My girlfriend has ocd
Dating Someone with OCD - Tips for Dating Someone with OCD
Even though you may hear people loosely throw around the term “OCD,” the reality of actually being diagnosed with obsessive-compulsive disorder goes much, much deeper than just being a neat freak or liking your desk organized a certain way. (And for the record, using it casually in that context is actually super offensive to people legitimately diagnosed with OCD.)
So if you are currently dating someone with OCD and want to be a supportive partner, good news: You’re in the right spot. Let’s start with the facts first.
A person who is diagnosed with OCD will “get caught in a cycle of obsessions and compulsions,” according to the International OCD Foundation
. The obsessions are categorized as “unwanted, intrusive thoughts, images, or urges that trigger intensely distressing feelings.” The compulsions are “the behaviors an individual engages in to attempt to get rid of the obsessions and/or decrease their distress. ”
And to put it into perspective for you, 1 in 100 adults suffers from these obsessions and compulsions, which adds up to more than 2 million adults in the United States alone, according to the International OCD Foundation. So yeah, consider it a very common disorder.
Another thing to realize: Every person with OCD looks different. The disorder is not solely related to cleaning or organizing, as some people think. Maybe someone with OCD is excessively double-checking to see if they turned off their straightener (even though they know they did so). Maybe someone with OCD repeatedly checks in with a loved one to make sure they are safe. It can show up in a number of ways.
So if you want to know how you can help your person, we’ve sourced a ton of helpful tips from actual mental health experts on how to better be there for someone with OCD.
Before we dive into all the details, remember: It’s great to do your own research and even ask your partner what they need from you. The most important thing is not to judge them for behavior that can sometimes be out of their control.
The most important thing is not to judge them for behavior that can sometimes be out of their control.
What to Expect
When you’re dating someone who has been diagnosed with OCD, it’s important to remember and understand that your partner might have habits or routines that might come off as excessive and repetitive to you, says Bianca Walker, a licensed professional counselor in Atlanta, Georgia, and owner and psychotherapist at The Self Care Institute of Atlanta, LLC.
A behavioral compulsion might look like excessive handwashing, which comes from the obsessive thought of germs. They might also suffer from mental compulsions, which can look like them asking for reassurance from someone they love, overanalyzing a situation, or unproductive problem-solving and planning. (An example of this would be if someone repeats a phrase, prayer, or mantra in order to convince themselves that if they say it enough times, their dog won’t get sick or their grandma won’t die. )
)
With that being said, dating someone with OCD requires patience and support as they try to navigate dealing with the disorder while also navigating a romantic relationship, says licensed professional clinical counselor Paula Muro.
Related Story
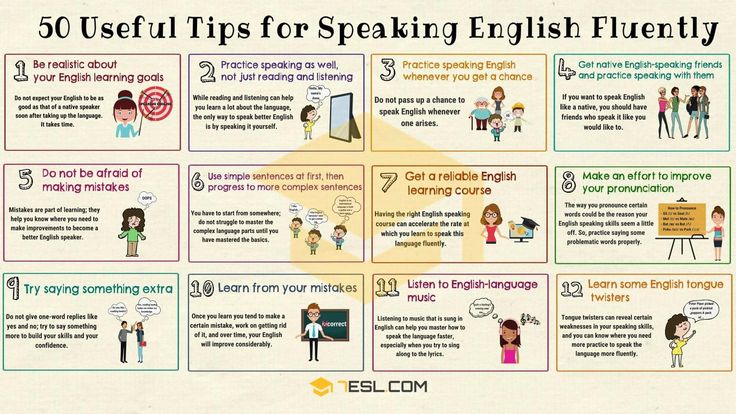
In order to have a healthy relationship with someone who has OCD, communication is vital. Walker suggests that you familiarize yourself with your partner’s OCD. Ask yourself: What are some of their most common intrusive thoughts? How do they respond or seek reassurance for those thoughts? How can I help, according to what their doctor says?”
“Knowing what to expect can help you prepare to respond in a way that supports your partner’s OCD recovery. It can also help you identify your own needs and boundaries,” says Walker. Because, yes, while you’ll want to support your partner, you can’t forget your own self-care.
It can also help you identify your own needs and boundaries,” says Walker. Because, yes, while you’ll want to support your partner, you can’t forget your own self-care.
You’ll also want to provide a safe and nonjudgmental space for your partner to be exactly who they are. “Having OCD can produce feelings of shame and frustration,” details Walker. This means that you should show kindness, patience, and have clear communication to create a safe space for you and your partner to share and build intimacy in spite of OCD.
