Warped sense of reality
Psychotic disorders | Mental health issues
Psychotic disorders or episodes arise when a person experiences a significantly altered or distorted perception of reality. Such distortions are often caused or triggered by hallucinations (false perceptions), delusions (false beliefs) and/or disrupted or disorganised thinking. Psychotic disorders are relatively common in young people, with around two in every 100 young adults experiencing some form of psychotic episode.
Signs this might be a problem:
- withdrawal from family and friends
- inability to maintain employment or engage in studies
- confusion
- confused speech
- inappropriate or erratic behaviour and reactions
- hearing voices when alone or that others cannot hear
- mood swings.
What is psychosis?
Psychosis is characterised by some sense of distorted reality. A psychotic episode may include many so-called 'positive symptoms; which include:
- Hallucinations: seeing, hearing, feeling sensations that are not actually occurring
- Delusions: believing in false realities, such as having superpowers.
Delusions may be also paranoid beliefs, such as thinking you're being watched or followed
- Thought disorder: characterized by jumbled or disorganised thoughts.
Negative symptoms include: Depressed or flattened mood. Difficulty engaging in conversation, such as difficulty following others or putting sentences together coherently, or engaging in unprompted or indirect speech.
Psychotic symptoms can be due to a psychotic disorder, but can also be caused by some drugs and prescription medications, or occasionally by medical conditions.
What are psychotic disorders?
Psychotic disorders cover a range of disorders and have a range of associated symptoms. Essentially psychotic disorders are those which involve some form of altered/distorted perception of reality that is persistent for a considerable period of time and interferes with daily functioning. As many as three in every 100 people will experience some form of a psychotic episode during their lifetime, and the first experience of psychosis most commonly occurs between the ages of 15-30 years.
Psychotic episodes can occur as an isolated event but are frequently an indication/symptom of an underlying psychotic disorder or mental health problem. Although psychotic disorders are not entirely understood, some risk factors associated include; a family history of psychotic disorders or episodes (especially schizophrenia) and drug use, specifically hallucinogenic drugs, amphetamines and cannabis. Stressful life events may trigger the onset of a psychotic episode.
The most common psychotic disorders include:
Schizophrenia
Schizophrenia is a psychotic illness that is considered present when a person suffers psychiatric symptoms (such as hallucinations or delusions) for at least six months (with two or more symptoms present for much of the time over a one month period), with changes in behaviour and interference in daily functioning (e.g. work or education commitments) occurring as a result.
Diagnosis is often complicated because the symptoms experienced can be present in other disorders, and the extent of the symptoms may not be communicated (e. g. people may not want to confide in anyone that they are hearing voices for fear of stigmatisation, or due to paranoid delusions and mistrust of doctors etc).
g. people may not want to confide in anyone that they are hearing voices for fear of stigmatisation, or due to paranoid delusions and mistrust of doctors etc).
Schizophreniform is similar to schizophrenia, only the symptoms have not persisted for six months. Schizoaffective disorder is diagnosed when a person is experiencing symptoms of psychosis and schizophrenia and another mood disorder.
Bipolar disorder
Bipolar is an affective disorder characterised by intense mood swings. People with bipolar often have intense highs (mania or hypomania) which are followed by intense lows (depression or major depressive episode). Not all people with bipolar will experience psychotic symptoms, but some will during the episodes of mania or depression. People in manic episodes may have extreme grandiose feelings, or believe they have unrealistic abilities (such as a guaranteed win in the lottery).
Major depression with psychotic features
Psychotic depression may be present when clinical depression presents with symptoms of psychosis. This is relatively uncommon and typically only occurs with severe depression.
This is relatively uncommon and typically only occurs with severe depression.
What students can do about psychosis
For most people, psychosis can be treated and psychotic disorders can be managed to minimise the occurrence of psychotic episodes. Discussing the situation with a trusted teacher, parent, counsellor or local GP (who can refer to a psychiatrist, if necessary) is an important first step for students worried about psychosis, either for themselves or a friend or relative.
