Buspirone and zoloft
Mixing Buspar with Other Drugs
As an anxiolytic medication, it is common to find Buspirone drug combined with other drugs to treat anxiety disorders. As of 2021, there are around 1,312 approved drug interactions for this drug. Because of this large number, it is important to understand that Buspar pills mixed with other drugs and substances can lead to major Buspirone interactions. As with any drug, certain Buspirone interactions can either be mild or fatal. Additionally, there are also food-drug interactions for this drug. Some of these foods include weed-infused foods, alcohol, and grapefruit.
In this article, information about the effects of mixing Buspirone with other medications, substances, and food, and how to avoid dangerous Buspirone interactions will be provided.
Buspirone Interactions With Substances And Food
According to a study of medical doctors from the United States, the drug Buspirone can be taken on an empty stomach or with food. However, when taking it with the latter, it is necessary to learn the foods and substances that cannot be consumed with this medication. In this section, information about the effects of this drug mixed with alcohol, weed, and grapefruit will be discussed.
Buspirone And Alcohol Combination
The drug Buspar is used to treat anxiety of alcoholic patients. This means that some alcoholic patients may still consume alcohol despite the use of Buspar. Moreover, even though the combination of Buspar and alcohol is not fatal, it does exacerbate the effects of alcohol. Consuming Buspirone and alcohol can increase its sedative effects, causing increased CNS depression, dizziness, and lightheadedness. Because of this, it is better to avoid consuming Buspirone and alcohol together. So, how long does it last when consumed with alcohol? According to a study published in the American Journal of Medicine, effects stay for a couple of hours when it is paired with alcohol. Lastly, understand that the absence of major alcohol and Buspirone interactions does not mean the safety of combined use. Before using Buspar and alcohol together, seek professional advice from a medical doctor.
Lastly, understand that the absence of major alcohol and Buspirone interactions does not mean the safety of combined use. Before using Buspar and alcohol together, seek professional advice from a medical doctor.
Buspar And Weed Interaction
According to a medical study, a Buspar tablet is an effective drug for treating weed / cannabis / marijuana dependence. In this study, it was reported that this anxiolytic improved the substance use outcome of individuals who want to wean off the illicit drug. However, take note that taking Buspar and weed together can still have undesirable effects such as impaired judgment, difficulty concentrating, and drowsiness. This happens because the metabolism of the drug decreases when it is taken with weed. As most users know, marijuana shows up on urinary drug tests. So, does taking Buspar and weed show up on a drug test? Yes, this combination can lead to false-positive results on a urinary drug test.
Buspar And Grapefruit
Buspar and grapefruit interaction raises the drug’s concentration in the body which can intensify its side effects. According to a study of medical doctors from London, though rare, typical side effects of combining Buspar and grapefruit include dizziness, drowsiness, and blurred vision. To avoid this interaction, one must limit the consumption of grapefruit or grapefruit juice while taking the drug. Even regular foods can cause interactions with subsequent unpleasant effects. Consult with the doctor on dietary habits upon the prescription of the medication, or search for alternatives to the drug, such as for example Buspar vs Xanax.
According to a study of medical doctors from London, though rare, typical side effects of combining Buspar and grapefruit include dizziness, drowsiness, and blurred vision. To avoid this interaction, one must limit the consumption of grapefruit or grapefruit juice while taking the drug. Even regular foods can cause interactions with subsequent unpleasant effects. Consult with the doctor on dietary habits upon the prescription of the medication, or search for alternatives to the drug, such as for example Buspar vs Xanax.
Buspirone Interactions With Other Drugs
Buspirone is a well-tolerated medication that produces lesser side effects and mild drug interactions compared to other anxiolytics. However, Buspirone interactions may alter the cognitive functions of patients. When mixing this drug with prescription drugs like antidepressants, anxiolytics, and stimulants, a patient may experience some discomforting effects.
Wellbutrin And Buspar
In Wellbutrin and Buspar interaction, the former is an antidepressant while the latter is an anxiolytic. Taking these two together is generally safe, and there are no known interactions with Wellbutrin. Some doctors may give a prescription for the Buspirone-Wellbutrin combination. Of course, one should always follow the correct directions from a doctor for such a combination. A poorly calculated dose combination of Wellbutrin and Buspar can cause paranoia and hallucinations as Wellbutrin can decrease the metabolism of Buspar. It is also important to note that neither drug should be used in combination with MAO inhibitors as the severity of the side effects of these drugs may be increased, such as for example Buspirone weight gain.
Taking these two together is generally safe, and there are no known interactions with Wellbutrin. Some doctors may give a prescription for the Buspirone-Wellbutrin combination. Of course, one should always follow the correct directions from a doctor for such a combination. A poorly calculated dose combination of Wellbutrin and Buspar can cause paranoia and hallucinations as Wellbutrin can decrease the metabolism of Buspar. It is also important to note that neither drug should be used in combination with MAO inhibitors as the severity of the side effects of these drugs may be increased, such as for example Buspirone weight gain.
Buspar And Xanax
In Buspar and Xanax interaction, both belong to the drug class anxiolytics and they work by decreasing the abnormal excitement in the brain. In one clinical trial, it was reported that taking Buspar and Xanax together does not affect their drug clearance from the body. This means that the time it takes for these medications to get out of the system will occur normally. However, even though this clearance is not affected by each other, take note that taking these two together can increase the severity of their side effects such as increased
dizziness, drowsiness, confusion, and difficulty of concentrating.
However, even though this clearance is not affected by each other, take note that taking these two together can increase the severity of their side effects such as increased
dizziness, drowsiness, confusion, and difficulty of concentrating.
Buspar And Zoloft
Buspar is an anxiolytic while Zoloft falls under the drug class SSRIs (Selective Serotonin Reuptake Inhibitors) antidepressant. The combination of Buspar and Zoloft leads to one of the more serious interactions. Taken together, the combination of Buspar and Zoloft can lead to serotonin syndrome, a condition that is manifested with symptoms like hallucinations, major changes in blood pressure, seizures, and muscle spasms. This is one of the Buspirone interactions that could even result in a coma or death. Always consult with the doctor before taking a combination of drugs to get more information about the safety of combination drugs. By doing so, one can prevent the presence of adverse reactions and minimize health risks.
Apart from drug interactions, one must also be wary of certain foods. There is a common food-drug interaction regarding a Buspar tablet and this is the grapefruit.
Lexapro And Buspar
Buspirone hydrochloride is an anti-anxiety drug that works by influencing serotonin levels in the brain. On the other hand, Lexapro is an SSRI drug, which means a Lexapro and Buspar interaction elevates the risk of serotonin syndrome. Other dangerous health effects of combining Lexapro and Buspar include seizure, excessive sweating, fever, shaking, and blurred vision. Because of this, it is important to remember that it happens on a rare occasion and requires immediate medical attention. Is Lexapro safe for women and can you take Buspar while pregnant? The answer would be yes, but these drugs may have some risks.
