Borderline personality relationship
How to Make It Work
Symptoms of borderline personality disorder (BPD) can cause constant changes in emotions. This means people with BPD may have rocky relationships, both romantic and platonic.
Romantic relationships present a unique set of challenges for people with BPD and for their partners.
For example, a person with BPD may be affectionate and doting, but within a few hours, their emotional state may switch. They may feel smothered or overwhelmed. This can lead them to push away the partner they had just been drawing closer.
With treatment and continual support from family and partners, people with BPD can have successful relationships. Read on to find out how it’s possible and what you can do if you or your partner has BPD.
Borderline personality disorder (BPD) is a condition that affects the way a person processes everyday emotions and reactions.
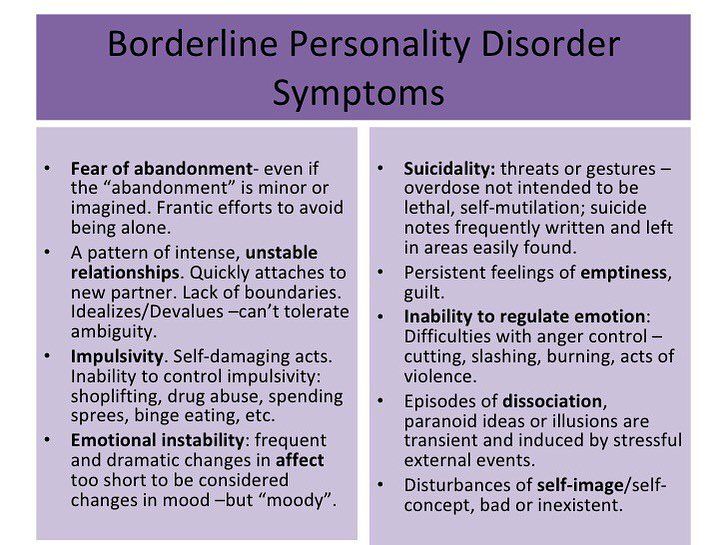
People with BPD are often impulsive and emotionally unstable. They may have intense episodes of anger, anxiety, and depression. These episodes can last several hours and be followed by a more stable period.
These episodes could also last several days and negatively affect the person’s work, relationships, or physical health. Some people with BPD are prone to self-injury, accidents, and fights. Suicide is also more common among people with BPD.
Another way to understand how a person with BPD experiences life is to realize they have a more difficult time returning to an emotional baseline.
When something exciting or positive happens, they may experience greater joy for longer. But the opposite is also true: If something bad happens, they may have trouble bouncing back.
For friends, family members, and potential partners of someone with BPD, these emotional peaks and valleys may seem chaotic, which can lead to intense, conflict-filled relationships.
A romantic relationship with someone with BPD can be, in a word, stormy. It’s not uncommon to experience a great deal of turmoil and dysfunction.
However, people with BPD can be exceptionally caring, compassionate, and affectionate. In fact, some people find this level of devotion from a partner pleasant. A person with BPD may also be very physical and eager to spend a lot of time with their partner.
At the same time, people with BPD are sensitive to abandonment or rejection. Many are hyperfocused on perceived signs that a romantic partner isn’t happy or may leave them.
When a person with BPD senses a shift in their partner’s feelings, whether real or imagined, they may immediately withdraw. They can become angry and hurt over something a person without BPD would not react to. They can even become obsessive.
These emotional switchbacks can be difficult to handle. Sometimes they can lead to uncomfortable public scenes. The impulsive behavior of a person with BPD may put that person or their partner at risk, too.
However, the stability of a partner may have a positive effect on the emotional sensitivities people with BPD experience.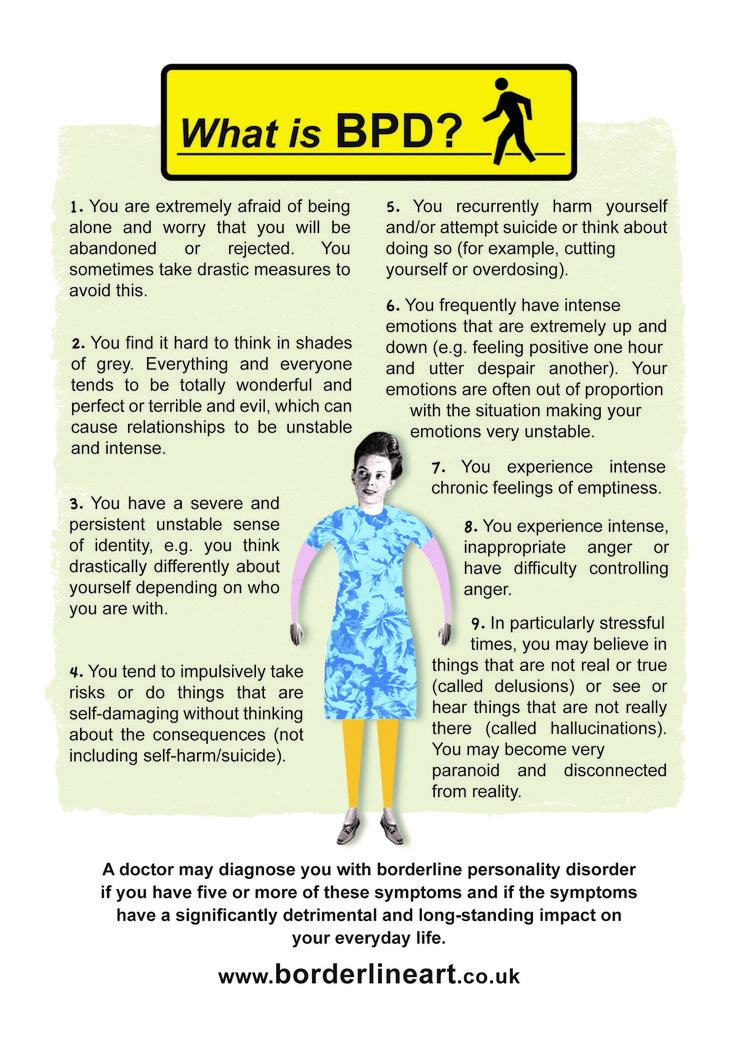 It may require a great deal of work from both partners, but long-term relationships and marriages are possible for people with BPD.
It may require a great deal of work from both partners, but long-term relationships and marriages are possible for people with BPD.
The most common BPD behaviors and symptoms could be detrimental to any relationship. If you have been diagnosed with the condition, you likely know this already. People with BPD are more likely to have many romantic relationships, which are often short-lived.
This could be because you purposefully broke off the relationship for fear your partner might do it first. It could also be because your partner wasn’t comfortable facing so much difficulty.
