Functions of serotonin neurotransmitter
Functions, normal range, side effects, and more
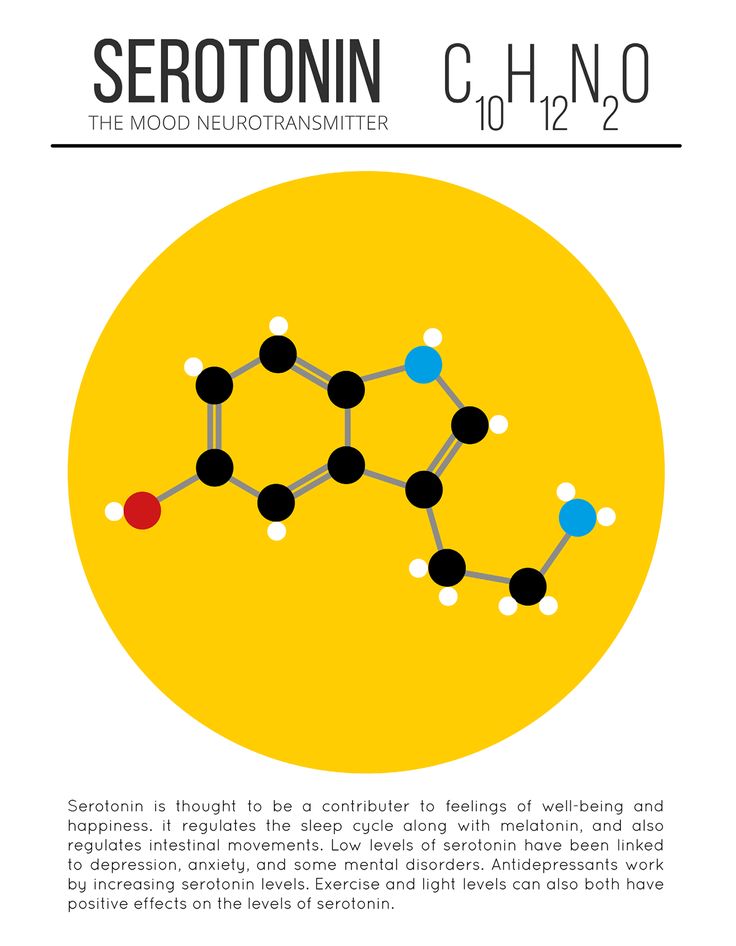
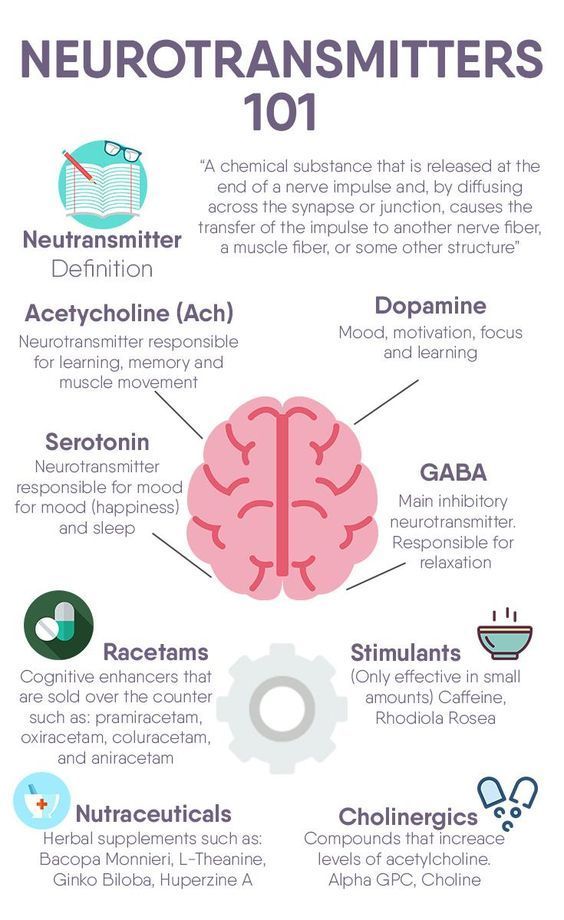
Serotonin has a wide variety of functions in the human body. People sometimes call it the “happy” chemical because it contributes to well-being and happiness.
The scientific name for serotonin is 5-hydroxytryptamine (5-HT). It is a natural chemical mainly present in the brain, bowels, and blood platelets.
Serotonin is a neurotransmitter, and some also consider it a hormone. The body uses it to send messages between nerve cells.
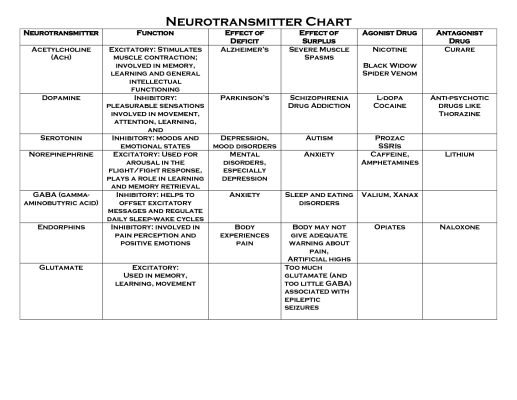
Serotonin appears to affect mood, emotions, appetite, and digestion. As the precursor for melatonin, it helps regulate sleep-wake cycles and the body clock.
Many investigations have looked at serotonin and its effects, but there is much to learn.
In this article, we look at the role of serotonin in the body, drugs that affect serotonin, side effects and symptoms of serotonin deficiency, and how to boost serotonin levels.
Serotonin results from tryptophan, a component of proteins, combining with tryptophan hydroxylase, a chemical reactor. Together, they form 5-HT, or serotonin.
The intestines and the brain produce serotonin. It is also present in blood platelets and plays a role in the central nervous system (CNS).
Serotonin occurs throughout the body and appears to influence a range of physical and psychological functions.
The substance is also present in animals, plants, and fungi. For this reason, some people have looked at food as a possible source of serotonin.
However, serotonin cannot cross the blood-brain barrier. This means that the brain must produce any serotonin it needs. Treatments for depression and other mental health issues do not supply serotonin directly but trigger reactions that can boost serotonin levels in the brain.
That said, research suggests that sources of serotonin in other areas, such as the digestive system, may work independently of serotonin in the brain. This could have implications for treating and preventing various physiological conditions, such as bone degeneration.
As a neurotransmitter, serotonin relays signals between nerve cells and regulates their intensity.
Scientists believe it plays a role in mood and the CNS and affects functions throughout the body. It may have an effect on:
- bone metabolism
- cardiovascular health
- eye health
- blood clotting
- neurological disorders
However, the relationship between serotonin and many bodily functions remains unclear.
Scientists do not precisely know what causes depression, but one theory is that it stems from an imbalance of neurotransmitters in the body.
Doctors commonly prescribe selective serotonin reuptake inhibitors (SSRIs) as antidepressants. Fluoxetine (Prozac) is one example.
Typically, the body reabsorbs a neurotransmitter after transmitting its neural impulse. SSRIs stop the body from reabsorbing serotonin, leaving higher serotonin levels to circulate.
Many people find SSRIs help relieve their symptoms, although the link between depression and serotonin remains unclear.
One problem for researchers is that, while they can measure serotonin levels in the bloodstream, they cannot measure its levels in the brain.
As a result, they do not know whether serotonin levels in the bloodstream reflect those in the brain. It is also impossible to know whether SSRIs can affect the brain.
Nevertheless, while scientists have not yet proven the serotonin theory of depression, SSRIs do appear to help many people.
Other disorders
Apart from depression, doctors may prescribe drugs that regulate serotonin levels to treat several other disorders, including:
- bipolar disorder
- post-traumatic stress disorder
- bulimia
- obsessive-compulsive disorder
- panic disorders
- migraine
As with depression, some scientists have questioned whether serotonin is the only factor affecting these conditions.
Learn more about how to stop a panic attack.
Medical professionals can measure a person’s serotonin blood levels but cannot measure serotonin levels in the brain.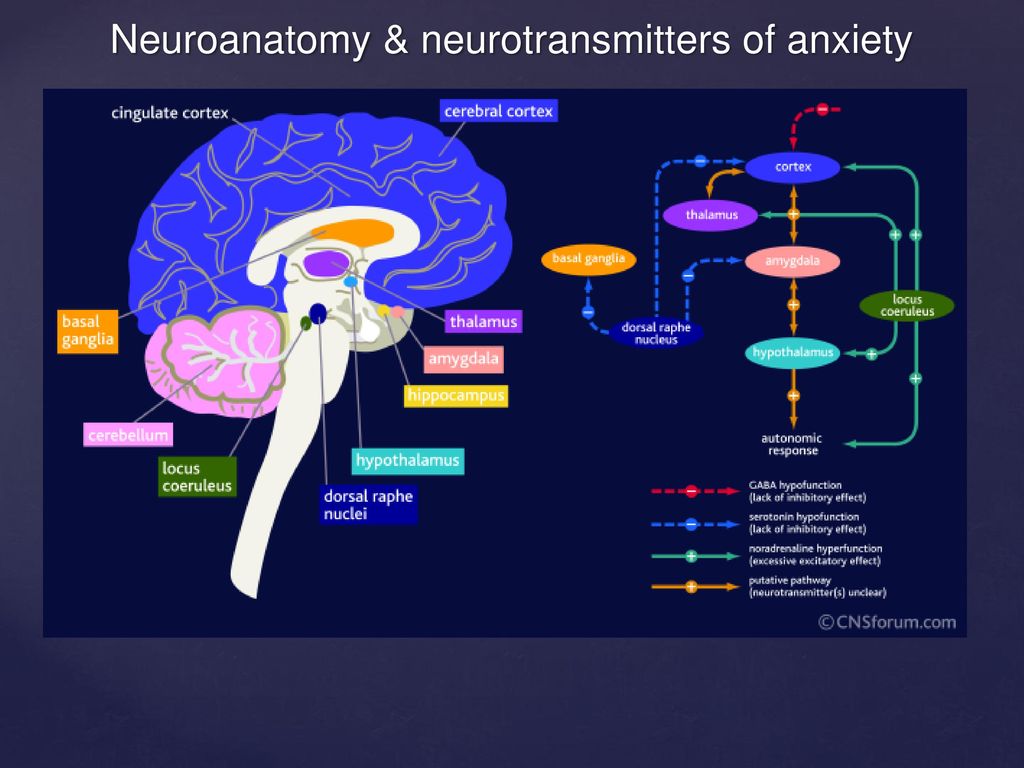
Typically, treatments aim to stabilize serotonin levels between 101 and 283 nanograms per milliliter.
According to the National Institute on Drug Abuse (NIDA), low serotonin levels can lead to memory problems and a low mood.
These are symptoms of depression, although scientists have not confirmed a link between low serotonin levels and depression.
NIDA notes that when people use certain recreational drugs, such as MDMA (ecstasy), the body releases large amounts of serotonin.
This can lead to serotonin depletion, low mood, confusion, and other symptoms lasting several days.
Animal studies have suggested that these drugs may damage the nerves that contain serotonin, with possible long lasting adverse effects.
Learn more about serotonin deficiency.
Medications, foods, and other natural remedies can alter serotonin levels.
SSRIs increase serotonin levels by preventing the body from reabsorbing serotonin neurotransmitters. Serotonin levels remain high in the brain, and this may elevate a person’s mood.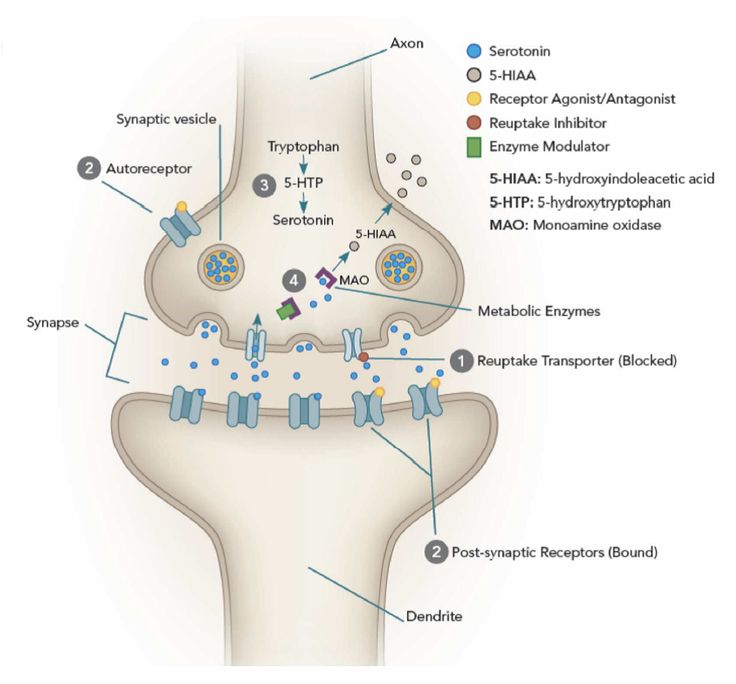
SSRIs that have approval from the Food and Drug Administration (FDA) for treating depression include:
- citalopram (Celexa)
- escitalopram (Lexapro)
- Prozac
- paroxetine (Paxil, Pexeva)
- sertraline (Zoloft)
- vilazodone (Viibryd)
Learn more about SSRIs and other antidepressants.
Adverse effects of SSRIs
SSRIs have some side effects, but these usually improve with time.
They include:
- nausea and vomiting
- restlessness and agitation
- indigestion
- diarrhea or constipation
- weight or appetite loss
- increased sweating
- dizziness
- blurred vision
- sleepiness or insomnia
- feeling shaky
- dry mouth
- headache
- low sex drive
- erectile dysfunction
- suicidal thoughts
Serotonin syndrome
Rarely, taking too much of a drug that boosts serotonin levels or combining two such drugs can lead to serotonin syndrome.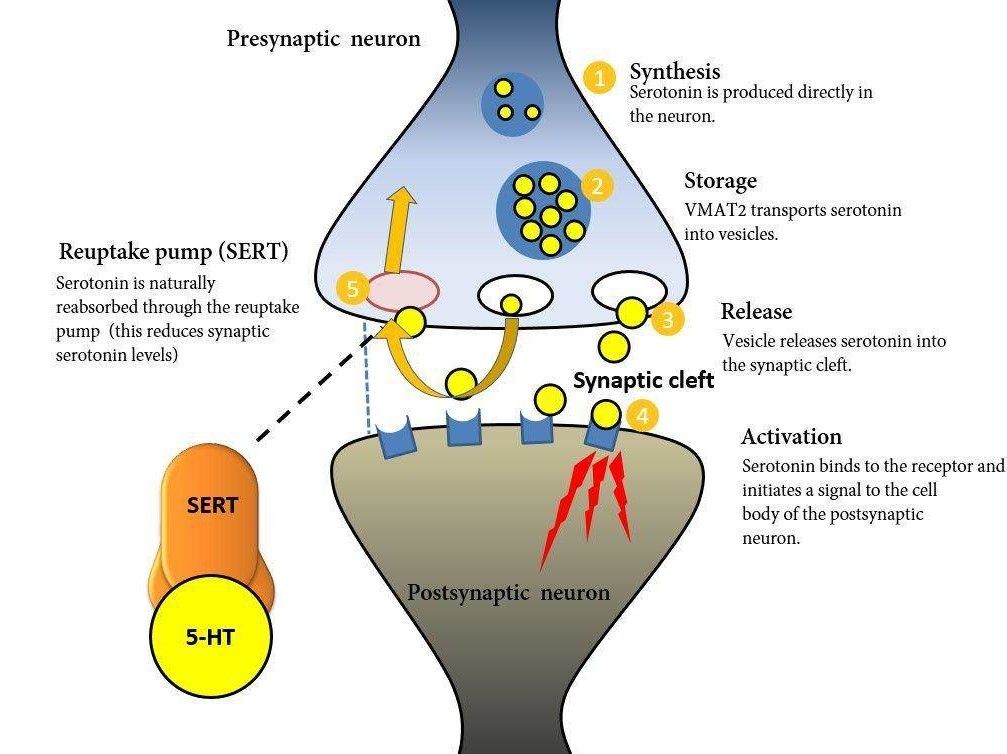 This is a potentially life threatening condition that may require emergency treatment.
This is a potentially life threatening condition that may require emergency treatment.
Learn more about serotonin syndrome.
SSRIs and suicide
A person who uses SSRIs for depression will not experience the benefits at once. At first, symptoms may worsen before improving. Anyone experiencing thoughts of suicide should seek help at once.
The FDA requires all antidepressants to carry a black box warning about the danger of suicide during the initial stages of treatment, especially in people under 25 years.
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Click here for more links and local resources.
Therapy
Doctors commonly recommend a combination of medication and therapy to treat depression.
Several forms of psychotherapy can help manage symptoms of depression and other mental health conditions.
Cognitive behavioral therapy and interpersonal therapy are the two main types.
Learn more about psychotherapy.
Natural remedies
Some natural remedies may help boost serotonin levels in the body. These include:
- practicing meditation
- having light therapy, already in use for seasonal affective disorder
- doing regular exercise
- consuming foods that are high in tryptophans
Though there is not enough evidence to confirm that these methods can boost serotonin levels, in moderation, they are unlikely to be harmful.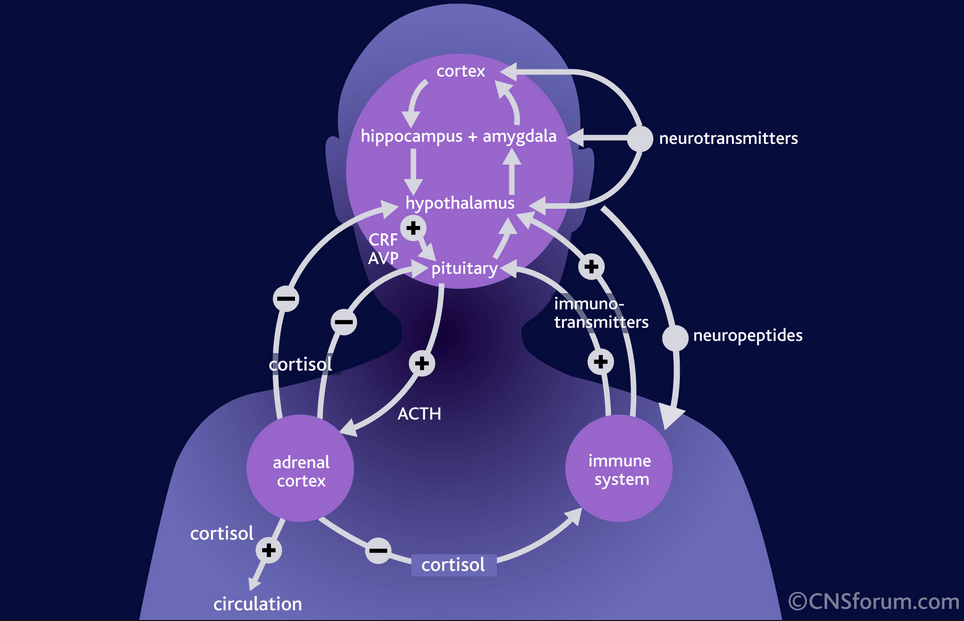
Learn more about how to boost serotonin levels.
Foods
Tryptophan is an amino acid that occurs in some foods. Some research links a higher intake of dietary tryptophan to more positive mood scores, possibly because tryptophan bolsters serotonin levels.
Foods that may contain tryptophan include:
- turkey
- eggs
- cheese
- soy products
- salmon
The body uses tryptophan to create serotonin. Eating foods that contain tryptophan may help support this process, but it does not mean that the body will necessarily absorb and use it.
There is a growing interest among scientists in the idea that gut microbiota might influence the nervous system — including behavior, mood, and thinking — through a link known as the gut-brain axis.
If so, serotonin could provide a crucial link. This suggests that diet and gut microbiota could play a role in preventing and treating conditions such as anxiety and depression.
