Stress causing fever
Psychogenic fever: how psychological stress affects body temperature in the clinical population
1. Bakwin H. Emotional deprivation in infants. J Pediatr 1949; 35:512-21; PMID:18143946; http://dx.doi.org/ 10.1016/S0022-3476(49)80071-0 [PubMed] [CrossRef] [Google Scholar]
2. White KL, Long WN Jr. The incidence of psychogenic fever in a university hospital. J Chronic Dis 1958; 8:567-86; PMID:13587612; http://dx.doi.org/ 10.1016/0021-9681(58)90050-X [PubMed] [CrossRef] [Google Scholar]
3. Meyer R, Beck D. Psychodynamics of psychogenic fever. Zeitschrift fur Psychosomatische Medizin und Psychoanalyse 1976; 22:169-70; PMID:941539 [PubMed] [Google Scholar]
4. Malleson N. Panic and phobia; a possible method of treatment. Lancet 1959; 1:225-7; PMID:13631975; http://dx.doi.org/ 10.1016/S0140-6736(59)90052-2 [PubMed] [CrossRef] [Google Scholar]
5. O'Toole JK, Dyck G. Report of psychogenic fever in catatonia responding to electroconvulsive therapy. Dis Nerv Syst 1977; 38:852-3; PMID:908250 [PubMed] [Google Scholar]
6. McNeil GN, Leighton LH, Elkins AM. Possible psychogenic fever of 103.5 degrees F in a patient with borderline personality disorder. Am J Psychiatry 1984; 141:896-7; PMID:6731643; http://dx.doi.org/ 10.1176/ajp.141.7.896 [PubMed] [CrossRef] [Google Scholar]
7. Weinstein L. Clinically benign fever of unknown origin: a personal retrospective. Rev Infect Dis 1985; 7:692-9; PMID:4059757; http://dx.doi.org/ 10.1093/clinids/7.5.692 [PubMed] [CrossRef] [Google Scholar]
8. Timmerman RJ, Thompson J, Noordzij HM, van der Meer JW. Psychogenic periodic fever. Neth J Med 1992; 41:158-60; PMID:1470287 [PubMed] [Google Scholar]
9. Miric D, Venet R, Aproh E, Nguyen-Duc H. Psychogenic fever or psychogenic hyperthermia? J Am Geriatr Soc 1997; 45:1287-8; PMID:9329503; http://dx.doi.org/ 10.1111/j.1532-5415.1997.tb03796.x [PubMed] [CrossRef] [Google Scholar]
10. Araki T, Oka T, Oyama N, Akamine M, Kubo C. A case of psychogenic fever treated successfully with art therapy. Jpn J Psychosom Med 2004; 44:289-94 [Google Scholar]
11. Nozu T, Uehara A. The diagnoses and outcomes of patients complaining of fever without any abnormal findings on diagnostic tests. Intern Med 2005; 44:901-2; PMID:16157998; http://dx.doi.org/ 10.2169/internalmedicine.44.901 [PubMed] [CrossRef] [Google Scholar]
Nozu T, Uehara A. The diagnoses and outcomes of patients complaining of fever without any abnormal findings on diagnostic tests. Intern Med 2005; 44:901-2; PMID:16157998; http://dx.doi.org/ 10.2169/internalmedicine.44.901 [PubMed] [CrossRef] [Google Scholar]
12. Kura N, Oka T, Ando T, Ishikawa T, Kubo C, Ago Y. A case of psychogenic fever treated successfully with tandospirone in combination with psychotherapy and autogenic training. Jpn J Psychosom Med 2004; 44:297-303 [Google Scholar]
13. Hiramoto T, Oka T, Yoshihara K, Kubo C. Pyrogenic cytokines did not mediate a stress interview-induced hyperthermic response in a patient with psychogenic fever: a case report. Psychosom Med 2009; 71:932-6; PMID:19875636; http://dx.doi.org/ 10.1097/PSY.0b013e3181bfb02b [PubMed] [CrossRef] [Google Scholar]
14. Oka T, Kanemitsu Y, Sudo N, Hayashi H, Oka K. Psychological stress contributed to the development of low-grade fever in a patient with chronic fatigue syndrome: a case report. Biopsychosoc Med 2013; 7:7; PMID:23497734; http://dx.doi.org/ 10.1186/1751-0759-7-7 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Biopsychosoc Med 2013; 7:7; PMID:23497734; http://dx.doi.org/ 10.1186/1751-0759-7-7 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Oka T, Oka K. Age and gender differences of psychogenic fever: a review of the Japanese literature. Biopsychosoc Med 2007; 1:11; PMID:17511878; http://dx.doi.org/ 10.1186/1751-0759-1-11 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Kaneda Y, Tsuji S, Oka T. Age distribution and gender differences in psychogenic fever patients. Biopsychosoc Med 2009; 3:6; PMID:19379524; http://dx.doi.org/ 10.1186/1751-0759-3-6 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
17. Friedmann M, Kohnstmann O. Zur Pathogenese und Psychotherapie bei Basodowsher Krankheit. Ztschr f d ges Neurol u Psychiat 1914; 23:357; http://dx.doi.org/ 10.1007/BF02867687 [CrossRef] [Google Scholar]
18. Falcon-Lesses M, Proger SH. Psychogenic fever. N Engl J Med 1930; 203:1034-6; http://dx.doi.org/ 10.1056/NEJM193011202032113 [CrossRef] [Google Scholar]
19. Bakwin H. Psychogenic fever in infants. Am J Dis Child 1944; 67:176-81 [Google Scholar]
Bakwin H. Psychogenic fever in infants. Am J Dis Child 1944; 67:176-81 [Google Scholar]
20. Kintner AR, Rowntree LG. Long continued, low grade, idiopathic fever. JAMA 1934;102:889-92; http://dx.doi.org/ 10.1001/jama.1934.02750120001001 [CrossRef] [Google Scholar]
21. Wolf S, Wolf HD. Intermittent fever of unknown origin. Arch Internal Med 1942;70:293-302; http://dx.doi.org/ 10.1001/archinte.1942.00200200113007 [CrossRef] [Google Scholar]
22. Singer R, Harker CT, Vander AJ, Kluger MJ. Hyperthermia induced by open-field stress is blocked by salicylate. Physiol Behav 1986; 36:1179-82; PMID:3725924; http://dx.doi.org/ 10.1016/0031-9384(86)90497-X [PubMed] [CrossRef] [Google Scholar]
23. Soszynski D, Kozak W, Kluger MJ. Endotoxin tolerance does not alter open field-induced fever in rats. Physiol Behav 1998; 63:689-92; PMID:9523916; http://dx.doi.org/ 10.1016/S0031-9384(97)00515-5 [PubMed] [CrossRef] [Google Scholar]
24. Butterweck V, Prinz S, Schwaninger M. The role of interleukin-6 in stress-induced hyperthermia and emotional behaviour in mice. Behav Brain Res 2003; 144:49-56; PMID:12946594; http://dx.doi.org/ 10.1016/S0166-4328(03)00059-7 [PubMed] [CrossRef] [Google Scholar]
Behav Brain Res 2003; 144:49-56; PMID:12946594; http://dx.doi.org/ 10.1016/S0166-4328(03)00059-7 [PubMed] [CrossRef] [Google Scholar]
25. Long NC, Vander AJ, Kunkel SL, Kluger MJ. Antiserum against tumor necrosis factor increases stress hyperthermia in rats. Am J Physiol 1990; 258:R591-5; PMID:2316707 [PubMed] [Google Scholar]
26. Morimoto A, Nakamori T, Morimoto K, Tan N, Murakami N. The central role of corticotrophin-releasing factor (CRF-41) in psychological stress in rats. J Physiol 1993; 460:221-9; PMID:8487193; http://dx.doi.org/ 10.1113/jphysiol.1993.sp019468 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
27. Oka T, Oka K, Kobayashi T, Sugimoto Y, Ichikawa A, Ushikubi F, Narumiya S, Saper CB. Characteristics of thermoregulatory and febrile responses in mice deficient in prostaglandin EP1 and EP3 receptors. J Physiol 2003; 551:945-54; PMID:12837930; http://dx.doi.org/ 10.1113/jphysiol.2003.048140 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Shibata H, Nagasaka T. Contribution of nonshivering thermogenesis to stress-induced hyperthermia in rats. Jpn J Physiol 1982; 32:991-5; PMID:7169705; http://dx.doi.org/ 10.2170/jjphysiol.32.991 [PubMed] [CrossRef] [Google Scholar]
Shibata H, Nagasaka T. Contribution of nonshivering thermogenesis to stress-induced hyperthermia in rats. Jpn J Physiol 1982; 32:991-5; PMID:7169705; http://dx.doi.org/ 10.2170/jjphysiol.32.991 [PubMed] [CrossRef] [Google Scholar]
29. Shibata H, Nagasaka T. Role of sympathetic nervous system in immobilization- and cold-induced brown adipose tissue thermogenesis in rats. Jpn J Physiol 1984; 34:103-11; PMID:6727066; http://dx.doi.org/ 10.2170/jjphysiol.34.103 [PubMed] [CrossRef] [Google Scholar]
30. Gao B, Kikuchi-Utsumi K, Ohinata H, Hashimoto M, Kuroshima A. Repeated immobilization stress increases uncoupling protein 1 expression and activity in Wistar rats. Jpn J Physiol 2003; 53:205-13; PMID:14529581; http://dx.doi.org/ 10.2170/jjphysiol.53.205 [PubMed] [CrossRef] [Google Scholar]
31. Ootsuka Y, Blessing WW, Nalivaiko E. Selective blockade of 5-HT2A receptors attenuates the increased temperature response in brown adipose tissue to restraint stress in rats. Stress 2008; 11:125-33; PMID:18311601; http://dx. doi.org/ 10.1080/10253890701638303 [PubMed] [CrossRef] [Google Scholar]
doi.org/ 10.1080/10253890701638303 [PubMed] [CrossRef] [Google Scholar]
32. Borsini F, Lecci A, Volterra G, Meli A. A model to measure anticipatory anxiety in mice? Psychopharmacology (Berl) 1989; 98:207-11; PMID:2502791; http://dx.doi.org/ 10.1007/BF00444693 [PubMed] [CrossRef] [Google Scholar]
33. Zethof TJ, Van der Heyden JA, Tolboom JT, Olivier B. Stress-induced hyperthermia as a putative anxiety model. Eur J Pharmacol 1995; 294:125-35; PMID:8788424; http://dx.doi.org/ 10.1016/0014-2999(95)00520-X [PubMed] [CrossRef] [Google Scholar]
