Brain fog anxiety symptom
Does Anxiety Cause Brain Fog?
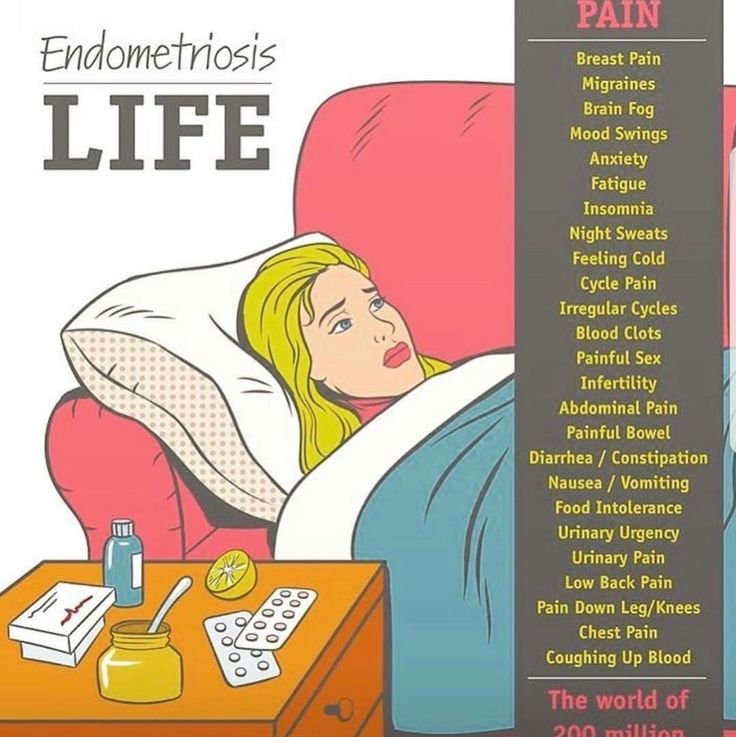
Struggling with a lack of concentration, muddied thinking, forgetfulness, memory problems, or other cognitive concerns? Occasional bouts of brain fog may be due to lack of sleep, overeating unhealthy foods, or the lingering aftermath of COVID-19. But, in certain cases of brain fog, there may be another underlying factor at work: anxiety.
Anxiousness is characterized by a range of symptoms, both relatively minor (feelings of nervousness, tendency to predict the worst, or physical symptoms like muscle tension) and more serious (panic attacks and suicidal thoughts). Anxiety disorders are the most common mental health condition in the country, affecting more than 40 million American adults (and disproportionately prevalent among women, teens, and those with ADD/ADHD).
When anxiety monopolizes the brain, other tasks suffer—including processing information, concentration, paying attention, and remembering. The result can feel like brain fog.The brain SPECT imaging work at Amen Clinics indicates that people with increased activity in the basal ganglia are vulnerable to anxiety. Other brain imaging research shows that ongoing stress actually causes shrinkage in the brain’s hippocampus, a region involved in the formation of memories. When anxiety takes over, the brain may not have the required capacity for other mental tasks, and a stress overload may decrease the generation of those neurons that typically form in the hippocampus.
In other words, an onslaught of anxiety can cause problems with how the brain functions and how it retains information. When anxiety monopolizes the brain, other tasks suffer—including processing information, concentration, paying attention, and remembering. The result can feel like brain fog, a state that causes people to act spaced-out, distracted, or forgetful.
SPECT can help determine if brain fog is anxiety-related, or if it might point to a serious long-term issue, such as dementia.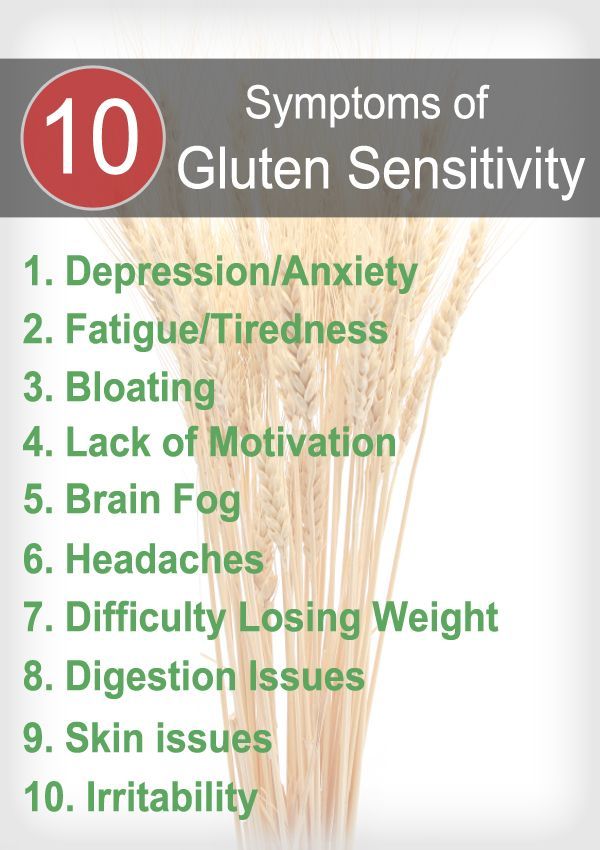 SPECT is a functional brain imaging technology that measures blood flow and activity in the brain and reveals areas with healthy levels of activity, or too much or too little activity. Because brain fog can point to a bigger problem (for example, if it has persisted and/or worsened over time or is starting to seriously interfere with everyday tasks), it’s important to pinpoint the root causes and develop an appropriate treatment plan as needed.