However, more research is necessary to confirm whether this is possible.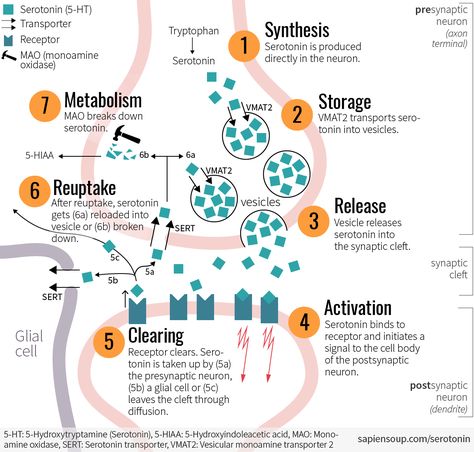
Learn more about foods that may help boost serotonin levels.
Serotonin, or the “happy” chemical, appears to play a role in various physical and psychological functions.
SSRIs are drugs that affect serotonin levels. They can help manage the symptoms of depression, although experts are still unsure exactly how it works.
Anyone considering taking a drug or supplement that affects serotonin levels should consult their doctor first to ensure it is safe for them to use.
Read the article in Spanish.
Functions, normal range, side effects, and more
Serotonin has a wide variety of functions in the human body. People sometimes call it the “happy” chemical because it contributes to well-being and happiness.
The scientific name for serotonin is 5-hydroxytryptamine (5-HT). It is a natural chemical mainly present in the brain, bowels, and blood platelets.
Serotonin is a neurotransmitter, and some also consider it a hormone. The body uses it to send messages between nerve cells.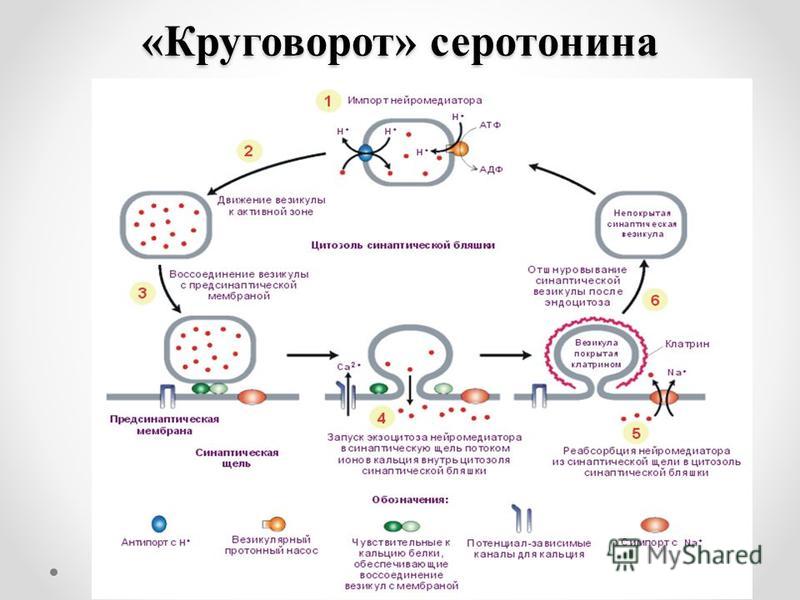
Serotonin appears to affect mood, emotions, appetite, and digestion. As the precursor for melatonin, it helps regulate sleep-wake cycles and the body clock.
Many investigations have looked at serotonin and its effects, but there is much to learn.
In this article, we look at the role of serotonin in the body, drugs that affect serotonin, side effects and symptoms of serotonin deficiency, and how to boost serotonin levels.
Serotonin results from tryptophan, a component of proteins, combining with tryptophan hydroxylase, a chemical reactor. Together, they form 5-HT, or serotonin.
The intestines and the brain produce serotonin. It is also present in blood platelets and plays a role in the central nervous system (CNS).
Serotonin occurs throughout the body and appears to influence a range of physical and psychological functions.
The substance is also present in animals, plants, and fungi. For this reason, some people have looked at food as a possible source of serotonin.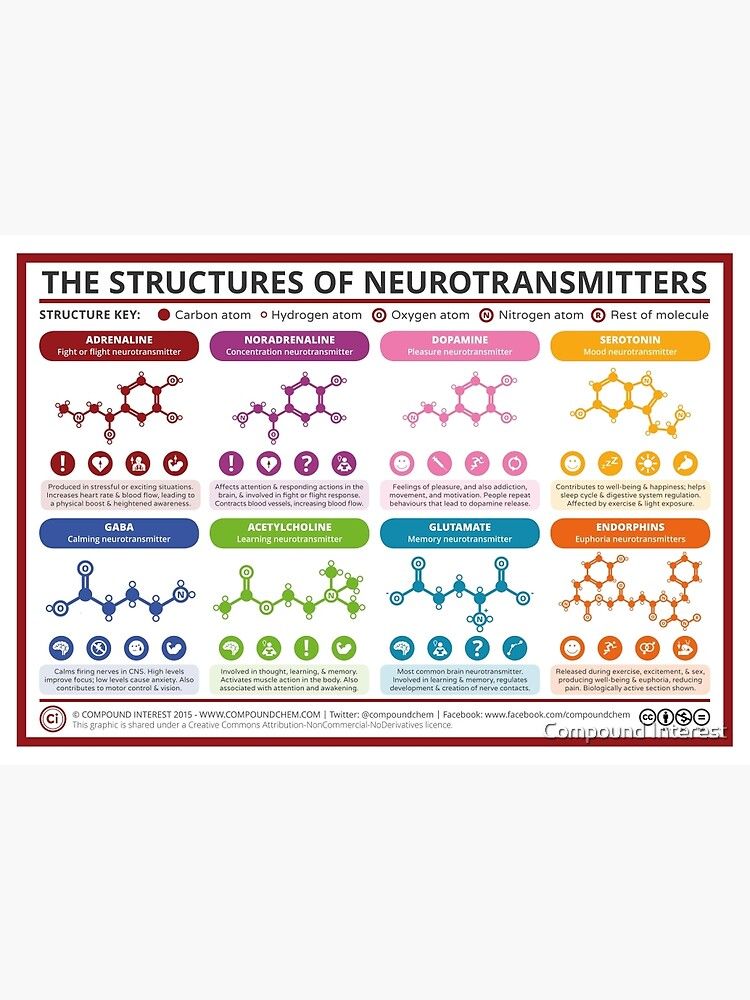
However, serotonin cannot cross the blood-brain barrier. This means that the brain must produce any serotonin it needs. Treatments for depression and other mental health issues do not supply serotonin directly but trigger reactions that can boost serotonin levels in the brain.
That said, research suggests that sources of serotonin in other areas, such as the digestive system, may work independently of serotonin in the brain. This could have implications for treating and preventing various physiological conditions, such as bone degeneration.
As a neurotransmitter, serotonin relays signals between nerve cells and regulates their intensity.
Scientists believe it plays a role in mood and the CNS and affects functions throughout the body. It may have an effect on:
- bone metabolism
- cardiovascular health
- eye health
- blood clotting
- neurological disorders
However, the relationship between serotonin and many bodily functions remains unclear.
Scientists do not precisely know what causes depression, but one theory is that it stems from an imbalance of neurotransmitters in the body.
Doctors commonly prescribe selective serotonin reuptake inhibitors (SSRIs) as antidepressants. Fluoxetine (Prozac) is one example.
Typically, the body reabsorbs a neurotransmitter after transmitting its neural impulse. SSRIs stop the body from reabsorbing serotonin, leaving higher serotonin levels to circulate.
Many people find SSRIs help relieve their symptoms, although the link between depression and serotonin remains unclear.
One problem for researchers is that, while they can measure serotonin levels in the bloodstream, they cannot measure its levels in the brain.
As a result, they do not know whether serotonin levels in the bloodstream reflect those in the brain. It is also impossible to know whether SSRIs can affect the brain.
Nevertheless, while scientists have not yet proven the serotonin theory of depression, SSRIs do appear to help many people.
Other disorders
Apart from depression, doctors may prescribe drugs that regulate serotonin levels to treat several other disorders, including:
- bipolar disorder
- post-traumatic stress disorder
- bulimia
- obsessive-compulsive disorder
- panic disorders
- migraine
As with depression, some scientists have questioned whether serotonin is the only factor affecting these conditions.
Learn more about how to stop a panic attack.
Medical professionals can measure a person’s serotonin blood levels but cannot measure serotonin levels in the brain.
Typically, treatments aim to stabilize serotonin levels between 101 and 283 nanograms per milliliter.
According to the National Institute on Drug Abuse (NIDA), low serotonin levels can lead to memory problems and a low mood.
These are symptoms of depression, although scientists have not confirmed a link between low serotonin levels and depression.
NIDA notes that when people use certain recreational drugs, such as MDMA (ecstasy), the body releases large amounts of serotonin.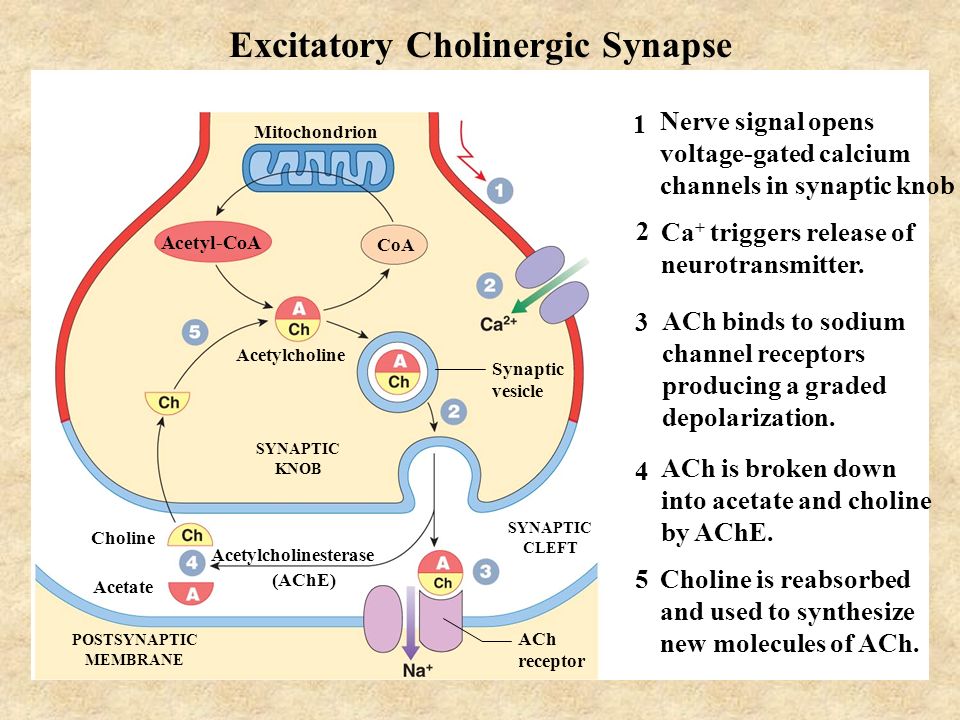
This can lead to serotonin depletion, low mood, confusion, and other symptoms lasting several days.
Animal studies have suggested that these drugs may damage the nerves that contain serotonin, with possible long lasting adverse effects.
Learn more about serotonin deficiency.
Medications, foods, and other natural remedies can alter serotonin levels.
SSRIs increase serotonin levels by preventing the body from reabsorbing serotonin neurotransmitters. Serotonin levels remain high in the brain, and this may elevate a person’s mood.
SSRIs that have approval from the Food and Drug Administration (FDA) for treating depression include:
- citalopram (Celexa)
- escitalopram (Lexapro)
- Prozac
- paroxetine (Paxil, Pexeva)
- sertraline (Zoloft)
- vilazodone (Viibryd)
Learn more about SSRIs and other antidepressants.
Adverse effects of SSRIs
SSRIs have some side effects, but these usually improve with time.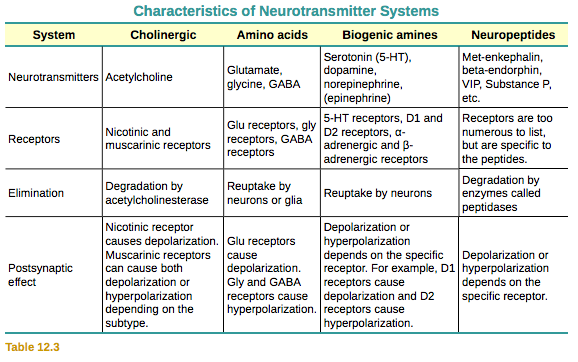
They include:
- nausea and vomiting
- restlessness and agitation
- indigestion
- diarrhea or constipation
- weight or appetite loss
- increased sweating
- dizziness
- blurred vision
- sleepiness or insomnia
- feeling shaky
- dry mouth
- headache
- low sex drive
- erectile dysfunction
- suicidal thoughts
Serotonin syndrome
Rarely, taking too much of a drug that boosts serotonin levels or combining two such drugs can lead to serotonin syndrome. This is a potentially life threatening condition that may require emergency treatment.
Learn more about serotonin syndrome.
SSRIs and suicide
A person who uses SSRIs for depression will not experience the benefits at once. At first, symptoms may worsen before improving. Anyone experiencing thoughts of suicide should seek help at once.
The FDA requires all antidepressants to carry a black box warning about the danger of suicide during the initial stages of treatment, especially in people under 25 years.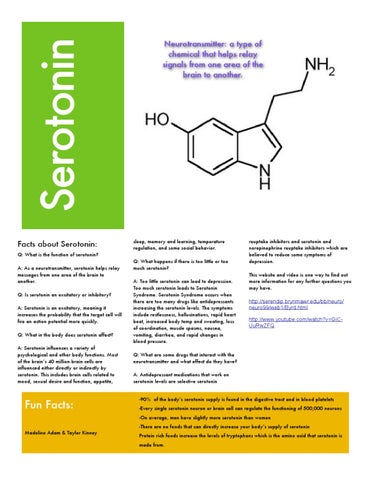
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Click here for more links and local resources.
Therapy
Doctors commonly recommend a combination of medication and therapy to treat depression.
Several forms of psychotherapy can help manage symptoms of depression and other mental health conditions.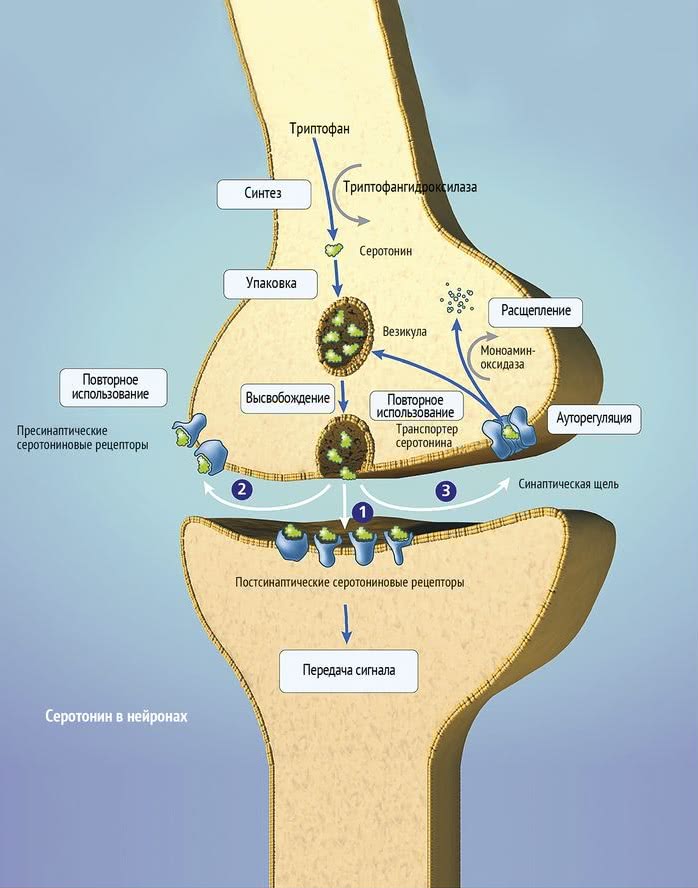
Cognitive behavioral therapy and interpersonal therapy are the two main types.
Learn more about psychotherapy.
Natural remedies
Some natural remedies may help boost serotonin levels in the body. These include:
- practicing meditation
- having light therapy, already in use for seasonal affective disorder
- doing regular exercise
- consuming foods that are high in tryptophans
Though there is not enough evidence to confirm that these methods can boost serotonin levels, in moderation, they are unlikely to be harmful.
Learn more about how to boost serotonin levels.
Foods
Tryptophan is an amino acid that occurs in some foods. Some research links a higher intake of dietary tryptophan to more positive mood scores, possibly because tryptophan bolsters serotonin levels.
Foods that may contain tryptophan include:
- turkey
- eggs
- cheese
- soy products
- salmon
The body uses tryptophan to create serotonin.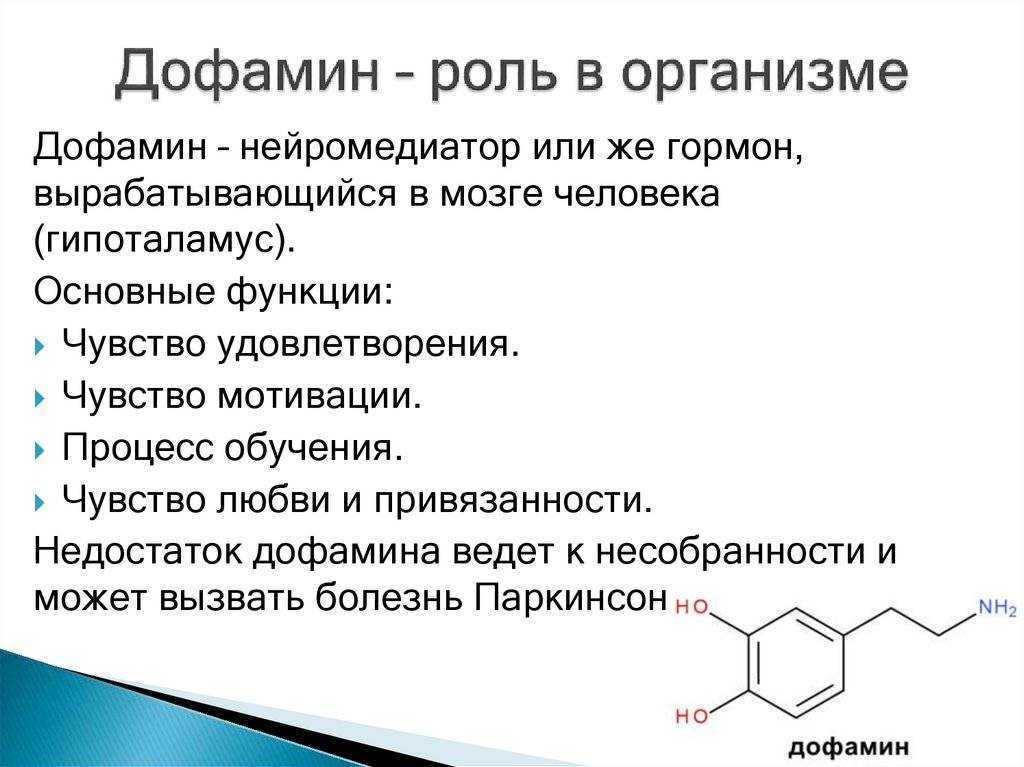 Eating foods that contain tryptophan may help support this process, but it does not mean that the body will necessarily absorb and use it.
Eating foods that contain tryptophan may help support this process, but it does not mean that the body will necessarily absorb and use it.
There is a growing interest among scientists in the idea that gut microbiota might influence the nervous system — including behavior, mood, and thinking — through a link known as the gut-brain axis.
If so, serotonin could provide a crucial link. This suggests that diet and gut microbiota could play a role in preventing and treating conditions such as anxiety and depression.
However, more research is necessary to confirm whether this is possible.
Learn more about foods that may help boost serotonin levels.
Serotonin, or the “happy” chemical, appears to play a role in various physical and psychological functions.
SSRIs are drugs that affect serotonin levels. They can help manage the symptoms of depression, although experts are still unsure exactly how it works.
