Borderline personality disorder dealing with
Helping Someone with Borderline Personality Disorder
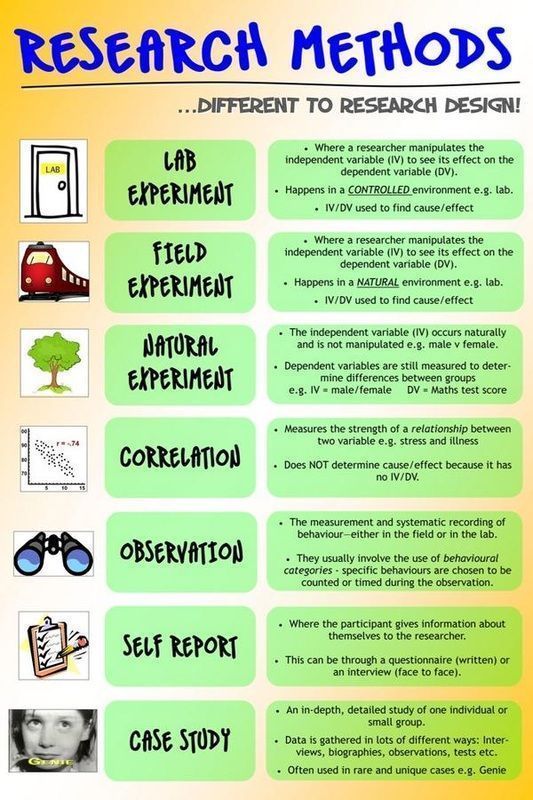
personality disorders
Have a loved one who's been diagnosed with BPD? While you can’t force them to seek treatment, you can take steps to improve communication, set healthy boundaries, and stabilize your relationship.
BPD and relationships
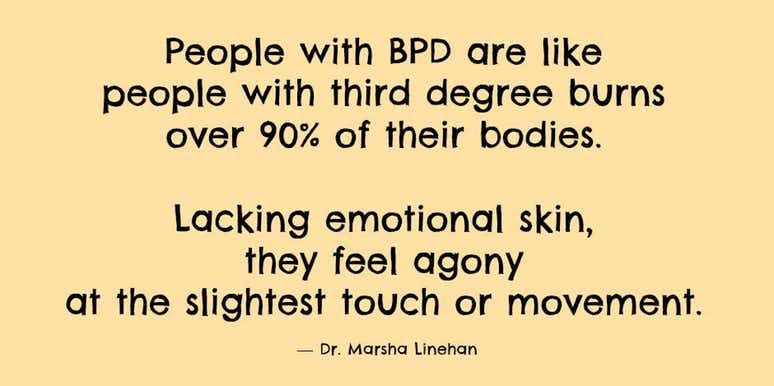
People with borderline personality disorder (BPD) tend to have major difficulties with relationships, especially with those closest to them. Their wild mood swings, angry outbursts, chronic abandonment fears, and impulsive and irrational behaviors can leave loved ones feeling helpless, abused, and off balance. Partners and family members of people with BPD often describe the relationship as an emotional roller coaster with no end in sight. You may feel like you're at the mercy of your loved one's BPD symptoms—trapped unless you leave the relationship or the person takes steps to get treatment. But you have more power than you think.
You can change the relationship by managing your own reactions, establishing firm limits, and improving communication between you and your loved one. There's no magic cure but with the right treatment and support, many people with BPD can and do get better and their relationships can become more stable and rewarding. In fact, patients with the most support and stability at home tend to show improvements sooner than those whose relationships are more chaotic and insecure.
Whether it's your partner, parent, child, sibling, friend, or other loved one with BPD, you can improve both the relationship and your own quality of life, even if the person with BPD isn't ready to acknowledge the problem or seek treatment.
Learning all you can
If your loved one has borderline personality disorder, it's important to recognize that he or she is suffering. The destructive and hurtful behaviors are a reaction to deep emotional pain. In other words, they're not about you. When your loved one does or says something hurtful towards you, understand that the behavior is motivated by the desire to stop the pain they are experiencing; it's rarely deliberate.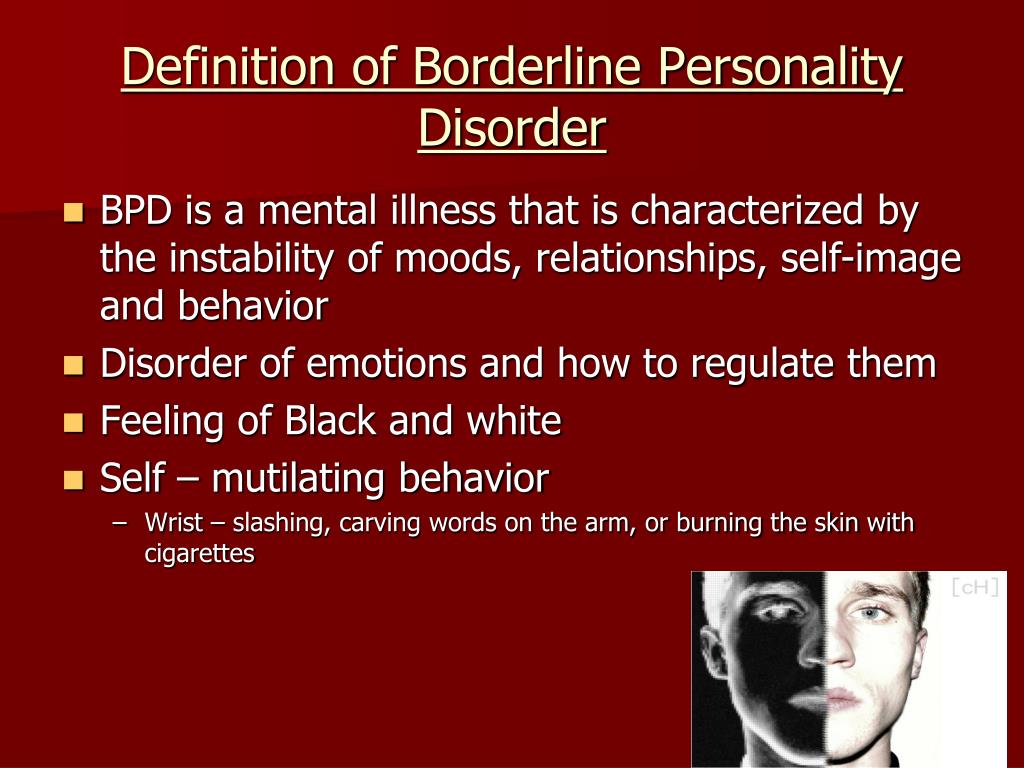
Learning about BPD won't automatically solve your relationship problems, but it will help you understand what you're dealing with and handle difficulties in more constructive ways.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. Sign up today and get matched.
GET 20% OFF
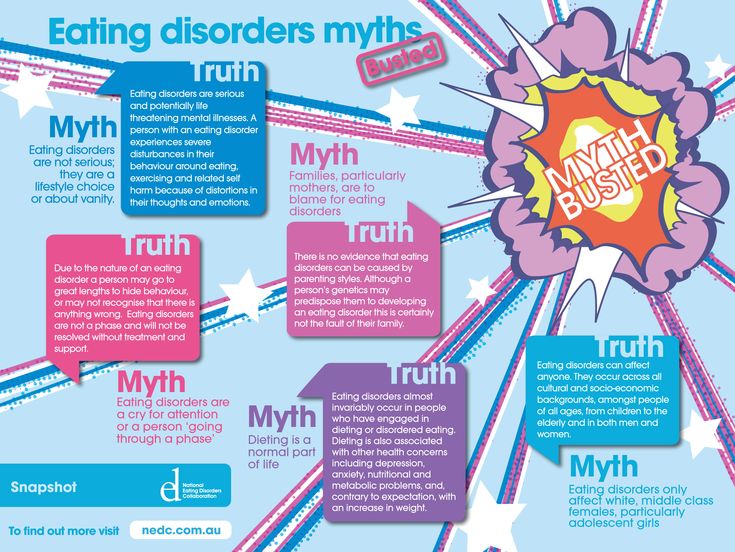
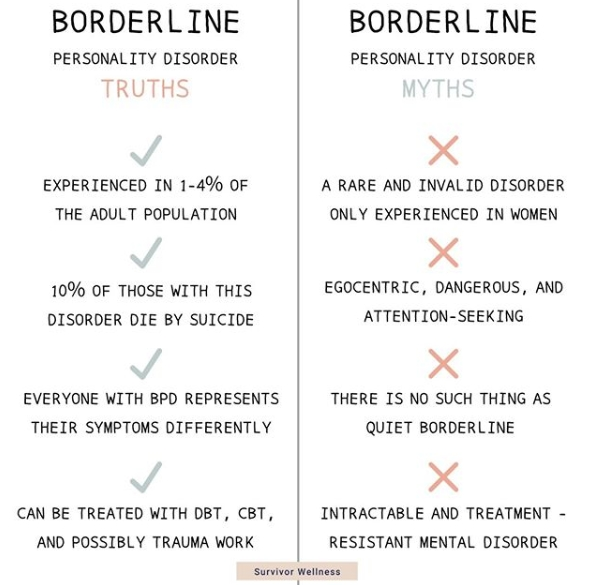
Recognizing the signs and symptoms of borderline personality disorder is not always easy. BPD is rarely diagnosed on its own, but often in conjunction with co-occurring disorders such as depression, bipolar disorder, anxiety, an eating disorder, or substance abuse. Your family member or loved one with BPD may be extremely sensitive, so small things can often trigger intense reactions.
Once upset, borderline people are often unable to think straight or calm themselves in a healthy way. They may say hurtful things or act out in dangerous or inappropriate ways. This emotional volatility can cause turmoil in their relationships and stress for family members, partners, and friends.
Many people in a close relationship with someone who suffers from BPD often know that there’s something wrong with their loved one, but have no idea what it is or if there is even a name for it. Learning a diagnosis of borderline personality disorder can come as a source of both relief and hope.