Related Story
- How to Take Care of Your Mental Health Rn
Oftentimes, people with OCD will suffer from anxiety as well, so don’t place any blame on them or even suggest they aren’t trying hard enough. Recognize that they will have ups and downs, and expect to see moments when they have positive results from treatments but also moments when they might relapse into obsessions and compulsions.
And if your partner is not seeking help for their OCD and you sense it’s become disruptive to their life, you may want to encourage them to find a therapist and a medical authority who could provide some proper coping mechanisms. They can start with a website like NOCD, which is an online service for those with OCD to talk to a qualified therapist about their diagnosis and potential coping mechanisms. You can book a free 15-minute call and decide whether the service is right for you.
They can start with a website like NOCD, which is an online service for those with OCD to talk to a qualified therapist about their diagnosis and potential coping mechanisms. You can book a free 15-minute call and decide whether the service is right for you.
The best thing you can do to support someone with OCD—whether that’s a partner or even a family member or friend—is to educate yourself on the disorder, says Brenda Wade, PhD, relationship adviser to Online for Love. “And not just yourself but also the person you’re dating who has OCD,” she explains.
This starts by being knowledgable of your partner’s treatment plan suggested by their psychologist, therapist, or psychiatrist. Once you’re familiar with their treatment plan, you can dive into some reading. We suggest adding When a Family Member Has OCD: Mindfulness and Cognitive Behavioral Skills to Help Families Affected by Obsessive-Compulsive Disorder, by Jon Hershfield and Jeff Bell, to your Amazon cart.
When a Family Member Has OCD: Mindfulness and Cognitive Behavioral Skills to Help Families Affected by Obsessive-Compulsive Disorder
When a Family Member Has OCD: Mindfulness and Cognitive Behavioral Skills to Help Families Affected by Obsessive-Compulsive Disorder
$11 at Amazon
You could also look for support groups (either in your city or online) that bring together the loved ones of OCD sufferers. Additionally, it would be beneficial to follow some of the leading OCD organizations, such as the International OCD Foundation and Made of Millions, on social media.
“This is not something either of you is alone in. These are opportunities to connect with the one you love and allow for a greater understanding of each other.”
Here are a few other tangible things you can do to support someone with OCD, according to Magdalena Cadet, MD:
- Be patient and don’t dismiss or minimize their pain.
 Make sure to acknowledge what your partner is feeling and offer empathy, especially because it can be hard for someone with OCD to open up about what’s going on in their head. If this is the case, encourage them to share a story about a character or an event that resembles what they’re feeling. You could say something like, “I’m all ears and I’m not here to judge. You can be honest with me.”
Make sure to acknowledge what your partner is feeling and offer empathy, especially because it can be hard for someone with OCD to open up about what’s going on in their head. If this is the case, encourage them to share a story about a character or an event that resembles what they’re feeling. You could say something like, “I’m all ears and I’m not here to judge. You can be honest with me.” - Understand their obsessive thoughts, their triggers, and anxieties that make up a particular OCD episode. Dr. Cadet suggests creating a secret code word or signal to let your partner know you are noticing their triggers.
- Practice self-care and keep strong, healthy boundaries in place so that OCD doesn’t dominate your lives entirely. You might feel like you need to look out for your partner at all times, but it’s just as important to keep yourself mentally and physically healthy. Don’t sacrifice the things you like to do, whether that’s going to the gym or reading a book.
 As for boundaries, it’d be good to talk to a professional on just how you can help your partner overcome an episode. For example, if you notice that your partner is having a particularly bad day, you might need to back off if that person is not in any danger. But if you notice your partner is having a good day, you can encourage them to continue resisting their compulsions as much as possible.
As for boundaries, it’d be good to talk to a professional on just how you can help your partner overcome an episode. For example, if you notice that your partner is having a particularly bad day, you might need to back off if that person is not in any danger. But if you notice your partner is having a good day, you can encourage them to continue resisting their compulsions as much as possible. - Try to destigmatize OCD with your partner or family member. Help them acknowledge that many individuals live with some form of illness and they aren’t alone.
- Allow your partner to perform the compulsive behavior and rituals even if there is a feeling of shame and discomfort. But as always, consult with your partner’s therapist on how you should respond to your partner’s OCD episodes, as it all depends on a person’s treatment course.
