Mental disorder pica
What It Is, Causes, Symptoms & Treatment
Overview
What is pica?
Pica is an eating disorder where a person compulsively eats things that aren’t food and don’t have any nutritional value or purpose. Depending on when and why a person does this, pica can be normal, expected and harmless. However, it can cause major problems if a person with this condition eats something toxic or dangerous.
Pronounced “PIKE-ah,” pica gets its name from a bird species, the Eurasian magpie (the formal Latin name for that species is Pica pica). This bird has a reputation for eating unusual objects.
Who does pica affect?
Pica can happen to anyone at any age but tends to happen in three specific groups of people:
- Young children, especially those under 6 years old.
- People who are pregnant.
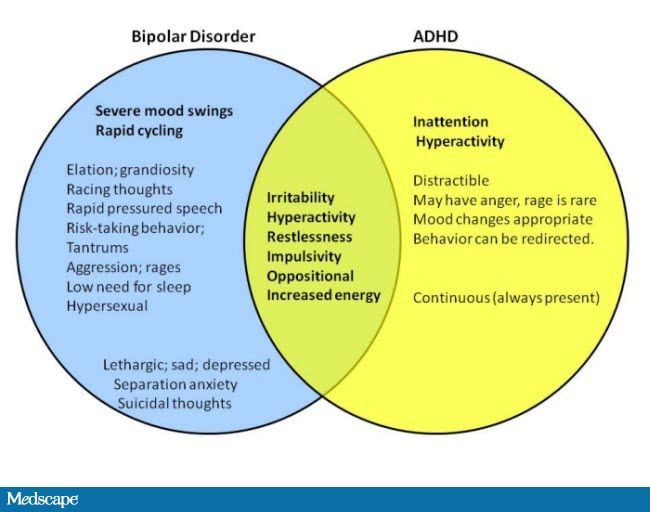
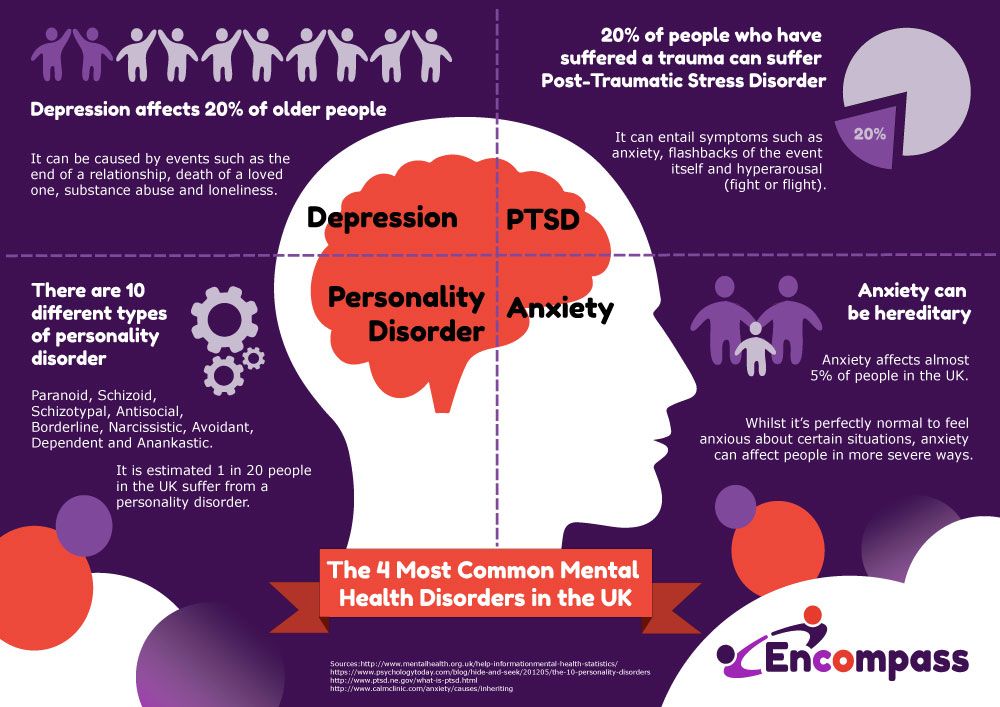
- People with certain mental health conditions, especially autism spectrum disorder, intellectual disabilities or schizophrenia.
How common is pica?
Pica is a relatively common condition, but experts aren’t sure exactly how common it is. That’s partly because research studies often don’t use the same definition for this condition.
It’s also common for healthcare providers to miss the condition entirely. This can happen when people don’t tell their doctor about it or don’t report signs of it in their children.
Yet another reason is that infants and young children often put things in their mouths, which is part of their normal development. This kind of pica usually goes away on its own very quickly.
How does this condition affect my body?
Pica is a condition where a person compulsively eats things that aren’t food and don’t have any nutritional value. Because it’s compulsive, people with this condition have a very hard time controlling the urge on their own.
Pica can have a wide range of effects depending on what non-food item(s) a person eats. For people who eat things like ice — a common behavior for someone who is pregnant — pica is harmless. For others, it can lead to eating dangerous or toxic items.
Depending on what you eat, pica can damage your teeth. It can also lead to dangerous problems even when you eat things that aren’t toxic. An example is when people eat hair (known as trichophagia), which can get stuck in their digestive tract, causing blockages, tearing or other damage.
Parasites that live in the soil can also infect people who eat dirt or clay (geophagia). People can also contract illnesses from eating feces (poop), especially pet feces that might contain parasites or other germs.
Mental health effects
People with pica often feel embarrassed or ashamed about this condition. Because of this, people with this condition often don’t seek treatment or are afraid to open up about it to their healthcare provider.
Symptoms and Causes
What are the symptoms of pica?