Anyone considering taking a drug or supplement that affects serotonin levels should consult their doctor first to ensure it is safe for them to use.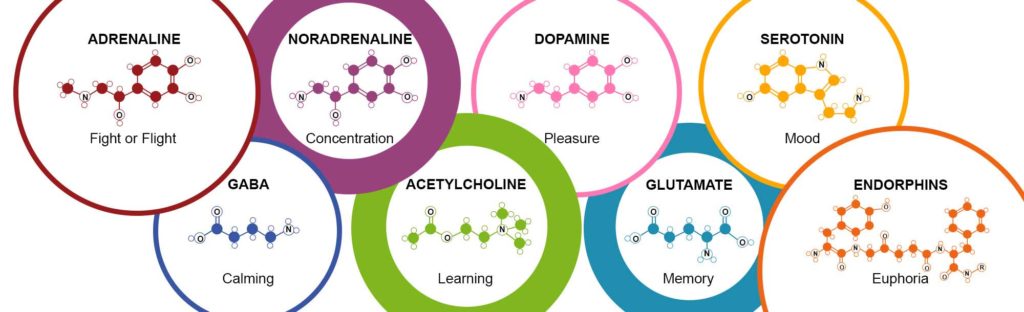
Read the article in Spanish.
The role of neurotransmitters in the regulation of energy homeostasis and the possibility of drug correction of its disorders in obesity | Dedov
Obesity is one of the most significant public health problems worldwide. WHO defines obesity as a chronic disease that is prevalent in both developed and developing countries and affects children and adults alike. The European Medical Agency defines obesity as a chronic disease caused by genetic, metabolic, behavioral and environmental factors and associated with increased morbidity and mortality. nine0003
According to the latest WHO data, between 1980 and 2013. In the world, there has been an increase in the proportion of adults with a body mass index (BMI) above 25 kg/m2, from 28.8% to 36.9% in men and from 29.8% to 38% in women.
The modern approach to the treatment of obesity is based on the recognition of the chronic nature of the disease, that is, the impossibility of its complete cure, and, consequently, the need for long-term treatment [1].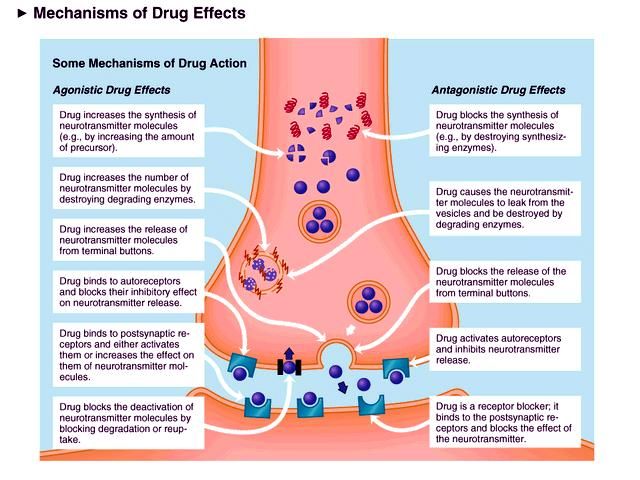 Often with obesity, mental disorders are noted, a person has an irresistible desire to consume food, and in some cases this does not bring him pleasure. Sometimes, even with a conscious attitude to diet therapy and sufficient motivation, reducing food intake and changing its composition is very difficult for patients to tolerate. In such cases, pharmacotherapy of obesity is indicated, including drugs that affect eating behavior. nine0003
Often with obesity, mental disorders are noted, a person has an irresistible desire to consume food, and in some cases this does not bring him pleasure. Sometimes, even with a conscious attitude to diet therapy and sufficient motivation, reducing food intake and changing its composition is very difficult for patients to tolerate. In such cases, pharmacotherapy of obesity is indicated, including drugs that affect eating behavior. nine0003
It should be noted that in some cases, even when pharmacotherapy of obesity is carried out with drugs that have proven their effectiveness, after stopping treatment, patients return to their eating habits and addictions. In this regard, the search for other methods of correcting eating behavior continues to be relevant. It is known that the activation of alimentary cortical zones is achieved by presenting various stimuli – visual, olfactory, and gustatory [2]. The brain's unique response to food and its associated stimuli may help explain the arousal of appetite in a given situation.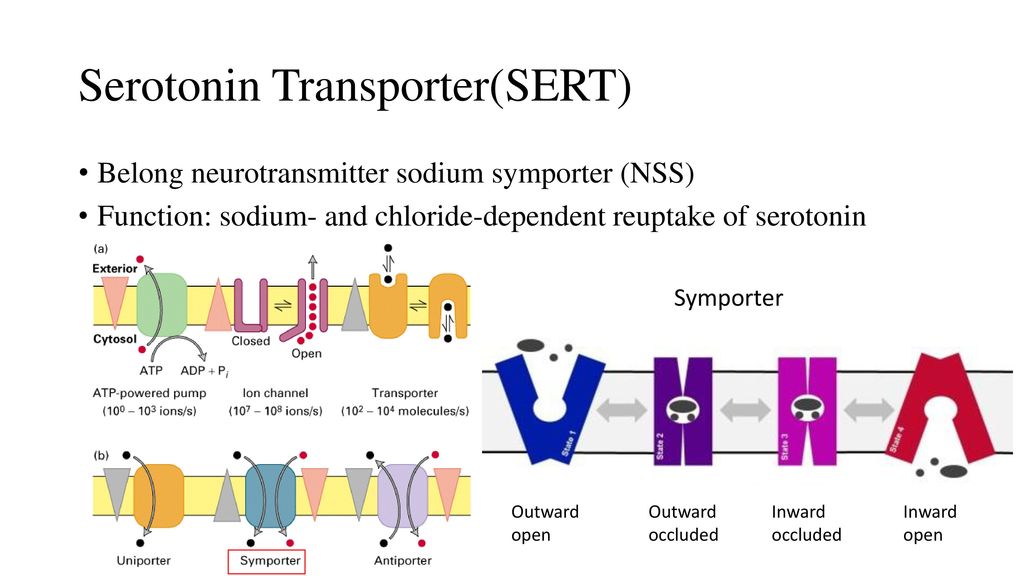 Search works aimed at identifying functionally significant areas of the cortex with subsequent individual mapping seem promising in terms of developing new methods and approaches to the treatment of obesity [3]. nine0003
Search works aimed at identifying functionally significant areas of the cortex with subsequent individual mapping seem promising in terms of developing new methods and approaches to the treatment of obesity [3]. nine0003
So, the amount of food a person eats is determined by an internal need called hunger. The type of food that the subject prefers is determined by appetite. These autoregulatory mechanisms are extremely important for an adequate supply of nutrients to the body. However, the functional organization of the hypothalamus or other nerve centers responsible for eating behavior in people with obesity differs from that in people who are not overweight [4]. These may be violations of mediator or receptor mechanisms, neuronal pathways of the hypothalamus that regulate eating behavior. This point of view is supported by observations of patients who managed to return to normal body weight on the background of dietary therapy and who usually develop a stronger feeling of hunger than ordinary people.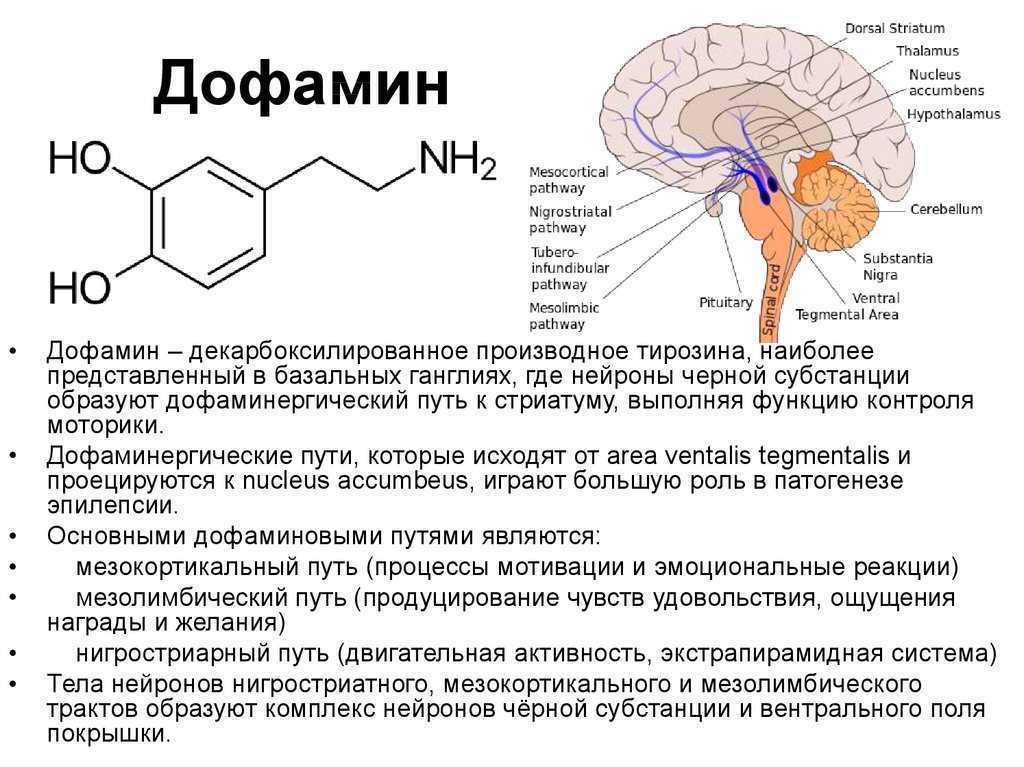 This means that the regulatory systems that control eating behavior in people with obesity are initially programmed to store nutrients at a higher level than in people with normal body weight. nine0003
This means that the regulatory systems that control eating behavior in people with obesity are initially programmed to store nutrients at a higher level than in people with normal body weight. nine0003
Energy balance is regulated by two types of neurons in the arcuate nuclei [5].
- Pro-opiomelanocortin neurons (POMC, POMC) that secrete alpha-melanocytostimulating hormone (α-MSH, alpha-MSH) and cocaine- and amphetamine-mediated transcripts (CART, CART) that reduce food intake and increase energy expenditure.
- Neurons that produce melanin-mediated protein (AGRP, or agouti-like peptide, APP) and neuropeptide Y (NPY, NPY), which increase food intake and decrease energy expenditure. nine0016
Alpha-melanocyte-stimulating hormone, secreted by POMC neurons, stimulates melanocortin receptors (MCR3 and MCR4) in the paraventricular nuclei, which then activate the neuronal pathway projecting to the nuclei of the solitary tract and increase sympathetic activity and energy expenditure.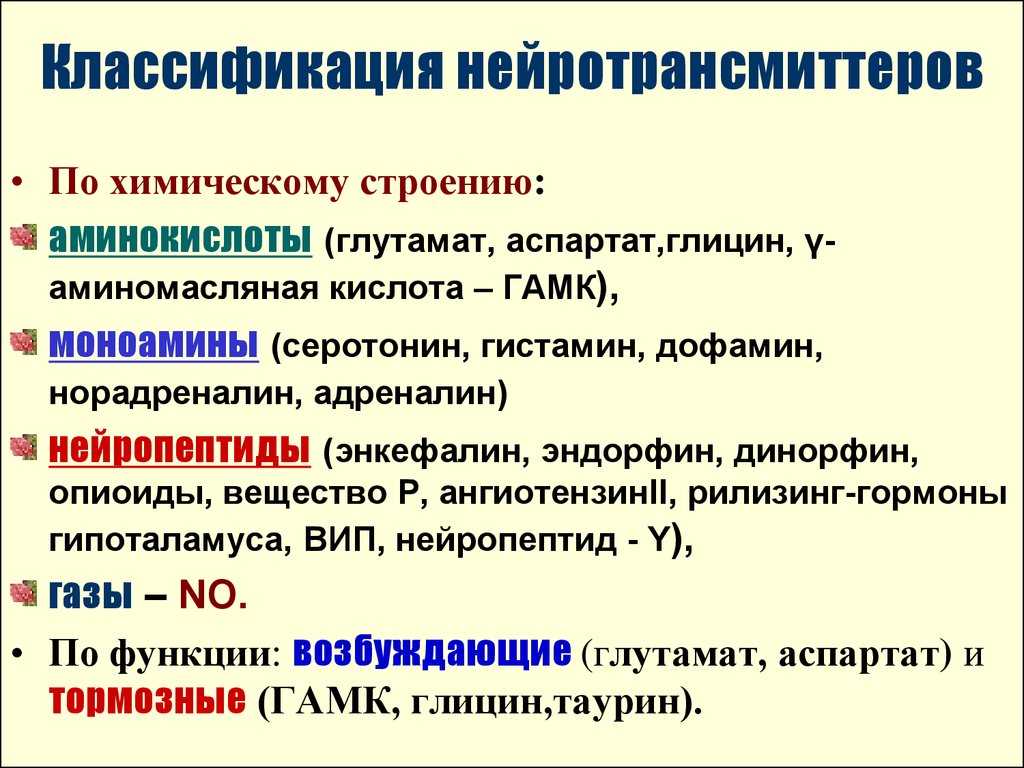 The melanin-mediated protein acts as an MCR4 antagonist [5].
The melanin-mediated protein acts as an MCR4 antagonist [5].
Insulin, leptin, and cholecystokinin (hormones that inhibit AGPG and NPY neurons and stimulate neighboring POMC and CART neurons) reduce food intake [6]. Ghrelin activates AGPG and NPY neurons and stimulates food intake. Gastric stretch receptors activate sensory afferent pathways within the vagus nerve and inhibit food intake. Peptide YY (PYY) and cholecystokinin are gastrointestinal hormones that are released during digestion and inhibit further food intake. Ghrelin secreted by the stomach, especially during fasting, stimulates appetite. Leptin, a hormone produced by fat cells in increasing amounts as they grow in size, inhibits food intake. nine0003
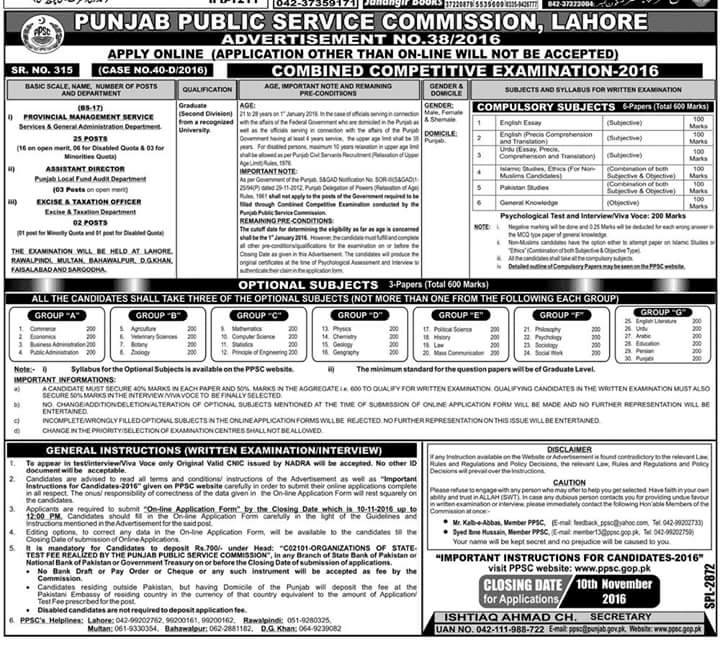
There are many chemical mediators that influence the structures of the hypothalamus, which together form the coordination center for eating behavior and satiety [7]. Some of them are summarized in table 1.
Table 1.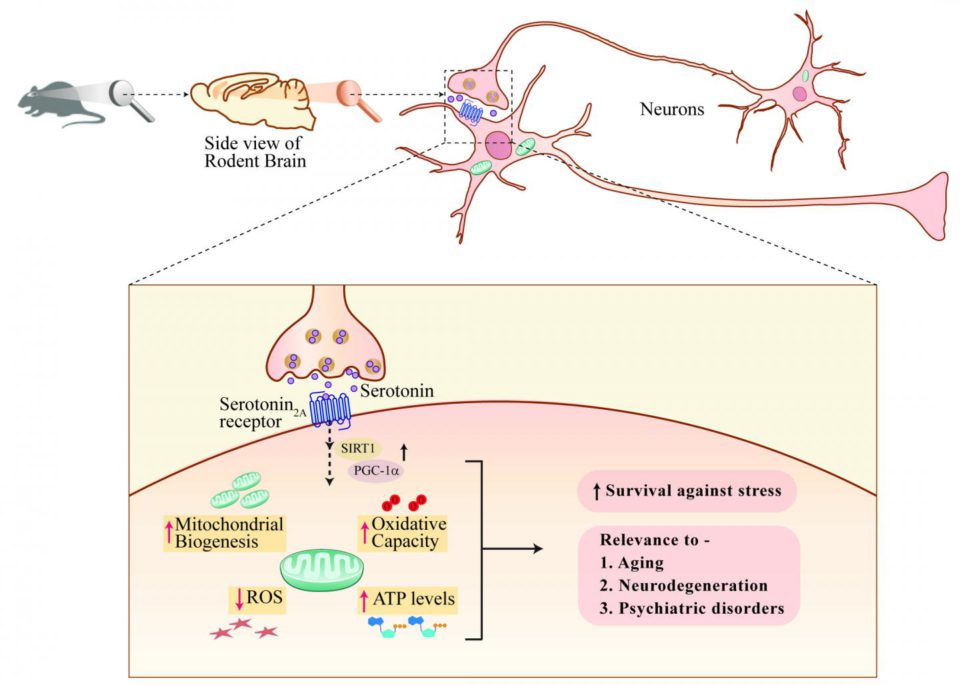 Hormones and neurotransmitters affecting the hypothalamic hunger centers and saturation Hormones and neurotransmitters affecting the hypothalamic hunger centers and saturation | |||
| anorexigenic | 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000
0003 | ||
The hypothalamus and brain stem structures (such as the arcuate nucleus, the paraventricular nucleus, the solitary tract nucleus, the dorsal motor nucleus of the vagus nerve, and others) are involved in the perception of satiety signals mediated by hormones, adipokines, neuropeptides and their metabolites and their metabolites. transformation of the received information into behavioral reactions [6]. The conversion of the peripheral signal occurs with the help of neurotransmitters, which include catecholamines (dopamine, adrenaline and norepinephrine) and indolamines (serotonin). To date, at least fifty chemical compounds are known that are able to function as synaptic mediators.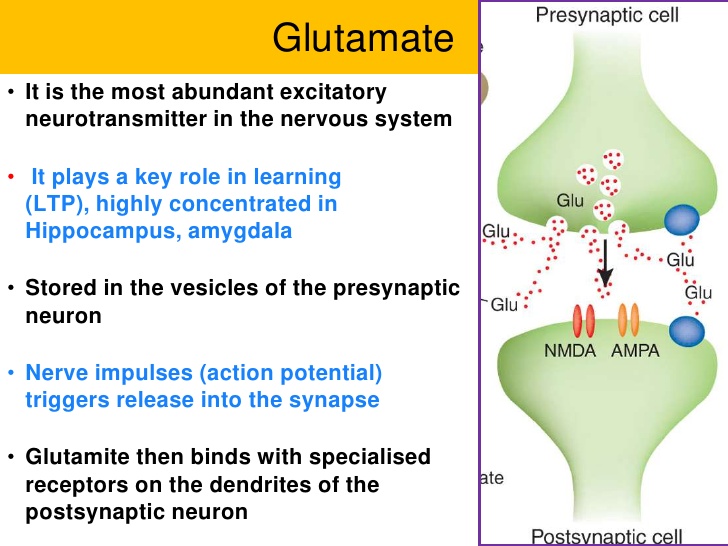 nine0003
nine0003
Dopamine, norepinephrine and adrenaline are consecutive links in the chain of transformations of the amino acid tyrosine. Although dopaminergic neurons make up 1-2% of the total neuron population, their role in the regulation of eating behavior is extremely important. There are 5 known types of dopamine receptors, which are divided into 2 subtypes depending on the effect on adenylate cyclase - D1-like (D1, D5) - activating and D2-like (D2, D3, D4) - inhibiting it. At present, the role of D1-like receptors in the regulation of eating behavior has not been proven. The role of D2-like receptors is determined not only by their number, but also by the location [8, 9].
Norepinephrine realizes its action in the cells of the paraventricular and ventromedial nuclei of the hypothalamus. The effect on α1-, β2- and β3-adrenergic receptors leads to a decrease in appetite, and stimulation of α2 receptors, on the contrary, stimulates appetite.
