What determines an alcoholic
SAMHSA’s National Helpline | SAMHSA
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
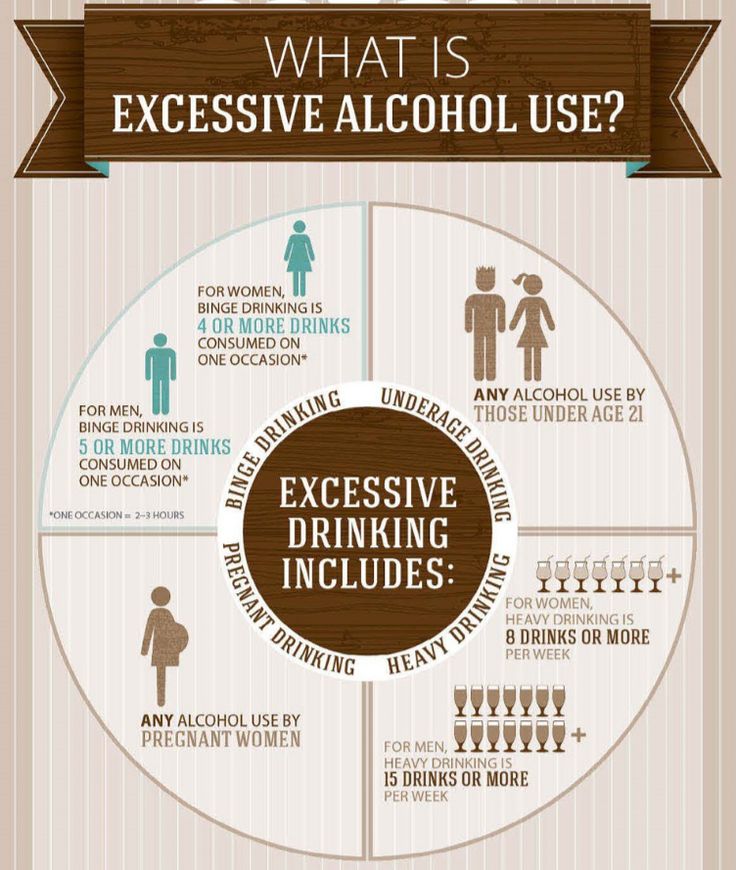
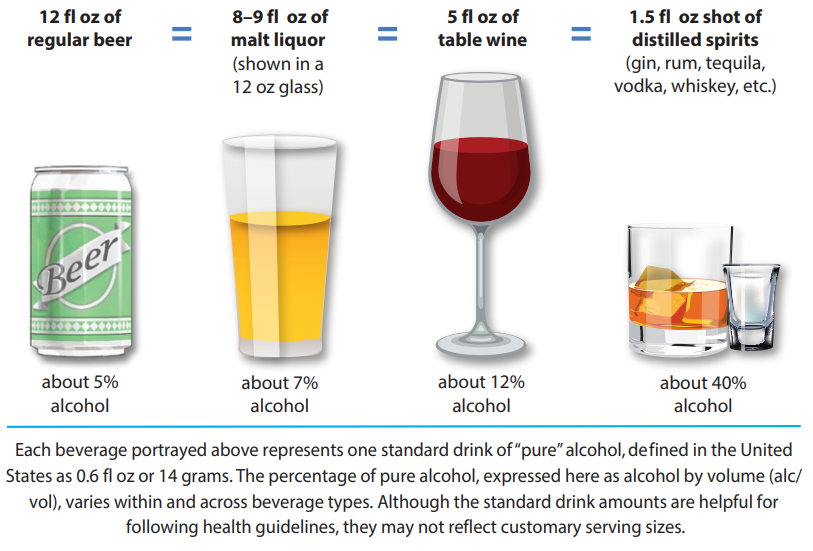
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
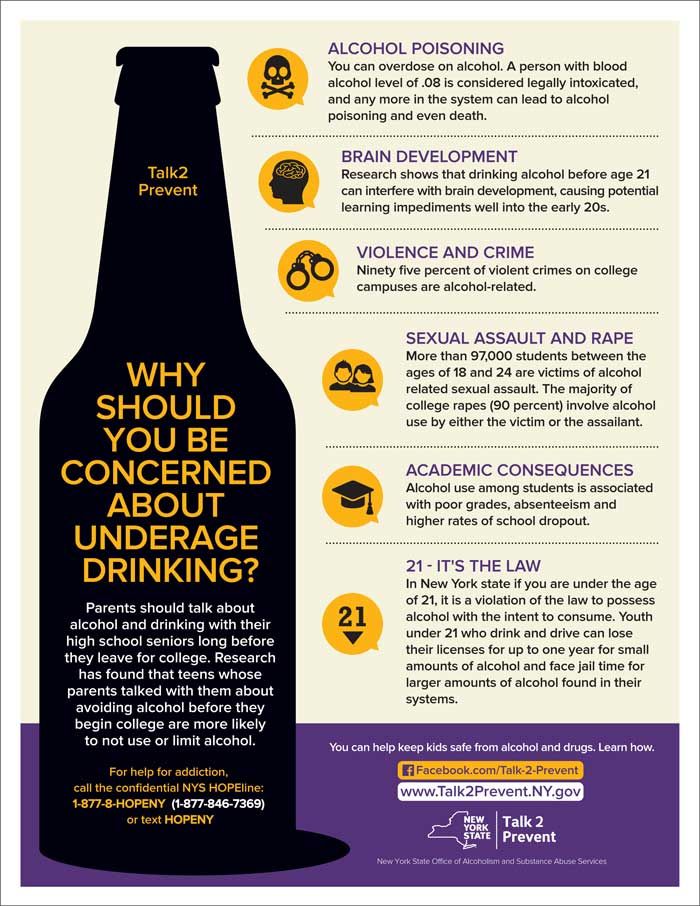
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
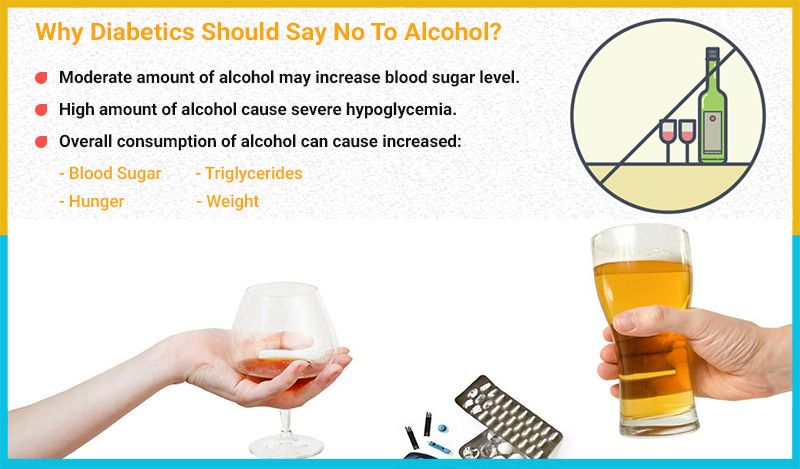
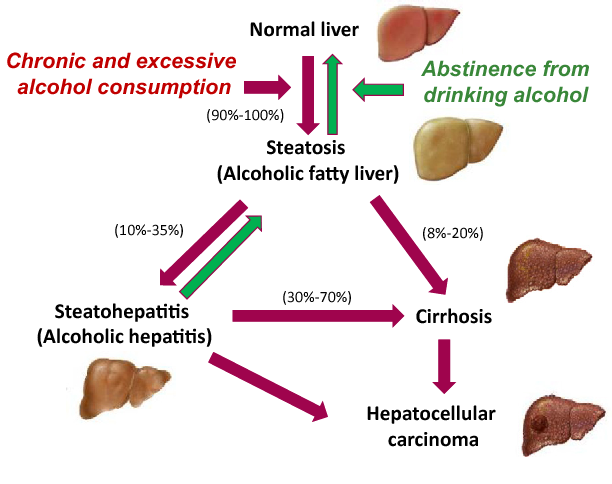
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated
Last Updated: 03/22/2023
treatment, stages, signs and prevention
Therapist, gastroenterologist, general practitioner
Sharhun
Olga Olegovna
Experience 25 years
Therapist, Doctor of Medical Sciences, Professor of the Department of Therapy, General Medical Practice and Nuclear Medicine of the Russian National Research University. N.I. Pirogova of the Ministry of