Acute stress syndrome
Acute Stress Disorder - Mental Health Disorders
By
John W. Barnhill
, MD, New York-Presbyterian Hospital
Full review/revision Apr 2020 | Modified Sep 2022
VIEW PROFESSIONAL VERSION
Acute stress disorder is an intense, unpleasant, and dysfunctional reaction beginning shortly after an overwhelming traumatic event and lasting less than a month. If symptoms persist longer than a month, people are diagnosed as having posttraumatic stress disorder Posttraumatic Stress Disorder (PTSD) Posttraumatic stress disorder (PTSD) involves intense, unpleasant, and dysfunctional reactions beginning after an overwhelming traumatic event. Events that threaten death or serious injury can... read more (PTSD).
(See also Overview of Trauma- and Stress-Related Disorders Overview of Trauma- and Stress-Related Disorders Trauma- and stress-related disorders result from exposure to a traumatic or stressful event. Specific disorders include acute stress disorder and posttraumatic stress disorder. These disorders... read more .)
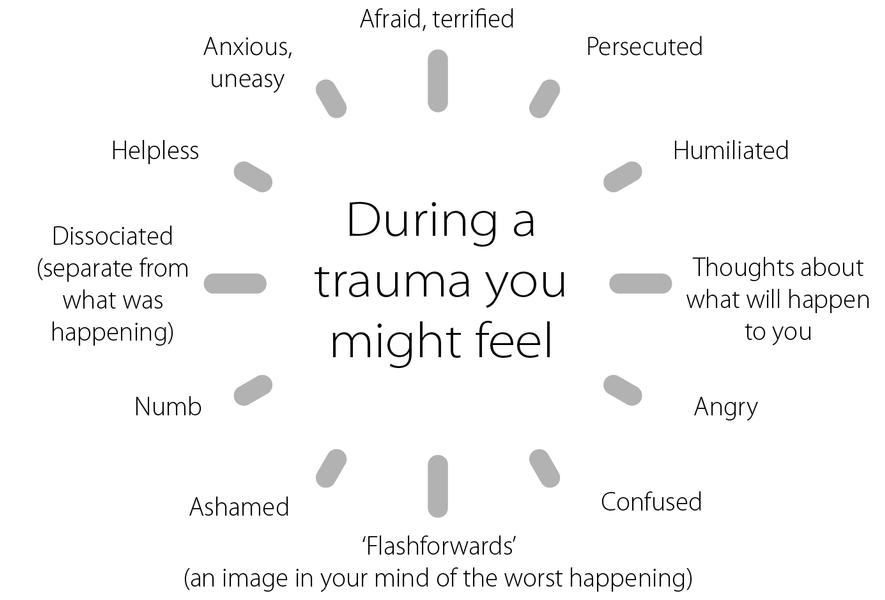
People with acute stress disorder have been exposed to a terrifying event. They may experience it directly or indirectly. For example, direct exposure may involve experiencing serious injury, violence, or the threat of death. Indirect exposure may involve witnessing events happening to others or learning of events that occurred to close family members or friends. People mentally re-experience the traumatic event, avoid things that remind them of it, and have increased anxiety.
People with this disorder may have dissociative symptoms Overview of Dissociative Disorders Occasionally everyone has minor problems integrating their memories, perceptions, identity, and consciousness. For example, people may drive somewhere and then realize that they do not remember... read more . For example, they may feel emotionally numb or disconnected from themselves. They may feel that they are not real.
They may feel that they are not real.
The number of people with acute stress disorder is unknown. The likelihood of developing acute stress disorder is greater when traumatic events are severe or recurrent.