Buspar And Adderall
Adderall is a stimulant medication that is used to treat ADHD while Buspar is an anxiolytic. Although these two can be taken together as a Buspar tablet also seems to improve ADHD symptoms, this interaction can elevate the risk of serotonin syndrome as they both affect serotonin levels. Serotonin syndrome can lead to dangerous health events such as coma or death if left unattended.
Serotonin syndrome can lead to dangerous health events such as coma or death if left unattended.
Buspirone And Caffeine
In the Buspirone and Caffeine interaction, the former is an anxiolytic while the latter is considered a stimulant substance. With regards to their uses, the former is used to relieve short-term symptoms of anxiety while Caffeine is used to improve mental alertness and treat migraine headaches. Although Buspirone and Caffeine come from different drug classes, it is still possible for patients taking these two substances together to experience interactions. According to a study, concomitant use of these medications causes cardiovascular health dangers and may exacerbate the side effects like blurred vision, dizziness, drowsiness, excitability, headache, lightheadedness, and nausea.
Buspirone And Melatonin
Buspirone is an anxiolytic while Melatonin is an organic compound. With regards to Buspirone and Melatonin uses, the former is used to treat mild symptoms of anxiety while the latter is used to treat insomnia, preoperative anxiety, shift-work disorder, circadian rhythm disorders, and nicotine withdrawal. Melatonin can increase the effects of the drug against anxiety. In a clinical review, it was reported that the combination of Buspirone and Melatonin can cause neurogenesis, can promote antidepressant effects, and can treat cognitive impairment.
Melatonin can increase the effects of the drug against anxiety. In a clinical review, it was reported that the combination of Buspirone and Melatonin can cause neurogenesis, can promote antidepressant effects, and can treat cognitive impairment.
Buspar And Prozac
In Buspar and Prozac interaction, the medication Prozac belongs to the drug class SSRIs and its main use is for the treatment of major depressive disorder. On the other hand, Buspirone is an anxiolytic that generally treats mild and short-term anxiety symptoms. Although rare, when Buspar and Prozac are taken together, the serum concentration of the former can be increased, causing confusion, hallucination, extreme blood pressure changes, increased heart rate, tremors, and fever.
Always Consult With Your Doctor To Avoid Dangerous Interactions
With Buspar, it is imperative to disclose all medications and health issues to a doctor. While the drug itself is slow acting and relatively safe, its concentration can be increased significantly with certain drug interactions. Thus, Buspar effects sex drive and may have some discomforting withdrawal symptoms when discontinued. The problem with most of these drug interactions is that if the correct dose is not taken, it can lead to fatal overdoses. So, can one overdose on Buspirone? Yes, it is possible to overdose on medicine alone. Abuse of this drug requires thorough substance abuse and addiction treatment. One can receive such services in a specialized rehabilitation facility for substance abusers. The role of the treatment course is to withdraw using dose reduction, detoxify, and recover from the addiction. This will help the victim of dependence to return to a previously healthy and meaningful life.
Thus, Buspar effects sex drive and may have some discomforting withdrawal symptoms when discontinued. The problem with most of these drug interactions is that if the correct dose is not taken, it can lead to fatal overdoses. So, can one overdose on Buspirone? Yes, it is possible to overdose on medicine alone. Abuse of this drug requires thorough substance abuse and addiction treatment. One can receive such services in a specialized rehabilitation facility for substance abusers. The role of the treatment course is to withdraw using dose reduction, detoxify, and recover from the addiction. This will help the victim of dependence to return to a previously healthy and meaningful life.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
(888)-212-1629
Most private insurances accepted
Marketing fee may apply
Page Sources
- Bailey, D. G., Dresser, G., & Arnold, J.
 M. O. (2013). Grapefruit–medication interactions: Forbidden fruit or avoidable consequences?. Cmaj, 185(4), 309-316.
M. O. (2013). Grapefruit–medication interactions: Forbidden fruit or avoidable consequences?. Cmaj, 185(4), 309-316. - Buch, A. B., Van Harken, D. R., Seidehamel, R. J., & Barbhaiya, R. H. (1993). A study of pharmacokinetic interaction between buspirone and alprazolam at steady state. The Journal of Clinical Pharmacology, 33(11), 1104-1109.
- Eison, A. S., & Temple Jr, D. L. (1986). Buspirone: review of its pharmacology and current perspectives on its mechanism of action. The American journal of medicine, 80(3), 1-9.
- Griffith, J. D., Jasinski, D. R., Casten, G. P., & McKinney, G. R. (1986). Investigation of the abuse liability of buspirone in alcohol-dependent patients. The American journal of medicine, 80(3), 30-35.
- Howland, R. H. (2015). Buspirone: back to the future. Journal of psychosocial nursing and mental health services, 53(11), 21-24.
- Kiani, J., & Imam, S. Z. (2007). Medicinal importance of grapefruit juice and its interaction with various drugs.
 Nutrition Journal, 6(1), 1-9.
Nutrition Journal, 6(1), 1-9. - Kumar, A., Kaur, G., & Rinwa, P. (2014). Buspirone along with melatonin attenuates oxidative damage and anxiety-like behavior in a mouse model of immobilization stress. Chinese journal of natural medicines, 12(8), 582-589.
- McRae-Clark, A. L., Carter, R. E., Killeen, T. K., Carpenter, M. J., Wahlquist, A. E., Simpson, S. A., & Brady, K. T. (2009). A placebo-controlled trial of buspirone for the treatment of marijuana dependence. Drug and alcohol dependence, 105(1-2), 132-138.
- Napoliello, M. J., & Domantay, A. G. (1991). Buspirone: a worldwide update. The British Journal of Psychiatry, 159(S12), 40-44.
- Pike, E., Stoops, W. W., & Rush, C. R. (2016). Acute buspirone dosing enhances abuse-related subjective effects of oral methamphetamine. Pharmacology Biochemistry and Behavior, 150, 87-93.
- Spencer, T., & Biederman, J. (2002). Non-stimulant treatment for attention-deficit/hyperactivity disorder. Journal of Attention Disorders, 6(1_suppl), 109-119.

Published on: July 10th, 2020
Updated on: February 15th, 2022
About Author
Isaak Stotts, LP
Isaak Stotts is an in-house medical writer in AddictionResource. Isaak learned addiction psychology at Aspen University and got a Master's Degree in Arts in Psychology and Addiction Counseling. After graduation, he became a substance abuse counselor, providing individual, group, and family counseling for those who strive to achieve and maintain sobriety and recovery goals.