Norepinephrine and dopamine are neurohumoral mediators at the endings of postganglionic nerve fibers and in some parts of the brain.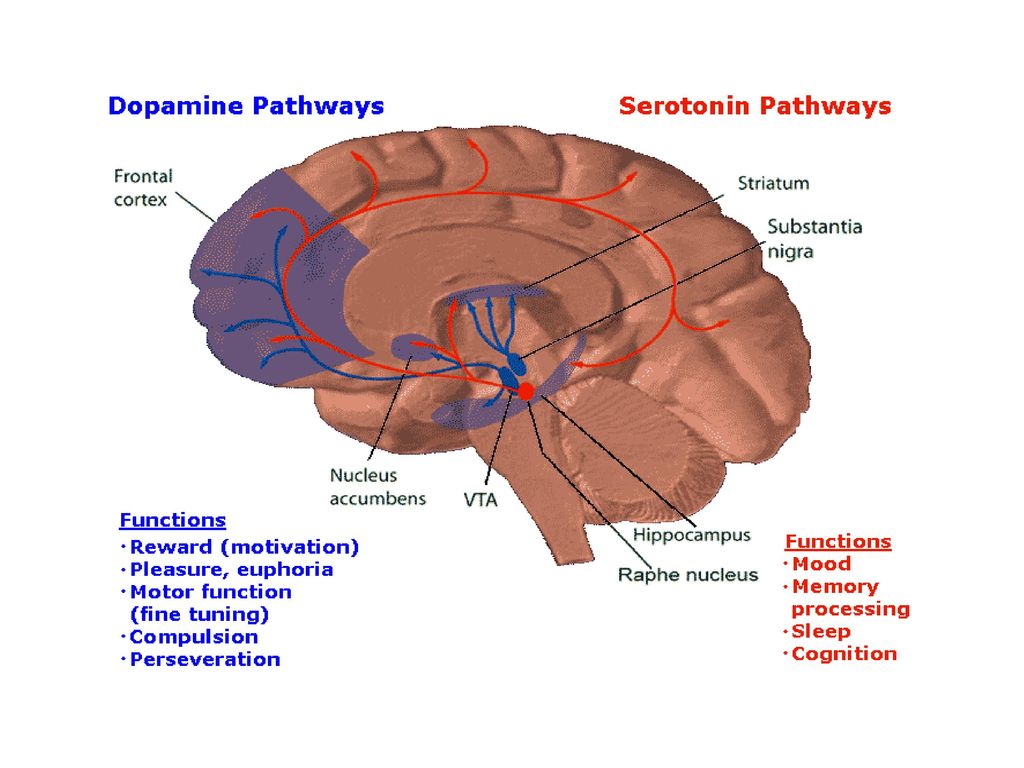 The highest concentrations of these amines are found in neuronal endings, where they are synthesized and stored in vesicles in the dilated terminal region. Three catecholamines are synthesized from phenylalanine: norepinephrine, adrenaline and dopamine. Enzymes involved in the biosynthesis of norepinephrine and adrenaline do not have high specificity. Thus, DOPA decarboxylase catalyzes the conversion of 5-hydroxytryptophan to 5-GTA and histidine to histamine. Adrenaline, released into the synaptic cleft, is partially destroyed, and part of it is again captured by the end of the sympathetic neuron. nine0003
The highest concentrations of these amines are found in neuronal endings, where they are synthesized and stored in vesicles in the dilated terminal region. Three catecholamines are synthesized from phenylalanine: norepinephrine, adrenaline and dopamine. Enzymes involved in the biosynthesis of norepinephrine and adrenaline do not have high specificity. Thus, DOPA decarboxylase catalyzes the conversion of 5-hydroxytryptophan to 5-GTA and histidine to histamine. Adrenaline, released into the synaptic cleft, is partially destroyed, and part of it is again captured by the end of the sympathetic neuron. nine0003
One of the most important transmitters involved in the regulation of energy homeostasis, which consists in the stimulation of some and inhibition of other neurons of the hypothalamus by peripheral hormones, is serotonin. Serotonin (5-hydroxytryptamine) 5-GTA was isolated in 1948. It is a compound that has the function of a hormone and a neurotransmitter in the human body. Serotonin has a wide variety of properties, found in tissues, mast cells and platelets.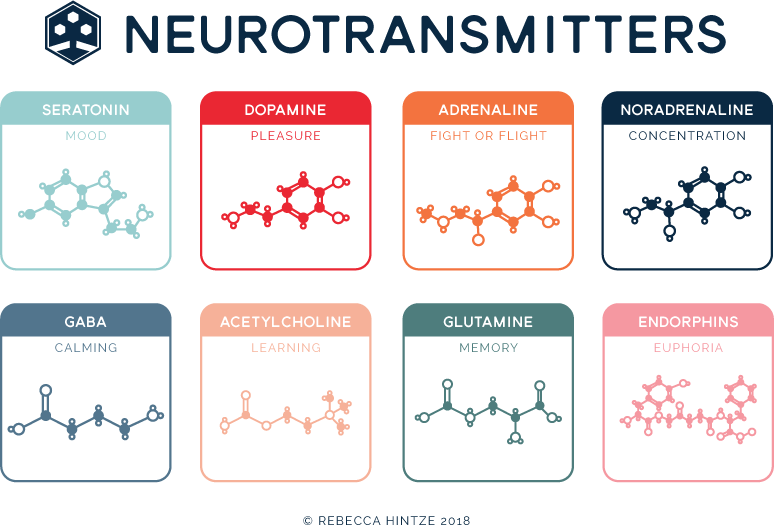 Its highest concentration is observed in the pineal gland and ranges from 60 to 180 micrograms per gram, where it serves as a precursor for melatonin biosynthesis. Serotonin is synthesized from tryptophan, the hydroxylation of which leads to the formation of 5-hydroxytryptophan (5-GTP). This reaction is catalyzed by 5-GTP-hydroxylase. Decarboxylation of 5 GTP by the enzyme 5 GTP decarboxylase is accompanied by the formation of 5 hydroxytryptamine (serotonin, 5 HT) [10]. This enzyme also decarboxylates histidine and DOPA. In the CNS and gastrointestinal tract, 5-GTA is deposited in cellular cytoplasmic granules, similar to chromaffin granules, in which catecholamines are deposited. Most serotonergic neurons are located in the hypothalamus and limbic system of the brain. Most of them are in the so-called "raphe nuclei" - areas of the brain stem. This is where the synthesis of serotonin occurs in the brain. Exogenous serotonin does not penetrate the blood-brain barrier [11], thus, the concentration of serotonin in the brain does not depend on its synthesis and secretion in the gastrointestinal tract, and the determination of the concentration of serotonin in the blood does not provide information about its concentration in the CNS.
Its highest concentration is observed in the pineal gland and ranges from 60 to 180 micrograms per gram, where it serves as a precursor for melatonin biosynthesis. Serotonin is synthesized from tryptophan, the hydroxylation of which leads to the formation of 5-hydroxytryptophan (5-GTP). This reaction is catalyzed by 5-GTP-hydroxylase. Decarboxylation of 5 GTP by the enzyme 5 GTP decarboxylase is accompanied by the formation of 5 hydroxytryptamine (serotonin, 5 HT) [10]. This enzyme also decarboxylates histidine and DOPA. In the CNS and gastrointestinal tract, 5-GTA is deposited in cellular cytoplasmic granules, similar to chromaffin granules, in which catecholamines are deposited. Most serotonergic neurons are located in the hypothalamus and limbic system of the brain. Most of them are in the so-called "raphe nuclei" - areas of the brain stem. This is where the synthesis of serotonin occurs in the brain. Exogenous serotonin does not penetrate the blood-brain barrier [11], thus, the concentration of serotonin in the brain does not depend on its synthesis and secretion in the gastrointestinal tract, and the determination of the concentration of serotonin in the blood does not provide information about its concentration in the CNS. However, there is no permeability barrier for the serotonin precursor 5-GTP. nine0003
However, there is no permeability barrier for the serotonin precursor 5-GTP. nine0003
The effects of serotonin are realized through its receptors. 14 types of serotonin receptors have been identified: 5-HT1A-F, 5-HT2A-C, 5HT3-7 [5]. However, only a part of the receptors has a role in the pathogenesis of obesity: 5-HT2C, 5-HT1A, and 5-HT2B [10, 12], as well as the still poorly studied 5-HT6 [13]. The point of application of serotonin is the melanocortin system. In the arcuate nuclei of the hypothalamus, serotonin activates POMC/CART neurons, which leads to an increase in the production of α-MSH and, accordingly, a decrease in food intake, while interaction with ACP neurons prevents the suppression of α-MSH secretion [5]. Serotonin produced in the gastrointestinal tract also contributes to energy regulation by stimulating gastrointestinal motility and the secretion of hydrochloric acid in the stomach and bicarbonate in the duodenum, and also implements vasoactive properties in the mucosa and submucosa and determines taste sensations.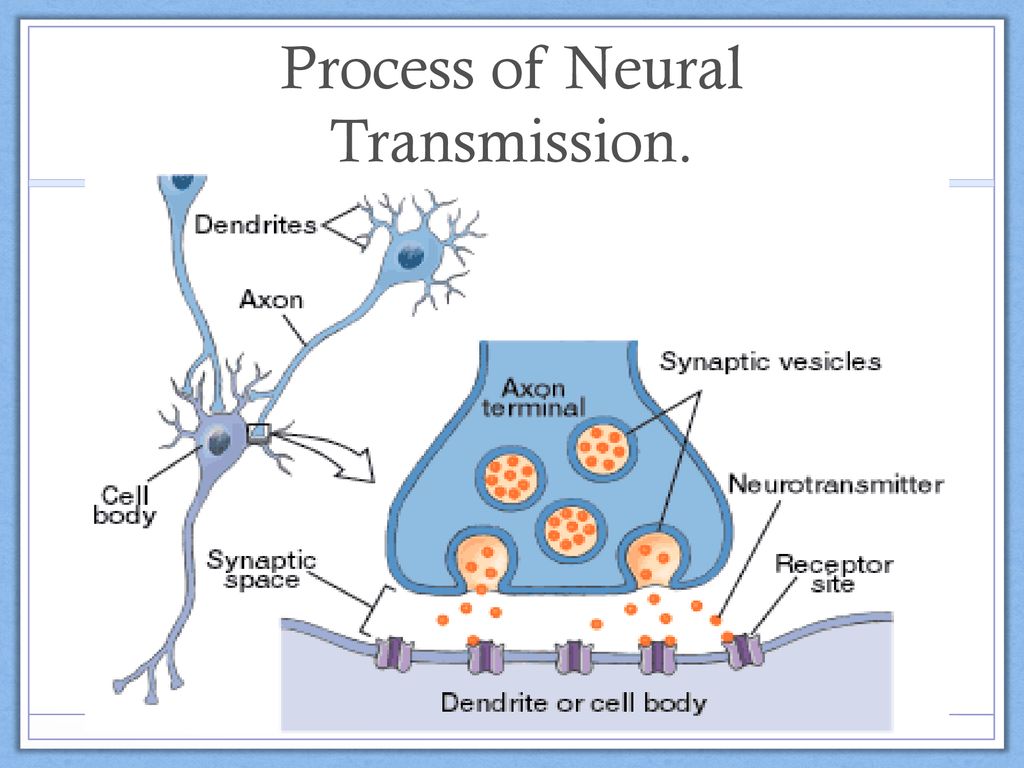 Serotonin constricts blood vessels, incl. renal, meningeal and pulmonary arteries. It also constricts veins and venules, but dilates skeletal muscle blood vessels, coronary vessels, and skin capillaries, provoking peripheral blood deposition. 5-GTA has a direct weak positive inotropic and chronotropic effect on the myocardium, but this is practically not manifested clinically in humans, since serotonin also causes reflex bradycardia. Serotonin affects blood pressure, this effect has the form of a three-phase process: first, there is a short-term decrease in pressure due to increased activity of the vagus nerve caused by stimulation of the chemoreceptors of the coronary vessels and carotid sinus, followed by a rapid increase in blood pressure due to peripheral vasoconstriction. Later, an increase in blood pressure is replaced by persistent hypotension due to the expansion of the blood vessels of the skeletal muscles. Serotonin stimulates all smooth muscle structures. nine0003
Serotonin constricts blood vessels, incl. renal, meningeal and pulmonary arteries. It also constricts veins and venules, but dilates skeletal muscle blood vessels, coronary vessels, and skin capillaries, provoking peripheral blood deposition. 5-GTA has a direct weak positive inotropic and chronotropic effect on the myocardium, but this is practically not manifested clinically in humans, since serotonin also causes reflex bradycardia. Serotonin affects blood pressure, this effect has the form of a three-phase process: first, there is a short-term decrease in pressure due to increased activity of the vagus nerve caused by stimulation of the chemoreceptors of the coronary vessels and carotid sinus, followed by a rapid increase in blood pressure due to peripheral vasoconstriction. Later, an increase in blood pressure is replaced by persistent hypotension due to the expansion of the blood vessels of the skeletal muscles. Serotonin stimulates all smooth muscle structures. nine0003
Serotonin is found in the nervous system.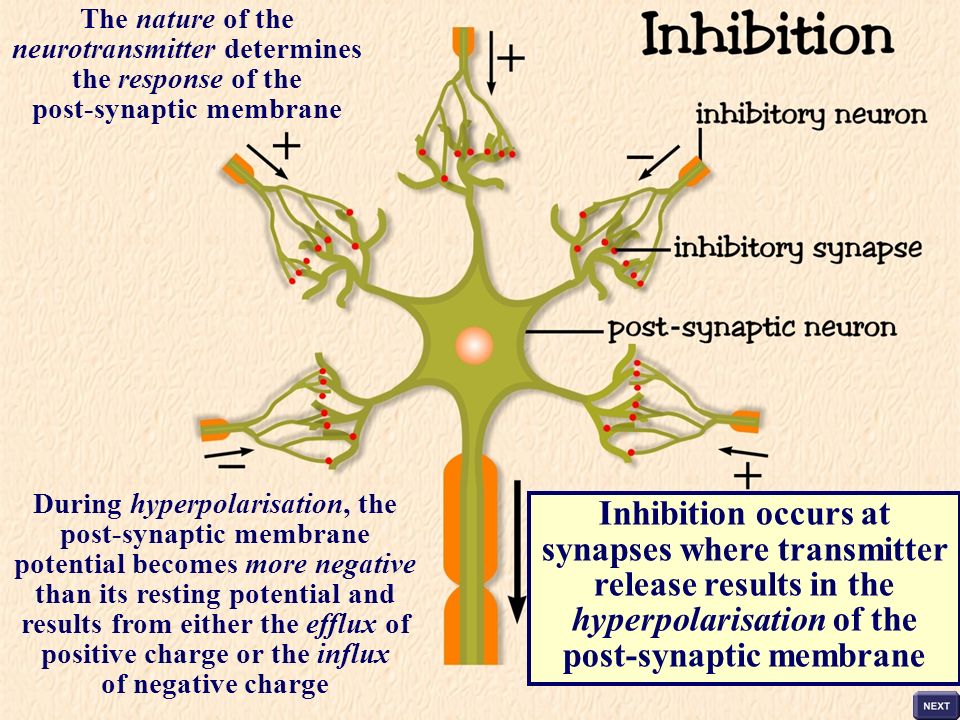 Large amounts of 5-GTA are found in the midbrain, limbic system, hypothalamus, caudate nucleus, and pituitary gland. 5-GTA is a chemical mediator released by tryptaminergic neurons, which are widely distributed in the brain. One of the important functions of neurons, where tryptamine serves as a mediator, is the inhibition of increased reactivity to various stimuli; alteration of tryptaminergic functions may cause disturbances in sleep, mood, pain perception, sexual and eating behavior, motor activity and perceptions [14]. Such neurons are also involved in the regulation of body temperature, control of endocrine functions and extrapyramidal activity. nine0003
Large amounts of 5-GTA are found in the midbrain, limbic system, hypothalamus, caudate nucleus, and pituitary gland. 5-GTA is a chemical mediator released by tryptaminergic neurons, which are widely distributed in the brain. One of the important functions of neurons, where tryptamine serves as a mediator, is the inhibition of increased reactivity to various stimuli; alteration of tryptaminergic functions may cause disturbances in sleep, mood, pain perception, sexual and eating behavior, motor activity and perceptions [14]. Such neurons are also involved in the regulation of body temperature, control of endocrine functions and extrapyramidal activity. nine0003
Disruption of 5-GTA metabolism in the brain is one of the suspected causes of certain psychiatric disorders, including eating disorders.
For the production of serotonin in the body, it is necessary:
- dietary intake of tryptophan, an amino acid necessary for the direct synthesis of serotonin in synapses [11];
- intake of glucose, stimulation of insulin release into the blood, stimulation of catabolism in tissues and, as a result, an increase in the level of tryptophan in the blood.
 nine0016
nine0016
Bulimia and cravings for carbohydrate-rich foods may be directly related to these facts. Serotonin can cause a subjective feeling of satiety, and when food enters the body, including those containing tryptophan, the production of serotonin increases, which improves mood. The brain quickly catches the connection between these phenomena - and in case of depression (serotonin starvation), it immediately “requires” additional intake of food with tryptophan or glucose. Foods richest in tryptophan are almost entirely carbohydrates, such as bread, bananas, chocolate, or pure carbohydrates such as sugar or fructose. nine0003
Serotonin is metabolized in the body by monoamine oxidase-A (MAO-A) to 5-hydroxyindoleacetic acid, which is then excreted in the urine. The first antidepressants were monoamine oxidase inhibitors, which also inhibit the destruction of norepinephrine by monoamine oxidase. However, due to the large number of side effects caused by the broad biological action of monoamine oxidase, "serotonin reuptake inhibitors" are currently used as antidepressants.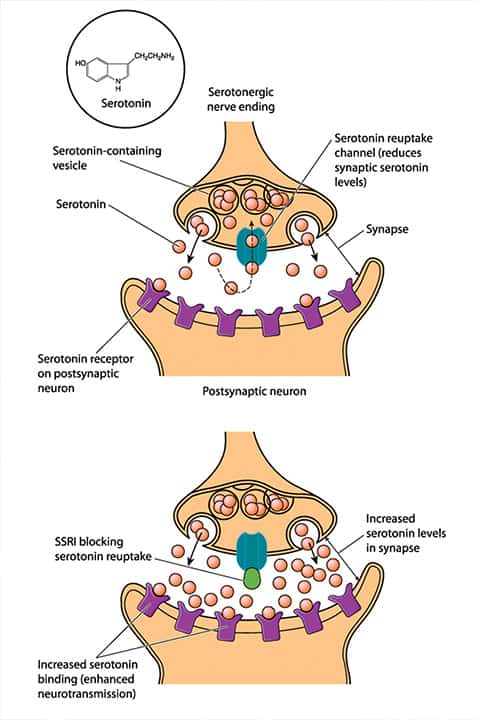 These substances also impede the reuptake of serotonin in the synapses, thereby increasing its concentration in the blood. It is noted that in addition to the antidepressant action, they can work as anorectics [14]. In particular, inhibition of serotonin reuptake leads to the fact that the effect of serotonin, which causes depolarization of POMC/CART neurons, where 5-HT2C receptors are concentrated, an increase in α-MSH production, and activation of MK4,3 receptors, is realized in a decrease in the amount of food intake. nine0003
These substances also impede the reuptake of serotonin in the synapses, thereby increasing its concentration in the blood. It is noted that in addition to the antidepressant action, they can work as anorectics [14]. In particular, inhibition of serotonin reuptake leads to the fact that the effect of serotonin, which causes depolarization of POMC/CART neurons, where 5-HT2C receptors are concentrated, an increase in α-MSH production, and activation of MK4,3 receptors, is realized in a decrease in the amount of food intake. nine0003
A synapse is a structure formed by the close contact of a neuron with a neuron or with an effector cell. It is shaped to transmit excitation or inhibition. The synapse between the preganglionic and postganglionic fibers is called the ganglion, and between the postganglionic fiber and the receptor, the neuroeffector junction. The synapse is a physiological, not anatomical extension of a neuron. The passage of an impulse through a synapse is called the process of transmission, while the movement of an impulse along a fiber, preganglionic or postganglionic, is called the process of conducting an impulse. The space between the presynaptic and postsynaptic fibers or between the nerve ending and the receptor is called the synaptic cleft. In the area of the ganglion, it is limited by the pre- and postsynaptic membrane, and in the area of the neuroeffector junction, by the surface membrane of the nerve ending on one side and the receptor zone on the other. The terminal parts of the pre- and postganglionic axons contain oval vesicles - synaptic vesicles that tend to cluster near the synaptic cleft. When a nerve impulse is transmitted, neurotransmitters from synaptic vesicles enter the synaptic cleft, after which they bind to receptors on the postsynaptic membrane. They are then removed from the synaptic cleft, either degraded by enzymes or reuptake by the corresponding receptors on the presynaptic membrane. nine0003
The space between the presynaptic and postsynaptic fibers or between the nerve ending and the receptor is called the synaptic cleft. In the area of the ganglion, it is limited by the pre- and postsynaptic membrane, and in the area of the neuroeffector junction, by the surface membrane of the nerve ending on one side and the receptor zone on the other. The terminal parts of the pre- and postganglionic axons contain oval vesicles - synaptic vesicles that tend to cluster near the synaptic cleft. When a nerve impulse is transmitted, neurotransmitters from synaptic vesicles enter the synaptic cleft, after which they bind to receptors on the postsynaptic membrane. They are then removed from the synaptic cleft, either degraded by enzymes or reuptake by the corresponding receptors on the presynaptic membrane. nine0003
The action of drugs associated with mediators can be classified as presynaptic and postsynaptic [15].