Acute stress disorder is diagnosed when people have been
In addition, they also must have had at least 9 of the following symptoms for 3 days up to 1 month:
Recurring, uncontrollable, and intrusive distressing memories of the event
Recurring distressing dreams of the event
Feelings that the traumatic event is recurring—for example, in flashbacks
Intense psychologic or physical distress when reminded of the event (for example, by entering a similar location, or by sounds similar to those heard during the event)
A persistent inability to experience positive emotions (such as happiness, satisfaction, or loving feelings)
An altered sense of reality (for example, feeling in a daze or as if time has slowed)
Memory loss for an important part of the traumatic event
Efforts to avoid distressing memories, thoughts, or feelings associated with the event
Efforts to avoid external reminders (people, places, conversations, activities, objects, and situations) associated with the event
Disturbed sleep
Irritability or angry outbursts
Excessive attention to the possibility of danger (hypervigilance)
Difficulty concentrating
An exaggerated response to loud noises, sudden movements, or other stimuli (startle response)
In addition, symptoms must cause significant distress or significantly impair functioning.
Doctors also check to see whether symptoms could result from use of a drug or another disorder.
- Self-care
Supportive measures
Many people recover from acute stress disorder once they are removed from the traumatic situation and given appropriate support in the form of understanding, empathy for their distress, and an opportunity to describe what happened and their reaction to it. Some people benefit from describing their experience several times. Friends and loved ones can often provide this support. Otherwise, doctors or other health care professionals are helpful.
Sometimes doctors temporarily give drugs to relieve anxiety or help people sleep, but other drugs (such as antidepressants) are usually not given.
Self-care is crucial during and after a crisis or trauma. Self-care can be divided into 3 components:
Personal safety
Physical health
Mindfulness
Personal safety is fundamental. After a single traumatic episode, people are better able to process the experience when they know that they and their loved ones are safe. It can be difficult, however, to gain complete safety during ongoing crises such as domestic abuse, war, or an infectious pandemic. During such ongoing difficulties, people should seek the guidance of experts on how they and their loved ones can be as safe as possible.
After a single traumatic episode, people are better able to process the experience when they know that they and their loved ones are safe. It can be difficult, however, to gain complete safety during ongoing crises such as domestic abuse, war, or an infectious pandemic. During such ongoing difficulties, people should seek the guidance of experts on how they and their loved ones can be as safe as possible.
Physical health can be put at risk during and after traumatic experiences. Everyone should try to maintain a healthy schedule of eating, sleeping, and exercise. Drugs that sedate and intoxicate (for example, alcohol) should be used sparingly, if at all.
A mindful approach to self-care aims to reduce the feelings of stress, boredom, anger, sadness, and isolation that traumatized people normally experience. If circumstances allow, at-risk individuals should make and follow a daily normal daily schedule, for example, get up, shower, get dressed, go outside and take a walk, and prepare and eat regular meals.
It is useful to practice familiar hobbies as well as activities that sound fun and distracting: draw a picture, watch a movie, or cook.
Community involvement can be crucial, even if it is difficult to maintain human connection during a crisis.
Stretching and exercise are terrific, but it can be equally helpful to sit still and count one's own breaths or listen carefully for surrounding sounds. People can become preoccupied with the trauma or crisis, and so it is useful to choose to think of other things: read a novel or get engaged with a puzzle. Unpleasant emotions may typically feel "frozen" during and after a trauma, and it can be a relief to find activities that shift the feeling state: laugh, watch a fun movie, do something silly, or draw with crayons. Under stress, people can become short-tempered, even with people they care about.
Spontaneous kindness can be a win/win solution for everyone: sending a nice note, making someone cookies, and offering up a smile may not only be a nice surprise for the recipient, but they can reduce the hopelessness and passivity that tends to be part of the sender's experience of trauma.
VIEW PROFESSIONAL VERSION
Copyright © 2023 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Acute Stress Disorder: Causes, Symptoms, and Diagnosis
Acute Stress Disorder: Causes, Symptoms, and Diagnosis- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Timothy J. Legg, PhD, PsyD — By Rose Kivi — Updated on Sep 29, 2018
Legg, PhD, PsyD — By Rose Kivi — Updated on Sep 29, 2018
Acute stress disorder (ASD) typically occurs within one month of a traumatic event. Symptoms are similar to those seen in post traumatic stress disorder (PTSD), however this disorder is temporary, lasing from a few days to a month. Some people with this disorder can go on to develop PTSD.