The sole symptom of pica is compulsively eating things that aren’t food or have no nutritional value or benefit. Most people with this condition prefer a single type of non-food item they eat.
However, pica can cause other conditions or issues, which have their own sets of symptoms. Other conditions that can happen because of pica include:
- Anemia (low iron).
- Ascariasis (roundworm infection).
- Constipation.
- Electrolyte imbalance.
- Irregular heart rhythms (arrhythmias).
- Lead poisoning.
- Small intestine and large intestine obstruction/blockage.
Common non-food items eaten
People with pica often eat the following:
- Ash.
- Baby or talcum powder.
- Chalk.
- Charcoal.
- Clay, dirt or soil.
- Coffee grounds.
- Eggshells.
- Feces (poop) of any kind.
- Hair, string or thread.
- Ice.
- Laundry starch.
- Paint chips.
- Paper.
- Pebbles.
- Pet food.
- Soap.
- Wool or cloth.
What causes pica?
Experts don’t know exactly why pica happens. However, researchers know certain factors increase the risk of developing it.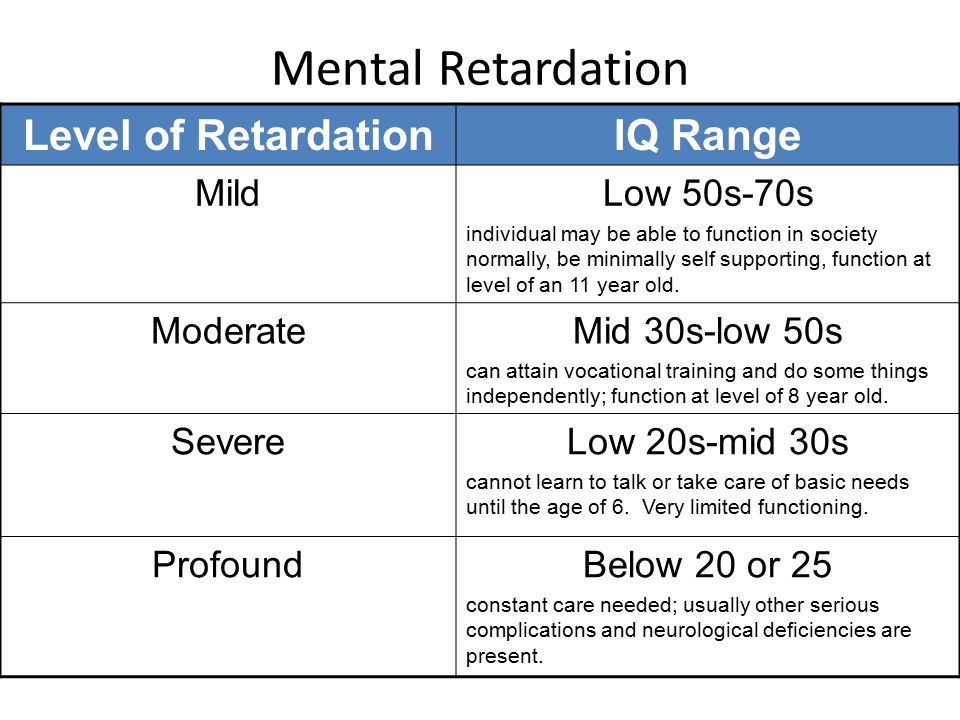
- Cultural or learned behaviors. Certain types of pica are common, socially accepted behaviors in certain cultures and religions. A religious example of this is the practice of eating dirt at El Santuario de Chimayó, a Roman Catholic shrine in New Mexico, USA. A cultural example of this commonly happens in cities in the country of South Africa, where it’s a common practice among young women.
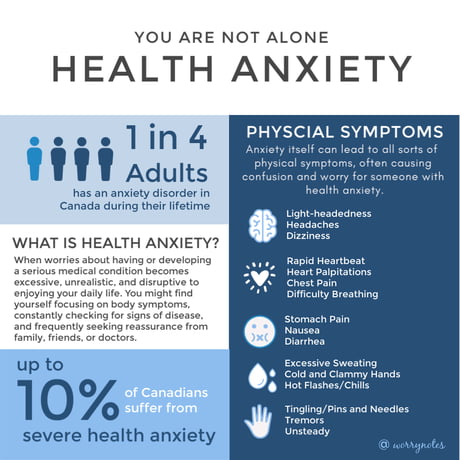
- Stress or anxiety. Pica might be an outlet or coping mechanism for people with these issues.
- Negative conditions during childhood. Pica is more common in children living in low socioeconomic situations (such as poverty), but why this happens is unknown. Some possible explanations include that pica is a coping mechanism for children to deal with situations of abuse or neglect. It also might be attention-seeking behavior, especially when one or both parents are absent for any reason.
- Nutritional deficiencies.
 People who show signs of pica often have mineral or other deficiencies in their diet. Iron (anemia), calcium and zinc deficiencies are some of the most common reasons people show these signs.
People who show signs of pica often have mineral or other deficiencies in their diet. Iron (anemia), calcium and zinc deficiencies are some of the most common reasons people show these signs. - Mental health conditions. These include conditions that a person might develop spontaneously, conditions they had at birth because of disruptions in how they developed in the womb and genetic disorders they inherited from their parents.
- Medical conditions. Pregnancy and sickle cell anemia are two conditions that have connections to pica.
- Certain medications increase the risk of someone developing pica or similar behaviors. But it’s unknown if these medications actually cause people to develop pica.
Diagnosis and Tests
How is pica diagnosed?
Diagnosing pica requires four criteria (with the mentioned exceptions explained after the list):
- Time. The diagnosis requires persistent eating items or substances with no food or nutrition value for at least one month.