Health, Member of the European Professional Association for Liver Disease, Member of the Russian Gastroenterological Association, Member of the Scientific Society of Gastroenterologists of Russia
Make an appointment
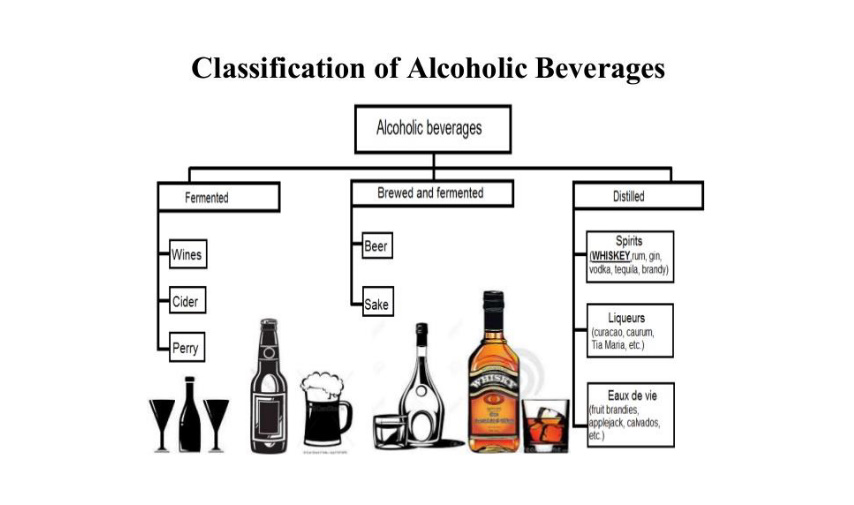
Despite the repeatedly proven harm that alcoholic beverages bring to a person, the share of their consumers is decreasing extremely slowly. A sufficiently large number of people are at risk of developing alcoholism - a mental illness, which is based on uncontrolled craving for alcohol. A person loses interest in all aspects of life that are not related to the use of strong drinks. As a result, he is destroyed as a person, acquires numerous serious illnesses, breaks social ties and literally slides to the bottom. However, modern medicine has tools that can bring the alcoholic back to normal life.