It’s important to know that you can have a healthy relationship despite your personality disorder. Treatment, along with a strong support network, can help you find stability in your emotional state and in your relationships.
Treatment won’t cure BPD, but these options can help you learn to cope with the symptoms and react in ways that aren’t as harmful to you or your partner.
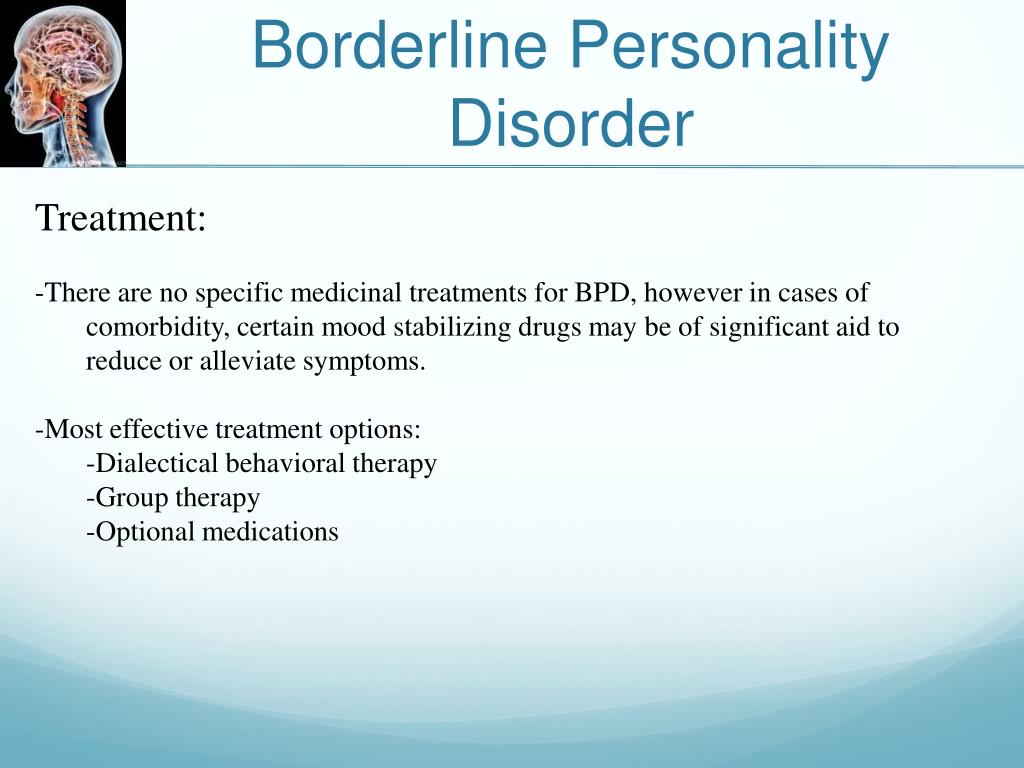
treatment for bpdThe most common treatments for BPD include:
- Therapy.
Dialectical behavioral therapy is commonly used with people who have BPD. A therapist will help you learn to respond to emotional situations with reason and proper judgment. This will reduce the dichotomous thinking (the belief that everything is black and white) that so many people with BPD have.
- Medication. There is no medication that can treat BPD, but antidepressants, antianxiety drugs, and antipsychotics may help treat some of the symptoms.
- Hospitalization. If you begin showing signs of self-harm or suicidal ideation, a doctor may hospitalize you for observation and intensive therapy.
If you or your partner has BPD, you can find ways to cope with the cycles of emotions that the condition causes. This can help you build a stronger, more resilient connection.
ways to improve bpd relationships
- Learn about BPD. Part of caring for a partner with BPD is understanding what they’re experiencing.
Understanding the level of emotional disorder they experience can help you respond in a way that protects both of you from additional chaos.
- Seek professional help. Therapy can help people with BPD learn to better process emotions and events that upset them. Partners of people with BPD can also benefit from therapy. A professional can help a partner understand how to react, understand, and be supportive.
- Offer emotional support. Someone with BPD may feel very isolated because of their past. Offer your partner understanding and patience. It is possible for them to learn and have better behaviors.
People with BPD are good and compassionate, and they can have healthy relationships. It takes work, and lifelong challenges will remain.
Therapists and doctors can work with you or your partner to develop a treatment plan. These healthcare providers can help you address the BPD symptoms that are most damaging to you and to your relationship.
Symptoms, Causes, and How to Cope
Our personalities are defined by the way we think, feel, and behave. They’re also shaped by our experiences, environment, and inherited traits. Our personalities are a big part of what make us different from the people around us.
Personality disorders are mental health conditions that cause you to think, feel, and behave differently than most people. When untreated, they can cause distress or problems in the lives of people who have them.
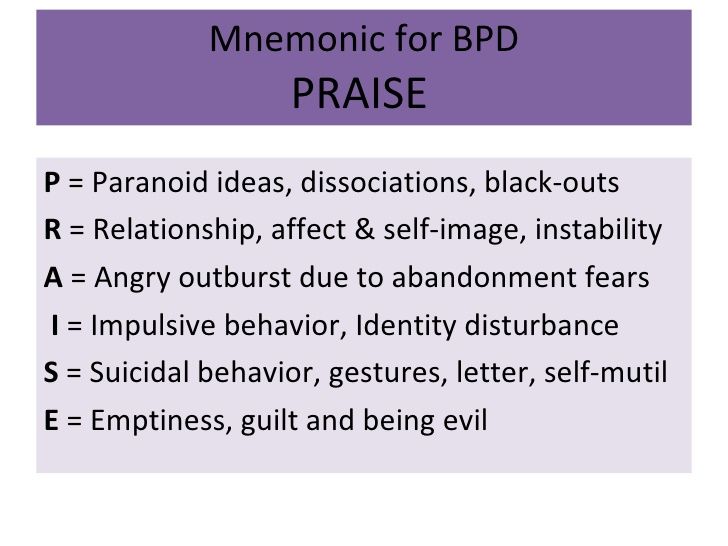
One very common personality disorder is called borderline personality disorder (BPD). It’s characterized by:
- self-image issues
- difficulty managing emotions and behavior
- unstable relationships
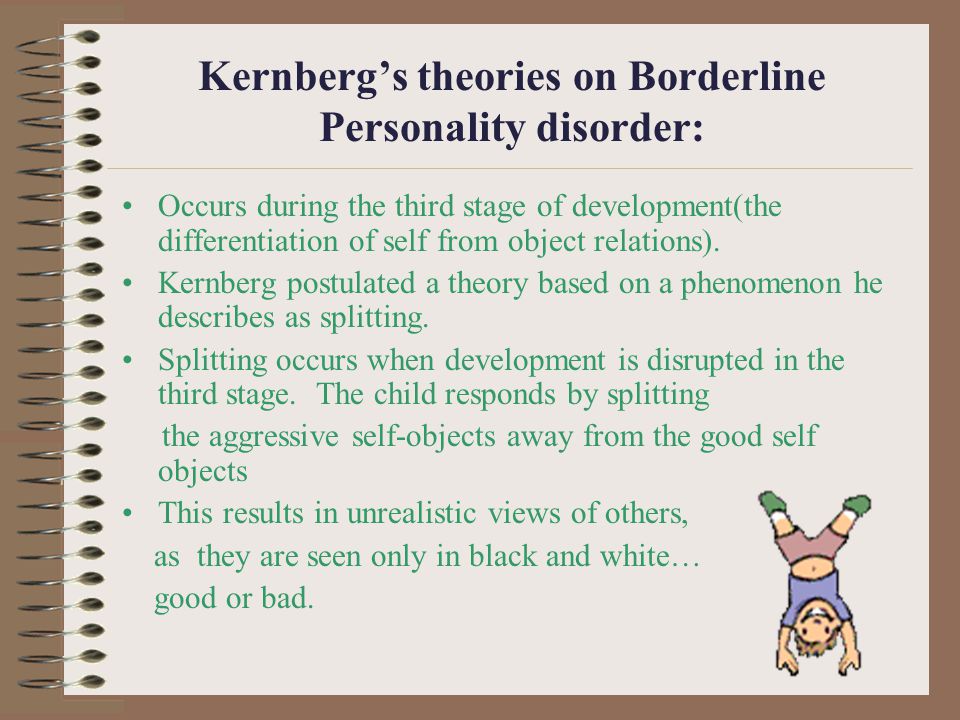
One key behavior shared by many with BPD is known as “splitting countertransference,” or simply “splitting.”