- Be aware of your partner’s treatment if they are willing to share it with you. Sometimes you can’t try to completely control your partner’s environments because allowing them to be exposed to the trigger is part of their treatment.
 Other times, constantly reassuring a person that their compulsions are okay may not be the best thing to do, as that can help reinforce the behavior. For this reason, it’s best to consult a professional.
Other times, constantly reassuring a person that their compulsions are okay may not be the best thing to do, as that can help reinforce the behavior. For this reason, it’s best to consult a professional. - Love your partner and make sure they know you are there for them. As in every other relationship, use your actions to let them know how much you care. Schedule a date night and be flexible if they need to change it up. Try to remember the reasons you fell in love and discover brand-new ones every day. Most importantly, understand that your partner has a disorder that is out of their control and you shouldn’t blame them whenever their intrusive thoughts or compulsions act up.
Although there is no one specific formula to what your relationship with someone who has OCD should look like, the foundations of communication and being understanding are key—just like any other relationship.
Be mindful when your partner reveals their diagnosis, and try to learn as much about OCD as possible. If you have no idea where to begin researching, check out resources like Peace of Mind or the International OCD Foundation.
If you have no idea where to begin researching, check out resources like Peace of Mind or the International OCD Foundation.
Related Story
- Legit Mental Health Care Hacks You Need Now
Sophia Melissa Caraballo Piñeiro
Sophia is a freelance writer based in New York City with experience in writing everything from beauty and lifestyle to health and wellness. She hails all the way from Puerto Rico and lately, you’ll find her writing stories that exhaust the Latinx voice in the United States.
If You Love Someone With OCD, You May Need to Stop Giving Them Reassurance All the Time
At the worst of my OCD, Jesse’s participation in these rituals didn’t quench my insatiable thirst for certainty—I’d rise wearily from bed multiple times a night, at the expense of sleep and peace, to check again. And again. As Yip explains, even when a spouse or loved one complies with a checking request, that doesn't always relieve someone with OCD. In fact, it may just reinforce their urge to keep checking.
Reminiscing on my love-hate relationship with excessive reassurance seeking (ERS), a common OCD behavior, I cringe at how the disorder cast a shadow over our marriage. “Text me when you get there,” I’d shout after Jesse every single morning, without fail, as he headed to work. As chipper as my voice must have sounded, a small torture unfolded in my head, with visions of being responsible for his untimely death in a car accident holding me hostage even as I went through the motions of the morning.
And almost without fail, my phone would buzz half an hour later with his one-word message: “Here.” If he forgot to text, or chose not to, or took a little longer than usual, panic would bubble up until I confirmed that he was safe. And during particularly stressful weeks (stress is thought to exacerbate OCD), the reassurance seeking questions would flow freely, and Jesse was usually the one caught in their path.
“The baby looks different. Do you think something’s wrong with her?”
“No. She’s fine.”
She’s fine.”
“I called my dad and he didn’t answer. Do you think he’s OK? What if something happened?”
“I’m sure he’s just busy.”
“My throat feels weird, do you think I have cancer?”
“Oh my God, no, you don’t have cancer.”
Both of us interpreted these responses as supportive, and that certainly was the intention, but they may have actually fueled the OCD cycle.
As kind as it might seem, telling someone with OCD that they don’t have cancer or that the baby is fine “are lies,” Yip points out. “How could a spouse possibly know that their loved one doesn’t have cancer without medical training and CAT scans?” she says. In most cases, a response that “everything is fine” is an educated and highly likely assumption, but it never quite fulfills what someone with OCD is craving.
And responding to these sorts of compulsions in such a matter-of-fact way also reinforces them, in a way. It made me believe my questions were reasonable and valid, and made me constantly seek the temporary comfort that the reassurance provided.
It’s also only a band-aid, a temporary solution. “If you respond with certainty, for example, ‘No, you won’t die,’ the person with OCD will still always wonder and have the same question and continue to ask in a hundred different ways,” Yip explains. “The best way you can support your loved one is to help him or her tolerate uncertainty.”
I’ve learned, sometimes the hard way, that the healthiest responses to my OCD can come off as counterintuitive and unsupportive. But it’s in my best interest to have Jesse (and any of my friends and family) acknowledge that reassurance can actually fuel my compulsion.
This can be tough given that your loved ones just want to do what they can to appease your OCD (or any mental illness). In my case, my spouse wanted to provide the reassurance that I was desperately seeking, since it often helped me feel better in the moment. But the best way for a loved one to respond to excessive reassurance seeking, according to Yip, is to respond vaguely. Yip says that phrases like, “I don’t know,” and, “Maybe you will, maybe you won’t,” are better replies.