A sufficiently large number of people are at risk of developing alcoholism - a mental illness, which is based on uncontrolled craving for alcohol. A person loses interest in all aspects of life that are not related to the use of strong drinks. As a result, he is destroyed as a person, acquires numerous serious illnesses, breaks social ties and literally slides to the bottom. However, modern medicine has tools that can bring the alcoholic back to normal life.
General information
The use of drinks containing ethyl alcohol adversely affects the physical health of a person. In the CIS countries, there are up to 14% of adults who abuse alcohol, and about 80% of the population drink moderately, from time to time. At the same time, liver damage caused by alcohol consumption is present in at least two million Russians. A third of all deaths in men under the age of 60 are due to alcohol-related cardiac arrest. The problem of alcoholism in our country is still extremely serious, although it has somewhat softened during the last decade.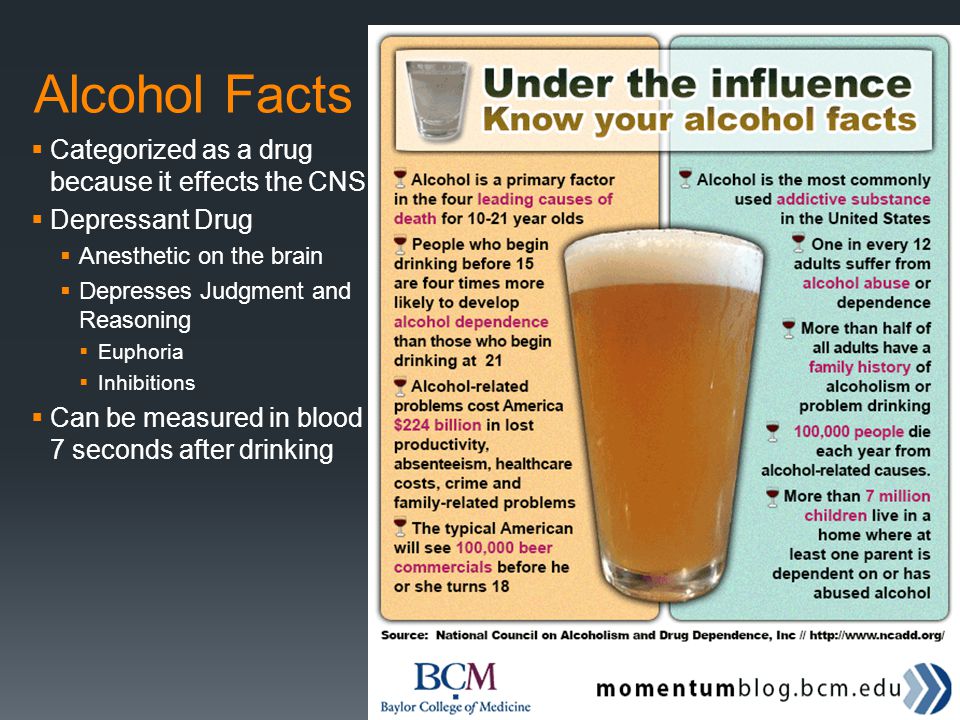
Development of disease
Doctors distinguish three main stages of alcoholism, each of which is characterized by a set of certain signs and characteristics.
- Psychological dependence, addiction to drinking is formed. There are no visible physical pathologies, the person looks quite healthy, maintains social ties, and is able to maintain his material well-being. At the same time, he cannot refuse an offer to drink, even if this is associated with certain problems. At the end of the first stage, there is a “dose collapse” syndrome, when a repeated dose of alcohol causes a sharp and deep intoxication. However, at this stage, a person can still overcome the addiction on their own.
