What does a behavioral therapist do
Behavioral Therapy: Definition, Types & Effectiveness
Behavioral therapy is an umbrella term for types of therapy that treat mental health disorders.
This form of therapy looks to identify and help change potentially self-destructive or unhealthy behaviors. It’s based on the idea that all behaviors are learned and that behaviors can be changed. The focus of treatment is often on current problems and how to change them.
Behavioral therapy can benefit people with a wide range of disorders.
People most commonly look for behavioral therapy to treat:
- depression
- anxiety
- panic disorders
- disorders involving excessive anger, like intermittent explosive disorder
It can also help treat conditions and disorders like:
- eating disorders
- post-traumatic stress disorder
- bipolar disorder
- attention deficit hyperactivity disorder (ADHD)
- phobias, including social phobias
- obsessive compulsive disorder
- self-harming behavior, like cutting
- substance use disorders
This type of therapy can benefit adults and children.
There are a number of different types of behavioral therapy.
Cognitive behavioral therapy
Cognitive behavioral therapy is extremely popular. It combines behavioral therapy, which focuses on patterns of action, with cognitive therapy, which focuses on patterns of thought.
Treatment is centered around how your thoughts and beliefs influence your actions and moods. It often focuses on your current problems and how to solve them. The long-term goal is to build thinking and behavioral patterns that help you achieve a better quality of life.
Cognitive behavioral play therapy
Cognitive behavioral play therapy is commonly used as a treatment for mental health conditions in children. By watching a child play, a therapist is able to gain insight into what a child is uncomfortable expressing or unable to express.
Children may be able to choose their own toys and play freely. They might be asked to draw a picture or use toys to create scenes in a sandbox.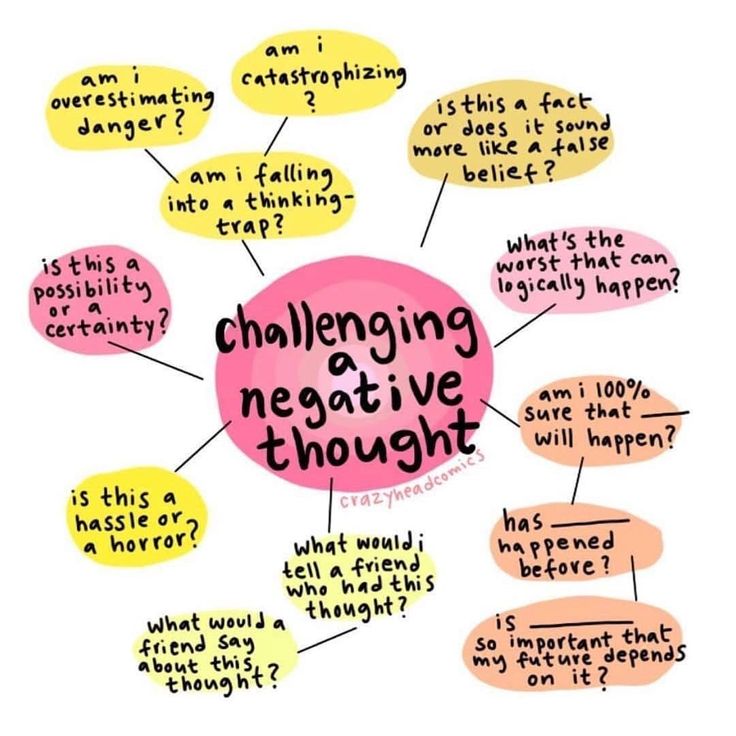 Therapists may teach parents how to use play to improve communication with their children.
Therapists may teach parents how to use play to improve communication with their children.
In this form of play therapy, the therapist also takes a more direct approach by working with both the child and the caregivers to teach the child how to cope well and achieve their defined goals. The therapist is doing more than just watching the child play.
Acceptance and commitment therapy (ACT)
ACT is a type of psychotherapy that includes behavioral analysis performed by a mental health clinician. While sometimes compared with CBT, ACT has its own specific approach. ACT is based on relational frame theory, which focuses on mental processes and human language.
In ACT, people are taught mindfulness skills and acceptance strategies with the goal of increasing psychological flexibility. Additionally, commitment and behavior change methods are used.
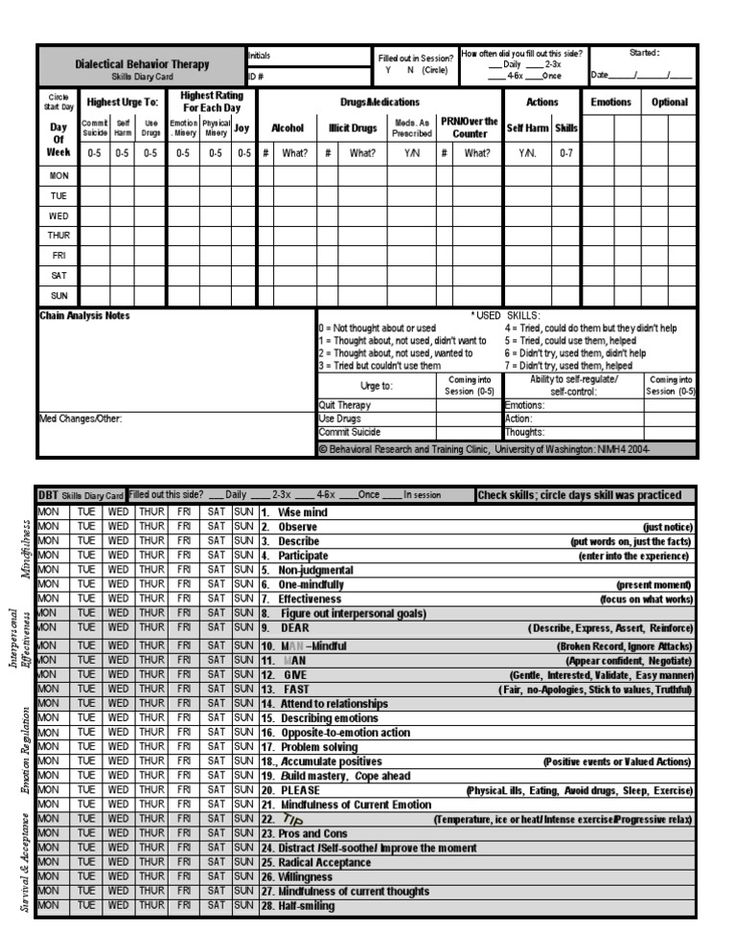
Dialectical behavioral therapy (DBT)
DBT was created by Dr. Marsha Linehan to help treat the symptoms of borderline personality disorder (BPD), an emotional regulation disorder marked by suicidal behavior, depression, unstable personal relationships, and other symptoms.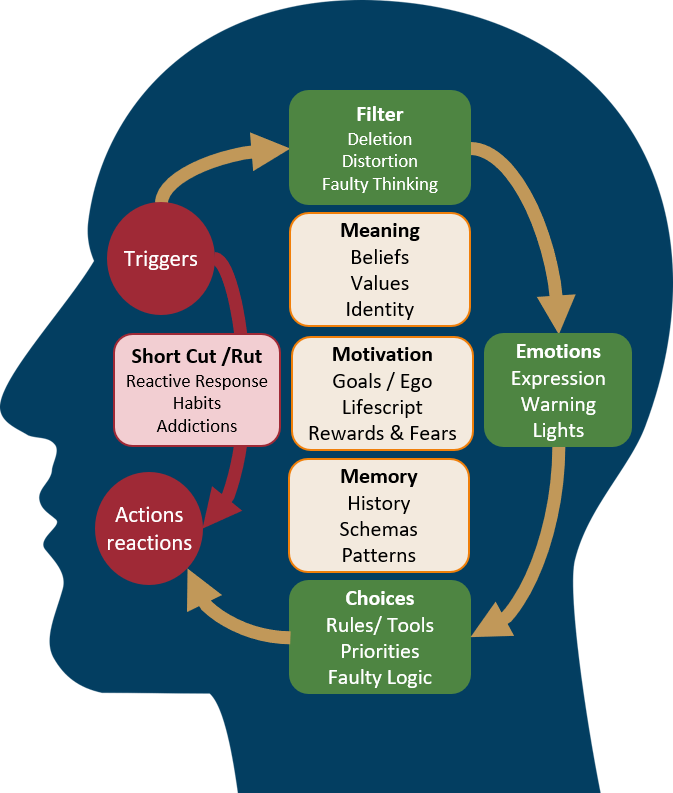
DBT can also be helpful for conditions other than BPD.
DBT consists of four elements, known as modules:
- core mindfulness
- interpersonal effectiveness, which is used to improve relationships with others and yourself
- emotional regulation
- distress tolerance
People receiving DBT are taught skills and coping strategies to help them lead healthier, happier lives.
Systematic desensitization
Systematic desensitization is a process that helps you to become less sensitive to certain triggers. It relies heavily on classical conditioning, a type of unconscious and automatic learning that creates behavior. It’s often used in the treatment of phobias.
During treatment, you’re taught to replace your fear responses with relaxation responses, which begins with learning relaxation and breathing techniques.
Once you’ve mastered these techniques, your therapist will have you face your fear or fears at slowly increasing levels while you use these techniques.
Aversion therapy
Aversion therapy is often used to treat disorders like substance use disorder and alcohol use disorder. It works by teaching people to associate a stimulus (something that triggers a response) that’s pleasant but unhealthy with an extremely unpleasant stimulus.
The unpleasant stimulus may be something that causes discomfort. For example, a therapist may teach you to associate alcohol with an unpleasant memory.
Behavioral therapy has successfully been used to treat a large number of conditions. It’s considered to be extremely effective.
About 75 percent of people who enter cognitive behavioral therapy experience some benefits from this treatment.
A 2012 study found that cognitive behavioral therapy is most effective when treating:
- anxiety disorders
- general stress
- bulimia
- anger-related disorders
- somatoform disorders, like somatic symptom disorder, in which bodily symptoms without an underlying physical cause are experienced
- depression
- substance use disorders
Studies have shown that play therapy is very effective in children ages 3 to 12 years.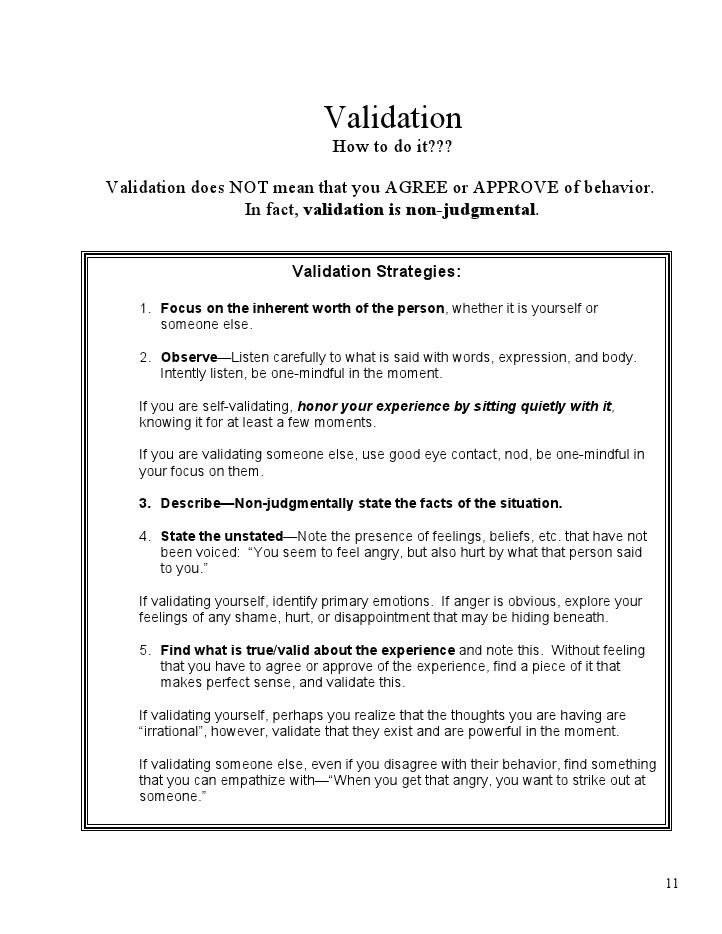 But this therapy is increasingly being used in people of all ages.
But this therapy is increasingly being used in people of all ages.
Applied behavioral therapy and play therapy are both used for children. Treatment involves teaching children different methods of responding to situations more positively.