Keep reading to learn more about splitting in BPD and how to cope with it.
To split something means to divide it. Those with BPD tend to characterize themselves, other people, and situations in black and white.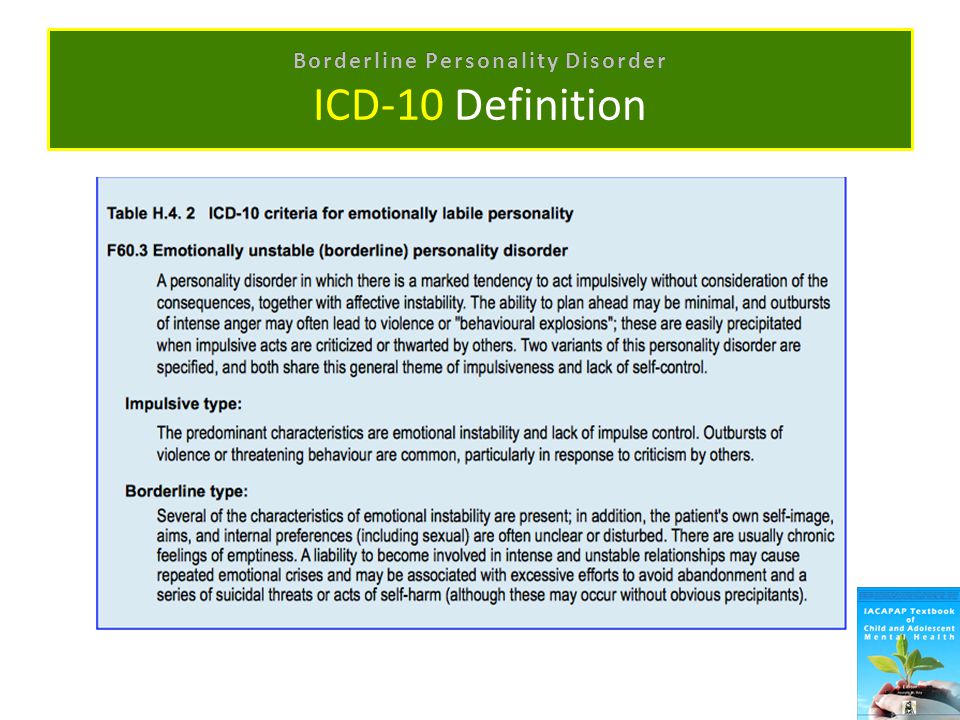 In other words, they may suddenly characterize people, objects, beliefs, or situations as either all good or all bad.
In other words, they may suddenly characterize people, objects, beliefs, or situations as either all good or all bad.
They may do this even though they know the world is complex, and good and bad can exist together in one.
Those with BPD often seek outside validation without considering their own emotions about themselves, others, objects, beliefs, and situations. This can make them more prone to splitting, as they attempt to shield themselves from anxiety caused by potential abandonment, loss of trust, and betrayal.
People with BPD often experience intense fears of abandonment and instability. To cope with these fears, they might use splitting as a defense mechanism. This means they might cleanly separate positive and negative feelings about:
- themselves
- objects
- beliefs
- other people
- situations
Splitting often occurs cyclically and very suddenly. A person with BPD can see the world in its complexity. But they often change their feelings from good to bad rather frequently.
A splitting episode can last for days, weeks, months, or even years before shifting.
What might trigger a splitting episode?
A split is typically triggered by an event that causes a person with BPD to take extreme emotional viewpoints. These events may be relatively ordinary, such as having to travel on a business trip or getting in an argument with someone.
Often, triggering events involve minor separations from someone they feel close to and sparks fear of abandonment.
You can identify splitting most commonly through the language of a person with BPD. They’ll often use extreme words in their characterizations of self, others, objects, beliefs, and situations, such as:
- “never” and “always”
- “none” and “all”
- “bad” and “good”
Here are a couple of examples:
Example 1
You’ve been feeling good about yourself, generally. You’re out on a road trip one day and make a wrong turn that gets you temporarily lost.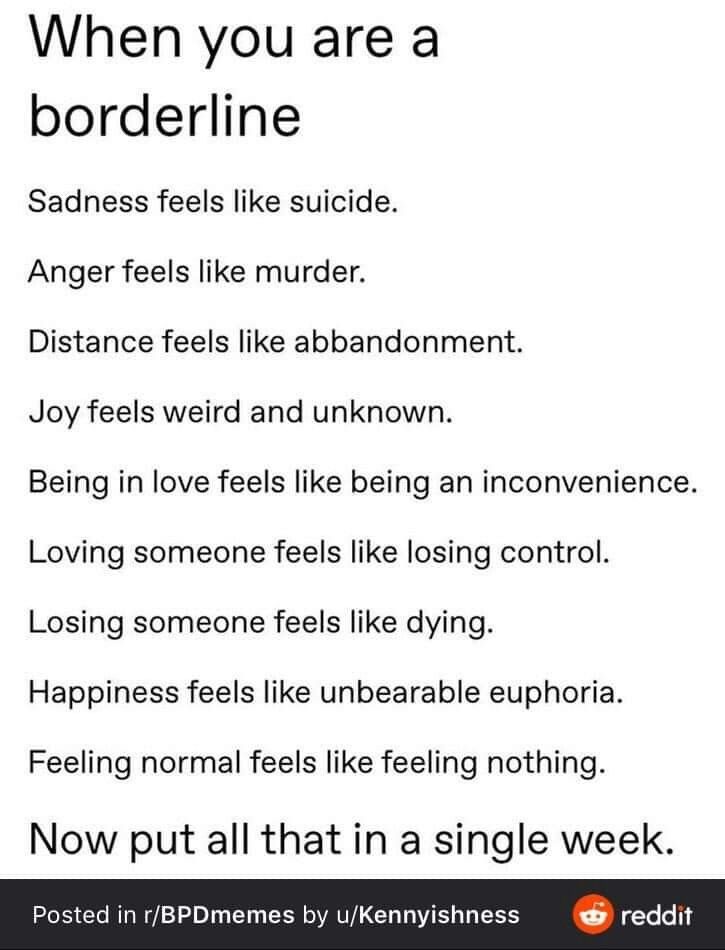 Suddenly, any good feelings you have about yourself disappear, and you get very down on yourself.
