How to deal with an ocd person
International OCD Foundation | Living With Someone Who Has OCD. Guidelines for Family Members
(From Learning to Live with OCD)
By Barbara Van Noppen, PhD and Michele Pato, MD
This article was initially published in the Spring 2009 edition of the OCD Newsletter.
In an effort to strengthen relationships between individuals with OCD and their family members, and to promote understanding and cooperation within households, we have developed the following list of useful guidelines. These guidelines are meant as tools for family members to be tailored for individual situations, sometimes more powerfully employed with the help of a therapist with expertise in working with OCD.
1. Recognize Signals
The first guideline stresses that family members learn to recognize the “warning signals” of OCD. Sometimes people with OCD are thinking things you don’t know about as part of the OCD, so watch for behavior changes. It is important to not dismiss significant behavioral changes as “just their personality. ” Remember that these changes can be gradual, but overall different from how the person has generally behaved in the past.
Signals to watch for include but are not limited to:
- Large blocks of unexplained time that the person is spending alone (in the bathroom, getting dressed, doing homework, etc.)
- Doing things again and again (repetitive behaviors)
- Constant questioning of self-judgment; excessive need for reassurance
- Simple tasks taking longer than usual
- Perpetual tardiness
- Increased concern for minor things and details
- Severe and extreme emotional reactions to small things
- Inability to sleep properly
- Staying up late to get things done
- Significant change in eating habits
- Daily life becomes a struggle
- Avoidance
- Increased irritability and indecisiveness
People with OCD usually report that their symptoms get worse the more they are criticized or blamed because these emotions generate more anxiety. So it is essential that you learn to view these features as signals of OCD and not as personality traits. This way you can join the person with OCD to combat the symptoms, rather than become alienated from them.
So it is essential that you learn to view these features as signals of OCD and not as personality traits. This way you can join the person with OCD to combat the symptoms, rather than become alienated from them.
2. Modify Expectations
People with OCD consistently report that change of any kind, even positive change can be experienced as stressful. It is often during these times that OC symptoms tend to flare up; however, you can help to moderate stress by modifying your expectations during these times of transition. Family conflict only fuels the fire and promotes symptom escalation, (“Just snap out of it!’). Instead a statement such as “No wonder your symptoms are worse— look at the changes you are going through,” is validating, supportive and encouraging. Remind yourself the impact of change will also change; that is the person with OCD has survived many ups and downs, and set backs are not permanent. You must adjust your expectations accordingly which does not mean to not expect something!
3.
 Remember That People Get Better at Different Rates
Remember That People Get Better at Different Rates There is a wide variation in the severity of OC symptoms between individuals. Remember to measure progress according to the individual’s own level of functioning, not to that of others. You should encourage the person to push him/herself and to function at the highest level possible; yet if the pressure to function “perfectly” is greater than a person’s actual ability it creates more stress which leads to more symptoms. Just as there is a wide variation between individuals regarding the severity of their OC symptoms, there is also wide variation in how rapidly individuals respond to treatment. Be patient. Slow, gradual improvement may be better in the end if relapses are to be prevented.
4. Avoid Day-To-Day Comparisons
You might hear your loved ones say they feel like they are “back at the start” during symptomatic times. Or you might be making the mistake of comparing your family member’s progress (or lack thereof) with how he/she functioned before developing OCD. It is important to look at overall changes since treatment began. Day-to-day comparisons are misleading because they don’t represent the bigger picture. When you see “slips” a gentle reminder of “tomorrow is another day to try” can combat self destructive labeling of “failure,” “imperfect,” or “out of control” which could result in a worsening of symptoms! You can make a difference with reminders of how much progress has been made since the worst episode and since beginning treatment. Encourage the use of questionnaires to have an objective measure of progress that both you and your loved one can refer back to (for example, the Yale Brown Obsessive Compulsive Scale) Even a 1-10 rating scale can be helpful. Ask “How would you rate yourself when OCD was at it’s worst? When was that? How is it today? Let’s think about this again in a week.”
It is important to look at overall changes since treatment began. Day-to-day comparisons are misleading because they don’t represent the bigger picture. When you see “slips” a gentle reminder of “tomorrow is another day to try” can combat self destructive labeling of “failure,” “imperfect,” or “out of control” which could result in a worsening of symptoms! You can make a difference with reminders of how much progress has been made since the worst episode and since beginning treatment. Encourage the use of questionnaires to have an objective measure of progress that both you and your loved one can refer back to (for example, the Yale Brown Obsessive Compulsive Scale) Even a 1-10 rating scale can be helpful. Ask “How would you rate yourself when OCD was at it’s worst? When was that? How is it today? Let’s think about this again in a week.”
5. Recognize “Small” Improvements
People with OCD often complain that family members don’t understand what it takes to accomplish something, such as cutting down a shower by five minutes, or resisting asking for reassurance one more time. While these gains may seem insignificant to family members, it is a very big step for your loved one. Acknowledgment of these seemingly small accomplishments is a powerful tool that encourages them to keep trying. This lets them know that their hard work to get better is being recognized and can be a powerful motivator.
While these gains may seem insignificant to family members, it is a very big step for your loved one. Acknowledgment of these seemingly small accomplishments is a powerful tool that encourages them to keep trying. This lets them know that their hard work to get better is being recognized and can be a powerful motivator.
6. Create a Supportive Environment
The more you can avoid personal criticism the better – remember that it is the OCD that gets on everyone’s nerves. Try to learn as much about OCD as you can. Your family member still needs your encouragement and your acceptance as a person, but remember that acceptance and support does not mean ignoring the compulsive behavior. Do your best to not participate in the compulsions. In an even tone of voice explain that the compulsions are symptoms of OCD and that you will not assist in carrying them out because you want them to resist as well. Gang up on the OCD, not on each other!
7. Set Limits, But Be Sensitive to Mood (refer to #14)
With the goal of working together to decrease compulsions, family members may find that they have to be firm about:
- Prior agreements regarding assisting with compulsions;
- How much time is spent discussing OCD;
- How much reassurance is given; or
- How much the compulsions infringe upon others’ lives.