Does your loved one have borderline personality disorder?
In your relationship:
- Do you feel like you have to tiptoe around your loved one, watching every little thing you say or do for fear of setting them off? Do you often hide what you think or feel in order to avoid fights and hurt feelings?
- Does your loved one shift almost instantaneously between emotional extremes? For example, are they calm one moment, raging the next, then suddenly despondent? Are these rapid mood swings unpredictable and seemingly irrational?
- Does your loved one tend to view you as all good or bad, with no middle ground? For example, either you're “perfect,” and the only one they can count on, or you're “selfish” and “unfeeling” and never truly loved them.
- Do you feel like you can't win: that anything you say or do will be twisted and used against you? Does it feel as if your loved one's expectations are constantly changing, so you're never sure how to keep the peace?
- Is everything always your fault? Do you feel constantly criticized and blamed for things that don't even make sense? Does the person accuse you of doing and saying things you never did? Do you feel misunderstood whenever you try to explain or reassure your partner?
- Do you feel manipulated by fear, guilt, or outrageous behavior? Does your loved one make threats, fly into violent rages, make dramatic declarations, or do dangerous things when they think you're unhappy or may leave?
If you answer “yes” to most of these questions, your partner or family member might have borderline personality disorder.
[Read: Borderline Personality Disorder Test]
To help someone with BPD, first take care of yourself
When a family member or partner has borderline personality disorder, it's all too easy to get caught up in heroic efforts to please and appease him or her. You may find yourself putting most of your energy into the person with BPD at the expense of your own emotional needs. But this is a recipe for resentment, depression, burnout, and even physical illness.
You may find yourself putting most of your energy into the person with BPD at the expense of your own emotional needs. But this is a recipe for resentment, depression, burnout, and even physical illness.
You can't help someone else or enjoy sustainable, satisfying relationships when you're run down and overwhelmed by stress. As in the event of an in-flight emergency, you must “put on your own oxygen mask first.”
Avoid the temptation to isolate. Make it a priority to stay in touch with family and friends who make you feel good. You need the support of people who will listen to you, make you feel cared for, and offer reality checks when needed.
You're allowed (and encouraged) to have a life! Give yourself permission to have a life outside of your relationship with the person with BPD. It's not selfish to carve out time for yourself to relax and have fun. In fact, when you return to your BPD relationship, you'll both benefit from your improved perspective.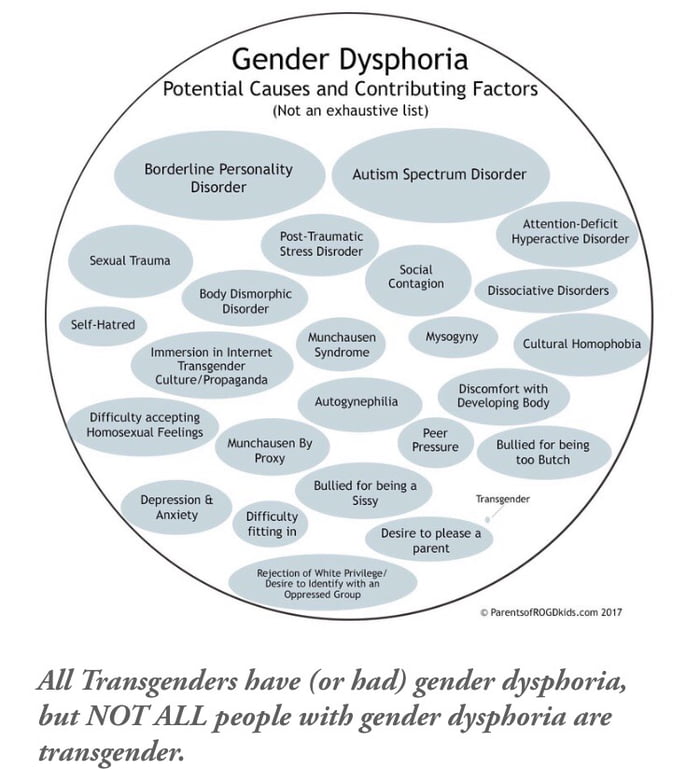
Join a support group for BPD family members. Meeting with others who understand what you're going through can go a long way. If you can't find an in-person support group in your area, you may want to consider joining an online BPD community.
Don't neglect your physical health. Eating healthfully, exercising, and getting quality sleep can easily fall by the wayside when you're caught up in relationship drama. Try to avoid this pitfall. When you're healthy and well rested, you're better able to handle stress and control your own emotions and behaviors.
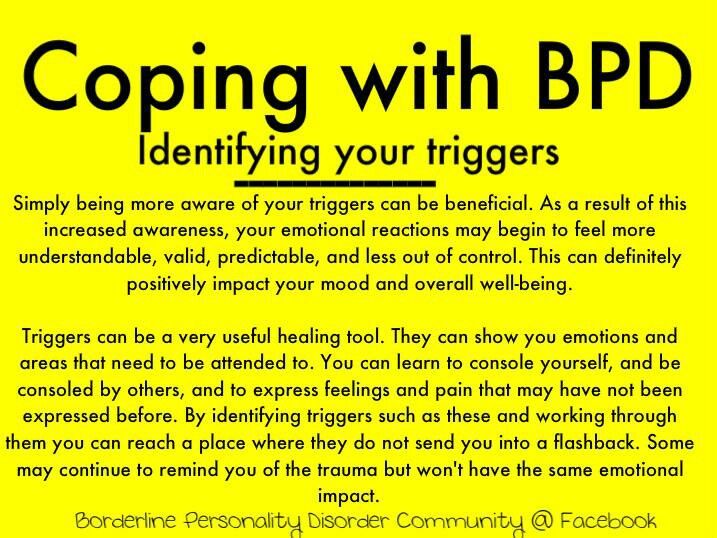
Learn to manage stress. Getting anxious or upset in response to problem behavior will only increase your loved one's anger or agitation. By practicing with sensory input, you can learn to relieve stress as it's happening and stay calm and relaxed when the pressure builds.
Remember the 3 C's rule
Many friends or family members often feel guilty and blame themselves for the destructive behavior of the borderline person.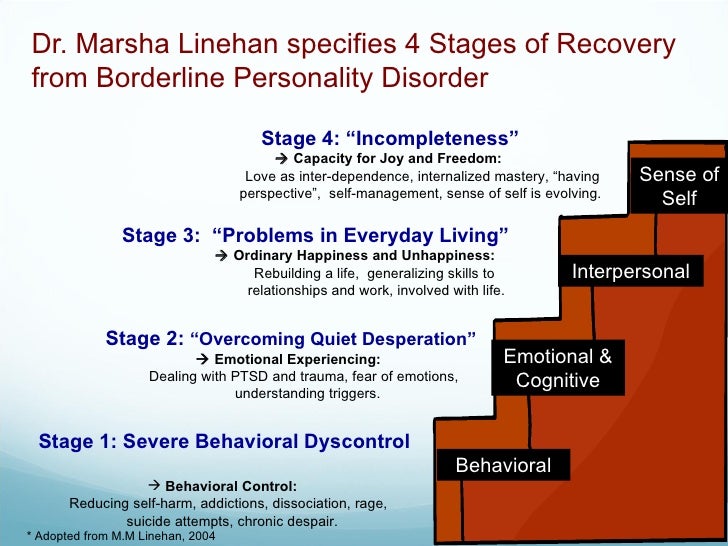 You may question what you did to make the person so angry, think you somehow deserve the abuse, or feel responsible for any failure or relapse in treatment.
You may question what you did to make the person so angry, think you somehow deserve the abuse, or feel responsible for any failure or relapse in treatment.
But it's important to remember that you're not responsible for another person. The person with BPD is responsible for their own actions and behaviors.
The 3 C's are:
- I didn't cause it.
- I can't cure it.
- I can't control it.
Source: Out of the Fog
Communicating with someone who has BPD
Communication is a key part of any relationship but communicating with a borderline person can be especially challenging. People in a close relationship with a borderline adult often liken talking with their loved one to arguing with a small child. People with BPD have trouble reading body language or understanding the nonverbal content of a conversation. They may say things that are cruel, unfair, or irrational. Their fear of abandonment can cause them to overreact to any perceived slight, no matter how small, and their aggression can result in impulsive fits of rage, verbal abuse, or even violence.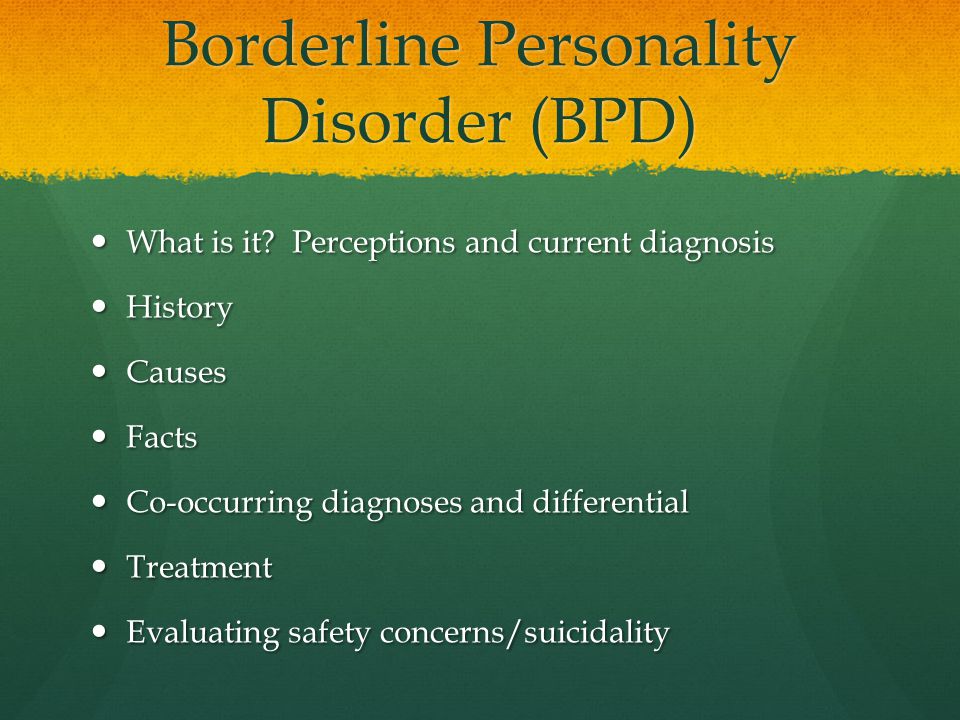
The problem for people with BPD is that the disorder distorts both the messages they hear and those they try to express. BPD expert and author, Randi Kreger, likens it to “having ‘aural dyslexia,' in which they hear words and sentences backwards, inside out, sideways, and devoid of context.”