What’s acute stress disorder?
In the weeks after a traumatic event, you may develop an anxiety disorder called acute stress disorder (ASD). ASD typically occurs within one month of a traumatic event. It lasts at least three days and can persist for up to one month. People with ASD have symptoms similar to those seen in post-traumatic stress disorder (PTSD).
Experiencing, witnessing, or being confronted with one or more traumatic events can cause ASD. The events create intense fear, horror, or helplessness. Traumatic events that can cause ASD include a:
- death
- threat of death to oneself or others
- threat of serious injury to oneself or others
- threat to the physical integrity of oneself or others
Approximately 6 to 33 percent of people who experience a traumatic event develop ASD, according to the U. S. Department of Veterans Affairs. This rate varies based on the nature of the traumatic situation.
S. Department of Veterans Affairs. This rate varies based on the nature of the traumatic situation.
Anyone can develop ASD after a traumatic event. You may have an increased risk of developing ASD if you have:
- experienced, witnessed, or been confronted with a traumatic event in the past
- a history of ASD or PTSD
- a history of certain types of mental problems
- a history of dissociative symptoms during traumatic events
The symptoms of ASD include:
Dissociative symptoms
You’ll have three or more of the following dissociative symptoms if you have ASD:
- feeling numb, detached, or being emotionally unresponsive
- a reduced awareness of your surroundings
- derealization, which occurs when your environment seems strange or unreal to you
- depersonalization, which occurs when your thoughts or emotions don’t seem real or don’t seem like they belong to you
- dissociative amnesia, which occurs when you cannot remember one or more important aspects of the traumatic event
Reexperiencing the traumatic event
You’ll persistently re-experience the traumatic event in one or more of the following ways if you have ASD:
- having recurring images, thoughts, nightmares, illusions, or flashback episodes of the traumatic event
- feeling like you’re reliving the traumatic event
- feeling distressed when something reminds you of the traumatic event
Avoidance
You may avoid stimuli that cause you to remember or re-experience the traumatic event, such as:
- people
- conversations
- places
- objects
- activities
- thoughts
- feelings
Anxiety or increased arousal
The symptoms of ASD may include anxiety and increased arousal. The symptoms of anxiety and increased arousal include:
The symptoms of anxiety and increased arousal include:
- having trouble sleeping
- being irritable
- having difficulty concentrating
- being unable to stop moving or sit still
- being constantly tense or on guard
- becoming startled too easily or at inappropriate times
Distress
The symptoms of ASD may cause you distress or disrupt important aspects of your life, such as your social or work settings. You may have an inability to start or complete necessary tasks, or an inability to tell others about the traumatic event.
Your primary doctor or mental healthcare provider will diagnose ASD by asking you questions about the traumatic event and your symptoms. It’s also important to rule out other causes such as:
