Thought disorders examples
Thought Disorder Symptoms, Diagnosis, and Treatment
A thought disorder can occur with schizophrenia and other conditions, including mania and traumatic brain injury. Certain subtypes may be more common with specific causes.
Thought disorder is a disorganized way of thinking that leads to abnormal ways of expressing language when speaking and writing. It’s one of the primary symptoms of schizophrenia, but it may be present in other mental disorders such as mania and depression.
Thought disorder is one of the most difficult mental disorders to diagnose and treat, as many people exhibit symptoms of thought disorder occasionally. Some people may demonstrate thought disorder only when they’re tired.
There are more than 20 subtypes of thought disorder. In this article, we’ll break down the symptoms of some of the most common types. We’ll also examine potential treatment options to help you or someone you know manage this disorder.
Thought disorder first appeared in scientific literature in the 1980s, when it was first described as a symptom of schizophrenia. Its loose definition is any disturbance in the organization and processing of ideas.
Each type of thought disorder has unique symptoms. However, a disruption in the interconnectivity of ideas is present in all types.
Even though it’s common for most people to display some of the symptoms of thought disorder occasionally, thought disorder isn’t classified until it negatively affects the ability to communicate.
These are some of the most common types of thought disorder:
Alogia
People with alogia, also known as poverty of speech, give brief and unelaborated responses to questions. People with this form of thought disorder rarely speak unless prompted. Alogia is often seen in people with dementia or schizophrenia.
Blocking
People with thought blocking often interrupt themselves abruptly mid-sentence. They might pause for several seconds or minutes. When they start talking again, they often change the topic of conversation. Thought blocking is common in people with schizophrenia.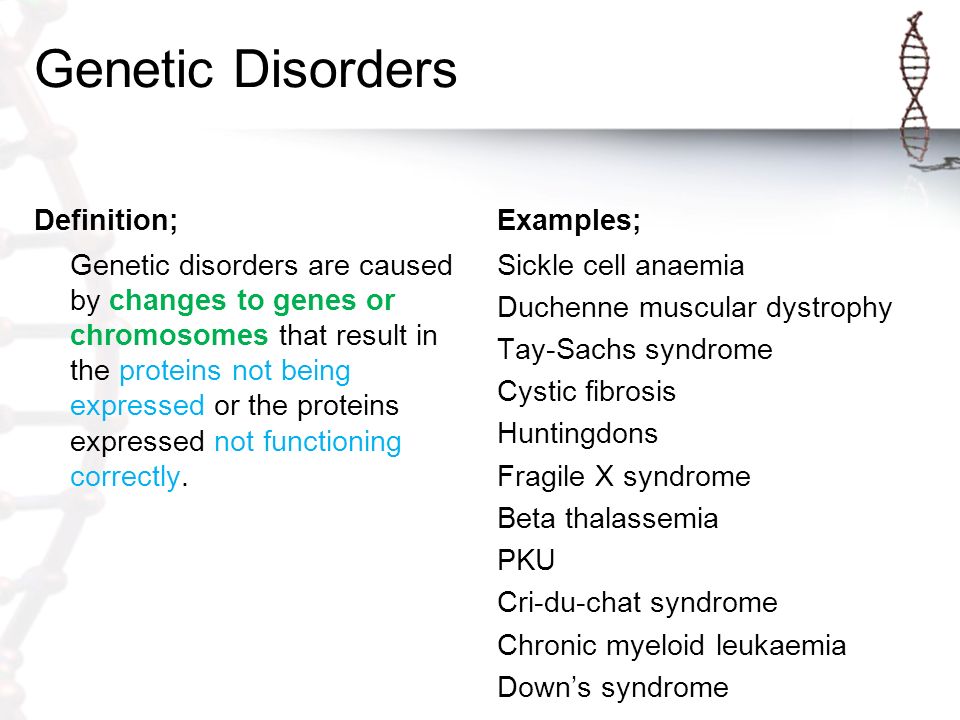
Circumstantiality
People with circumstantiality, also known as circumstantial thinking, or circumstantial speech, often include excessive irrelevant details in their speaking or writing. They maintain their original train of thought but provide a lot of unnecessary details before circling back to their main point.
Clanging or clang association
A person with clanging thought process makes word choices based on the sound of the word rather than the meaning of the word. They may rely on using rhymes, alliterations, or puns and create sentences that don’t make sense. Clanging thought process is a common symptom of mania.
Derailment
A person with derailment talks in chains of only semi-related ideas. Their ideas often fall further and further from the topic of conversation. For example, a person with derailment thought disorder might jump from talking about rabbits to the hair on their head to your sweater.
Distractible speech
A person with distractible speech thought disorder has trouble maintaining a topic. They shift quickly between topics and get distracted by internal and external stimuli. It’s commonly seen in people with mania.
They shift quickly between topics and get distracted by internal and external stimuli. It’s commonly seen in people with mania.
For example, somebody exhibiting distractible speech might abruptly ask where you got your hat mid-sentence while telling you about a recent vacation.
Echolalia
People with echolalia struggle to communicate. They often repeat noises and words they hear instead of expressing their thoughts. For example, instead of answering a question, they may repeat the question.
Other types of thought disorder
The Johns Hopkins Psychiatry Guide lists 20 types of thought disorder. These include:
- Paraphasic error: constant word mispronunciation or slips of the tongue
- Stilted speech: using unusual language that’s overly formal or outdated
- Perseveration: leads to a repetition of ideas and words
- Loss of goal: trouble maintaining a topic and an inability to come to a point
- Neologism: creating new words
- Incoherence: speaking in seemingly random collections of words, known as “word salad”
The cause of thought disorder isn’t well known. Thought disorder isn’t a symptom of any particular disorder, but it’s commonly seen in people with schizophrenia and other mental health conditions.
Thought disorder isn’t a symptom of any particular disorder, but it’s commonly seen in people with schizophrenia and other mental health conditions.
The cause of schizophrenia also isn’t known, but it’s thought that biological, genetic, and environmental factors can all contribute.
Thought disorder is loosely defined and the symptoms vary widely, so it’s difficult to find a single underlying cause. Researchers are still debating about what might lead to the symptoms of thought disorder.
Some believe it might be caused by changes in language-related parts of the brain, while others think it could be caused by problems in more general parts of the brain.
Thought disorder is one of the defining symptoms of schizophrenia and psychosis. People have a heightened risk of developing thought disorder if they also have:
- mood disorders
- bipolar disorder
- depression
- traumatic brain injury
- anxiety
According to research from 2005, people with epilepsy have an increased risk of developing schizophrenia and psychosis compared to the general population.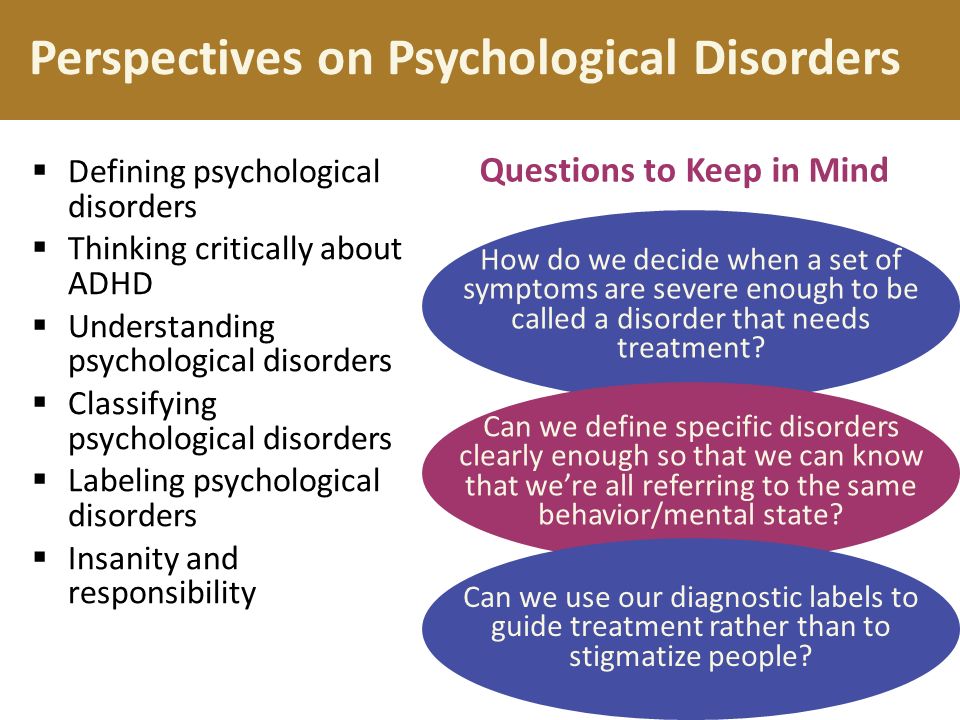
A traumatic brain injury increases your risk of developing schizophrenia and other mental disorders, such as depression, bipolar disorder, and anxiety disorders.
