Disorders similar to ocd
Obsessive-compulsive disorder and its related disorders: a reappraisal of obsessive-compulsive spectrum concepts
1. Angst J, Gamma A, Endrass J, et al. Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity, and course. Eur Arch Psychiatry Clin Neurosci. 2004;254:156–164. [PubMed] [Google Scholar]
2. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. [PubMed] [Google Scholar]
3. Murray CJ, Lopez AD. Evidence-based health policy--lessons from the Global Burden of Disease Study. Science. 1996;274:740–743. [PubMed] [Google Scholar]
4. Altman SE, Shankman SA. What is the association between obsessivecompulsive disorder and eating disorders? Clin Psychol Rev. 2009;29:638–46. [PubMed] [Google Scholar]
5. Fallon BA, Qureshi AI, Laje G, Klein B. Hypochondriasis and its relationship to obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:605–616. [PubMed] [Google Scholar]
6. Ferrao YA, Miguel E, Stein DJ. Tourette's syndrome, trichotillomania, and obsessive-compulsive disorder: how closely are they related? Psychiatry Res. 2009;170:32–42. [PubMed] [Google Scholar]
7. Fineberg NA, Sharma P, Sivakumaran T, Sahakian B, Chamberlain SR. Does obsessive-compulsive personality disorder belong within the obsessive-compulsive spectrum? CNS Spectr. 2007;12:467–482. [PubMed] [Google Scholar]
8. Phillips KA, Pinto A, Menard W, Eisen JL, Mancebo M, Rasmussen SA. Obsessive-compulsive disorder versus body dysmorphic disorder: a comparison study of two possibly related disorders. Depress Anxiety. 2007;24:399–409. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
9. Hermesh H, Hoffnung RA, Aizenberg D, Molcho A, Munitz H. Catatonic signs in severe obsessive compulsive disorder. J Clin Psychiatry. 1990;51:259–259. [Google Scholar]
10. Hutton J, Goode S, Murphy M, Le Couteur A, Rutter M. New-onset psychiatric disorders in individuals with autism. Autism. 2008;12:373–390. [PubMed] [Google Scholar]
11. Castle DJ, Phillips KA. Obsessive-compulsive spectrum of disorders: a defensible construct? Aust N Z J Psychiatry. 2006;40:114–120. [PMC free article] [PubMed] [Google Scholar]
12. Hollander E, Kim S, Braun A, Simeon D, Zohar J. Cross-cutting issues and future directions for the OCD spectrum. Psychiatry Res. 2009;170:3–6. [PubMed] [Google Scholar]
13. Lochner C, Seedat S, Stein DJ. Chronic hair-pulling: phenomenologybased subtypes. J Anxiety Disord.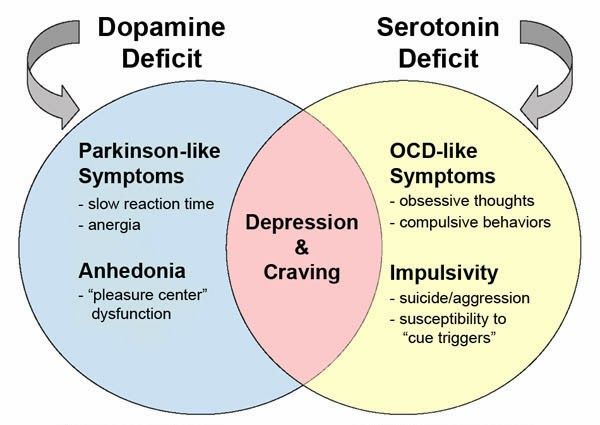 2009 [PubMed] [Google Scholar]
2009 [PubMed] [Google Scholar]
14. Storch EA, Abramowitz J, Goodman WK. Where does obsessive-compulsive disorder belong in DSM-V? Depress Anxiety. 2008;25:336–347. [PubMed] [Google Scholar]
15. Hollander E, Wong CM. Obsessive-compulsive spectrum disorders. J Clin Psychiatry. 1995;56 Suppl 4:3–6. discussion 53–55. [PubMed] [Google Scholar]
16. Hollander E. Obsessive-compulsive spectrum disorders: an overview. Psychiatric Annals. 1993;23:355–358. [Google Scholar]
17. Lochner C, Hemmings SM, Kinnear CJ, et al. Cluster analysis of obsessive-compulsive spectrum disorders in patients with obsessive-compulsive disorder: clinical and genetic correlates. Compr Psychiatry. 2005;46:14–19. [PubMed] [Google Scholar]
18. Durdle H, Gorey KM, Stewart SH. A meta-analysis examining the relations among pathological gambling, obsessive-compulsive disorder, and obsessive-compulsive traits.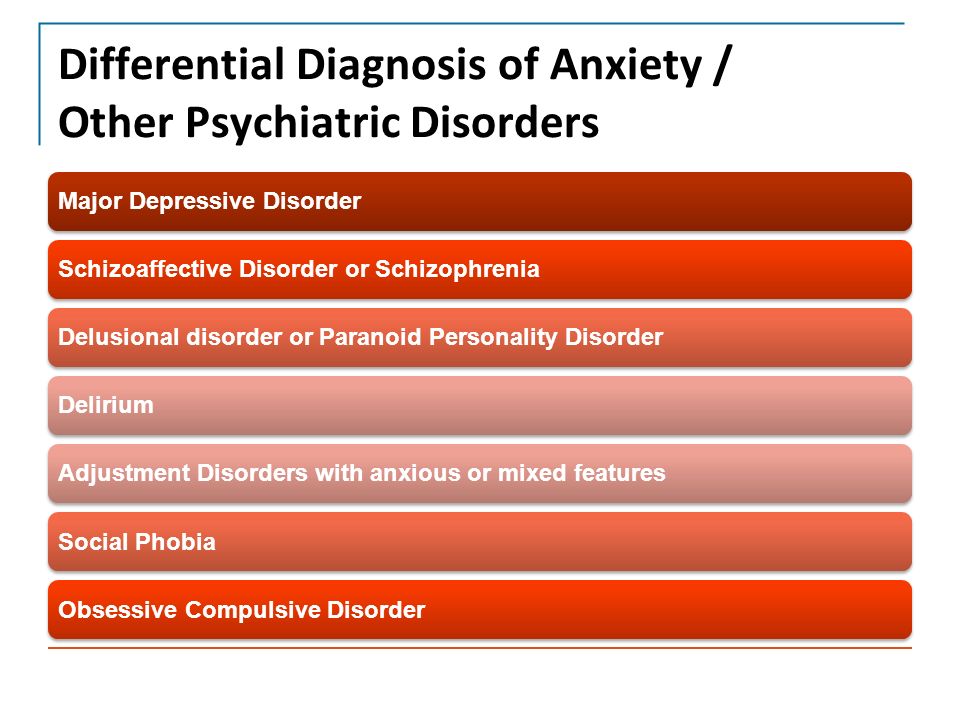 Psychol Rep. 2008;103:485–498. [PubMed] [Google Scholar]
Psychol Rep. 2008;103:485–498. [PubMed] [Google Scholar]
19. Mataix-Cols D, Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. Am J Psychiatry. 2005;162:228–238. [PubMed] [Google Scholar]
20. Potenza MN, Koran LM, Pallanti S. The relationship between impulsecontrol disorders and obsessive-compulsive disorder: a current understanding and future research directions. Psychiatry Res. 2009;170:22–31. [PMC free article] [PubMed] [Google Scholar]
21. Abramowitz JS, Taylor S, McKay D. Obsessive-compulsive disorder. Lancet. 2009;374:491–499. [PubMed] [Google Scholar]
22. Regier DA. Obsessive-compulsive behavior spectrum: refining the research agenda for DSM-V. Psychiatry Res. 2009;170:1–2. [PubMed] [Google Scholar]
23. Hollander E, Kim S, Khanna S, Pallanti S. Obsessive-compulsive disorder and obsessive-compulsive spectrum disorders: diagnostic and dimensional issues.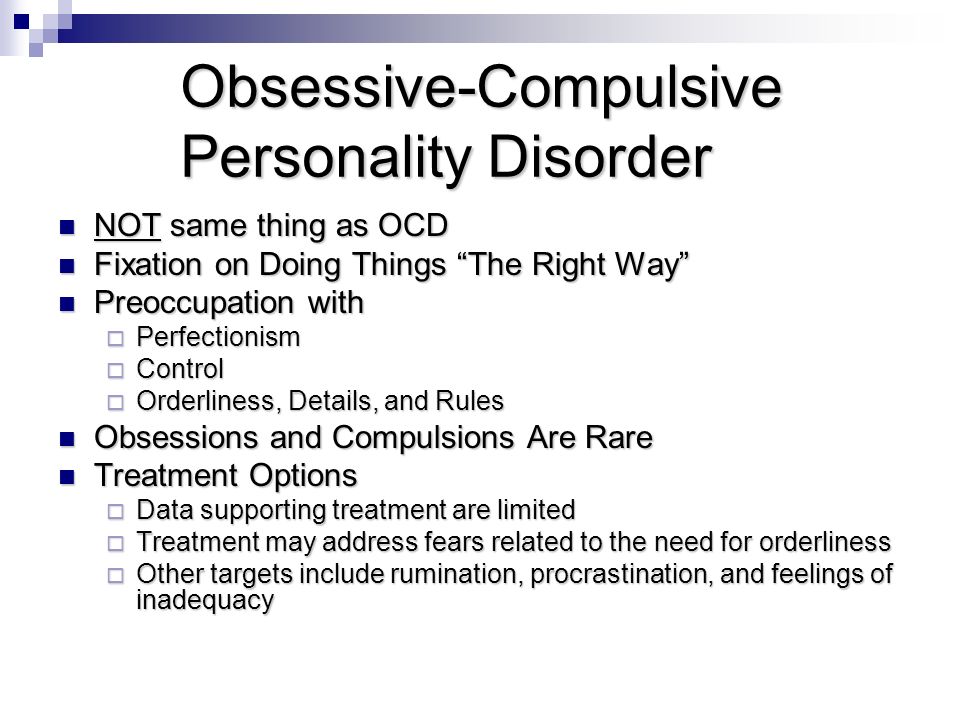 CNS Spectr. 2007;12:5–13. [Google Scholar]
CNS Spectr. 2007;12:5–13. [Google Scholar]
24. Mataix-Cols D, van den Heuvel OA. Common and distinct neural correlates of obsessive-compulsive and related disorders. Psychiatr Clin North Am. 2006;29:391–410, viii. [PubMed] [Google Scholar]
25. McKay D, Abramowitz JS, Calamari JE, et al. A critical evaluation of obsessive-compulsive disorder subtypes: symptoms versus mechanisms. Clin Psychol Rev. 2004;24:283–313. [PubMed] [Google Scholar]
26. Miguel EC, Leckman JF, Rauch S, et al. Obsessive-compulsive disorder phenotypes: implications for genetic studies. Mol Psychiatry. 2005;10:258–275. [PubMed] [Google Scholar]
27. Leckman JF, Bloch MH, King RA. Symptom dimensions and subtypes of obsessive-compulsive disorder: a developmental perspective. Dialogues Clin Neurosci. 2009;11:21–33. [PMC free article] [PubMed] [Google Scholar]
28. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th ed. Washington, DC: American Psychiatric Association . 1994 [Google Scholar]
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th ed. Washington, DC: American Psychiatric Association . 1994 [Google Scholar]
29. Hasler G, LaSalle-Ricci VH, Ronquillo JG, et al. Obsessive-compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Res. 2005;135:121–132. [PubMed] [Google Scholar]
30. Schooler C, Revell AJ, Timpano KR, Wheaton M, Murphy DL. Predicting genetic loading from symptom patterns in obsessive-compulsive disorder: a latent variable analysis. Depress Anxiety. 2008;25:680–688. [PMC free article] [PubMed] [Google Scholar]
31. Abramowitz JS, Wheaton MG, Storch EA. The status of hoarding as a symptom of obsessive-compulsive disorder. Behav Res Ther. 2008;46:1026–1033. [PubMed] [Google Scholar]
32. Pertusa A, Fullana MA, Singh S, Alonso P, Menchon JM, Mataix-Cols D. Compulsive hoarding: OCD symptom, distinct clinical syndrome, or both? Am J Psychiatry. 2008;165:1289–1298. [PubMed] [Google Scholar]
Compulsive hoarding: OCD symptom, distinct clinical syndrome, or both? Am J Psychiatry. 2008;165:1289–1298. [PubMed] [Google Scholar]
33. Wu KD, Watson D. Hoarding and its relation to obsessive. Behav Res Ther. 2005;43:897–921. [PubMed] [Google Scholar]
34. Rettew DC, Swedo SE, Leonard HL, Lenane MC, Rapoport JL. Obsessions and compulsions across time in 79 children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 1992;31:1050–1056. [PubMed] [Google Scholar]
35. Mataix-Cols D, Rauch SL, Baer L, et al. Symptom stability in adult obsessive-compulsive disorder: data from a naturalistic two-year followup study. Am J Psychiatry. 2002;159:263–268. [PubMed] [Google Scholar]
36. Rufer M, Grothusen A, Mass R, Peter H, Hand I. Temporal stability of symptom dimensions in adult patients with obsessive-compulsive disorder. J Affect Disord. 2005;88:99–102. [PubMed] [Google Scholar]
J Affect Disord. 2005;88:99–102. [PubMed] [Google Scholar]
37. Hasler G, Pinto A, Greenberg BD, et al. Familiality of factor analysisderived YBOCS dimensions in OCD-affected sibling pairs from the OCD Collaborative Genetics Study. Biol Psychiatry. 2007;61:617–625. [PubMed] [Google Scholar]
38. Samuels J, Shugart YY, Grados MA, et al. Significant linkage to compulsive hoarding on chromosome 14 in families with obsessive-compulsive disorder: results from the OCD Collaborative Genetics Study. Am J Psychiatry. 2007;164:493–499. [PubMed] [Google Scholar]
39. Wendland JR, Moya PR, Timpano KR, et al. A haplotype containing quantitative trait loci for SLC1A1 gene expression and its association with obsessive-compulsive disorder. Arch Gen Psychiatry. 2009;66:408–416. [PMC free article] [PubMed] [Google Scholar]
40. Saxena S, Brody AL, Maidment KM, et al. Cerebral glucose metabolism in obsessive-compulsive hoarding. Am J Psychiatry. 2004;161:1038–1048. [PubMed] [Google Scholar]
Saxena S, Brody AL, Maidment KM, et al. Cerebral glucose metabolism in obsessive-compulsive hoarding. Am J Psychiatry. 2004;161:1038–1048. [PubMed] [Google Scholar]
41. Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L. Use of factoranalyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 1999;156:1409–1416. [PubMed] [Google Scholar]
42. Alonso P, Menchon JM, Pifarre J, et al. Long-term follow-up and predictors of clinical outcome in obsessive-compulsive patients treated with serotonin reuptake inhibitors and behavioral therapy. J Clin Psychiatry. 2001;62:535–540. [PubMed] [Google Scholar]
43. Janet P. Les Obsessions et la Psychasthenie 2nd ed. Paris, France: Bailliere . 1904 [Google Scholar]
44. Rasmussen SA, Eisen JL. The epidemiology and differential diagnosis of obsessive compulsive disorder. J Clin Psychiatry. 1994;55 (suppl):5–10. discussion 11–14. [PubMed] [Google Scholar]
Rasmussen SA, Eisen JL. The epidemiology and differential diagnosis of obsessive compulsive disorder. J Clin Psychiatry. 1994;55 (suppl):5–10. discussion 11–14. [PubMed] [Google Scholar]
45. Pitman RK. Pierre Janet on obsessive-compulsive disorder (1903). Review and commentary. Arch Gen Psychiatry. 1987;44:226–232. [PubMed] [Google Scholar]
46. Coles ME, Heimberg RG, Frost RO, Steketee G. Not just right experiences and obsessive-compulsive features: experimental and self-monitoring perspectives. Behav Res Ther. 2005;43:153–167. [PubMed] [Google Scholar]
47. Ecker W, Gonner S. Incompleteness and harm avoidance in OCD symptom dimensions. Behav Res Ther. 2008;46:895–904. [PubMed] [Google Scholar]
48. Summerfeldt LJ. Understanding and treating incompleteness in obsessive-compulsive disorder. J Clin Psychol.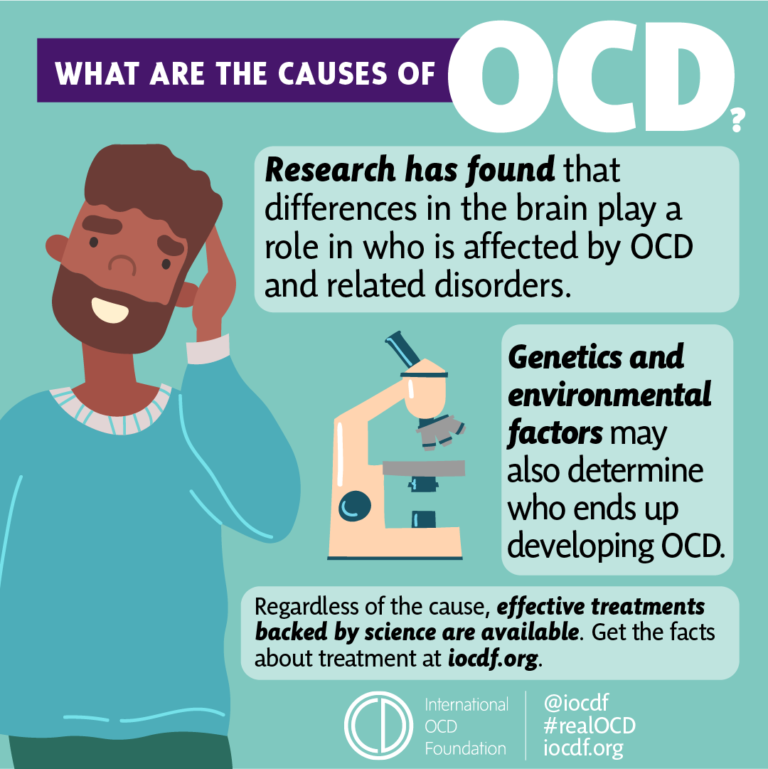 2004;60:1155–1168. [PubMed] [Google Scholar]
2004;60:1155–1168. [PubMed] [Google Scholar]
49. Miguel EC, do Rosario-Campos MC, Prado HS, et al. Sensory phenomena in obsessive-compulsive disorder and Tourette's disorder. J Clin Psychiatry. 2000;61:150–156. [PubMed] [Google Scholar]
50. Goodman WK, Price LH, Rasmussen SA, Delgado PL, Heninger GR, Charney DS. Efficacy of fluvoxamine in obsessive-compulsive disorder. A double-blind comparison with placebo. Arch Gen Psychiatry. 1989;46:36–44. [PubMed] [Google Scholar]
51. Goodman WK, Price LH, Rasmussen SA, Heninger GR, Charney DS. Fluvoxamine as an antiobsessional agent. Psychopharmacol Bull. 1989;25:31–35. [PubMed] [Google Scholar]
52. Slattery MJ, Dubbert BK, Allen AJ, Leonard HL, Swedo SE, Gourley MF. Prevalence of obsessive-compulsive disorder in patients with systemic lupus erythematosus. J Clin Psychiatry. 2004;65:301–306. [PubMed] [Google Scholar]
53. Catapano F, Perris F, Fabrazzo M, et al. Obsessive-compulsive disorder with poor insight: A three-year prospective study. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:323–330. [PubMed] [Google Scholar]
Catapano F, Perris F, Fabrazzo M, et al. Obsessive-compulsive disorder with poor insight: A three-year prospective study. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:323–330. [PubMed] [Google Scholar]
54. Eichstedt JA, Arnold SL. Childhood-onset obsessive-compulsive disorder: a tic-related subtype of OCD? Clin Psychol Rev. 2001;21:137–157. [PubMed] [Google Scholar]
55. de Mathis MA, Diniz JB, Shavitt RG, et al. Early onset obsessive-compulsive disorder with and without tics. CNS Spectr. 2009;14:362–370. [PubMed] [Google Scholar]
56. Janowitz D, Grabe HJ, Ruhrmann S, et al. Early onset of obsessivecompulsive disorder and associated comorbidity. Depress Anxiety. 2009;26:1012–1017. [PubMed] [Google Scholar]
57. Carmin C, Wiegartz PS, Wu KD. Obsessive-Compulsive disorder with poor insight. In: Abramowitz JS, McKay D, Taylor S, eds. Clinical Handbook of Obsessive-Compulsive Disorder and Related Problems Baltimore, MD: Johns Hopkins University Press . 2008:109–125. [Google Scholar]
Clinical Handbook of Obsessive-Compulsive Disorder and Related Problems Baltimore, MD: Johns Hopkins University Press . 2008:109–125. [Google Scholar]
58. Lochner C, Kinnear CJ, Hemmings SM, et al. Hoarding in obsessivecompulsive disorder: clinical and genetic correlates. J Clin Psychiatry. 2005;66:1155–1160. [PubMed] [Google Scholar]
59. Storch EA, Lack CW, Merlo LJ, et al. Clinical features of children and adolescents with obsessive-compulsive disorder and hoarding symptoms. Compr Psychiatry. 2007;48:313–318. [PubMed] [Google Scholar]
60. Nestadt G, Di CZ, Riddle MA, et al. Obsessive-compulsive disorder: subclassification based on co-morbidity. Psychol Med. 2008:1–11. [PMC free article] [PubMed] [Google Scholar]
61. Hollander E, Braun A, Simeon D. Should OCD leave the anxiety disorders in DSM-V? The case for obsessive-compulsive-related disorders.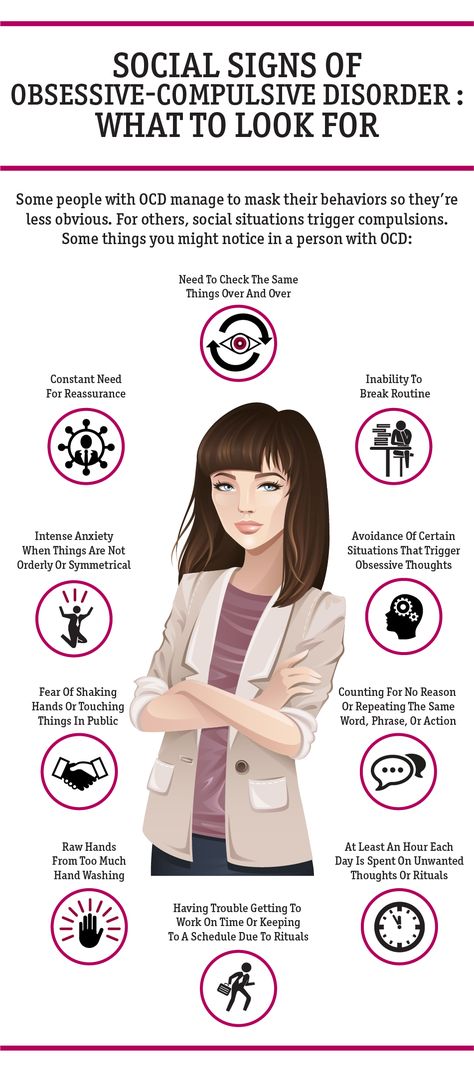 Depress Anxiety. 2008;25:317–329. [PubMed] [Google Scholar]
Depress Anxiety. 2008;25:317–329. [PubMed] [Google Scholar]
62. McKay D, Neziroglu F. Methodological issues in the obsessive-compulsive spectrum. Psychiatry Res. 2009;170:61–65. [PubMed] [Google Scholar]
63. Mataix-Cols D, Pertusa A, Leckman JF. Issues for DSM-V: how should obsessive-compulsive and related disorders be classified? Am J Psychiatry. 2007;164:1313–1314. [PubMed] [Google Scholar]
64. Demal U, Lenz G, Mayrhofer A, Zapotoczky HG, Zitterl W. Obsessivecompulsive disorder and depression. A retrospective study on course and interaction. Psychopathology. 1993;26:145–150. [PubMed] [Google Scholar]
65. Freeman MP, Freeman SA, McElroy SL. The comorbidity of bipolar and anxiety disorders: prevalence, psychobiology, and treatment issues. J Affect Disord. 2002;68:1–23. [PubMed] [Google Scholar]
66. Masi G, Perugi G, Toni C, et al. Obsessive-compulsive bipolar comorbidity: focus on children and adolescents. J Affect Disord. 2004;78:175–183. [PubMed] [Google Scholar]
Obsessive-compulsive bipolar comorbidity: focus on children and adolescents. J Affect Disord. 2004;78:175–183. [PubMed] [Google Scholar]
67. Hantouche EG, Angst J, Demonfaucon C, Perugi G, Lancrenon S, Akiskal HS. Cyclothymic OCD: a distinct form? J Affect Disord. 2003;75:1–10. [PubMed] [Google Scholar]
68. Wheaton M, Timpano KR, Lasalle-Ricci VH, Murphy D. Characterizing the hoarding phenotype in individuals with OCD: associations with comorbidity, severity and gender. J Anxiety Disord. 2008;22:243–252. [PMC free article] [PubMed] [Google Scholar]
69. Hollander E, Greenwald S, Neville D, Johnson J, Hornig CD, Weissman MM. Uncomplicated and comorbid obsessive-compulsive disorder in an epidemiologic sample. Depress Anxiety. 1996;4:111–119. [PubMed] [Google Scholar]
70. Huppert JD, Simpson HB, Nissenson KJ, Liebowitz MR, Foa EB. Quality of life and functional impairment in obsessive-compulsive disorder: a comparison of patients with and without comorbidity, patients in remission, and healthy controls. Depress Anxiety. 2009;26:39–45. [PMC free article] [PubMed] [Google Scholar]
Depress Anxiety. 2009;26:39–45. [PMC free article] [PubMed] [Google Scholar]
71. LaSalle VH, Cromer KR, Nelson KN, Kazuba D, Justement L, Murphy DL. Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive-compulsive disorder. Depress Anxiety. 2004;19:163–173. [PubMed] [Google Scholar]
72. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63. [PMC free article] [PubMed] [Google Scholar]
73. Geller DA. Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatr Clin North Am. 2006;29:353–3570. [PubMed] [Google Scholar]
74. Fornaro M, Gabrielli F, Albano C, et al. Obsessive-compulsive disorder and related disorders: a comprehensive survey. Ann Gen Psychiatry. 2009;8:13–13. [PMC free article] [PubMed] [Google Scholar]
Ann Gen Psychiatry. 2009;8:13–13. [PMC free article] [PubMed] [Google Scholar]
75. Hantouche EG, Lancrenon S. [Modern typology of symptoms and obsessive-compulsive syndromes: results of a large French study of 615 patients] Encephale. 1996;22 Spec No 1:9–21. [PubMed] [Google Scholar]
76. Murphy DL, Timpano KR, Wendland JR. Genetic contributions to obsessive-compulsive disorder (OCD) and OCD-related disorders. In: Nurnberger J, Berrettini W, eds. Principles of Psychiatric Genetics. Cambridge, UK: Cambridge University Press . 2010 [Google Scholar]
77. Nestadt G, Samuels J, Riddle MA, et al. The relationship between obsessive-compulsive disorder and anxiety and affective disorders: results from the Johns Hopkins OCD Family Study. Psychol Med. 2001;31:481–487. [PubMed] [Google Scholar]
78. Kessler RC, McGonagle KA, Zhao S, et al.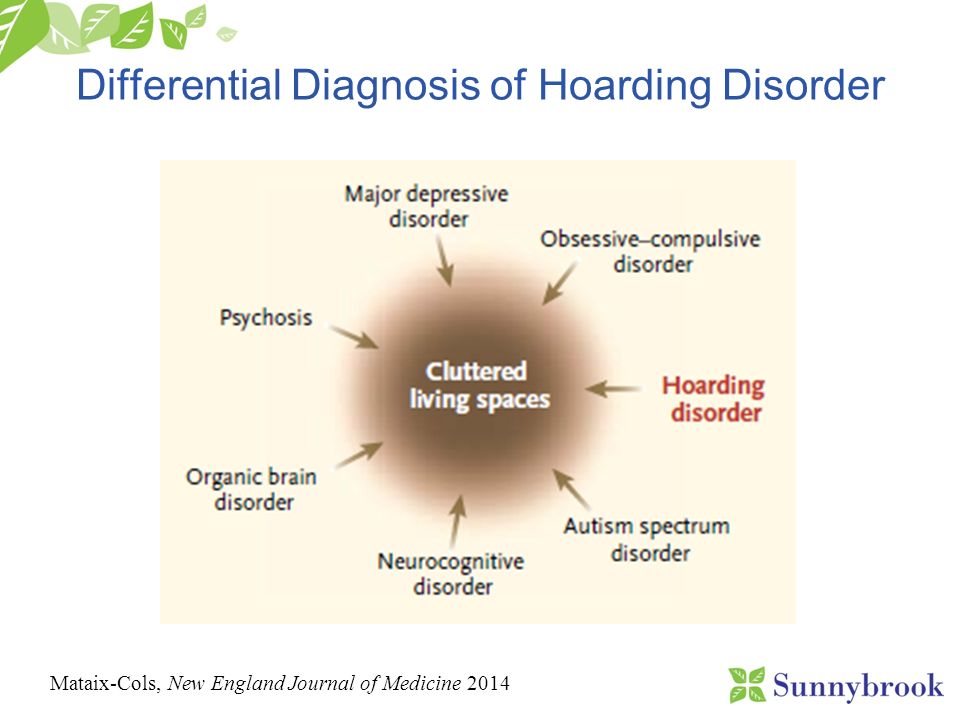 Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. [PubMed] [Google Scholar]
Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. [PubMed] [Google Scholar]
79. Miguel EC, Ferrao YA, Rosario MC, et al. The Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr. 2008;30:185–196. [PubMed] [Google Scholar]
80. Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J. Examining the relationship between obsessive-compulsive disorder and attentiondeficit/hyperactivity disorder in children and adolescents: a familial risk analysis. Biol Psychiatry. 2007;61:316–321. [PubMed] [Google Scholar]
81. Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J. Further evidence for co-segregation between pediatric obsessive compulsive disorder and attention deficit hyperactivity disorder: a familial risk analysis. Biol Psychiatry. 2007;61:1388–1394. [PubMed] [Google Scholar]
Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J. Further evidence for co-segregation between pediatric obsessive compulsive disorder and attention deficit hyperactivity disorder: a familial risk analysis. Biol Psychiatry. 2007;61:1388–1394. [PubMed] [Google Scholar]
82. Asbahr FR, Garvey MA, Snider LA, Zanetta DM, Elkis H, Swedo SE. Obsessive-compulsive symptoms among patients with Sydenham chorea. Biol Psychiatry. 2005;57:1073–1076. [PubMed] [Google Scholar]
83. Kirvan CA, Swedo SE, Heuser JS, Cunningham MW. Mimicry and autoantibody-mediated neuronal cell signaling in Sydenham chorea. Nat Med. 2003;9:914–920. [PubMed] [Google Scholar]
84. Swedo SE, Leonard HL, Garvey M, et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am J Psychiatry. 1998;155:264–271. [PubMed] [Google Scholar]
85. Alvarenga PG, Hounie AG, Mercadante MT, et al. Obsessive-compulsive symptoms in heart disease patients with and without history of rheumatic fever. J Neuropsychiatry Clin Neurosci. 2006;18:405–408. [PubMed] [Google Scholar]
86. de Alvarenga PG, Floresi AC, Torres AR, et al. Higher prevalence of obsessive-compulsive spectrum disorders in rheumatic fever. Gen Hosp Psychiatry. 2009;31:178–180. [PubMed] [Google Scholar]
87. Hounie AG, Pauls DL, Mercadante MT, et al. Obsessive-compulsive spectrum disorders in rheumatic fever with and without Sydenham's chorea. J Clin Psychiatry. 2004;65:994–999. [PubMed] [Google Scholar]
88. Mercadante MT, Busatto GF, Lombroso PJ, et al. The psychiatric symptoms of rheumatic fever. Am J Psychiatry. 2000;157:2036–2038. [PubMed] [Google Scholar]
89. Hounie AG, Pauls DL, do Rosario-Campos MC, et al.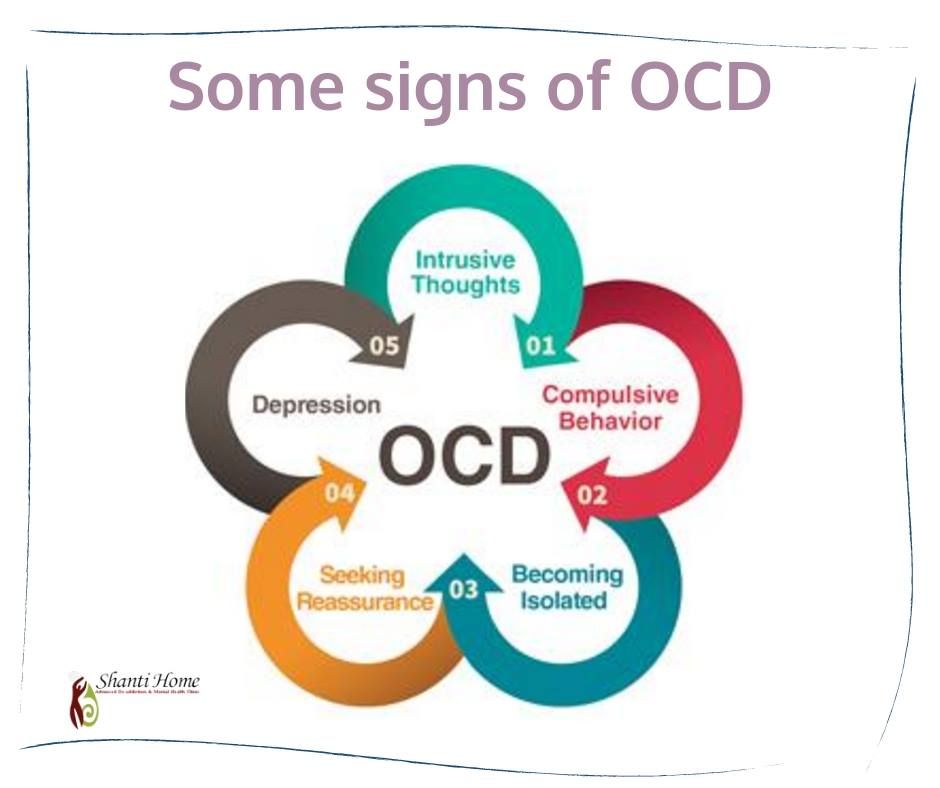 Obsessive-compulsive spectrum disorders and rheumatic fever: a family study. Biol Psychiatry. 2007;61:266–272. [PubMed] [Google Scholar]
Obsessive-compulsive spectrum disorders and rheumatic fever: a family study. Biol Psychiatry. 2007;61:266–272. [PubMed] [Google Scholar]
90. Seixas AA, Hounie AG, Fossaluza V, et al. Anxiety disorders and rheumatic fever: is there an association? CNS Spectr. 2008;13:1039–1046. [PubMed] [Google Scholar]
91. Hounie AG, Cappi C, Cordeiro Q, et al. TNF-alpha polymorphisms are associated with obsessive-compulsive disorder. Neurosci Lett. 2008;442:86–90. [PubMed] [Google Scholar]
92. Ramasawmy R, Fae KC, Spina G, et al. Association of polymorphisms within the promoter region of the tumor necrosis factor-alpha with clinical outcomes of rheumatic fever. Mol Immunol. 2007;44:1873–1878. [PubMed] [Google Scholar]
93. Snider LA, Swedo SE. PANDAS: current status and directions for research. Mol Psychiatry.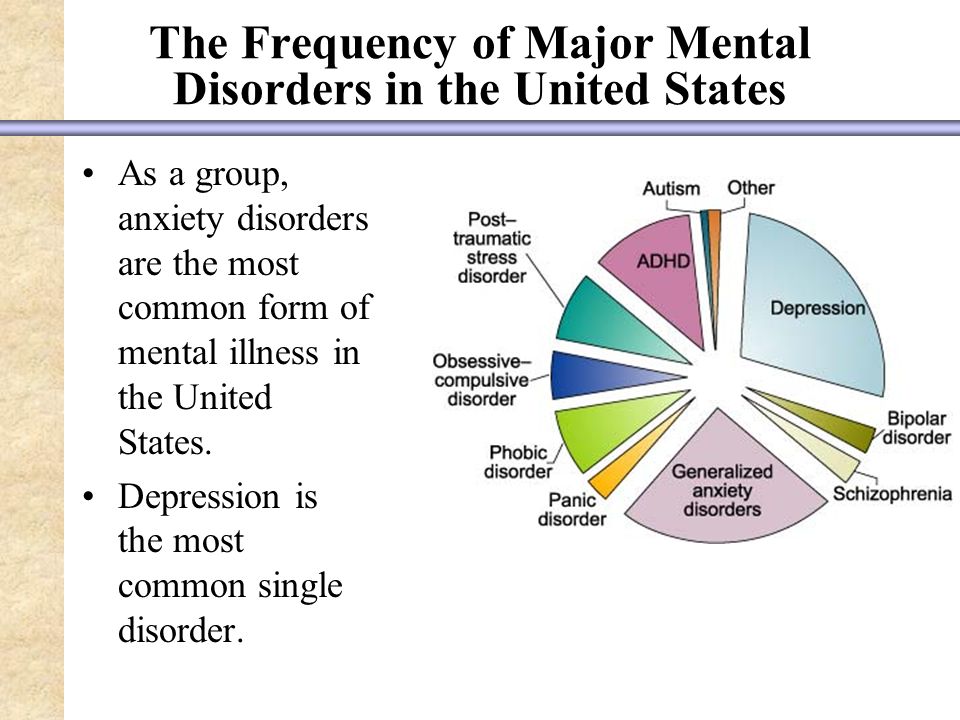 2004:900–907. [PubMed] [Google Scholar]
2004:900–907. [PubMed] [Google Scholar]
94. Swedo SE, Grant PJ. Annotation: PANDAS: a model for human autoimmune disease. J Child Psychol Psychiatry. 2005;46:227–234. [PubMed] [Google Scholar]
95. Hoffman KL, Hornig M, Yaddanapudi K, Jabado O, Lipkin WI. A murine model for neuropsychiatric disorders associated with group A beta-hemolytic streptococcal infection. J Neurosci. 2004;24:1780–1791. [PMC free article] [PubMed] [Google Scholar]
96. Lougee L, Perlmutter SJ, Nicolson R, Garvey MA, Swedo SE. Psychiatric disorders in first-degree relatives of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) J Am Acad Child Adolesc Psychiatry. 2000;39:1120–1126. [PubMed] [Google Scholar]
97. Shulman ST. Pediatric autoimmune neuropsychiatric disorders associated with streptococci (PANDAS): update.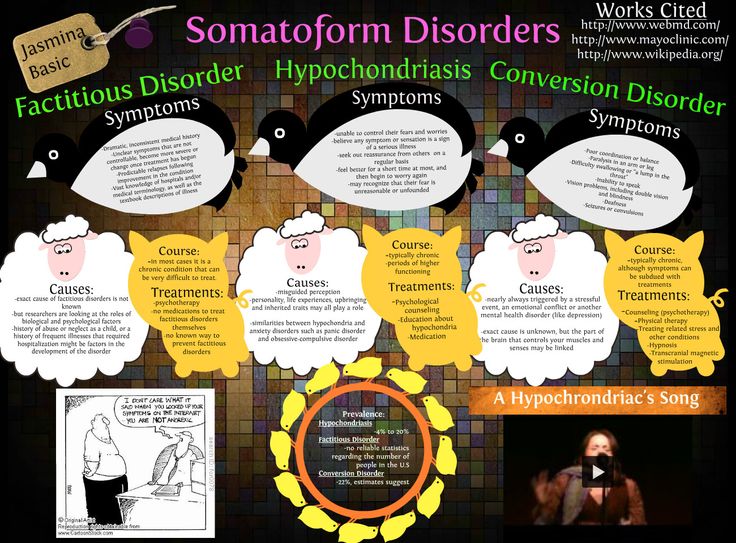 Curr Opin Pediatr. 2009;21:127–130. [PubMed] [Google Scholar]
Curr Opin Pediatr. 2009;21:127–130. [PubMed] [Google Scholar]
98. Kurlan R, Johnson D, Kaplan EL. Streptococcal infection and exacerbations of childhood tics and obsessive-compulsive symptoms: a prospective blinded cohort study. Pediatrics. 2008;121:1188–1197. [PubMed] [Google Scholar]
99. Lin H, Williams KA, Katsovich L, et al. Streptococcal upper respiratory tract infections and psychosocial stress predict future tic and obsessive-compulsive symptom severity in children and adolescents with Tourette syndrome and obsessive-compulsive disorder. Biol Psychiatry. 2010;67:684–691. [PMC free article] [PubMed] [Google Scholar]
100. Rizzo R, Gulisano M, Pavone P, Fogliani F, Robertson MM. Increased antistreptococcal antibody titers and anti-basal ganglia antibodies in patients with Tourette syndrome: controlled cross-sectional study.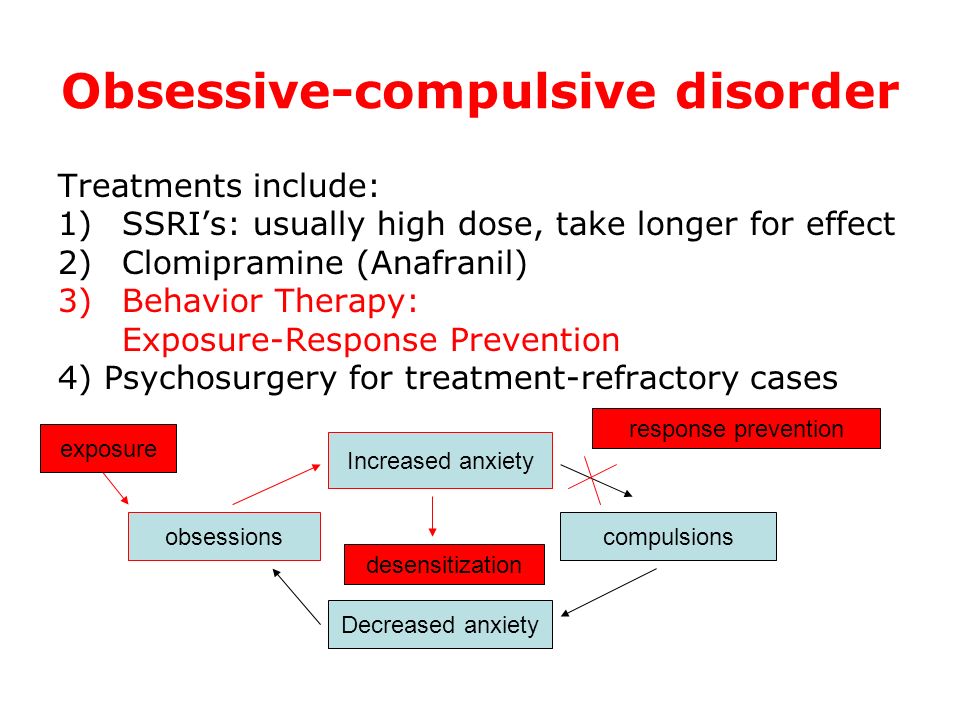 J Child Neurol. 2006;21:747–753. [PubMed] [Google Scholar]
J Child Neurol. 2006;21:747–753. [PubMed] [Google Scholar]
101. Termine C, Uggetti C, Veggiotti P, et al. Long-term follow-up of an adolescent who had bilateral striatal necrosis secondary to Mycoplasma pneumoniae infection. Brain Dev. 2005;27:62–65. [PubMed] [Google Scholar]
102. Budman C, Sarcevic A. An unusual case of motor and vocal tics with obsessive-compulsive symptoms in a young adult with Behcet's syndrome. CNS Spectr. 2002;7:878–881. [PubMed] [Google Scholar]
103. Bode L, Durrwald R, Rantam FA, Ferszt R, Ludwig H. First isolates of infectious human Borna disease virus from patients with mood disorders. Mol Psychiatry. 1996;1:200–212. [PubMed] [Google Scholar]
104. Cheyette SR, Cummings JL. Encephalitis lethargica: lessons for contemporary neuropsychiatry. J Neuropsychiatry Clin Neurosci. 1995;7:125–134. [PubMed] [Google Scholar]
105. Ercan TE, Ercan G, Severge B, Arpaozu M, Karasu G. Mycoplasma pneumoniae infection and obsessive-compulsive disease: a case report. J Child Neurol. 2008;23:338–340. [PubMed] [Google Scholar]
Ercan TE, Ercan G, Severge B, Arpaozu M, Karasu G. Mycoplasma pneumoniae infection and obsessive-compulsive disease: a case report. J Child Neurol. 2008;23:338–340. [PubMed] [Google Scholar]
106. Yaramis A, Herguner S, Kara B, Tatli B, Tuzun U, Ozmen M. Cerebral vasculitis and obsessive-compulsive disorder following varicella infection in childhood. Turk J Pediatr. 2009;51:72–75. [PubMed] [Google Scholar]
107. Berthier ML, Kulisevsky J, Gironell A, Lopez OL. Obsessive-compulsive disorder and traumatic brain injury: behavioral, cognitive, and neuroimaging findings. Neuropsychiatry, Neuropsychol Behav Neurol. 2001;14:23–31. [PubMed] [Google Scholar]
108. Coetzer R, Stein DJ, Du Toit PL. Executive function in traumatic brain injury and obsessive-compulsive disorder: an overlap? Psychiatry Clin Neurosci. 2001;55:83–87. [PubMed] [Google Scholar]
109. Grados MA. Obsessive-compulsive disorder after traumatic brain injury. Int Rev Psychiatry. 2003;15:350–358. [PubMed] [Google Scholar]
Grados MA. Obsessive-compulsive disorder after traumatic brain injury. Int Rev Psychiatry. 2003;15:350–358. [PubMed] [Google Scholar]
110. Silver JM, Kramer R, Greenwald S, Weissman M. The association between head injuries and psychiatric disorders: findings from the New Haven NIMH Epidemiologic Catchment Area Study. Brain Injury. 2001;15:935–945. [PubMed] [Google Scholar]
111. McKeon J, Roa B, Mann A. Life events and personality traits in obsessive-compulsive neurosis. Br J Psychiatry. 1984;144:185–189. [PubMed] [Google Scholar]
112. Kant R, Smith-Seemiller L, Duffy JD. Obsessive-compulsive disorder after closed head injury: review of literature and report of four cases. Brain Inj. 1996;10:55–63. [PubMed] [Google Scholar]
113. Roth RM, Jobst BC, Thadani VM, Gilbert KL, Roberts DW. New-onset obsessive-compulsive disorder following neurosurgery for medicationrefractory seizure disorder. Epilepsy Behav. 2009;14:677–680. [PubMed] [Google Scholar]
Epilepsy Behav. 2009;14:677–680. [PubMed] [Google Scholar]
114. Kurlan R. Disabling repetitive behaviors in Parkinson's disease. Mov Disord. 2004;19:433–437. [PubMed] [Google Scholar]
115. Maia AF, Pinto AS, Barbosa ER, Menezes PR, Miguel EC. Obsessivecompulsive symptoms, obsessive-compulsive disorder, and related disorders in Parkinson's disease. J Neuropsychiatry Clin Neurosci. 2003;15:371–374. [PubMed] [Google Scholar]
116. Correia S, Hubbard E, Hassenstab J, et al. Basal ganglia MR relaxometry in obsessive-compulsive disorder: T2 depends upon age of symptom onset. Brain Imag Behav In press [PMC free article] [PubMed] [Google Scholar]
117. Ruta L, Mugno D, D'Arrigo VG, Vitiello B, Mazzone L. Obsessive-compulsive traits in children and adolescents with Asperger syndrome. Eur Child Adolesc Psychiatry. 2010;19:17–24. [PubMed] [Google Scholar]
118. Zandt F, Prior M, Kyrios M. Similarities and differences between children and adolescents with autism spectrum disorder and those with obsessive compulsive disorder: executive functioning and repetitive behaviour. Autism. 2009;13:43–57. [PubMed] [Google Scholar]
Zandt F, Prior M, Kyrios M. Similarities and differences between children and adolescents with autism spectrum disorder and those with obsessive compulsive disorder: executive functioning and repetitive behaviour. Autism. 2009;13:43–57. [PubMed] [Google Scholar]
119. Bottas A, Cooke RG, Richter MA. Comorbidity and pathophysiology of obsessive-compulsive disorder in schizophrenia: is there evidence for a schizo-obsessive subtype of schizophrenia? J Psychiatry Neurosci. 2005;30:187–193. [PMC free article] [PubMed] [Google Scholar]
120. Poyurovsky M, Koran LM. Obsessive-compulsive disorder (OCD) with schizotypy vs. schizophrenia with OCD: diagnostic dilemmas and therapeutic implications. J Psychiatr Res. 2005;39:399–408. [PubMed] [Google Scholar]
121. Sa AR, Hounie AG, Sampaio AS, Arrais J, Miguel EC, Elkis H. Obsessivecompulsive symptoms and disorder in patients with schizophrenia treated with clozapine or haloperidol. Compr Psychiatry. 2009;50:437–442. [PubMed] [Google Scholar]
Obsessivecompulsive symptoms and disorder in patients with schizophrenia treated with clozapine or haloperidol. Compr Psychiatry. 2009;50:437–442. [PubMed] [Google Scholar]
122. Jeste DV, Dolder CR. Treatment of non-schizophrenic disorders: focus on atypical antipsychotics. J Psychiatr Res. 2004;38:73–103. [PubMed] [Google Scholar]
123. Eisen JL, Beer DA, Pato MT, Venditto TA, Rasmussen SA. Obsessivecompulsive disorder in patients with schizophrenia or schizoaffective disorder. Am J Psychiatry. 1997;154:271–273. [PubMed] [Google Scholar]
124. Poyurovsky M, Fuchs C, Weizman A. Obsessive-compulsive disorder in patients with first-episode schizophrenia. Am J Psychiatry. 1999;156:1998–2000. [PubMed] [Google Scholar]
125. Dowling FG, Pato MT, Pato CN. Comorbidity of obsessive-compulsive and psychotic symptoms: a review.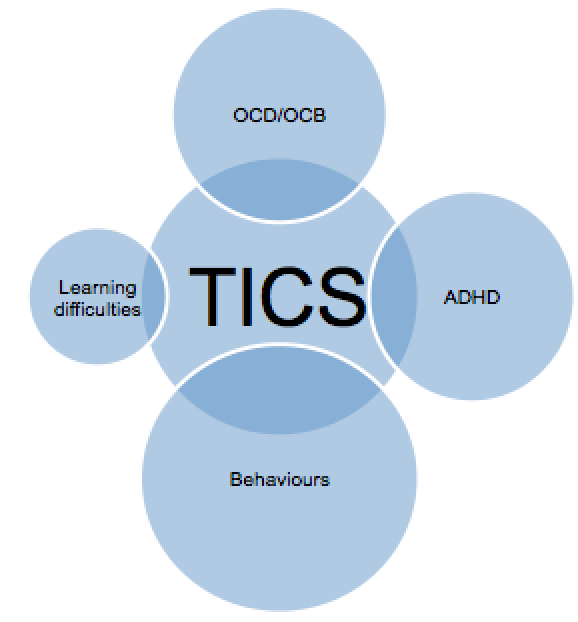 Harv Rev Psychiatry. 1995;3:75–83. [PubMed] [Google Scholar]
Harv Rev Psychiatry. 1995;3:75–83. [PubMed] [Google Scholar]
126. Fontenelle LF, do Rosario-Campos MC, De Mathis MA, et al. "Posttraumatic" obsessive-compulsive disorder: a neglected psychiatric phenotype? Inaugural Scientific Meeting of the International College of Obsessive Compulsive Spectrum Disorders. Barcelona, Spain. 2008 [Google Scholar]
127. Gershuny BS, Baer L, Radomsky AS, Wilson KA, Jenike MA. Connections among symptoms of obsessive-compulsive disorder and posttraumatic stress disorder: a case series. Behav Res Ther. 2003;41:1029–1041. [PubMed] [Google Scholar]
128. Dias-Ferreira E, Sousa JC, Melo I, et al. Chronic stress causes frontostriatal reorganization and affects decision-making. Science. 2009;325:621–625. [PubMed] [Google Scholar]
129. Guillem F, Satterthwaite J, Pampoulova T, Stip E. Relationship between psychotic and obsessive compulsive symptoms in schizophrenia. Schizophr Res. 2009;115:358–362. [PubMed] [Google Scholar]
Schizophr Res. 2009;115:358–362. [PubMed] [Google Scholar]
130. Pauls DL. The genetics of obsessive compulsive disorder: a review of the evidence. Am J Med Genet C Semin Med Genet. 2008;148C:133–139. [PubMed] [Google Scholar]
131. Nicolini H, Arnold P, Nestadt G, Lanzagorta N, Kennedy JL. Overview of genetics and obsessive-compulsive disorder. Psychiatry Res. 2009;170:7–14. [PubMed] [Google Scholar]
132. Samuels JF. Recent advances in the genetics of obsessive-compulsive disorder. Curr Psychiatry Rep. 2009;11:277–282. [PubMed] [Google Scholar]
133. Grados M, Wilcox HC. Genetics of obsessive-compulsive disorder: aresearch update. Expert Rev Neurother. 2007;7:967–980. [PubMed] [Google Scholar]
134. Bloch MH, Landeros-Weisenberger A, Sen S, et al. Association of the serotonin transporter polymorphism and obsessive-compulsive disorder: systematic review.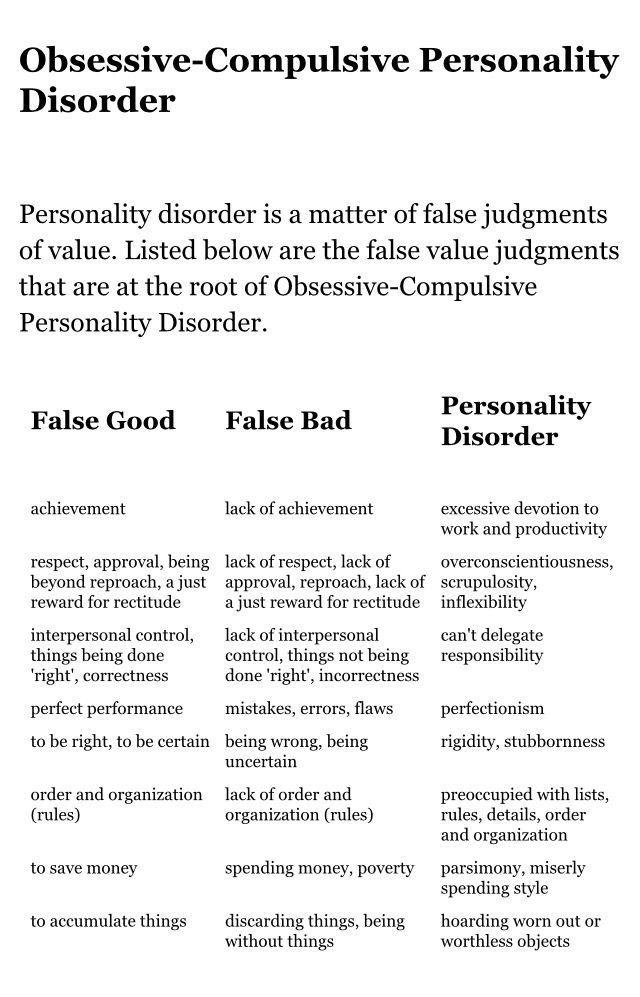 Am J Med Genet B Neuropsychiatr Genet. 2008;147B:850–858. [PubMed] [Google Scholar]
Am J Med Genet B Neuropsychiatr Genet. 2008;147B:850–858. [PubMed] [Google Scholar]
135. Wendland JR, DeGuzman TB, McMahon F, Rudnick G, DeteraWadleigh SD, Murphy DL. SERT Ileu425Val in autism, Asperger syndrome and obsessive-compulsive disorder. Psychiatr Genet. 2008;18:31–39. [PubMed] [Google Scholar]
136. Zhang H, Leckman JF, Pauls DL, Tsai CP, Kidd KK, Campos MR. Genomewide scan of hoarding in sib pairs in which both sibs have Gilles de la Tourette syndrome. Am J Hum Genet. 2002;70:896–904. [PMC free article] [PubMed] [Google Scholar]
137. Shugart YY, Samuels J, Willour VL, et al. Genomewide linkage scan for obsessive-compulsive disorder: evidence for susceptibility loci on chromosomes 3q, 7p, 1q, 1 5q, and 6q. Mol Psychiatry. 2006;11:763–770. [PubMed] [Google Scholar]