SPECT is a functional brain imaging technology that measures blood flow and activity in the brain and reveals areas with healthy levels of activity, or too much or too little activity. Because brain fog can point to a bigger problem (for example, if it has persisted and/or worsened over time or is starting to seriously interfere with everyday tasks), it’s important to pinpoint the root causes and develop an appropriate treatment plan as needed.
In some cases, it’s possible to clear brain fog and optimize cognitive function through brain healthy dietary choices, such as consuming filtered water, antioxidant-rich foods, and lean proteins, while aiming for the optimal nutrition-packed calorie counts on a daily basis. Additionally, nutritional supplements, including GABA, can help calm an overactive brain.
But if anxiety, specifically, is at the root of brain fog symptoms, there are a variety of practices designed to help tackle that issue. A number of studies, for example, have shown that holistic and natural solutions—think yoga, tai chi, biofeedback, and meditation—are often helpful, and usually can be undertaken without the risk of negative side effects.
A number of studies, for example, have shown that holistic and natural solutions—think yoga, tai chi, biofeedback, and meditation—are often helpful, and usually can be undertaken without the risk of negative side effects.
Rather than reaching for anti-anxiety medications, which can carry serious side effects, try these techniques to lessen anxiety and thus free up some brainpower for healthier brain functioning:
1. Try diaphragmatic breathing.
Did you know stress negatively affects your breathing? Rapid, shallow breaths—common during bouts of anxiety—can actually impact the blood’s oxygen levels and increase anxiety further. Calm your nervous system by repeating 10 cycles of this diaphragmatic breathing cycle: Inhale through the nose for 3 seconds, hold for 1 second, exhale for 6 seconds, and hold for 1 second. A bevy of research shows that diaphragmatic breathing practices are associated with reducing the negative consequences of stress, with the added benefit of improving cognitive performance.
Saying a prayer or meditating can help distract a brain that’s riddled with worry, while also stimulating prefrontal cortex activity (an area of the brain associated with focus). Even reading religious or spiritual texts, writing out personal prayers or gratitude lists, chanting, or memorizing inspirational passages can work to calm stress. A review of 32 clinical studies showed that religious practices such as these were associated with reduced anxiety.
3. Decrease the stress response.
Tactics like hypnosis, guided imagery, or progressive muscle relaxation may mitigate anxiety and even offer up ancillary benefits like better sleep. Alternatively, soothing music may help calm the brain, reduce anxiety, and sharpen focus. Aim for tunes with a slower tempo (between 60 and 80 beats per minute) versus more aggressive genres (120 to 200 or more beats per minute). You can even compile your own relaxing playlist with happy-making melodies—simply press “play” in those moments when stress threatens to overwhelm.
If calming anxiousness with these strategies doesn’t alleviate brain fog, it’s a good idea to consider getting a memory evaluation to determine what’s causing your symptoms.
Brain fog, anxiety, and other mental health issues can’t wait. At Amen Clinics, we’re here for you. We offer in-clinic brain scanning and appointments, as well as mental telehealth, remote clinical evaluations, and video therapy for adults, children, and couples. Find out more by speaking to a specialist today at 888-288-9834 or visit our contact page here.
Anxiety and brain fog: Symptoms, causes, and treatment
Anxiety brain fog happens when a person feels anxious and has difficulty concentrating or thinking clearly.
Many conditions may cause anxiety and brain fog, including mental health diagnoses and physical illnesses.