The following risk factors might also be risk factors for schizophrenia, and by extension, thought disorder:
- stress
- use of mind-altering drugs
- inflammatory and autoimmune disease
- exposure to toxic chemicals before birth
It’s not uncommon for people to demonstrate symptoms of thought disorder occasionally. However, if these symptoms are frequent or severe enough to cause problems communicating, it’s a good idea to speak with a doctor.
Thought disorder may be a symptom of a mental disorder. Many mental disorders such as schizophrenia are progressive and don’t improve without treatment. However, people with mental disorders are often unaware of their symptoms and need help from a family member or friend.
If you notice any other symptoms of schizophrenia in somebody you know, you may want to encourage them to see a doctor:
- delusions
- hallucinations
- disorganized thinking or speech
- neglecting personal hygiene
- lack of emotion
- lack of facial expression
- withdrawing from social life
When diagnosing thought disorder, a medical professional will consider a person’s intelligence, culture, and education to see if they’re acting inconsistently.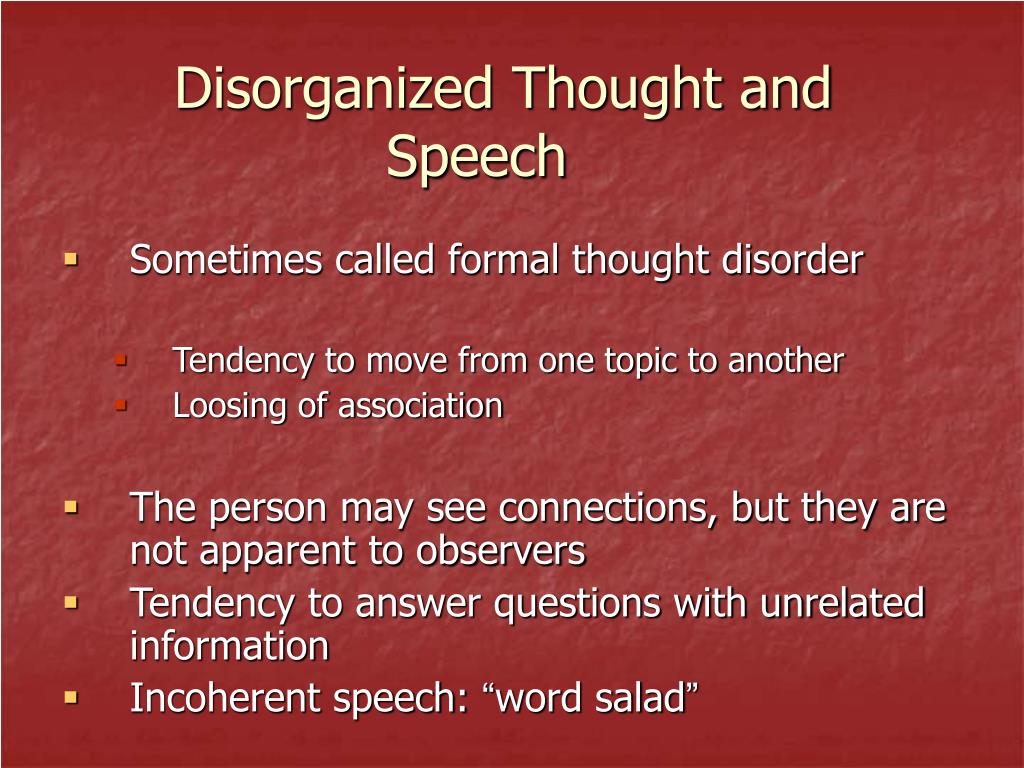
Rorschach inkblot test
The Rorschach inkblot test was first invented by Hermann Rorschach in 1921. The test uses a series of 10 inkblots to identify a potential thought disorder.
The inkblots are ambiguous and the patient gives their interpretation of each. The administrating psychologist then interprets the patient’s responses to search for potentially disordered thinking.
Thought Disorder Index
After engaging a patient in an open-ended conversation, a medical professional will transcribe the conversation and score it using the thought disorder index.
The Thought Disorder Index, also called Delta Index, is the first standardized test to identify thought disorder. It measures 23 areas of potential thought disturbance and weighs the severity of each on a scale from zero to one.
Treatment for thought disorder targets the underlying medical condition. The two primary types of treatment are medication and psychotherapy.
Medication
Antipsychotic medication may be prescribed depending on the cause of thought disorder. These medications can balance out the brain chemical dopamine and serotonin.
These medications can balance out the brain chemical dopamine and serotonin.
Psychotherapy
Psychotherapy helps people replace their thoughts with more realistic ones and teach them ways to manage an illness.
Cognitive behavior therapy, a form of psychotherapy, and cognitive enhancement therapy may both be beneficial for people with schizophrenia.
If you suspect that a loved one has a thought disorder, encourage them to seek medical attention. Treatments that can effectively manage thought disorder symptoms are available, and a doctor can help determine the right treatment method based on the underlying condition.
Thought disorder is a disorganized way of thinking that leads to unusual speech and writing. People with thought disorder have trouble communicating with others and may have trouble recognizing that they have an issue.
If you suspect that somebody close to you has a thought disorder, it’s a good idea to encourage them to see a doctor as soon as possible.
Thought Disorder Symptoms, Diagnosis, and Treatment
A thought disorder can occur with schizophrenia and other conditions, including mania and traumatic brain injury. Certain subtypes may be more common with specific causes.
Thought disorder is a disorganized way of thinking that leads to abnormal ways of expressing language when speaking and writing. It’s one of the primary symptoms of schizophrenia, but it may be present in other mental disorders such as mania and depression.
Thought disorder is one of the most difficult mental disorders to diagnose and treat, as many people exhibit symptoms of thought disorder occasionally. Some people may demonstrate thought disorder only when they’re tired.
There are more than 20 subtypes of thought disorder. In this article, we’ll break down the symptoms of some of the most common types. We’ll also examine potential treatment options to help you or someone you know manage this disorder.
Thought disorder first appeared in scientific literature in the 1980s, when it was first described as a symptom of schizophrenia. Its loose definition is any disturbance in the organization and processing of ideas.
Its loose definition is any disturbance in the organization and processing of ideas.
Each type of thought disorder has unique symptoms. However, a disruption in the interconnectivity of ideas is present in all types.
Even though it’s common for most people to display some of the symptoms of thought disorder occasionally, thought disorder isn’t classified until it negatively affects the ability to communicate.
These are some of the most common types of thought disorder:
Alogia
People with alogia, also known as poverty of speech, give brief and unelaborated responses to questions. People with this form of thought disorder rarely speak unless prompted. Alogia is often seen in people with dementia or schizophrenia.
Blocking
People with thought blocking often interrupt themselves abruptly mid-sentence. They might pause for several seconds or minutes. When they start talking again, they often change the topic of conversation. Thought blocking is common in people with schizophrenia.