- drug abuse
- side effects of medications
- health problems
- other psychiatric disorders
If you don’t already have a primary care doctor or a mental healthcare professional, you can browse doctors in your area through the Healthline FindCare tool.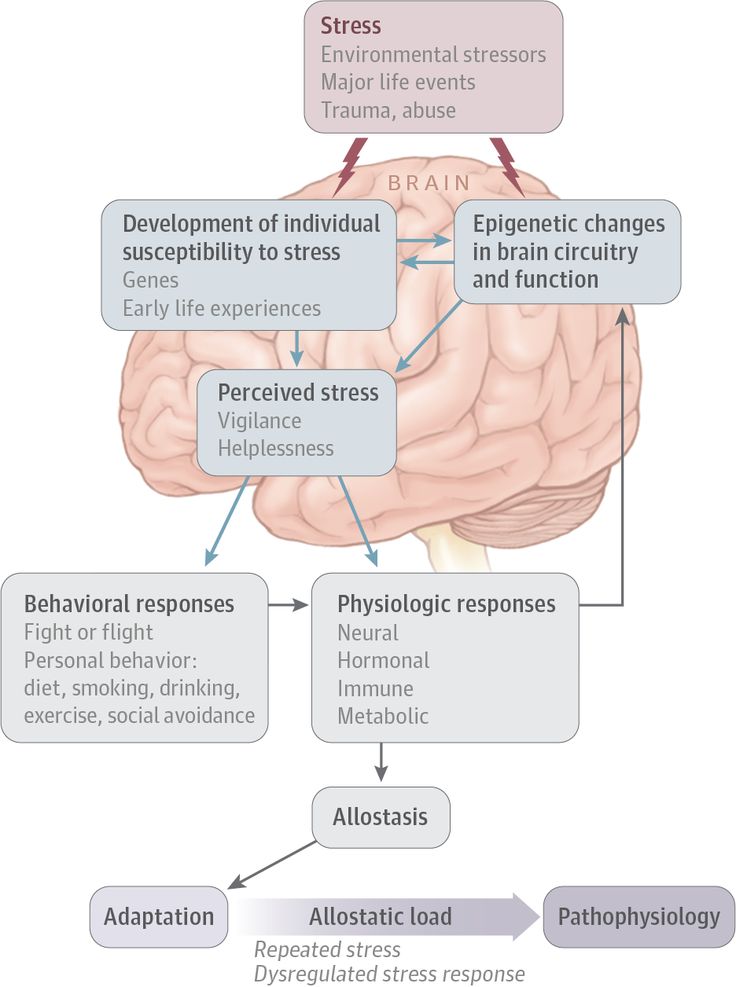
Your doctor may use one or more of the following methods to treat ASD:
- a psychiatric evaluation to determine your specific needs
- hospitalization if you’re at risk of suicide or harming others
- assistance in obtaining shelter, food, clothing, and locating family, if necessary
- psychiatric education to teach you about your disorder
- medication to relieve symptoms of ASD, such as antianxiety medications, selective serotonin reuptake inhibitors (SSRIs), and antidepressants
- cognitive behavioral therapy (CBT), which may increase recovery speed and prevent ASD from turning into PTSD
- exposure-based therapies
- hypnotherapy
Online therapy options
Read our review of the best online therapy options to find the right fit for you.
Many people with ASD are later diagnosed with PTSD. A diagnosis of PTSD is made if your symptoms persist for more than a month and cause a significant amount of stress and difficulty functioning.
Treatment may reduce your chances of developing PTSD. Approximately 50 percent of PTSD cases resolve within six months, whereas others may persist for years.
Because there’s no way to ensure that you never experience a traumatic situation, there’s no way to prevent ASD. However, there are things that can be done to reduce your likelihood of developing ASD.
Getting medical treatment within a few hours of experiencing a traumatic event may reduce the likelihood that you’ll develop ASD. People who work in jobs that carry a high risk for traumatic events, such as military personnel, may benefit from preparation training and counseling to reduce their risk of developing ASD or PSTD if a traumatic event does occur. Preparation training and counseling may involve fake enactments of traumatic events and counseling to strengthen coping mechanisms.
Last medically reviewed on November 28, 2017
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Acute stress disorder. (2015).
ptsd.va.gov/public/problems/acute-stress-disorder.asp - American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington, DC: American Psychiatric Association.
- Gibson LE. (2016). Acute stress disorder.
ptsd.va.gov/professional/treatment/early/acute-stress-disorder.asp - McFarlane AC. (2010). The long-term costs of traumatic stress: Intertwined physical and psychological consequences. DOI:
doi.org/10.1002/j.2051-5545.2010.tb00254.x - Ursano RJ, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. (2010).
psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd. pdf
pdf
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Sep 29, 2018
Written By
Rose Kivi
Edited By
Frank Crooks
Nov 28, 2017
Medically Reviewed By
Timothy J. Legg, PhD, PsyD
Share this article
Medically reviewed by Timothy J. Legg, PhD, PsyD — By Rose Kivi — Updated on Sep 29, 2018
Read this next
Traumatic Events
Medically reviewed by Matthew Boland, PhD
Traumatic events can cause physical, emotional, or psychological, harm. Learn how to cope and when you should talk with a professional.