It is normal to experience occasional brain fog and anxiety, especially during high stress. However, people who find that anxiety and brain fog regularly interfere with their everyday activities should seek medical attention.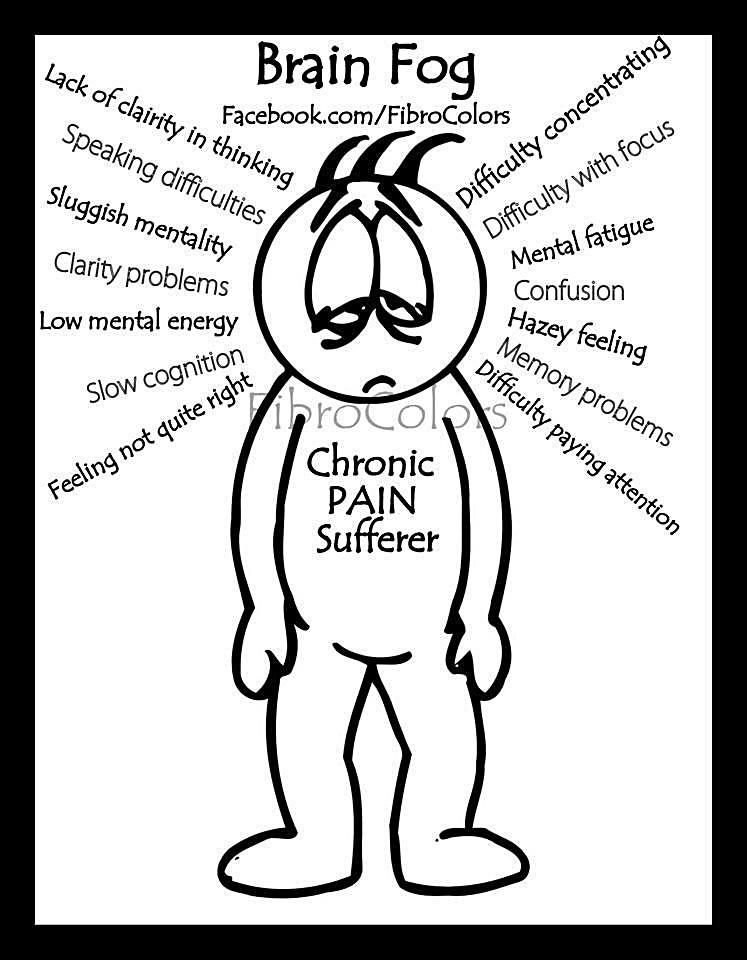
Keep reading to learn more about brain fog, why it occurs alongside anxiety, and some other potential causes.
With brain fog, a person might feel less mentally sharp than usual. They might feel numb, and everyday activities may require more effort. Some people describe it as a foggy haze that makes accessing their thoughts or plans harder.
Some examples of things a person might do because of brain fog include:
- forgetting about a task they had to complete
- taking much longer than usual to complete simple tasks
- feeling frequently distracted
- feeling tired when working
Anxiety takes up mental resources. A person may have to use more energy to focus on something other than their anxiety. They may feel that their anxious thoughts constantly intrude on their thought processes. This can make it more difficult to concentrate and think clearly.
For example, research shows that anxiety notably impacts a person’s working memory and many other mental processes.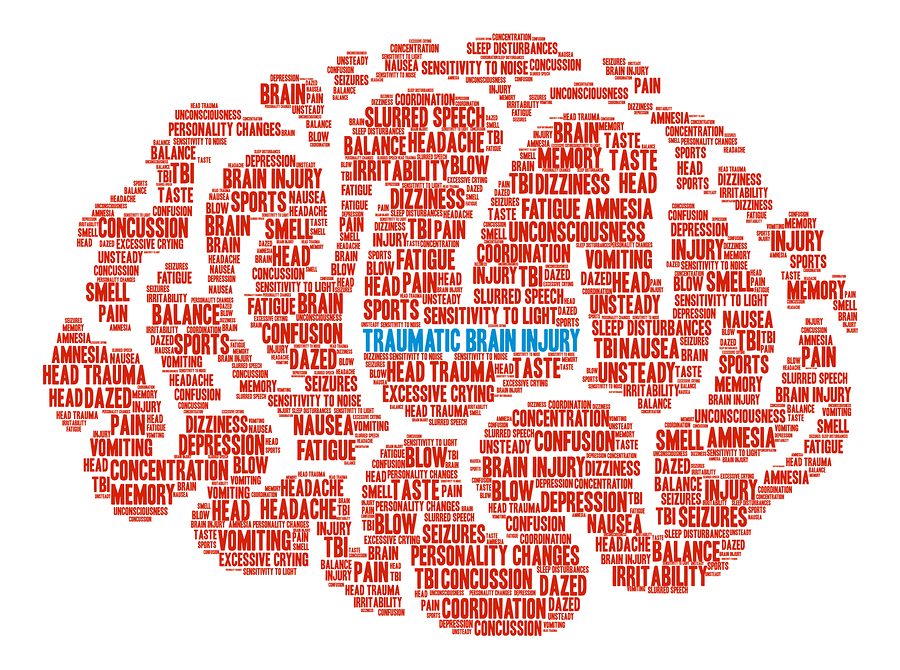
Some mental health conditions that may cause anxiety and brain fog include:
- depression
- anxiety disorders, such as generalized anxiety and post-traumatic stress disorder (PTSD)
- attention deficit hyperactivity disorder (ADHD)
Physical health issues may also cause anxiety and brain fog. For example, people with long COVID-19 may also experience brain fog and PTSD.
Additionally, chronic fatigue syndrome, which can cause a person to feel frequently exhausted, may cause anxiety and brain fog.