A central part of this therapy is rewarding adaptive behaviors that benefit a child’s functioning and discourage maladaptive behaviors, or those that interfere with a child’s best possible functioning.
This therapy often requires multiple people in a child’s environment to be committed to the process, including parents, teachers, and other important figures.
It may take children some time to trust their counselor. This is to be expected.
With time, patience, and focus on building trust, a child may warm up to the point of being able to fully express themselves. This also is heavily dependent on the age of the child.
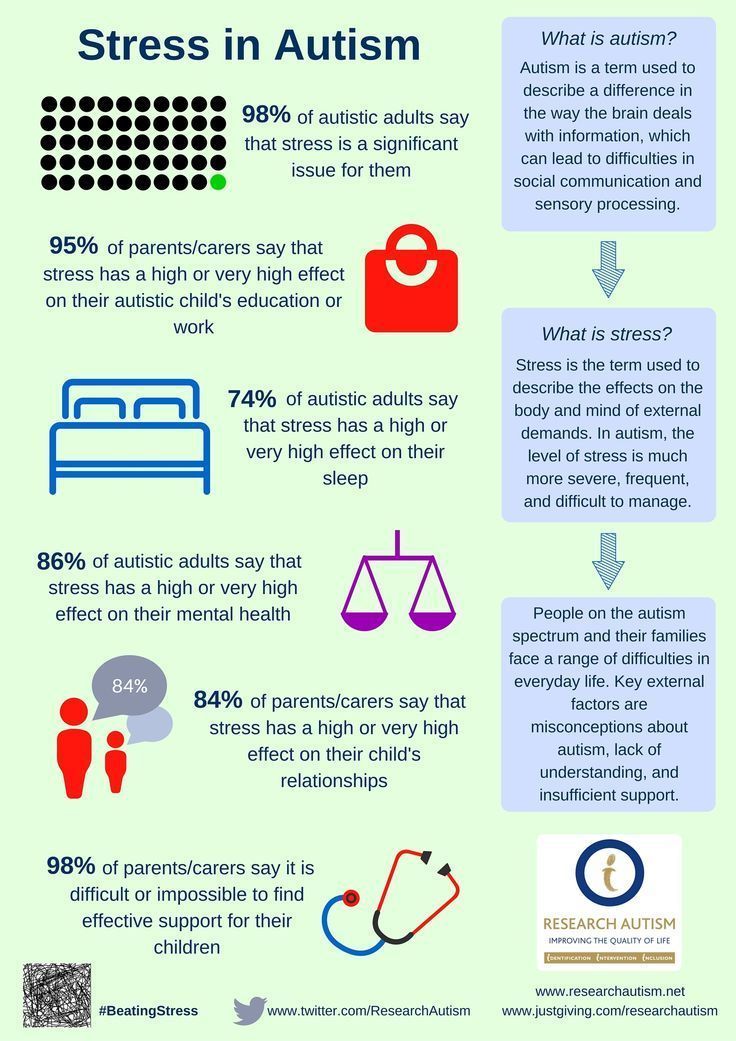
Autistic children with ADHD often benefit from behavioral therapy.
Finding a therapist can feel overwhelming, but there are many resources that can make it easier.
When finding a therapist or mental health professional, you can choose from:
- social workers
- faith-based counselors
- non-faith-based counselors
- psychologists
- psychiatrists
You should make sure that the therapist you choose has the necessary certifications and degrees. Some therapists will focus on treating certain conditions, like eating disorders or depression.
If you don’t know how to get started with finding a therapist, you can ask a general practitioner, a doctor who treats a broad range of conditions, for a recommendation. The general practitioner may recommend a psychiatrist if this is appropriate for you.
Psychiatrists are able to write prescriptions for medication if they think you might benefit from it. The Healthline FindCare tool can also provide options in your area if you need help finding a therapist.
Most insurance plans will cover therapy for mental health conditions. Some therapists offer grants or sliding-scale payment options for individuals from low-income households.
A therapist will ask you many detailed questions in order to accurately assess your concerns and formulate a specific treatment plan.
You’ll know you’ve found the right therapist when you feel comfortable talking with them and are experiencing the gains or improvements you’ve been looking for. You may have to meet with several therapists before you find the right one.
Cognitive Behavioral Therapy for Depression: How Does It Work?
Cognitive behavioral therapy (CBT) is a type of psychotherapy. This form of therapy modifies thought patterns to help change moods and behaviors.
It’s based on the idea that negative actions or feelings are the results of current distorted beliefs or thoughts, not unconscious forces from the past.
CBT is a blend of cognitive therapy and behavioral therapy. Cognitive therapy focuses on your moods and thoughts. Behavioral therapy specifically targets actions and behaviors.
A therapist practicing the combined approach of CBT works with you in an agreed-upon location, offering guidance and direction.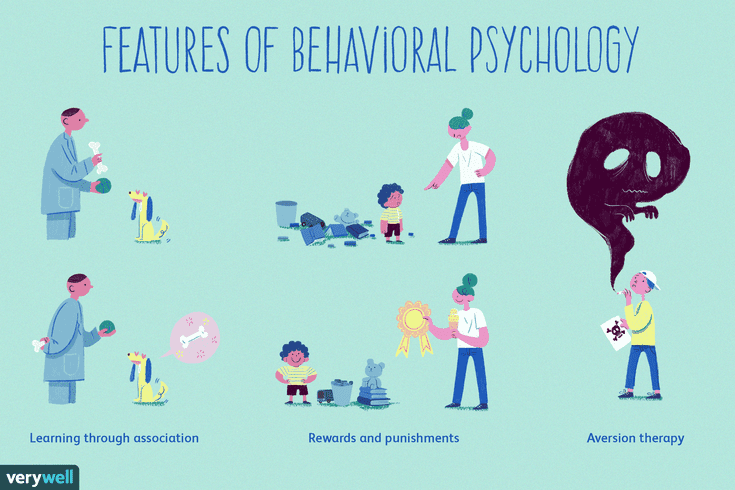 You and your therapist may work to identify specific negative thought patterns and behavioral responses to challenging or stressful situations.
You and your therapist may work to identify specific negative thought patterns and behavioral responses to challenging or stressful situations.
This type of therapy is commonly used for a wide range of mental health challenges and diagnoses, including:
- depression
- anxiety
- eating disorders
- post-traumatic stress disorder (PTSD)
- insomnia
- obsessive-compulsive disorder (OCD)
- bipolar disorder
- phobias
- chronic pain
- panic attacks
Treatment typically involves developing more balanced and constructive ways to respond to stressors. Ideally, these new responses will help you cope with or recover from challenging mental health conditions or unwanted behaviors.
The principles of CBT can be applied outside of the therapist’s office, providing you with coping tools to help you through life’s challenges. CBT teaches you to become aware of and adjust negative patterns, which can help you reframe your thinking during moments of heightened anxiety or panic.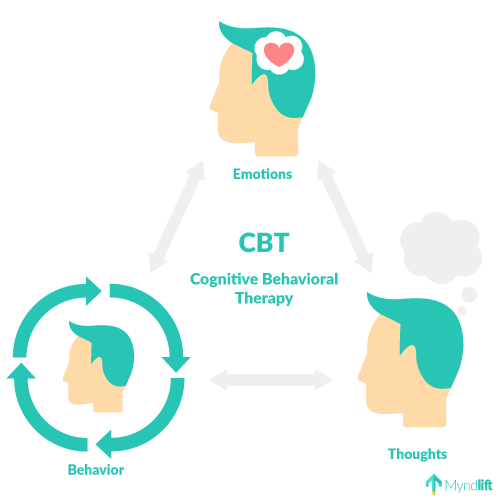
It can also provide new coping skills, like meditation or journaling, for those struggling with a substance use disorder or depression.
CBT is a more short-term approach than psychoanalysis and psychodynamic therapies. Other types of therapies may require several years for discovery and treatment.
CBT often requires only up to 20 sessions, according to the National Health Services, but you can continue seeing your therapist for as long as you need. Every situation is unique, so how long you pursue treatment is up to you and your therapist.
CBT sessions provide opportunities to identify current life situations that may be causing or contributing to your mental health conditions, like anxiety or depression. CBT allows you and your therapist to identify patterns of thinking or distorted perceptions that are no longer serving you.
This is different from psychoanalysis. This type of therapy involves working backward through your life history to discover an unconscious source of the problems you’re facing.
You may be asked to keep a journal as part of CBT. The journal provides a place for you to record life events and your reactions. Your therapist can help you break down reactions and thought patterns into several categories of self-defeating thought (also known as cognitive distortions).
These may include:
- all-or-nothing thinking: viewing the world in absolute, black-and-white terms
- disqualifying the positive: rejecting positive experiences by insisting they “don’t count” for some reason
- automatic negative reactions: having habitual, scolding thoughts
- magnifying or minimizing the importance of an event: making a bigger deal about a specific event or moment
- overgeneralization: drawing overly broad conclusions from a single event
- personalization: taking things too personally or feeling actions are specifically directed at you
- mental filter: picking out a single negative detail and dwelling on it exclusively so that the vision of reality becomes darkened
You and your therapist can also use the journal to help replace negative thought patterns or perceptions with more constructive ones. This can be done through a series of well-practiced techniques, such as:
This can be done through a series of well-practiced techniques, such as:
- learning to manage and modify distorted thoughts and reactions
- learning to accurately and comprehensively assess external situations and reactions or emotional behavior
- practicing self-talk that is accurate and balanced
- using self-evaluation to reflect and respond appropriately
You can practice these coping methods on your own or with your therapist. Alternately, you can practice them in controlled settings in which you’re confronted with challenges. You can use these settings to build on your ability to respond successfully.
If you’re someone who struggles with depression, your therapist may use CBT techniques to help you uncover unhealthy patterns of thought and identify how they may be affecting:
- your mood
- beliefs about yourself
- your overall outlook on life
You may also be assigned “homework” so that you can practice replacing negative thoughts with more positive thoughts in real time.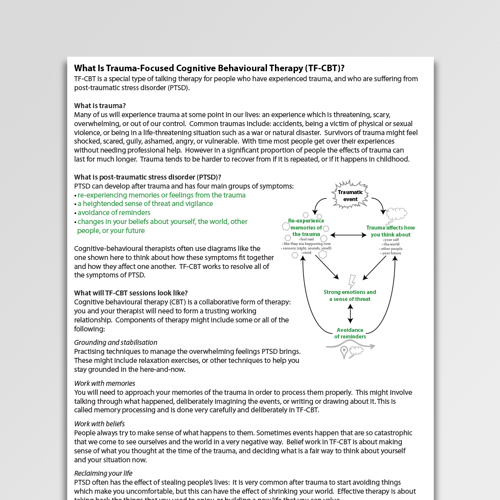
CBT has been proven to be effective in treating mild to moderate levels of depression. In some cases, it can be combined with other treatments, like antidepressants or other medications, to treat depression.
Cognitive behavioral therapy is widely used to treat an array of mental health conditions in children, adolescents, and adults. These may include:
- antisocial behaviors (including lying, stealing, and hurting animals or other people)
- anxiety
- attention deficit hyperactivity disorder
- bipolar disorder
- conduct disorder
- depression
- eating disorders such as binge eating, anorexia, and bulimia
- general stress
- personality disorders
- phobias
- schizophrenia
- sexual disorders
- insomnia
- social skill problems
- substance use disorder
In certain cases, cognitive behavioral therapy may be combined with other treatments to help with depression.
There is little long-term emotional risk associated with CBT. But exploring painful feelings and experiences can be stressful. Treatment may involve facing situations you’d otherwise avoid.
But exploring painful feelings and experiences can be stressful. Treatment may involve facing situations you’d otherwise avoid.
For instance, you may be asked to spend time in public places if you have a fear of crowds. Alternately, you may need to confront difficult sources of trauma, like the death of a loved one.
These scenarios can provide opportunities to practice altered responses to stressful or adverse situations. The eventual goal of therapy is to teach you how to deal with anxiety and stress in a safe and constructive manner.
“There is a massive tidal wave of evidence for cognitive behavioral therapy that suggests it is very effective at treating certain problems,” Simon Rego, PsyD of Montefiore Medical Center in New York, told Healthline. “The breadth of evidence isn’t as extensive for other forms of psychotherapy.”
