Fluoxetine sex drive
When an SSRI medication impacts your sex life
The popular medications known as selective serotonin reuptake inhibitors or SSRIs (see box) can help lift people out from under a dark cloud of depression. But there are some side effects from antidepressants, including those that can affect your sex life. In addition to reducing interest in sex, SSRI medications can make it difficult to become aroused, sustain arousal, and reach orgasm. Some people taking SSRIs aren't able to have an orgasm at all. These symptoms tend to become more common with age.
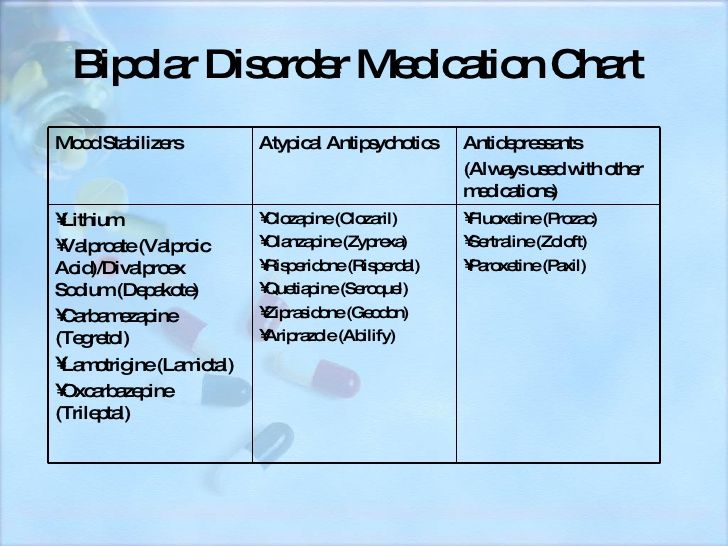
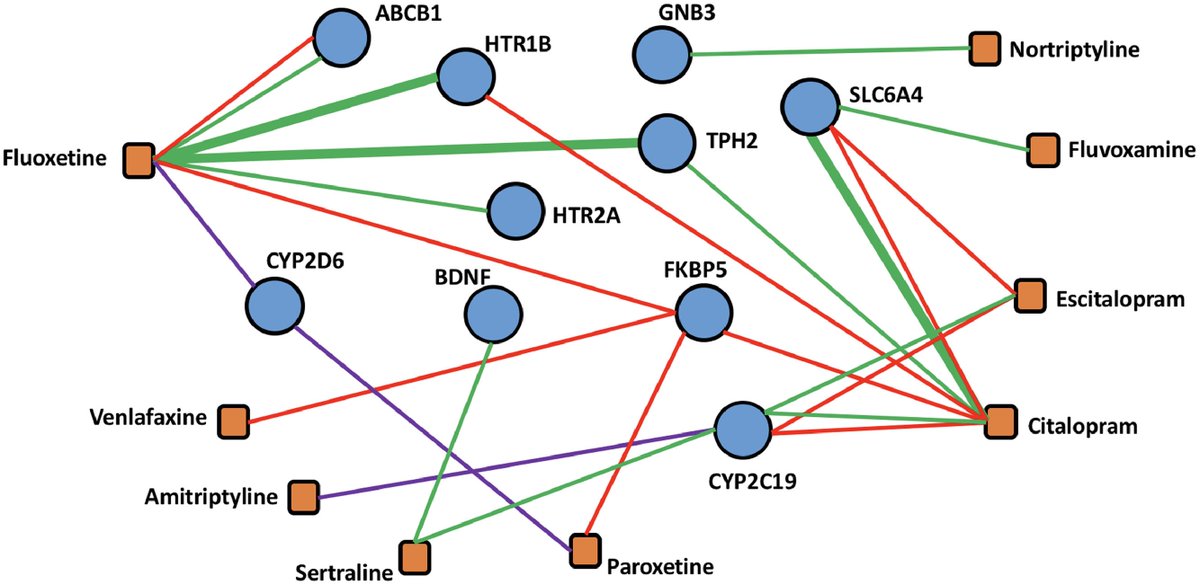
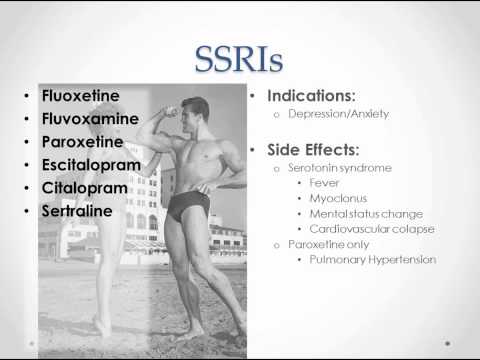
SSRI medications include
|
If you experience any sexual problems while taking an SSRI medication, talk with your doctor or therapist. About 35% to 50% of people with untreated major depression experience some type of sexual dysfunction prior to treatment. So, in some cases, sexual difficulties may stem not from the SSRI, but rather from the underlying depression. If medication is the problem, sexual side effects sometimes subside with time, so it's worth waiting a while to see if problems diminish. This is a particularly good strategy if the medication is easing your depression significantly. But if side effects from antidepressants persist, your doctor or therapist may suggest one of the following strategies, as found in the Harvard Special Health Report Understanding Depression:
Lowering the dose. Sexual side effects may subside at a lower, although still therapeutic, dose.