Brain fog is a symptom, not a medical diagnosis. It can feel different to different people, and they might not use the same term to refer to various symptoms. Some characteristics of brain fog include:
- feeling “spacy” or confused
- feeling fatigued
- thinking more slowly than usual and needing more time to complete simple tasks
- being easily distracted
- having trouble organizing thoughts or activities
- forgetfulness, such as forgetting daily tasks or losing a train of thought
- having difficulty finding the right word
Since brain fog is a symptom rather than a medical diagnosis, there is no specific treatment for it. However, managing the anxiety, or any condition causing it, may help.
However, managing the anxiety, or any condition causing it, may help.
Some treatment options could include the following:
- medications, including antianxiety medications, antidepressants, or stimulants for ADHD
- psychotherapy to talk about anxiety and develop coping skills
- support groups
- time management systems to help a person remain focused
- adjustments at school or work, such as extra test-taking time
- exercise, deep breathing, and meditation
Getting enough sleep, drinking plenty of water, and remaining nourished may also help reduce the risk of brain fog. This is especially helpful for people with anxiety that distracts them from self-care.
Some people find that specific self-care strategies may also help. These could include following a schedule, using a reminder app, or taking frequent breaks from whatever could be heightening their anxiety.
Learn more about treatments for anxiety here.
Occasional brain fog is normal, especially when a person can identify a clear cause, such as being tired, having a cold, or experiencing family stress.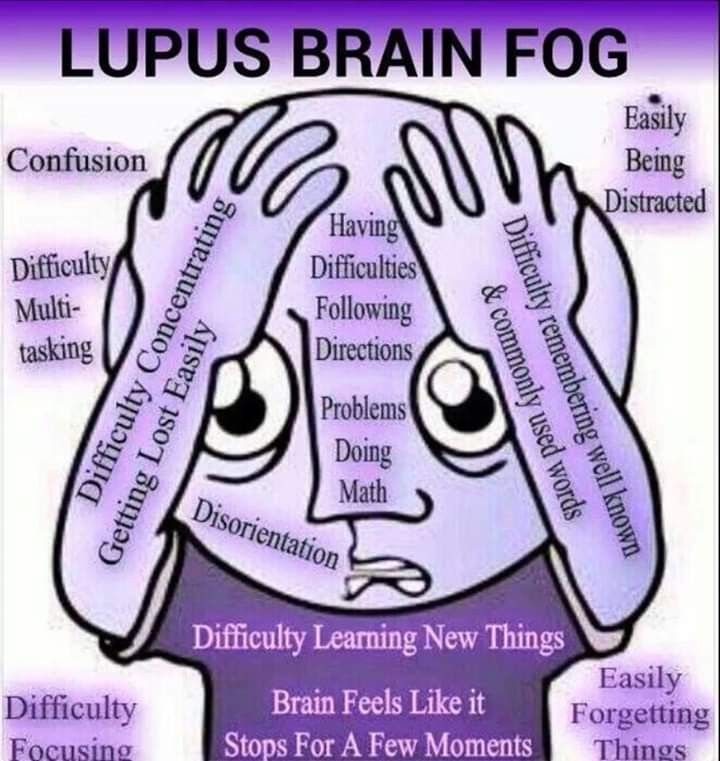
However, people should see a doctor if:
- their brain fog regularly interferes with their ability to complete daily tasks
- they have problems with daily functioning, for example, they forget to pay bills or get lost often
- their memory seems to be getting steadily worse
- self-care interventions do not help with their brain fog
- they experience brain fog much of the time
- their anxiety is very intense and does not get better with home treatments
Numerous medical conditions can cause brain fog. It is important not to ignore this symptom, especially if it does not improve with home treatments.
Some potential reasons a person might develop brain fog include:
- hunger, dehydration, or vitamin deficiencies
- neurological conditions, such as dementia or a head injury
- chronic illnesses, such as lupus
- illegal drugs and alcohol
- certain medications, such as chemotherapy medications and mood stabilizers
Learn more about other causes of brain fog here.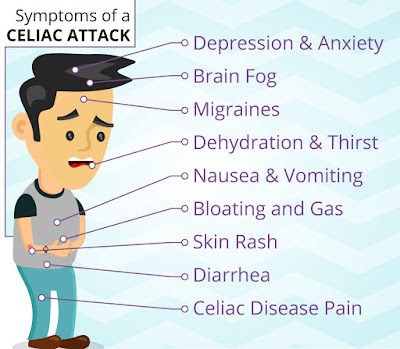
Below are some frequently asked questions relating to brain fog and anxiety.
Does brain fog go away?
The duration of a person’s brain fog will depend on its underlying cause. It can last days to years but typically resolves with treatment of its cause.
What vitamins help with brain fog?
Nutrient deficiencies may worsen brain fog symptoms. Some research suggests that an adequate intake of vitamins B12, C, and D, may help maintain or improve cognitive function.
Is brain fog a mental illness?
Brain fog is not a mental illness. It is a term for a collection of symptoms including memory and concentration difficulties.
Should I go to a neurologist for brain fog?
