Confronting borderline personality disorder
Communicating With Someone With Borderline Personality Disorder - OPI Residential Treatment Center for Young Adults
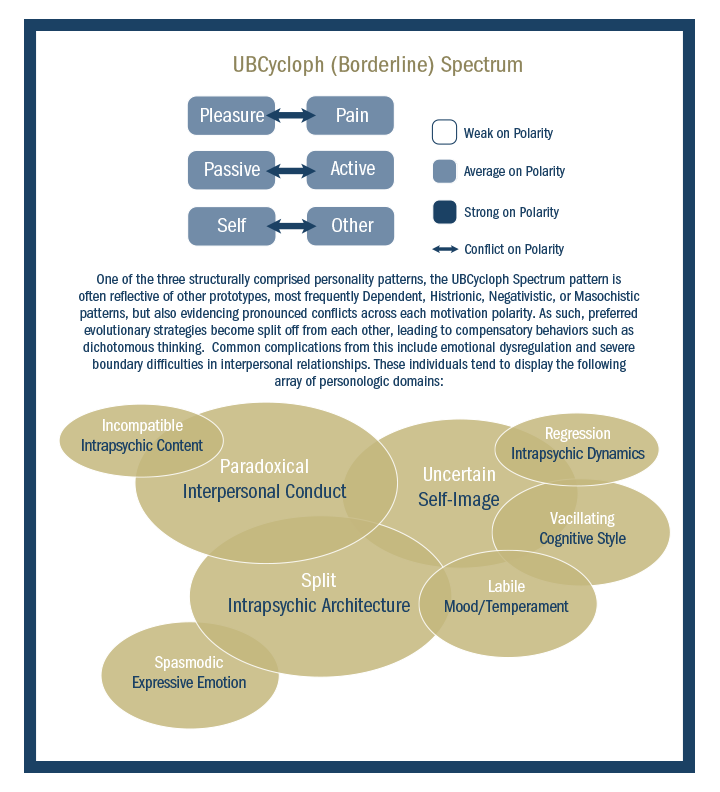
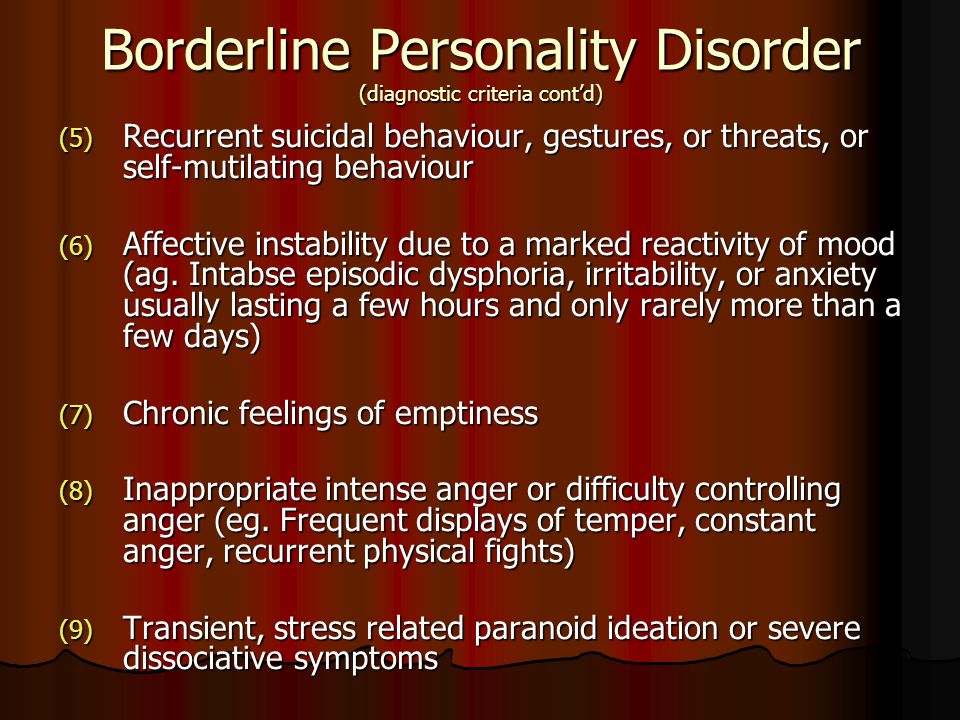
Borderline personality disorder, or BPD, can seem like a daunting and scary diagnosis. It is a mental disorder characterized by extreme mood swings, trouble with interpersonal relationships, a tendency toward impulsivity, intense fear of abandonment, and an unstable self-image.
Sufferers may demonstrate self-harming and risky behaviors, and the NIMH reports that 80 percent of those diagnosed with BPD exhibit suicidal behaviors as well. It is important to understand, however, that these behaviors are a symptom of the disorder and usually actual suicide is likely not the intent or the outcome.
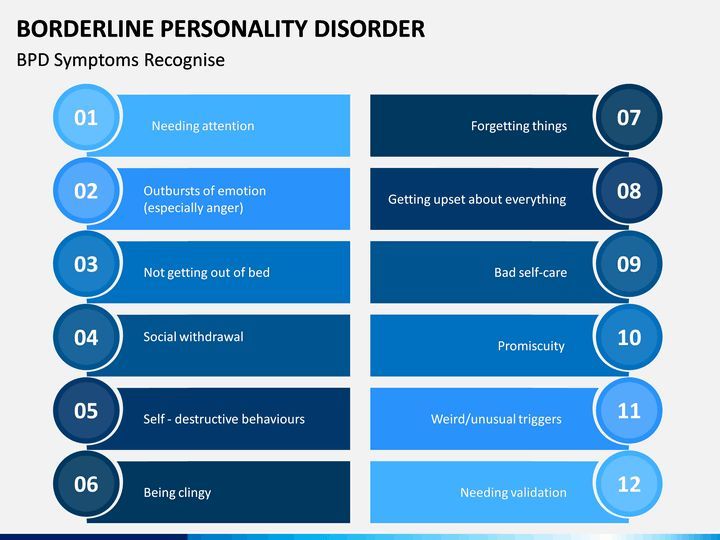
What to Expect When Someone Is Suffering From BPD
Understanding the signs and symptoms of borderline personality disorder is the first step in understanding how to manage and cope with the disorder, whether you or a loved one are affected. You can expect many if not all of the following symptoms:
- Impulsive conduct
- Risk-taking actions
- Self-mutilating behavior
- Suicidal actions or thoughts
- Intense euphoria
- Dejection and avoidance
- Reckless driving habits
- Impulsive and inappropriate spending
- Fear of separation, abandonment and rejection, real or perceived
- Clingy behavior
- Self-loathing
- Distorted self-image
- Eating disorders
- Chronic boredom
- Feelings of emptiness
- Depression
- Substance abuse
- Paranoia caused by stress
- Dissociative feelings
- Mood swings
- Trouble controlling bouts of intense anger
- Risky sexual behavior
A borderline personality diagnosis usually occurs in young adulthood and is reached when a pattern of these symptoms is observed over a period of time. The first step toward recovery is a diagnosis. If you are, or someone you love is, suffering from BPD, there are ways to get help.
How to Help
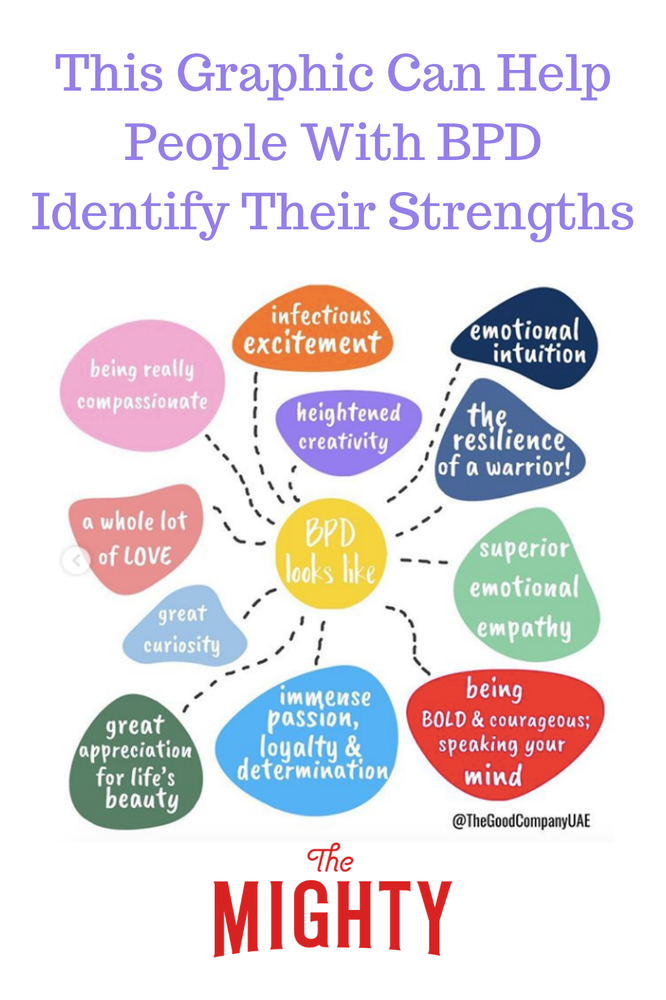
While a borderline personality disorder diagnosis may seem overwhelming, there are ways to manage and minimize symptoms, and there is even the possibility of reaching a full recovery. It is important to be understanding and patient and to know that while moods and feelings can be intense, they are not intended to be manipulative or destructive even if it may seem that way. Studies have shown that borderline personality disorder hinders a person’s ability to process negative emotions properly, and many turn this internally into anger and self-loathing.
If your loved one suffers from BPD, it is important to realize that they will have an intense fear of being rejected and abandoned, so much so that if you’re five minutes late or tell them of an upcoming vacation, it may be a trigger for their anger and withdrawal. While it may seem counterintuitive, one of the best ways to communicate with someone suffering from BPD may be to acknowledge their feelings before the facts of the situation.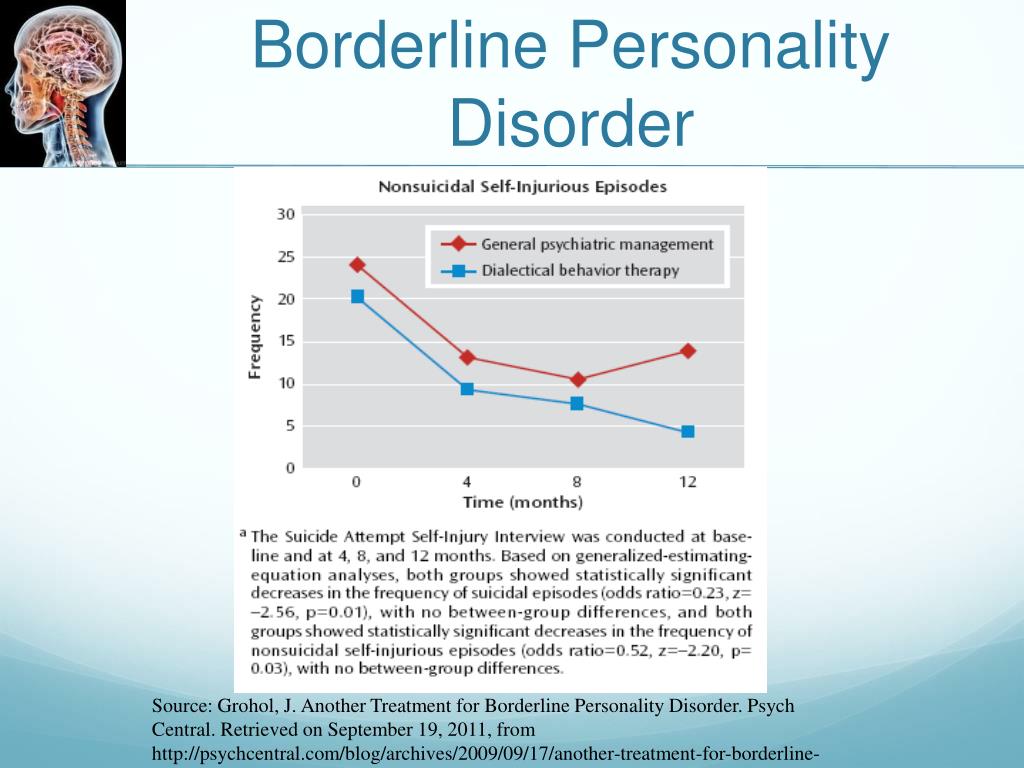 BPD causes intense moods and mood swings, and sufferers have trouble regulating their emotions. By verifying their feelings first, you may be able to diffuse a possible volatile situation.