Listening to your loved one and acknowledging their feelings is one of the best ways to help someone with BPD calm down. When you appreciate how a borderline person hears you and adjust how you communicate with them, you can help diffuse the attacks and rages and build a stronger, closer relationship.
Communication tips
It's important to recognize when it's safe to start a conversation. If your loved one is raging, verbally abusive, or making physical threats, now is not the time to talk. Better to calmly postpone the conversation by saying something like, “Let's talk later when we're both calm. I want to give you my full attention but that's too hard for me to do right now.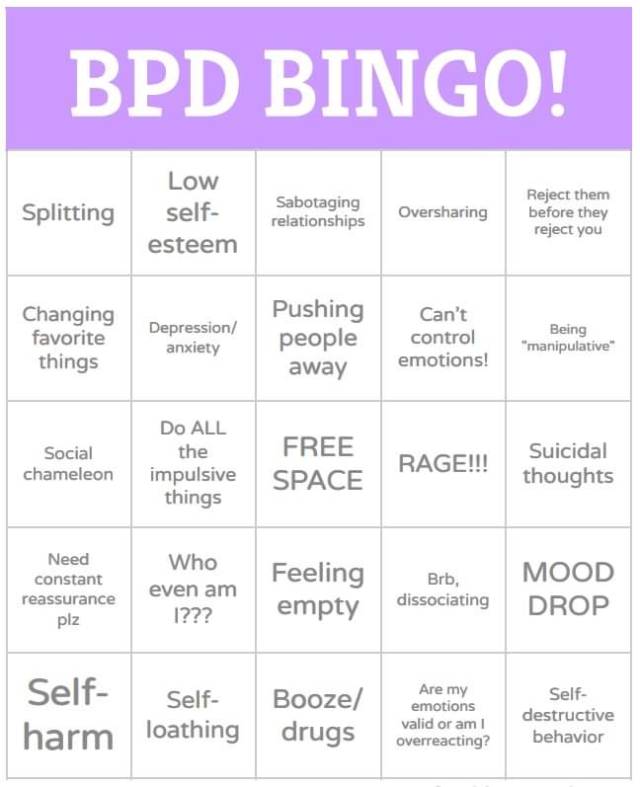 ”
”
When things are calmer:
Listen actively and be sympathetic. Avoid distractions such as the TV, computer, or cell phone. Try not to interrupt or redirect the conversation to your concerns. Set aside your judgment, withhold blame and criticism, and show your interest in what's being said by nodding occasionally or making small verbal comments like “yes” or “uh huh.” You don't have to agree with what the person is saying to make it clear that you're listening and sympathetic.
Focus on the emotions, not the words. The feelings of the person with BPD communicate much more than what the words he or she is using. People with BPD need validation and acknowledgement of the pain they're struggling with. Listen to the emotion your loved one is trying to communicate without getting bogged down in attempting to reconcile the words being used.
Try to make the person with BPD feel heard. Don't point out how you feel that they're wrong, try to win the argument, or invalidate their feelings, even when what they're saying is totally irrational.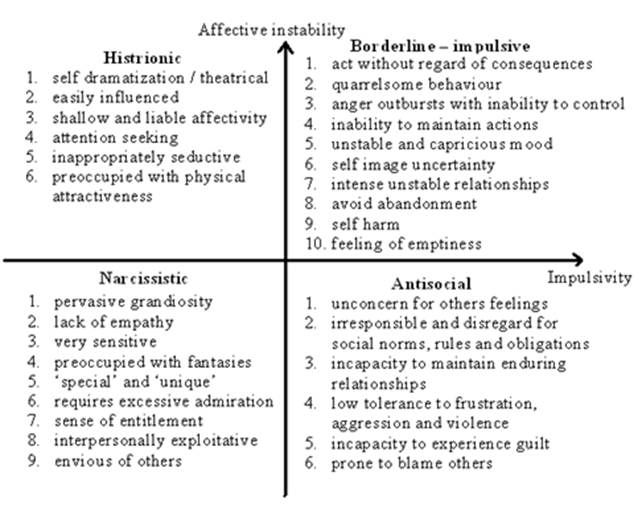
Do your best to stay calm, even when the person with BPD is acting out. Avoid getting defensive in the face of accusations and criticisms, no matter how unfair you feel they are. Defending yourself will only make your loved one angrier. Walk away if you need to give yourself time and space to cool down.
Seek to distract your loved one when emotions rise. Anything that draws your loved one's attention can work, but distraction is most effective when the activity is also soothing. Try exercising, sipping hot tea, listening to music, grooming a pet, painting, gardening, or completing household chores.
Talk about things other than the disorder. You and your loved one's lives aren't solely defined by the disorder, so make the time to explore and discuss other interests. Discussions about light subjects can help to diffuse the conflict between you and may encourage your loved one to discover new interests or resume old hobbies.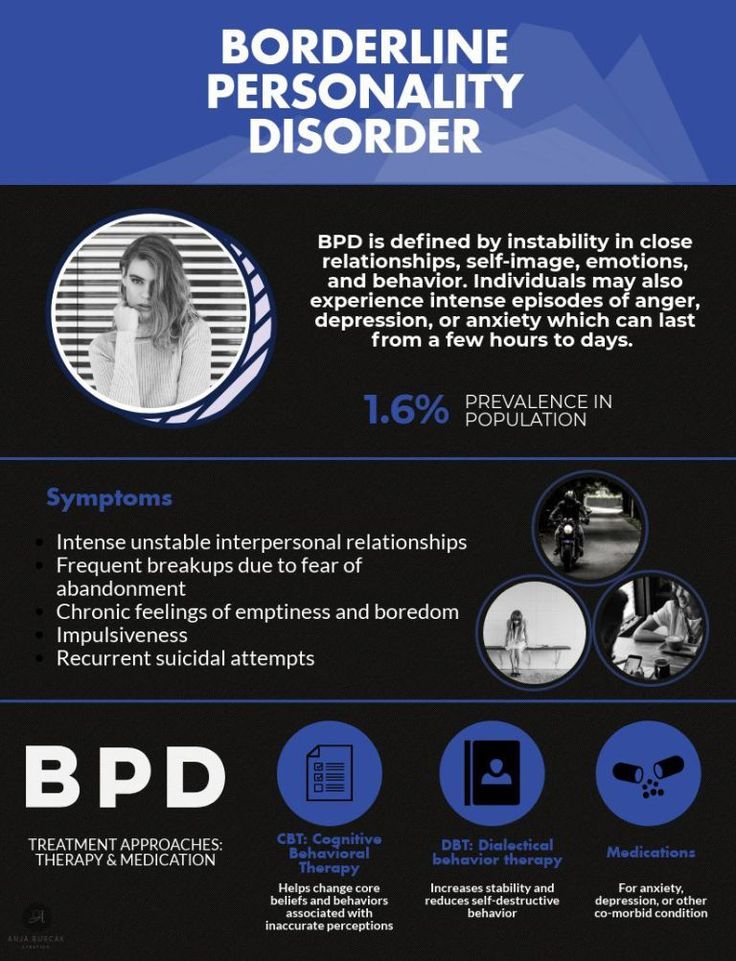
Don't ignore self-destructive behaviors and suicidal threats
If you believe your loved one is at an immediate risk for suicide Do NOT leave the person alone. Call your loved one's therapist or:
- In the U.S., dial 911 or call the National Suicide Prevention Lifeline at 1-800-273-TALK.
- In other countries, call your country's emergency services number or visit IASP to find a suicide prevention helpline.
Setting healthy boundaries with a borderline loved one
One of the most effective ways to help a loved one with BPD gain control over their behavior is to set and enforce healthy limits or boundaries. Setting limits can help your loved one better handle the demands of the outside world, where schools, work, and the legal system, for example, all set and enforce strict limits on what constitutes acceptable behavior.
Establishing boundaries in your relationship can replace the chaos and instability of your current situation with an important sense of structure and provide you with more choices about how to react when confronted by negative behavior.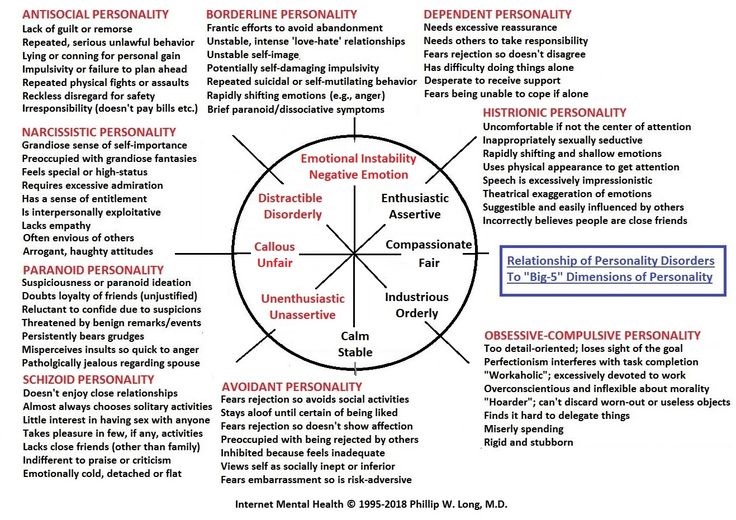 When both parties honor the boundaries, you'll be able to build a sense of trust and respect between you, which are key ingredients for any meaningful relationship.