Yip says that phrases like, “I don’t know,” and, “Maybe you will, maybe you won’t,” are better replies.
"In the middle of my sophomore year, I started drinking heavily." A girl with obsessive-compulsive disorder - about being late, toxic relationships and the “rules” of life
In the 6th grade, Tanya began to be often late for classes, and skipped classes in college. The teachers decided that the girl was lazy and simply did not want to study. But at the age of 18, our heroine learned that the reason for everything is obsessive-compulsive disorder (OCD). Together with the Living Library Center we recorded her monologue – about childhood, alcohol addiction and how to live “correctly”. nine0003
– At the end of my last, third, course, there was a prevention tip: they said that I would be kicked out of college. I received support from only a few people - the rest thought that I was lazy, worthless, and in general I needed to be reprimanded, expelled and not bathe.
Once, when I couldn't leave the house to study again, my dad threw the phrase: "You're just being lazy. " I became very embarrassed. I grabbed a knife and said: “Yes, I would rather die! Why did you give birth to me at all? I hate my life and I don't want to live like this." Then I thought I was going crazy. nine0003
" I became very embarrassed. I grabbed a knife and said: “Yes, I would rather die! Why did you give birth to me at all? I hate my life and I don't want to live like this." Then I thought I was going crazy. nine0003
I made an appointment with a psychotherapist, but I thought that they would put me in a hospital, lock me up there, and register me. And when I told the specialist about my relationship with my fiancé, about my life, it turned out that in addition to the depression that I was in at that time, I had OCD. I feel better.
“I wash my face 10 times: if more or less, I will feel discomfort, as if I didn’t do something” rituals). Thoughts, as a rule, are associated with numbers (for example, wash five times, comb three times), cleanliness, correctness or incorrectness of actions. nine0003
To get rid of them, a person performs certain rituals. For example, I have this: to be clean, you need to wash a certain number of times. Which? I dont know. So, we rely on the figure of age: I am 21 years old - but for washing it is a lot. Therefore, I divide this number by two and choose the one that is less: I carry out the procedure 10 times - and only then will I be clean. If you do less or more, I will feel discomfort, as if something is not done.
Therefore, I divide this number by two and choose the one that is less: I carry out the procedure 10 times - and only then will I be clean. If you do less or more, I will feel discomfort, as if something is not done.
But, since I am now working with a cognitive behavioral therapist, many rituals have been cut or simplified: say, now I need to know the number, and what it will be is not important. As my specialist explained, once in childhood I did not learn to rely on myself, on my feelings, so I came up with such a ritual. nine0003
“My parents raised me with care as best they could, but excessive control made itself felt”
The disorder began to manifest itself in childhood: I placed toys exactly around the perimeter of the table, and if something fell or moved, hysteria began. Then she shook the clothes out the window a certain number of times, because everything seemed to be dusty. Then came the ritual of washing and brushing your teeth.
It was also always difficult for me to sort out potatoes in the village: I divided the fruits into large, medium and small ones. Because everything in the world is relative, I've often hung around to decide which category to put the potato in. nine0003
Because everything in the world is relative, I've often hung around to decide which category to put the potato in. nine0003
My parents didn't really notice my oddities: I didn't advertise much in front of them. They usually attributed my slowness to laziness and character traits. And at this time, some rituals were replaced by others.
In general, I do not know such children with mental disorders who grew up in a normal family. Fights, scandals, quarrels - it all affects the child. Of course, my parents love me very much, they raised me with care, as best they could, but excessive control made itself felt. nine0003
In our family there were such attitudes: “there is no word “I want”, there is a word “must”, “I am the last letter of the alphabet”. All this gradually forms a child's self-esteem. Yes, this is how many parents raise their children, but, probably, my psyche turned out to be more fragile.
Plus dad often used the word "right", so my frustration is based on the belief that there are "right" and "wrong" actions. Even if there is no rule, I will still come up with it: for example, cleaning should be done on a certain day, and not when you want, and in a certain way, and products should be taken from a certain shelf. What happens if you break the rule? Nothing, I'll just feel uncomfortable. nine0003
Even if there is no rule, I will still come up with it: for example, cleaning should be done on a certain day, and not when you want, and in a certain way, and products should be taken from a certain shelf. What happens if you break the rule? Nothing, I'll just feel uncomfortable. nine0003
Adults often think that if something happens between a husband and wife, it does not affect the child in any way. But children very well read the emotional background of their parents: anxiety appears, from which he tries to escape somewhere, followed by obsessive thoughts and then rituals.