Circumstantiality
People with circumstantiality, also known as circumstantial thinking, or circumstantial speech, often include excessive irrelevant details in their speaking or writing. They maintain their original train of thought but provide a lot of unnecessary details before circling back to their main point.
Clanging or clang association
A person with clanging thought process makes word choices based on the sound of the word rather than the meaning of the word. They may rely on using rhymes, alliterations, or puns and create sentences that don’t make sense. Clanging thought process is a common symptom of mania.
Derailment
A person with derailment talks in chains of only semi-related ideas. Their ideas often fall further and further from the topic of conversation. For example, a person with derailment thought disorder might jump from talking about rabbits to the hair on their head to your sweater.
Distractible speech
A person with distractible speech thought disorder has trouble maintaining a topic. They shift quickly between topics and get distracted by internal and external stimuli. It’s commonly seen in people with mania.
They shift quickly between topics and get distracted by internal and external stimuli. It’s commonly seen in people with mania.
For example, somebody exhibiting distractible speech might abruptly ask where you got your hat mid-sentence while telling you about a recent vacation.
Echolalia
People with echolalia struggle to communicate. They often repeat noises and words they hear instead of expressing their thoughts. For example, instead of answering a question, they may repeat the question.
Other types of thought disorder
The Johns Hopkins Psychiatry Guide lists 20 types of thought disorder. These include:
- Paraphasic error: constant word mispronunciation or slips of the tongue
- Stilted speech: using unusual language that’s overly formal or outdated
- Perseveration: leads to a repetition of ideas and words
- Loss of goal: trouble maintaining a topic and an inability to come to a point
- Neologism: creating new words
- Incoherence: speaking in seemingly random collections of words, known as “word salad”
The cause of thought disorder isn’t well known. Thought disorder isn’t a symptom of any particular disorder, but it’s commonly seen in people with schizophrenia and other mental health conditions.
Thought disorder isn’t a symptom of any particular disorder, but it’s commonly seen in people with schizophrenia and other mental health conditions.
The cause of schizophrenia also isn’t known, but it’s thought that biological, genetic, and environmental factors can all contribute.
Thought disorder is loosely defined and the symptoms vary widely, so it’s difficult to find a single underlying cause. Researchers are still debating about what might lead to the symptoms of thought disorder.
Some believe it might be caused by changes in language-related parts of the brain, while others think it could be caused by problems in more general parts of the brain.
Thought disorder is one of the defining symptoms of schizophrenia and psychosis. People have a heightened risk of developing thought disorder if they also have:
- mood disorders
- bipolar disorder
- depression
- traumatic brain injury
- anxiety
According to research from 2005, people with epilepsy have an increased risk of developing schizophrenia and psychosis compared to the general population.
A traumatic brain injury increases your risk of developing schizophrenia and other mental disorders, such as depression, bipolar disorder, and anxiety disorders.
The following risk factors might also be risk factors for schizophrenia, and by extension, thought disorder:
- stress
- use of mind-altering drugs
- inflammatory and autoimmune disease
- exposure to toxic chemicals before birth
It’s not uncommon for people to demonstrate symptoms of thought disorder occasionally. However, if these symptoms are frequent or severe enough to cause problems communicating, it’s a good idea to speak with a doctor.
Thought disorder may be a symptom of a mental disorder. Many mental disorders such as schizophrenia are progressive and don’t improve without treatment. However, people with mental disorders are often unaware of their symptoms and need help from a family member or friend.
If you notice any other symptoms of schizophrenia in somebody you know, you may want to encourage them to see a doctor:
- delusions
- hallucinations
- disorganized thinking or speech
- neglecting personal hygiene
- lack of emotion
- lack of facial expression
- withdrawing from social life
When diagnosing thought disorder, a medical professional will consider a person’s intelligence, culture, and education to see if they’re acting inconsistently.
Rorschach inkblot test
The Rorschach inkblot test was first invented by Hermann Rorschach in 1921. The test uses a series of 10 inkblots to identify a potential thought disorder.
The inkblots are ambiguous and the patient gives their interpretation of each. The administrating psychologist then interprets the patient’s responses to search for potentially disordered thinking.
Thought Disorder Index
After engaging a patient in an open-ended conversation, a medical professional will transcribe the conversation and score it using the thought disorder index.
The Thought Disorder Index, also called Delta Index, is the first standardized test to identify thought disorder. It measures 23 areas of potential thought disturbance and weighs the severity of each on a scale from zero to one.
Treatment for thought disorder targets the underlying medical condition. The two primary types of treatment are medication and psychotherapy.
Medication
Antipsychotic medication may be prescribed depending on the cause of thought disorder. These medications can balance out the brain chemical dopamine and serotonin.
These medications can balance out the brain chemical dopamine and serotonin.
Psychotherapy
Psychotherapy helps people replace their thoughts with more realistic ones and teach them ways to manage an illness.
Cognitive behavior therapy, a form of psychotherapy, and cognitive enhancement therapy may both be beneficial for people with schizophrenia.
If you suspect that a loved one has a thought disorder, encourage them to seek medical attention. Treatments that can effectively manage thought disorder symptoms are available, and a doctor can help determine the right treatment method based on the underlying condition.
Thought disorder is a disorganized way of thinking that leads to unusual speech and writing. People with thought disorder have trouble communicating with others and may have trouble recognizing that they have an issue.
If you suspect that somebody close to you has a thought disorder, it’s a good idea to encourage them to see a doctor as soon as possible.
Thinking and its disorders (V.V. Dunaevsky)
Thinking
Thinking is a basic and human-specific cognitive process, during which internal (semantic) connections are established dialectically, characterizing the structure of objects of reality, their relationship with each other and to the subject of cognitive activity. Thinking is closely connected with another basic cognitive process - the process of perception, and must have arisen as a result of its progressive evolutionary development. The struggle for existence, which is the main mechanism of species dynamics, forced at each moment of conflict interaction of competing individuals first to the maximum tension of physical forces (stress mobilization) in order to satisfy their unconditional needs (food, sexual, self-preservation), thereby ensuring the survival of the individual and the preservation of the species. . At a certain stage of development, when purely physical resources were exhausted, a more effective adaptive mechanism became the possibility of first generalizing, based on individual experience, the uniqueness of problem situations and their algorithmic resolution, and then the need to search for new non-standard (creative) solutions.
These circumstances have become a stimulus that provides a qualitative leap - the transition from a concretely perceived moment of being to an analytical-synthetic assessment of past experience and predicting one's behavior in the future. Thus, its temporal boundaries were expanded and prerequisites were created for the intensive development of other mental functions (long-term and short-term memory, imagination, perspective thinking, etc. - that is, consciousness and self-consciousness in the broad sense of this concept). In parallel and interdependently with these processes, new purely human properties arose and developed - the symbolism of language and speech, fine arts, the rudiments of religious feeling, the scientific consciousness of the world and one's place in it.
Thus, the transition was made from the system of ideas about the surrounding world, which gradually took shape on the basis of its individual and collective perception to the system of concepts . The latter reflected the most essential features of phenomena and objects, allowing generalizations to be made, and developed into a picture of understanding of the surrounding world. The symbolism of language as a function of communication from a means of designating realities has increasingly turned into a means of communication, information exchange, forming the collective consciousness of the population. Along with specific concepts describing individual objects, phenomena (cat, table, fire) arose abstract, generalizing specific realities (animals, furniture, natural disasters).
The latter reflected the most essential features of phenomena and objects, allowing generalizations to be made, and developed into a picture of understanding of the surrounding world. The symbolism of language as a function of communication from a means of designating realities has increasingly turned into a means of communication, information exchange, forming the collective consciousness of the population. Along with specific concepts describing individual objects, phenomena (cat, table, fire) arose abstract, generalizing specific realities (animals, furniture, natural disasters).