Early treatment for psychosis and psychotic disorders is associated with better treatment outcomes and recovery. Upon consultation with a psychiatrist or GP, medication may be considered the most appropriate course of action, especially if diagnosed with schizophrenia and major depression with psychotic features. Other treatments may involve counselling, education programs focusing on raising awareness about the signs and symptoms associated with psychotic disorders so that they can be recognised at their very onset.
Given stress may trigger a psychotic episode, minimising stress and enhancing coping strategies may be helpful. For people with bipolar, establishing regular sleeping patterns can minimise the onset and/or severity of mood swings and consequently psychotic features. Avoiding drugs, particularly hallucinogenic drugs, cannabis and amphetamines is especially important for people with a history of psychosis.
ReachOut.com resources on psychotic disorders
- What is psychosis?
- What is schizophrenia?
- Bipolar disorder
- How to call a helpline
- What are mental health professionals?
- Psychiatrists
- Ben's experience with unwelcome voices
- Jennifer talks about getting help for schizoaffective disorder
Recommended professional resources
Orygen Youth Health has excellent resources for understanding young people with psychosis and how to help. We recommend:
We recommend:
- Orygen Youth Health: Psychosis + young people
- Orygen Youth Health: How can I help someone with psychosis?
- Orygen Youth Health: Medications for psychosis
What to Do About Early Signs of Psychosis
Brain Health
Author
Kara Gavin
October 12, 2020 12:20 PM
Seeing, hearing or perceiving things that aren’t really there may seem like something to hide, but seeking help early can make a big difference.
Getty Images
Maybe it’s a glimpse of a person that no one else seems to see. Or hearing voices that no one else seems to hear. Or an overwhelming feeling that the innocent gesture of someone on the street actually means something sinister.
These experiences, and others that make it feel like reality is cracking, can be embarrassing, or even frightening.
They can also be the first signs that someone is experiencing a mental health symptom called psychosis.
This means they may be heading for one of several mental health conditions that include it as a symptom, such as bipolar disorder, schizophrenia or schizoaffective disorder. Or in some cases, it may reflect a medical condition.
But if someone gets proper help in the early months of having these experiences – when they can still understand that something’s not right with the way they’re experiencing the world – they may be able to avoid getting worse.
Since these symptoms most often start in the teen and young adult years, when the brain is changing and maturing, early action can make a major difference, says Stephan Taylor, M.D., who leads a team at Michigan Medicine that specializes in early care for psychosis.
And even if someone has already begun to experience more serious signs of psychosis, and threatening to harm themselves or others, modern therapy can still help if those around them help them get care, he says.
Taylor recently spoke about identifying the early signs of psychosis in a live video chat on the Instagram feeds of Michigan Medicine and the University of Michigan. He described the care provided by the Program for Risk Evaluation and Prevention (PREP) Early Psychosis Clinic team, and some of its research studies that are currently seeking volunteers to help uncover the roots of psychosis.
He described the care provided by the Program for Risk Evaluation and Prevention (PREP) Early Psychosis Clinic team, and some of its research studies that are currently seeking volunteers to help uncover the roots of psychosis.
“When a person is experiencing the early phases of psychosis, they’re very embarrassed and frightened,” Taylor says. “They may not want to admit it’s happening to them because they’re afraid they’re ‘going crazy’, and they don’t understand there is help available.”
Facts about psychosis:-
Psychosis is a disruption to the way our brains process the world around us, and the narrative inside our own heads about what we’re experiencing when we’re alone or with others – what Taylor calls the “stories” that we constantly tell ourselves in order to navigate the world.
-
Hallucinations, hearing voices, feeling paranoia about the actions or intentions of others when no one else seems to feel that way and interpreting experiences completely differently from others can all be psychosis signs.
 In the early stages, people understand that what they’re experiencing isn’t real, but over time they lose the ability to distinguish reality from hallucination.
In the early stages, people understand that what they’re experiencing isn’t real, but over time they lose the ability to distinguish reality from hallucination. -
Psychosis is often stigmatized and misunderstood, which can get in the way of getting help. But research has shown that three-quarters of people who do get effective help early can experience relief from their symptoms.
