What is ekg in medical terms
Holter monitor - Mayo Clinic
Overview
Holter monitor
Holter monitor
A Holter monitor uses electrodes and a recording device to track the heart's rhythm for 24 to 72 hours. A health care provider can print an electrocardiogram strip using the data on the recording device to see the heart's rhythm during the period the monitor was worn.
A Holter monitor is a small, wearable device that records the heart's rhythm. It's used to detect or determine the risk of irregular heartbeats (arrhythmias).
A Holter monitor test may be done if a traditional electrocardiogram (ECG or EKG) doesn't provide enough details about the heart's condition. If the irregular heartbeats are infrequent, a longer term monitor called an event recorder may be needed.
Some personal devices, such as smartwatches, offer electrocardiogram monitoring. Ask your health care provider if this is an option for you.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
A health care provider may recommend a Holter monitor if you have:
- Signs and symptoms of an irregular heart rhythm (arrhythmia)
- Unexplained fainting
- A heart condition that increases the risk of arrhythmias
Before you get a Holter monitor, you'll have an electrocardiogram (ECG or EKG). An ECG is a quick and painless test that uses sensors (electrodes) taped to the chest to check the heart's rhythm.
If you have infrequent arrhythmias, an ECG may not detect them. A Holter monitor may be able to spot irregular heart rhythms that an ECG missed.
If standard Holter monitoring doesn't capture an irregular heartbeat, a device called an event monitor may be recommended to record heartbeats over several weeks.
More Information
- Atrial fibrillation
- Atrial flutter
- Bradycardia
- Ebstein anomaly
- Heart arrhythmia
- Heart disease
- Hypertrophic cardiomyopathy
- Long QT syndrome
- Mitral valve regurgitation
- Mitral valve stenosis
- Myocardial ischemia
- Myocarditis
- Premature ventricular contractions (PVCs)
- Sick sinus syndrome
- Tachycardia
- Ventricular fibrillation
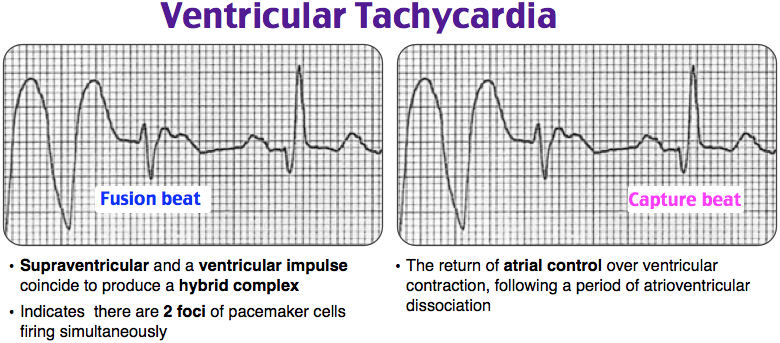
- Ventricular tachycardia
- Wolff-Parkinson-White (WPW) syndrome
Request an Appointment at Mayo Clinic
Risks
There are no significant risks involved in wearing a Holter monitor.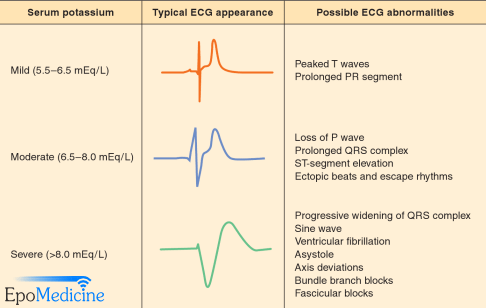 Some people have minor discomfort or skin irritation where the sensors (electrodes) were placed.
Some people have minor discomfort or skin irritation where the sensors (electrodes) were placed.
Holter monitors aren't usually affected by other electrical appliances. But some devices may interrupt the signal from the electrodes to the Holter monitor. If you have a Holter monitor, you should avoid the following:
- Electric blankets
- Electric razors and toothbrushes
- Magnets
- Metal detectors
- Microwave ovens
Also, keep cellphones and portable music players at least 6 inches from the Holter monitor for the same reason.
How you prepare
A Holter monitor is placed at a care provider's office during a scheduled appointment. Unless your health care provider tells you otherwise, plan to bathe before this appointment. Most monitors can't be removed and must be kept dry once monitoring begins.
A care provider will place sensors (electrodes) on your chest. These electrodes detect the heartbeat. They're about the size of a silver dollar.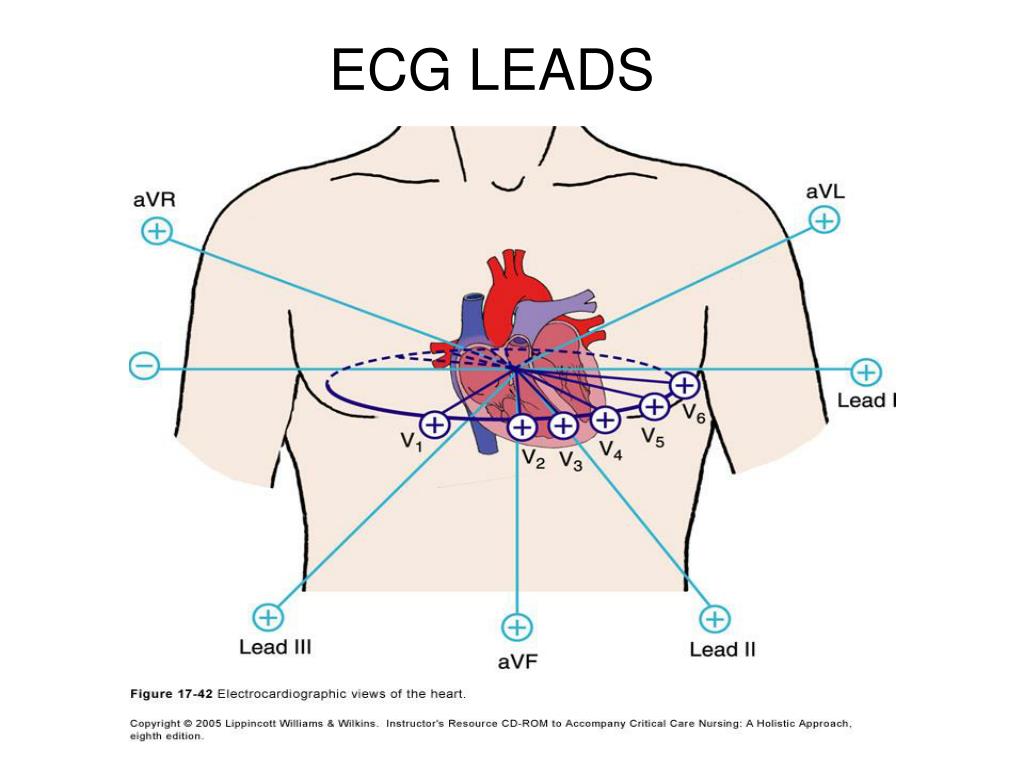 If you have hair on your chest, some of it may be shaved to make sure the electrodes stick.
If you have hair on your chest, some of it may be shaved to make sure the electrodes stick.
Wires attached to the electrodes connect to the Holter monitor recording device. The device is about the size of a deck of cards.
Once your Holter monitor is fitted and you've received instructions on how to wear it, you can leave your provider's office and return to everyday activities.
What you can expect
During
A Holter monitor is typically worn for 1 to 2 days. During that time, the device records all of the heartbeats.
Holter monitoring is painless and noninvasive. The sensors (electrodes) and wires can be hidden under clothing. The device is worn on a belt or attached to a strap.
Don't take the Holter monitor off — it must be worn during the entire recording period, even while sleeping.
Water can damage a Holter monitor. Don't swim, shower or bathe for the entire time you're wearing a Holter monitor. If you have a wireless Holter monitor, you'll be shown how to disconnect and reconnect the sensors and the monitor so that you can shower or bathe.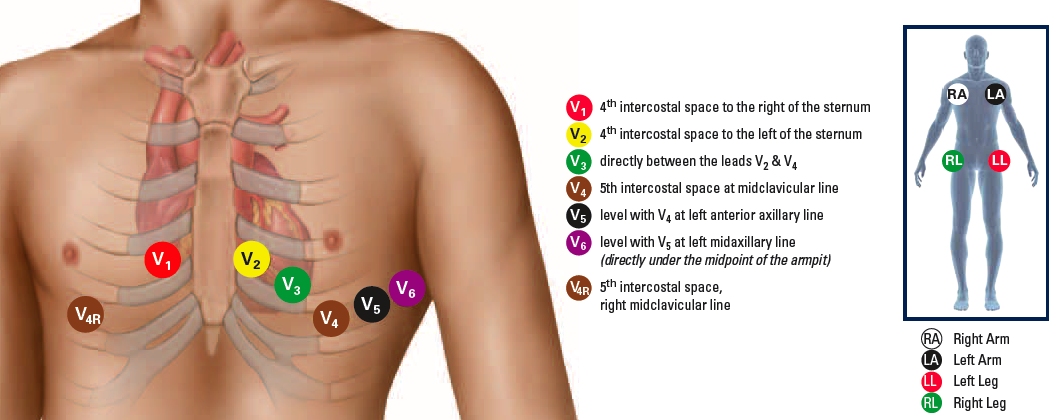
While you wear a Holter monitor, you can do most other daily activities unless your provider tells you otherwise. You may be given a form to record your activities and any symptoms. It's particularly important to note if and when you have any of the following symptoms:
- Pounding, fluttering or skipped heartbeats
- Shortness of breath
- Chest pain
- Lightheadedness
Write down what activities you do and exactly what time you do them.
After
Once your monitoring period is over, you'll return the device to your health care provider's office. If you were asked to keep a record of symptoms that you had while wearing the device, your provider can compare the Holter monitor's data with your notes. This can help your provider make an accurate diagnosis.