Many centrally acting drugs alter the response to 5-GTA or its storage, synthesis, uptake, release, or catabolism.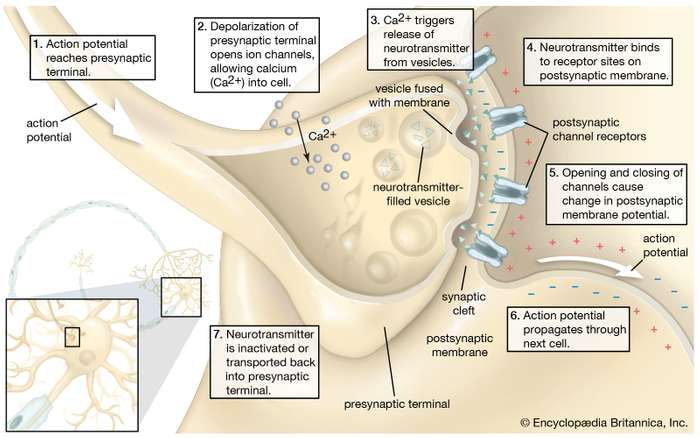 Since many studies have shown the decisive role of serotonergic deficiency as a cause of eating disorders, the use of serotonin reuptake inhibitors is relevant in the treatment of obesity [16, 17]. Indeed, obesity is characterized by lower cerebral levels of serotonin, which leads to a delayed signal to stop eating (or not) due to insufficient receptor stimulation. A decrease in the level of serotonin compensatory increases the density of receptors, leading to the development of disorders resembling depressive ones. nine0003
Since many studies have shown the decisive role of serotonergic deficiency as a cause of eating disorders, the use of serotonin reuptake inhibitors is relevant in the treatment of obesity [16, 17]. Indeed, obesity is characterized by lower cerebral levels of serotonin, which leads to a delayed signal to stop eating (or not) due to insufficient receptor stimulation. A decrease in the level of serotonin compensatory increases the density of receptors, leading to the development of disorders resembling depressive ones. nine0003
Synaptic cleft serotonin reuptake inhibitors bind competitively to 5-GTA reuptake receptors. As a result, the concentration of serotonin in the synaptic cleft increases, which enhances the transmission of the nerve impulse. This effect underlies the action of drugs that increase mental activity, relieve emotional stress and model eating behavior.
Sibutramine
Sibutramine is a neurotransmitter reuptake inhibitor: serotonin (53%), norepinephrine (54%) and dopamine (16%) [18], resulting in an increase in the concentration of these mediators in the synaptic space.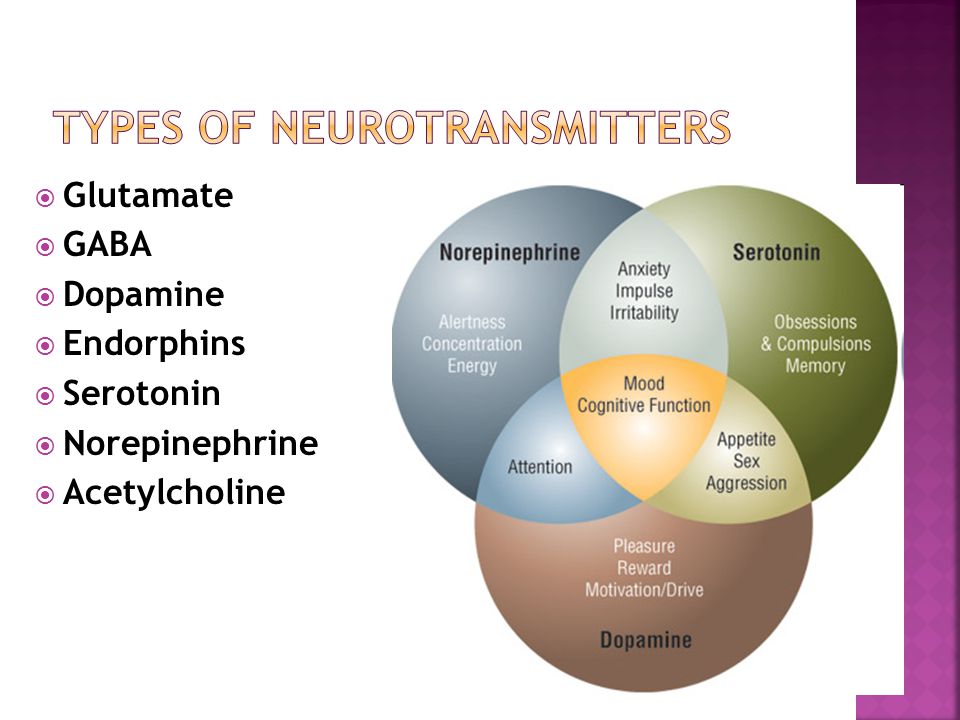 Due to this dual mechanism of action, the drug affects both sides of the energy balance, i.e., increasing and prolonging the feeling of satiety, reduces energy intake by reducing the amount of food consumed and increases its consumption due to increased thermogenesis. nine0003
Due to this dual mechanism of action, the drug affects both sides of the energy balance, i.e., increasing and prolonging the feeling of satiety, reduces energy intake by reducing the amount of food consumed and increases its consumption due to increased thermogenesis. nine0003
Sibutramine forms active metabolites in the body (primary and secondary amines), which are significantly superior to sibutramine in their ability to inhibit the reuptake of serotonin and norepinephrine. Sibutramine differs in mechanism of action from other centrally acting drugs in that it does not affect the dopaminergic system and therefore does not cause addiction and drug dependence.
The main side effects of the drug - dry mouth, constipation, lack of appetite, insomnia, increased blood pressure, increased heart rate - are mild and transient. Sibutramine is not prescribed during pregnancy and lactation, with severe renal and hepatic insufficiency, mental illness, hypertension, coronary artery disease and cardiac arrhythmias, heart failure, pheochromocytoma, glaucoma, as well as simultaneously with monoamine oxidase inhibitors and psychotropic drugs.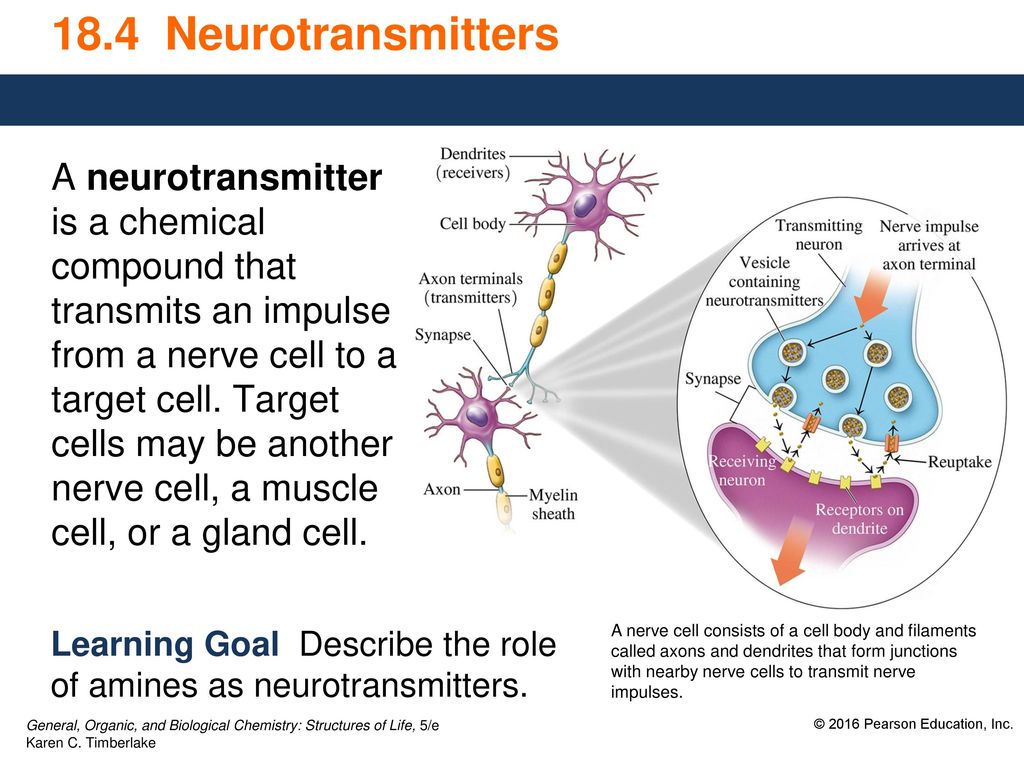 The initial dose of sibutramine (10 mg) is used once in the morning. If in 4 weeks the weight loss is less than 2 kg, then with good tolerability of the drug, the dose can be increased to 15 mg. The drug is discontinued if, after 3 months of treatment, body weight has decreased by less than 5%. Duration of taking the drug is not more than 12 months. Treatment with sibutramine helps patients in the formation of proper eating habits. At 1998, the drug was registered in the US, and a year later in Europe, as a drug for the treatment of obesity.
The initial dose of sibutramine (10 mg) is used once in the morning. If in 4 weeks the weight loss is less than 2 kg, then with good tolerability of the drug, the dose can be increased to 15 mg. The drug is discontinued if, after 3 months of treatment, body weight has decreased by less than 5%. Duration of taking the drug is not more than 12 months. Treatment with sibutramine helps patients in the formation of proper eating habits. At 1998, the drug was registered in the US, and a year later in Europe, as a drug for the treatment of obesity.
Meta-analysis of obesity treatment, which included 10 double-blind, placebo-controlled trials (n=2623) over 1 year of treatment, showed 4.2 kg more weight loss in patients treated with sibutramine (95% CI 3.6 to 4.7 kg) than patients who received placebo, which increased the number of people who lost weight without medication by 5% and 10% of baseline weight, by 32% and 18%, respectively [19]. Among patients treated with sibutramine, there were 10-30% more people who successfully maintained the achieved result (success was considered to be 80-100% of weight loss).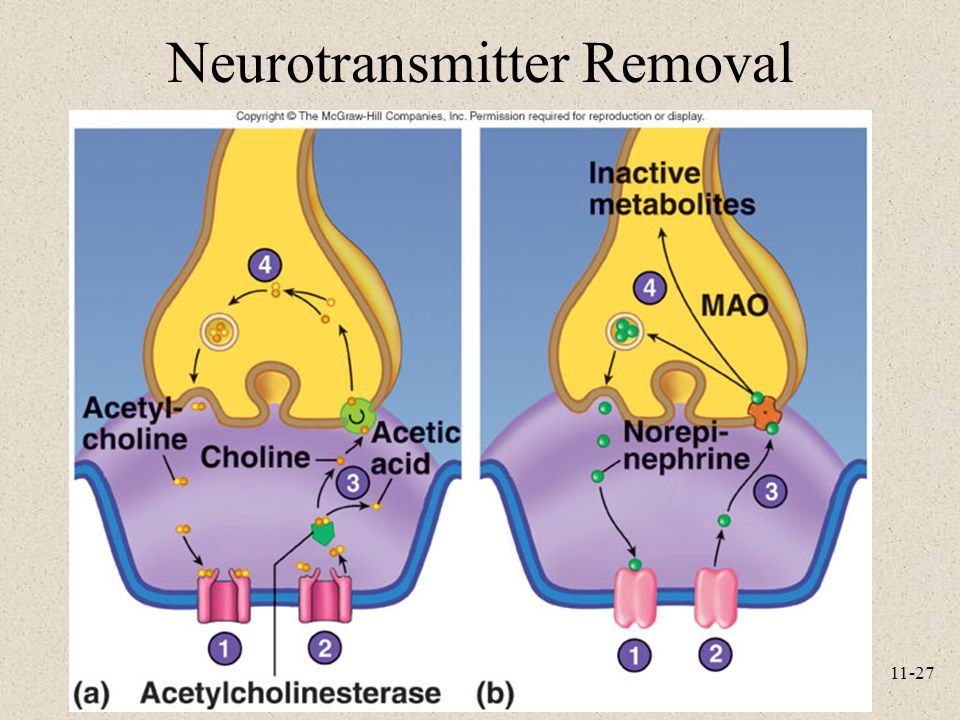 Similar results were obtained according to other meta-analyses [20]. Among the metabolic effects of sibutramine, there was a significant decrease in BMI, waist circumference, a decrease in TG levels, an increase in HDL levels, and a slight decrease in glycated hemoglobin and fasting glycemia in patients with diabetes mellitus and obesity. The use of sibutramine led to an increase in systolic and diastolic blood pressure by 1–3 mm Hg. and an increase in heart rate by 4–5 beats per minute [18]. The most common side effects of sibutramine, such as dry mouth, anorexia, constipation, headache, and insomnia, are generally associated with sympathomimetic properties, with adverse events ranging from 7% to 20%. nine0003
Similar results were obtained according to other meta-analyses [20]. Among the metabolic effects of sibutramine, there was a significant decrease in BMI, waist circumference, a decrease in TG levels, an increase in HDL levels, and a slight decrease in glycated hemoglobin and fasting glycemia in patients with diabetes mellitus and obesity. The use of sibutramine led to an increase in systolic and diastolic blood pressure by 1–3 mm Hg. and an increase in heart rate by 4–5 beats per minute [18]. The most common side effects of sibutramine, such as dry mouth, anorexia, constipation, headache, and insomnia, are generally associated with sympathomimetic properties, with adverse events ranging from 7% to 20%. nine0003
The SCOUT study (Sibutramine Cardiovascular OUTcomes) was designed to evaluate the outcome of weight loss during sibutramine pharmacotherapy in patients at high cardiovascular risk. Of the 10,742 patients included in the preliminary period of the study, the vast majority (91. 9%) had contraindications to prescribing the drug, provided for by the current instruction: cardiovascular diseases and blood pressure above 145/90 mm Hg. Art. A 6-week treatment period demonstrated good tolerability and efficacy in patients with high cardiovascular risk [29]. SCOUT was then continued as a randomized, double-blind, placebo-controlled study that included 9804 men and women aged ≥55 years with a BMI ≥27 kg/m2 and ≤45 kg/m2 or ≥25 kg/m2 and <27 kg /m2 with waist circumference ≥102/≥88 cm (men/women, respectively) [21]. All patients had a history of cardiovascular disease such as ischemic heart disease, stroke or peripheral vascular disease and/or type 2 diabetes mellitus with at least one additional cardiovascular risk factor (hypertension, dyslipidaemia, smoking or diabetic nephropathy) . The exclusion criteria were symptoms of heart failure above functional class II (classification of the New York Heart Association), BP>160/100 mm Hg. Art., pulse >100 beats per minute, planned heart or coronary artery surgery, and recent weight loss.
9%) had contraindications to prescribing the drug, provided for by the current instruction: cardiovascular diseases and blood pressure above 145/90 mm Hg. Art. A 6-week treatment period demonstrated good tolerability and efficacy in patients with high cardiovascular risk [29]. SCOUT was then continued as a randomized, double-blind, placebo-controlled study that included 9804 men and women aged ≥55 years with a BMI ≥27 kg/m2 and ≤45 kg/m2 or ≥25 kg/m2 and <27 kg /m2 with waist circumference ≥102/≥88 cm (men/women, respectively) [21]. All patients had a history of cardiovascular disease such as ischemic heart disease, stroke or peripheral vascular disease and/or type 2 diabetes mellitus with at least one additional cardiovascular risk factor (hypertension, dyslipidaemia, smoking or diabetic nephropathy) . The exclusion criteria were symptoms of heart failure above functional class II (classification of the New York Heart Association), BP>160/100 mm Hg. Art., pulse >100 beats per minute, planned heart or coronary artery surgery, and recent weight loss. The average duration of treatment was 3.4 years. According to the results of the study, the average weight loss during the lead-in 6-week period (sibutramine at a dose of 10 mg) was 2.6 kg; after randomization, patients treated with sibutramine continued to lose weight further (-1.7 kg per year), while patients in the placebo group noted a reverse weight gain (0.7 kg per year). During the introductory period, there was a decrease in blood pressure - an average of 4.7 mm Hg. systolic and 1.7 mm Hg. diastolic. After randomization, the mean BP values remained below baseline in both observation groups, but in the sibutramine group they were statistically significantly higher than in the placebo group - the mean differences in the groups ranged from -0.3 to 1.2 mmHg. SBP and 0.6 to 1.4 mm Hg. DBP. The pulse rate was also higher in the sibutramine group, 3.7 and 2.2 beats per minute, respectively. There was a 16% increase in the risk of primary cardiovascular events in the sibutramine group, and the number of all cases was 11.
The average duration of treatment was 3.4 years. According to the results of the study, the average weight loss during the lead-in 6-week period (sibutramine at a dose of 10 mg) was 2.6 kg; after randomization, patients treated with sibutramine continued to lose weight further (-1.7 kg per year), while patients in the placebo group noted a reverse weight gain (0.7 kg per year). During the introductory period, there was a decrease in blood pressure - an average of 4.7 mm Hg. systolic and 1.7 mm Hg. diastolic. After randomization, the mean BP values remained below baseline in both observation groups, but in the sibutramine group they were statistically significantly higher than in the placebo group - the mean differences in the groups ranged from -0.3 to 1.2 mmHg. SBP and 0.6 to 1.4 mm Hg. DBP. The pulse rate was also higher in the sibutramine group, 3.7 and 2.2 beats per minute, respectively. There was a 16% increase in the risk of primary cardiovascular events in the sibutramine group, and the number of all cases was 11.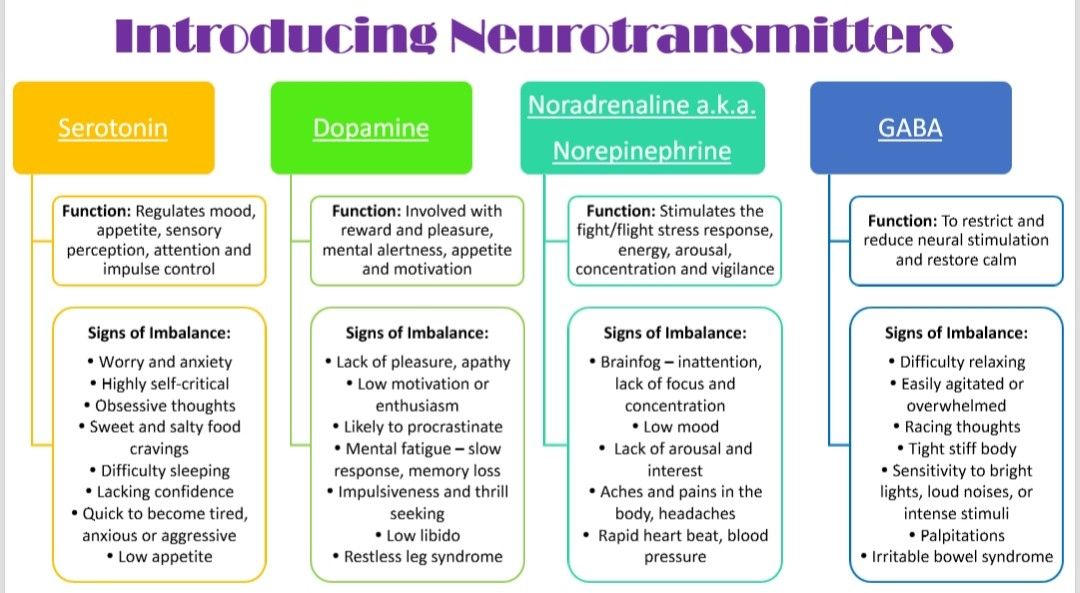 4% in the sibutramine group compared to 10.0% in the placebo group; including the risk of developing non-fatal myocardial infarction and non-fatal stroke were 4.1% and 2.6% in the sibutramine group and 3.2% and 1.9% in the placebo group. At the same time, the risk of death from cardiovascular events or death from all causes was comparable with the placebo group [21].