BPD causes intense moods and mood swings, and sufferers have trouble regulating their emotions. By verifying their feelings first, you may be able to diffuse a possible volatile situation.
It is also important to avoid giving in to a BPD person’s impulsive acts. While there are extreme lows associated with BPD, there are also extreme highs, and it can be easy to get sucked in. Be careful and understand these highs are also a symptom and can plummet to a low very quickly. Here are a few basic pointers for communicating with someone with borderline personality disorder in a healthy and productive way:
- Be patient.
- Be realistic.
- Try to separate facts from feelings.
- Validate feelings first.
- Listen actively and be sympathetic.
- Seek to distract when emotions rise.
- Do not allow yourself to be the product of the intense anger; attempt to diffuse it but sometimes you may have to walk away.
- Understand the symptoms and triggers.
- Offer constructive criticism.
- Help to set realistic goals.
- Keep schedules consistent.
- Encourage treatment.
- Attend therapy together.
In managing BPD, remember to be consistent and predictable in your actions and reactions. Keep your word and also be honest. It is easy to go along with a tangent or rage about how awful someone or something is, but it is important to offer honest feedback since they may not even realize how their behavior is affecting others.
Do not take responsibility for their impulsive and irresponsible actions; do not try to save the situation or come to the rescue no matter how tempting it is. If they have wrecked their car, be supportive but encourage them to be responsible for their own actions. As difficult as it can be, keep your cool and don’t let arguments escalate.
Being aware of the triggers for an individual with borderline personality disorder can help to avoid them and the outbursts that accompany them. Understand you are not alone. The National Institute of Mental Health reports that one in four American adults suffer from a mental health disorder while 1.6 percent of Americans over 18 suffer from borderline personality disorder.
Understand you are not alone. The National Institute of Mental Health reports that one in four American adults suffer from a mental health disorder while 1.6 percent of Americans over 18 suffer from borderline personality disorder.
Helping Someone with Borderline Personality Disorder
BPD and relationships
People with borderline personality disorder (BPD) tend to have major difficulties with relationships, especially with those closest to them. Their wild mood swings, angry outbursts, chronic abandonment fears, and impulsive and irrational behaviors can leave loved ones feeling helpless, abused, and off balance. Partners and family members of people with BPD often describe the relationship as an emotional roller coaster with no end in sight. You may feel like you're at the mercy of your loved one's BPD symptoms—trapped unless you leave the relationship or the person takes steps to get treatment. But you have more power than you think.
You can change the relationship by managing your own reactions, establishing firm limits, and improving communication between you and your loved one. There's no magic cure but with the right treatment and support, many people with BPD can and do get better and their relationships can become more stable and rewarding. In fact, patients with the most support and stability at home tend to show improvements sooner than those whose relationships are more chaotic and insecure.
There's no magic cure but with the right treatment and support, many people with BPD can and do get better and their relationships can become more stable and rewarding. In fact, patients with the most support and stability at home tend to show improvements sooner than those whose relationships are more chaotic and insecure.
Whether it's your partner, parent, child, sibling, friend, or other loved one with BPD, you can improve both the relationship and your own quality of life, even if the person with BPD isn't ready to acknowledge the problem or seek treatment.
Learning all you can
If your loved one has borderline personality disorder, it's important to recognize that he or she is suffering. The destructive and hurtful behaviors are a reaction to deep emotional pain. In other words, they're not about you. When your loved one does or says something hurtful towards you, understand that the behavior is motivated by the desire to stop the pain they are experiencing; it's rarely deliberate.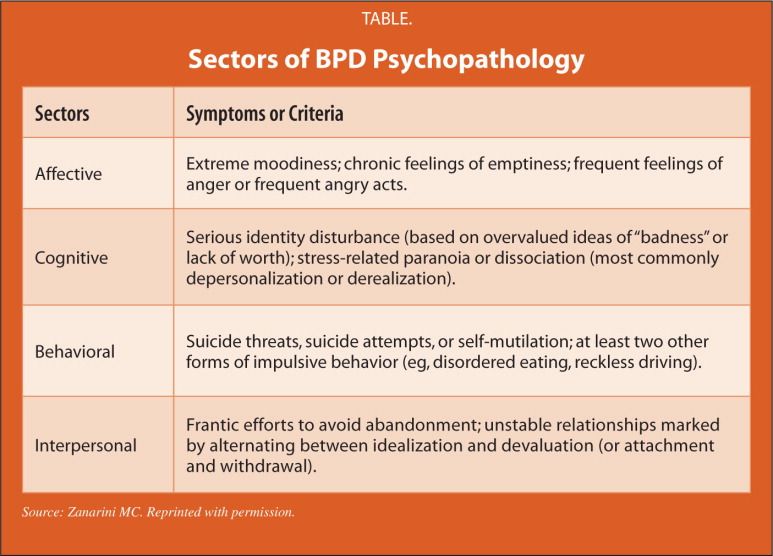
Learning about BPD won't automatically solve your relationship problems, but it will help you understand what you're dealing with and handle difficulties in more constructive ways.
Speak to a Licensed Therapist
The world's largest therapy service. 100% online. Get matched with a professional, licensed, and vetted therapist in less than 48 hours.
Get 20% off
Affiliate Disclosure
Recognizing the signs and symptoms of BPD
Recognizing the signs and symptoms of borderline personality disorder is not always easy. BPD is rarely diagnosed on its own, but often in conjunction with co-occurring disorders such as depression, bipolar disorder, anxiety, an eating disorder, or substance abuse. Your family member or loved one with BPD may be extremely sensitive, so small things can often trigger intense reactions.
Once upset, borderline people are often unable to think straight or calm themselves in a healthy way.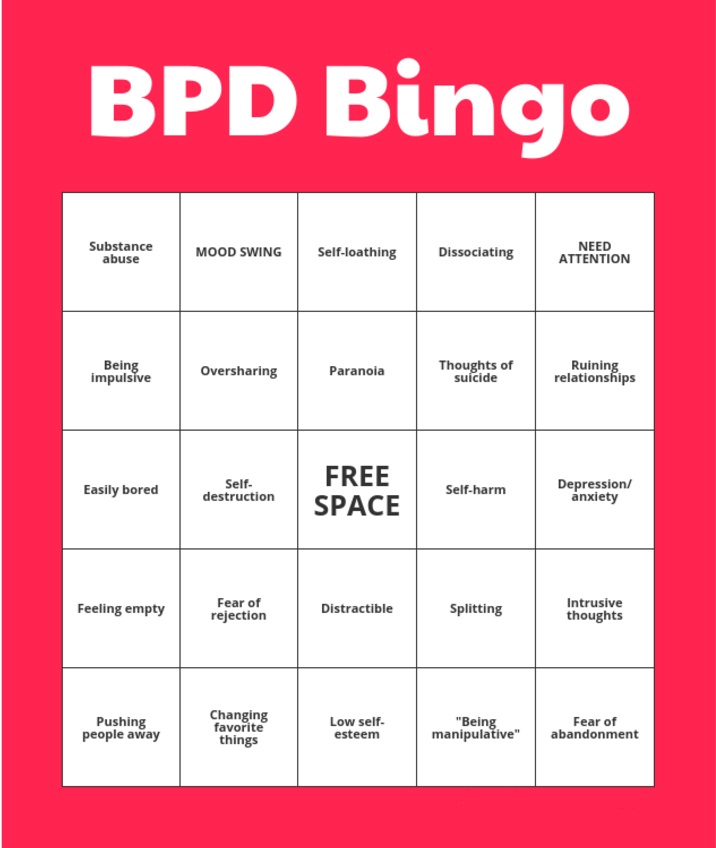 They may say hurtful things or act out in dangerous or inappropriate ways. This emotional volatility can cause turmoil in their relationships and stress for family members, partners, and friends.
They may say hurtful things or act out in dangerous or inappropriate ways. This emotional volatility can cause turmoil in their relationships and stress for family members, partners, and friends.
Many people in a close relationship with someone who suffers from BPD often know that there’s something wrong with their loved one, but have no idea what it is or if there is even a name for it. Learning a diagnosis of borderline personality disorder can come as a source of both relief and hope.
Does your loved one have borderline personality disorder?
In your relationship:
- Do you feel like you have to tiptoe around your loved one, watching every little thing you say or do for fear of setting them off? Do you often hide what you think or feel in order to avoid fights and hurt feelings?
- Does your loved one shift almost instantaneously between emotional extremes? For example, are they calm one moment, raging the next, then suddenly despondent? Are these rapid mood swings unpredictable and seemingly irrational?
- Does your loved one tend to view you as all good or bad, with no middle ground? For example, either you're “perfect,” and the only one they can count on, or you're “selfish” and “unfeeling” and never truly loved them.
- Do you feel like you can't win: that anything you say or do will be twisted and used against you? Does it feel as if your loved one's expectations are constantly changing, so you're never sure how to keep the peace?
- Is everything always your fault? Do you feel constantly criticized and blamed for things that don't even make sense? Does the person accuse you of doing and saying things you never did? Do you feel misunderstood whenever you try to explain or reassure your partner?
- Do you feel manipulated by fear, guilt, or outrageous behavior? Does your loved one make threats, fly into violent rages, make dramatic declarations, or do dangerous things when they think you're unhappy or may leave?
If you answer “yes” to most of these questions, your partner or family member might have borderline personality disorder.
[Read: Borderline Personality Disorder Test]
To help someone with BPD, first take care of yourself
When a family member or partner has borderline personality disorder, it's all too easy to get caught up in heroic efforts to please and appease him or her.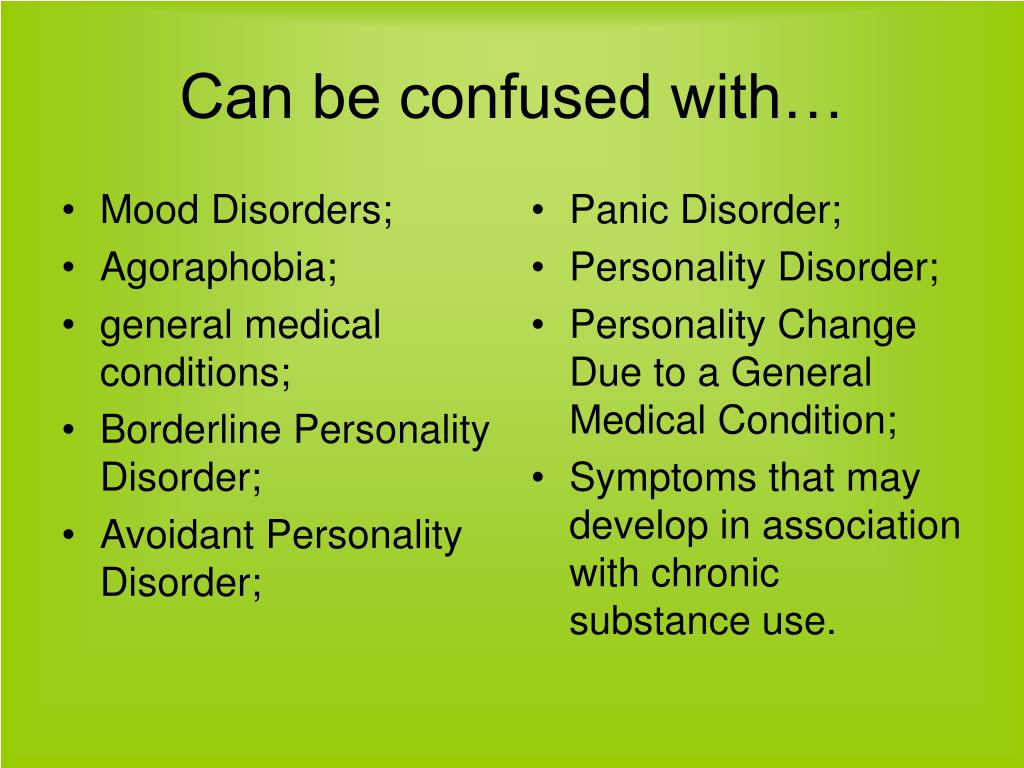 You may find yourself putting most of your energy into the person with BPD at the expense of your own emotional needs. But this is a recipe for resentment, depression, burnout, and even physical illness.
You may find yourself putting most of your energy into the person with BPD at the expense of your own emotional needs. But this is a recipe for resentment, depression, burnout, and even physical illness.
You can't help someone else or enjoy sustainable, satisfying relationships when you're run down and overwhelmed by stress. As in the event of an in-flight emergency, you must “put on your own oxygen mask first.”