-
For people who show signs of a possible psychosis, sometimes called “attenuated psychosis syndrome,” only about one-third go on to develop a full-blown psychosis. However, they usually have symptoms of depression and anxiety, which can benefit from treatment.
SEE ALSO: How to Talk to Children and Teens About Suicide: A Guide for Parents
How to help someone else experiencing symptoms of psychosis:-
Often, family and friends help identify someone who is struggling with psychosis, and suffering from their symptoms, so they’re important to getting them in touch with professionals who can help.

-
Stressful life events, such as going off to college or breaking up with a significant other, can trigger psychosis. Further research is needed into why this is, but a low underlying “stress tolerance” level is often seen.
-
It’s all right to mention to someone that you’re worried about them, and open the door to discussing it at that point or later. You can find out if there’s an early-psychosis clinic like U-M’s near you, and provide information or offer to contact them.
-
If you notice signs that they’re harming themselves, that’s the time to seek immediate help, often by starting with contacting suicide hotline or nearby psychiatric emergency room for advice. People with psychosis have 10 to 15 times the risk of suicidal thoughts or behaviors than others.
SEE ALSO: Getting Through a Pandemic When You Have a Mental Health Condition
Treatment, support and how to help find answers for people struggling with psychosis:-
Treatments for people showing potential signs of psychosis mostly focus on talk therapy, also called cognitive behavioral therapy.
 Family and group therapy are also important, and can be done virtually.
Family and group therapy are also important, and can be done virtually. -
For people who show clear breaks with reality, antipsychotic medication can help greatly. The vast majority of people who receive these medicines experience improvement in their symptoms, but they may also experience side effects, so it’s important to work with a trained professional to find the best fit.
-
Women who experienced postpartum psychosis after having a baby are at high risk of experiencing it again if they have another pregnancy, and should receive special attention during and after pregnancy.
-
A very small number of people with psychosis may be driven by their paranoia or hallucinations to act strangely in public or try to harm others. If you find yourself having to call the police because of such behaviors, make sure they understand and acknowledge that the person you’re calling about has a mental health condition and needs help getting to appropriate care.
-
Just like many infectious diseases can cause a fever, psychosis is part of many mental health conditions – but what exactly causes it isn’t well understood. That’s why the U-M team needs people with psychosis to consider taking part in the studies they’re running.
“Psychosis strikes in the years when people are just starting to be truly independent in life, work and school, which can make it especially devastating to the person and the family,” says Taylor. “The process of brain maturation depends on a lot of things going right inside our brains and if they don’t, things can go askew. The longer they go untreated, the higher the chance they may experience damage to the brain and be worse off even when they get treatment.”
E-mail to reach the Michigan Medicine PREP clinic for early-stage psychosis or call 734-764-0231.
More Articles About:
Mental Health Assessment
,
Adolescent Psychiatric Treatment
,
Adult Psychiatric Treatment
,
Mental Health
,
TweetSharePinShareEmailShare
Depersonalization: what it is and how to bring yourself back to reality
12 561
Man among peopleKnow yourselfAntistress
- Photo
- Getty Images
The earth is slipping away from under your feet, but it seems impossible to put what is happening in your head.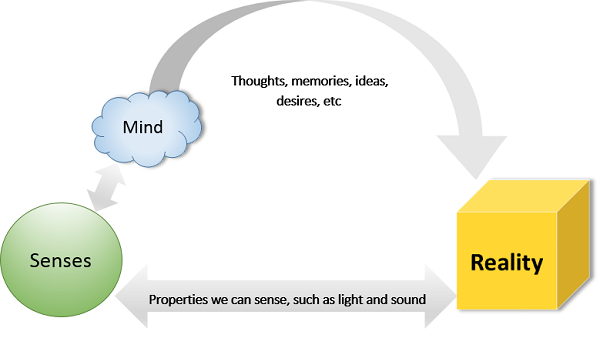 On days like these, advice to quit caffeine and get grounded feels like psyllium. Useful in the moment, they can seem empty under prolonged stress.