Scheduling sex. Your medication may produce more pronounced side effects at particular times of the day, for example, within a few hours of taking it. If so, you can try scheduling sexual activity for the time when side effects are least bothersome—or take the drug at a different time.
Taking a drug holiday. Depending on how long the drug usually remains in your body, you might stop taking it for a few days—for example, before a weekend, if that's when you hope to have sex. This isn't spontaneous, but it can work if you carefully follow your doctor's directions about how to stop and resume your medication. However, there is always a chance that this might cause a relapse, especially if it is one of the drugs that leaves your system relatively rapidly.
Switching to a different drug. Certain antidepressants, such as bupropion (Wellbutrin), and mirtazapine (Remeron) are less likely to cause sexual problems. Bupropion, which affects both norepinephrine and dopamine, can sometimes improve sexual response.
Adding a drug. For some men, taking sildenafil (Viagra) or tadalafil (Cialis) can alleviate SSRI-induced erectile dysfunction. Both men and women may benefit from adding bupropion to their treatment. This medication has been found to counter SSRI-induced sexual dysfunction, boost sexual drive and arousal, and increase the intensity or duration of an orgasm.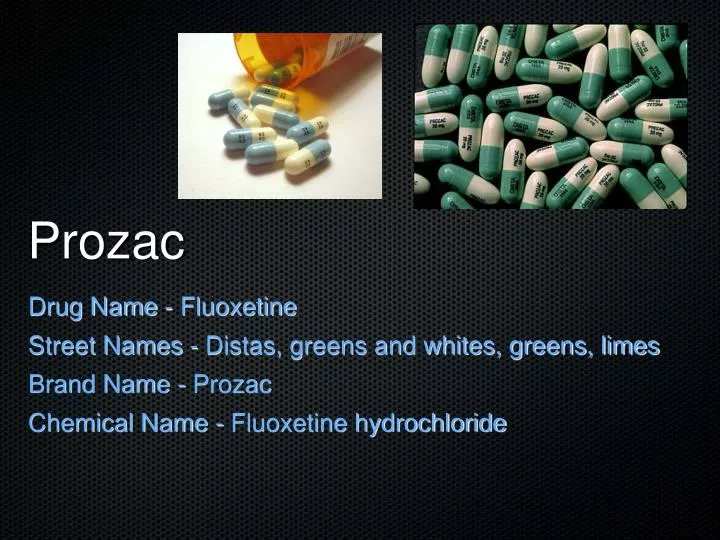 In some people, the anti-anxiety drug buspirone (BuSpar) may help increase libido and restore the ability to have an orgasm.
In some people, the anti-anxiety drug buspirone (BuSpar) may help increase libido and restore the ability to have an orgasm.
Meeting with a therapist. Even when physical issues or medication are at the root of sexual problems, psychological issues often become interwoven. For example, a few episodes of erectile dysfunction may cause a man to withdraw from sex and his partner to feel rejected. These issues can lead the couple to retreat further from intimacy. Working with a sex therapist or general therapist can help couples explore their sexual concerns, learn to better communicate, and expand their repertoire of sexual activities.
– By Julie Corliss
Executive Editor, Harvard Heart Letter
Improvement in fluoxetine-associated sexual dysfunction in patients switched to bupropion
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
. 1993 Dec;54(12):459-65.