138. Samuels JF, Bienvenu OJ, Grados MA, et al. Prevalence and correlates of hoarding behavior in a community-based sample. Behav Res Ther. 2008;46:836–844. [PMC free article] [PubMed] [Google Scholar]
Behav Res Ther. 2008;46:836–844. [PMC free article] [PubMed] [Google Scholar]
139. Samuels JF, Bienvenu OJ, Pinto A, et al. Sex-specific clinical correlates of hoarding in obsessive-compulsive disorder. Behav Res Ther. 2008;46:1040–1046. [PMC free article] [PubMed] [Google Scholar]
140. Grisham JR, Brown TA, Liverant GI, Campbell-Sills L. The distinctiveness of compulsive hoarding from obsessive-compulsive disorder. J Anxiety Disord. 2005;19:767–779. [PubMed] [Google Scholar]
141. Frost RO, Steketee G, Williams LF, Warren R. Mood, personality disorder symptoms and disability in obsessive compulsive hoarders: a comparison with clinical and nonclinical controls. Behav Res Ther. 2000;38:1071–1081. [PubMed] [Google Scholar]
142. Gothelf D, Presburger G, Zohar AH, et al. Obsessive-compulsive disorder in patients with velocardiofacial (22q1 1 deletion) syndrome. Am J Med Genet B Neuropsychiatr Genet. 2004;126:99–105. [PubMed] [Google Scholar]
Am J Med Genet B Neuropsychiatr Genet. 2004;126:99–105. [PubMed] [Google Scholar]
143. Feinstein C, Eliez S, Blasey C, Reiss AL. Psychiatric disorders and behavioral problems in children with velocardiofacial syndrome: usefulness as phenotypic indicators of schizophrenia risk. Biol Psychiatry. 2002;51:312–318. [PubMed] [Google Scholar]
144. Papolos DF, Faedda GL, Veit S, et al. Bipolar spectrum disorders in patients diagnosed with velo-cardio-facial syndrome: does a hemizygous deletion of chromosome 22q11 result in bipolar affective disorder? Am J Psychiatry. 1996;153:1541–1547. [PubMed] [Google Scholar]
145. Pulver AE, Nestadt G, Goldberg R, et al. Psychotic illness in patients diagnosed with velo-cardio-facial syndrome and their relatives. J Nerv Ment Dis. 1994;182:476–478. [PubMed] [Google Scholar]
146. Saunders-Pullman R, Shriberg J, Heiman G, et al. Myoclonus dystonia: possible association with obsessive-compulsive disorder and alcohol dependence. Neurology. 2002;58:242–245. [PubMed] [Google Scholar]
Myoclonus dystonia: possible association with obsessive-compulsive disorder and alcohol dependence. Neurology. 2002;58:242–245. [PubMed] [Google Scholar]
147. Doheny D, Danisi F, Smith C, et al. Clinical findings of a myoclonus-dystonia family with two distinct mutations. Neurology. 2002;59:1244–1246. [PubMed] [Google Scholar]
148. Marechal L, Raux G, Dumanchin C, et al. Severe myoclonus-dystonia syndrome associated with a novel epsilon-sarcoglycan gene truncating mutation. Am J Med Genet B Neuropsychiatr Genet. 2003;119:114–117. [PubMed] [Google Scholar]
149. Zimprich A, Grabowski M, Asmus F, et al. Mutations in the gene encoding epsilon-sarcoglycan cause myoclonus-dystonia syndrome. Nat Genet. 2001;29:66–69. [PubMed] [Google Scholar]
150. Verkerk AJ, Mathews CA, Joosse M, Eussen BH, Heutink P, Oostra BA. CNTNAP2 is disrupted in a family with Gilles de la Tourette syndrome and obsessive compulsive disorder.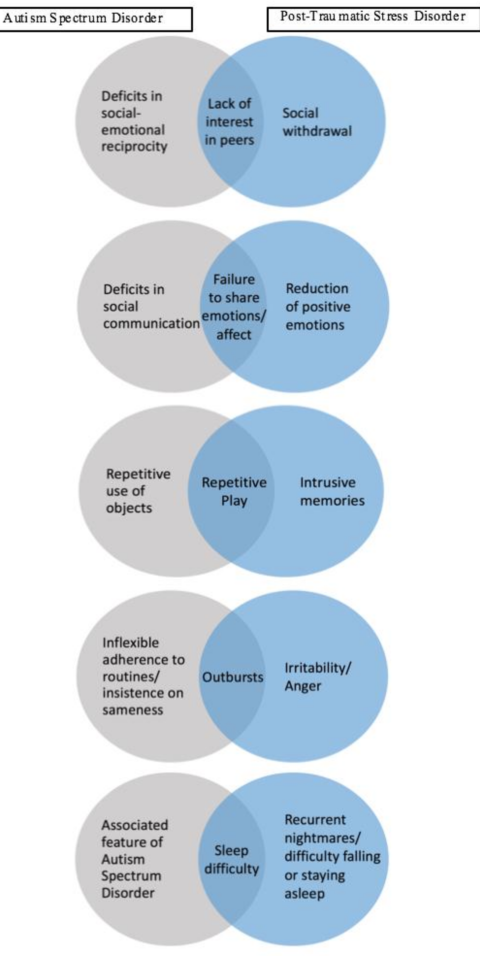 Genomics. 2003;82:1–9. [PubMed] [Google Scholar]
Genomics. 2003;82:1–9. [PubMed] [Google Scholar]
151. Boghosian-Sell L, Comings DE, Overhauser J. Tourette syndrome in a pedigree with a 7;18 translocation: identification of a YAC spanning the translocation breakpoint at 18q22.3. Am J Hum Genet. 1996;59:999–1005. [PMC free article] [PubMed] [Google Scholar]
152. Petek E, Windpassinger C, Vincent JB, et al. Disruption of a novel gene (IMMP2L) by a breakpoint in 7q31 associated with Tourette syndrome. Am J Hum Genet. 2001;68:848–858. [PMC free article] [PubMed] [Google Scholar]
153. Diaz-Anzaldua A, Joober R, Riviere JB, et al. Association between 7q31 markers and Tourette syndrome. Am J Med Genet A. 2004;127:17–20. [PubMed] [Google Scholar]
154. Bihari K, Hill JL, Murphy DL. Obsessive-compulsive characteristics in patients with idiopathic spasmodic torticollis.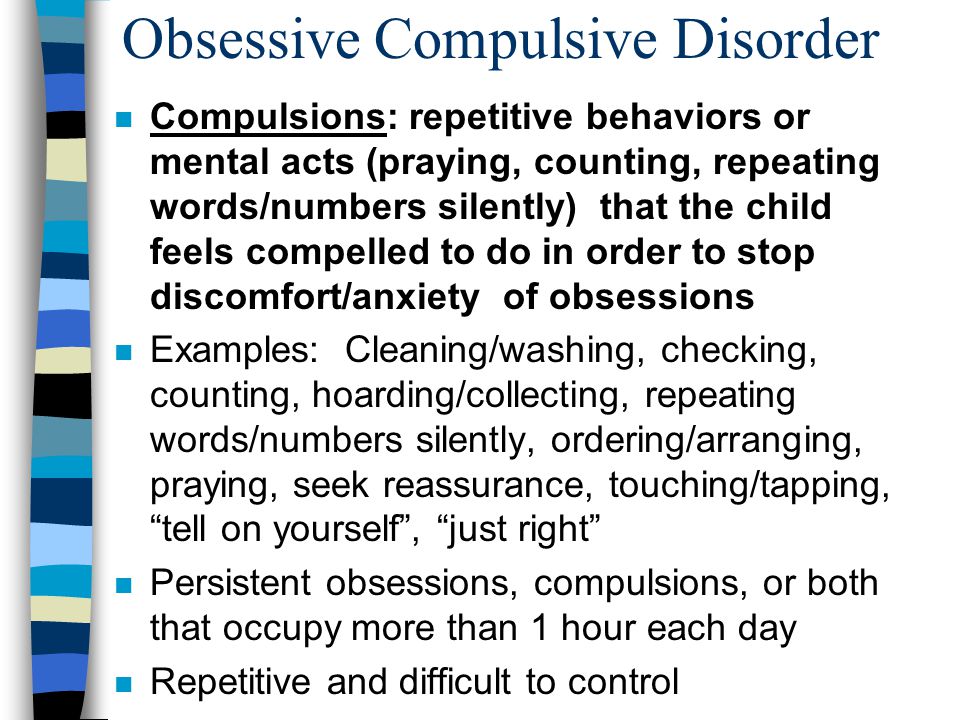 Psychiatry Res. 1992;42:267–272. [PubMed] [Google Scholar]
Psychiatry Res. 1992;42:267–272. [PubMed] [Google Scholar]
155. Bihari K, Pigott TA, Hill JL, Murphy DL. Blepharospasm and obsessivecompulsive disorder. J Nerv Ment Dis. 1992;180:130–132. [PubMed] [Google Scholar]
156. Defazio G, Livrea P. Epidemiology of primary blepharospasm. Mov Disord. 2002;17:7–12. [PubMed] [Google Scholar]
157. Marks WA, Honeycutt J, Acosta F, Reed M. Deep brain stimulation for pediatric movement disorders. Semin Pediatr Neurol. 2009;16:90–98. [PubMed] [Google Scholar]
158. Hoehn-Saric R, Ninan P, Black DW, et al. Multicenter double-blind comparison of sertraline and desipramine for concurrent obsessive-compulsive and major depressive disorders. Arch Gen Psychiatry. 2000;57:76–82. [PubMed] [Google Scholar]
159. Matsumoto R, Ichise M, Ito H, et al. Reduced serotonin transporter binding in the insular cortex in patients with obsessive-compulsive disorder: a [11C]DASB PET study. Neuroimage. 2010;49:121–126. [PubMed] [Google Scholar]
Neuroimage. 2010;49:121–126. [PubMed] [Google Scholar]
160. MacMaster FP, O'Neill J, Rosenberg DR. Brain imaging in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:1262–1272. [PMC free article] [PubMed] [Google Scholar]
161. Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive-compulsive disorder. Arch Gen Psychiatry. 2004;61:564–576. [PubMed] [Google Scholar]
162. Chamberlain SR, Menzies L. Endophenotypes of obsessive-compulsive disorder: rationale, evidence and future potential. Expert Rev Neurother. 2009;9:1133–1146. [PubMed] [Google Scholar]
163. Hajcak G, Franklin ME, Foa EB, Simons RF. Increased error-related brain activity in pediatric obsessive-compulsive disorder before and after treatment.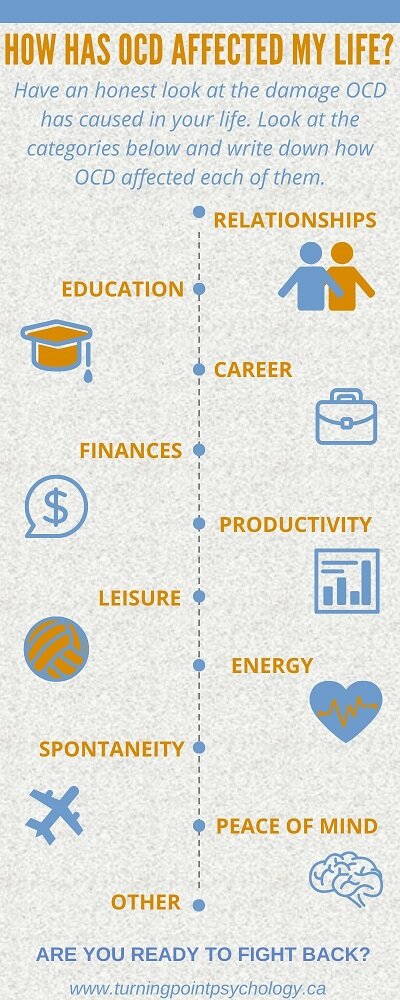 Am J Psychiatry. 2008;165:116–123. [PubMed] [Google Scholar]
Am J Psychiatry. 2008;165:116–123. [PubMed] [Google Scholar]
164. Bedard MJ, Joyal CC, Godbout L, Chantal S. Executive functions and the obsessive-compulsive disorder: on the importance of subclinical symptoms and other concomitant factors. Arch Clin Neuropsychol. 2009;24:585–598. [PubMed] [Google Scholar]
165. Joshi G, Wilens T T. Child Adolesc Psychiatr Clin N Am. 2009;18:291–319. [PMC free article] [PubMed] [Google Scholar]
166. Welch JM, Lu J, Rodriguiz RM, et al. Cortico-striatal synaptic defects and OCD-like behaviours in Sapap3-mutant mice. Nature. 2007;448:894–900. [PMC free article] [PubMed] [Google Scholar]
167. Zuchner S, Wendland JR, Ashley-Koch AE, et al. Multiple rare SAPAP3 missense variants in trichotillomania and OCD. Mol Psychiatry. 2009;14:6–9. [PMC free article] [PubMed] [Google Scholar]
International OCD Foundation | Disorders Related to OCD
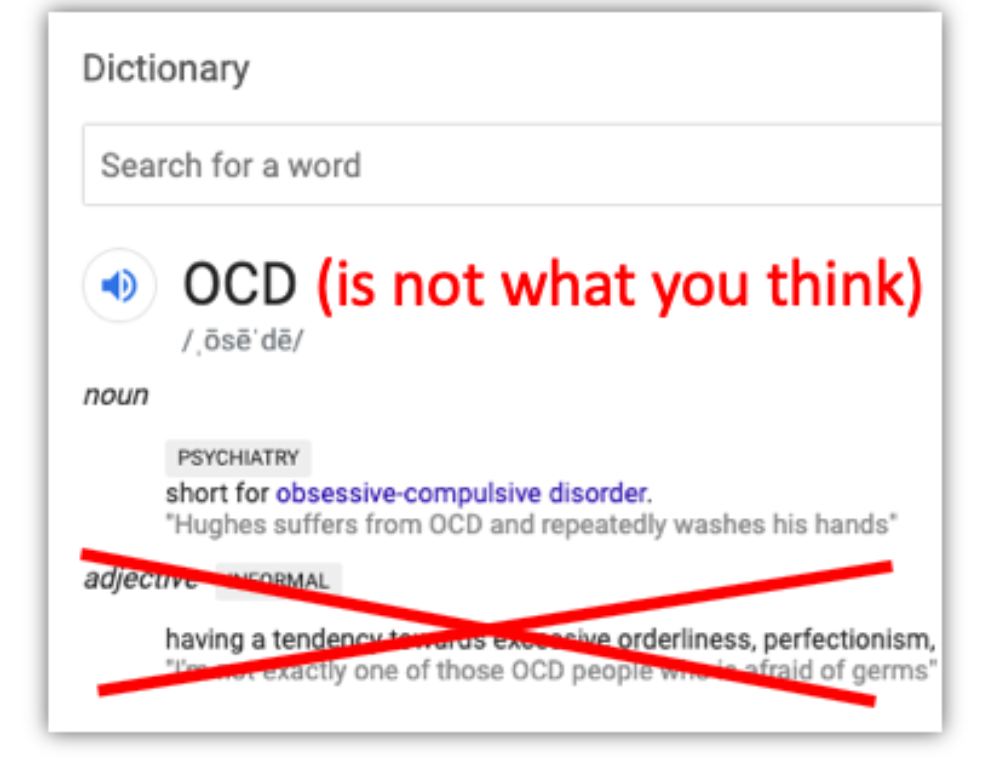
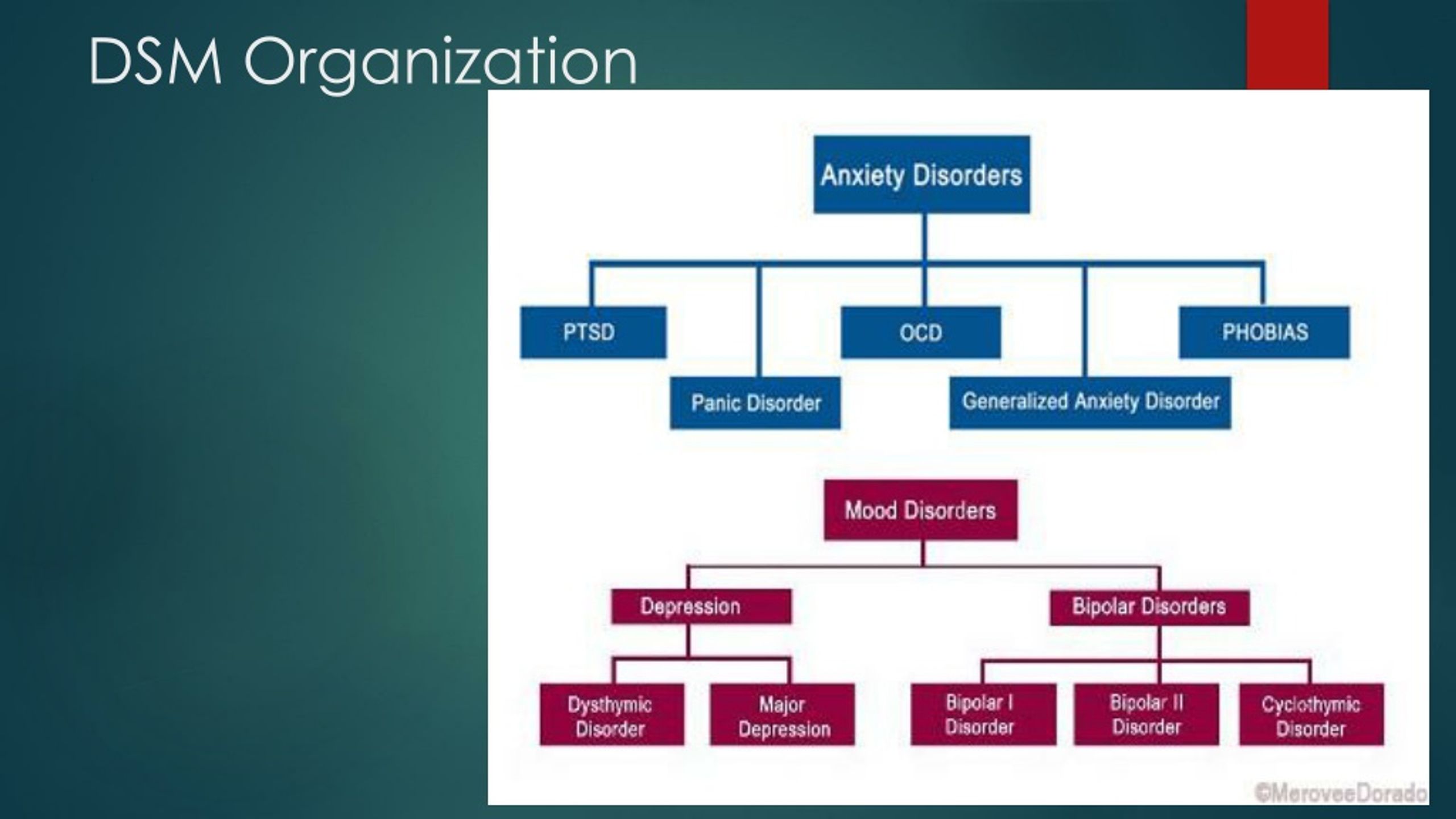
One of the stumbling blocks to accessing effective treatment for individuals with OCD is that OCD can sometimes be confused with other disorders. The newest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) — which mental health professionals use to help diagnose mental health disorders — in fact, groups together these “related disorders” in the same chapter.
The newest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) — which mental health professionals use to help diagnose mental health disorders — in fact, groups together these “related disorders” in the same chapter.
While some disorders can have overlapping symptoms with each other, being diagnosed with the right disorder has incredibly important implications for treatment, and therefore it is important to make sure you receive the right diagnosis. Even similar disorders can have very different treatments. And providing the wrong treatment for someone can result in extended, unnecessary suffering, wasted time, wasted resources, and potentially feeling hopeless about getting better.
Disorders Related to OCD
Below is a list of disorders grouped together with OCD in a “chapter” in the DSM-5. As you can see, these disorders share some common characteristics, but can also be differentiated in important ways. These are all referred to as Obsessive Compulsive Related Disorders or OC Related Disorders (they are also sometimes called OC Spectrum Disorders):
Hoarding Disorder (HD) Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Hoarding DisorderTo learn more:
| People with Hoarding Disorder and people with OCD both:
| People with Hoarding Disorder:
People with OCD:
|
Body Dysmorphic Disorder (BDD) Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Body Dysmorphic Disorder (BDD)To learn more:
| People with BDD and people with OCD both:
| People with BDD:
People with OCD:
|
Body Focused Repetitive Behaviors (BFRBs) Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Body Focused Repetitive Behaviors (BFRBs) (Trichotillomania / Hair-pulling Disorder and Skin-picking / Dermotillomania / Excoriation Disorder)To learn more:
| People with BFRBs and people with OCD both:
| People with BFRBs:
People with OCD:
|
Olfactory Reference Syndrome (ORS) Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
| Olfactory Reference Syndrome (ORS) To learn more:
| People with ORS and people with OCD both:
| People with ORS:
People with OCD:Can have obsessions related to a wide variety of topics. |
Misophonia Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
| Misophonia To learn more:
| People with Misophonia and people with OCD both:
| People with Misophonia:
People with OCD:Can have obsessions related to a wide variety of topics. |
Emetophobia Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
| Emetophobia To learn more:
| People with Emetophobia and people with OCD both:
| People with Emetophobia:
People with OCD:Can have fears (obsessions) related to a wide variety of topics. |
Disorders Related to PANDAS/PANS
In 1998, Dr. Susan Swedo identified a subtype of OCD in kids which she referred to as PANDAS. The importance of this observation is that these children tend to show OCD symptoms in a more extreme way and need medical attention in addition to psychological help. It is important, in cases where a child shows OCD symptoms "seemingly overnight" and with a severe onset, that they be evaluated by their pediatrician as soon as possible.
Susan Swedo identified a subtype of OCD in kids which she referred to as PANDAS. The importance of this observation is that these children tend to show OCD symptoms in a more extreme way and need medical attention in addition to psychological help. It is important, in cases where a child shows OCD symptoms "seemingly overnight" and with a severe onset, that they be evaluated by their pediatrician as soon as possible.
PANDAS/PANS Expand
Related Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
PANDAS / PANS(Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections) / (Pediatric Acute-onset NeuropsychiatricSyndrome) To learn more:
| Children and teens with OCD and PANDAS/PANS both:
| Children with OCD:
While PANDAS/PANS:
Additionally, children with PANDAS/PANS will show additional symptoms not typically seen in kids with OCD including:
|
Disorders Confused with OCD
In addition to the Related Disorders there are some additional disorders that are commonly confused with OCD. These disorders show some common characteristics and overlapping features, but can also be distinguished from OCD and one another by a well-trained mental health provider. These disorders include:
These disorders include:
Tic Disorders/Tourette Syndrome Expand
Similar Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Tic Disorders/Tourette SyndromeTo learn more:
| People with Tics/Tourette Syndrome and people with OCD both:
| People with Tics or Tourette Syndrome:
People with OCD:
|
Impulse Control Disorders Expand
Similar Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Impulse Control Disorders(addictions to gambling, sexual activity, excessive shopping)To learn more:
| People with Impulse Control Disorders and people with OCD both may have:
| People with Impulse Control Disorders:
People with OCD:
|
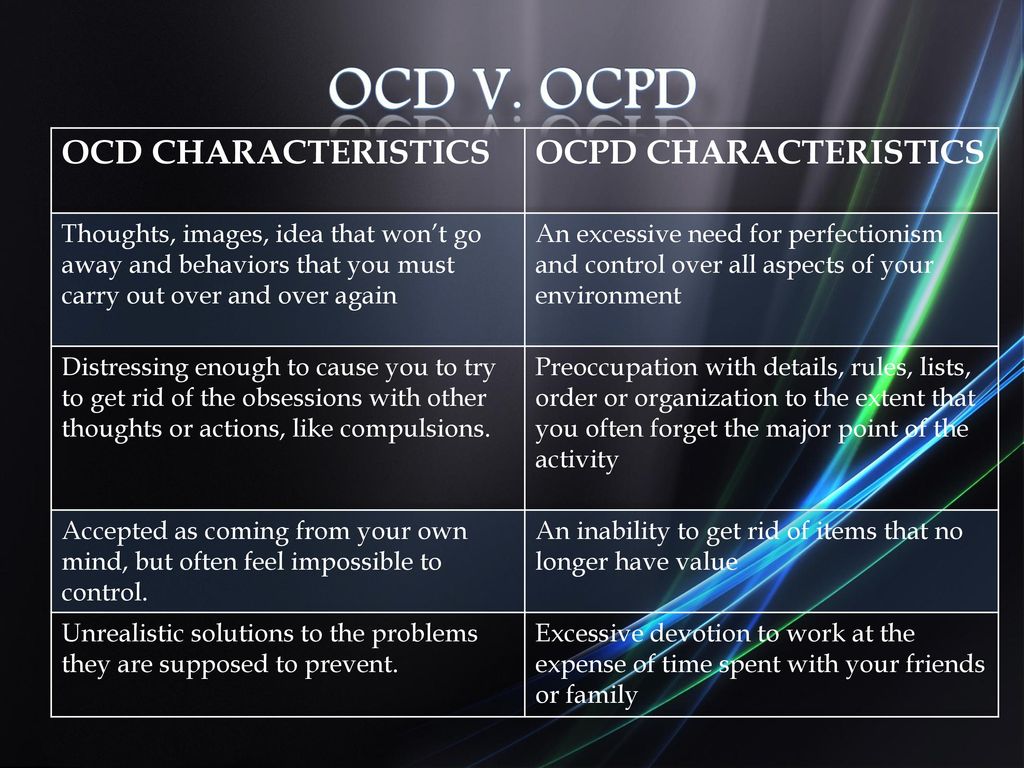
Obsessive Compulsive Personality Disorder (OCPD) Expand
Similar Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Obsessive Compulsive Personality Disorder (OCPD)To learn more:
| People with OCPD and people with OCD both have problems with:
| People with OCPD:
People with OCD:
|
Autism Spectrum Disorders Expand
Similar Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Autism Spectrum DisordersTo learn more:
| People with Autism Spectrum Disorders and people with OCD all may have:
| People with Autism Spectrum Disorders:
People with OCD:
|
Psychotic Disorders/ Schizophrenia Expand
Similar Disorder | How This Disorder "Looks Like" OCD | How This Disorder Differs from OCD |
Psychotic Disorders/ Schizophrenia | People with Psychotic Disorders/Schizophrenia and people with OCD both may have:
| People with Psychotic Disorders/Schizophrenia:
People with OCD:
|
Obsessive-compulsive disorder
A prominent role among mental illnesses is played by syndromes (complexes of symptoms), united in the group of obsessive-compulsive disorder (OCD), which received its name from the Latin terms obsessio and compulsio.
Obsession (lat. obsessio - taxation, siege, blockade).
Compulsions (lat. compello - I force). 1. Obsessive drives, a kind of obsessive phenomena (obsessions). Characterized by irresistible attraction that arises contrary to the mind, will, feelings.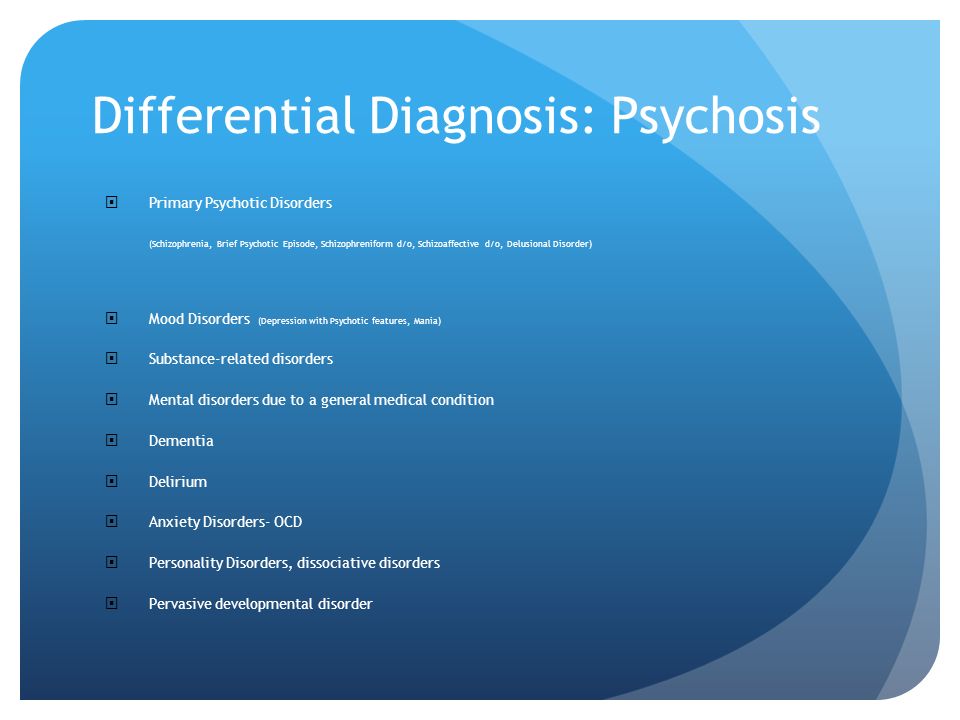 Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
In domestic psychiatry, obsessive states were understood as psychopathological phenomena, characterized by the fact that phenomena of a certain content repeatedly appear in the mind of the patient, accompanied by a painful feeling of coercion [Zinoviev PM, 193I]. For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them.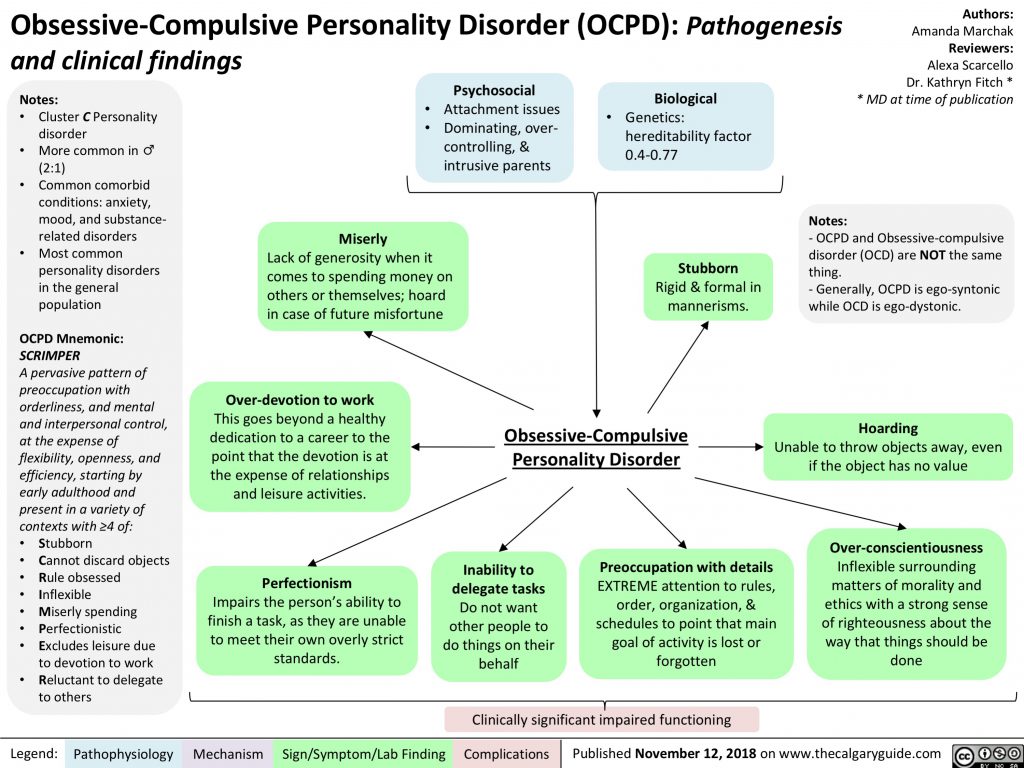 They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.
They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account. Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.
Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A. M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
Currently, almost all obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder".
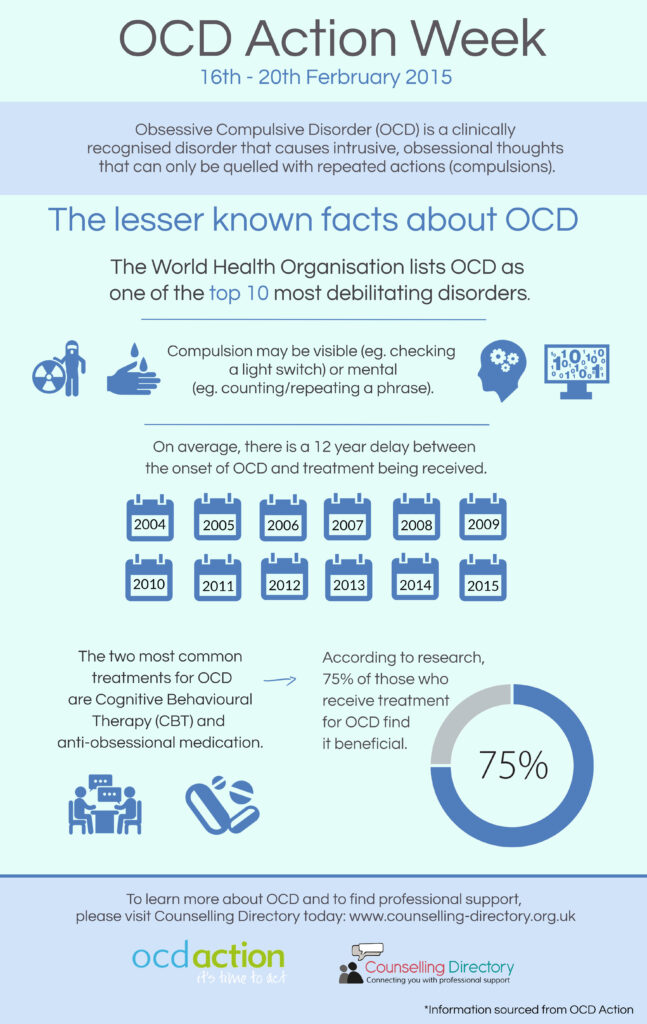
OKR concepts have undergone a fundamental reassessment over the past 15 years. During this time, the clinical and epidemiological significance of OCD has been completely revised. If it was previously thought that this is a rare condition observed in a small number of people, now it is known that OCD is common and causes a high percentage of morbidity, which requires the urgent attention of psychiatrists around the world. Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD. And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
The discovery that intense serotonin reuptake inhibition (SSRI) was the key to effective treatment for OCD was the first step in a revolution and spurred clinical research that showed the efficacy of such selective inhibitors.
As described in ICD-10, the main features of OCD are repetitive intrusive (obsessive) thoughts and compulsive actions (rituals).