That’s not to say other therapies aren’t equally effective and beneficial. “They just don’t fit as neatly into anything that can be studied,” Rego says.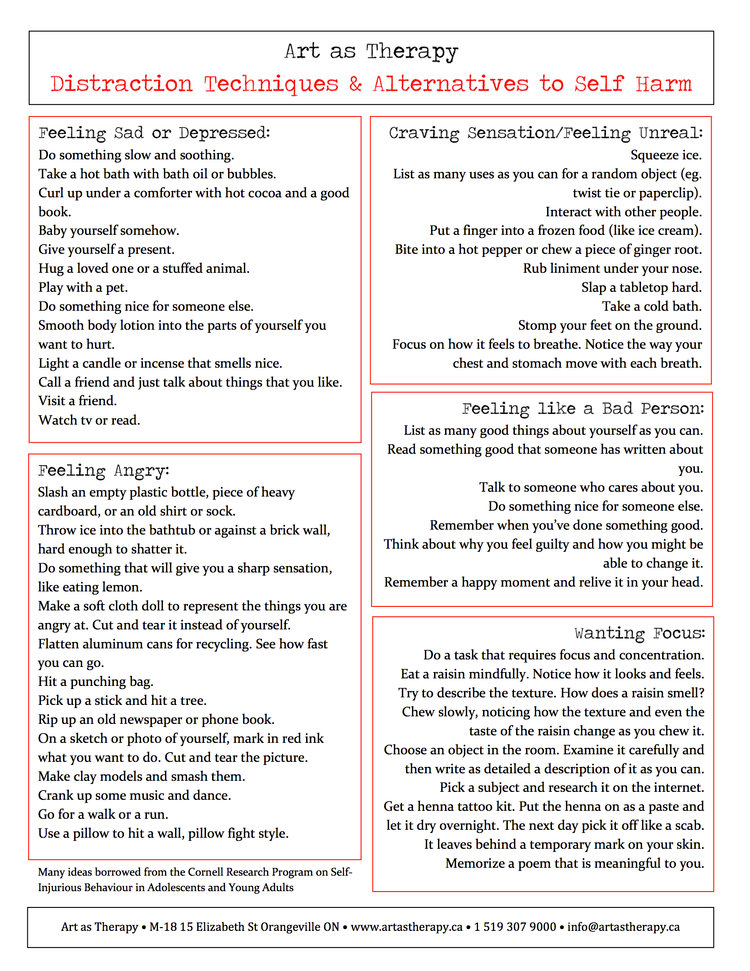 “More evidence-based studies have been conducted on the results of cognitive behavioral therapy than any other kind.”
“More evidence-based studies have been conducted on the results of cognitive behavioral therapy than any other kind.”
Online therapy for CBT
If you feel that you or a loved one could benefit from CBT, there are several telehealth platforms that can virtually connect you with a trained therapist. Here are some to consider:
- TalkSpace. After taking an initial assessment and choosing your subscription plan, you’ll be connected with someone from their network of over 3,000 licensed therapists.
- BetterHelp. This telehealth company has one of the largest networks of licensed therapists and offers individual, couples, and family counseling.
- Amwell. Along with talk therapy, Amwell can also connect you with online psychiatrists who can prescribe medications.
- 7 Cups. This telehealth network is significantly less expensive than other online therapy platforms. Plus, 7 Cups offers emotional support and access to speak to a trained volunteer (not a licensed counselor) at no charge.
How can I find a CBT therapist?
If you think CBT may be a fit for you, there are several ways to find a therapist.
You can:
- talk with your doctor
- search the directory of certified therapists
- reach out to an online therapy program
- contact your health insurance company to see if your plan covers therapy visits
What can I expect from CBT?
Your CBT experience will be unique based on your situation but know that there is no right or wrong way to experience therapy.
Your therapist will take time to get to know you, so be prepared to discuss:
- what brought you to therapy
- your mental health history
- current circumstances
CBT has been found to be effective in treating those with mild to moderate depression. It has also been proven effective when combined with other treatment options, like antidepressants or other medications.
Remember that change is often gradual, requiring a time commitment and the willingness to be open to the experience.
Cognitive behavioral therapy (CBT) is a type of psychotherapy that helps you recognize and replace negative or unhelpful thought and behavior patterns. It can be a highly rewarding and effective form of mental health support for those affected by anxiety, depression, OCD, insomnia, substance use disorder, and more.
CBT requires a willingness to be open to change, along with a time commitment to do the work with your trusted therapist.
The goal of CBT is to help you develop the skills to help deal with difficulties on your own, at the moment when they come up, ideally giving you tools that last a lifetime.
Behavioral Therapy (BBT) - Psychologos
The term behavioral therapy encompasses a range of different therapeutic methods based on the principles of conditioning and learning described in Chapter 7. Behavioral therapists believe that maladapted behavior is made up of a number of learned ways cope with stress and that some methods developed in learning experiments can help to replace maladapted responses with more appropriate ones. While psychoanalysis seeks to understand how conflict from the past affects an individual's behavior, behavioral therapy mostly addresses behavior itself.
While psychoanalysis seeks to understand how conflict from the past affects an individual's behavior, behavioral therapy mostly addresses behavior itself.
Behavioral therapists point out that while insight is a worthwhile goal, it does not guarantee behavior change. It often happens that a person understands why he behaves the way he does, but he cannot behave otherwise. If, for example, you are very afraid of speaking in front of the whole class, then you may be able to trace how this fear arose in the past (father criticized your opinions whenever you expressed them; mother set herself the task of correcting your grammar; you had little experience in public speaking in high school because you were afraid to argue with your older brother who was the captain of a sports team), but understanding the reasons for your fears does not necessarily make it easier for you to participate in class discussions.
Unlike psychodynamic therapy, which aims to change certain aspects of the personality, behavioral therapy seeks to change maladapted behavior that manifests itself in specific situations.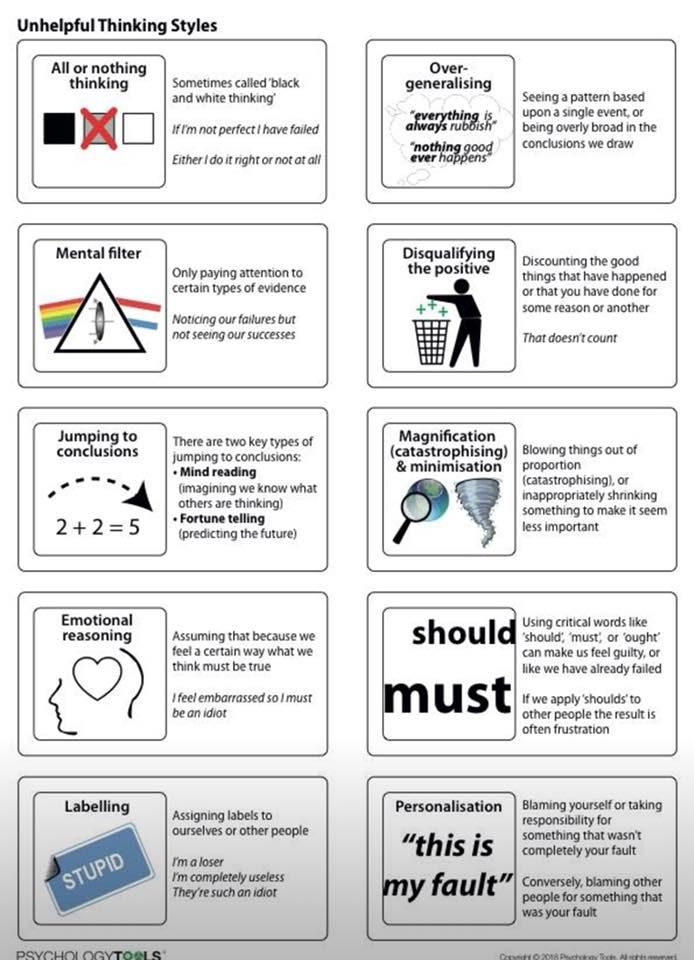 In addition, behavioral therapists are more interested than psychoanalysts in experimental evaluations of their methods. At the beginning of the session, the behavioral therapist listens carefully to the patient's presentation of their problem. What exactly does the client want to change? Is he afraid of flying or public speaking? Does he have an eating problem? Feelings of inadequacy or helplessness? Inability to focus and finish things? The first step is to clearly define the problem and break it down into a set of specific therapeutic goals. If, for example, the client complains of a general feeling of inadequacy, the therapist should try to get the client to describe these feelings more specifically, specifying in what situations they arise and with what behavior they are associated.
In addition, behavioral therapists are more interested than psychoanalysts in experimental evaluations of their methods. At the beginning of the session, the behavioral therapist listens carefully to the patient's presentation of their problem. What exactly does the client want to change? Is he afraid of flying or public speaking? Does he have an eating problem? Feelings of inadequacy or helplessness? Inability to focus and finish things? The first step is to clearly define the problem and break it down into a set of specific therapeutic goals. If, for example, the client complains of a general feeling of inadequacy, the therapist should try to get the client to describe these feelings more specifically, specifying in what situations they arise and with what behavior they are associated.
What exactly is he unable to do? Speak up in class or in social situations? Do the task on time? Control your food intake? Once the behaviors to be corrected have been identified, the therapist and client develop a treatment program that includes some of the procedures that we will describe. The therapist chooses a treatment method that is appropriate for a particular problem.
The therapist chooses a treatment method that is appropriate for a particular problem.
Systematic desensitization and enactment in vivo
Systematic desensitization and enactment in vivo (a technique similar to systematic desensitization except that the client is actually placed in the situation) can be considered a process of deconditioning or counterconditioning (Wolpe, 1958). These procedures are very successful in removing fears and phobias. The principle of such treatment is to develop a replacement response that is incompatible with anxiety, namely, the reaction of relaxation, or relaxation. You can't feel relieved and anxious at the same time. First, the client is taught deep relaxation. To do this, you can gradually relax various muscles, starting, for example, from the feet and ankles and moving up the body to the neck and facial muscles. A person learns how muscles feel when they are really relaxed, and how to distinguish between different degrees of their tension. To help people who cannot relax in any way, tranquilizers and hypnosis are sometimes used.
To help people who cannot relax in any way, tranquilizers and hypnosis are sometimes used.
The next step is to compile a hierarchy of anxiety situations. Situations are arranged in order from the least disturbing to the most frightening. In systematic desensitization, the client is then asked to relax and imagine each situation in this hierarchy, starting with the least disturbing. In vivo enactment requires the client to actually experience anxiety situations. In vivo enactment is a more effective procedure than just imagining troubling situations, but some clients need to start with imagining and gradually move on to experiencing fearful situations.
Let's take an example to understand these procedures. Suppose the client is a woman who has a phobia of snakes. Her phobia is so strong that for fear of meeting a snake, she is afraid to go out into her own backyard, not to mention a walk in the countryside or a vacation in the forest. Her hierarchy of anxiety should start with a picture of a snake in the book. Somewhere in the middle of the hierarchical list would be looking at a snake in a terrarium at a zoo. At the top of this list will be the actual handling of a live snake. Once this woman has learned to relax and her hierarchy is in place, the therapist should begin to move her down the list. In systematic desensitization, she should sit with her eyes closed in a comfortable chair while the therapist describes the least disturbing situation to her. If she can imagine the situation herself without any increase in muscle tension, the therapist moves on to the next item on the list. If the woman reports any anxiety while visualizing the scene, she concentrates on relaxing; the same scene is rendered until the anxiety is neutralized. This process is repeated in a number of sessions until the situation that initially caused the most anxiety becomes only relaxing. It can then be said that this woman has been systematically desensitized to anxiety-provoking situations by reinforcing an incompatible response—relaxation.