Results
Your care provider will review the Holter monitor test results and discuss them with you. Information from Holter monitor testing can tell your provider if you have a heart condition and if any heart medicines you currently take are or aren't working.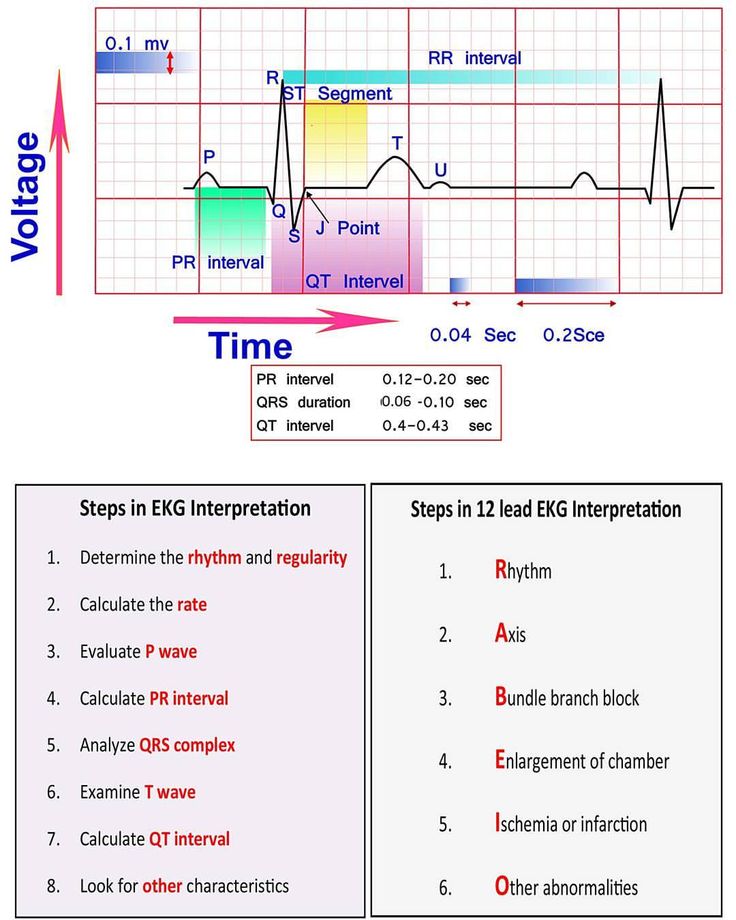
If you didn't have any irregular heart rhythms while you wore the monitor, your provider may recommend a wireless Holter monitor or an event recorder, both of which can be worn longer than a standard Holter monitor. Event recorders are similar to Holter monitors and generally require you to push a button when you feel symptoms. There are several different types of event recorders.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
News from Mayo Clinic
Products & Services
definition of EKG by Medical dictionary
electrocardiogram
(ECG, EKG) [e-lek″tro-kahr´de-o-gram″]the record produced by electrocardiography; a tracing representing the heart's electrical action derived by amplification of the minutely small electrical impulses normally generated by the heart.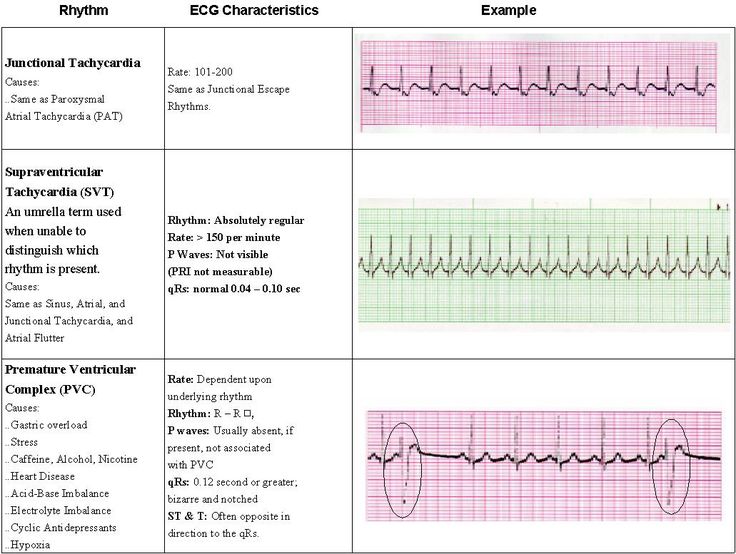
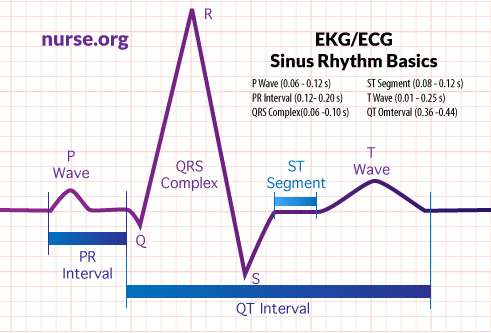
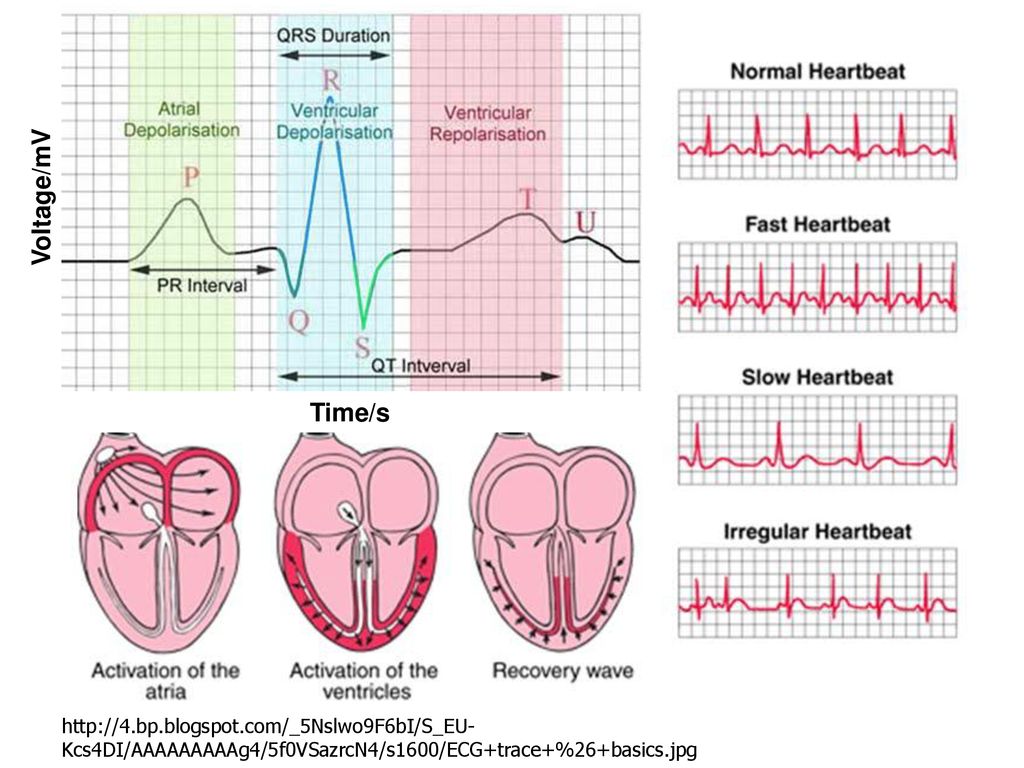
Normal electrocardiogram. Heart action during P-R interval: (1) Atrial contraction begins at peak of P wave. (2) P-R interval—atrial contraction. (3) Ventricles relaxed. Heart action during QRS complex: (1) Ventricular contraction begins at peak of R. (2) A-V (mitral and tricuspid) valves close, causing S1 sound. (3) Ventricles contract. (4) Atrial relaxation begins. Heart action during S-T segment: (1) Semilunar valves open (aortic and pulmonic). (2) Ejection of blood from ventricles–systole. Heart action during T wave: (1) Slowing of ejection from ventricles. (2) Closure of semilunar valves (aortic and pulmonic) causing S2 sound. Heart action during T-P interval: (1) Relaxation of ventricles. (2) A-V valves open. (3) Filling of ventricles, causing S3 sound.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.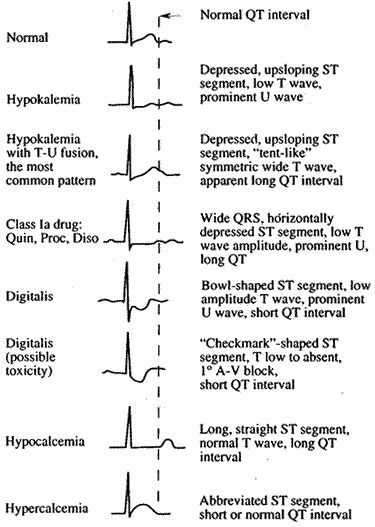
EKG
Abbreviation for electrocardiogram.
Farlex Partner Medical Dictionary © Farlex 2012
EKG
(ē-kā-jē′)n.
1. An electrocardiogram.
2. An electrocardiograph.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
EKG
Electrocardiogram, see there.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
EKG
Abbreviation for electrocardiogram, but more correctly ECG.
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
EKG
Electrocardiogram, used to study and record the electrical activity of the heart.
Mentioned in: Angioplasty, Lithotripsy
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
Electrocardiogram
Synonym/acronym: ECG, EKG.
Common use
To evaluate the electrical impulses generated by the heart during the cardiac cycle to assist with diagnosis of cardiac arrhythmias, blocks, damage, infection, or enlargement.
Area of application
Heart.
Contrast
None.
Description
The cardiac muscle consists of three layers of cells: the inner layer called the endocardium, the middle layer called the myocardium, and the outer layer called the epicardium. The systolic phase of the cardiac cycle reflects the contraction of the myocardium, whereas the diastolic phase takes place when the heart relaxes to allow blood to rush in. All muscle cells have a characteristic rate of contraction called depolarization. Therefore, the heart will maintain a predetermined heart rate unless other stimuli are received.
The monitoring of pulse and blood pressure evaluates only the mechanical activity of the heart.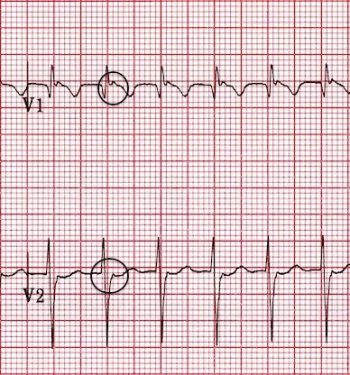 The electrocardiogram (ECG), a noninvasive study, measures the electrical currents or impulses that the heart generates during a cardiac cycle (see figure of a normal ECG at end of monograph). Electrical impulses travel through a conduction system beginning with the sinoatrial (SA) node and moving to the atrioventricular (AV) node via internodal pathways. From the AV node, the impulses travel to the bundle of His and onward to the right and left bundle branches. These bundles are located within the right and left ventricles. The impulses continue to the cardiac muscle cells by terminal fibers called Purkinje fibers. The ECG is a graphic display of the electrical activity of the heart, which is analyzed by time intervals and segments. Continuous tracing of the cardiac cycle activity is captured as heart cells are electrically stimulated, causing depolarization and movement of the activity through the cells of the myocardium.
The electrocardiogram (ECG), a noninvasive study, measures the electrical currents or impulses that the heart generates during a cardiac cycle (see figure of a normal ECG at end of monograph). Electrical impulses travel through a conduction system beginning with the sinoatrial (SA) node and moving to the atrioventricular (AV) node via internodal pathways. From the AV node, the impulses travel to the bundle of His and onward to the right and left bundle branches. These bundles are located within the right and left ventricles. The impulses continue to the cardiac muscle cells by terminal fibers called Purkinje fibers. The ECG is a graphic display of the electrical activity of the heart, which is analyzed by time intervals and segments. Continuous tracing of the cardiac cycle activity is captured as heart cells are electrically stimulated, causing depolarization and movement of the activity through the cells of the myocardium.
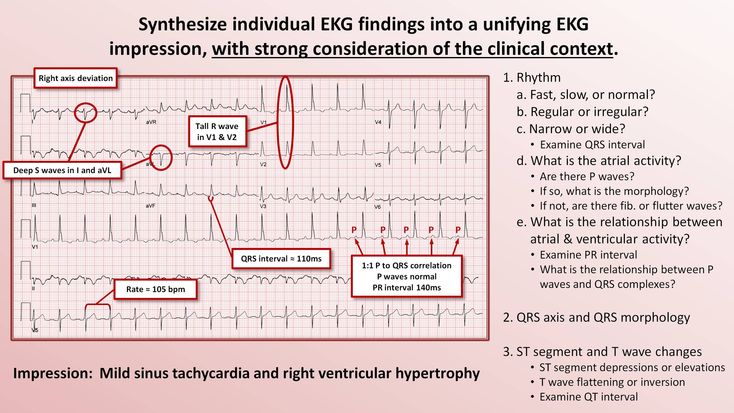
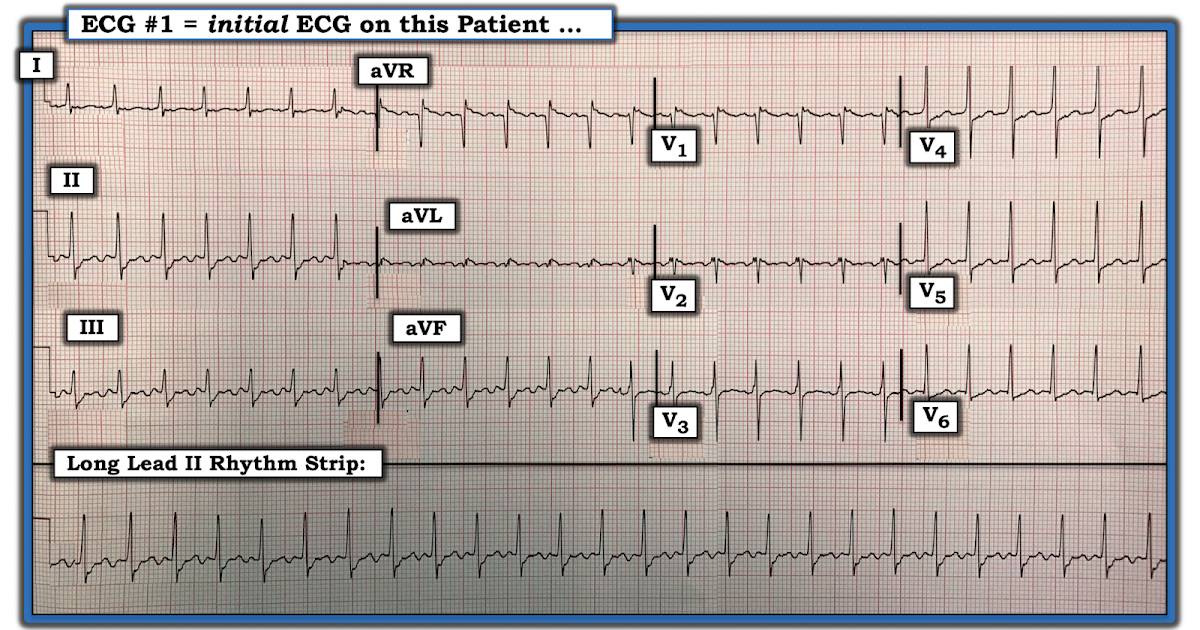
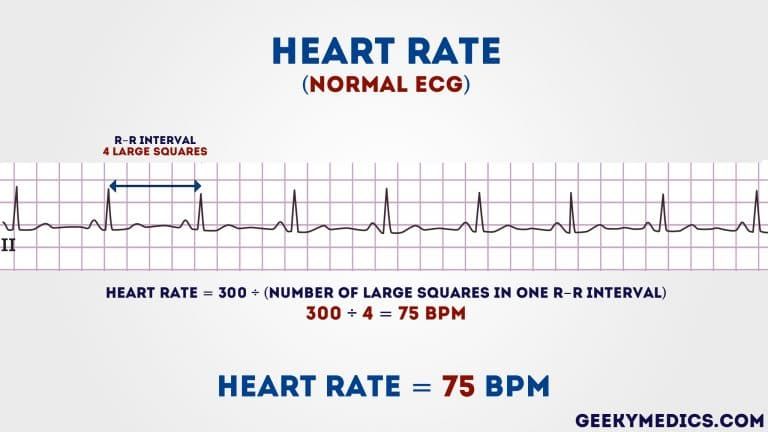
The ECG study is completed by using 12, 15, or 18 electrodes attached to the skin surface to obtain the total electrical activity of the heart.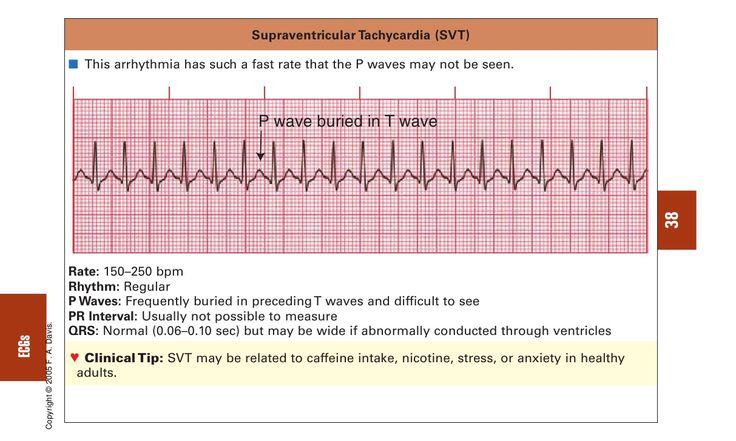 Each lead records the electrical potential between the limbs or between the heart and limbs. The ECG machine records and marks the 12 leads (most common system used) on the strip of paper in the machine in proper sequence, usually 6 in. of the strip for each lead. The ECG pattern, called a
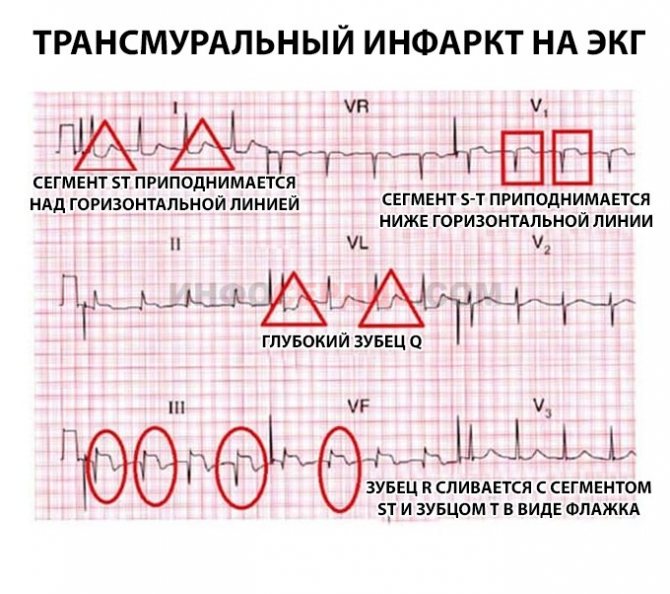
heart rhythm, is recorded by a machine as a series of waves, intervals, and segments, each of which pertains to a specific occurrence during the contraction of the heart. The ECG tracings are recorded on graph paper using vertical and horizontal lines for analysis and calculations of time, measured by the vertical lines (1 mm apart and 0.04 sec per line), and of voltage, measured by the horizontal lines (1 mm apart and 0.5 mV per 5 squares). A pulse rate can be calculated from the ECG strip to obtain the beats per minute. The P wave represents the depolarization of the atrial myocardium; the QRS complex represents the depolarization of the ventricular myocardium; the P-R interval represents the time from beginning of the excitation of the atrium to the beginning of the ventricular excitation; and the ST segment has no deflection from baseline, but in an abnormal state may be elevated or depressed.