Medically Reviewed by
Michael Espelin APRN
8 years of nursing experience in wide variety of behavioral and addition settings that include adult inpatient and outpatient mental health services with substance use disorders, and geriatric long-term care and hospice care. He has a particular interest in psychopharmacology, nutritional psychiatry, and alternative treatment options involving particular vitamins, dietary supplements, and administering auricular acupuncture.
Have something to say?
Share your story in our Addiction Treatment Communities
The efficacy of the combination of sertraline with buspirone for smoking cessation.
 A randomized clinical trial in nondepressed smokers
A randomized clinical trial in nondepressed smokersClinical Trial
. 2007 Oct;257(7):383-8.
doi: 10.1007/s00406-007-0726-2.
Jorge Luiz Carrão 1 , Leila Beltrami Moreira, Flávio Danni Fuchs
Affiliations
Affiliation
- 1 Department of Internal Medicine, Faculdade de Medicina, Universidade de Passo Fundo, Marcelino Ramos 111/401, Passo Fundo, RS 99010-160, Brazil.
- PMID: 17902008
- DOI: 10.1007/s00406-007-0726-2
Clinical Trial
Jorge Luiz Carrão et al. Eur Arch Psychiatry Clin Neurosci. 2007 Oct.
Eur Arch Psychiatry Clin Neurosci. 2007 Oct.
. 2007 Oct;257(7):383-8.
doi: 10.1007/s00406-007-0726-2.
Authors
Jorge Luiz Carrão 1 , Leila Beltrami Moreira, Flávio Danni Fuchs
Affiliation
- 1 Department of Internal Medicine, Faculdade de Medicina, Universidade de Passo Fundo, Marcelino Ramos 111/401, Passo Fundo, RS 99010-160, Brazil.
- PMID: 17902008
- DOI: 10.1007/s00406-007-0726-2
Abstract
In a double-blind placebo-controlled trial, we evaluated the efficacy of the combination of sertraline and buspirone plus cognitive-behavioral treatment to promote tobacco abstinence in individuals referred to a chemical dependency clinic. Ninety eight individuals 18-65 years of age were randomized to placebo or sertraline 25 mg/day for 2 days, followed by 50 mg from day 3 to 90, and buspirone 5 mg three times a day for 7 days, and 10 mg from day 8 to 90. The rate of continuous abstinence at the 26th week of follow-up, informed by the patient, was 43.5% in the active treatment group and 17.3% in the control group (p = 0.01). The odds ratio for continuous abstinence for the intervention group was 4.74 (95% CI 1.50-14.55) (adjusted for smoker households and number of cognitive sessions). Nicotine withdrawal symptoms were common in both groups (98.7% vs. 95.5% p = 0.37). The combination of sertraline and buspirone with cognitive-behavioral therapy was more effective than placebo and cognitive-behavioral therapy to promote smoking cessation.
Ninety eight individuals 18-65 years of age were randomized to placebo or sertraline 25 mg/day for 2 days, followed by 50 mg from day 3 to 90, and buspirone 5 mg three times a day for 7 days, and 10 mg from day 8 to 90. The rate of continuous abstinence at the 26th week of follow-up, informed by the patient, was 43.5% in the active treatment group and 17.3% in the control group (p = 0.01). The odds ratio for continuous abstinence for the intervention group was 4.74 (95% CI 1.50-14.55) (adjusted for smoker households and number of cognitive sessions). Nicotine withdrawal symptoms were common in both groups (98.7% vs. 95.5% p = 0.37). The combination of sertraline and buspirone with cognitive-behavioral therapy was more effective than placebo and cognitive-behavioral therapy to promote smoking cessation.
Similar articles
-
A randomized trial of sertraline as a cessation aid for smokers with a history of major depression.

Covey LS, Glassman AH, Stetner F, Rivelli S, Stage K. Covey LS, et al. Am J Psychiatry. 2002 Oct;159(10):1731-7. doi: 10.1176/appi.ajp.159.10.1731. Am J Psychiatry. 2002. PMID: 12359680 Clinical Trial.
-
Maintenance treatment with varenicline for smoking cessation in patients with schizophrenia and bipolar disorder: a randomized clinical trial.
Evins AE, Cather C, Pratt SA, Pachas GN, Hoeppner SS, Goff DC, Achtyes ED, Ayer D, Schoenfeld DA. Evins AE, et al. JAMA. 2014 Jan 8;311(2):145-54. doi: 10.1001/jama.2013.285113. JAMA. 2014. PMID: 24399553 Free PMC article. Clinical Trial.
-
Buspirone effect on tobacco withdrawal symptoms: a randomized placebo-controlled trial.
Robinson MD, Pettice YL, Smith WA, Cederstrom EA, Sutherland DE, Davis H.
 Robinson MD, et al. J Am Board Fam Pract. 1992 Jan-Feb;5(1):1-9. J Am Board Fam Pract. 1992. PMID: 1561909 Clinical Trial.
Robinson MD, et al. J Am Board Fam Pract. 1992 Jan-Feb;5(1):1-9. J Am Board Fam Pract. 1992. PMID: 1561909 Clinical Trial. -
Patients with severe depression may benefit from buspirone augmentation of selective serotonin reuptake inhibitors: results from a placebo-controlled, randomized, double-blind, placebo wash-in study.
Appelberg BG, Syvälahti EK, Koskinen TE, Mehtonen OP, Muhonen TT, Naukkarinen HH. Appelberg BG, et al. J Clin Psychiatry. 2001 Jun;62(6):448-52. doi: 10.4088/jcp.v62n0608. J Clin Psychiatry. 2001. PMID: 11465522 Clinical Trial.
-
A controlled trial of bupropion added to nicotine patch and behavioral therapy for smoking cessation in adults with unipolar depressive disorders.
Evins AE, Culhane MA, Alpert JE, Pava J, Liese BS, Farabaugh A, Fava M.
 Evins AE, et al. J Clin Psychopharmacol. 2008 Dec;28(6):660-6. doi: 10.1097/JCP.0b013e31818ad7d6. J Clin Psychopharmacol. 2008. PMID: 19011435 Free PMC article. Clinical Trial.
Evins AE, et al. J Clin Psychopharmacol. 2008 Dec;28(6):660-6. doi: 10.1097/JCP.0b013e31818ad7d6. J Clin Psychopharmacol. 2008. PMID: 19011435 Free PMC article. Clinical Trial.
See all similar articles
Cited by
-
Antidepressants for smoking cessation.
Howes S, Hartmann-Boyce J, Livingstone-Banks J, Hong B, Lindson N. Howes S, et al. Cochrane Database Syst Rev. 2020 Apr 22;4(4):CD000031. doi: 10.1002/14651858.CD000031.pub5. Cochrane Database Syst Rev. 2020. PMID: 32319681 Free PMC article.