It is commonly reported by individuals with OCD that mood dictates the degree to which they can divert obsessions and resist compulsions. Likewise, family members have commented that they can tell when someone with OCD is “having a bad day.” Those are the times when family may need to “back off,” unless there is potential for a life-threatening or violent situation. On “good days” individuals should be encouraged to resist compulsions as much as possible. Limit setting works best when these expectations are discussed ahead of time and not in the middle of a conflict. It is critical to minimize family accommodation to OCD.
8. Support Taking Medication as Prescribed
Be sure to not undermine the medication instructions that have been prescribed. All medications have side effects that range in severity. Ask your family member if you could periodically attend their appointments with the prescribing physician. In this way you can ask questions learn about side effects and report any behavioral changes that you notice
9.
 Keep Communication Clear and Simple
Keep Communication Clear and Simple Avoid lengthy explanations. This is often easier said than done because most people with OCD constantly ask those around them for reassurance. “Are you sure I locked the door?” or “Did I really clean well enough?” You have probably found that the more you try to prove that the individual need not worry the more he disproves you. Even the most sophisticated explanations won’t work. There is always that lingering “What if?” Tolerating this uncertainty is an exposure for the individual with OCD and it may be tough. Recognize that the person with OCD is triggered by doubt, label the problem as one of trying to gain total certainty about something that cannot be provided, this is the essence of OCD and the goal is to accept uncertainty in life. Avoid lengthy rationales and debates.
10. Separate Time Is Important
Family members often have the natural tendency to feel like they should protect the individual with OCD by being with him all the time. This can be destructive because family members need their private time, as do people with OCD. Give them the message that they can be left alone and can care for themselves. Also, OCD cannot run everybody’s life; you have other responsibilities besides “babysitting.” You need and deserve time to pursue your interests too! This not only keeps you from resenting the OCD it is also a good role model to the person with the OCD that there is more to life than anxiety.
This can be destructive because family members need their private time, as do people with OCD. Give them the message that they can be left alone and can care for themselves. Also, OCD cannot run everybody’s life; you have other responsibilities besides “babysitting.” You need and deserve time to pursue your interests too! This not only keeps you from resenting the OCD it is also a good role model to the person with the OCD that there is more to life than anxiety.
11. It Has Become All About the OCD!
Whether it is about asking and providing reassurance to the family member with OCD or talking about the desperation and anxiety that the illness causes, families struggle with the challenge of engaging in conversations that are “symptom free,” an experience that feels liberating when achieved. We have found that it is often difficult for family members to stop engaging in conversations around the anxiety because it has become a habit and such a central part of their life. It is okay not to ask ”How is your OCD today?” Some limits on talking about OCD and the various worries is an important part of establishing a more normative routine. It also makes a statement that OCD is not allowed to run the household.
It also makes a statement that OCD is not allowed to run the household.
12. Keep Your Family Routine “Normal”
Often families ask how to undo all of the effects of months or years of going along with OC symptoms. For example, to “keep the peace” a husband allowed his wife’s contamination fear to prohibit their children from having any friends into the household. An initial attempt to avoid conflict by giving in just grows; however, obsessions and compulsions must be contained. It is important that children have friends in their home, or that family members use any sink, sit on any chair, etc. Through negotiation and limit setting, family life and routines can be preserved. Remember it is in the individual’s best interest to tolerate the exposure to their fears and to be reminded of others’ needs. As they begin to regain function, their wish to be able to do more increases.
13. Be Aware of Family Accommodation Behaviors (refer to #14)
First there must be an agreement between all parties that it is in everyone’s best interest for family members to not participate in rituals (Family Accommodation Behaviors).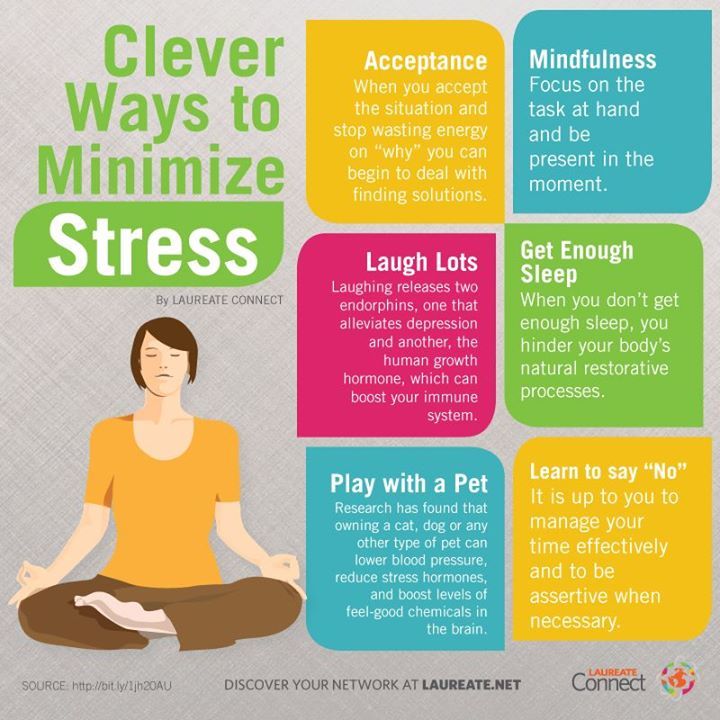 However, in this effort to help your loved one reduce compulsive behavior, you may be easily perceived as being mean or rejecting, even though you are trying to be helpful. It may seem obvious that family members and individuals with OCD are working toward the common goal of symptom reduction but the ways in which people do this varies. Attending a family educational support group for OCD, or seeing a family therapist with expertise in OCD, often facilitates family communication.
However, in this effort to help your loved one reduce compulsive behavior, you may be easily perceived as being mean or rejecting, even though you are trying to be helpful. It may seem obvious that family members and individuals with OCD are working toward the common goal of symptom reduction but the ways in which people do this varies. Attending a family educational support group for OCD, or seeing a family therapist with expertise in OCD, often facilitates family communication.
14. Consider Using a Family Contract
The primary objective of a family contract is to get family members and individuals with OCD to work together to develop realistic plans for managing the OC symptoms in behavioral terms. Creating goals as a team reduces conflict, preserves the household, and provides a platform for families to begin to “take back” the household in situations where most routines and activities have been dictated by an individual’s OCD. By improving communication, and developing a greater understanding of each other’s perspective, it is easier for the individual to have family members help them to reduce OC symptoms instead of enable. It is essential that all goals are clearly defined, understood, and agreed upon by any family members involved with carrying out the tasks in the contract. Families who decide to enforce rules, without discussing it with the person with OCD first, find that their plans tend to backfire. Some families are able to develop a contract by themselves, while most need some professional guidance and instruction. Be sure to reach out for professional assistance if you think that you could benefit from it.