- Mental development. This means a person has developed past a certain point mentally and should know not to eat things that aren’t food or have no nutritional value.
- No social and cultural factors. This means the person doesn’t have social or cultural background reasons to explain the behavior.
- No medical or mental health conditions. This means pica isn’t happening because of any other conditions.
Reasons to not diagnose pica
While pica is an extremely common behavior for several reasons, many of those also disqualify diagnosing it. These include:
- Cultural or social practices. True pica is a compulsive behavior that you can’t control. People with pica behaviors for cultural or social reasons have control of their actions.
- Nutritional deficiencies. People who have low iron or calcium deficiencies often try to compensate for these by eating non-food items.
 This is actually why pica is acceptable behavior in some cultures. People in certain places around the world eat clay or soil to make up for a lack of iron, calcium or other vitamins and minerals in their diet.
This is actually why pica is acceptable behavior in some cultures. People in certain places around the world eat clay or soil to make up for a lack of iron, calcium or other vitamins and minerals in their diet. - Other medical or mental health conditions. The criteria for diagnosing pica make exceptions for when it happens because of medical and mental health conditions. The only reason to diagnose pica in those circumstances is when it’s severe enough to cause health problems or need specific care.
What tests will be done to diagnose pica?
Most of the tests for pica are looking for problems that happen because of this condition. These can include a variety of lab, diagnostic and imaging tests, such as:
- Blood, urine (pee) and stool (poop) tests. These look for signs of infections, poisoning and electrolyte imbalances.
- Imaging tests. These are looking for any signs of blockage or internal damage from this condition.
 These can include X-rays, computerized tomography (CT) scans, magnetic resonance imaging (MRI), ultrasound and more.
These can include X-rays, computerized tomography (CT) scans, magnetic resonance imaging (MRI), ultrasound and more. - Diagnostic tests. These tests look for indications of serious health problems that can happen with pica. An example of one of these tests is an electrocardiogram (ECG or EKG), which looks for problems with your heart’s electrical rhythm that can happen with certain electrolyte imbalances or parasitic infections.
Management and Treatment
How is pica treated, and is there a cure?
Pica in people who are pregnant usually goes away on its own. Children also usually grow out of pica, especially as someone teaches them the difference between edible and non-edible items and objects. For children with intellectual disabilities (or other problems that interfere with learning), removing problematic items and supervision are both very important.
The main form of treatment for pica is therapy, with different therapy methods available depending on the situation and individual needs. A few therapy methods that are possible include:
A few therapy methods that are possible include:
- Mild aversive therapy. This method involves teaching people to avoid pica behaviors using mild aversions (consequences) to teach people to avoid non-food items and positively reinforcing (rewarding) healthy eating behaviors.
- Behavioral therapy. This therapy method involves teaching a person coping mechanisms and strategies to help them change their behavior.
- Differential reinforcement. In this method, people learn to avoid pica behaviors by focusing on other behaviors and activities.
What medications are used?
There are very few medications that are likely to help with pica. Antipsychotic medications might help, but the possible side effects usually keep these medications from seeing widespread use.
Complications/side effects of the treatment
There are very few complications that are possible with treatments for pica. If medications are part of the treatment, the possible side effects depend entirely on the medications themselves. Your healthcare provider is the best person to talk to about possible side effects, what to watch for and what you can do to help minimize their impact on your life.
Your healthcare provider is the best person to talk to about possible side effects, what to watch for and what you can do to help minimize their impact on your life.
How to take care of myself or manage symptoms?
Pica is a condition that’s usually benign but can become harmful depending on what a person eats. If you have pica, it’s important to have an honest discussion with your healthcare provider about it. They can offer guidance and resources to help you or refer you to a healthcare provider who has special training in this condition.
How soon after treatment will I feel better?
The recovery time for pica depends on the treatment and how well you do with it. Your healthcare provider is the person to ask for information about how long it’ll likely take for you to recover and what you can do to help the process happen smoothly.
Prevention
How can I prevent pica or reduce my risk of developing it?
Pica happens unpredictably, so there’s no way to prevent developing it. There’s also no way to reduce your risk of developing this condition.
There’s also no way to reduce your risk of developing this condition.
The only thing you can do that relates to pica is to make sure you eat a balanced diet and don’t have any deficiencies in essential vitamins or minerals. While this isn’t exactly prevention or reducing risk, because nutritional deficiencies don’t count toward a pica diagnosis, this is still important overall.
Outlook / Prognosis
What can I expect if I have this condition?
Pica is a condition that’s sometimes dangerous on its own, depending on what non-food items a person eats. The main risks with this condition are when people eat items that are:
- Toxic.
- Sharp-edged.
- A risk for blocking your digestive tract.
- That can cause infections, especially fungi, parasites, bacteria and viruses.
How long does this condition last?
Pica is technically a life-long condition because it’s not considered curable. People who stop the behavior, either through treatment or who stop on their own, are considered “in remission” as long as they don’t resume the behavior.
What’s the outlook for pica?
Pica very commonly goes away on its own in children and in people who are pregnant. The condition is usually benign (harmless) for people in these circumstances. The condition itself isn’t dangerous, but it can lead to people eating dangerous items. With treatment, this condition can go into remission, and people can live their lives without difficulty from it.
Living With
How do I take care of myself?
If you have pica, talking to your healthcare provider is an important first step in getting help for it. Their job is to help you while also making sure you feel safe and not judged. They can also help by offering you guidance directly or suggesting an expert who can.
If you have pica and it’s causing issues that affect your life, it’s important to keep the following in mind:
- Be honest with your healthcare provider. Pica can be a source of embarrassment or shame for many people. That can make it hard for them to talk about how this condition affects their lives.