Brain fog is often a sign of an underlying condition. If brain fog persists for several weeks, a person should contact a neurologist for assessment. Identifying the cause of brain fog enables doctors to treat the condition accordingly.
Both anxiety and brain fog can severely disrupt a person’s daily life.
Brain fog may make completing simple tasks more difficult. This may worsen anxiety due to missed deadlines and conflicts with work or loved ones.
The right treatment can help the anxiety and thus, the brain fog it causes.
A doctor may also recommend self-care strategies. People concerned about their anxiety or brain fog should not delay seeking help, especially if the symptoms are severe.
“Unclear head” syndrome, its complex diagnostics and treatment
“Unclear head” is one of the main signs of astheno-neurotic syndrome
If "Unclear head", "Muddy head" - the feeling with which you get up and lie down, and if increased irritability, fatigue and poor sleep are added to this - most likely, we are talking about astheno-neurotic syndrome .
Main symptoms: A lot of people complain about "fog in the head", "head like cotton wool", "unclear head" and similar symptoms.
If you notice overwork, sleep disturbance, constant irritability, then you may have a mental disorder called astheno-neurotic syndrome.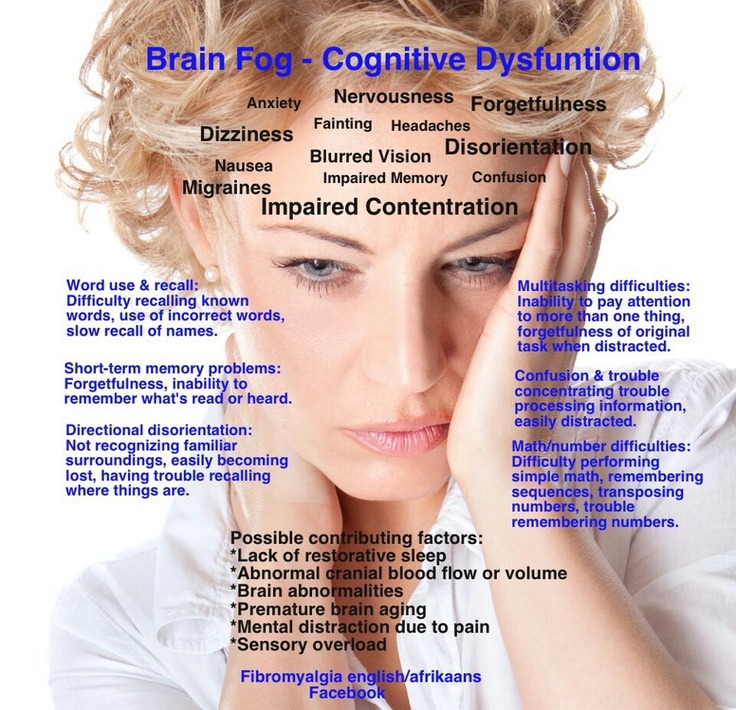
Prevalence: This disease is one of the most common "diseases of civilization". It is often referred to as the "management flu".
The disease affects people who are educated and prosperous. The most characteristic age is from 20 to 40 years. These are entrepreneurs, managers, doctors, teachers. In a special risk group are people whose work is associated with increased responsibility, for example, air traffic controllers.
In the past, astheno-neurotic syndrome was called "nervous exhaustion"
Also at risk are creative individuals.
Causes of occurrence: The main causes of occurrence are stress, prolonged nervous excitement, chronic lack of sleep, constant overwork. Also, factors contributing to the emergence of astheno-neurotic syndrome are past diseases, including colds, some viruses, poisoning, and poor environmental conditions.
Similar symptomatology: What diseases can be manifested as "head as if in a fog", poor sleep, weakness and irritability, except for neurasthenia? First of all, these are asthenic conditions with incipient serious illnesses.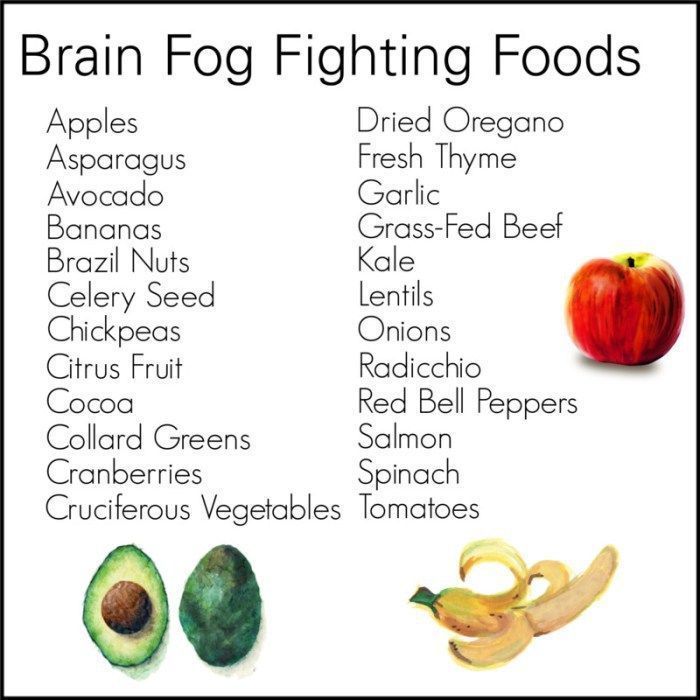 In the second - masked depression, which at the beginning can easily be confused with astheno-neurotic syndrome. And chronic fatigue syndrome can manifest itself in a similar way.