Each lead records the electrical potential between the limbs or between the heart and limbs. The ECG machine records and marks the 12 leads (most common system used) on the strip of paper in the machine in proper sequence, usually 6 in. of the strip for each lead. The ECG pattern, called a
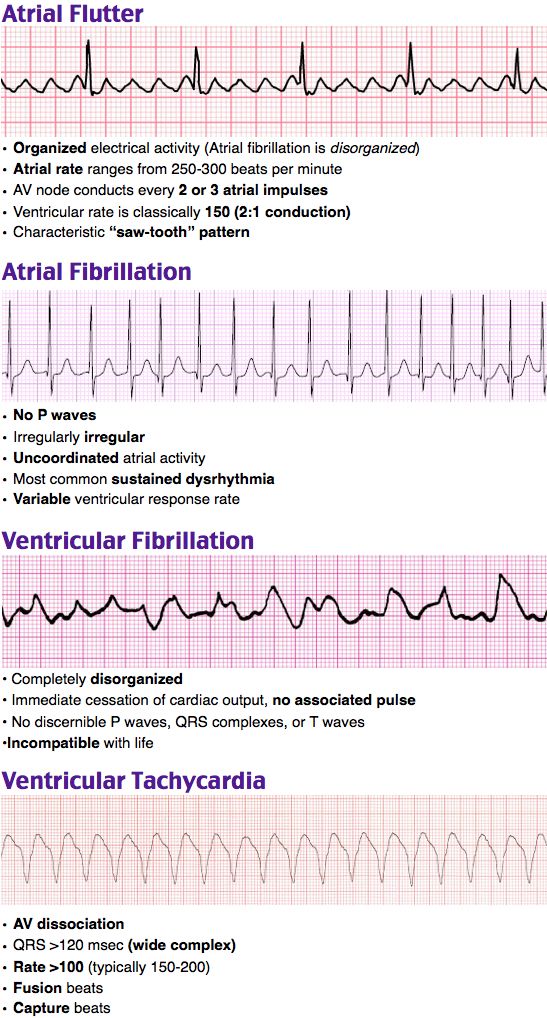
heart rhythm, is recorded by a machine as a series of waves, intervals, and segments, each of which pertains to a specific occurrence during the contraction of the heart. The ECG tracings are recorded on graph paper using vertical and horizontal lines for analysis and calculations of time, measured by the vertical lines (1 mm apart and 0.04 sec per line), and of voltage, measured by the horizontal lines (1 mm apart and 0.5 mV per 5 squares). A pulse rate can be calculated from the ECG strip to obtain the beats per minute. The P wave represents the depolarization of the atrial myocardium; the QRS complex represents the depolarization of the ventricular myocardium; the P-R interval represents the time from beginning of the excitation of the atrium to the beginning of the ventricular excitation; and the ST segment has no deflection from baseline, but in an abnormal state may be elevated or depressed.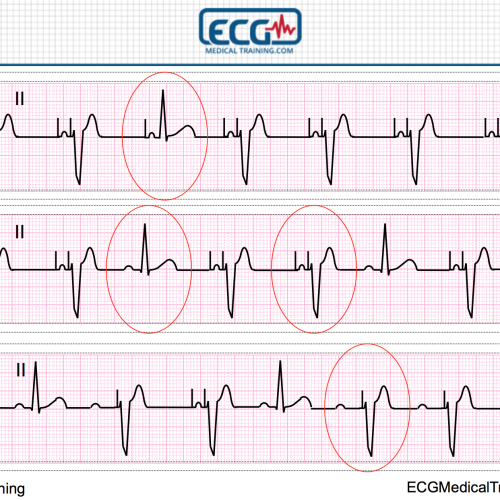 An abnormal rhythm is called an arrhythmia
An abnormal rhythm is called an arrhythmia
The ankle-brachial index (ABI) can also be assessed during this study. This noninvasive, simple comparison of blood pressure measurements in the arms and legs can be used to detect peripheral artery disease (PAD). A Doppler stethoscope is used to obtain the systolic pressure in either the dorsalis pedis or the posterior tibial artery. This ankle pressure is then divided by the highest brachial systolic pressure acquired after taking the blood pressure in both arms of the patient. This index should be greater than 1. When the index falls below 0.5, blood flow impairment is considered significant. Patients should be scheduled for a vascular consult for an abnormal ABI. Patients with diabetes or kidney disease, as well as some elderly patients, may have a falsely elevated ABI due to calcifications of the vessels in the ankle causing an increased systolic pressure. The ABI test approaches 95% accuracy in detecting PAD. However, a normal ABI value does not absolutely rule out the possibility of PAD for some individuals, and additional tests should be done to evaluate symptoms.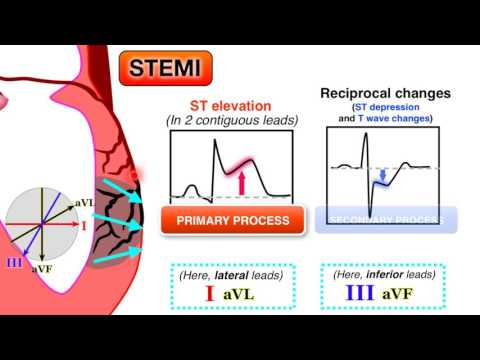
This procedure is contraindicated for
- N/A
Indications
- Assess the extent of congenital heart disease
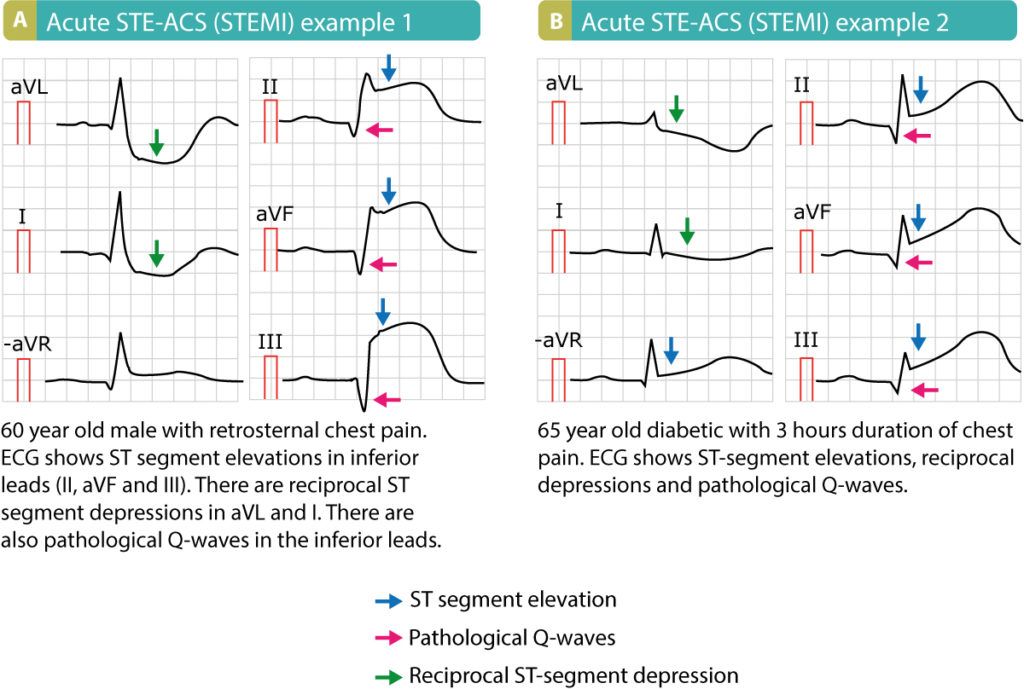
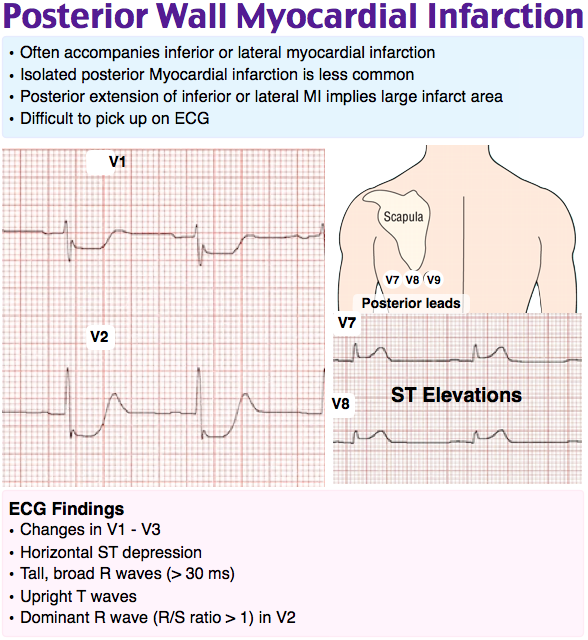
- Assess the extent of myocardial infarction (MI) or ischemia, as indicated by abnormal ST segment, interval times, and amplitudes
- Assess the function of heart valves
- Assess global cardiac function
- Detect arrhythmias, as evidenced by abnormal wave deflections
- Detect peripheral artery disease (PAD)
- Detect pericarditis, shown by ST segment changes or shortened P-R interval
- Determine electrolyte imbalances, as evidenced by short or prolonged Q-T interval
- Determine hypertrophy of the chamber of the heart or heart hypertrophy, as evidenced by P or R wave deflections
- Evaluate and monitor cardiac pacemaker function
- Evaluate and monitor the effect of drugs, such as digitalis, antiarrhythmics, or vasodilating agents
- Monitor ECG changes during an exercise test
- Monitor rhythm changes during the recovery phase after an MI
Potential diagnosis
Normal findings
- Normal heart rate according to age: range of 60 to 100 beats/min in adults
- Normal, regular rhythm and wave deflections with normal measurement of ranges of cycle components and height, depth, and duration of complexes as follows:
- P wave: 0.
 12 sec or three small blocks with amplitude of 2.5 mm
12 sec or three small blocks with amplitude of 2.5 mm - Q wave: less than 0.04 mm
- R wave: 5 to 27 mm amplitude, depending on lead
- T wave: 1 to 13 mm amplitude, depending on lead
- QRS complex: 0.1 sec or two and a half small blocks
- ST segment: 1 mm
Abnormal findings related to
- Arrhythmias
- Atrial or ventricular hypertrophy
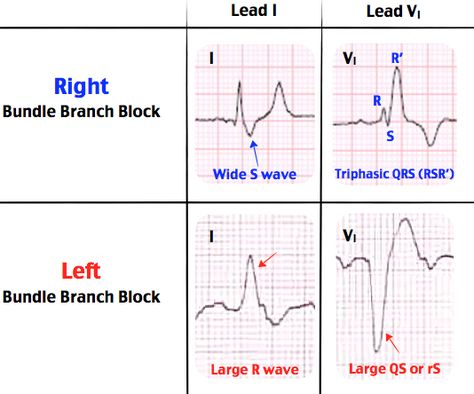
- Bundle branch block
- Electrolyte imbalances
- Heart rate of 40 to 60 beats/min in adults
- MI or ischemia
- PAD
- Pericarditis
- Pulmonary infarction
- P wave: An enlarged P wave deflection could indicate atrial enlargement; an absent or altered P wave could suggest that the electrical impulse did not come from the SA node
- P-R interval: An increased interval could imply a conduction delay in the AV node
- QRS complex: An enlarged Q wave may indicate an old infarction; an enlarged deflection could indicate ventricular hypertrophy; increased time duration may indicate a bundle branch block
- ST segment: A depressed ST segment indicates myocardial ischemia; an elevated ST segment may indicate an acute MI or pericarditis; a prolonged ST segment (or prolonged QT) may indicate hypocalcemia.
 A shortened ST segment may indicate hypokalemia
A shortened ST segment may indicate hypokalemia - Tachycardia greater than 120 beats/min
- T wave: A flat or inverted T wave may indicate myocardial ischemia, infarction, or hypokalemia; a tall, peaked T wave with a shortened QT interval may indicate hyperkalemia
Critical findings
- Acute changes in ST elevation are usually associated with acute MI or pericarditis.