Suddenly, any good feelings you have about yourself disappear, and you get very down on yourself.
You may say negative things to yourself or others, such as “I’m such an idiot, I always get lost” or “I’m so worthless, I can’t do anything right.”
Of course, making a wrong turn when driving doesn’t mean a person is worthless. But a person with BPD can split their perception to avoid the anxiety of others perceiving them as worthless if they do the job first.
Example 2
You have a mentor you deeply admire. They’ve helped you professionally and personally, and you begin to idealize them. They must be without flaw if they’re so successful in their professional and personal lives. You want to be like them, and you tell them so.
Then one day your mentor undergoes turmoil in their marriage. You view this as a sign of weakness. Suddenly, you view your mentor as a complete fraud and failure.
You want nothing to do with them. You completely separate yourself and your work from them and look for a new mentor elsewhere.
Such splitting can leave the person being hurt, annoyed, and confused by the sudden shift in your perception.
Splitting is an unconscious attempt to safeguard ego and prevent anxiety. Splitting often leads to extreme — and sometimes destructive — behavior and personal turmoil in relationships. Splitting often confuses those who are trying to help people with BPD.
Splitting is an unconscious attempt to safeguard ego and prevent anxiety.
Those with BPD often report having intense and unstable relationships. A person who’s a friend one day may be perceived as an enemy the next. Some relationship traits of a person with BPD include:
- difficulty trusting others
- irrationally fearing others’ intentions
- quickly cutting off communication with someone they think might end up abandoning them
- rapidly changing feelings about a person, from intense closeness and love (idealization) to intense dislike and anger (devaluation)
- rapidly initiating physically and/or emotionally intimate relationships
Splitting is a defense mechanism commonly developed by people who have experienced early life traumas, such as abuse and abandonment.
Long-term treatment involves development of coping mechanisms that improve your perspective of the events happening in your life. Reducing anxiety can also help.
If you need help dealing with a splitting episode in the moment, here’s what you can do:
- Calm your breathing. A surge of anxiety often accompanies splitting episodes. Taking long, deep breaths can help calm you and prevent your extreme feelings from taking over.
- Focus on all your senses. Grounding yourself in what’s happening around you at a given moment can be a good way to distract yourself from extreme feelings and help you better put into perspective what’s happening around you. What can you smell, taste, touch, hear, and see in a moment?
- Reach out. If you find yourself splitting, consider reaching out to your mental healthcare professional. They may be able to calm you and help ease the split while it’s happening.
It’s not easy to help a person with BPD who experiences splitting. You may feel at the mercy of their symptoms. If you feel capable enough to help, here are some tips:
You may feel at the mercy of their symptoms. If you feel capable enough to help, here are some tips:
- Learn as much as you can about BPD. It’s easy to get offended by the up-and-down behavior of someone with BPD. But the more you know about the condition and how it can affect behavior, the more understanding you’ll have about your loved one’s behavior.
- Know your loved one’s triggers. Often, the same events over and over again are a BPD trigger. Knowing your loved one’s triggers, alerting them, and helping them avoid or cope with those triggers may prevent a splitting cycle.
- Understand your own limits. If you feel unequipped to help your loved one cope with their BPD splitting episodes, be honest. Tell them when they should seek professional help. Here’s how to access therapy for every budget.
BPD is a mental health disorder characterized by extremes in the way a person thinks, feels, and acts. Many people with BPD form extreme characterizations about themselves, others, objects, beliefs, and situations during episodes called splitting.
Situations associated with anxiety often trigger splitting episodes. While it may be difficult at times, coping with splitting symptoms is possible.
Getting professional help can best prepare you to cope with your BPD and splitting cycles.
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
Now officially: BPD is a diagnosis
Borderline personality disorder is one of the ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.