 But pica is a mental health condition, meaning it’s a medical concern, just like a broken arm or a sinus infection. And, like those conditions, it’s good to ask for help and get treatment for this condition.
But pica is a mental health condition, meaning it’s a medical concern, just like a broken arm or a sinus infection. And, like those conditions, it’s good to ask for help and get treatment for this condition. - See your healthcare provider as recommended. Your healthcare provider can set up a schedule of visits as needed. As you progress in treatment, you’ll likely need to see them less and less. If this condition starts affecting your life again and you resume pica behaviors, you should return to your healthcare provider and resume treatment.
- Try to take away items or objects you commonly eat or make it inconvenient to get to them. One way to prevent or reduce pica behaviors is to remove problematic items or objects as much as possible. If removing them isn’t possible, try to make it inconvenient for you to return to pica behaviors.
When should I go to the ER?
Your healthcare provider can guide you in situations where you might need emergency medical care. Overall, you should seek medical attention if you have symptoms of more dangerous conditions, including the following:
Overall, you should seek medical attention if you have symptoms of more dangerous conditions, including the following:
- Ascariasis (roundworm infection).
- Electrolyte imbalance.
- Irregular heart rhythms (arrhythmias).
- Lead poisoning or other signs of toxic effects.
- Small intestine and large intestine obstruction/blockage.
You should also seek medical attention for children who swallow any potentially toxic or dangerous items. One example of this is any toy that involves small, magnetic objects, which can easily stick together in the digestive tract and cause life-threatening blockages.
A note from Cleveland Clinic
Pica is a very common condition around the world, especially in some circumstances. While it’s usually a condition that people grow out of or stop on their own, for some, it can be a serious problem. The greatest risk is for people who consume items that are toxic, sharp or that can block their digestive tract. Fortunately, mental healthcare treatments and techniques can help this condition go into remission. If you have pica, it’s normal to feel embarrassed about it. But your healthcare provider isn’t there to judge you. Their job is to help you get the care and resources you need to overcome this condition. That way, you can move on with your life and focus on the things that are most important or that you most enjoy.
Fortunately, mental healthcare treatments and techniques can help this condition go into remission. If you have pica, it’s normal to feel embarrassed about it. But your healthcare provider isn’t there to judge you. Their job is to help you get the care and resources you need to overcome this condition. That way, you can move on with your life and focus on the things that are most important or that you most enjoy.
What It Is, Causes, Symptoms & Treatment
Overview
What is pica?
Pica is an eating disorder where a person compulsively eats things that aren’t food and don’t have any nutritional value or purpose. Depending on when and why a person does this, pica can be normal, expected and harmless. However, it can cause major problems if a person with this condition eats something toxic or dangerous.
Pronounced “PIKE-ah,” pica gets its name from a bird species, the Eurasian magpie (the formal Latin name for that species is Pica pica). This bird has a reputation for eating unusual objects.
Who does pica affect?
Pica can happen to anyone at any age but tends to happen in three specific groups of people:
- Young children, especially those under 6 years old.
- People who are pregnant.
- People with certain mental health conditions, especially autism spectrum disorder, intellectual disabilities or schizophrenia.
How common is pica?
Pica is a relatively common condition, but experts aren’t sure exactly how common it is. That’s partly because research studies often don’t use the same definition for this condition.
It’s also common for healthcare providers to miss the condition entirely. This can happen when people don’t tell their doctor about it or don’t report signs of it in their children.
Yet another reason is that infants and young children often put things in their mouths, which is part of their normal development. This kind of pica usually goes away on its own very quickly.
How does this condition affect my body?
Pica is a condition where a person compulsively eats things that aren’t food and don’t have any nutritional value. Because it’s compulsive, people with this condition have a very hard time controlling the urge on their own.
Because it’s compulsive, people with this condition have a very hard time controlling the urge on their own.
Pica can have a wide range of effects depending on what non-food item(s) a person eats. For people who eat things like ice — a common behavior for someone who is pregnant — pica is harmless. For others, it can lead to eating dangerous or toxic items.
Depending on what you eat, pica can damage your teeth. It can also lead to dangerous problems even when you eat things that aren’t toxic. An example is when people eat hair (known as trichophagia), which can get stuck in their digestive tract, causing blockages, tearing or other damage.
Parasites that live in the soil can also infect people who eat dirt or clay (geophagia). People can also contract illnesses from eating feces (poop), especially pet feces that might contain parasites or other germs.
Mental health effects
People with pica often feel embarrassed or ashamed about this condition. Because of this, people with this condition often don’t seek treatment or are afraid to open up about it to their healthcare provider.
Symptoms and Causes
What are the symptoms of pica?
The sole symptom of pica is compulsively eating things that aren’t food or have no nutritional value or benefit. Most people with this condition prefer a single type of non-food item they eat.
However, pica can cause other conditions or issues, which have their own sets of symptoms. Other conditions that can happen because of pica include:
- Anemia (low iron).
- Ascariasis (roundworm infection).
- Constipation.
- Electrolyte imbalance.
- Irregular heart rhythms (arrhythmias).
- Lead poisoning.
- Small intestine and large intestine obstruction/blockage.
Common non-food items eaten
People with pica often eat the following:
- Ash.
- Baby or talcum powder.
- Chalk.
- Charcoal.
- Clay, dirt or soil.
- Coffee grounds.
- Eggshells.
- Feces (poop) of any kind.
- Hair, string or thread.
- Ice.
- Laundry starch.
- Paint chips.
- Paper.
- Pebbles.
- Pet food.
- Soap.
- Wool or cloth.
What causes pica?
Experts don’t know exactly why pica happens. However, researchers know certain factors increase the risk of developing it.