Avoid the temptation to isolate. Make it a priority to stay in touch with family and friends who make you feel good. You need the support of people who will listen to you, make you feel cared for, and offer reality checks when needed.
You're allowed (and encouraged) to have a life! Give yourself permission to have a life outside of your relationship with the person with BPD. It's not selfish to carve out time for yourself to relax and have fun. In fact, when you return to your BPD relationship, you'll both benefit from your improved perspective.
Join a support group for BPD family members. Meeting with others who understand what you're going through can go a long way. If you can't find an in-person support group in your area, you may want to consider joining an online BPD community.
Don't neglect your physical health. Eating healthfully, exercising, and getting quality sleep can easily fall by the wayside when you're caught up in relationship drama. Try to avoid this pitfall. When you're healthy and well rested, you're better able to handle stress and control your own emotions and behaviors.
Learn to manage stress. Getting anxious or upset in response to problem behavior will only increase your loved one's anger or agitation. By practicing with sensory input, you can learn to relieve stress as it's happening and stay calm and relaxed when the pressure builds.
Remember the 3 C's rule
Many friends or family members often feel guilty and blame themselves for the destructive behavior of the borderline person. You may question what you did to make the person so angry, think you somehow deserve the abuse, or feel responsible for any failure or relapse in treatment.
You may question what you did to make the person so angry, think you somehow deserve the abuse, or feel responsible for any failure or relapse in treatment.
But it's important to remember that you're not responsible for another person. The person with BPD is responsible for their own actions and behaviors.
The 3 C's are:
- I didn't cause it.
- I can't cure it.
- I can't control it.
Source: Out of the Fog
Communicating with someone who has BPD
Communication is a key part of any relationship but communicating with a borderline person can be especially challenging. People in a close relationship with a borderline adult often liken talking with their loved one to arguing with a small child. People with BPD have trouble reading body language or understanding the nonverbal content of a conversation. They may say things that are cruel, unfair, or irrational.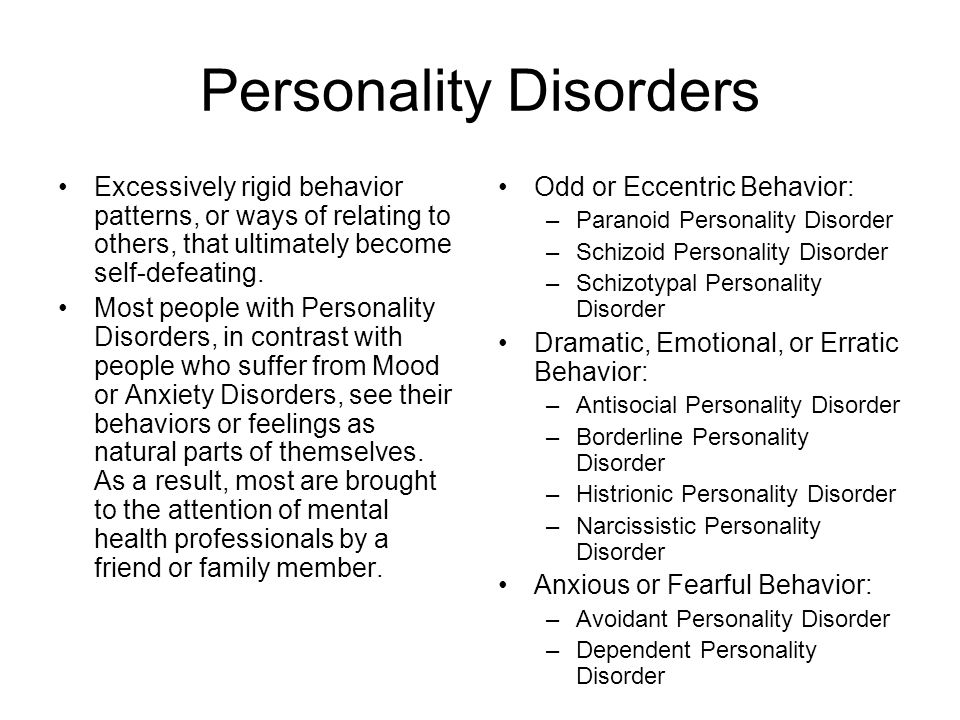 Their fear of abandonment can cause them to overreact to any perceived slight, no matter how small, and their aggression can result in impulsive fits of rage, verbal abuse, or even violence.
Their fear of abandonment can cause them to overreact to any perceived slight, no matter how small, and their aggression can result in impulsive fits of rage, verbal abuse, or even violence.
The problem for people with BPD is that the disorder distorts both the messages they hear and those they try to express. BPD expert and author, Randi Kreger, likens it to “having ‘aural dyslexia,' in which they hear words and sentences backwards, inside out, sideways, and devoid of context.”
Listening to your loved one and acknowledging their feelings is one of the best ways to help someone with BPD calm down. When you appreciate how a borderline person hears you and adjust how you communicate with them, you can help diffuse the attacks and rages and build a stronger, closer relationship.
Communication tips
It's important to recognize when it's safe to start a conversation. If your loved one is raging, verbally abusive, or making physical threats, now is not the time to talk. Better to calmly postpone the conversation by saying something like, “Let's talk later when we're both calm. I want to give you my full attention but that's too hard for me to do right now.”
Better to calmly postpone the conversation by saying something like, “Let's talk later when we're both calm. I want to give you my full attention but that's too hard for me to do right now.”
When things are calmer:
Listen actively and be sympathetic. Avoid distractions such as the TV, computer, or cell phone. Try not to interrupt or redirect the conversation to your concerns. Set aside your judgment, withhold blame and criticism, and show your interest in what's being said by nodding occasionally or making small verbal comments like “yes” or “uh huh.” You don't have to agree with what the person is saying to make it clear that you're listening and sympathetic.
Focus on the emotions, not the words. The feelings of the person with BPD communicate much more than what the words he or she is using. People with BPD need validation and acknowledgement of the pain they're struggling with. Listen to the emotion your loved one is trying to communicate without getting bogged down in attempting to reconcile the words being used.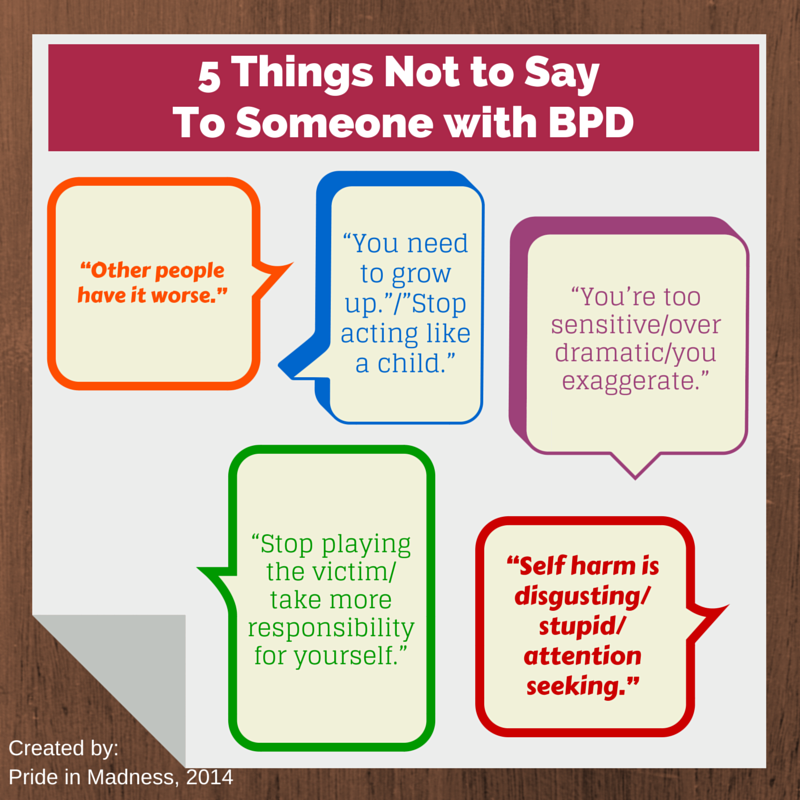
Try to make the person with BPD feel heard. Don't point out how you feel that they're wrong, try to win the argument, or invalidate their feelings, even when what they're saying is totally irrational.
Do your best to stay calm, even when the person with BPD is acting out. Avoid getting defensive in the face of accusations and criticisms, no matter how unfair you feel they are. Defending yourself will only make your loved one angrier. Walk away if you need to give yourself time and space to cool down.
Seek to distract your loved one when emotions rise. Anything that draws your loved one's attention can work, but distraction is most effective when the activity is also soothing. Try exercising, sipping hot tea, listening to music, grooming a pet, painting, gardening, or completing household chores.
Talk about things other than the disorder. You and your loved one's lives aren't solely defined by the disorder, so make the time to explore and discuss other interests.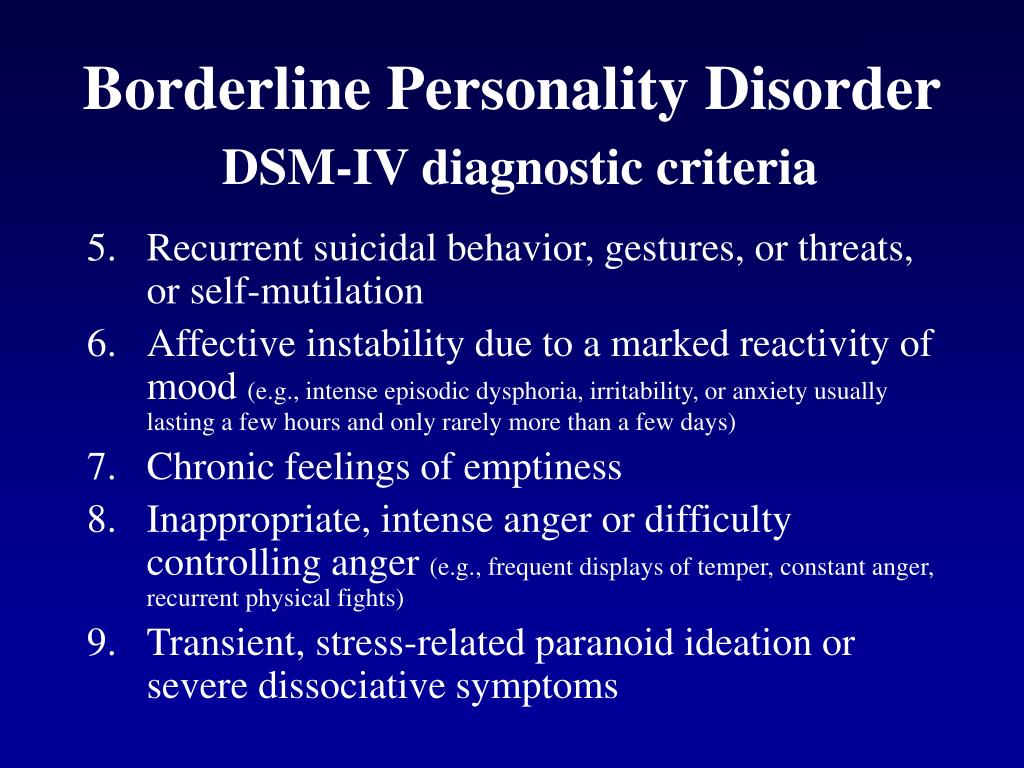 Discussions about light subjects can help to diffuse the conflict between you and may encourage your loved one to discover new interests or resume old hobbies.
Discussions about light subjects can help to diffuse the conflict between you and may encourage your loved one to discover new interests or resume old hobbies.
Setting healthy boundaries with a borderline loved one
One of the most effective ways to help a loved one with BPD gain control over their behavior is to set and enforce healthy limits or boundaries. Setting limits can help your loved one better handle the demands of the outside world, where schools, work, and the legal system, for example, all set and enforce strict limits on what constitutes acceptable behavior.
Establishing boundaries in your relationship can replace the chaos and instability of your current situation with an important sense of structure and provide you with more choices about how to react when confronted by negative behavior. When both parties honor the boundaries, you'll be able to build a sense of trust and respect between you, which are key ingredients for any meaningful relationship.
Setting boundaries is not a magic fix for a relationship, though. In fact, things may initially get worse before they get better. The person with BPD fears rejection and is sensitive to any perceived slight. This means that if you've never set boundaries in your relationship before, your loved one is likely to react badly when you start. If you back down in the face of your loved one's rage or abuse, you'll only be reinforcing their negative behavior and the cycle will continue. But, remaining firm and standing by your decisions can be empowering to you, benefit your loved one, and ultimately transform your relationship.