-
Current pharmacologic treatments for smoking cessation and new agents undergoing clinical trials.
Nagano T, Katsurada M, Yasuda Y, Kobayashi K, Nishimura Y. Nagano T, et al.
 Ther Adv Respir Dis. 2019 Jan-Dec;13:1753466619875925. doi: 10.1177/1753466619875925. Ther Adv Respir Dis. 2019. PMID: 31533544 Free PMC article. Review.
Ther Adv Respir Dis. 2019 Jan-Dec;13:1753466619875925. doi: 10.1177/1753466619875925. Ther Adv Respir Dis. 2019. PMID: 31533544 Free PMC article. Review. -
Why are Antidepressant Drugs Effective Smoking Cessation Aids?
Shoaib M, Buhidma Y. Shoaib M, et al. Curr Neuropharmacol. 2018;16(4):426-437. doi: 10.2174/1570159X15666170915142122. Curr Neuropharmacol. 2018. PMID: 28925882 Free PMC article. Review.
-
Antidepressants for smoking cessation.
Hughes JR, Stead LF, Hartmann-Boyce J, Cahill K, Lancaster T. Hughes JR, et al. Cochrane Database Syst Rev. 2014 Jan 8;2014(1):CD000031. doi: 10.1002/14651858.CD000031.pub4. Cochrane Database Syst Rev. 2014. PMID: 24402784 Free PMC article.
 Updated. Review.
Updated. Review. -
A double-blind randomized clinical trial of different doses of transdermal nicotine patch for smoking reduction and cessation in long-term hospitalized schizophrenic patients.
Chen HK, Lan TH, Wu BJ. Chen HK, et al. Eur Arch Psychiatry Clin Neurosci. 2013 Feb;263(1):75-82. doi: 10.1007/s00406-012-0338-3. Epub 2012 Jun 23. Eur Arch Psychiatry Clin Neurosci. 2013. PMID: 22729212 Clinical Trial.
See all "Cited by" articles
References
-
- N Engl J Med. 1999 Mar 4;340(9):685-91 - PubMed
-
- Arch Intern Med.
 1998 Oct 12;158(18):2035-9 - PubMed
1998 Oct 12;158(18):2035-9 - PubMed
- Arch Intern Med.
-
- Psychopharmacology (Berl). 1989;99(1):64-9 - PubMed
-
- Chest. 2000 Apr;117(4 Suppl 1):169S-175S - PubMed
-
- Lancet. 2002 Nov 2;360(9343):1347-60 - PubMed
Publication types
MeSH terms
Substances
Spitomin (buspirone).
 A new "classic" in the treatment of anxiety disorders
A new "classic" in the treatment of anxiety disorders partners Keywords / keywords: Spitomin, Neuropsychiatry, Anxiolytics, Psychiatry, Anxiety disorders
Introduction to the problem
According to large-scale epidemiological studies conducted in the United States and Europe in 2005 and 2010, anxiety disorders of varying severity are observed in 21-30% of the population 1 . According to WHO, the problem is in the top 10 most significant health problems 2 .
It has been proven that anxiety disorders are characterized by a chronic course 3 and a high degree of comorbidity with other mental and behavioral disorders. First of all, this concerns depression, which in more than 50% of cases 4 accompanies panic disorder or generalized anxiety disorder. Often, the combination of anxiety and depressive disorders leads to a more severe course of the disease and resistance to standard treatment.
Often, the combination of anxiety and depressive disorders leads to a more severe course of the disease and resistance to standard treatment.
Therapy of anxiety-depressive disorders, which include generalized anxiety disorder (GAD), panic disorder with agoraphobia, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), social phobias, as a rule, long-term and combined, requires careful selection of doses , their episodic correction and monitoring of side effects.
Complex therapy should be directed to:
- elimination of mental and somatic symptoms (anxiety, restlessness, muscle tension, sleep disturbances, pain syndrome, blood pressure fluctuations, arrhythmias, etc.),
- treatment of comorbid conditions,
- improving the quality of life,
- achieving complete remission (relapse prevention).
Among the means of pharmacotherapy today, combinations of tricyclic antidepressants, antidepressants of the SSRI and SNRI groups, benzodiazepines are most often used.
Existing problems in the classical treatment of anxiety disorders
Antidepressants
The therapeutic effect of SSRIs, like other antidepressants, is realized mainly from the 2nd–3rd week of therapy, and the 1st week may be marked by an increase in anxiety, which is subjectively difficult to tolerate by patients 5 . In addition, there is the possibility of developing, despite a generally favorable tolerability profile, potentially dangerous side effects (serotonin syndrome), as well as a withdrawal syndrome 6 .
Benzodiazepines
It is generally recognized that tranquilizers of this group have pronounced undesirable effects: muscle relaxant, sedative, excessive hypnotic, amnestic, negative effects on psychomotor functions, a high risk of developing addiction and withdrawal syndrome 7 .
Pregabalin
Recently, the psychotropic activity of the drug pregabalin, a structural analogue of GABA, has been discussed in the literature. It reduces the stimulation of postsynaptic neurons, causing anxiolytic, anticonvulsant and analgesic effects. However, when using the drug for 8 weeks, only 52% of patients had a 50% reduction in symptoms according to the Hamilton anxiety scale (HAM-A) 8 .
It reduces the stimulation of postsynaptic neurons, causing anxiolytic, anticonvulsant and analgesic effects. However, when using the drug for 8 weeks, only 52% of patients had a 50% reduction in symptoms according to the Hamilton anxiety scale (HAM-A) 8 .
Taking into account the goals of therapy and existing problems, a list of requirements was determined that the main clinical and pharmacological characteristics of anxiolytics must meet:
- a distinct anxiolytic effect, both in relation to the mental and somatic components of anxiety;
- lack of sedative, muscle relaxant and additive properties;
- the action of the drug should be aimed not only at eliminating the mental symptoms of the disorder, but also at treating comorbid conditions;
- decrease in maladaptation;
- improving the quality of life.
Spitomin (buspirone), the only representative of the class of serotonergic anxiolytics, azapirones, is perhaps most consistent with these criteria.
Spitomin (buspirone): mechanism of action
Buspirone differs in its chemical structure from all other previously known anxiolytics and belongs to the azaspirone class.
Its anxiolytic action is associated with stimulation of presynaptic serotonin autoreceptors, and, unlike SSRIs, does not depend on the nature of the basal release of serotonin 9 . Buspirone has proven to be an effective pharmacotherapy for the most difficult treatable forms of anxiety disorders and was the first nonbenzodiazepine anxiolytic to be approved by the FDA in 1986, for the treatment of patients with GAD 10 .
Spitomin (buspirone) occupies a special place among all neuropharmacological agents and can be considered as a drug that combines the properties of an anxiolytic and antidepressant, which is of great value in the treatment of mixed anxiety-depressive disorders.
