What are the signs of adhd in toddlers
Signs and Symptoms of ADHD in Toddlers
Mental health professionals do not diagnose attention deficit hyperactivity disorder (ADHD) in children under age 4. Certain behaviors associated with ADHD in school aged children may be considered typical in toddlers.
Professionals typically diagnose ADHD in school aged children 12 or younger. According to the American Academy of Pediatrics, doctors and healthcare professionals should not diagnose the condition in children before age 4.
ADHD is more than just typical toddler behavior. According to the National Institutes of Health (NIH), the condition must occur over a long period and impair functioning. This is part of the reason ADHD is not typically diagnosed in toddlerhood.
While toddlers may show some signs of ADHD, it does not necessarily mean they have the condition. At this age, they may have difficulty paying attention or be hyperactive or impulsive.
But some toddler behaviors may lead some parents to wonder whether or not their child has ADHD or has a chance of developing it.
Read on for a checklist of symptoms to watch out for.
What is ADHD?
ADHD is a neurodevelopmental disorder that may cause hyperactivity (constantly active behavior) and impulsive behaviors. People with ADHD, including children, typically have trouble focusing on one task. They may also have difficulty sitting still for long periods.
According to a 2019 study, some behaviors noted in toddlerhood could be related to the development of ADHD. However, considerably more research is needed.
According to the NIH, these are the three main signs of the condition in kids over age 3:
- inattention
- hyperactivity
- impulsivity
These behaviors also occur in children without ADHD. A child won’t receive an ADHD diagnosis unless they have several symptoms that have been present for at least 6 months and that affect their functioning. These symptoms may affect their ability to participate in age-appropriate activities.
Great care must be taken in diagnosing ADHD in children, particularly when considering medication.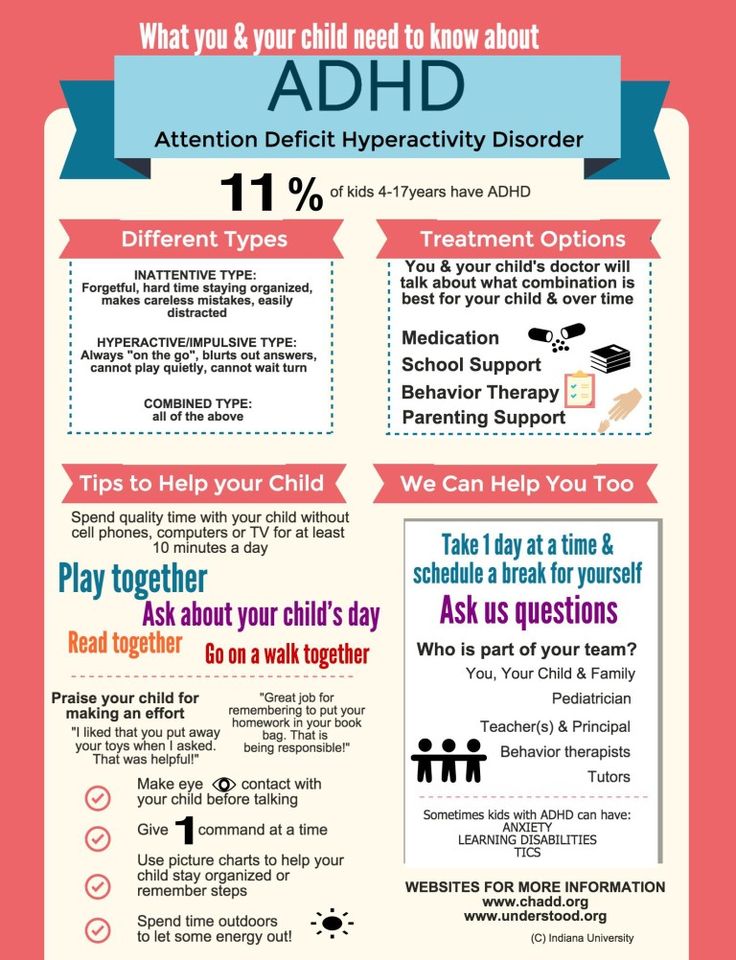 A mental health professional or pediatrician will be the best at making a diagnosis at this young age.
A mental health professional or pediatrician will be the best at making a diagnosis at this young age.
Many mental health professionals will not make a diagnosis until the child has been in school. This is because a key criterion for ADHD is that the symptoms are present in two or more settings. For example, a child shows symptoms at home and school, or with a parent and with friends or relatives.
Several behaviors can indicate your child has difficulty with attention, a key sign of ADHD. In school aged children, symptoms of inattention may look like:
- difficulty with sustaining attention, in play or completing work
- difficulty listening and following directions
- difficulty paying attention to detail and making seemingly small mistakes
- challenges staying organized
- avoiding tasks at home or school that require more sustained attention
Note, however, that these behaviors can also be typical in a toddler and expected for their developmental phase.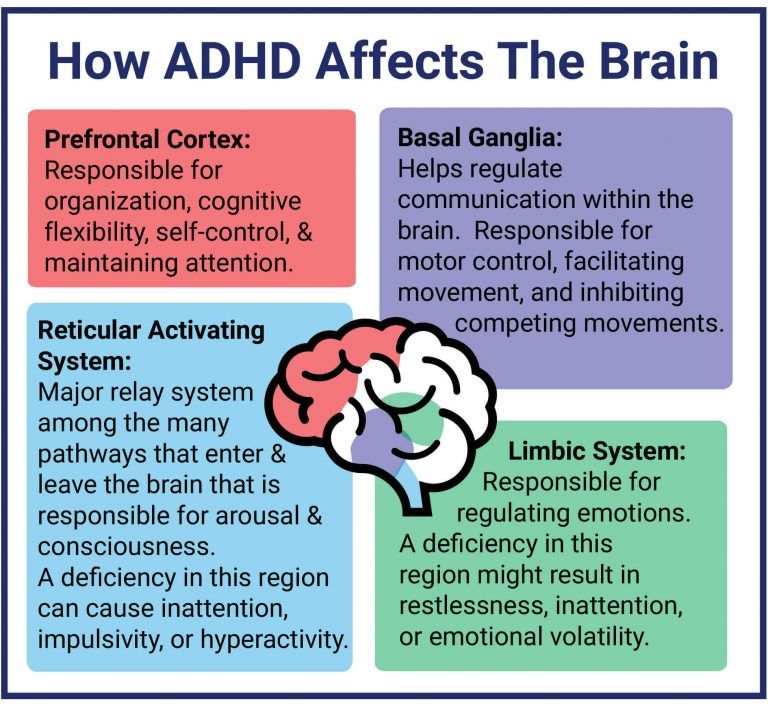
In the past, ADHD was called attention deficit disorder.