How to set and reinforce healthy boundaries
Talk to your loved one about boundaries at a time when you're both calm, not in the heat of an argument. Decide what behavior you will and will not tolerate from the person and make those expectations clear. For example, you may tell your loved one, “If you can't talk to me without screaming abuse at me, I will walk out. ”
”
Do…
- Calmly reassure the person with BPD when setting limits. Say something like, “I love you and I want our relationship to work, but I can't handle the stress caused by your behavior. I need you to make this change for me.”
- Make sure everyone in the family agrees on the boundaries—and how to enforce the consequences if they're ignored.
- Think of setting boundaries as a process rather than a single event. Instead of hitting your loved one with a long list of boundaries all at once, introduce them gradually, one or two at a time.
Don't…
- Make threats and ultimatums that you can't carry out. As is human nature, your loved one will inevitably test the limits you set. If you relent and don't enforce the consequences, your loved one will know the boundary is meaningless and the negative behavior will continue. Ultimatums are a last resort (and again, you must be prepared to follow through).
- Tolerate abusive behavior.
 No one should have to put up with verbal abuse or physical violence. Just because your loved one's behavior is the result of a personality disorder, it doesn't make the behavior any less real or any less damaging to you or other family members.
No one should have to put up with verbal abuse or physical violence. Just because your loved one's behavior is the result of a personality disorder, it doesn't make the behavior any less real or any less damaging to you or other family members. - Enable the person with BPD by protecting them from the consequences of their actions. If your loved one won't respect your boundaries and continues to make you feel unsafe, then you may need to leave. It doesn't mean you don't love them, but your self-care should always take priority.
Supporting your loved one's BPD treatment
Borderline personality disorder is highly treatable, yet it's common for people with BPD to avoid treatment or deny that they have a problem. Even if this is the case with your loved one, you can still offer support, improve communication, and set boundaries while continuing to encourage your friend or family member to seek professional help.
While medication options are limited, the guidance of a qualified therapist can make a huge difference to your loved one's recovery. BPD therapies, such as Dialectical Behavior Therapy (DBT) and schema-focused therapy, can help your loved one work through their relationship and trust issues and explore new coping techniques. In therapy, they can learn how to calm the emotional storm and self-soothe in healthy ways.
BPD therapies, such as Dialectical Behavior Therapy (DBT) and schema-focused therapy, can help your loved one work through their relationship and trust issues and explore new coping techniques. In therapy, they can learn how to calm the emotional storm and self-soothe in healthy ways.
How to support treatment
If your loved one won't acknowledge that they have a problem with BPD, you may want to consider couple's therapy. Here, the focus is on the relationship and promoting better communication, rather than on your loved one's disorder. Your partner may more readily agree to this and eventually consider pursuing BPD therapy in the future.
Encourage your loved one to explore healthy ways of handling stress and emotions by practicing mindfulness and employing relaxation techniques such as yoga, deep breathing, or meditation. Sensory-based stimulation can also help them to relieve stress in the moment. Again, you can participate in any of these therapies with your loved one, which can strengthen your bond and may encourage them to pursue other avenues of treatment as well.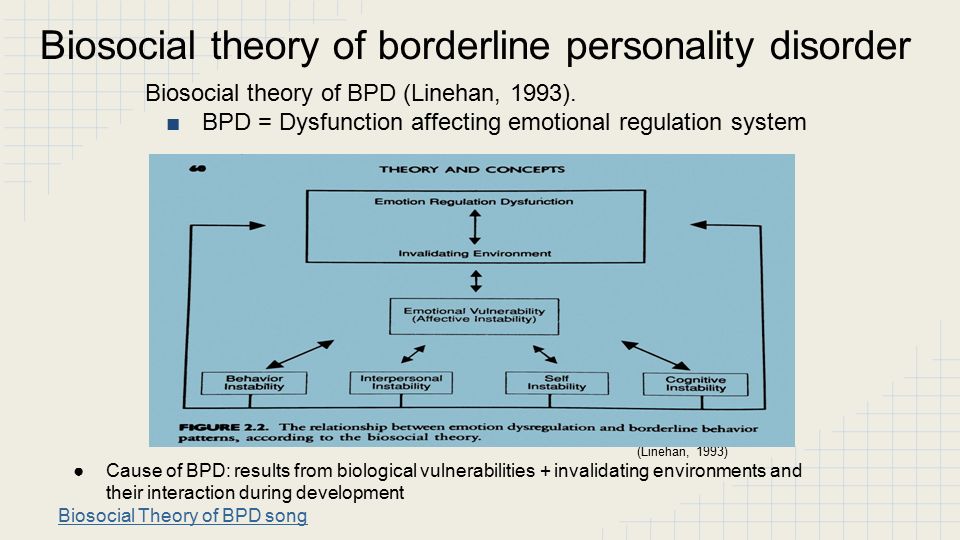
By developing an ability to tolerate distress, your loved one can learn how to press pause when the urge to act out or behave impulsively strikes. HelpGuide's free Emotional Intelligence Toolkit offers a step-by-step, self-guided program to teach your loved one how to ride the “wild horse” of overwhelming feelings while staying calm and focused.
Setting goals for BPD recovery: Go slowly
When supporting your loved one's recovery, it's important to be patient and set realistic goals. Change can and does happen but, as with reversing any kind of behavior pattern, it takes time.
- Take baby steps rather than aiming for huge, unattainable goals that set you and your loved one up for failure and discouragement. By lowering expectations and setting small goals to be achieved step by step, you and your loved one have a greater chance of success.
- Supporting your loved one's recovery can be both extremely challenging and rewarding. You need to take care of yourself, but the process can help you grow as an individual and strengthen the relationship between you.
Helplines and support
- In the U.S.
Call the NAMI HelpLine at 1-800-950-6264
- UK
Call the the Mind infoline at 0300 123 3393
- Australia
Call the Sane Helpline at 1800 187 263
- Canada
Find Your CMHA for a helpline near you
- India
Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated or reviewed on February 23, 2023
Help for people with borderline personality disorder //Psychological newspaper
Psychologists and psychotherapists are often approached by people who, in the process of psychodiagnostics and initial interviews, have borderline personality disorder or "emotionally unstable personality disorder" according to ICD-10.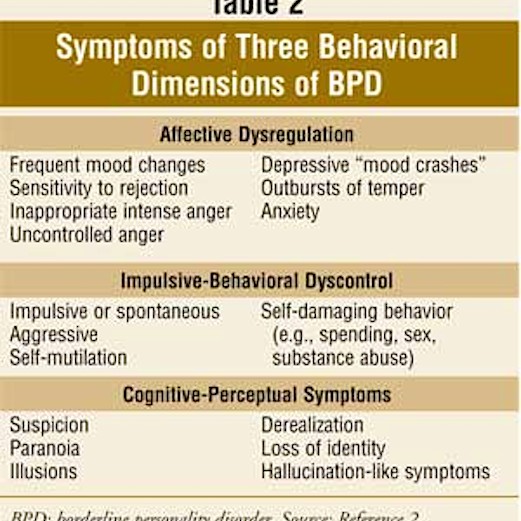 What are its signs? How is life for people with page personality disorder? What do experts think about healing? What self-help techniques can people with BPD use in difficult situations? I will talk about this in the article.
What are its signs? How is life for people with page personality disorder? What do experts think about healing? What self-help techniques can people with BPD use in difficult situations? I will talk about this in the article.
Borderline personality disorder (BPD) is a group of personality disorders characterized by self-injurious behavior and difficulties in interpersonal relationships. Some people characterize BPD as "the apocalypse."
I highlight such signs of BPD as: constant anxiety, people with BPD may be anxious because of the crises that accompany their lives, changing events. Often there is an alarming suspiciousness in connection with the state of health. Anxiety leads to psychosomatic illnesses, which reinforces the "vicious circle" - going to the doctors. Anxiety is associated with fear in the lives of people with BPD. A lot of things can scare them, these are new relationships, and intimacy, and parting, and other situations. Numerous spheres of life of people with BPD are “saturated” with fear, as in children aged 3-5 years, who are prone to various fears and anxieties.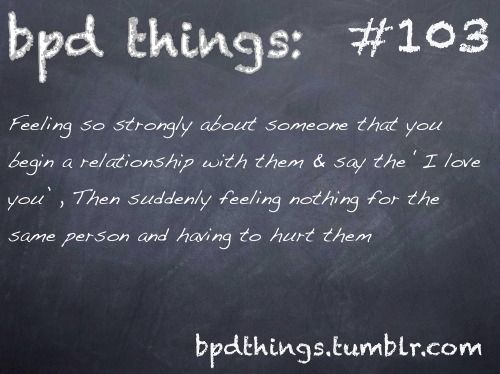 Especially fear and suspicion can increase in situations of stress. People with BPD have low self-esteem. It is as if a constant critic, distinguished by self-criticism, “sits” inside, and self-doubt and doubts are born from this.
Especially fear and suspicion can increase in situations of stress. People with BPD have low self-esteem. It is as if a constant critic, distinguished by self-criticism, “sits” inside, and self-doubt and doubts are born from this.
It is worth noting that it is difficult for people with BPD to answer the question: “who am I?”, “What do I want?”, The so-called diffuse identity manifests itself, where there are no strong goals, values and beliefs. When there is a series of events associated with parting with a loved one, with failures in work or in the sphere of relationships with others, which is typical for people with BPD due to emotional instability, emotional or mental pain arises - it resembles an uncomfortable feeling inside, close to despair. People with BPD may have problems controlling their emotions, which manifests itself in uncontrollable anger and anger, chronic conflicts with others. It is very difficult for them to be in a relationship with one partner for a long time, therefore, changes often occur in relationships, even some chaos, the search for more and more new partners.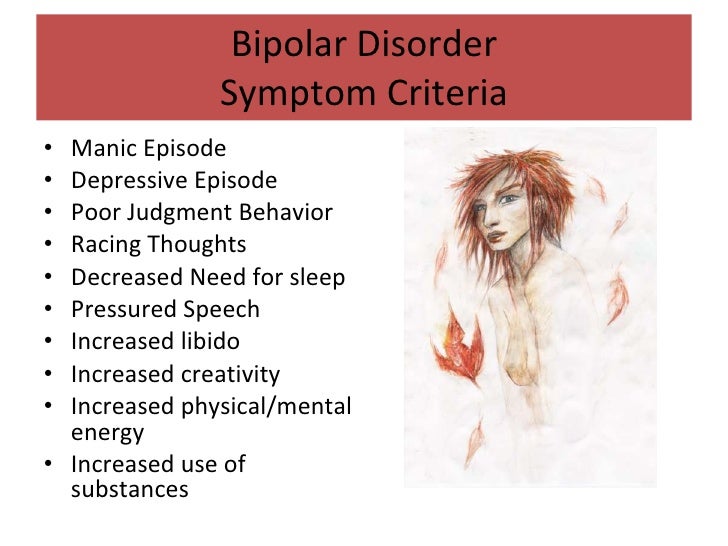
People with BPD tend to change jobs frequently. The work book is literally teeming with notes about various organizations in which I had to work. As a result, they may face certain difficulties in finding employment in the future. The litmus test for BPD in people's behavior is self-harm and suicide. At the same time, self-harm can manifest itself in different ways, from suicidal attempts to masochistic tendencies in behavior, when people with BPD want the other person to scold, offend, hurt. For some people with BPD, various kinds of addictions are characteristic, for example, alcoholism, drug addiction, gambling, Internet addiction. People with BPD are characterized by unreasonable spending of money, risky driving, and promiscuity. Often, after traumatic events, there may be problems with sleep, nightmares, obsessive thoughts about unpleasant situations, memories that disturb and do not allow you to live in peace. In general, the signs of BPD are characterized by polymorphism, and behavioral patterns - by a variety of manifestations.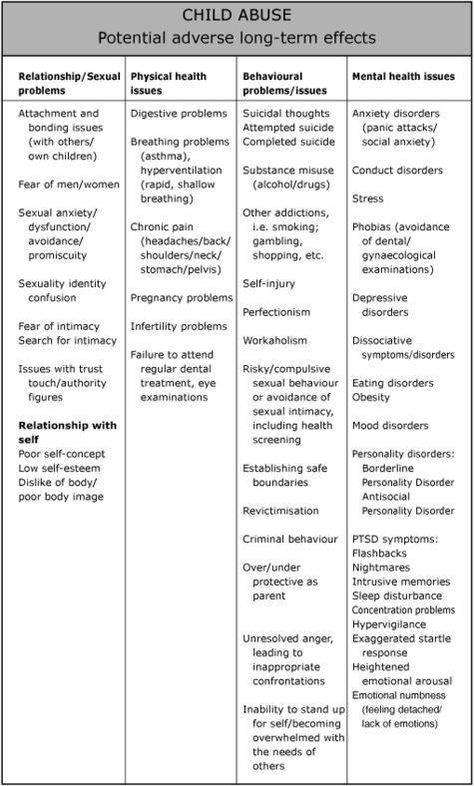
You can describe borderline personality disorder with the word: INSTABILITY, where:
N - hate. People with BPD are characterized by a feeling of hatred as a long, intense, negative feeling, reflecting disgust, hostility, rejection of someone.