“I realized that alcohol helps to get rid of obsessions: you just don’t care”
At school, when the workload increased, there was less time for rituals. But without them, I simply could not leave the house. Therefore, I began to be late for classes: the director yelled at me, brought me to tears. I said that I didn’t understand why this was happening: I had always been a diligent girl, I studied well - and now I’m late. nine0003
nine0003
And at the age of 12, when my parents and I moved to live in another apartment (which became stressful for me), I found a way to alleviate my condition - I started tearing myself apart, damaging my face. And if initially these actions were conscious, now I just hang on to it and only after a while I understand what I'm doing. Every morning I wake up and believe: from today I don’t tear myself apart, but by the evening I still break down.
It seemed to me that after school (I graduated from the 9th grade) everything would change. Went to college, but it got even worse. The first year I somehow unlearned, met my fiancé (we met for 3 years and lived together for 1.5 of them), and in the middle of the second year I started drinking hard. I realized that alcohol helps to get rid of obsession: you just don’t care. This went on until 19years old.
Of course, that period could not but affect my social life: at first my parents tried to control me, but they realized that it was useless. In college - absenteeism, lateness. But I didn't care. When you are trying your best not to be late and not to skip, to study well, and the teachers say that you are just lazy ... It's so insulting and so painful.
In college - absenteeism, lateness. But I didn't care. When you are trying your best not to be late and not to skip, to study well, and the teachers say that you are just lazy ... It's so insulting and so painful.
After all, I am a perfectionist: I must be better in everything, I must know and be able to do everything. I wanted to devote myself to studying as much as possible, but it did not work out. And when you are consciously lazy, thump, score - well, okay. nine0003
As a result, this whole situation led me to a psychotherapist, as I described above. She immediately began to drink medicine (but continued to thump) and after some time got a job in a store.
But, after the specialist said that I had a co-dependent relationship with my fiancé, that I had to live separately from my parents and from him, I got offended and didn’t come to the sessions anymore, abruptly stopped taking the drugs. And later I was fired from my job because my obsessions escalated - and I fell into depression again. nine0003
nine0003
“I am very afraid that the disease will interfere with my studies at the university”
And we really had a toxic relationship with a young man: I came from such a family - how can I find any other partner? Fights, drunkenness, betrayal - there was everything, but at the same time we loved each other ( laughs ). There was physical violence on his part (for example, he broke my nose), and on my part it was emotional.
True, I am grateful to him for the way he supported me in depression: he will cook, and bring, and bring, and help¸ and calm, and stroke - he is very empathic. nine0003
At some point, I dragged a young man to a cool, expensive psychotherapist, saying: “You have childhood traumas, you need it.” We came to the specialist together, and he said that he agreed to take on my fiancé, and he advised me to another specialist.
And now we have been working with Daria for more than a year and a half - this is really cool. Helps a lot. For a while, my partner and I were still together, but eventually parted. Now we are on friendly terms, we respect each other - as it was, so it was. nine0003
For a while, my partner and I were still together, but eventually parted. Now we are on friendly terms, we respect each other - as it was, so it was. nine0003
And, probably, approximately from the beginning of therapy, I began to give up alcohol: it was no longer so important to me. And now I'm learning to get high without him at all: it's so cool when you consciously dance, communicate with friends!
I also graduated from college - crawled out of there ( laughs ). Now I am 21 years old, I don’t study and don’t work - I just plan to enter the university next year, and also go to work as a guide: right now I’m preparing to defend the excursion (they send you a text, you learn it and then tell the commission). Since I want to study either as a psychologist or a psychiatrist, I am slowly preparing for the CT in four subjects at once. nine0003
Of course, I am very afraid that the disease will interfere with my studies. We have a lot of homework, independent study of the material, a lot of useless papers. But what to do? If it doesn’t work out, then I’ll try a second time, the tenth…
But what to do? If it doesn’t work out, then I’ll try a second time, the tenth…
“I started going to my friends at four o’clock in the evening, but left the house only at 2 am – I couldn’t choose clothes”
I feel better now: thanks to the fact that I work with different specialists, we managed to remove some rituals, but still, sometimes it takes a lot of time to get ready. Usually my day looks like this: I wake up and immediately think about how my day should go right. Maybe you need to recharge? Or read a prayer? Or do some cleaning? And if cleaning, then with what subject to start? From the sofa? Or out of bed? Or from a chair? And wipe off the dust? How about cleaning inside? nine0003
In the end, you don't take on anything, because you either have to do everything perfectly or don't do it at all. These are my two usual extremes, so I am learning to find the middle. But in this case, there is discomfort that something has not been done. Any charges, cleaning of the apartment are given to me very hard. But it’s good that we managed to cope with the number of times.