4% in the sibutramine group compared to 10.0% in the placebo group; including the risk of developing non-fatal myocardial infarction and non-fatal stroke were 4.1% and 2.6% in the sibutramine group and 3.2% and 1.9% in the placebo group. At the same time, the risk of death from cardiovascular events or death from all causes was comparable with the placebo group [21].
The design of the SCOUT study caused a number of comments from experts, namely, the inclusion in the study of patients who already had contraindications to sibutramine, and the long duration of treatment (on average 3.4 years, while the instructions provided for continuous treatment only for 2 years). Despite this, in 2010, on the recommendation of the American and European drug regulatory authorities (FDA, EMA), the sale of the drug in the EU countries was completely discontinued, in the USA the drug was restricted for use in patients with cardiovascular diseases (CVD). nine0003
The lack of other effective drugs for the treatment of obesity led to further studies of the drug, as well as a revision of the SCOUT study - the safety of using sibutramine in patients with CVD during a short treatment period (up to 6 months) was demonstrated [22, 23], as well as the safety of its short-term [24, 25] and long-term [26] use in patients with no history of CVD.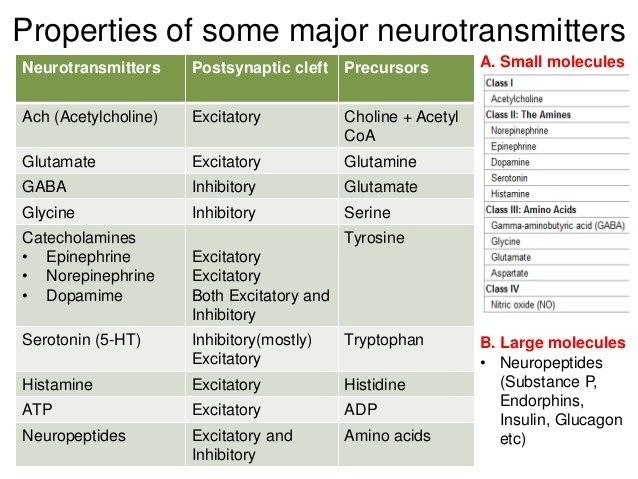
In Russia, the experience of using sibutramine is summarized in the form of the results of large observational programs. Thus, more than 34 thousand patients and 1520 doctors in 52 cities of the Russian Federation took part in the VESNA observation program (2011–2012) [25]. The program collected epidemiological data on the efficacy and safety of Reduxin® (sibutramine and microcrystalline cellulose) in everyday medical practice. The VESNA surveillance program has greatly contributed to the introduction of rational therapy with drugs containing sibutramine in Russia. Reasonable prescribing of the drug by doctors and a systematic assessment of the patient's condition during treatment contributed to the prevention of a number of complications in the pharmacotherapy of obesity and a decrease in the frequency and severity of possible adverse events. nine0003
The PrimaVera program, led by the Endocrinological Research Center and the Russian Association of Endocrinologists, continued the practice of observational programs in the treatment of such socially significant diseases as obesity and type 2 diabetes, and was aimed at introducing a monitoring algorithm into the clinical practice of doctors of various specialties efficacy and safety of obesity therapy.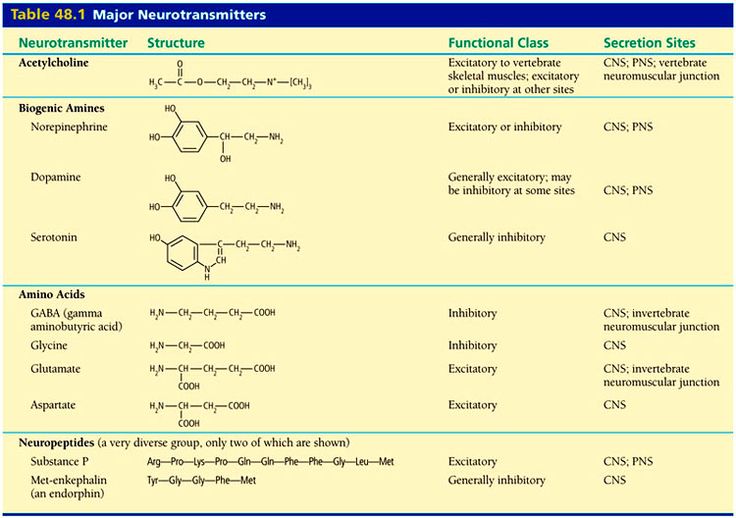 The implementation of this algorithm allows a doctor of any specialty to correctly select patients for whom the use of Reduxin® (sibutramine and microcrystalline cellulose) is indicated, adjust the dose depending on the results of treatment and its effect on the cardiovascular system, and also track those who did not respond to therapy in the early stages. patients in whom continued use of sibutramine may increase cardiovascular risk. More than 3,000 doctors and about 100,000 patients have taken part in the program. The results of the implementation of the PrimaVera program confirmed the favorable safety profile of Reduxin® for a long period of obesity treatment (up to 1 year) and its high efficiency. So, for 3 months of therapy, a significant decrease in body weight by 5% or more from the initial values was observed in 9 patients.2.4% of patients. Within twelve months of therapy, 51.2% of patients had a BMI decrease below 30 kg/m2, and 11.5% of patients with morbid obesity achieved a BMI decrease below 40 kg/m2, 37.
The implementation of this algorithm allows a doctor of any specialty to correctly select patients for whom the use of Reduxin® (sibutramine and microcrystalline cellulose) is indicated, adjust the dose depending on the results of treatment and its effect on the cardiovascular system, and also track those who did not respond to therapy in the early stages. patients in whom continued use of sibutramine may increase cardiovascular risk. More than 3,000 doctors and about 100,000 patients have taken part in the program. The results of the implementation of the PrimaVera program confirmed the favorable safety profile of Reduxin® for a long period of obesity treatment (up to 1 year) and its high efficiency. So, for 3 months of therapy, a significant decrease in body weight by 5% or more from the initial values was observed in 9 patients.2.4% of patients. Within twelve months of therapy, 51.2% of patients had a BMI decrease below 30 kg/m2, and 11.5% of patients with morbid obesity achieved a BMI decrease below 40 kg/m2, 37.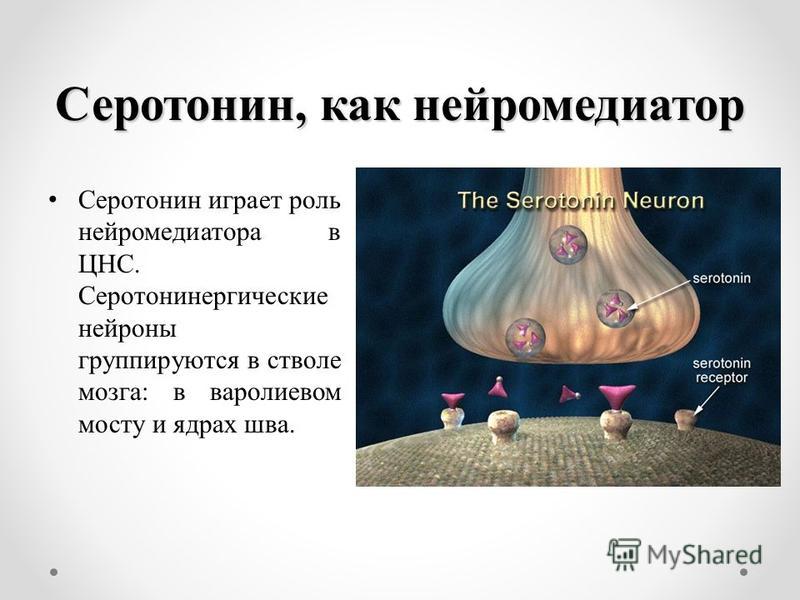 3% of patients who completed therapy reached their "ideal" body weight. At the same time, the frequency of adverse events did not exceed 2.5% of cases [26].
3% of patients who completed therapy reached their "ideal" body weight. At the same time, the frequency of adverse events did not exceed 2.5% of cases [26].
With long-term calorie restriction, patients often experience a physiological plateau effect, i.e. stop in the process of weight loss. At this point, interaction with the doctor is especially important to find out the reasons for this stoppage, timely correction of therapy, and also to overcome the decrease in motivation to continue treatment. Regular communication between the patient and the doctor, carried out within the framework of observational programs, allows this to be done and to achieve the desired results of therapy. Among patients who received long-term (more than 3 months) therapy with Reduxin® at a dose of 10 mg, in 22.1% of cases (N=3446) a "plateau" effect was observed. It is important to note that in patients who did not respond to Reduxin therapy for three months, but continued treatment, the "plateau" effect was manifested 1.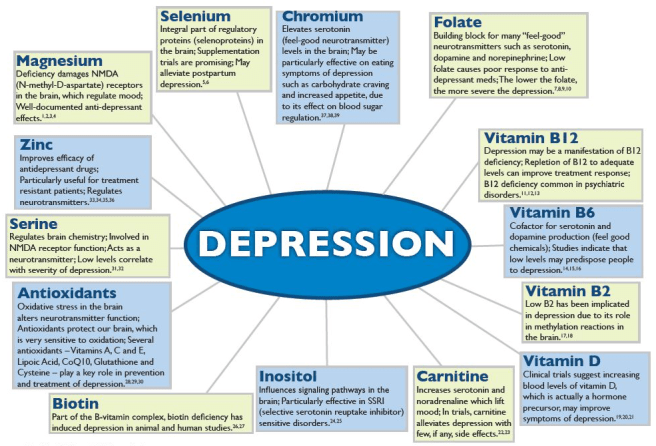 7 times more often than in patients who met the "response" criterion to therapy, but had a temporary character. Overall, the plateau effect was temporary in 20.4% (N=3180) [27]. nine0003
7 times more often than in patients who met the "response" criterion to therapy, but had a temporary character. Overall, the plateau effect was temporary in 20.4% (N=3180) [27]. nine0003
Another parameter of therapy control, which is important to evaluate in the framework of long-term (4-6 months) use of Reduxin, is the return of body weight, i.e. its increase by 3 kg from the previously achieved. Among patients who responded to therapy (based on the results of 3 months of treatment), weight gain was registered only in 0.41% of cases. A possible reason was the lack of adherence of patients to therapy and doctor's recommendations.
Thus, we can confidently speak about the advisability of at least a six-month course of therapy with Reduxin to achieve a target weight loss of 10–14% from the initial one and consolidate the result obtained, as well as the possibility and expediency, depending on the results of treatment, of extending therapy up to twelve months. nine0003
It can be argued that the results of weight loss with the combination preparation of sibutramine and microcrystalline cellulose not only meet surrogate criteria for treatment efficacy (improvement in physiological and biochemical parameters), but also contribute to the achievement of some so-called clinical endpoints of therapy - a decrease in the incidence of complications associated with with diseases associated with obesity and improve the quality of life of patients.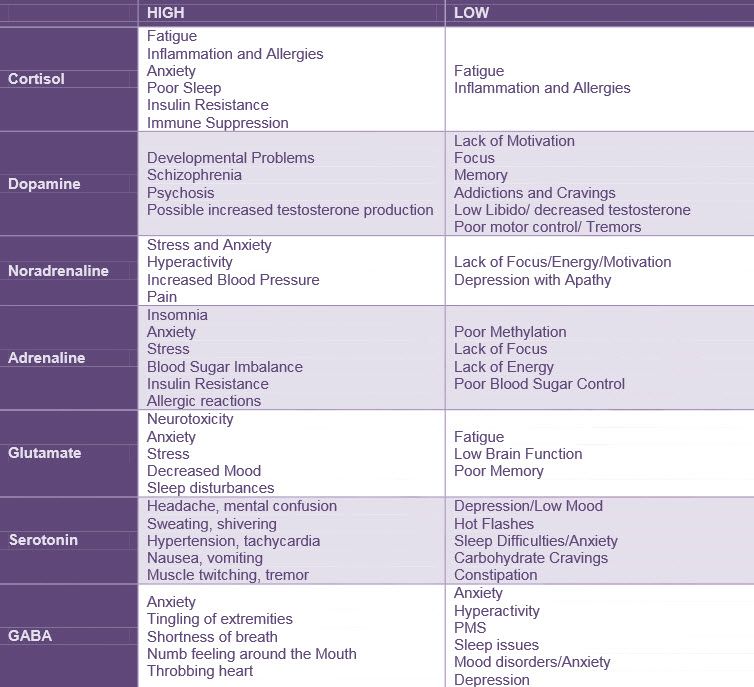
In recent years, new data has emerged illustrating the safety of using sibutramine as part of the instructions. For example, a large cohort study (23 937 patients), evaluating the effect of prescribing sibutramine on cardiovascular outcomes in routine clinical practice, conducted in the UK, the results of which were published in May 2015, demonstrated a low risk of developing cardiovascular complications when taking sibutramine in a group of patients without cardiovascular diseases [ 28]. The authors write that in the SCOUT study, an increased risk of adverse events was observed in patients who are contraindicated in the use of sibutramine in accordance with the instructions for use, therefore, the significance of the results of this study for the general population of obese patients is highly controversial. In conclusion, it was concluded that the approval for the use of sibutramine in a group of patients without cardiovascular disease was unreasonably withdrawn. nine0003
Thus, obesity is often associated with a change in the functional organization of the hypothalamus or other nerve centers responsible for eating behavior, as well as with impaired metabolism of certain neurotransmitters, which determines the rationale for prescribing centrally acting drugs to such patients.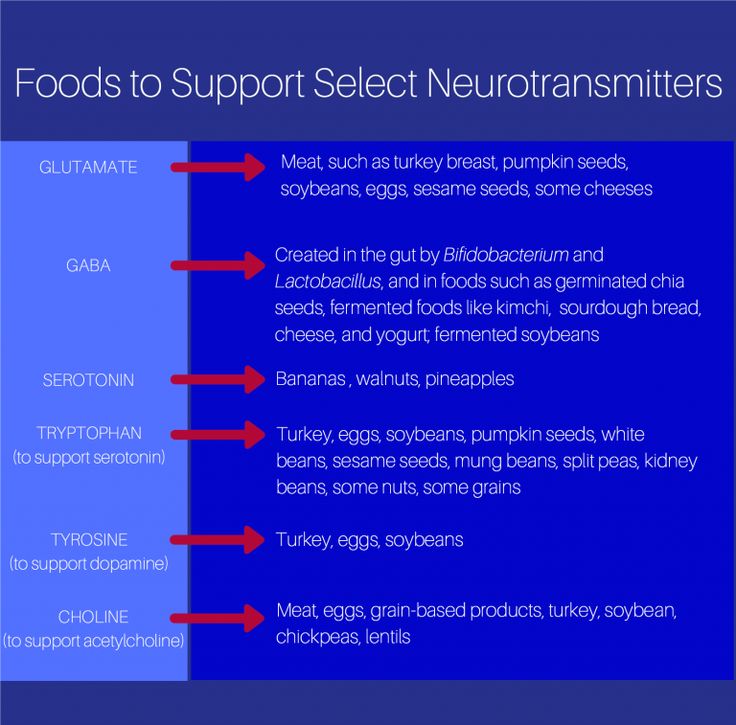 Sibutramine in combination with microcrystalline cellulose (Reduxin®), prescribed in accordance with the instructions for medical use, allows for safe and effective treatment of obesity and helps to reduce the incidence of complications of comorbid conditions and improve the quality of life of patients. nine0003
Sibutramine in combination with microcrystalline cellulose (Reduxin®), prescribed in accordance with the instructions for medical use, allows for safe and effective treatment of obesity and helps to reduce the incidence of complications of comorbid conditions and improve the quality of life of patients. nine0003
Funding and conflict of interest information
The authors declare no apparent or potential conflicts of interest related to the publication of this article.
The work was completed without attracting additional funding from third parties.
1. Diagnosis and treatment of obesity in adults. Recommendations of the Russian Association of Endocrinologists. Edited by I.I. Grandfather. - Moscow, 2010. [Diagnostika I lechenie ozhireniya u vzroslyh. Rekomendacii Rossijskoj Associacii Ehndokrinologov. Ed by Dedov I.I. Moscow; 2010 (In Russ.)]
2. Carnell S, Gibson C, Benson L, et al. Neuroimaging and obesity: current knowledge and future directions. Obes Rev. 2012;13(1):43-56. doi: 10.1111/j.1467-789X.2011.00927.x.
2012;13(1):43-56. doi: 10.1111/j.1467-789X.2011.00927.x.
3. Kremneva E.I., Suslin A.S., Govorin A.N., et al. fMRI mapping of alimentary areas of the brain. Annals of clinical and experimental neurology. Volume 9. No. 1 2015; 32-36. [Kremneva EI, Suslin AS, Govorin AN, et al. Mapping of the brain regions responsible for behavioral regulation with functional MRI. Annals of clinical and experimental neurology. 2015;9(1): 32-36 (In Russ.)]
4. Obesity. Edited by Dedov I.I., Melnichenko G.A. / Moscow: Medical Information Agency, 2004. [Obesity. Ed by Dedov II, Melnichenko G.A. Moscow: Medicinskoe informacionnoe agency; 2004 (In Russ.)]
5. Yeo G, Heisler L. Unraveling the brain regulation of appetite: lessons from genetics. Nat Neurosci 2012; 15(10): 1343–1349. doi: 10.1038/nn.3211.
6. Fry M, Hoyda T, Ferguson A. Making sense of it: roles of the sensory circumventricular organs in feeding and regulation of energy homeostasis. Exp Biol Med (Maywood) 2007; 232:14–26.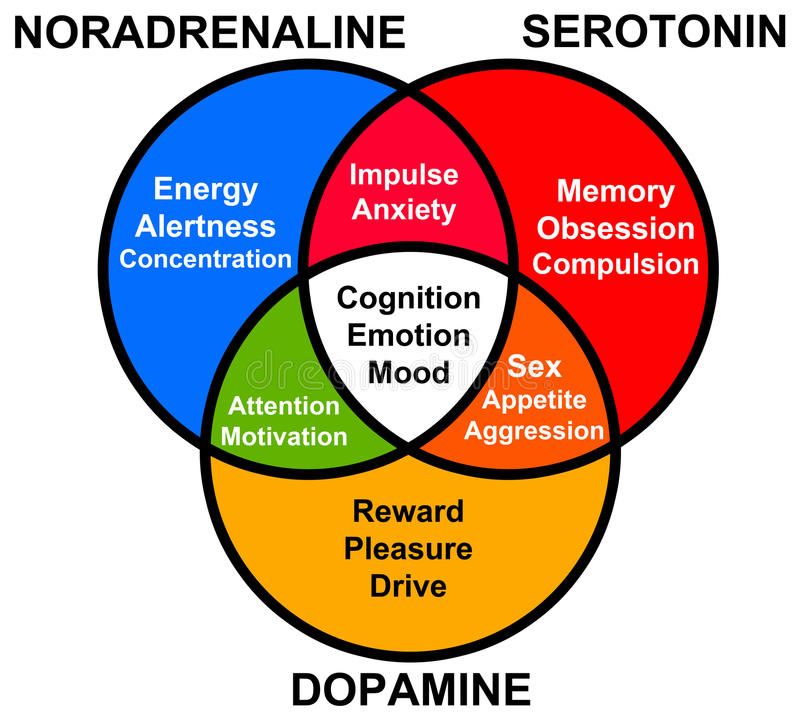 nine0003
nine0003
7. Guyton A.C., Hall D.E. Medical physiology. Moscow: Logosphere, 2008.- 1296p. [Gayton AK, Kholl DE. Textbook of Medical Physiology. Moscow: Logosfera, 2008; 1296 (In Russ.)].