1993 Dec;54(12):459-65.
P W Walker 1 , J O Cole, E A Gardner, A R Hughes, J A Johnston, S R Batey, C G Lineberry
Affiliations
Affiliation
- 1 Department of Psychiatry, University of Tennessee, Memphis.
- PMID: 8276736
P W Walker et al. J Clin Psychiatry. 1993 Dec.
. 1993 Dec;54(12):459-65.
Authors
P W Walker 1 , J O Cole, E A Gardner, A R Hughes, J A Johnston, S R Batey, C G Lineberry
Affiliation
- 1 Department of Psychiatry, University of Tennessee, Memphis.

- PMID: 8276736
Abstract
Background: This study was conducted to determine the effect of bupropion on the sexual functioning of male and female outpatients who developed anorgasmia or delayed orgasm while receiving fluoxetine treatment for depression.
Method: Thirty-nine patients who satisfied criteria for participation in the study discontinued fluoxetine treatment and entered a 2-week washout phase followed by an open 8-week bupropion treatment phase. Three parameters of sexual functioning were followed throughout the study: orgasm function, libido, and satisfaction with overall sexual functioning. Depression was also evaluated at each visit.
Results: All patients reported orgasm delay and/or failure at the time of fluoxetine discontinuation. Orgasm function, libido, and satisfaction with sexual functioning improved during the 2-week fluoxetine washout period and during the bupropion treatment phase. Ninety-four percent of patients (29/31) had complete or partial resolution of their orgasm dysfunction at the end of bupropion treatment, and 81% of patients (25/31) were "much" or "very much" more satisfied with their overall sexual functioning. Most patients entered the study with decreased libido on fluoxetine. Libido was "much" or "very much" increased for 81% of patients (25/31) at the end of the study. In addition, depression scores on the Hamilton Rating Scale for Depression and Clinical Global Impressions-Severity scale significantly improved during the bupropion treatment phase. Finally, bupropion was well tolerated by most patients.
Conclusion: Bupropion may be an appropriate antidepressant for patients who develop sexual dysfunction during fluoxetine treatment or for whom sexual dysfunction is a concern.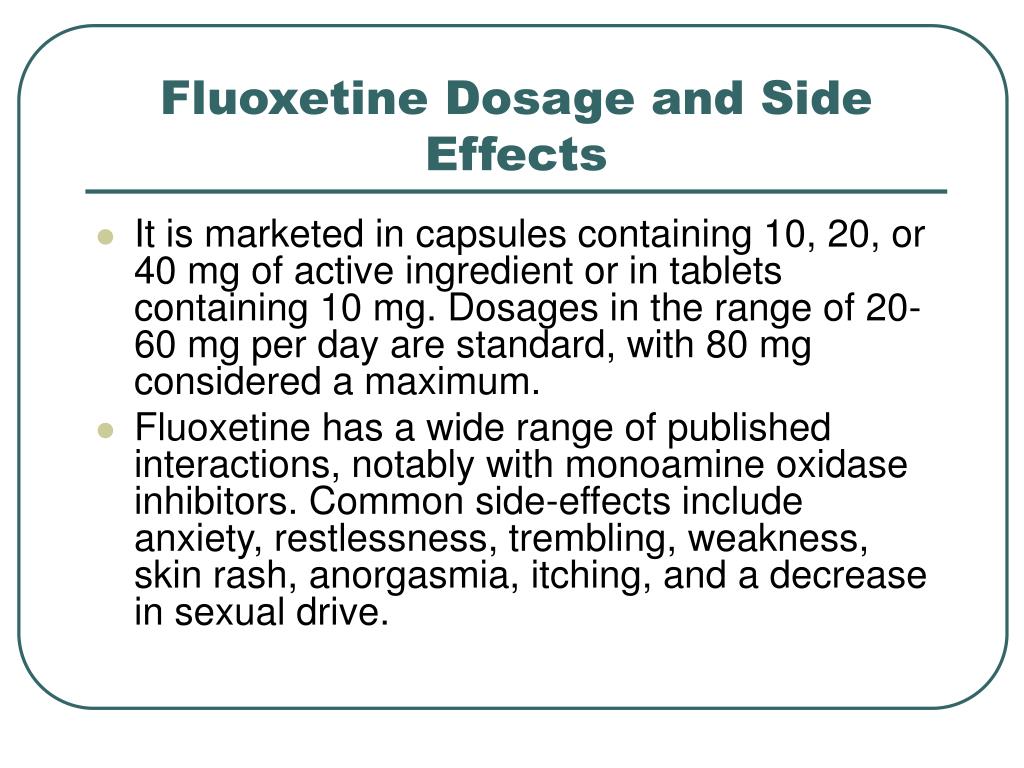
Similar articles
-
Fluoxetine-induced sexual dysfunction and an open trial of yohimbine.