On days like these, advice to quit caffeine and get grounded feels like psyllium. Useful in the moment, they can seem empty under prolonged stress.
When circumstances are intense, large-scale and impossible to control, we all find ourselves in a borderline situation for some time. At such moments, it becomes easier to understand people with anxiety disorder, depression, borderline personality disorder (BPD), and bipolar affective disorder (BAD).
From extreme to extreme: do you find it difficult to inhale or exhale?
“I was whole and I was broken, I was alive and I was killed,” the words from the song of the group “Spleen” are, perhaps, one of the most accurate descriptions of a person living in a difficult, borderline situation. It is normal to be inconsistent, unstable and confused.
An indicator of the intensity of the anxiety experienced by a person can be breathing. Psychologist Anastasia Dolganova offers pay attention to what is more difficult to do in a situation of extreme excitement: inhalation or exhalation.
If you catch air but cannot let it out slowly, we are talking about neurotic anxiety
A person can feel it at the moments when he is face to face with repressed, forbidden feelings: aggression, greed, lust, jealousy.
It is in this case that breath recovery techniques and mobile meditation apps, as well as self-soothing and returning to reality techniques, are effective for relieving symptoms. In the long run, this can be work on accepting the shadow sides, recognizing ambiguous emotions, and forming a more realistic self-image.
It is more difficult if a person cannot breathe: such a reaction may indicate intense psychotic anxiety
And the techniques for overcoming it will be different. Such anxiety arises against the background of fear of death, meaninglessness, despair and isolation.
In Existential Psychotherapy, Irvin Yalom gives a personal example of dealing with the fear of death after a car accident. The psychologist speaks of a background experience that he experiences for several months after: "the world began to seem unreliable." He becomes sinister, loses his comfort. The internal boundaries of a person in such a situation are blurred, the usual supports are crumbling.
The psychologist speaks of a background experience that he experiences for several months after: "the world began to seem unreliable." He becomes sinister, loses his comfort. The internal boundaries of a person in such a situation are blurred, the usual supports are crumbling.
“We can respond to a crisis of meaning by repressing the theme defensively, splitting off from the consciousness of the suffering part of the personality… We can succumb to despair and become cynical,” write Ursula Wirtz and Jörg Zobeli in The Thirst for Meaning. Man in extreme situations. The limits of psychotherapy.
Another option is to look for meaning in "dialogue filled with love." If there is a topic for discussion and space for disclosure, there is a real meeting with another person. Thus, according to Wirtz and Zobeli, intimacy is formed, as a deep interaction of people.
In a situation of existential "heaving" there is no more effective way to relieve anxiety than to share it with the Other
Those who are here and now able to hear, understand and accept. Then inexpressible despair and fear begin to take on boundaries, impotence does not go away, but becomes bearable.
Then inexpressible despair and fear begin to take on boundaries, impotence does not go away, but becomes bearable.
If the dialogue becomes more and more like a game of ping-pong, the interlocutors cannot hear each other and the conversation resembles two alternating monologues, pulling back and increasing the distance is a saving tactic.
Absurdity, Surprise and Alienation: How to Survive Derealization
When circumstances overwhelm you, it can be difficult to cope with it, and sometimes unbearable. In such situations, the human psyche resorts to the most powerful defenses. One of these is depersonalization of . It can act as an independent symptom, be one of the manifestations of bipolar affective disorder, schizophrenia or depression, as well as a mechanism for protecting a healthy psyche in extreme situations.
If you look at the reflection in the mirror for a long time, for a few seconds your own face may seem unfamiliar, strange and alien. This is one of the simple and short options for depersonalization. At such moments, a person ceases to feel himself and feel at all. And reality begins to seem like the frames of a surreal film.
This is one of the simple and short options for depersonalization. At such moments, a person ceases to feel himself and feel at all. And reality begins to seem like the frames of a surreal film.