It is essential that all goals are clearly defined, understood, and agreed upon by any family members involved with carrying out the tasks in the contract. Families who decide to enforce rules, without discussing it with the person with OCD first, find that their plans tend to backfire. Some families are able to develop a contract by themselves, while most need some professional guidance and instruction. Be sure to reach out for professional assistance if you think that you could benefit from it.
Barbara Livingston Van Noppen, PhD is an Associate Professor in the Department of Psychiatry and Human Behavior and Assistant Chair of Education Keck School of Medicine University of Southern California.Dr. Van Noppen provides CBT supervision and didactic education to psychiatric residents in the USC Keck School of Medicine program.
Michele Tortora Pato, MD is the Della Martin Chair in Psychiatry and Associate Dean for Academic Scholarship at the Keck School of Medicine-USC.
Back to Expert Opinions
International OCD Foundation | Families: “What Can I Do to Help?”
By Barbara Van Noppen, PhD and Michele Pato, MD
Finally, after years of not knowing where to turn, someone has given it a name. A family member has been diagnosed as having Obsessive Compulsive Disorder (OCD) and you want to learn all you can about the disorder. Caring about your loved one with OCD, you have undoubtedly wondered “What can I do to help?”
After years of working with families who have a member with OCD, we have found some repetitive themes: feelings of isolation, frustration, shame, even guilt. Families wonder, “Why don’t they just stop?” Foremost, is a plea for help, “What should we do?” Family members usually feel distraught, bewildered, overwhelmed and frustrated. In an effort to help, you have probably tried to demand that the person with OCD stop his/her “silly,” “ridiculous” behavior. Or, at the other extreme, you have assisted him/her with rituals or actually performed compulsions, such as hand washing or checking, just to “keep the peace” (known as Family Accommodation). Either extreme has a disruptive effect on your family’s functioning, results in family member stress, and can lead to an increase in obsessive-compulsive symptoms. Family conflict inevitably results. As your attempts to “help” the person with OCD are rejected or ineffective you begin to feel helpless or impotent. Below are four suggestions about how you can be helpful to your family member:
Either extreme has a disruptive effect on your family’s functioning, results in family member stress, and can lead to an increase in obsessive-compulsive symptoms. Family conflict inevitably results. As your attempts to “help” the person with OCD are rejected or ineffective you begin to feel helpless or impotent. Below are four suggestions about how you can be helpful to your family member:
- Become educated about OCD.
- Learn to recognize and reduce “Family Accommodation.”
- Help your family member find appropriate, effective treatment by a qualified professional.
- Learn strategies about how to respond if your family member refuses treatment.
Getting Educated
Education is the first step. Learn as much about OCD as you can: read books, join the Obsessive Compulsive Foundation (www.ocfoundation.org), find out if the state you live in has an OCF affiliate, attend OCD support groups, research online, etc. As you learn more about the disorder, you begin to feel hopeful that you can do things to help the person with OCD overcome their disorder. OCD is a biochemically-based disorder with clinical symptoms that go beyond personality traits. As your understanding increases, you will be able to view the irrational behaviors from a non-personalized perspective. If you have been neglecting yourself, engage in self-care that will impact your ability to problem solve and respond to your family member more constructively. Your family relationships will improve and the person with OCD will feel more supported. Positive family relationships and feeling understood greatly enhance the therapeutic benefits of treatment.
OCD is a biochemically-based disorder with clinical symptoms that go beyond personality traits. As your understanding increases, you will be able to view the irrational behaviors from a non-personalized perspective. If you have been neglecting yourself, engage in self-care that will impact your ability to problem solve and respond to your family member more constructively. Your family relationships will improve and the person with OCD will feel more supported. Positive family relationships and feeling understood greatly enhance the therapeutic benefits of treatment.
Recognizing and Reducing Family Accommodation Behaviors
Families are constantly affected by the demands of OCD. Results from research investigating family and OCD suggest that family responses may play a role in maintaining or even facilitating OCD symptoms. The more that family members can learn about their responses to OCD and the impact that their responses have on the person with OCD, the more the family becomes empowered to make a difference! Consider the following responses you might engage in when responding to your family member’s struggle with OCD symptoms.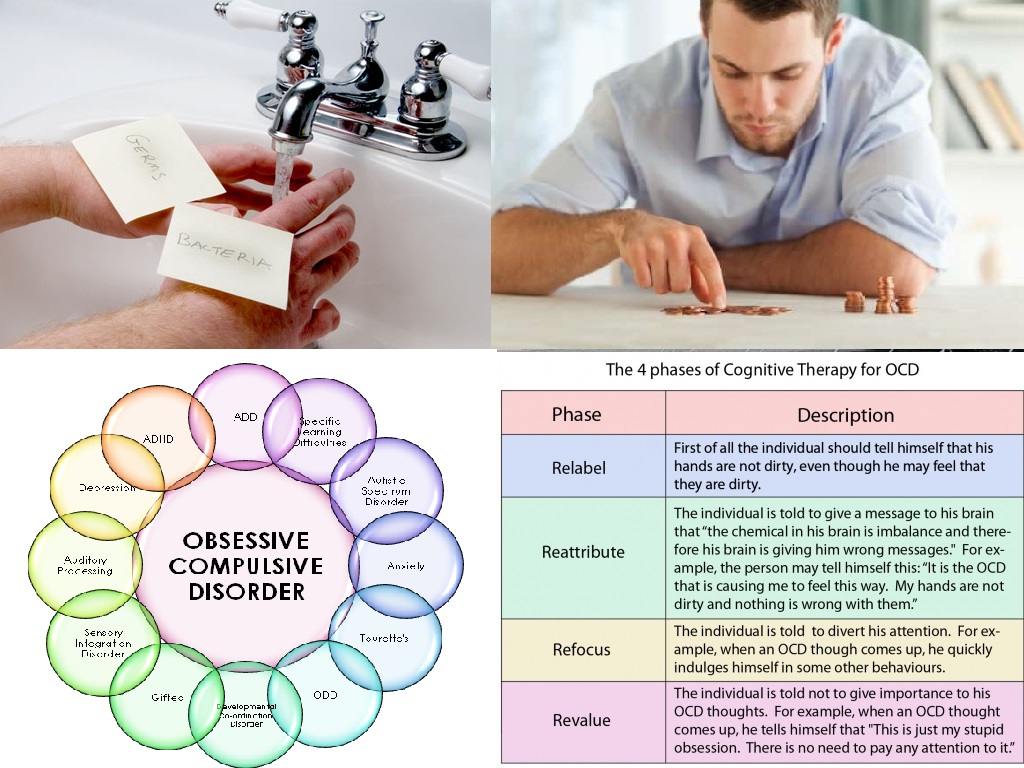 Is this is something you never do, do sometimes, or do all of the time?:
Is this is something you never do, do sometimes, or do all of the time?:
- Participate in the OCD behavior. You participate in your family member’s OCD behavior along with them. For example, washing your hands whenever they wash their hands or ask you to wash your hands; providing excessive reassurance; performing extensive checking rituals.