Jacobsen FM. Jacobsen FM. J Clin Psychiatry. 1992 Apr;53(4):119-22. J Clin Psychiatry. 1992. PMID: 1564046 Clinical Trial.
-
Fluoxetine-induced sexual dysfunction.
Herman JB, Brotman AW, Pollack MH, Falk WE, Biederman J, Rosenbaum JF. Herman JB, et al. J Clin Psychiatry. 1990 Jan;51(1):25-7. J Clin Psychiatry. 1990. PMID: 2295587
-
Switching to moclobemide to reverse fluoxetine-induced sexual dysfunction in patients with depression.
Ramasubbu R. Ramasubbu R. J Psychiatry Neurosci.
 1999 Jan;24(1):45-50. J Psychiatry Neurosci. 1999. PMID: 9987207 Free PMC article.
1999 Jan;24(1):45-50. J Psychiatry Neurosci. 1999. PMID: 9987207 Free PMC article. -
SSRI-induced sexual dysfunction: fluoxetine, paroxetine, sertraline, and fluvoxamine in a prospective, multicenter, and descriptive clinical study of 344 patients.
Montejo-González AL, Llorca G, Izquierdo JA, Ledesma A, Bousoño M, Calcedo A, Carrasco JL, Ciudad J, Daniel E, De la Gandara J, Derecho J, Franco M, Gomez MJ, Macias JA, Martin T, Perez V, Sanchez JM, Sanchez S, Vicens E. Montejo-González AL, et al. J Sex Marital Ther. 1997 Fall;23(3):176-94. doi: 10.1080/00926239708403923. J Sex Marital Ther. 1997. PMID: 9292833 Review.
-
Antidepressant-related erectile dysfunction: management via avoidance, switching antidepressants, antidotes, and adaptation.

Labbate LA, Croft HA, Oleshansky MA. Labbate LA, et al. J Clin Psychiatry. 2003;64 Suppl 10:11-9. J Clin Psychiatry. 2003. PMID: 12971811 Review.
See all similar articles
Cited by
-
Drug-Induced Sexual Dysfunction: An Analysis of Reports to a National Pharmacovigilance Database.
Valeiro C, Matos C, Scholl J, van Hunsel F. Valeiro C, et al. Drug Saf. 2022 Jun;45(6):639-650. doi: 10.1007/s40264-022-01174-3. Epub 2022 Apr 7. Drug Saf. 2022. PMID: 35386045
-
Pharmacological Augmentation in Unipolar Depression: A Guide to the Guidelines.
Taylor RW, Marwood L, Oprea E, DeAngel V, Mather S, Valentini B, Zahn R, Young AH, Cleare AJ. Taylor RW, et al.
 Int J Neuropsychopharmacol. 2020 Dec 3;23(9):587-625. doi: 10.1093/ijnp/pyaa033. Int J Neuropsychopharmacol. 2020. PMID: 32402075 Free PMC article.
Int J Neuropsychopharmacol. 2020 Dec 3;23(9):587-625. doi: 10.1093/ijnp/pyaa033. Int J Neuropsychopharmacol. 2020. PMID: 32402075 Free PMC article. -
Frequency of Sexual Dysfunction in Patients Treated with Desvenlafaxine: A Prospective Naturalistic Study.
Montejo AL, Becker J, Bueno G, Fernández-Ovejero R, Gallego MT, González N, Juanes A, Montejo L, Pérez-Urdániz A, Prieto N, Villegas JL. Montejo AL, et al. J Clin Med. 2019 May 21;8(5):719. doi: 10.3390/jcm8050719. J Clin Med. 2019. PMID: 31117203 Free PMC article.
-
Improving reproducibility by using high-throughput observational studies with empirical calibration.
Schuemie MJ, Ryan PB, Hripcsak G, Madigan D, Suchard MA. Schuemie MJ, et al. Philos Trans A Math Phys Eng Sci.