34. Vinkers CH, van Bogaert MJ, Klanker M, Korte SM, Oosting R, Hanania T, Hopkins SC, Olivier B, Groenink L. Translational aspects of pharmacological research into anxiety disorders: the stress-induced hyperthermia (SIH) paradigm. Eur J Pharmacol 2008; 585:407-25; PMID:18420191; http://dx.doi.org/ 10.1016/j.ejphar.2008.02.097 [PubMed] [CrossRef] [Google Scholar]
35. Beig MI, Baumert M, Walker FR, Day TA, Nalivaiko E. Blockade of 5-HT2A receptors suppresses hyperthermic but not cardiovascular responses to psychosocial stress in rats. Neuroscience 2009;159: 1185-91; PMID:19356699; http://dx.doi.org/ 10.1016/j.neuroscience.2009.01.038 [PubMed] [CrossRef] [Google Scholar]
Neuroscience 2009;159: 1185-91; PMID:19356699; http://dx.doi.org/ 10.1016/j.neuroscience.2009.01.038 [PubMed] [CrossRef] [Google Scholar]
36. Hayashida S, Oka T, Mera T, Tsuji S. Repeated social defeat stress induces chronic hyperthermia in rats. Physiol Behav 2010; 101:124-31; PMID:20438740; http://dx.doi.org/ 10.1016/j.physbeh.2010.04.027 [PubMed] [CrossRef] [Google Scholar]
37. Lkhagvasuren B, Nakamura Y, Oka T, Sudo N, Nakamura K. Social defeat stress induces hyperthermia through activation of thermoregulatory sympathetic premotor neurons in the medullary raphe region. Eur J Neurosci 2011; 34:1442-52; PMID:21978215; http://dx.doi.org/ 10.1111/j.1460-9568.2011.07863.x [PubMed] [CrossRef] [Google Scholar]
38. Lkhagvasuren B, Oka T, Nakamura Y, Hayashi H, Sudo N, Nakamura K. Distribution of Fos-immunoreactive cells in rat forebrain and midbrain following social defeat stress and diazepam treatment. Neuroscience 2014; 272:34-57; PMID:24797330; http://dx.doi.org/ 10.1016/j. neuroscience.2014.04.047 [PubMed] [CrossRef] [Google Scholar]
neuroscience.2014.04.047 [PubMed] [CrossRef] [Google Scholar]
39. Mohammed M, Ootsuka Y, Blessing W. Brown adipose tissue thermogenesis contributes to emotional hyperthermia in a resident rat suddenly confronted with an intruder rat. Am J Physiol Regul Integr Comp Physiol 2014; 306:R394-400; PMID:24452545; http://dx.doi.org/ 10.1152/ajpregu.00475.2013 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Yokoi Y. Effect of ambient temperature upon emotional hyperthermia and hypothermia in rabbits. J Appl Physiol 1966; 21:1795-8; PMID:5929304 [PubMed] [Google Scholar]
41. Snow AE, Horita A. Interaction of apomorphine and stressors in the production of hyperthermia in the rabbit. J Pharmacol Exp Ther 1982; 220:335-9; PMID:7199085 [PubMed] [Google Scholar]
42. Kohlhause S, Hoffmann K, Schlumbohm C, Fuchs E, Flugge G. Nocturnal hyperthermia induced by social stress in male tree shrews: relation to low testosterone and effects of age. Physiol Behav 2011; 104:786-95; PMID:21827778; http://dx.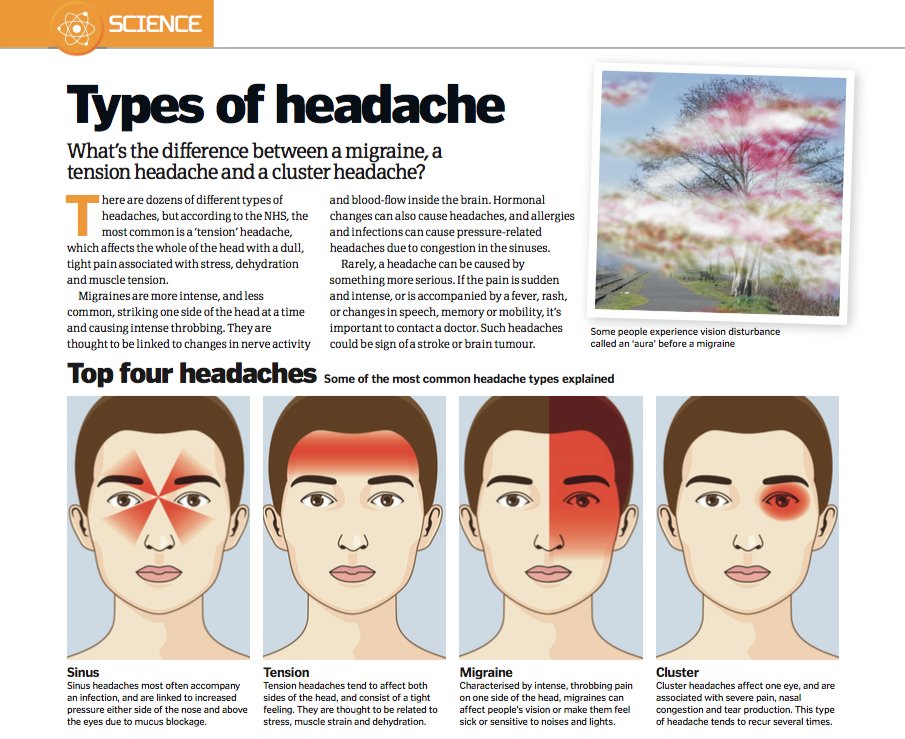 doi.org/ 10.1016/j.physbeh.2011.07.023 [PubMed] [CrossRef] [Google Scholar]
doi.org/ 10.1016/j.physbeh.2011.07.023 [PubMed] [CrossRef] [Google Scholar]
43. Schmelting B, Corbach-Sohle S, Kohlhause S, Schlumbohm C, Flugge G, Fuchs E. Agomelatine in the tree shrew model of depression: effects on stress-induced nocturnal hyperthermia and hormonal status. Eur Neuropsychopharmacol 2014; 24:437-47; PMID:23978391; http://dx.doi.org/ 10.1016/j.euroneuro.2013.07.010 [PubMed] [CrossRef] [Google Scholar]
44. Pedernera-Romano C, Ruiz de la Torre JL, Badiella L, Manteca X. Effect of perphenazine enanthate on open-field test behaviour and stress-induced hyperthermia in domestic sheep. Pharmacol Biochem Behav 2010; 94:329-32; PMID:19799930; http://dx.doi.org/ 10.1016/j.pbb.2009.09.013 [PubMed] [CrossRef] [Google Scholar]
45. Muchlinski AE, Baldwin BC, Padick DA, Lee BY, Salguero HS, Gramajo R. California ground squirrel body temperature regulation patterns measured in the laboratory and in the natural environment. Comp Biochem Physiol A Mol Integr Physiol 1998; 120:365-72; PMID:9773514; http://dx. doi.org/ 10.1016/S1095-6433(98)10037-5 [PubMed] [CrossRef] [Google Scholar]
doi.org/ 10.1016/S1095-6433(98)10037-5 [PubMed] [CrossRef] [Google Scholar]
46. Lee BY, Padick DA, Muchlinski AE. Stress fever magnitude in laboratory-maintained California ground squirrels varies with season. Comp Biochem Physiol A Mol Integr Physiol 2000; 125:325-30; PMID:10794961; http://dx.doi.org/ 10.1016/S1095-6433(00)00157-4 [PubMed] [CrossRef] [Google Scholar]
47. Parr LA, Hopkins WD. Brain temperature asymmetries and emotional perception in chimpanzees, Pan troglodytes. Physiol Behav 2000; 71:363-71; PMID:11150569; http://dx.doi.org/ 10.1016/S0031-9384(00)00349-8 [PubMed] [CrossRef] [Google Scholar]
48. Meyer LC, Fick L, Matthee A, Mitchell D, Fuller A. Hyperthermia in captured impala (Aepyceros melampus): a fright not flight response. J Wildl Dis 2008; 44:404-16; PMID:18436672; http://dx.doi.org/ 10.7589/0090-3558-44.2.404 [PubMed] [CrossRef] [Google Scholar]
49. Gray DA, Maloney SK, Kamerman PR. Restraint increases afebrile body temperature but attenuates fever in Pekin ducks (Anas platyrhynchos). Am J Physiol Regul Integr Comp Physiol 2008; 294:R1666-71; PMID:18337310; http://dx.doi.org/ 10.1152/ajpregu.00865.2007 [PubMed] [CrossRef] [Google Scholar]
Am J Physiol Regul Integr Comp Physiol 2008; 294:R1666-71; PMID:18337310; http://dx.doi.org/ 10.1152/ajpregu.00865.2007 [PubMed] [CrossRef] [Google Scholar]
50. Bittencourt Mde A, Melleu FF, Marino-Neto J. Stress-induced core temperature changes in pigeons (Columba livia). Physiol Behav 2015; 139:449-58; PMID:25479572; http://dx.doi.org/ 10.1016/j.physbeh.2014.11.067 [PubMed] [CrossRef] [Google Scholar]
51. Oka T, Oka K, Hori T. Mechanisms and mediators of psychological stress-induced rise in core temperature. Psychosom Med 2001; 63:476-86; PMID:11382276; http://dx.doi.org/ 10.1097/00006842-200105000-00018 [PubMed] [CrossRef] [Google Scholar]
52. Vinkers CH, Groenink L, van Bogaert MJ, Westphal KG, Kalkman CJ, van Oorschot R, Oosting RS, Olivier B, Korte SM. Stress-induced hyperthermia and infection-induced fever: two of a kind? Physiol Behav 2009; 98:37-43; PMID:19375439; http://dx.doi.org/ 10.1016/j.physbeh.2009.04.004 [PubMed] [CrossRef] [Google Scholar]
53. Ivanov AI, Pero RS, Scheck AC, Romanovsky AA. Prostaglandin E(2)-synthesizing enzymes in fever: differential transcriptional regulation. Am J Physiol Regul Integr Comp Physiol 2002; 283:R1104-17; PMID:12376404; http://dx.doi.org/ 10.1152/ajpregu.00347.2002 [PubMed] [CrossRef] [Google Scholar]
Prostaglandin E(2)-synthesizing enzymes in fever: differential transcriptional regulation. Am J Physiol Regul Integr Comp Physiol 2002; 283:R1104-17; PMID:12376404; http://dx.doi.org/ 10.1152/ajpregu.00347.2002 [PubMed] [CrossRef] [Google Scholar]
54. Ivanov AI, Romanovsky AA. Prostaglandin E2 as a mediator of fever: synthesis and catabolism. Front Biosci 2004; 9:1977-93; PMID:14977603; http://dx.doi.org/ 10.2741/1383 [PubMed] [CrossRef] [Google Scholar]
55. Steiner AA, Ivanov AI, Serrats J, Hosokawa H, Phayre AN, Robbins JR, Roberts JL, Kobayashi S, Matsumura K, Sawchenko PE, et al.. Cellular and molecular bases of the initiation of fever. PLoS Biol 2006; 4:e284; PMID:16933973; http://dx.doi.org/ 10.1371/journal.pbio.0040284 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
56. Romanovsky AA, Steiner AA, Matsumura K. Cells that trigger fever. Cell Cycle 2006; 5:2195-7; PMID:16969135; http://dx.doi.org/ 10.4161/cc.5.19.3321 [PubMed] [CrossRef] [Google Scholar]
57. Yamagata K, Matsumura K, Inoue W, Shiraki T, Suzuki K, Yasuda S, Sugiura H, Cao C, Watanabe Y, Kobayashi S. Coexpression of microsomal-type prostaglandin E synthase with cyclooxygenase-2 in brain endothelial cells of rats during endotoxin-induced fever. J Neurosci 2001; 21:2669-77; PMID:11306620 [PMC free article] [PubMed] [Google Scholar]
Yamagata K, Matsumura K, Inoue W, Shiraki T, Suzuki K, Yasuda S, Sugiura H, Cao C, Watanabe Y, Kobayashi S. Coexpression of microsomal-type prostaglandin E synthase with cyclooxygenase-2 in brain endothelial cells of rats during endotoxin-induced fever. J Neurosci 2001; 21:2669-77; PMID:11306620 [PMC free article] [PubMed] [Google Scholar]
58. Engblom D, Saha S, Engstrom L, Westman M, Audoly LP, Jakobsson PJ, Blomqvist A. Microsomal prostaglandin E synthase-1 is the central switch during immune-induced pyresis. Nat Neurosci 2003; 6:1137-8; PMID:14566340; http://dx.doi.org/ 10.1038/nn1137 [PubMed] [CrossRef] [Google Scholar]
59. Schiltz JC, Sawchenko PE. Signaling the brain in systemic inflammation: the role of perivascular cells. Front Biosci 2003; 8:s1321-9; PMID:12957837; http://dx.doi.org/ 10.2741/1211 [PubMed] [CrossRef] [Google Scholar]
