Mental disorder where you have no emotions
Is There A Mental Health Reason For Showing No Emotions?
Talking to someone who appears to be displaying no emotion or feelings toward people or situations can feel frustrating at times, especially if the reason for the lack of emotion is not understood. No display of emotion can indicate emotional detachment or the presence of mental health or personality disorder.
Lacking Expression Can Make Communicating Difficult
Find Ways To Express Yourself With Therapy
Understanding Emotional Detachment
Emotional detachment and its related word or synonym is the avoidance of developing and showing emotional connections. Being emotionally detached or showing no emotions , often referred to as having a flat affect, involves the lack of positive or negative feelings or emotions.
It may be a temporary state of being in response to an emotionally traumatic event or the result of a chronic condition, such as depersonalization disorder. The lack of role models who exhibit healthy emotional responses, a history of failed relationships, or fear of being emotionally hurt may also contribute to the development of emotional detachment.
When a lack of emotions or emotional detachment occurs, it can be difficult to imagine the happiness of any kind. Although the person may be clinically depressed, the absence of any emotion may make it difficult to diagnose depression. An online therapist can help you navigate why you might get emotionally detached and can help you make a number of changes.
Types of Personality Disorders
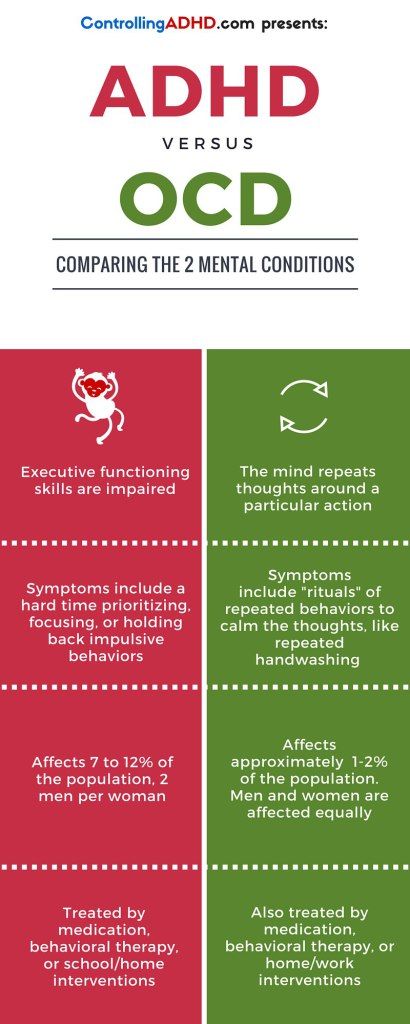
While feeling emotionally numb or feeling like you have no emotions can be a symptom of different medical conditions or medication side effects, a complete lack of passion could indicate the presence of a personality disorder.
A personality disorder is a type of mental health disorder that causes a person to have an unhealthy pattern of functioning, thinking, and behaving. People with a personality disorder generally have trouble perceiving and relating to other people and situations. One of the most significant symptoms of a personality disorder is a person’s lack of emotion or inability to express emotions.
One of the most significant symptoms of a personality disorder is a person’s lack of emotion or inability to express emotions.
Schizoid Personality Disorder
A schizoid personality disorder is a mental health condition that is characterized by an avoidance of social activities and interpersonal relationships. People who have schizoid personality disorder have a limited range of types of emotional expressions if they express emotions at all.
People with schizoid personality disorder are often viewed as loners or may be accused of being dismissive of others. They typically lack the desire and/or skills to form close personal relationships with others. Due to their lack of emotional responses, people can appear to be unconcerned or uncaring.
Symptoms of a schizoid personality disorder usually manifest by early adulthood. However, some signs may be evident during childhood or teenage years. Features of the disorder may contribute to difficulty functioning in school or work and may cause disruptions in personal and professional areas of life.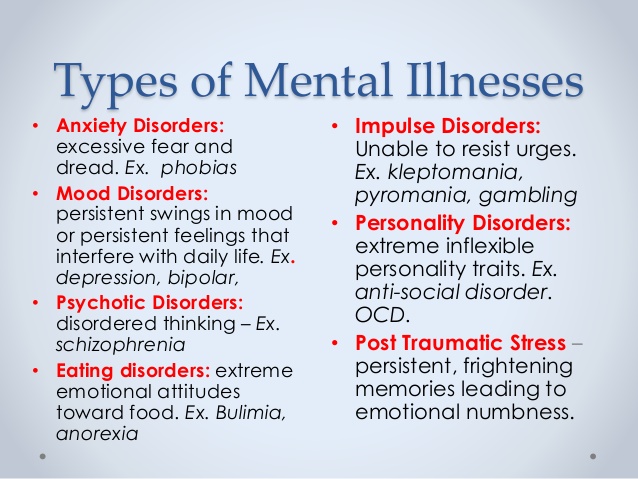 People with schizoid personality disorder usually prefer to work jobs that can be done alone. Prominent features of schizoid personality disorder include avoiding close relationships, no desire for sexual relationships, no response to praise and/or critical remarks from others, and lack of motivation or goals.
People with schizoid personality disorder usually prefer to work jobs that can be done alone. Prominent features of schizoid personality disorder include avoiding close relationships, no desire for sexual relationships, no response to praise and/or critical remarks from others, and lack of motivation or goals.
Schizotypal Personality Disorder
Individuals with schizotypal personality disorder may be described as eccentric or odd. They usually have few, if any, close relationships. They are unable to understand how relationships are formed or to appreciate the impact their behaviors may have on others. People with this disorder may misinterpret the motivations or behaviors of others and feel an overwhelming distrust of others. Despite their feelings, they rarely show any amount of emotion.
A schizotypal personality disorder is usually diagnosed with the presence of five or more of these symptoms:
- Inability to interpret events correctly
- Persistent and excessive social anxiety
- Being a loner
- Having few, if any, friends
- Inappropriate emotional response
- Flat affect
- Vague or unusual patterns of speaking
A schizotypal personality disorder is usually diagnosed in early adulthood, and symptoms typically last across the lifespan.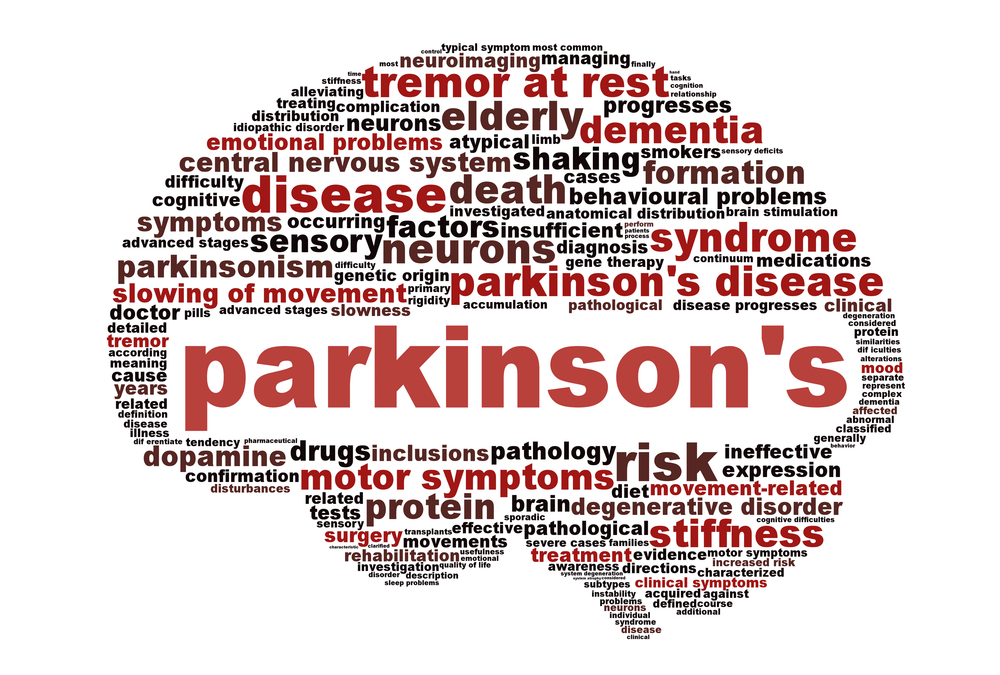 Treatment such as medication and some therapies may improve symptoms.
Treatment such as medication and some therapies may improve symptoms.
Schizophrenia
Schizophrenia is a serious mental disorder that causes disruptions in the way a person interprets reality. It may cause delusions, hallucinations, and disorganized behavior or thinking that impair daily functioning. Although people with schizophrenia may appear to have erratic behavior at times, when symptoms are active, the affected person will likely show little to no emotions.
Negative symptoms of schizophrenia refer to a reduced or lack of ability to function normally. When negative symptoms are present, the person may not make eye contact, might speak in a monotone, or will not change facial expressions. Social withdrawal and lack of ability to experience pleasure often occur, as well.