 2018 Sep 13;376(2128):20170356. doi: 10.1098/rsta.2017.0356. Philos Trans A Math Phys Eng Sci. 2018. PMID: 30082302 Free PMC article.
2018 Sep 13;376(2128):20170356. doi: 10.1098/rsta.2017.0356. Philos Trans A Math Phys Eng Sci. 2018. PMID: 30082302 Free PMC article. -
The Black Book of Psychotropic Dosing and Monitoring.
Schatzberg AF, Charles D. Schatzberg AF, et al. Psychopharmacol Bull. 2018 Jan 15;48(1):64-153. Psychopharmacol Bull. 2018. PMID: 29382960 Free PMC article. Review. No abstract available.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Antidepressant OOO "Ozon" Fluoxetine - "Appetite, sleep, mood, libido - everything will change.
 And not the fact that for the better.
And not the fact that for the better. Before using medicines, consult a specialist.
A lot has already been written and said about fluoxetine, both good and bad. But I want to tell you about my own experience of taking it, how this medicine affected me.
I started taking it when my youngest son was three years old. It was a period of great stress for me, because the usual sitting at home was replaced by going to work and a very busy schedule. There was little time left for sleep, and waking up in the morning was like death for me. At that period of life, problems began in the relationship with her husband, which eventually led to a sad denouement. Irritability, apathy, depression came. It's like a vicious circle - when you're depressed, no one needs you. And from your own uselessness you have depression. It is almost impossible to break this circle without losses. nine0003
It was during this period of my life that I started taking Fluoxetine for the first time. The first time I took it for about three months, one tablet a day. Almost a year later, when I again felt that I was plunging into depression, I drank another course. In both cases, the medicine helped me a lot psychologically. After a week of admission, all problems and sorrows will fade into the background. An even, workable mood comes without psychosis and hysteria. I can give advice, do not drop the pills as soon as you feel better. Otherwise, all the symptoms will return (checked on myself). nine0003
The first time I took it for about three months, one tablet a day. Almost a year later, when I again felt that I was plunging into depression, I drank another course. In both cases, the medicine helped me a lot psychologically. After a week of admission, all problems and sorrows will fade into the background. An even, workable mood comes without psychosis and hysteria. I can give advice, do not drop the pills as soon as you feel better. Otherwise, all the symptoms will return (checked on myself). nine0003
My sleep cycles have normalized. More precisely, the need for sleep has become less. While taking Fluoxetine, I sleep 6-7 hours, get enough sleep, and easily jump up at the first wake-up call. By the way, many in their reviews wrote that strange dreams were beginning to occur, I personally had no effect on dreams. Rarely dreamed at all at least something. Probably because I was very tired during the day.
Appetite has really decreased. At the time of the first course, I had problems with being overweight (about 82 kg with a height of 170 cm), and I really lost a little weight - not radically, but the effect was. The need for food (as well as for sleep) at the time of taking the drug has become less. I didn’t want sweets so much, I began to calmly walk past my favorite bakery with fresh pastries, and at the same time I didn’t feel any suffering. nine0003
The need for food (as well as for sleep) at the time of taking the drug has become less. I didn’t want sweets so much, I began to calmly walk past my favorite bakery with fresh pastries, and at the same time I didn’t feel any suffering. nine0003
Libido has also decreased. So, if you live a regular sex life, be prepared that its quality may decline.
But like all antidepressants, fluoxetine has a temporary effect. And if during the time you are taking it, you do not take any steps to radically change your life, then depression will return. And it is impossible to eat it with pills all your life without consequences for your health.
tani1309recommends
Read all reviews 104
Other reviews
Read all reviews 104
See also
Featured reviews
Antidepressant-related sexual dysfunction
… this problem is widely underestimated and very rarely addressed in consultations.