- Assist in avoidance behavior. You help your family member avoid things that upset them. For example, doing their laundry for them and following prescribed orders so it is done the “right” way; opening doors, handling raw meet, changing diapers.
- Facilitate symptomatic behavior/rituals. You do things for your family member that allows them to engage in symptomatic behavior. For example, buying excessive amounts of cleaning products for them, providing extra storage space for hoarding.
- Modifying Family Routine. For example, you change the time of day that you shower or when you change your clothes in order to accommodate your family members’ OCD demands that seem to take precedence.
- Take on Extra Responsibilities of Others. For example, going out of your way to drive the person with OCD places when they could otherwise drive themselves, but feel unable due to OCD fears or anxiety, doing homework or other household chores for the person.
- Modify Leisure Activities. For example, your family member encourages you to not leave the house without them. This type of modification interferes with your interests in movies, dinners out, time with friends, etc. Another example of this is complying with the request not to have company over due to disruption in OCD rituals.
- Interference in Work Functioning. For example, you cut back on hours at your job in order to take care of your family member go in late because of assisting the person with OCD.
Parents have often talked to us about the fact that they give in to unreasonable demands because their son/daughter is so unhappy most of the time, and because they themselves feel so powerless over the symptoms. We have worked with families that go out at midnight to buy fast food or cleaning supplies for a son or daughter who has OCD because he/she demanded it and the parents felt it could make them more comfortable and or happy. Although understandable this type of accommodation only inflates the person’s sense of power and control and can be detrimental to normal child and adolescent development. Blaming family members is unproductive. Rather, family members can learn how to become involved in the treatment in OCD and may play a critical role in facilitating improvement in functioning, as opposed to enabling the continuation of symptoms. By learning supportive behaviors that extract you from the compulsions as a family member, you can make a difference in the course of your loved one’s symptoms and in their life!
We have worked with families that go out at midnight to buy fast food or cleaning supplies for a son or daughter who has OCD because he/she demanded it and the parents felt it could make them more comfortable and or happy. Although understandable this type of accommodation only inflates the person’s sense of power and control and can be detrimental to normal child and adolescent development. Blaming family members is unproductive. Rather, family members can learn how to become involved in the treatment in OCD and may play a critical role in facilitating improvement in functioning, as opposed to enabling the continuation of symptoms. By learning supportive behaviors that extract you from the compulsions as a family member, you can make a difference in the course of your loved one’s symptoms and in their life!
What to do Instead
It has been our observation that education and an emotional understanding of what it is like to experience the symptoms of OCD should accompany the family’s efforts to intervene. Since many people with OCD are otherwise very functional it is no wonder that you may tend to see the compulsions as behaviors that are within the person’s control to initiate or cease. This is a common misunderstanding. Coming to terms with the reality that your family member has “something wrong” with him/her which requires professional attention can be a painful process. Before you can effectively help, you must acknowledge the OCD and learn about it. You must know what the problem is before beginning to solve it!
Since many people with OCD are otherwise very functional it is no wonder that you may tend to see the compulsions as behaviors that are within the person’s control to initiate or cease. This is a common misunderstanding. Coming to terms with the reality that your family member has “something wrong” with him/her which requires professional attention can be a painful process. Before you can effectively help, you must acknowledge the OCD and learn about it. You must know what the problem is before beginning to solve it!
If you have been an “accomplice” in the OCD and now recognize, this gently withdraw and hold the line, explaining that your continual involvement (accommodation) only worsens the disorder. On the other hand, if you have refused to have anything to do with the OCD besides yelling “knock it off,” you must stop that too and learn more so that you can say the same thing, but in a way that feels more supportive and shows your understanding of the struggle the person with OCD is experiencing. In any case it is essential to be consistent. This may mean talking with other family members to ensure a unified approach, otherwise your good intentions could be undermined. For example, in one family the mother stopped doing the laundry for her 28 year old son but her husband did it instead because they did not have an agreed upon plan on how to handle the OCD symptoms.
In any case it is essential to be consistent. This may mean talking with other family members to ensure a unified approach, otherwise your good intentions could be undermined. For example, in one family the mother stopped doing the laundry for her 28 year old son but her husband did it instead because they did not have an agreed upon plan on how to handle the OCD symptoms.
Helping Your Loved One Find the Right Treatment
Experienced clinicians agree that a multimodal treatment approach that includes medication, behavior therapy, and family education and support is optimal.
Medication
Several medications are available which have a beneficial effect for individuals with OCD. Medications that are typically tried first are ones that affect a chemical in your brain called serotonin. We believe that serotonin levels in the brain are associated with OCD. A number of these medications are marketed as antidepressants as well. This is fortunate since many patients with OCD additionally suffer with symptoms of depression including loss of interest and energy, poor concentration, difficulty with sleep, diminished sex drive, perhaps even suicidal thoughts. It is not always clear if these symptoms are secondary to the OCD, that is, depression in response to living with OCD or a separate illness (primary depression). Fortunately, the medications prescribed treat both the OC and the depressive symptoms.
It is not always clear if these symptoms are secondary to the OCD, that is, depression in response to living with OCD or a separate illness (primary depression). Fortunately, the medications prescribed treat both the OC and the depressive symptoms.