60. Kluger MJ. Fever: role of pyrogens and cryogens. Physiol Rev 1991; 71:93-127; PMID:1986393 [PMC free article] [PubMed] [Google Scholar]
61. Leon LR. Invited review: cytokine regulation of fever: studies using gene knockout mice. J Appl Physiol 2002; 92:2648-55; PMID:12015385; http://dx.doi.org/ 10.1152/japplphysiol.01005.2001 [PubMed] [CrossRef] [Google Scholar]
Leon LR. Invited review: cytokine regulation of fever: studies using gene knockout mice. J Appl Physiol 2002; 92:2648-55; PMID:12015385; http://dx.doi.org/ 10.1152/japplphysiol.01005.2001 [PubMed] [CrossRef] [Google Scholar]
62. Nakamura K, Matsumura K, Hubschle T, Nakamura Y, Hioki H, Fujiyama F, Boldogkoi Z, Konig M, Thiel HJ, Gerstberger R, et al.. Identification of sympathetic premotor neurons in medullary raphe regions mediating fever and other thermoregulatory functions. J Neurosci 2004; 24:5370-80; PMID:15190110; http://dx.doi.org/ 10.1523/JNEUROSCI.1219-04.2004 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
63. Rathner JA, Madden CJ, Morrison SF. Central pathway for spontaneous and prostaglandin E2-evoked cutaneous vasoconstriction. Am J Physiol Regul Integr Comp Physiol 2008; 295:R343-54; PMID:18463193; http://dx.doi.org/ 10.1152/ajpregu.00115.2008 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
64. Kerman IA, Enquist LW, Watson SJ, Yates BJ.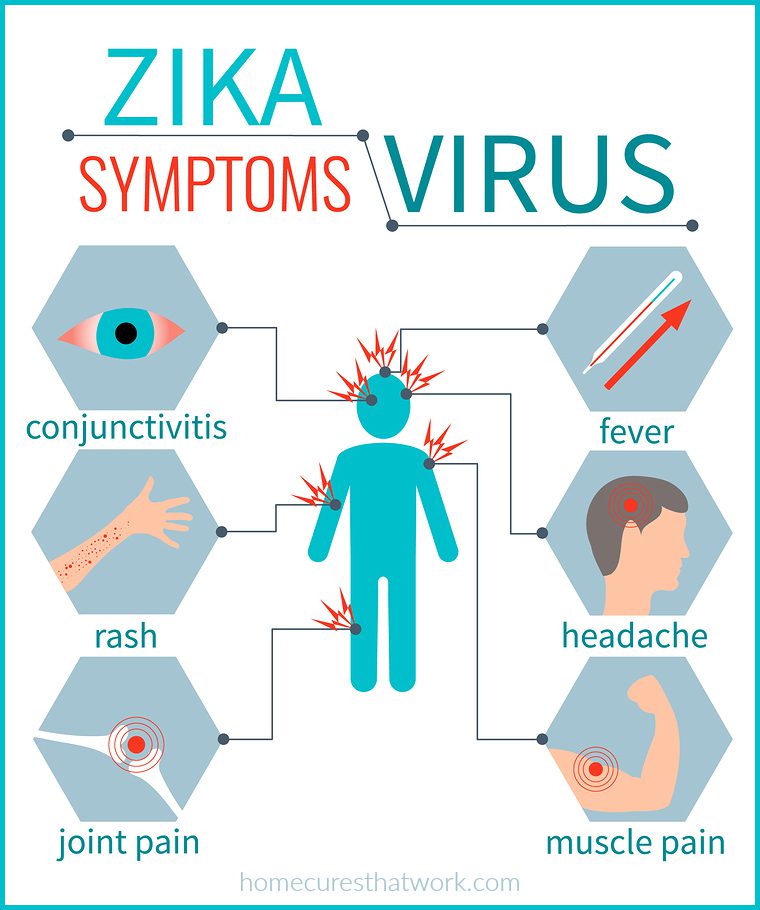 Brainstem substrates of sympatho-motor circuitry identified using trans-synaptic tracing with pseudorabies virus recombinants. J Neurosci 2003; 23:4657-66; PMID:12805305 [PMC free article] [PubMed] [Google Scholar]
Brainstem substrates of sympatho-motor circuitry identified using trans-synaptic tracing with pseudorabies virus recombinants. J Neurosci 2003; 23:4657-66; PMID:12805305 [PMC free article] [PubMed] [Google Scholar]
65. Tanaka M, Owens NC, Nagashima K, Kanosue K, McAllen RM. Reflex activation of rat fusimotor neurons by body surface cooling, and its dependence on the medullary raphe. J Physiol 2006; 572:569-83; PMID:16484305; http://dx.doi.org/ 10.1113/jphysiol.2005.102400 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
66. Nakamura K, Morrison SF. Central efferent pathways for cold-defensive and febrile shivering. J Physiol 2011; 589:3641-58; PMID:21610139; http://dx.doi.org/ 10.1113/jphysiol.2011.210047 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
67. Nakamura K, Matsumura K, Kaneko T, Kobayashi S, Katoh H, Negishi M. The rostral raphe pallidus nucleus mediates pyrogenic transmission from the preoptic area. J Neurosci 2002; 22:4600-10; PMID:12040067 [PMC free article] [PubMed] [Google Scholar]
68. Lazarus M, Yoshida K, Coppari R, Bass CE, Mochizuki T, Lowell BB, Saper CB. EP3 prostaglandin receptors in the median preoptic nucleus are critical for fever responses. Nat Neurosci 2007; 10:1131-3; PMID:17676060; http://dx.doi.org/ 10.1038/nn1949 [PubMed] [CrossRef] [Google Scholar]
Lazarus M, Yoshida K, Coppari R, Bass CE, Mochizuki T, Lowell BB, Saper CB. EP3 prostaglandin receptors in the median preoptic nucleus are critical for fever responses. Nat Neurosci 2007; 10:1131-3; PMID:17676060; http://dx.doi.org/ 10.1038/nn1949 [PubMed] [CrossRef] [Google Scholar]
69. Morrison SF, Nakamura K. Central neural pathways for thermoregulation. Front Biosci 2011; 16:74-104; PMID:21196160; http://dx.doi.org/ 10.2741/3677 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
70. DiMicco JA, Sarkar S, Zaretskaia MV, Zaretsky DV. Stress-induced cardiac stimulation and fever: common hypothalamic origins and brainstem mechanisms. Auton Neurosci 2006; 126–127:106-19; PMID:16580890; http://dx.doi.org/ 10.1016/j.autneu.2006.02.010 [PubMed] [CrossRef] [Google Scholar]
71. Dimicco JA, Zaretsky DV. The dorsomedial hypothalamus: a new player in thermoregulation. Am J Physiol Regul Integr Comp Physiol 2007; 292:R47-63; PMID:16959861; http://dx.doi.org/ 10.1152/ajpregu.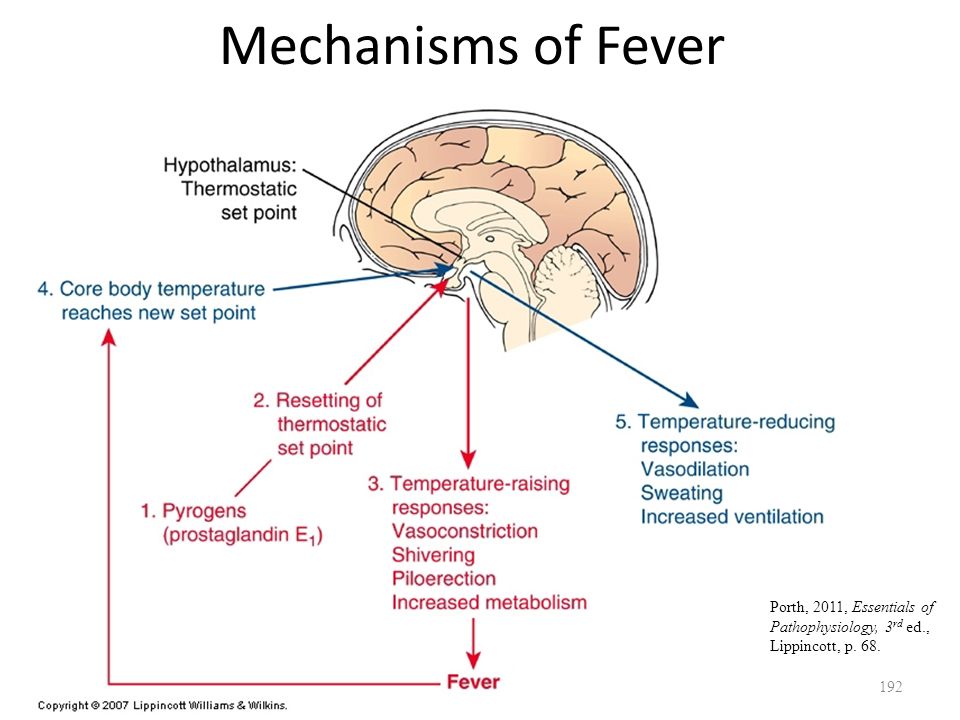 00498.2006 [PubMed] [CrossRef] [Google Scholar]
00498.2006 [PubMed] [CrossRef] [Google Scholar]
72. Kataoka N, Hioki H, Kaneko T, Nakamura K. Psychological stress activates a dorsomedial hypothalamus-medullary raphe circuit driving brown adipose tissue thermogenesis and hyperthermia. Cell Metab 2014; 20:346-58; PMID:2498183715677520 [PubMed] [Google Scholar]
73. Saha S, Engstrom L, Mackerlova L, Jakobsson PJ, Blomqvist A. Impaired febrile responses to immune challenge in mice deficient in microsomal prostaglandin E synthase-1. Am J Physiol Regul Integr Comp Physiol 2005; 288:R1100-7; PMID:15677520; http://dx.doi.org/ 10.1152/ajpregu.00872.2004 [PubMed] [CrossRef] [Google Scholar]
74. Lecci A, Borsini F, Volterra G, Meli A. Pharmacological validation of a novel animal model of anticipatory anxiety in mice. Psychopharmacology (Berl) 1990; 101:255-61; PMID:1971957; http://dx.doi.org/ 10.1007/BF02244136 [PubMed] [CrossRef] [Google Scholar]
75. Bouwknecht JA, Hijzen TH, van der Gugten J, Maes RA, Olivier B. Stress-induced hyperthermia in mice: effects of flesinoxan on heart rate and body temperature. Eur J Pharmacol 2000; 400:59-66; PMID:10913585; http://dx.doi.org/ 10.1016/S0014-2999(00)00387-3 [PubMed] [CrossRef] [Google Scholar]
Eur J Pharmacol 2000; 400:59-66; PMID:10913585; http://dx.doi.org/ 10.1016/S0014-2999(00)00387-3 [PubMed] [CrossRef] [Google Scholar]
76. Olivier B, Bouwknecht JA, Pattij T, Leahy C, van Oorschot R, Zethof TJ. GABAA-benzodiazepine receptor complex ligands and stress-induced hyperthermia in singly housed mice. Pharmacol Biochem Behav 2002; 72:179-88; PMID:11900786; http://dx.doi.org/ 10.1016/S0091-3057(01)00759-6 [PubMed] [CrossRef] [Google Scholar]
77. Pecoraro N, de Jong H, Ginsberg AB, Dallman MF. Lesions of the medial prefrontal cortex enhance the early phase of psychogenic fever to unexpected sucrose concentration reductions, promote recovery from negative contrast and enhance spontaneous recovery of sucrose-entrained anticipatory activity. Neuroscience 2008; 153:901-17; PMID:18455879; http://dx.doi.org/ 10.1016/j.neuroscience.2008.03.043 [PubMed] [CrossRef] [Google Scholar]
78. Pae YS, Lai H, Horita A. Hyperthermia in the rat from handling stress blocked by naltrexone injected into the preoptic-anterior hypothalamus.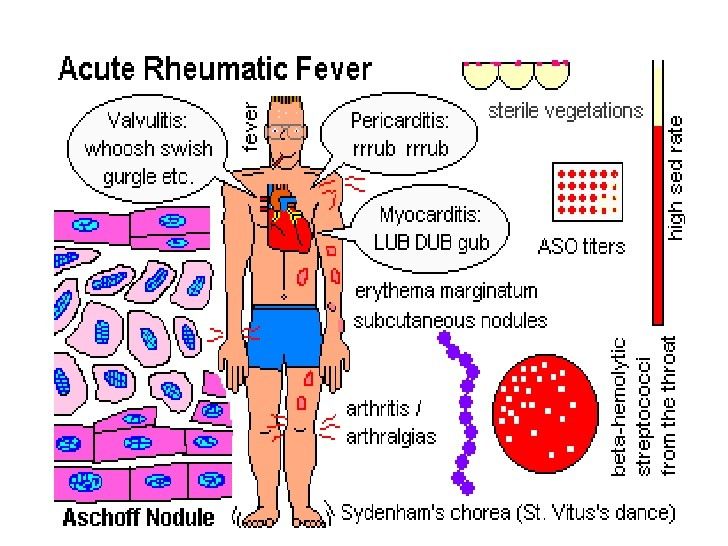 Pharmacol Biochem Behav 1985; 22:337-9; PMID:4039067; http://dx.doi.org/ 10.1016/0091-3057(85)90400-9 [PubMed] [CrossRef] [Google Scholar]
Pharmacol Biochem Behav 1985; 22:337-9; PMID:4039067; http://dx.doi.org/ 10.1016/0091-3057(85)90400-9 [PubMed] [CrossRef] [Google Scholar]
79. Egawa M, Yoshimatsu H, Bray GA. Preoptic area injection of corticotropin-releasing hormone stimulates sympathetic activity. Am J Physiol 1990; 259:R799-806; PMID:2221147 [PubMed] [Google Scholar]
80. Vinkers CH, Bijlsma EY, Houtepen LC, Westphal KG, Veening JG, Groenink L, Olivier B. Medial amygdala lesions differentially influence stress responsivity and sensorimotor gating in rats. Physiol Behav 2010; 99:395-401; PMID:20006965; http://dx.doi.org/ 10.1016/j.physbeh.2009.12.006 [PubMed] [CrossRef] [Google Scholar]
81. Ootsuka Y, Mohammed M. Activation of the habenula complex evokes autonomic physiological responses similar to those associated with emotional stress. Physiol Rep 2015; 3:e12297; PMID:25677551; http://dx.doi.org/ 10.14814/phy2.12297 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
82. Zhang W, Sunanaga J, Takahashi Y, Mori T, Sakurai T, Kanmura Y, Kuwaki T.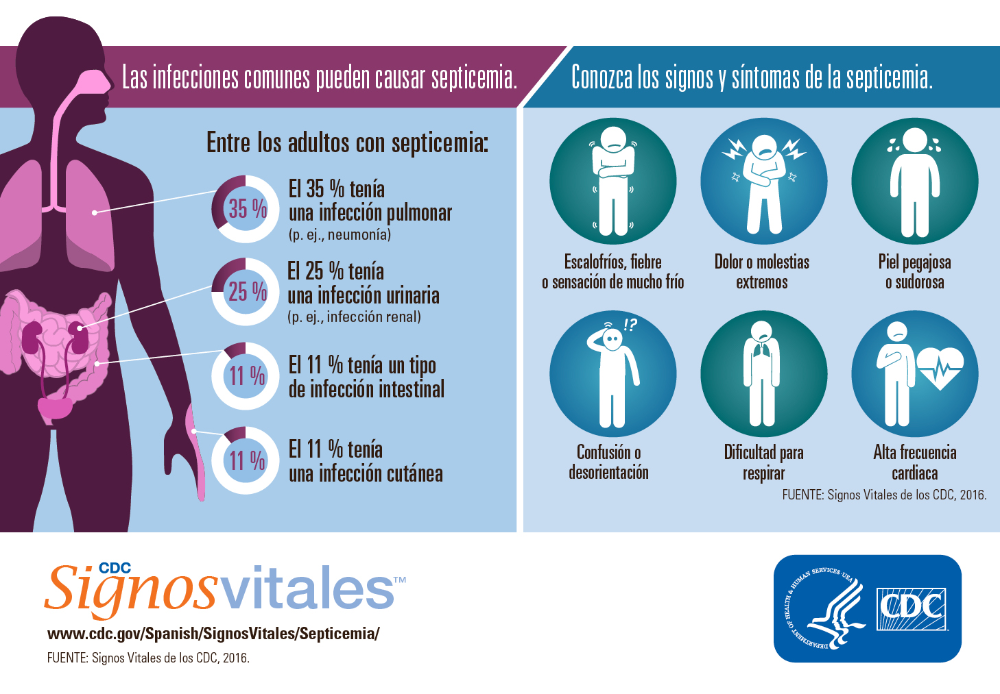 Orexin neurons are indispensable for stress-induced thermogenesis in mice. J Physiol 2010; 588:4117-29; PMID:20807795; http://dx.doi.org/ 10.1113/jphysiol.2010.195099 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Orexin neurons are indispensable for stress-induced thermogenesis in mice. J Physiol 2010; 588:4117-29; PMID:20807795; http://dx.doi.org/ 10.1113/jphysiol.2010.195099 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
83. Eikelboom R. Learned anticipatory rise in body temperature due to handling. Physiol Behav 1986; 37:649-53; PMID:3749329; http://dx.doi.org/ 10.1016/0031-9384(86)90299-4 [PubMed] [CrossRef] [Google Scholar]
84. Pardon MC, Kendall DA, Perez-Diaz F, Duxon MS, Marsden CA. Repeated sensory contact with aggressive mice rapidly leads to an anticipatory increase in core body temperature and physical activity that precedes the onset of aversive responding. Eur J Neurosci 2004; 20:1033-50; PMID:15305872; http://dx.doi.org/ 10.1111/j.1460-9568.2004.03549.x [PubMed] [CrossRef] [Google Scholar]
85. Kant GJ, Bauman RA, Pastel RH, Myatt CA, Closser-Gomez E, D'Angelo CP. Effects of controllable vs. uncontrollable stress on circadian temperature rhythms. Physiol Behav 1991; 49:625-30; PMID:2062941; http://dx.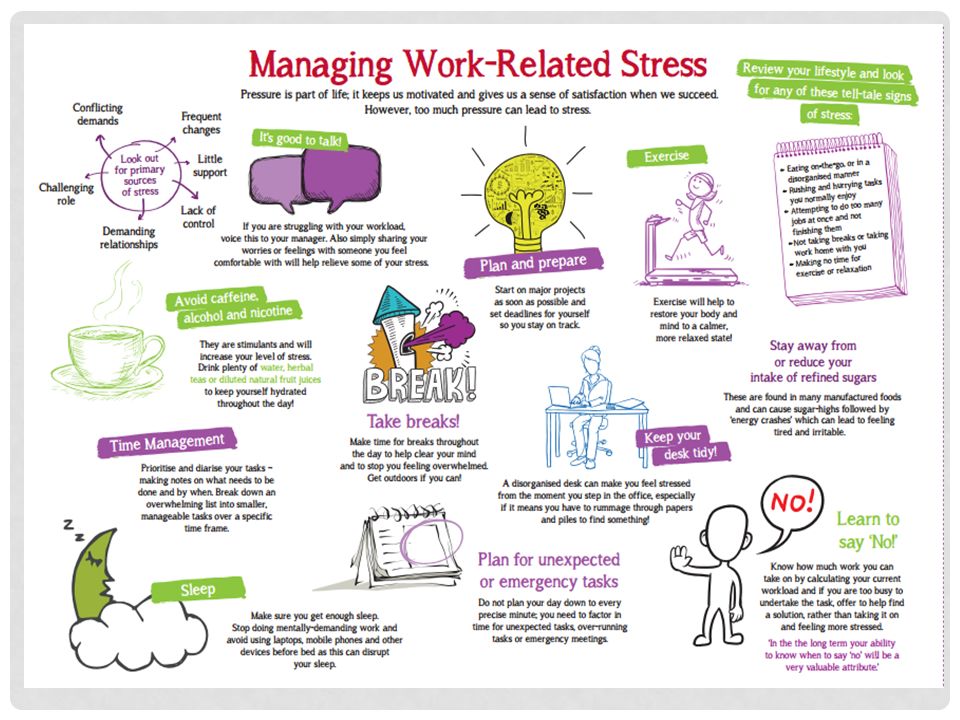 doi.org/ 10.1016/0031-9384(91)90289-Z [PubMed] [CrossRef] [Google Scholar]
doi.org/ 10.1016/0031-9384(91)90289-Z [PubMed] [CrossRef] [Google Scholar]
86. Endo Y, Shiraki K. Behavior and body temperature in rats following chronic foot shock or psychological stress exposure. Physiol Behav 2000; 71:263-8; PMID:11150557; http://dx.doi.org/ 10.1016/S0031-9384(00)00339-5 [PubMed] [CrossRef] [Google Scholar]
87. Bhatnagar S, Vining C, Iyer V, Kinni V. Changes in hypothalamic-pituitary-adrenal function, body temperature, body weight and food intake with repeated social stress exposure in rats. J Neuroendocrinol 2006; 18:13-24; PMID:16451216; http://dx.doi.org/ 10.1111/j.1365-2826.2005.01375.x [PubMed] [CrossRef] [Google Scholar]
88. Nozu T, Okano S, Kikuchi K, Yahata T, Kuroshima A. Effect of immobilization stress on in vitro and in vivo thermogenesis of brown adipose tissue. Jpn J Physiol 1992; 42:299-308; PMID:1434095; http://dx.doi.org/ 10.2170/jjphysiol.42.299 [PubMed] [CrossRef] [Google Scholar]
89. Rygula R, Abumaria N, Havemann-Reinecke U, Ruther E, Hiemke C, Zernig G, Fuchs E, Flugge G.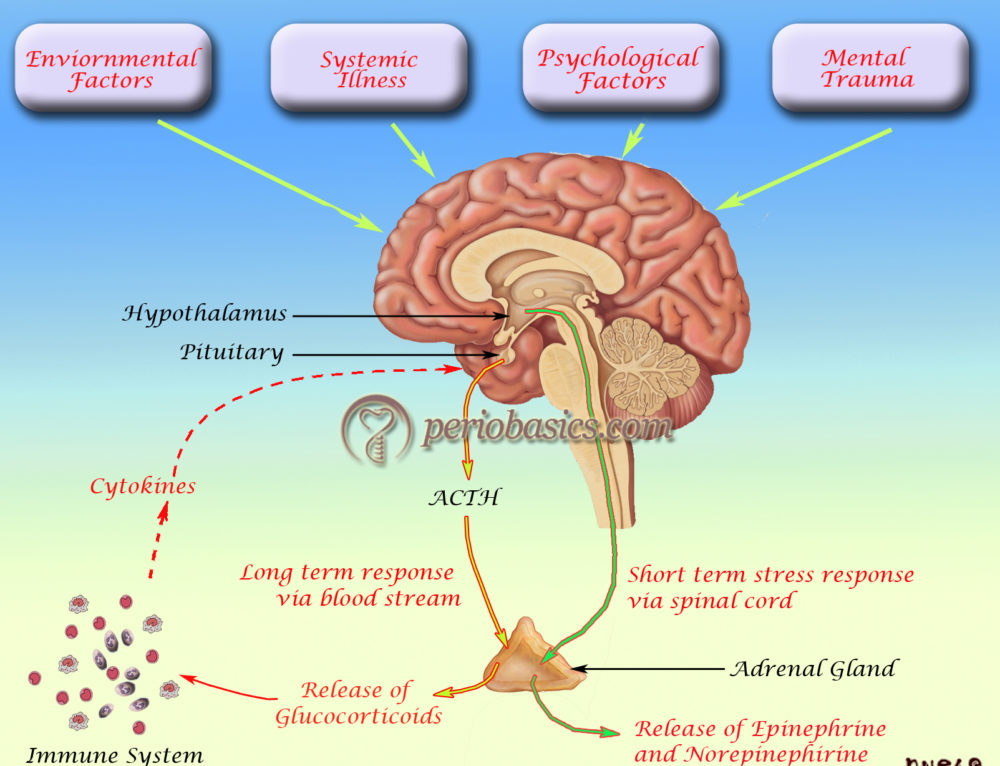 Pharmacological validation of a chronic social stress model of depression in rats: effects of reboxetine, haloperidol and diazepam. Behav Pharmacol 2008; 19:183-96; PMID:18469536; http://dx.doi.org/ 10.1097/FBP.0b013e3282fe8871 [PubMed] [CrossRef] [Google Scholar]
Pharmacological validation of a chronic social stress model of depression in rats: effects of reboxetine, haloperidol and diazepam. Behav Pharmacol 2008; 19:183-96; PMID:18469536; http://dx.doi.org/ 10.1097/FBP.0b013e3282fe8871 [PubMed] [CrossRef] [Google Scholar]
90. Marks A, Vianna DM, Carrive P. Nonshivering thermogenesis without interscapular brown adipose tissue involvement during conditioned fear in the rat. Am J Physiol Regul Integr Comp Physiol 2009; 296:R1239-47; PMID:19211724; http://dx.doi.org/ 10.1152/ajpregu.90723.2008 [PubMed] [CrossRef] [Google Scholar]
91. Carrive P, Gorissen M. Premotor sympathetic neurons of conditioned fear in the rat. Eur J Neurosci 2008; 28:428-46; PMID:18702716; http://dx.doi.org/ 10.1111/j.1460-9568.2008.06351.x [PubMed] [CrossRef] [Google Scholar]
92. Kuroshima A, Habara Y, Uehara A, Murazumi K, Yahata T, Ohno T. Cross adaption between stress and cold in rats. Pflugers Arch 1984; 402:402-8; PMID:6522247; http://dx.doi.org/ 10.1007/BF00583941 [PubMed] [CrossRef] [Google Scholar]
93. Kuroshima A, Yahata T. Changes in the colonic temperature and metabolism during immobilization stress in repetitively immobilized or cold-acclimated rats. Jpn J Physiol 1985; 35:591-7; PMID:4068366; http://dx.doi.org/ 10.2170/jjphysiol.35.591 [PubMed] [CrossRef] [Google Scholar]
Kuroshima A, Yahata T. Changes in the colonic temperature and metabolism during immobilization stress in repetitively immobilized or cold-acclimated rats. Jpn J Physiol 1985; 35:591-7; PMID:4068366; http://dx.doi.org/ 10.2170/jjphysiol.35.591 [PubMed] [CrossRef] [Google Scholar]
94. Sugama S, Fujita M, Hashimoto M, Conti B. Stress induced morphological microglial activation in the rodent brain: involvement of interleukin-18. Neuroscience 2007; 146:1388-99; PMID:17433555; http://dx.doi.org/ 10.1016/j.neuroscience.2007.02.043 [PubMed] [CrossRef] [Google Scholar]
95. Hinwood M, Morandini J, Day TA, Walker FR. Evidence that microglia mediate the neurobiological effects of chronic psychological stress on the medial prefrontal cortex. Cereb Cortex 2012; 22:1442-54; PMID:21878486; http://dx.doi.org/ 10.1093/cercor/bhr229 [PubMed] [CrossRef] [Google Scholar]
96. Hinwood M, Tynan RJ, Charnley JL, Beynon SB, Day TA, Walker FR. Chronic stress induced remodeling of the prefrontal cortex: structural re-organization of microglia and the inhibitory effect of minocycline. Cereb Cortex 2013; 23:1784-97; PMID:22710611; http://dx.doi.org/ 10.1093/cercor/bhs151 [PubMed] [CrossRef] [Google Scholar]
Cereb Cortex 2013; 23:1784-97; PMID:22710611; http://dx.doi.org/ 10.1093/cercor/bhs151 [PubMed] [CrossRef] [Google Scholar]
97. Johnson JD, Zimomra ZR, Stewart LT. Beta-adrenergic receptor activation primes microglia cytokine production. J Neuroimmunol 2013; 254:161-4; PMID:22944319; http://dx.doi.org/ 10.1016/j.jneuroim.2012.08.007 [PubMed] [CrossRef] [Google Scholar]
98. Oka T, Aou S, Hori T. Intracerebroventricular injection of interleukin-1 β induces hyperalgesia in rats. Brain Res 1993; 624:61-8; PMID:8252417; http://dx.doi.org/ 10.1016/0006-8993(93)90060-Z [PubMed] [CrossRef] [Google Scholar]
99. Oka T, Oka K, Hosoi M, Hori T. Intracerebroventricular injection of interleukin-6 induces thermal hyperalgesia in rats. Brain Res 1995; 692:123-8; PMID:8548295; http://dx.doi.org/ 10.1016/0006-8993(95)00691-I [PubMed] [CrossRef] [Google Scholar]
100. Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol 2006; 27:24-31; PMID:16316783; http://dx.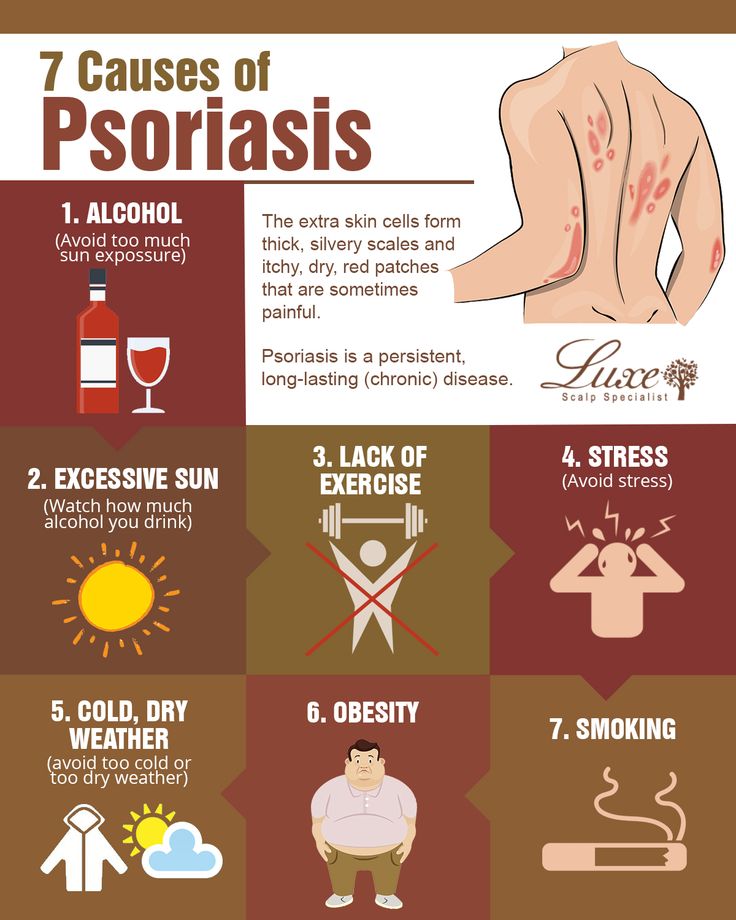 doi.org/ 10.1016/j.it.2005.11.006 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
doi.org/ 10.1016/j.it.2005.11.006 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
101. Song C, Wang H. Cytokines mediated inflammation and decreased neurogenesis in animal models of depression. Prog Neuropsychopharmacol Biol Psychiatry 2011; 35:760-8; PMID:20600462; http://dx.doi.org/ 10.1016/j.pnpbp.2010.06.020 [PubMed] [CrossRef] [Google Scholar]
102. Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 2009; 65:732-41; PMID:19150053; http://dx.doi.org/ 10.1016/j.biopsych.2008.11.029 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
103. Wynn FR. The psychic factor as an element in temperature disturbance. JAMA 1919; 73:31-4; http://dx.doi.org/ 10.1001/jama.1919.02610270035010 [CrossRef] [Google Scholar]
104. Kleitman N. The effect of motion pictures on body temperature. Science 1945; 102:430-1; PMID:17730629; http://dx.doi.org/ 10.1126/science.102.2652.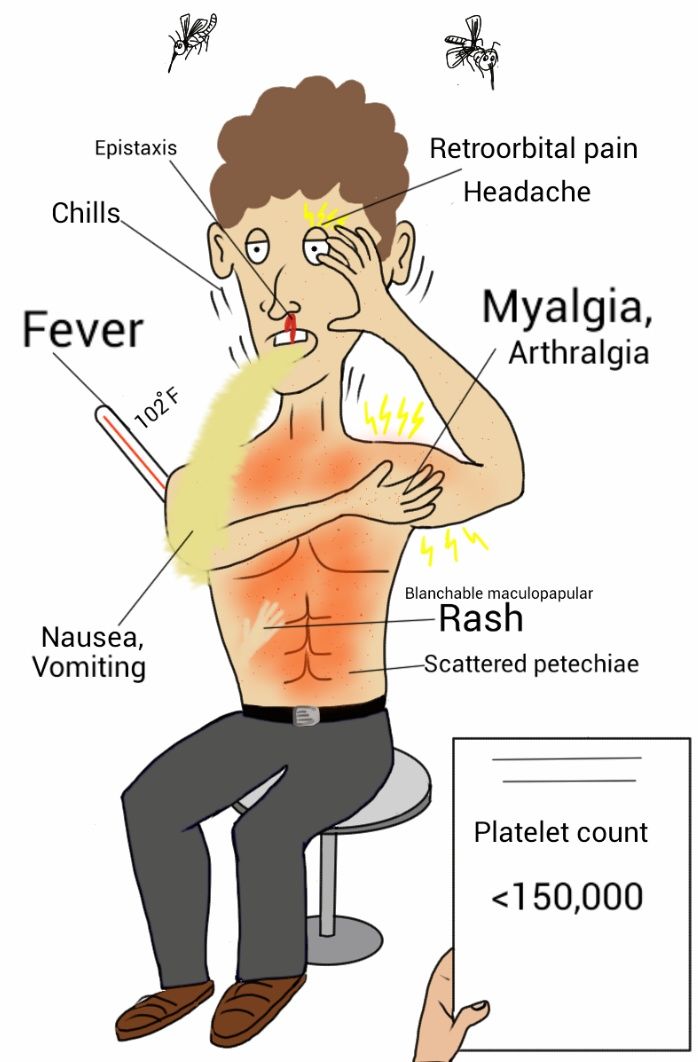 430 [PubMed] [CrossRef] [Google Scholar]
430 [PubMed] [CrossRef] [Google Scholar]
105. Gotsev T, Ivanov A. Psychogenic elevation of body temperature in healthy persons. Acta Physiol Hung 1950; 1:53-62; PMID:14782995 [PubMed] [Google Scholar]
106. Aschoff J, Fatranska M, Gerecke U, Giedke H. Twenty-four-hour rhythms of rectal temperature in humans: effects of sleep-interruptions and of test-sessions. Pflugers Arch 1974; 346:215-22; PMID:4856415; http://dx.doi.org/ 10.1007/BF00595708 [PubMed] [CrossRef] [Google Scholar]
107. Renbourn ET. Body temperature and pulse rate in boys and young men prior to sporting contests. A study of emotional hyperthermia: with a review of the literature. J Psychosom Res 1960; 4:149-75; PMID:14437326; http://dx.doi.org/ 10.1016/0022-3999(60)90008-8 [PubMed] [CrossRef] [Google Scholar]
108. Marazziti D, Di Muro A, Castrogiovanni P. Psychological stress and body temperature changes in humans. Physiol Behav 1992; 52:393-5; PMID:1326118; http://dx.doi.org/ 10.1016/0031-9384(92)90290-I [PubMed] [CrossRef] [Google Scholar]
109. Briese E. Emotional hyperthermia and performance in humans. Physiol Behav 1995; 58:615-8; PMID:8587973; http://dx.doi.org/ 10.1016/0031-9384(95)00091-V [PubMed] [CrossRef] [Google Scholar]
Briese E. Emotional hyperthermia and performance in humans. Physiol Behav 1995; 58:615-8; PMID:8587973; http://dx.doi.org/ 10.1016/0031-9384(95)00091-V [PubMed] [CrossRef] [Google Scholar]
110. Shah SJ, PAtel HM. Effect of examination stress on parameters of autonomic functions in medical students. Int J Sci Res 2014; 3:273-6 [Google Scholar]
111. Vinkers CH, Penning R, Hellhammer J, Verster JC, Klaessens JH, Olivier B, Kalkman CJ. The effect of stress on core and peripheral body temperature in humans. Stress 2013; 16:520-30; PMID:23790072; http://dx.doi.org/ 10.3109/10253890.2013.807243 [PubMed] [CrossRef] [Google Scholar]
112. Oka T, Kaneda Y, Takenaga M, Hayashida S, Tamagawa Y, Kodama N, Tsuji S. Efficacy of paroxetine for treating chronic stress-induced low-grade fever. Jpn J Psychosom Intern Med 2006; 10:5-8 [Google Scholar]
113. Reimann HA. The problem of long, continued, low grade fever. JAMA 1936;107:1089-94; http://dx.doi.org/ 10.1001/jama.1936.02770400001001 [CrossRef] [Google Scholar]
114. Ziegler LH, Cash PT. A study of the influence of emotions and affects on the surface temperature of the human body. Am J Psychiatr 1938;95:677-96; http://dx.doi.org/ 10.1176/ajp.95.3.677 [CrossRef] [Google Scholar]
Ziegler LH, Cash PT. A study of the influence of emotions and affects on the surface temperature of the human body. Am J Psychiatr 1938;95:677-96; http://dx.doi.org/ 10.1176/ajp.95.3.677 [CrossRef] [Google Scholar]
115. Duras FP. Hyperpyrexia due to hysteria. Lancet 1942; 11:39; http://dx.doi.org/ 10.1016/S0140-6736(00)62135-9 [CrossRef] [Google Scholar]
116. Oka T, Oka K. Mechanisms of psychogenic fever. Adv Neuroimmune Biol 2012; 3:3-17 [Google Scholar]
117. Bohorfoush JG, Craig JB, Patterson HS. Catatonia as a cause of fever of undetermined origin. J Med Assoc Ga 1965; 54:324-5; PMID:5887902 [PubMed] [Google Scholar]
118. Buchwald D, Goldenberg DL, Sullivan JL, Komaroff AL. The “chronic, active Epstein-Barr virus infection” syndrome and primary fibromyalgia. Arthritis Rheum 1987; 30:1132-6; PMID:2823835; http://dx.doi.org/ 10.1002/art.1780301007 [PubMed] [CrossRef] [Google Scholar]
119. Enerback S. Human brown adipose tissue. Cell Metab 2010; 11:248-52; PMID:20374955; http://dx.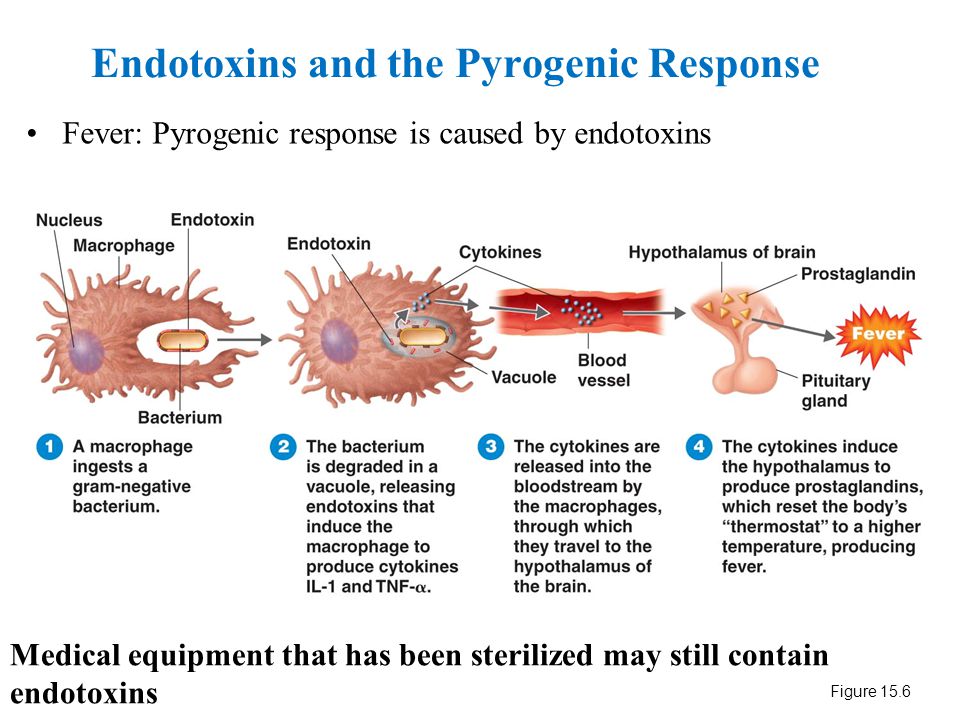 doi.org/ 10.1016/j.cmet.2010.03.008 [PubMed] [CrossRef] [Google Scholar]
doi.org/ 10.1016/j.cmet.2010.03.008 [PubMed] [CrossRef] [Google Scholar]
120. van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JM, Kemerink GJ, Bouvy ND, Schrauwen P, Teule GJ. Cold-activated brown adipose tissue in healthy men. N Engl J Med 2009; 360:1500-8; PMID:19357405; http://dx.doi.org/ 10.1056/NEJMoa0808718 [PubMed] [CrossRef] [Google Scholar]
121. Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB, Kuo FC, Palmer EL, Tseng YH, Doria A, et al.. Identification and importance of brown adipose tissue in adult humans. N Engl J Med 2009; 360:1509-17; PMID:19357406; http://dx.doi.org/ 10.1056/NEJMoa0810780 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
122. Virtanen KA, Lidell ME, Orava J, Heglind M, Westergren R, Niemi T, Taittonen M, Laine J, Savisto NJ, Enerback S, et al.. Functional brown adipose tissue in healthy adults. N Engl J Med 2009; 360:1518-25; PMID:19357407; http://dx.doi.org/ 10.1056/NEJMoa0808949 [PubMed] [CrossRef] [Google Scholar]
123. Saito M, Okamatsu-Ogura Y, Matsushita M, Watanabe K, Yoneshiro T, Nio-Kobayashi J, Iwanaga T, Miyagawa M, Kameya T, Nakada K, et al.. High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes 2009; 58:1526-31; PMID:19401428; http://dx.doi.org/ 10.2337/db09-0530 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Saito M, Okamatsu-Ogura Y, Matsushita M, Watanabe K, Yoneshiro T, Nio-Kobayashi J, Iwanaga T, Miyagawa M, Kameya T, Nakada K, et al.. High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes 2009; 58:1526-31; PMID:19401428; http://dx.doi.org/ 10.2337/db09-0530 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
124. Lkhagvasuren B, Masuno T, Kanemitsu Y, Sudo N, Kubo C, Oka T. Increased prevalence of postural orthostatic tachycardia syndrome in psychogenic fever patients. Psychother Psychosom 2013; 82:269-70; PMID:23735890; http://dx.doi.org/ 10.1159/000345171 [PubMed] [CrossRef] [Google Scholar]
125. Lkhagvasuren B, Tanaka H, Sudo N, Kubo C, Oka T. Characteristics of the orthostatic cardiovascular response in adolescent patients with psychogenic fever. Psychother Psychosom 2014; 83:318-9; PMID:25116930; http://dx.doi.org/ 10.1159/000360999 [PubMed] [CrossRef] [Google Scholar]
126. Oka T. Mechanism and treatment of psychogenic fever. Jpn J Psychosom Intern Med 2005; 9:117-21. [Google Scholar]
Mechanism and treatment of psychogenic fever. Jpn J Psychosom Intern Med 2005; 9:117-21. [Google Scholar]
127. Oka T, Hayashida S, Kaneda Y, Kodama N, Hashimoto T, Tsuji S. Why do chronic stress-induced hyperthermia patients worry about slightly elevated body temperature? Jpn J Psychosom Intern Med 2006; 10:243-6 [Google Scholar]
128. Oka T. Influence of psychological stress on chronic fatigue syndrome. Adv Neuroimmune Biol 2013; 4:301-9 [Google Scholar]
129. Almeida MC, Steiner AA, Branco LG, Romanovsky AA: Neural substrate of cold-seeking behavior in endotoxin shock. PLoS One 2006; 1:e1; PMID:17183631; http://dx.doi.org/ 10.1371/journal.pone.0000001 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
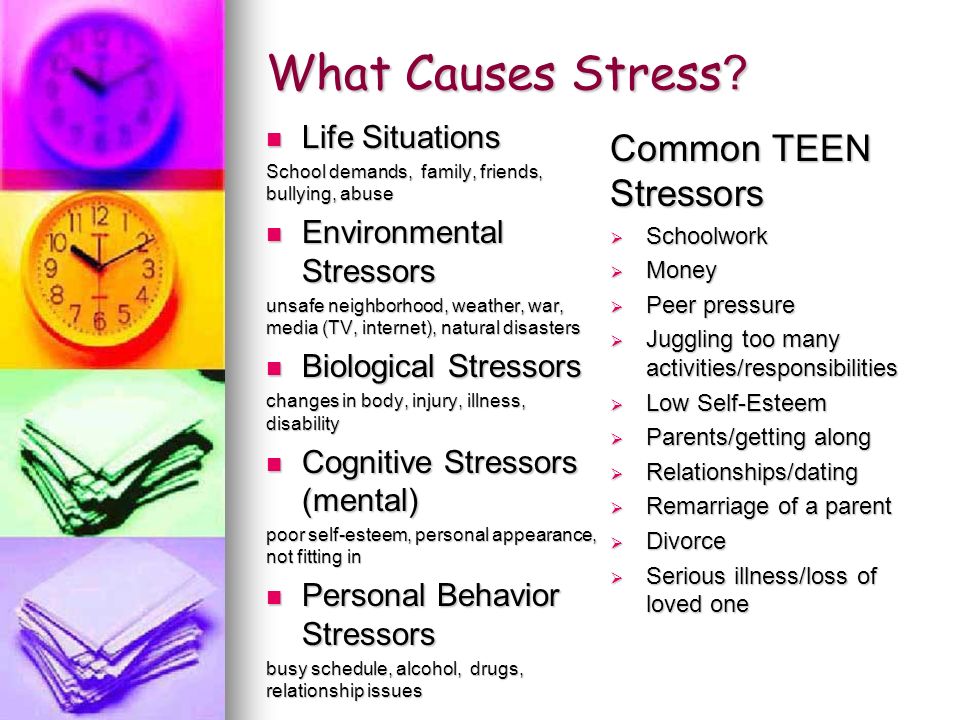
Can Stress Make You Sick? Fever, Hemorrhoids, and More
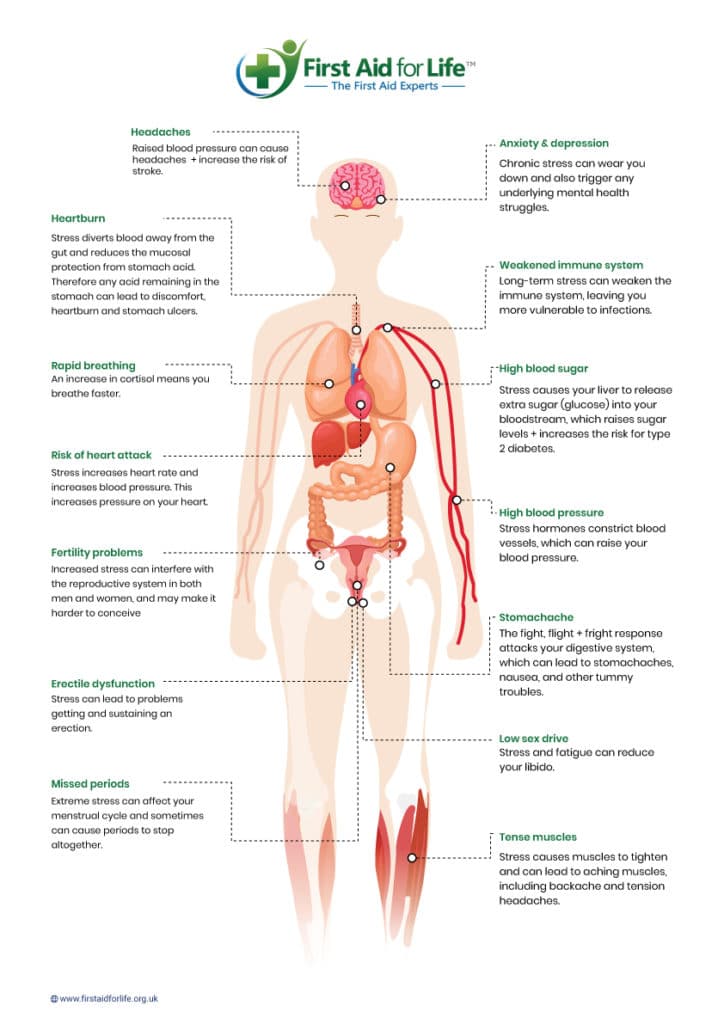
Overview
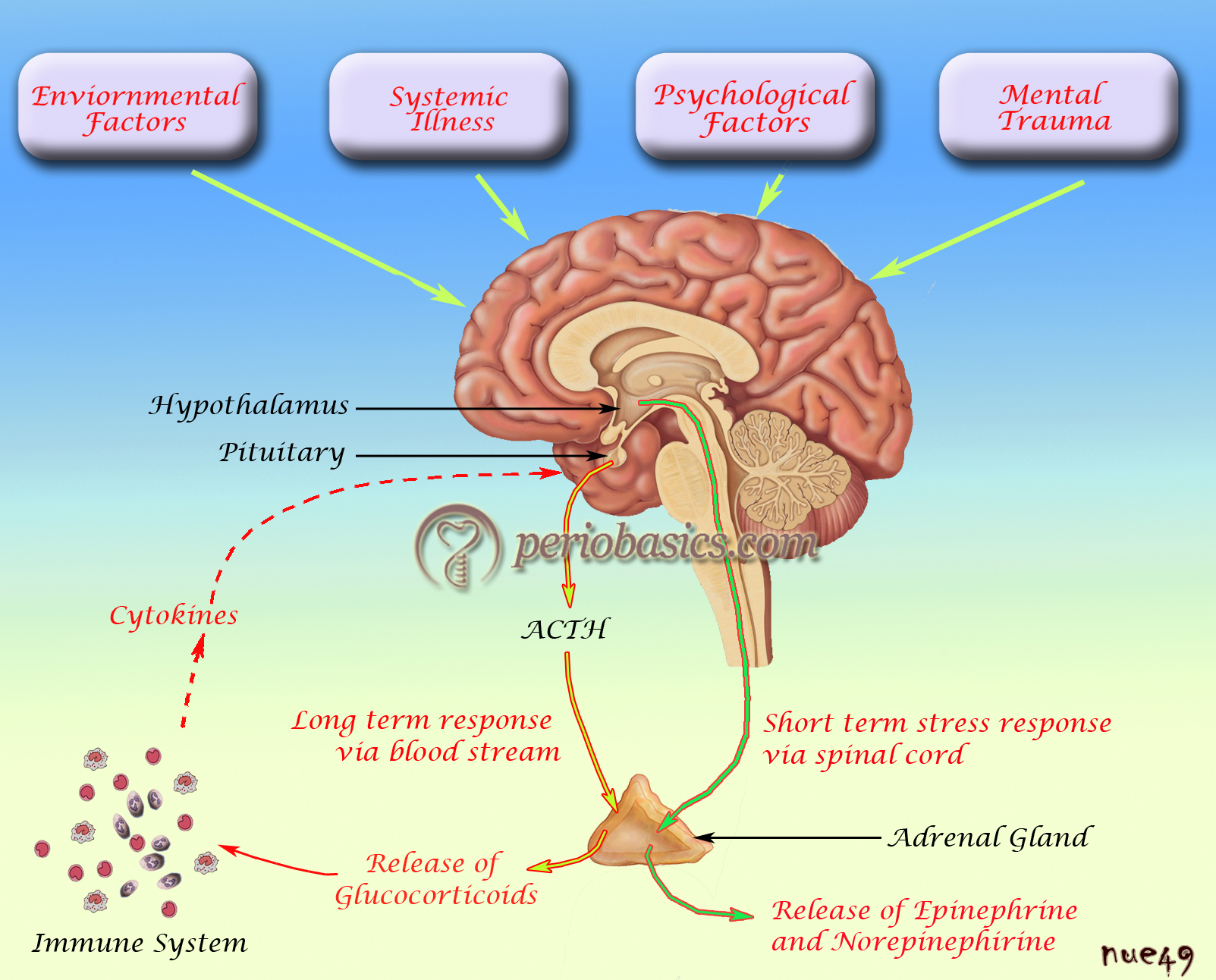
Stress is your body’s response to an actual or perceived threat. Some stress is good for you and drives you to take action, like looking for a job when you’ve been fired. Too much stress, however, can suppress your immune system and cause you to get sick more easily.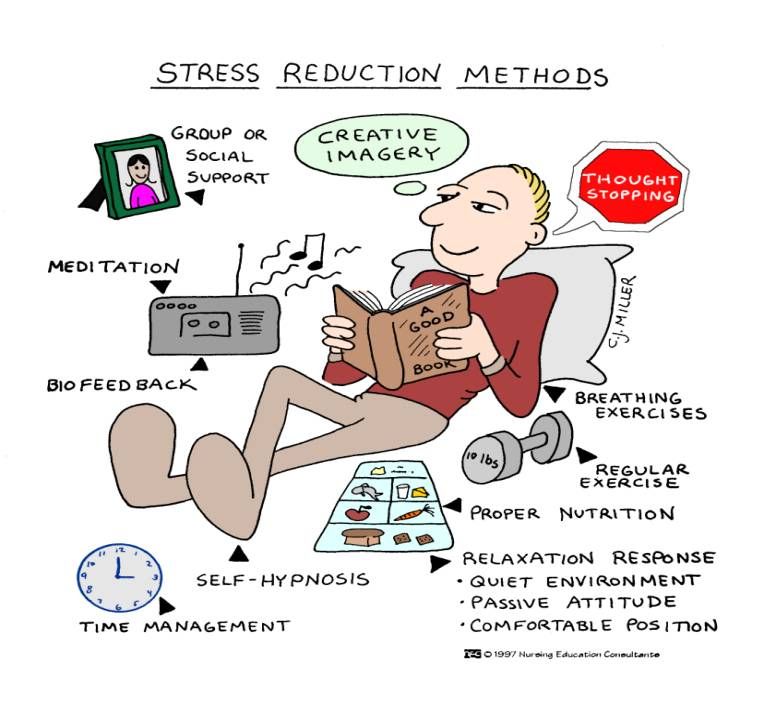
Prolonged periods of stress can also increase your risk of several diseases, including heart disease and cancer. According to a study, 60 to 80 percent of doctor’s office visits may be stress-related.
Stress can cause a number of physical symptoms and illnesses. Symptoms can come on as soon as your level of stress increases and worsen as stress continues. These symptoms usually go away once your stress level lowers.
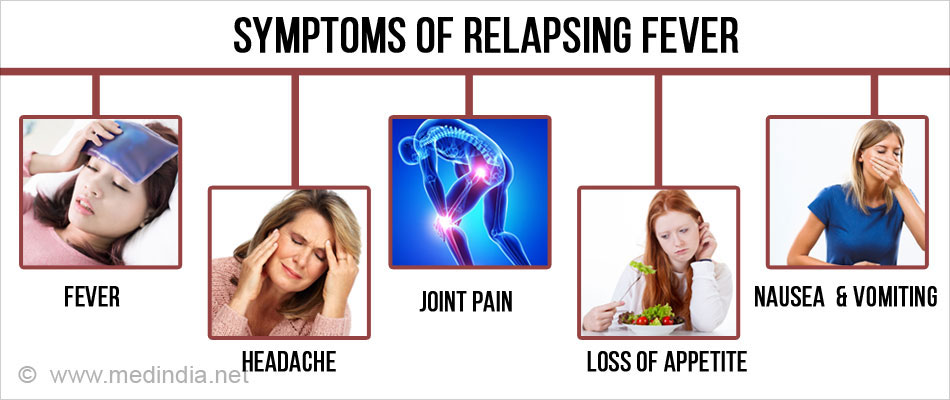
Some of the symptoms commonly caused by stress include:
- increased heart rate
- increased blood pressure
- rapid breathing
- shortness of breath
- muscle tension
- headache
- nausea
- dizziness
If your stress levels remain high or you experience frequent stress, your risk of getting sick increases.
Fever
Chronic stress and exposure to emotional events can cause a psychogenic fever. This means the fever is caused by psychological factors instead of a virus or other type of inflammatory cause. In some people, chronic stress causes a persistent low-grade fever between 99 and 100˚F (37 to 38°C). Other people experience a spike in body temperature that can reach as high as 106˚F (41°C) when they’re exposed to an emotional event.
In some people, chronic stress causes a persistent low-grade fever between 99 and 100˚F (37 to 38°C). Other people experience a spike in body temperature that can reach as high as 106˚F (41°C) when they’re exposed to an emotional event.
Psychogenic fever can happen to anyone under stress, but it most commonly affects young women.
The common cold
A 2012 study found that chronic psychological stress prevents the body from properly regulating the inflammatory response. Inflammation has been linked to the development and progression of many diseases. People who are exposed to long periods of stress are more likely to develop colds upon exposure to the cold-causing germs.
Stomach issues
Evidence shows that stress stops your gastrointestinal system from working properly, affecting your stomach and large bowel. Stress can cause a wide range of gastrointestinal symptoms, including:
- abdominal pain
- nausea
- indigestion
- diarrhea
- constipation
Stress has also been shown to aggravate the symptoms of irritable bowel syndrome (IBS), and it may be one of the main causes of IBS.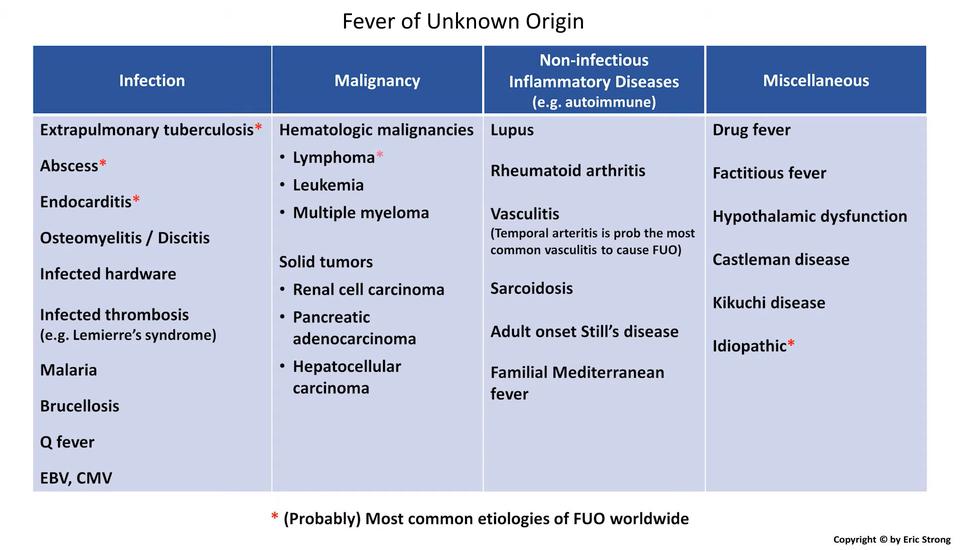 If you suffer from stomach acid reflux with heartburn, stress can worsen your symptoms by increasing your sensitivity to stomach acid. If not well-controlled, inflammation from stomach acid erosion raises your risk of peptic ulcers. Chronic diarrhea or constipation can lead to conditions such as hemorrhoids.
If you suffer from stomach acid reflux with heartburn, stress can worsen your symptoms by increasing your sensitivity to stomach acid. If not well-controlled, inflammation from stomach acid erosion raises your risk of peptic ulcers. Chronic diarrhea or constipation can lead to conditions such as hemorrhoids.
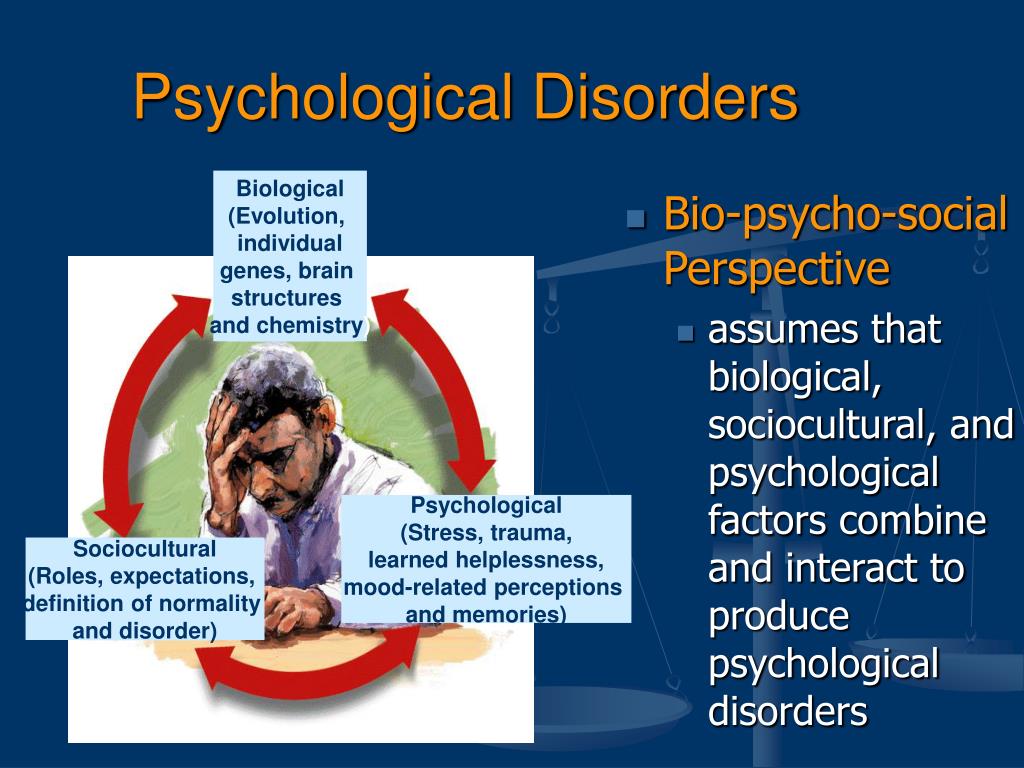
Depression
Research has linked both chronic stress and shorter periods of acute stress to depression. Stress throws several of your brain chemicals out of balance, including serotonin, dopamine, and norepinephrine. It also elevates your cortisol level. All of these are linked to depression. When this type of chemical imbalance occurs, it negatively affects your:
- mood
- sleep pattern
- appetite
- sex drive
Headaches and migraines
Stress is a common trigger of headaches, including tension and migraine headaches. One study found that relaxing after experiencing a period of stress can lead to an acute migraine headache episode within the next 24 hours. This is thought to be caused by what’s known as the “let-down” effect. The study concluded that medication or behavioral modification could help prevent headaches for those who have migraines related to stress reduction.
This is thought to be caused by what’s known as the “let-down” effect. The study concluded that medication or behavioral modification could help prevent headaches for those who have migraines related to stress reduction.
Allergies and asthma
Life stress has been linked to the onset and worsening of mast cell-associated diseases, including asthma and allergies. Histamine causes allergy symptoms and is released by your body’s mast cells as a response to stress. Prolonged or heightened levels of stress can worsen or possibly even lead to an allergic reaction.
This can cause skin symptoms, such as a rash or hives, or other allergy symptoms, such as runny nose and watery eyes. Stress can also trigger an asthma attack in people with asthma.
Obesity
Stress is believed to a play a major role in obesity. Studies have found that higher cortisol levels caused by chronic stress can influence several factors that contribute to weight gain, including poor sleep, which raises your cortisol levels further and leads to increases in belly fat.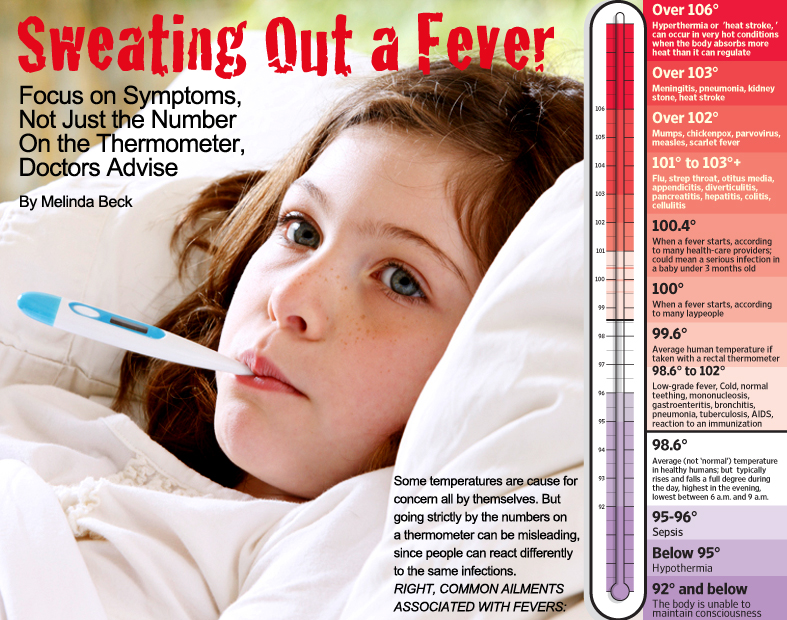 It also contributes to poor nutrition by increasing your cravings for sweets and refined carbohydrates.
It also contributes to poor nutrition by increasing your cravings for sweets and refined carbohydrates.
High stress levels have also been shown to increase your chances of being unsuccessful at weight loss programs. Obesity is a risk factor in several diseases, including heart disease, diabetes, and cancer.
Heart disease
Research has found that all types of stress, including emotional stress, work stress, financial stress, and major life events, increase the risk of heart disease. Stress raises your blood pressure and cholesterol, which are directly linked to heart disease. Stress also significantly increases your risk of dying from a heart attack.
Pain
Stress can cause you to ache all over. Stress causes your muscles to tense, which can cause or worsen neck, shoulder, and back pain. Research shows that stress can also increase your sensitivity to pain. People with fibromyalgia, arthritis, and other conditions often report an increase in pain during times of stress.
Learning how to manage stress can help ease your symptoms and lower your risk of getting sick.
Some things that have been proven to help lower stress levels include:
- getting regular exercise
- listening to music
- yoga and meditation
- deep breathing exercises
- cutting back on obligations
- cuddling a pet
- getting enough sleep
If you’re having trouble managing stress, speak to your doctor about getting professional help. A counselor or therapist can help you identify the sources of your stress and teach you coping strategies that can help you to better deal with stress.
How Stress Works and Why It Makes Us Stronger - T&P
Stress training is often used to train NASA astronauts or emergency workers to not only survive in difficult situations, but also to act as efficiently as possible. Psychologists call it stress inoculation. T&P publishes an excerpt from Stanford professor Kelly McGonigal's book Good Stress as a Way to Get Stronger and Better, in which she explains how "good" stress differs from "bad" stress.

How did stress get infamous?
Good stress as a way to become stronger and better
In 1936, the Hungarian endocrinologist Hans Selye injected laboratory rats with a hormone isolated from the ovaries of a cow. The results were very unpleasant for rodents. The rats began to develop bloody ulcers. Their adrenal glands swelled, while their thymus glands, spleens, and lymph nodes—parts of the immune system—were shrunken. They were very sad and sick rats.
But was the bovine hormone really to blame? Selye set up control experiments by injecting some rats with a saline solution, and others with a hormone from a cow's placenta. And they showed the same symptoms. He tried using extracts from the kidneys and spleen. And those rats got sick. No matter what he injected into the rats, they got sick, and with the same symptoms.
In the end, it dawned on Selye that the rats got sick not because of the substances they were injected with, but because of what they were experiencing. They just didn't like being pricked with needles. Selye discovered that he could cause the same symptoms in rats by exposing them to various unpleasant influences: extreme heat or cold, incessant physical exertion, loud noises, the action of toxic substances. Within 48 hours, muscle tone dropped in rats, ulcers developed in the intestines, and suppression of the immune system began.
They just didn't like being pricked with needles. Selye discovered that he could cause the same symptoms in rats by exposing them to various unpleasant influences: extreme heat or cold, incessant physical exertion, loud noises, the action of toxic substances. Within 48 hours, muscle tone dropped in rats, ulcers developed in the intestines, and suppression of the immune system began.
Then they died.
Thus the science of stress was born. Selye chose the word stress to describe the state he put rats in and their physiological response to that state (we now call it the stress response). But what does all this have to do with you? Before starting his research, Selye was a physician. Then he saw many patients whose body began to fail for no reason at all. They showed some general symptoms - loss of appetite, fever, weakness - that could not be called characteristic of specific diseases. They just looked extremely tired of life. At that moment, Selye called this condition "the syndrome of suffering.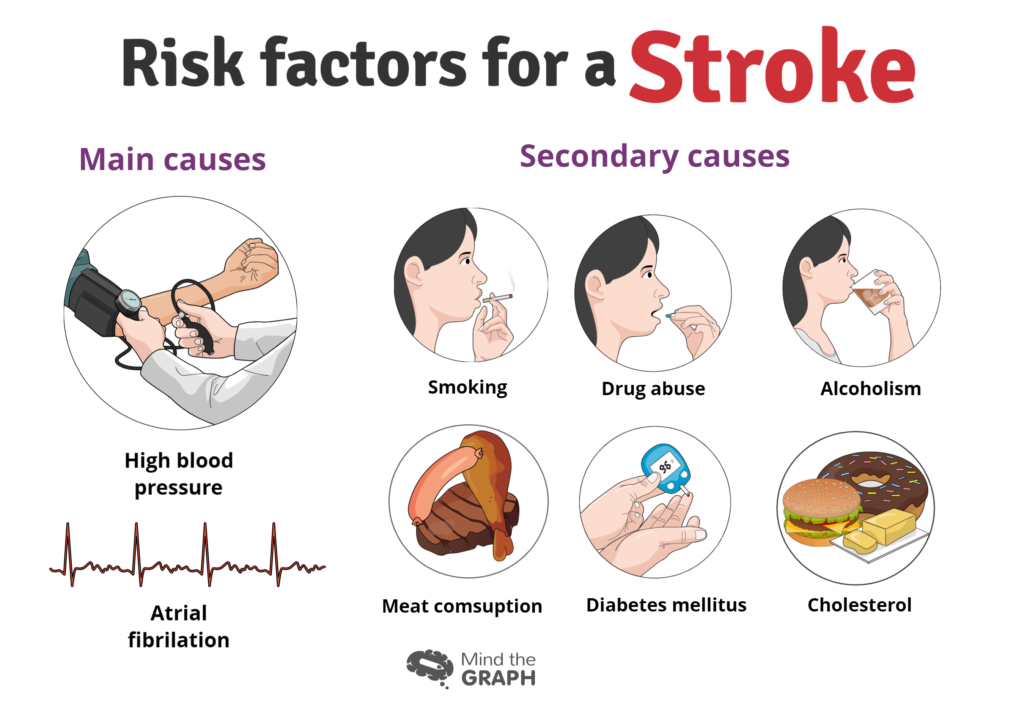 "
"
How to look at life from the bright side and successfully deal with stress? Learn this in the Antifragility course.
Many years later, when Selye began to conduct his laboratory experiments, sick and dying rats reminded him of his patients. Maybe, he thought, the body is weakening from the loads that one has to cope with in difficult life situations? And here Selye made a giant leap from experiments with rats to the study of human stress. He suggested that many health problems, from allergies to heart attacks, could be the result of a process he observed in rats. This analogy for Selye remained purely theoretical; he studied laboratory animals all his life. However, this did not prevent him from building hypotheses regarding humans. And, having made this speculative logical transfer, Selye made another decision that forever changed the world's attitude to stress. He gave it a definition that goes far beyond laboratory methods of working with rats. According to Selye, stress is the reaction of the body to any impact on it .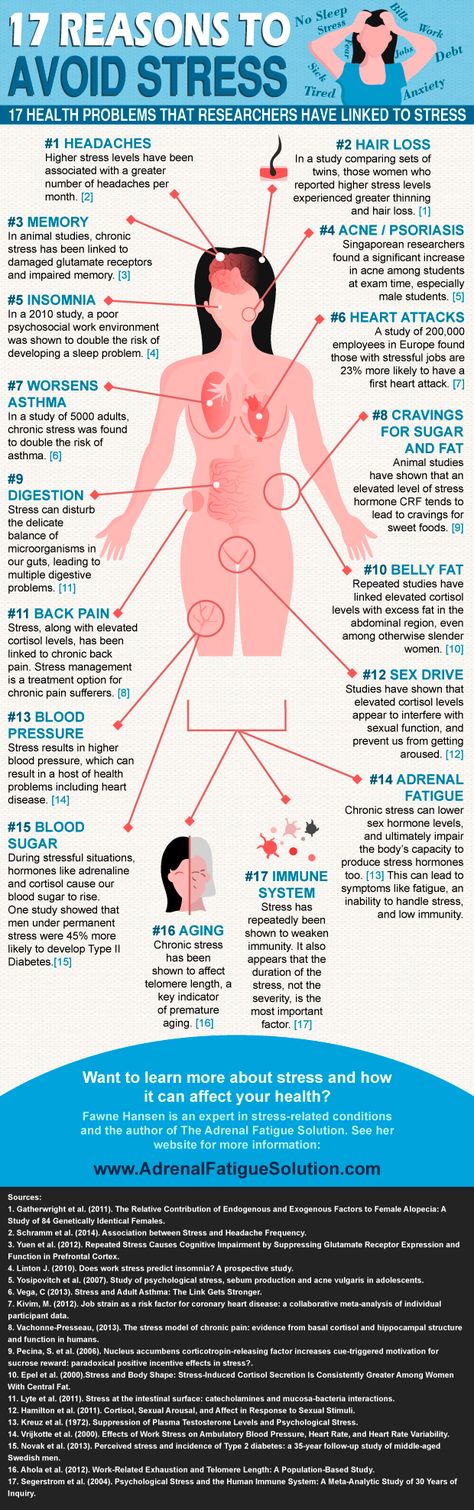 That is, it is not just a reaction to painful injections, traumatic injuries or harsh laboratory conditions, but a response to any impact that requires response or adaptation. By defining stress in this way, Selye laid the foundation for the negative attitudes towards it that we see today.
That is, it is not just a reaction to painful injections, traumatic injuries or harsh laboratory conditions, but a response to any impact that requires response or adaptation. By defining stress in this way, Selye laid the foundation for the negative attitudes towards it that we see today.
Selye devoted his entire subsequent career to promoting his ideas about stress, was nicknamed "the grandfather of the science of stress" and was nominated ten times for the Nobel Prize. He even wrote what could be considered the first official guide to stress management. Sometimes he received research funds from unexpected admirers. For example, tobacco manufacturers paid him to write articles about the harmful effects of stress on human health. At their request, he even gave a speech to the US Congress on how smoking helps fight the dangerous effects of stress.
But Selye's main contribution is that he first convinced the world of the dangers of stress. If you tell a colleague, "I'm going to get an ulcer on this project," or complain to your spouse, "This stress is killing me," you're paying homage to Selye's rats.
advertisement for cigarettes as a stress reliever
Was he wrong? Not really. If you are in the same position as his rats - subjected to deprivation, torment and other negative influences - your body will undoubtedly pay for it. There is a lot of scientific evidence that very severe or traumatic stress can damage your health. However, Selye's definition of stress is very broad: it includes not only injuries, violence, and abuse, but also almost everything that can happen to you . For Selye , stress was synonymous with the body's response to life as such.
Over time, Selye realized that not all stressful experiences lead to illness. He started talking about good stress (which he called eustress ) and bad stress ( distress ). In one of the later interviews, the scientist said: “We experience stress all the time, so the only thing you can do is try to make it useful for you and those around you.” But it was already too late. Thanks to Selye's work, a general attitude towards stress as a very dangerous condition has taken root in society and the medical environment.
Thanks to Selye's work, a general attitude towards stress as a very dangerous condition has taken root in society and the medical environment.
The legacy of Hans Selye has been developed in stress research conducted with the help of laboratory animals. To this day, much of what you hear about the negative effects of stress scientists learn from experiments on rats. But the stress that these animals experience actually has little to do with everyday human stress. If you are a guinea pig, then your day will look something like this: you will be shocked unexpectedly; thrown into a bucket of water and forced to swim until you start to sink; they will put them in a solitary cell or, conversely, in an overcrowded cage with a very small amount of food, for which they will have to fight fiercely. It's not stress; it's the Hunger Games for rodents. […]
Is the stress response normal?
Hans Selye is often blamed for the bad reputation of stress, but he is not the only culprit. There is also Walter Cannon with cats and dogs. Cannon, a physiologist at Harvard Medical School, first described the fight-or-flight stress response in 1915. He studied how fear and anger affect the physiology of animals. In order to anger and frighten the test subjects, he used two methods: he pinched the mouth and nose of the cat with his fingers until her breath was disturbed, and put dogs and cats in the same room to fight.
There is also Walter Cannon with cats and dogs. Cannon, a physiologist at Harvard Medical School, first described the fight-or-flight stress response in 1915. He studied how fear and anger affect the physiology of animals. In order to anger and frighten the test subjects, he used two methods: he pinched the mouth and nose of the cat with his fingers until her breath was disturbed, and put dogs and cats in the same room to fight.
According to Cannon, frightened animals release adrenaline and become in a state of heightened sympathetic activity. Their heart rate and breathing speed up, their muscles tense - thus they prepare for action. Digestion and other physiological functions that are not required at the moment slow down or stop. The body prepares for the fight by storing energy and mobilizing the immune system. All these changes are automatically launched when a threat to life occurs.
The fight-or-flight instinct is not unique to dogs and cats; it is present in all animals.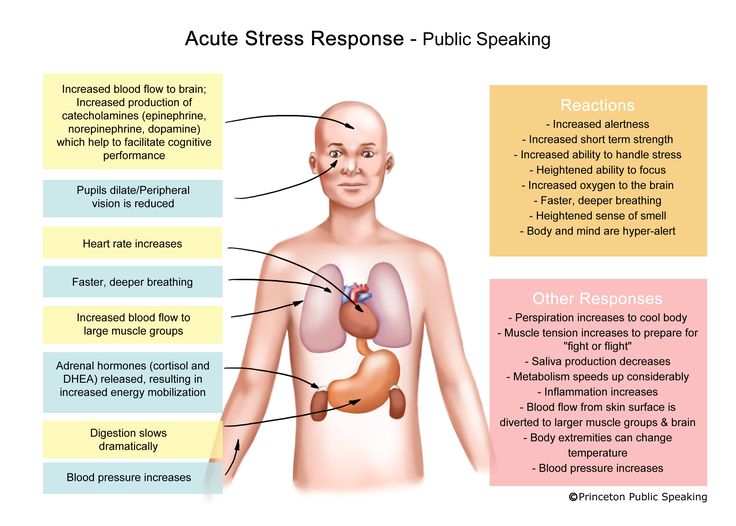 He often saves lives - both animals and humans. That is why it is so stable in evolution, and we should be grateful to nature for writing it into our DNA.
He often saves lives - both animals and humans. That is why it is so stable in evolution, and we should be grateful to nature for writing it into our DNA.
Walter Cannon
However, many scholars point out that close combat or a hasty escape are not the best strategies for situations that modern man faces every day. How can this reaction help you survive traffic jams or the threat of being fired? What will happen if, when any difficulty arises, you simply run away from relationships, children, work? You can't beat up a late mortgage payment and disappear every time you have a conflict at home or work.
From this point of view, you should suppress the stress response at all times, except in cases of purely physical danger, such as escaping a burning building or rescuing a drowning child. In all other situations, this is just a senseless waste of energy that prevents successful counteraction to stress. This is evidenced by the theory of inconsistency of the stress reaction of a stressful situation: the reactions that saved our ancestors are not suitable for you and me.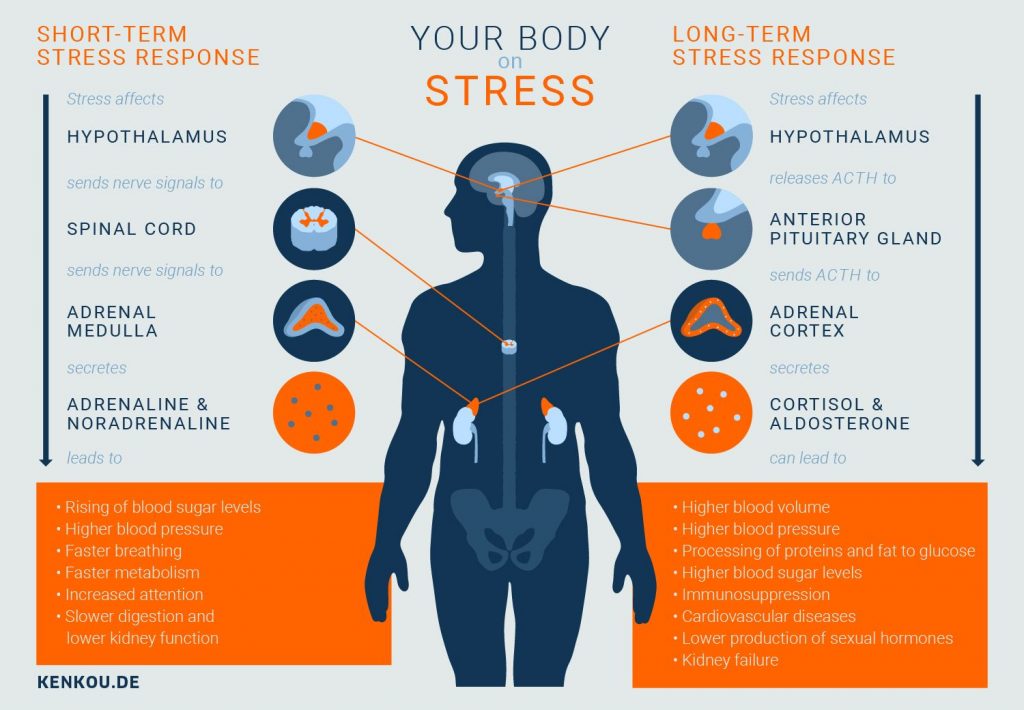 A stress reaction that has no adaptive value in the modern world only hinders us. […]
A stress reaction that has no adaptive value in the modern world only hinders us. […]
Let's be clear: a reaction that supports only two survival strategies - fight or flight - really does not correspond to modern life at all. But it turns out that human stress responses are actually much more complex. They have evolved along with man, adapting to the changing world over time. The stress response can activate various biological systems that support various behavioral strategies. Thanks to this, you can not only run out of a burning building, but also understand problems, receive social support and learn from the experience. […]
How to look at life from the bright side and successfully deal with stress? Learn this in the Antifragility course.
There are several types of stress responses, and each has a different biological profile that motivates different strategies for coping with stress. For example, the goal response increases self-confidence, motivates action and helps to use the experience gained, while the care and friendship response stimulates courage, generates a desire to care for others and strengthens social bonds.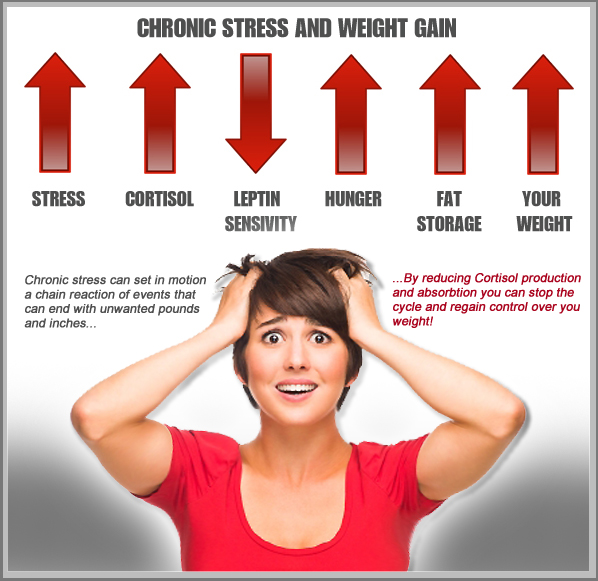 These responses, along with the fight-or-flight response, make up your body's complex stress responses. To understand how stress stimulates these very different responses, let's take a closer look at the biology of stress.
These responses, along with the fight-or-flight response, make up your body's complex stress responses. To understand how stress stimulates these very different responses, let's take a closer look at the biology of stress.
Stress gives you the strength to cope.
As Walter Cannon noted, the fight-or-flight response is triggered by the activation of your sympathetic nervous system. To make you more alert and ready for action, this system forces your entire body to mobilize all available energy resources. The liver releases fat and sugar into the blood to serve as fuel. Breathing becomes deeper to bring more oxygen to the heart. The heart rate speeds up so that oxygen, fat and sugar reach the muscles and brain more quickly. Stress hormones like adrenaline and cortisol help your muscles and brain use this energy more efficiently. As a result, you are ready to overcome any obstacles.
It is this response to stress that provides a person with exceptional physical abilities in special situations. You can often find reports in the news about the incredible strength that a person acquires in stressful situations - for example, the story of two teenage girls from Lebanon, Oregon, who managed to lift a 1.5-ton tractor, under which their father was trapped. “I don’t know how I was able to lift it, it was very heavy,” one of the girls told reporters. “But we just took it and raised it.” Many people experience something similar when under severe stress. When something very important is at stake, the body uses all the energy resources to do what is needed.
You can often find reports in the news about the incredible strength that a person acquires in stressful situations - for example, the story of two teenage girls from Lebanon, Oregon, who managed to lift a 1.5-ton tractor, under which their father was trapped. “I don’t know how I was able to lift it, it was very heavy,” one of the girls told reporters. “But we just took it and raised it.” Many people experience something similar when under severe stress. When something very important is at stake, the body uses all the energy resources to do what is needed.
The energy that stress gives you not only helps the body, but also stimulates the brain. Adrenaline sharpens the senses. The pupils dilate to let in more light, and hearing becomes more acute. At the same time, the brain processes the signals coming from the sense organs faster. Unnecessary thoughts are turned off, less important tasks temporarily lose their relevance. Attention is concentrated, you absorb and process more information.
A chemical cocktail of endorphins, adrenaline, testosterone and dopamine kicks in. This is one of the reasons why some people like to experience stress - it gives them a pleasant arousal. The combination of the above substances increases your sense of self-confidence. You can act more purposefully and strive for what can give you satisfaction. Some scientists refer to this aspect of stress as "excitement and awe." Skydivers, skydivers, and lovers also experience such sensations. If you have pleasant goosebumps running down your back from participating in a game of chance or trying to complete a difficult job on time, then you know what it is.
When it comes to true survival, these physiological changes are most pronounced, and you may have the classic fight-or-flight response. But if nothing directly threatens your life, the body and brain switch to another state - the reaction of striving for the goal . Like the fight-or-flight response, this stress response empowers you and helps you perform in challenging environments. The heart rate increases, adrenaline levels soar, muscles and brain get more fuel, and "feel good hormones" are released into the bloodstream. But this reaction differs from the previous one in several important ways. You feel focused, but not fearful. The level of stress hormones is also different, in particular, the level of DHEA is increased, which helps to recover faster from stress and learn useful experience. As a result, your Stress Response Growth Index rises—that is, there is a favorable balance of stress hormones that determines how harmful or beneficial stress will be for you.
The heart rate increases, adrenaline levels soar, muscles and brain get more fuel, and "feel good hormones" are released into the bloodstream. But this reaction differs from the previous one in several important ways. You feel focused, but not fearful. The level of stress hormones is also different, in particular, the level of DHEA is increased, which helps to recover faster from stress and learn useful experience. As a result, your Stress Response Growth Index rises—that is, there is a favorable balance of stress hormones that determines how harmful or beneficial stress will be for you.
People who are completely immersed in what they are doing and enjoy it show clear signs of a goal-seeking reaction. Artists, athletes, surgeons, gamers, musicians, completely surrendering to their favorite pastime, experience just such a reaction to stress. The best in these fields of activity do not at all remain cold-blooded under the pressure of difficult circumstances; it would be more accurate to say that they have a stress reaction of striving for a goal. It gives them access to mental and physical resources, which, in turn, provide increased confidence, concentration, and performance.
It gives them access to mental and physical resources, which, in turn, provide increased confidence, concentration, and performance.
Stress helps communication and stimulates social connections
Your stress response does more than just provide you with energy. In many situations, it also forces you to connect with other people. This side of stress is predominantly controlled by the hormone oxytocin. Oxytocin has become widely known as the “love molecule” and “cuddle hormone” because it is actually produced by the pituitary gland when you hug someone. However, in reality, the functions of oxytocin are much more complex. It is a neurohormone that fine-tunes the social instincts in your brain. Its main function is to create and strengthen social attachments, which is why it stands out during hugs, as well as during sexual intercourse and breastfeeding. Increased levels of oxytocin make you reach out to people. It generates a desire for personal contact - through touch, SMS or meeting over a glass of beer. In addition, oxytocin helps the brain better understand what other people are thinking and feeling. It enhances empathy and intuition. With high levels of oxytocin, you are more likely to trust and help the people you care about. Oxytocin makes the brain more receptive to social contact and thereby enhances the warm feeling you get when you care for others.
In addition, oxytocin helps the brain better understand what other people are thinking and feeling. It enhances empathy and intuition. With high levels of oxytocin, you are more likely to trust and help the people you care about. Oxytocin makes the brain more receptive to social contact and thereby enhances the warm feeling you get when you care for others.
But the functions of oxytocin are not limited to the social sphere. It is also the hormone of courage. Oxytocin suppresses the fear response in the brain, the instinct that makes you freeze in place or run. Not only does this hormone urge you to seek out hugs; he makes you brave.
Oxytocin is as much a part of the stress response as adrenaline, which makes your heart race. During times of stress, the pituitary gland releases oxytocin to stimulate social bonding. This means that stress makes you a better person without additional investment in personal growth and socialization training.
Hans Selye
Released during the stress response, oxytocin causes you to turn to those who can support you. It also strengthens the connections that matter most to you, making you more responsive. Scientists call this the care and friendship response . Unlike the fight-or-flight response, which is primarily about self-preservation, this response forces you to protect those you care about. And most importantly, it gives you courage.
It also strengthens the connections that matter most to you, making you more responsive. Scientists call this the care and friendship response . Unlike the fight-or-flight response, which is primarily about self-preservation, this response forces you to protect those you care about. And most importantly, it gives you courage.
When you feel like talking to a friend or loved one, this stress response prompts you to seek support. If something bad happens and you immediately think of your children, pets, relatives or friends, this stress reaction motivates you to protect your “tribe”. When someone is dishonest and you rush to stand up for your team, your company, or your community, it's all part of the prosocial stress response.
Oxytocin has another amazing quality: this so-called love hormone has a beneficial effect on the cardiovascular system. The heart has special receptors for oxytocin, which promotes the regeneration of heart muscle cells after microtrauma.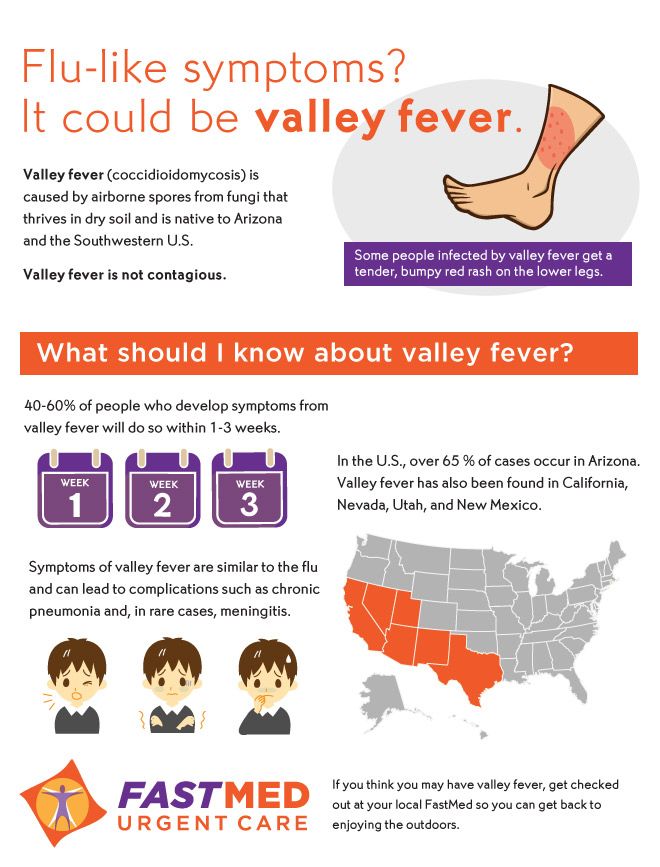 If your stress response involves the release of oxytocin, stress literally strengthens your heart. We usually hear that stress can cause a heart attack! Yes, stress-induced heart attacks really sometimes happen, and they are usually caused by a sharp release of adrenaline, but not every stress reaction causes damage to your heart. I found one study that showed that when rats are stressed and then chemically attacked, they exhibit a very significant resistance to heart injury. However, when rats were given an oxytocin-blocking substance, stress no longer had such a beneficial effect on them. This study reveals to us one of the most surprising aspects of stress. It turns out that the stress response is our innate stability mechanism that makes us care for others, but also strengthens our heart.
If your stress response involves the release of oxytocin, stress literally strengthens your heart. We usually hear that stress can cause a heart attack! Yes, stress-induced heart attacks really sometimes happen, and they are usually caused by a sharp release of adrenaline, but not every stress reaction causes damage to your heart. I found one study that showed that when rats are stressed and then chemically attacked, they exhibit a very significant resistance to heart injury. However, when rats were given an oxytocin-blocking substance, stress no longer had such a beneficial effect on them. This study reveals to us one of the most surprising aspects of stress. It turns out that the stress response is our innate stability mechanism that makes us care for others, but also strengthens our heart.
Stress helps you learn and grow
The last stage of any stress response is recovery, bringing your body and mind back to a state of calm. The body needs stress hormones to recover.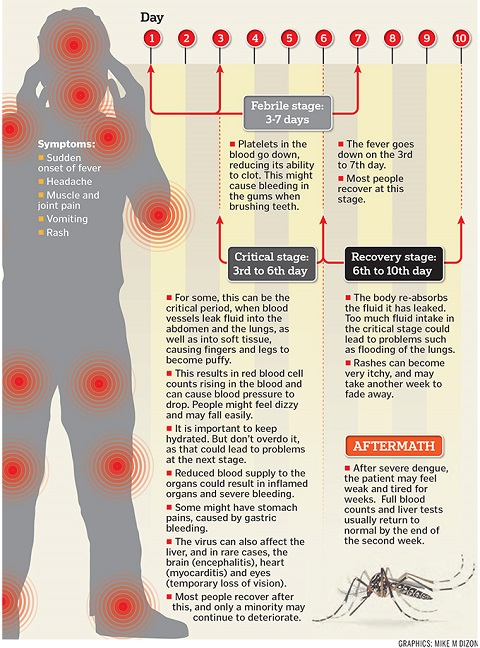 For example, cortisol and oxytocin fight inflammatory reactions and support the work of the autonomic nervous system. DHEA and Neuronal Growth Factor (NGF) increase neuroplasticity so your brain can learn from stressful experiences. You may feel like your body needs to repair itself after exposure to stress hormones, but in fact the opposite is true - it is these hormones that have a restorative function. People who produce more of these hormones during times of stress tend to recover much faster and with minimal consequences.