- Photo
- Getty Images
There is another similar condition. Do you know that strange feeling when a familiar simple word suddenly turned into a meaningless, empty sound? You repeat it, but you don't seem to recognize it. When something like this happens to the outside world, it's called derealization . The familiar space of a room can become a completely unfamiliar place in a second. This feeling of alienation and unrecognition can be unpleasant, intense, and difficult to bear. For example, Jean-Paul Sartre called this condition nausea.
"Any human activity - the work that we go to every day, the conduct of religious ceremonies, the daily natural functions - seems strange, if not absurd, if you look at it without emotions and full involvement" - this is how the state of depersonalization is described by Daphne Simeon and Jeffrey Abugel in "I'm not Me. What is depersonalization and how to live with it."
What is depersonalization and how to live with it."
Such detachment can be depressing, frightening and hard to bear. Or, on the contrary, when experiencing the death of a loved one, loss and in a difficult life situation, give the person some relief.
Not living one's own life, apathy and feeling absurd can last several minutes, days or months
The duration depends on whether the person has a tendency to depersonalize or is it a single reaction to an excessive stimulus. Short-term depersonalization or derealization is quite normal.
Simeon and Abugel say that the ideal way to break the vicious circle of fear and anxiety is to remove the stressful situations that started it. However, this is not always possible. The authors also talk about the healing power of a psychotherapeutic (and not only) conversation, an attempt to gain control over circumstances (through any creative action).
Checklist: how to recognize depersonalization
-
You don't feel anything.
 Linkin Park's biggest hit "Numb" describes a state of numbness, a weak sense of oneself ("I'm so numb that I don't feel you're here anymore. / I'm so tired, I understand much more" * ). This may be a fairly accurate description of depersonalization.
Linkin Park's biggest hit "Numb" describes a state of numbness, a weak sense of oneself ("I'm so numb that I don't feel you're here anymore. / I'm so tired, I understand much more" * ). This may be a fairly accurate description of depersonalization. -
You are living yourself in a third person. Thoughts, feelings, memories and the body - all this is as if not yours.
-
You don't recognize yourself. Your perception distorts the way you see yourself, body parts seem alien and/or altered, your head is foggy and thoughts come with effort. You look at your own hand and seem to take a moment to recognize it as part of you.
-
You do not feel in control of your body. It seems to move not by your will, but by itself. Speech sounds like from the outside and you do not control it.
Checklist: how to recognize derealization
-
You are dreaming.
 It is difficult to recognize in the state in which you are, reality. Everything is experienced as unreal.
It is difficult to recognize in the state in which you are, reality. Everything is experienced as unreal. -
You don't feel attached. Close people are perceived as strangers.
-
You distort time and forms. The intervals between the past and the future are inadequately expanded: recent events are subjectively perceived as long past. The shapes of objects and their appearance look strange, distorted, unrecognizable - for example, the room seems to be compressed or stretched.
What can be done to overcome alienation from reality?
Establish sleep patterns
Circadian rhythm disorders can be a trigger for depersonalization/derealization, and also affect the degree of its manifestation
Refuse alcohol and other substances that cause an altered state of consciousness
Researchers have not yet found a direct causal relationship, but often these factors stimulate and prolong the feeling of detachment, insensibility.
Check the list of side effects of the medications that you take regularly
If you endure depersonalization/derealization painfully and you associate its intensity with a specific drug, this is a reason to consult a specialist, change the pills.
Remember that the experienced state has a beginning and an end
It will not last forever.
Repeating to yourself that depersonalization/derealization is a defensive reaction of the psyche
This is an attempt to separate from the world and avoid a potential threat. Try not to focus on anxiety from the occurrence of such a condition, concentrate on simple routine activities.
Seek contact with another person
With a friend, relative or person with a similar experience. Discuss, share and express feelings.
Talk to a psychologist or psychiatrist
Request feedback and support from a specialist.
* I've become so numb I can't feel you there
I've become so tired so much more aware .