In a broad sense, the core of OCD is the syndrome of obsession, which is a condition with a predominance in the clinical picture of feelings, thoughts, fears, memories that arise in addition to the desire of patients, but with awareness of their pain and a critical attitude towards them. Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them.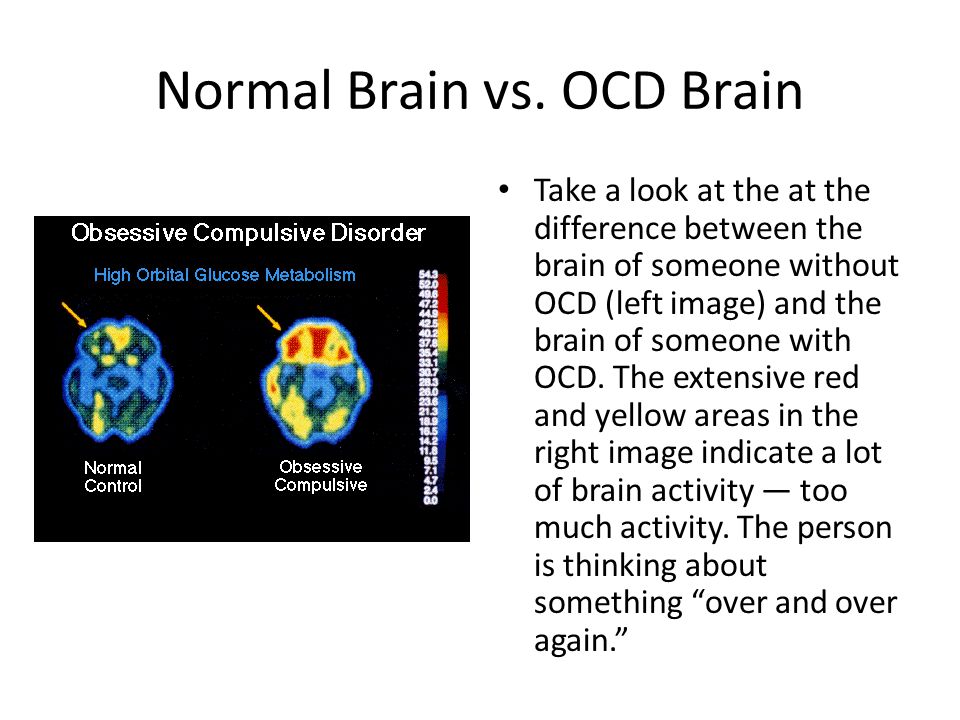 Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessions in the ICD-10 are included in the group of neurotic disorders.
The prevalence of OCD in the population is quite high. According to some data, it is determined by an indicator of 1.5% (meaning "fresh" cases of diseases) or 2-3%, if episodes of exacerbations observed throughout life are taken into account. Those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. It is believed that men and women are affected approximately equally.
CLINICAL PICTURE
The problem of obsessive-compulsive disorders attracted the attention of clinicians already at the beginning of the 17th century.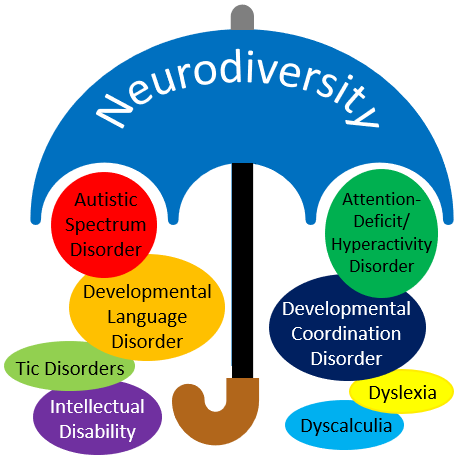 They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
Main clinical manifestations of OCD:
Obsessional thoughts - painful, arising against the will, but recognized by the patient as their own, ideas, beliefs, images, which in a stereotyped form forcibly invade the patient's consciousness and which he tries to resist in some way. It is this combination of an inner sense of compulsive urge and efforts to resist it that characterizes obsessional symptoms, but of the two, the degree of effort exerted is the more variable. Obsessional thoughts may take the form of single words, phrases, or lines of poetry; they are usually unpleasant to the patient and may be obscene, blasphemous, or even shocking.
Obsessional imagery is vivid scenes, often violent or disgusting, including, for example, sexual perversion.
Obsessional impulses are urges to do things that are usually destructive, dangerous or shameful; for example, jumping into the road in front of a moving car, injuring a child, or shouting obscene words while in society.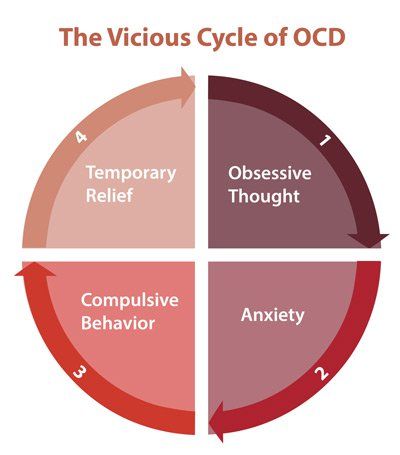
Obsessional rituals include both mental activities (eg, counting repeatedly in a particular way, or repeating certain words) and repetitive but meaningless acts (eg, washing hands twenty or more times a day). Some of them have an understandable connection with the obsessive thoughts that preceded them, for example, repeated washing of hands - with thoughts of infection. Other rituals (for example, regularly laying out clothes in some complex system before putting them on) do not have such a connection. Some patients feel an irresistible urge to repeat such actions a certain number of times; if that fails, they are forced to start all over again. Patients are invariably aware that their rituals are illogical and usually try to hide them. Some fear that such symptoms are a sign of the onset of insanity. Both obsessive thoughts and rituals inevitably lead to problems in daily activities.
Obsessive rumination (“mental chewing gum”) is an internal debate in which the arguments for and against even the simplest everyday actions are endlessly revised.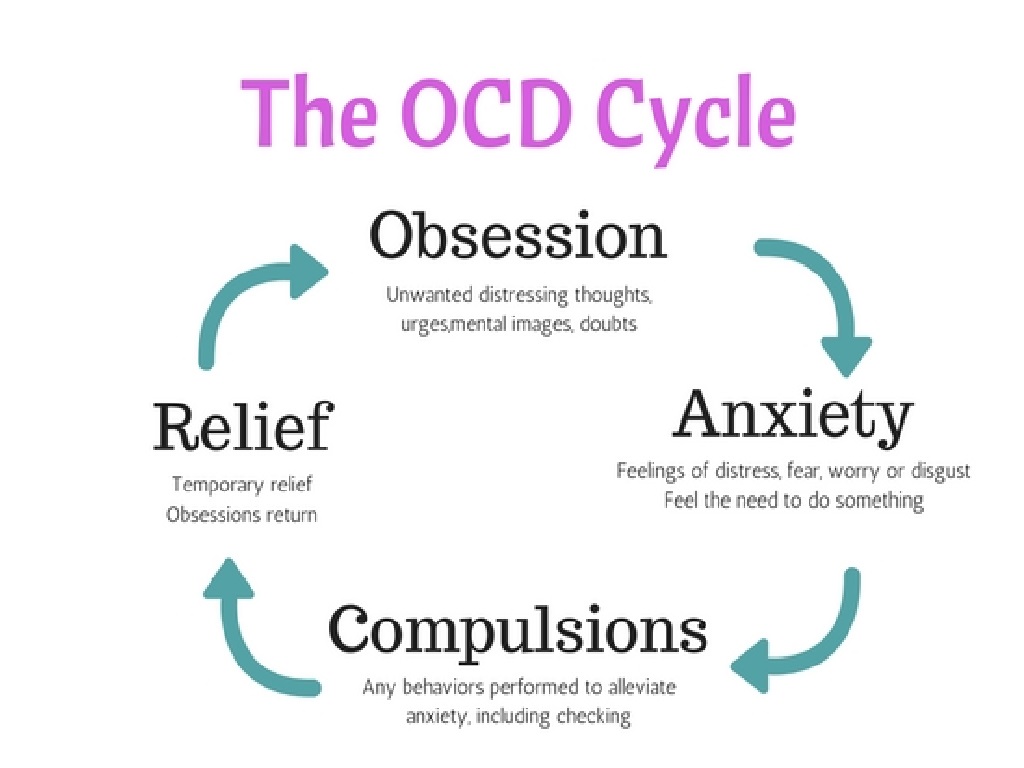 Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Compulsive actions - repetitive stereotypical actions, sometimes acquiring the character of protective rituals. The latter are aimed at preventing any objectively unlikely events that are dangerous for the patient or his relatives.
In addition to the above, in a number of obsessive-compulsive disorders, a number of well-defined symptom complexes stand out, and among them are obsessive doubts, contrasting obsessions, obsessive fears - phobias (from the Greek. phobos).
Obsessive thoughts and compulsive rituals may intensify in certain situations; for example, obsessive thoughts about harming other people often become more persistent in the kitchen or some other place where knives are kept.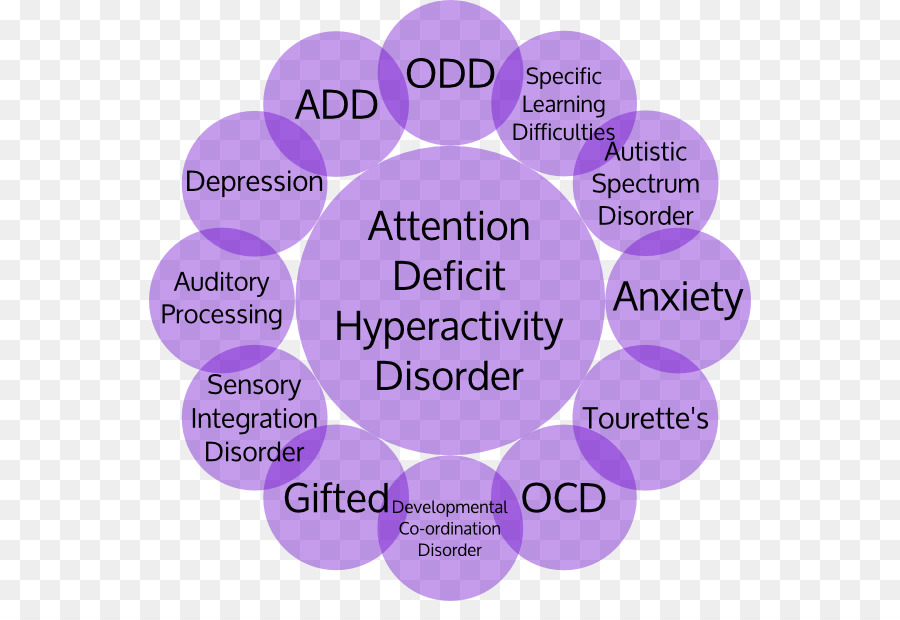 Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Obsessions (obsessions) are divided into figurative or sensual, accompanied by the development of affect (often painful) and obsessions of affectively neutral content.
Sensual obsessions include obsessive doubts, memories, ideas, drives, actions, fears, an obsessive feeling of antipathy, an obsessive fear of habitual actions.
Obsessive doubts - intrusively arising contrary to logic and reason, uncertainty about the correctness of committed and committed actions. The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
Obsessive memories include persistent, irresistible painful memories of any sad, unpleasant or shameful events for the patient, accompanied by a sense of shame, remorse. They dominate the mind of the patient, despite the efforts and efforts not to think about them.
Obsessive impulses - urges to commit one or another tough or extremely dangerous action, accompanied by a feeling of horror, fear, confusion with the inability to get rid of it. The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
Manifestations of obsessive ideas can be different. In some cases, this is a vivid "vision" of the results of obsessive drives, when patients imagine the result of a cruel act committed. In other cases, obsessive ideas, often referred to as mastering, appear in the form of implausible, sometimes absurd situations that patients take for real. An example of obsessive ideas is the patient's conviction that the buried relative was alive, and the patient painfully imagines and experiences the suffering of the deceased in the grave. At the height of obsessive ideas, the consciousness of their absurdity, implausibility disappears and, on the contrary, confidence in their reality appears. As a result, obsessions acquire the character of overvalued formations (dominant ideas that do not correspond to their true meaning), and sometimes delusions.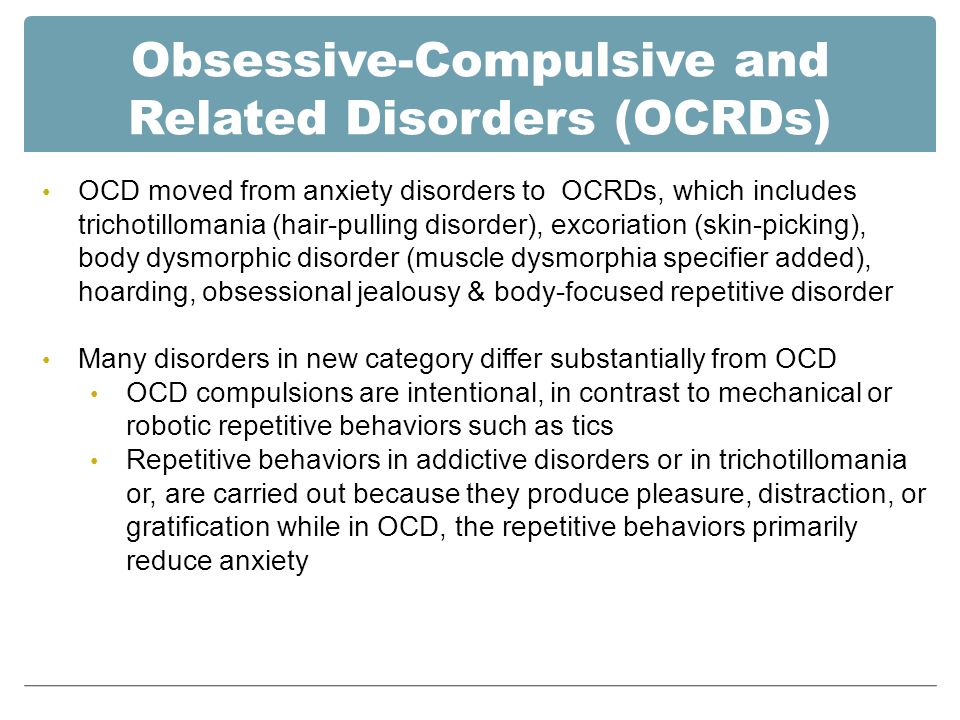
An obsessive feeling of antipathy (as well as obsessive blasphemous and blasphemous thoughts) - unjustified, driven away by the patient from himself antipathy towards a certain, often close person, cynical, unworthy thoughts and ideas in relation to respected people, in religious persons - in relation to saints or ministers churches.
Obsessive acts are acts done against the wishes of the sick, despite efforts made to restrain them. Some of the obsessive actions burden the patients until they are realized, others are not noticed by the patients themselves. Obsessive actions are painful for patients, especially in those cases when they become the object of attention of others.
Obsessive fears, or phobias, include an obsessive and senseless fear of heights, large streets, open or confined spaces, large crowds of people, the fear of sudden death, the fear of falling ill with one or another incurable disease. Some patients may develop a wide variety of phobias, sometimes acquiring the character of fear of everything (panphobia).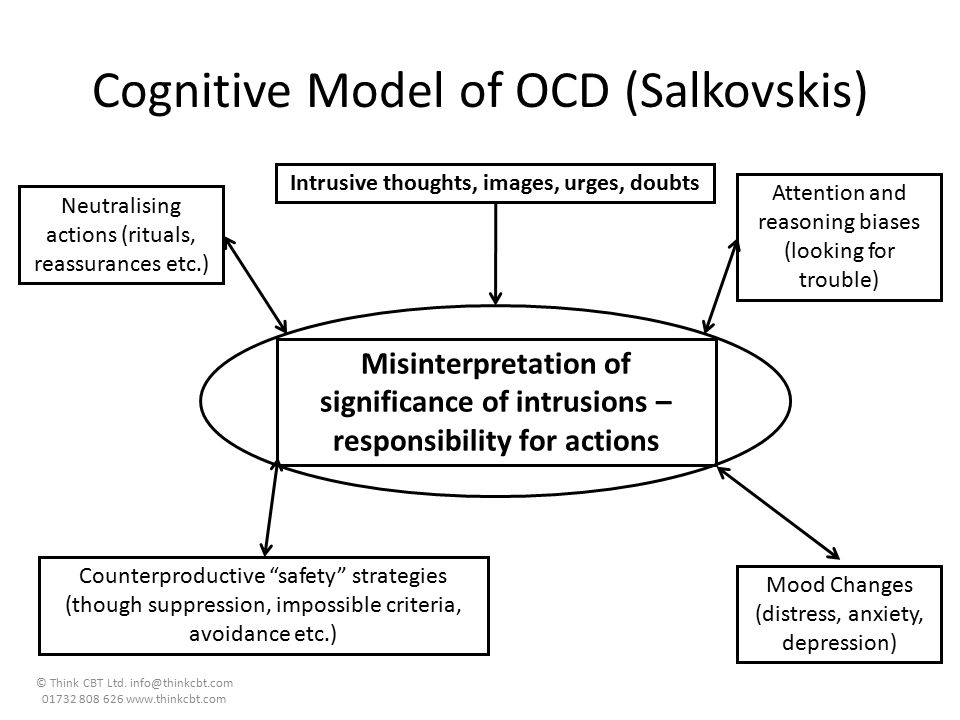 And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
Hypochondriacal phobias (nosophobia) - an obsessive fear of some serious illness. Most often, cardio-, stroke-, syphilo- and AIDS phobias are observed, as well as the fear of the development of malignant tumors. At the peak of anxiety, patients sometimes lose their critical attitude to their condition - they turn to doctors of the appropriate profile, require examination and treatment. The implementation of hypochondriacal phobias occurs both in connection with psycho- and somatogenic (general non-mental illnesses) provocations, and spontaneously. As a rule, hypochondriacal neurosis develops as a result, accompanied by frequent visits to doctors and unreasonable medication.
Specific (isolated) phobias - obsessive fears limited to a strictly defined situation - fear of heights, nausea, thunderstorms, pets, treatment at the dentist, etc. Since contact with situations that cause fear is accompanied by intense anxiety, the patients tend to avoid them.
Obsessive fears are often accompanied by the development of rituals - actions that have the meaning of "magic" spells that are performed, despite the critical attitude of the patient to obsession, in order to protect against one or another imaginary misfortune: before starting any important business, the patient must perform some that specific action to eliminate the possibility of failure. Rituals can, for example, be expressed in snapping fingers, playing a melody to the patient or repeating certain phrases, etc. In these cases, even relatives are not aware of the existence of such disorders. Rituals, combined with obsessions, are a fairly stable system that usually exists for many years and even decades.
Obsessions of affectively neutral content - obsessive sophistication, obsessive counting, recalling neutral events, terms, formulations, etc. Despite their neutral content, they burden the patient, interfere with his intellectual activity.
Contrasting obsessions ("aggressive obsessions") - blasphemous, blasphemous thoughts, fear of harming oneself and others.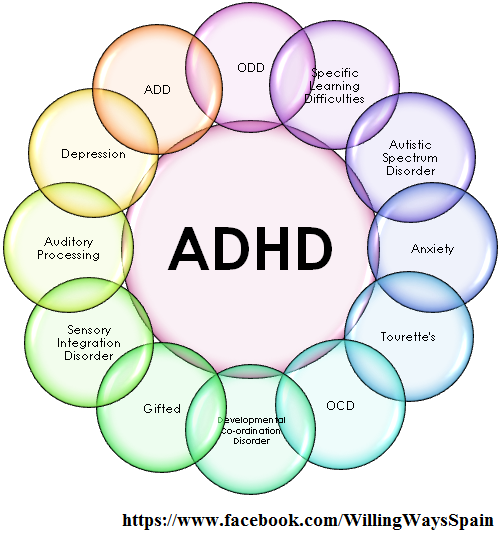 Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.
Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc. ). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
Obsessions of pollution (mysophobia). This group of obsessions includes both the fear of pollution (earth, dust, urine, feces and other impurities), as well as the fear of penetration into the body of harmful and toxic substances (cement, fertilizers, toxic waste), small objects (glass fragments, needles, specific types of dust), microorganisms. In some cases, the fear of contamination can be limited, remain at the preclinical level for many years, manifesting itself only in some features of personal hygiene (frequent change of linen, repeated washing of hands) or in housekeeping (thorough handling of food, daily washing of floors). , "taboo" on pets). This kind of monophobia does not significantly affect the quality of life and is evaluated by others as habits (exaggerated cleanliness, excessive disgust).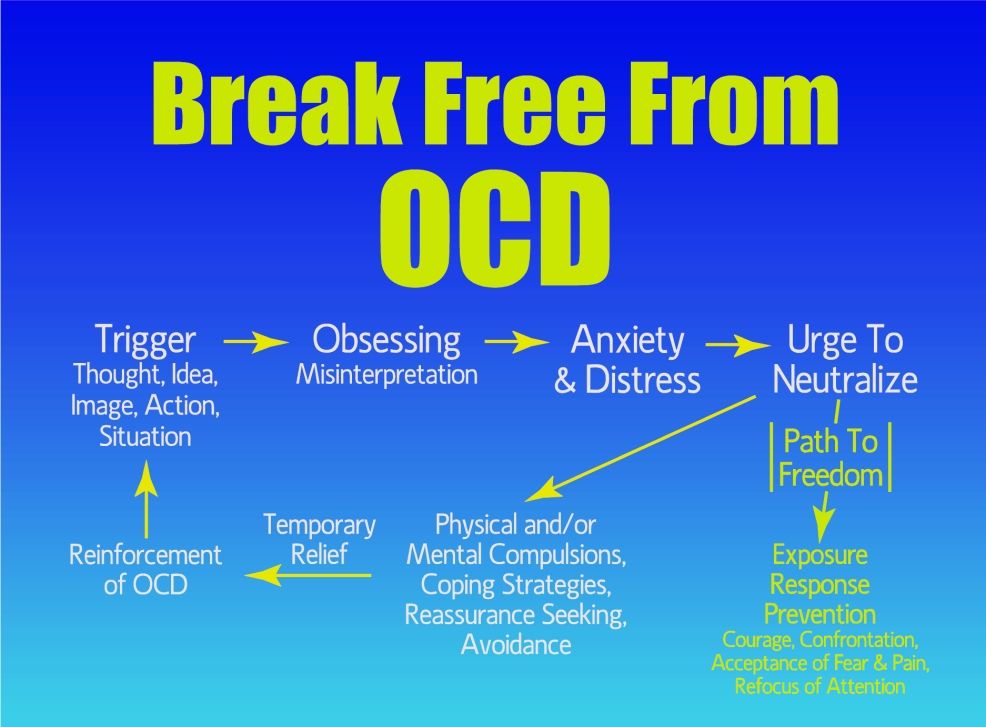 Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.
Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.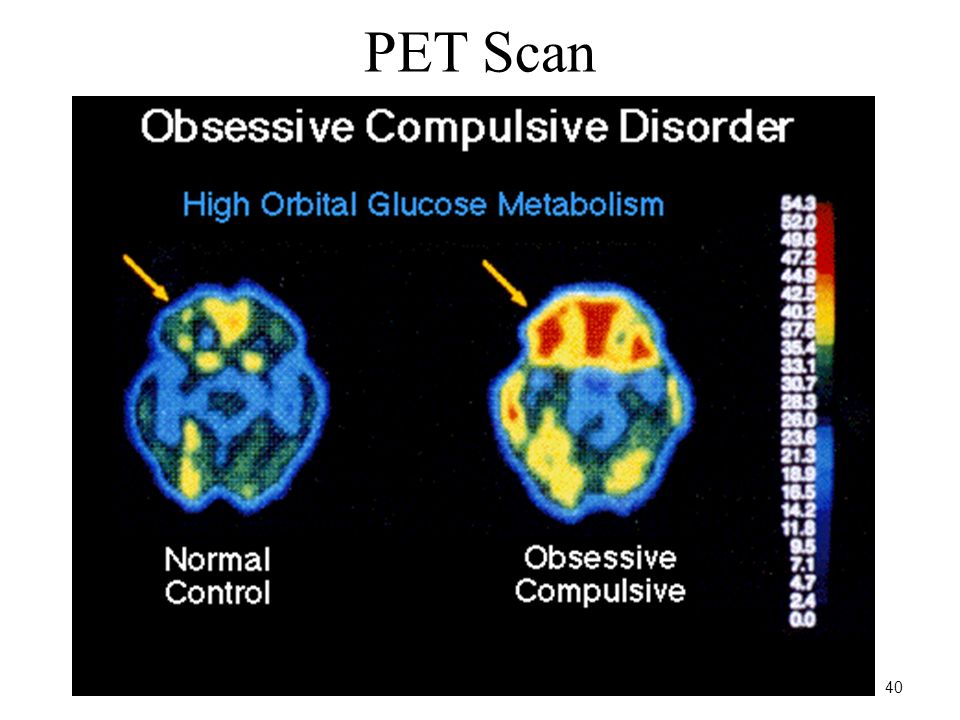 In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
A special place in the series of obsessions is occupied by obsessive actions in the form of isolated, monosymptomatic movement disorders. Among them, especially in childhood, tics predominate, which, unlike organically conditioned involuntary movements, are much more complex motor acts that have lost their original meaning. Tics sometimes give the impression of exaggerated physiological movements. This is a kind of caricature of certain motor acts, natural gestures. Patients suffering from tics can shake their heads (as if checking whether the hat fits well), make hand movements (as if discarding interfering hair), blink their eyes (as if getting rid of a mote). Along with obsessive tics, pathological habitual actions (lip biting, gnashing of teeth, spitting, etc.) are often observed, which differ from obsessive actions proper in the absence of a subjectively painful sense of persistence and experience them as alien, painful.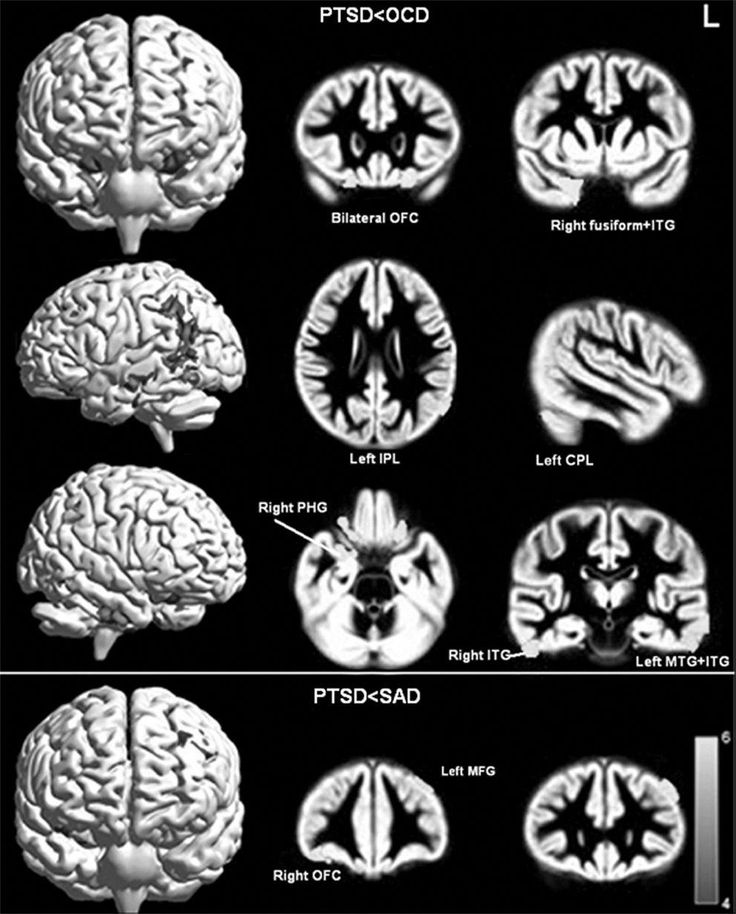 Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
The course of obsessive-compulsive disorder.
Unfortunately, chronization must be indicated as the most characteristic trend in the OCD dynamics. Cases of episodic manifestations of the disease and complete recovery are relatively rare. However, in many patients, especially with the development and preservation of one type of manifestation (agoraphobia, obsessive counting, ritual handwashing, etc.), a long-term stabilization of the condition is possible. In these cases, there is a gradual (usually in the second half of life) mitigation of psychopathological symptoms and social readaptation. For example, patients who experienced fear of traveling on certain types of transport, or public speaking, cease to feel flawed and work along with healthy people. In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
More severe and complex OCDs such as phobias of infection, pollution, sharp objects, contrasting performances, multiple rituals, on the other hand, may become persistent, resistant to treatment, or show a tendency to recur with disorders that persist despite active therapy. Further negative dynamics of these conditions indicates a gradual complication of the clinical picture of the disease as a whole.
DIFFERENTIAL DIAGNOSIS
It is important to distinguish OCD from other disorders that involve compulsions and rituals. In some cases, obsessive-compulsive disorder must be differentiated from schizophrenia, especially when the obsessive thoughts are unusual in content (eg, mixed sexual and blasphemous themes) or the rituals are exceptionally eccentric. The development of a sluggish schizophrenic process cannot be ruled out with the growth of ritual formations, their persistence, the emergence of antagonistic tendencies in mental activity (inconsistency of thinking and actions), and the uniformity of emotional manifestations.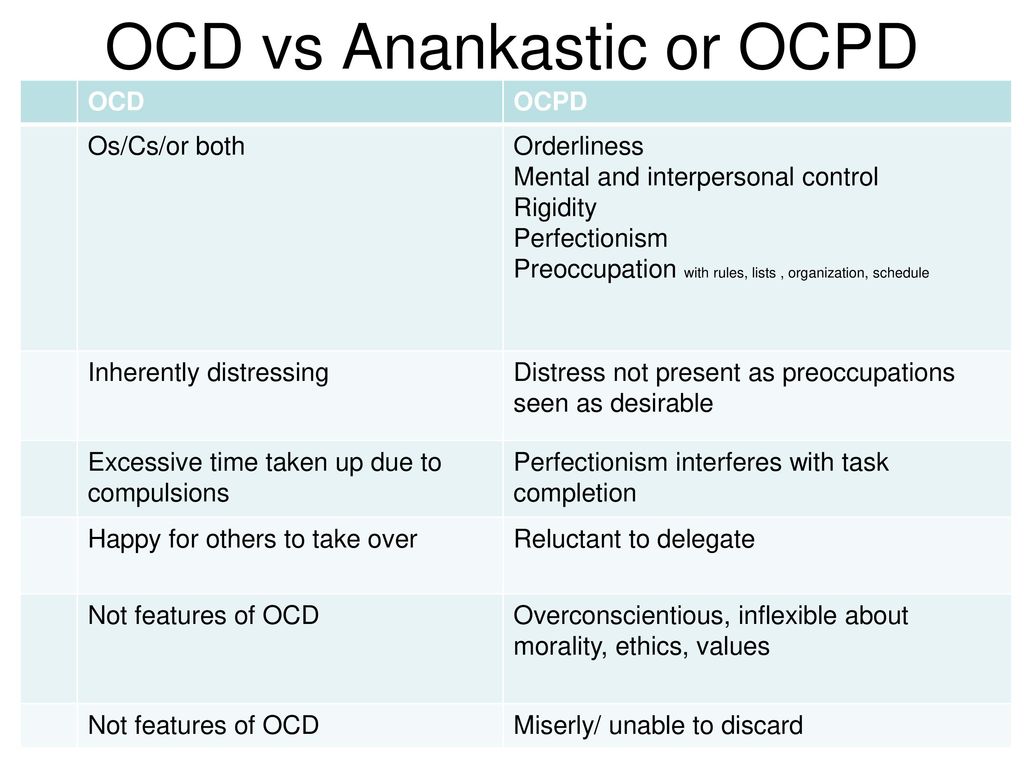 Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.
Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.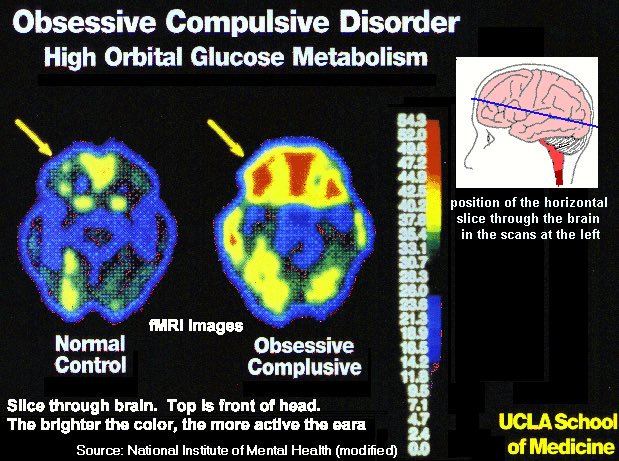 In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
Genetic factors
Speaking about hereditary predisposition to OCD, it should be noted that obsessive-compulsive disorders are found in approximately 5-7% of parents of patients with such disorders. Although this figure is low, it is higher than in the general population. While the evidence for a hereditary predisposition to OCD is still uncertain, psychasthenic personality traits can be largely explained by genetic factors.
FORECAST
Approximately two-thirds of OCD patients improve within a year, more often by the end of this period. If the disease lasts more than a year, fluctuations are observed during its course - periods of exacerbations are interspersed with periods of improvement in health, lasting from several months to several years. The prognosis is worse if we are talking about a psychasthenic personality with severe symptoms of the disease, or if there are continuous stressful events in the patient's life. Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
TREATMENT: BASIC METHODS AND APPROACHES
Despite the fact that OCD is a complex group of symptom complexes, the principles of treatment for them are the same. The most reliable and effective method of treating OCD is considered to be drug therapy, during which a strictly individual approach to each patient should be manifested, taking into account the characteristics of the manifestation of OCD, age, gender, and the presence of other diseases. In this regard, we must warn patients and their relatives against self-treatment. If any disorders similar to mental ones appear, it is necessary, first of all, to contact the specialists of the psycho-neurological dispensary at the place of residence or other psychiatric medical institutions to establish the correct diagnosis and prescribe competent adequate treatment.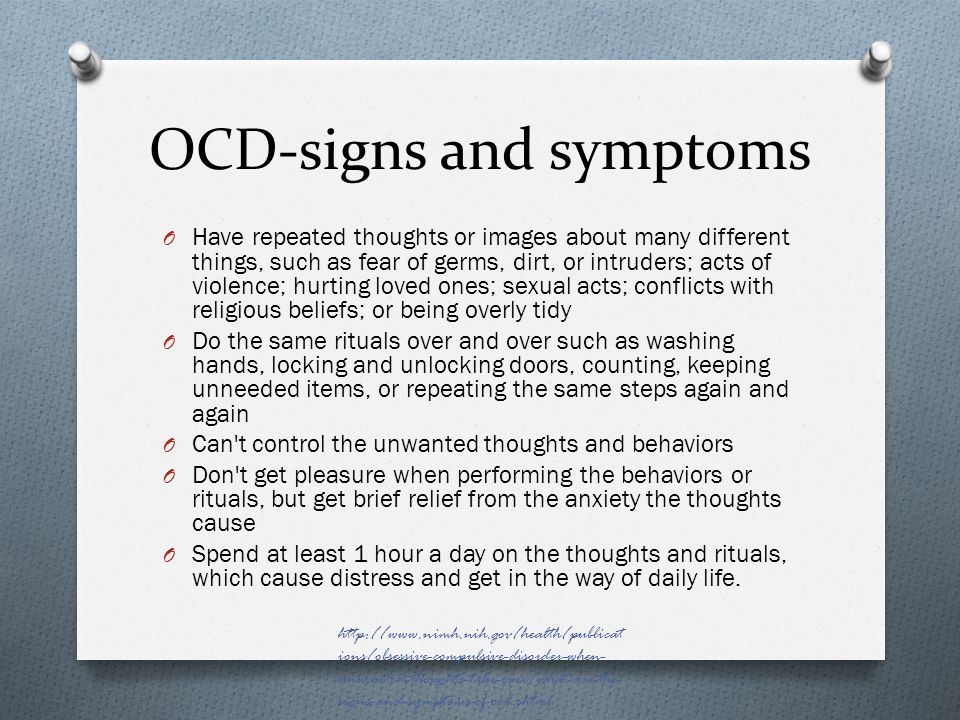 At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
When treating, it must be borne in mind that obsessive-compulsive disorders often have a fluctuating course with long periods of remission (improvement). The apparent suffering of the patient often seems to call for vigorous effective treatment, but the natural course of the condition must be kept in mind in order to avoid the typical error of over-intensive therapy. It is also important to consider that OCD is often accompanied by depression, the effective treatment of which often leads to an alleviation of obsessional symptoms.
The treatment of OCD begins with an explanation of the symptoms to the patient and, if necessary, with reassurance that they are the initial manifestation of insanity (a common concern for patients with obsessions).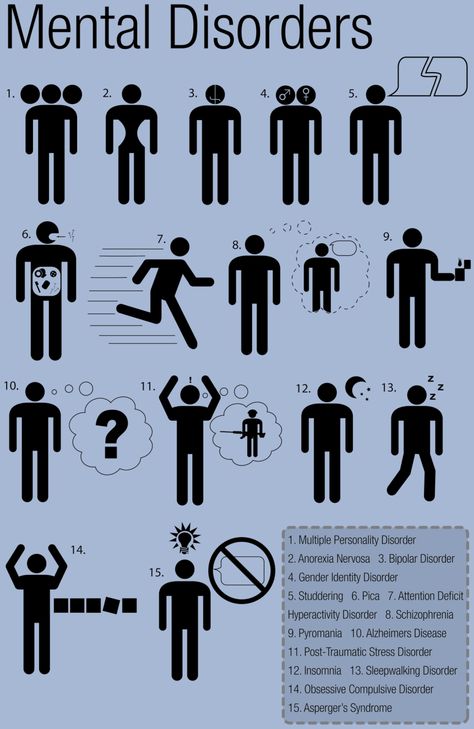 Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Drug therapy
The following therapeutic approaches exist for the currently identified types of OCD. Of the pharmacological drugs for OCD, serotonergic antidepressants, anxiolytics (mainly benzodiazepine), beta-blockers (to stop autonomic manifestations), MAO inhibitors (reversible) and triazole benzodiazepines (alprazolam) are most often used. Anxiolytic drugs provide some short-term relief of symptoms, but should not be given for more than a few weeks at a time. If anxiolytic treatment is required for more than one to two months, small doses of tricyclic antidepressants or small antipsychotics sometimes help. The main link in the treatment regimen for OCD, overlapping with negative symptoms or ritualized obsessions, are atypical antipsychotics - risperidone, olanzapine, quetiapine, in combination with either SSRI antidepressants or other antidepressants - moclobemide, tianeptine, or with high-potency benzodiazepine derivatives ( alprazolam, clonazepam, bromazepam).
Any comorbid depressive disorder is treated with antidepressants at an adequate dose. There is evidence that one of the tricyclic antidepressants, clomipramine, has a specific effect on obsessive symptoms, but the results of a controlled clinical trial showed that the effect of this drug is insignificant and occurs only in patients with distinct depressive symptoms.
In cases where obsessive-phobic symptoms are observed within the framework of schizophrenia, intensive psychopharmacotherapy with proportional use of high doses of serotonergic antidepressants (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram) has the greatest effect. In some cases, it is advisable to connect traditional antipsychotics (small doses of haloperidol, trifluoperazine, fluanxol) and parenteral administration of benzodiazepine derivatives.
Psychotherapy
Behavioral psychotherapy
One of the main tasks of the specialist in the treatment of OCD is to establish fruitful cooperation with the patient.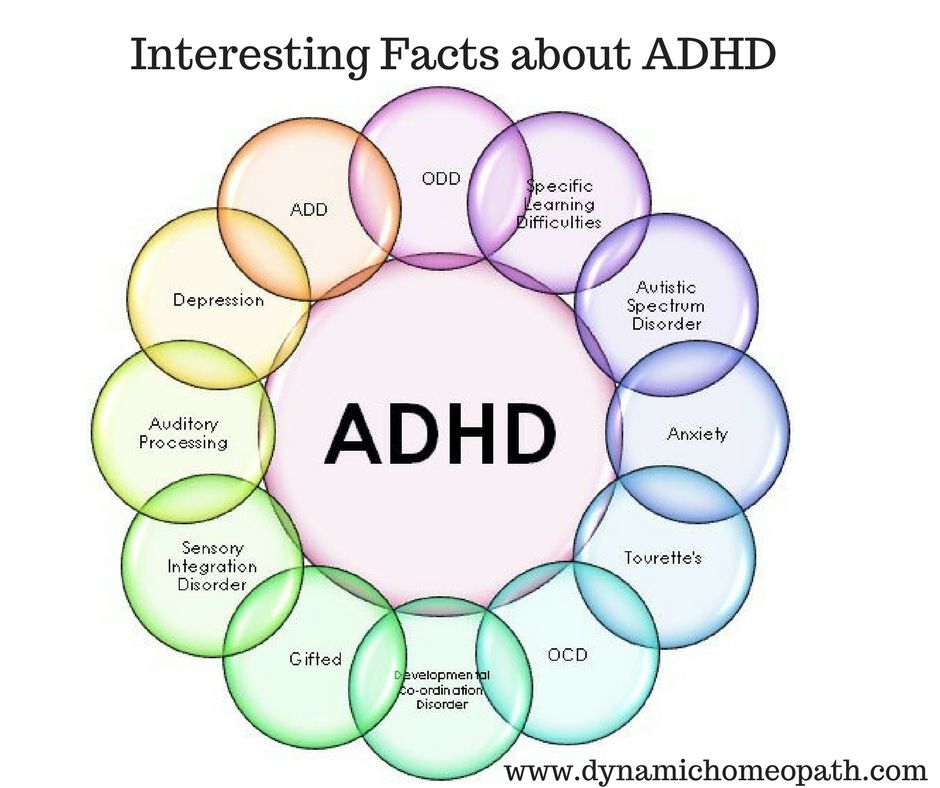 It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.
It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.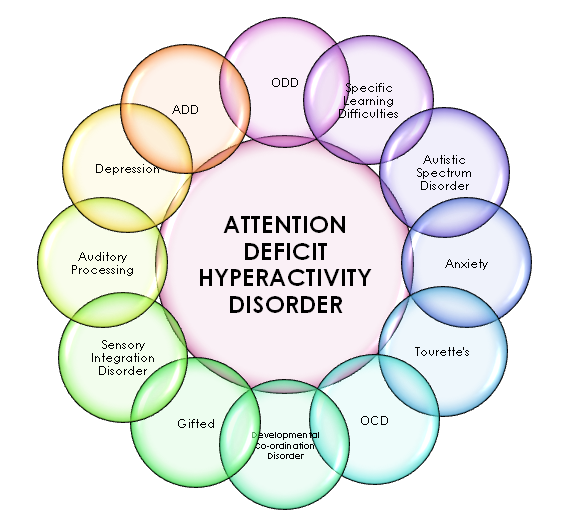 In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
Social rehabilitation
We have already noted that obsessive-compulsive disorder has a fluctuating (fluctuating) course and over time the patient's condition may improve regardless of which particular methods of treatment were used. Until recovery, patients can benefit from supportive conversations that provide continued hope for recovery. Psychotherapy in the complex of treatment and rehabilitation measures for patients with OCD is aimed at both correcting avoidant behavior and reducing sensitivity to phobic situations (behavioral therapy), as well as family psychotherapy to correct behavioral disorders and improve family relationships. If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.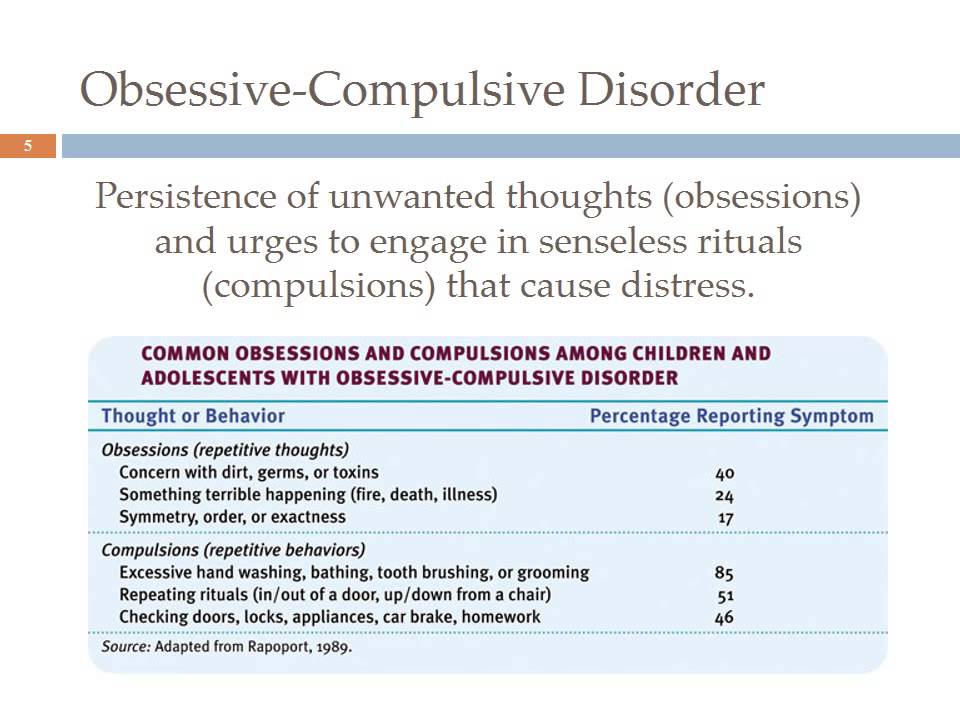
All of these methods, when used judiciously, can increase the effectiveness of drug therapy, but are not capable of completely replacing drugs. It should be noted that explanatory psychotherapy does not always help, and some patients with OCD even worsen because such procedures encourage them to think painfully and unproductively about the subjects discussed in the course of treatment. Unfortunately, science still does not know how to cure mental illness once and for all. OCD often has a tendency to recur, which requires long-term prophylactic medication.
Treatment of obsessive-compulsive disorder OCD - KGBUZ City hospital No. 12, Barnaul: Articles
Country obsessive disorder, in other words, "obsessive-compulsive disorder" is a living copy of borderline mental disorders and is a very common mental illness. The approved medical name for this disease includes two etymologies and obsessions in Latin, obsession and obsession.
Osnovtia means "obsession" in Latin, and in the aspect of this disease means "obsession with thoughts and ideas.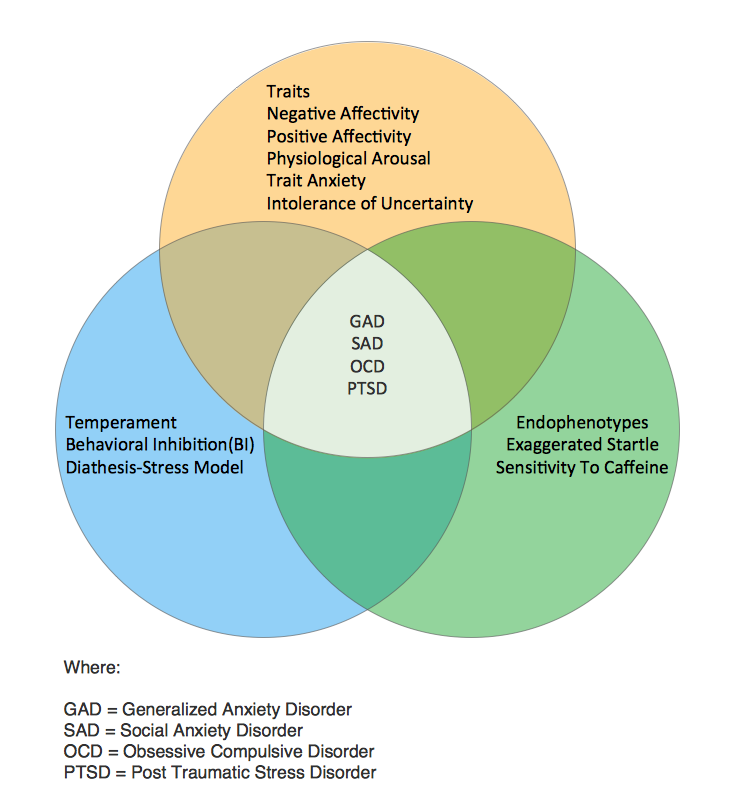 " Occupational obsession with pain in OCD often contains terribly unhealthy and unpleasant thoughts in its content, and sometimes aggressive.
" Occupational obsession with pain in OCD often contains terribly unhealthy and unpleasant thoughts in its content, and sometimes aggressive.
Nullable is interpreted as a "compulsive action", and as a symptom always confirms everything, such as whether the door is closed, the power of electrical appliances is turned off, and the hands are sufficiently washed. This is true.
Simply put, obsessive-compulsive disorder means an obsession with all pathology that literally interferes with human life. Pathological thinking leads to the need to repeat the same action for the patient forever, and the condition worsens it rationally. So, for example, a patient who is afraid of infectious diseases may "wash their hands" until they shave. He relentlessly returns home, checks home appliances, reads the same pages of a book one million times, and tries to figure out the time. Naturally, such a curing method is a stressful situation and neurosis, because it lowers, dies out and torments the quality of a person's life.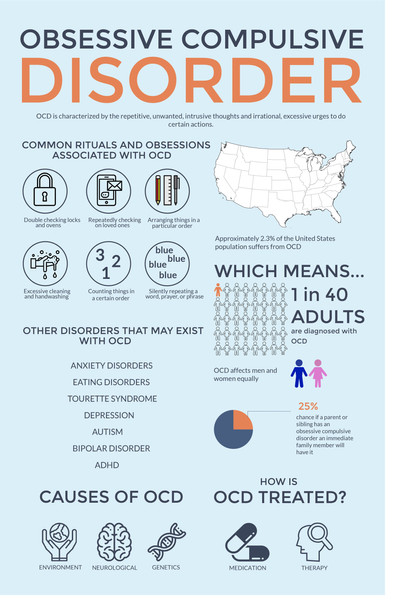
I will see how to associate and which method of self-planting is in the second half of this article. Among them, we pay attention to the cause of the formation of this disease. Catalyst for the development of an obsessive syndrome.
- Experience 11 years or more
- Principal Investigator
Causes of OCD
There are basically three factors at the root of failure.
- Biological factors include neurotransmitter function, brain cell metabolism, vegetable nerve activity, traumatic and hereditary, and the second is not a fundamental cause.
- Social things are associated with strict structures and rules defined by families and other systems where children live and socialize during childhood.
- Psychological things emphasize personality (a highly exposed feature that influences action) and a state of mental trauma.
From the point of view of Gestalt psychology, the formation of disability is perfectly shown in the famous film "Pharmacist" and it is highly recommended to see patients with this syndrome. In the case of the protagonist, there were two types of biological factors (genetic background inherited from the mother), and social factors were involved (unhealthy behavior patterns given by the mother). Every time she washed her baby, she blamed everyone like the mantra was the infection that everyone died. In this way, she changed her child's anxiety and hyperlopec. In other words, from a social point of view, the boy grew up in an artificial environment, in any stressful situation that emphasized and began to increase the symptoms.
In the case of the protagonist, there were two types of biological factors (genetic background inherited from the mother), and social factors were involved (unhealthy behavior patterns given by the mother). Every time she washed her baby, she blamed everyone like the mantra was the infection that everyone died. In this way, she changed her child's anxiety and hyperlopec. In other words, from a social point of view, the boy grew up in an artificial environment, in any stressful situation that emphasized and began to increase the symptoms.
How OCD is formed
Some of us are located in an instinctive urge called the "unconscious" and the "apex of the self" called the "super ego". This creates a contradiction. Primitive animal instinct, censorship and society concept. “Want”, “must”, “can” and “cannot” enter the fight. Then, if the conflict of motivation under the influence of the above is not controlled, the level of anxiety of a person increases and begins to form a neurosis.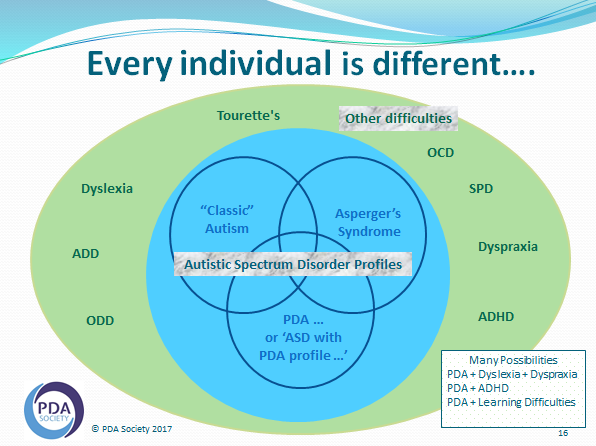 From a psychological point of view, an increase in anxiety leads to obsessive-compulsive disorders. What is worry?
From a psychological point of view, an increase in anxiety leads to obsessive-compulsive disorders. What is worry?
According to this condition, it is the fear of unknown things, and in the case of this illness, the feelings of childhood emotions and feelings are connected. But the brain's job is to protect your body from things you can't handle. Therefore, in the context of anxiety, the compensation mechanism works, and eventually the patient realizes that he is afraid and is aware of his fear. For example, those who are afraid of bacteria go to wash their hands, and as a result they calm down, but obsessive e-compulsive disorder is a kind of addiction, that is, every time they need to wash their hands more thoroughly. It. is.
Why is this happening? For self-esteem, the spirit will intentionally take people outside and will not give them the opportunity to look deeply inside. In the process of disposal, the precautions of the patient are not immersed in the problems or sadness of life inside, but are directed towards the external ritual process.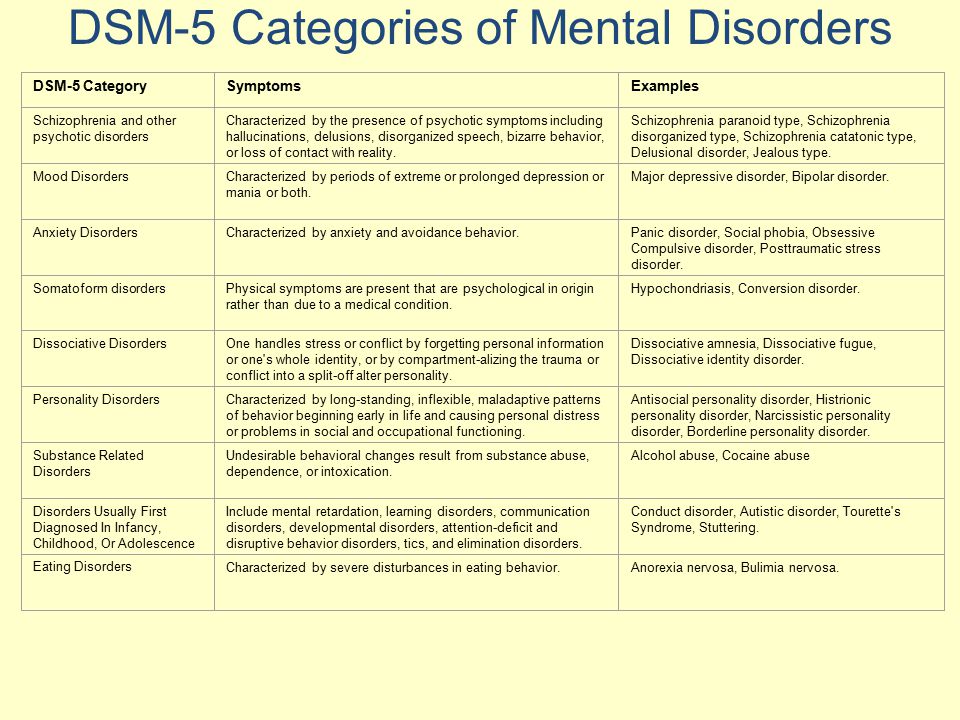 It is impossible for patients with this syndrome to dive into the pain of their spirit translating outside.
It is impossible for patients with this syndrome to dive into the pain of their spirit translating outside.
How OCD manifests itself
As mentioned earlier, the main symptoms are strange and repetitive ideas and ideas that a series of irrational behavior causes. It should be noted that “ridiculous” isolated thinking generally enters a person’s head without a reason. However, the problem is that it says "it's not moving" and stay there without going anywhere.
Sometimes you think you can harm others. Hit someone under a car on the street, hit or cut him with a knife. In addition, there is a tendency to always confirm whether they were at the scene of the incident. This is because people may not remember the details or order of their actions. This is due to one of the symptoms of obsessive-compulsive syndrome, for example, a person in "deep sleep". Depressed emotions and feelings are immersed in a comfortable and safe interior space for patients. In other words, people are walking down the road, taking a vehicle or an elevator, but don't remember what they were doing at the time. Now that the level of consciousness in “Here is almost zero, there is an obsession with all consideration.
Now that the level of consciousness in “Here is almost zero, there is an obsession with all consideration.
Symptoms of OCD
Patient behavior pattern according to the form of neurosis.
Adult symptoms of disease are essentially divided into clinical images of fear and obsession as follows.
- Opposing obligation. A very vivid picture with a terrible heart that "leaves" the patient. These obsessions may include sexual interest, killing someone, violence against those who have done nothing wrong with the patient, and a god-brown color. The patient himself is aware of the horror and absurdity of his thoughts, but cannot be controlled, controlled and eliminates the fear of reincarnation.
- Fear for infection and disease. For patients, dirt and pathogens often form everywhere. Theoretically admits that he does not die, but for him that he will get dirty. This fear is always washing your hands, rubbing it with soap and alcohol, and producing countless obsessions.
 The fear of square phobia and crowds is also assigned to this category. In the case of patients who are afraid of infectious diseases, the crowd will increase their anxiety many times over, so they try to avoid them.
The fear of square phobia and crowds is also assigned to this category. In the case of patients who are afraid of infectious diseases, the crowd will increase their anxiety many times over, so they try to avoid them. - "Resurrection" belongs to the category of obsession and contains such a series of actions that are always repeated. After visiting many times, you will have to check many times, for example, if the power of the appliances has not been turned off, the door has been closed or changed.
- Desire for symmetry. People can use books alphabetically or delete every 30 minutes per hour on the table. All these actions are similar to a kind of ritual to eliminate obsession. However, if the desire of the patient wants to break everything around him symmetrically and rationalize, sure that the help of experts.
In addition to the above symptoms, the following group symptoms may be combined with conditions.
- Physical symptoms of Providence, sleep disorders, headaches.
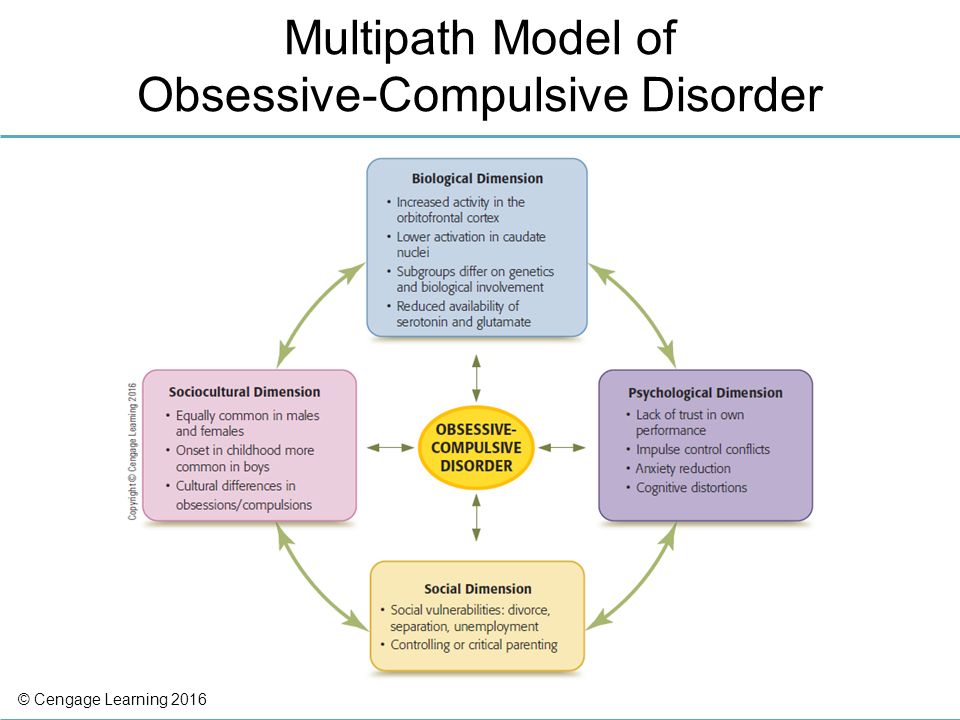
- Emotional things-loads, depression, depression, phobia.
- Cognitive impairment amnesia and training issues.
- Act e-aggressive or rebellious behavior, obsessive-compulsive behavior.
- Acquisition of e-exaggerated mania and anomaly mania.
Stages of OCD
Unlike many other mental illnesses and neurosis, the stage of obsessive-compulsive disorder has more to do with the patient's perceptions than worsening symptoms. Thus, most people suffer from OCD, which goes through three conditional stages.