- Cultural or learned behaviors. Certain types of pica are common, socially accepted behaviors in certain cultures and religions. A religious example of this is the practice of eating dirt at El Santuario de Chimayó, a Roman Catholic shrine in New Mexico, USA. A cultural example of this commonly happens in cities in the country of South Africa, where it’s a common practice among young women.
- Stress or anxiety. Pica might be an outlet or coping mechanism for people with these issues.
- Negative conditions during childhood. Pica is more common in children living in low socioeconomic situations (such as poverty), but why this happens is unknown.
 Some possible explanations include that pica is a coping mechanism for children to deal with situations of abuse or neglect. It also might be attention-seeking behavior, especially when one or both parents are absent for any reason.
Some possible explanations include that pica is a coping mechanism for children to deal with situations of abuse or neglect. It also might be attention-seeking behavior, especially when one or both parents are absent for any reason. - Nutritional deficiencies. People who show signs of pica often have mineral or other deficiencies in their diet. Iron (anemia), calcium and zinc deficiencies are some of the most common reasons people show these signs.
- Mental health conditions. These include conditions that a person might develop spontaneously, conditions they had at birth because of disruptions in how they developed in the womb and genetic disorders they inherited from their parents.
- Medical conditions. Pregnancy and sickle cell anemia are two conditions that have connections to pica.
- Certain medications increase the risk of someone developing pica or similar behaviors. But it’s unknown if these medications actually cause people to develop pica.

Diagnosis and Tests
How is pica diagnosed?
Diagnosing pica requires four criteria (with the mentioned exceptions explained after the list):
- Time. The diagnosis requires persistent eating items or substances with no food or nutrition value for at least one month.
- Mental development. This means a person has developed past a certain point mentally and should know not to eat things that aren’t food or have no nutritional value.
- No social and cultural factors. This means the person doesn’t have social or cultural background reasons to explain the behavior.
- No medical or mental health conditions. This means pica isn’t happening because of any other conditions.
Reasons to not diagnose pica
While pica is an extremely common behavior for several reasons, many of those also disqualify diagnosing it. These include:
- Cultural or social practices.
 True pica is a compulsive behavior that you can’t control. People with pica behaviors for cultural or social reasons have control of their actions.
True pica is a compulsive behavior that you can’t control. People with pica behaviors for cultural or social reasons have control of their actions. - Nutritional deficiencies. People who have low iron or calcium deficiencies often try to compensate for these by eating non-food items. This is actually why pica is acceptable behavior in some cultures. People in certain places around the world eat clay or soil to make up for a lack of iron, calcium or other vitamins and minerals in their diet.
- Other medical or mental health conditions. The criteria for diagnosing pica make exceptions for when it happens because of medical and mental health conditions. The only reason to diagnose pica in those circumstances is when it’s severe enough to cause health problems or need specific care.
What tests will be done to diagnose pica?
Most of the tests for pica are looking for problems that happen because of this condition. These can include a variety of lab, diagnostic and imaging tests, such as:
- Blood, urine (pee) and stool (poop) tests.
 These look for signs of infections, poisoning and electrolyte imbalances.
These look for signs of infections, poisoning and electrolyte imbalances. - Imaging tests. These are looking for any signs of blockage or internal damage from this condition. These can include X-rays, computerized tomography (CT) scans, magnetic resonance imaging (MRI), ultrasound and more.
- Diagnostic tests. These tests look for indications of serious health problems that can happen with pica. An example of one of these tests is an electrocardiogram (ECG or EKG), which looks for problems with your heart’s electrical rhythm that can happen with certain electrolyte imbalances or parasitic infections.
Management and Treatment
How is pica treated, and is there a cure?
Pica in people who are pregnant usually goes away on its own. Children also usually grow out of pica, especially as someone teaches them the difference between edible and non-edible items and objects. For children with intellectual disabilities (or other problems that interfere with learning), removing problematic items and supervision are both very important.
The main form of treatment for pica is therapy, with different therapy methods available depending on the situation and individual needs. A few therapy methods that are possible include:
- Mild aversive therapy. This method involves teaching people to avoid pica behaviors using mild aversions (consequences) to teach people to avoid non-food items and positively reinforcing (rewarding) healthy eating behaviors.
- Behavioral therapy. This therapy method involves teaching a person coping mechanisms and strategies to help them change their behavior.
- Differential reinforcement. In this method, people learn to avoid pica behaviors by focusing on other behaviors and activities.
What medications are used?
There are very few medications that are likely to help with pica. Antipsychotic medications might help, but the possible side effects usually keep these medications from seeing widespread use.
Complications/side effects of the treatment
There are very few complications that are possible with treatments for pica. If medications are part of the treatment, the possible side effects depend entirely on the medications themselves. Your healthcare provider is the best person to talk to about possible side effects, what to watch for and what you can do to help minimize their impact on your life.
How to take care of myself or manage symptoms?
Pica is a condition that’s usually benign but can become harmful depending on what a person eats. If you have pica, it’s important to have an honest discussion with your healthcare provider about it. They can offer guidance and resources to help you or refer you to a healthcare provider who has special training in this condition.
How soon after treatment will I feel better?
The recovery time for pica depends on the treatment and how well you do with it. Your healthcare provider is the person to ask for information about how long it’ll likely take for you to recover and what you can do to help the process happen smoothly.
Prevention
How can I prevent pica or reduce my risk of developing it?
Pica happens unpredictably, so there’s no way to prevent developing it. There’s also no way to reduce your risk of developing this condition.
The only thing you can do that relates to pica is to make sure you eat a balanced diet and don’t have any deficiencies in essential vitamins or minerals. While this isn’t exactly prevention or reducing risk, because nutritional deficiencies don’t count toward a pica diagnosis, this is still important overall.