In the second - masked depression, which at the beginning can easily be confused with astheno-neurotic syndrome. And chronic fatigue syndrome can manifest itself in a similar way.
So the correct diagnosis can only be made by a psychotherapist or psychiatrist. To make a diagnosis, professional psychological diagnostics (psychotests) are usually used, which you can go through on your own (following this link).
How the disease develops: The syndrome occurs gradually, with a combination of emotional and physical overstrain, constant fatigue. Most often, patients complain of a breakdown, general weakness, increased irritability, "fog" in the head, inability to cope with the usual amount of work.
If a person continues to be stressed further and does not seek medical help, his condition worsens - tearfulness, complaints about the heart, fog in the head join the usual set of complaints about a "cotton" head. Irritability increases to an extreme degree, but irritation is quickly replaced by weakness. Sleep is usually unstable, does not bring a feeling of rest, after sleep the head is “like cotton wool”. Appetite worsens, constipation or diarrhea may disturb. Sexual desire decreases in both men and women. The condition worsens before a change in the weather (the so-called "weather sensitivity"). In the absence of treatment at this stage, apathy, lethargy, severe weakness and a persistent decrease in mood follow. Interest in life is reduced, the patient thinks only about his painful condition, about his "obscure" head.
Sleep is usually unstable, does not bring a feeling of rest, after sleep the head is “like cotton wool”. Appetite worsens, constipation or diarrhea may disturb. Sexual desire decreases in both men and women. The condition worsens before a change in the weather (the so-called "weather sensitivity"). In the absence of treatment at this stage, apathy, lethargy, severe weakness and a persistent decrease in mood follow. Interest in life is reduced, the patient thinks only about his painful condition, about his "obscure" head.
Left untreated, psychotic disorders can develop.
Treatment: Treatment prospects are positive, usually psychotherapeutic methods give excellent results up to a complete cure. In severe cases, a combination of psychotherapy with psychopharmacotherapy is used.
Self-medication usually worsens the condition and leads to the progression of the disease.
At the initial stage of the disease, a psychotherapist, in order to make a correct diagnosis, needs to exclude all diseases in which similar symptoms appear, because the more accurate the diagnosis, the more successful the treatment will be.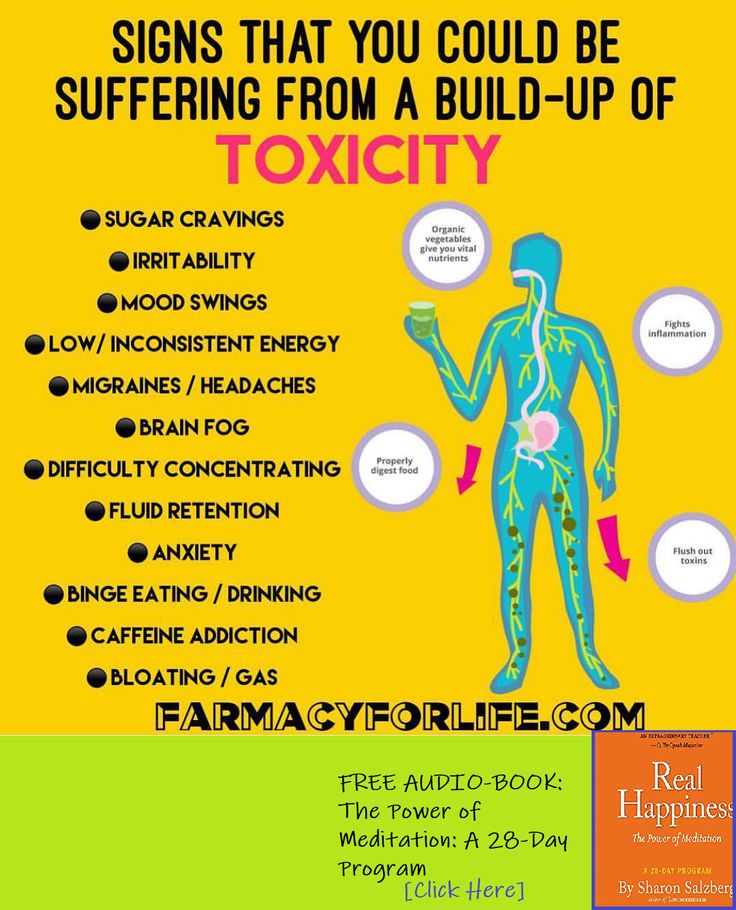
Different diseases with similar symptoms need to be treated differently. Therefore, it is necessary to consult a psychotherapist. A good psychotherapist selects therapy that is appropriate for the specific manifestations of the disease and the individual characteristics of each patient.