It is important for people with OCD and family members to recognize that medication alone rarely takes away all the symptoms. Adding other treatment modalities helps the person with OCD to better control their symptoms. To date, it appears that medication only works to control and not to “cure” symptoms in most cases. Again, contrary to popular belief, medication by itself hardly ever completely obliterates the symptoms of OCD. When the medications are effective, most people with OCD say that it helps them to dismiss the worries and resist the compulsions more easily. Some effort by the person with OCD is necessary to decrease symptoms and medication may help to facilitate this process. Studies show that without cognitive behavior therapy, when the medication is stopped, symptoms usually return within several weeks and it once again becomes more difficult to resist urges to perform compulsions. Adding cognitive behavioral therapy particularly exposure and response prevention (ERP) offers the best hope of getting by with less medication or no medication in the long run.
Adding cognitive behavioral therapy particularly exposure and response prevention (ERP) offers the best hope of getting by with less medication or no medication in the long run.
Exposure and Response Prevention Therapy – The Gold Standard
Cognitive behavior therapy (CBT) is the clinically researched and proven effective treatment of choice for OCD, whether with or without medication. In particular for OCD, exposure and response prevention (ERP) is the potent ingredient of CBT. To proceed with ERP one must first generate a list of feared or avoided situations objects thoughts images or impulses that evoke distress. To decrease symptoms, people with OCD must expose themselves directly to those situations that are feared or avoided in a stepwise fashion, starting with the less distressing trigger and working up. Next, the person needs to be encouraged to resist or at least delay the compulsions they feel must be performed because of a feared consequence or heightened anxiety. This part is called “response prevention” As exposure and response prevention is practiced over and over the person with OCD learns that “nothing bad happens” when the rituals are resisted and his or her anxiety starts to decrease on its own (“habituation”). Be aware that exposure and response prevention often evokes an initial increase in anxiety. However, if the person sticks with response prevention, their anxiety will eventually come down. We have had patients and family members return to a session complaining that the OCD seems worse and that the treatment is not working. Although compulsions may decrease rapidly, anxiety and often obsessions can increase in the short term. It takes longer for anxiety and obsessions to extinguish. Persistence and repetition are essential.
This part is called “response prevention” As exposure and response prevention is practiced over and over the person with OCD learns that “nothing bad happens” when the rituals are resisted and his or her anxiety starts to decrease on its own (“habituation”). Be aware that exposure and response prevention often evokes an initial increase in anxiety. However, if the person sticks with response prevention, their anxiety will eventually come down. We have had patients and family members return to a session complaining that the OCD seems worse and that the treatment is not working. Although compulsions may decrease rapidly, anxiety and often obsessions can increase in the short term. It takes longer for anxiety and obsessions to extinguish. Persistence and repetition are essential.
ERP takes annormous amount of practice and patience as well as a strong sense of motivation to tolerate increasingly high levels of anxiety. A good analogy for exposure and response prevention is exercise. When a person begins to run for example, they start off at a slow pace and a small distance. As strength and endurance is built, greater distances can be covered at faster paces. Sore muscles along they way are interpreted as signs of good use in areas that were lacking conditioning. Have you ever heard anyone say they are giving up exercise because their muscles were sore and that it must be bad for them?
When a person begins to run for example, they start off at a slow pace and a small distance. As strength and endurance is built, greater distances can be covered at faster paces. Sore muscles along they way are interpreted as signs of good use in areas that were lacking conditioning. Have you ever heard anyone say they are giving up exercise because their muscles were sore and that it must be bad for them?
As a person begins ERP an initial increase in anxiety is often viewed as “I must be doing something wrong because this is supposed to make me feel better,” instead of ,”This anxiety is a good sign that I’m confronting the things that make me distressed, so I will feel more uncomfortable at first.” Too often people stop behavioral treatment because of the initial increase in anxiety, unaware that the habituation process takes time to occur. Compared to the length of time someone is symptomatic with OCD, decreases in distress and compulsions occur quite quickly with consistent use of exposure and response prevention. Despite this, most people are impatient and expect the worries to go away more speedily than is realistic. Even after compulsions stop, worries will linger because behaviors change faster than thoughts and feelings. Understanding all of this helps you as a support person to be a better coach.
Despite this, most people are impatient and expect the worries to go away more speedily than is realistic. Even after compulsions stop, worries will linger because behaviors change faster than thoughts and feelings. Understanding all of this helps you as a support person to be a better coach.
Family Therapy
Family intervention is an important adjunct to medication and behavioral treatment. One format that has been effective is the multifamily psycho-educational group. This can follow a support group format or be run by a professional (this is called Multi-Family Behavioral Treatment or MFBT). The intention of these groups is to gather together individuals with OCD, along with their family members, for the purpose of learning about OCD, its impact on the family, and strategies to cope. A group format provides a rare opportunity for family members and individuals with OCD to feel less isolated and less estranged. It is an empowering process to learn about OCD, share similar experiences and discuss alternative problem-solving approaches. You will feel relieved to know that others are struggling with the same fears concerns questions and conflicts related to OCD.
You will feel relieved to know that others are struggling with the same fears concerns questions and conflicts related to OCD.
What to Do If They Refuse Treatment
I have received calls and letters describing perhaps the most difficult situation, when you have a family member who absolutely refuses any treatment or may even deny that the symptoms of a disorder exist. These are extremely trying situations that evoke feelings of despair. Sometimes you may have no choice left but to carry on with your life while reminding the sufferer periodically that you are willing to help, that you recognize their shame and distress, and that people get better from OCD. In general, people with OCD cannot begin behavioral or medication treatment unless they are willing to, or the stakes are so high that it acts as a motivator. Sometimes, when the discomfort or impairment becomes so great that it affects a job, relationships, enjoyment of life, the person with OCD will come forward to accept professional advice. Families have told me of watching the bottom “fall out” and just how badly things deteriorated before their loved one would admit to a problem. This is a painful process and you have choices as a support person. Often admission to “a problem” does not mean acceptance of the problem or giving into it; admission is the first step in being able to identify that the person has a legitimate neurobiological disorder with distinct treatment, rather than the problems stemming from character flaws. For the whole family acceptance is a process that takes time.