Somewhere in the middle of the hierarchical list would be looking at a snake in a terrarium at a zoo. At the top of this list will be the actual handling of a live snake. Once this woman has learned to relax and her hierarchy is in place, the therapist should begin to move her down the list. In systematic desensitization, she should sit with her eyes closed in a comfortable chair while the therapist describes the least disturbing situation to her. If she can imagine the situation herself without any increase in muscle tension, the therapist moves on to the next item on the list. If the woman reports any anxiety while visualizing the scene, she concentrates on relaxing; the same scene is rendered until the anxiety is neutralized. This process is repeated in a number of sessions until the situation that initially caused the most anxiety becomes only relaxing. It can then be said that this woman has been systematically desensitized to anxiety-provoking situations by reinforcing an incompatible response—relaxation.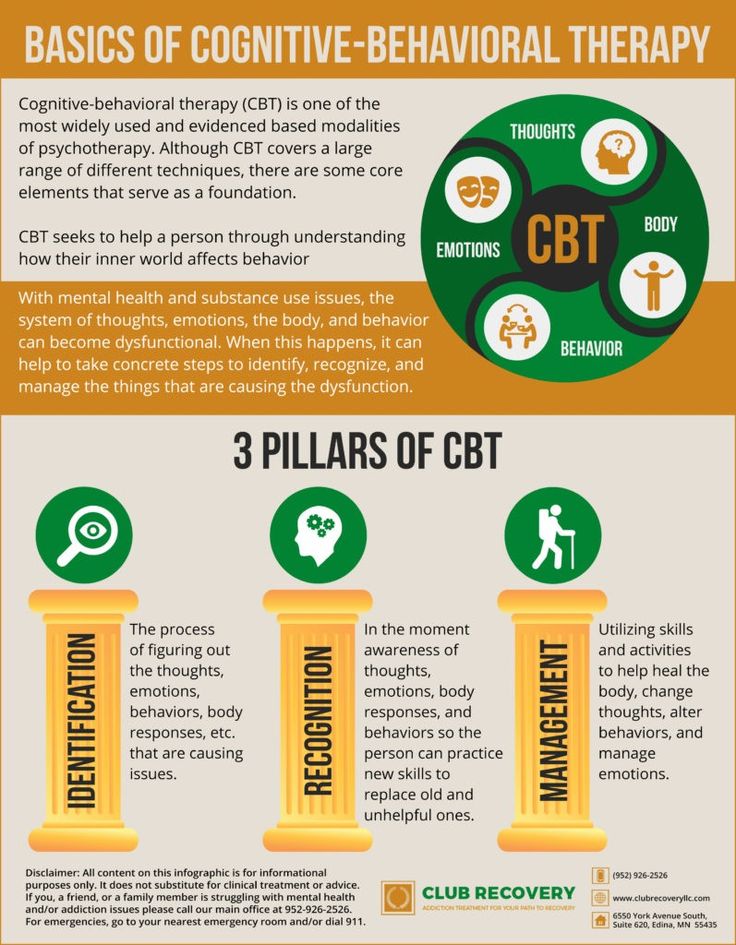
During the in vivo enactment, the woman needs to actually experience each of the situations on her list, starting with the least frightening, and under the guidance of a therapist. Before this woman herself can handle the snake without fear, the therapist must hold the snake in the presence of the client and express a lack of concern. In time, the woman will be able to hold the snake herself, let it crawl on her own, controlling her anxiety through relaxation. This type of in vivo enactment therapy has proven to be very effective in the treatment of phobias (Bandura, Blanchard & Rifter, 1969).
In specific cases, the process of learning and enactment in vivo can proceed not as counterconditioning, but as the extinction of the reaction. If a person exposes himself to a fearful stimulus and finds that nothing bad is happening, the conditioned fear response fades. Relaxation can simply serve as a way to encourage a person to face what they are afraid of. Indeed, if a phobic individual can force himself to remain for a long time in a situation that causes fear (for example, if a person with claustrophobia sits in a closet for hours or a person who is afraid of getting infected walks for several days without washing), the initial horror gradually subsides. This procedure of exposing a person to the most frightening situation or object for a long time without being able to get out of it is called drowning (flooding). She has been particularly successful in treating agoraphobia (fear of leaving a safe place such as one's home) and obsessive-compulsive disorder (Steketee & White, 1990; Emmelkamp & Kuipus, 1979).
This procedure of exposing a person to the most frightening situation or object for a long time without being able to get out of it is called drowning (flooding). She has been particularly successful in treating agoraphobia (fear of leaving a safe place such as one's home) and obsessive-compulsive disorder (Steketee & White, 1990; Emmelkamp & Kuipus, 1979).
Selective Reinforcement
Whether learning is counter-conditioning or extinction, systematic in vivo desensitization and enactment are based on the principles of classical conditioning. Selective reinforcement based on the principles of operant conditioning (see Chapter 7) has also proved to be an effective method of behavior modification, especially in children.
This procedure can be illustrated with a 3rd grade student who was inattentive in school, refused to complete assignments or participate in class, and spent most of her time daydreaming. In addition, she had poor social skills and few friends. Reinforced behaviors were defined as "set" and included paying attention to school work and teacher directions, completing reading assignments, and participating in class discussions. Reinforcement consisted of peas, which she could then exchange for privileges she especially valued, such as the ability to be first in line (3 peas) or stay after school to help a teacher with a special project (9peas). Whenever the teacher saw that this student was engaging in a "set" behavior, she would put one pea in the jar.
Reinforcement consisted of peas, which she could then exchange for privileges she especially valued, such as the ability to be first in line (3 peas) or stay after school to help a teacher with a special project (9peas). Whenever the teacher saw that this student was engaging in a "set" behavior, she would put one pea in the jar.
In the first 3 months of treatment, this girl completed 12 units of work compared to 0 units in the 3 months prior to starting the reinforcement regimen. In the final 3 months, she completed 36 units and did just as well as other children. The next year showed that the girl continued to do well in her studies. She also improved her social skills and was noticed by other children (Walker et al., 1981). This is a common result: improving behavior in one area often entails additional benefits (Kazdin, 1982).
Reinforcement of desirable reactions may be accompanied by extinction of undesirable ones. For example, if a little boy usually screams to get his mother's attention, then she may ignore him every time he does so, and reinforce him with attention only when he approaches her and addresses her in a normal tone.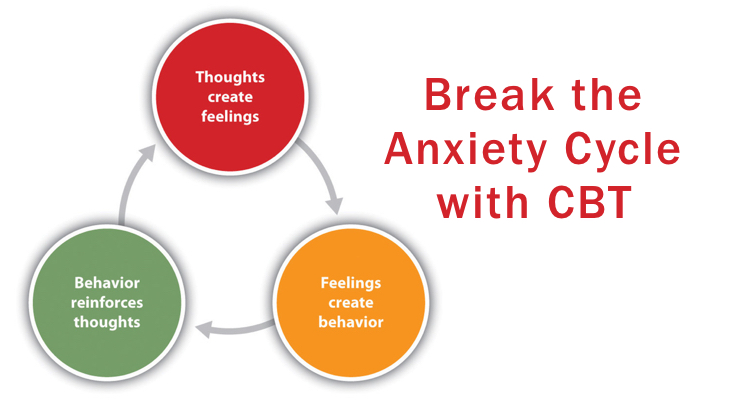
Operant conditioning procedures that reward desirable responses and not reward undesirable responses have been successfully applied to a wide variety of childhood problems, including bedwetting, aggressiveness, temper tantrums, classroom misbehavior, poor school performance, and social withdrawal. Similar procedures have been applied to children with autism, adults with developmental delays, and patients with severe psychiatric disorders.
A token economy has been introduced in a number of psychiatric wards that housed chronic patients with severe disabilities to encourage socially acceptable behaviour. Tokens (which could be exchanged for food and privileges such as watching TV) were given out in exchange for properly wearing clothes, talking to other patients, stopping "psychotic speech", helping to clean the room, etc. Such programs have been successful in improving behavior as well. patients, and for the overall functioning of the wards (Paul & Lentz, 1977).
Modeling
Fig. 16.3. Treating snake phobia. Mean number of snake approach responses before and after being treated with various behavioral therapies (adapted from: Bandura, Blanchard & Ritter, 1969).
Another effective means of correcting behavior, which we have already briefly mentioned, is modeling. Modeling uses learning through observation. Because observation of patterns is the primary mode of human learning, by observing people exhibiting adaptive behavior, people with maladapted behavior should learn better strategies for coping with situations. Observing the model's behavior (live or on video) proved to be an effective means of reducing fears and learning new skills. On fig. Figure 16.3 shows the results of a study in which modeling was combined with gradual training in the treatment of snake phobia.
Fig. 16.3. Treating snake phobia. Mean number of snake approach responses before and after being treated with various behavioral therapies (adapted from: Bandura, Blanchard & Ritter, 1969).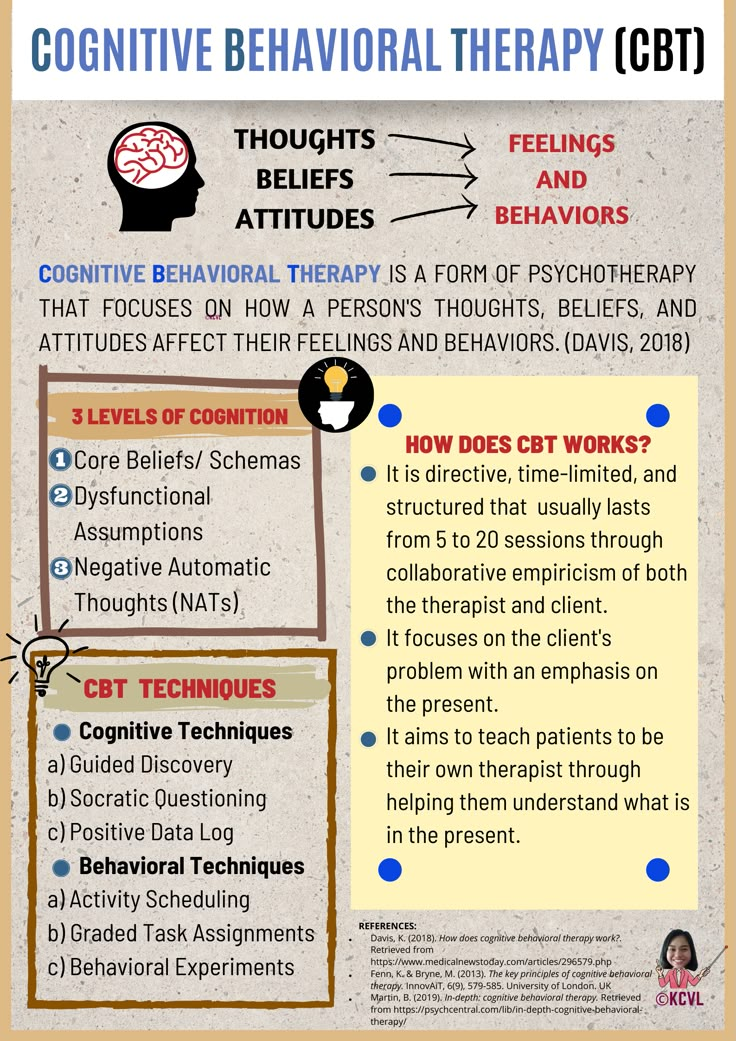
Simulation helps to successfully cope with fear and anxiety, because it allows a person to observe someone else who is in a disturbing situation without harming himself. Watching videos of models enjoying visiting the dentist or undergoing various hospital procedures has been successful in helping both children and adults overcome the fear associated with such experiences (Melamed & Siegel, 1975; Shaw & Thoresen, 1974).
Behavior rehearsal
In psychotherapy sessions, simulation is often combined with role play or behavior rehearsal. With the help of a psychotherapist, a person rehearses or trains more adaptive behaviors. The following excerpt shows how a therapist helps a young man overcome his anxiety about asking women out. The young man pretends to talk to a woman on the phone and at the end asks her for a date.
Client: Um, I was wondering if you'd like to meet up on a Saturday night or something, what do you say?
Therapist: Okay, that's a start. Can you think of another way to ask her to come over that's a little more positive and trusting? For example: "There is a concert on Saturday night that I want to go to, and I would really like to take you with me if you are free."
Can you think of another way to ask her to come over that's a little more positive and trusting? For example: "There is a concert on Saturday night that I want to go to, and I would really like to take you with me if you are free."
C: Awesome!
T: Okay, try it.
K: Um, I have two tickets to the concert on Saturday night. If you have nothing to do, maybe you would like to come with me?
T: It's already better. Try again, but now try to express that you really really want her to agree.
K: I have two tickets for the Saturday concert. And it would be great if you would come with me if you are not busy.
T: Excellent! Just practice a couple more times and you're ready to pick up the phone.