Astheno-neurotic syndrome is one of the most common "diseases of civilization". It is often referred to as the "management flu".
The treatment of the syndrome depends on the severity of the painful symptoms, but is primarily aimed at eliminating psychotraumatic factors. It is necessary to reduce both mental and physical stress. This is the most important condition for treatment, without such measures it will not be possible to defeat the disease. In the early stages of the development of the disease, normalization of the rhythm of life, elimination of stress and psychotherapy may be enough to significantly improve the state of health. And, of course, at this stage, psychotherapy methods that do not use drugs give a very good effect - cognitive-behavioral, psychoanalysis, group psychotherapy methods are very effective.
In any case, you need to contact a psychotherapist.
In more advanced cases, additional psychopharmacotherapy may be required. General tonic drugs, tranquilizers, if necessary, sleeping pills and antidepressants are used. Psychotherapy is also actively used in the treatment of advanced astheno-neurotic syndrome.
The first indicator of improvement is the normalization of sleep and the disappearance of the feeling of "fog" in the head. With timely prescribed treatment, the problem can usually be completely overcome, however, if the tense situation and stress at work and in personal life continue to persist, various complications are possible.
Terminology and other names: In the past, astheno-neurotic syndrome, together with diseases of similar symptoms, was called "nervous exhaustion".
In modern psychiatry, the term "neurasthenia" is more often used to refer to neuro-asthenic syndrome (synonyms). In the everyday sense, neurasthenia is usually perceived as a painfully nervous, unbalanced state, characteristic of weak-willed people, easily amenable to various influences and moods, in a state of acute mental crisis.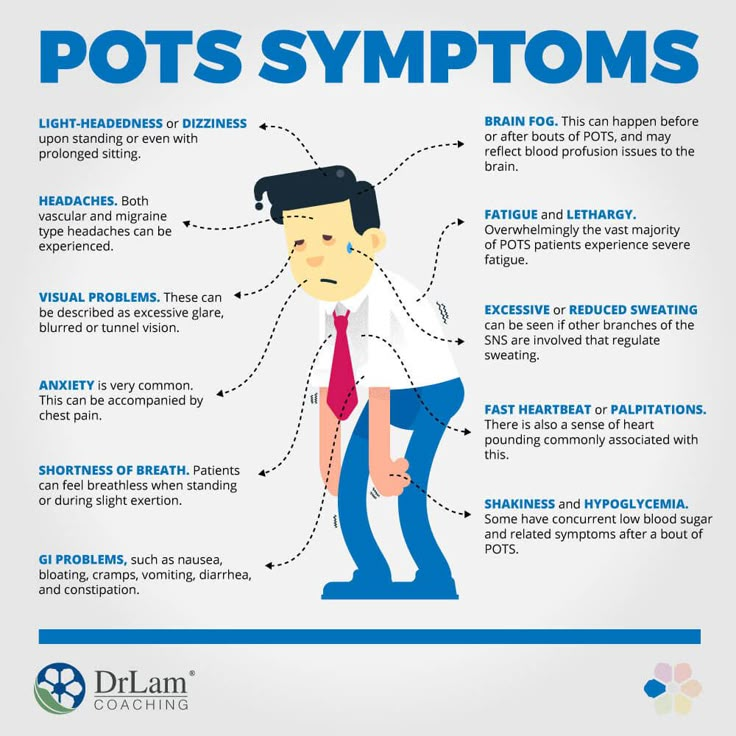 And in the medical sense, this is a state of depression, irritability, "a vague head."
And in the medical sense, this is a state of depression, irritability, "a vague head."
Psychogenic dizziness - City Hospital No. 40
Sestroretsk, st. Borisova, 9
Online appointment Search Accessible environment
At present, such “classic” functional disorders of the nervous system as hysterical paralysis and blindness have practically disappeared. In their place came, mainly, somatoform disorders, including those manifested by dizziness, with a tendency to a protracted course. Statistics of calls to the clinic of nervous diseases of the Military Medical Academy. CM. Kirov of patients with complaints of dizziness shows that psychogenic dizziness ranks third among other clinical forms. At the same time, it can develop within the framework of a depressive or neurotic state, schizophrenia, panic attack, phobia, hysteria, somatoform dysfunction of the autonomic nervous system, etc.
Despite the fact that psychogenic dizziness should always remain a diagnosis of exclusion, it is important to diagnose this condition in a timely manner, explain to the patient the reasons for his complaints, and prescribe adequate treatment. Below we will consider one of the most common variants of psychogenic dizziness encountered in clinical practice - phobic postural dizziness.