The ability to form and assimilate semantic, generic concepts arises at a certain stage of the historical and ontogenetic development of mental activity and is called abstract thinking. Inability to operate with abstract concepts, subjective thinking based on non-essential signs does not reveal the meaning of phenomena or leads to a contradictory (illogical) interpretation of their essence.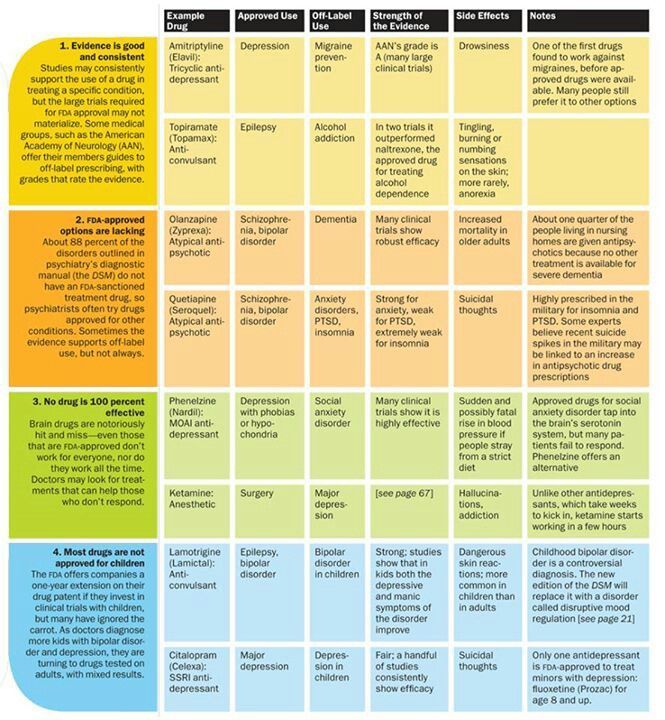 This, in turn, indicates either an atavistic delay in its development, or the presence of a mental disorder.
This, in turn, indicates either an atavistic delay in its development, or the presence of a mental disorder.
The thinking of normal people organizes pictures of the surrounding and inner world on the basis of an analysis of cause-and-effect relationships, subjecting its results to experimental verification, and sooner or later it turns out to be able to reveal the internal connections of objects and phenomena.
Creative, or so-called dialectical, thinking, which is the basis of professional clinical, as the most productive form, is based on analysis and synthesis. Analysis involves finding out how a given object, object, phenomenon, due to its individual characteristics, differs from others that are outwardly similar. In order to establish this, it is necessary to study its structural and dynamic originality. In relation to the patient, this means the need to study the exclusivity of personal phenomenology, including the study of biological, mental and social status.
Synthesis, on the contrary, means striving to establish internal connections of outwardly dissimilar objects, which is impossible either at the level of perception or at the level of specific formal thinking. Sometimes this connection is represented by only one characteristic, which, nevertheless, is fundamental. According to legend, the law of universal gravitation was revealed to Newton at the moment when an apple fell on his head. Perception of external signs indicates only the similarity of forms. Understanding the internal connections allows us to consider in the same row completely different objects that have only one common quality - mass. The human mind, thanks to this property, is also capable of extrapolating a known internal connection beyond the limits of the experimental perception of space and time, which makes its possibilities practically unlimited. This is how a person realizes the laws that govern the world, and the constant revision of existing ideas.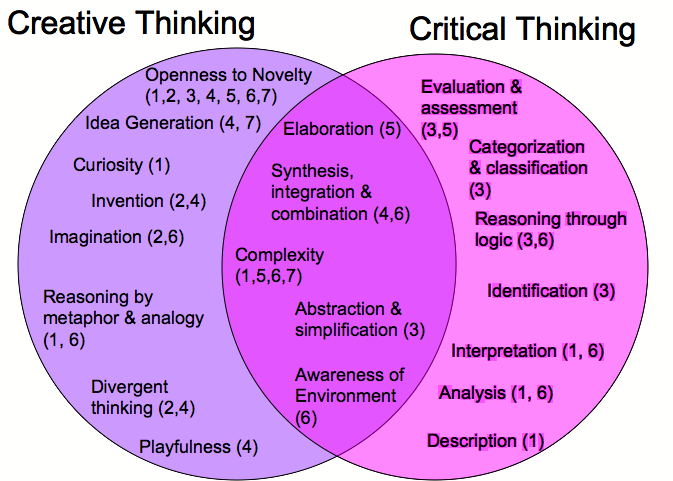
So-called formal thinking, which is atavistic or has painful causes, follows the path of analogies, which are established on the basis of external similarities, and therefore cannot be creatively productive. In medicine, it is called paramedical, but it is by no means the prerogative of paramedics. A doctor who thinks in this way, completing his special education, has canonized ideas about the register of existing, in his opinion, forms of diseases in their descriptive characteristics with an appropriate algorithm for subsequent actions. The diagnostic task is most often solved on the basis of a formal calculation of symptoms with the assignment of their array to a known nosological matrix. This happens according to the principle of answering the question: who does the bat look more like - a bird or a butterfly? In fact, a horse (both are mammals). Cognitive activity organized in this way can only cliché standard situations within the framework of solving the simplest problems. It needs guidance, control, and can only be acceptable to those who aspire to the role of an executor.
It needs guidance, control, and can only be acceptable to those who aspire to the role of an executor.
Thinking disorders are detected either using test procedures (pathopsychologically) or on the basis of a clinical method in the analysis of the speech and written production of the subject.
There are formal disorders of thinking (disorders of the associative process) and the so-called pathological ideas.
Disorders of thinking in form (disorders of the associative process)
This heading includes a number of disorders in the way of thinking in form: changes in its pace, mobility, harmony, purposefulness.
Disturbances in the pace of thinking
Painfully accelerated thinking. It is characterized by an increase in speech production per unit of time. The basis is the acceleration of the flow of the associative process. The flow of thought is determined by external associations, each of which is an impetus for a new topic of reasoning. The accelerated nature of thinking leads to superficial, hasty judgments and conclusions. Patients speak hastily, without pauses, separate parts of the phrase are interconnected by superficial associations. Speech takes on the character of a "telegraphic style" (patients skip conjunctions, interjections, "swallow" prepositions, prefixes, endings). "Leap of ideas" - the extreme degree of accelerated thinking.
The flow of thought is determined by external associations, each of which is an impetus for a new topic of reasoning. The accelerated nature of thinking leads to superficial, hasty judgments and conclusions. Patients speak hastily, without pauses, separate parts of the phrase are interconnected by superficial associations. Speech takes on the character of a "telegraphic style" (patients skip conjunctions, interjections, "swallow" prepositions, prefixes, endings). "Leap of ideas" - the extreme degree of accelerated thinking.
Painfully accelerated thinking is observed in manic syndrome, euphoric states.