- Asystole
- Heart block, second- and third-degree with bradycardia less than 60 beats/min
- Pulseless electrical activity
- Pulseless ventricular tachycardia
- Premature ventricular contractions (PVCs) greater than three in a row, pauses greater than 3 sec, or identified blocks
- Unstable tachycardia
- Ventricular fibrillation
- Asystole
- Bradycardia less than 60 beats/min
- Pulseless electrical activity
- Pulseless ventricular tachycardia
- Supraventricular tachycardia
- Ventricular fibrillation
It is essential that a critical finding be communicated immediately to the requesting health-care provider (HCP).
 A listing of these findings varies among facilities.
A listing of these findings varies among facilities.Timely notification of a critical finding for lab or diagnostic studies is a role expectation of the professional nurse. Notification processes will vary among facilities. Upon receipt of the critical value the information should be read back to the caller to verify accuracy. Most policies require immediate notification of the primary HCP, Hospitalist, or on-call HCP. Reported information includes the patient’s name, unique identifiers, critical value, name of the person giving the report, and name of the person receiving the report. Documentation of notification should be made in the medical record with the name of the HCP notified, time and date of notification, and any orders received. Any delay in a timely report of a critical finding may require completion of a notification form with review by Risk Management.
Adult
Pediatric
Interfering factors
Nursing Implications and Procedure
Pretest
- Positively identify the patient using at least two unique identifiers before providing care, treatment, or services.
.jpg)
- Patient Teaching: Inform the patient this procedure can assist in assessing cardiac (heart) function.
- Obtain a history of the patient’s complaints or clinical symptoms, including a list of known allergens, especially allergies or sensitivities to latex, anesthetics, or sedatives. Ask if the patient has had a heart transplant, implanted pacemaker, or internal cardiac defibrillator.
- Obtain a history of the patient’s cardiovascular system, symptoms, and results of previously performed laboratory tests and diagnostic and surgical procedures.
- Obtain a list of the patient’s current medications, including herbs, nutritional supplements, and nutraceuticals (see Effects of Natural Products on Laboratory Values online at DavisPlus).
- Review the procedure with the patient. Inform the patient that it may be necessary to remove hair from the site before the procedure. Address concerns about pain related to the procedure and explain that there should be no discomfort related to the procedure.
 Inform the patient that the procedure is performed by an HCP and takes approximately 15 min.
Inform the patient that the procedure is performed by an HCP and takes approximately 15 min. - Sensitivity to social and cultural issues, as well as concern for modesty, is important in providing psychological support before, during, and after the procedure.
- Instruct the patient to remove jewelry and other metallic objects from the area to be examined.
- Note that there are no food, fluid, or medication restrictions unless by medical direction.
Intratest
- Potential complications: N/A
- Observe standard precautions, and follow the general guidelines in Patient Preparation and Specimen Collection. Positively identify the patient.
- Ensure the patient has complied with pretesting preparations.
- Ensure the patient has removed all external metallic objects from the area to be examined prior to the procedure.
- Instruct the patient to void prior to the procedure and to change into the gown, robe, and foot coverings provided.
- Record baseline values.
- Place patient in a supine position. Expose and appropriately drape the chest, arms, and legs.
- Instruct the patient to cooperate fully and to follow directions. Instruct the patient to remain still throughout the procedure because movement produces unreliable results.
- Prepare the skin surface with alcohol and remove excess hair. Use clippers to remove hair from the site, if appropriate. Dry skin sites.
- Avoid the use of equipment containing latex if the patient has a history of allergic reaction to latex.
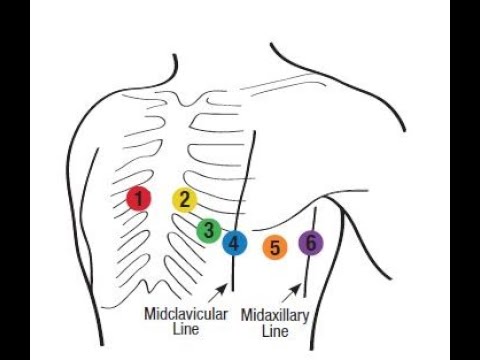
- Apply the electrodes in the proper position. When placing the six unipolar chest leads, place V1 at the fourth intercostal space at the border of the right sternum, V2 at the fourth intercostal space at the border of the left sternum, V3 between V2 and V4, V4 at the fifth intercostal space at the midclavicular line, V5 at the left anterior axillary line at the level of V4 horizontally, and V6 at the level of V4 horizontally and at the left midaxillary line.
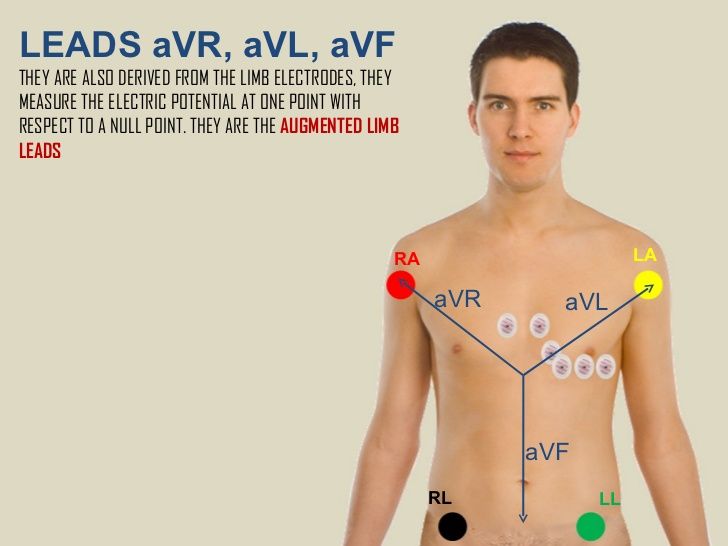 The wires are connected to the matched electrodes and the ECG machine. Chest leads (V1, V2, V3, V4, V5, and V6) record data from the horizontal plane of the heart.
The wires are connected to the matched electrodes and the ECG machine. Chest leads (V1, V2, V3, V4, V5, and V6) record data from the horizontal plane of the heart. - Place three limb bipolar leads (two electrodes combined for each) on the arms and legs. Lead I is the combination of two arm electrodes, lead II is the combination of right arm and left leg electrodes, and lead III is the combination of left arm and left leg electrodes. Limb leads (I, II, III, aVl, aVf, and aVr) record data from the frontal plane of the heart.
- The machine is set and turned on after the electrodes, grounding, connections, paper supply, computer, and data storage device are checked.
- If the patient has any chest discomfort or pain during the procedure, mark the ECG strip indicating that occurrence.
Post-Test
- Inform the patient that a report of the results will be made available to the requesting HCP, who will discuss the results with the patient.
- When the procedure is complete, remove the electrodes and clean the skin where the electrode was applied.
- Evaluate the results in relation to previously performed ECGs. Denote cardiac rhythm abnormalities on the strip.
- Monitor vital signs and compare with baseline values. Protocols may vary among facilities.
- Instruct the patient to immediately notify an HCP of chest pain, changes in pulse rate, or shortness of breath.
- Recognize anxiety related to the test results and be supportive of perceived loss of independence and fear of shortened life expectancy. Discuss the implications of abnormal test results on the patient’s lifestyle. Provide teaching and information regarding the clinical implications of the test results, as appropriate.
- Nutritional Considerations: Abnormal findings may be associated with cardiovascular disease. Nutritional therapy is recommended for the patient identified to be at risk for developing coronary artery disease (CAD) or for individuals who have specific risk factors and/or existing medical conditions (e.
 g., elevated LDL cholesterol levels, other lipid disorders, insulin-dependent diabetes, insulin resistance, or metabolic syndrome). Other changeable risk factors warranting patient education include strategies to encourage patients, especially those who are overweight and with high blood pressure, to safely decrease sodium intake, achieve a normal weight, ensure regular participation of moderate aerobic physical activity three to four times per week, eliminate tobacco use, and adhere to a heart-healthy diet. If triglycerides also are elevated, the patient should be advised to eliminate or reduce alcohol. The 2013 Guideline on Lifestyle Management to Reduce Cardiovascular Risk published by the American College of Cardiology (ACC) and the American Heart Association (AHA) in conjunction with the National Heart, Lung, and Blood Institute (NHLBI) recommends a “Mediterranean”-style diet rather than a low-fat diet. The new guideline emphasizes inclusion of vegetables, whole grains, fruits, low-fat dairy, nuts, legumes, and nontropical vegetable oils (e.
g., elevated LDL cholesterol levels, other lipid disorders, insulin-dependent diabetes, insulin resistance, or metabolic syndrome). Other changeable risk factors warranting patient education include strategies to encourage patients, especially those who are overweight and with high blood pressure, to safely decrease sodium intake, achieve a normal weight, ensure regular participation of moderate aerobic physical activity three to four times per week, eliminate tobacco use, and adhere to a heart-healthy diet. If triglycerides also are elevated, the patient should be advised to eliminate or reduce alcohol. The 2013 Guideline on Lifestyle Management to Reduce Cardiovascular Risk published by the American College of Cardiology (ACC) and the American Heart Association (AHA) in conjunction with the National Heart, Lung, and Blood Institute (NHLBI) recommends a “Mediterranean”-style diet rather than a low-fat diet. The new guideline emphasizes inclusion of vegetables, whole grains, fruits, low-fat dairy, nuts, legumes, and nontropical vegetable oils (e. g., olive, canola, peanut, sunflower, flaxseed) along with fish and lean poultry. A similar dietary pattern known as the Dietary Approach to Stop Hypertension (DASH) makes additional recommendations for the reduction of dietary sodium. Both dietary styles emphasize a reduction in consumption of red meats, which are high in saturated fats and cholesterol, and other foods containing sugar, saturated fats, trans fats, and sodium.
g., olive, canola, peanut, sunflower, flaxseed) along with fish and lean poultry. A similar dietary pattern known as the Dietary Approach to Stop Hypertension (DASH) makes additional recommendations for the reduction of dietary sodium. Both dietary styles emphasize a reduction in consumption of red meats, which are high in saturated fats and cholesterol, and other foods containing sugar, saturated fats, trans fats, and sodium. - Social and Cultural Considerations: Numerous studies point to the prevalence of excess body weight in American children and adolescents. Experts estimate that obesity is present in 25% of the population ages 6 to 11 yr. The medical, social, and emotional consequences of excess body weight are significant. Special attention should be given to instructing the child and caregiver regarding health risks and weight control education.
- Recognize anxiety related to test results, and be supportive of fear of shortened life expectancy. Discuss the implications of abnormal test results on the patient’s lifestyle.
 Provide teaching and information regarding the clinical implications of the test results, as appropriate. Educate the patient regarding access to counseling services. Provide contact information, if desired, for the American Heart Association (www.americanheart.org), the NHLBI (www.nhlbi.nih.gov), or the Legs for Life (www.legsforlife.org).
Provide teaching and information regarding the clinical implications of the test results, as appropriate. Educate the patient regarding access to counseling services. Provide contact information, if desired, for the American Heart Association (www.americanheart.org), the NHLBI (www.nhlbi.nih.gov), or the Legs for Life (www.legsforlife.org). - Reinforce information given by the patient’s HCP regarding further testing, treatment, or referral to another HCP. Answer any questions or address any concerns voiced by the patient or family.
- Depending on the results of this procedure, additional testing may be performed to evaluate or monitor progression of the disease process and determine the need for a change in therapy. Evaluate test results in relation to the patient’s symptoms and other tests performed.
Related Monographs
- Related tests include antiarrhythmic drugs, apolipoprotein A and B, AST, atrial natriuretic peptide, BNP, blood gases, blood pool imaging, calcium, chest x-ray, cholesterol (total, HDL, LDL), CT cardiac scoring, CT thorax, CRP, CK and isoenzymes, echocardiography, echocardiography transesophageal, exercise stress test, glucose, glycated hemoglobin, Holter monitor, homocysteine, ketones, LDH and isos, lipoprotein electrophoresis, lung perfusion scan, magnesium, MRI chest, MI infarct scan, myocardial perfusion heart scan, myoglobin, PET heart, potassium, pulse oximetry, sodium, triglycerides, and troponin.

- Refer to the Cardiovascular System table at the end of the book for related tests by body system.
Exercise Stress Test
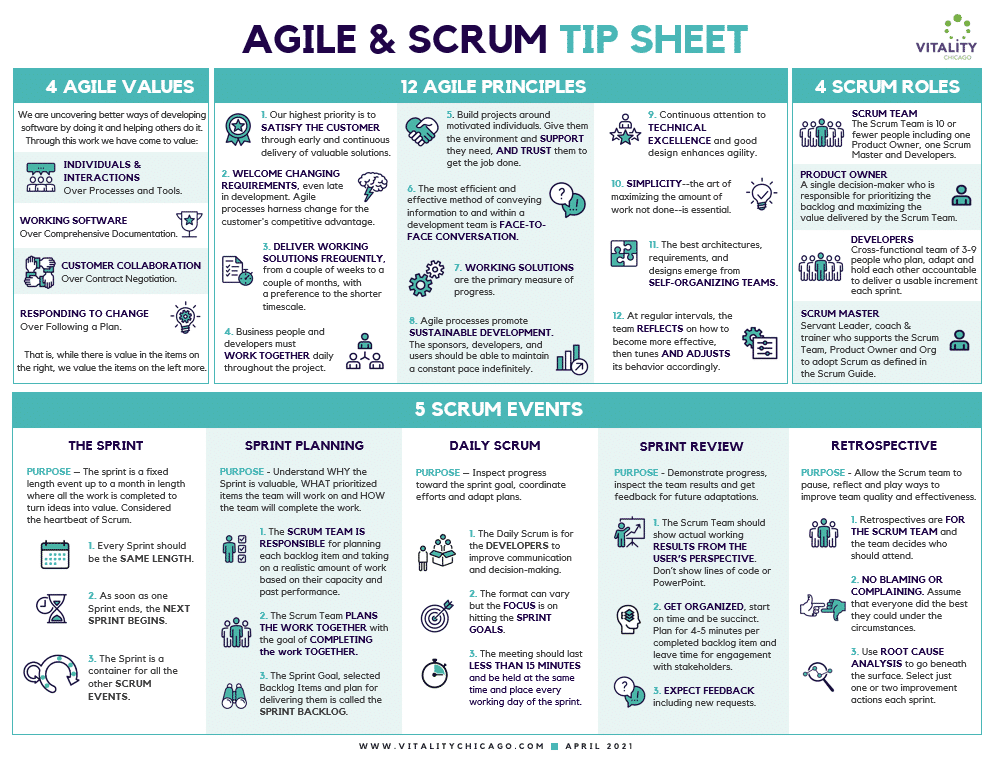
Synonym/acronym: Exercise electrocardiogram, ECG, EKG, graded exercise tolerance test, stress testing, treadmill test.