Sociopathic Personality Disorder and Psychopathic Personality Disorder
Also referred to as antisocial personality disorder, a sociopathic personality disorder is a personality disorder that involves pervasive lying and deception, physical aggression, disregard for the safety and well-being of others, and lack of remorse for any actions.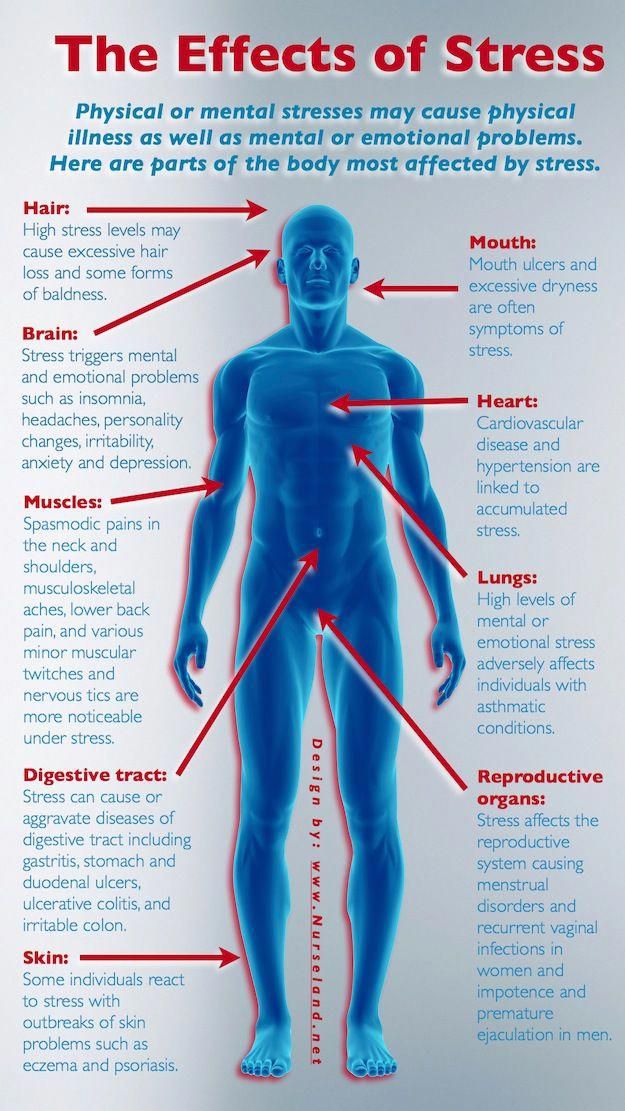
A psychopathic personality disorder is thought of as a more severe form of sociopathy, and an affected person usually exhibits more symptoms. Psychopathic traits include a lack of deep emotional attachments, superficial charm, reckless behavior, lack of empathy for others, lack of guilt or remorse, and manipulativeness.
What Causes Personality Disorders?
Although the exact cause of personality disorders is not quite clear, certain factors are believed to increase the risk of developing or triggering personality disorder traits. History of a childhood conduct disorder, changes in brain structure and chemistry, abusive or unstable family relationships, and a family history of personality disorders or other mental illness are all possible contributing factors.
Personality disorders can cause significant disruptions in the lives of the affected person and in the lives of the people who care for them. They can have negative impacts on personal and professional relationships, school, or work performance and may lead to social isolation, alcohol, or drug abuse.
Although there is no cure for most personality disorders, if the condition is detected early in life, some improvement in behaviors may be experienced. Because people with personality disorders do not process social experiences or emotions the same way unaffected people do, they are generally unable to experience emotional responses such as bonding, empathy, or caring. Further, their emotional behavior, or lack thereof, rarely changes.
Autism
Autism is the term used to describe a range of neurological conditions that may affect a person’s ability to communicate or interact socially and may present other behaviors. Autism symptoms may be mild or severe.
The first symptoms of autism may become apparent in infancy when babies appear abnormally withdrawn and unresponsive to emotional bonding. As some children and adults with autism grow, they may be unable to engage in social situations similar to neurotypical children.
Alzheimer’s Disease
Alzheimer’s is a form of dementia.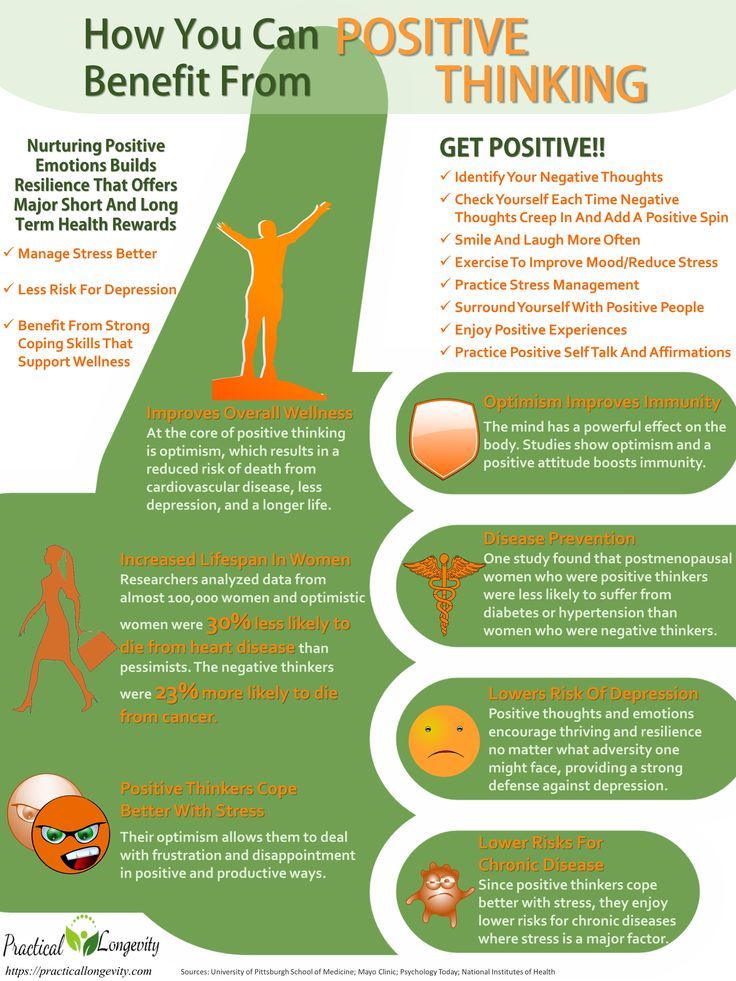 It affects memory, behavior, and mood, which can cause confusion and difficulty recognizing or relating to others. People with Alzheimer’s disease may first exhibit mild personality changes and a lack of spontaneity. As the disease progresses, increased memory loss occurs. Decreased cognition and emotional responses become more pronounced with time, and the disease eventually causes the affected individual to revert to a child-like state requiring total care.
It affects memory, behavior, and mood, which can cause confusion and difficulty recognizing or relating to others. People with Alzheimer’s disease may first exhibit mild personality changes and a lack of spontaneity. As the disease progresses, increased memory loss occurs. Decreased cognition and emotional responses become more pronounced with time, and the disease eventually causes the affected individual to revert to a child-like state requiring total care.
Is There a Treatment to Help People Without Emotions?
The underlying cause for a feeling of no emotions is the determining factor of whether a treatment option may be successful.
Some people, such as those with a personality disorder, may not see a problem with their lack of emotion and may be unwilling to seek treatment. However, if you are in a relationship with a person or have a family member who is exhibiting personality disorder traits, it is important to reach out for help. Although you cannot force someone else to get help, being in a relationship with someone who shows no emotional responses can have a profound effect on even the strongest person.
If you are concerned about someone who shows signs of impaired cognition and emotion, or if you are personally experiencing symptoms that make you uncomfortable, reach out to your primary care provider or mental health professional. Take the time to talk about your concerns. Talking to a counselor or therapist can help you make sense of the symptoms you are experiencing or witnessing. Besides, a mental health professional can help you establish a plan to protect your safety and well-being.
Mental health care options include individual and family therapy, psychosocial support that focuses on developing communication and vocational skills, and monitoring of any medications that may be prescribed. Some people prefer to develop an in-person relationship with a therapist, psychiatrist, or counselor. Others are more comfortable with an approach that allows them to experience counseling in a more relaxed personal setting. For those people, online counseling may be an effective option.
Lacking Expression Can Make Communicating Difficult
Find Ways To Express Yourself With Therapy
Online Therapy Can Help
There is a growing body of evidence pointing to online therapy as an effective means of helping individuals manage symptoms of emotional impairment. In one wide-ranging review published in Schizophrenia Research, the efficacy of online therapy for those living with psychosis (80% were living with schizophrenia-spectrum disorders) was examined. The report aggregated the results of 12 studies, finding that 74-86% of participants successfully utilized online treatments, and 75-92% perceived them as helpful. Researchers noted that online therapy is cost-effective, accessible, and flexible, finding that it could improve socialization and social connectedness.