Painfully slow thinking. In terms of tempo, it is the opposite of the previous disorder. Often combined with hypodynamia, hypothymia, hypomnesia. It is expressed in speech retardation, stuckness. Associations are poor, switching is difficult. Patients in their thinking are not able to cover a wide range of issues. A few inferences are formed with difficulty.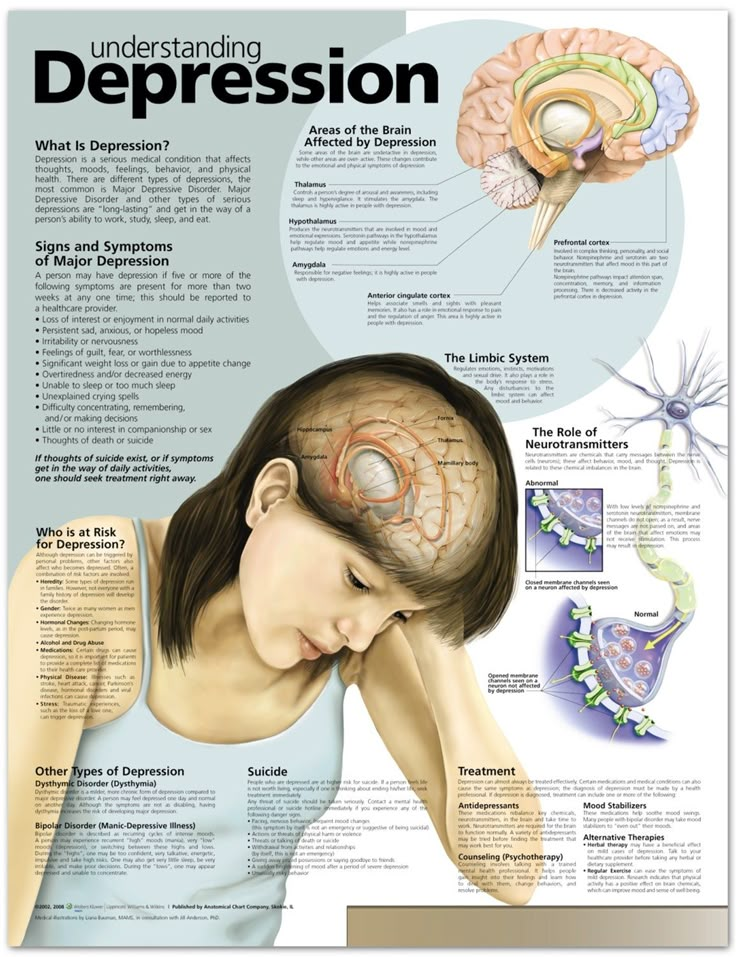 Patients rarely show speech activity spontaneously, their answers are usually laconic, monosyllabic. Sometimes contact cannot be established at all. This disorder is observed in depressions of any origin, with traumatic brain damage, organic, infectious diseases, epilepsy.
Patients rarely show speech activity spontaneously, their answers are usually laconic, monosyllabic. Sometimes contact cannot be established at all. This disorder is observed in depressions of any origin, with traumatic brain damage, organic, infectious diseases, epilepsy.
Violations of harmonious thinking
Broken thinking is characterized by the absence of logical concordances between words in the speech of patients, while grammatical connections can be preserved. Nevertheless, the patient's speech can be completely incomprehensible, devoid of any meaning, for example: "Who can single out the temporal divergence of the relativity of concepts included in the structure of the universe," etc.
With incoherent thinking not only logical, but also grammatical connections between words are missing. The speech of patients turns into a set of separate words or even sounds: “I’ll take . .. I’ll get myself ... a day-stump ... ah-ha-ha ... laziness”, etc. This thought disorder occurs in schizophrenia, exogenous organic psychoses, accompanied by amental clouding of consciousness.
.. I’ll get myself ... a day-stump ... ah-ha-ha ... laziness”, etc. This thought disorder occurs in schizophrenia, exogenous organic psychoses, accompanied by amental clouding of consciousness.
Violation of purposeful thinking
Reasoning (futile philosophizing, reasoning). Thinking with a predominance of lengthy, abstract, vague, often of little content reasoning on general topics, about well-known truths, for example, when a doctor asks “how do you feel?” talk for a long time about the benefits of nutrition, rest, vitamins. This kind of thinking is most common in schizophrenia.
Autistic thinking (from the word autos - itself) - thinking, cut off from reality, contrary to reality, not corresponding to reality and not corrected by reality. Patients lose touch with reality, plunge into the world of their own bizarre experiences, ideas, fantasies, incomprehensible to others. Autistic thinking is one of the main symptoms of schizophrenia, but can also occur in other diseases and pathological conditions: schizoid psychopathy, schizotypal disorders.
Autistic thinking is one of the main symptoms of schizophrenia, but can also occur in other diseases and pathological conditions: schizoid psychopathy, schizotypal disorders.
Symbolic thinking . Thinking, in which ordinary, commonly used words are given a special, abstract meaning, understandable only to the sickest person. At the same time, words and concepts are often replaced by symbols or new words (neologisms), patients develop their own language systems. Examples of neologisms: "mirror aster, pince-necho, electric ekskvozochka." This kind of thinking occurs in schizophrenia.
Pathological thoroughness (detailedness, viscosity, inertia, stiffness, torpid thinking). It is characterized by a tendency to detail, getting stuck on particulars, “marking time”, inability to separate the main from the secondary, the essential from the unimportant. The transition from one circle of ideas to another (switching) is difficult. It is very difficult to interrupt the speech of patients and direct them in the right direction. This kind of thinking is most often found in patients with epilepsy, with organic diseases of the brain.
It is very difficult to interrupt the speech of patients and direct them in the right direction. This kind of thinking is most often found in patients with epilepsy, with organic diseases of the brain.
Perseveration of thinking . It is characterized by the repetition of the same words, phrases, due to the pronounced difficulty in the switchability of the associative process and the dominance of any one thought, idea. This disorder occurs in epilepsy, organic diseases of the brain, and in depressed patients.
Thought disorders by content
Includes delusional, overvalued and obsessive ideas.
Crazy ideas.
They are false, erroneous judgments (inferences) that arose on a painful basis and are inaccessible to criticism and correction. A mistaken, but healthy person, sooner or later, can either be dissuaded, or he himself will understand the fallacy of his views. Delusion, being one of the manifestations of a disorder of mental activity in general, can be eliminated only through special treatment. According to psychopathological mechanisms, delusional ideas are divided into primary and secondary.
Delusion, being one of the manifestations of a disorder of mental activity in general, can be eliminated only through special treatment. According to psychopathological mechanisms, delusional ideas are divided into primary and secondary.
Primary delusion, or delusion of interpretation , interpretation follows directly from mental disorders and comes down to establishing incorrect connections, misunderstanding of the relationship between real objects. Perception here usually does not suffer. In isolation, primary delusional ideas are observed in relatively mild mental illnesses. The morbid basis here is most often a pathological character or personality changes.
Secondary or sensual delirium is a derivative of other primary psychopathological disorders (perception, memory, emotions, consciousness). Allocate hallucinatory, manic, depressive, confabulatory, figurative nonsense. It follows from the foregoing that secondary delirium occurs at a deeper level of mental disorder.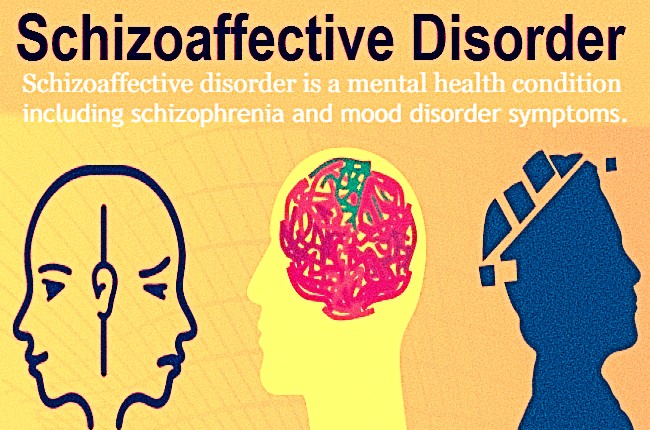 This level or "register", as well as the delusions genetically associated with it, are called paranoid (in contrast to the primary - paranoid).
This level or "register", as well as the delusions genetically associated with it, are called paranoid (in contrast to the primary - paranoid).
According to the content (on the topic of delusions), all delusions can be divided into three main groups: persecution, grandeur and self-abasement.
The group of ideas of persecution includes delusions of poisoning, relationships, influence, persecution proper, "love charm".
Delusions of grandeur are also varied in content: delusions of invention, reformism, wealth, high birth, delusions of grandeur.
delusional ideas of self-abasement (depressive delirium) include delusions of self-accusation, self-abasement, sinfulness, guilt.
Depressive plots are usually accompanied by depression and are presented asthenic. Paranoid delusions can be both asthenic and sthenic (“persecuted pursuer”).
