommend this medicine in the conclusion, arguing that not all clinical trial data have been published and are available for consideration.
The authors of a 2008 review reviewed the benefits of serotonin reuptake inhibitors (including fluoxetine) in obsessive-compulsive disorder and concluded that they help better than placebo, and the associated side effects are much more significant, among which nausea is most common , insomnia and headache.:max_bytes(150000):strip_icc()/prozac-withdrawal-symptoms-timeline-and-treatment-4766892_final_edit-ddf616fc766d4651afa6b5d804721eea.png) According to a 2013 review, the usefulness of this same group of drugs in autism and related OCD is unclear, and the data are insufficient to conclude.
According to a 2013 review, the usefulness of this same group of drugs in autism and related OCD is unclear, and the data are insufficient to conclude.
The most popular subject of fluoxetine reviews was the fight against depression. But the authors of most of them note the lack of data (for example, in this 2013 review). In a broad inclusion criteria review of 1177 randomized controlled trials of fluoxetine for depression in adults, the authors conclude that it is about as effective as other antidepressants but less toxic. However, they warn against hasty decisions, since most of the studies were conducted on small groups of people (100 or less) and were funded by the manufacturer, which is more profitable to publish only positive results, hiding information about failures. Data on postpartum depression are also found to be insufficient and inconsistent. The same issues are highlighted by a review of articles on the effectiveness of antidepressants against dementia-related senile depression.
Indicator.Ru concludes: one of the best stimulant antidepressants is still not perfect
A large number of studies confirm the effectiveness of fluoxetine, a key component of Prozac. But part of the reviews of the Cochrane Collaboration note that not all trial data have been published by manufacturers. And this accusation is not an empty phrase: according to Eli Lilly's internal documents, manufacturers during trials often attributed suicide cases to worsening depression or overdosing on the drug.
As a result, following numerous reports of suicide by patients prescribed this drug, the US Food and Drug Administration (FDA) has issued a warning label to the drug's packaging.
This does not mean that the harm from the medicine always outweighs its benefit, but such dishonest behavior of manufacturers does not allow us to assess the risks more accurately. Given the difficulty with the selection of an individual dose and the slow effect, adjusting the dosage is really not easy.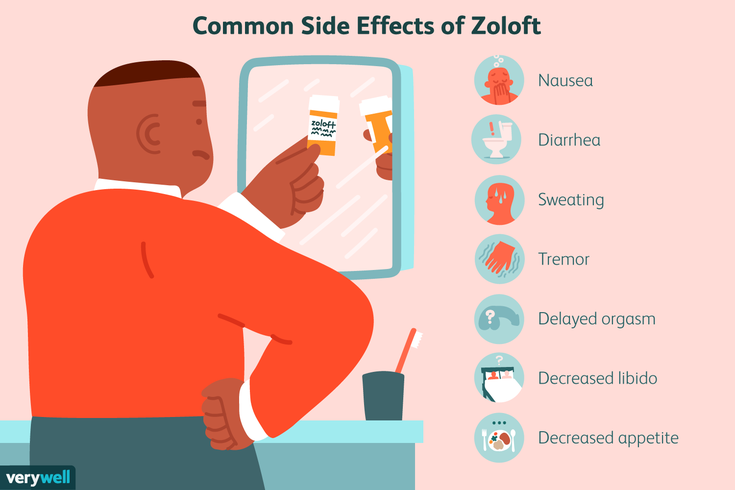
Prozac is also classified as a serotonin reuptake inhibitor, but if the cause of your condition is something else, you need to pay more attention to finding and eliminating them than fighting depression. As we wrote above, somatic diseases (for example, cirrhosis of the liver, cancer or diabetes), and even a lack of vitamins, can also cause depression. In addition, depression or another disorder may be the result of psychological trauma that will be difficult to deal with without psychotherapy.
All this suggests that the drug should be used under the supervision of a doctor (most likely, it will not be sold without a prescription), and that its action alone may not be enough for a complete recovery. And don't forget that serotonin is involved in many other processes in the body. Therefore, you should not use the drug in violation of the functions of the liver and kidneys, an increased risk of thrombosis, and not only during pregnancy and lactation. With manic states and suicidal moods, it is also better to abandon the drug. If you notice allergic reactions or nausea and headache, you need to see a doctor and ask if you should stop taking the medicine.
If you notice allergic reactions or nausea and headache, you need to see a doctor and ask if you should stop taking the medicine.
Our advice cannot be compared to a doctor's prescription. Before you start taking this or that drug, be sure to consult a specialist.
Subscribe to Indicator.Ru on social networks: Facebook, VKontakte, Twitter, Telegram, Odnoklassniki.
Author: Ekaterina Mishchenko
‹‹Depression in General Medicine: A Guide for Physicians››
One of the main arguments in favor of the use of first-line antidepressants in the treatment of affective disorders in general medical practice is the minimal (compared to second-line drugs) severity of side effects.
Differences in the complications of thymoanaleptic therapy are clearly seen when comparing the main manifestations of the undesirable effect of representatives of first-line antidepressants (SSRIs, SSOZS) and TCAs, which is clearly demonstrated by the data given in Table.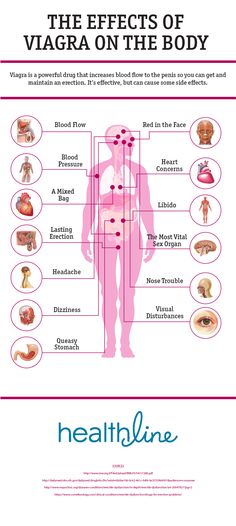 fourteen.
fourteen.