As discussed above, if you are experiencing issues with emotional impairment, online therapy can help you find ways of expressing yourself. With online therapy through BetterHelp, you’ll be able to connect with a therapist through live chat, videoconference, voice call, or messaging.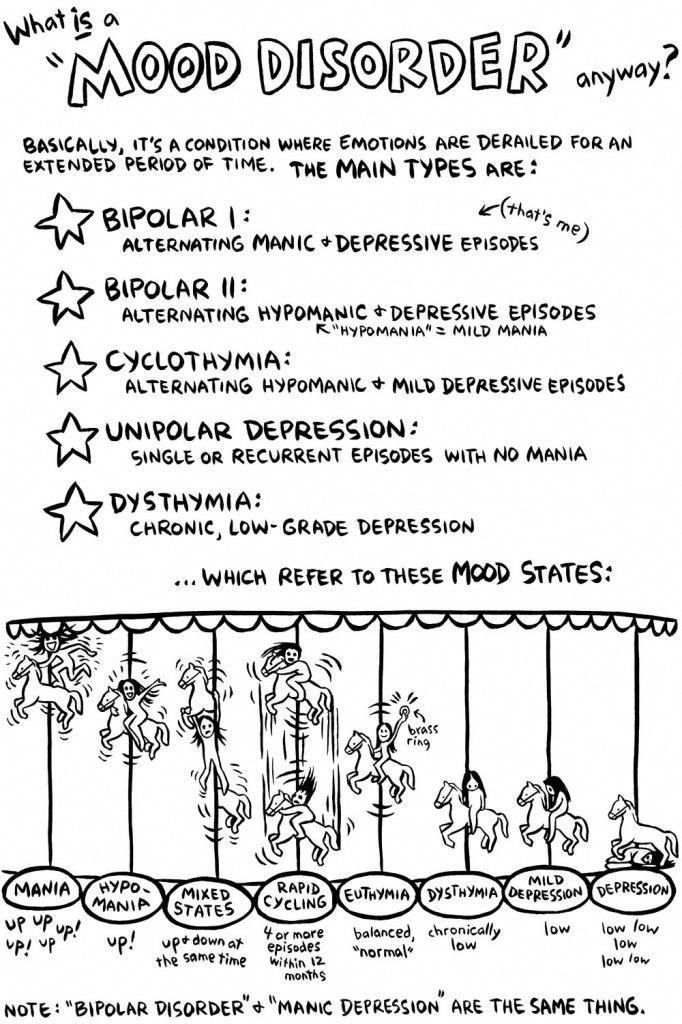 Plus, you’ll be able to reach out to your counselor outside of sessions. If you need to discuss something, have a question, or simply want to chat, send your therapist a message and they will get back to you as soon as possible. The mental health professionals at BetterHelp know how to provide you with the tools to become more in tune with your emotions. Read below for counselor reviews, from those who have sought help in the past.
Plus, you’ll be able to reach out to your counselor outside of sessions. If you need to discuss something, have a question, or simply want to chat, send your therapist a message and they will get back to you as soon as possible. The mental health professionals at BetterHelp know how to provide you with the tools to become more in tune with your emotions. Read below for counselor reviews, from those who have sought help in the past.
BetterHelp Therapist Reviews
"Dr. Anais has given me the tools to understand my emotions, befriend them and accept them. If I were to return I would 100% want to be matched with Dr. Anais again. After just 5 weeks I feel lighter and brighter, her professionalism and sensitivity are second to none."
“Jillian has been amazing! I felt like I was talking to one of my friends (but more qualified to offer advice) she made me feel comfortable expressing myself and helped me to understand what it is I’m feeling and how to manage unwanted feelings like anxiety. I will be recommending her to everyone I know. Thank you for everything!”
I will be recommending her to everyone I know. Thank you for everything!”
A Final Word
As disheartening as interacting with someone who shows no emotional response may feel, it is important to care for yourself and promote your mental well-being. Reaching out for help can help you focus on behaviors that can foster emotional and physical well-being and help you cope with the experiences of having someone with a lack of emotion in your life.
Alexithymia: Causes, Symptoms, and Treatments
Alexithymia is a broad term to describe problems with feeling emotions. In fact, this Greek term used in Freudian psychodynamic theories loosely translates to “no words for emotion.” While the condition is not well-known, it’s estimated that 1 in 10 people has it.
While Freudian theories are largely considered dated, this condition seems to be increasing in awareness. It’s often seen as a secondary diagnosis in other preexisting mental health conditions and disabilities, including depression and autism.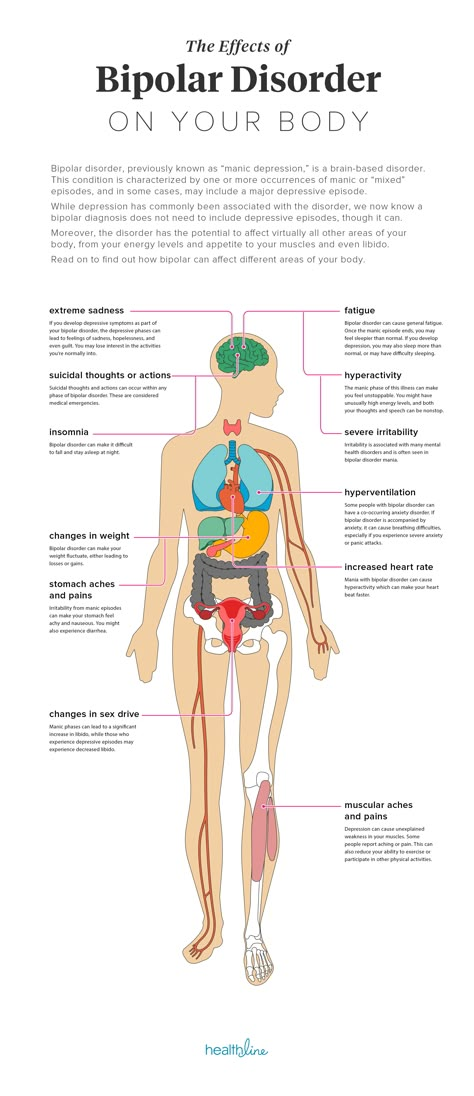
However, this does not mean that everyone with these conditions has problems expressing with and identifying emotions. In fact, studies show that it only affects a small percentage.
People who do have alexithymia may describe themselves as having difficulties with expressing emotions that are deemed socially appropriate, such as happiness on a joyous occasion. Others may furthermore have trouble identifying their emotions.
Such individuals don’t necessarily have apathy. They instead may not have as strong of emotions as their peers, and may have difficulties feeling empathy.
Read on to learn more about the possible causes of alexithymia, as well as treatments and therapies for this condition.
Alexithymia isn’t well understood. There’s a possibility it may be genetic.
The condition may also be a result of brain damage to the insula. This part of the brain is known for its role in social skills, empathy, and emotions, with some studies linking insula lesions to apathy and anxiety.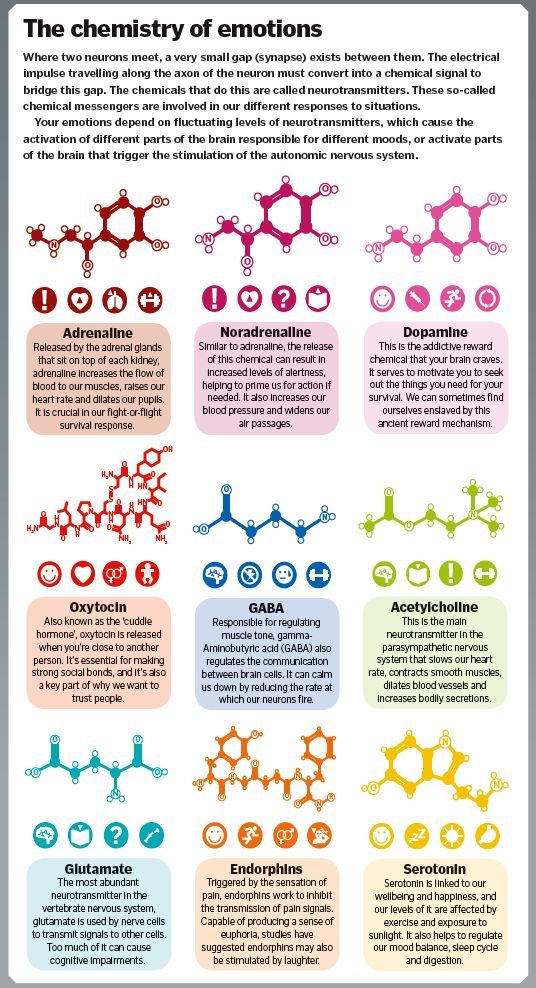
Links to autism
The symptoms of autism spectrum disorder are wide-ranging, but there are still some stereotypes associated with this condition. One major stereotype is a lack of empathy, something that has largely been debunked.
At the same time, some research indicates that up to half of people with autism also experience alexithymia. In other words, it’s alexithymia that causes the lack of empathy, and not autism itself.
Emotions and depression
It’s also possible to experience alexithymia with depression. It has been noted in major depressive and postpartum disorders, as well as schizophrenia. Research indicates that between 32 and 51 percent of people with depressive disorders also have alexithymia.