Many medical and mental health communities call the condition ADHD because the disorder often includes components of both hyperactivity and impulsivity. This is particularly true when diagnosed in preschool aged children.
Signs of hyperactivity that your toddler may display include:
- being overly fidgety and squirmy when seated
- being unable to sit still for calm activities like eating and having books read to them
- talking and making noise excessively
- running from toy to toy, or constantly being in motion
- running around or climbing at inappropriate times
Another symptom of ADHD is impulsivity. Signs that your child has overly impulsive behaviors can include:
- displaying extreme impatience with others
- having difficulty waiting for their turn when playing with other children
- interrupting when others are talking
- speaking at inappropriate times
- answering questions before they are fully asked or finishing other people’s sentences
Again, these can be expected behaviors in toddlers.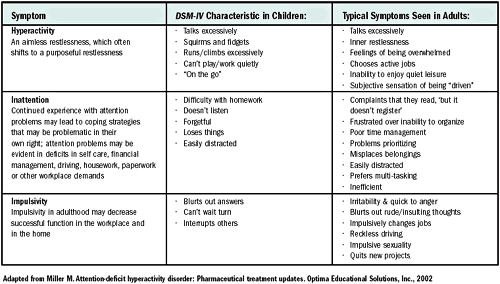 They would only be a reason for concern if they’re extreme when compared to those of children of a similar age or if they’re affecting your toddler’s functioning.
They would only be a reason for concern if they’re extreme when compared to those of children of a similar age or if they’re affecting your toddler’s functioning.
A school aged child with ADHD may show other symptoms as well. These may include:
- more frustration, anger, and outbursts than their peers
- endangering oneself or others due to fearlessness
- difficulty calming down
- aggressive behaviors (toward self or others)
- little need for sleep
While mental health professionals should not diagnose ADHD in toddlers, you may want to discuss your concerns with a pediatrician or mental health professional. This may help determine a diagnosis when your child reaches school age. These healthcare professionals may also offer suggestions to help with hyperactivity, impulsivity, and inattention.
Children can only receive an ADHD diagnosis when they have reached school age. Pediatricians and mental health professionals may base an ADHD diagnosis on the child’s behaviors and other symptoms.
It’s sometimes easy for parents and teachers to mistake certain behaviors for ADHD.
For example, toddlers sitting quietly and behaving in preschool may not be paying attention. Children with hyperactivity may have challenges listening to, understanding, or carrying out instructions.
Most toddlers may show hyperactivity, impulsivity, and inattention at times. This may look like excessive energy or trouble following directions.
If you’re concerned about your child’s behavior, you may want to speak with a pediatrician or mental health professional.
The NIH notes that ADHD can be very common among children. The CDC estimates that 2% of children ages 3 to 5 have ADHD.
If you think your toddler may be showing signs of ADHD, consider sharing your concerns with a pediatrician. They may be able to help you and your child manage the condition. They may also point out other signs to look for and guide the diagnosis process when your child is old enough.
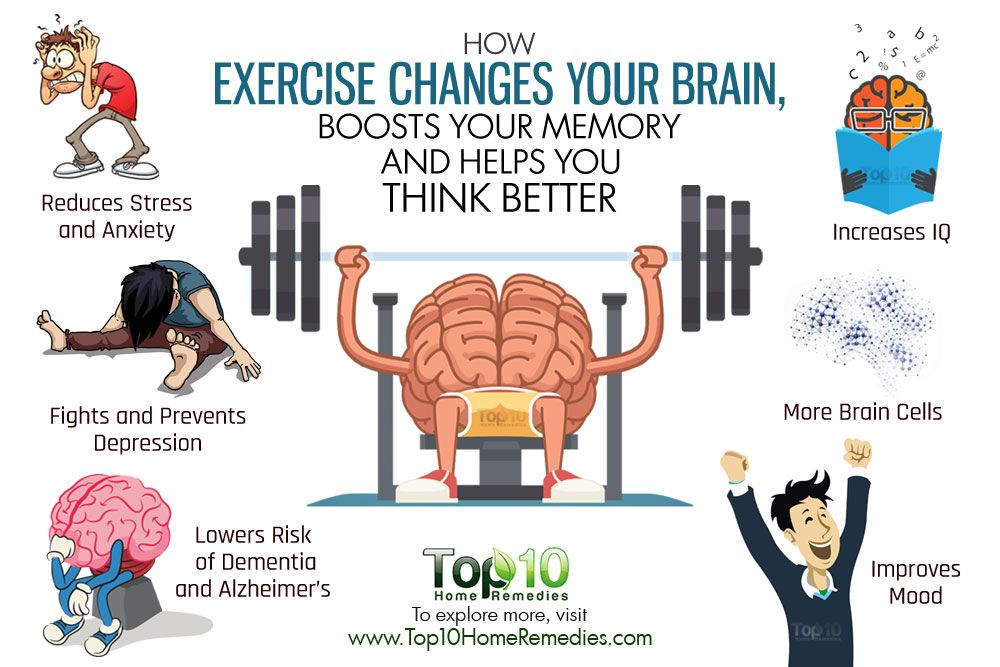
While there is no cure for ADHD, treatment can help improve your child’s symptoms.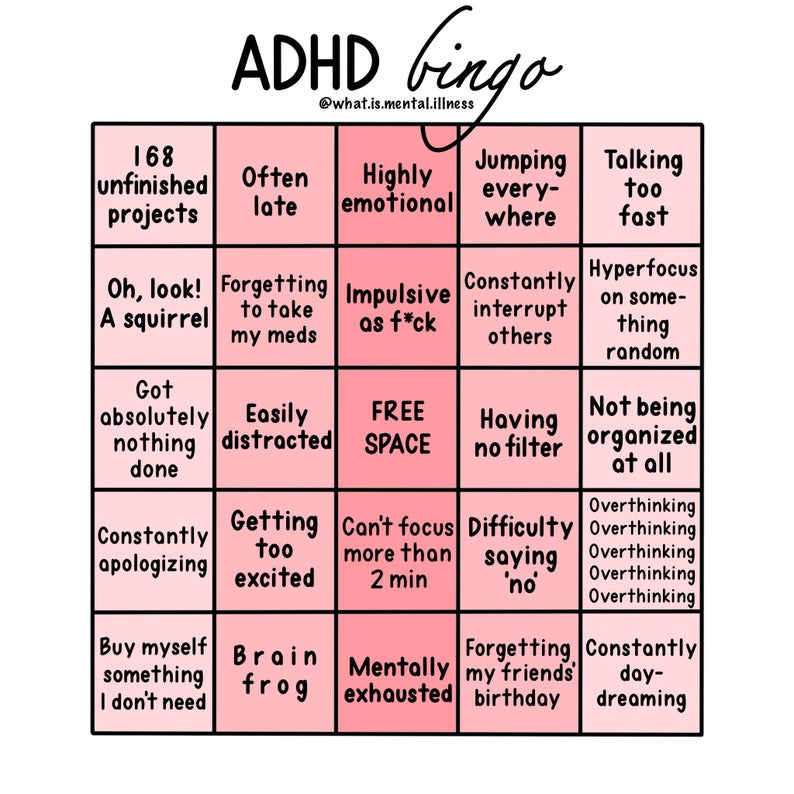 This may include:
This may include:
- medication
- psychotherapy, including family therapy, behavioral therapy, and cognitive behavioral therapy
- lifestyle measures
For success at school, certain classroom management tactics may also help improve your child’s attention.