- There is a misunderstanding. In general, it's misunderstood what's going on. One person suddenly has a strange idea, and sometimes the characteristic behavior appears voluntarily. Of course, this is very scary, especially people who do not know anything about this disease and do not have the possibility of onset, so they feel the highest level of anxiety.
- Understand without consciousness. OCD is an independent single diagnosis and is communicated to the patient.
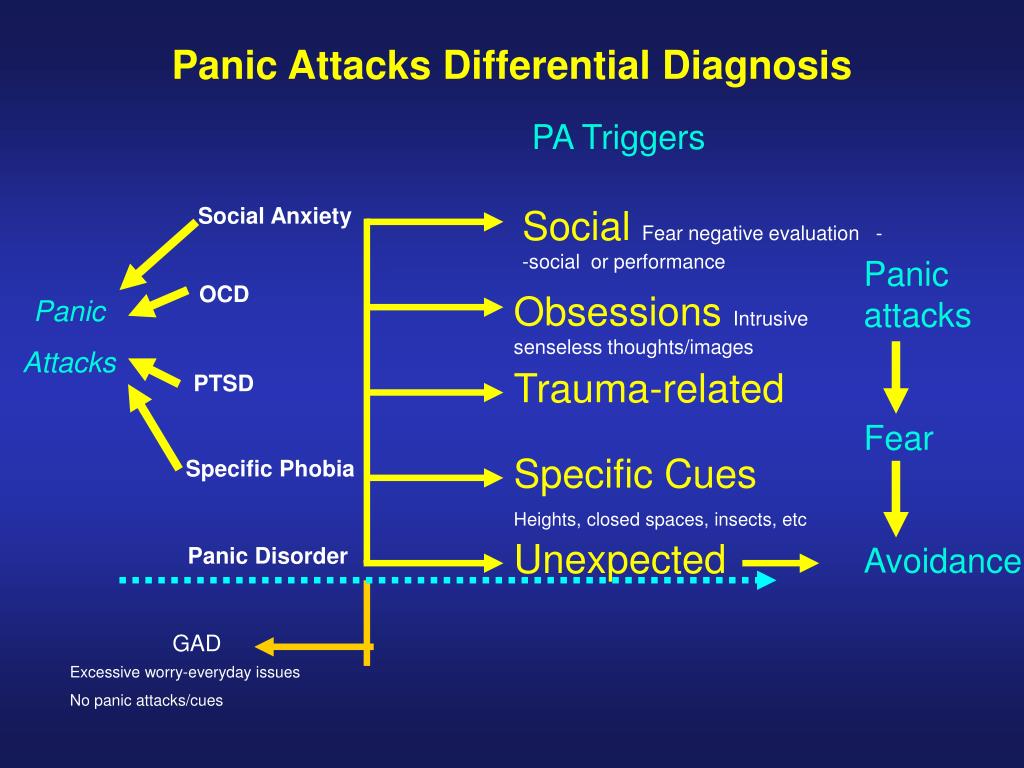 Thus, people, of course, know that they have developed such a neurosis, but they do not try to believe it, they believe that everything passes, and the work of the compensation mechanism is revealed. Be. In addition, men often come into the fight with his obsession in order to win, which is very difficult at this stage, which is self-confidence and does not include her to help.
Thus, people, of course, know that they have developed such a neurosis, but they do not try to believe it, they believe that everything passes, and the work of the compensation mechanism is revealed. Be. In addition, men often come into the fight with his obsession in order to win, which is very difficult at this stage, which is self-confidence and does not include her to help. - In addition. This is an important time to understand that possession is a symptom and due to brain dysfunction, and recognize the existence of an abnormality that should be treated with deeper perception and research.
The important thing in the treatment of obsessive-compulsive disorder is that he has information about the cause of this type of neurosis, the cause and the mechanism. If you have this obstacle, the ability and ability to use the self-equipment method will play an important role in giving people the opportunity to see the essence of fear, that is, you will be able to control your own condition.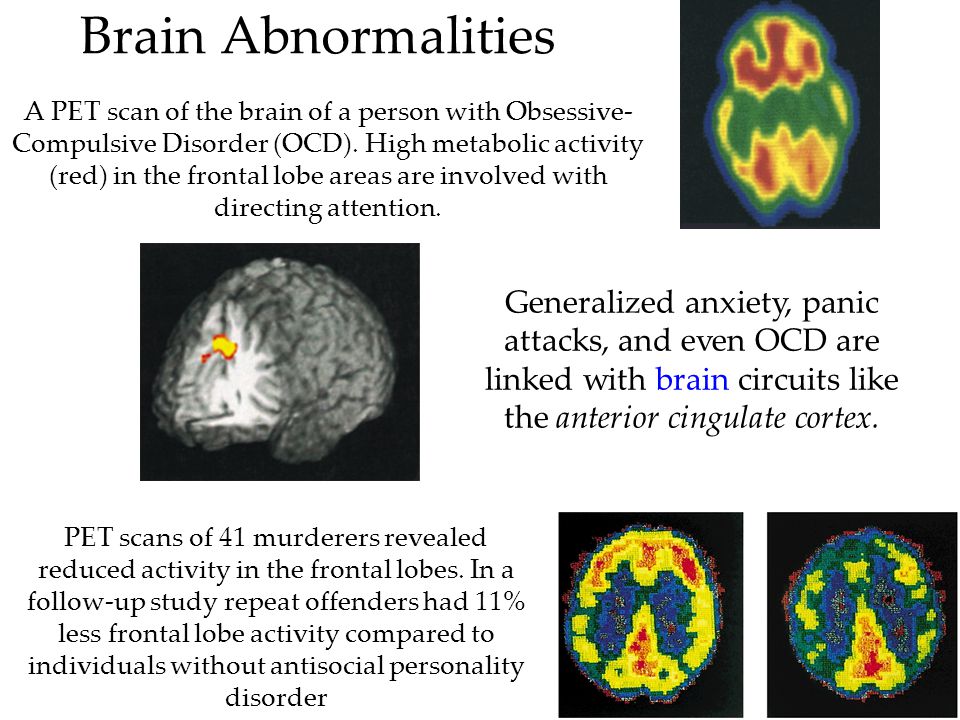 This is true.
This is true.
Self-help methods
In the previous paragraph, the form of disability was classified into categories, taking into account the behavior patterns of patients with obsessive-compulsive disorder. Based on the properties and background symptoms of compulsive x-subsessions and compulsive activity, the following practice is recommended in the world of psychotherapy.
First of all, there is a very common method of inner self-awareness and awareness of denial (attachment). The patient can say to himself. “Yes, this is my sick thinking that happened for various reasons and needs to be neutralized.” How to neutralize obligations. The I-Reconstruction Consciousness Society is followed by an approach from the hit "Kusabi" when it is suggested to translate the image and the image in order to reinforce the situation that causes fear. If you're afraid of dirt, you have to imagine that dirt is literally anywhere and terrible. It is necessary to overcome this state as long as possible and increase anxiety. It is used to treat obsessions associated with fear of infectious diseases.
It is used to treat obsessions associated with fear of infectious diseases.
Psychotherapy provides a complete set of existence when confronted with obsessions and obsessions. I imagine what happens with bad results and give advice to take it. For example, if you iron, the apartment will eventually burn down. In other words, any situation and results must be accepted from the end.
You can do anything without thinking or thinking. The point is to decide.
By the way, this approach is also effective in all other cases, such as healthy people, sick people, people who deal with neurosis and anxiety, or those who feel very comfortable. Acceptance of an existing issue, which today may be the last day, will bring greater awareness and approach to it in any situation.
In addition, keeping a diary of feelings and introspection is a great way to meet yourself. This is based on the fact that people write down everything they happen. Who said you said you felt what kind of dream you had. Details can be prescribed or drawn by more comfortable people. As a result, problems arise in the field of conscious perception and in the field of independent control.
Details can be prescribed or drawn by more comfortable people. As a result, problems arise in the field of conscious perception and in the field of independent control.
Treatment of OCD
As with other neurological diseases, high profile cases should attract experts (psychotherapists, neurologists and psychiatrists) who can take a number of measures, including pharmacotherapy.
The stress of imageophobia destroys nerve cells, the function of the functional center of the brain deteriorates. It is impossible to normalize and accelerate this process without the use of drugs, so the patient is prescribed sedatives and antidepressants. When brain activity is restored to some extent, the application of psychotherapeutic approaches that play an important role in the treatment of the disorder becomes more effective.
methods of psychotherapy
The essence of psychotherapy is to recognize and accept your repressed emotions and feelings. It is important to remember that psychotherapy is very multifaceted and includes many different techniques. For example, cognitive behavioral therapy helps patients recognize the irrationality of their behavior and beliefs. This involves gradually increasing the hypersensitive stimulus and immersing the patient in a stressful situation until the level of reaction decreases. This method, already mentioned in the "Methods of Self-Development", is called the "method of influence" and has proven itself very well. The task of behavioral intervention may have different mechanisms depending on the symptoms. Treatment for obsessions involves the deliberate, sometimes repeated, thought. If you get stuck 5 times, deliberately repeat 10 times and write something even better. It's kind of like a ritual. By increasing the irritant or fear factor and consciously immersing yourself in it, the patient's symptoms disappear, but, unfortunately, the problem itself does not disappear. So at some stage of cognitive behavioral therapy, gestalt and psychoanalytic techniques are linked.
For example, cognitive behavioral therapy helps patients recognize the irrationality of their behavior and beliefs. This involves gradually increasing the hypersensitive stimulus and immersing the patient in a stressful situation until the level of reaction decreases. This method, already mentioned in the "Methods of Self-Development", is called the "method of influence" and has proven itself very well. The task of behavioral intervention may have different mechanisms depending on the symptoms. Treatment for obsessions involves the deliberate, sometimes repeated, thought. If you get stuck 5 times, deliberately repeat 10 times and write something even better. It's kind of like a ritual. By increasing the irritant or fear factor and consciously immersing yourself in it, the patient's symptoms disappear, but, unfortunately, the problem itself does not disappear. So at some stage of cognitive behavioral therapy, gestalt and psychoanalytic techniques are linked.
gestalt therapy
It consists of a dialogue between personality and subpersonality and encourages inner deviation.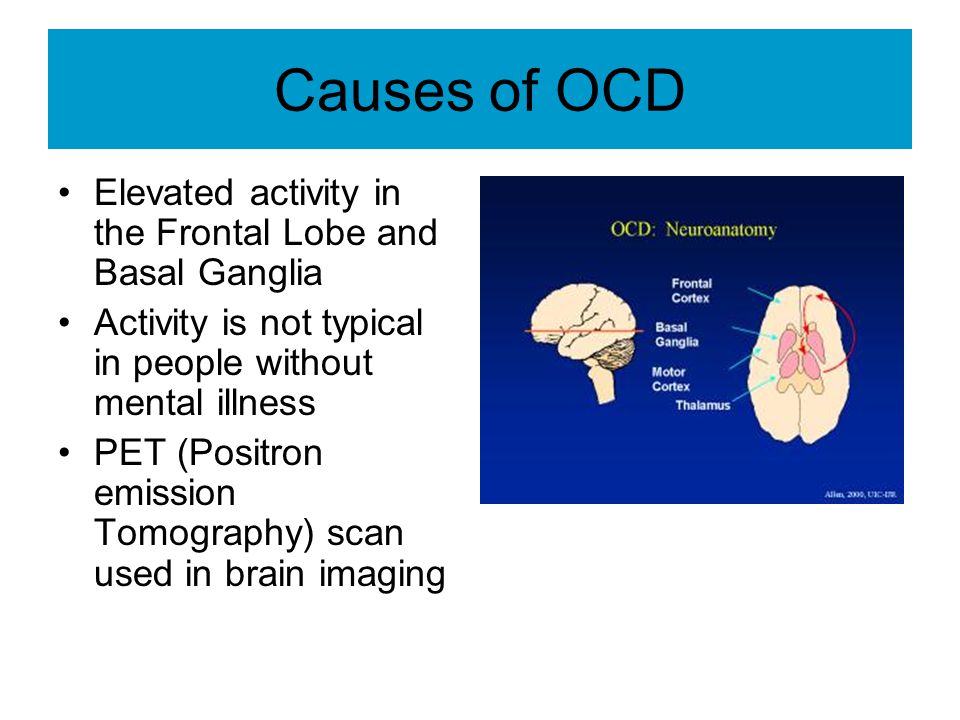 A conversation with a subpersonality is a kind of acquaintance that can provide answers to many internal questions and gradually reveal unresolved grievances and repressed emotions that torment the patient. In this method, superficial personal conflicts are very simple, but there are deeper layers.
A conversation with a subpersonality is a kind of acquaintance that can provide answers to many internal questions and gradually reveal unresolved grievances and repressed emotions that torment the patient. In this method, superficial personal conflicts are very simple, but there are deeper layers.
psychoanalysis or deep psychotherapy
Find the source of anxiety and deal with it. In many cases, the root cause is associated with intimate relationships that suppress the emotional sphere of the patient. For example, in childhood they were forbidden to express their feelings, denied attachment and empathy, which led to anxiety, obsessions and their symptoms.
internal dialogue
This is another method of treatment and necessity. For through this the sick person can distinguish between sick and healthy thoughts in his mind and begins to influence the sick with his healthy parts. Fear is a manifestation of the inner child that the adult part can cooperate with.
In general, any psychotherapeutic technique is aimed at understanding the problem and identifying internal obsessions. When the unconscious comes to the level of consciousness, it comes under our control, and we can control it.
Doctors call obsessive personality disorders a mental illness that characterizes the strength of the patient's anxiety. The obsession (obsession) is always repeated, causing disturbing emotions (disgust and anxiety) and people cannot control it. Many people with obsessive-compulsive disorder know that their images and thoughts are products of their hearts, they are out of place, and they are exaggerated. However, obsessions are not resolved in theory or logical thinking.
Yusupov Hospital provides a comfortable treatment environment for patients suffering from obsessive-compulsive disorders.
Causes
To date, scientists have not identified the exact cause of OCD. As shown in many research findings, obsessive-compulsive disorder is the result of a disruption in the connection between the frontal lobe and the deep structure of the brain (the bottle and the basal nucleus).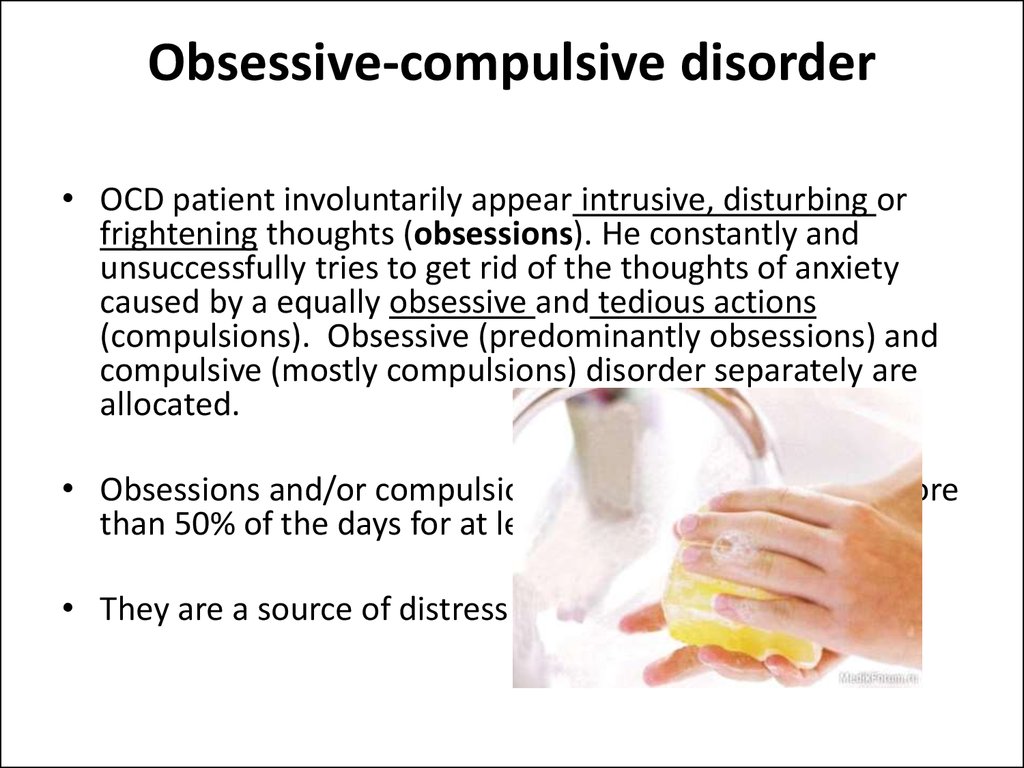
They use serotonin, a neurotransmitter (hormone), to transmit impulse. This disease occurs in many families, suggesting that the gene is involved in causing the disease. The exact fact that it stimulates onset has not been identified by researchers.
Scientists have developed two theories, the information integration theory and the neurotomy hypothesis, for the onset of obsessive-compulsive disorder. It is not appropriate to focus on one model because they are not supported by applied research results. Psychotherapy at the Yusupov Hospital has been focused on removing the signs of diseases that degrade the quality of patients, since the treatment of unknown diseases is inappropriate and ineffective.
Symptoms
The symptoms of obsessive-compulsive disorder are almost the same for both children and adults. Patients may have an obsession.
- Body fluid
- Microorganisms, infectious diseases (herpes, HIV guide) pathogens.
- Environmental object (radiation, asbestos).
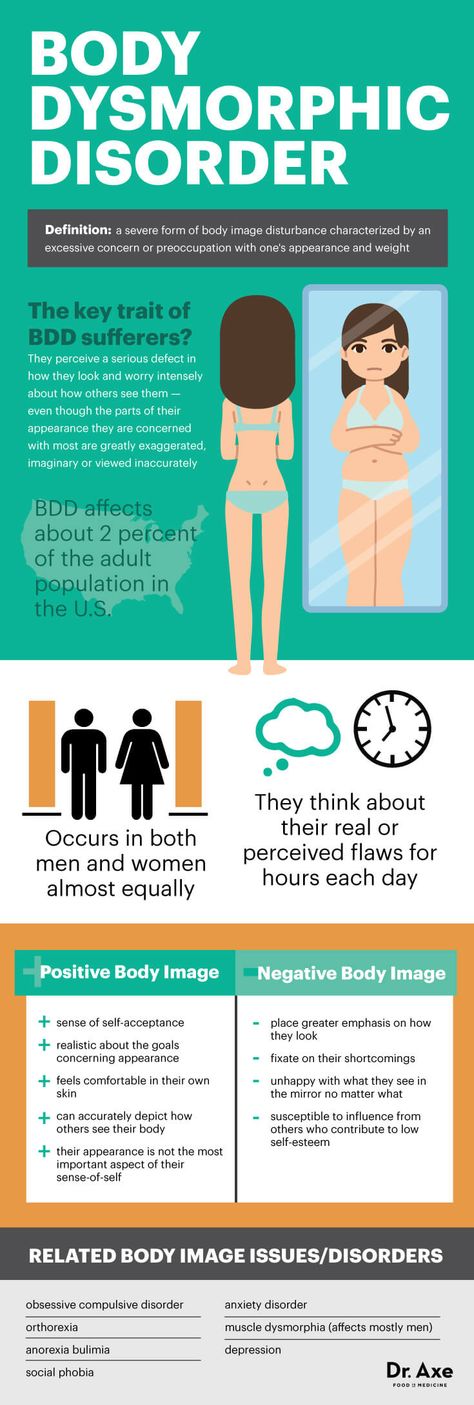
- Household chemical (cleaner, solvent).
2. It becomes impossible to control.
- Fear acts impulsively so as not to hurt yourself or others.
- Fear that terrible images and violent images come to mind
- I'm afraid to say insults and obscene things.
- Fear of stealing things.
- Fear of being involved in something terrible (robbery, fire).
- Fear of harm to others and negligence (rejects anything that could harm others to the ground).
4. Outstanding excellence associated with perfectionism.
- Excessive adherence to precision and regularity.
- Anxiety that you have to remember or know something.
- When you throw something away, you may be afraid of forgetting or losing important information.
- Fear of losing things.
- I can't decide whether to keep it or throw it away.
Patients may experience arousal or forbidden sexual images, thoughts, impulses, and obsessions associated with homosexuality and incest, and involve children in sexual intercourse.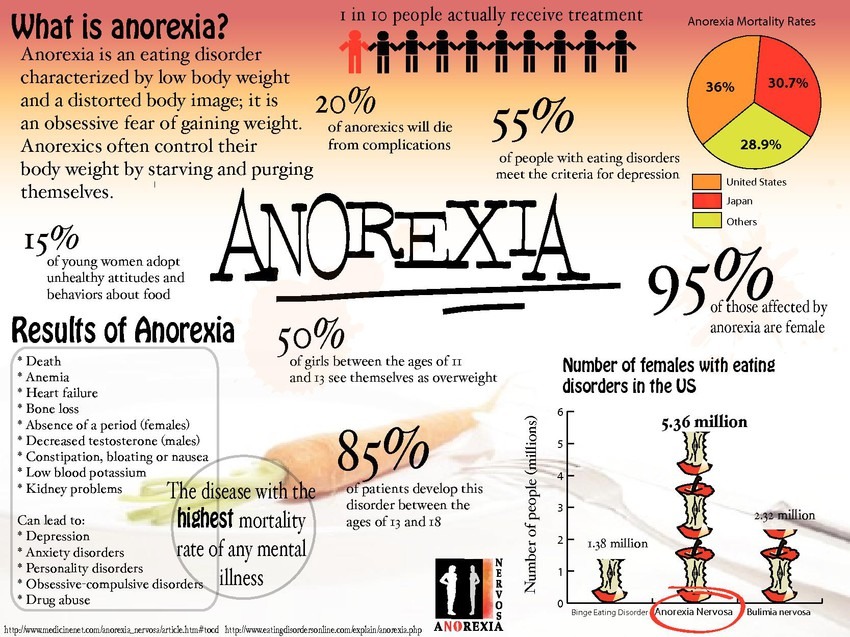 Patients with obsessive-compulsive disorder may be obsessed with aggressive sexual activity against others. You are consumed by religious obsession, i.e. blasphemy or offensive to God, or excessive adherence to morality, right and wrong behavior. In addition, there is an obsession with superstition, such as ominous numbers, lucky numbers, colors, and fears of physical harm.
Patients with obsessive-compulsive disorder may be obsessed with aggressive sexual activity against others. You are consumed by religious obsession, i.e. blasphemy or offensive to God, or excessive adherence to morality, right and wrong behavior. In addition, there is an obsession with superstition, such as ominous numbers, lucky numbers, colors, and fears of physical harm.
Retention is the movement and behavior of the heart that occurs in response to some kind of stimulus. Forced, there are some hidden mental actions that can be observed for others, such as confirming that the gas stove will be turned off and repeating specific phrases in the mind. It is more difficult for patients to control and control covert possession than visible possession. In case of severe illnesses, rituals are repeated continuously throughout the day, which hinders daily work. Forced to be alone does not bring joy. This is different from impulsive behavior (such as shopping and gambling) with immediate gratification. "Ritual" is synonymous with forced, but usually refers to behavior that others can see.
"Ritual" is synonymous with forced, but usually refers to behavior that others can see.
The symptom of compulsive disorder in obsessive-compulsive disorder is as follows.
- Cleaning and maintenance
- Wash your hands too often in a certain way.
- Excessive bathing, showering, hygiene procedure, body care, mouse care.
- Always clean household goods
Patients can test whether they are harmful to themselves or others, doing something terrible or doing something wrong. When a body part is in a fixed position. It is characterized by repetitive daily activities, rewriting the same sentence, reading and repeating the same activity over and over again (3 is a "safe" number, so complete the tasks three times).
Mental compulsions are made by thinking of good things so that you don't harm yourself or others, thinking of terrible events and counting "good" numbers while performing tasks. The following are the physical signs of obsessive-compulsive disorder.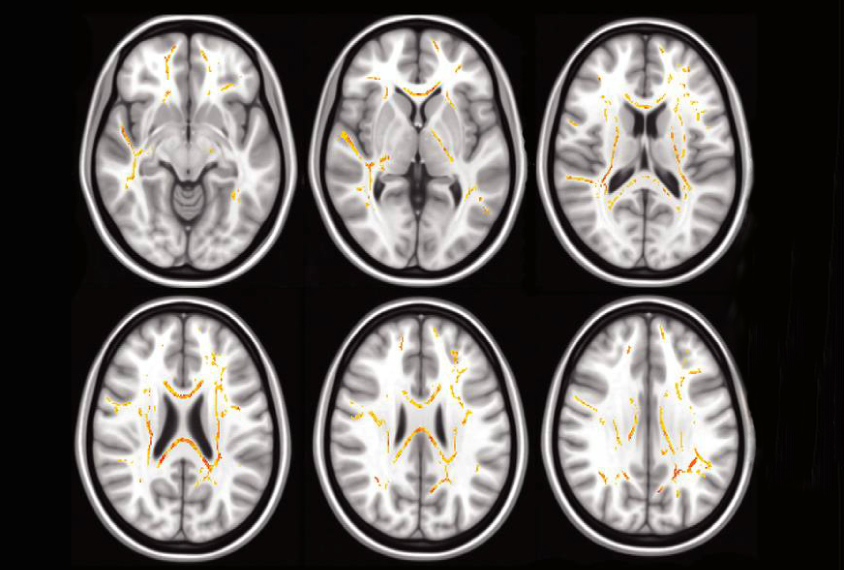
- Feel dizzy.
- Headache
- Epidemiological pain
- Increase heart rate
- Shallow breathing
- Numbness (body sensation).
- People who suffer from obsessive-compulsive disorders have a reduced quality of life. You are suffering from possession, and when this happens, you will have to do several rituals to remove it. The symptoms of obsessive-compulsive disorder interfere with building relationships between patients and others.
Compulsive disorder is one of the mental illnesses. Diagnosis and treatment by a psychiatrist and psychosomatic doctor is required. In this case, you need to consult an expert.
I am unsure of my actions ("transaction" with myself - needing to find symptoms of a non-existent pathology, additional gas stoves, etc.).
- Attention for certain rituals: wash your hands according to the specific algorithm, close doors and windows.
- Inability to do away with fear in anxiety and fall into anxiety.

- The life of people with obsessive compulsive disorder is quite difficult. You are concerned that you need to perform a specific ritual to remove withdrawal anxiety, which is a typical symptom of patients diagnosed with obsessive-compulsive disorder. In psychology, obsessive-compulsive disorder is classified as an anxiety disorder.
Examples
The symptoms of obsessive-compulsive disorder interfere with the person's normal life and relationships with others.
The onset of obsessive-compulsive disorder does not cause much fear. Some obsessions are well known. For example, many people know the need to always wash their hands and check their worksheets. Nassessive e-compulsive disorders can also appear due to pathological accumulation, spiritual and fear of harming others. In many cases, obsessive-compulsive disorder manifests itself in paralysis of fear associated with sexual orientation.
Since OCD is a mental illness, it must be understood that the help of a professional doctor (psychotherapist, psychiatrist) can only be identified.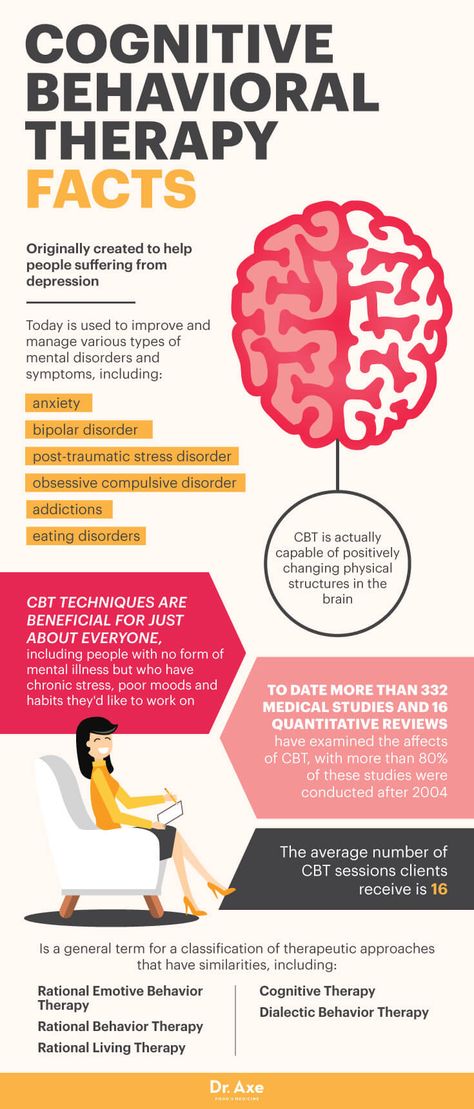 However, according to experts, there are symptoms that may indicate obsessive-compulsive disorder.
However, according to experts, there are symptoms that may indicate obsessive-compulsive disorder.
A “transaction” with oneself is the uncertainty in their actions. The need for additional control over the stove in search of symptoms of diseases that do not exist.
- The feeling of following a certain ritual. How to close the door, wash your hands, etc.
- Being unable to convince unfair fear and continue to be awkward.
- Obviously, understanding the expression of mental illness is typical for most patients.
- There is a certain reason, anxiety, which always interferes with normal functions and is always absorbed.
- There are two approaches to treating an obsession. Firstly, the psychotherapist in the psychiatric clinic at Yusupov's hospital is focused on eliminating the obsessive act. In addition, the measures to save patients are taken from the obsession.
Therapy
The treatment of compulsive compulsive activity is performed using the intervention method.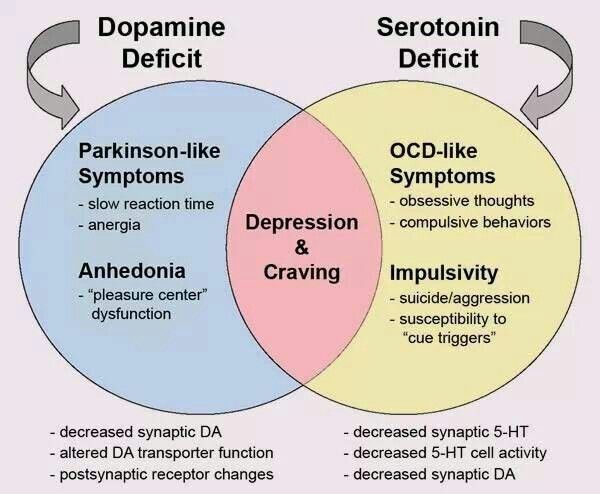 The essence of this method is to consciously reinforce the patient's obsessive reaction and transform it into irrationality. Hence, it causes irrational anxiety and diminishes its power. As a result, therapists can work more effectively on the first components of OCD, the idea and motivation.