Spitomin (buspirone) affects:
- Serotonin neurotransmission system.
 When it is hyperactive, it stimulates presynaptic 5-HT1A receptors that block the release of serotonin into the synapse (antiserotonergic effect). When it is weakened, it stimulates postsynaptic 5-HT1A receptors (activates serotonergic processes) 11 .
When it is hyperactive, it stimulates presynaptic 5-HT1A receptors that block the release of serotonin into the synapse (antiserotonergic effect). When it is weakened, it stimulates postsynaptic 5-HT1A receptors (activates serotonergic processes) 11 . - Dopamine neurotransmission system. By selectively blocking pre and postsynaptic D2 receptors, it increases the rate of excitation of dopamine neurons in the midbrain 12 and enhances its independent antidepressant effect.
- Norepinephrine system of neurotransmission. The active metabolites of buspirone have an adrenergic effect 13 . The associated general mood elevation explains the antidepressant effect in SSRI-resistant patients.
Spitomin (buspirone) does not affect either GABA or benzodiazepine receptors, and therefore does not have the side effects of such tranquilizers. Nevertheless, in terms of its effectiveness, by the 7-14th day of therapy, the drug is comparable to typical benzodiazepines.
Indications for use
Spitomin (buspirone) has shown its clinical efficacy in the treatment of the following diseases:
- Generalized Anxiety Disorder (GAD).
- panic disorder.
- Syndrome of autonomic dysfunction.
- Alcohol withdrawal syndrome (as adjuvant therapy).
- Depressive disorders (as adjuvant therapy).
Clinical efficacy
Based on numerous clinical studies (Murphy, Owen and Tyrer; Schramm et al., Pato et al., Goodman et al., Jenike et al., Robinson et al., etc.), buspirone has been proven to be a very promising and safe agent for long-term mono- or combination therapy.
For generalized anxiety disorder
The anxiolytic effect of buspirone does not differ from that of diazepam (after use for 3 or more weeks) 14 . Buspirone is much more effective than benzodiazepines in reducing depressive symptoms associated with anxiety disorder. Adverse events of a sedative nature when taking buspirone occur much less frequently than with benzodiazepines 15 .
Adverse events of a sedative nature when taking buspirone occur much less frequently than with benzodiazepines 15 .
For anxiety and depression
The efficacy of buspirone in the treatment of GAD in combination with depressive symptoms is 1.3 times superior to placebo in reducing anxiety and 1.6 times superior to placebo in reducing depressive symptoms 16 . The tolerability of buspirone is comparable to placebo.
For obsessive-compulsive disorder (OCD)
- Clomipramine and buspirone show the same result on the OCD scale and the depression scale.
- Buspirone added to OCD therapy with fluoxetine improves the effectiveness of treatment.
- Simultaneous administration of buspirone and antipsychotics is well suited for patients who are not amenable to therapy with selective serotonin reuptake inhibitors.
In the treatment of depression
Numerous open studies have unambiguously proven the positive effect of buspirone on depressive symptoms, including resistant depression. When buspirone was added to antidepressant therapy, there was a significant improvement in the condition, compared with the placebo group. Some symptoms such as depressed mood, unwillingness to work, lethargy improved after the first week of taking the drug.
When buspirone was added to antidepressant therapy, there was a significant improvement in the condition, compared with the placebo group. Some symptoms such as depressed mood, unwillingness to work, lethargy improved after the first week of taking the drug.
Buspirone, already an effective antidepressant in itself, when added to enhance classical antidepressant therapy, presumably via the serotonergic and noradrenergic systems, may improve treatment outcomes 17 . Buspirone is an effective and safe agent for improving the results of antidepressant therapy.
In the treatment of panic disorder
Buspirone significantly reduces the severity of generalized anxiety, agoraphobia, panic attacks and depression in a short time 18 . The positive effect of buspirone has been demonstrated in relation to both cognitive and somatic components of anxiety.
For anxiety disorder in the elderly
The use of buspirone by elderly people suffering from anxiety disorder is more favorable than benzodiazepine treatment. Often, in the treatment of such patients, a prolonged anxiolytic effect is achieved while maintaining muscle tone, normal breathing, and the speed of cognitive and psychomotor reactions. In addition, it is important that buspirone improves mood.
Often, in the treatment of such patients, a prolonged anxiolytic effect is achieved while maintaining muscle tone, normal breathing, and the speed of cognitive and psychomotor reactions. In addition, it is important that buspirone improves mood.
For alcohol addiction
In the buspirone group, compared with placebo, there was a significant improvement in the following psychopathological parameters: anxiety disorder, depression, irritability, interpersonal relationships, and global psychopathological score. A meta-analysis has shown that buspirone improves the treatment of alcohol dependence and anxiety disorders. The researchers concluded that the main effect of buspirone on patients with alcohol dependence is not in reducing alcohol consumption, but in a positive effect on psychopathological symptoms. It improves mood, which is very important in the treatment of anxiety disorders, does not cause addiction, and does not adversely affect the psychomotor reaction.
Output
Thus, Spitomin (buspirone) can successfully replace classic drugs that cause intolerance or side effects, or supplement therapy to achieve a more complete and faster effect.
Buspirone is a powerful selective serotonergic anxiolytic, which, due to its pharmacodynamics, has a pronounced anxiolytic effect without disturbing cognitive functions and psychomotor reaction speed, which is perfect for both the elderly and active business people.