But it’s good that we managed to cope with the number of times.
It is interesting that my friends learned about the diagnosis just recently - this summer (then I had already accepted my disease and did not separate it from myself: here I am, but OCD). I had to go to visit them, I began to gather at four o'clock in the evening, but I left the house only at 2 in the morning. All evening I cried, hysteria, could not choose clothes in any way: is it warm or cold? shall we go to the forest? and here the button does not match. nine0003
At that moment, I realized that I couldn't just take and put on everything that came to my mind and go out - I had to choose a certain pattern, because I still couldn't do it any other way. At 12 at night, I recorded a voice message to my friends, confessed my diagnosis, that I couldn’t get myself together. But they supported me, they said that they understand me. Since then, our relationship has improved: we can discuss things that we could not talk about before.
But unfamiliar people, when they hear about my disorder, often say that I came up with something for myself, that vitamins, sports and fresh air will help me - and everything will be great. Before accepting OKR, I tried to justify myself to a person, but now I have built boundaries: you don’t know what it is, the topic is closed. nine0003
On the website of the Living Library Center, which teaches us to accept other people and strive for a more tolerant society, you will find many other people's stories and interesting events.
Reprint of CityDog.by materials is possible only with the written permission of the editors. Details here.
Photo: Paval Hadzinski for CityDog.by.
share
Obsessive-compulsive disorder (OCD) - causes, symptoms, signs, examples, diagnosis (test), treatment
Features
Causes
Symptoms
Diagnosis
Treatment
Signs of obsessive-compulsive disorder (OCD) do not depend on the will of the person, as they relate to mental illness. There are two main signs:
There are two main signs:
- obsessions - obsessive thoughts, ideas, images;
- compulsions are repetitive actions or rituals.
The second name of the disease is obsessive-compulsive disorder. The content of thoughts and images is perceived by the patient as alien, their pain is recognized, but it is not possible to get rid of them on their own. nine0003
Features of obsessive-compulsive disorder