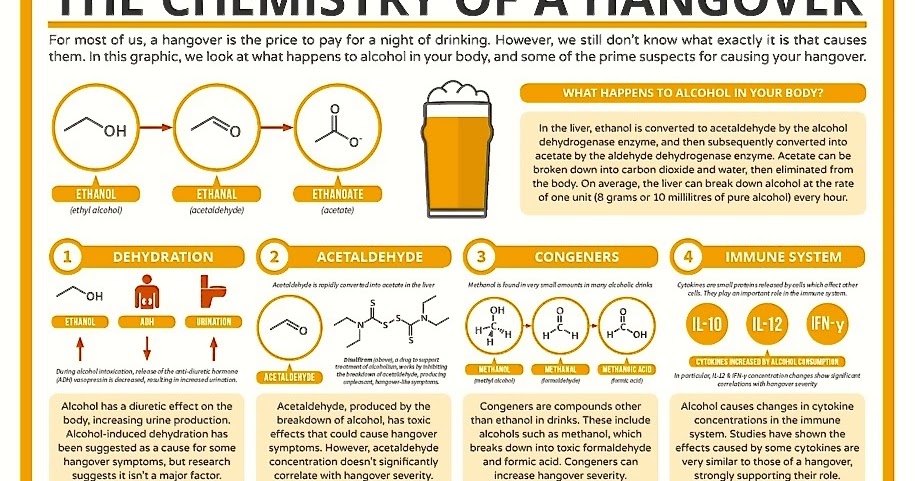
- An obsessive craving for alcohol appears, a person loses the opportunity to concentrate on work, enjoy communication with relatives and friends without drinking. Control over the amount of drink is lost, alcohol ceases to bring pleasure and becomes a vital need. There are signs of damage to the body, a hangover (withdrawal) syndrome develops.
 Multi-day binges begin, when trying to give up alcohol on their own, various complications develop, including meth-alcohol psychoses.
Multi-day binges begin, when trying to give up alcohol on their own, various complications develop, including meth-alcohol psychoses. - Complete loss of social connections and interest in anything other than alcohol. Damage to the nervous system and internal organs is irreversible. The patient consumes alcohol every day, in the absence of alcohol, meth-alcohol psychosis quickly develops, forced sobering up can lead to death. In 95% of cases, the third stage ends with the death of an alcoholic from a heart attack or cerebral hemorrhage.
The listed stages of alcoholism and their manifestations are typical for all people who abuse alcohol.
How to recognize a dangerous border
The hallmark symptoms of alcoholism are:
- lack of control over the amount drunk, inability to stop;
- the absence of a negative reaction of the body when drinking alcohol in large doses;
- memory lapses after drinking;
- hangover syndrome;
- drunken periods, i.
 e. drinking alcohol for two or more days in a row;
e. drinking alcohol for two or more days in a row; - the appearance of external signs of alcoholism - rapid aging of the skin, protruding veins and small bruises formed due to rupture of skin capillaries.
Health disorders characteristic of alcoholism also signal trouble:
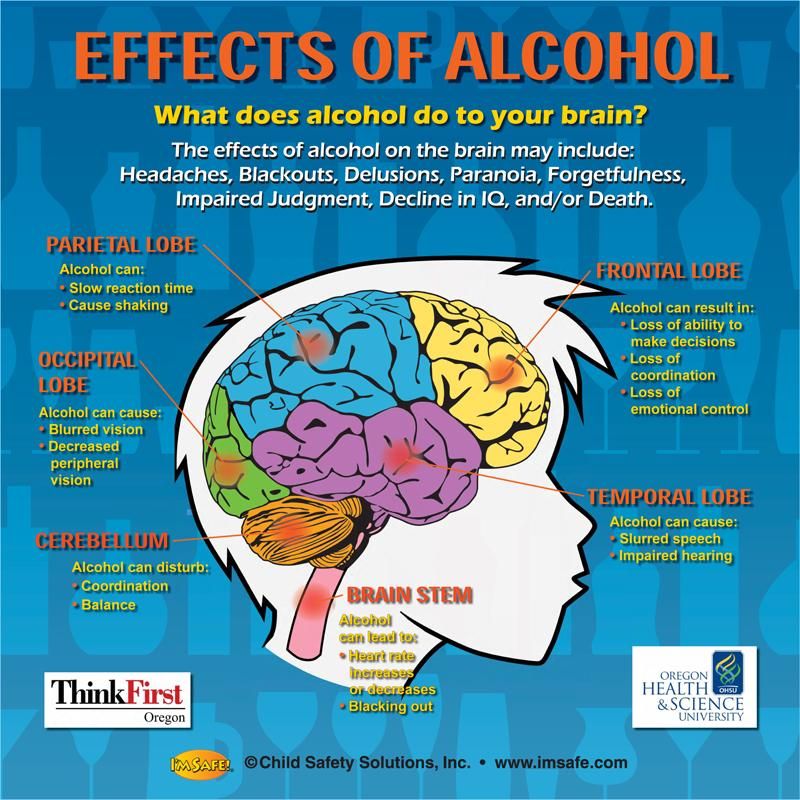
- heart and blood vessels, as the metabolism of potassium and magnesium salts is disturbed, which worsens myocardial contractility, arrhythmia appears, heart pain, blood pressure rises, heart attacks and strokes are not uncommon;
- digestion, since alcohol causes burns of the gastric and intestinal mucosa, destroys the cellular structures of the digestive tract, provokes increased secretion of gastric juice, which leads to the development of gastritis and ulcerative lesions;
- kidneys, since alcohol and its metabolites destroy the renal tubules and parenchyma, which leads to the development of pyelonephritis and glomerulonephritis;
- liver, whose cells are destroyed by ethanol, which is why alcoholics develop hepatitis and cirrhosis;
- of the nervous system, since under the influence of ethanol and its metabolites peripheral nerve fibers are destroyed, alcoholic polyneuropathy develops.