Possible traumaAdditionally, this condition has been noted in people who have experienced trauma, especially during early childhood. Trauma and neglect at this stage may cause changes in the brain that can make it difficult to feel and identify emotions later in life.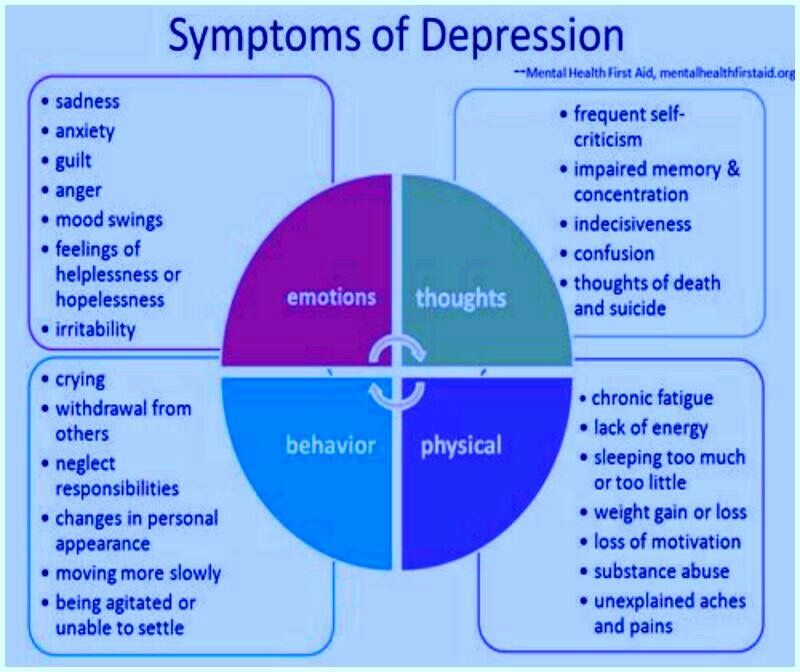
Other associated conditions
Research also indicates that this condition may be present in certain neurological diseases and injuries. These include:
- Alzheimer’s disease
- dystonia
- epilepsy
- Huntington’s disease
- multiple sclerosis
- Parkinson’s disease
- stroke
- traumatic brain injury
As a condition marked by lack of feelings, it can be difficult to recognize the symptoms of alexithymia. Since this condition is associated with an inability to express feelings, an affected person might come across as being out of touch or apathetic.
However, a person with alexithymia might personally experience the following in social contexts:
- anger
- confusion
- difficulty “reading faces”
- discomfort
- emptiness
- increased heart rate
- lack of affection
- panic
This condition may also make it difficult for a person to interpret body changes as emotional responses.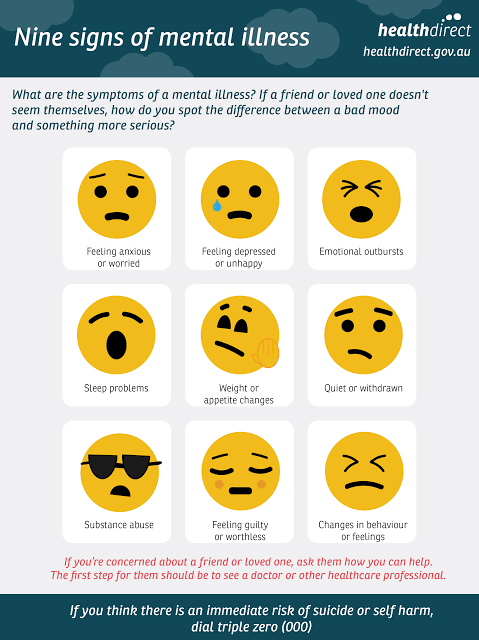 For example, you might have trouble linking a racing heart to excitement or fear, but are still able to acknowledge that you’re experiencing a physiological response in the moment.
For example, you might have trouble linking a racing heart to excitement or fear, but are still able to acknowledge that you’re experiencing a physiological response in the moment.
Alexithymia is diagnosed by a mental health professional. It’s not officially recognized by the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Instead, your mental health provider will likely ask you questions and provide a diagnosis based on your answers. You may also be asked to provide a self-reported questionnaire.
Another possible test is an MRI performed by a neurologist. This will provide images of the insula in the brain.
There’s no one single test for alexithymia, much like neurological disorders and mental illnesses in general. It can take time to receive the right diagnosis.
To date, there isn’t a single individual treatment for alexithymia. The exact treatment approach depends on your overall health needs. For example, if you have depression or anxiety, taking certain medications for these conditions could also help mental health symptoms.
Therapies may also be helpful for this condition. These allow you to participate in exercises to help improve mental health.
Possible therapy options include:
- cognitive behavioral therapy (CBT)
- group therapy
- psychotherapy (also known as “talk therapy”)
One possible step towards emotional recognition is to start being mindful of your own physiological responses. Some research has suggested the importance of beginning with your heart rate.
Notice whether your heart rate goes up in certain situations, and explore the possibilities of why this could be. A heart rate monitor or fitness watch can also help. With practice, you may become better able to distinguish anger from excitement and fear, for example. A journal can also help you document your physical responses and emotional patterns.
It’s also important to keep in mind that negative emotions are just as important as positive ones. Learning how to identify these emotions and work with them (not against them) can help you lead a more fulfilling life.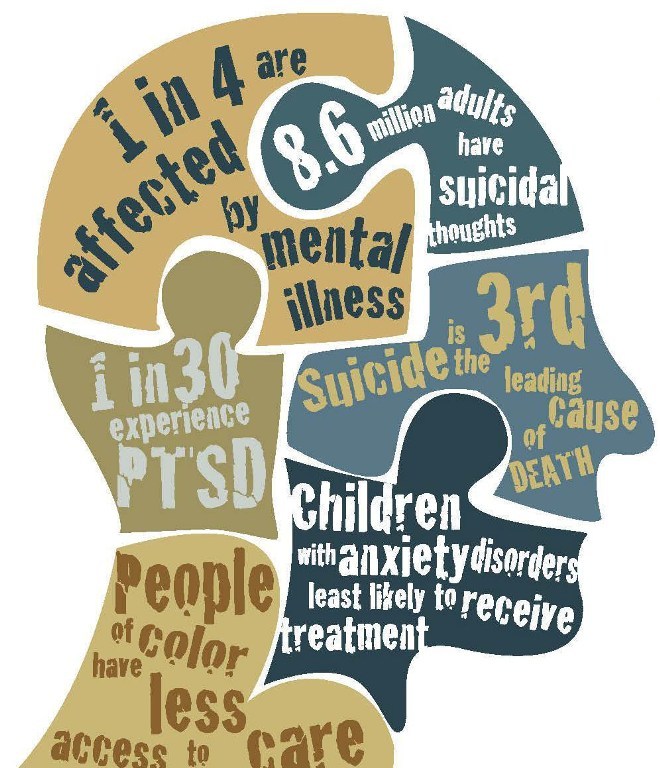
Alexithymia can cause frustration for people who experience it, as well as friends and loved ones. If you think you’re having trouble with recognizing or describing feelings, consider talking to a doctor about it. They can help guide you to the right therapy options to help improve on these important life skills.
If you don’t already have a mental health professional, our Healthline FindCare tool can help you connect to doctors in your area.
Alexithymia isn’t widely known, but this condition has been studied for more than four decades. It’s presented in individuals who have difficulty recognizing and expressing feelings, and it often coincides with another underlying neurological condition or mental health disorder.