People with BPD are reverse solipsists: they are convinced of the inviolability of the world around them, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
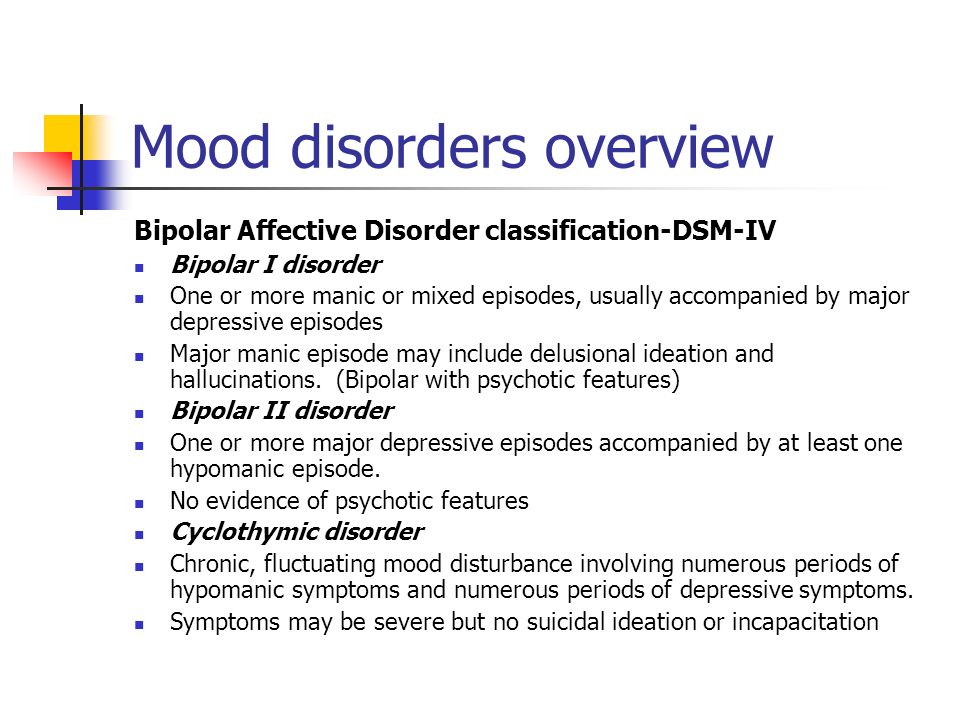
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
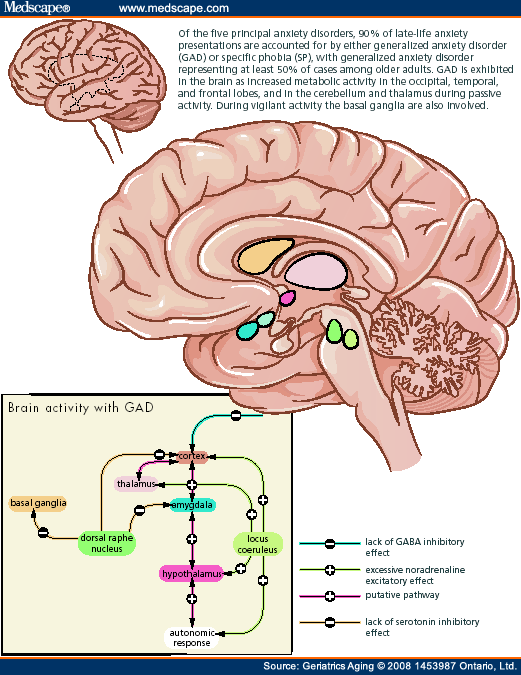
Borderline personality disorder can be accompanied by alcohol, drug, gambling addiction and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health information resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone.
 You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
You constantly worry about people leaving you and are ready to do everything to prevent this from happening. - Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control. In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
- Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.

“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with an interruption in communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires identifying the cause. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations.
 For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder. - Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of.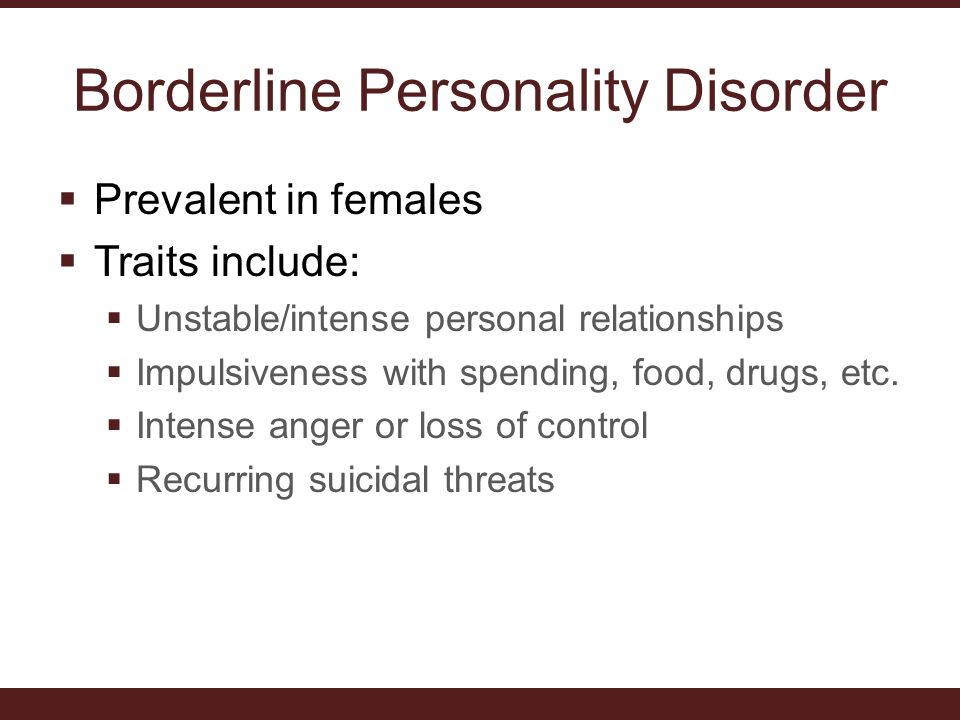 At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself.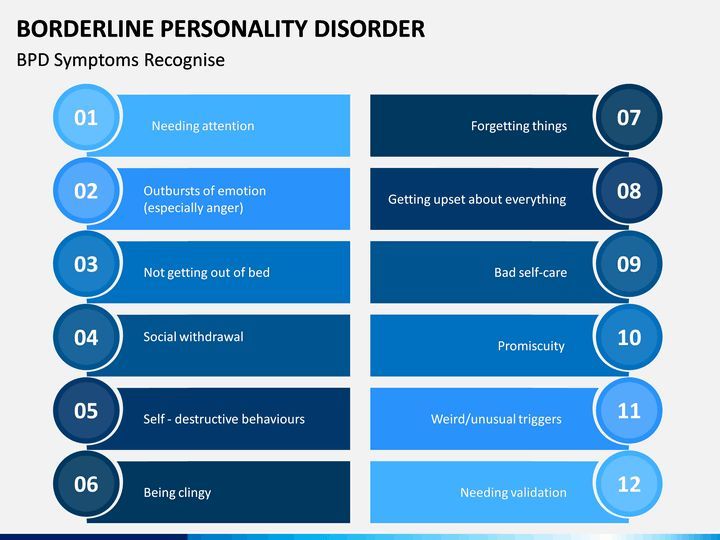 If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
 Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”.
Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”. Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills.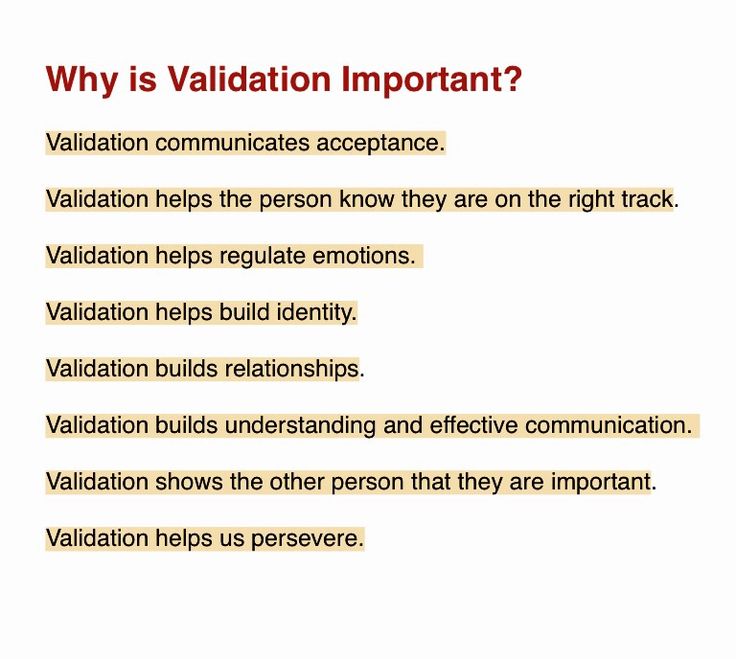 Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT). Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
- Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Psychotherapy (TFP) teaches to perceive positive and negative qualities simultaneously, to get out of the "deification/devaluation" paradigm.