Alcoholism is a serious disease that inevitably leads a person to a painful death. It is necessary to start treatment as early as possible to give the patient a chance to return to a full life.
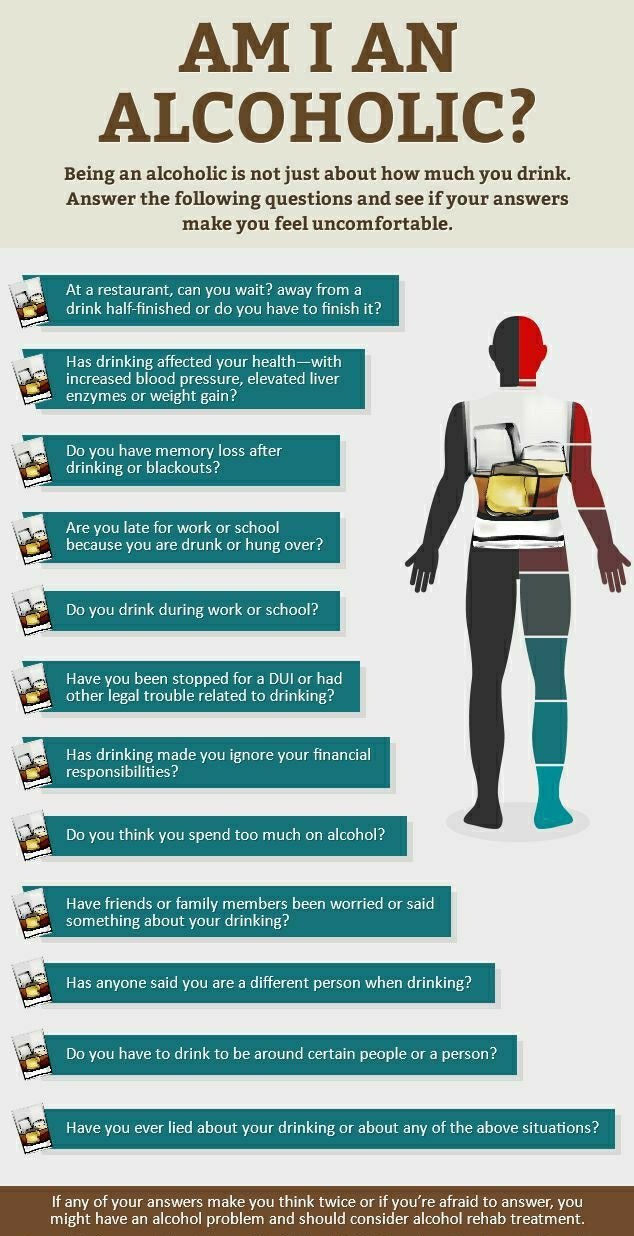
Features of the diagnosis
The diagnosis of alcoholism is based on clinical symptoms, which are supported by the results of laboratory tests. There are standard questionnaires that allow you to identify alcohol addiction in a patient with almost 100% certainty. Laboratory tests of urine and blood reveal markers of chronic drinking. The doctor may prescribe an enzyme test that detects the level of activity of the enzyme complex in relation to alcohol intoxication, as well as tests for the level of the hormones testosterone and prolactin.
If necessary, hardware studies can be prescribed to diagnose the state of internal organs: ultrasound of the abdominal cavity, CT scan of the liver and spleen, ECG, endoscopy of the digestive tract, study of nerve conduction, etc.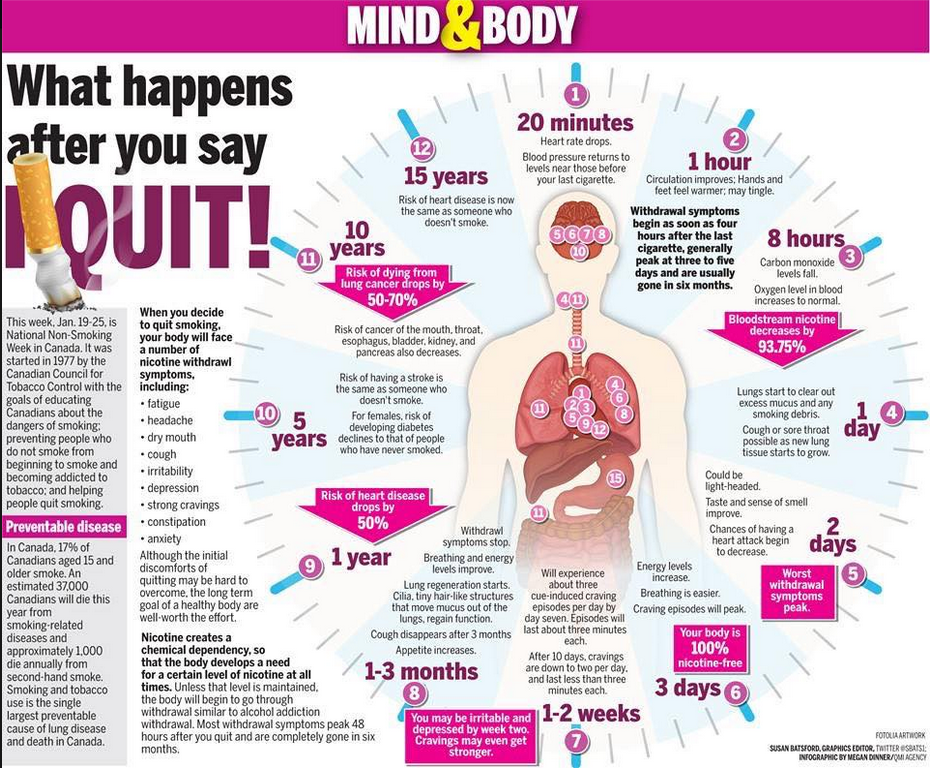
How to get rid of drunkenness
Alcoholism treatment is a complex process that includes:
- aversive therapy, the purpose of which is to develop an aversion to alcohol with the help of certain drugs;
- psychotherapy, the effectiveness of which reaches 80%, but only if the patient himself strives for recovery;
- body detoxification, the methodology of which is similar to the set of measures for any food or non-food poisoning;
- social adaptation, which allows the patient to refrain from drinking alcohol after the end of the course of treatment.