Delusional syndromes
Paranoid syndrome is characterized by systematized delusions of attitude, jealousy, invention. The judgments and conclusions of patients outwardly give the impression of being quite logical, but they proceed from incorrect premises and lead to incorrect conclusions. This delirium is closely connected with the life situation, the personality of the patient, either altered by a mental illness, or being pathological from birth. Hallucinations are usually absent. The behavior of patients with paranoid delusions is characterized by litigation, querulant tendencies, and sometimes aggressiveness. Most often, this syndrome is observed in alcoholic, presenile psychoses, as well as in schizophrenia and psychopathy.
The judgments and conclusions of patients outwardly give the impression of being quite logical, but they proceed from incorrect premises and lead to incorrect conclusions. This delirium is closely connected with the life situation, the personality of the patient, either altered by a mental illness, or being pathological from birth. Hallucinations are usually absent. The behavior of patients with paranoid delusions is characterized by litigation, querulant tendencies, and sometimes aggressiveness. Most often, this syndrome is observed in alcoholic, presenile psychoses, as well as in schizophrenia and psychopathy.
Paranoid syndrome. Characterized by secondary delirium. The group of paranoid syndromes includes hallucinatory-delusional, depressive-delusional, catatonic-delusional and some other syndromes. Paranoid syndromes occur in both exogenous and endogenous psychoses.
In schizophrenia, one of the most typical variants of hallucinatory-paranoid syndrome is often observed - Kandinsky-Clerambault syndrome , which consists of the following symptoms: pseudohallucinations, mental automatisms, delusional ideas of influence. Automatisms are called the phenomenon of loss of a sense of belonging to oneself thoughts, emotional experiences, actions. For this reason, mental actions of patients are subjectively perceived as automatic. G. Clerambault (1920) described three types of automatisms: known to others (symptom of openness), "echo of thoughts", violent inner speech, verbal pseudo-hallucinations, perceived as a feeling of transferring thoughts over a distance.
Automatisms are called the phenomenon of loss of a sense of belonging to oneself thoughts, emotional experiences, actions. For this reason, mental actions of patients are subjectively perceived as automatic. G. Clerambault (1920) described three types of automatisms: known to others (symptom of openness), "echo of thoughts", violent inner speech, verbal pseudo-hallucinations, perceived as a feeling of transferring thoughts over a distance.
Sensory (senestopathic, sensory) automatism. It is characterized by the perception of various unpleasant sensations in the body (senestopathy), a burning sensation, twisting, pain, sexual arousal as made, specially caused. Gustatory and olfactory pseudohallucinations can be considered as variants of this automatism.
Motor (kinaesthetic, motor) automatism is manifested by a feeling of compulsion of certain actions, actions of the patient, which are performed against his will or caused by external influences. At the same time, patients often experience a painful feeling of physical lack of freedom, calling themselves “robots, phantoms, puppets, automata,” etc. (feeling of mastery).
At the same time, patients often experience a painful feeling of physical lack of freedom, calling themselves “robots, phantoms, puppets, automata,” etc. (feeling of mastery).
Explanation of such inner experiences with the help of hypnosis, cosmic rays or various technical means is called delusions of influence and sometimes has a rather absurd (autistic) character. Affective disorders in this case are most often represented by a feeling of anxiety, tension, in acute cases - fear of death.
Paraphrenic syndrome . It is characterized by a combination of fantastic, absurd ideas of grandeur with expansive affect, phenomena of mental automatism, delusions of influence and pseudo-hallucinations. Sometimes the patients' delusional statements are based on fantastic, fictitious memories (confabulatory delirium). In paranoid schizophrenia, paraphrenic syndrome is the final stage in the course of psychosis.
In addition to the chronic delusional syndromes described above, in clinical practice there are acutely developing delusional states with a better prognosis (acute paranoia, acute paranoid, acute paraphrenia). They are characterized by the severity of emotional disorders, a low degree of systematization of delusional ideas, the dynamism of the clinical picture and correspond to the concept of acute sensory delirium. At the height of these states, there may be signs of gross disorganization of mental activity in general, including signs of impaired consciousness (oneiroid syndrome).
They are characterized by the severity of emotional disorders, a low degree of systematization of delusional ideas, the dynamism of the clinical picture and correspond to the concept of acute sensory delirium. At the height of these states, there may be signs of gross disorganization of mental activity in general, including signs of impaired consciousness (oneiroid syndrome).
Acute sensual delirium can also be represented by Capgras syndrome (Kapgras J., 1923), which includes, in addition to anxiety and ideas of staging, the symptom of twins. With symptom of the negative twin , the patient claims that a close person, for example, a mother or father, is not such, but is a dummy figure, disguised as his parents. Symptom of the positive double consists in the conviction that unfamiliar faces, who have specially changed their appearance, appear to the patient as close people.
Cotard's syndrome (nihilistic delirium, delirium of denial), (Cotard Zh. , 1880) is expressed in erroneous conclusions of a megalomaniac, hypochondriacal nature about one's health. Patients are convinced that they have a serious, fatal disease (syphilis, cancer), “inflammation of all the viscera”, they talk about the defeat of individual organs or parts of the body (“the heart has stopped working, the blood has thickened, the intestines have rotted, food is not processed and comes from the stomach through lungs to the brain”, etc.). Sometimes they claim to have died, turned into a rotting corpse, perished.
, 1880) is expressed in erroneous conclusions of a megalomaniac, hypochondriacal nature about one's health. Patients are convinced that they have a serious, fatal disease (syphilis, cancer), “inflammation of all the viscera”, they talk about the defeat of individual organs or parts of the body (“the heart has stopped working, the blood has thickened, the intestines have rotted, food is not processed and comes from the stomach through lungs to the brain”, etc.). Sometimes they claim to have died, turned into a rotting corpse, perished.
Overvalued ideas
Overvalued ideas are judgments that arise on the basis of real facts, which are emotionally overestimated, exaggerated and occupy an unreasonably large place in the minds of patients, crowding out competing ideas. Thus, at the height of this process, with overvalued ideas, as well as with delirium, criticism disappears, which makes it possible to classify them as pathological.
Inferences arise both on the basis of the logical processing of concepts, ideas (rationally), and with the participation of emotions that organize and direct not only the process of thinking, but evaluate its result. For personalities of the artistic type, the latter can be decisive according to the principle: “if you can’t, but you really want to, then you can.” The balanced interaction of rational and emotional components is called affective coordination of thinking. Emotional disorders observed in various diseases and anomalies cause its violations. Overvalued ideas are a special case of an inadequately excessive saturation with the affect of any particular group of ideas, depriving all others of the competitiveness. This psychopathological mechanism is called mechanism cathymia . It is quite clear that pathological ideas arising in this way can have not only a personal, painful, situational conditionality, but also meaningfully related to life topics that cause the greatest emotional resonance.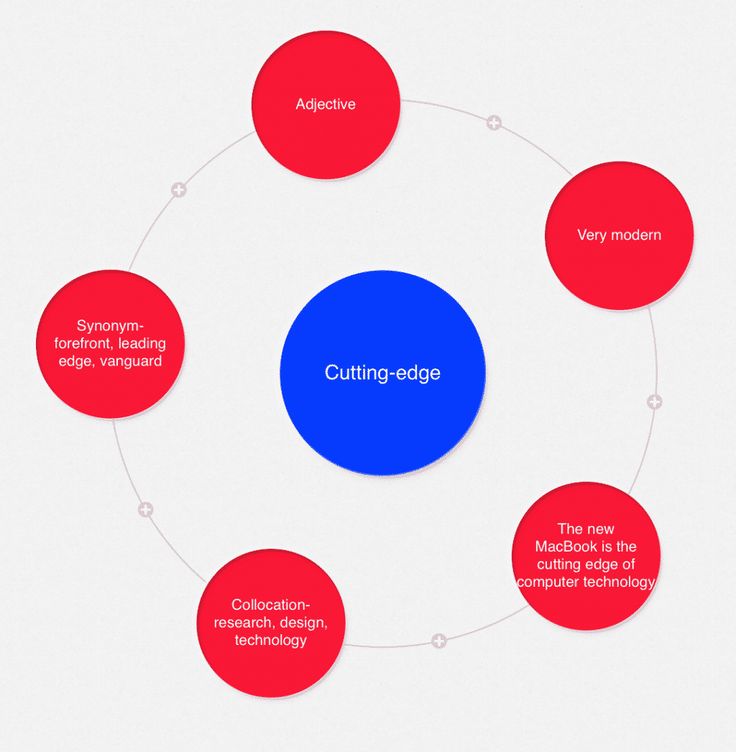
These topics are most often love and jealousy, the significance of one's own activity and the attitude of others, one's own well-being, health and the threat of losing both.