1 Kessler RC, Chiu WT, Demler O et al. Prevalence, severity and comorbidity of 12-month DSM-IV disorders in NCSR. Arch Gen Psychiatr 2005; 62:617–27; Terrie E, HonaLee H, Avshalom C et al. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a Birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry 2007;
2 Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic. NY: Guilford Press 2002; European Status Report on Alcohol and Health 2010. WHO Euro, Copenhagen;
WHO Euro, Copenhagen;
3 Hirschfeld RM. Placebo response in the treatment of panic disorder. Bull Menning Clin 1996; 60(2): 76–86;. Keller MB. The clinical course of panic disorder and depression. J Clin Psychiat 1992; 53 (Suppl.): 5–8;
4 Kalinin V.V. / Anxiety disorders - Rijeka: In Tech, 2011 - 323p;
5 Nutt DJ. Overview of diagnosis and drug treatments of anxiety disorders. CNS Spectr 2005; 10(1): 49–56;
6 Schatzberg AF, Haddad P, Kaplan EM et al. Serotonin reuptake inhibitor discontinuation syndrome: a hypothetical definition. Discontinuation consensus panel. J Clin Psychiat 1997; 58 (Suppl. 7): 5–10;
7 Avedisova A.S., Yastrebov D.V., Kostacheva E.A. Pharmacoepidemiological analysis of outpatient prescription of benzodiazepine tranquilizers in psychiatric institutions. Ros. Psychiatrist. magazine 2005; 4:10–2;
8 Instructions for use for pregabalin (Lyrica).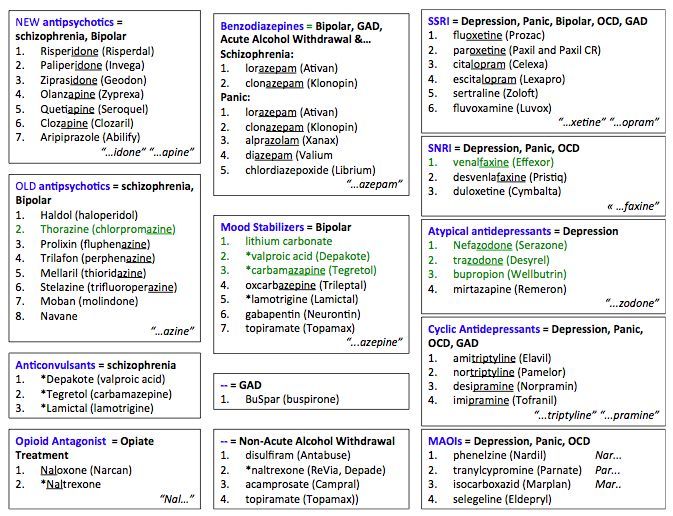
9 Baldwin D, I. Anderson, D. Nutt et al. Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2005; 19: 567–96
10 Loane C, Politis M. Buspirone: what is it all about? Brain Res. 2012 Jun 21; 1461: 111-8
11 Anon A. Buspiron bei Angst und Depression // Pharm Ztg. - 1996. - Vol. 34. – P. 43.
12 Instructions for medical use.
13 S.G. Burchinsky, Buspiron: new possibilities for the treatment of anxiety and depressive disorders in neurological practice. Institute of Gerontology, AMS of Ukraine, Kyiv
14 RickelsK., Wiseman K., Norstad N., et al. Buspirone and diazepam in anxiety: a controlled Study// J. Clin. Psychiatry, 1982, 43(12), 81-86;
15 BY HAROLD L. GOLDBERG, M.D., AND RICHARD J. FINNERTY, Ph.D. he Comparative Efficacy of Buspirone and Diazepam in the Treatment of Anxiety. m J Psychiatry 136:9September 1979.
m J Psychiatry 136:9September 1979.
16 Sramek JJ1, Tansman M, Suri A, Hornig-Rohan M, Amsterdam JD, Stahl SM, Weisler RH, Cutler NR. Efficacy of buspirone in generalized anxiety disorder with coexisting mild depressive symptoms. J Clin Psychiatry. 1996 Jul;57(7):287-91. http://www.ncbi.nlm.nih.gov/pubmed/8666569
17 Dimitriou, Evangelos C. MD; Dimitriou, Christos E. MD. Buspirone Augmentation of Antidepressant Therapy. Journal of Clinical Psychopharmacology:December 1998 - Volume 18 - Issue 6 - pp 465-469.
18 Cottraux J, Note ID, Cungi C, Légeron P, Heim F, Chneiweiss L, Bernard G, Bouvard M. A controlled study of cognitive behavior therapy with buspirone or placebo in panic disorder with agoraphobia. Br J Psychiatry. Nov 1995; 167(5):635-41;. http://www.ncbi.nlm.nih.gov/pubmed/8564320
Treatment of anxiety in general practice
Article No. 64. Anxiety disorders are common in general medical practice in patients with somatic diseases: more than 20% of patients who come to medical consultations have clinically significant symptoms of anxiety. However, the word “anxiety” itself is rarely found in the complaints made. More often you can hear complaints about anxiety over trifles, insecurity, constant concern about your future, excessive fears, a feeling of constant expectation, easily arising excitement, difficulty falling asleep or interrupted sleep, unpleasant dreams, irritability, inability to concentrate. These complaints are mental in nature and directly indicate the presence of anxiety. More difficult in differential diagnosis are complaints of a somatic nature, such as fussiness, tension headaches, tremors, inability to relax, tachycardia, sweating, dry mucous membranes, difficulty breathing, nausea, dyspepsia, diarrhea, chills, persistent weakness, interruptions in the heart, feeling compression or compression in the chest, increased blood pressure (BP), spastic abdominal pain, back and lower back pain, myalgia, pallor or redness, goose bumps, itching, urticaria, sexual dysfunction, etc. [1]. Most of the complaints of a somatic nature are due to muscle tension and autonomic dysfunction, which is typical for a state of anxiety.
However, the word “anxiety” itself is rarely found in the complaints made. More often you can hear complaints about anxiety over trifles, insecurity, constant concern about your future, excessive fears, a feeling of constant expectation, easily arising excitement, difficulty falling asleep or interrupted sleep, unpleasant dreams, irritability, inability to concentrate. These complaints are mental in nature and directly indicate the presence of anxiety. More difficult in differential diagnosis are complaints of a somatic nature, such as fussiness, tension headaches, tremors, inability to relax, tachycardia, sweating, dry mucous membranes, difficulty breathing, nausea, dyspepsia, diarrhea, chills, persistent weakness, interruptions in the heart, feeling compression or compression in the chest, increased blood pressure (BP), spastic abdominal pain, back and lower back pain, myalgia, pallor or redness, goose bumps, itching, urticaria, sexual dysfunction, etc. [1]. Most of the complaints of a somatic nature are due to muscle tension and autonomic dysfunction, which is typical for a state of anxiety.
The ability to recognize possible somatic symptoms of anxiety is important for somatic physicians to differentiate between anxiety disorders and somatic diseases, given their frequent combination with each other.
The diagnostic criteria for generalized anxiety disorder (F41.1) according to ICD-10 are as follows.
1. Generalized persistent anxiety, not limited to any specific circumstances (or arising mainly under these circumstances).
2. Related:
- fears (fears) for health and one's life, life and health of loved ones, other bad forebodings;
- motor (muscle) tension - fussiness, tremor, inability to relax;
- vegetative and vegetative-pain symptoms.
3. Presence of symptoms most days of the week for several weeks or months [2].
In clinical practice, it often happens that in the presence of psychological and somatic symptoms of increased anxiety, their number or duration is insufficient to make a definite diagnosis; then one speaks of subsyndromal anxiety. Often it is due to a high level of personal anxiety. According to neurophysiological studies, such individuals tend to have a background increase in heart rate, blood pressure, cardiac dysfunction, as well as large shifts in these indicators during mental activity and stress [3]. The question of the need to prescribe pharmacotherapy for subsyndromal anxiety is decided individually, in contrast to clinically expressed anxiety disorders. Numerous studies have shown that anxiety disorders have a long-term undulating course, aggravated after stress. After 5 years, spontaneous complete remission is observed only in 1/3 of patients. In this regard, the mandatory appointment of anti-anxiety pharmacotherapy becomes clear.