When both parties honor the boundaries, you'll be able to build a sense of trust and respect between you, which are key ingredients for any meaningful relationship.
Setting boundaries is not a magic fix for a relationship, though. In fact, things may initially get worse before they get better. The person with BPD fears rejection and is sensitive to any perceived slight. This means that if you've never set boundaries in your relationship before, your loved one is likely to react badly when you start. If you back down in the face of your loved one's rage or abuse, you'll only be reinforcing their negative behavior and the cycle will continue. But, remaining firm and standing by your decisions can be empowering to you, benefit your loved one, and ultimately transform your relationship.
How to set and reinforce healthy boundaries
Talk to your loved one about boundaries at a time when you're both calm, not in the heat of an argument. Decide what behavior you will and will not tolerate from the person and make those expectations clear. For example, you may tell your loved one, “If you can't talk to me without screaming abuse at me, I will walk out.”
For example, you may tell your loved one, “If you can't talk to me without screaming abuse at me, I will walk out.”
Do…
- Calmly reassure the person with BPD when setting limits. Say something like, “I love you and I want our relationship to work, but I can't handle the stress caused by your behavior. I need you to make this change for me.”
- Make sure everyone in the family agrees on the boundaries—and how to enforce the consequences if they're ignored.
- Think of setting boundaries as a process rather than a single event. Instead of hitting your loved one with a long list of boundaries all at once, introduce them gradually, one or two at a time.
Don't…
- Make threats and ultimatums that you can't carry out. As is human nature, your loved one will inevitably test the limits you set. If you relent and don't enforce the consequences, your loved one will know the boundary is meaningless and the negative behavior will continue.
 Ultimatums are a last resort (and again, you must be prepared to follow through).
Ultimatums are a last resort (and again, you must be prepared to follow through). - Tolerate abusive behavior. No one should have to put up with verbal abuse or physical violence. Just because your loved one's behavior is the result of a personality disorder, it doesn't make the behavior any less real or any less damaging to you or other family members.
- Enable the person with BPD by protecting them from the consequences of their actions. If your loved one won't respect your boundaries and continues to make you feel unsafe, then you may need to leave. It doesn't mean you don't love them, but your self-care should always take priority.
Supporting your loved one's BPD treatment
Borderline personality disorder is highly treatable, yet it's common for people with BPD to avoid treatment or deny that they have a problem. Even if this is the case with your loved one, you can still offer support, improve communication, and set boundaries while continuing to encourage your friend or family member to seek professional help.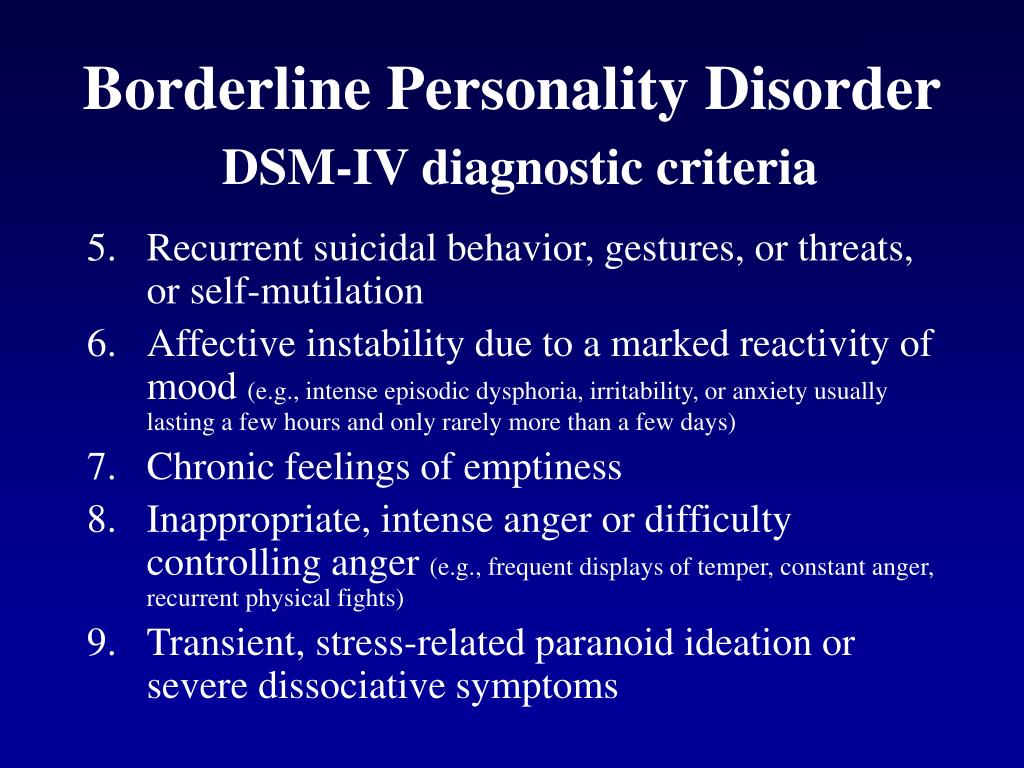
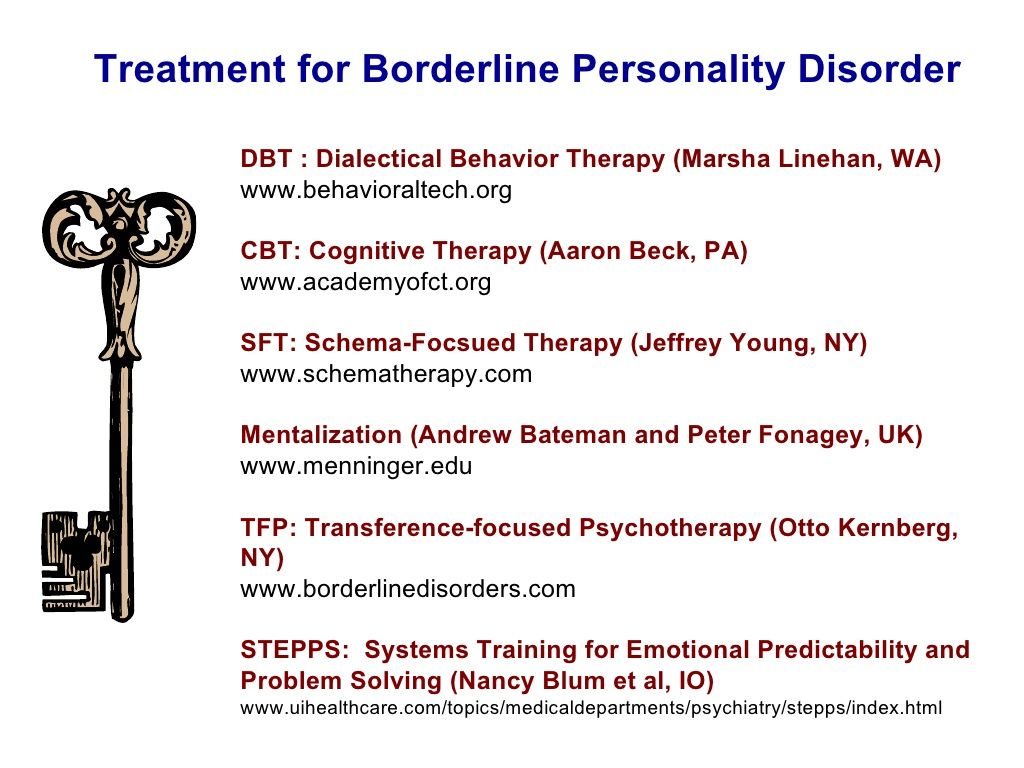
While medication options are limited, the guidance of a qualified therapist can make a huge difference to your loved one's recovery. BPD therapies, such as Dialectical Behavior Therapy (DBT) and schema-focused therapy, can help your loved one work through their relationship and trust issues and explore new coping techniques. In therapy, they can learn how to calm the emotional storm and self-soothe in healthy ways.
How to support treatment
If your loved one won't acknowledge that they have a problem with BPD, you may want to consider couple's therapy. Here, the focus is on the relationship and promoting better communication, rather than on your loved one's disorder. Your partner may more readily agree to this and eventually consider pursuing BPD therapy in the future.
Encourage your loved one to explore healthy ways of handling stress and emotions by practicing mindfulness and employing relaxation techniques such as yoga, deep breathing, or meditation. Sensory-based stimulation can also help them to relieve stress in the moment.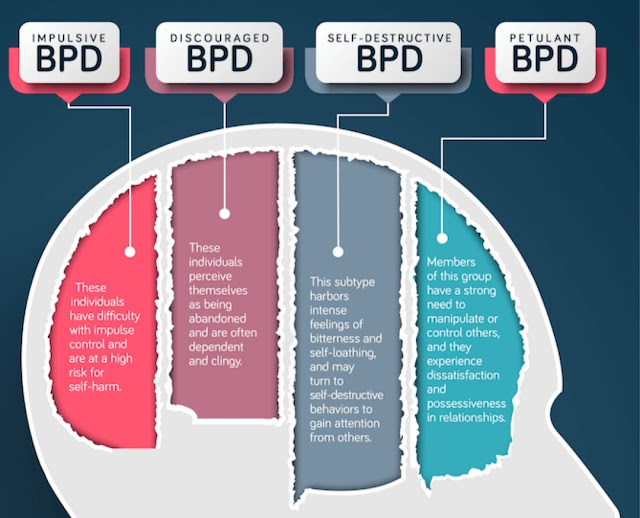 Again, you can participate in any of these therapies with your loved one, which can strengthen your bond and may encourage them to pursue other avenues of treatment as well.
Again, you can participate in any of these therapies with your loved one, which can strengthen your bond and may encourage them to pursue other avenues of treatment as well.
By developing an ability to tolerate distress, your loved one can learn how to press pause when the urge to act out or behave impulsively strikes. HelpGuide's free Emotional Intelligence Toolkit offers a step-by-step, self-guided program to teach your loved one how to ride the “wild horse” of overwhelming feelings while staying calm and focused.