Text: Ekaterina Lakizo
New on the site
Stress hormone: how to keep cortisol levels normal — 5 doctor’s tips
How to prepare for the New Year: beauty treatments, makeup trends and fashion styling
“I don't understand why I was born. I have no purpose”
“The Same Rake”: 5 Reasons We Attract Similar Troubles
Forward to Success: 4 Steps to Get the Most Out of Life – Try Now
“Never Never developed relationships with men. Maybe I'm in the wrong orientation?
"How to learn to argue and defend yourself in conflicts?"
"Bad Mood - Binging Attack": What You Need to Know About Bulimia Nervosa
Where does derealization come from and what to do about it
5 May Likbez Health
If you have ever experienced deja vu, this is not a cause for concern.
What is derealization
Derealization is a constant or periodic feeling of the unreality of the surrounding world. In moments of fear or anxiety, a person may feel as if he is abstracting from what is happening and watching from the side. This is necessary to protect the brain and psyche from a strong shock.
In moments of fear or anxiety, a person may feel as if he is abstracting from what is happening and watching from the side. This is necessary to protect the brain and psyche from a strong shock.
Symptoms usually first appear in adolescents or young adults. Constant or periodic derealization makes you constantly check what is real and what only seems to be. It feels like you're going crazy. This interferes with relationships and work, scares and even limits the fullness of life: it becomes difficult to concentrate on everyday affairs, a feeling of hopelessness arises, anxiety and depression increase.
Derealization is often mentioned together with depersonalization. So called detachment or alienation of the individual from himself. A person experiencing this feels like a robot or an outside observer of his body and mind. Derealization and depersonalization can occur together—for example, in dissociative disorders—or they can occur separately.
About 50% of people in the world at least once in their lives felt the unreality of what was happening. So there is no need to worry about it. But if derealization happens often and interferes with life, then you need to find out why it appeared.
So there is no need to worry about it. But if derealization happens often and interferes with life, then you need to find out why it appeared.
Why derealization occurs
Until now, doctors do not know the exact causes. Some people are more susceptible to it due to genetic factors or personality traits. For example, if a person avoids difficult situations, it is harder for him to adapt to stress.
Derealization often occurs in response to severe traumatic events, especially in childhood. For example, due to domestic abuse. It occurs in people with post-traumatic stress disorder, severe lingering depression, and panic attacks.
Derealization can also be a symptom of:
- epilepsy;
- brain lesions;
- disorders of the vestibular apparatus or labyrinthitis;
- severe sleep disorders;
- different personality disorders;
- schizophrenia.
Sometimes manifestations of derealization occur due to the use of alcohol, benzodiazepines and certain illegal drugs.
What are the symptoms of derealization
People describe their symptoms in different ways. For example, they feel that:
- they are in a movie or in a dream, and the whole environment is unfamiliar to them;
- close people became indifferent, as if they were separated by a glass wall;
- everything around is distorted, blurred, colorless, two-dimensional or artificial, or, on the contrary, more clear and distinct;
- time does not flow correctly - for example, recent events seem to have happened in the distant past;
- distance, sizes and shapes of objects are surreal and implausible;
- "have already seen" something unfamiliar - déjà vu, or "have never seen" something familiar - jamais vu.
What to do if you feel derealized
Patients with derealization often improve without intervention, especially if the symptoms are caused by short-term stress. To distract yourself from your subjective self-perceptions, you can try to focus on other thoughts or actions.
If the symptoms persist for a long time and reduce the quality of life, a psychotherapist should be consulted. He will ask about the manifestations and medications taken, conduct an examination and prescribe treatment.
Psychotherapy
Depersonalization is usually treated with psychotherapy. It helps:
- to find out why problems are occurring;
- work through the traumas that led to derealization;
- learn to be distracted from its manifestations;
- deal with stress so that it occurs less frequently;
- Treat comorbid mental conditions such as anxiety or depression.
For treatment, psychodynamic therapy is used, which examines the influence of unresolved past conflicts on human behavior. They also use cognitive-behavioral therapy - it helps to realize past actions in order to change behavior now.
Medicines
There are no medicines for derealization. However, a doctor may recommend supplements to help reduce symptoms of anxiety or depression.