Unfortunately …
Major depressive disorder (MDD) affects about 6% of men and 18% of women. The lifetime risk of the disease is 7-12% for men and 20-25% for women. In somatic patients, the prevalence of depression reaches 20-35% and is comparable to the prevalence of arterial hypertension or even exceeds it. The risk of depression is highest in patients with medical conditions (eg, cardiovascular disease, diabetes mellitus and other endocrine disorders, cancer, HIV/AIDS, and hepatitis C). Targeted screening reveals depression in 45 to 95% (average - 69%) of patients seeking medical help for somatic symptoms. It is the sole reason for 10 - 20% of visits to general practitioners. The prevalence of depression among patients with severe somatic diseases reaches 20-60%. In the global structure of the disease burden (death + disability), MDD is 4.4% and is in fourth place among all pathologies. It is predicted that by 2020 they will move to second place after coronary artery disease. One should also keep in mind such widespread diseases in the population as panic disorder, adjustment disorder, anxious depression, phobic and anxiety disorder, chronic pain (chronic pain disorder), etc., which are also accompanied by depressive symptoms and have some common etio-pathogenetic ( neurotransmitter) mechanisms with MDD. nine0003
One should also keep in mind such widespread diseases in the population as panic disorder, adjustment disorder, anxious depression, phobic and anxiety disorder, chronic pain (chronic pain disorder), etc., which are also accompanied by depressive symptoms and have some common etio-pathogenetic ( neurotransmitter) mechanisms with MDD. nine0003
Fortunately …
Doctors have at their disposal drugs that can stop or significantly reduce the manifestations of depressive symptoms - antidepressants depressive disorder). The effectiveness of antidepressants in major depression has been proven in numerous placebo-controlled studies, in the aggregate covering tens of thousands of patients (on average, antidepressants are effective in 55-65% of patients). Antidepressants have a selective effect on depression (and anxiety symptoms), that is, they improve mood, reduce or relieve melancholy, lethargy, apathy, anxiety and emotional stress, increase mental activity, normalize the phase structure and duration of sleep, appetite. The main effect of antidepressants is that they block the breakdown of monoamines (serotonin, norepinephrine, dopamine, phenylethylamine, etc.) under the action of monoamine oxidases (MAO) or block the neuronal reuptake of monoamines, as a result of which the concentration of these mediators in the synaptic cleft increases, due to this, their effects are enhanced (according to modern concepts, one of the leading mechanisms for the development of depression is the lack of monoamines in the synaptic cleft - especially serotonin and dopamine). nine0003
The main effect of antidepressants is that they block the breakdown of monoamines (serotonin, norepinephrine, dopamine, phenylethylamine, etc.) under the action of monoamine oxidases (MAO) or block the neuronal reuptake of monoamines, as a result of which the concentration of these mediators in the synaptic cleft increases, due to this, their effects are enhanced (according to modern concepts, one of the leading mechanisms for the development of depression is the lack of monoamines in the synaptic cleft - especially serotonin and dopamine). nine0003
Unfortunately …
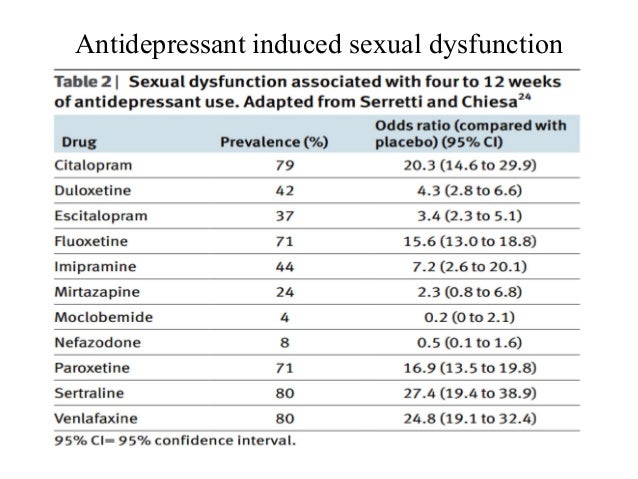
Most antidepressants are described - more or less pronounced - disorders of sexual function (sexual dysfunction - SDP): decrease and loss of libido, impotence, erectile dysfunction, priapism, lubrification disorders, clitoral disorders, retention or inhibition of ejaculation / orgasm, painful retrograde ejaculation, anorgasmia, partial or complete, dyspareunia and vaginismus, vaginal or penile anesthesia, decreased sexual satisfaction, etc. For example, tricyclic antidepressants (TCAD), having a wide range of effects on neurotransmitter systems and their receptors (serotonin-, norepinephrine- and dopaminergic, blocking α1-adrenergic and h2-histamine receptors, anticholinergic effect on peripheral and central Ach M1 receptors) mainly reduce sexual arousal, as well as desire, cause anorgasmia (delayed or painful ejaculation), and selective inhibitors Serotonin reuptake ryers (SSRIs), by increasing the content of serotonin in the blood, reduce sexual activity, cause anorgasmia and delayed ejaculation. Mood stabilizers - lithium salts - have negative effects on sexual function due to the development of hypothyroidism, weight gain, slowing down of thought processes. Trazodone inhibits serotonin reuptake and acts as a 5-HT2a and 5-HT2c receptor antagonist. It has very few undesirable effects on sexual function, but can sometimes be the cause of priapism. nine0003