The essence of this method is to consciously reinforce the patient's obsessive reaction and transform it into irrationality. Hence, it causes irrational anxiety and diminishes its power. As a result, therapists can work more effectively on the first components of OCD, the idea and motivation.
The application of the method of influence is not justified in all cases, because there is no realistic obsession, and the protagonist is the treatment of patients who belong to the idea of intrusion, image and fear. It's inefficient. In such a case, treatment focuses on how the patient interacts with the connection between emotions and logic and their separation. Treatment of this type of obsessive-compulsive disorder is more of a problem because it is more difficult. In such a case, the therapist's job is to change the relationship between the established concept, the logic of thought, and their emotional content.
In many cases, patients with obsessive-compulsive disorder are highly intelligent and have non-verbal inferences.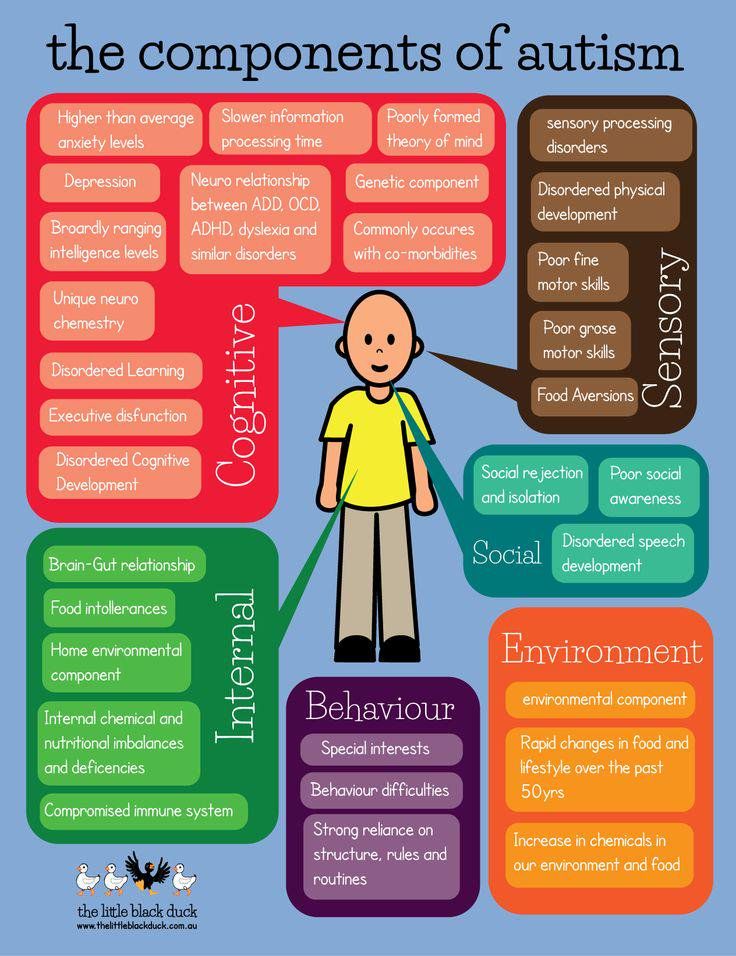 The existence of OKR lies in the fact that the patient works in obvious logic and ignores the emotional elements of the disability. Patients do not understand that they will gradually change the causal relationships formed at the level of emotions and logical connections. Thus, their own questions and fears seem harmless to them, but they lack a comfortable attempt to overcome them.
The existence of OKR lies in the fact that the patient works in obvious logic and ignores the emotional elements of the disability. Patients do not understand that they will gradually change the causal relationships formed at the level of emotions and logical connections. Thus, their own questions and fears seem harmless to them, but they lack a comfortable attempt to overcome them.
Obsessive-compulsive disorder (OCD) is being treated at the Yusupov Hospital Psychiatric Clinic. Medication can help relieve mental symptoms that interfere with cognitive behavioral therapy.
Medication treatment
Stress and depression make it difficult for people with OCD to focus on the emotions and thoughts associated with the disorder. Therefore, patients are prescribed sedatives, antidepressants, and serotonin reuptake inhibitors (enzymes produced in the brain).
Drug therapy is a rather crude tool for the treatment of the mentally ill, but its proper use supports psychotherapy.
Although treatment for OCD has a good prognosis, it is a dangerous disease that dominates throughout life, such as the inability to build friendships and families, be successful at work, and lead a normal life. Obsessions and the anxiety associated with them can lead to poor performance and attention, sleep disturbances, and sexual dysfunction.
The course of obsessive-compulsive disorder is so long that most people seek professional help years after the first attack, which complicates the recovery process. Psychotherapists at the Yusupov Hospital offer proven therapies to help patients return to a fulfilling life faster and free themselves from paralysis caused by obsessive thoughts.
Obsessive Compulsive Disorder, or OCD for short, is an illness with a range of disturbing psychotic symptoms. Obsessions, behaviors and memories are the main symptoms of this disease, and certain rituals must be observed to get rid of them.
Obsessive-compulsive disorder is considered a benign disorder and does not pose a threat to others.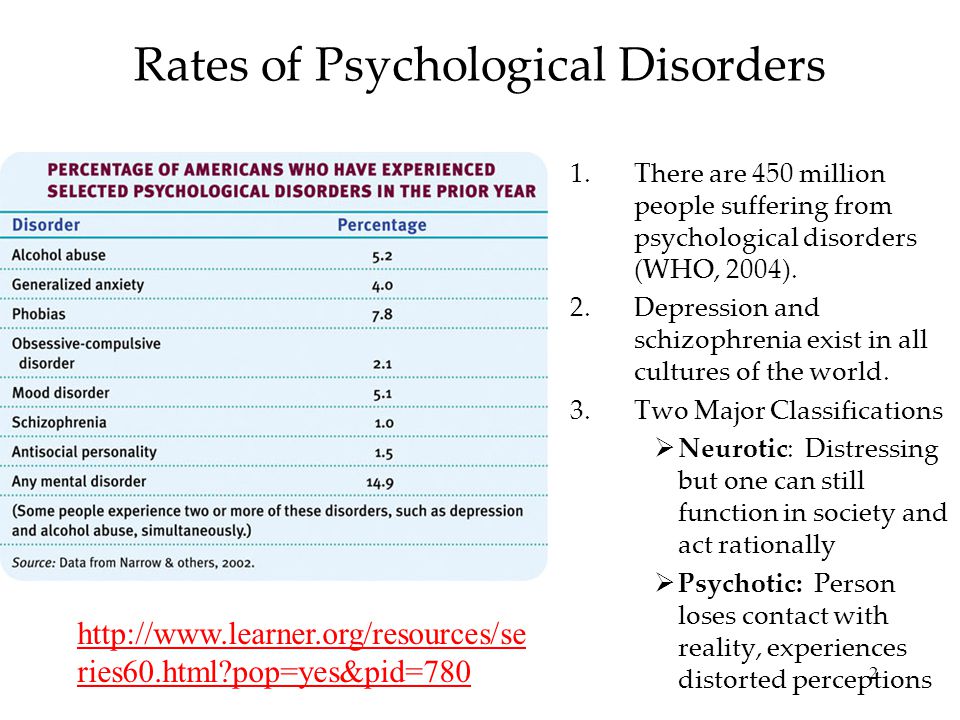 However, this disease is very unpleasant for patients and their loved ones. Modern psychotherapy and drug therapy can completely eliminate the disease or stop all the unpleasant symptoms and restore a normal standard of living. The main thing is to get professional help in a timely manner.
However, this disease is very unpleasant for patients and their loved ones. Modern psychotherapy and drug therapy can completely eliminate the disease or stop all the unpleasant symptoms and restore a normal standard of living. The main thing is to get professional help in a timely manner.
Psychiatric appointment, psychotherapist appointment — 4700
- There are several factors that can trigger the development of this mental illness.
Causes and prerequisites for the development of the disease
There is a genetic predisposition.
- Prolonged exposure to hazardous situations.
- On the genetic side, a predisposition to certain mental disorders can be inherited, and there are certain personality traits that lead to the development of obsessive-compulsive disorder under adverse conditions. Certain patterns of behavior in traumatic situations that developed in childhood can also accelerate the development of the disorder.
- Mental trauma and painful memories of it may prevent patients from causing obsessive-compulsive disorders.
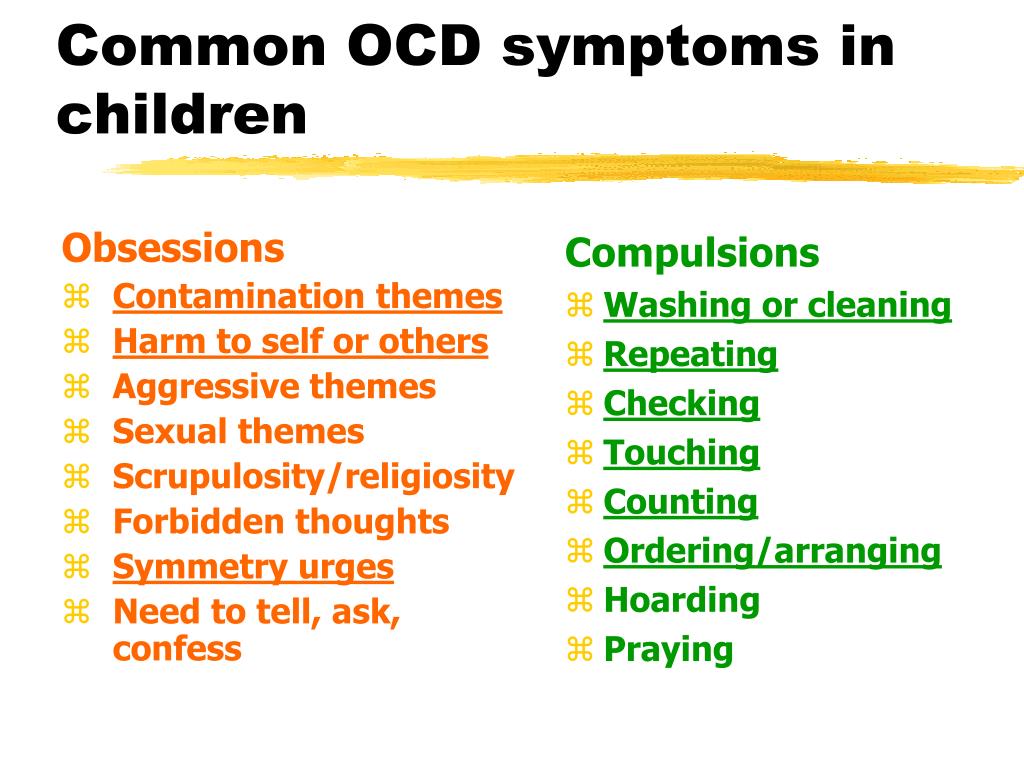 It is also said that mental fatigue and long-term unforgivable conditions also increase the risk of obsessive-compulsive disorder. And, of course, personality characteristics and personal behavior patterns also play an important role.
It is also said that mental fatigue and long-term unforgivable conditions also increase the risk of obsessive-compulsive disorder. And, of course, personality characteristics and personal behavior patterns also play an important role. - Usually, the first signs of this disease appear in adolescents or young adults (sometimes there are individual signs in childhood). And the first obsession and thoughts appear. At the same time, patients also know that their actions and thoughts are irrational and have little to do with reality.
The disability of this country contains two main elements, expenditure thinking and compulsive action. These are aspects of the patient's consciousness.
The purpose of the assessment is the image, thinking, impression, movement and memory, which causes severe pain, which has nothing to do with the will of the patient. Patients try to resist and avoid flashes and blocks, which is very difficult. However, the obsessions reappear and cannot be focused on other things.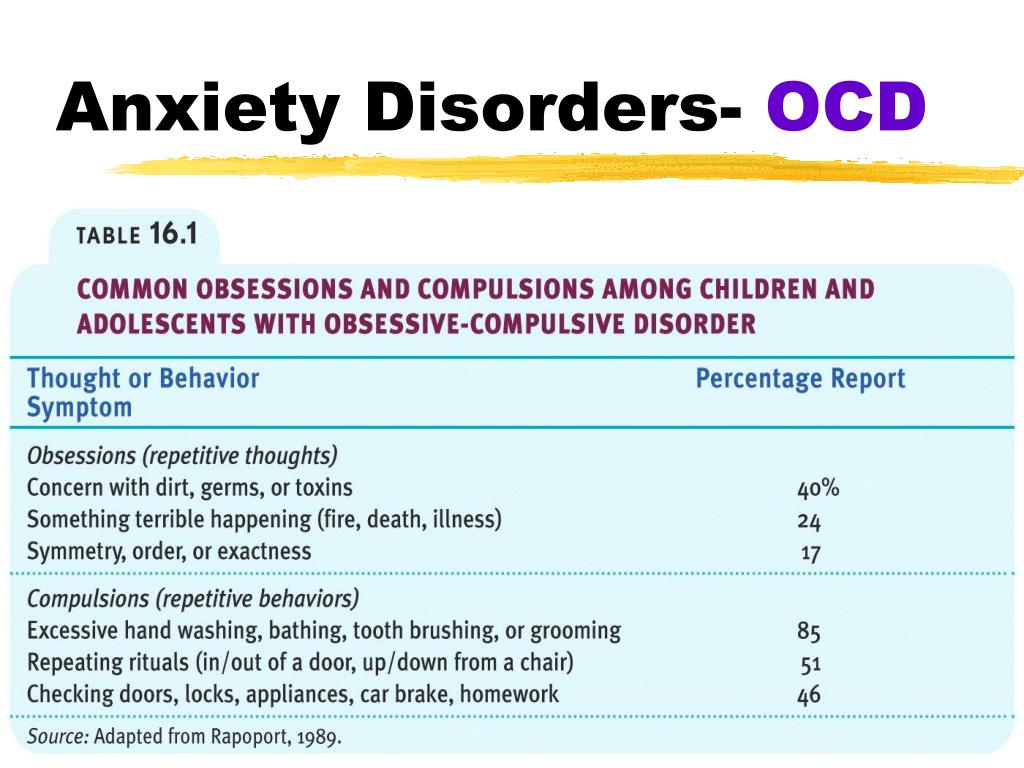 It's really different, just obnoxious, weird or terrible.
It's really different, just obnoxious, weird or terrible.
Symptoms and manifestations
The delay varies from patient to patient. At present, such a classification is accepted as an obsession.
Question?
Considering
Obsessions
Suspicion is characterized by always thinking about committed actions. The patient suspects if the door is closed, the gas is stopped, or the telephone fee has been paid. Such thinking has the property of returning again when you reconsider. Patients may go to already closed doors many times a day without any calculation. Interestingly, normal questions can happen to anyone, and a problem occurs when it gets in the way, unreasonably, or annoying.
- Attaching to the opposite is a nasty idea that looks ugly, unnatural, and blasphemous. The most common image is harm and fear of loved ones. Patients may be afraid to show aggressive thoughts or immoral behavior. Insulting the patient's ideals (his view of the world, religious self-respect) is another category of inconsistent phobia and is the obsession with keeping birds - as a special version of obsession, in principle, people appearing in thinking and ideas that oblige the patient.
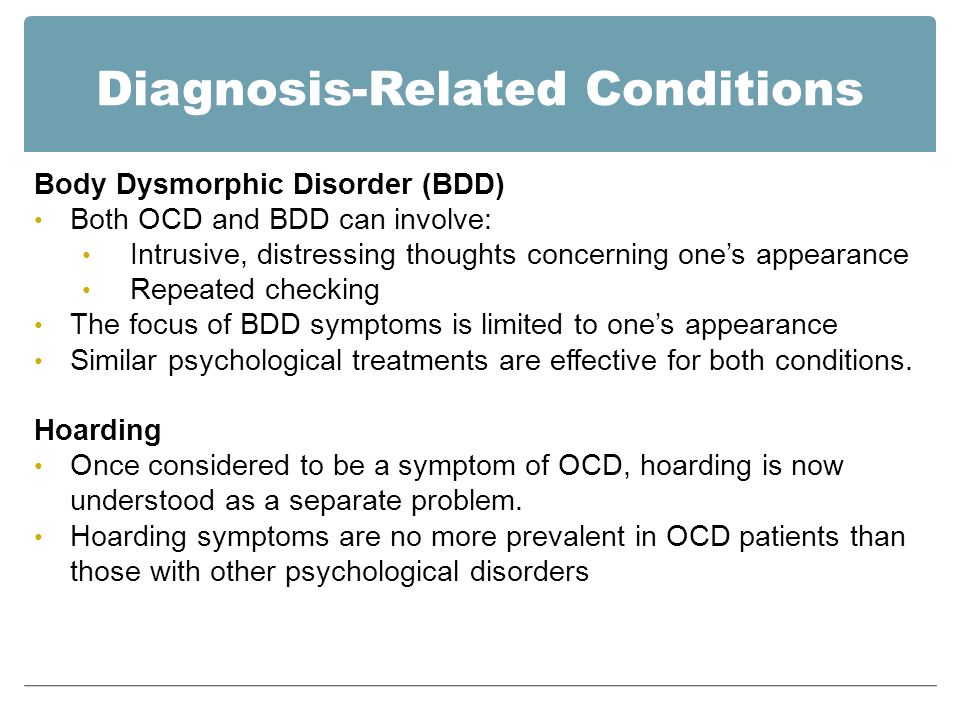 Offensive and obscene in dealings with God, Virgin and Saints (most of the various religions in various religions are the "wrong thoughts" of the instrument performer, and when they send the symptoms of mental illness, to the doctor. In addition, you can judge that you will be blessed for treatment by a psychiatrist ).
Offensive and obscene in dealings with God, Virgin and Saints (most of the various religions in various religions are the "wrong thoughts" of the instrument performer, and when they send the symptoms of mental illness, to the doctor. In addition, you can judge that you will be blessed for treatment by a psychiatrist ). - Another category is the ideological idea of pollution. It is so popular that it has a special name. The public phobia is called my Sofovia. Patients are afraid of pollution and afraid of bacteria. To overcome fear, you can wash your hands every hour and clean your hands many times a day.
- If the thought is difficult, the patient begins to invent actions and rituals to calm down. After such a ceremony, the person himself becomes lighter. In the case of fear of pollution, it is the fear of specific things and places, and the strict order is washed away.
This is a stereotypical repetition, a rational basis. Logically, one cannot explain why patients need obsessive compulsive acts.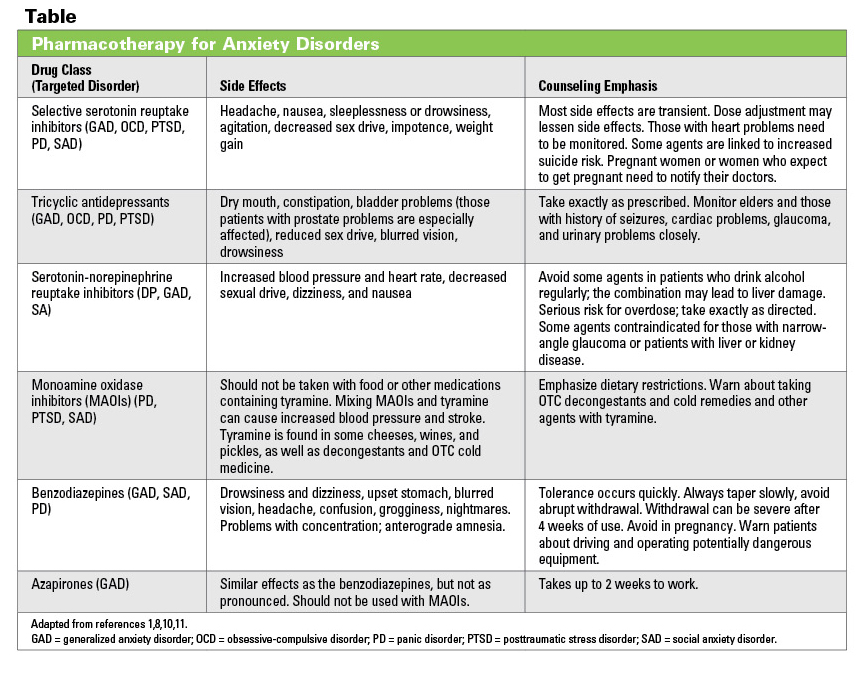 For the patient himself, he has a ritual-like character to protect himself. If you take a certain action, nothing bad will happen.
For the patient himself, he has a ritual-like character to protect himself. If you take a certain action, nothing bad will happen.
Such actions can be really different, such as touching hair and touching pincers. It is noteworthy that this disease becomes dominant in puberty. At first, this is accepted by doctors as a physical dysfunction, but it becomes apparent due to more complex operations.
You cannot stop this, realizing that your actions are meaningless. If the ritual is interrupted, the patient will be attacked with intense discomfort and will immediately resume the ritual if possible.
If you have a bad habit, such as chewing your lips or correcting unevenness, don't diagnose OKR right away. They chase a lot. The difference from a mentally healthy person is that if you have the appropriate self-control, you can deny repeated actions. He often doesn't notice until others are pointed out. OCD patients know exactly what to do and how to capture them in time. Without the help of an expert, you cannot cure this habit.
Without the help of an expert, you cannot cure this habit.
Compulsive acts
It is important to distinguish obsessive-compulsive disorder from other mental illnesses, including the more dangerous and serious schizophrenia. Therefore, it is important to consult a specialist and have a diagnosis when certain symptoms appear.
Treatment for obsessive-compulsive disorder can be adjusted to a course that combines drug therapy and psychotherapy and can restore a normal rhythm of life.
Sweat suppresses is inflammation of the axillae, nipples, perineum, scrotum, large lips, and apocrine sweat glands around the anus. Edema dermatitis on the scalp is extremely rare. The apocrine glands have a special structure in which the upper cells are constantly being destroyed and then mixed together. The secrets of these glands include a lot of cholesterol and fat, an increase in its density and a unique smell. Hydatopathy often develops in the armpit with a large number of sweat glands, and dirt will envelop the sweat glands.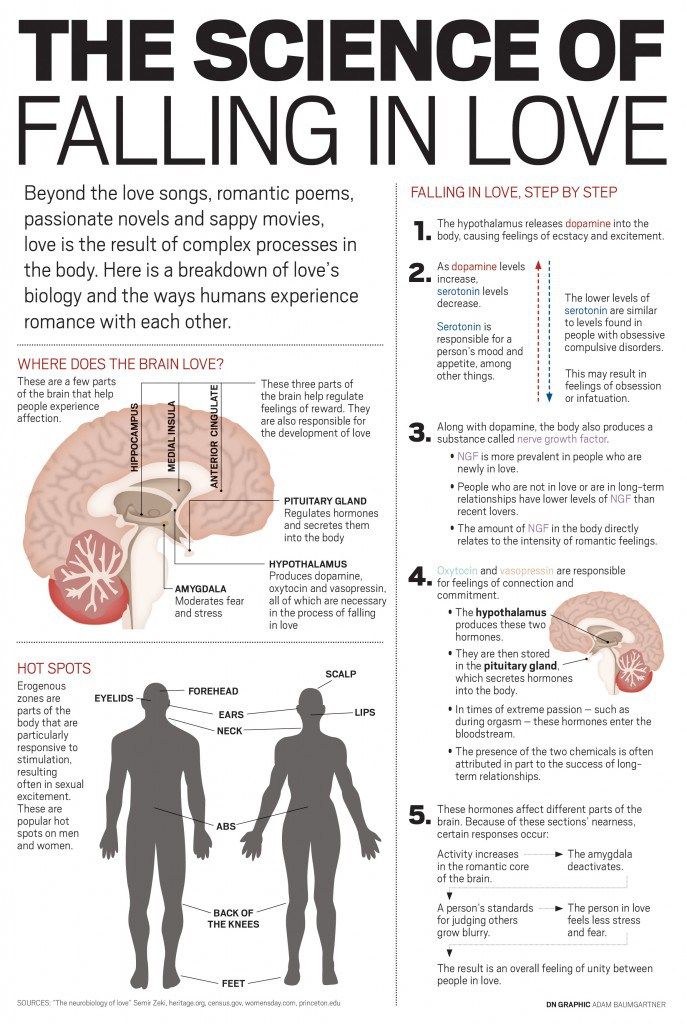 This is a disease that refers to Pederma and skin purulent lesions.
This is a disease that refers to Pederma and skin purulent lesions.
Middle-aged women often develop axillary flooding and scratching during flossing and shaving. In the case of men, the perineum becomes painful. In general, people between the ages of 15 and 55 are said to develop because they develop in the second stage of actively functioning apocrine glands. In many cases, breaking personal hygiene habits makes it more likely to cause inflammation. This disease can repeat the repetition.
Black people are dangerous and dangerous because the breast tubes are wide and small.
The most common bacteria caused by hydrophrite include the most common stripcocci and grape staph, but Escherichia coli and other microorganisms may be present.
The most common cause and induced substance is hydrofol.
Who gets hidradenitis most often?
There is a lot of sweating.
Euresis; Euresis;
Causes of hidradenitis
Skin diseases - rash, eczema.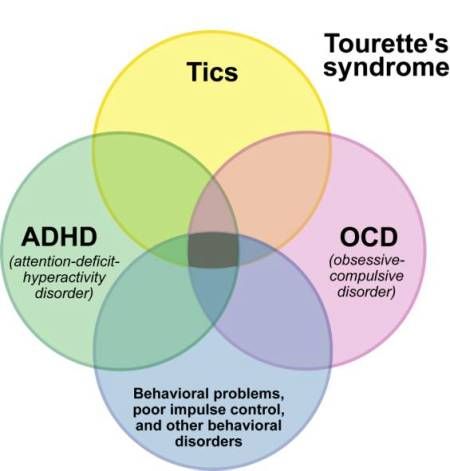
Endocrine diseases (especially diabetes).
- Violation of personal hygiene rules
- Too much use of deodorant
- Harsh working conditions such as dust and harmful exhaust gas.
- Immunity
- Coarse wax, shave scratches, combs.
- Because I wear tight clothes, my skin scratches.
- The presence or absence of a bacterial infection in the body.
- Alert sign-.
- Genetic characteristics of the anatomy of the structure of the apocrine gland.
- The symptoms of Hydronniez are typical and difficult to confuse with other diseases. The initial symptoms are stubborn itching, and small subcutaneous nodules appear, increasing day by day. There is pain, discomfort, and even movement restrictions in the process. The nodules gradually increase and begin to appear on the skin. The surrounding tissue swells and becomes bluish. In addition, many nodules are softened, holes open, pus is secreted, and sometimes blood is mixed.
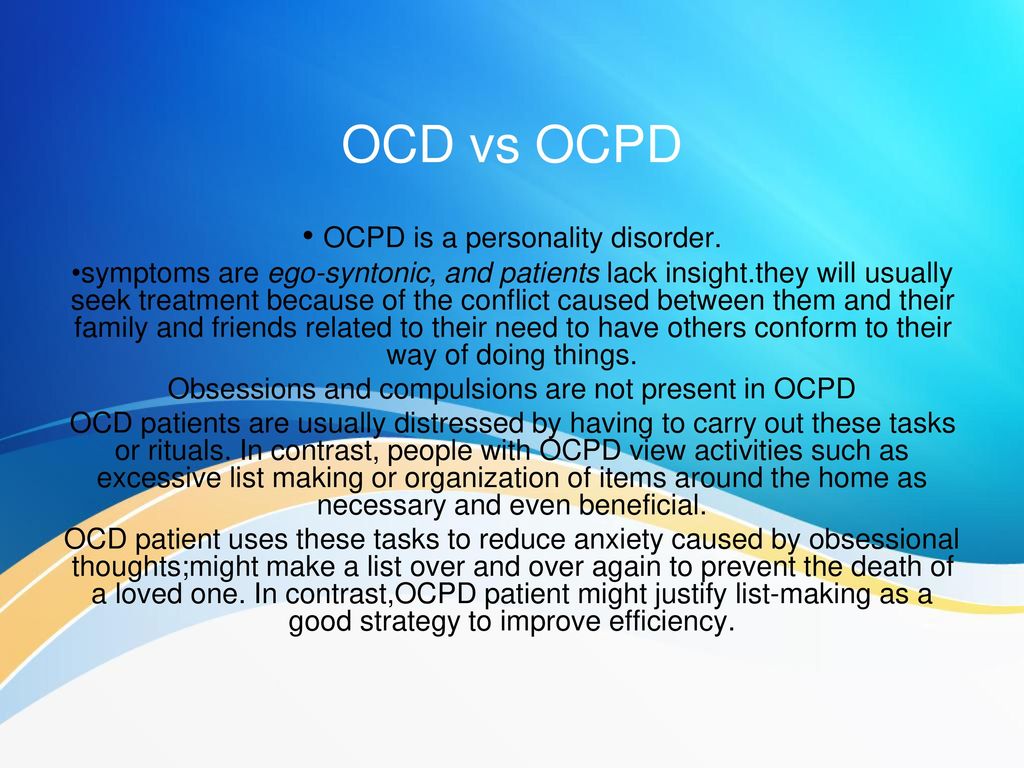
- And because of the characteristic appearance of the affected area with swollen red and white discharge, it was commonly called "bitch's breast".
- The general condition does not bother, usually there is no heat. You may feel discomfort and slight malaise. If the symptoms of general malaise are included, this means an extension of the infection or the occurrence of complications.
- Opening abscess improves whole body condition, pain and increased exercise. Without complications, the abscess will be completely empty, formed and treated with traces. The total cycle of the outbreak and due to timely care is two weeks.
How does hydradenitis manifest itself?
If inflammation occurs in the nearby sweat tube, progress can become chronic. In this case, the old scar and due to the healing of the ulcer and the fresh part of the violation appear alternately in the affected area. Painful infiltration, swelling and inflammation of the skin above it.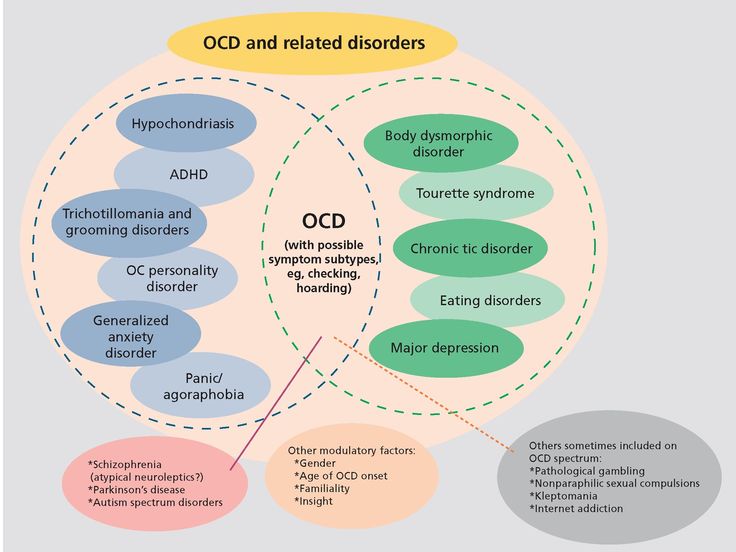 This situation can last for more than a month. In this case, hospitalization may be required.