To return the patient to a normal life, great efforts and long-term painstaking work of many specialists are required. Therefore, the prevention of alcoholism is of great importance - measures aimed at preventing the development of alcohol dependence in healthy people. But if trouble has already happened to you or your loved one, you need to contact a specialist as soon as possible, because the further the process of alcoholization goes, the more difficult it will be the way back to health.
Frequently Asked Questions
What are the causes of alcoholism in men and women?
There are a number of causes of alcoholism - psychological, biological and social.
- Psychological. This includes loneliness, lack of confidence in oneself and one's abilities, low self-esteem, lack of opportunities for self-realization, etc.
- Biological. Metabolic abnormalities are inherited or formed during the development of the organism and determine a high susceptibility to alcohol. A negative effect is caused by a lack in the body of certain enzymes involved in the breakdown of ethyl alcohol, as well as some features of the nervous system and the presence of neuropsychiatric diseases.
- Social. The cultural environment in which a person lives shapes his attitude towards alcohol: in countries where alcohol is not tabooed, the level of alcoholism is much higher than where drinking is strongly condemned by society. The personal level of development and education, the possibility of social growth, the presence of strong social ties are also important.

Which doctor should be consulted for the treatment of alcoholism?
Alcoholism develops as a result of damage to the body by a chemical substance - ethyl alcohol, therefore, regarding the diagnosis and the start of treatment, it is necessary to contact a narcologist. Subsequently, other specialized specialists will work with the patient.
Which people are most at risk of becoming an alcoholic?
An irresistible craving for alcohol most often develops in people:
- infantile, not formed as a person;
- suggestible;
- unsure of themselves and their abilities;
- prone to addiction;
- lonely, with an unsatisfied need for psychological intimacy;
- biological - genetic predisposition, nervous and mental diseases of early childhood, features of the functioning of the nervous system in the form of the prevalence of excitation processes;
- social - the habitat in which drinking traditions are formed, libations for any reason with a low level of moral values;
- psychological - initially low self-esteem, anxiety, insecurity, inability to cope with stress, only drinking alcohol brings pleasure and causes euphoria.
- Pathological attraction - all needs are ignored, except for drinking. Determining that a person will still become an alcoholic is simple: the patient always finds hidden alcohol, anywhere and at any time, and does this by smell.

- Extinction of the gag reflex - the protective reflex "turns off".
- Loss of quantitative control - there is no measure, drinking "to the stop", sometimes to the point of losing consciousness.
- An increase in tolerance with a subsequent decrease - if in the initial stages it takes liters to achieve intoxication, then in the final - glasses.
- prodromal - a risk group, a person never refuses to drink alcohol when there is such an opportunity, especially in a company;
- the first - there are mental and physical addictions, a severe hangover, episodes of memory lapses (amnesia), mood swings, but family and work remain;
- the second, often referred to as "chronic alcoholism" - binges are formed (continuous use), but there are light intervals, lesions of the central and peripheral nervous systems join, the number grows to a maximum, many lose their jobs, there is discord in the family;
- the third - complications in the form of alcoholic psychoses and convulsive attacks join, the personality falls apart, all organs and systems are affected, social ties are lost, a minimum dose is required for intoxication.
Call +7 (495) 775-73-60 or leave a request, we will call you back
processing of personal data in JSC "Medicina".
The consent of the patient (his representative) to the processing of his PD for the purpose of advertising communication is not collected.