While not inherently dangerous, this condition may inadvertently lead to interpersonal and relationship issues. The good news is that there are therapies available that can help you improve on mental health skills. Not only will this help with relationships with others, but more importantly, you may feel better, too.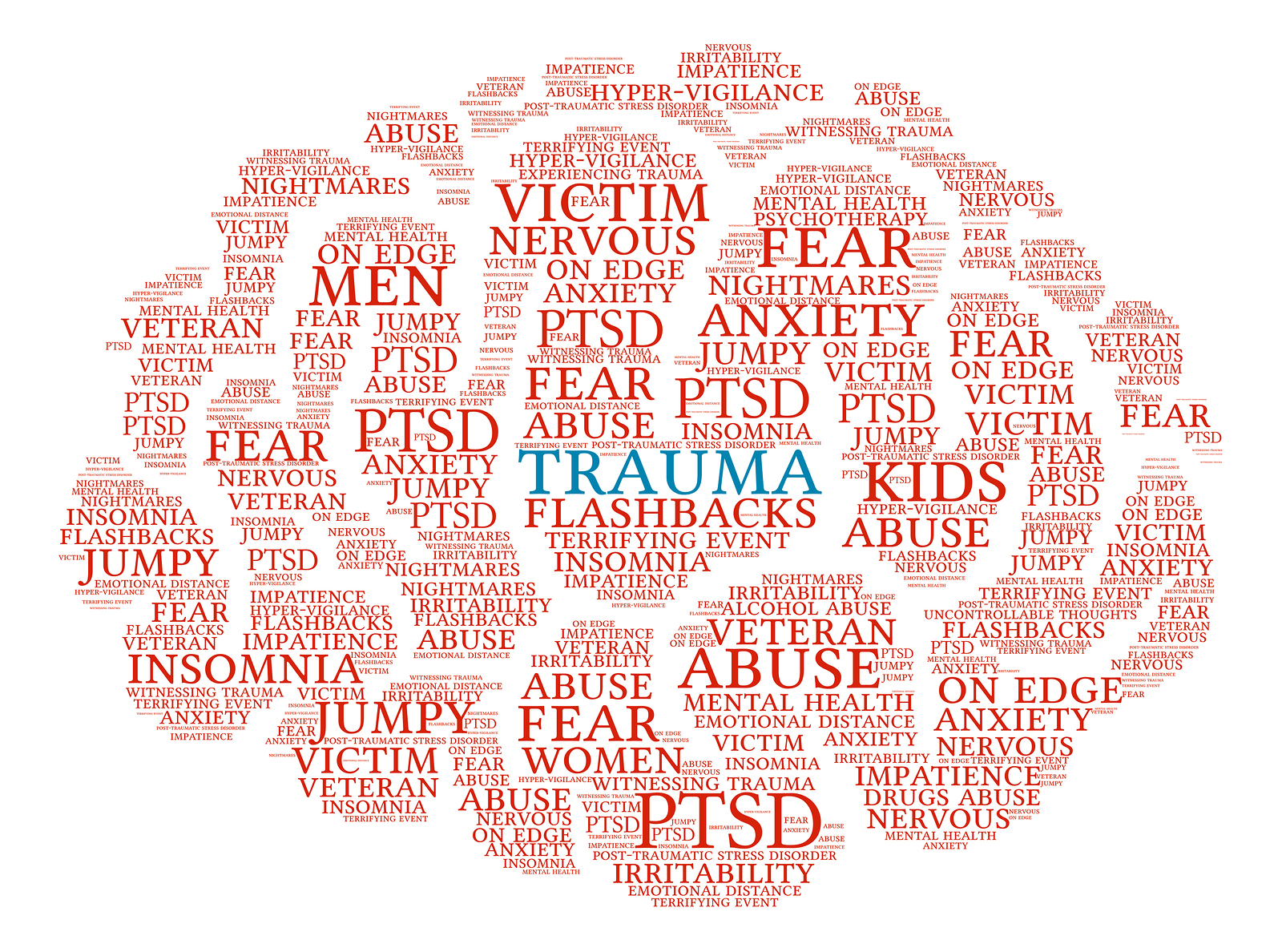
Read this article in Spanish.
Alexithymia: an emotional gap hiding under the mask of normality
Alexithymia is a psychological state of a person in which a person, having lost the ability to determine and display his own emotions, is forced to try to look normal in the eyes of others. The psychiatrist Saito Satoru talks about this disorder using examples from his own practice, as well as the example of the heroes of the novel "Man of the convenience store" ( Kombini ningen , by Murata Sayaka), awarded the Akutagawa Prize for 2016.
In psychiatry there is a term "alexithymia". It consists of the negative prefix "ἀ" and two stems: "λέξις" (word) and "θυμός" (feelings, emotions). This term describes a psychological state where a person is unable to evaluate and describe their own emotions. In order to have a holistic view of one's own life, the individual must be aware of and distinguish what he feels. However, there are people who are incapable of this - they do not understand in what situations this or that emotion arises in them. Features of alexithymia appear in such people in those moments when they are overcome by anger, sadness, or any other strong feeling that they are not able to define and express.
Features of alexithymia appear in such people in those moments when they are overcome by anger, sadness, or any other strong feeling that they are not able to define and express.
In fact, with the exception of babies, there are practically no people in modern society who would cry or scream, completely without restraint. It is understood that an adult member of society should control himself and not show such primitive emotions outwardly. And if he is not able to restrain himself, then he needs treatment.
Young people striving to conform to the notions of "normality" learn from the older generation to suppress the expression of emotions. Over time, some of them lose the ability to recognize their own feelings. Suppressed anger, sadness become the cause of psychosomatic diseases and hypochondriacal disorders. Hypochondriacs are characterized by a clear manifestation of somatic symptoms in the absence of any significant pathological abnormalities. As a result of an anxious set and constant concern about health, the functions of the heart, gastrointestinal tract and other autonomically innervated systems can be disturbed. And this, in turn, leads to the development of arterial hypertension, peptic ulcer, etc. That is why hypochondria is considered a psychosomatic disease.
And this, in turn, leads to the development of arterial hypertension, peptic ulcer, etc. That is why hypochondria is considered a psychosomatic disease.
However, with alexithymia, not only negative emotions are blurred, but also positive ones - a person is not able to experience such feelings as joy or inspiration. The loss of the ability to experience pleasure is called anhedonia. This disorder is characterized by a loss of motivation for activities that the individual enjoyed in the past. The development of anhedonia is an important indicator in the diagnosis of pathological depression.
Under the guise of normality
I have my own psychiatric practice in Tokyo, and I encounter people suffering from depression and hypochondria on a daily basis at work. During the first meeting, most of them show no signs of suffering or despair. And I have to pull off their mask of normality, under which they hide their illness, which needs treatment.
Cover of "Convenience Store Man" (illustration courtesy of Bungei Shunju)
I thought about this when I read the novel "Convenience Store Man" for which Murata Sayaka recently won the Akutagawa Prize. Indeed, in this story we are talking about a person suffering from alexithymia. The heroine, a woman named Kokura Keiko, worked for 18 years as a saleswoman in the same minimarket ( combi) - it is on her behalf that the story is being told. She made it a rule never to show her feelings or express judgment. Instead, she has created a "patchwork personality" by copying the behavior and adopting the habits and mannerisms of the women around her (mostly work colleagues), whom she considers correct and admires for their style. This effective and convenient strategy allows it to adapt to its own environment. The moment she arrives at work shortly before the start of her shift and changes into her work uniform, Keiko becomes a function, a convenience store man. Now all that is required of her is to perform the prescribed duties for the appointed time, using the skills she has learned and the judgments she has borrowed appropriate to the occasion. The school years of the heroine passed under the endless complaints of parents who were dissatisfied with their individualistic daughter, and constant pressure from school teachers.
Indeed, in this story we are talking about a person suffering from alexithymia. The heroine, a woman named Kokura Keiko, worked for 18 years as a saleswoman in the same minimarket ( combi) - it is on her behalf that the story is being told. She made it a rule never to show her feelings or express judgment. Instead, she has created a "patchwork personality" by copying the behavior and adopting the habits and mannerisms of the women around her (mostly work colleagues), whom she considers correct and admires for their style. This effective and convenient strategy allows it to adapt to its own environment. The moment she arrives at work shortly before the start of her shift and changes into her work uniform, Keiko becomes a function, a convenience store man. Now all that is required of her is to perform the prescribed duties for the appointed time, using the skills she has learned and the judgments she has borrowed appropriate to the occasion. The school years of the heroine passed under the endless complaints of parents who were dissatisfied with their individualistic daughter, and constant pressure from school teachers.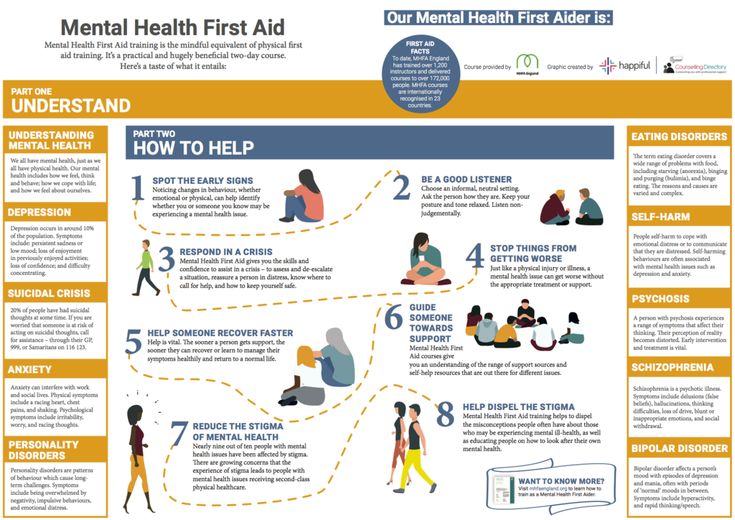 As an adult, she is grateful for the opportunity to hide her identity under a faceless uniform.
As an adult, she is grateful for the opportunity to hide her identity under a faceless uniform.