This situation can last for more than a month. In this case, hospitalization may be required.
Leaving weak people or medical care can cause abscess and sputum, which can rarely cause sepsis. HIV/AIDS often causes complications.
The most likely cause of the complications is that the skin surrounding the inflammatory gland is not well cared for. Dirty skin, immersion skin, and bleeding skin will spread very quickly and include all new details. To make an abscess, some of the nearby glands can cause inflammation. At the same time, the abscess can coalesce, dissolve adjacent tissue, destroy subcutaneous tissue, and sometimes reach the muscles.
Fregmon is the next step when an abscess grows. This is a spilled inflammation that grows more violently in the subcutaneous tissue. Phlegmon is found in both distant places near the place where the primary inflammation occurred.
Abscess and sputum with signs of systemic poisoning and remarkable weight.
Complications of hidradenitis
Sepsis occurs when pathogens enter the general circulation.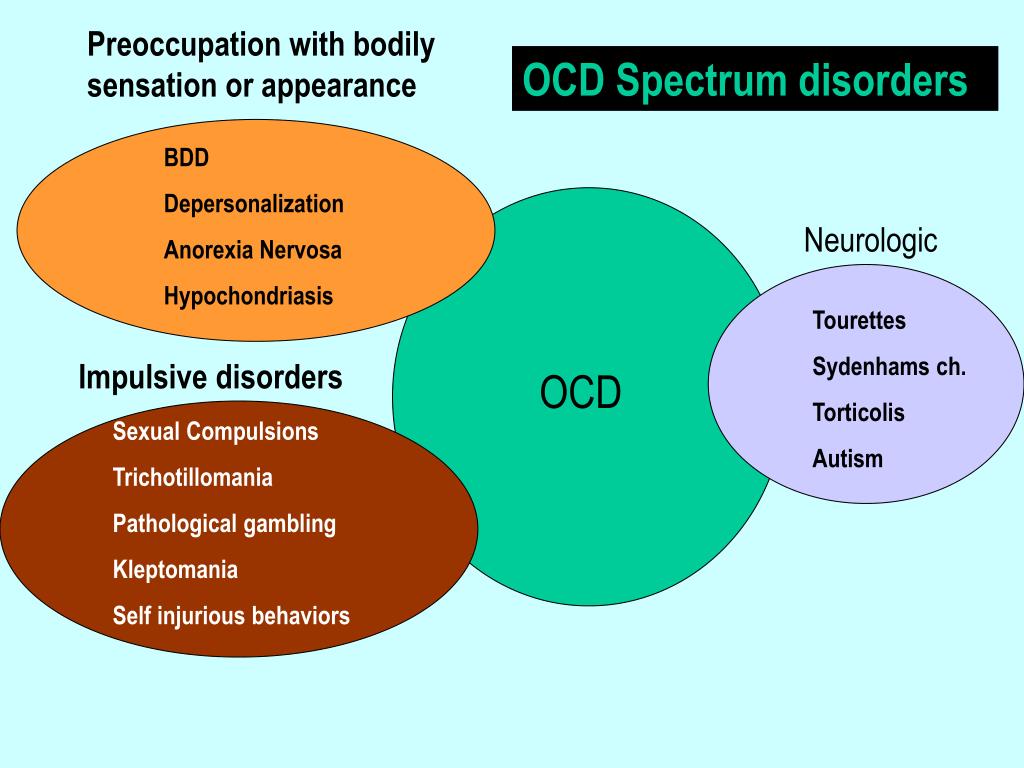 At the same time, there is a possibility that all organs may have an abscess, which is very dangerous.
At the same time, there is a possibility that all organs may have an abscess, which is very dangerous.
The characteristic clinic, in principle, has no doubts. In hydropholinism, there is no necrotic stick as a result. If a pathogen (tuberculosis, lymphatic disease) is suspect, cultures of separated bacteria are settled to adjust for antibiotic susceptibility. In all calculations of blood cells, inflammatory changes (leukocytes, increased SBP) can be tolerated. In the course of chronic and relapse, the immunological state is determined.
The highest success rate in treating hydropholysma is in the early stages of inflammation with only glands or one or two. Patients can ask dermatologists for help.
First consultation fee a-4000
Resale fee i-2500
Diagnosis features
Treatment depends on many factors such as site of hydrofolism, age, sex, transformed diseases and health status.
Conservative treatment
The most important thing about inflammation in one gland or a place far apart is to carefully care for the surrounding skin by repeatedly wiping any alcohol (boron, salicylic acid, Kampala).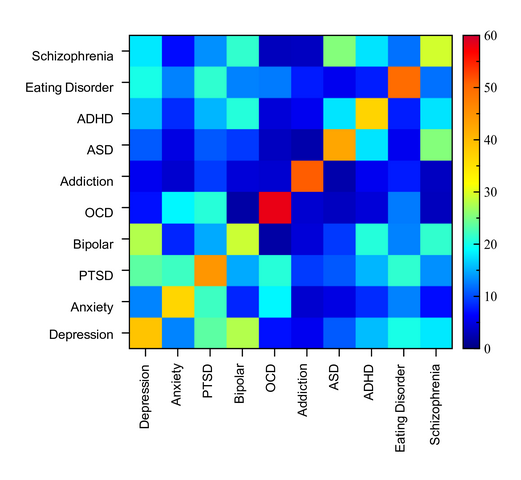 Removal always removal can prevent the spread of infections in combination with the effects of alcohol. The hair around the inflammatory area should be carefully cut.
Removal always removal can prevent the spread of infections in combination with the effects of alcohol. The hair around the inflammatory area should be carefully cut.
- You do not need to take a bath when you are sick. Bathing promotes the spread of infection. It is necessary to cover the inflamed area in a thick bandage, fix it with a patch and use the shower.
- To eventually recover, you need to protect sweets, alcohol, spices, and spices for at least three months. Food treatment is recommended to increase protection. Eat plenty of vegetables and fruits that contain many natural ingredients such as cabbage, apple, citrus fruits, carrots, roses, and walnuts. Natural irritants such as Tinky Agents for Ginseng, Ginseng, Giant Juice and Roasted Rose Juice. Pharmacies are recommended for adding polychloride to food.
Preservative therapy prescribed by a doctor. In many cases, the antibiotic semi-synthetic tetraicin and other groups are selected according to the results of bacterial tests.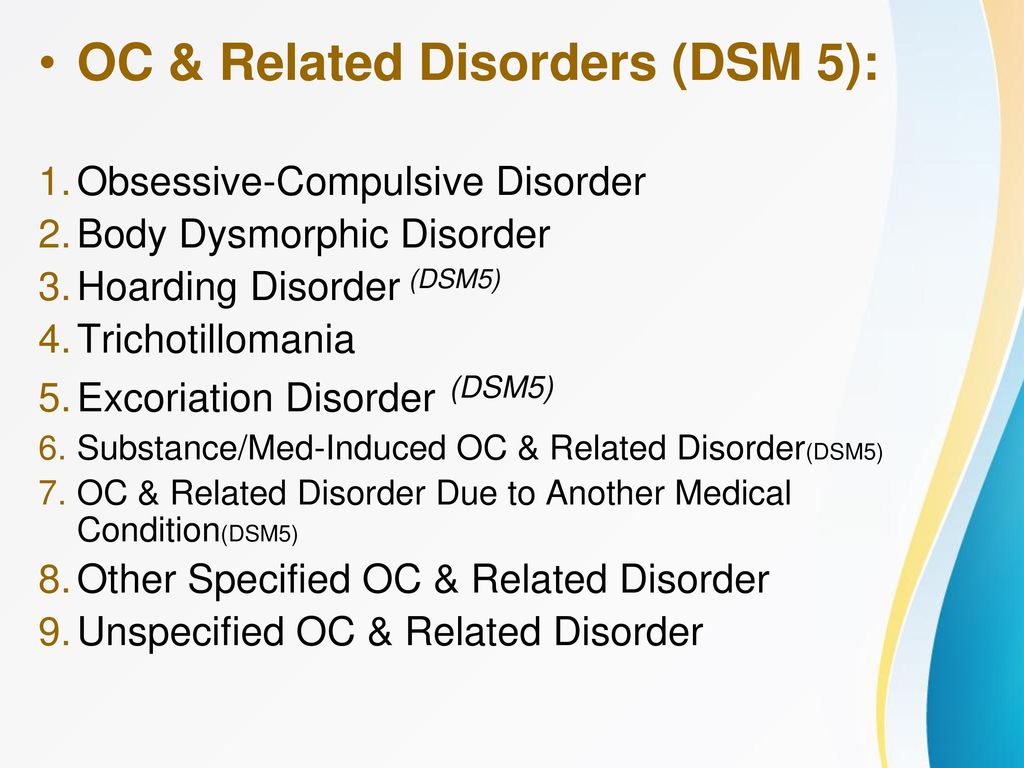 In the case of staphylococci, an appropriate γ-posophyllin or vaccine can be used.
In the case of staphylococci, an appropriate γ-posophyllin or vaccine can be used.
Until an abscess forms, skin treatment with various disinfectants such as strong (96%) alcohol, green diamond and iodine is required. If the inflammatory site is extensive, choose an antibiotic solution containing Novocaine. Gender y-writer's clothes that change when dry may be required. The ointment cannot be used, the corresponding area will increase.
Also, do not press or open the abscess yourself. Inappropriate treatment only spreads the pus into the tissue and only leads to worsening of the symptoms. In this method the possibility of complications can arise many times.
Surgery is required if the center of inflammation is already subsided or the abscess opens naturally. At the same time, it is pointless to open and discharge abscesses. Because there are many small formulas in the thickness of the fabric. Wide incision that can access all inflammatory invasions. The incision must reach the border with a healthy organization.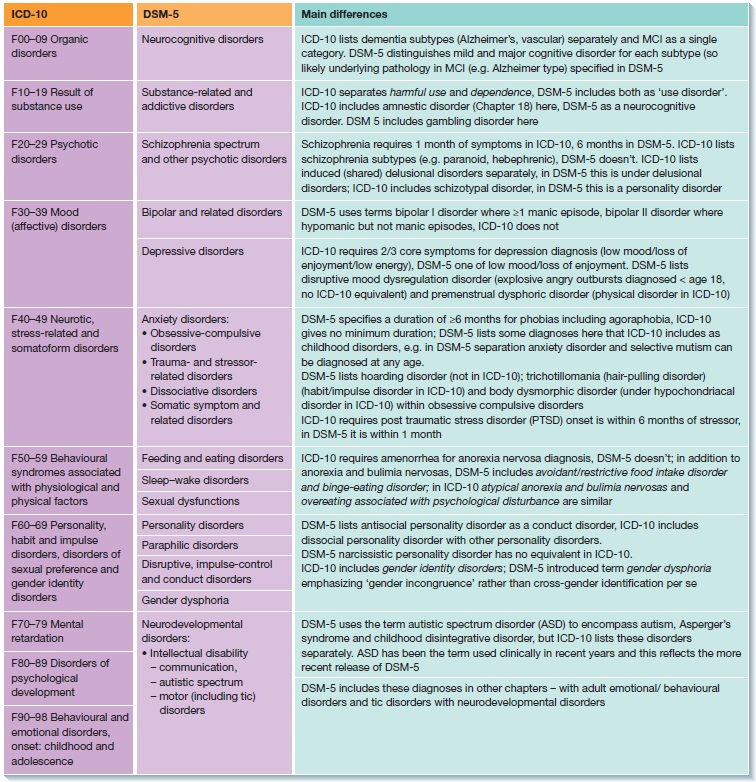 Take all the pus and then remove all the fatty fiber in the inflammatory part. When a drain is established, healing occurs with secondary force.
Take all the pus and then remove all the fatty fiber in the inflammatory part. When a drain is established, healing occurs with secondary force.
First consultation board a-3000
Follow-up consultation-2000
If the inflammation recurs over and over and due to recurrence or chronic progression, it is necessary to perform an operation for treatment. This treatment is performed in two stages.
Surgical treatment of hidradenitis
First, a large incision is made from chronic inflammation, and all subcutaneous tissues in the affected area are resected. The surgical creation is openly treated and the necessary antibiotics are used.
- When the wound is clean and healthy granulation appears, removal of the diseased skin and subcutaneous tissue is complete. The resulting deficiency is covered by a patient's skin flap harvested from another part. Maintaining the blood supply to the grafted flap can greatly accelerate healing. This technology is called "self-mountain formation".

Learn more
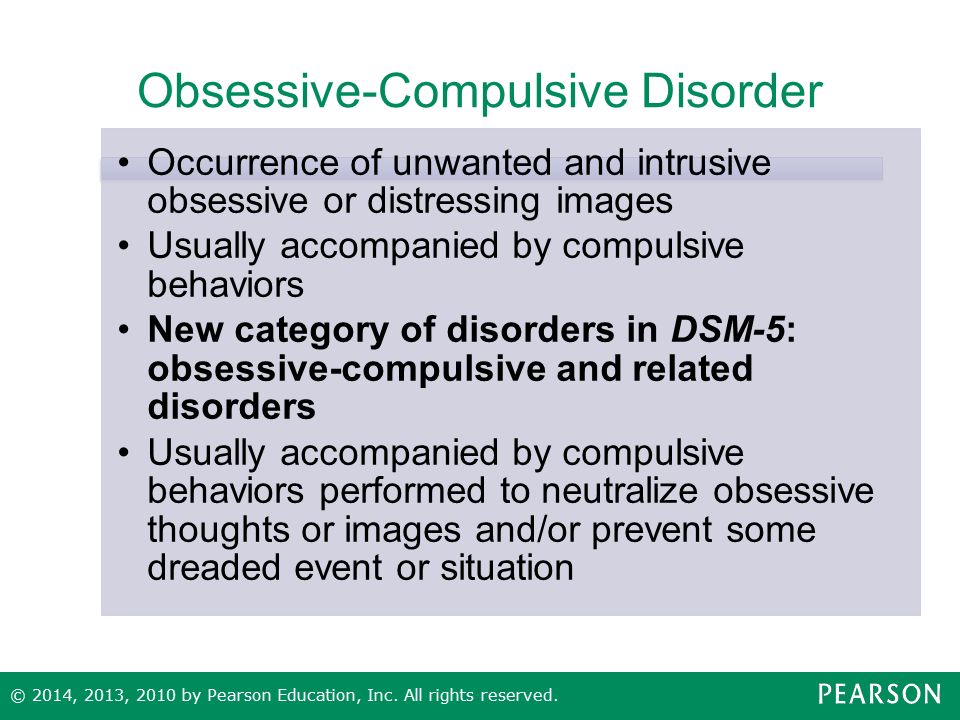
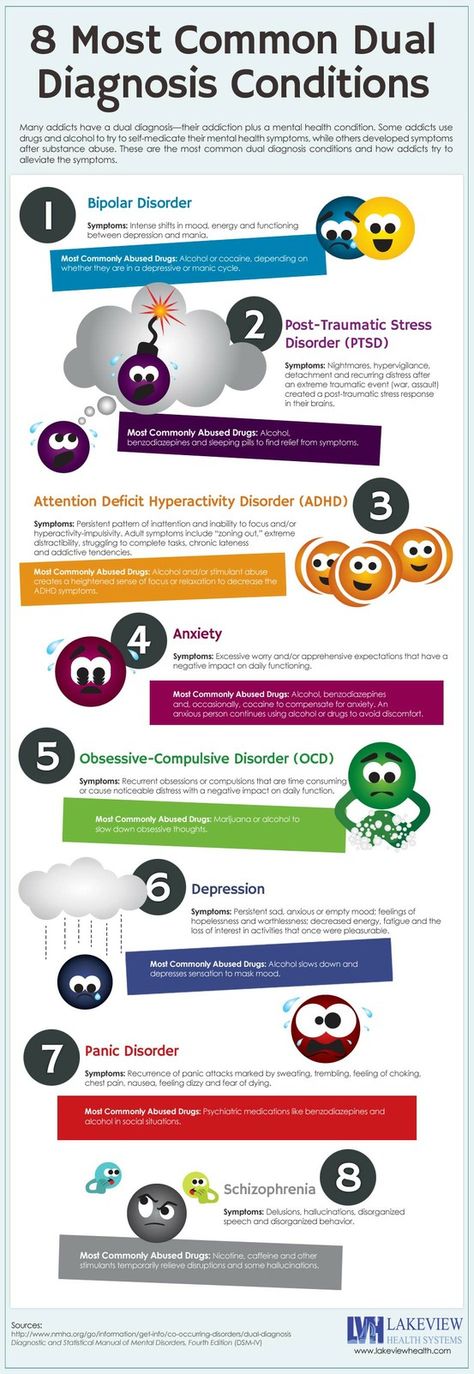
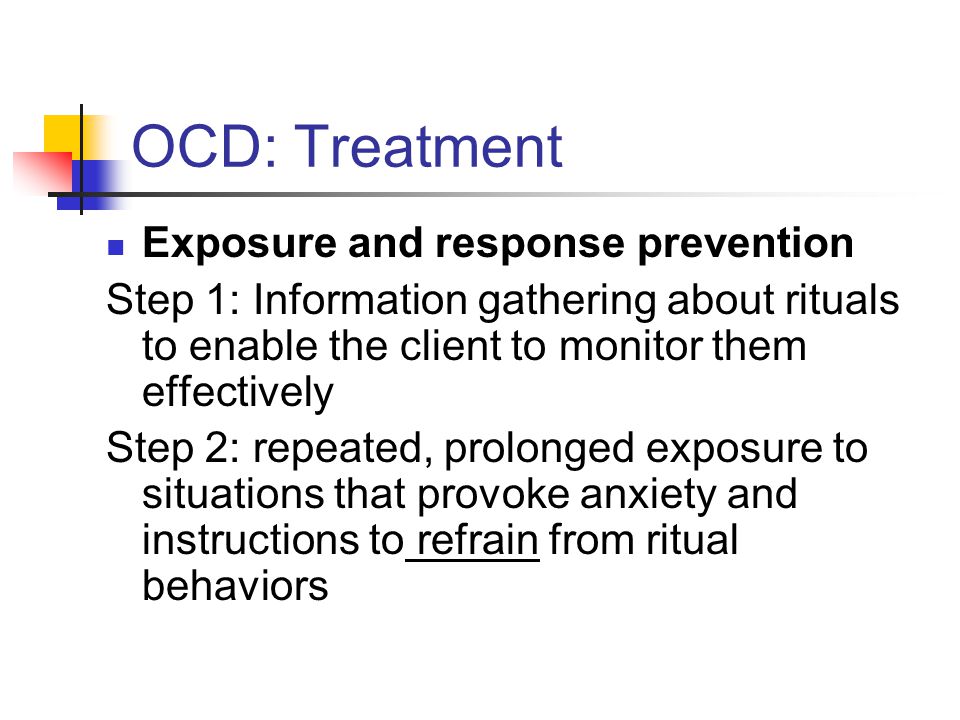
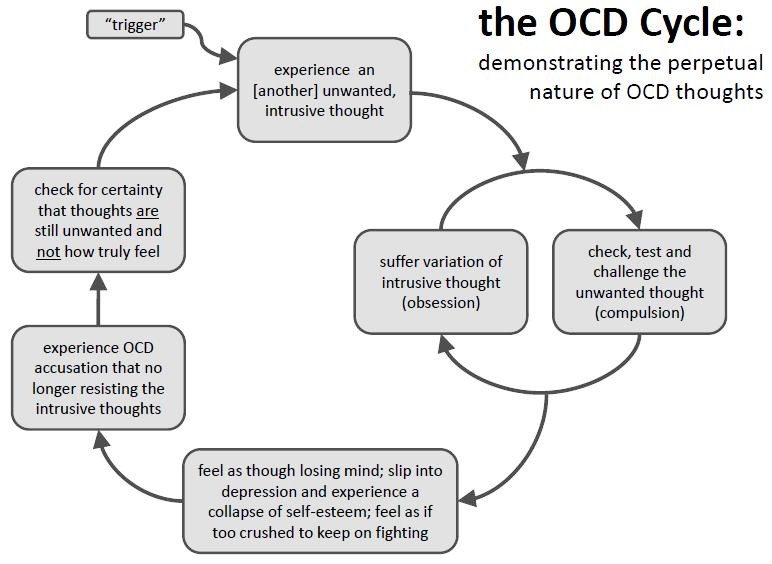
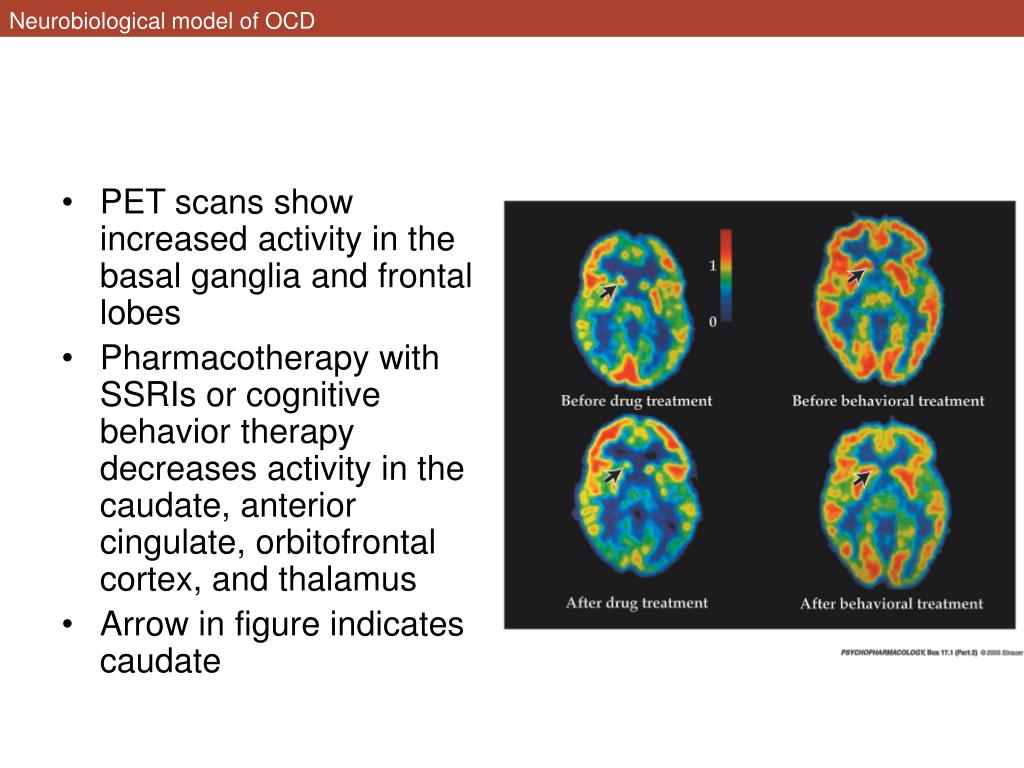
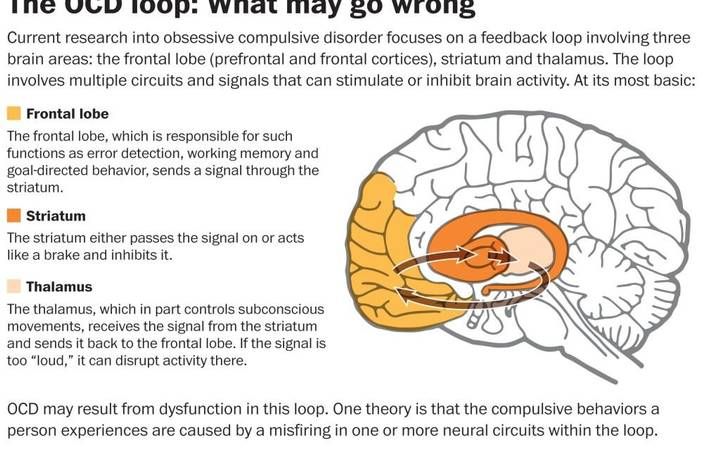 )
)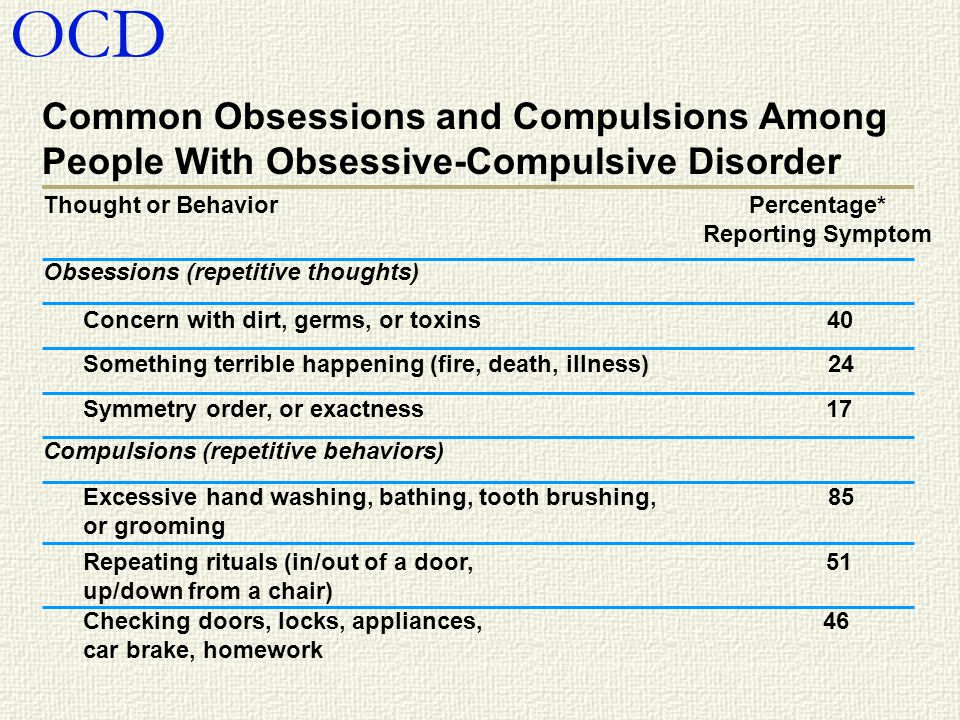

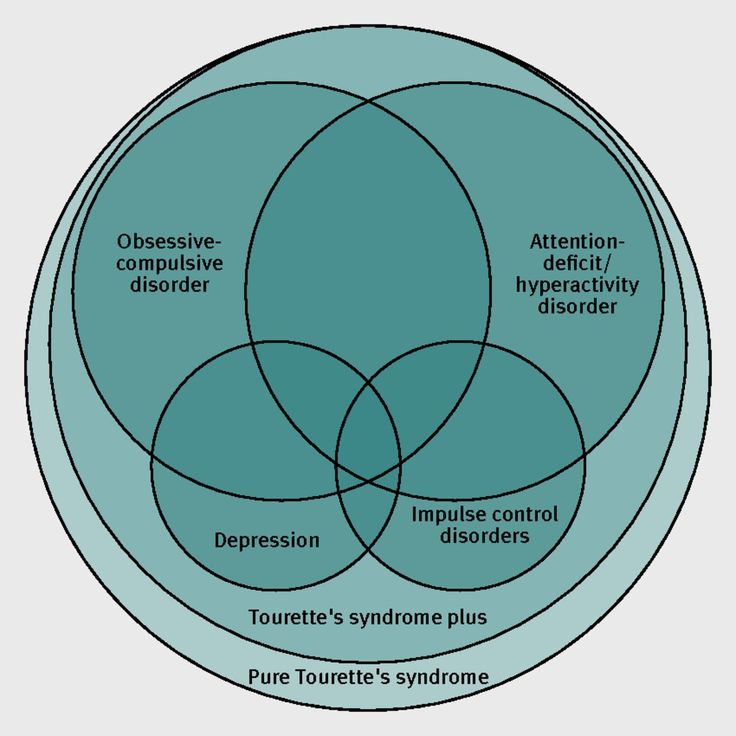
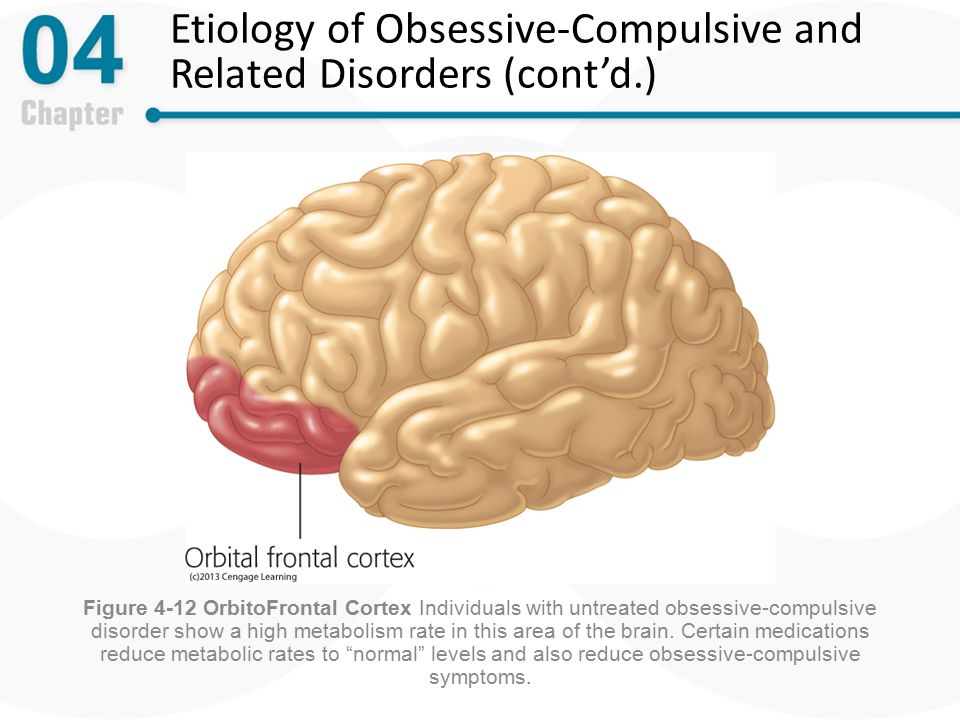 Thoughts that include sexual violent or religious themes
Thoughts that include sexual violent or religious themes