READ MORE
Post-Traumatic Stress Disorder (PTSD)
Medically reviewed by Kendra Kubala, PsyD
Post-traumatic stress disorder (PTSD) occurs after experiencing or witnessing a traumatic event.
 Learn more about who’s most at risk and available…
Learn more about who’s most at risk and available…READ MORE
Drugs to Treat Anxiety Disorder
Medically reviewed by Rebecca Barnhart, PharmD, BCPP
Most people feel anxious at some point in their lives, and the feeling often goes away by itself. An anxiety disorder is different.
READ MORE
Sleep Disorders: How Parental Stress Can Rise With Family Sleeping Difficulties
Researchers say poor sleep quality in adults as well as children can increase the stress levels of parents. Here's some tips on better sleep for the…
READ MORE
Can Stress Cause Low Sodium Levels?
The effects of stress on sodium levels may vary from person to person. And there’s not yet enough evidence to determine cause and effect.
READ MORE
How Can You Measure Stress?
Not sure if your stress levels are healthy? There are several stress trackers available.
READ MORE
How to Cover Up a Cold Sore, with and Without Makeup
Medically reviewed by Cynthia Cobb, DNP, APRN, WHNP-BC, FAANP
Cold sores often show up when we are the busiest, so it's only natural to wonder how to cover up a cold sore when you're leaving the house. Here are a…
READ MORE
Stress and post-traumatic condition in children
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the website
Other services of the section "Psychology"
- Child psychologist consultation
- Complete diagnosis of the child's mental health (Joint appointment with a neurologist, psychologist, psychiatrist)
Surveys
- Diagnostic session
- Course of psychological correction / psychotherapy
Frequent calls
- Family problems
- The appearance of the baby in the family
- "No one is friends with me!" - Difficulty communicating with peers
- "Again deuce" - learning difficulties, conflicts with teachers
- “I won’t go to kindergarten / school anymore!” - difficulty adapting
- Career guidance for teenagers
- Psychosomatic disorders in children
- Emotional difficulties in children
- Transitional age (crisis of 3 years, school, teenage difficulties)
- Addictions in children and adolescents
- Panic attacks in children
Online payment
Documents online
Online services
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal reaction
for severe traumatic events.
This booklet deals with symptoms,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident.
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died and I survived.
- I sleep badly and experience muscle tension.

PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It's not your fault that you got sick and you shouldn't suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event. you try to hold on away from anything that might remind you of the experience.
you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last?
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this disease?
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men. The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
What other conditions can accompany PTSD?
Comorbid depression, alcohol and drug addiction, or other common anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD.
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What can I do to help myself in this situation?
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
Ask your doctor if he has previously had patients suffering from post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medication to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work.
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
Experts say PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.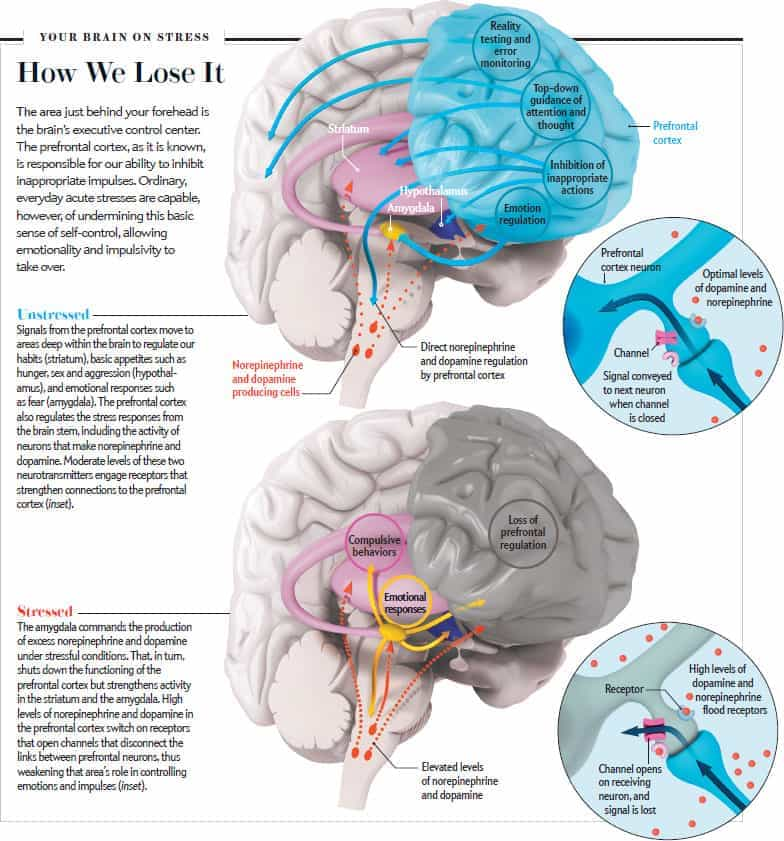
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear. The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on the genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
GRP (gastrin-releasing peptide/ GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). 4
The storage of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
Research on PTSD
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate.