E - Yeralash. Characterized by disorder, confusion, confusion. Chaotic interpersonal, incl. intimate relationships, lack of structure.
C - Self harm. Among people with BPD, there are suicide attempts, cutting, poisoning, self-harm with the help of other people in interpersonal relationships, self-infliction of pain.
T - Spending. Unreasonable spending of money on unnecessary purchases, unreasonable expenditure of effort.
A - Ambivalence. Opposite feelings in a short amount of time. For example, love and hate.
B - Pain. Characterized by mental pain with repeated unsuccessful attempts, for example, in building interpersonal relationships, employment, etc.
I - Idealization. The tendency to idealize other people and depreciate them after a short period of time.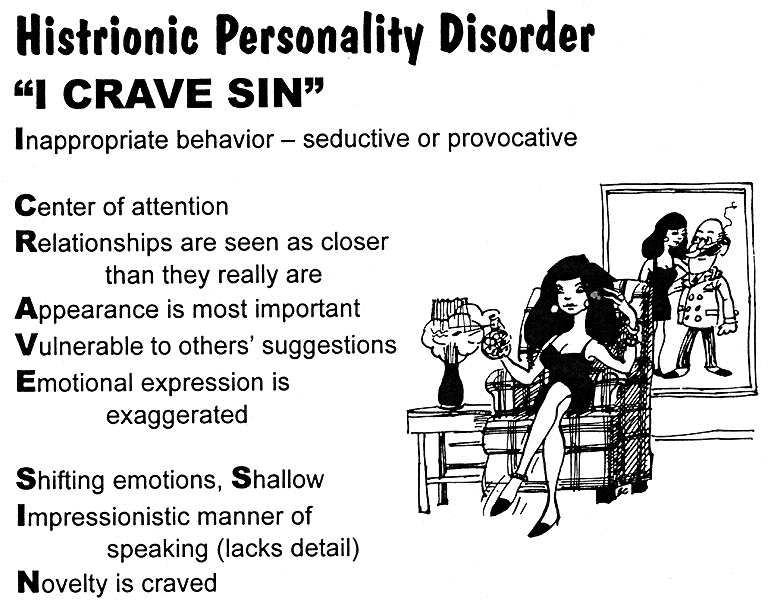
L - Lie. People with BPD are prone to deceit, lies, embellishment of reality.
N - Troubles. People with BPD often find themselves in conflict situations, quarrels, unfriendly relationships.
Oh - emptiness. People with BPD often feel empty inside, lack of interest.
S - Boredom. A feeling of boredom, a decrease in activity, a lack of prolonged interest in any activity, the world around and other people are characteristic.
T - Branding, branding. They often brand themselves. After hospitalization in a hospital, they feel the stigma of the mentally ill, acutely experience such a state, and isolate themselves.
INSTABILITY characterizes the lives of people with BPD, these are interpersonal relationships, and situations related to employment, and mood, and behavior in general.
Expert opinions on borderline personality disorder
Anton Yezhov, PhD in Psychiatry. Institute of Neurology, Psychiatry and Narcology of the Academy of Sciences of Ukraine, Kharkiv, full member of the Russian Psychotherapeutic Association, certified and accredited by the Moscow Gestalt Institute (according to the standards of the European Association of Gestalt Therapists).
- Anton Vladimirovich, what is borderline personality disorder?
- In ICD-10: F60.3 it is “Emotionally labile personality disorder. Impulsive and borderline type. With borderline character disorder ( BPD), patients generally test reality, however, during diagnosis, there may be a slight distortion in the description of events occurring with the patient, as a result of a poorly developed ability for reflection, mentalization, the impact of strong affects and primitive defenses on cognitive processes. In some cases, there may be quasi-psychotic episodes in the form of short paranoid reactions, usually provoked by any dual and uncertain situation, as well as episodes of dissociation. But, as a rule, all these phenomena do not develop into stable delusional and hallucinatory symptoms. Patients with PPH also have a rather high suicidal risk, but the main motive is most often a demonstrative protest, jealousy, a desire to “punish” a partner and make him feel guilty. In PPH, rage, hatred, resentment dominate in suicidal behavior. Auto-aggressive actions are usually performed impulsively, at the peak of affect, often in a demonstrative style.
In PPH, rage, hatred, resentment dominate in suicidal behavior. Auto-aggressive actions are usually performed impulsively, at the peak of affect, often in a demonstrative style.
- How can BPD be corrected?
- In the therapy of CPH, the pathogenetic is long-term psychotherapy focused on the client-therapeutic relationship - this is the main type of treatment! Pharmacotherapy acts as a maintenance therapy. Drugs in the treatment of BPH include selective serotonin reuptake inhibitors, low dose antipsychotics, and mood stabilizers. The general approach in the pharmacotherapy of BPH is to reduce the unnecessary use of medications (!), medicating the target symptoms with an understanding of pharmacodynamics.
Irina Mlodik, Ph.D. in Psychology, psychologist, Gestalt therapist, existential psychotherapist, author of books and articles on child and adult practical psychology, author's training courses.
- Irina Yurievna, please tell me, is it possible to recover from borderline personality disorder?
- About the treatment: it's hard to say.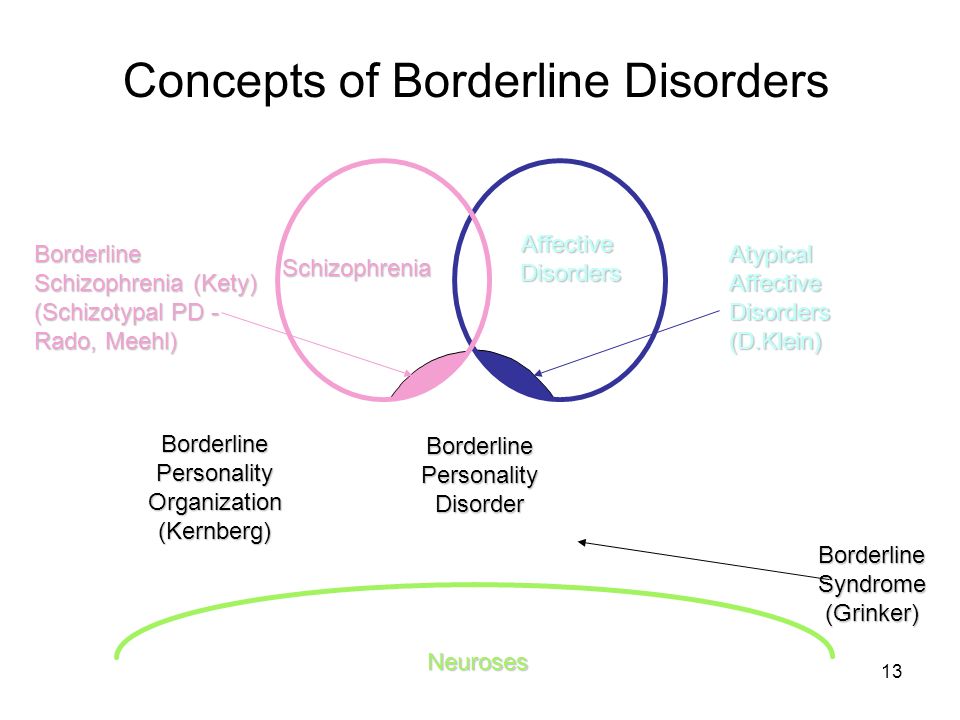 I do not have a psychiatric, not a medical position on this matter. I believe that in each of us there can be a borderline arranged and borderline functioning part. In that sense, there's no cure for the way you're made. One can only reduce the consequences of border effects. Including and mainly with the help of high-quality and long-term, for example, humanistically oriented or analytical psychotherapy. Long-term and regular therapy creates a special type of relationship with the therapist, which allows, being in high-quality and constant contact: to live through many difficult and not processed by the psyche affects from childhood, to create and maintain with the help of therapeutic contact an important, permanent, uninterrupted connection with the therapist (which there was almost certainly no person with BPD), who becomes an important “adult” in the life of a “border guard” who can be relied upon. Subsequently, from relying on the connection and the figure of the therapist, inside and the person with BPD, other relationships grow both inside themselves (to their internal objects) and outside, they have the opportunity to maintain closeness not only with the therapist, but also with other people and build with them a long-term relationship.
I do not have a psychiatric, not a medical position on this matter. I believe that in each of us there can be a borderline arranged and borderline functioning part. In that sense, there's no cure for the way you're made. One can only reduce the consequences of border effects. Including and mainly with the help of high-quality and long-term, for example, humanistically oriented or analytical psychotherapy. Long-term and regular therapy creates a special type of relationship with the therapist, which allows, being in high-quality and constant contact: to live through many difficult and not processed by the psyche affects from childhood, to create and maintain with the help of therapeutic contact an important, permanent, uninterrupted connection with the therapist (which there was almost certainly no person with BPD), who becomes an important “adult” in the life of a “border guard” who can be relied upon. Subsequently, from relying on the connection and the figure of the therapist, inside and the person with BPD, other relationships grow both inside themselves (to their internal objects) and outside, they have the opportunity to maintain closeness not only with the therapist, but also with other people and build with them a long-term relationship. Affects become rarer, not so amplitude, endurable. There is an opportunity to know one’s own painful places better, take care of oneself more, be less exposed to destructive relationships and processes, better understand one’s reactions, features and manifestations, learn to treat oneself like this in the world of people, sometimes explaining to them one’s own characteristics and properties.
Affects become rarer, not so amplitude, endurable. There is an opportunity to know one’s own painful places better, take care of oneself more, be less exposed to destructive relationships and processes, better understand one’s reactions, features and manifestations, learn to treat oneself like this in the world of people, sometimes explaining to them one’s own characteristics and properties.
Advice for People with BPD to Use in a Crisis
Calming an emotional storm
Stop fighting, avoiding, repressing, or denying what you are feeling. Give yourself permission to feel, this will take away the power of feelings over you. Try to simply experience your feelings without judgment or criticism.
Awareness
Let go of the past and the future, focus solely on the present moment. Mindfulness techniques can be very effective in this regard.
• Start by observing your emotions, step back and just observe them.
• Watch them come and go (it can help to think of them as waves that come and go).
• Focus on physical sensations that are accompanied by emotions.
• Tell yourself that you accept your emotions, accept what you feel right now.
• Remind yourself that just because you feel something doesn't mean it's real.
Do something to change your bad feelings
You will need to experiment to find out what works best for you. What can help when you are angry or have very strong feelings, when you are depressed, etc.
Some ideas for working on yourself
Tactile sensations . Try running your hand in cold or hot (but not scalding) water; hold a piece of ice in your hand; grab the edge of the piece of furniture as hard as you can. If you're feeling anxious and need to calm down, try taking a hot bath or shower; cover yourself with a blanket or cuddle with a pet.
Taste . If you feel empty or bored inside, try putting strong flavored sweets or mints in your mouth, slowly eating something with an intense taste, such as something salty. If you want to calm down, try something calming like hot tea or soup.
If you want to calm down, try something calming like hot tea or soup.
Smell . Light a candle, smell the flowers, try aromatherapy, spritz on your favorite perfume, or smell something that smells good in the kitchen. You may find you respond best to strong odors such as citrus, spices, etc.
Landmark . Focus on an image that grabs your attention. It could be something in your immediate environment (a great view, a beautiful flower, the location of a building, a favorite painting or photo) or something you imagine.
Sound . Try listening to loud music or a bell or whistle when you need a boost. To calm down, play soothing music or listen to soothing sounds of nature such as the wind, birds, or the ocean. The sound of a car can help a lot if you can't hear something more real.