Doctors and healthcare professionals do not diagnose ADHD in toddlers. They may diagnose the condition in school aged children.
Many behaviors associated with hyperactivity, impulsivity, and inattention in school aged children may be typical behavior in toddlers.
If you have concerns about your toddler’s behavior, you may want to discuss them with a pediatrician or mental health professional.
When Toddler Tantrums Are Actually ADHD: Early Signs of ADD
Some children exhibit signs of attention deficit hyperactivity disorder (ADHD or ADD) as young as 2 (and, in some cases, even earlier). Of course, disentangling normal Terrible Two behavior from ADHD is tricky, to say the least.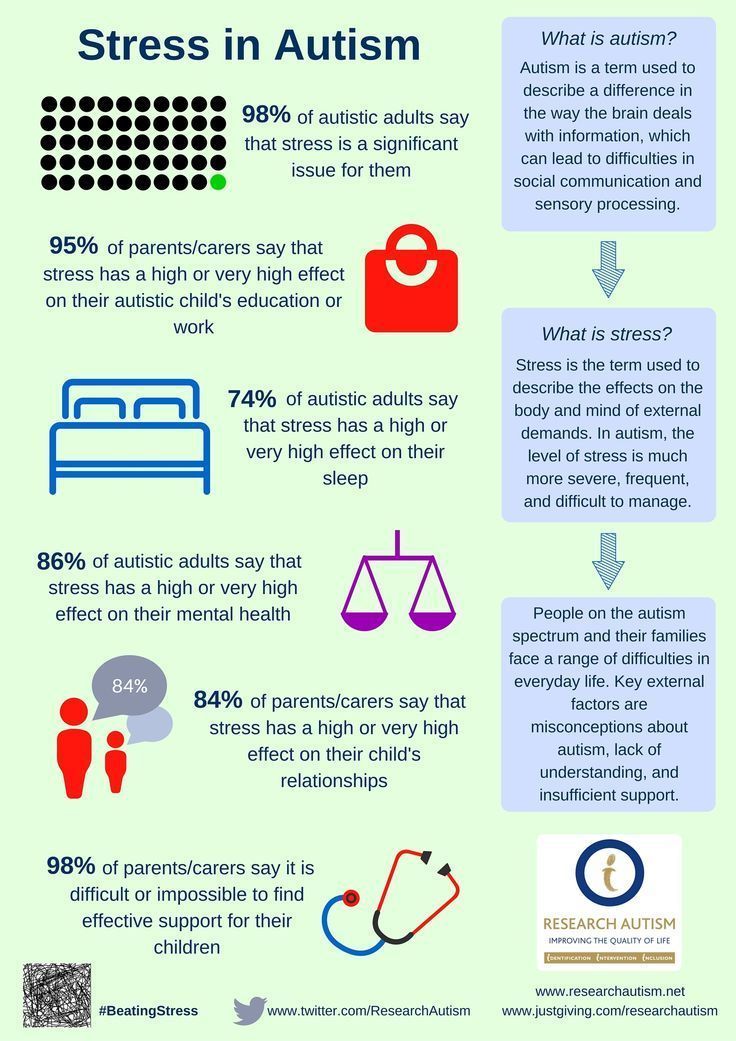 Most toddlers have an abundance of energy, talk excessively, jump from one activity to another, and get distracted easily. They are impatient and howl over silly things — like getting the dark blue cup instead of the light blue one at lunch.
Most toddlers have an abundance of energy, talk excessively, jump from one activity to another, and get distracted easily. They are impatient and howl over silly things — like getting the dark blue cup instead of the light blue one at lunch.
So how can parents and practitioners identify ADHD red flags in this sea of crimson? By honing their focus on a child’s emotional control — or lack thereof.
Early Signs of ADHD in Babies: Poor Sleep, Feeding, Frustration
The American Academy of Pediatrics says children may be diagnosed with ADHD no younger than age 4, but that doesn’t mean ADHD in toddlers isn’t real.1 There are real differences in the ADHD brain that are present at birth, and waiting too long to intervene may burden a child unnecessarily.
It’s easy to spot children with severely hyperactive or impulsive behaviors — they’re the ones who are extremely active and spontaneous and seem to need less sleep than their peers. Their parents and caregivers are exhausted.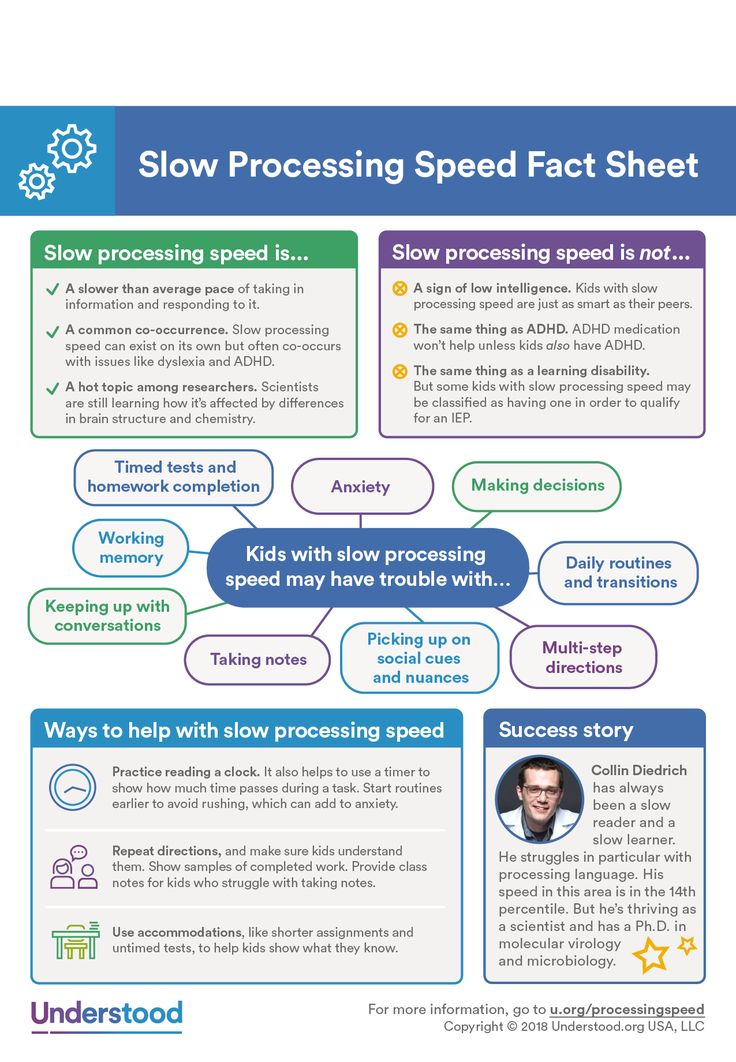 But hyperactive behavior is not a hallmark of ADHD for all children; a better predictor for the development of ADHD is actually a child’s ability to regulate their emotions.