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH researchers found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug.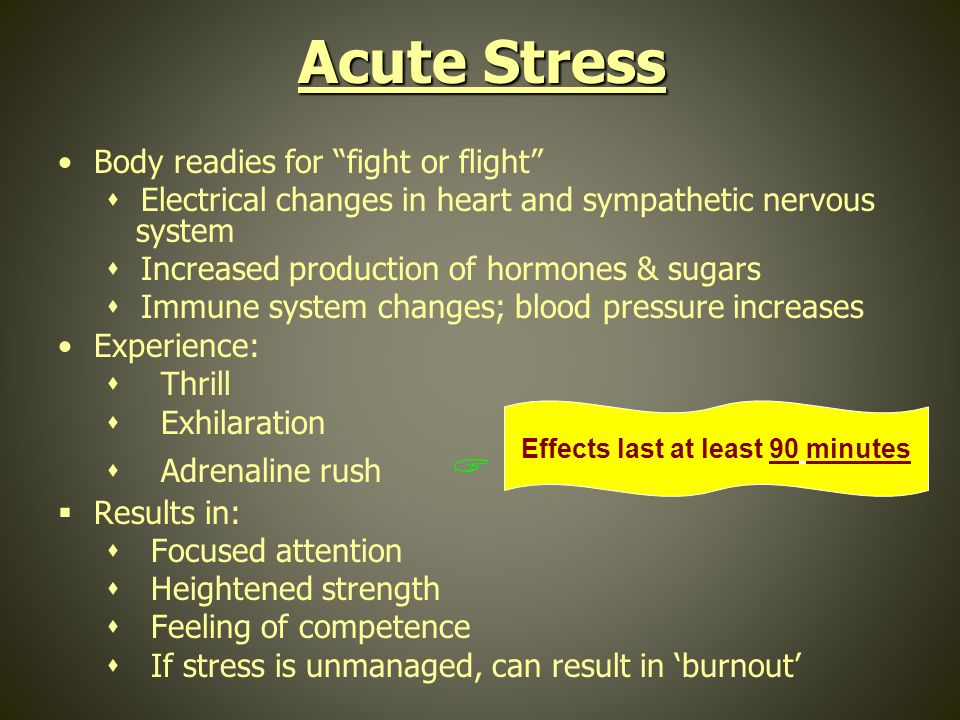 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal.
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease. During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: [email protected]
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www. ncptsd.va.gov
ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction. Nature. Nov 7 2002;420(6911):70-74.
- 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus.
 Nat Neurosci. Mar 2005;8(3):365-371.
Nat Neurosci. Mar 2005;8(3):365-371. - Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711.
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder. Biol Psychiatry. Feb 3 2006.
- Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear.
 Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
Arch Gen Psychiatry. Nov 2004;61(11):1136-1144. - Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634.
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Division of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Department of Mental Health
Department of Public Relations and Outreach]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.