Need to reduce emotional vulnerability
You are more likely to experience negative emotions when you are stressed. That is why it is very important to take care of your physical and mental well-being.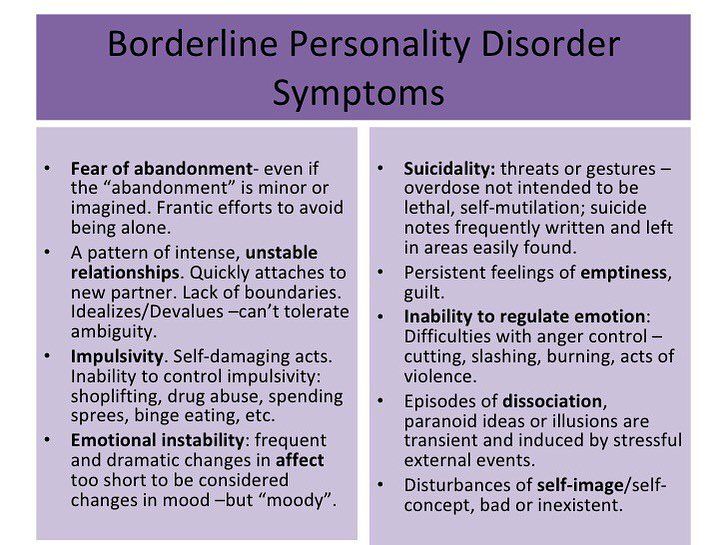
Take care of yourself :
- Avoid drugs.
- Eat a balanced, nutritious diet.
- Sleep well and rest.
- Practice self-help skills regularly.
- Minimize stressful situations.
- Practice relaxation techniques.
Basic methods of psychotherapy for BPD
- Dialectical Behavioral Therapy (DBT).
- Schematic (schematic) therapy.
- Psychotherapy based on mentalization (MBT).
- Transference-Focused Psychotherapy (TFP) is a psychotherapy focused on the analysis of transference.
Borderline personality disorder is not a sentence. Change is possible if there is a desire to change and improve the quality of life. I hope this article has helped you better understand the structure and manifestations of BPD, as well as approaches to psychotherapeutic treatment and self-help methods in a difficult situation.
What to do with BPD? Advice for “border guards”
Medical issues
Text: Masha Pushkina,
Ekaterina Tarasova
Illustrations: Alena Belyakova
November 09, 2017
Borderline personality disorder (BPD) is a mental illness associated with instability in interpersonal relationships and self-image, emotional instability and impulsivity.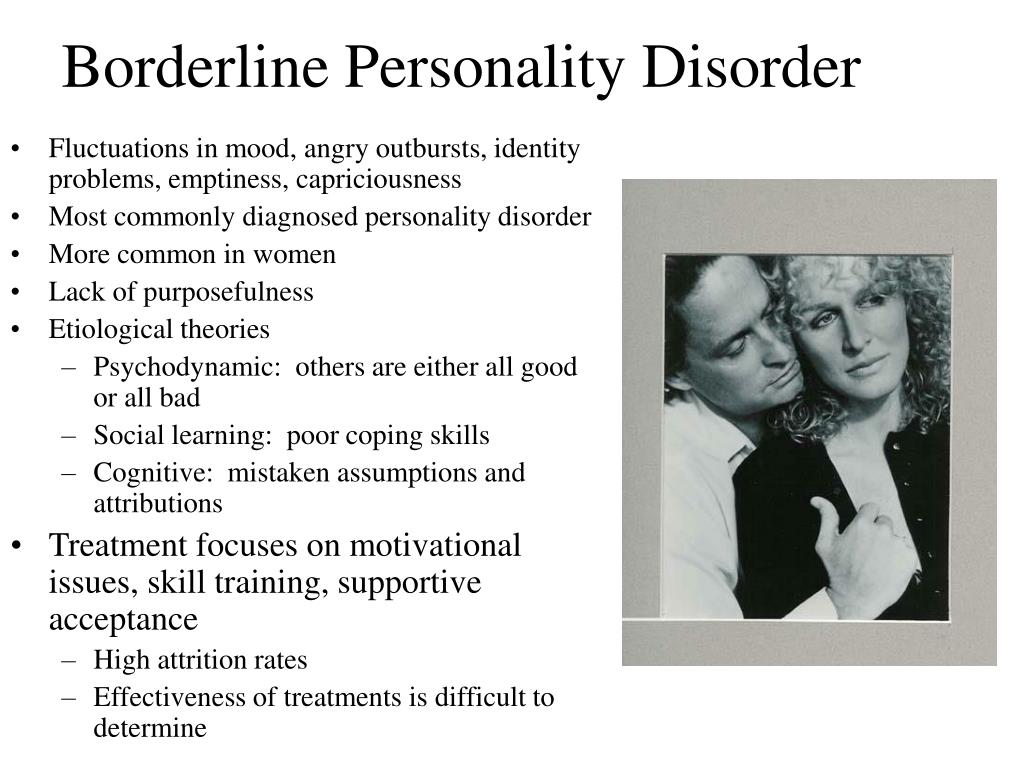 We have already talked about how people with BPD live, and today we will figure out what types of therapy are effective for borderline disorder and what experts advise border guards and their loved ones.
We have already talked about how people with BPD live, and today we will figure out what types of therapy are effective for borderline disorder and what experts advise border guards and their loved ones.
Anastasia Umanskaya, Gestalt psychotherapist: “Long-term psychotherapy is the main treatment for borderline personality disorder. And the most efficient. Therapy helps a person learn the skills to cope with strong emotions and maintain long-term relationships. The effectiveness of dialectical-behavioral psychotherapy has been studied the most. In addition to it, psychotherapy based on mentalization, psychotherapy focused on transference, psychodynamic therapy are effective in the treatment of BPD. The therapist draws up a treatment plan taking into account the characteristics of the character, personality and living conditions of the patient and includes individual therapy and group sessions.
BPD Therapy
The service market offers many types of therapeutic treatment, in which an ignorant patient can become confused. We have compiled the main types of therapies with proven effectiveness.
We have compiled the main types of therapies with proven effectiveness.
Dialectical Behavior Therapy (DBT)
A type of behavioral therapy developed specifically for people with BPD by American psychologist Marsha Linehan, author of Cognitive Behavioral Therapy for Borderline Personality Disorder. Within its framework, the patient is invited to realize that there are different points of view on the situation, which he perceives as “unbearable” and “hopeless”, so that he can eventually choose a more adequate behavior. The main point in this therapy is the need to accept patients as they are, while at the same time trying to teach them to change. During the DBT process, the therapist teaches the patient the necessary skills for emotional regulation, interpersonal effectiveness, stress coping skills, general mental engagement, and self-control. The emphasis in DBT is on acknowledging the person's emotional responses so that the person suffering from BPD feels supported. The duration of such therapy is usually from twenty-four to forty-eight weeks.
The duration of such therapy is usually from twenty-four to forty-eight weeks.
Dmitry Pushkarev, psychotherapist , develops DBT in Russia: “Every person, finding himself in a crisis situation, is looking for ways to cope with it. But they can be destructive: alcohol, aggression, suicide. Accordingly, the task of therapy is to teach the patient practical skills that will help to get out of the crisis. These are techniques of awareness, control of emotions, accepting a situation or finding a way out of it. DBT is a direction of therapy that has become very widespread in recent years. Initially, the technique was developed for people with chronic suicidal behavior - for those who repeat attempts to kill themselves and injure themselves even after treatment in a hospital (it is important to remember that young men and women often end up in Russian hospitals with a third or fourth suicide attempt). Today, DBT is used in the treatment of severe patients, including those with serious mental disorders - with borderline personality disorder or depression.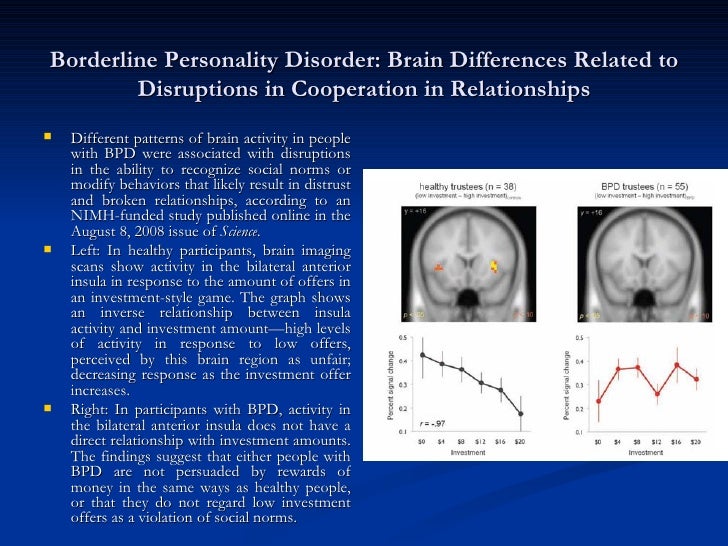
Russian experts have founded the first Dialectical Behavior Therapy community to spread this practice. Here, psychotherapists can learn DBT, and patients can undergo group and personal trainings.”
Mentalization Based Therapy (MBT)
Aimed at stabilizing the sense of self and helping the patient manage emotions in relationships. Mentalization is the process by which one person forms an idea of the behavior, thoughts, words, and reactions of other people. This process allows you to explain the behavior of others and requires an analysis of the circumstances of the actions. People suffering from BPD most often misinterpret the actions and actions of other people, putting their own subjective meaning into everything, which is why they do not accurately understand the states of others. In the process of therapy, the patient learns to accurately perceive the motives of the actions of other people. The therapist explains that any situation can be perceived from different angles, teaches you to ask clarifying questions about what a person might think, feel and do in the context of interaction with a person suffering from BPD. The task of therapy is to form the ability to reflect and teach the patient other skills of interpersonal interaction.
The task of therapy is to form the ability to reflect and teach the patient other skills of interpersonal interaction.
Transfer Focused Therapy (TFP)
TFP is a psychodynamic psychotherapy with step by step instructions. It was developed specifically for the treatment of borderline pathology and is based on the idea that the patient experiences external reality through his split inner world - and therefore sees others in black and white (idealization or devaluation). The task of the therapist is to help the patient become aware of this distortion and learn to perceive both the negative and positive traits of people at the same time.
Phrases every border guard should learn:
How do I feel now?
What do you mean?
What exactly do you want from me?
Is this reality or my fantasy?
I need time to answer you.
I am worthy of love and respect. But close people deserve a respectful attitude.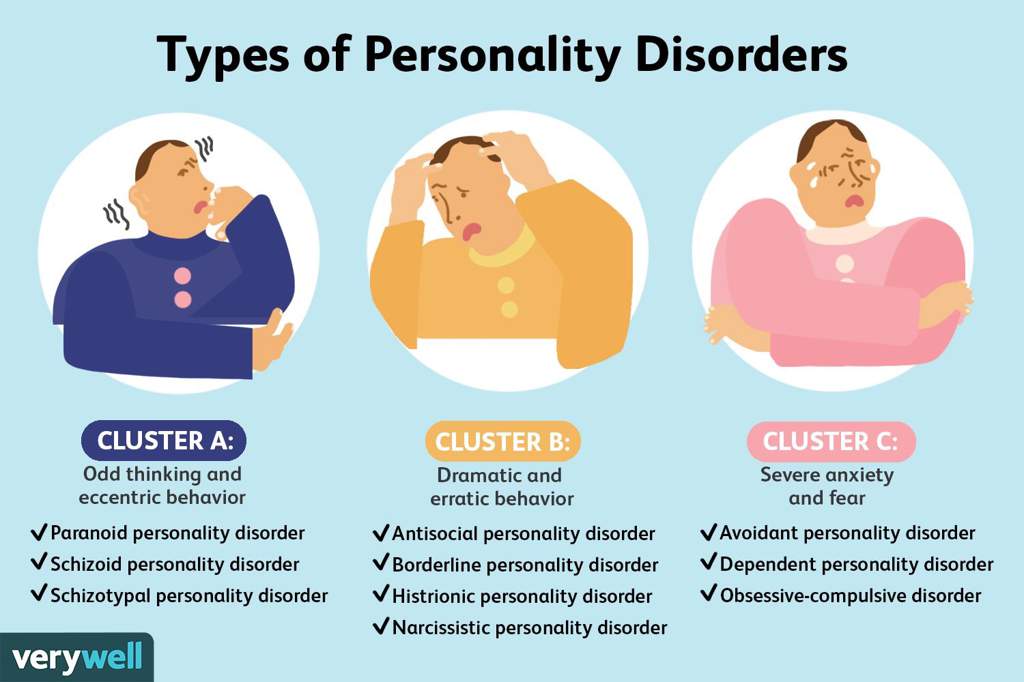
It will soon pass, we must wait a little.