Families have told me of watching the bottom “fall out” and just how badly things deteriorated before their loved one would admit to a problem. This is a painful process and you have choices as a support person. Often admission to “a problem” does not mean acceptance of the problem or giving into it; admission is the first step in being able to identify that the person has a legitimate neurobiological disorder with distinct treatment, rather than the problems stemming from character flaws. For the whole family acceptance is a process that takes time.
Possible Responses
- Bring literature, video tapes, and/or audio tapes on OCD into the house. Offer the information to your family member with OCD or leave it around (strategically) so they can read/listen to it on their own.
- Encourage the person with the assurance that through available treatments most people experience a significant decrease in symptoms. There is help and there are others with the same problems.

- Discuss the ways in which you have been accommodating the OCD (when applicable) and how you need to work together as you disengage, so the person with the OCD knows you are doing so to support and help hem overcome the disorder not out of spite.
- Suggest the person with OCD attend support groups, with or without you, talk to an OCD buddy through online support groups, or speak to a professional in a local OCD clinic.
Get support and help yourself
- Seek professional advice/support for yourself from someone experienced with OCD.
- Find a family buddy (another family member going through something similar).
- Talk to other family members so you can share your feelings of anger sadness guilt shame and isolation.
- Attend a support group or find out about Multi-Family Behavior Therapy to discuss how other families handle the symptoms and get feedback about how you can deal with your family member’s OCD.
Allow natural consequences to occur for the person with OCD. Inform your loved one that it is in their best interest for you to be involved as little as possible with the behaviors they feel they need to perform to reduce discomfort. You are here to help them resist their compulsions, but you cannot assist or do them. Explain that you are doing all you can to understand their pain, but that your giving in to the unreasonable demands will only make the situation worse. In severe cases when the person with OCD is simply unwilling to cooperate, to negotiate agreements, to reduce accommodation, you may need to refuse to be involved with the OCD—no reassurance giving, no extra hand washes, no checking, no avoidance. Remind him/her that your giving in may make him/her feel better temporarily, but that it doesn’t help the symptoms to decrease, in fact it only makes them spiral downward. This may motivate them to seek treatment particularly if they start to be late for work, or miss school more often. In some very severe cases, a sufferer will eventually choose to move out of the house or need to be encouraged to do so.
Inform your loved one that it is in their best interest for you to be involved as little as possible with the behaviors they feel they need to perform to reduce discomfort. You are here to help them resist their compulsions, but you cannot assist or do them. Explain that you are doing all you can to understand their pain, but that your giving in to the unreasonable demands will only make the situation worse. In severe cases when the person with OCD is simply unwilling to cooperate, to negotiate agreements, to reduce accommodation, you may need to refuse to be involved with the OCD—no reassurance giving, no extra hand washes, no checking, no avoidance. Remind him/her that your giving in may make him/her feel better temporarily, but that it doesn’t help the symptoms to decrease, in fact it only makes them spiral downward. This may motivate them to seek treatment particularly if they start to be late for work, or miss school more often. In some very severe cases, a sufferer will eventually choose to move out of the house or need to be encouraged to do so. If the sufferer is not a minor, lives alone and is not a danger to him/herself or others, there may be only so much you can do to get him/her to seek help.
If the sufferer is not a minor, lives alone and is not a danger to him/herself or others, there may be only so much you can do to get him/her to seek help.
Above all, remember you have a life to and a right to that life! Self care is critical as is maintaining your work and social functioning as optimally as possible. You and other family members may need to seek advice/support/CBT from a clinician experienced in OCD. The best thing you can do is take action now. Don’t wait !
Barbara Livingston Van Noppen, PhD is an Associate Professor in the Department of Psychiatry and Human Behavior and Assistant Chair of Education Keck School of Medicine University of Southern California. Dr. Van Noppen provides CBT supervision and didactic education to psychiatric residents in the USC Keck School of Medicine program.
Michele Tortora Pato, MD is the Della Martin Chair in Psychiatry and Associate Dean for Academic Scholarship at the Keck School of Medicine-USC.
Back to Expert Opinions
My loved one has obsessive-compulsive disorder
Together with a psychologist, we figure out how to communicate with a loved one with OCD so that he feels cared for and does not feel pressure.
If you're thinking about going into psychotherapy but don't understand how it works, check out this free onboarding course.
OCD is a mental state. A person with OCD has intrusive thoughts that cause intense anxiety called obsessions. To cope with them, he performs certain actions - compulsions.
For example, a person is worried that he has not turned off the hair dryer or the iron, and there will definitely be a fire at home. To make sure everything is in order, he goes around the apartment exactly five times before leaving the house. And he can also come back, double-check the appliances and take pictures of the sockets.
Important: please do not diagnose your loved one yourself. This can misinform or offend the person. If a loved one seems to have signs of OCD, say that you are worried about him and advise you to go to a specialist.
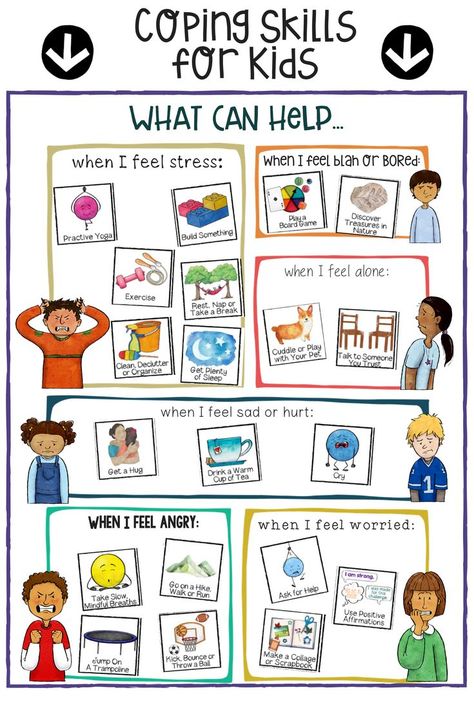
Be patient
The person with OCD is not to blame for not being able to get rid of obsessive thoughts. Don't judge the disorder or criticize your loved one - consider OCD as a feature of their character. Exactly the same as a good sense of humor or a short temper.
Don't judge the disorder or criticize your loved one - consider OCD as a feature of their character. Exactly the same as a good sense of humor or a short temper.