Licenses
License for medical activities No. LO 77-01-017705
Your browser is outdated, we recommend updating it to the latest version
or using another more modern one.
causes, stages, symptoms, signs, consequences, treatment, prevention
Features
Causes
Symptoms and stages
Diagnosis
Treatment
The main difference between an alcoholic and a domestic drunkard is mental and physical dependence. A drunkard drinks according to circumstances, he practically never has binges. May abstain after a domestic row or when money runs out. An alcoholic does not pay attention to such “little things” as a career or a collapsing family, because the use of alcohol-containing liquids is in the first place. Alcoholism is always, in 100% of cases, accompanied by the degradation of the personality and the destruction of internal organs.
Features of alcoholism
Alcoholism belongs to the group of substance abuse. The World Health Organization claims that alcohol consumption is increasing along with an improvement in the quality of life.
The World Health Organization claims that alcohol consumption is increasing along with an improvement in the quality of life.
Russian statistics are somewhat different: in our country, the number of alcoholics increased in difficult years, and over the decade from 2008 to 2017, it decreased by more than 1 million people.
More than 140 million people in the world bear the burden of this heavy addiction. It is undeniably established that the disease is incurable. The ancient Greek hereditary physician Hippocrates said that drunkenness is voluntary madness. The expression is relevant to this day, because the only thing that can save the mind and body of an alcoholic is a complete, absolute rejection of alcohol.
Causes of alcoholism
Researchers divide the causes of the formation of the disease into 3 equivalent groups:
Physicians attach particular importance to heredity when the patient's parents have signs of alcoholism. Children of alcoholics risk repeating the path of their parents 30% more than their healthy peers. Painful manifestations are introduced to children too early, when criticism is not yet possible, and they easily follow the beaten path.
The insidiousness of addiction is that the body of any person produces endogenous ethanol, which is necessary for biochemical processes. External ethanol is no different from what is produced inside. In addition, patients lack the enzyme that breaks down ethanol, alcohol dehydrogenase.
Symptoms and stages of alcoholism
Addiction goes through several stages:
Doctors distinguish several stages of alcoholism:
Alcoholism in men and women has no fundamental difference, except that women go through all the stages three times faster than men, completely losing their attractiveness and sliding into uncontrolled sexuality.
Diagnosis of alcoholism
Diagnostics includes a full-fledged examination, in which, in addition to a narcologist and a psychiatrist, a therapist and, according to the situation, a cardiologist, a neurologist and a gastroenterologist participate. The narcologist establishes the leading syndromes of alcoholism - tolerance or tolerance of the dose, binges and their duration. The psychiatrist, together with a clinical psychologist, examines the structure of the personality, intellectual-mnestic decline, paying attention to accidents while intoxicated, evaluates professional and personal decline. The psychiatrist also deals with the treatment of acute hallucinosis and chronic delusional formations.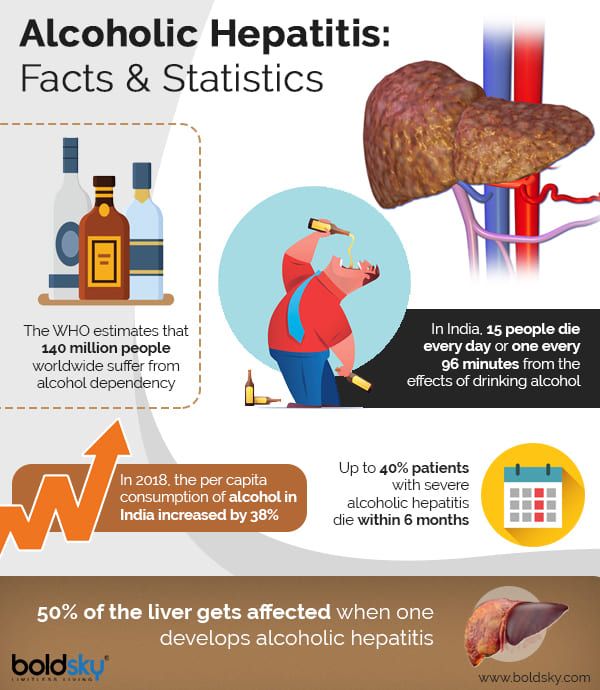
Neurologist treats convulsions, encephalopathies (brain damage), peripheral neuropathies, gait and static disorders, sensory disorders, strokes and thrombosis.
The therapist deals with problems of the heart (hypertension, arrhythmias) and the respiratory system, the gastroenterologist deals with liver diseases, especially cirrhosis.
Female alcoholism requires the participation of a gynecologist, since ethanol destroys the reproductive organs, disrupts the menstrual cycle, depriving the patient of the opportunity to become a mother.
The necessary and most important stage of diagnostics is the patient's acceptance of his problem, awareness of himself as a sick person. At the initial stage, the efforts of physicians are aimed precisely at ensuring that the patient recognizes himself as an alcoholic. Without this, it is impossible to move on, otherwise the treatment will turn out to be formal, the patient will “break loose” at the first opportunity.
It is useful for diagnosis to place the patient in a hospital, where he has the opportunity to visually and "in all its glory" observe the consequences of alcoholism in the form of acquired dementia, a series of convulsive attacks or the inability to walk independently. A patient who has not lost the ability to think critically (in the first or second stages) usually realizes the severity of the problem, sometimes stopping drinking alcohol forever.