Most often, overvalued ideas arise in situations of conflict in psychopathic personalities, in the debut manifestations of exogenous-organic and endogenous diseases, as well as in cases of their mild course.
In the absence of a persistent disorganization of the emotional background, they can be of a transient nature and, when it is ordered, be accompanied by a critical attitude. Stabilization of affective disorders in the process of developing a mental illness or chronization of a conflict in abnormal personalities leads to a persistent decrease in the critical attitude, which some authors (A.B. Smulevich) propose to call "overvalued nonsense."
Obsessions
Obsessions or obsessions , are pathological ideas that arise spontaneously, are of an obsessive nature, to which there is always a critical attitude. Subjectively, they are perceived as painful and in this sense are "foreign bodies" of mental life. Most often, obsessive thoughts are observed in diseases of the neurotic circle, but they can also occur in practically healthy people with an anxious and suspicious nature, rigidity of mental processes. In these cases, they are usually unstable and do not cause significant concern. In mental illness, on the contrary, concentrating on oneself and on the fight against them all the activity of the patient, they are experienced as extremely painful and painful. Depending on the degree of emotional saturation, firstly, abstract (abstract) obsessions are distinguished. They can be represented by obsessive sophistication (“thinking chewing gum”), obsessive counting ( arithmomania) .
Subjectively, they are perceived as painful and in this sense are "foreign bodies" of mental life. Most often, obsessive thoughts are observed in diseases of the neurotic circle, but they can also occur in practically healthy people with an anxious and suspicious nature, rigidity of mental processes. In these cases, they are usually unstable and do not cause significant concern. In mental illness, on the contrary, concentrating on oneself and on the fight against them all the activity of the patient, they are experienced as extremely painful and painful. Depending on the degree of emotional saturation, firstly, abstract (abstract) obsessions are distinguished. They can be represented by obsessive sophistication (“thinking chewing gum”), obsessive counting ( arithmomania) .
Emotionally intense obsessions include obsessive doubts and contrast obsessions. With them, patients can return home many times, experiencing anxious doubts whether they closed the door, turned off the gas, iron, etc. At the same time, they are well aware of the absurdity of their experiences, but they are unable to overcome the doubts that arise again and again. With contrasting obsessions, patients are seized with fear of doing something unacceptable, immoral, illegal. Despite all the burdensomeness of these experiences, patients never try to realize the impulses that have arisen.
At the same time, they are well aware of the absurdity of their experiences, but they are unable to overcome the doubts that arise again and again. With contrasting obsessions, patients are seized with fear of doing something unacceptable, immoral, illegal. Despite all the burdensomeness of these experiences, patients never try to realize the impulses that have arisen.
Obsessions are usually the ideational component of obsessive states and rarely occur in their pure form. Their structure also has an emotional component (obsessive fears - phobias), obsessive inclinations - compulsions , motor disorders - obsessive actions, rituals. In the most complete form, these violations are presented in the framework of obsessive-phobic syndrome . Obsessive fears (phobias) can have different content. With neurosis, they are most often understandable in nature, closely related to the real life situation of the patient: fears of pollution and infection ( mysophobia) , indoors ( claustrophobia ), crowds and open spaces ( agoraphobia) , death ( thanatophobia ). Most often there are obsessive fears of a serious illness ( nosophobia ), especially in cases provoked psychogenically: cardiophobia, carcinophobia, syphilophobia, speedophobia .
Most often there are obsessive fears of a serious illness ( nosophobia ), especially in cases provoked psychogenically: cardiophobia, carcinophobia, syphilophobia, speedophobia .
In schizophrenia, obsessive experiences often have an absurd, incomprehensible, out-of-life content - for example, thoughts that ptomaine, needles, pins may be present in food consumed; domestic insects can crawl into the ear, nose, enter the brain, etc.
Anxious and tense affect in these cases is quite often eased by rituals - original symbolic protective actions, the absurdity of which the patients can also understand, but their performance brings relief to the patients. For example, to distract themselves from obsessive thoughts about infection, patients wash their hands a certain number of times using soap of a certain color. To suppress claustrophobic thoughts, before entering the elevator, they turn around their axis three times. Such actions patients are forced to repeat many times with all the understanding of their meaninglessness.
Most often, obsessive-phobic syndrome is observed in obsessive-compulsive disorder. It can also occur within the framework of endogenous psychoses, for example, with neurosis-like debuts of schizophrenia, as well as with constitutional anomalies (psychasthenia).
One of the variants of obsessive-phobic syndrome is dysmorphophobic (dysmorphomanic) syndrome . At the same time, the patient's experiences are focused on the presence of either an imaginary or a real physical defect or deformity. They can be both intrusive fears and overvalued thoughts with a decrease or absence of a critical attitude, intense affect, secondary ideas of attitude, and incorrect behavior. In these cases, patients try to eliminate existing shortcomings on their own, for example, get rid of freckles with acid, fight excessive fullness by resorting to debilitating fasting, or turn to specialists in order to surgically eliminate the deformity that they think is existing.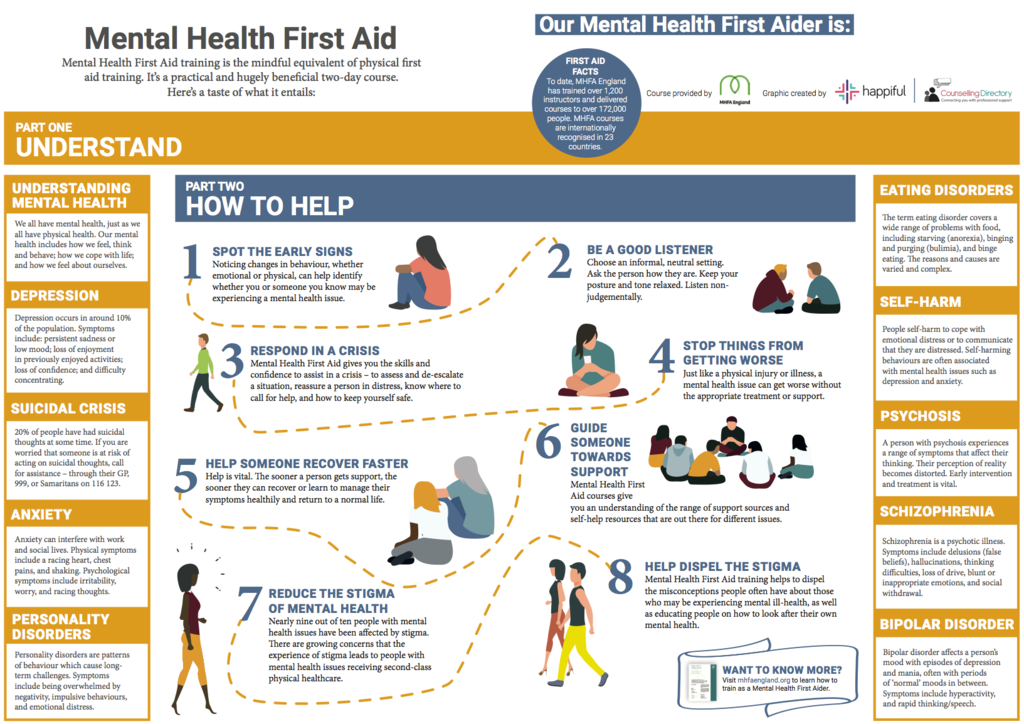
Dysmorphomania syndrome can be observed in abnormal personalities in adolescence and youth, more often in girls. They also often have similar syndromes - anorexia nervosa syndrome and hypochondriasis. The delusional variant of the dysmophomania syndrome is most typical for the debut manifestations of paranoid schizophrenia.