But hyperactive behavior is not a hallmark of ADHD for all children; a better predictor for the development of ADHD is actually a child’s ability to regulate their emotions.
Specifically, early negative emotionality (poor response to stress and a tendency to react with unpleasant emotions) is highly predictive of ADHD. The babies who may be at risk for ADHD are the ones who cry constantly and have trouble self-soothing; who are angry, fussy, and difficult to control; who have problems feeding and falling and/or staying asleep; or who are intolerant of frustration.
[Could Your Child Have ADHD? Take This Self-Test]
Early Signs of ADHD in Toddlers: Intense, Uncontrolled Emotions
When negative emotionality persists into toddlerhood, it looks quite different than a few typical toddler tantrums. Children with ADHD show more aggressive and emotionally intense behaviors when a prize is taken away from them. When presented with challenging tasks, such as puzzles with missing pieces, the young children with ADHD show more frustration, negative expressions, emotional outbursts, and anger than do their neurotypical peers. They are also quicker to give up.2,3,4,5
They are also quicker to give up.2,3,4,5
In short, toddlers and preschoolers with ADHD are overly reactive. Why? Because they feel emotions more deeply and hold on to them longer than do those without ADHD. They overreact with positive emotions, such as excitement, which can mean screaming and jumping for joy over small things (like when my daughter with ADHD ran around the house screaming like a maniac when I told her we were going for ice cream). They also overreact with negative emotions, disappointment, and frustration, which often lead to tantrums or aggressive behaviors.
As neurotypical toddlers reach age 3 or 4 years old, they can begin, for example, to wait until after dinner for ice cream without having a major meltdown (though they may whine a bit if tired or stressed). Preschoolers with ADHD, however, cry or scream regularly over minor situations. “Small deals” are almost always “BIG deals” with these kids, and they show it with their emotional outbursts. Waiting is nearly impossible; they feel extreme pressure to get things now.
Waiting is nearly impossible; they feel extreme pressure to get things now.
Early Signs of ADHD in Toddlers: Emotional Sensitivity and Overwhelm
Toddlers with ADHD tend to be easily frustrated, moody, and even rude. They may worry too much or too long about even the smallest of things and have more difficulty transitioning. They’re also extremely sensitive to corrective feedback – asking them to put on a coat to go outside can result in an angry scream. These children become overwhelmed with their feelings and have a hard time calming down.
[Watch This Video: The Emotionality of ADHD]
Young children with ADHD are also extremely irritable — which can result in whining, demanding, or screaming every request they make — and prone to aggressive and angry outbursts.
In the preschool classroom, students may whine if there are too many kids at the station or center where they want to play. Children without ADHD will generally move to another center.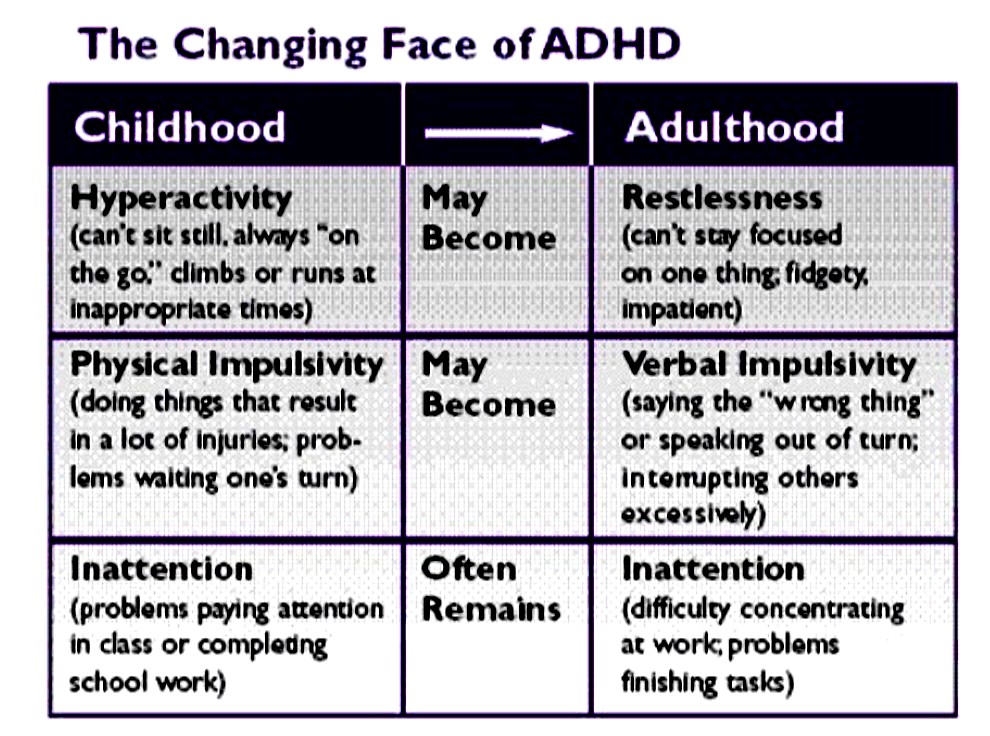 Children with ADHD, however, may drop to the ground screaming or push another child and tell them to leave. And not just once. Instances like these happen over and over. Preschoolers with ADHD tend to be more controlling and react with more hostility, anger, and aggression when upset and are more likely to get calls home than are their non-ADHD peers.