Setting goals for BPD recovery: Go slowly
When supporting your loved one's recovery, it's important to be patient and set realistic goals. Change can and does happen but, as with reversing any kind of behavior pattern, it takes time.
- Take baby steps rather than aiming for huge, unattainable goals that set you and your loved one up for failure and discouragement. By lowering expectations and setting small goals to be achieved step by step, you and your loved one have a greater chance of success.
- Supporting your loved one's recovery can be both extremely challenging and rewarding. You need to take care of yourself, but the process can help you grow as an individual and strengthen the relationship between you.
Authors: Melinda Smith, M.A, Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
Personality Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x18_Personality_Disorders
Choi-Kain, Lois W., Ellen F. Finch, Sara R. Masland, James A. Jenkins, and Brandon T. Unruh. “What Works in the Treatment of Borderline Personality Disorder.” Current Behavioral Neuroscience Reports 4, no.
 1 (March 1, 2017): 21–30. https://doi.org/10.1007/s40473-017-0103-z
1 (March 1, 2017): 21–30. https://doi.org/10.1007/s40473-017-0103-zStoffers-Winterling, Jutta M., Birgit A. Völlm, Gerta Rücker, Antje Timmer, Nick Huband, and Klaus Lieb. “Psychological Therapies for People with Borderline Personality Disorder.” Cochrane Database of Systematic Reviews, no. 8 (2012). https://doi.org/10.1002/14651858.CD005652.pub2
Kulacaoglu, Filiz, and Samet Kose. “Borderline Personality Disorder (BPD): In the Midst of Vulnerability, Chaos, and Awe.” Brain Sciences 8, no. 11 (November 18, 2018): 201. https://doi.org/10.3390/brainsci8110201
Bozzatello, Paola, Silvio Bellino, Marco Bosia, and Paola Rocca. “Early Detection and Outcome in Borderline Personality Disorder.” Frontiers in Psychiatry 10 (2019): 710. https://doi.org/10.3389/fpsyt.2019.00710
Ripoll, Luis H. “Psychopharmacologic Treatment of Borderline Personality Disorder.” Dialogues in Clinical Neuroscience 15, no. 2 (June 2013): 213–24. https://www.ncbi.
 nlm.nih.gov/pmc/articles/PMC3811092/
nlm.nih.gov/pmc/articles/PMC3811092/Ng, Fiona Y. Y., Marianne E. Bourke, and Brin F. S. Grenyer. “Recovery from Borderline Personality Disorder: A Systematic Review of the Perspectives of Consumers, Clinicians, Family and Carers.” PLOS ONE 11, no. 8 (August 9, 2016): e0160515. https://doi.org/10.1371/journal.pone.0160515
Sutherland, Ruth, John Baker, and Sharon Prince. “Support, Interventions and Outcomes for Families/Carers of People with Borderline Personality Disorder: A Systematic Review.” Personality and Mental Health 14, no. 2 (2020): 199–214. https://doi.org/10.1002/pmh.1473
Angstman, Kurt, and Norman H. Rasmussen. “Personality Disorders: Review and Clinical Application in Daily Practice.” American Family Physician 84, no. 11 (December 1, 2011): 1253–60. https://www.aafp.org/afp/2011/1201/p1253.html
Borderline Personality Disorder – Overview of symptoms, causes, and treatment. (National Institute of Mental Health)
Borderline Personality Disorder (BPD) –Explains borderline personality disorder (BPD) including possible causes, how you can access treatment and support, and tips for helping yourself.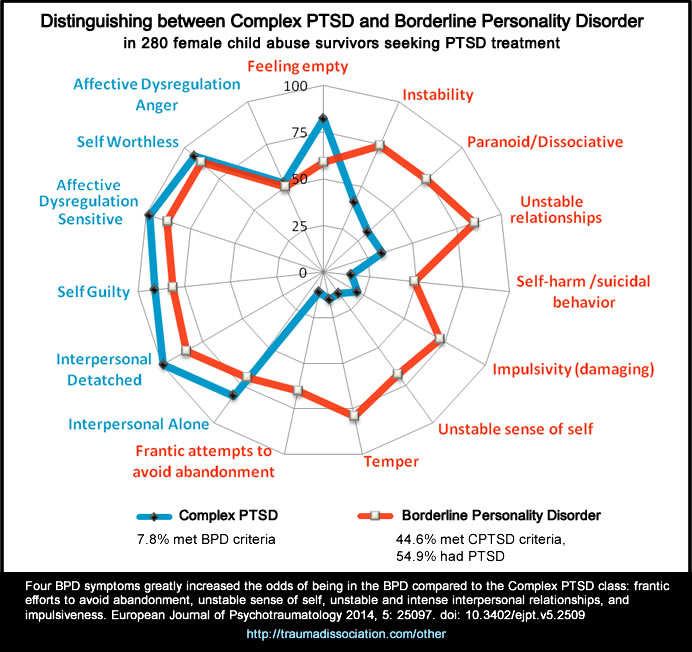 (Mind)
(Mind)
What is Dialectical Behavior Therapy (DBT)? – A comprehensive article with ten shot videos. (Behavioral Tech)
Last updated: December 5, 2022
How to Handle a Relationship With Someone Who Has It
Written by Kate Rope
People who live with borderline personality disorder (BPD) have a hard time regulating their emotions, which can be very intense, and handling stress. This can lead them to lash out at the people in their lives. As a result, they often have turbulent relationships that are as hard for the other people in them as BPD is for the person living with it. If you live with someone who has BPD, this isn’t news to you, but you may feel be at a loss about how to do anything about it.
Daniel S. Lobel, PhD, a clinical psychologist who specializes in supporting the loved ones of people with BPD, has advice on how to help yourself, your partner, and your relationship get to a healthier place.
Learn About Borderline Personality Disorder
Living with borderline personality disorder -- or living with someone who has it -- can be isolating. People with BPD and the people who live with them often feel totally alone. Education is critical, especially when it comes to the behaviors that come with the condition.
People with BPD and the people who live with them often feel totally alone. Education is critical, especially when it comes to the behaviors that come with the condition.
People with BPD tend to lash out and attack the person who doesn’t have it, Lobel says. “So people who are with people who have BPD end up feeling bad about themselves.”
Learning about how BPD causes this helps people who don’t have it understand that it isn’t them. Lobel suggests these sites to learn more about borderline personality disorder and find support:
- BPDcentral.com
- Personality Disorder Awareness Network
- National Alliance on Mental Illness
Take Care of Yourself First
Before you do anything else, “you have to stop the person from hurting you in order to make progress in the relationship,” Lobel says. Trying to help them when you’re being treated poorly -- being yelled at, living with passive aggressive behavior -- isn’t safe for you and isn’t likely to help your partner.
Instead, he says, the first step is setting a boundary about your well-being. He suggests telling your partner, “I can’t be with you unless I am well, and in order for me to be well, I have to stop you from hurting me.”
If your partner says they can’t stop, they’ll likely need professional help before you can make any progress. The goal in this step, Lobel says, is to let your partner know, “you have to stop abusing me or we have nowhere to go.”
Set -- and Stick With -- Boundaries
“People with BPD try to get other people to do for them what they should be doing for themselves,” Lobel says. And often they succeed, because the other person just wants to stop the yelling, so they give in.
Instead, tell your partner, “I will not participate in things that are unhealthy.” That might mean insisting they don’t use drugs or alcohol in the house, or not joining in if they do. It could mean leaving if your partner is yelling at you or belittling you.
Enforce Emotional Boundaries, Too
People with borderline personality disorder often bring the people near them into their emotions.
“They think, ‘If I’m angry, you need to be angry too,’ so they will create a circumstance that makes the other person angry,” Lobel says.
If you can spot these trends, it will go a long way toward stopping this co-dependent cycle.
Lobel suggests telling your partner, “You’re angry. I understand. I don’t need to be angry to understand that you’re angry. We can talk about your anger, but you can’t yell at me or be abusive.”
If they can’t stop the behavior, you can tell them “You have to handle this on your own.”
Replace Unhealthy Connection With Healthy Connection
Fighting with or defending yourself from a partner who’s treating you badly saps your interest and ability to do enjoyable things with them. That makes it harder to connect.
Lobel says making a change, like walking away when they’re treating you badly, frees up time and emotional space for you to have positive interactions, like watching a movie or taking a walk together. These are more positive ways of showing love.
Be Consistent
“Consistency is so important,” Lobel says, “because people with BPD test boundaries. If you set a limit, they may see what ways they can push or encroach on the limit.” If the pattern between you has been to let boundaries be stretched or broken over a long time, it won’t change overnight.
“You can’t just change up the boundary one day and expect them to comply,” he says. “In the short-term they will test it more.” That means things are likely to get worse before they get better.
“But if you can get past that part, and if you are very consistent,” Lobel says, “they will start to accept your boundaries.” They won’t stop testing your limits, but they will do it less and less.
Support Your Partner’s Treatment
There’s no medication that specifically treats borderline personality disorder. But there are therapies, like dialectical behavior therapy (DBT), which is the go-to treatment. “Trying to get them into a DBT program is very helpful,” Lobel says, because it teaches people with BPD healthier ways to respond and interact. You’ll want to find a therapist who’s has experience working with DBT and with people who have borderline personality disorder.
You’ll want to find a therapist who’s has experience working with DBT and with people who have borderline personality disorder.
Let your loved one know DBT can help anyone, not just folks with BPD, because it “helps people communicate and increase their tolerance for stress.”
Provide recognition when they make progress. “Compliment and comment on any positive changes and behaviors you notice,” Lobel says.
Know When You Need to Protect Yourself
“The ultimate boundary in a relationship with someone who has BPD, is telling them, ‘I just can’t stay,’” Lobel says. How do you know when it’s time to draw that line? Here are a few things to watch out for.