Cognitive behavioral therapy
A type of psychotherapy that aims to change the way you think, with the result that you change your mood and behavior, is one of the first to be proven effective. Based on the notion that negative actions or feelings are the result of current distorted observations and thoughts, and not unconscious problems from the past.
The patient works with the therapist to identify specific patterns of negative thoughts and behavioral responses to difficult and stressful situations. Treatment involves developing more balanced and constructive ways to respond to stress. The therapist teaches the patient constructive forms of behavior, correcting dysfunctional thoughts and patterns of behavior. The result can be achieved in ten to twenty sessions.
Schema Therapy
Schema (or schematic) therapy was developed by the American psychologist Jeffrey Young based on cognitive behavioral therapy, psychoanalysis, object relations theory, attachment theory and gestalt therapy.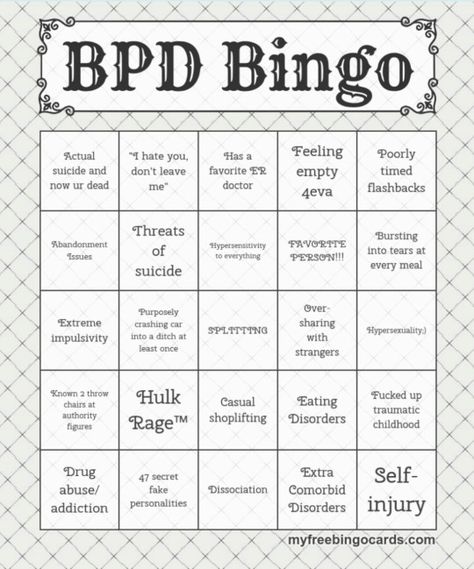 Schema uses various therapeutic techniques: interpersonal skills, one-on-one dialogues, group discussions. The name of Young's therapy emphasizes the idea that the "borderline" is acting according to a pattern formed in childhood. Such a schema is formed under the influence of traumatic events or maltreatment in childhood and is activated in adulthood under the influence of similar circumstances, provoking a certain perception of the world and reactions to it. The goal of schema therapy is to help the patient become aware of their schemas and the source of the emotions that arise when these schemas are activated, to experience these emotions and find ways to respond to events differently, destroying old patterns of behavior.
Schema uses various therapeutic techniques: interpersonal skills, one-on-one dialogues, group discussions. The name of Young's therapy emphasizes the idea that the "borderline" is acting according to a pattern formed in childhood. Such a schema is formed under the influence of traumatic events or maltreatment in childhood and is activated in adulthood under the influence of similar circumstances, provoking a certain perception of the world and reactions to it. The goal of schema therapy is to help the patient become aware of their schemas and the source of the emotions that arise when these schemas are activated, to experience these emotions and find ways to respond to events differently, destroying old patterns of behavior.
Alexander Erichev, a researcher at the Bekhterev Research Institute, presented a new direction for Russia in cognitive behavioral therapy. In Russia, this direction is just beginning its journey, so there are only a few certified specialists who can be contacted.
Self-help
Anastasia Umanskaya, Gestalt psychotherapist: “For a person suffering from borderline personality disorder, a sense of security is extremely important. This means minimizing stress in your personal life and at work so that responsibilities in business and at home are clearly defined, without ambiguities and generalizations. Stress will destabilize him.
It is important for a person with BPD to be aware of their own impulses and moods. Psychotherapy will help to distinguish between real needs and painful impulses caused by the imagination. A simple yet powerful way to become more self-aware is to ask yourself, “How do I feel?” several times a day.
It is important to inhibit impulsive behavior. “Measure twice, cut once” is the motto for a person with BPD who wants to improve their quality of life.
It is necessary to master self-soothing techniques. It can be meditation, breathing techniques, yoga classes, soothing music, aromatic bath.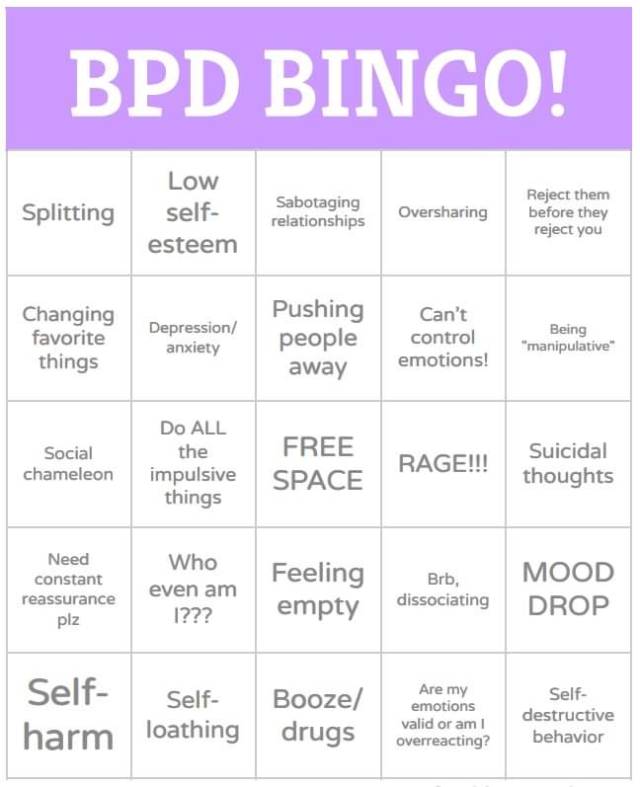 Breathing techniques will help you pause to respond to the stimulus more slowly and less impulsively.
Breathing techniques will help you pause to respond to the stimulus more slowly and less impulsively.
It is important to learn how to express both positive and negative emotions in an ecological way. If the former are welcome in our society, then it is more difficult with negative emotions. But if you just suppress them, they accumulate, and sooner or later an emotional outburst will follow. Therefore, one should learn to express them, but in a form acceptable to others.
It is helpful to remind yourself that you are worthy of love and respect. As an exercise, often remember your merits, achievements and reasons for pride. Set realistic goals for yourself. Many small achievements will support you much better than one big and difficult achievement.
It is important not to give in to criticism within yourself and to scold yourself as little as possible. Remind yourself that even the most difficult period is temporary and will end sooner or later.
A healthy lifestyle is always useful. Sports activities help relieve excessive anxiety and anxiety. Physical exercise releases endorphins, the happy hormone. And what seems absolutely terrible to you, perhaps after a run, will no longer be so scary. But you need to know the measure in sports, so as not to get the opposite effect of overload and stress.
Sports activities help relieve excessive anxiety and anxiety. Physical exercise releases endorphins, the happy hormone. And what seems absolutely terrible to you, perhaps after a run, will no longer be so scary. But you need to know the measure in sports, so as not to get the opposite effect of overload and stress.
It is important to keep a regular schedule. Mood instability and self-doubt create inner chaos. And the schedule of food, sleep, exercise will make the world more stable and predictable.”
In case of severe mental pain, it is necessary to distract yourself, switch your attention to watching a movie, socializing, shopping - that is, to do everything to change painful emotions with the help of events. Sometimes you need to give yourself a break or take a little vacation.
If you are in a serious crisis, you have suicidal thoughts, you can put your hands down and wash yourself with cold water, and then try to focus on what you see: describe objects and their shape to switch focus.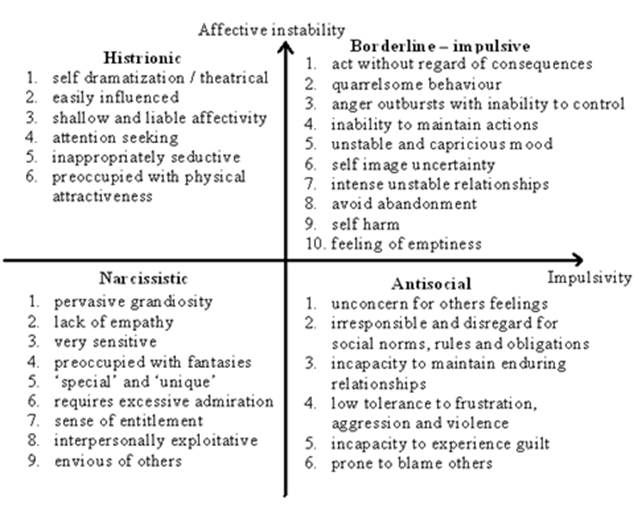 Then - perform breathing exercises: inhale for three counts and exhale for five counts. After a couple of minutes of such breathing, you need to try to approach the problem again and try to think in a constructive way. Start analyzing your behavior: understand what event provoked pain and destructive behavior, what emotions and thoughts arose. Try to imagine what the consequences of your different behaviors in this situation will be.
Then - perform breathing exercises: inhale for three counts and exhale for five counts. After a couple of minutes of such breathing, you need to try to approach the problem again and try to think in a constructive way. Start analyzing your behavior: understand what event provoked pain and destructive behavior, what emotions and thoughts arose. Try to imagine what the consequences of your different behaviors in this situation will be.
It is worth learning to tell yourself:
Stop! Step back. Inhale-exhale.
What happened is not yet a catastrophe: it's just a specific situation.
I can do it! I can handle! I will survive! I can!
I am not you. I have my own interests, needs, values.
This person is not only bad and not only good, he can be different, and I can be different.
I can take it!
I accept myself.
I will take care of myself, I will do something nice for myself.
My life is worth living!
"Pill against borderline"
There is no consensus on the medical treatment of BPD.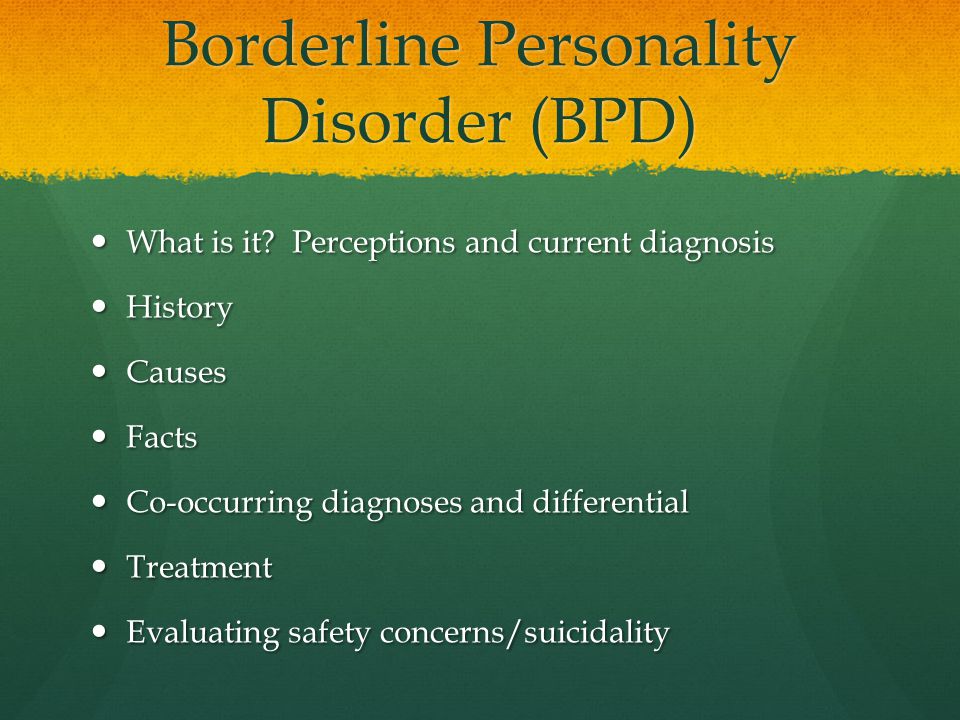 There are no “BPD pills” (like lithium for bipolar disorder or antidepressants for depression, for example). But BPD rarely comes alone. There is evidence that in 85% of cases, patients also have other disorders. Most often, these are different types of anxiety disorders, including post-traumatic (probably severe trauma and "starts" the development of BPD), panic attacks, addictions, anorexia and bulimia, obsessive-compulsive disorder, dissociative disorder.
There are no “BPD pills” (like lithium for bipolar disorder or antidepressants for depression, for example). But BPD rarely comes alone. There is evidence that in 85% of cases, patients also have other disorders. Most often, these are different types of anxiety disorders, including post-traumatic (probably severe trauma and "starts" the development of BPD), panic attacks, addictions, anorexia and bulimia, obsessive-compulsive disorder, dissociative disorder.
Anxiety, depression, irritability, attacks of aggression and suspicion, mood swings and short-term psychotic episodes can be treated with traditional medicines, so that part of the unpleasant symptoms can be eliminated relatively quickly.