A patient who has not lost the ability to think critically (in the first or second stages) usually realizes the severity of the problem, sometimes stopping drinking alcohol forever.
Beer alcoholism (gambrinism) deserves special attention. This form of the disease is not included in the official classification of diseases, injuries and causes of death, since it refers to journalistic clichés. Doctors say that there is only one disease, and the drink that caused the addiction does not matter.
However, this form is common in practice. Patients and, unfortunately, relatives do not take this form seriously, starting treatment only at the stage of complications. So, the "beer heart" was described by the doctors of Bavaria in 1914 at the workers of the brewery. The disease develops slowly and as if imperceptibly, but the changes are irreversible.
The most accurate and simple test for alcoholism (MAST) was developed in 1971 at the University of Michigan. This is a questionnaire that describes attitudes towards alcohol, frequency of use, hangover characteristics, binges, protective reflexes, attitudes of relatives, a reason to drink, and other features.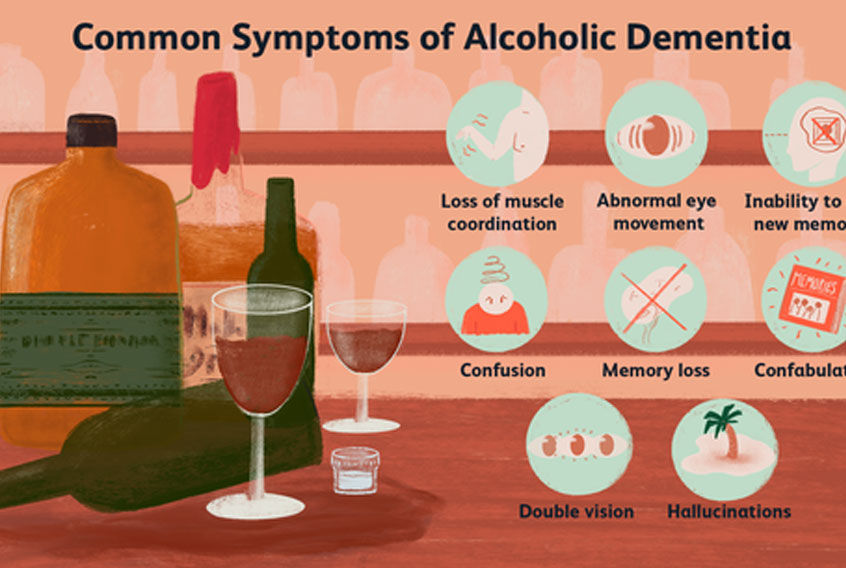 There are several variants of the questionnaire, they have minor differences.
There are several variants of the questionnaire, they have minor differences.
A conversation with an experienced doctor, testing, medical examination guide the patient on the path to recovery. Sometimes a meaningful excursion to the narcological department with a demonstration of patients in the terminal stage is enough to obtain informed consent for treatment.
A narcologist and even more so a psychiatrist have a tremendous experience in dealing with patients of this profile, they are able to find the pain points of a person in the first minutes, to find words for persuasion. It is possible that the patient will not agree to be treated at the first visit, but he will definitely remember the meeting and will be able to apply in a critical situation.
Alcoholism treatment
Treatment tactics are determined by the stage of the disease and the personality of the patient.
It all starts with withdrawal from drinking, which is reasonable to carry out in stationary conditions. The patient's condition may be so severe that the involvement of a resuscitator is required.
The patient's condition may be so severe that the involvement of a resuscitator is required.
Several days are allotted for detoxification. There is no universal cure for alcoholism; medicines are used to correct acid-base balance, antiarrhythmic and hypotensive drugs, diuretics, decongestants, antiemetics, anticonvulsants, antipsychotics and others.
In mild cases, when there is no threat to life, the detoxification stage is carried out on an outpatient basis or at home. After the binge is interrupted, the patient is discussed in detail, revealing his true attitudes and aspirations.
An excellent result is given by the coding for alcoholism, which can be medicated or hypnotic. With a medical option (filing), disulfiram is implanted through a small incision, which gives a sharp vegetative reaction when drinking alcohol - palpitations, sweating, trembling, and an increase in blood pressure. The patient is warned about the consequences, usually they take a receipt in order to avoid litigation in case of death.
During hypnotic coding, the patient is immersed in a trance (a borderline state between sleep and wakefulness), fixing the sobriety setting in his psyche. This option is suitable for suggestible patients undergoing treatment for the first time or with previous positive experience. It is useful to support this method with drops and tablets for alcoholism containing chemical compounds and herbal preparations.
A patient who lives with a family and has a job can be kept from relapse for a long time. There are no former alcoholics, of course, but during remission the patient manages to feel the taste and advantages of ordinary life, independently makes efforts not to return to addiction.
The best prevention of alcoholism is real life goals that cannot be achieved with drinking: family, children, career growth, welfare. Psychological correction is also required from the wife and other important relatives for the patient, since getting rid of such a destructive addiction can only be achieved by joint efforts.