Disorders of thought
Disorders of thought are distinguished by form (disturbances in the associative process) and by content (overvalued ideas, delusions, obsessions).
Violations of the associative process
Acceleration of thinking is expressed in the accelerated flow of associative processes; thoughts very quickly replace each other, there are so many of them that the patients, despite very fast (“machine-gun”) speech, still do not have time to express them. Outwardly, such speech of patients may resemble schizophasia (broken speech), but if it is recorded, for example, on a tape recorder, then you can then find a certain meaning in it, which is not the case with schizophasia.
The pathologically accelerated course of associative processes is also characterized by distractibility: the patient's thinking becomes superficial, prone to instantaneous switching; everything that comes into the field of view of such a patient immediately attracts his attention, occupies his thoughts, gives a new direction to his ideas. The extreme degree of distractibility is expressed in a leap of ideas (fuga idearum), when the thoughts of patients, replacing each other with lightning speed, switch from one subject to another so quickly that it is already difficult to catch any general meaning in them.
Slowing down of thinking is characterized by the poverty of associations, the slowed down course of the associative process, its inhibition. Patients with such phenomena complain that they “have no thoughts in their heads for hours”, “nothing comes to mind”. They usually answer questions very succinctly, in monosyllables, sometimes only with the words “yes” or “no”, often after a very long pause, when the questioner may already have the impression that the patient did not hear or understand the question. Patients themselves in this state do not begin to speak, they do not turn to anyone for anything.
Patients themselves in this state do not begin to speak, they do not turn to anyone for anything.
Thoroughness of thinking lies in the extreme viscosity, stiffness of mental processes; it is very difficult for patients to switch from one topic to another, they get stuck on the most insignificant details, everything seems important to them, necessary - every little thing, every stroke; they cannot single out the main, basic, essential.
A patient with epilepsy, wishing to inform the doctor about another seizure, describes her condition as follows: “So, when I got up, I went to wash, there was no towel yet, it must have been taken by Ninka the Viper, I will remember it for her. While I was looking for a towel, I had to go to breakfast, and I also didn’t brush my teeth, the nanny says to me: “Go quickly,” and I told her about the towel, then I just fell, and I don’t remember what happened next.
The pathological thoroughness of thinking is characterized by very low productivity, sometimes it is not at all clear what the patient wanted to say, what was the meaning of his long ornate speech (labyrinth thinking).
Perseveration thinking (lat. perseveratio - perseverance, perseverance) - pathological stuck, delay in the same ideas, which is clinically expressed in the repetition (sometimes very long) of the same phrases or words. Most often, such patients can correctly answer only the first question of the doctor, and then repeat the same answer or parts of it in a monotonous manner.
A patient suffering from severe cerebral atherosclerosis is asked where he is being treated. The patient replies: "In the Solovyov hospital." - "How long have you been here?" - "Hospital Solovyov". - "What was your specialty before the illness?" - "Hospital Solovyov". -"What did you do today?" - "Hospital Solovyov".
Verbigeration (lat, verbum - word + gero - lead, perform) - speech stereotypy - senseless, often rhythmic repetition of the same words, less often - phrases or their fragments.
Paralogical thinking is characterized by the absence of a logical connection in thinking; the conclusions that the patient makes in such cases are not only illogical, but often completely absurd: “I fell ill with schizophrenia because I ate little semolina porridge as a child” or “I want to sleep, and therefore please teach me music. ”
”
Reasoning - a tendency to empty reasoning, when, as they say, "a lot of words and few thoughts." Such thinking is characterized by futility, lack of specificity, purposefulness: “You see how important this is, I would like to say and note that this is very important, the importance is significant, this should be noted, but you will not think that this is not important.”
Discontinuity thinking (schizophasia) is expressed in the lack of connection between individual thoughts or even individual words. The speech of such a patient can be completely incomprehensible, devoid of any meaning, and therefore it is often called verbal okroshka, verbal salad.
Paralogical thinking, reasoning and fragmentation of thinking are the most characteristic of schizophrenia.
Incoherence thinking (incoherence), incoherent thinking; lat. in - particle of denial + cohaerentia - adhesion, connection) is characterized by complete chaos, meaninglessness of thinking, speech consists of a set of separate words that are not connected in any way: “A miracle, a miracle . .. once upon a time ... oh, how cold .. day, stump, laziness... goodbye...». Incoherence may resemble broken thinking, but the main difference is that broken thinking occurs against the background of clear consciousness, while incoherence is always a consequence of clouding of consciousness (usually like an amental syndrome, amentia).
.. once upon a time ... oh, how cold .. day, stump, laziness... goodbye...». Incoherence may resemble broken thinking, but the main difference is that broken thinking occurs against the background of clear consciousness, while incoherence is always a consequence of clouding of consciousness (usually like an amental syndrome, amentia).
Disorders of thought in terms of content
Overvalued ideas (hyperquantivalent ideas: gr. hyper - over, over + lat. quantum - how much + valenti - strength) - thoughts that arise in connection with some real facts or events, but acquiring special significance for a person, determining all his behavior. They are characterized by great emotional richness, pronounced emotional reinforcement. For example, a person who really writes poetry and, perhaps, was once praised for this, begins to think that he is an extraordinary poet, extremely talented, brilliant, and behave accordingly. His non-recognition by those around him is regarded as the intrigues of ill-wishers, envy, misunderstanding, and in this conviction he no longer takes into account any real facts.
Such overvalued ideas of one's own exclusivity can also arise in connection with other extremely overestimated abilities: musical, vocal, writing. One's own propensity for scientific activity, invention, and reformism can also be overestimated. Overvalued ideas of a physical defect, an unfriendly attitude, litigation are possible.
A person who actually has a small cosmetic defect, for example, slightly protruding ears, believes that this is a tragedy of his whole life, that those around him treat him badly because of this, that all his failures are only in connection with this "ugliness" . Or someone really offended a person, and after that he can no longer think about anything else, all his thoughts, all his attention are directed only to this, he already sees only one thing in the most harmless actions of others and even in their benevolent actions. - the desire to infringe on his interests, offend him again. The same may apply to litigation (querulanism; lat. querulus - complaining) - a tendency to endless complaints sent to all kinds of instances, and the number of these instances is increasing, since in the end each instance (for example, a newspaper, a court, etc. ) .), where such a quarrel first complained, not recognizing his “rightness”, itself becomes the object of another complaint.
) .), where such a quarrel first complained, not recognizing his “rightness”, itself becomes the object of another complaint.
Overvalued ideas are especially characteristic of psychopathic personalities.
Delusional ideas (delusions) - incorrect conclusions, erroneous judgments, false conviction. From ordinary human delusions (for example, from superstition - belief in the existence of witches, sorcerers, "evil spirits") or from an incorrect assumption about the unfriendly attitude of others, delusions differ in the following:
- always arises on a painful basis, it is always a symptom of an illness;
- people are fully convinced of the validity of their erroneous ideas;
- delirium is not amenable to any correction, any dissuasion from outside;
- delusional beliefs are extremely important for the patient, one way or another they influence his behavior, determine his actions.
A simply deluded person (for example, due to lack of knowledge or peculiarities of upbringing, believing in “evil spirits”), with persistent dissuasion, can abandon his delusions, as well as a person who, for one reason or another, thinks about the bad attitude of others towards him.