Obsessive-compulsive personality disorder was described in the first half of the 19th century by the French psychiatrist Esquirol, and was called the "disease of doubt." Subsequently, scientists identified the main difference between the disease - the patient's perception of the alienation of the experienced. All other mental illnesses absorb the personality, changing it beyond recognition. A mentally ill person becomes completely different than before the illness. In OCD, the core of the personality remains intact, but the accompanying rituals and experiences are overwhelming, making life difficult.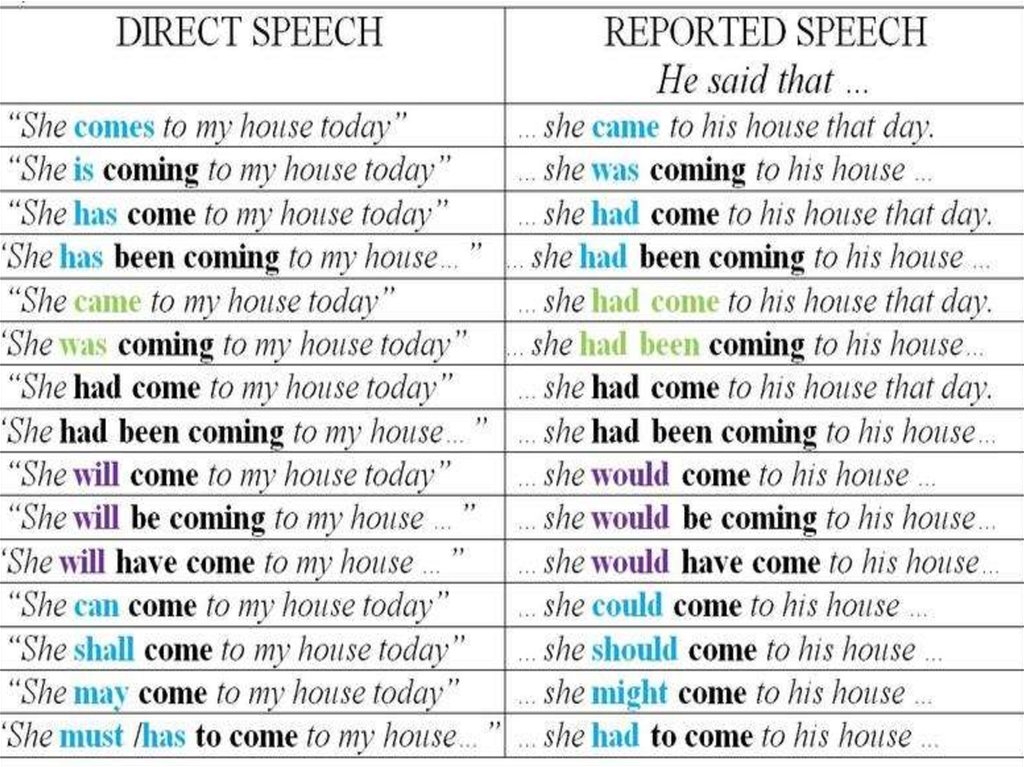 However, there have been cases where a major psychiatric illness (schizophrenia, bipolar disorder) began as OCD. nine0003
However, there have been cases where a major psychiatric illness (schizophrenia, bipolar disorder) began as OCD. nine0003
The morbid state must be distinguished from the natural fear necessary for survival. The fear of depth, the desire to move away from a moving train or a landslide, the desire to hide in an explosion are just reasonable behavior, although tinged with intense fear.
Obsessive-compulsive disorder in women and men occurs with the same frequency of 2 to 5%. Some authors argue that women are more likely to get sick. Statistics are kept only in developed countries where medical care is available. It is not known if the disease occurs elsewhere. nine0107
Causes of obsessive-compulsive disorder
There is no final coherent theory regarding the reasons yet. The following options are discussed:
- hereditary predisposition – violations of the synthesis of neurotransmitters (chemical substances involved in the transmission of nerve impulses) are always of a genetic nature;
- increased activity of some parts of the brain, namely in the limbic system - the dentate gyrus, the prefrontal part of the cerebral cortex; nine0111
- a decrease in the concentration of substances responsible for emotions (serotonin, dopamine) in the thalamus, cortical circuit;
- deviations in the work of brain receptors;
- anomalies in the development of certain zones, in particular the cerebellum and the inferior frontal gyrus;
- congenital or acquired disorders of nerve impulse transmission.
Changes in the work of the cortex and limbic system occur both for genetic reasons and under the influence of adverse external factors. nine0003
Provoking factors are:
- immune system malfunctions;
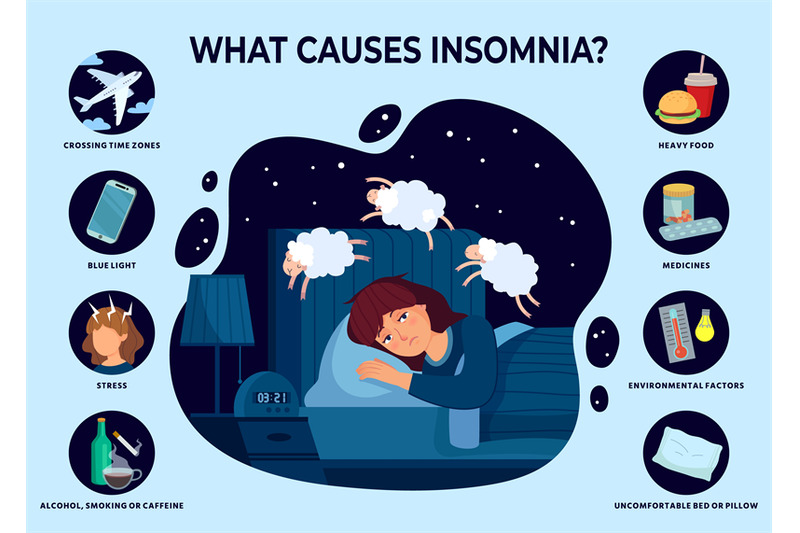
- stress, especially chronic;
- physiological fluctuations in hormonal status in women during pregnancy, childbirth and lactation, as well as during the menstrual cycle;
- encephalopathies of various origins, especially vascular ones;
- trauma and surgery on the brain;
- personal life problems, especially loneliness; nine0111
- alcoholism and drug use;
- infectious diseases - hepatitis, herpetic lesions, HIV;
- severe somatic pathology - a chronic increase in thyroid function, inflammation of the kidneys, pancreas, liver, stomach.