Common use
To assess cardiac function in relation to increased workload, evidenced by dysrhythmia or pain during exercise.
Area of application
Heart.
Contrast
None.
Description
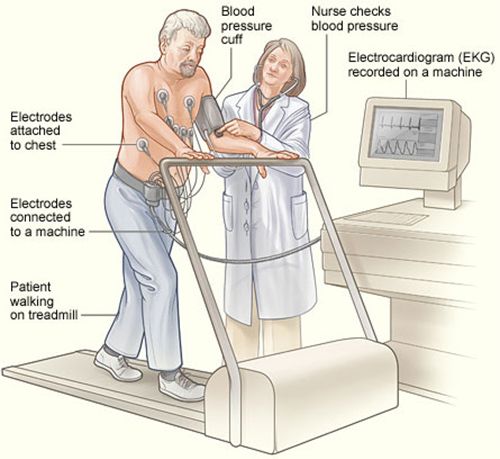
The exercise stress test is a noninvasive study to measure cardiac function during physical stress. Exercise electrocardiography is primarily useful in determining the extent of coronary artery occlusion by the heart’s ability to meet the need for additional oxygen in response to the stress of exercising in a safe environment. The patient exercises on a treadmill or pedals a stationary bicycle to increase the heart rate to 80% to 90% of maximal heart rate determined by age and gender, known as the target heart rate.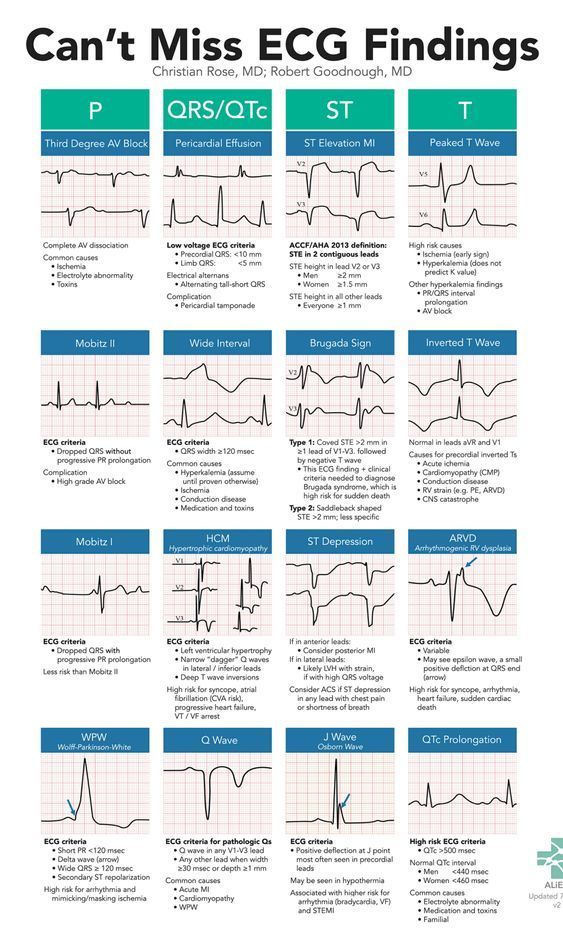 Every 2 to 3 min, the speed and/or grade of the treadmill is increased to yield an increment of stress. The patient’s electrocardiogram (ECG) and blood pressure are monitored during the test. The test proceeds until the patient reaches the target heart rate or experiences chest pain or fatigue. The risks involved in the procedure are possible myocardial infarction (1 in 500) and death (1 in 10,000) in patients experiencing frequent angina episodes before the test. Although useful, this procedure is not as accurate as cardiac nuclear scans for diagnosing coronary artery disease (CAD).
Every 2 to 3 min, the speed and/or grade of the treadmill is increased to yield an increment of stress. The patient’s electrocardiogram (ECG) and blood pressure are monitored during the test. The test proceeds until the patient reaches the target heart rate or experiences chest pain or fatigue. The risks involved in the procedure are possible myocardial infarction (1 in 500) and death (1 in 10,000) in patients experiencing frequent angina episodes before the test. Although useful, this procedure is not as accurate as cardiac nuclear scans for diagnosing coronary artery disease (CAD).
For patients unable to complete the test, pharmacological stress testing can be done. Medications used to pharmacologically exercise the patient’s heart include vasodilators such as dipyridamole and adenosine or dobutamine (which stimulates heart rate and pumping force). Stress testing should be discontinued when maximal performance has been reached or if certain criteria occur as noted in the Contraindications section.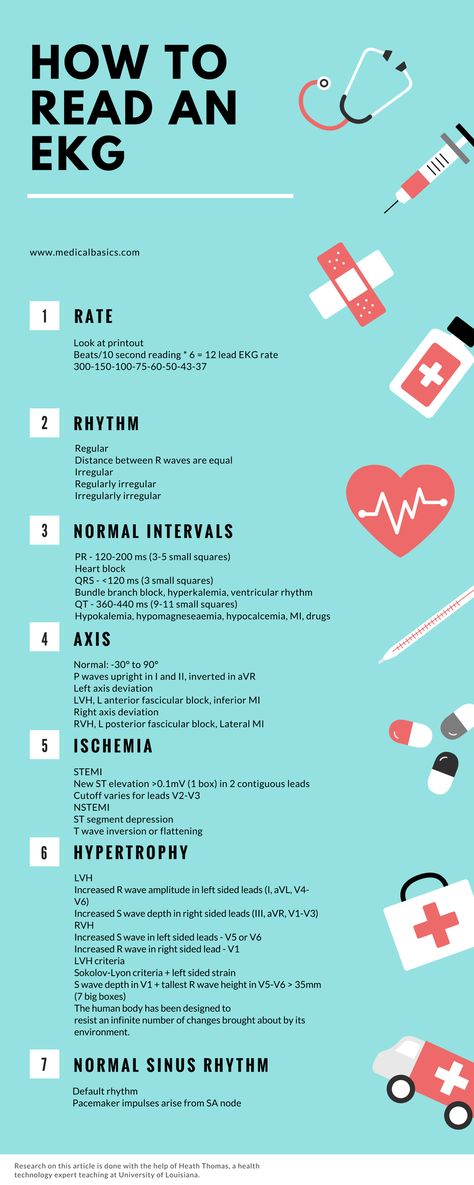 The patient’s ECG and blood pressure are monitored during the exercise phase. The test proceeds until the stimulated exercise portion is completed when a radiotracer, such as technetium-99m or sestamibi, is injected and images are taken by a gamma camera during the stimulated portion to compare with images taken at rest.
The patient’s ECG and blood pressure are monitored during the exercise phase. The test proceeds until the stimulated exercise portion is completed when a radiotracer, such as technetium-99m or sestamibi, is injected and images are taken by a gamma camera during the stimulated portion to compare with images taken at rest.
This procedure is contraindicated for
Indications
- Detect dysrhythmias during exercising, as evidenced by ECG changes
- Detect peripheral artery disease (PAD), as evidenced by leg pain or cramping during exercising
- Determine exercise-induced hypertension
- Evaluate cardiac function after myocardial infarction or cardiac surgery to determine safe exercise levels for cardiac rehabilitation as well as work limitations
- Evaluate effectiveness of medication regimens, such as antianginals or antiarrhythmics
- Evaluate suspected CAD in the presence of chest pain and other symptoms
- Screen for CAD in the absence of pain and other symptoms in patients at risk
Potential diagnosis
Normal findings
- Normal heart rate during physical exercise.
 Heart rate and systolic blood pressure rise in direct proportion to workload and to metabolic oxygen demand, which is based on age and exercise protocol. Maximal heart rate for adults is normally 150 to 200 beats/min.
Heart rate and systolic blood pressure rise in direct proportion to workload and to metabolic oxygen demand, which is based on age and exercise protocol. Maximal heart rate for adults is normally 150 to 200 beats/min.
Abnormal findings related to
- Activity intolerance related to oxygen supply and demand imbalance
- Bradycardia
- CAD
- Chest pain related to ischemia or inflammation
- Decreased cardiac output
- Dysrhythmias
- Hypertension
- PAD
- ST segment depression of 1 mm (considered a positive test), indicating myocardial ischemia
- Tachycardia
Critical findings
- N/A
Interfering factors
Nursing Implications and Procedure
Pretest
- Positively identify the patient using at least two unique identifiers before providing care, treatment, or services.
- Patient Teaching: Inform the patient this procedure can assist in assessing the heart’s ability to respond to an increasing workload.
- Obtain a history of the patient’s complaints or clinical symptoms, including a list of known allergens, especially allergies or sensitivities to latex or medications used to pharmacologically exercise the patient’s heart.
- Obtain a history of the patient’s cardiovascular system, symptoms, and results of previously performed laboratory tests and diagnostic and surgical procedures.
- Inquire if the patient has had any chest pain within the past 48 hr or has a history of anginal attacks; if either of these has occurred, inform the health-care provider (HCP) immediately because the stress test may be too risky and should be rescheduled in 4 to 6 wk.
- Obtain a list of the patient’s current medications, including herbs, nutritional supplements, and nutraceuticals (see Effects of Natural Products on Laboratory Values online at DavisPlus).
- Review the procedure with the patient. Address concerns about pain related to the procedure and explain that some discomfort may be experienced during the stimulated portion of the test.
 Inform the patient that the procedure is performed in a special department by an HCP specializing in this procedure and takes approximately 30 to 60 min.
Inform the patient that the procedure is performed in a special department by an HCP specializing in this procedure and takes approximately 30 to 60 min. - Sensitivity to social and cultural issues, as well as concern for modesty, is important in providing psychological support before, during, and after the procedure.
- Record a baseline 12-lead ECG and vital signs.
- Instruct the patient to wear comfortable shoes and clothing for the exercise.
- Instruct the patient to fast, restrict fluids, and avoid tobacco products for 4–6 hr prior to the procedure. Protocols may vary among facilities.
- Make sure a written and informed consent has been signed prior to the procedure and before administering any medications.
Intratest
Post-Test
- Inform the patient that a report of the results will be made available to the requesting HCP, who will discuss the results with the patient.
- Instruct the patient to resume usual activity, as directed by the HCP.
- Instruct the patient to contact the HCP to report any anginal pain or other discomforts experienced after the test.
- Nutritional Considerations: Abnormal findings may be associated with cardiovascular disease. Nutritional therapy is recommended for the patient identified to be at risk for developing CAD or for individuals who have specific risk factors and/or existing medical conditions (e.g., elevated LDL cholesterol levels, other lipid disorders, insulin-dependent diabetes, insulin resistance, or metabolic syndrome). Other changeable risk factors warranting patient education include strategies to encourage patients, especially those who are overweight and with high blood pressure, to safely decrease sodium intake, achieve a normal weight, ensure regular participation of moderate aerobic physical activity three to four times per week, eliminate tobacco use, and adhere to a heart-healthy diet. If triglycerides also are elevated, the patient should be advised to eliminate or reduce alcohol.
 The 2013 Guideline on Lifestyle Management to Reduce Cardiovascular Risk published by the American College of Cardiology (ACC) and the American Heart Association (AHA) in conjunction with the National Heart, Lung, and Blood Institute (NHLBI) recommends a “Mediterranean”-style diet rather than a low-fat diet. The new guideline emphasizes inclusion of vegetables, whole grains, fruits, low-fat dairy, nuts, legumes, and nontropical vegetable oils (e.g., olive, canola, peanut, sunflower, flaxseed) along with fish and lean poultry. A similar dietary pattern known as the Dietary Approach to Stop Hypertension (DASH) diet makes additional recommendations for the reduction of dietary sodium. Both dietary styles emphasize a reduction in consumption of red meats, which are high in saturated fats and cholesterol, and other foods containing sugar, saturated fats, trans fats, and sodium.
The 2013 Guideline on Lifestyle Management to Reduce Cardiovascular Risk published by the American College of Cardiology (ACC) and the American Heart Association (AHA) in conjunction with the National Heart, Lung, and Blood Institute (NHLBI) recommends a “Mediterranean”-style diet rather than a low-fat diet. The new guideline emphasizes inclusion of vegetables, whole grains, fruits, low-fat dairy, nuts, legumes, and nontropical vegetable oils (e.g., olive, canola, peanut, sunflower, flaxseed) along with fish and lean poultry. A similar dietary pattern known as the Dietary Approach to Stop Hypertension (DASH) diet makes additional recommendations for the reduction of dietary sodium. Both dietary styles emphasize a reduction in consumption of red meats, which are high in saturated fats and cholesterol, and other foods containing sugar, saturated fats, trans fats, and sodium. - Social and Cultural Considerations: Numerous studies point to the prevalence of excess body weight in American children and adolescents.
 Experts estimate that obesity is present in 25 % of the population ages 6 to 11 yr. The medical, social, and emotional consequences of excess body weight are significant. Special attention should be given to instructing the child and caregiver regarding health risks and weight control education.