This example illustrates a behavior rehearsal in one type of confidence training. Like the young man in this example, many people find it difficult to ask for what they want or deny others the opportunity to use it.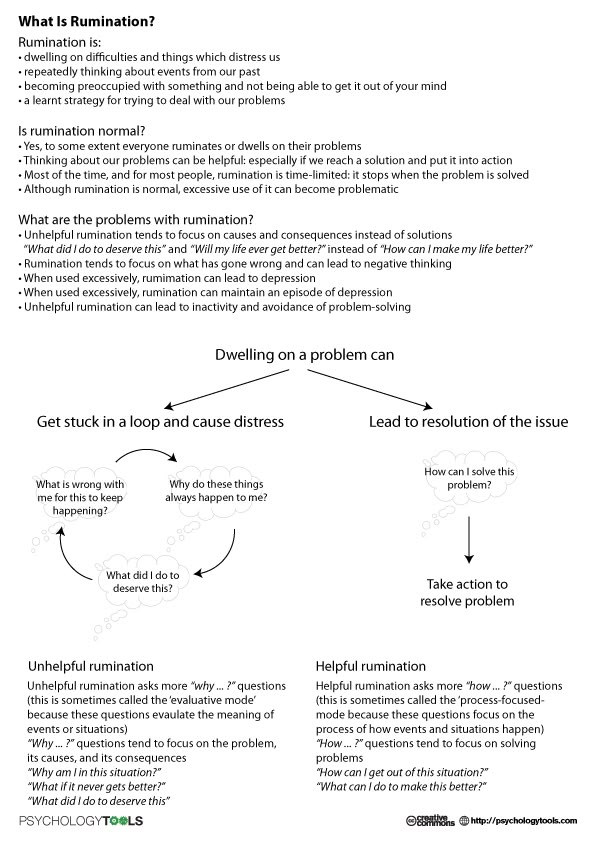 By practicing assertive responses (first in role play with a therapist and then in real life situations), the individual not only reduces anxiety, but also develops more successful coping strategies. The therapist finds out in which situations the person behaves passively, and then helps him to imagine and put into practice confident reactions that can lead to success. In a number of therapeutic sessions, the following situations can be played:
By practicing assertive responses (first in role play with a therapist and then in real life situations), the individual not only reduces anxiety, but also develops more successful coping strategies. The therapist finds out in which situations the person behaves passively, and then helps him to imagine and put into practice confident reactions that can lead to success. In a number of therapeutic sessions, the following situations can be played:
- Someone gets in line ahead of you.
- A friend asks you to do something you don't want to.
- Your boss criticizes you unfairly.
- You are returning a defective purchase to the store.
- At the cinema, people in the back rows disturb you by talking noisily,
- The mechanic did a poor job of repairing your car.
Most people do not like to face such situations, but some are so afraid to show their confidence that they do not say anything and instead create feelings of resentment and inadequacy.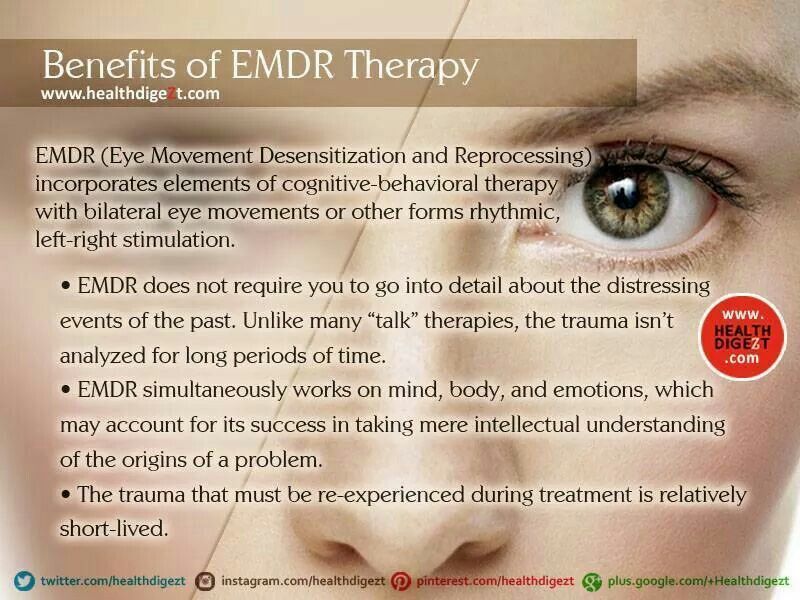 In confidence training, the client rehearses successful therapist actions that can be applied in such situations, and gradually tries them out in real life. The therapist tries to teach the client to express his needs directly and effectively, but without others seeing them as hostile and threatening (Table 16.2).
In confidence training, the client rehearses successful therapist actions that can be applied in such situations, and gradually tries them out in real life. The therapist tries to teach the client to express his needs directly and effectively, but without others seeing them as hostile and threatening (Table 16.2).
Table 16.2. Some elements of confident reactions
--------
- Decide what you want to say and stand your ground and don't let others disagree with you. For example, when a salesperson says you can't return a defective item, keep saying "It's defective and I want to return it" until he agrees to pick it up or calls a manager to whom you'll say "It's defective, and I want to return it" until you get your money back.
- Demand not global, but small changes in the situation or in the behavior of another person. For example, don't say, "I want you to love me more," but say, "I want you to listen when I talk."
- When discussing a difficult situation with another person, use phrases beginning with "I" instead of accusatory phrases.
 Here are 4 fragments for sayings with "I":
Here are 4 fragments for sayings with "I":
- I think...
- If (when) you...
- Because...
- What I want...
For example, "I get mad when you don't show up for a meeting because I'm wasting my time. What I want is for you to call me and cancel an appointment when you feel like you can't come."
-------
Self-Regulation
Since the client and therapist typically meet no more than once a week, the client must learn to control or regulate their behavior so that progress occurs outside of class hours. In addition, if a person feels responsible for improving his condition, he will better keep what he has gained. Self-regulation involves observing one's behavior and applying various methods (self-reinforcement, self-punishment, control of stimulus conditions, development of incompatible reactions) in order to change maladapted behavior. A person monitors his behavior by keeping a careful record of the situations that caused his inappropriate behavior, and reactions that are incompatible with it. A person concerned about alcohol abuse registers situations in which he is most tempted by alcohol and tries to control them or develop reactions that are incompatible with drinking. A person who finds it difficult not to join colleagues for an afternoon cocktail can schedule lunch at the workplace, sparing himself the temptation to join the company by controlling his surroundings. If he tries to relax with alcohol upon returning home, this can be replaced by playing tennis or jogging around the block as a way to relieve tension. Both of these activities will be incompatible with drinking.
A person concerned about alcohol abuse registers situations in which he is most tempted by alcohol and tries to control them or develop reactions that are incompatible with drinking. A person who finds it difficult not to join colleagues for an afternoon cocktail can schedule lunch at the workplace, sparing himself the temptation to join the company by controlling his surroundings. If he tries to relax with alcohol upon returning home, this can be replaced by playing tennis or jogging around the block as a way to relieve tension. Both of these activities will be incompatible with drinking.
Self-reinforcement is rewarding oneself immediately after achieving a specific goal; the reward can be praise, watching your favorite TV program, calling a friend, your favorite food. Self-punishment is the creation of some unpleasant consequences for not achieving a goal, such as depriving yourself of something that you like (not watching your favorite TV program), or forcing yourself to do unpleasant work (cleaning the room). Depending on what behavior a person wants to change, different combinations of self-reinforcement, self-punishment, or control of stimuli and responses can be used. In table. 16.3 is a summary of the program for self-regulation of food intake.
Depending on what behavior a person wants to change, different combinations of self-reinforcement, self-punishment, or control of stimuli and responses can be used. In table. 16.3 is a summary of the program for self-regulation of food intake.
Table 16.3. Self-regulation of food intake
We remind you that self-restriction of food without consulting a nutritionist can have the most serious health consequences. In addition, reducing body weight is not the same as improving the figure. — Approx. ed.
Cognitive Behavioral Therapy
The behavioral therapy procedures we have discussed so far focus on direct behavior modification and do not pay attention to the individual's thought and reasoning processes. Initially, behavioral therapists ignored the importance of cognitive processes, preferring a strictly stimulus-reactive approach. They perceived any appeal to the beliefs and attitudes of a person as a return to unscientific introspection, which Watson opposed at the beginning of the 20th century. However, in response to evidence showing that cognitive factors (a person's thoughts, expectations, and interpretation of events) are important determinants of behavior, many behaviorists have turned their attention to cognition, incorporating it into their concepts of therapy. See →
However, in response to evidence showing that cognitive factors (a person's thoughts, expectations, and interpretation of events) are important determinants of behavior, many behaviorists have turned their attention to cognition, incorporating it into their concepts of therapy. See →
Cognitive Behavioral Therapy (CBT) or Cognitive Behavioral Psychotherapy (CBT)
FIND A PSYCHOLOGIST
We tell you how one of the most popular psychotherapy methods works, which allows you to correct thinking and emotional reactions.
alter
DIRECTION GUIDE
Contents
Behaviorism and cognitivism
Basic concepts
Techniques and exercises
When will CBT help?
Course duration
Evidence-based medicine and CBT
Medical therapy and CBT
Case studies
What to read
What is CBT?
Cognitive Behavioral Therapy (or CBT) is a technique that highlights a person's unconscious motivations, transfers them to a conscious level, helps to change beliefs and behavior that cause neurotic and other pathological conditions.
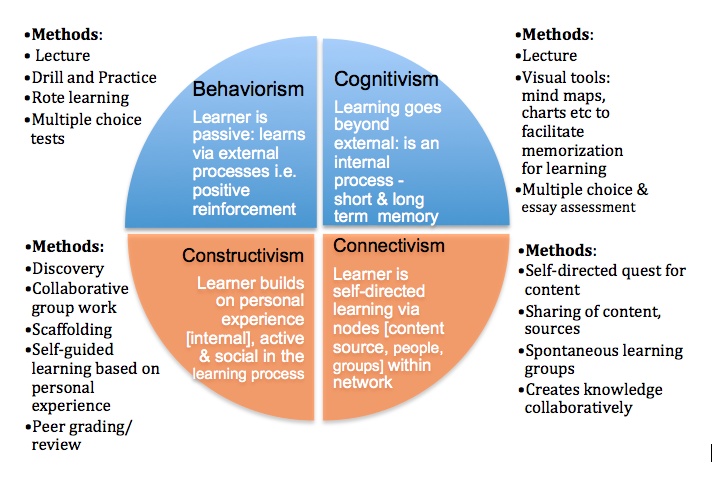
From the name it is clear that CBT combines two scientific psychological approaches: cognitive and behavioral (behavioristic). The first states that psychological problems and neuropsychiatric disorders are caused by thoughts and beliefs, stereotypes of thinking acquired during life. The second argues that human (as well as animal) behavior can be changed by encouraging desirable forms of action and not reinforcing undesirable behavior.
Behaviorism and cognitivism
The theory of behaviorism (from the English behavior - behavior) was developed in the early twentieth century. It considers behavior as a set of reactions (reflexes) to environmental stimuli. One of the basic concepts of behaviorism is positive and negative reinforcement. Positive reinforcement, or encouragement, is applied when the individual has done the right thing, and helps to reinforce the desired form of behavior. Negative reinforcement implies a negative reaction to the undesirable behavior of the trainee.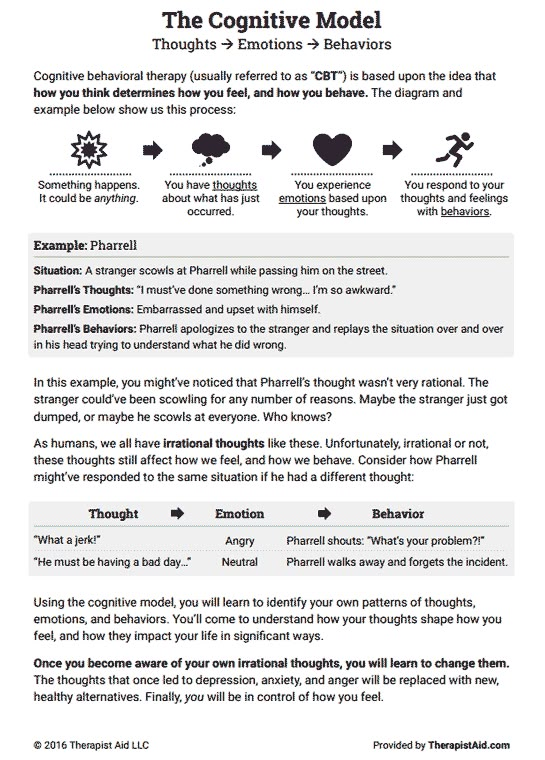 As a rule, the first form of reinforcement is used in CBT: it works faster, clearly indicates what needs to be achieved.
As a rule, the first form of reinforcement is used in CBT: it works faster, clearly indicates what needs to be achieved.