Often it is due to a high level of personal anxiety. According to neurophysiological studies, such individuals tend to have a background increase in heart rate, blood pressure, cardiac dysfunction, as well as large shifts in these indicators during mental activity and stress [3]. The question of the need to prescribe pharmacotherapy for subsyndromal anxiety is decided individually, in contrast to clinically expressed anxiety disorders. Numerous studies have shown that anxiety disorders have a long-term undulating course, aggravated after stress. After 5 years, spontaneous complete remission is observed only in 1/3 of patients. In this regard, the mandatory appointment of anti-anxiety pharmacotherapy becomes clear.
There is a constant search for the most effective drugs for the treatment of anxiety disorders. It is known that neurochemical and neuroendocrine levels are involved in the development of anxiety: GABAergic, noradrenergic, serotonergic, histaminergic systems, as well as hormones or peptides like corticotropic releasing hormone associated with corticosteroid, neurosteroid hormones, the hypothalamic-pituitary axis and cholecystokinin. This explains such a wide range of pharmacological drugs used to relieve anxiety disorders.
This explains such a wide range of pharmacological drugs used to relieve anxiety disorders.
At the beginning of the XX century. bromides have been used to treat anxiety and insomnia; in the 1940s, ethyl alcohol and its structural analogues, such as Paraldehyde and Chloral Hydrate; in the 50s. - barbiturates and propanediol derivatives, including meprobamate. In the 1960s benzodiazepines appeared, which are still the most commonly prescribed drugs [4]. In modern medicine, in addition to the latter, "small" antipsychotics, antidepressants and non-benzodiazepine anxiolytics are also used. Let's take a closer look at each of these groups.
The effect of taking benzodiazepine drugs for anxiety is due to inhibition of the central nervous system through GABA receptors. At relatively low doses, they exhibit anxiolytic properties, while at higher doses they exhibit sedative-hypnotic properties. Based on the varying degrees of evidence from the studies performed, as well as their pharmacokinetic properties for each of the drugs, a predominant indication was derived. So, for example, Phenazepam, Flurazepam, Temazepam and Triazolam are used more often for the treatment of insomnia due to a pronounced hypnotic effect.
So, for example, Phenazepam, Flurazepam, Temazepam and Triazolam are used more often for the treatment of insomnia due to a pronounced hypnotic effect.
Diazepam (Sibazon, Relanium, Seduxen) is effective in the medical treatment of situational anxiety at a dosage of 5 mg 3 times a day. If necessary, the dose can be increased to 30 mg / day. In the case of generalized anxiety disorder, the daily dose may be increased from 15–30 mg to 40–50 mg. In some patients, stable improvement occurs after 2-6 weeks of therapy, but in most cases, discontinuation of therapy leads to a relapse of anxiety. In this regard, it is recommended to combine psychopharmacotherapy with cognitive-behavioral psychotherapy [4].
Alprazolam and Clonazepam have a clear advantage in efficacy and pharmacokinetic parameters in the treatment of panic attacks. Alprazolam is usually prescribed at 2-6 mg / day, divided into 3-4 doses. Consider the main problems associated with taking Alprazolam. He has a higher risk of developing addiction, which leads to more severe relapses and severe withdrawal symptoms. Due to the short half-life, some patients develop anxiety relapses between doses. Despite the frequent use of Alprazolam, patients may experience significant discomfort when the effect of the last dose wears off. They constantly monitor the time of taking the drug and often increase the dosage on their own.
Due to the short half-life, some patients develop anxiety relapses between doses. Despite the frequent use of Alprazolam, patients may experience significant discomfort when the effect of the last dose wears off. They constantly monitor the time of taking the drug and often increase the dosage on their own.
When using Clonazepam, due to the longer half-life, it is possible to avoid the above problems. Its daily dose is 1-4 mg and is divided into 2 doses, although the therapeutic range varies from 0.5 to 6.0 mg / day. The disadvantage of clonazepam therapy compared with alprazolam is a higher risk of developing depression [4].
The widespread use of benzodiazepines in general medical practice in patients with complaints of anxiety and insomnia is due to a combination of efficacy and relative safety. However, over the past 20 years, cases of addiction and abuse have become more frequent. Indeed, with prolonged use of even therapeutic doses of benzodiazepines (6 months or more), the risk of developing dependence or withdrawal syndrome is high. Most often, addiction is caused by drugs with a pronounced, but short-term effect, such as Alprazolam and Lorazepam. The use of benzodiazepines is also limited by their diverse side effects, such as muscle relaxation, daytime sleepiness, ataxia, memory impairment, decreased concentration, recoil syndrome and the above-mentioned addiction, drug dependence and withdrawal syndrome [4].
Most often, addiction is caused by drugs with a pronounced, but short-term effect, such as Alprazolam and Lorazepam. The use of benzodiazepines is also limited by their diverse side effects, such as muscle relaxation, daytime sleepiness, ataxia, memory impairment, decreased concentration, recoil syndrome and the above-mentioned addiction, drug dependence and withdrawal syndrome [4].
To date, there are no well-established, generally accepted guidelines for the management of long-term benzodiazepine withdrawal in outpatients. For these purposes, SSRIs (trittiko) are most commonly used [5]. In GNTS and SP them. V.P. Serbsky, a study was conducted using the atypical antipsychotic Eglek (Sulpiride) as a “cover therapy” for the period of withdrawal and, subsequently, replacement therapy. Having a pronounced anti-anxiety effect already at a dose of 200 mg / day, Eglek effectively affected the prevailing anxiety disorders, both paroxysmal and generalized. No less important is the somatotropic and vegetostabilizing effects of Eglek [6].
Due to its pronounced anxiolytic and sedative effect in general medical practice, another “small” neuroleptic, Thioridazine (Sonapax), is often prescribed. The experience of using it in clinical practice, especially in outpatient practice, has established its strong position as a tool necessary in the treatment of a wide range of anxiety-neurotic disorders. Undoubted indications for the appointment of Thioridazine are anxiety disorders proper, anxiety-phobic disorders with various content of phobias, somatoform neurotic disorders, the so-called latent depressions with senesto-hypochondriac and vegetative-vascular manifestations, acting under the guise of vegetative-vascular dystonia or various algic syndromes. The daily dose of the drug can vary from 10 to 300 mg. In general, Thioridazine is well tolerated, however, when prescribing high doses and long-term use, manifestations of arterial hypotension, especially orthostatic, are possible, although extremely rare, which are functional and reversible [7]. Neuroendocrine disorders may manifest as weight gain.
Neuroendocrine disorders may manifest as weight gain.