Do not convince your loved one that nothing terrible will happen
Fears that seem meaningless to you, for a person with OCD have real power. It’s better to ask what exactly worries a loved one and why. Offer to talk about it. If you have a trusting relationship, advise him to contact a specialist.
Be there
Living with heavy obsessive thoughts and scary images is not easy. Imagine how you feel if you watch ten horror movies in a day. A person with OCD rewinds such films in his head every day. Let your loved one know that you are always ready to listen and support him.
Let a loved one perform rituals
If you know that it is important for a person to wash the dishes three times, do not interfere with him doing this - otherwise he will be bothered. Rather, focus on what will help shift focus and reduce anxiety. For example, offer to help with chores or take a walk.
For example, offer to help with chores or take a walk.
Stay close when times are tough
OCD can be exacerbated by stress, such as when a person changes jobs or has a fight with a partner. If a loved one is having a difficult period, draw his attention to the fact that he has already coped with difficulties before. Remind him of his strengths. Say that there are people next to him who you can rely on.
Try to learn more about OCD
You can find scientific resources and stories of people who have experienced the disorder on the Internet.
When choosing a resource, pay attention to how the materials are written. They should be without negative evaluation and criticism. Emotional overtones are only acceptable if the person with OCD is telling their personal story. See if the author of the material refers to scientific sources and disease classifiers (ICD or DSM). It is good if the author or expert quoted in the article is a representative of the scientific community, a doctor or a psychotherapist.
We advise you to listen to the episode of the podcast "One Disorder" about OCD. This will help you understand what your loved one is dealing with. Discuss with him what you read: a loved one will tell you which symptoms he has are more pronounced, and which ones hardly interfere with him.
You can also read our article:
What is obsessive-compulsive disorder
Remember why a person is important to you
A friend or partner with OCD is, first of all, your loved one. Personality should always come first. The disorder does not determine the whole life of a loved one, it is not a hindrance to a warm relationship.
If you feel that communication with your loved one takes a lot of strength from you and you yourself need support, contact a psychologist. It can be found in our service .