Nevertheless, it is impossible to completely exclude complications even when using sparing psychotropic drugs. The greatest likelihood of developing side effects of psychopharmacotherapy occurs in patients with somatic diseases, as well as in elderly people who show hypersensitivity to psychotropic drugs; in these contingents, even with careful dose titration, in addition to the main thymoanaleptic effect, side effects may also occur.
The main side effects of antidepressants include anticholinergic disorders of the central and autonomic nervous system, cardiovascular system, complications from the hematopoietic organs, metabolic and endocrine disorders (weight changes, sexual dysfunction, allergic reactions).
Side effects often appear in the initial stages of treatment (in the first 2 weeks) and sometimes persist for 3-4 weeks of therapy, and then reverse development. For more persistent and at the same time severe disorders, dose reduction is indicated, and, if necessary, therapy is discontinued.
Treatment with tianeptine (SSOZS) is accompanied by a minimum of undesirable effects. Side effects of the drug are most often limited to complaints of dry mouth, nausea, and drowsiness during the day. Only in some cases, phenomena of transient orthostatic hypotension, dizziness, headaches, skin allergic reactions are also observed. The most common side effects of SSRIs are:
- nausea,
- dry mouth
- loss of appetite,
- vomit,
- diarrhea,
- constipation.
Along with this, undesirable effects from the autonomic and central nervous system are possible:
- dizziness,
headaches (citalopram)
- insomnia,
- increase (or appearance) of anxiety,
- nervousness
- a sense of inner tension.
The latter appear in the first weeks of treatment or with increasing doses.
There are transient extrapyramidal disorders in the form of tremor. As for other disorders (parkinsonism, akathisia, dyskinesias), judging by the data of a number of publications, they are recorded only in individual cases. The use of fluoxetine and paroxetine may be accompanied by increased bleeding and even bleeding.
The use of fluoxetine and paroxetine may be accompanied by increased bleeding and even bleeding.
During SSRI therapy, neurotoxic reactions (serotonin syndrome) affecting the gastrointestinal tract and nervous system are possible (colic in the abdomen , flatulence, loose stools, nausea, vomiting; tremor, dysarthria, muscle hypertonicity, hyperreflexia, myoclonic twitching, ataxia). In more severe cases, hyperthermia, confusion, symptoms of disorientation join [Malin D.I., 2000].
Severe complications often occur in the process of drug interaction with combined use:
- SSRIs and MAOIs,
- SSRIs and OIMAO-A (moclobemide),
- TCA (anafranil) and OIMAO-A.
Along with side effects, the effects of antidepressants associated with overdose are of great importance (especially in the context of a general medical network). The risk of deliberately taking large amounts of drugs for suicidal purposes poses a safety advantage to first-line antidepressants.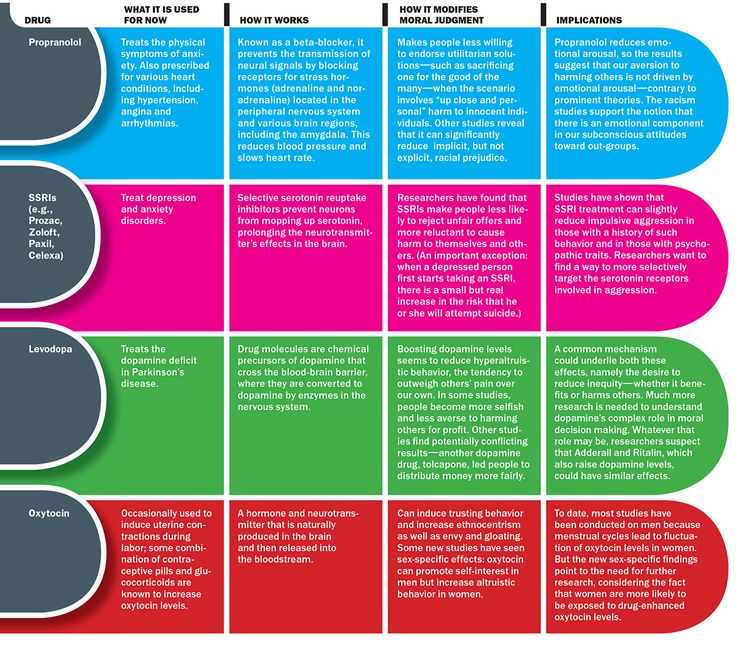 This is evidenced by comparative data on the safety of some first-line and second-line antidepressants, presented in Table. fifteen.
This is evidenced by comparative data on the safety of some first-line and second-line antidepressants, presented in Table. fifteen.
The safety of first-line drugs is indicated by the data of C. Las-mier et al. (1991) in relation to tianeptine. Taking large doses of this drug (from 12 to 60 tablets) (12 cases of suicidal use of tianeptine are summarized) does not lead to death and is not accompanied by significant (compared with the norm) deviations of the clinical and electrocardiological parameters of the cardiovascular system.
Table 15. Safety of antidepressants [based on R. Priest, D. Baldwin, 1994]
| Preparations | Hazard measure (number of deaths from overdose per 1 million prescriptions) | Degree of danger |
| First line antidepressants | ||
| Fluoxetine (Prozac) Fluvoxamine (Fevarin) Mianserin (Lerivon) | Less than 10 | Relatively dangerous |
| Second line antidepressants | ||
| Clomipramine (Anafranil) Maprotiline (Ludiomil) Trazadone (Tritgiko) | More than 10 | Potentially dangerous |
| Imipramine (Melipramine) Phenelzine (Nardil) | Over 20 | Dangerous |
| Amitriptyline Trianylcypramine (transamine) | Over 40 | Very dangerous |
With an overdose of milnacipran (ixel), vomiting, hyperventilation, and tachycardia are observed.