- Cognitive Behavioral Therapy helps to change the way of thinking, reactions to stress and correct affective patterns of behavior.
- Schematic therapy is a complex treatment based on psychoanalysis and gestalt therapy. It changes the behavioral patterns laid down in childhood or adolescence.
- Self help. It consists in tracking the dynamics of emotions, asking yourself questions like “how do I feel now?”, “What does he (a) specifically want from me?”, “Is this reality or my fiction?”.
To improve their inner state, people with BPD are advised to start meditating, exercising, walking more often in the fresh air, trying to rationalize their own mood swings, learning self-soothing techniques and training willpower in order to stop emotional breakdowns in time.
Related material
Causes, Symptoms and Treatments
Borderline Personality Disorder (abbreviated as BPD ) is increasingly common among children today.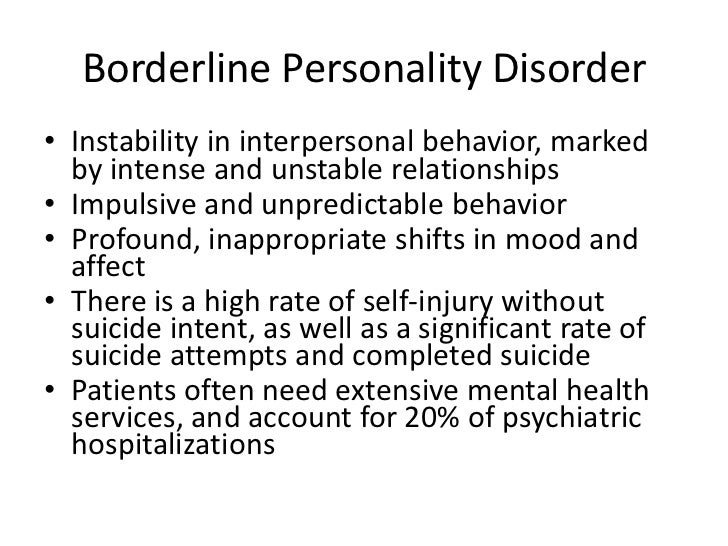 The pathogenesis of this type of psychopathy is usually accompanied by a complex of unfavorable factors.
The pathogenesis of this type of psychopathy is usually accompanied by a complex of unfavorable factors.
It is quite difficult to recognize this type of disease in everyday life. Often, it is confused with narcissism or simply the bad character of the individual, since the behavior of the "border guards" can be characterized by an extreme degree of unpredictability and hysteria, as well as a tendency to manipulation. For example, they confess their love to a partner, and after a couple of hours they leave “forever”, they can sincerely sympathize with someone, and then hit. It is also very common for patients of this type to constantly violate the boundaries of other people, shifting their problems onto them, and avoiding responsibility. Consider the symptoms of borderline in more detail.
Symptoms of borderline personality disorder (BPD)
The main symptomatic difference of this type of disorder is prolonged abnormal behavior of the patient .
While in many other psychopathy periods of instability alternate with remission, in the case of BPD the patient behaves destructively over a long period of time. In the field of psychological anomalies are such manifestations as:
In the field of psychological anomalies are such manifestations as:
- aggressive behavior leading to problems in relationships,
- unstable emotional background and inadequate self-image,
- high anxiety,
- total fear of loneliness and permanent feeling of boredom,
- dichotomous thinking and changeable mood, dividing the world only into "black and white" (today I love, but tomorrow I hate).
Also among the main symptoms can be noted: sociopathy and fear of society associated with low self-esteem and, as a result, separation anxiety (it is experienced by a person when separated from home or loved ones). Patients often exhibit reckless irresponsible "risky" behavior, the extreme form of which may be self-harm or suicide attempt.
Types of spontaneous actions that accompany mental borderline personality disorders
Due to difficulties in self-identification, lack of one's own opinion and a tendency to polarity, spontaneous destructive actions are characteristic of BPD sufferers.
Panic fear of loneliness and the lack of an inner core pushes them into contact with sociopathic personalities who are characterized by destructive behavior: gambling, theft, vandalism, promiscuous relationships, drug addiction. This also includes self-harm, which was mentioned above.
One of the reasons for this uncontrolled behavior is the problem with holding the internal impulse. The level of impulsivity is so high that a person is not able to control it.
Andrey Nikolaevich Cherednichenko
Chief physician of the Korsakov medical centers network, psychiatrist-narcologist
- Experience for more than 12 years
Consultation
Record for reception
Emotively unstable personality disorder of the 10th Restraif personality disorder is defined as "Emotionally unstable personality disorder (F60.3)". In the clinical community on the territory of the Russian Federation, this name is used quite often and is used due to the fact that the main symptom, as described above, manifests itself in the form of an emotionally unstable mental state of a person.
Pathogenesis of BPD
In the pathogenesis of the disease lies an incorrectly or incompletely formed intrapersonal self-awareness, in other words, “self-identification”. Border guards hardly realize how they relate to the main areas of life. They have problems with the concept of their opinions, interests, hobbies, and their character as well. Hence the more common definition of the disorder - "borderline". In this aspect, it means maneuvering on the verge between psychopathy and a stable state. The word "borderline" in a particular case means a precarious state between the norm and deviation, as if a person lives on the verge between "mental illness" (psychosis) and "mental health". That is why, the slang name for patients of this type is “borderliners” (from the English expression “border line”, which literally translates as “border”).