8. Guo J, Simmons W, Herscovitch P, et al. Striatal dopamine D2-like receptor correlation patterns with human obesity and opportunistic eating behavior. Mol Psychiatry. 2014;19(10):1078-84. doi: 10.1038/mp.2014.102
9. Van Strien T, Snoek H, Van der Zwaluw C, Engels R. Parental control and the dopamine D2 receptor gene (DRD2) interaction on emotional eating in adolescence. Appetite. 2010; 54(2): 255-61. doi:10.1016/j.appet.2009.11.006
10. Lam D, Garfield A, Marston O, et al. Brain serotonin system in the coordination of food intake and body weight. Pharmacol Biochem Behav 2010; 97(1): 84–91. doi:10.1016/j.pbb.2010.09.003.
11. Best J, Nijhout H, Reed M. Serotonin synthesis, release and reuptake in terminals: a mathematical model. Theoretical Biology and Medical Modeling 2010; 7: 34. doi:10.1186/1742-4682-7-34
doi:10.1186/1742-4682-7-34
12. Heath MJ, Hen R. Serotonin receptors. Genetic insights into serotonin function. Curr Biol. nineteen95; 5:997–999. doi: 10.1016/S0960-9822(95)00199-0
13. Garfielda A, Burkea L, Shawa J, et al. Distribution of cells responsive to 5-HT6 receptor antagonist-induced hypophagia. Behavioral Brain Research 2014; 266:201–206. doi: 10.1016/j.bbr.2014.02.018
14. Wurtman R, Wurtman J. Brain serotonin, carbohydrate-craving, obesity and depression.
15 Obes Res. 1995; 3 (4): 477-480 doi: 10.1002/j.1550-8528.1995.tb00215.x
16. Satoskar RS, Bhandarkar SD, Rege NN. Pharmacology and Pharmacotherapeutics; 20th ed. Mumbai: Popular Prakashan; 2007.
17. Smith S, Weissman N, Anderson C, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010; 363(3): 245–256. doi: 10.1056/NEJMoa0909809
18. Chan E, He Y, Chui C, et al. Efficacy and safety of lorcaserin in obese adults: a meta-analysis of 1-year randomized controlled trials (RCTs) and narrative review on short-term RCTs.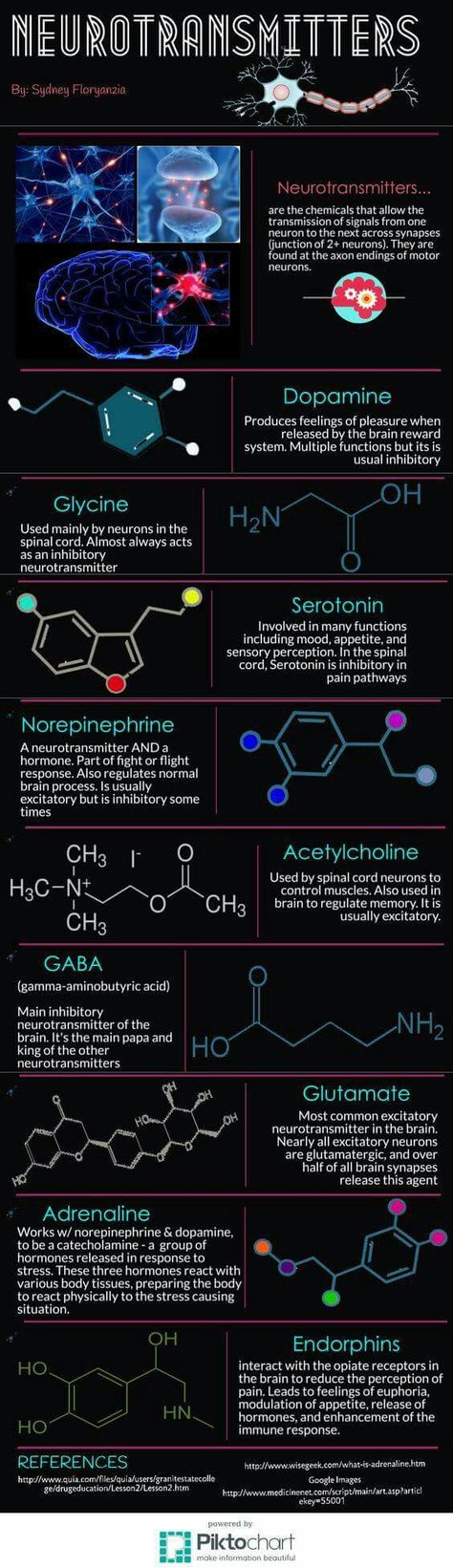 Obes Rev. 2013;14(5):383-92. doi: 10.1111/obr.12015.
Obes Rev. 2013;14(5):383-92. doi: 10.1111/obr.12015.
19. Karam J, McFarlane S. Tackling obesity: new therapeutic agents for assisted weight loss. Diabetes Metab Syndr Obes. 2010; 3:95–112
20. Rucker D, Padwal R, Li S, et al. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007; 335 (7631): 1194–1199. doi:10.1136/bmj.39385.413113.25
21. Zhou YH, Ma XQ, Wu C, et al. Effect of anti-obesity drug on cardiovascular risk factors: a systematic review and meta-analysis of randomized controlled trials. PLOS One. 2012; 7(6): e39062. doi: 10.1371/journal.pone.0039062
22. James W, Caterson I, Coutinho W, et al. SCOUT Investigators Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med. 2010; 363(10):905–917. doi: 10.1056/NEJMoa1003114
23. Seimon R., Espinoza D., Ivers L. et al. Changes in body weight and blood pressure: paradoxical outcome events in overweight and obese subjects with cardiovascular disease.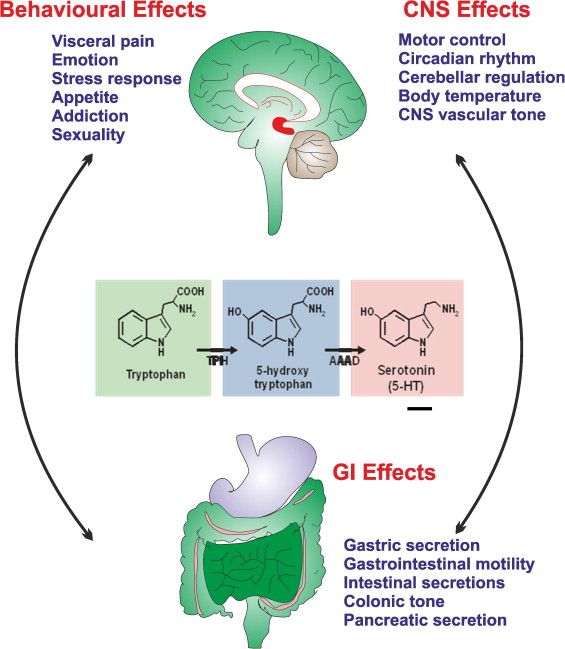 Int J Obes. 2014;38(9): 1165-1171 doi: 10.1038/ijo.2014.2.
Int J Obes. 2014;38(9): 1165-1171 doi: 10.1038/ijo.2014.2.
24. Caterson I, Finer N, Coutinho W, et al. Maintained intentional weight loss reduces cardiovascular outcomes: results from the Sibutramine Cardiovascular OUTcomes (SCOUT) trial. Diabetes, Obesity and Metabolism. 2012; 14(6):523-30. doi: 10.1111/j.1463-1326.2011.01554.x. nine0003
25. Pavlik V, Fajfrova J, Slovacek L, Drahokoupilova E. The role of sibutramine in weight reduction. Bratisl Lek Listy. 2013; 114(3): 155-157.
26. Ametov A.S. Report on the VESNA program. Effective treatment of obesity is the way to fight the Diabetus mellipidus epidemic. // Effective pharmacotherapy. Special issue. - 2013. - S. 7-11. [Ametov AS. Report about program VESNA. Effektivnoe lechenie ozhireniya - put borbyi s epidemiey Diabetus mellipidus. Effektivnaya farmakoterapiya. special edition. 2013; 7-11. (In Russ.)]. nine0003
27. Melnichenko G.A., Romantsova T.I., Zhuravleva M.V. All-Russian program for safe weight loss “PrimaVera”.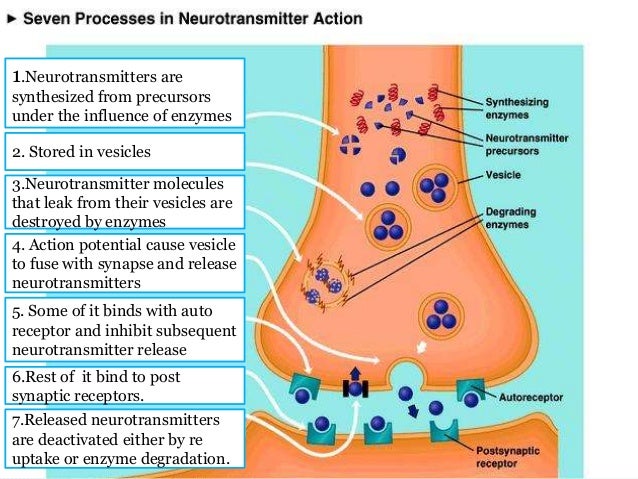 Results of the first year. Obesity and metabolism. 2014; 1(38): 62-67. [Melnichenko GA, Romantsova TI, Zhuravleva MV. Vserossiyskaya programma bezopasnogo snizheniya vesa "PrimaVera". Itogi pervogo goda provedeniya. obesity and metabolism. 2014; 1(38): 62-67. (In Russ.)]. doi:10.14341/omet2014162-68
Results of the first year. Obesity and metabolism. 2014; 1(38): 62-67. [Melnichenko GA, Romantsova TI, Zhuravleva MV. Vserossiyskaya programma bezopasnogo snizheniya vesa "PrimaVera". Itogi pervogo goda provedeniya. obesity and metabolism. 2014; 1(38): 62-67. (In Russ.)]. doi:10.14341/omet2014162-68
28. Troshina E.A., Mazurina N.V., Galieva M.O. Creation of strategies for the treatment of obesity and comorbid diseases based on observational programs: intermediate results of the All-Russian observational program PrimaVera. // Almanac of Clinical Medicine. - 2015. - №S1. – p. 95-101. [Troshina EA, Mazurina NV, Galieva MO. Development of therapeutic strategies for obesity and comorbid disorders based on observational programs: interim results of the Russian observational program PrimaVera. Almanah klinicheskoj medicine. 2015; (S1): 95-101 (In Russ.)].
29. Hayes JF, Bhaskaran K, Batterham R, Smeeth L, Douglas I. The effect of sibutramine prescribing in routine clinical practice on cardiovascular outcomes: a cohort study in the United Kingdom.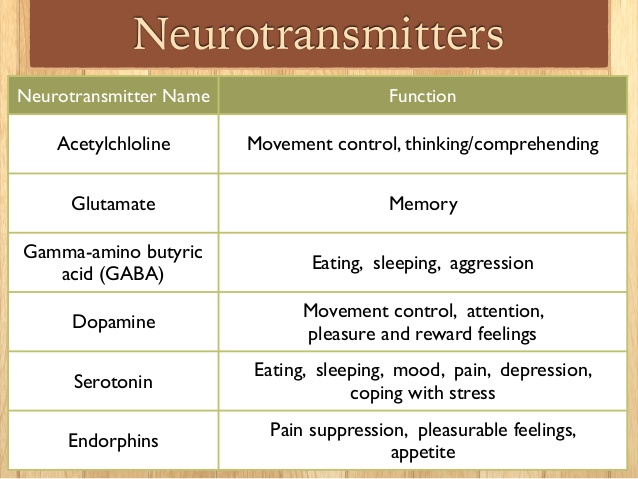 Int J Obes.. 2015;39(9):1359-1364. doi:10.1038/ijo.2015.86.
Int J Obes.. 2015;39(9):1359-1364. doi:10.1038/ijo.2015.86.
30. Caterson I, Coutino V, Finer N et al. Early response to sibutramine in patients not meeting current label criteria: preliminary analysis of SCOUT lead-in period. Obesity (Silver Spring). 2010;18(5):987-94. doi: 10.1038/oby.2009.327.
Neurotransmitters: what they are, their functions and how they relate to emotions
Neurotransmitters play an important role in our body and affect everything from mood to the ability to learn. How do they differ from hormones, what types are there, and what disease can their deficiency lead to? nine0003
What are neurotransmitters
Neurotransmitters are biologically active substances. Their main function is to transmit signals from nerve cells. That is, neurotransmitters are substances through which the nervous system communicates within itself. One neuron, being excited, transmits the necessary signals to another neuron through neurotransmitters.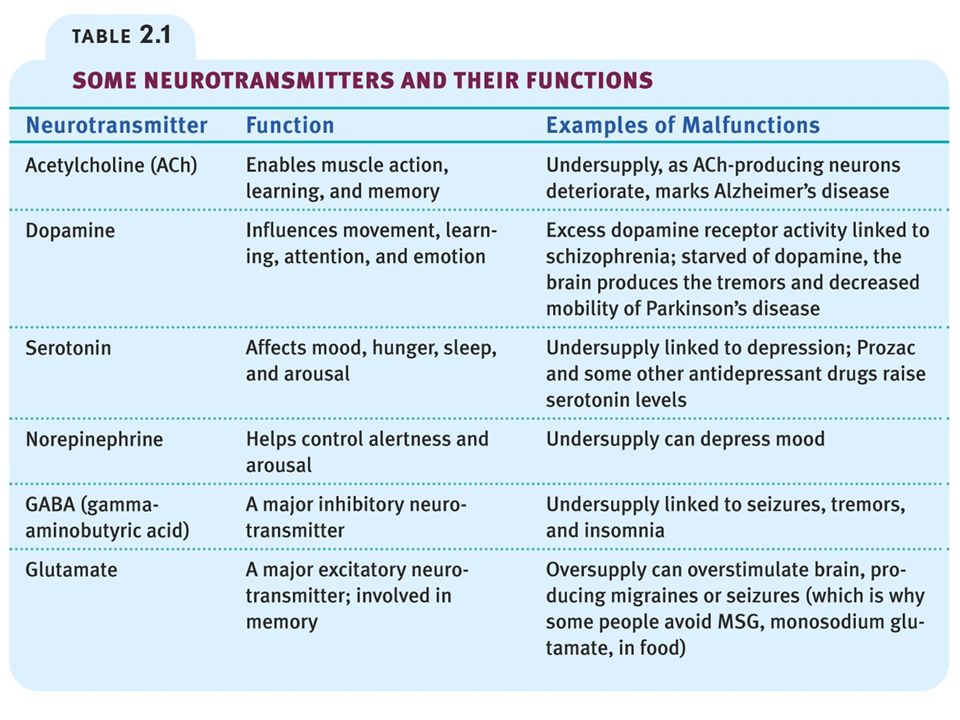
The study of neurotransmitters began at the beginning of the 20th century. Then scientists tried to figure out how neurons communicate with each other - chemistry or electricity. Santiago Ramón y Cajal and Camillo Golgi simultaneously received the Nobel Prize for their research on the nervous system at 1906, although they held opposite opinions. Ramon y Cajal was convinced that neurons communicate with each other using chemicals. Golgi held a different point of view - neurons communicate using electricity.
“And only in the middle of the 20th century was it possible to take an electronic photograph of the synapse, in which vesicles with neurotransmitters were visible. It turned out that most of the neurons communicate with each other using neurotransmitters. There are also electrical synapses, but they are rare,” Elena Belova, Ph.D. nine0003
A synapse is a point of contact between two neurons, or between a neuron and a receiving effector cell.
An effector cell is a type of cell in the body that performs some action in response to stimulation (for example, a muscle cell contracts when it receives a signal from a neuron across a synapse).
Vesicles are small vesicles that carry various substances inside them: from hormones to neurotransmitters.
There are substances that simultaneously work as neurotransmitters and hormones. For example, if norepinephrine and adrenaline are secreted in the brain, they work as neurotransmitters. If they are secreted by the adrenal cortex, they work like hormones. There is a fine line between neurotransmitters and hormones. It is not so easy to draw a dividing line between them. nine0003
- A hormone is a substance secreted in the endocrine glands that affects the tissues (cells) of the body.
- A neurotransmitter is a substance released by a neuron to transmit a signal, most often to another neuron.
“When everyone was just starting to study, it seemed that these were different things. But the deeper we explore, the more we find substances that transmit signals between neurons, and more and more often we find in other cells (for example, immune cells) receptors for compounds that were considered classical neurotransmitters. It turns out that these two systems are much more tightly connected with each other, these are two finely intertwined systems,” adds Elena Belova. nine0003
It turns out that these two systems are much more tightly connected with each other, these are two finely intertwined systems,” adds Elena Belova. nine0003
Functions and actions of neurotransmitters
Neurons are separate cells that have to constantly communicate with each other. The signal from one neuron to another is transmitted through a contact where the cells are adjacent to each other almost closely, leaving only a tiny gap. This connection between two nerve cells is called a synapse.
Nerve impulses in the brain run along the processes of neurons, and when they reach the synapse, vesicles with a neurotransmitter are released there, transmitting signals to the next neuron. How it reacts depends on the receptors: some neurotransmitters can activate some cells and inhibit others - it all depends on the type of receptors inside the synapses that receive signals. nine0003
An imbalance of certain neurotransmitters causes various diseases and disorders, from epilepsy to depression. Although there is no consensus on this issue among scientists either.
Although there is no consensus on this issue among scientists either.
“Parkinson's disease is perhaps the only disease for which the reinforced concrete cause is a lack of the neurotransmitter dopamine. For other states, there is no such unambiguity,” Belova believes.
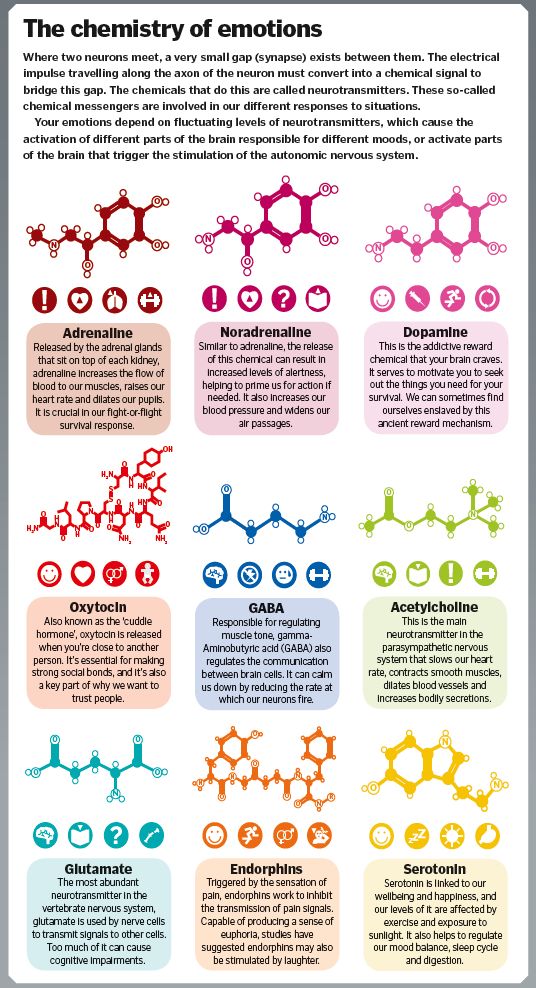
Types of neurotransmitters
The most common neurotransmitters are of one of two types - excitatory and inhibitory. The first type are those that excite the next neuron (if one neuron in the chain is active, the next one will also be so). The second type inhibits neighboring neurons. There are also neuromodulators - they do not just transmit an excitatory or inhibitory signal, but change the neuron's susceptibility to such signals. nine0003
Neurotransmitters are also grouped according to their chemical structure. Among them are: amino acids, monoamines, peptides. Let's talk about the features of each on the examples of neurotransmitters.