Children with ADHD, however, may drop to the ground screaming or push another child and tell them to leave. And not just once. Instances like these happen over and over. Preschoolers with ADHD tend to be more controlling and react with more hostility, anger, and aggression when upset and are more likely to get calls home than are their non-ADHD peers.
Early Signs of ADHD in Toddlers: Frequent, Severe Tantrums
When upset, young children with ADHD also tend to engage in tantrums that are more frequent, intense, severe, and disruptive than do other children their age. Typically developing toddlers may have weekly tantrums and parents can usually tell why the tantrum is happening (the child is likely tired or doesn’t want to do something).
In toddlers with ADHD, the tantrums occur more frequently, last longer, and seem to come out of nowhere. The child’s reactions are excessive, completely disproportionate to the event, and/or inappropriate to the context. The tantrum can last for 20 minutes or more and the child has trouble calming down on their own and may even retaliate.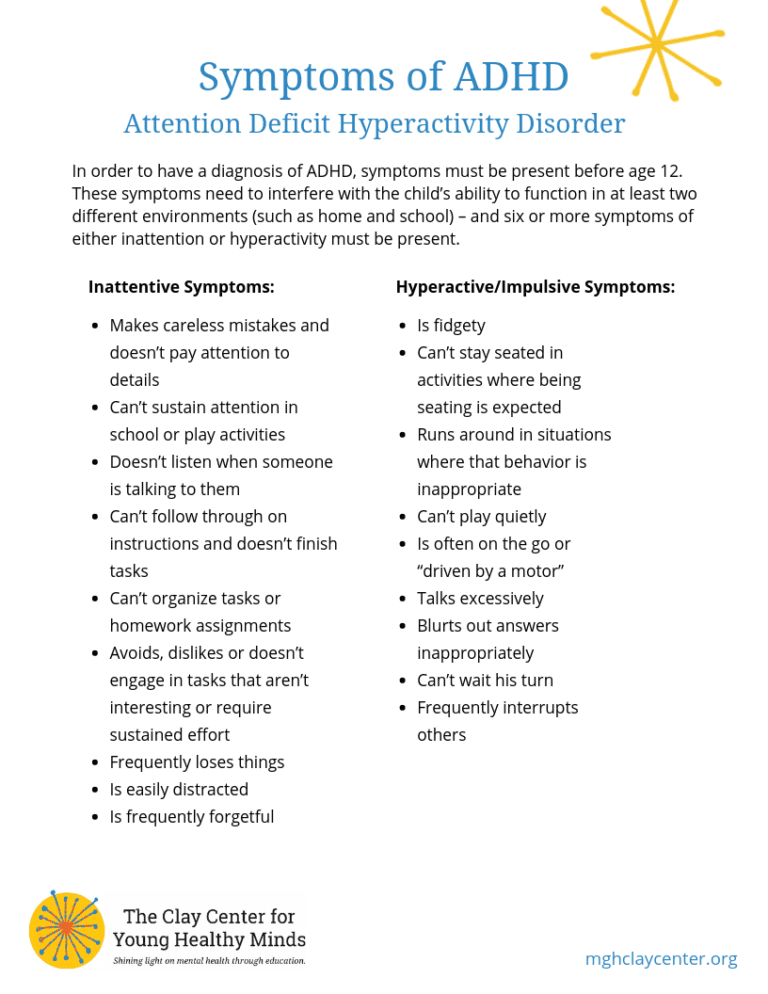 Many will experience “full-blown” tantrums that they have zero control over — even if promised their most favorite thing in the world, they simply cannot stop.
Many will experience “full-blown” tantrums that they have zero control over — even if promised their most favorite thing in the world, they simply cannot stop.
Typical Toddler Behavior
The table below outlines and compares typical toddler behavior and ADHD toddler behavior.
| Behavior | Neurotypical | Possible ADHD |
| Tantrums | 2-3 times/week for less than 15 minutes; frequency and intensity lessens over 6 months | 3+/week for more than 15 minutes at a time; frequency and intensity persist for 6 or more months |
| Aggressive behaviors (e.g., biting) | 1-2 times/month (between 12-36 months) and/or with little expressive language | 36+ months, occurring more than once or twice (i.e., often during tantrums), and/or possess good language skills |
| Self-injury (e.g., bite or hit self, head-banging) | n/a | Occurs at any time |
When children with ADHD become over-stimulated (e.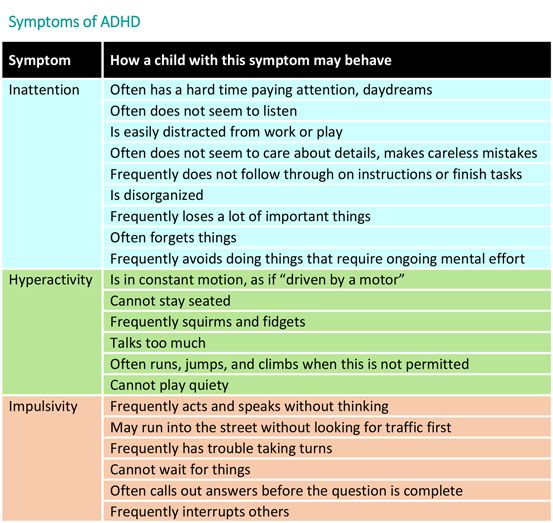 g., busy events or loud environments), their emotional reactions can be even more unpredictable and severe than usual. My daughter had emotional meltdowns at birthday parties and the worst of them always occurred at her own parties. It was just way too over-stimulating for her and resulted in screams, cries, throwing things, and demanding that everyone leave at once. She spent most of her fourth birthday party alone in her room while I led activities for her friends.
g., busy events or loud environments), their emotional reactions can be even more unpredictable and severe than usual. My daughter had emotional meltdowns at birthday parties and the worst of them always occurred at her own parties. It was just way too over-stimulating for her and resulted in screams, cries, throwing things, and demanding that everyone leave at once. She spent most of her fourth birthday party alone in her room while I led activities for her friends.
Early Signs of ADHD in Toddlers: My Daughter’s Early Symptoms
Unfortunately, these youngsters typically receive a lot of negative feedback for their behaviors, which can contribute to low self-esteem, anxiety, and even depression. My daughter developed significant anxiety by the time she started school. She was the typical active child with ADHD early on. She developed all her motor skills early and was walking with a push car by the time other babies were just learning to crawl. She literally ran circles around the other babies and when she learned to talk, she didn’t stop (until she became a teenager).