For example, tricyclic antidepressants (TCAD), having a wide range of effects on neurotransmitter systems and their receptors (serotonin-, norepinephrine- and dopaminergic, blocking α1-adrenergic and h2-histamine receptors, anticholinergic effect on peripheral and central Ach M1 receptors) mainly reduce sexual arousal, as well as desire, cause anorgasmia (delayed or painful ejaculation), and selective inhibitors Serotonin reuptake ryers (SSRIs), by increasing the content of serotonin in the blood, reduce sexual activity, cause anorgasmia and delayed ejaculation. Mood stabilizers - lithium salts - have negative effects on sexual function due to the development of hypothyroidism, weight gain, slowing down of thought processes. Trazodone inhibits serotonin reuptake and acts as a 5-HT2a and 5-HT2c receptor antagonist. It has very few undesirable effects on sexual function, but can sometimes be the cause of priapism. nine0003
However, it should be taken into account that assessment of the true contribution of antidepressants to the development of PDD is difficult, since depressive disorder is classically associated with sexual dysfunction. For example, depression is characterized by a loss of the ability to experience joy (anhedonia) in almost all areas of life, including libido. Loss of interest in sexuality has been reported in approximately 70% of patients with unipolar depression and in approximately 75% of patients with bipolar disorder. nine0003
For example, depression is characterized by a loss of the ability to experience joy (anhedonia) in almost all areas of life, including libido. Loss of interest in sexuality has been reported in approximately 70% of patients with unipolar depression and in approximately 75% of patients with bipolar disorder. nine0003
Fortunately …
Currently, there are a number of methods that can limit the adverse effects of drugs, including antidepressants, on sexual function. Important questions such as general satisfaction with sexual life and the nature of sexual problems (decreased desire, problems with erection/lubrification, orgasm, ejaculation, frequency of sexual intercourse and/or masturbation) should be clarified with the patient before prescribing treatment aimed at eliminating PDP. In patients receiving antidepressants for whom sexual function is essential, treatment must be carefully selected. If possible, antidepressants that do not activate the serotonin system should be prescribed; in this case, bupropion, mirtazapine, or trazodone may be the first choice. If the therapeutic effect on serotonin receptors is important, duloxetine is prescribed. nine0003
If the therapeutic effect on serotonin receptors is important, duloxetine is prescribed. nine0003
The following approaches are available for treating sexual side effects of antidepressants:
► 1 . Wait out the period of adaptation to the side effects of the drug. Improved mood may be associated with a more satisfying sex life. This approach is rarely used due to the fact that only 10% of patients develop tolerance to the side effects of antidepressants; usually ineffective against anorgasmia induced by TCAD; can be applied to patients with low frequency of sexual activity. nine0003
► 2 . Reduce dose. This approach is almost never used. The main problem is to find a dose that will reduce the side effects on the sexual sphere without causing symptoms of depression.
► 3 . Plan sexual activity before taking an antidepressant. This means that the drug is prescribed immediately after sexual activity, for example, before bedtime. This tactic may only be useful for antidepressants with a short half-life. nine0003
nine0003
► 4 . Temporarily stop the drug. You can partially reduce the dose of the antidepressant or stop taking it for several days (for example, from Friday evening to Sunday morning) and consider sexual activity at the end of this period. This approach may be effective for drugs with a short half-life (eg, paroxetine, sertraline) and not at all effective for drugs with a long half-life, such as fluoxetine (Prozac).
► 5 . Change antidepressant. This tactic has been described as the most successful. SSRIs can be replaced by bupropion or mirtazapine, which rarely cause PDP. However, changing the antidepressant does not always achieve such a therapeutic effect and is associated with other side effects, such as weight gain. For patients with anxiety, an alternative would be to switch to duloxetine, an antidepressant that responds to depression with anxiety and causes the least negative effect on sexual function. nine0003
► 6 . Apply correctors. The use of corrective treatment is by far the most commonly used tactic in clinical practice.