- Physical violence. Nobody should stay in a relationship where there’s continued physical violence, Lobel says. “Someone will get hurt, the police will be involved, nothing good can come from that."
- Too many boundaries. When there are so many topics or kinds of interactions you need to avoid to prevent your partner from lashing out, you’ve removed most of the sources of potential communication, intimacy, and connection.
- Your partner is unwilling to make changes. “If the person insists, ‘there is nothing wrong with me, it’s all you,’ that’s a red flag, and you probably have to pack your bags,” Lobel says.
- Your mood is consistently bad. “Are you walking around miserable all the time?” Lobel asks. “If you feel crappy about this relationship all day, every day, you gotta go.”
Know When to Protect Your Partner
One symptoms of BPD is self-harm, like cutting, or suicidal gestures such as overdose. If you see your partner injuring themselves, call 911.
Borderline personality disorder
Borderline personality disorder is associated with unstable mood and behavior that has a significant impact on a person's daily life
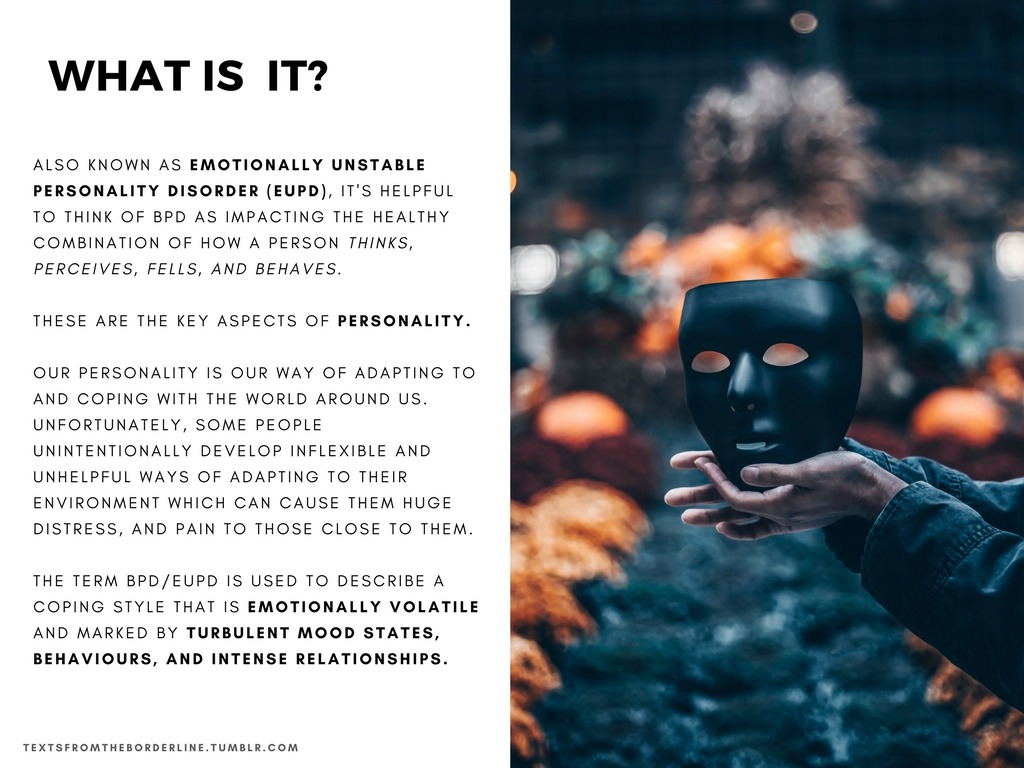
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable moods and behaviors, and an altered "feeling of self". 1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
Borderline personality disorder is a serious illness associated with self-harm and suicidal attempts. One in ten patients complete suicide. 2
Facts About Borderline Personality Disorder
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable mood and behavior, and an altered sense of self. 1
One in ten patients complete suicide. 2
Patients with borderline personality disorder are very sensitive to changes in their environment, and may respond inappropriately and acutely to such changes. They may, for example, be afraid of being abandoned by a loved one.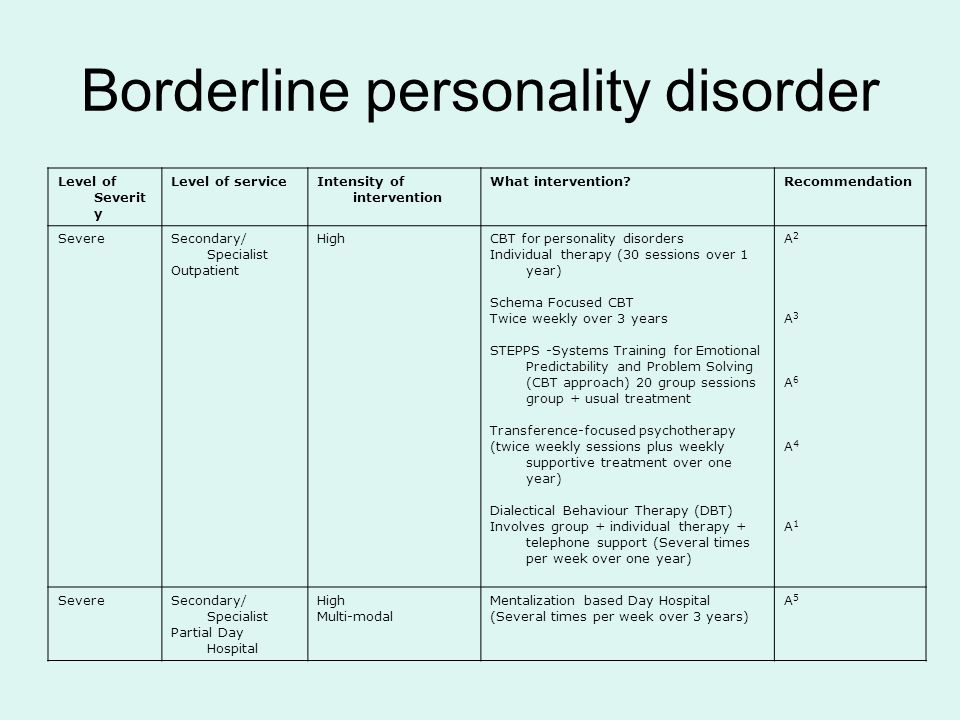 2 If the person whom patient
2 If the person whom patient
is expecting arrives late, the patient easily changes the feeling of attachment to dislike or anger.1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
People with borderline personality disorder are often insecure, may suddenly change their life goals and views on career, life values and friends. .2 They may develop intense unwarranted anger or feelings of emptiness, and are prone to self-harm.2 Patients with borderline personality disorder may also experience depression and anxiety.1,2
Facts about Borderline Personality Disorder
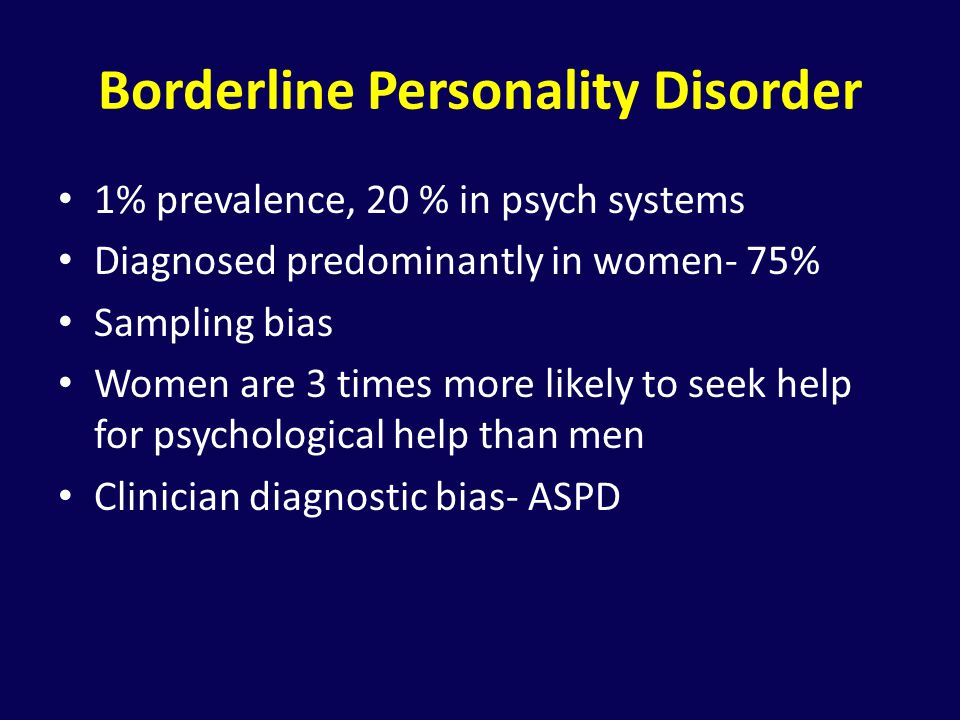
Estimates of the proportion of people who have borderline personality disorder vary from less than 1% to around 6%. 2-4
Borderline personality disorder affects a roughly equal number of men and women, but appears to be more disabling in women the same frequency in men and women, but in women it is more severe.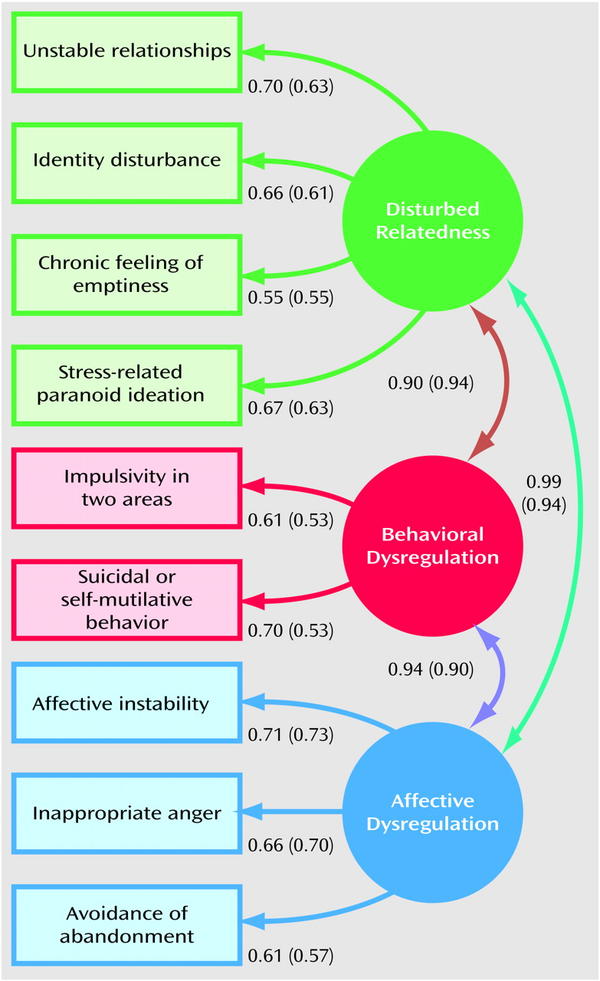 3
3
Symptoms of borderline personality disorder most often first appear during adolescence.4 The disease is most severe and problematic in young adults and tends to improve with age.2 Symptoms may persist throughout life, but most patients with borderline personality disorder by the age of 30-40 have a stable job and a home.2
People with borderline personality disorder are emotionally and functionally unstable, which places a significant burden on their families.5 Mood swings are a source of stress for both the patient and his/her others, which can lead to the development of mental disorders in the latter.1,5
People who are concerned that they – or their loved ones – are experiencing symptoms of borderline personality disorder should see their doctor for help and advice.