However, when Keiko suddenly realizes that those around her feel sorry for her - a single woman who worked as a saleswoman in a minimarket for 18 consecutive years - she becomes extremely worried. At this moment, she meets a new minimarket employee, a man who is the complete opposite of her. He is convinced that society has turned its back on him and that everyone is hounding and persecuting him. So he doesn't even try to appear normal, and very soon he is fired from the convenience store. Keiko invites him to stay with her. At first glance, it seems that they are a very harmonious couple, but their relationship is built on a cold calculation. For a workaholic Keiko, this is an opportunity to create the appearance of a romantic relationship; for a lazy man, life with Keiko is an excellent hiding place from the injustice of a cruel world. But their life together upsets the fragile mental balance that Keiko has maintained and strengthened in herself throughout all these eighteen years.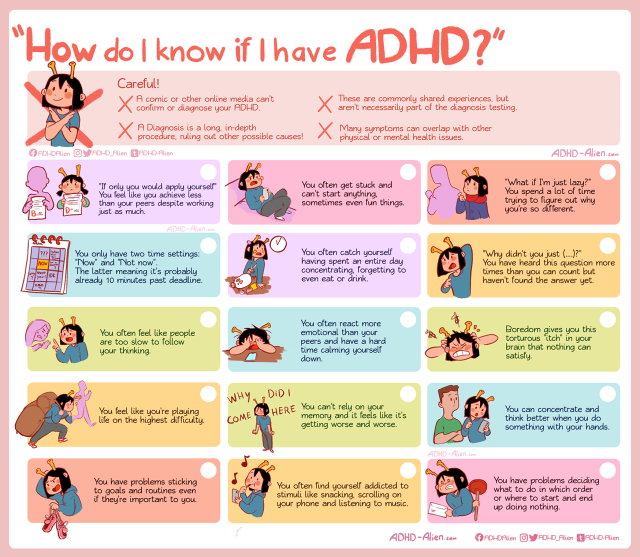
The caustic remarks of her roommate expose her spiritual emptiness, the gaping emptiness of her personal space, which Keiko had refused to notice for so many years. Refusal, denial is a primitive psychological defense mechanism, a subconscious attempt to ignore the problem, the existence of which is obvious to any outside observer. And the one who denies the obvious looks infantile and eccentric in the eyes of others.
Realizing the hopelessness of his situation, Keiko quits his job and ceases to be a "man of the convenience store". She has no choice but to lie all day under the covers, on the futon, which she spread out inside the closet. I call this phase "bed addiction" and I believe that it is the starting point for the development of other types of addiction: from drug or alcohol addiction to sexual addiction. In fact, both addictive behavior and "show normality" are desperate attempts to get out of the quicksands of the emotional vacuum.
This story has a somewhat happy ending - Keiko starts working at the convenience store again.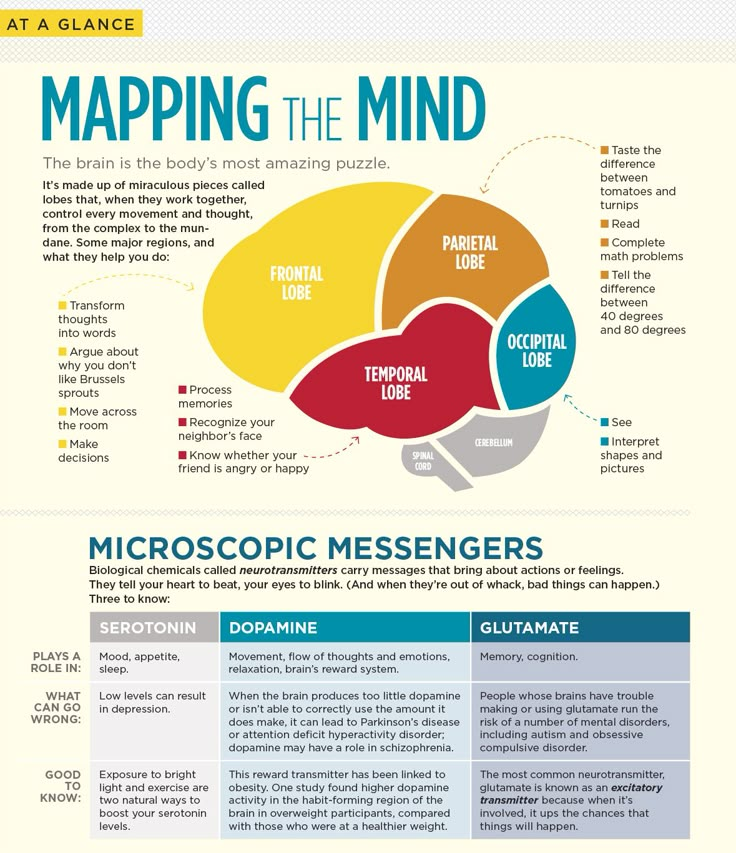 But I do not think that this will make many readers laugh too much, as they notice the connection between excessive obsession with work and the meaninglessness of the heroine's personal space.
But I do not think that this will make many readers laugh too much, as they notice the connection between excessive obsession with work and the meaninglessness of the heroine's personal space.
Refusal to feel
"Bed addiction" is essentially a regression to the so-called "primal sleep" - a dream-like state characteristic of infants. This is exactly the state that heroin addicts so passionately desire to achieve. A similar process of regression is also experienced by recluses.0003 hikikomori . Every day this quagmire sucks in hikikomori more and more, and getting them out of it is not an easy task.
Here it is important to pay attention to one point. A baby who falls asleep while nursing and wakes up to find that he has been taken from his mother's breast will feel restless, angry, flushed and crying.
Older babies (between a year and a half) also live in a world of basic emotions such as anger, anxiety, depression, or sadness. But adults hikikomori are deaf to these emotions.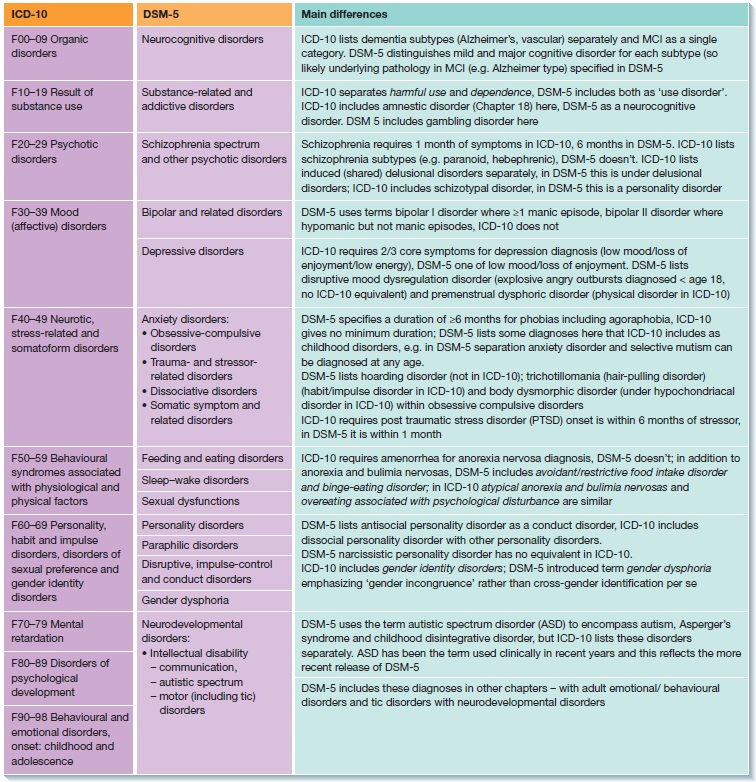 At first they themselves refuse to feel anything, and then they simply lose this ability and fall into a state of alexithymia.
At first they themselves refuse to feel anything, and then they simply lose this ability and fall into a state of alexithymia.
Break free from the spell of "normality"
Such people sometimes come to my clinic for help, mistaking their condition for depression. For example, a housewife came to me who told me that after graduating from university she got a job at a firm right away, but worked for only a year, because office work seemed boring to her. She then found a part-time job at a sadomasochistic (SM) club, a place she liked so much that she worked there for four years. Shortly before she turned thirty, she resigned from the club, judging that sooner or later she would have to do it anyway. Some time later, after an active search for a suitable party ( konkatsu ) she got married, had a baby, and began to lead a "normal" life as a housewife. And then she suddenly found that she spends most of the day in bed or in close proximity to it.
Her husband - a typical sissy, who also suffers from atopic dermatitis - quickly realized that his wife would not take care of him to the same extent as his mother did, and divorced her.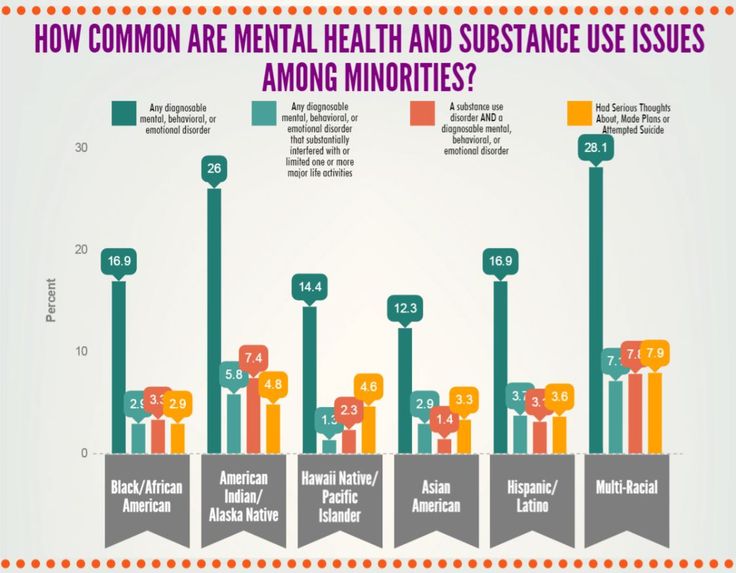 At the time of her visit to me, about a month had passed since the divorce.