Obsessive-compulsive disorder in children develops between the ages of 3 and 12 years, it practically does not occur in babies. The closer to adolescence, the higher the incidence. The biological prerequisites are:
The closer to adolescence, the higher the incidence. The biological prerequisites are:
- intrauterine and early childhood brain damage;
- violations of the transmission of a nerve impulse, including changes in the number of neurotransmitters;
- mutation in the gene responsible for the production of serotonin;
- streptococcal infection in the first year of life.
Psychologists have a slightly different view of the nature of the disorder. The main hypothesis is considered to be psychoanalytic, namely the conflict of internal sexual aggression and parental prohibition on such relationships. It is also noted that OCD is more often formed in people with anancastic (stuck) personality traits. One of the undoubted reasons is a difficult, destructive family environment with constant scandals. The death of a mother in early childhood and the loss of a father after the age of 3 years have an extremely unfavorable effect on health. Too strict upbringing, lack of affection and understanding, excessive parental requirements have a negative impact on children. nine0003
Too strict upbringing, lack of affection and understanding, excessive parental requirements have a negative impact on children. nine0003
Russian physiologist Pavlov believed that the disease develops in people of the thinking type with sluggish (inert) processes of excitation-inhibition.
Symptoms of obsessive-compulsive disorder
Obsessive fears or phobias have many varieties, each of which has its own name:
- cancerophobia - fear of getting cancer;
- claustrophobia - closed space;
- agoraphobia - open areas; nine0111
- thanatophobia - death;
- arachnophobia - spiders;
- nosophobia - infection.
Fear has an irrational nature, no beliefs, arguments and evidence have any effect on the patient. To protect against imaginary danger, the patient creates his own rituals or repetitive actions that he performs in strict sequence.
A classic example of obsessive-compulsive disorder: a patient with nosophobia cannot touch anything before washing his hands with hot water and soap three times. In some patients, the fear of infection is so strong that it forces them to wash the floors several times a day with an undiluted disinfectant solution. The fact that there is nothing to breathe in the room and the skin on the hands cracks to blood does not matter to the patient. In such a neglected case, we are no longer talking about any social adaptation, the patient simply cannot leave the house to get to work or walk to the store. nine0107
Diagnosis of obsessive-compulsive disorder
Establishing a diagnosis is the task of a psychiatrist, to whom, unfortunately, the patient does not always get right away. Often, a patient, who is certainly convinced that he has a somatic disease, undergoes a series of various examinations and treatments that do not bring results. Internists (doctors in internal medicine) refer to a psychiatrist after the failure of their own attempts.
Internists (doctors in internal medicine) refer to a psychiatrist after the failure of their own attempts.
It is essential for the diagnosis that the obsessive thoughts or actions take up at least one hour a day. There is a "gold standard" psychological examination for obsessive-compulsive disorder - the Yale Brown test. This is a 10 section questionnaire. Each section has 5 answer options, you need to choose one, the answer is estimated in points. The scores are added up and scored on a scale from 0 to 40, with the highest score indicating extreme OCD. The questionnaire is freely available, you can complete it yourself. nine0003
The result of a neurological examination gives non-specific data characteristic of many nervous disorders: trembling of closed eyelids and outstretched arms, increased tendon reflexes, signs of autonomic imbalance. If the organic nature of the disease is suspected, neuroimaging methods (CT, MRI, and the like) are used.
Treatment of obsessive-compulsive disorder
Therapy is selected strictly individually, it takes time. Usually combine several methods: both drug and non-drug. nine0003
Usually combine several methods: both drug and non-drug. nine0003
For obsessive-compulsive disorder, psychotropic drugs from the following groups are used:
- third-generation antidepressants;
- tranquilizers;
- atypical neuroleptics.
Psychotropic drugs do not act immediately, it is possible to increase the dose with an interval of 7-14 days. The selection and combination of drugs is a delicate matter, there can be no general recommendations. However, the earlier a person sees a doctor, the less time is required to select a treatment. nine0003
Of the psychotherapeutic methods, the following types of therapy have proven themselves well:
- cognitive-behavioral;
- exposure method - collision and working out of a disturbing situation;
- stopping thought - learning to stop the influx of specific obsessions;
- hypnosis;
- auto-training;
- games and fairy tale therapy in children.