Outlook / Prognosis
What can I expect if I have this condition?
Pica is a condition that’s sometimes dangerous on its own, depending on what non-food items a person eats. The main risks with this condition are when people eat items that are:
- Toxic.
- Sharp-edged.
- A risk for blocking your digestive tract.
- That can cause infections, especially fungi, parasites, bacteria and viruses.
How long does this condition last?
Pica is technically a life-long condition because it’s not considered curable. People who stop the behavior, either through treatment or who stop on their own, are considered “in remission” as long as they don’t resume the behavior.
People who stop the behavior, either through treatment or who stop on their own, are considered “in remission” as long as they don’t resume the behavior.
What’s the outlook for pica?
Pica very commonly goes away on its own in children and in people who are pregnant. The condition is usually benign (harmless) for people in these circumstances. The condition itself isn’t dangerous, but it can lead to people eating dangerous items. With treatment, this condition can go into remission, and people can live their lives without difficulty from it.
Living With
How do I take care of myself?
If you have pica, talking to your healthcare provider is an important first step in getting help for it. Their job is to help you while also making sure you feel safe and not judged. They can also help by offering you guidance directly or suggesting an expert who can.
If you have pica and it’s causing issues that affect your life, it’s important to keep the following in mind:
- Be honest with your healthcare provider.
 Pica can be a source of embarrassment or shame for many people. That can make it hard for them to talk about how this condition affects their lives. But pica is a mental health condition, meaning it’s a medical concern, just like a broken arm or a sinus infection. And, like those conditions, it’s good to ask for help and get treatment for this condition.
Pica can be a source of embarrassment or shame for many people. That can make it hard for them to talk about how this condition affects their lives. But pica is a mental health condition, meaning it’s a medical concern, just like a broken arm or a sinus infection. And, like those conditions, it’s good to ask for help and get treatment for this condition. - See your healthcare provider as recommended. Your healthcare provider can set up a schedule of visits as needed. As you progress in treatment, you’ll likely need to see them less and less. If this condition starts affecting your life again and you resume pica behaviors, you should return to your healthcare provider and resume treatment.
- Try to take away items or objects you commonly eat or make it inconvenient to get to them. One way to prevent or reduce pica behaviors is to remove problematic items or objects as much as possible. If removing them isn’t possible, try to make it inconvenient for you to return to pica behaviors.

When should I go to the ER?
Your healthcare provider can guide you in situations where you might need emergency medical care. Overall, you should seek medical attention if you have symptoms of more dangerous conditions, including the following:
- Ascariasis (roundworm infection).
- Electrolyte imbalance.
- Irregular heart rhythms (arrhythmias).
- Lead poisoning or other signs of toxic effects.
- Small intestine and large intestine obstruction/blockage.
You should also seek medical attention for children who swallow any potentially toxic or dangerous items. One example of this is any toy that involves small, magnetic objects, which can easily stick together in the digestive tract and cause life-threatening blockages.
A note from Cleveland Clinic
Pica is a very common condition around the world, especially in some circumstances. While it’s usually a condition that people grow out of or stop on their own, for some, it can be a serious problem. The greatest risk is for people who consume items that are toxic, sharp or that can block their digestive tract. Fortunately, mental healthcare treatments and techniques can help this condition go into remission. If you have pica, it’s normal to feel embarrassed about it. But your healthcare provider isn’t there to judge you. Their job is to help you get the care and resources you need to overcome this condition. That way, you can move on with your life and focus on the things that are most important or that you most enjoy.
The greatest risk is for people who consume items that are toxic, sharp or that can block their digestive tract. Fortunately, mental healthcare treatments and techniques can help this condition go into remission. If you have pica, it’s normal to feel embarrassed about it. But your healthcare provider isn’t there to judge you. Their job is to help you get the care and resources you need to overcome this condition. That way, you can move on with your life and focus on the things that are most important or that you most enjoy.
Pick's disease. What is Pick's Disease?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Pick's disease is a variant of senile dementia with atrophic changes localized mainly in the temporal and frontal lobes of the brain. It is clinically manifested by a violation of behavior with antisocial inclinations and disinhibition of instincts, a progressive disintegration of cognitive functions. The list of diagnostic measures includes EEG, ultrasound of cerebral vessels, Echo-EG, psychiatric consultation, CT, SCT or MRI of the brain. The treatment consists in long-term use of anticholinesterase drugs, memantine, nootropics, but it does not prevent the complete intellectual-mnestic disintegration of the personality.
It is clinically manifested by a violation of behavior with antisocial inclinations and disinhibition of instincts, a progressive disintegration of cognitive functions. The list of diagnostic measures includes EEG, ultrasound of cerebral vessels, Echo-EG, psychiatric consultation, CT, SCT or MRI of the brain. The treatment consists in long-term use of anticholinesterase drugs, memantine, nootropics, but it does not prevent the complete intellectual-mnestic disintegration of the personality.