In classical psychiatry, borderline personality disorder is also referred to as a type of ego syntonic disorder. Ego syntonicity implies that the patient does not assess his condition as painful, is not critical of him and calmly accepts deviations in behavior, not believing that they harm him in any way.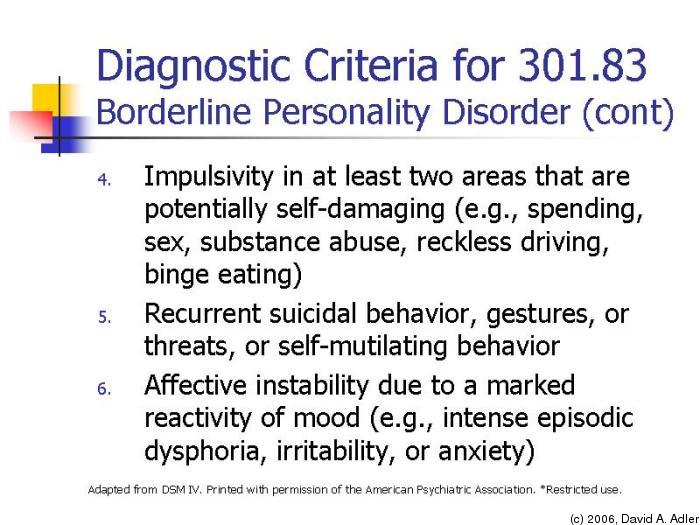 Moreover, the patient, as it were, “defends” his symptom, preventing his own cure due to the difficulty in identifying his own “I”.
Moreover, the patient, as it were, “defends” his symptom, preventing his own cure due to the difficulty in identifying his own “I”.
Causes of BPD
The underlying causes of BPD are currently not clearly defined, however, like most other disorders, BPD is caused by a group of factors.
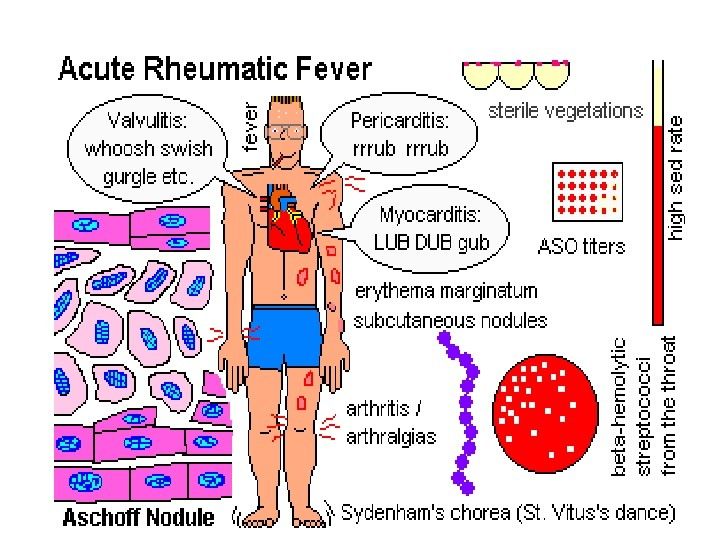
Hereditary (genetic determinism), physiological (disturbances in the brain) and social factors (low stress resistance and psychological traumatic factor).
Unfavorable social environment
According to statistics, groups of people exposed to an unfavorable social environment, for example, in the family, are more susceptible to the disease. These include:
- difficult childhood,
- abuse,
- tyranny,
- physical or emotional domestic violence,
- early loss of parents.
It is worth noting that "borderliness" occurs 3 times more often among women than among men.
Post-traumatic stress disorder (PTSD) , as a variation of an unfavorable social factor, can act not only as a cause, but also as a concomitant individual disease that is in a pathogenetic relationship with the diagnosis in question.
Childhood chronic emotional trauma can contribute to the development of BPD, but in rare cases it is the only cause. Personal qualities that are responsible for the ability to cope with a stressful situation in this aspect also play a big role. Here it is worth noting that, according to statistics, an injury received in childhood (especially before the age of 10) can lead to a subsequent disorder much more likely than an injury received at an older age. Also, scientists note that situations not associated with direct violence, such as natural disasters or catastrophes, are less likely to lead to the development of post-traumatic syndrome.
Physiology
Another group of factors considers a possible cause of the development of the disease - disorders in the work of neural brain connections, namely the destruction of the functioning of the frontal-limbic neurons
Heredity
diagnosis. It is quite difficult to achieve clear indicators in this vein, however, according to European studies, BPD is located in 3rd place out of 10 in terms of the genetic determinant among personality disorders. It is logical to note that deviations in the work of certain parts of the brain can be inherited and lead to a number of psychological problems, the development of which is aggravated by the social factor. Most studies show that most often borderlineness is transmitted from the mother.
It is logical to note that deviations in the work of certain parts of the brain can be inherited and lead to a number of psychological problems, the development of which is aggravated by the social factor. Most studies show that most often borderlineness is transmitted from the mother.
Borderline mental state in psychiatry and severity of personality disorders
In clinical psychiatry, three levels of mental disorder are traditionally distinguished:
- Neurotic . These include neuroses of a different nature, implying reversible temporary conditions that can be treated.
- Psychopathic level . In its plane lie personality disorders, which include anomalies in the nature of various pathogenesis or painful changes in its features, with which nothing can be done, since they relate to the personality structure of the individual.
- And finally, the deepest lesion of the psyche manifests itself at the psychotic level .
 This includes such manifestations as delirium, hallucinations, twilight consciousness.
This includes such manifestations as delirium, hallucinations, twilight consciousness.
Modern psychoanalysis distinguishes 4 levels of deviations. Between the state of psychosis and neurosis, it is conditionally located just “ borderline level”, also called borderline state . A borderline state can mean both the disorder itself and the designation of the level of mental damage.
How to reliably identify borderline personality disorder (BPD)
Borderline personality disorder is extremely difficult to diagnose and differentiate, as it has a high level of comorbidity, in other words, it is combined with a large number of concomitant disorders. For example, panic anxiety, eating disorders, bipolar affective disorder, attention deficit disorder, sociopathy, and so on. In connection with the above, the patient has to undergo a long diagnostic process and special tests.