Experts estimate that obesity is present in 25 % of the population ages 6 to 11 yr. The medical, social, and emotional consequences of excess body weight are significant. Special attention should be given to instructing the child and caregiver regarding health risks and weight control education. - Recognize anxiety related to test results, and be supportive of fear of shortened life expectancy. Discuss the implications of abnormal test results on the patient’s lifestyle. Provide teaching and information regarding the clinical implications of the test results, as appropriate. Educate the patient regarding access to counseling services. Provide contact information, if desired, for the American Heart Association (www.americanheart.org), the NHLBI (www.nhlbi.nih.gov), or the Legs for Life (www.legsforlife.org). Reinforce information given by the patient’s HCP regarding further testing, treatment, or referral to another HCP. Answer any questions or address any concerns voiced by the patient or family.
- Depending on the results of this procedure, additional testing may be performed to evaluate or monitor progression of the disease process and determine the need for a change in therapy. Evaluate test results in relation to the patient’s symptoms and other tests performed.
Related Monographs
- Related tests include antiarrhythmic drugs, apolipoprotein A and B, AST, atrial natriuretic peptide, BNP, blood gases, blood pool imaging, calcium, chest x-ray, cholesterol (total, HDL, LDL), CT cardiac scoring, CT thorax, CRP, CK and isoenzymes, echocardiography, echocardiography transesophageal, electrocardiogram, glucose, glycated hemoglobin, Holter monitor, homocysteine, ketones, LDH and isos, lipoprotein electrophoresis, lung perfusion scan, magnesium, MRI chest, MI infarct scan, myocardial perfusion heart scan, myoglobin, PET heart, potassium, pulse oximetry, sodium, triglycerides, and troponin.
- Refer to the Cardiovascular System table at the end of the book for related tests by body system.
Handbook of Laboratory and Diagnostic Tests, © 2013 Farlex and Partners
How the ECG procedure is carried out: indications, preparation, conducting at home
Call us right now at
+7 (812) 435 55 55
Call a doctor at home
Content of the article:
- Indications for an ECG 9001
- ECG diagnostic algorithm
- ECG technique
- How to read an ECG
- What kind of heart diseases does ECG show
- Holter monitoring: readings
- Ambulatory monitoring technique
- Stress Electrocardiography: Indications and Preparation
- Stress test technique
- Difference between ECG and Echo-KG
- ECG at home
ECG (electrocardiography, or cardiogram) of the heart is the simplest and most commonly used method for assessing the work of the heart. The device for recording a cardiogram is called an electrocardiograph.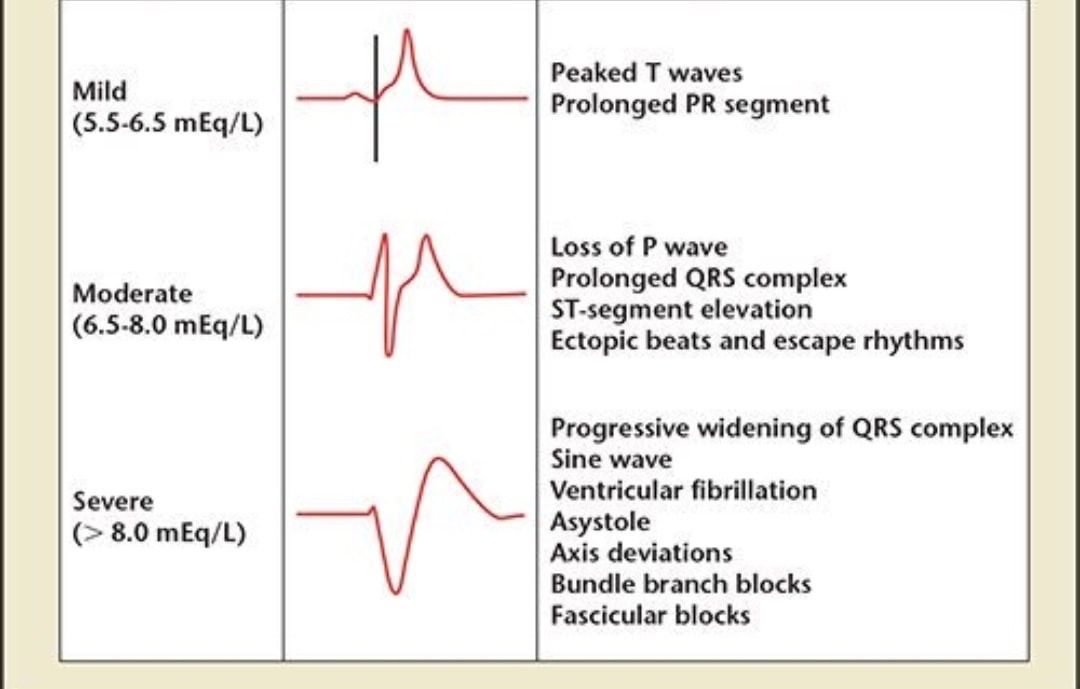 It captures and registers electrical impulses that occur in the heart muscle. The method is non-invasive - it does not require a violation of the skin, penetration into the cavities of the body.
It captures and registers electrical impulses that occur in the heart muscle. The method is non-invasive - it does not require a violation of the skin, penetration into the cavities of the body.
Indications for ECG
Electrocardiography is done for preventive purposes, for the primary diagnosis of diseases and to track the dynamics of the condition in patients with already diagnosed heart pathologies.
Preventive purposes:
- medical examinations of children at a certain age, before entering the children's
kindergarten, school, sports sections, camps;
- professional examinations of young men of military age;
- professional examinations of employees of enterprises, professional athletes;
- medical examination of citizens;
- commission for obtaining a driver's license, weapons permit;
- examination before hospitalization for planned surgical treatment;
- Examination of pregnant women when registering in a antenatal clinic.
For initial diagnosis, electrocardiography is given to people who have symptoms of heart disease. For patients with an already established diagnosis, the cardiogram is recorded during treatment, at periodic examinations after recovery.
ECG diagnostic algorithm
The human heart spontaneously generates electrical impulses that cause it to contract and relax. Impulses pass through the muscle tissue of the heart from the point of their origin to the point of contraction. It is a cyclical and continuous process. The impulses are captured by the electrodes of the cardiograph, amplified, recorded by a galvanometer and displayed as a graph on special paper - ECG film or in electronic form.
A curve drawn on film will not tell the patient anything. Its decoding is carried out by a cardiologist or special software. Often, in addition to an electrocardiogram, an ultrasound (Echo-KG study) of the heart is done.
Preparing for the procedure
An ECG is usually sent by a cardiologist, internist or pediatrician.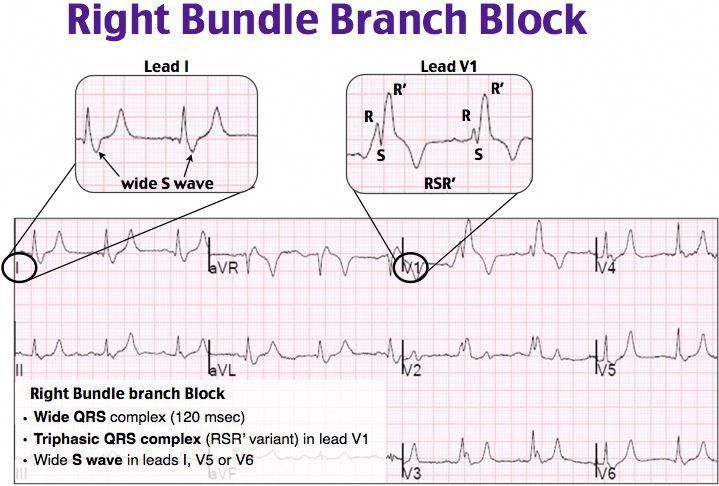 The patient must warn the doctor in advance about taking antiarrhythmic drugs, drugs for hypertension, cardiac glycosides. General rules for preparing a patient for an ECG:
The patient must warn the doctor in advance about taking antiarrhythmic drugs, drugs for hypertension, cardiac glycosides. General rules for preparing a patient for an ECG:
- 2-3 hours before the examination, do not drink tea, coffee, energy drinks, do not smoke;
- do not take sedatives on the day of the procedure;
- avoid physical activity, do not play sports before recording the electrocardiogram;
- Wear clothing that allows you to easily free your chest, ankles and wrists.
The electrocardiography nurse is responsible for recording the cardiogram. Therefore, if the patient wants to discuss something with the doctor, you need to do this in advance. The result will also be reported by the doctor, some time after the procedure, sufficient to prepare a description. The time of the ECG takes from 5 to 10 minutes (at rest), the ECG with a load is carried out for 15-20 minutes.
ECG technique
The patient lies on a couch, exposing the shins, forearms and upper body.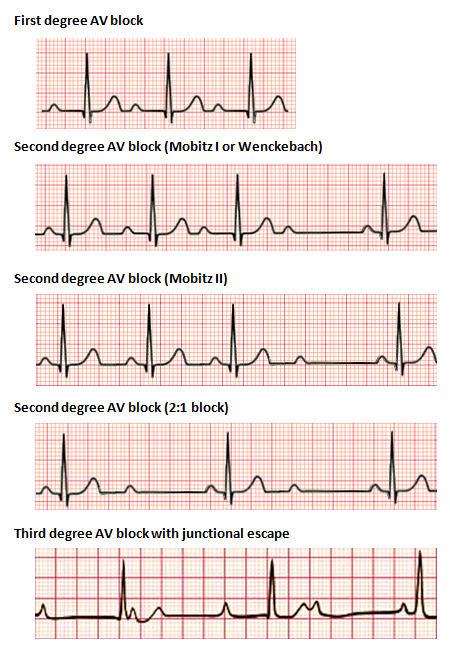 The nurse degreases the skin areas on which the electrodes will be applied by wiping them with a tissue moistened with isotonic sodium chloride solution. The surface of the electrodes is also degreased, a gel is applied to it or to the skin to improve electrical conductivity.
The nurse degreases the skin areas on which the electrodes will be applied by wiping them with a tissue moistened with isotonic sodium chloride solution. The surface of the electrodes is also degreased, a gel is applied to it or to the skin to improve electrical conductivity.
The electrodes are fixed on the patient's body in a certain order. A red electrode is applied to the right hand, and a yellow electrode to the left. The black electrode is for the right leg, and the green electrode for the left leg. 6 electrodes are applied to the chest in certain positions (V1 - red, V2 - yellow, V3 - green, V4 - brown, V5 - black, V6 - blue) or one electrode is sequentially moved to different points.
Before recording an ECG, the patient needs to calm down, while recording - do not move, do not take deep breaths. An ECG of the heart can be done as often as necessary, the procedure does not have any effect on the body.
How to read a cardiogram
It is almost impossible for people without special medical training to evaluate the result of electrocardiography. The interpretation of the ECG in adults and children is done either by the doctor who sent the patient to this study, or by the doctor of the functional diagnostics department.
The interpretation of the ECG in adults and children is done either by the doctor who sent the patient to this study, or by the doctor of the functional diagnostics department.
The ECG film displays a graph in the form of a broken curve with peaks (teeth) and intervals between them located on a straight line, which is called an isoline. The teeth are indicated by the letters of the Latin alphabet - P, Q, R, S, T, intervals - P-Q, P-R, QRST (QT), QRS, S-T. To interpret the results of the cardiogram, the doctor evaluates the duration of the teeth in seconds and their amplitude in standard leads in millimeters, as well as the duration of the intervals in seconds.
There are established norms for these values. Comparing the ECG result with normal values, the doctor may suspect an abnormal heart rate, the presence of arrhythmias, diagnose acute conditions such as myocardial infarction, an angina pectoris attack.
What kind of heart disease is shown by ECG
ECG is one of the most accurate methods for diagnosing rhythm disturbances.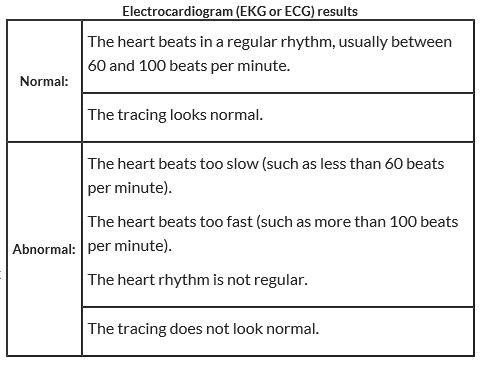 With its help, you can identify the cause of rhythm disturbance, the location of the pathological focus of excitation, the type of arrhythmia. Partial or complete blockade of the conduction pathways of the heart is also well displayed on the electrocardiogram.
With its help, you can identify the cause of rhythm disturbance, the location of the pathological focus of excitation, the type of arrhythmia. Partial or complete blockade of the conduction pathways of the heart is also well displayed on the electrocardiogram.
Electrocardiography plays an important role in the diagnosis of acute myocardial infarction. Changes in a heart attack are clearly displayed on the tape, in combination with the clinic, this allows you to start treatment in a timely manner and in many cases save the patient. Therefore, doctors or paramedics on calls to patients with complaints of pain in the heart always have a portable device with them in order to be able to make a cardiogram of the heart at home.