Borderline personality disorder is diagnosed by a mental health professional using interviews and discussions about symptoms and medical history. 1
1
Psychotherapy can help people with borderline personality disorder by, for example, teaching them how to interact with others and to express their thoughts and feelings more clearly. 1 It may also be beneficial for caregivers and family members of those affected to receive therapy and guidance on how best to care for a person with borderline personality disorder. 1 There is currently no cure, but one study showed that, after 10 years, 50% of people with borderline personality disorder had recovered, being able to function at work and maintain personal relationships. 6
- National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
 5th ed. Arlington, VA: American Psychiatric Association; 2013.
5th ed. Arlington, VA: American Psychiatric Association; 2013. - Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
- National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
- Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258.
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study.
 Am J Psychiatry. 2010;167(6):663–667.
Am J Psychiatry. 2010;167(6):663–667.
1. National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
3. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
4. National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
Access to Brain Health
We are dedicated to improving access to brain health in accordance with WHO.
Our Science
Lundbeck has developed some of the world’s most widely prescribed therapies.
This is Lundbeck
A specialized pharmaceutical company focused exclusively on brain diseases.
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
Finished reading here
Now officially: BPD is a diagnosis
Borderline personality disorder is one of ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.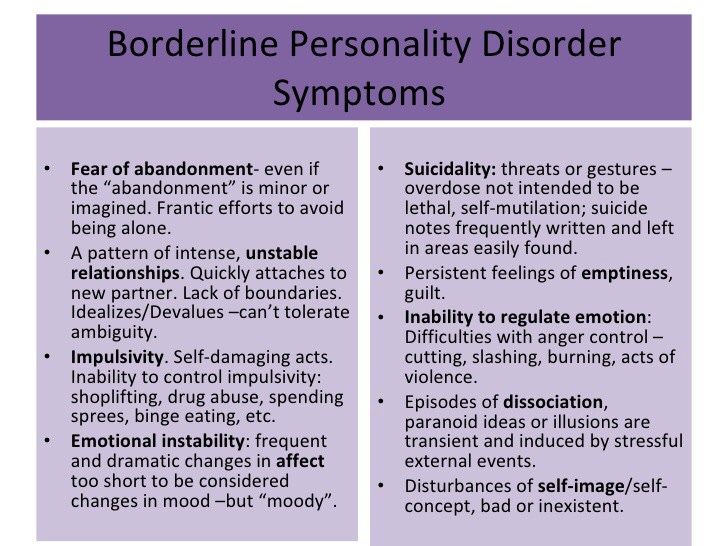
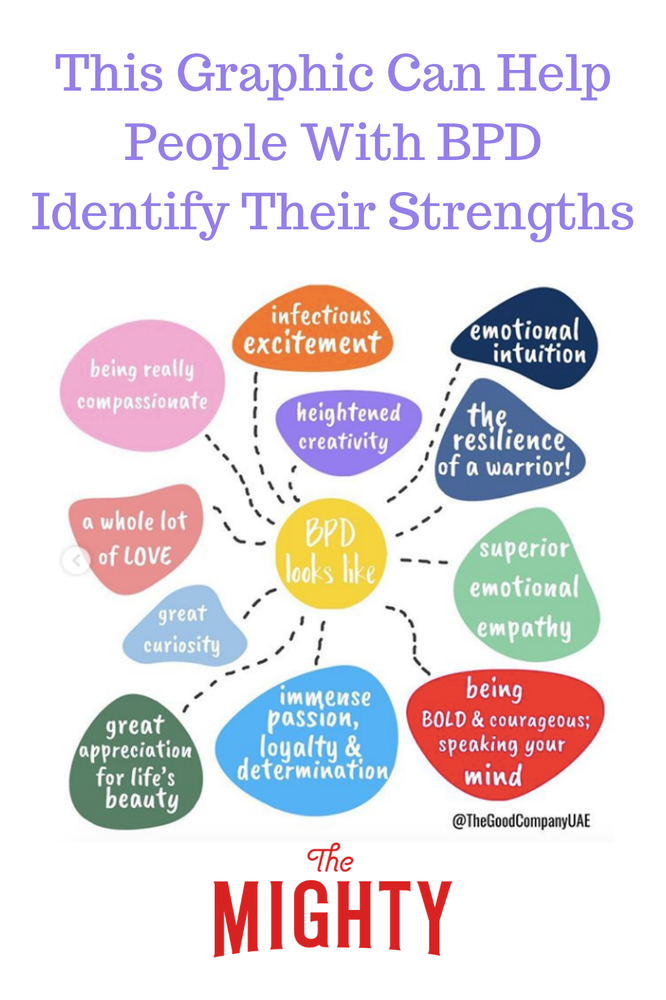
People with BPD are reverse solipsists: they are convinced of the inviolability of the world around them, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases.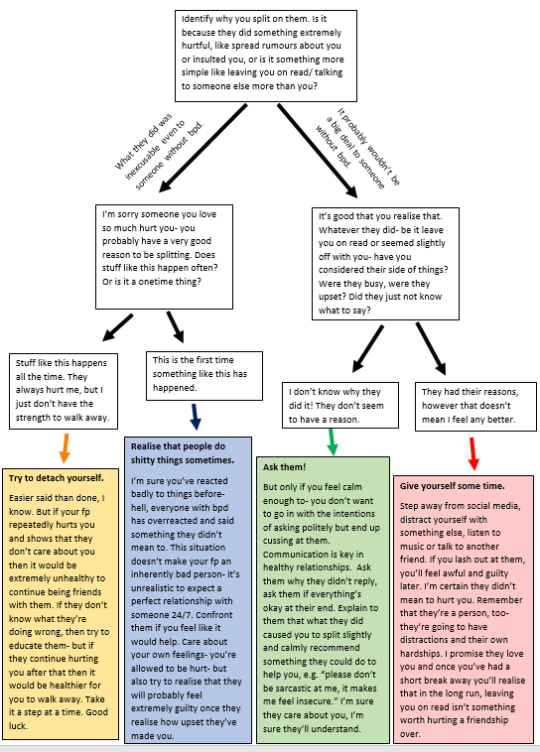 It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
Diagnosis is not a sentence, the boundary between normal and pathological is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards.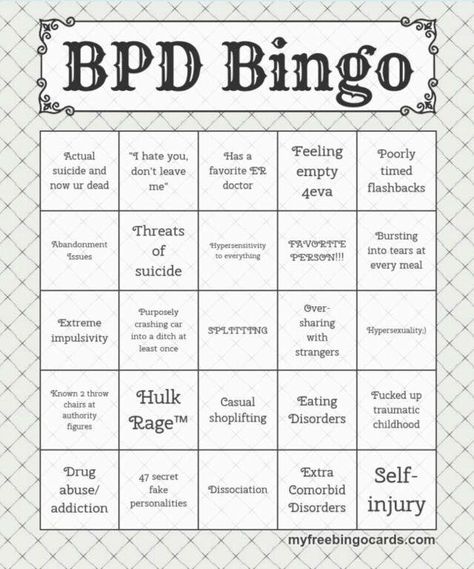 Psychotherapeutic assistance to clients with borderline disorders.
Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
Borderline personality disorder may be accompanied by alcohol, drug, gambling and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
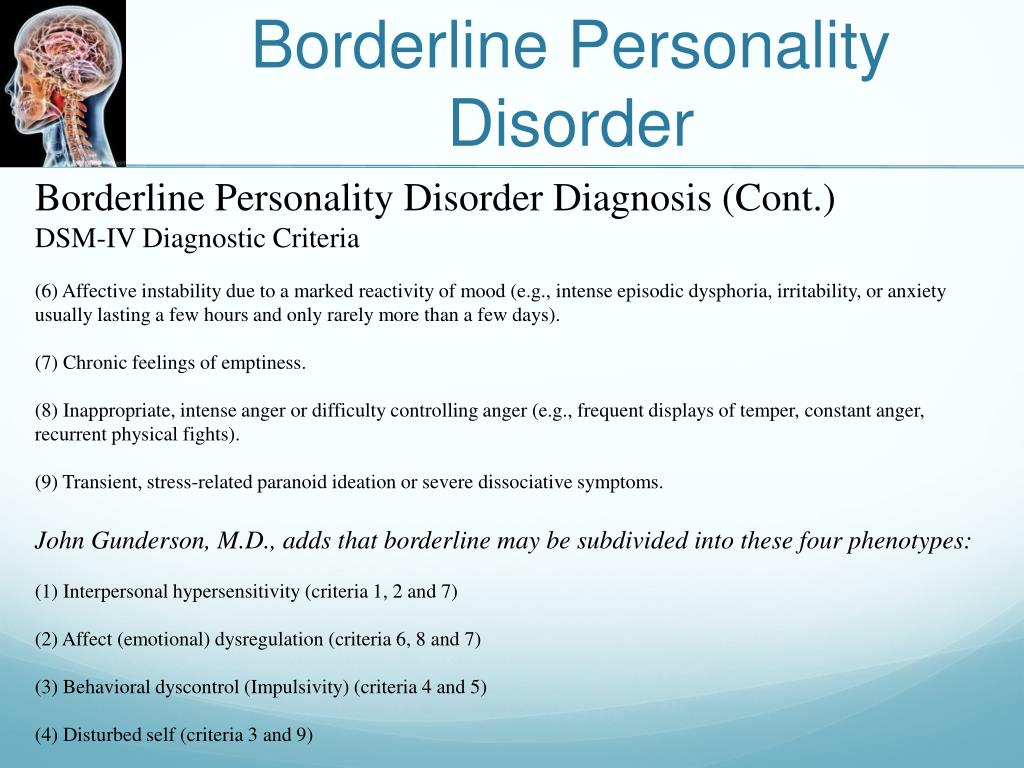
Mind, a British mental health resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone. You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
- Impulsivity and affectivity. You are overcome by strong emotions that last from a few hours to several days and can change quickly (for example, from feeling happy and confident to suddenly feeling overwhelmed and sad). This is especially evident in a state of anger, which is difficult to control.
 In a state of severe stress, you can also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
In a state of severe stress, you can also experience paranoia or dissociation (as if everything is not happening to you, but to someone else). - Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books.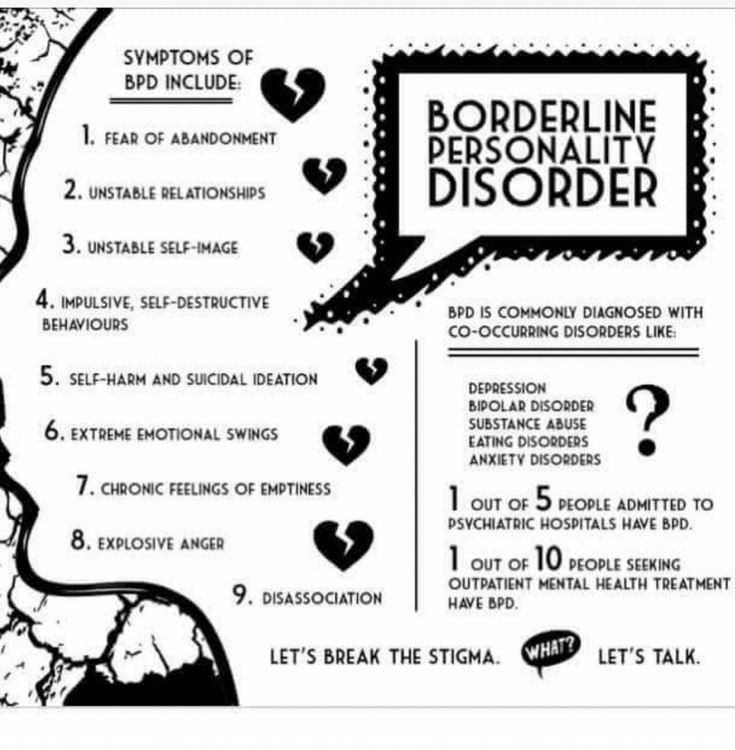 If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with interruption of communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available.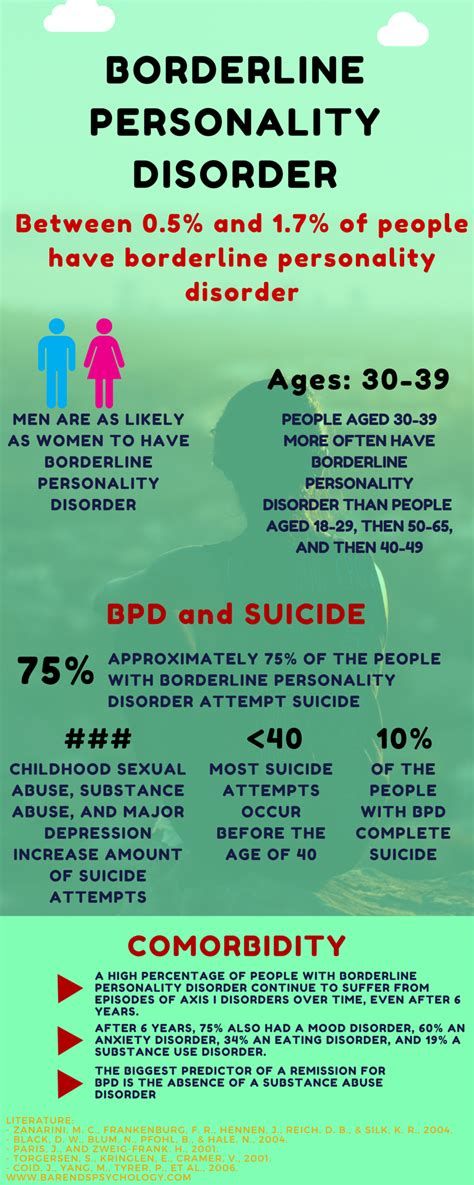 It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires identifying the cause. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.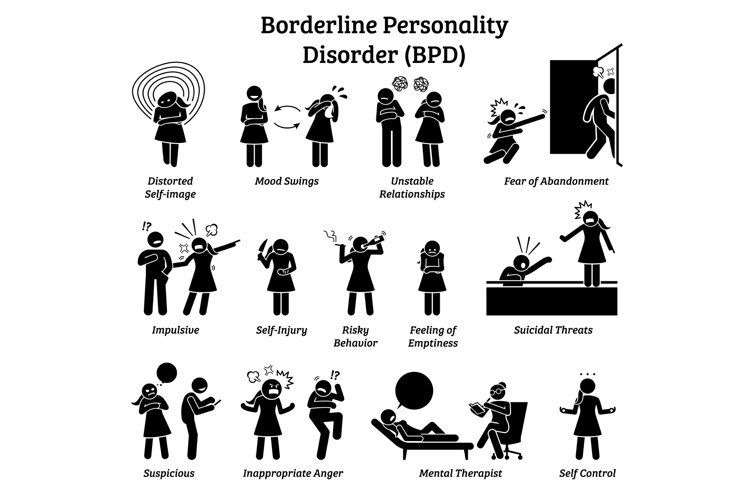
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations. For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
- Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.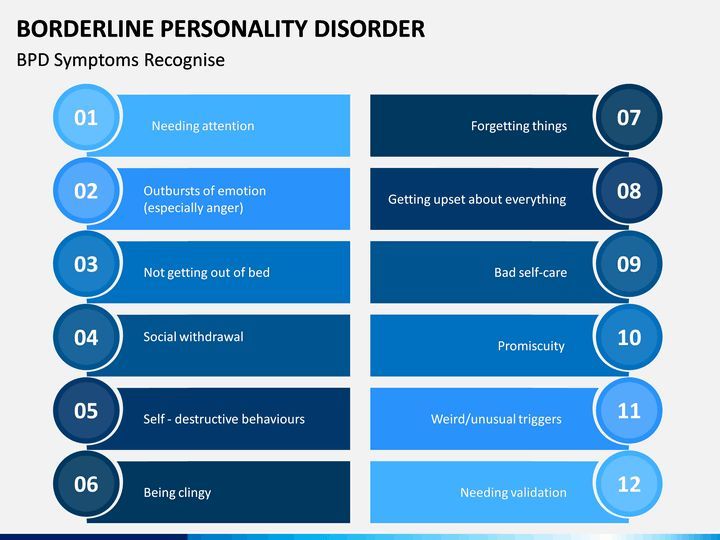
Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.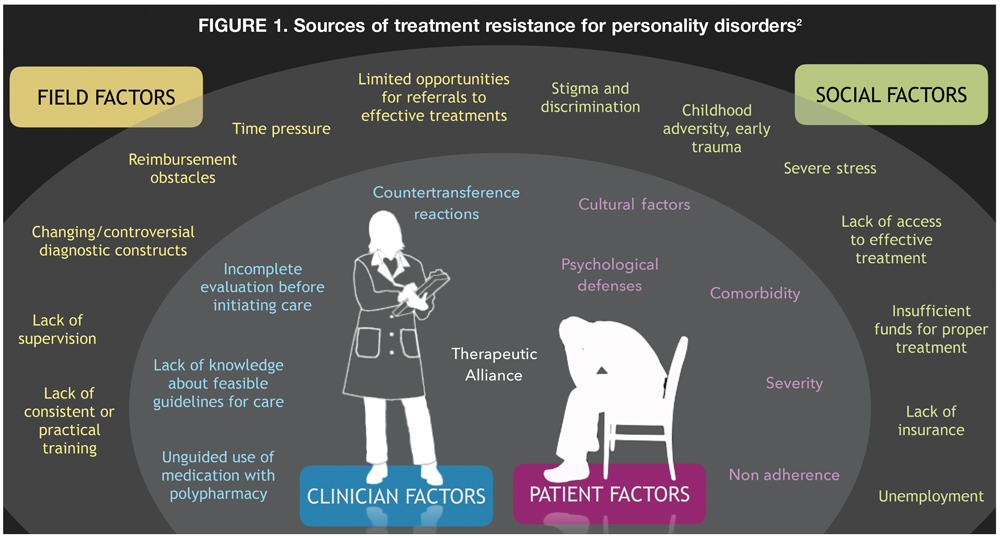 ) and syndromes (it is often necessary to treat alcohol withdrawal symptoms) syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
) and syndromes (it is often necessary to treat alcohol withdrawal symptoms) syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills. Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT).