Dsm 5 mood disorder list
Appendix D—DSM-IV-TR Mood Disorders - Managing Depressive Symptoms in Substance Abuse Clients During Early Recovery
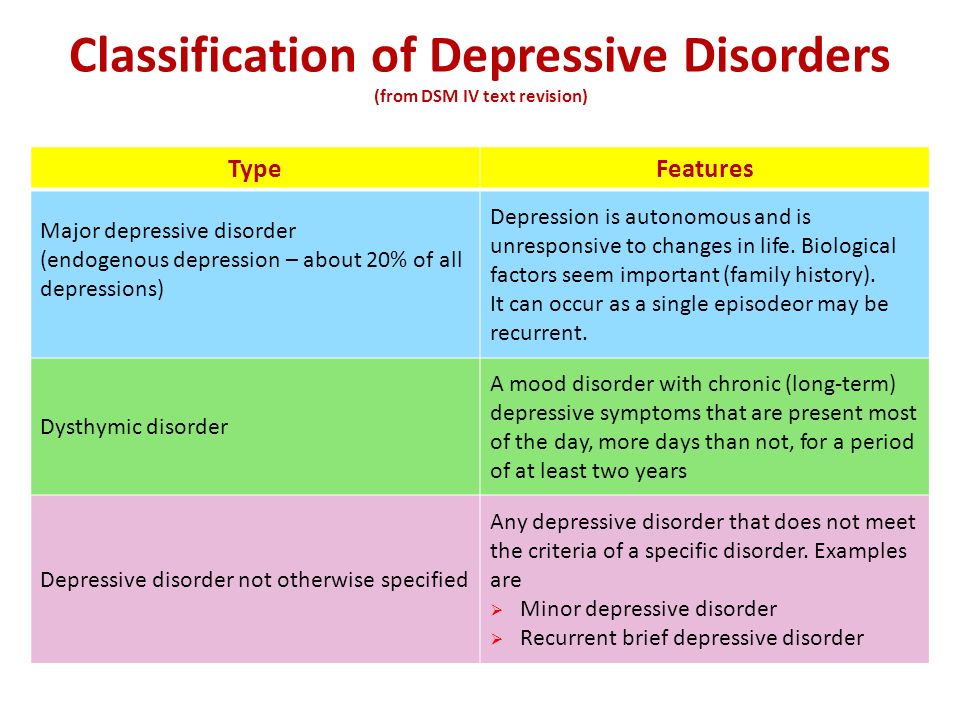
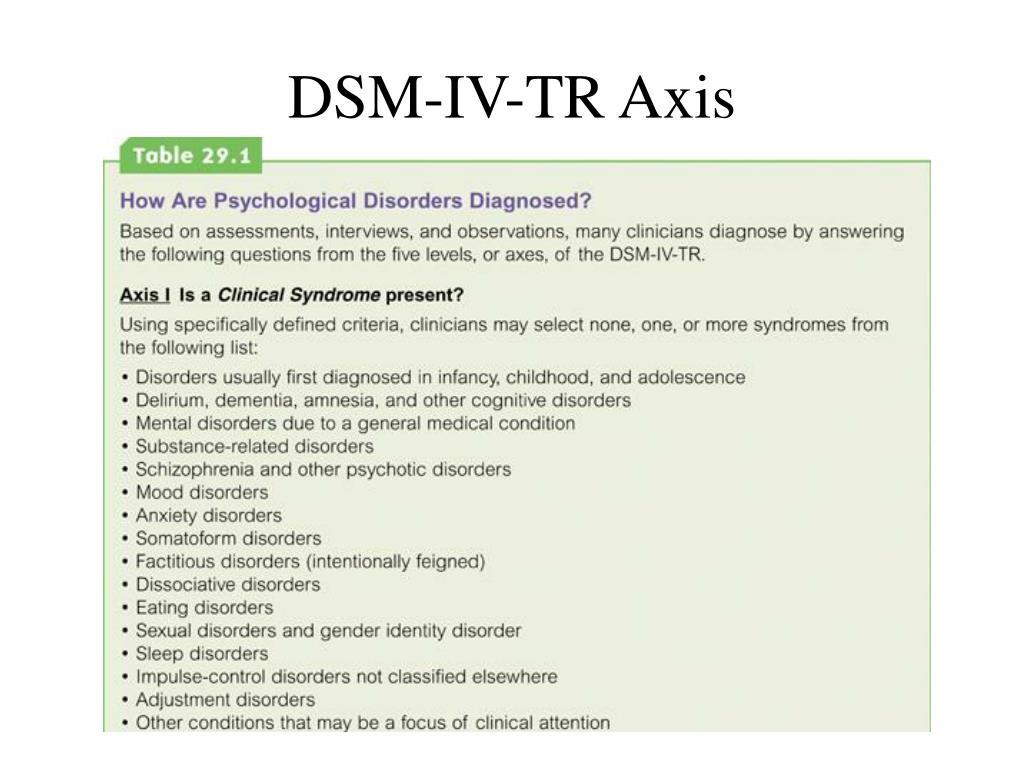
In substance abuse treatment settings, you are likely to encounter clients with a variety of diagnoses of depressive illnesses. Most of these diagnoses fall in the category of Mood Disorders, as specified in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR; APA, 2000). You can, however, also work with people who have a diagnosis of Adjustment Disorder with Depressed Mood. Additionally, people with a variety of other psychiatric illnesses are susceptible to depression, and some of those illnesses are described in this appendix.
The descriptions of depressive disorders and their primary symptoms are taken from DSM-IV-TR. Please refer to the source document for a more complete description of these disorders.
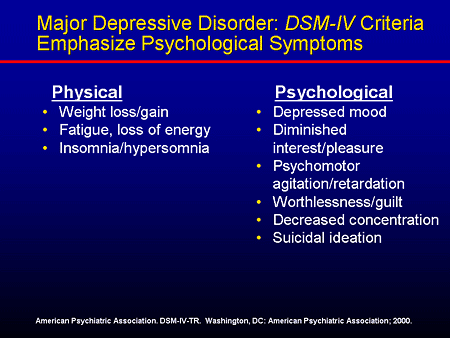
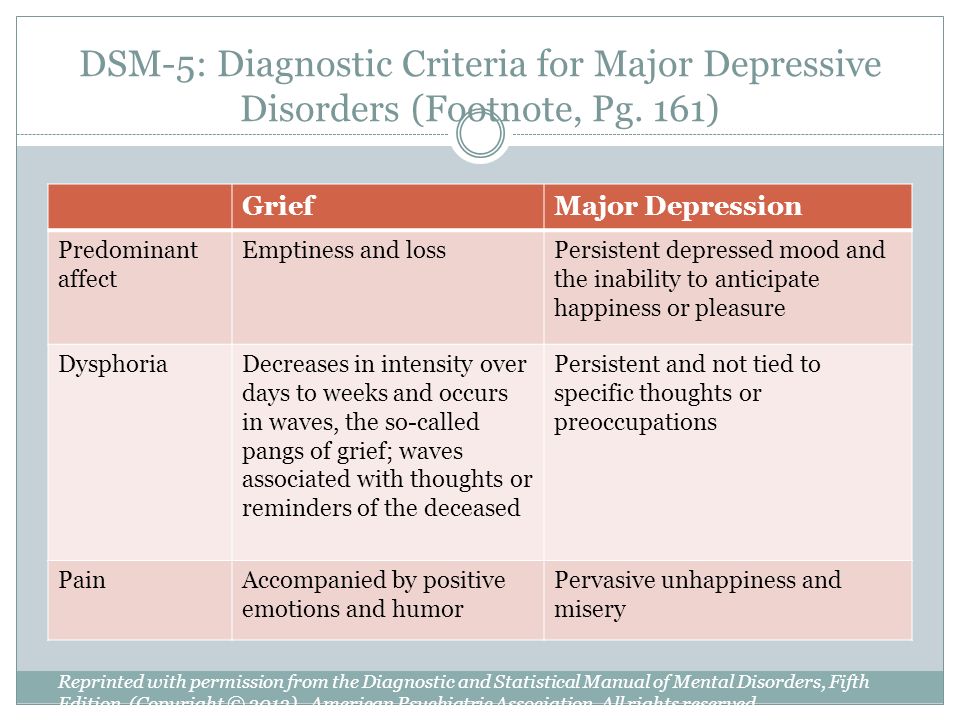
1. Major Depressive Episode and Major Depressive Disorder
Major Depressive Disorder requires two or more major depressive episodes.
Diagnostic criteria:
Depressed mood and/or loss of interest or pleasure in life activities for at least 2 weeks and at least five of the following symptoms that cause clinically significant impairment in social, work, or other important areas of functioning almost every day
- 1.
Depressed mood most of the day.
- 2.
Diminished interest or pleasure in all or most activities.
- 3.
Significant unintentional weight loss or gain.
- 4.
Insomnia or sleeping too much.
- 5.
Agitation or psychomotor retardation noticed by others.
- 6.
Fatigue or loss of energy.
- 7.
Feelings of worthlessness or excessive guilt.
- 8.
Diminished ability to think or concentrate, or indecisiveness.
- 9.
Recurrent thoughts of death (APA, 2000, p. 356).
2. Dsythymic Disorder
Diagnostic criteria:
Depressed mood most of the day for more days than not, for at least 2 years, and the presence of two or more of the following symptoms that cause clinically significant impairment in social, work, or other important areas of functioning:
- 1.
Poor appetite or overeating.
- 2.
Insomnia or sleeping too much.
- 3.
Low energy or fatigue.
- 4.
Low self-esteem.
- 5.
Poor concentration or difficulty making decisions.
- 6.
Feelings of hopelessness (APA, 2000, p. 380).
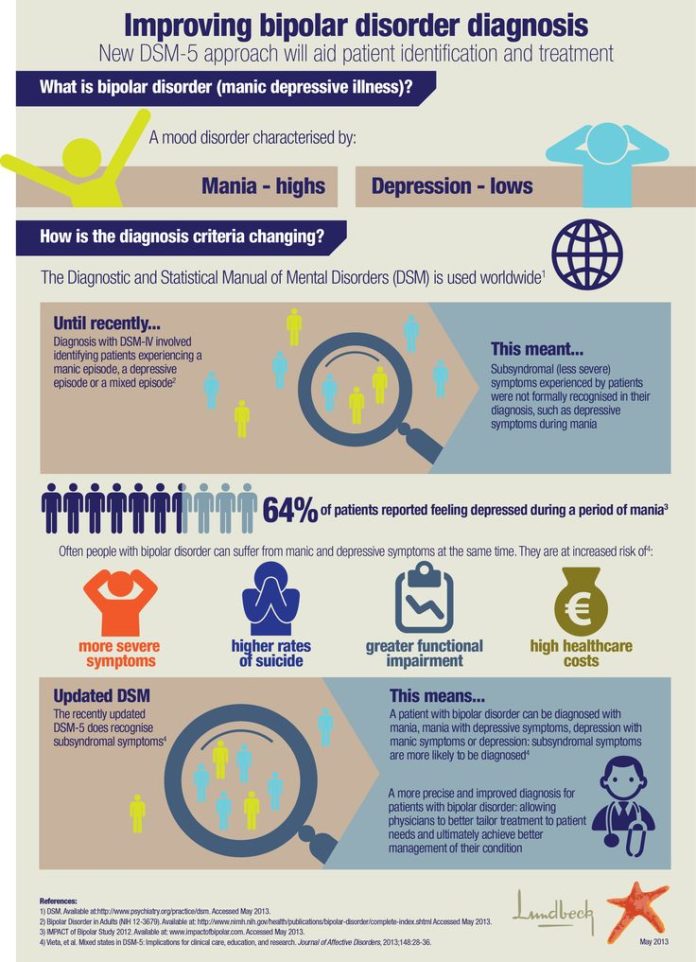
3. Bipolar Episode and Bipolar Disorder
Bipolar disorder is characterized by more than one bipolar episode.
There are three types of bipolar disorder:
- 1.
Bipolar 1 Disorder, in which the primary symptom presentation is manic, or rapid (daily) cycling episodes of mania and depression.
- 2.
Bipolar 2 Disorder, in which the primary symptom presentation is recurrent depression accompanied by hypomanic episodes (a milder state of mania in which the symptoms are not severe enough to cause marked impairment in social or occupational functioning or need for hospitalization, but are sufficient to be observable by others).
- 3.
Cyclothymic Disorder, a chronic state of cycling between hypomanic and depressive episodes that do not reach the diagnostic standard for bipolar disorder (APA, 2000, pp. 388–392).
Manic episodes are characterized by:
- A.
A distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least 1 week (or any duration if hospitalization is necessary)
- B.
During the period of mood disturbance, three (or more) of the following symptoms have persisted (4 if the mood is only irritable) and have been present to a significant degree:
- (1)
increased self-esteem or grandiosity
- (2)
decreased need for sleep (e.g., feels rested after only 3 hours of sleep)
- (3)
more talkative than usual or pressure to keep talking
- (4)
flight of ideas or subjective experience that thoughts are racing
- (5)
distractibility (i.
 e., attention too easily drawn to unimportant or irrelevant external stimuli)
e., attention too easily drawn to unimportant or irrelevant external stimuli)- (6)
increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation
- (7)
excessive involvement in pleasurable activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments)” (APA, 2000, p. 362).
Depressive episodes are characterized by symptoms described above for Major Depressive Episode.
4. Substance-Induced Mood Disorder
Substance-Induced Mood Disorder is a common depressive illness of clients in substance abuse treatment. It is defined in DSM-IV-TR as “a prominent and persistent disturbance of mood … that is judged to be due to the direct physiological effects of a substance (i.e., a drug of abuse, a medication, or somatic treatment for depression, or toxin exposure)” (APA, 2000, p.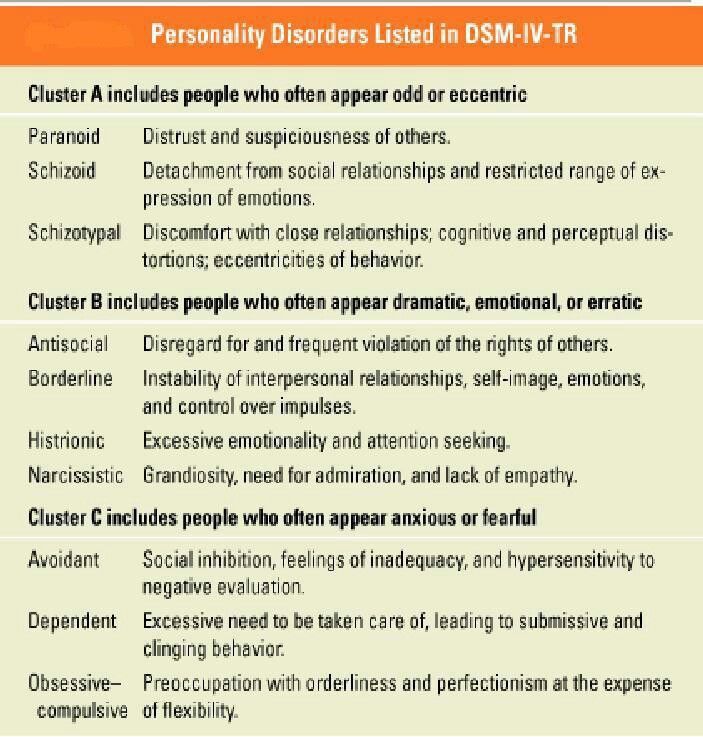 405). The mood can manifest as manic (expansive, grandiose, irritable), depressed, or a mixture of mania and depression.
405). The mood can manifest as manic (expansive, grandiose, irritable), depressed, or a mixture of mania and depression.
Generally, substance-induced mood disorders will only present either during intoxication from the substance or on withdrawal from the substance and therefore do not have as lengthy a course as other depressive illnesses.
5. Mood Disorder Due to a General Medical Condition
It is not as common to find depression due to a general medical condition in substance-abuse treatment settings, but it is important to note that depression can be a result of a medical condition, such as hypothyroidism or Parkinson's disease. The criteria for diagnosis are similar to Major Depressive Episode or a manic episode; however, the full criteria for these diagnoses need not be met. It is important in diagnosis to establish that the depressive symptoms are a direct physiological result of the medical condition, not just a psychological response to a medical problem.
6.
 Adjustment Disorder With Depressed Mood
Adjustment Disorder With Depressed MoodAdjustment disorder is a psychological reaction to overwhelming emotional or psychological stress, resulting in depression or other symptoms. Some situations in which an adjustment disorder can occur include divorce, imprisonment of self or a significant other, business or employment failures, or a significant family disturbance. The stressor may be a one-time event or a recurring situation. Because of the turmoil that often occurs around a crisis in substance use patterns, clients in substance abuse treatment may be particularly susceptible to Adjustment Disorders. Some of the common depressive symptoms of an adjustment disorder include tearfulness, depressed mood, and feelings of hopelessness. The symptoms of an adjustment disorder normally do not reach the proportions of a Major Depressive Disorder, nor do they last as long as a Dysthymic Disorder. An acute adjustment disorder normally lasts only a few months, while a chronic adjustment disorder may be ongoing after the termination of the stressor.
7. Other Psychiatric Conditions in Which Depression Can Be a Primary Symptom
Sometimes depression is symptomatic of another mental disorder. This is particularly true when the nature of the mental disorder causes excessive distress to the individual. While, in this context, the depression is a symptom, it is still important to recognize its impact on the person and his or her ability to respond to substance abuse treatment.
Some of the psychiatric disorders in which depression can play a major role include:
- A.
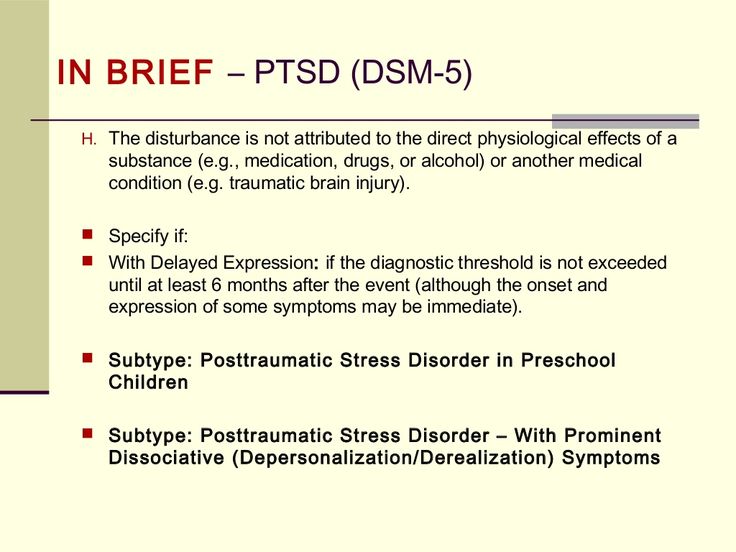
Posttraumatic Stress Disorder (PTSD)
Symptoms include episodes of reexperiencing the traumatic event or reexperiencing the emotions attached to the event; nightmares, exaggerated startle responses; and social, interpersonal, and psychological withdrawal. Chronic symptoms may include anxiety and depression. PTSD is categorized as an anxiety disorder.
- B.
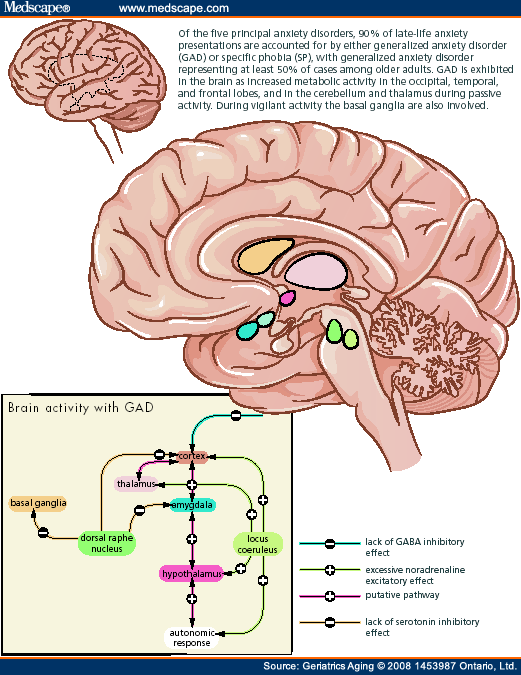
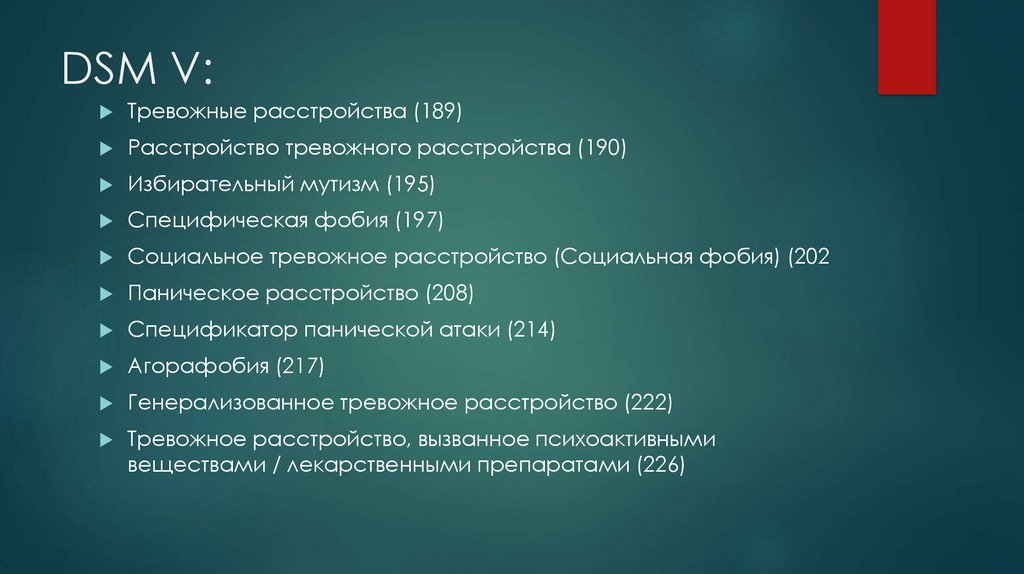
Anxiety Disorders, including Panic Disorder, Agoraphobia (fear of public places), Social Phobias, and Generalized Anxiety Disorder
Symptoms of anxiety disorders are most often on the anxiety spectrum, but the chronic stress faced by individuals with anxiety disorders can produce depressive symptoms including irritability, hopelessness, despair, emptiness, and chronic fatigue.
- C.
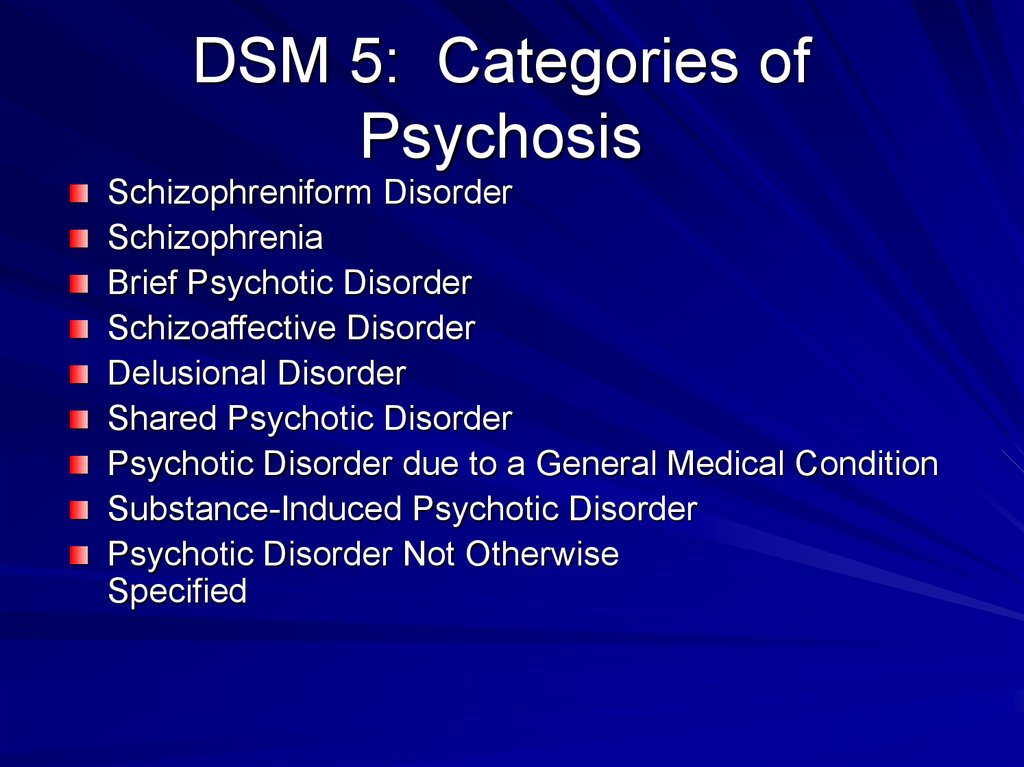
Schizoaffective Disorder and Schizophrenia
Individuals with schizoaffective disorder have, in addition to many of the symptoms of schizophrenia, a chronic depression with most of the features of Major Depressive Disorder. Because of the difficulty individuals with schizophrenia have in coping with the daily demands of living, depression is often a symptom. With both schizoaffective disorder and schizophrenia, the depression adds an additional dimension to treatment, specifically in helping the person mobilize in the face of their depression to cope with their illness.
- D.
Personality Disorders
People with personality disorders are particularly susceptible to depression. These individuals are at high risk for substance use disorders. As a result, it is not uncommon to find clients in substance abuse treatment with all three diagnoses. Because personality disorders are categorized in DSM-IV-TR as Axis 2 disorders (see DSM-IV-TR for a description of multiaxial assessment), it is common to find their depression diagnosed separately (from the personality disorder) as an adjustment disorder, dysthymia, or major depressive disorder.
Mood Disorders | Johns Hopkins Medicine
A mood disorder is a mental health class that health professionals use to broadly describe all types of depression and bipolar disorders.
Children, teens, and adults can have mood disorders. However, children and teens don’t always have the same symptoms as adults. It’s harder to diagnose mood disorders in children because they aren’t always able to express how they feel.
Therapy, antidepressants, and support and self-care can help treat mood disorders.
What are the different types of mood disorders?
These are the most common types of mood disorders:
-
Major depression. Having less interest in usual activities, feeling sad or hopeless, and other symptoms for at least 2 weeks may indicate depression.
-
Dysthymia. This is a chronic, low-grade, depressed, or irritable mood that lasts for at least 2 years.
-
Bipolar disorder. This is a condition in which a person has periods of depression alternating with periods of mania or elevated mood.
-
Mood disorder related to another health condition. Many medical illnesses (including cancer, injuries, infections, and chronic illnesses) can trigger symptoms of depression.
-
Substance-induced mood disorder. Symptoms of depression that are due to the effects of medicine, drug abuse, alcoholism, exposure to toxins, or other forms of treatment.
What causes mood disorders?
Many factors contribute to mood disorders. They are likely caused by an imbalance of brain chemicals. Life events (such as stressful life changes) may also contribute to a depressed mood. Mood disorders also tend to run in families.
Who is at risk for mood disorders?
Anyone can feel sad or depressed at times.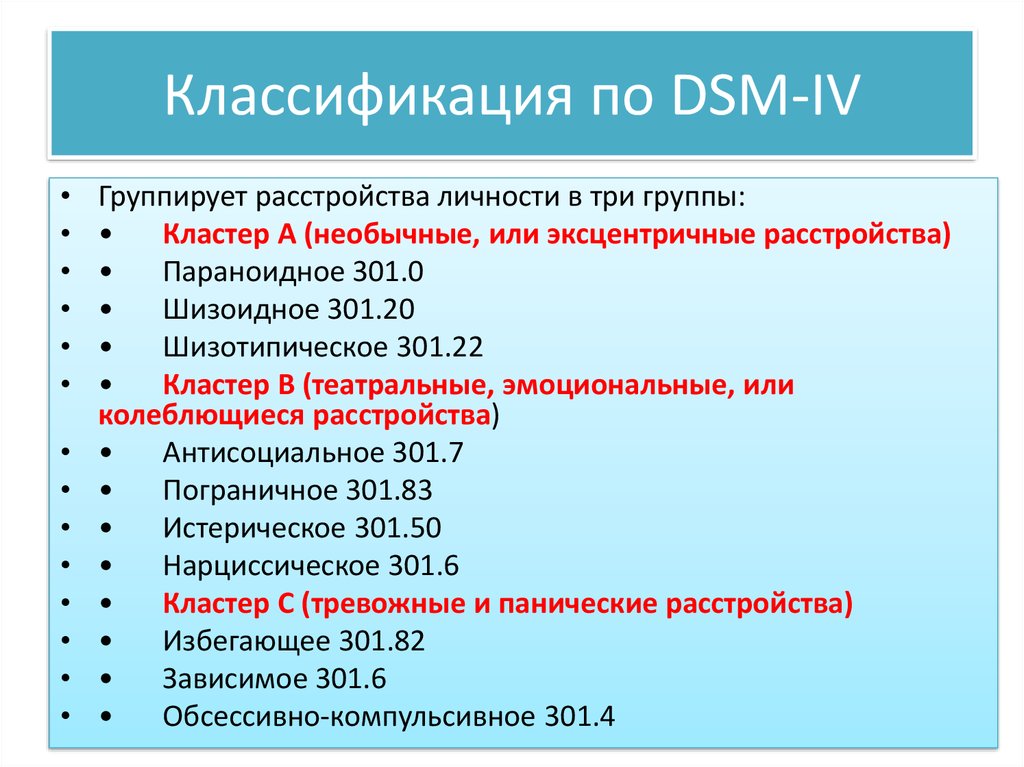 However, mood disorders are more intense and harder to manage than normal feelings of sadness. Children, teens, or adults who have a parent with a mood disorder have a greater chance of also having a mood disorder. However, life events and stress can expose or worsen feelings of sadness or depression. This makes the feelings harder to manage.
However, mood disorders are more intense and harder to manage than normal feelings of sadness. Children, teens, or adults who have a parent with a mood disorder have a greater chance of also having a mood disorder. However, life events and stress can expose or worsen feelings of sadness or depression. This makes the feelings harder to manage.
Sometimes, life's problems can trigger depression. Being fired from a job, getting divorced, losing a loved one, death in the family, and financial trouble, to name a few, all can be difficult and coping with the pressure may be troublesome. These life events and stress can bring on feelings of sadness or depression or make a mood disorder harder to manage.
The risk of depression in women is nearly twice as high as it is for men. Once a person in the family has this diagnosis, their brothers, sisters, or children have a higher chance of the same diagnosis. In addition, relatives of people with depression are also at increased risk for bipolar disorder .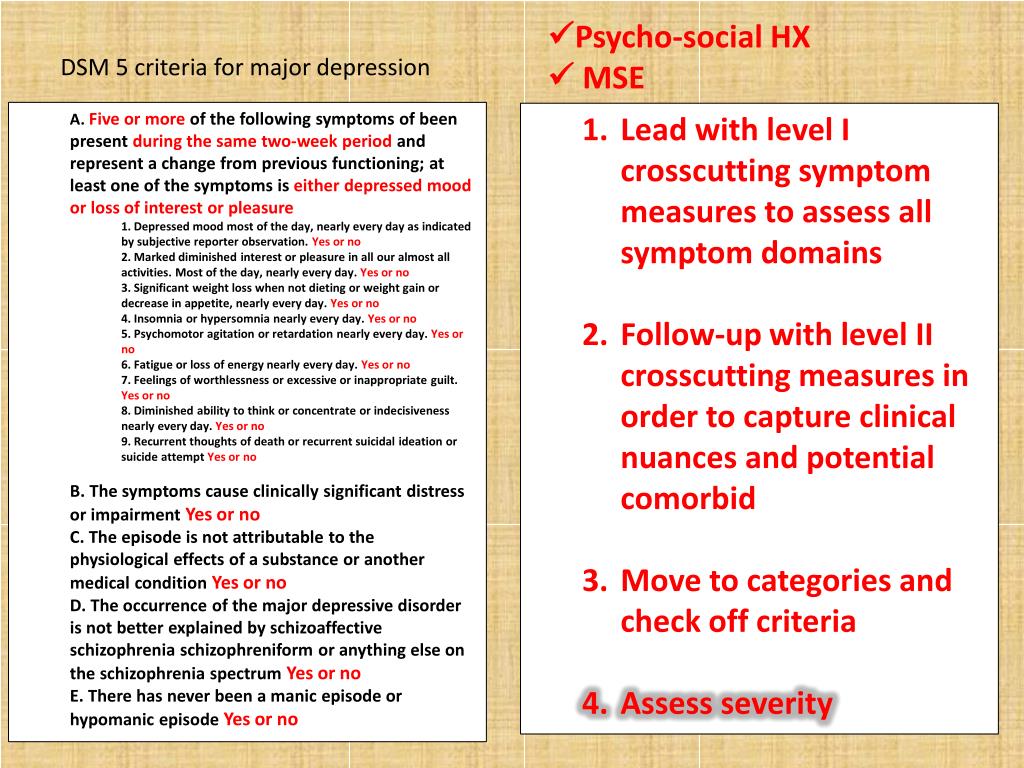
Once a person in the family has a diagnosis of bipolar disorder, the chance for their brothers, sisters, or children to have the same diagnosis is increased. Relatives of people with bipolar are also at increased risk for depression.
What are the symptoms of mood disorders?
Depending on age and the type of mood disorder, a person may have different symptoms of depression. The following are the most common symptoms of a mood disorder:
-
Ongoing sad, anxious, or “empty” mood
-
Feeling hopeless or helpless
-
Having low self-esteem
-
Feeling inadequate or worthless
-
Excessive guilt
-
Repeating thoughts of death or suicide, wishing to die, or attempting suicide (Note: People with this symptom should get treatment right away!)
-
Loss of interest in usual activities or activities that were once enjoyed, including sex
-
Relationship problems
-
Trouble sleeping or sleeping too much
-
Changes in appetite and/or weight
-
Decreased energy
-
Trouble concentrating
-
A decrease in the ability to make decisions
-
Frequent physical complaints (for example, headache, stomachache, or tiredness) that don’t get better with treatment
-
Running away or threats of running away from home
-
Very sensitive to failure or rejection
-
Irritability, hostility, or aggression
In mood disorders, these feelings are more intense than what a person may normally feel from time to time.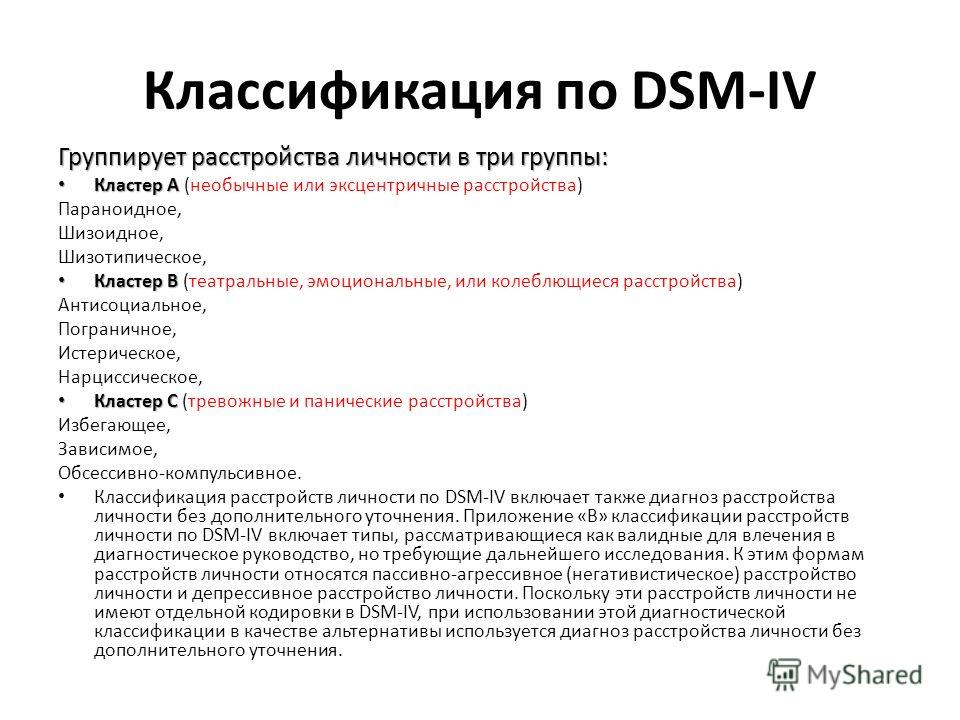 It’s also of concern if these feelings continue over time, or interfere with one's interest in family, friends, community, or work. Any person who expresses thoughts of suicide should get medical help right away.
It’s also of concern if these feelings continue over time, or interfere with one's interest in family, friends, community, or work. Any person who expresses thoughts of suicide should get medical help right away.
The symptoms of mood disorders may look like other conditions or mental health problems. Always talk with a healthcare provider for a diagnosis.
How are mood disorders diagnosed?
Mood disorders are a real medical disorder. A psychiatrist or other mental health professional usually diagnoses mood disorders through a complete medical history and psychiatric evaluation.
How are mood disorders treated?
Mood disorders can often be treated with success. Treatment may include:
-
Antidepressant and mood stabilizing medicines—especially when combined with psychotherapy have shown to work very well in the treatment of depression
-
Psychotherapy—most often cognitive-behavioral and/or interpersonal therapy.
 This therapy is focused on changing the person’s distorted views of himself or herself and the environment around him or her. It also helps to improve interpersonal relationship skills, and identifying stressors in the environment and how to avoid them
This therapy is focused on changing the person’s distorted views of himself or herself and the environment around him or her. It also helps to improve interpersonal relationship skills, and identifying stressors in the environment and how to avoid them -
Family therapy
-
Other therapies, such as electroconvulsive therapy and transcranial stimulation
Families play a vital supportive role in any treatment process.
When correctly diagnosed and treated, people with mood disorders can live, stable, productive, healthy lives.
Can mood disorders be prevented?
At this time, there are no ways to prevent or reduce the incidence of mood disorders. However, early diagnosis and treatment can reduce the severity of symptoms, enhance the person’s normal growth and development, and improve the quality of life of people with mood disorders.
Key points about mood disorders
-
A mood disorder is a mental health class that health professionals use to broadly describe all types of depression and bipolar disorders.
-
The most common types of mood disorders are major depression, dysthymia (dysthymic disorder), bipolar disorder, mood disorder due to a general medical condition, and substance-induced mood disorder.
-
There is no clear cause of mood disorders. Healthcare providers think they are a result of chemical imbalances in the brain. Some types of mood disorders seem to run in families, but no genes have yet been linked to them.
-
In general, nearly everyone with a mood disorder has ongoing feelings of sadness, and may feel helpless, hopeless, and irritable. Without treatment, symptoms can last for weeks, months, or years, and can impact quality of life.
-
Depression is most often treated with medicine, psychotherapy or cognitive behavioral therapy, family therapy, or a combination of medicine and therapy. In some cases, other therapies, such as electroconvulsive therapy and transcranial stimulation may be used.
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
The good news is that personality disorders can still be managed—there is a cure.
Now officially: BPD is a diagnosis
Borderline personality disorder is one of the ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.
People with BPD are reverse solipsists: they are convinced of the inviolability of the world around them, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves.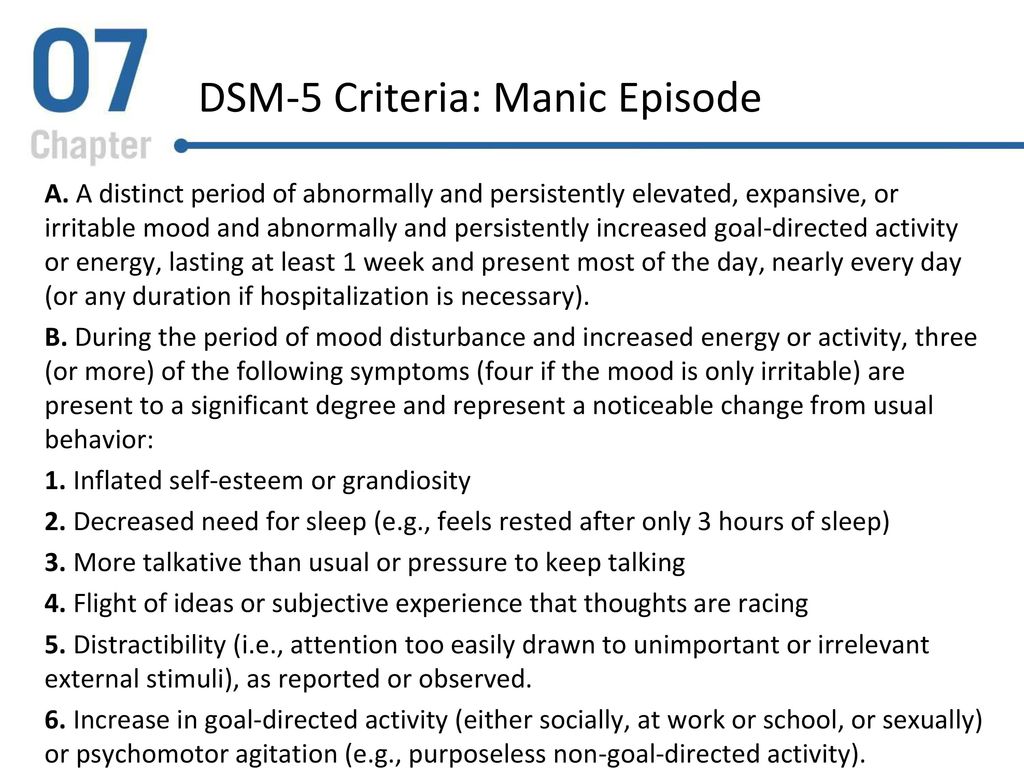 "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
"Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.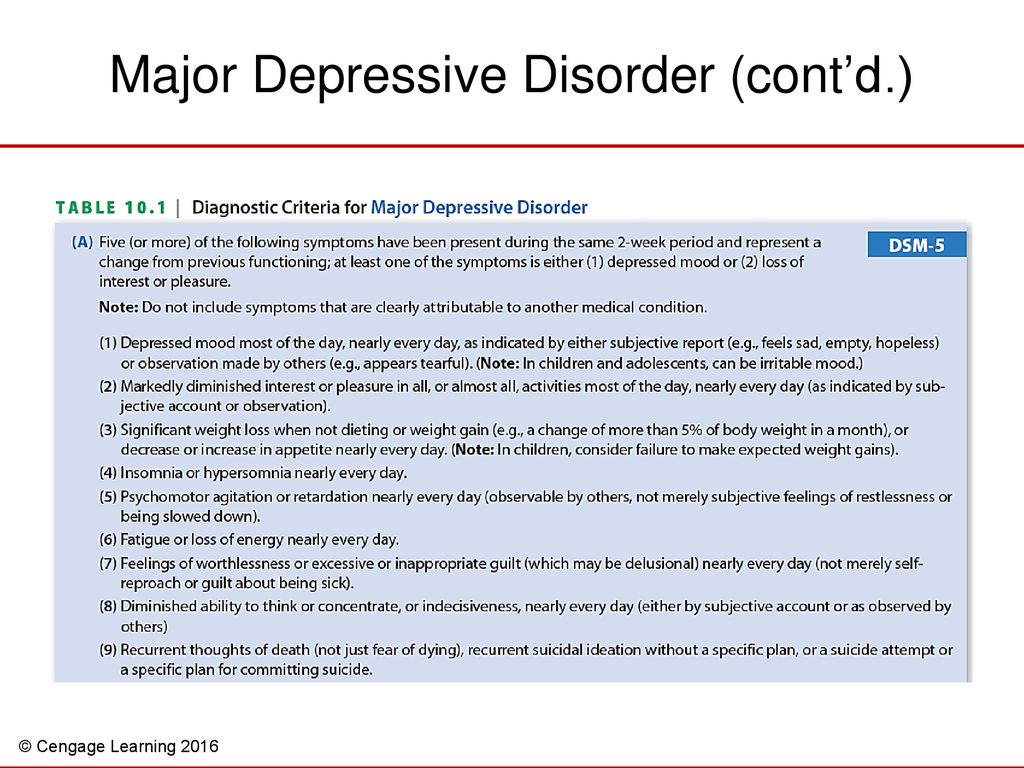
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances.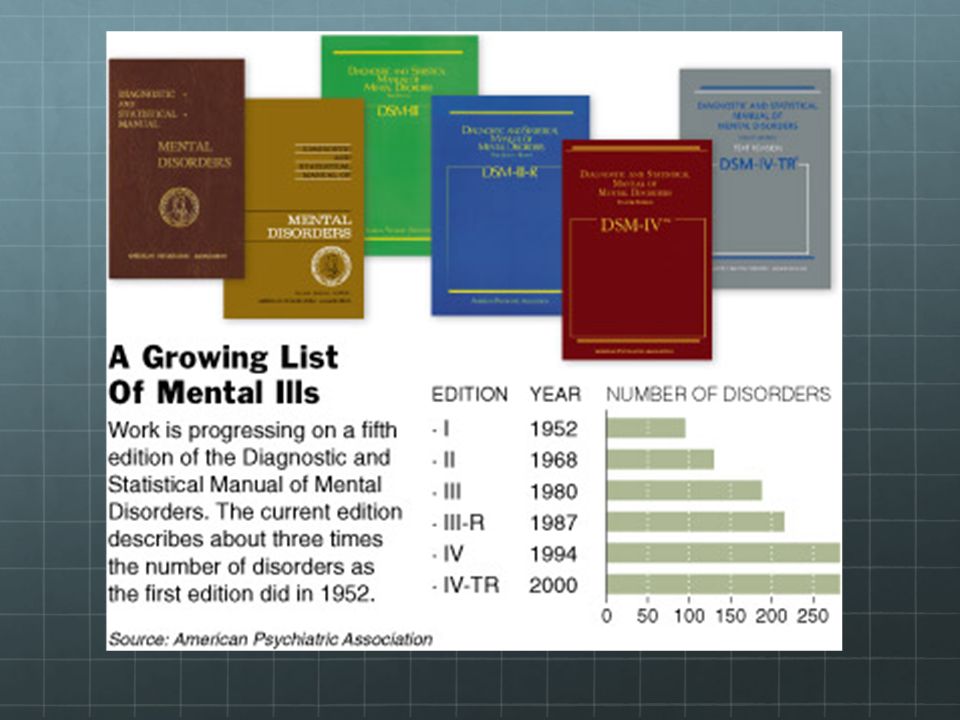 The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).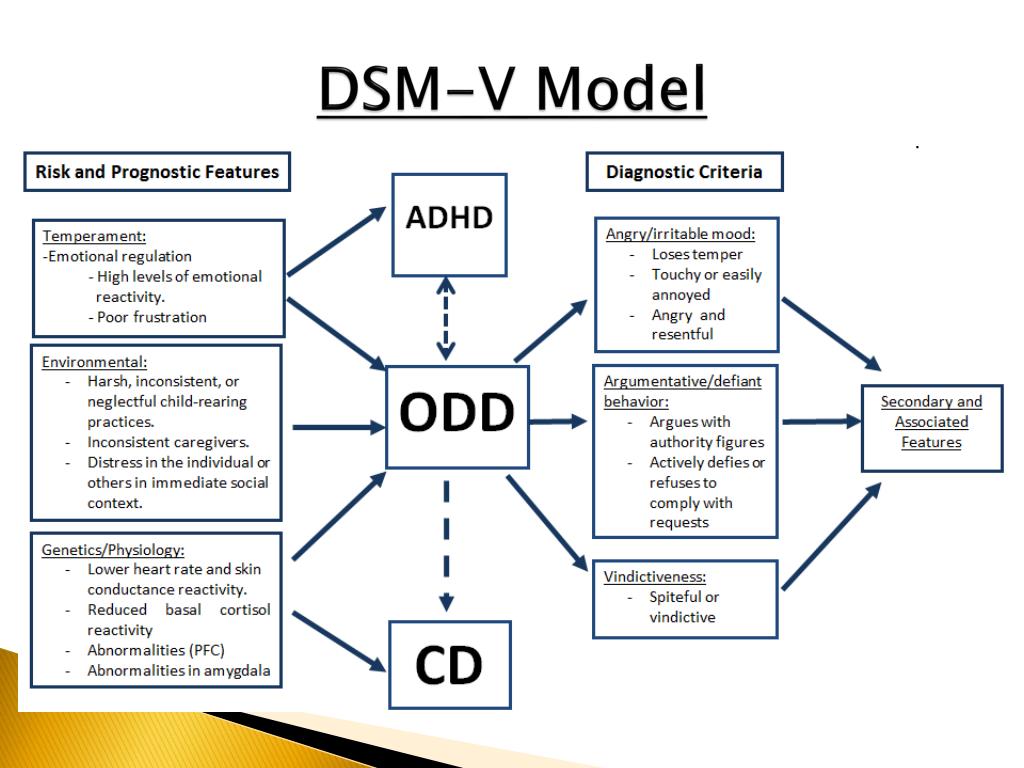
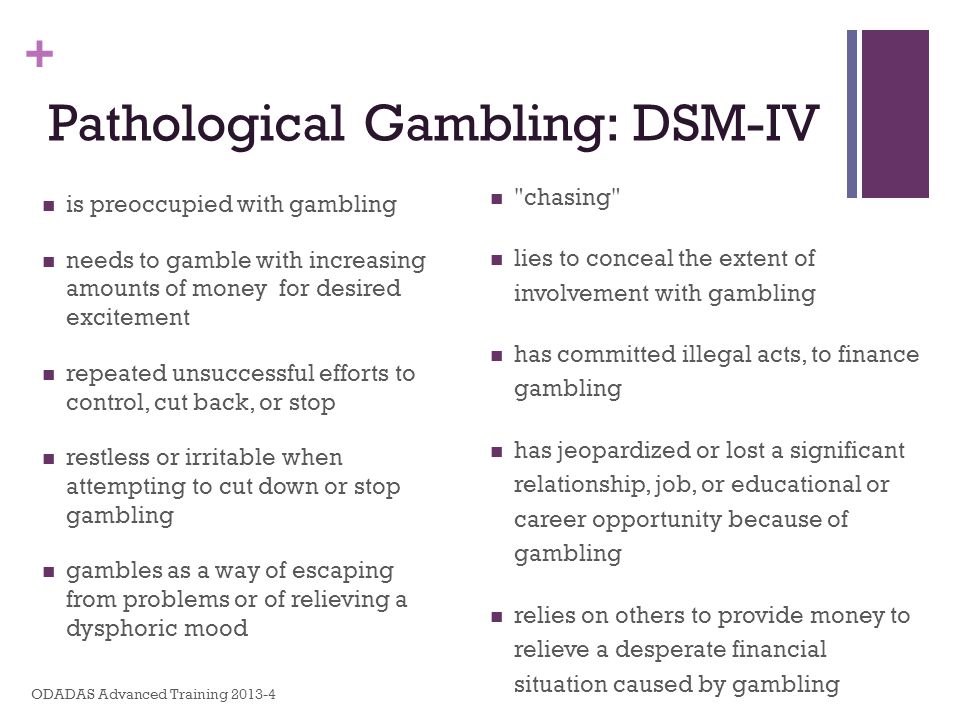
Borderline personality disorder can be accompanied by alcohol, drug, gambling addiction and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health information resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone. You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
- Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control. In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
- Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with an interruption in communication, because not everyone is able to endure such a bolt from the blue.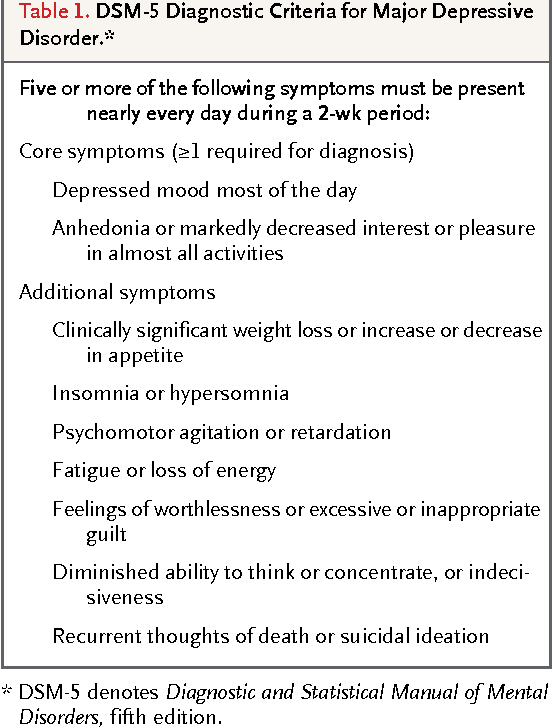 And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires identifying the cause. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality.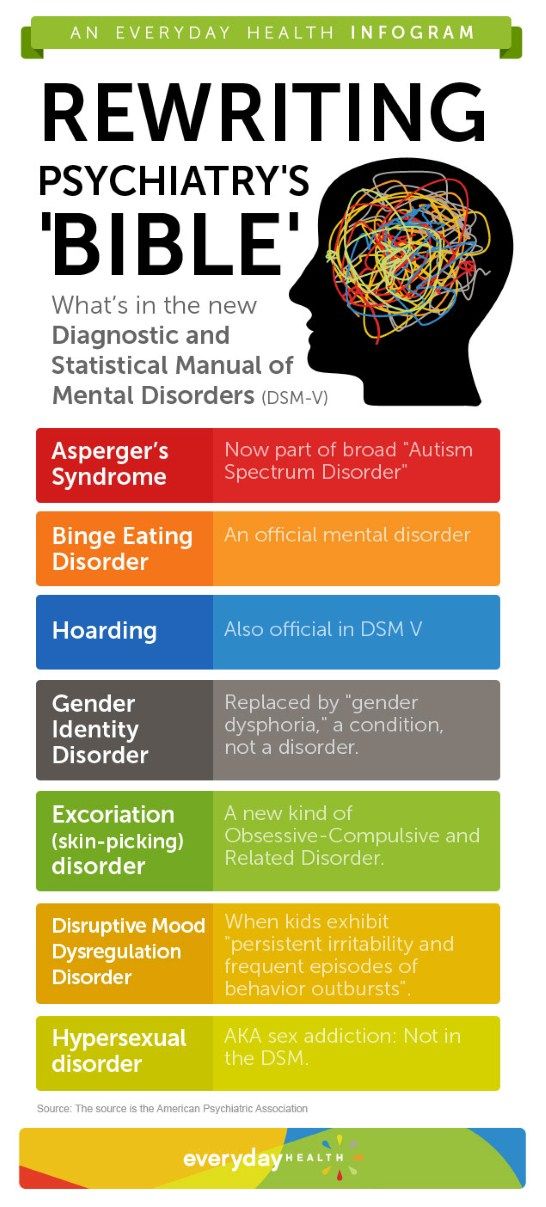 That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations.
 For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder. - Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of.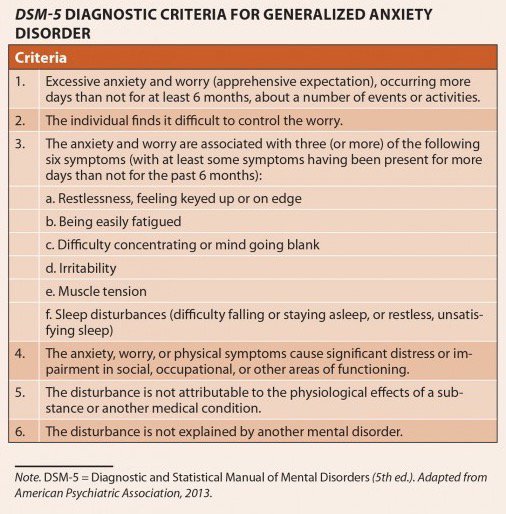 At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
 Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”.
Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”. Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills.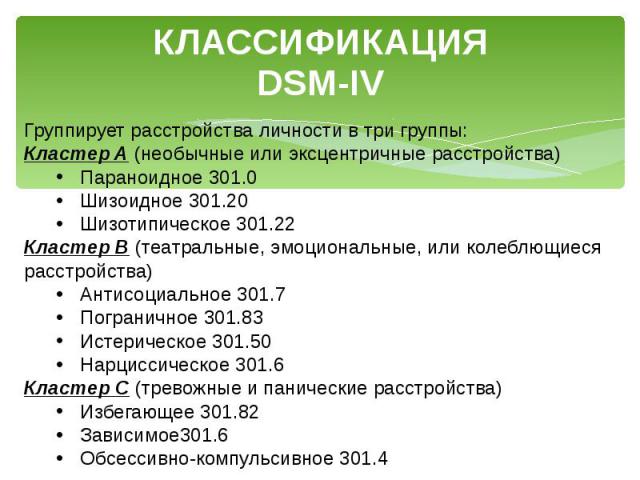 Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT). Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
- Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Psychotherapy (TFP) teaches to perceive positive and negative qualities simultaneously, to get out of the "deification/devaluation" paradigm.
- Cognitive Behavioral Therapy helps to change the way of thinking, reactions to stress and correct affective patterns of behavior.
- Schematic therapy is a complex treatment based on psychoanalysis and gestalt therapy. It changes the behavioral patterns laid down in childhood or adolescence.
- Self help. It consists in tracking the dynamics of emotions, asking yourself questions like “how do I feel now?”, “What does he (a) specifically want from me?”, “Is this reality or my fiction?”.
To improve their inner state, people with BPD are advised to start meditating, exercising, walking more often in the fresh air, trying to rationalize their own mood swings, learning self-soothing techniques and training willpower in order to stop emotional breakdowns in time.
Related material
Borderline personality disorder
Borderline personality disorder is associated with unstable mood and behavior that has a significant impact on a person's daily life
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable moods and behaviors, and an altered "feeling of self. "1 everyday life. 1.2
"1 everyday life. 1.2
Borderline personality disorder is a serious illness associated with self-harm and suicidal attempts. One in ten patients complete suicide. 2
Facts About Borderline Personality Disorder
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable mood and behavior, and an altered sense of self. 1
One in ten patients complete suicide. 2
Patients with borderline personality disorder are very sensitive to changes in their environment, and may respond inappropriately and acutely to such changes. They may, for example, be afraid of being abandoned by a loved one.2 If the person whom patient
is expecting arrives late, the patient easily changes the feeling of attachment to dislike or anger.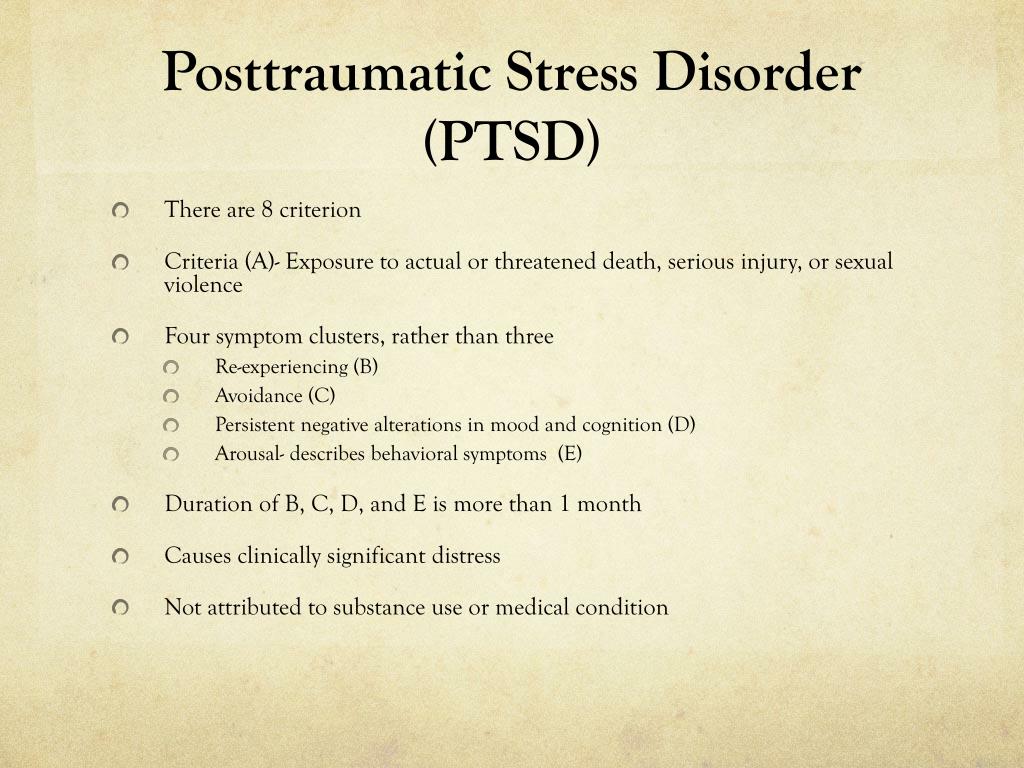 1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
People with borderline personality disorder are often insecure, may suddenly change their life goals and views on career, life values and friends.2 Such patients have impulsive and dangerous behavior: reckless spending, unsafe driving, addiction to chemicals. 2 They may develop intense unwarranted anger or feelings of emptiness, and are prone to self-harm.2 Patients with borderline personality disorder may also experience depression and anxiety.1,2
Facts about Borderline Personality Disorder
Estimates of the proportion of people who have borderline personality disorder vary from less than 1% to around 6%. 2-4
Borderline personality disorder affects a roughly equal number of men and women, but appears to be more disabling in women the same frequency in men and women, but in women it is more severe.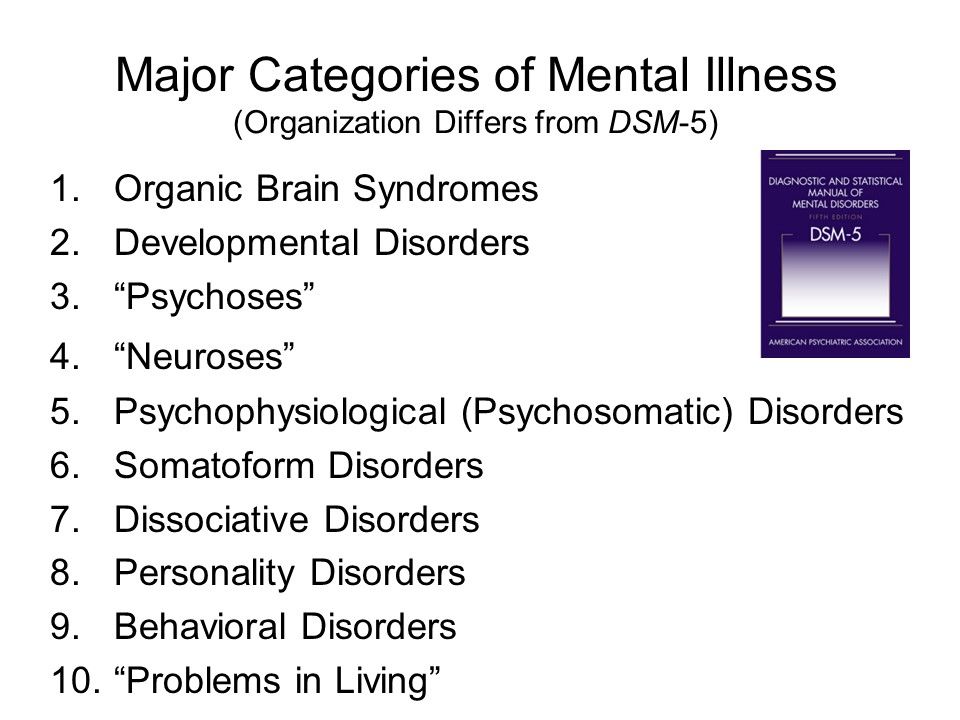 3
3
Symptoms of borderline personality disorder most often first appear during adolescence.4 The disease is most severe and problematic in young adults and tends to improve with age.2 Symptoms may persist throughout life, but most patients with borderline personality disorder by the age of 30-40 have a stable job and a home.2
People with borderline personality disorder are emotionally and functionally unstable, which places a significant burden on their families.5 Mood swings are a source of stress for both the patient and his or her others, which can lead to the development of mental disorders in the latter.1,5
People who are concerned that they – or their loved ones – are experiencing symptoms of borderline personality disorder should see their doctor for help and advice.
Borderline personality disorder is diagnosed by a mental health professional using interviews and discussions about symptoms and medical history.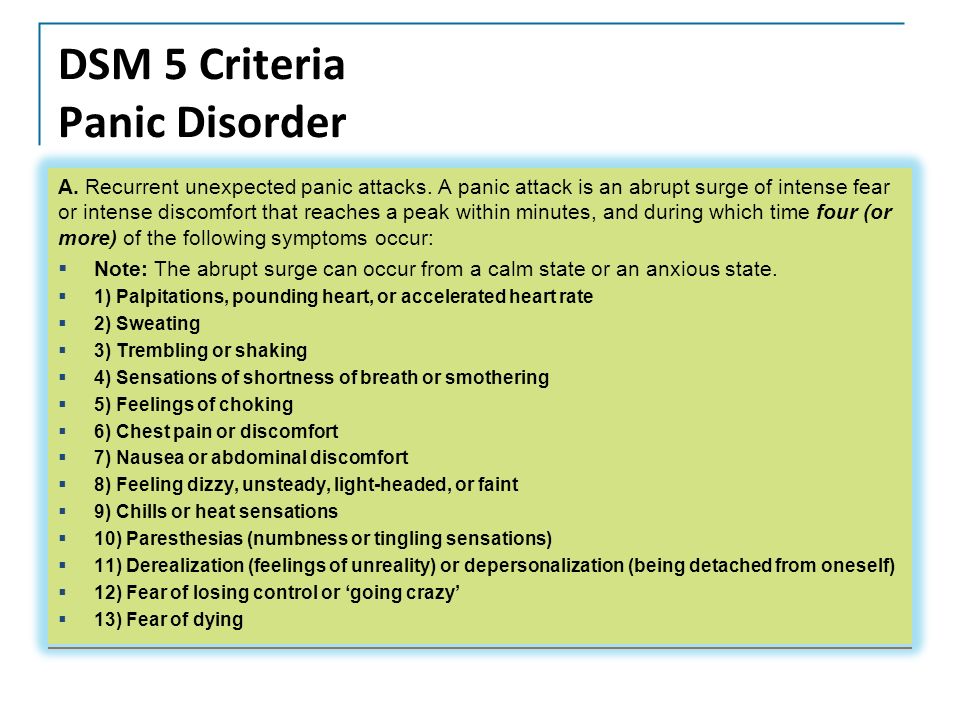 1
1
Psychotherapy can help people with borderline personality disorder by, for example, teaching them how to interact with others and to express their thoughts and feelings more clearly. 1 It may also be beneficial for caregivers and family members of those affected to receive therapy and guidance on how best to care for a person with borderline personality disorder. 1 There is currently no cure, but one study showed that, after 10 years, 50% of people with borderline personality disorder had recovered, being able to function at work and maintain personal relationships. 6
- National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
 5th ed. Arlington, VA: American Psychiatric Association; 2013.
5th ed. Arlington, VA: American Psychiatric Association; 2013. - Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
- National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
- Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258.
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study.
 Am J Psychiatry. 2010;167(6):663–667.
Am J Psychiatry. 2010;167(6):663–667.
1. National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
3. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
4. National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].