ICD-10
G31.0 Limited cerebral atrophy
- Causes of Pick's disease
- Symptoms of Pick's disease
- Pick's disease diagnostics
- Treatment and prognosis of Pick's disease
- Prices for treatment
General
Pick's disease is a rare type of frontotemporal dementia with a characteristic onset at the age of 50-60 years and predominant atrophy of the cortex of the temporal and frontal lobes of the brain.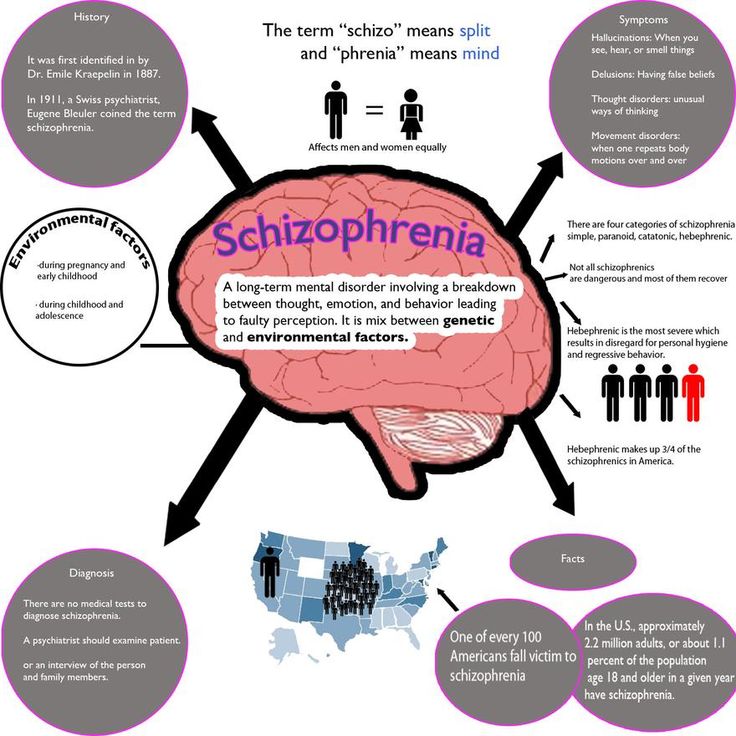 Named after the one who described it in 1892 d. Arnold Pick. Peak himself considered the pathology described by him to be only a separate clinical variant of senile dementia. However, later, after the identification of distinctive morphological features confirmed by pathoanatomical studies, Pick's disease was isolated as an independent nosology.
Named after the one who described it in 1892 d. Arnold Pick. Peak himself considered the pathology described by him to be only a separate clinical variant of senile dementia. However, later, after the identification of distinctive morphological features confirmed by pathoanatomical studies, Pick's disease was isolated as an independent nosology.
Data on the prevalence of the disease are not collected due to its rarity and difficulties in intravital diagnosis. There is evidence in the literature that Pick's dementia occurs 4 times less often than Alzheimer's disease. Men get sick a little less often than women. The steadily and rapidly progressing nature of the pathology, the difficulties of its diagnosis and therapy make Pick's disease an urgent problem of modern gerontology and neurology.
Pick's disease
Causes of Pick's disease
The etiology remains unclear. Familial cases of the disease lead researchers to think about its hereditary nature. However, sporadic cases are observed much more often than familial cases, and brothers and sisters are more likely to get sick within the same family than relatives in different generations. Among the possible etiofactors are long-term effects on the brain of harmful chemicals. This also includes the use of anesthesia, especially in cases of its frequent use or inadequate dosing. Some authors believe that Pick's disease may develop in connection with a previous mental disorder. Along with this, researchers are inclined to believe that factors such as intoxication, traumatic brain injury, infections, mental disorders, hypovitaminosis of vitamins gr. They play only a provocative role.
However, sporadic cases are observed much more often than familial cases, and brothers and sisters are more likely to get sick within the same family than relatives in different generations. Among the possible etiofactors are long-term effects on the brain of harmful chemicals. This also includes the use of anesthesia, especially in cases of its frequent use or inadequate dosing. Some authors believe that Pick's disease may develop in connection with a previous mental disorder. Along with this, researchers are inclined to believe that factors such as intoxication, traumatic brain injury, infections, mental disorders, hypovitaminosis of vitamins gr. They play only a provocative role.
Morphologically, atrophic processes are determined in the frontal and temporal lobes of the brain, often more pronounced in the dominant hemisphere. Atrophy affects both the cortex and subcortical structures. There are no inflammatory changes. Vascular disorders are not typical or mild. Senile plaques and neurofibrillary tangles typical of Alzheimer's disease are absent. Intraneuronal argentophilic inclusions are considered pathognomonic for Pick's disease.
Senile plaques and neurofibrillary tangles typical of Alzheimer's disease are absent. Intraneuronal argentophilic inclusions are considered pathognomonic for Pick's disease.
Symptoms of Pick's disease
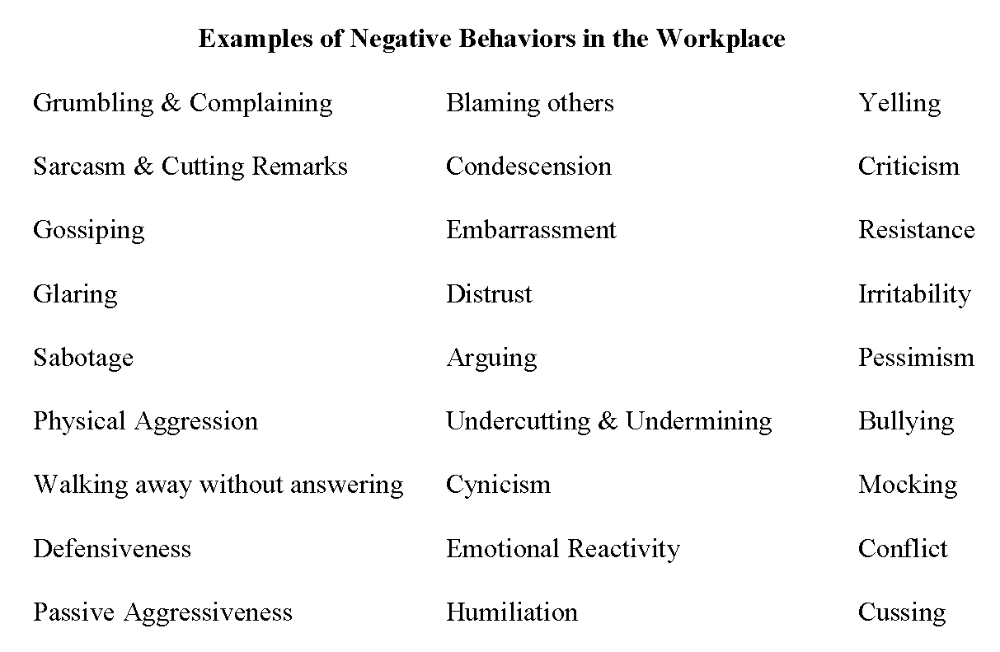
In its development, Pick's disease goes through 3 successive stages. In the initial stage, personality changes predominate with the loss of developed moral principles. The person becomes extremely selfish, antisocial behavior is observed. The disinhibition of instincts and the loss of control over one's actions lead to the immediate realization of the instinct (physiological needs, sexual desire), regardless of the environment and situation. The patient's criticism is significantly reduced and he explains his behavior by saying that he "couldn't resist", "it just happened", "I couldn't wait". Against this background, the development of bulimia, hypersexuality and other disorders is possible. Speech changes are reduced to multiple repetitions of words, phrases, jokes, stories or secrets (the symptom of "gramophone record"). There is euphoria or apathy.