Naps ended early and we gave them up completely when she was 14 months, otherwise, she wouldn’t sleep at night. Even then I wondered how much she slept. We had to switch her to a “big girl” bed because she constantly climbed out of her crib. Because we couldn’t keep her contained, we would hear her banging around all night in her room. We removed her toys, but she amused herself by climbing the shelves in her closet. On more than one occasion, I found her in the morning sleeping in the closet.
She was also a terrible eater who somehow grew normally though I was convinced she was starving because she couldn’t stop to nurse for more than two minutes at a time. She was way too impatient and needed to constantly look around the room.
And her emotional meltdowns? Epic.
I remember telling friends and family that the Terrible Twos were way worse than I had ever imagined (or saw based on my friends’ kids). I knew that behavior problems tend to peak at 2 years and then decline as they get older, but I found my daughter’s 3s were worse than her 2s. And, when I thought it just had to get better, the behaviors continued when she turned 4…. When was it going to stop!?
Many parents fall into this trap of waiting for behaviors to improve. Though it was clear my daughter was quite different from other kids, everyone told me to wait. They said she was just an active, imaginative, gifted child. So, we waited.
While we waited for the hyperactive behaviors to go away, we overlooked the fact that she should have started showing more emotional control by the time she was 3. She was just a sensitive girl! More excuses. And then we ended up waiting too long. She continued to lash out emotionally, which interfered with her ability to build friendships and her self-esteem plummeted.
Early Signs of ADHD in Toddlers: Critical Parental Supports
I cannot overstress the importance of early intervention. Children who display emotional dysregulation — less frustration tolerance, more anger — are at great risk. And the more severe their anger outbursts, the more severe their ADHD symptoms tend to be. Similarly, dysregulated happiness is associated with greater inattention.6 Worse still, only about 40-50 percent of young children with ADHD receive the early intervention behavioral support they need.
It’s important to know the early warning signs so we can help these kids as quickly as possible. Do not wait to see what happens. Begin logging your observations and concerns as soon as your baby is born. What’s fascinating is that babies actually start to show the ability to regulate their emotions within months of being born. For example, babies learn to look away from things that are upsetting them to self-soothe and control anger, frustration, and upset. Children with ADHD did not do those things as babies.
As they move into preschool and their language capacity grows, typically developing children can better regulate their emotions and begin to respond to situations with flexibility and in socially appropriate ways. Children with ADHD, on the other hand, continue to have trouble managing challenging situations and reducing their distress. They cannot cope with negative emotions effectively and continue to vent (verbally or physically), show aggression, or engage in more avoidance behaviors to try and self-regulate.
Early Signs of ADHD in Toddlers: 5 Complements to Behavior Therapy
Our emotion systems develop earlier than our control systems. What’s more, the emotional brain is much stronger than the thinking brain (the one that helps us keep cool and make good behavioral choices). This means we must start supporting our kids by tapping into their emotional brain very early.
The National Institute of Mental Health (NIMH) funded the Preschool ADHD Treatment Study (PATS) assesses the short- and long-term efficacy and safety of methylphenidate (Ritalin) in preschoolers (ages 3-5.5 years).7 Before starting the medication trials, all families completed an intensive 10-week behavioral therapy program, which included counseling supports for parents. One of the most significant findings from this study was that one-third of the children showed a significant reduction of ADHD symptoms after the behavior therapy program and, therefore, did not need to also receive medications. From that study, researchers concluded that behavior interventions designed to reduce symptoms of ADHD in preschoolers should be the first-line treatment for young children.
The parent training component of behavior therapy is critical because parent behaviors influence children’s’ emotion regulation skills from an early age. Here’s how you can get started today.
1. Understand the ADHD brain. The brain continues to develop throughout childhood – a child’s thinking brain is the last to develop in adulthood. Further, when a child is upset, stress hormones are released into the body and all of the blood rushes out of the rational/thinking/calming part of the brain and into the motor cortex, preparing the body to either fight or run away. The emotional brain automatically takes over at this point, so any talking, scolding, punishing, or lecturing is useless because the brain that reads and interprets those messages is offline.
It’s best to avoid engaging kids when they are upset. Get out of the heat! Give them space but stay close by so they don’t feel you are abandoning them.
2. Form strong bonds. As is true of any child, kids with ADHD benefit from strong caregiver relationships. They need to know they are loved and accepted no matter what. When we have strong bonds, we can strengthen positive and prosocial emotions, which helps with emotion regulation. Capitalize on small moments throughout your day where you can connect with your kids. Very important times are first thing in the morning and at bedtime. During these times, give them your full attention. Say something positive like, “I love seeing your sunshiny face first thing in the morning.” And smile! Always be on your child’s team. Teamwork helps build compassion — another strong prosocial emotion that builds the emotional brain.
3. Be warm and responsive. Parents are most effective in supporting their kids’ emotion regulation skills when they are supportive, sensitive, and warmly responsive to their toddlers’ positive and negative emotions. Instead of reacting emotionally, validate their feelings. Saying “Hey, kiddo, I can see that your sister really upset you” is more helpful then demanding that they stop crying. Then create space to let them talk about what happened if they want to. If they don’t add more, or if they aren’t yet talking, create the space for them to cry, give you a hug, or whatever else they need at the moment. (Save learning about appropriate behaviors for a different time.)
When we validate, we do not tell them “It’s no big deal.” It is a big deal to them and so when we say that we minimize how they feel and send the message that we do not want to hear how they feel. It’s important to calmly acknowledge that they are upset and let them know you are there to help.
Kids react emotionally to create safety but also to be heard. When we create that space for our kids, they feel safe, heard, and understood. Showing empathy will help develop their empathy and they’ll learn they don’t need to react in overly emotional ways.
4. Highlight positive behaviors. Though it may not seem like it, your kids keep their cool all the time — we just take those instances for granted. Capitalize on these times by showing appreciation for doing the very things we want them to do, such as using their words for help or saying they are frustrated (vs. screaming and kicking).
5. Create opportunities. Talking to kids about our rules and expectations about keeping calm is not enough. Still, that is often all we do. We tell them what is expected, we send them off to play, and then we are exasperated when they scream 30 seconds later. Remember: they do not have the cognitive controls to keep it together in the heat of the moment. Instead, create opportunities for them to demonstrate how to ask for help when they are upset instead of getting frustrated and melting down.
Create opportunities for independence. Kids who can learn to problem solve on their own learn to regulate behaviors on their own. What are the things they are fighting with you to do by themselves? It is likely time to let them take ownership.
Create opportunities for mindfulness. We are finding more and more that mindfulness is important for emotion regulation and self-control. No child is too young to practice being mindful. Look for simple moments throughout the day — smell the dandelion they picked. Talk about what we feel and taste. Pet the dog and describe how the fur feels.