Amino acids
- Gamma-aminobutyric acid (GABA) is the main inhibitory neurotransmitter in the brain.
 For example, some psychoactive substances that are aimed at treating anxiety act specifically on GABA receptors.
For example, some psychoactive substances that are aimed at treating anxiety act specifically on GABA receptors. - Glutamate is the main excitatory neurotransmitter in the brain. It plays an important role in cognitive functions: memorization and learning. An excess of glutamate is detrimental to nerve cells and can contribute to the emergence of certain diseases (epilepsy, Alzheimer's disease). nine0016
Peptides
- Oxytocin . It is both a hormone and a neurotransmitter. In the body of a woman, it stimulates childbirth and the production of milk, in the brain it is responsible for the feeling of affection between parents and children. However, this is not a molecule of universal love. The feeling of falling in love is a complex cocktail, primarily associated with the work of the hypothalamus, attachment formation and sexual arousal. “When we find the right person, it triggers the release of oxytocin and the formation of attachment, the release of sex hormones and sexual arousal.
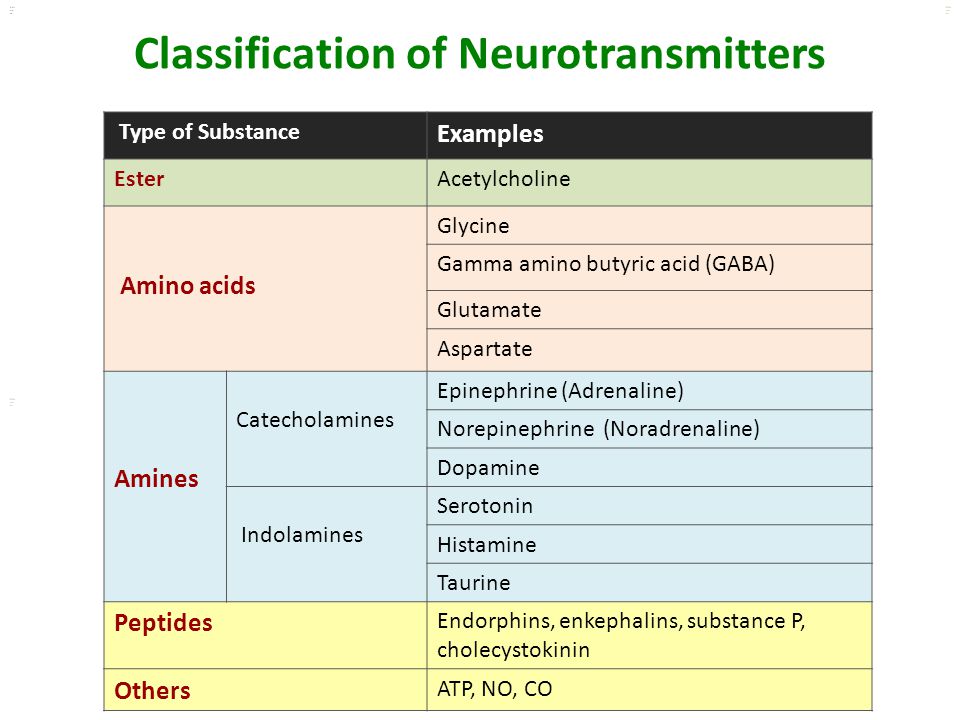 Further, if people approached each other and the oxytocin bond formed, they have a long-term relationship. “Love lives for three years” (actually several months) is the primary stage of a relationship where oxytocin bonds are just being formed,” Belova explained. nine0016
Further, if people approached each other and the oxytocin bond formed, they have a long-term relationship. “Love lives for three years” (actually several months) is the primary stage of a relationship where oxytocin bonds are just being formed,” Belova explained. nine0016 - Endorphins . They dampen pain signals and induce a feeling of euphoria.
Monoamines
- Adrenaline and norepinephrine . They can be attributed not only to neurotransmitters, but also to hormones. Our response to stress, external threats, and our mode of concentration or relaxation is carried out through the sympathetic and parasympathetic branches of the peripheral nervous system. The brain sees the danger, but in order to respond to it, you need to activate the muscles. The sympathetic system is the “fight and flight” signaling system when the work of skeletal muscles, heart rate, and so on increases. The adrenal glands secrete adrenaline, norepinephrine, and cortisol, which act on the body.
 At the same time, norepinephrine and adrenaline are also produced inside the brain, and this is a signal that we are in an excited state. When we leave the "acute" mode, the parasympathetic system becomes more active, and we go into the "lay down and digest" mode: the digestive organs work and the process of storing fats starts. nine0016
At the same time, norepinephrine and adrenaline are also produced inside the brain, and this is a signal that we are in an excited state. When we leave the "acute" mode, the parasympathetic system becomes more active, and we go into the "lay down and digest" mode: the digestive organs work and the process of storing fats starts. nine0016 - Dopamine is associated with reward expectation. And if the reward from our actions matches the forecast, and even better - more than expected, this is a reason to repeat the actions again and again. This is how habits are formed. But everything is not so simple. For example, when a person wants to lose weight, the desire to be slim, refusing high-calorie food, fights in him with the biological need for food, controlled by the hypothalamus. “This is an ancient system. People have only recently entered a situation where access to food is almost unlimited. Weaning yourself from the habit of checking social networks is a hundred times easier than forcing yourself to maintain a calorie deficit, because there is an internal system that says that losing weight is very bad, ”Belova notes.
 Some dangerous illicit drugs imitate the action of dopamine, causing a person to be in an elevated state, anticipation of something pleasant, a feeling of excitement. nine0016
Some dangerous illicit drugs imitate the action of dopamine, causing a person to be in an elevated state, anticipation of something pleasant, a feeling of excitement. nine0016 - Serotonin regulates sleep, anxiety, appetite and sexuality.
There are neurotransmitters that are not of these types, and the longer scientists study this topic, the more different types they find. But the very first discovered neurotransmitter, acetylcholine, also belongs to the “other” group. Its functions include the regulation of memory, the processes of awakening and falling asleep. For example, patients with Alzheimer's disease have low levels of acetylcholine.
About feelings and neurotransmitters
Neurotransmitters are not there to make us feel. Feelings are the activity of certain parts of the brain under the influence of a cocktail of different neurotransmitters and their mutual influence.
“We cannot say that if we add some neurotransmitter to the brain, we will cause a certain feeling.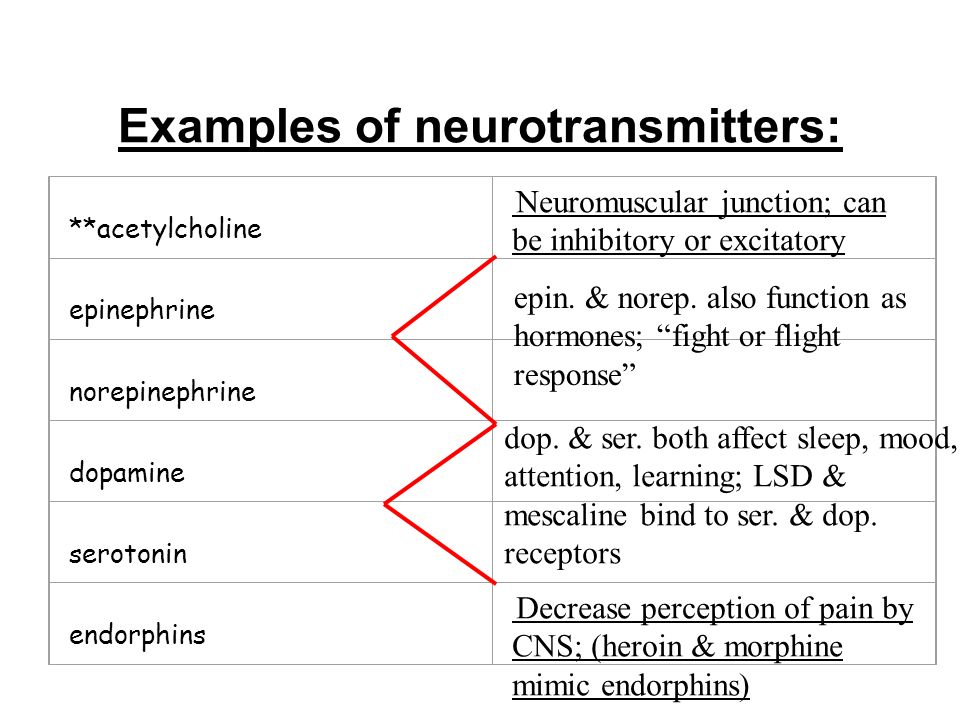 Our feelings are influenced not only by what is released in the brain, but also by what we see around us and how we interpret it. Strong excitement can be regarded by us both as positive excitement and as negative. Although in both cases, the main note will be a high concentration of adrenaline and norepinephrine, ”explains Elena Belova. nine0003
Our feelings are influenced not only by what is released in the brain, but also by what we see around us and how we interpret it. Strong excitement can be regarded by us both as positive excitement and as negative. Although in both cases, the main note will be a high concentration of adrenaline and norepinephrine, ”explains Elena Belova. nine0003
There are neurotransmitters that are responsible for the level of arousal and the level of tone. For example, there is a structure in the brain called the reticular formation. This is a dispersed system of neurons and their clusters, which is responsible, among other things, for the level of cheerfulness or lethargy. Serotonin, norepinephrine and adrenaline, acetylcholine and dopamine are released there. The purpose of this structure is to regulate the level of alertness. The peculiarity of this system is that thanks to it, we can quickly perk up to sudden stimuli - for example, a roar or a flash of light - so that we are ready to quickly make a decision in response to an unexpected threat.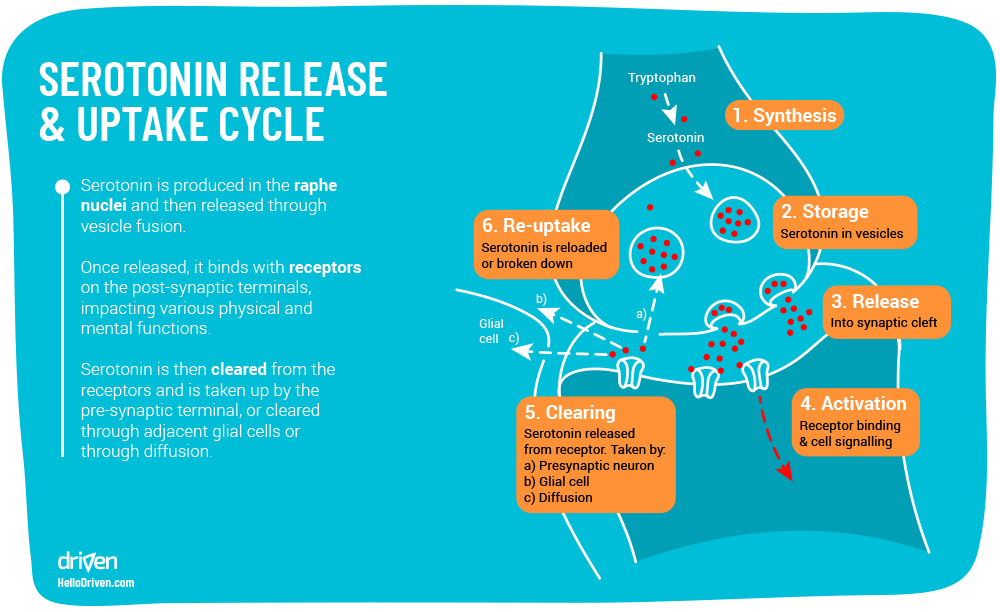 nine0003
nine0003
There are also structures associated with the hypothalamus (a small area in the diencephalon) that are responsible for different conditions and needs. They regulate the level of stress: a calm state, acute or chronic stress. This whole system, in addition to the level of vivacity, determines the level of our combat readiness. Immediately there is a change in state associated with feelings of hunger, fatigue, drowsiness, sexual desire and feelings of affection - all this is also associated with the hypothalamus. For example, oxytocin is responsible for the level of attachment. The brain also contains systems related to motivation, learning, and pleasure. Their main neurotransmitter is dopamine. nine0003
Neurotransmitters and depression
Depression is a violation of the motivational mechanism. A person ceases to enjoy what he does, the endorphin component "I'm done well" is turned off. When there is not enough endorphin and there is no feedback (when we are talking about depression caused by external influences, not clinical), motivation is weakened, and a person comes to a state where he does not have enough strength and energy to support his life.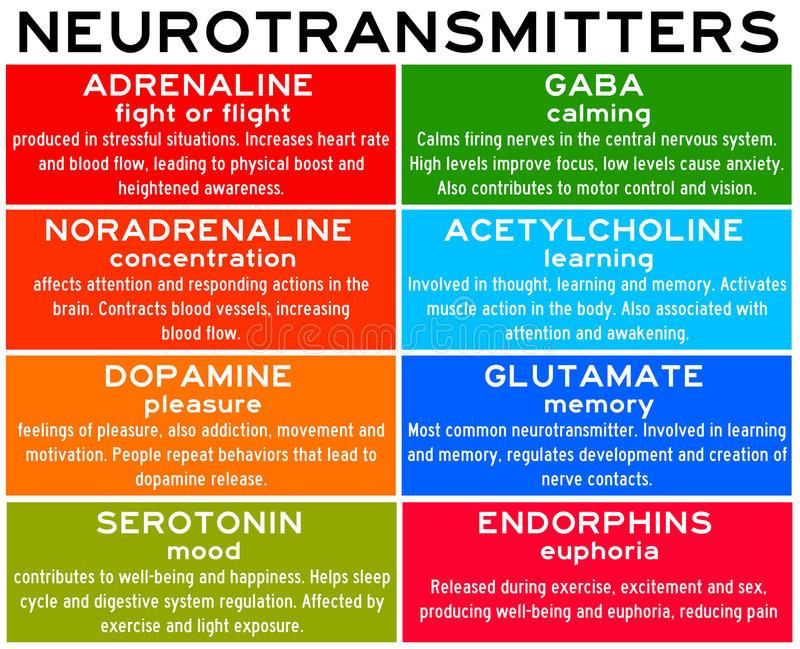
So, at 19In the 1960s, American psychologist Martin Seligman discovered a phenomenon he called "learned helplessness." He did an experiment on dogs. Animals were divided into two control groups and placed in different rooms. Each dog had its own box, the floor of which was supplied with a weak electric current. The dogs in the first room could go free if they found the right spot in the box. By clicking on it, they got the opportunity to leave the box. Everything was different in the second room. The boxes of these dogs were opened by the actions of the dogs from the first group. There was also a third group. Dogs were not electrocuted in it. The first stage of the experiment showed that the dogs from the same room managed to quickly recover from the torment. They returned to their habits and physical characteristics. But such results were not observed in the dogs from the second room. Animals fell into apathy. nine0003
After this part of the experiment, all dogs were placed in the same room, where the floor was current.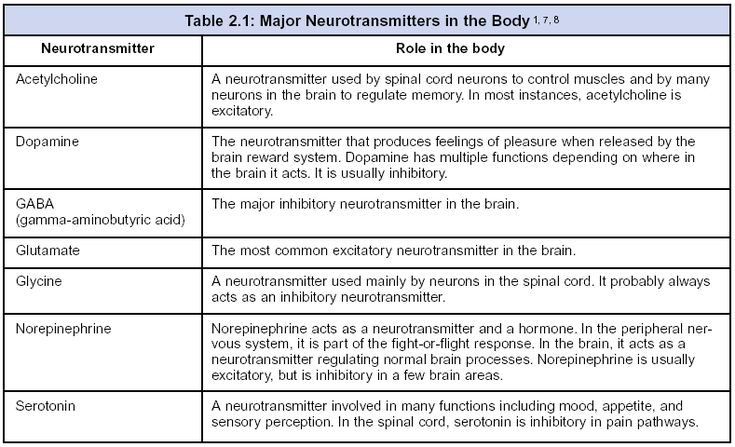 The animals were given the opportunity to get out of there. To do this, it was necessary to jump over the partition. Dogs from the first and third groups guessed to do it. And most of the dogs from the second - first whined, and then lay down on the floor. At the same time, they no longer paid attention to pain.
The animals were given the opportunity to get out of there. To do this, it was necessary to jump over the partition. Dogs from the first and third groups guessed to do it. And most of the dogs from the second - first whined, and then lay down on the floor. At the same time, they no longer paid attention to pain.
Martin Seligman after the experiment suggested that the state of learned helplessness, the lack of attempts to avoid stress, this is the experimental model of depression. A person is not able to control the unpleasant that happens to him. nine0003
If our sense of self-control fails, our serotonin neurons bring us back to a more primitive initial state in which the psyche is not trying to do anything. Serotonin as a neurotransmitter is also capable of blocking negative emotions. Dysregulation of the serotonin system leads to the fact that negative emotions are much stronger. The system moves from an equilibrium state to an unbalanced state when the body lacks the motivation to act actively and achieve goals.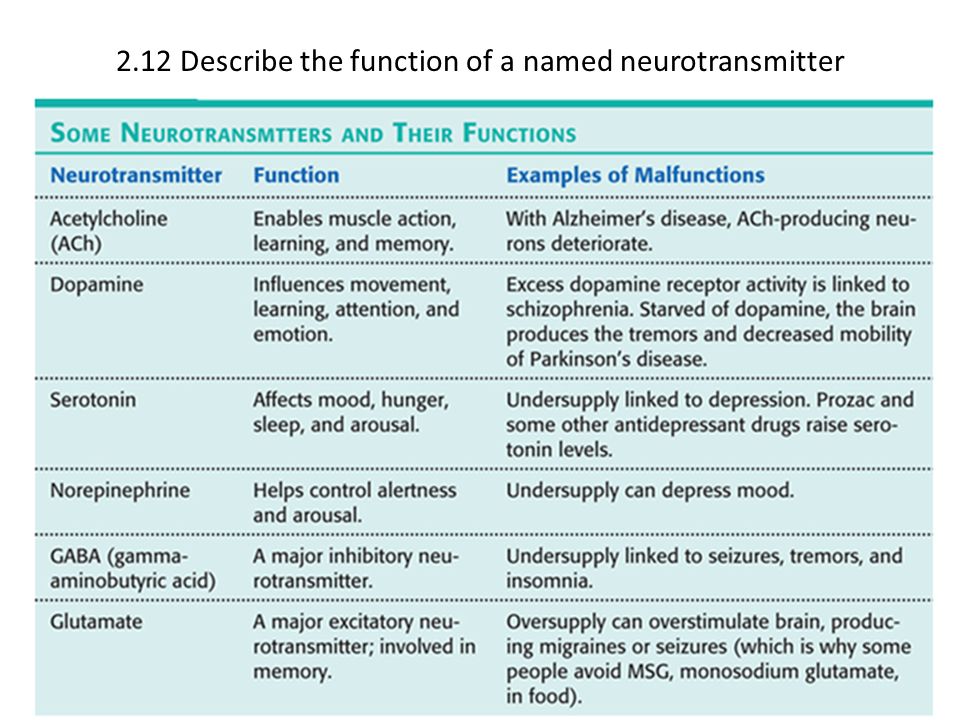 To bring the system back into balance, antidepressants were developed. nine0003
To bring the system back into balance, antidepressants were developed. nine0003
“Classic antidepressants – serotonin reuptake inhibitors. They do not allow serotonin to quickly disappear from the place of contact, prolonging its effect on neurons. For a neurotransmitter to work, it must bind to a receptor, and the properties of the receptor greatly influence how the neurotransmitter will act. It is assumed that when serotonin is released, it acts not only on the next neuron, but also on the one from where it was released. At the end of the neuron itself, which secretes serotonin, there are also receptors. When serotonin is released, it acts on this receptor and actually causes the ending to stop working. The cell released serotonin, he contacted and shut down the system. For antidepressants to have an effect, these receptors must first change their susceptibility to the neurotransmitter. Apparently, this explains that such antidepressants need to be taken for quite a long time to alleviate depression, ”explains the expert.