Cognitivism is a scientific movement that originated in the 1960s. It focuses on mental processes: how people perceive, think, remember, learn, solve problems, where they direct their attention. Cognitions are any thoughts and ideas that become the fruits of our thinking. According to the cognitive approach, it is inefficient to work only with a person’s behavior to solve his psychological problems: first, you need to identify beliefs, ideas and thoughts that make him act destructively or feel discomfort, get rid of them, and only then work on the behavioral aspect.
“Cognitions are basically all mental processes, both adequate and dysfunctional. When children are born, they don't know anything about the world yet. Over time, they begin to encounter people and their ideas about the environment. Parents and society help them formulate both adequate and dysfunctional beliefs.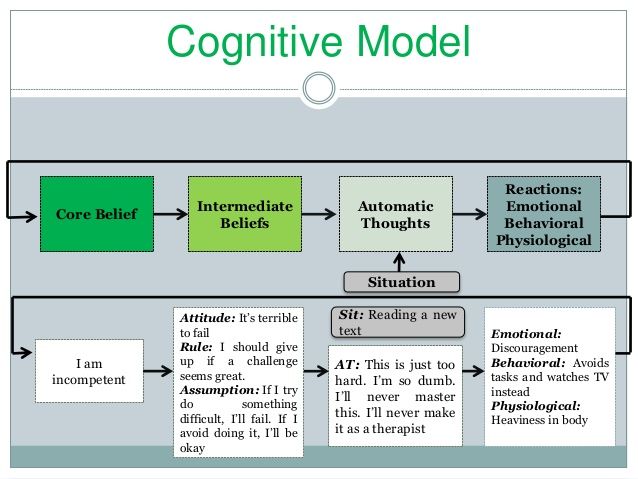 Dysfunctional and maladaptive views make it difficult to adequately assess life situations. Fears, complexes are formed, the child has a feeling that he is doing something wrong. It is this feeling that in the future leads to neurotic and other psychological problems.
Dysfunctional and maladaptive views make it difficult to adequately assess life situations. Fears, complexes are formed, the child has a feeling that he is doing something wrong. It is this feeling that in the future leads to neurotic and other psychological problems.
Anastasia Afanasyeva, Psychotherapist KPT:
Historically, the development of KPT is divided into 4 waves:
The first wave
(1910s-1950s)
Behavioral therapy
Second wave
(1960s)
Classical approach of CBT and rational-emotive psychotherapy
Third wave
(1990s)
Development of new currents within CBT: dialectical-behavioral psychotherapy, schema therapy, mindfulness therapy, acceptance and obligation therapy (ACT)
The fourth wave
(2010s)
The emerging stage associated with the use of modern technologies in therapy: augmented reality gadgets and software applications
In 1913, the American psychologist John Watson publishes the first articles on behaviorism. He urges his colleagues to focus exclusively on the study of human behavior, the study of the connection "external stimulus - external reaction (behavior)". Instead of analyzing the structural components of consciousness, behaviorists looked for reproducible connections between observed events, in particular between stimuli (environment) and responses (observed and measured reactions of people or animals to stimuli). Learning theories were the main model in the psychology of that time. Behaviorists have tried to formulate an explanation for how an organism establishes new connections between stimulus and response. Despite its early and sustained success, the behavioral approach placed many limitations on the therapy process.
He urges his colleagues to focus exclusively on the study of human behavior, the study of the connection "external stimulus - external reaction (behavior)". Instead of analyzing the structural components of consciousness, behaviorists looked for reproducible connections between observed events, in particular between stimuli (environment) and responses (observed and measured reactions of people or animals to stimuli). Learning theories were the main model in the psychology of that time. Behaviorists have tried to formulate an explanation for how an organism establishes new connections between stimulus and response. Despite its early and sustained success, the behavioral approach placed many limitations on the therapy process.
In 1955, the founder of rational-emotional psychotherapy, Albert Ellis, announced the influence of our thoughts and ideas (cognitions) on mental processes. His colleague Aaron Beck begins to study the field of knowledge. After evaluating the results of various methods of therapy, he comes to the conclusion that our emotions and behavior depend on the way we think.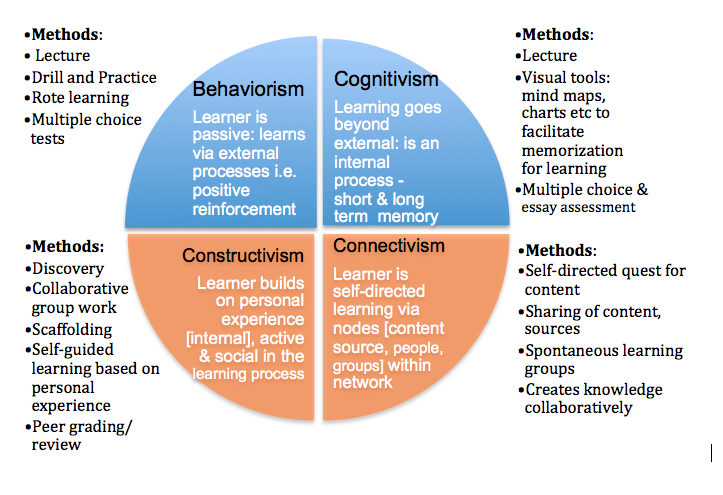
Despite attempts by behavioral therapists to maintain their position in the late 1950s and early 1960s, the ideas of cognitivism became increasingly influential. Publication of the book by A.T. Beck on Cognitive Therapy for Depression (Beck et al., 1979), as well as studies showing that cognitive therapy treats depression as effectively as antidepressants (Rush, Beck, Kovacs & Hollon, 1977), changed psychotherapy forever. In subsequent years, behavioral and cognitive therapy developed together and influenced each other so strongly that they eventually merged into a single cognitive-behavioral approach.
Historical reference
Basic concepts: automatic thoughts, cognitive distortions
Search and awareness automatic thoughts - the basis of the CBT method. About 20 thousand of such quick thoughts arise in our head per day, which are a response to what is happening to us. They are always appreciated. Evolutionarily automatic thoughts are necessary so that we can quickly respond to changes in the environment.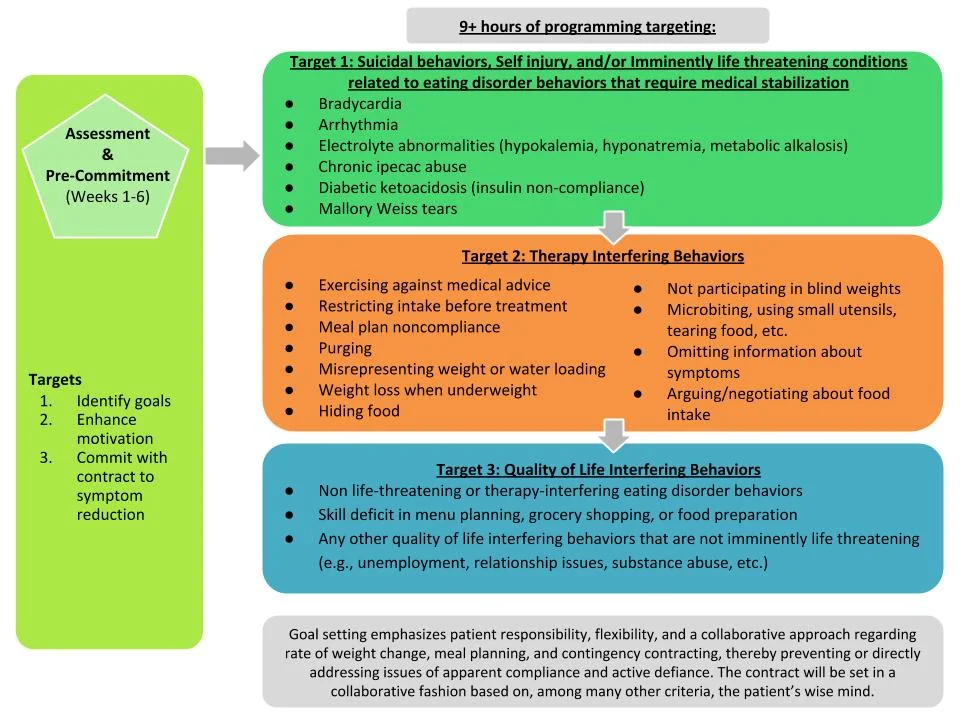.jpg) Most of them we do not have time to realize. These thoughts trigger our emotional response. In order to understand why our state has changed (anxiety, fear appeared, mood fell), it is necessary to identify what kind of thought caused this change. CBT suggests looking for quick thoughts in order to process them and translate your judgments into a rational channel.
Most of them we do not have time to realize. These thoughts trigger our emotional response. In order to understand why our state has changed (anxiety, fear appeared, mood fell), it is necessary to identify what kind of thought caused this change. CBT suggests looking for quick thoughts in order to process them and translate your judgments into a rational channel.
“There is always a situation that triggers a state change. For example, a person is walking in the dark and hears something rustling in the bushes. He becomes anxious. Most likely, the thought flashed that there was a danger nearby. In response to this thought and feeling of anxiety, the person decides to leave quickly. However, a quick thought and a reaction to it are not always rational. For example, you are doing a work task and realize that you do not have time to complete it on time. A neurotic person may have automatic thoughts: I am not responsible enough, I will be fired. The emotional response to them is anxiety, fear.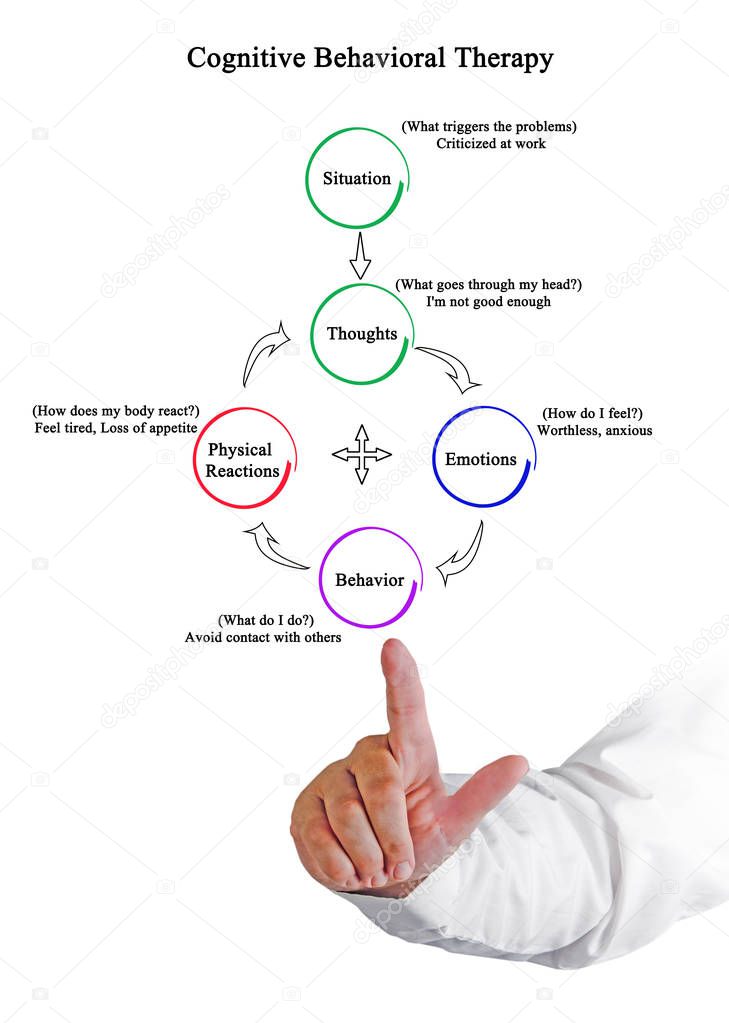 Although if you think rationally, it is unlikely that one missed deadline will negatively affect your entire career.
Although if you think rationally, it is unlikely that one missed deadline will negatively affect your entire career.
Anastasia Afanasyeva, psychotherapist CBT:
Cognitive Behavioral Therapy works on cognitive distortions (or errors) that arise from automatic thoughts. Cognitive distortions are erroneous conclusions, irrational ideas that ultimately lead a person to psychological problems. There are over 100 types of cognitive distortions. Here are just a few examples:
Generalization
“I never have relationships”, “I always spoil everything”, “I always have bad luck”. A person carries over the characteristics of a single incident for life.
Catastrophe
“Everything is very bad”, “This is a failure”, “Irreparable happened”. Under the influence of negative judgments and emotions, the feeling of the situation is pumped up to complete hopelessness.
Duty
“I owe”, “They owe me”, “Everything should have turned out this way, and not otherwise. ” Social roles and responsibilities become immutable truths, neither the specifics of the situation, nor the state of the person, nor the complexity of relationships are taken into account.