Holter monitoring: indications
For a more accurate diagnosis of certain diseases of the heart and blood vessels, additional types of ECG studies are prescribed. One of them is a continuous recording of an electrocardiogram for 24 (rarely 48, 72) hours, or Holter monitoring.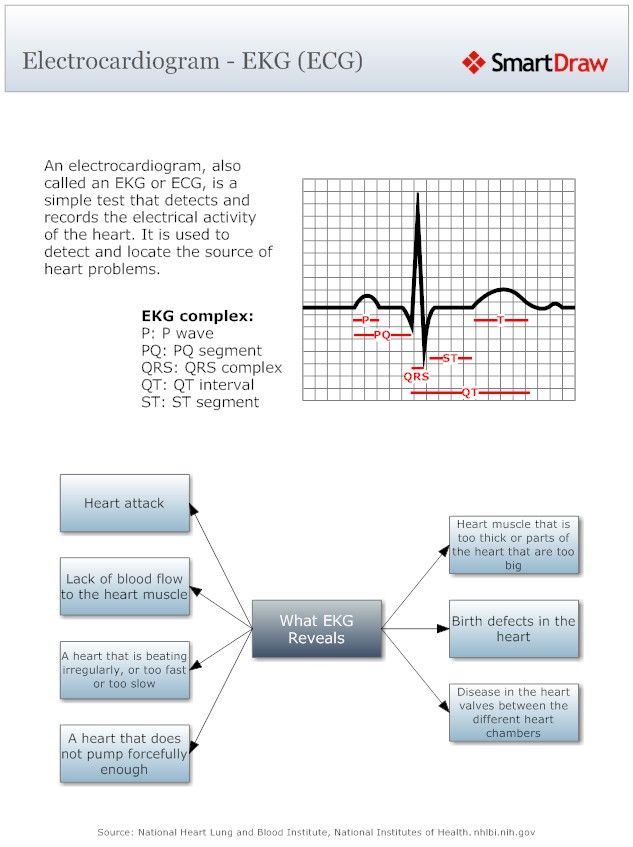 It is indicated in the following situations:
It is indicated in the following situations:
- recovery period after myocardial infarction;
- diagnostics and monitoring of the dynamics of various cardiomyopathies;
- assessment of the work of the cardiovascular system in congenital and acquired heart defects;
- hypertension;
- chronic heart failure;
- suspected arrhythmias;
- pain behind the sternum of an unknown nature without changes on the cardiogram at rest;
- causeless dizziness and fainting.
24-hour monitoring technique
Electrodes are placed on the patient's chest, just as when taking a cardiogram at rest, they are additionally fixed with an adhesive plaster. The electrodes are connected to a recorder, which the patient wears in a special case all the time of monitoring.
Electrocardiography recording during monitoring can be fragmentary (the patient presses the button on the recorder when the condition worsens) or permanent (all cardiac cycles are recorded for a day or more).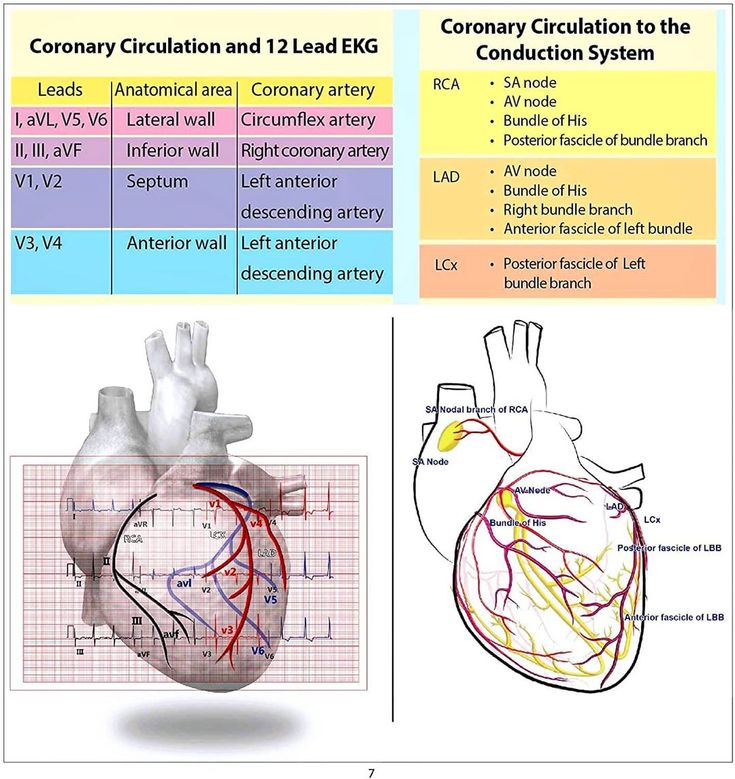 At the same time, the subject keeps a special diary, where he records the time of sleep, wakefulness, the presence of physical activity, stress and other significant events. Additionally, the patient can perform stress tests as prescribed by the doctor.
At the same time, the subject keeps a special diary, where he records the time of sleep, wakefulness, the presence of physical activity, stress and other significant events. Additionally, the patient can perform stress tests as prescribed by the doctor.
Stress electrocardiography: indications and preparation
ECG under stress (stress test, or treadmill test) is done to clarify the diagnosis of coronary heart disease, to monitor cardiac activity after coronary artery bypass grafting in myocardial infarction, to diagnose and monitor the dynamics of some heart defects.
The study is also conducted for healthy people - professional athletes, pilots of civil and military aviation, candidates for service in law enforcement agencies, contract service in the army.
To prepare for an exercise ECG, you should avoid tea, coffee, alcoholic and energy drinks, and smoking during the day before the procedure. The last meal should be 3-4 hours before the recording of the electrocardiogram.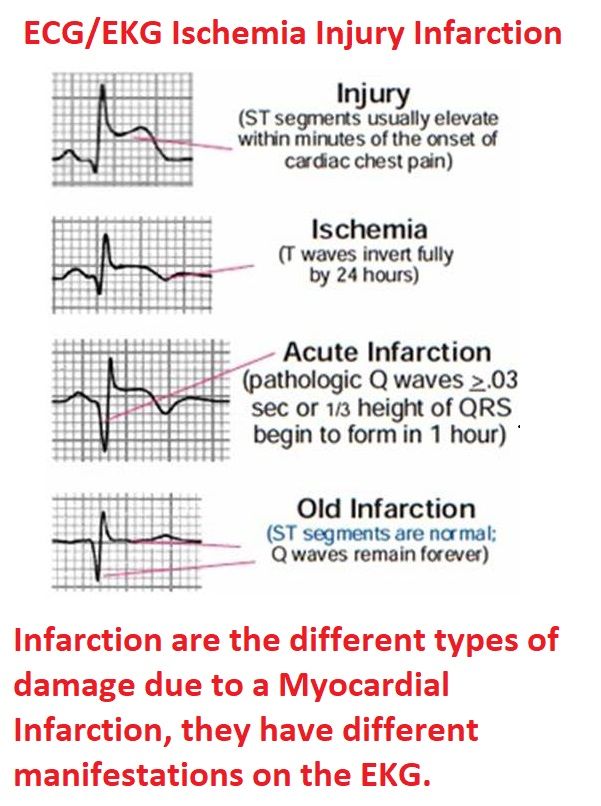 Intense physical activity must be stopped two days before the study. Three days before the procedure, men should refuse to take potency-improving drugs (Viagra, Cialis).
Intense physical activity must be stopped two days before the study. Three days before the procedure, men should refuse to take potency-improving drugs (Viagra, Cialis).
Stress test technique
An ECG is recorded at rest, then during or immediately after exercise, if necessary, a few minutes after exercise.
Load:
- squats - 20 times in 40-60 seconds;
- ascent and descent of the step platform with feet - 20 times in 40-60 seconds;
- running on a treadmill at a moderate pace for 20-25 seconds;
- three-minute load on a bicycle ergometer.
The doctor assesses the heart rate, their rhythm at rest, changes in these indicators during exercise and during the recovery period. Sometimes, simultaneously with recording an electrocardiogram under load, blood pressure is measured and the indicators are evaluated in combination.
After the procedure, the health worker should monitor the patient's condition until the pulse rate returns to normal.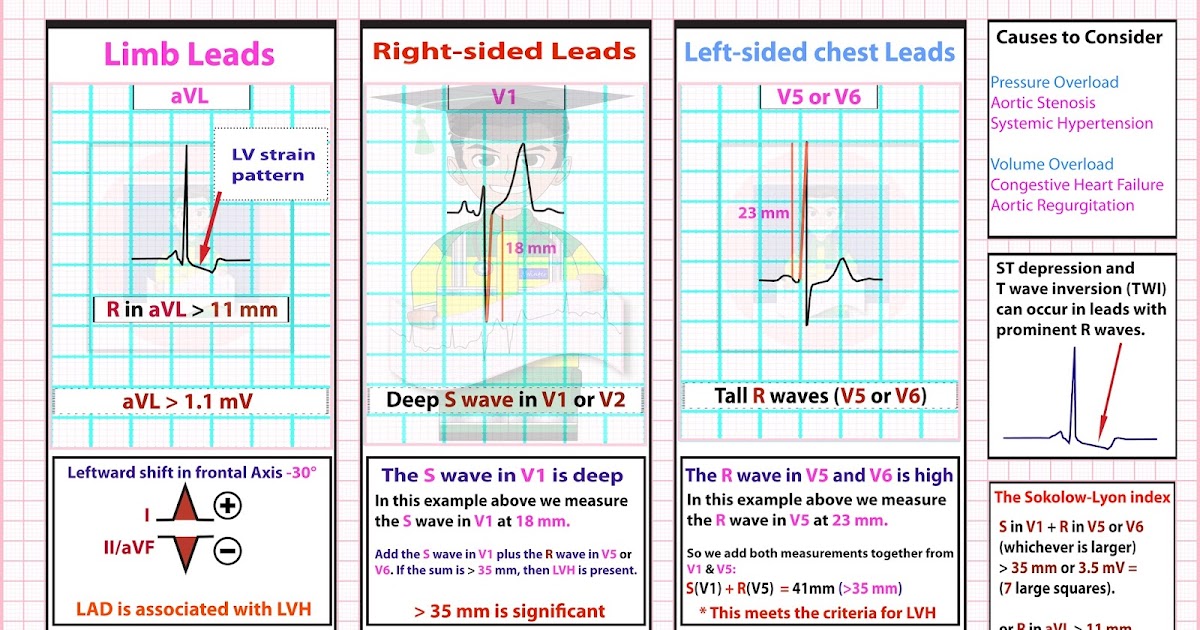
ECG differs from Echo-KG
Echo-KG, or echocardiography, which is also called cardiac ultrasound, is a procedure that is fundamentally different from ECG.
Echocardiography is a non-invasive ultrasound examination of the heart and blood vessels. The high-frequency sound emitted by the echocardiograph transducer, passing through the tissues of the heart, is reflected from them and recorded by the same transducer. The result is displayed as an image on the monitor.
Echo-KG data allow you to evaluate the size of the heart, the thickness, integrity and structure of the heart muscle, the size of the cavities of the ventricles and atria, myocardial contractility, the condition of the valves and large vessels.
Ultrasound and ECG are different methods, so it cannot be said that it is better to check the condition of the heart with one of them. To assess the activity of the cardiovascular system, these studies are assigned in combination.
ECG at home
ECG at home is possible not only in emergency cases.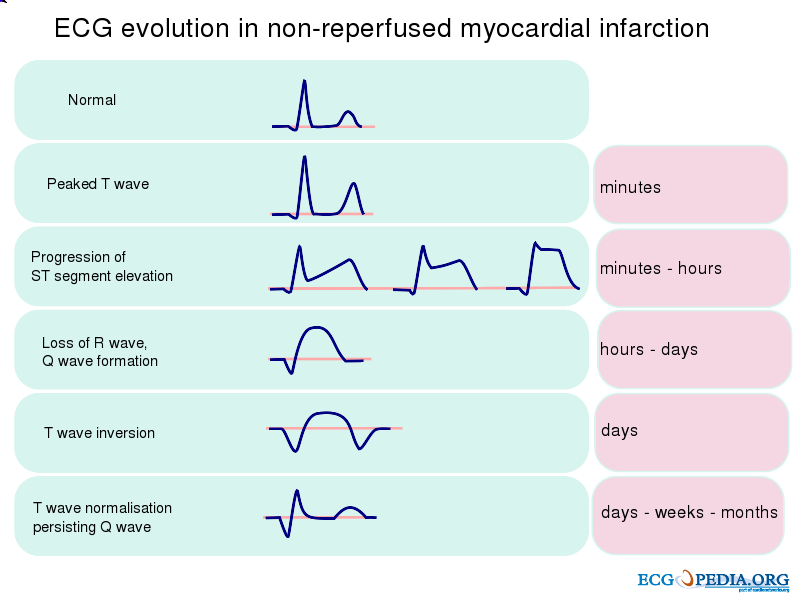 The ECG recording service with its simultaneous interpretation and consultation with a cardiologist is in demand among the elderly, people with limited mobility, the disabled, and patients who are indicated for bed rest. The reason for conducting an ECG at home and at a convenient time may be the reluctance to visit the clinic (especially during a pandemic), the patient's irregular work schedule. In addition, in polyclinics, waiting for an appointment for a procedure is often stretched out for weeks in advance.
The ECG recording service with its simultaneous interpretation and consultation with a cardiologist is in demand among the elderly, people with limited mobility, the disabled, and patients who are indicated for bed rest. The reason for conducting an ECG at home and at a convenient time may be the reluctance to visit the clinic (especially during a pandemic), the patient's irregular work schedule. In addition, in polyclinics, waiting for an appointment for a procedure is often stretched out for weeks in advance.
Indications for recording an ECG at home are the same conditions as listed above. The technique of the procedure is also no different from an ECG in a medical institution. The doctor comes to the patient's home at a prearranged time, with a portable device for recording electrocardiography. After removing the cardiogram, the doctor deciphers it. The patient is given a conclusion, which he sends to the attending physician or uses for other purposes (commissions, professional examinations).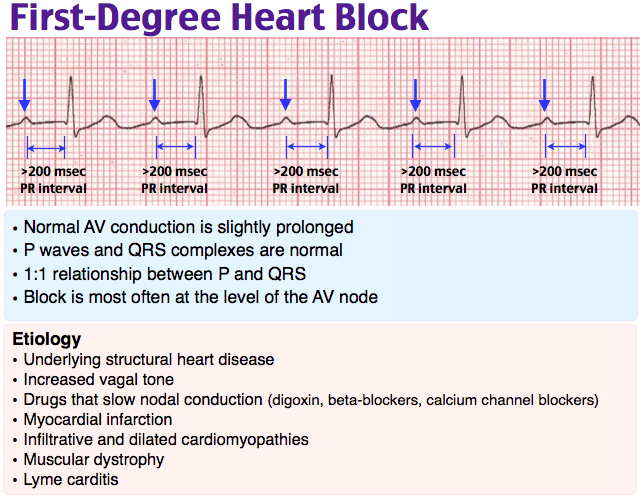
Stress electrocardiography | Children's medical center "Miracle Children"
What is an electrocardiogram (ECG)?