At the time of her visit to me, about a month had passed since the divorce.
I think some of my colleagues would have diagnosed this patient with depression or adjustment disorder and would have given her antidepressants. But I noticed how strong her desire to be, or at least seem normal. It was it that made her suppress her individuality and doom herself to life in a world that causes nothing but boredom in her.
Everyday work in the SM club was fraught with danger, but at the same time excited her – the idea that she was working in a “non-standard”, “abnormal” job served as a strong source of emotional excitement. Thus, "normality" is just an illusion, an ideal that can be different for different people.
My patient says that she is already thirty-five, the figure is no longer the same, and that "what was in the past cannot be returned." I do not dispute this point of view. But whether she returns to work at the SM club or not, I think she needs to remember and rethink the strong, exciting feelings she experienced while working at a job she loved. My task is to return to this woman the ability to feel strong emotions, restoring her connection with her own eroticism. I have to convince her that she doesn't need to hide behind a mask of normality.
My task is to return to this woman the ability to feel strong emotions, restoring her connection with her own eroticism. I have to convince her that she doesn't need to hide behind a mask of normality.
Title picture: Design Pics/AFLO
(Japanese article published November 18, 2016)
Depersonalization: a syndrome that interferes with feeling - BBC News si
Subscribe to our ”Context” newsletter: it will help you understand the events.
Image caption,Sarah says that her illness makes familiar places look like scenery
For people with depersonalization syndrome, the world seems unreal, two-dimensional, as if in a fog. Every hundredth suffers from this disorder, but despite this, British doctors are not taught to work with such patients, experts say.
"The connections that you consider valuable lose their original meaning.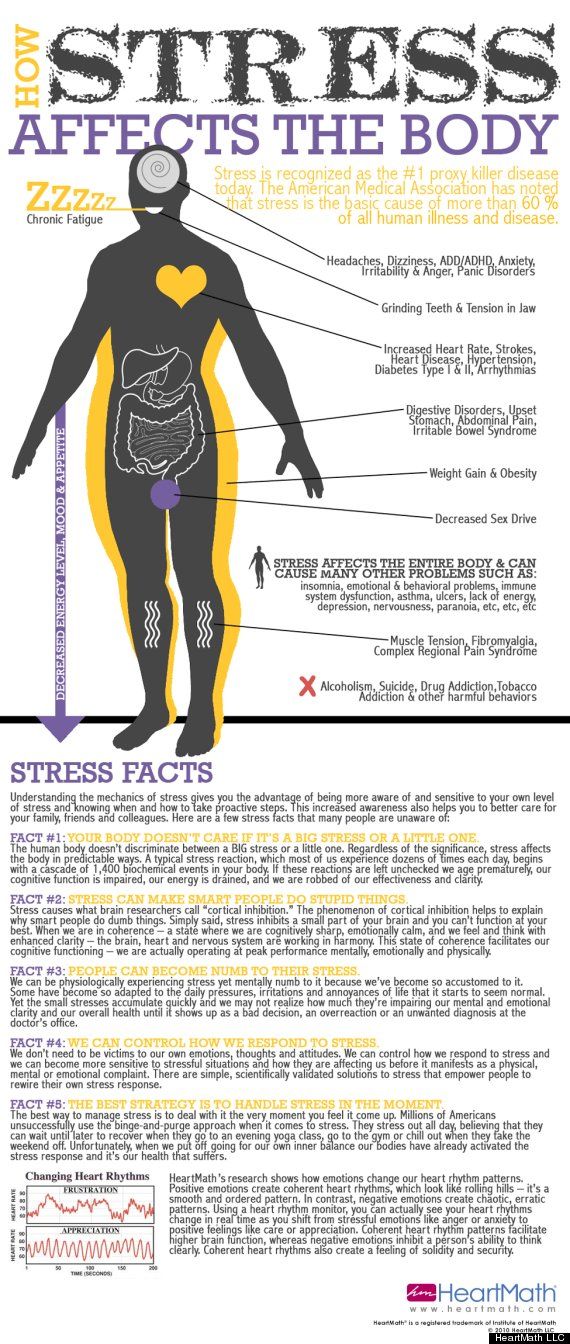 You know that you love your family. But the fact is that you are more aware of it with your mind than you feel," Sarah says on the Victoria Derbyshire program on Bee -bc.
You know that you love your family. But the fact is that you are more aware of it with your mind than you feel," Sarah says on the Victoria Derbyshire program on Bee -bc.
Sarah is an actress, she constantly tries on different images and reproduces other people's emotions. But in reality, for most of her conscious life, she is emotionally paralyzed and unable to experience any feelings.
The reason for this is a little-studied mental disorder called depersonalization.
Sarah had the syndrome three times. The first time it happened was when she was preparing for her final exams.
The main sign of depersonalization is the feeling that a person is losing physical connection with the world around him and his own body.
It is believed that this is how a defense mechanism manifests itself when, during stress or a serious shock, consciousness is disconnected from reality. Some drugs, such as marijuana, can cause the same effect.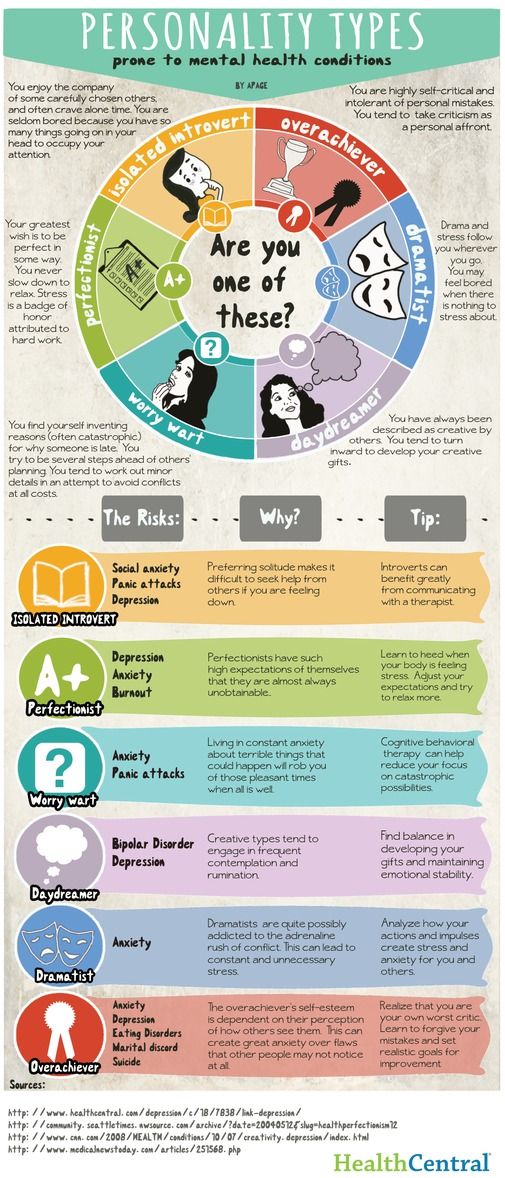
- Depression: a breakthrough in understanding the nature of the disease and its
- What your selfies can tell about you
- Google helps users recognize depression
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
For people with depersonalization syndrome, the world can change in a second.
"It was an unexpected switch. Everything around seemed alien and even intimidating. Suddenly, the apartment and other places where you used to be become a film set for you, and all your things become scenery," says Sarah.
Other patients report feeling that they are outside their body, that it does not belong to them, and that the world around them seems two-dimensional and flat.
This happened to Sarah during the second episode.
"I was reading, I had a book in my hands. And suddenly my hands began to look like a picture on which two hands were drawn. There was a feeling that the real world and my perception of it did not coincide."
Sarah's disorder is not uncommon. Three independent studies have proven that it occurs in one person out of a hundred.
Experts say the disorder has long been recognized as a medical condition. It is as common as obsessive-compulsive disorder or schizophrenia.
Some untreated patients may suffer lifelong depersonalization symptoms. And yet, not all doctors know what it is.
A doctor who recently graduated and suffers from this disorder himself stated that depersonalization was not taught in medical school or in continuing education courses for therapists.