” Social roles and responsibilities become immutable truths, neither the specifics of the situation, nor the state of the person, nor the complexity of relationships are taken into account.
Conformity
“Everyone does/behaves like this. Those who do otherwise are bad/inferior, etc.” Ideas about norms received from the outside make one stigmatize the slightest deviation in oneself and others.
The task of the CBT therapist is to identify cognitive distortions that negatively affect the client's quality of life and help develop rational, constructive thought patterns in their place.
Techniques and exercises
One of the main techniques of the method is keeping a CBT diary . Usually it is a table in which you need to enter daily events that caused a strong emotional reaction, and analyze them according to the proposed scheme. Further cases are discussed with the therapist at the session.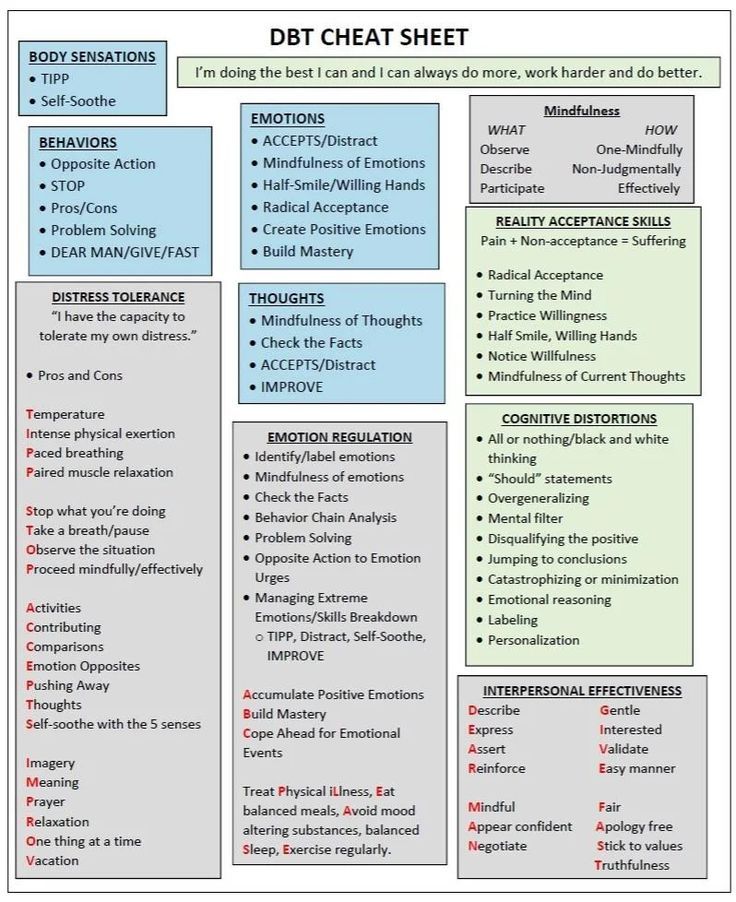
An example of what columns a CBT diary can contain. Each therapist offers his own diary system.
“After the client has learned to identify his automatic thoughts, he begins to keep a diary for a week. We look at what thoughts most often arise in different situations. This may be the fear that the person will look in someone's eyes as optional (that is, bad), or a feeling that he is not successful, or a feeling that he is vulnerable and will not cope. From the automatic thoughts we recognize, core beliefs begin to emerge. Not quick, superficial thoughts, but the foundation on which the human psyche is based. We are working on changing this array of beliefs in a rational direction.”
Anastasia Afanasyeva, CBT psychotherapist:
Another important technique for CBT is exposure . It is especially useful in all kinds of phobias. Exposure helps the client learn not to avoid disturbing situations, but to experience them.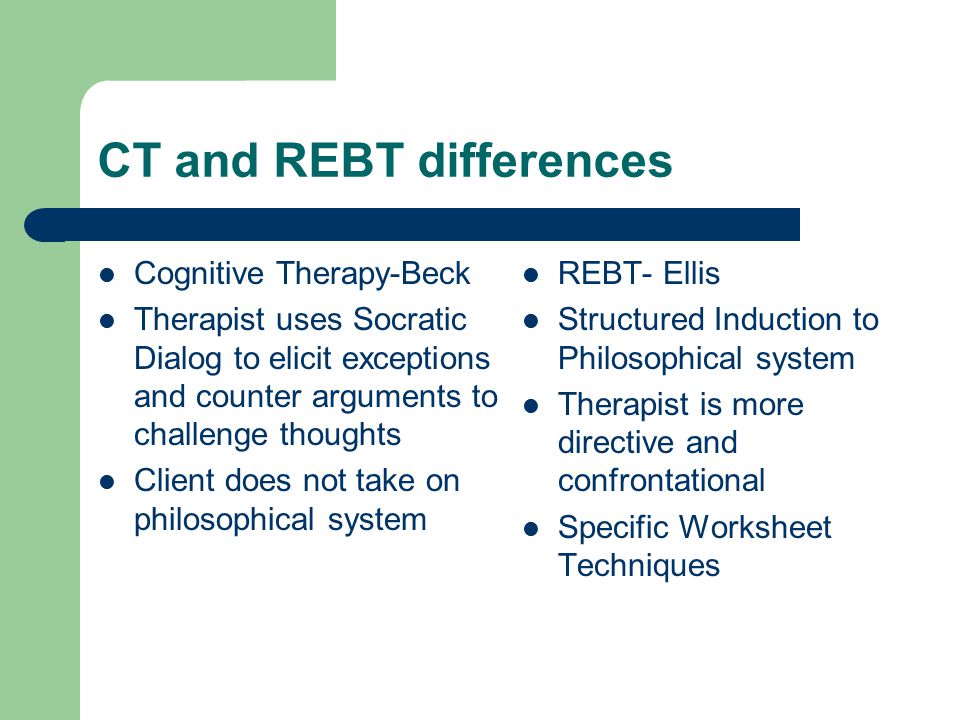
For example, a person is afraid to enter an elevator. When using the exposure technique, the client and therapist approach the booth, stop, and begin to observe the client's reaction. When the anxiety rises, they do exercises with the therapist to help them cope with the anxiety. If the reaction is managed, the client and therapist move on to the next step: they enter the elevator together. The level of anxiety rises again, the therapist again works out with the client his condition. The intensity of the situation gradually increases until the client receives all the necessary skills in order to be aware and rationally assess his condition, to cope with it.
When will CBT help?
The effectiveness of the CPT was proved for the following states:
All types of phobias
Alarm
Panic disorder and panic attacks
Depression
Obsession-compulsive (OKR) 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 thoughts, actions, rituals
Psychosomatic disorders
irritable intestine, headaches and other
post -traumatic stress disorder
Eating disorders
Difficulties with communication, building contacts and their maintenance, constancy in the work and family relations
Dependence 9000
Physical and physical mental
Aggressive behavior
CBT in panic attacks
Panic attacks are spontaneous panic attacks that are accompanied by rapid breathing, palpitations, dizziness, tremor, nausea, sweating and other somatic manifestations.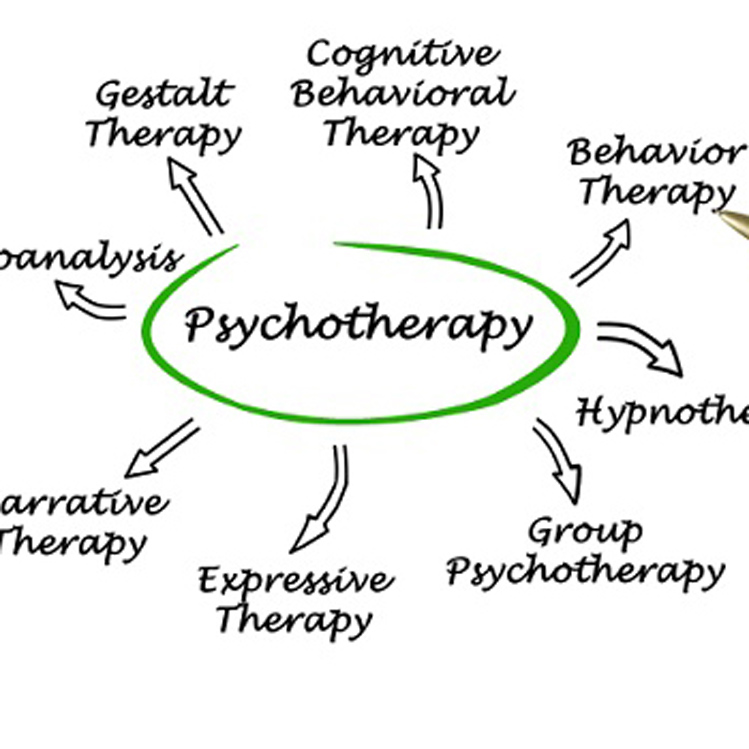
A panic attack may be the result of other psychiatric disorders rather than a single illness. Recurrent panic attacks without other symptoms may be manifestations of panic disorder. Cognitive behavioral therapy is the proven and most effective treatment for it.
“Panic attacks can occur in depressive disorders, generalized anxiety disorder, and hypochondriacal disorders. This is a very non-specific symptom, such as fever. It is found in various diseases. To make an accurate diagnosis, before starting treatment, you need to be diagnosed by a psychiatrist or psychotherapist.
Anastasia Afanasyeva, psychotherapist CBT:
The exposure technique mentioned above is very well the main tool for working with panic attacks. The psychotherapist teaches the patient to recognize what is happening to him at the time of the attack, how and to what his body reacts. Gradually, the patient learns to cope with his condition.
“First, there is a stage of psycho-education: we tell what happens in the patient's body at the time of the attack.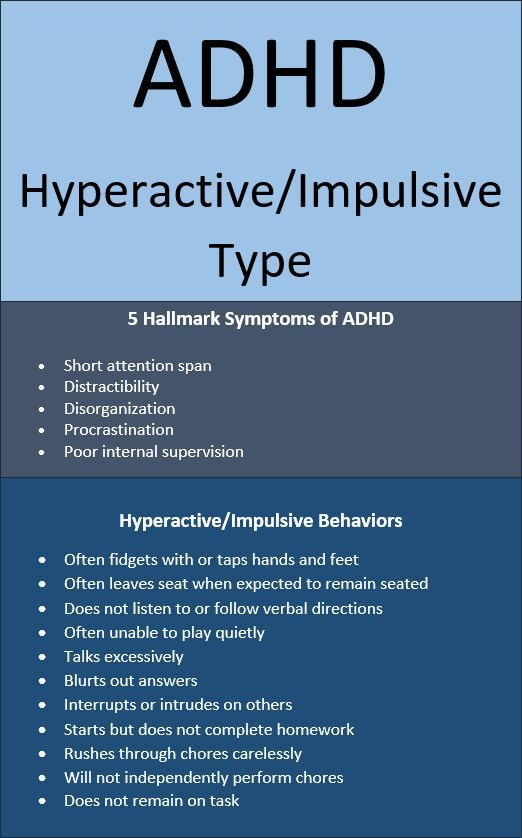 We analyze cycles, thoughts, emotions, behavior, we are looking for the reason that starts the process. Further work is based on the fact that in the office we learn to cause symptoms: dizziness, palpitations, hyperventilation. We practice techniques to endure the anxiety that these symptoms cause. Thus, gradually we build tolerance. Anxiety decreases and eventually disappears.
We analyze cycles, thoughts, emotions, behavior, we are looking for the reason that starts the process. Further work is based on the fact that in the office we learn to cause symptoms: dizziness, palpitations, hyperventilation. We practice techniques to endure the anxiety that these symptoms cause. Thus, gradually we build tolerance. Anxiety decreases and eventually disappears.
Shortness of breath can be caused by hyperventilation - rapid shallow breathing. Dizziness - spinning in place. Palpitations - squats or running up the stairs. All exercises are performed together with the therapist. We say that it is not dangerous, the person understands this. When during the session I breathe with the patient, he sees that I normally endure this state. In doing so, he observes what happens to his own sensations.