Since the middle of the XX century. Antidepressants are increasingly being used in the treatment of anxiety disorders. Numerous studies have shown that the use of classical (tricyclic) antidepressants (amitriptyline, imipramine, clomipramine) gives a more pronounced and persistent clinical effect. Moreover, antidepressant therapy eliminates the possibility of developing frequent complications that occur when using anxiolytics, such as changes in tolerance, the formation of drug dependence and withdrawal syndrome. However, it also has many complications - side effects. If it is necessary to use high doses of tricyclic antidepressants for long courses (from six months or more), such undesirable effects as an excessive sedative effect, weakening of concentration of attention, a decrease in the speed of reaction impede social and professional, especially intellectual activity, study, create restrictions in work that requires speed and accuracy of actions (including driving a car). It should also be noted that the use of tricyclic antidepressants is impossible with some concomitant somatic diseases (severe cardiovascular pathology, prostate diseases, open-angle glaucoma) [8, 9].
It should also be noted that the use of tricyclic antidepressants is impossible with some concomitant somatic diseases (severe cardiovascular pathology, prostate diseases, open-angle glaucoma) [8, 9].
Antidepressants of the next generations, due to their selective effect, are safer when prescribed to patients with concomitant somatic diseases. Currently, selective serotonin reuptake inhibitors are most often used: Fluvoxamine, Fluoxetine, Trazodone, Citalopram, Escitalopram, Paroxetine, Sertraline, etc. Due to the fact that the therapeutic effect of antidepressants develops only on the 2-4th week of their use, In practice, if a somatic patient has a depressive disorder and severe anxiety symptoms, in about 80% of cases, doctors prescribe both an antidepressant and an anxiolytic at the same time. In about 75% of cases, it is benzodiazepine, which causes problems associated with its side effects and pharmacokinetic interactions between them. The result of a study conducted in France was the conclusion that the joint appointment of SSRIs and benzodiazepines is inappropriate, due to the fact that the latter reduce the antidepressant effect. The investigators suggest that a non-benzodiazepine anxiolytic be used when co-prescribing an SSRI and an anti-anxiety drug is needed. Representatives of this group are Atarax, Buspirone and Azofen.
The investigators suggest that a non-benzodiazepine anxiolytic be used when co-prescribing an SSRI and an anti-anxiety drug is needed. Representatives of this group are Atarax, Buspirone and Azofen.
Atarax (Hydroxyzine) is a histamine H1 receptor antagonist. It is used at a dose of 25-100 mg / day, divided into 3 doses. The advantages of Atarax are the absence of dependence and withdrawal syndrome. Due to the pronounced M-anticholinergic effect, it is recommended not to prescribe or to prescribe Atarax with caution in patients with glaucoma, prostate hypertrophy, difficulty urinating, and constipation. Also, the drug during the 1st week reduces attention and ability to respond, which limits its use in outpatient practice.
Buspirone is a partial 5-HT1A receptor agonist, whereby it reduces serotonin turnover. In terms of the degree of effectiveness of monotherapy for generalized anxiety disorders, it is comparable to benzodiazepines, but only with regular use. Significant advantages of Buspirone are the absence of sedation, dependence and withdrawal symptoms, as well as the presence of an antidepressant effect, manifested when taking large doses of the drug. An obstacle to use is the lack of registration of the drug in Russia [4].
An obstacle to use is the lack of registration of the drug in Russia [4].
As a result of a long search for the most optimal drug, a new selective anxiolytic, Afobazole, has been created at the Research Institute of Pharmacology of the Russian Academy of Medical Sciences. It prevents the development of membrane-dependent changes in the GABA receptor. Afobazole has both anxiolytic and mild stimulating (activating) effects, which compares favorably with its predecessors. Reducing or eliminating anxiety (concern, bad feelings, apprehensions, irritability), tension (shyness, tearfulness, feelings of anxiety, inability to relax, insomnia, fear), and therefore somatic (muscular, sensory, cardiovascular, respiratory, gastrointestinal intestinal symptoms), vegetative (dry mouth, sweating, dizziness), cognitive (difficulties in concentrating, impaired memory) disorders are observed on the 5-7th day of treatment. The drug is taken at 30 mg / day, divided into 3 doses. The duration of the course is 2-4 weeks. If necessary, the daily dose can be increased to 60 mg. Afobazole has passed clinical trials in many leading clinics in Moscow and St. Petersburg. A small number of contraindications contributes to the wider prescription of Afobazole by general medical practitioners. The advantages of the drug are also the absence of muscle relaxant properties, negative effects on cognitive processes, drug dependence and withdrawal syndrome. Due to the fact that anxiety affect is often accompanied by severe vegetative disorders, attention should be paid to the vegetotropic effect of Afobazole [10].
If necessary, the daily dose can be increased to 60 mg. Afobazole has passed clinical trials in many leading clinics in Moscow and St. Petersburg. A small number of contraindications contributes to the wider prescription of Afobazole by general medical practitioners. The advantages of the drug are also the absence of muscle relaxant properties, negative effects on cognitive processes, drug dependence and withdrawal syndrome. Due to the fact that anxiety affect is often accompanied by severe vegetative disorders, attention should be paid to the vegetotropic effect of Afobazole [10].
Thus, Afobazole is an effective drug both for monotherapy and for combined treatment with antidepressants in patients with generalized anxiety disorders and adjustment disorders, which are so common in general medical practice.
References
1. Starostina E. G. Generalized anxiety disorder and anxiety symptoms in general medical practice // BC. 2004. V. 12. No. 22. S. 2–7.
S. 2–7.
2. Classification of diseases in psychiatry and narcology: A guide for doctors / Ed. M. M. Milevsky. M., 2003.
3. Autonomic disorders: clinic, diagnosis, treatment / Ed. A. M. Veyna. M., 2003.
4. Arana J., Rosenbaum J. Pharmacotherapy of mental disorders / Per. from English. M., 2004.
5. Register of medicines of Russia. RLS - Encyclopedia of drugs. 14th issue / Ed. G. L. Vyshkovsky. M.: RLS-2006, 2005.
6. Yastrebov D.V., Cheberda O.A., Kostycheva E.A. The effectiveness of the drug "Eglek" as a means of substitution therapy in patients taking long-term benzodiazepine tranquilizers//Psychiatry and psychopharmacotherapy. 2005. V. 7. No. 4. S. 200–205.
7. Raisky V. A. Psychotropic drugs in the clinic of internal diseases. M., 1988.
8. Kolyutskaya E. V. Anxiety disorders (diagnosis and therapy) // RMJ. 2004. V. 132. No. 15. S. 1019–1021.
9. Mosolov S. N. Anxiety and depression: problems of diagnosis and therapy//Psychopharmacotherapy of depression.