Phobic postural vertigo
“Phobic postural vertigo” (PPG) is a clinical syndrome that includes, firstly, dizziness, described by patients as “fog in the head”, unsteadiness, a feeling of intoxication, which are usually associated with special conditions (downstairs, walking along a busy street, at night) or situations that are perceived by the patient as provoking factors (being in the subway, a public place, driving a car), secondly, anxiety and autonomic reactions (nausea, vomiting , lability of pulse and blood pressure) and, thirdly, avoidance behavior in relation to these situations in the absence of objective clinical signs of organic neurological disorders.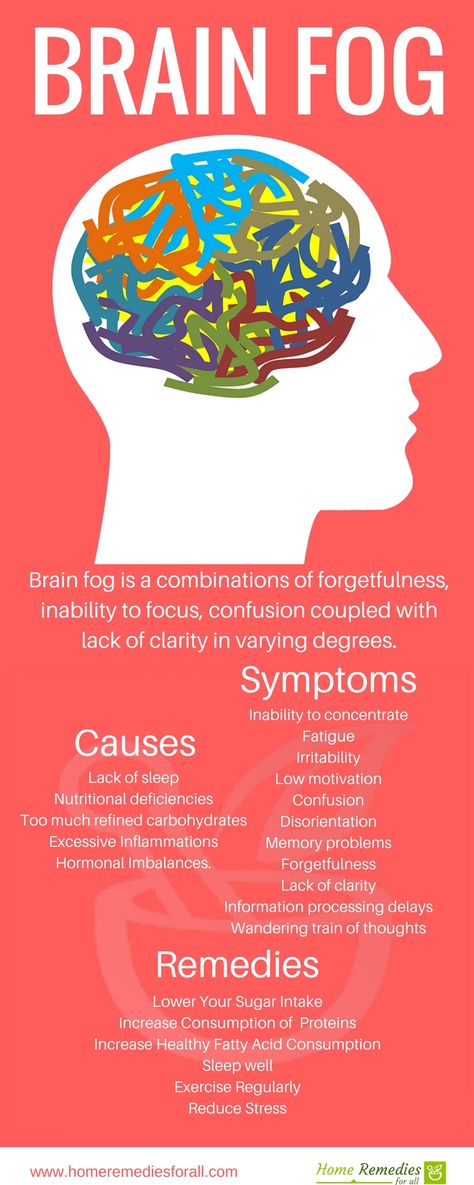
PPH is typical of obsessive-compulsive individuals and usually develops after significant irritation of the vestibular apparatus (especially in benign paroxysmal positional vertigo, vestibular neuronitis) or stress.
Clinic
PPH is characterized by attacks of imbalance, fear that occur without episodes of real falls (falls are possible that precede the formation of secondary PPH), but with the formation of avoidant behavior.
The severity of symptoms improves with distraction of the patient, as well as after taking small doses of alcohol, in some patients during sports. The quality of life of patients with PPH significantly decreases with the generalization of vegetative-somatic symptoms and the increase in the patient's social maladaptation. In the premorbid character structure, predominantly obsessive traits and perfectionism are revealed, predisposing to the formation of stable obsessive-compulsive disorders and psychogenic depressions.
The manifestations of PPH largely correspond to the structure of panic disorder, including periodic anxiety attacks, an obsessive fear of a recurrence of an attack accompanied by dizziness, and avoidance behavior. However, it should be borne in mind that the fear of repeated dizziness with avoidant behavior can also be observed in patients with vestibular dysfunctions, which makes it possible to distinguish between primary and secondary panic disorder that develops on the basis of otological pathology.
Diagnostics. For differential diagnosis, it is important to conduct a comprehensive examination of such patients (brain MRI, consultation with a neurologist, ENT doctor), exclude possible concomitant somatic pathology (endocrine disorders, anemic syndrome, arrhythmias, etc.), convince the patient of the benign nature of his disease. After all, sometimes such patients find themselves without the help of specialists: otorhinolaryngologists exclude their pathology, therapists and neurologists also do not find any significant deviations, which fixes the patient even more on his own experiences, forming a feeling that he has a “rare, incomprehensible” disease with a dubious prognosis for recovery. Criteria for the diagnosis of PPG are given in the table.
Criteria for the diagnosis of PPG are given in the table.
Treatment
Treatment of patients with PPH should be based on a combination of medicinal and non-drug (psychotherapy, vestibular and respiratory gymnastics) methods of treatment. First-line drugs are antidepressants (selective serotonin reuptake inhibitors - paroxetine, venlafaxine - and tricyclic antidepressants - amitriptyline). Benzodiazepines (phenazepam, diazepam, alprazolam, etc.) are also used. In some cases, a positive effect in the treatment of anxiety disorders is achieved with the use of "small" antipsychotics (sulpiride, tiapride, thioridazine). As an additional therapy, the drug betahistine is used, which reduces the excitability of the vestibular apparatus and is effective for all types of dizziness, including psychogenic. Mandatory is the treatment of underlying somatic and neurological pathology, which leads to a deterioration in postural and vestibular functions (for example, treatment of diabetes mellitus, vitamin B12 deficiency, hypo- or hyperthyroidism).