The essence of a panic attack is that it always goes away. The fear that it will start, most often becomes the trigger for its start. It brings other problems as well, such as avoiding certain situations or carefully checking one's condition.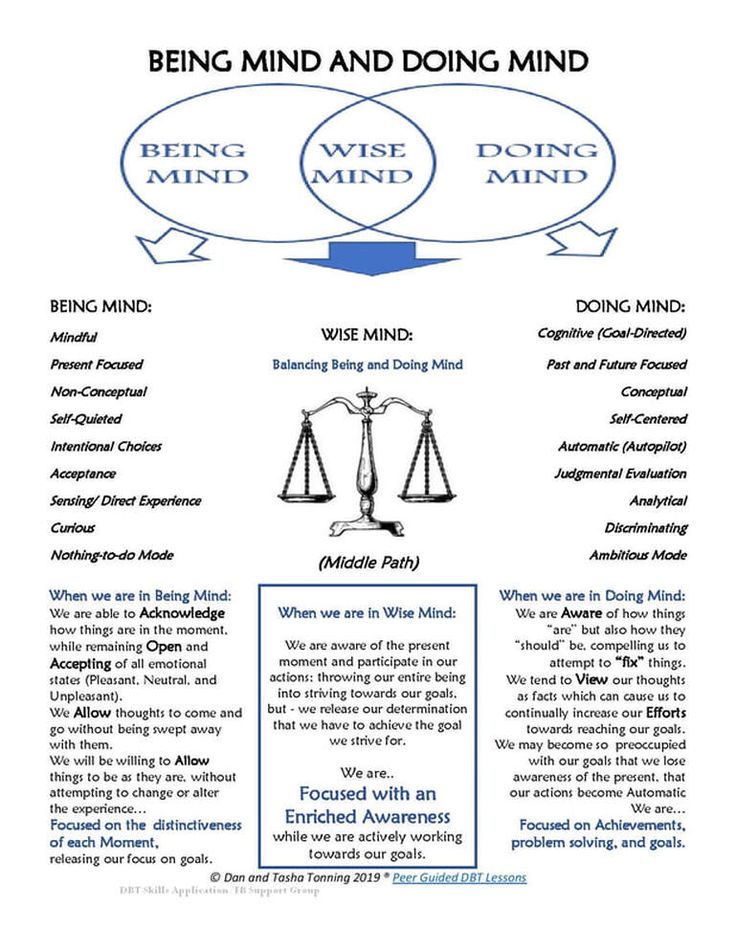 "
"
Anastasia Afanasyeva, psychotherapist CBT:
Duration of the course
CBT is considered a short-term therapy, but the duration of the course depends on many factors. For a specific request, such as a phobia or difficulty falling asleep, about 10 sessions are needed. However, this format involves solving only one problem. For multiple problems and more complex conditions, the course will last from a few months to a year. Treating personality disorders will require even longer work.
Therapy involves a meeting once a week, at a pre-selected time. The duration of the session is 50 minutes. Outside of sessions, the client does homework.
Each session has a structure: agenda, checking homework, discussing specific requests, working through them, debriefing, receiving homework, feedback.
« Terms are always individual and depend on the severity of the condition.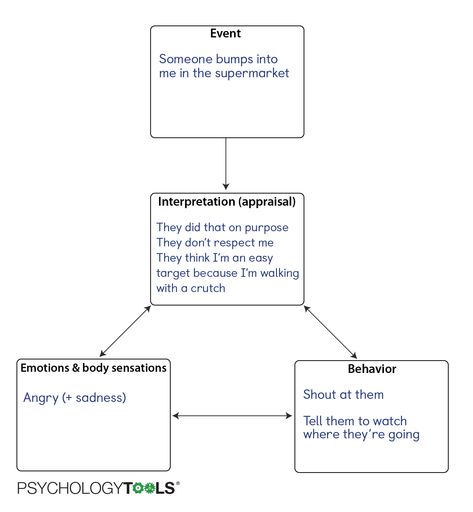 For panic attacks or depression, this is six months to a year. For complex diseases or personality disorders, therapy can be very long. In addition to the form and severity of the disease, the ability and desire of a person to get involved in work play a role. There are people who are more prone to reflection, it is easier for them to realize their own mental processes. There are people who find it harder.
For panic attacks or depression, this is six months to a year. For complex diseases or personality disorders, therapy can be very long. In addition to the form and severity of the disease, the ability and desire of a person to get involved in work play a role. There are people who are more prone to reflection, it is easier for them to realize their own mental processes. There are people who find it harder.
As with any therapy, one should not expect miracles from CBT. You cannot change in a couple of months, and even in six months. But you can learn to see the relationship between your thoughts, emotions and behavior, and this will allow you to weed out unnecessary thoughts, change reactions, not be led by your beliefs left by your parents and the outside world, and not let anxiety and fear rule your life.
Anastasia Afanasyeva, psychotherapist CBT:
Evidence-based medicine and CBT
Cognitive Behavioral Therapy (CBT) is one of the most researched methods of psychotherapy.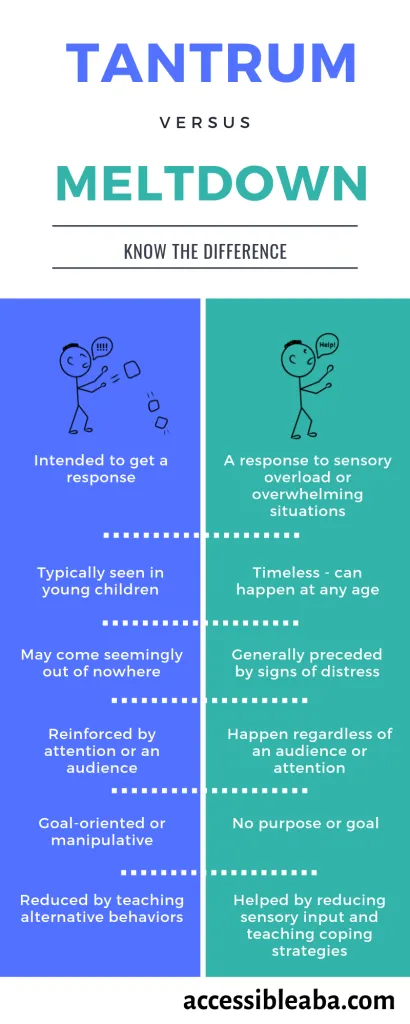 In 2012, a Boston University Department of Psychology Working Group released a seminal systematic review of meta-analyses (1) of various studies, which is the most comprehensive scientific paper on the effectiveness of CBT to date. Based on 269 papers, the researchers concluded that the referral was extremely effective in dealing with anxiety and mood disorders, highly effective in treating phobias, insomnia, and significantly effective in reducing workplace stress. The full text of the review in English can be found here.
In 2012, a Boston University Department of Psychology Working Group released a seminal systematic review of meta-analyses (1) of various studies, which is the most comprehensive scientific paper on the effectiveness of CBT to date. Based on 269 papers, the researchers concluded that the referral was extremely effective in dealing with anxiety and mood disorders, highly effective in treating phobias, insomnia, and significantly effective in reducing workplace stress. The full text of the review in English can be found here.
1 Meta-analysis is a type of data analysis in which the results of a number of randomized clinical trials are combined and analyzed as a single large study. In evidence-based medicine, meta-analysis is assigned the highest level of evidence (IA).
Medication and CBT
There are a number of conditions that can be treated with non-medicated CBT, such as mild generalized anxiety disorder, panic disorder, mild OCD, mild depression.![]() However, in a number of conditions, it is recommended to combine psychotherapy with pharmacotherapy. These include moderate depression and severe depression.
However, in a number of conditions, it is recommended to combine psychotherapy with pharmacotherapy. These include moderate depression and severe depression.
« Fear of pharmacotherapy is quite common and I deal with it regularly. I can say that many fears are unfounded. There is a myth that antidepressants are addictive. According to all studies, no antidepressant causes either mental or physical dependence.
If you have a fear of medication, see a qualified doctor who is trained in psychotherapy and pharmacotherapy. He will conduct a medical diagnosis, decide whether it is really necessary to carry out drug therapy, and help work through your fear using CBT techniques.”
Anastasia Afanasyeva, psychotherapist CBT:
Case reports
“A young man asked for help: after breaking up with a girlfriend, he suffered from depressed mood, anxiety, difficulty falling asleep, obsessive thoughts before going to bed, loss of appetite .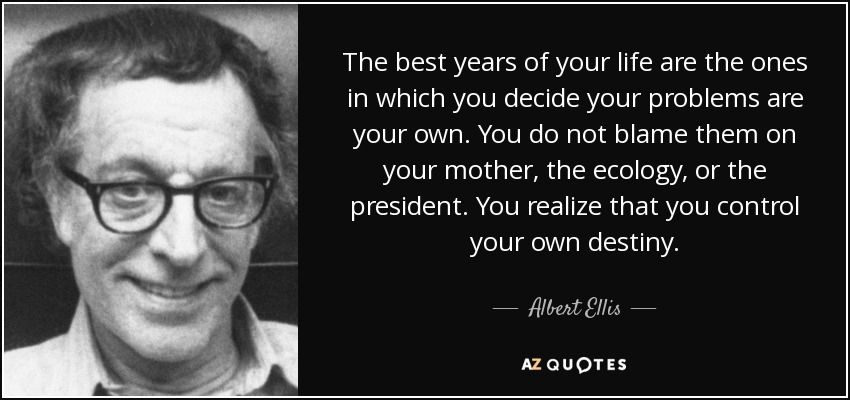 In the course of therapy, we uncovered the hidden beliefs that generated these reactions. He believed that if he could not "keep" the relationship, then this indicates his unreliability, if he failed to choose an "adequate" partner, this indicates weakness. Also, the client could not understand what he needed, he relied on ideas about how "should be".
In the course of therapy, we uncovered the hidden beliefs that generated these reactions. He believed that if he could not "keep" the relationship, then this indicates his unreliability, if he failed to choose an "adequate" partner, this indicates weakness. Also, the client could not understand what he needed, he relied on ideas about how "should be".
During three months of work, the client has learned to be aware of his needs, desires, track thoughts and engage in polemics with them. The young man was able to emotionally distance himself from obsessive thoughts, the mood background leveled off. He built his schedule in accordance with his own goals and values, acquired awareness skills.
Anastasia Afanasyeva, psychotherapist CBT:
What to read?
Cognitive Behavioral Therapy for Anxiety, Fear, Worry and Panic. Michelle Skin, Matthew McKay, Patrick Fanning
This book is for those who are already in therapy and want to understand the basics of the method and get the most out of CBT.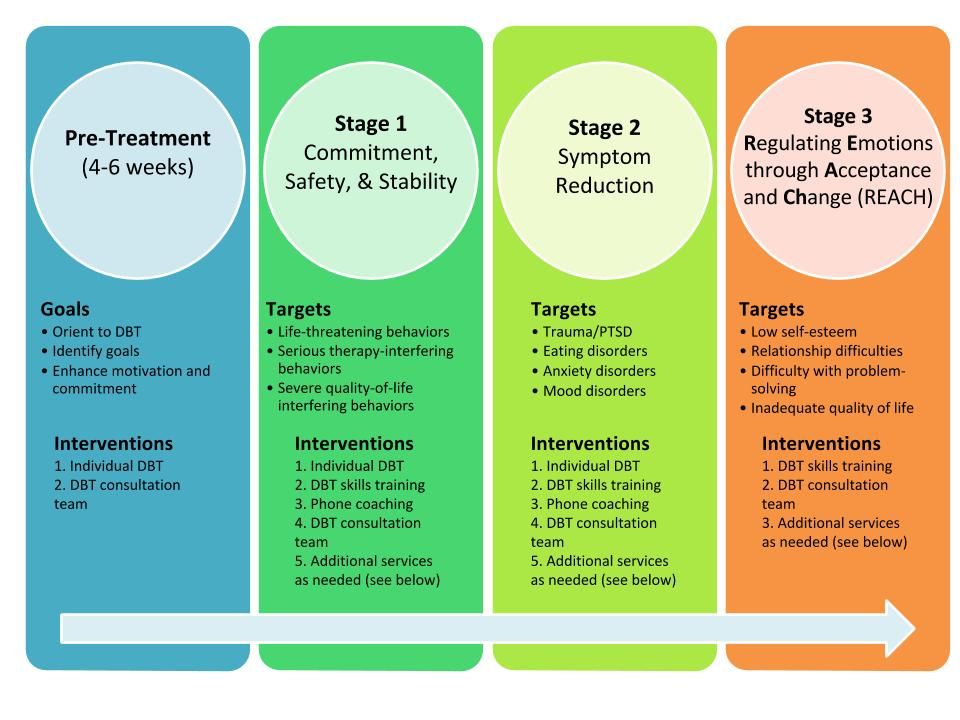


-Cap-30mg-UK-2.jpg)