An electrocardiogram records the electrical activity of a child's heart. Sometimes this study is called an ECG. A diagnostic procedure is used to check if the pulse and rhythm of the heart is normal. An ECG also helps doctors determine if a child has certain heart problems, including:
- A larger than normal heart (heart enlargement)
- Electrolyte imbalance
- Pericarditis and other diseases of the heart
- Electrical anomalies such as Wolff-Parkinson-White syndrome or long QT syndrome.
In addition, the ECG is used to check the heart before and after heart surgery or a cardiac catheterization procedure. An ECG can also be used to check for a pacemaker or the effects of certain heart medications.
How does an ECG work?
Cardiogram is a non-invasive test. The doctor will attach up to 13 wires (electrodes) with stickers to the arms, legs and chest of the child. The electrodes pick up tiny electrical signals from the heart and send them to a computer, which prints out the information on a piece of paper for the doctor to interpret.
The electrodes pick up tiny electrical signals from the heart and send them to a computer, which prints out the information on a piece of paper for the doctor to interpret.
An ECG allows the physician to "see" the electrical activity of the heart simultaneously from multiple perspectives. The result looks like a group of wavy lines. Each of the waves on the ECG tells the doctor about the electrical activity in different parts of the heart and can help diagnose various heart defects and abnormalities. The doctor will use the ECG to look for any abnormal heart rhythms that may affect your baby.
Children generally have a higher resting heart rate than adults, up to 180 beats per minute in an infant. An adult's resting heart rate is typically between 60 and 100 beats per minute.
What happens during an ECG?
The child lies down on the couch. The nurse will attach up to 13 sticker electrodes to the baby's chest. These electrodes will record electrical signals from the heart.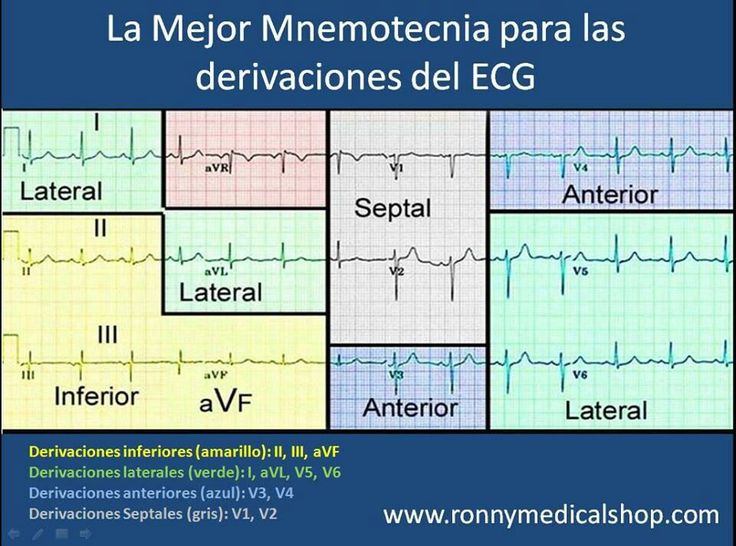 An EKG takes 5 to 10 minutes. If an ECG is done during a clinic visit, the results will be provided during that visit.
An EKG takes 5 to 10 minutes. If an ECG is done during a clinic visit, the results will be provided during that visit.
What is a stress ECG?
An exercise test, also called a cardiac stress test or exercise ECG, is used to assess the range of a child's heart. When the child is sitting or lying down, the heart does not work very hard. When a child walks fast, swims or runs, the heart has to work harder. The idea behind the exercise test is to objectively assess how well the heart is working when the activity is increased. This is a very good way to assess heart health. Cardiac stress testing works on the principle of demonstrating induced ischemia as workload increases (either due to exercise or pharmacological stress). A decrease in blood pressure during exercise is one of the most significant signs of ischemia.
Examination is usually done when the heart beats first at rest and then after exercise. In this study, the child is asked to run on a treadmill with an increase in its incline, or to pedal on an exercise bike to increase the heart rate.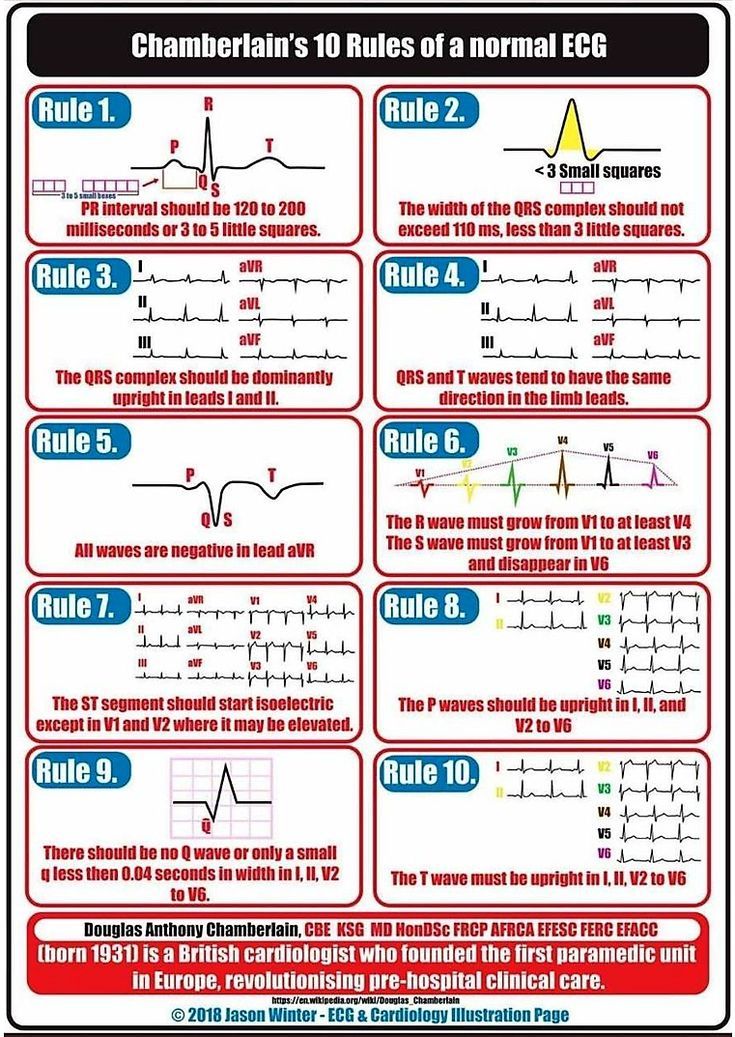 For young children, the drug dobutamine may be used instead of exercise to increase the heart rate. This type of stress test can also be combined with ultrasound imaging of the heart to physically see how well the heart is working.
For young children, the drug dobutamine may be used instead of exercise to increase the heart rate. This type of stress test can also be combined with ultrasound imaging of the heart to physically see how well the heart is working.
During the examination, the child is monitored closely to find out his pulse rate and blood pressure. The electrical activity of the heart is also recorded using an ECG. The exercise treadmill test usually lasts no more than 12 minutes and does not pose a significant risk as it will be done under controlled conditions. The study will be stopped long before the child reaches the level of stress at which the heart will be very fast. It may take 10-15 minutes for the child to return to normal, but this is just the usual rest period as after any type of exercise.
Will additional testing be required after the stress test?
Of course, additional research may be required. An exercise ECG is often used as a screening test. If the result is normal, then no further tests are usually required.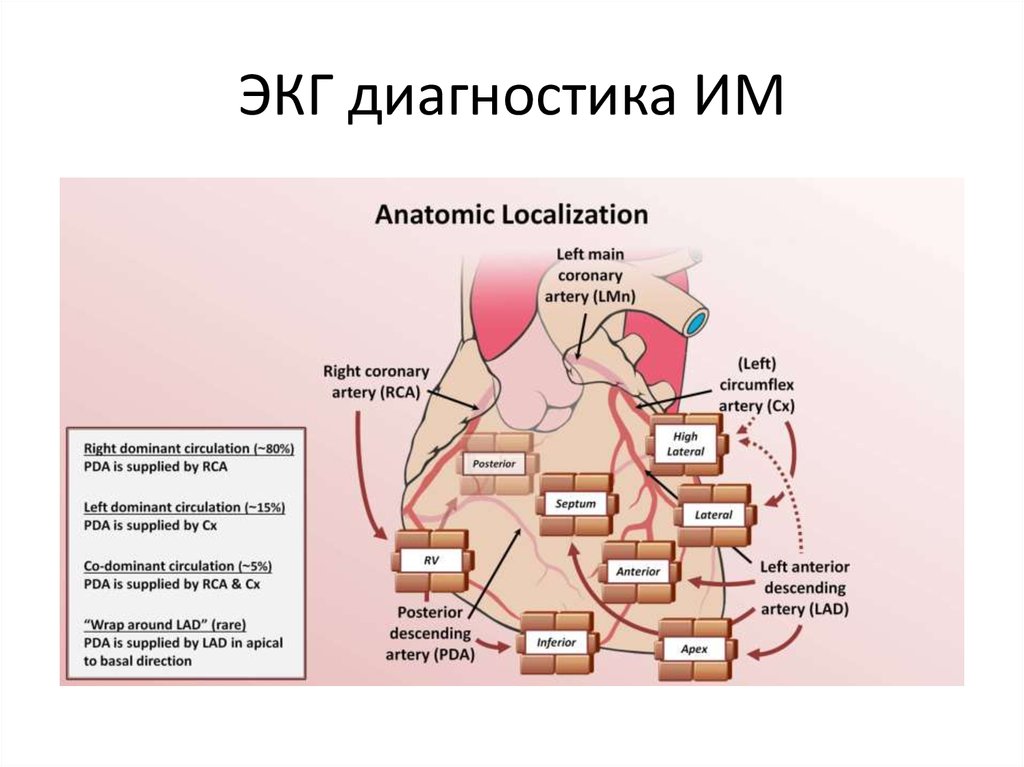 If this is not the case, the child may need further testing, depending on the type of problem identified. Stress ECG and stress echocardiography are functional tests and cannot determine the percentage of coronary stenosis. While stress echocardiography can determine which artery may be stenotic, stress ECG does not indicate which coronary artery is causing ischemia. To identify a problematic vessel, a coronary angiogram is used - one of the most common types of studies, which is carried out according to the results of a stress test.
If this is not the case, the child may need further testing, depending on the type of problem identified. Stress ECG and stress echocardiography are functional tests and cannot determine the percentage of coronary stenosis. While stress echocardiography can determine which artery may be stenotic, stress ECG does not indicate which coronary artery is causing ischemia. To identify a problematic vessel, a coronary angiogram is used - one of the most common types of studies, which is carried out according to the results of a stress test.
Are there any contraindications to the study?
Absolute contraindications to cardiac stress testing include acute myocardial infarction (including new left bundle branch block, high-risk unstable angina, symptomatic severe aortic stenosis, uncontrolled arrhythmia causing symptoms or hemodynamic instability, unstable heart failure, acute pulmonary embolism and acute aortic dissection
Relative contraindications include left coronary artery stenosis, severe hypertension, electrolyte disturbances, hypertrophic obstructive cardiomyopathy, and uncontrolled arrhythmias.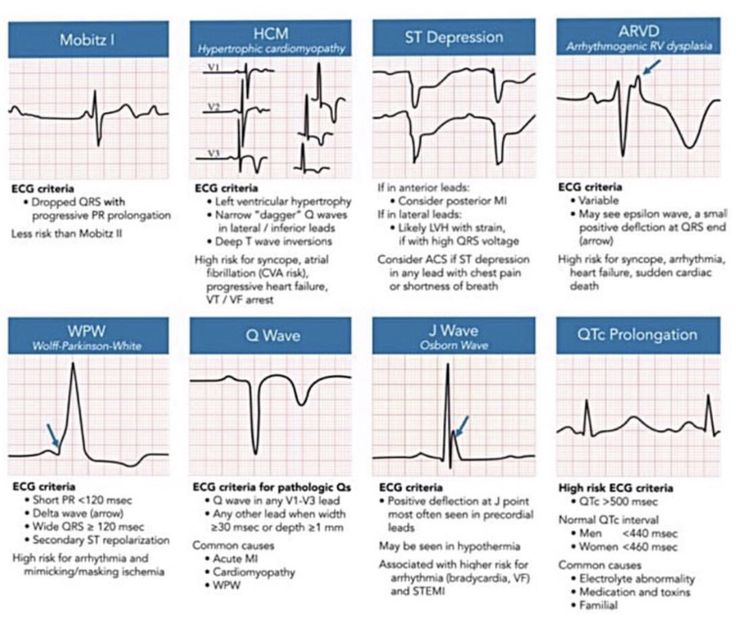 In the presence of relative contraindications, the study may be performed if the benefit of detecting ischemia outweighs the risk of testing.
In the presence of relative contraindications, the study may be performed if the benefit of detecting ischemia outweighs the risk of testing.
Explanation of the results
The results of the study contain a conclusion about the presence or absence of signs of impaired blood supply to the heart muscle during exercise, about the reaction to the load of the level of blood pressure and the rate of recovery of initial indicators after exercise. Based on the study, recommendations can be made about the acceptable level of physical activity for your child. In some cases, it may be necessary to repeat an electrocardiographic study or a special type of ECG, accompanied by other types of studies (ultrasound of the heart, dopplerography of blood vessels).
Exercise electrocardiography is a special type of study of the characteristics of the child's heart during physical activity, which allows you to identify hidden diseases, accurately diagnose and carry out the required treatment with maximum efficiency, or get rid of worries and doubts about your baby's health.
Learn more

-Cap-30mg-UK-2.jpg)