Create opportunities to be a team. Feeling like they belong is another crucial part of building the emotional brain and there’s no better way to do this than making them feel like they belong on a team. My daughter is my favorite sidekick for just about everything, from going to the grocery store to walking the dogs to cleaning the bathroom. We talk about how we work together to get things done together as a team so we can go and have fun together. She likes to say, “we make a good team.” And we do.
ADHD in Toddlers: Next Steps
- Read This Next: Is Preschool Too Early to Diagnose ADHD?
- Get the eBook: “What Do I Have? The Big Book of Symptom Tests”
- Think Your Preschooler or Toddler Has ADHD? Ask These Four Questions
View Article Sources
1Subcommittee on Attention-Deficit/Hyperactivity Disorder; Steering Committee on Quality Improvement and Management, Wolraich M, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007‐1022. doi:10.1542/peds.2011-2654
2 Martel MM. Research review: a new perspective on attention-deficit/hyperactivity disorder: emotion dysregulation and trait models. J Child Psychol Psychiatry. 2009;50(9):1042‐1051. doi:10.1111/j.1469-7610.2009.02105.x
3Olson SL, Bates JE, Sandy JM, Schilling EM: Early developmental precursors of impulsive and inattentive behavior: from infancy to middle childhood. J Child Psychol Psychiatry 2002; 43:435–447
4Shaw, P., Stringaris, A., Nigg., J., Leibenluft, E. (2014). Emotion dysregulation in Attention Deficit Hyperactivity Disorder. The American Journal of Psychiatry, 171, 176-293.
5 Steinberg EA, Drabick DA. A Developmental Psychopathology Perspective on ADHD and Comorbid Conditions: The Role of Emotion Regulation. Child Psychiatry Hum Dev. 2015;46(6):951‐966. doi:10.1007/s10578-015-0534-2
6O’Neill S, Rajendran K, Mahbubani SM, Halperin JM. Preschool Predictors of ADHD Symptoms and Impairment During Childhood and Adolescence. Current Psychiatry Reports. 2017 Oct;19(12):95. DOI: 10.1007/s11920-017-0853-z.
7Riddle MA, Yershova K, Lazzaretto D, et al. The Preschool Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS) 6-year follow-up. J Am Acad Child Adolesc Psychiatry. 2013;52(3):264‐278.e2. doi:10.1016/j.jaac.2012.12.007
SUPPORT ADDITUDE
To support ADDitude’s mission of providing ADHD education and support, please consider subscribing. Your readership and support help make our content and outreach possible. Thank you.
Previous Article Next Article
Attention deficit hyperactivity disorder (ADHD) in children - description of the disease, causes, symptoms
Attention deficit hyperactivity disorder (ADHD) is a condition in which a child's activity and excitability exceed the norm.
Causes
- Pregnancy complications: toxicosis, high blood pressure, intrauterine fetal asphyxia.
- Violations of the normal lifestyle of a pregnant woman: difficult working conditions and bad habits, such as smoking.
- Complications of the course of labor: prolonged or, conversely, rapid labor.
Symptoms almost always appear between 2 and 3 years of age. The average age of going to the doctor is 8-10 years: at this age, study and housework begin to require independence and concentration from the child.
Symptoms
- Restlessness, fussiness, restlessness.
- Impulsivity, emotional instability, tearfulness.
- Ignoring the rules and norms of behavior.
- Sleep problems.
- Delayed speech development.
- Tendency to perform simultaneously without completing several tasks at once.
Suspecting such violations in a child at any age, parents should definitely consult a neurologist for an examination, since sometimes the cause of hyperactive behavior in a child is another, more severe disease.
Of the additional methods, electro- and echoencephalography are used, in some cases - computed tomography, electroneuromyography, emission spectrometry, etc.
Prophylaxis
Correction of ADHD should include a set of techniques, i.e. be multimodal. The main directions are: physical activity, psychological and pedagogical correction, family psychotherapy, behavioral therapy, relaxation techniques, treatment of comorbidities.
More about pediatric neurology at the YugMed clinic
By leaving your personal data, you give your voluntary consent to the processing of your personal data. Personal data refers to any information relating to you as a subject of personal data (name, date of birth, city of residence, address, contact phone number, email address, occupation, etc.). Your consent extends to the implementation by the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention "YugMed" of any actions in relation to your personal data that may be necessary for the collection, systematization, storage, clarification (updating, changing), processing (for example, sending letters or making calls), etc. subject to current legislation. Consent to the processing of personal data is given without a time limit, but can be withdrawn by you (it is enough to inform the Limited Liability Company Scientific and Production Association "Volgograd Center for Disease Prevention" YugMed "). By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data".
causes, symptoms, signs, diagnosis, treatment of attention deficit hyperactivity disorder in children and adults
Symptoms of ADHD in children
Causes of pathology
Diagnosis
Treatment methods for ADHD
Prevention
Today, more and more children are being diagnosed with ADHD (Attention Deficit Hyperactivity Disorder). As a rule, it is diagnosed in children aged 6-8 years, when the child goes to school. It is at this time that it becomes obvious that the child has pronounced problems with behavior and perception of information.
ADHD is a neurological-behavioral developmental disorder. Pathology makes itself felt in childhood, but in the absence of timely therapy, it can persist into adulthood. According to statistics, ADHD is most common in boys, but can also occur in girls. If the pathology is not diagnosed and treated in a timely manner, this is fraught with poor school performance, the child may develop serious social problems, which increases the risk of substance abuse in the future.
Symptoms of ADHD in children
Consider some of the signs that may signal ADHD in children:
- The child is constantly distracted, inattentive, when communicating with him there is a feeling that he is not listening to you.
- It is difficult for him to keep his attention on the teacher's words for a long time, because of which the understanding of information also suffers.
- Increased activity is observed - the child literally cannot sit in one place. Even during school hours, he can get up and walk around the classroom.
- The child is impatient, cannot wait for his turn, constantly interrupts, answers questions without waiting for them to finish.
- Children with ADHD are characterized by emotional instability, which can be manifested by frequent mood swings: a child can suddenly become irritable, tearful, and restless for no reason.
- Lack of concentration is characteristic - children with this diagnosis often lose their belongings (for example, school supplies, money, keys).
- Problems with sleep and appetite, with daily routine.
Additionally, some neurological abnormalities may be observed. For example, a child with ADHD may have poor motor coordination, resulting in some clumsiness. Also, in some cases, twitching of the facial muscles and trembling of the limbs are observed.
The first signs of attention deficit hyperactivity disorder are observed at the age of 2-3 years, but at this age it is difficult to determine whether they are a manifestation of pathology or normal age-related features.