BPD patients often end up in a psychiatric hospital, usually after a suicide attempt. There they are treated primarily with medication to help them survive the most difficult period. A patient on medication should strictly follow the doctor's recommendations: do not prescribe or cancel drugs on their own and do not change the dosage without consulting a doctor.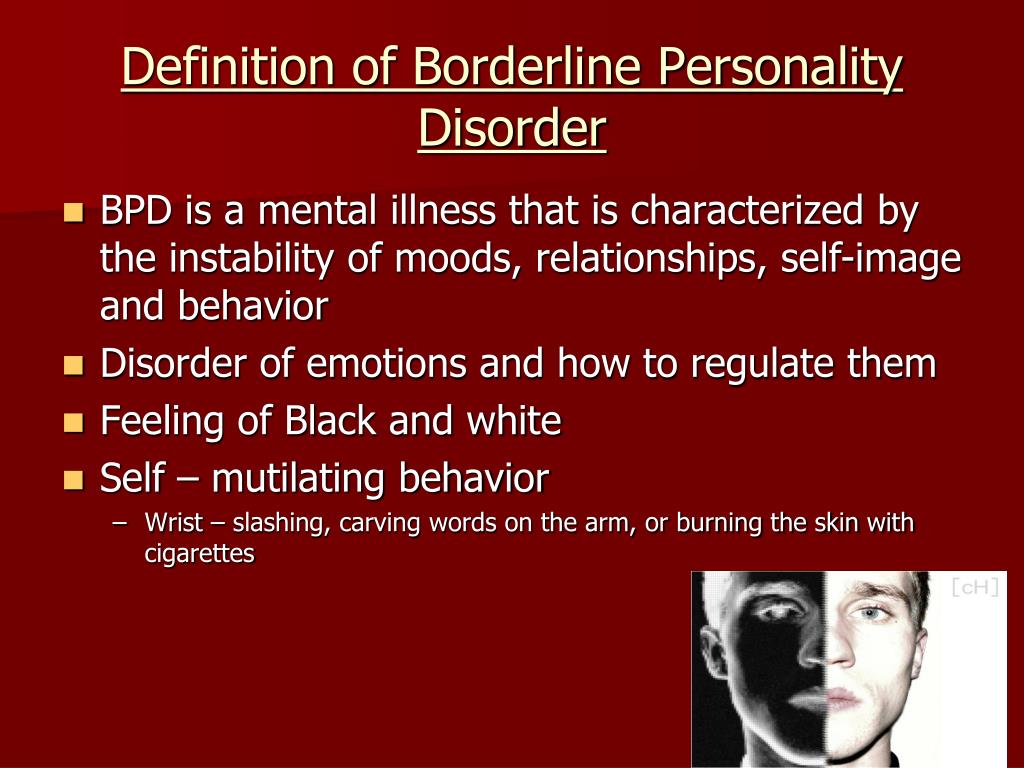
Blogger Ksenia Ivanenko: “The easiest way to get psychiatric help is to contact the PND or outpatient departments at hospitals (when anyone in need can sign up for a consultation with a doctor of their choice). You can also consult a psychiatrist privately. For free hospitalization in most state psychiatric hospitals, you must first contact the PND, get a referral, come to the hospital for a commission, go through it, wait for the doctors' decision. You can go to a public hospital on a paid basis, but even in this case, there may be queues and you have to wait until a place appears in the right department.”
How to understand that you need the help of a psychiatrist and other methods you can not cope with BPD?
Anna Ushkalova, psychiatrist: If you often feel uncontrollable anxiety, excitement, your emotional state is constantly deteriorating, the desire to harm yourself increases, suicidal thoughts appear, something strange seems or sees you, be sure to contact a psychiatrist.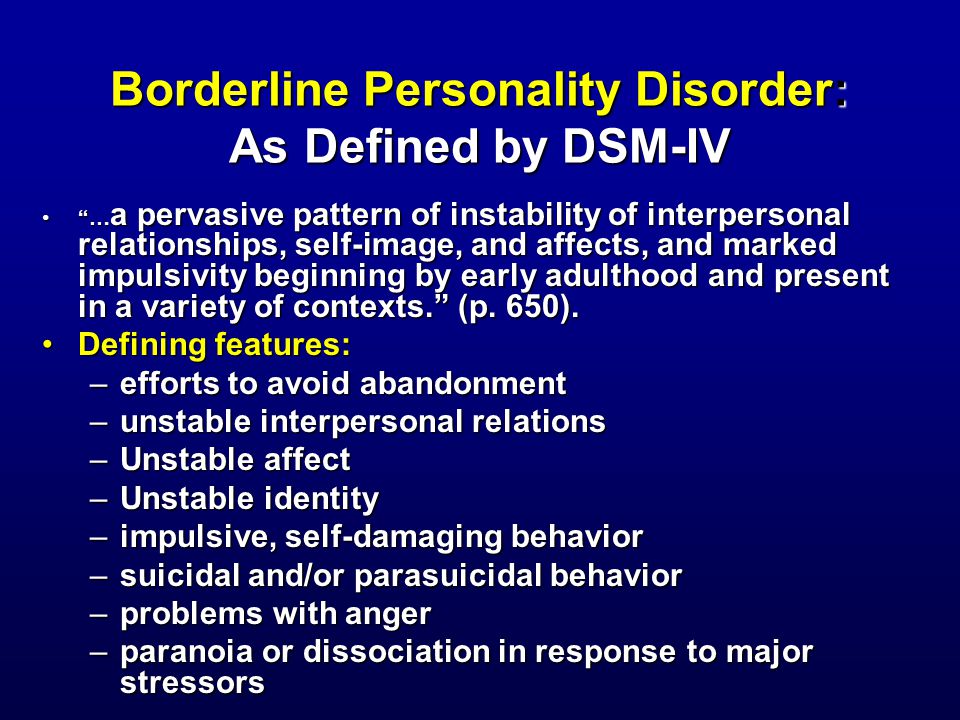
How effective are medications in treating BPD?
A.U.: Although psychotherapy is the mainstay of treatment for BPD, medications can significantly improve well-being. They reduce the severity of emotional fluctuations, depression, manifestations of impulsivity, aggression and auto-aggression.
Is hospitalization necessary and in what cases?
A.U.: The need for hospitalization arises in case of suicidal intent, life-threatening or health-threatening behavior. Hospitalization may also be indicated for psychotic symptoms.
It must be remembered that drugs will not help in solving the specific problems of "border guards", such as violation of self-identification, emotional chaos, fear of loneliness, weak self-control. Psychotherapy has proved its effectiveness here.
What to do if a person close to you is a “border guard”?
Anastasia Umanskaya: “People with BPD are usually described as 'difficult', 'manipulative', 'demanding' and 'requiring too much attention'.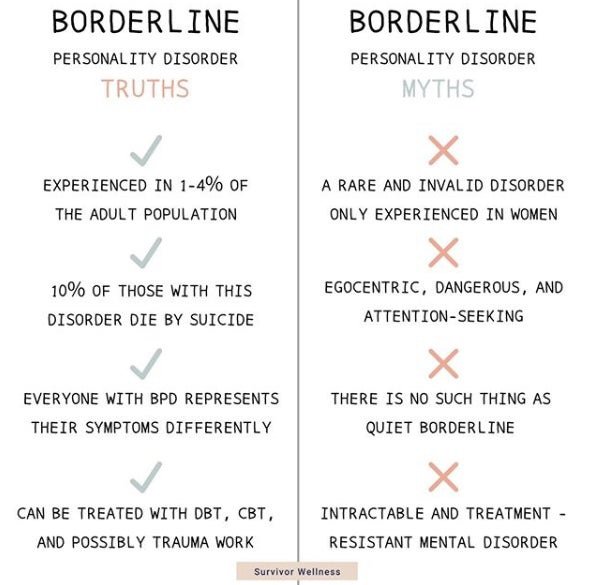 They get angry at their relatives and move away from them, they do not know how to manage destructive emotions and withstand difficulties. So the family of a person with BPD often feels emotional stress and even hostility.
They get angry at their relatives and move away from them, they do not know how to manage destructive emotions and withstand difficulties. So the family of a person with BPD often feels emotional stress and even hostility.
In romantic relationships, people with BPD also tend to create chaos, stress, and conflict. Often they are chronically dissatisfied with their partner. Such features can undermine relationships with family members, friends, colleagues.
Despite all this, constructive relationships are possible. They are more likely with a stable partner who is able to withstand the emotional outbursts of the "border guard" and peacefully respond to them without breaking off the relationship. And it’s good if he has patience and the ability to soften mood swings.
1. If your partner has borderline personality disorder, it is important that you create a safe environment at home with clear boundaries of what is and is not acceptable and a clear distance between you.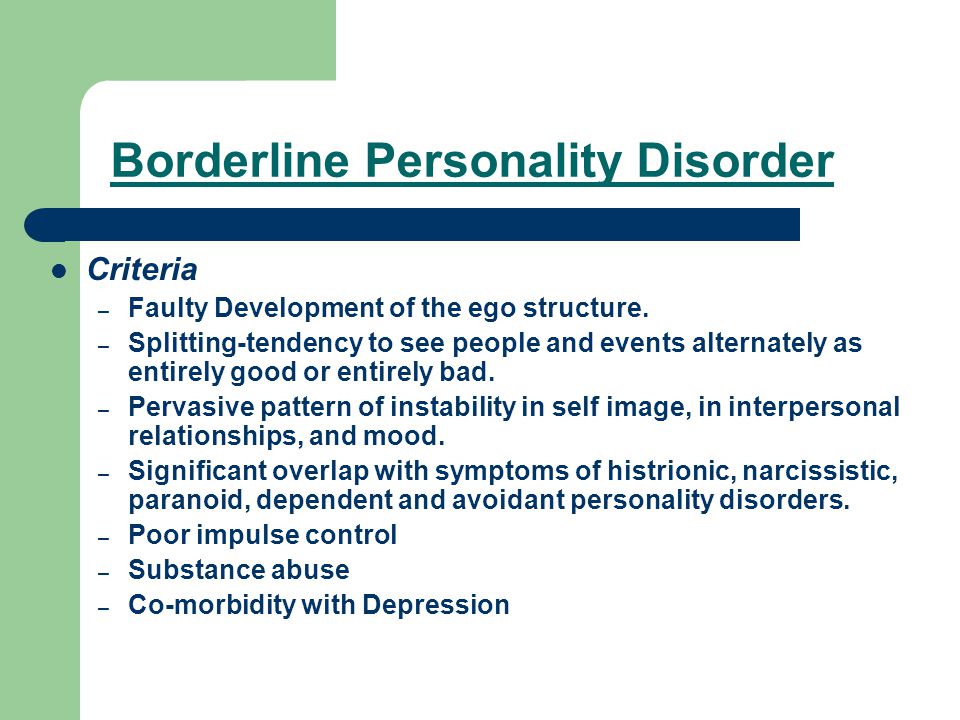 Your loved one is very important clarity, consistency and predictability of your behavior.
Your loved one is very important clarity, consistency and predictability of your behavior.
2. Be aware of the cycles of devaluation-idealization: adoration can quickly turn into hatred, and vice versa, so do not take emotional outbursts as true attitude towards you.
3. Always take seriously the BPD sufferer's threats to harm or commit suicide. This is not manipulation, he really can do this.
4. It is important not to discount the feelings of a person with BPD, even if those close to them do not understand at all what is happening. The feelings that he experiences are the most real, and it is important for him that they be recognized.
5. Don't forget to take care of yourself: get enough sleep, eat on time, rest. Organize support for yourself and don't focus on a partner who can take all of your time. Communicate with friends who understand you, relax alone. Maybe see a therapist."
With adequate treatment, the prognosis for the "border guard" looks quite optimistic: there are chances of a complete cure (as doctors say, "achieve a long-term remission").
Studies show that after six years of therapy, seventy percent of patients have resolved their main symptoms. After two years of treatment, remission occurred in a third of patients, after four years - in almost half. Only in six percent of patients the disease returned again after remission.
Useful resources about BPD
In 2017, the first Russian Resource Center was opened - an information portal for people suffering from borderline personality disorder, created on the basis of the experience of colleagues from the USA and Australia.
At the Center for Cognitive Behavioral Therapy, you can sign up for practical training on coping with stress and controlling emotions.
Russia's first community of dialectical behavior therapy (DBT).
Psychology Today Magazine: Borderline Personality Disorder
The largest English-language resource on BPD
BPD section at mind.