Borderline personality disorder BPD test
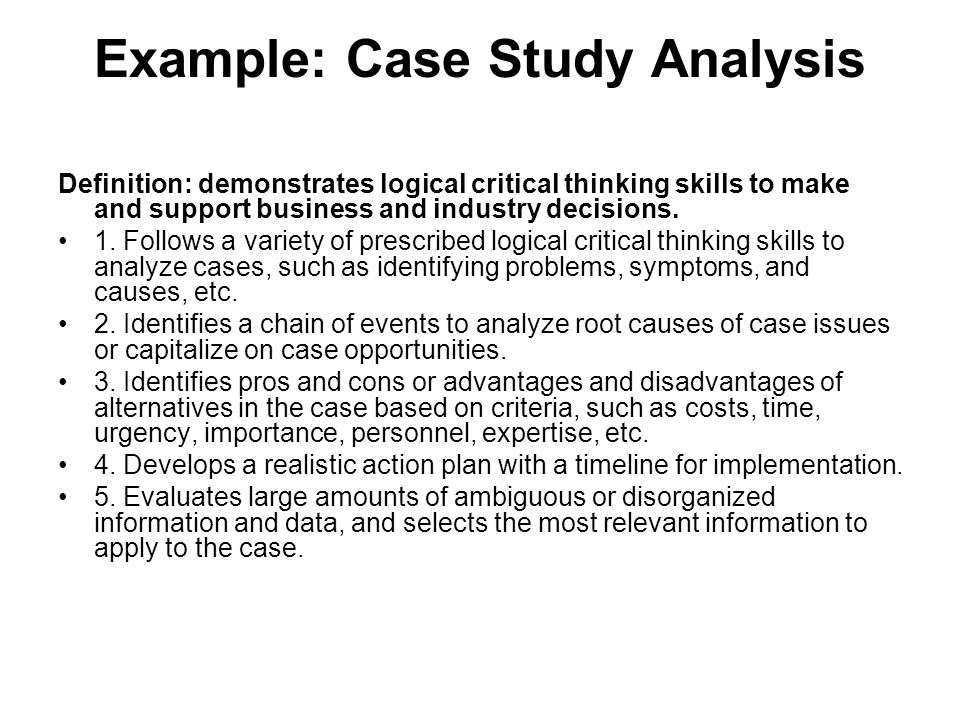
One of the fairly popular tools for detecting the presence of psychopathy are tests, which are, in fact, a personality questionnaire.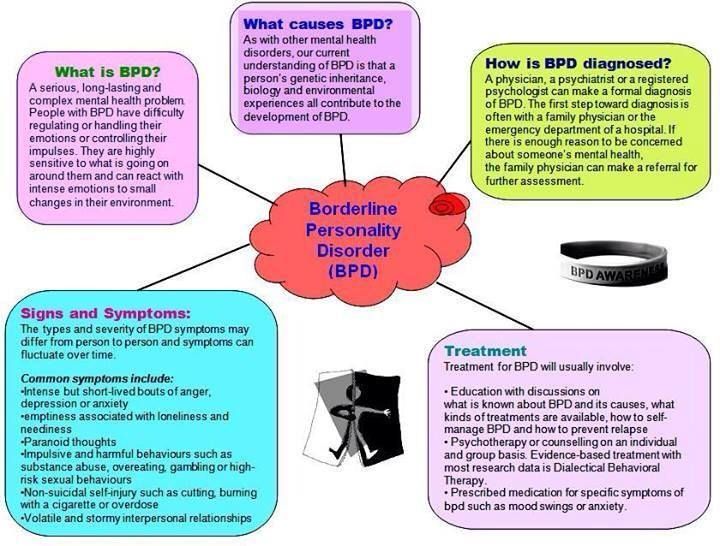 Used in modern clinical psychology, a test for screening for the bright signs of BPD was developed in 2012 by a group of scientists. In their work, the authors relied on the basic criteria for differentiating borderline disorder.
Used in modern clinical psychology, a test for screening for the bright signs of BPD was developed in 2012 by a group of scientists. In their work, the authors relied on the basic criteria for differentiating borderline disorder.
The questionnaire edited by them is a fairly effective tool for diagnostic verification and confirmation of symptoms. It is used both in psychiatric and general clinical, and in other practices that are not directly related to medicine.
The test itself consists of 20 questions and asks the subject to answer only yes or no. For each answer, the system counts a certain number of points. The probability of diagnosing BPD appears if the respondent scored more than 25 points.
Treatment of borderline personality disorder (BPD)
Cherednichenko Andrey Nikolaevich
Head doctor of the network of medical centers "Korsakov", psychiatrist-narcologist
- Experience over 12 years
Consultation
Appointment
Like most other mental disorders, borderline disorder is not treated at home and requires complex occupational therapy, including both medication (taking antidepressants and antipsychotics) and psychotherapy.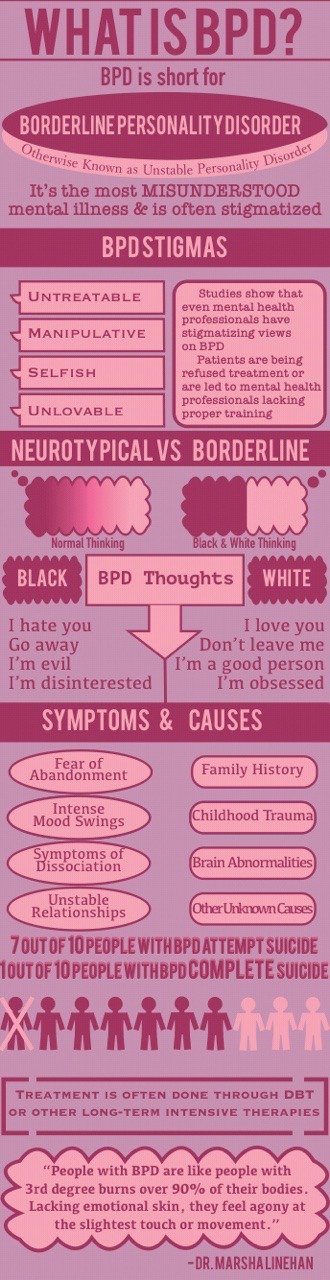 And only a psychiatrist, often in tandem with a clinical psychologist, can competently develop an effective course of treatment.
And only a psychiatrist, often in tandem with a clinical psychologist, can competently develop an effective course of treatment.
The drug course is developed in accordance with the individual characteristics of the patient's body and includes the following drug groups:
- Selective inhibitors of are aimed at preventing depressive episodes and reducing anxiety/panic/borderline states.
- Mood stabilizers .
One of the most popular remedies is Lamotrigine. It is also used to neutralize depression, mood lability and impulsivity.
- Atypical antipsychotics .
Now the 2nd generation of drugs of this cluster has already been developed, which have proven themselves in neutralizing the symptoms of the cognitive sphere, such as: aggression, distortion of the perception of reality, paranoia, thought dichotomy and disorganization.
As for the group of benzodiazepines and stimulants, they are used in modern therapy extremely rarely due to the high risk of dependence and, accordingly, overdose.
Thus, the main task of drug therapy in borderline personality disorder is to reduce the severity of symptoms and alleviate the general condition of the patient.
It is worth noting that BPD is the most difficult to treat due to the patient's ego syntony, which we discussed above. It is the patient with BPD who is the most difficult to respond to any therapy due to the rigidity of the psyche and the clear conviction that everything is generally normal with them.
However, when it comes to Selective Inhibitors, Dialectical Behavioral Therapy (DBT), one of the varieties of Cognitive Behavioral Therapy (CBT), is considered the most effective method in the modern clinical community. As part of the treatment, the patient is taught to look at the problem from different points of view and evaluate the causal relationship in different ways. Due to satisfaction with their symptoms and rigidity, "border guards" are difficult to treat, so the psychotherapeutic process can be lengthy.