We thank the psychologist Irina Permyakova for the professional recommendations that are described in this article.
symptoms, how to get rid and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, everything had come to naught, and in my teens I decided that these were just childish oddities.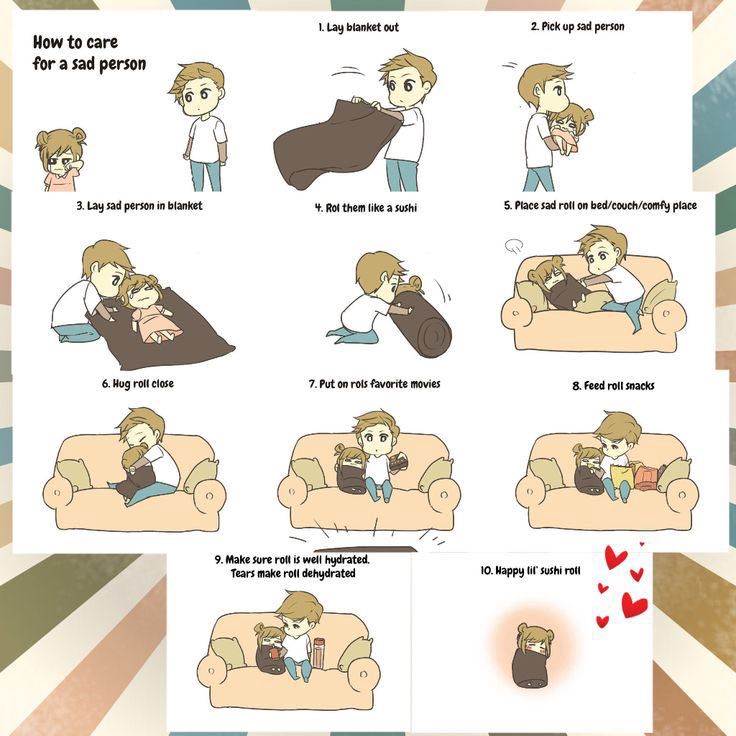 But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
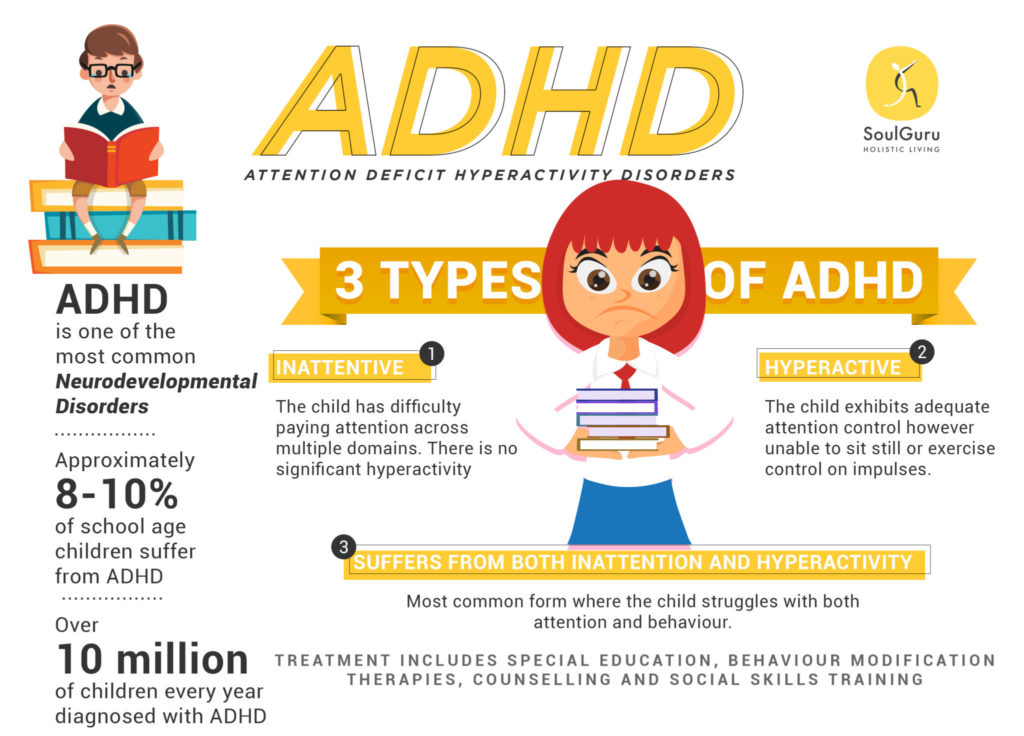
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is obsessive-compulsive disorder - Mayo Clinic
Intrusive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".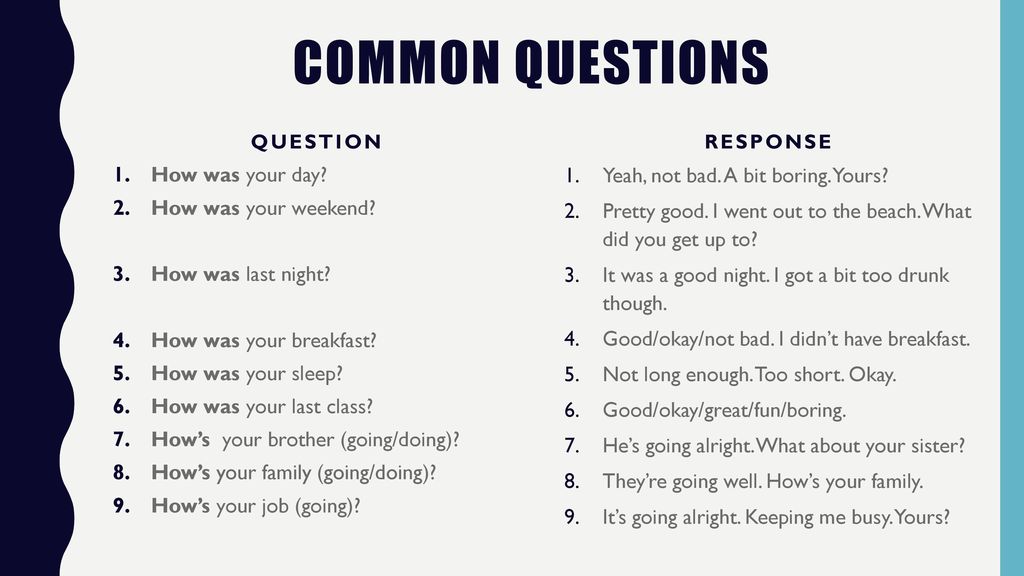
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person’s condition does not interfere with himself or others, then everything is in order; if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that one unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasant. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other medications: tranquilizers, antipsychotics, or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive Behavioral Therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16.2003 No. 438 "On Psychotherapeutic Care"
OCD in Russia is treated by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a psycho-neurological dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
It was possible to move freely and receive visitors in the day hospital. The only limitation that distinguished the hospital from a regular hospital was that there were no forks and knives in the dining room. Part of the drugs used to treat psychiatric diseases cause drowsiness. Therefore, in the hospital there are wards where you can sleep. For example, after drip About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on depression treatment
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
Treatment
Visiting a local psychiatrist After I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 P |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 P |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refused
I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refused Treatment
Second hospitalization and psychotherapyAfter six months of outpatient treatment, the local psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive actions to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital - 3202 Р
| Item of expenditure | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them.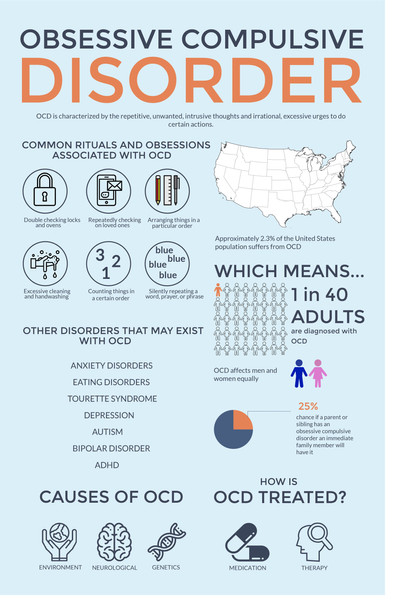 Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.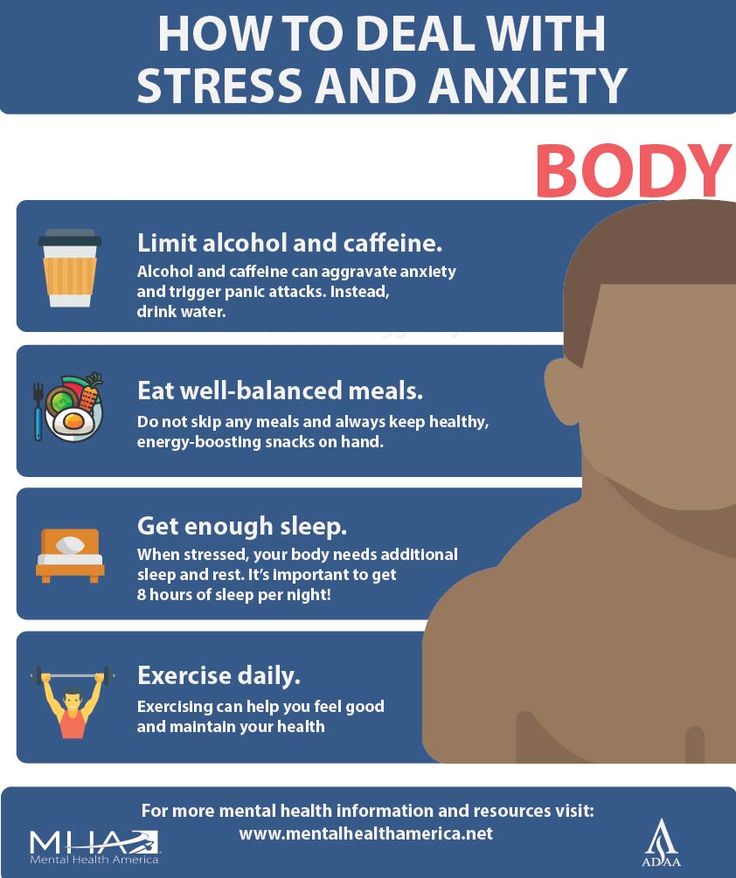
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 P |
| Transport during hospitalization | 1380 R |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs.

Learn more