For example, cortisol and oxytocin fight inflammatory reactions and support the work of the autonomic nervous system. DHEA and Neuronal Growth Factor (NGF) increase neuroplasticity so your brain can learn from stressful experiences. You may feel like your body needs to repair itself after exposure to stress hormones, but in fact the opposite is true - it is these hormones that have a restorative function. People who produce more of these hormones during times of stress tend to recover much faster and with minimal consequences.
Recovering from stress does not happen instantly - it is a process that takes time. In the first few hours after a strong stress reaction, the brain rewires, remembering and assimilating the experience. At this time, the activity of stress hormones increases in those areas of the brain that are responsible for learning and memory. The brain processes the experience, which is why you can't stop thinking about what happened. You may want to discuss this with someone.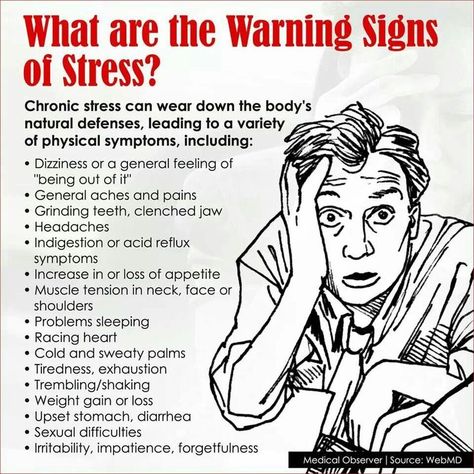 If everything ended well, you replay what happened in your head, remembering everything you did and what it led to. If the result was not very successful, you try to understand what happened, imagine what would have happened if you had acted differently, and mentally construct a positive outcome.
If everything ended well, you replay what happened in your head, remembering everything you did and what it led to. If the result was not very successful, you try to understand what happened, imagine what would have happened if you had acted differently, and mentally construct a positive outcome.
A person often experiences strong emotions during the recovery process. There is still energy in him, and he is too excited to immediately calm down. After stress, you may experience fear, shock, anger, guilt, or sadness. But you can also feel relief, joy or gratitude. Moreover, these emotions can fill you at the same time - this is part of the process of understanding the experience with the brain. They encourage reflection and learning from experience, which in turn helps prepare for future stresses. In addition, thanks to emotions, you better remember what happened. These emotions are driven by chemical changes that make the brain more flexible—it can rewire itself based on experience.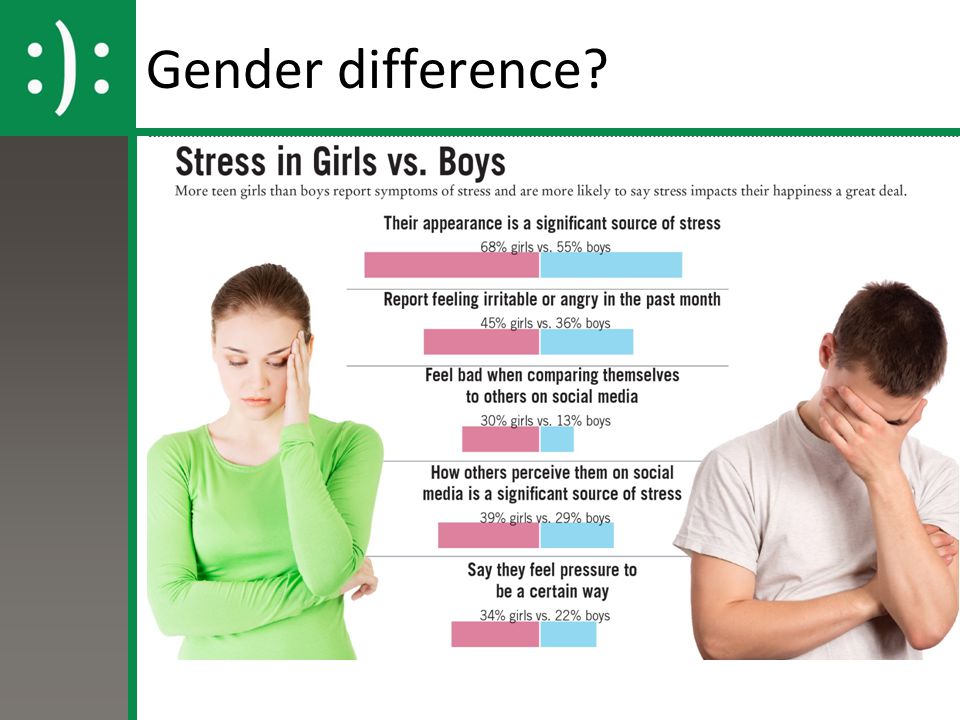 Thus, the emotions that accompany the recovery process from stress help you learn and find meaning in what is happening.
Thus, the emotions that accompany the recovery process from stress help you learn and find meaning in what is happening.
Based on all the above processes, the brain and body are trained to cope with stress. It leaves an imprint in your mind that will help you know how to behave next time. It doesn’t happen with every little adversity, but if you face a really difficult task, your brain and body will definitely learn from it. Psychologists in such cases say that a person receives a stress inoculation . This is a kind of "vaccination" for the brain. That is why stress training is one of the key training methods for NASA astronauts, emergency workers, professional athletes and representatives of other specialties who need to learn not only to survive in stressful situations, but also to act as efficiently as possible. Stress vaccination is used in preparing children for emergency evacuation, work training to adapt to harsh working conditions, and even teaching communication to autistic children.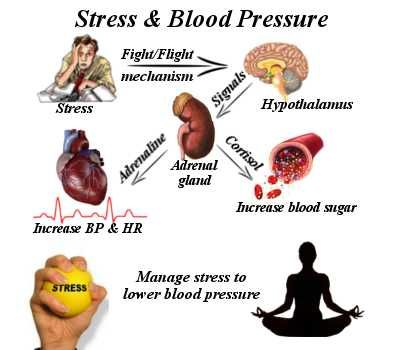
If you recognize that stress gives you the positive experience you need, you will be more comfortable with each new challenge. Research shows that when the benefits of stress for learning and resilience are recognized, the physiological response to it can also change. As we saw with Alia Crum's work, watching videos of the benefits of stress increased participants' DHEA levels before and after the mock interview. Other research also shows that perceiving a stressful situation as an opportunity to hone one's skills, improve one's knowledge, or become stronger elicits a goal-seeking response rather than a fight and flight response. And this, in turn, increases the chances that the experience gained will bring significant benefits to the person in the future.
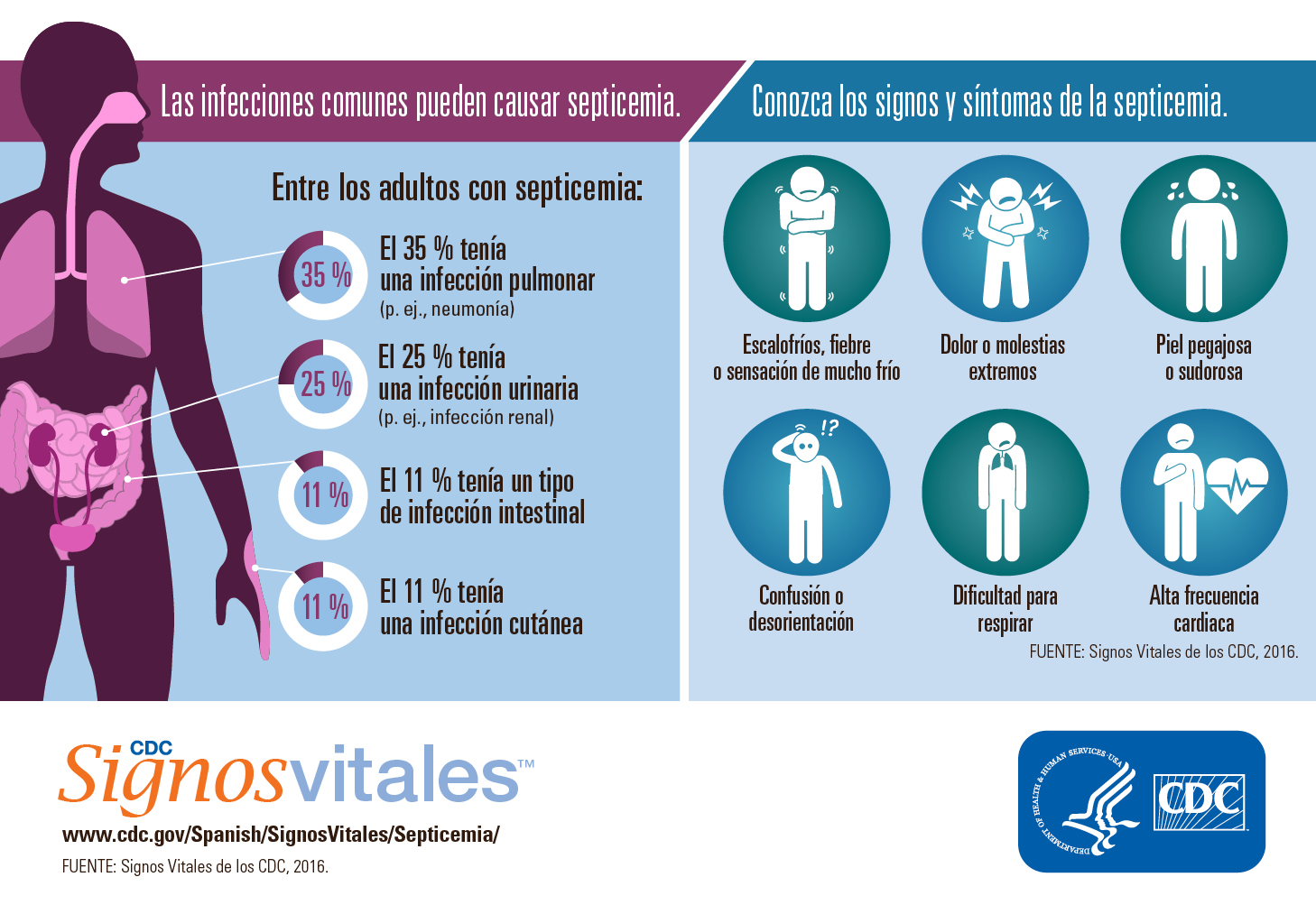
Mouse fever (Hemorrhagic fever) in children and adults: symptoms, signs, treatment
Hemorrhagic fever with renal syndrome (the second name is mouse fever) is a disease of the infectious group, often associated with the beginning of the summer season and agricultural work. Every year, about 7,000 cases of infection are recorded in the country, which makes itself felt with characteristic symptoms - a hemorrhagic rash, vascular damage, malfunctioning of the kidneys and a general deterioration in a person's condition. In the absence of timely assistance, the disease can cause serious complications and death. Only timely seeking medical help will help preserve the health of the patient and return him to normal life.
Every year, about 7,000 cases of infection are recorded in the country, which makes itself felt with characteristic symptoms - a hemorrhagic rash, vascular damage, malfunctioning of the kidneys and a general deterioration in a person's condition. In the absence of timely assistance, the disease can cause serious complications and death. Only timely seeking medical help will help preserve the health of the patient and return him to normal life.
Causes of mouse fever
For a long time, the beginning of the summer season was marked by a sharp increase in patients who went to the doctor with the same symptoms - impaired excretory function, skin rashes, changes in blood composition, weakness and malaise. Detailed studies have identified the culprits who are carriers of a dangerous infection.
These are rodents, in the body of which there is a sufficient amount of pathogenic microflora. Together with secretions, it enters the soil and on the skin of a person during summer work, digging the soil, outdoor recreation and sports. Through dirty hands, pathogens enter the body, penetrate the respiratory system and blood vessels, causing the appearance of characteristic symptoms. Most of the sick are lovers of summer holidays and employees of agricultural enterprises involved in planting plants and harvesting in the fields and gardens.
Through dirty hands, pathogens enter the body, penetrate the respiratory system and blood vessels, causing the appearance of characteristic symptoms. Most of the sick are lovers of summer holidays and employees of agricultural enterprises involved in planting plants and harvesting in the fields and gardens.
A significant part of the rodents that are carriers of hemorrhagic fever infection move through fields, broad-leaved forests, garden plots, abandoned agricultural land, auxiliary buildings, etc. With the onset of cold weather, they tend to penetrate into houses, where they continue to actively breed. Their waste products remain on the surfaces of the floor and walls, tables and shelves, which significantly increases the risk of infection during cleaning and tidying up.
Routes of infection include:
- airborne - inhalation of dust containing small particles of excrement;
- alimentary - consumption of water contaminated by rodents;
- contact - in contact with human skin of the remains of waste products and contaminated soil.

Cases of transmission of the disease from an infected person to healthy people have not been registered.
Mouse Fever Symptoms
The disease manifests itself in several stages:
In the initial stage, which takes about 3 days, the first signs of mouse fever resemble the flu or an acute viral infection. There is an increase in temperature, aches and pain in the muscles, chills and weakness, thirst, a decrease in pressure and a slowing of the pulse. Many patients complain of inflammation of the mucous membrane of the eyes, conjunctivitis, and a rash.
At the next stage, the patient has nausea and vomiting, swelling of the face and body, bloating of the abdominal cavity, back pain in the lumbar region. The duration of this period is about 10-11 days. In the absence of medical attention, with symptoms of mouse fever, there is a risk of internal bleeding with subsequent death.
Thanks to timely medical care, the patient's recovery takes about one to one and a half months. Complete disposal of the body from the pathogen and symptoms of mouse fever in men and women is observed after 4-6 months.
Complete disposal of the body from the pathogen and symptoms of mouse fever in men and women is observed after 4-6 months.
Consequences of mouse fever
The presence in the body of complex diseases of internal organs, the general depressed state of the immune system and the rapid development of the disease against the background of the lack of timely medical care can cause the development of the following pathologies:
- pancreatitis;
- myocarditis;
- sepsis;
- edematous phenomena in the lungs;
- meningitis, cerebral hemorrhage;
- renal failure.
The combination of the listed consequences of mouse fever contributes to the rapid deterioration of the patient's condition and can lead to irreversible consequences in the body.
Diagnostic methods
Some signs of an infectious disease can be detected at the stage of visual examination and history taking. Confirm the doctor's assumptions allow the analysis of PCR (polymerase chain reaction) enzyme immunoassay, showing the presence of antibodies to the pathogen in the blood. Radiography, ultrasound diagnostics and urinalysis allow to clarify the state of internal organs.
Radiography, ultrasound diagnostics and urinalysis allow to clarify the state of internal organs.
How to treat?
Putting off going to the doctor, hoping for the results of folk methods, is a serious risk. The result of such a decision can be a significant deterioration in the patient's condition up to the failure of internal organs, extensive internal bleeding and death. Moreover, the medical institution will offer comprehensive treatment aimed at eliminating the symptoms and causes of the pathology:
- intravenous injections of ribavirin;
- the introduction of saline and glucose solution to restore the basic functions and nutrition of the body;
- a course of multivitamin preparations;
- blood transfusion, excluding the consequences of its infection with a pathogen.
A therapeutic diet with the complete exclusion of spicy and spicy foods, alcohol, vinegar and seasonings can speed up recovery.
Ways to Prevent Infection with Mouse Fever
You can avoid infection by following these guidelines:
- regular cleaning of the premises of a country house and an agricultural enterprise using automatic equipment and disinfectants;
- protection of the skin of the hands and respiratory tract when cleaning or working with open ground;
- destruction of food spoiled by rodents;
- sealing joints and seams through which uninvited vectors of infection can enter the room;
- storage of foodstuffs in hermetically sealed containers;
- thorough heat treatment of food before eating.
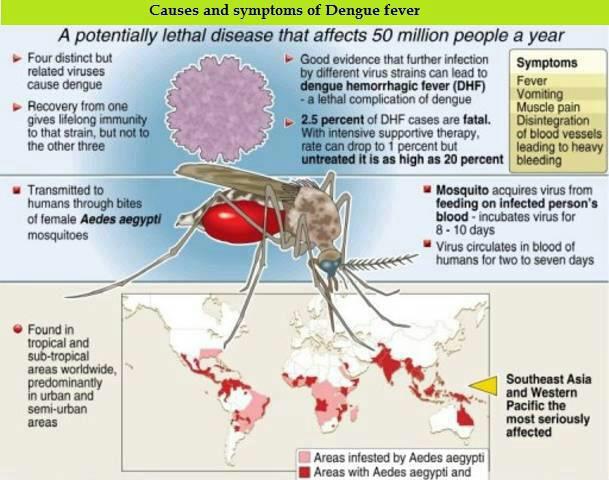
Other recommendations for infection prevention can be obtained from the attending physician who supervises the treatment of murine fever.
Diagnosis and treatment of mouse fever in Moscow
The qualified staff of the clinic of JSC "Medicina" in the Central Administrative District of Moscow invites patients with the first signs of the disease for an initial consultation, diagnosis and treatment of mouse fever. All the necessary examinations and procedures can be done at the medical center, equipped with advanced equipment from leading world manufacturers. Each patient is guaranteed an attentive attitude, careful development of an individual treatment course, control of specialists and confidentiality of personal information. You can make an appointment on the clinic's website or by calling the indicated numbers in Moscow.
Questions and answers
What is mouse fever?
Mouse fever is the second name for hemorrhagic fever with renal syndrome.