He admitted that he had misdiagnosed his patients at least twice.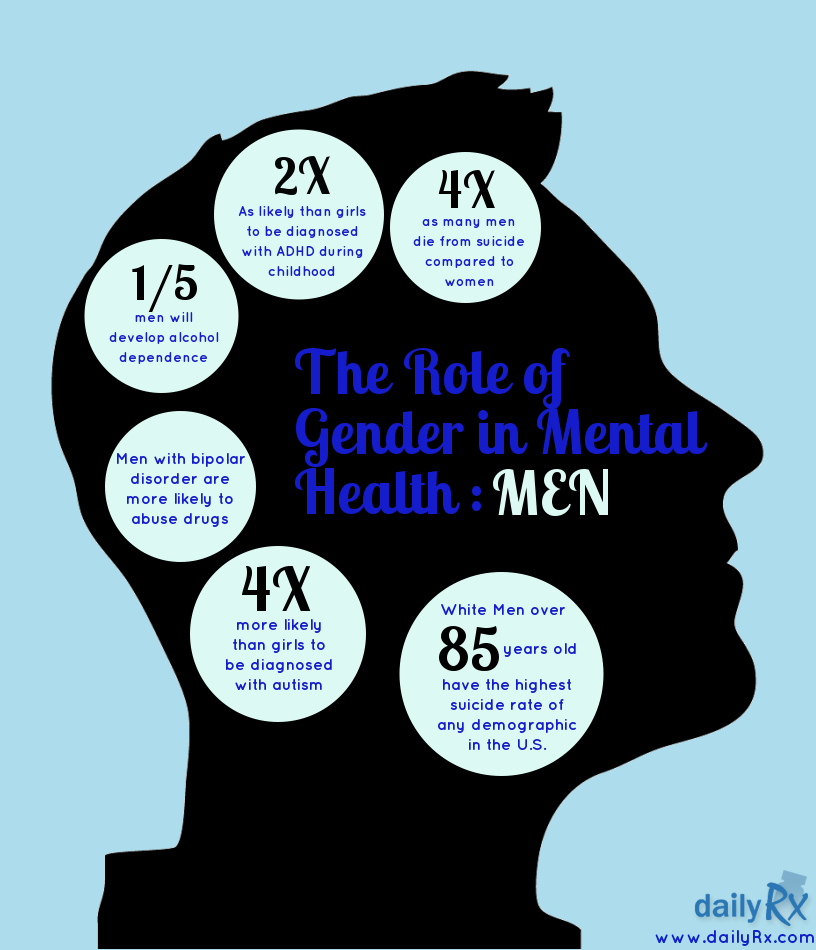 According to him, he will be very surprised if it turns out that at least one of his colleagues has heard about this syndrome.
According to him, he will be very surprised if it turns out that at least one of his colleagues has heard about this syndrome.
Sarah says that in her life she encountered at least 20 professionals who had no idea what she was talking about. Among them are consultants, therapists, district psychiatrists and doctors.
The Royal College of General Practitioners (RCGP) in London said that mental health was a key element of an expanded medical training course.
The Institute added that the study of more complex psychological problems is still in development.
The Royal College of Psychiatry stressed the need to make sure these disorders are properly understood.
Image caption,Dr. Elaine Hunter runs the only referral center in the UK that treats patients with depersonalization
Poor diagnosis is only part of the problem, access to treatment is another complication.
There is only one specialized clinic in the UK.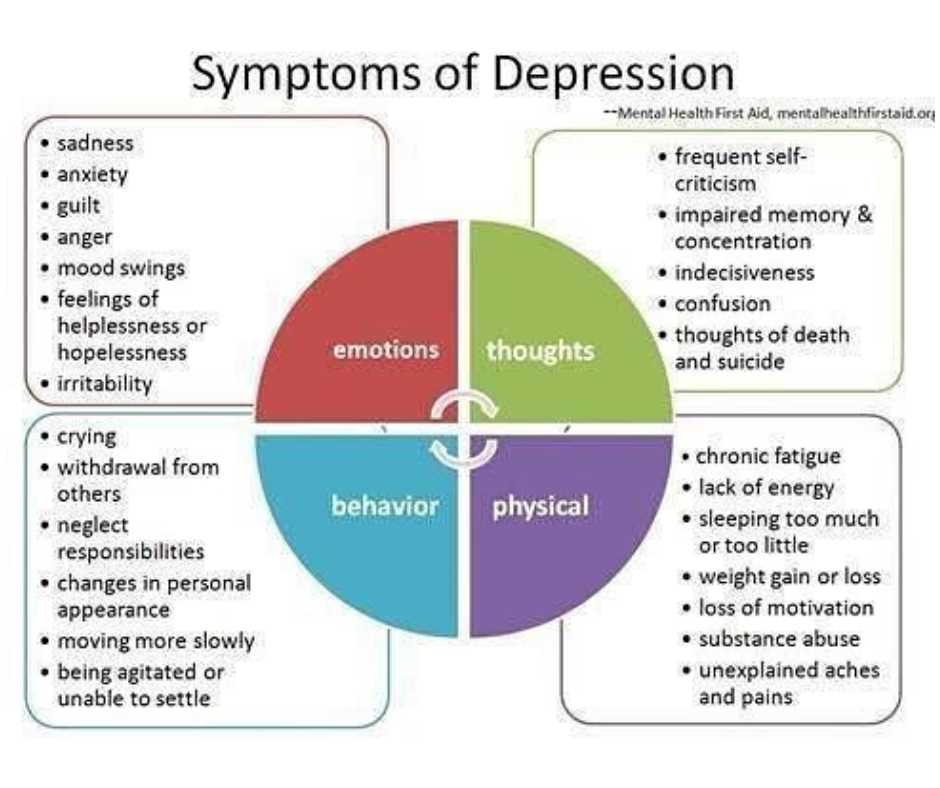 Its resources are limited, it can only accept 80 patients a year. Despite the fact that 650 thousand people can potentially suffer from this disease.
Its resources are limited, it can only accept 80 patients a year. Despite the fact that 650 thousand people can potentially suffer from this disease.
A referral from a local doctor is required to access this health center free of charge. And even if the patient is diagnosed with depersonalization, treatment will have to wait several months or longer.
After a year of waiting in line, Sarah decided that the only way out was to pay for the treatment herself.
"I used to have panic attacks all the time. It's really scary. I knew it was a crisis," she says.
A specialist center for patients with depersonalization syndrome operates at the Maudsley Hospital in south London. However, there are restrictions for patients under 18 years of age; the center only treats adults.
Often the disease occurs in adolescence. Dr. Elaine Hunter, who heads the center, is concerned that she has to withhold care for children and adolescents.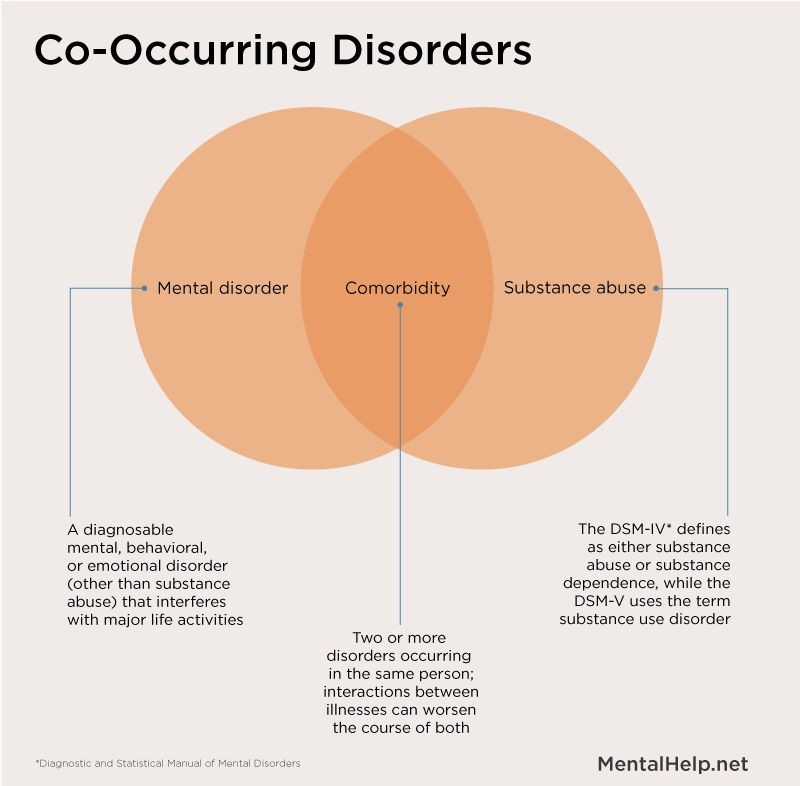
"Sometimes 15-year-old patients come to us deeply depressed and frightened, but we have nothing to offer them," she says.
One of the adult patients of the center developed the syndrome at the age of 13. For two years she could not leave the house, she experienced ten panic attacks a day caused by the disorder.
At the beginning of her treatment, she did not even recognize her own parents.
Dr. Hunter hopes that over time, the right treatment will be available to underage patients.
She believes that treatment should be organized in every district. Physicians in local centers for psychological assistance should undergo special training, then disseminate information among other specialists.
Image caption,Sarah Ashley couldn't eat or sleep until she was treated by Dr. Hunter
Hunter developed Cognitive Behavioral Therapy (CBT) specifically for patients with depersonalization.