However, if by the age of 6-8 years the child has not become more attentive and collected, this is an alarming sign that makes it possible to assume ADHD with a high degree of probability. That is why, if you have the above symptoms, you should definitely consult a doctor and start treatment.
Causes of pathology
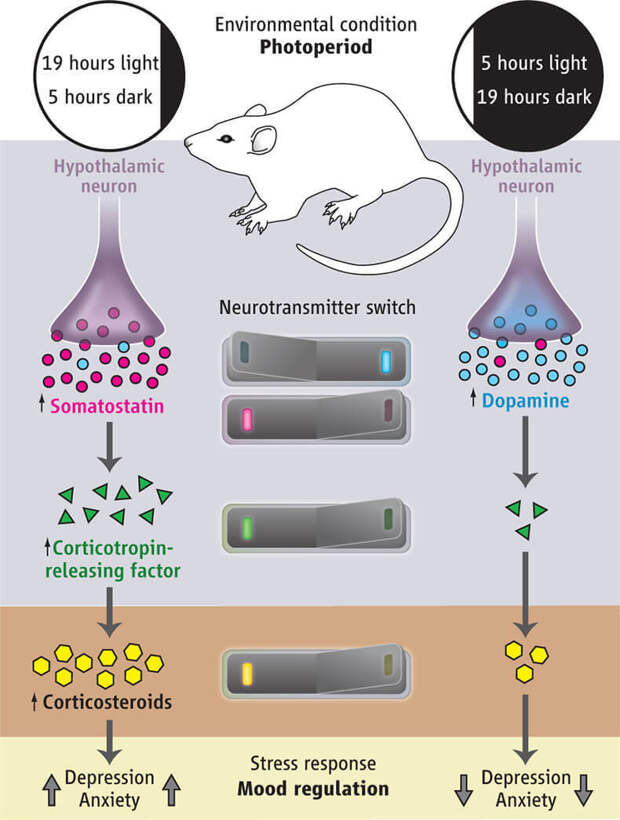
There is no single reason for the development of ADHD. Many experts agree that the most common cause may be genetic mutations that lead to a disruption in the production of dopamine and the work of dopamine receptors.
Also, the causes of the development of attention deficit hyperactivity disorder may be the following factors:
- Severe pregnancy, complicated delivery, including prolonged or rapid.
- Use by the expectant mother during pregnancy of potent drugs, alcoholic beverages, toxic substances.
- Serious pathologies suffered by a child at an early age, including craniocerebral trauma.
- Psychological trauma in a child.
- Fetal asphyxia.
It is also worth noting that this pathology has a hereditary predisposition. It was found that the presence of ADHD in parents significantly increases the likelihood of developing this syndrome in a child.
Diagnostics
The diagnosis of ADHD is not established only on the basis of existing complaints. To accurately confirm the diagnosis, it is necessary to conduct some examinations. First of all, you need to visit a neurologist, psychiatrist and psychologist.
During the consultation, the doctor collects an anamnesis, conducts various tests, conversations, and diagnostic surveys.
In order to identify the cause of the development of ADHD, consultations with other specialists may also be required, as well as instrumental and laboratory examination methods, such as: EEG, MRI of the brain, general and biochemical blood tests.
Treatments for ADHD
It should be noted that attention deficit hyperactivity disorder most often has a favorable prognosis (provided that therapy is started in a timely manner). It is possible to significantly improve the behavior and learning of the child.
Depending on the severity of the pathological process and the causes of its occurrence, the doctor may prescribe such types of treatment as:
- Medical treatment: the patient may be prescribed sedatives, antidepressants, neurostimulants.
- Cognitive behavioral therapy.
- A clear daily routine: a balanced diet, good sleep.
- Family therapy: if there are conflicts in the family, ADHD often develops against this background.
- Biofeedback therapy: this method of treatment is aimed at training the child's ability to self-regulate their conditions with the help of computer game tasks.
- Physiotherapy techniques, eg massage, exercise, kinesiotherapy.
Additionally, other methods of treatment can be used.
Prophylaxis
Unfortunately, it is not always possible to prevent the development of ADHD. However, there are some factors that significantly reduce the risk of developing pathology. For example, the expectant mother should follow a healthy lifestyle, eat a balanced diet, give up bad habits. Before conception, it is desirable to undergo a complete examination, if necessary, to pre-treat existing pathologies.
Also, as a prevention of ADHD, the following recommendations should be observed:
- The child should be active, walk outdoors more often.
- The regimen of the day and meals must be clear.
- Monitor the child's behavior, immediately stop unacceptable behavior on his part.
- It is very important to build a trusting relationship between parents and children.
- Family conflicts should be avoided.
At the first signs of ADHD, it is recommended to contact specialists who will help minimize the risk of developing more serious pathologies in the future.
You can learn more about the treatment of attention deficit hyperactivity disorder at a face-to-face appointment with a doctor. Be healthy!
Author of the article:
Markelov Gleb Vladimirovich
neurologist, online consultations
work experience 4 years
reviews Leave a review
Clinic
m. Sukharevskaya
Reviews
Services
- Title
- Appointment, consultation of a neurologist primary 2300
- Appointment, consultation of a neurologist repeated1900
Health articles
All articlesAllergistGastroenterologistHematologistGynecologistDermatologistImmunologistInfectionistCardiologistENT doctor (otolaryngologist)MammologistNeurologistNephrologistOncologistOphthalmologistProctologistPsychotherapistPulmonologistRheumatologistTraumatologist-orthopedistTrichologistUrologistPhlebologistSurgeonEndocrinologist 905 years.Dmitrieva Olga Nikolaevna
Chief physician of "Polyclinika.ru" on Frunzenskaya, neurologist, ENMG specialist
reviews
Clinic
m. Frunzenskaya
Sumina Evgenia Yurievna
Head physician "Polyanka.ru" on Polyanka, neurologist
reviews
Clinic
m. Polyanka
Demina Evgenia Sergeevna
neurologist, reflexologist, ENMG specialist
reviews Make an appointment
Clinic
m. Sukharevskaya
Kuzmina Irina Vladimirovna
neurologist, reflexologist, hirudotherapist
reviews Make an appointment
Clinic
m. Street 1905 year
Shcherbenkova Alina Lvovna
neurologist, specialist in ENMG, KMN
reviews Make an appointment
Clinic
m. Frunzenskaya
Agayeva Takhmina Khanovna
neurologist
reviews Make an appointment
Clinic
m. Polyanka
Alexandrova Tatyana Sergeevna
neurologist
reviews Make an appointment
Clinic
m.