There is euphoria or apathy.
The predominance of certain manifestations in the clinic of the initial period of Peak dementia depends on the localization of the emerging atrophic processes in the brain. Thus, basal frontal atrophy is accompanied by personality disorders, emotional instability, alternating periods of rigidity and disinhibition; convexital atrophy of the frontal lobe - a combination of asocial behavior with apathy and abulia - loss of motives and desires, complete lack of will. With the predominance of atrophy in the left hemisphere, behavioral disorders are manifested against the background of depression. Right hemispheric atrophy is characterized by inappropriate behavior combined with euphoria.
In the second stage, cognitive impairments appear and grow. There is sensorimotor aphasia - the patient cannot formulate his thoughts and loses the ability to understand the speech of others. There are alexia, agraphia and acalculia - loss of reading, writing and counting skills. Amnesia is noted - memory loss, agnosia - a change in the perception of the world and violations of praxis - the ability to consistently perform actions. Initially, cognitive dysfunction may be episodic, then it becomes permanent and progresses up to the complete intellectual destruction of the personality. In a number of patients, skin hyperalgesia (hypersensitivity) becomes a peculiar manifestation.
The third stage of Pick's disease is profound dementia. Patients are immobilized due to extreme apraxia, disoriented, unable to perform basic self-care activities, and need constant care. This condition leads to the death of patients due to cerebral insufficiency or intercurrent infections (infection of bedsores with the development of sepsis, congestive pneumonia, ascending pyelonephritis, etc.).
Pick's disease diagnostics
Of no small importance in the diagnosis is the questioning of the patient and his relatives, the study of anamnesis, and an objective examination. Pyramidal symptoms in the neurological status are not typical. When the subcortex is involved in the atrophic process, it is possible to identify signs of damage to the extrapyramidal system (hyperkinesis, manifestations of secondary parkinsonism). Somatic condition in stages 1-2 of Peak's dementia, as a rule, is satisfactory. In the course of diagnosis, Pick's disease should be differentiated from vascular dementia, Alzheimer's disease, intracerebral tumors localized in the frontal lobes, arteriovenous malformation of the brain, and schizophrenia.
Clinical data (age of onset of the disease, its manifestation from behavioral disorders followed by the addition of cognitive dysfunction, the absence of cerebral and pyramidal symptoms, etc.) allow the neurologist to suggest Pick's disease only in the second stage, when there are cognitive impairments. Behavioral changes that characterize the onset of the disease are often mistaken for mental disorders, in connection with which the patient's relatives first of all turn to a psychiatrist for help.
When conducting an EEG in patients with Pick's dementia, a decrease in the voltage of bioelectrical activity in the frontal leads is revealed. REG and transcranial ultrasound do not reveal significant vascular disorders. According to Echo-EG, moderate hydrocephalus can be diagnosed. Visualization of atrophic changes in the brain allows tomographic methods: CT, MSCT and MRI. MRI of the brain reveals thinning of the cortex, areas of atrophic decrease in the density of the medulla in the frontal and temporal lobes, and expansion of the subarachnoid spaces.
Treatment and prognosis of Pick's disease
Specific therapy has not been developed. The treatment regimen, as a rule, includes anticholinesterase pharmaceuticals (choline alfoscerate, galantamine, rivastigmine, donepezil), nootropics (piracetam, phenylpiracetam, gamma-aminobutyric acid), memantine. In the presence of aggressive behavior, antipsychotics are prescribed: alimemazine, chlorprothixene. In the initial stages, psychotherapy, participation in cognitive training, counseling by a psychologist are recommended; in later ones - a sensory room, art therapy, simulation of presence.
All of the above methods are aimed at slowing the progression of symptoms. However, their effectiveness in Pick's dementia is significantly lower than in Alzheimer's disease. Despite ongoing therapy, the state of deep dementia occurs on average 5-6 years after the onset of the disease. Life expectancy from the onset of the disease does not exceed 10 years.
Sources
- 0016
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Pick's disease: causes, features, treatment options
Pick's disease: causes, features, treatment optionsPanacea Medical Center
+7 (495) 373-20-18
Callback
- home
- Helpful information
- mental illness
- Causes, features and treatment options for Pick's disease
- Book a consultation
- Order a doctor's home visit
Pick's disease (frontotemporal dementia) is a neurodegenerative disease that leads to the early onset of dementia. The age of patients is from 55 years. The disease develops due to the destruction of the cerebral cortex. Deposits of a defective tau protein appear in the composition of neurons, which forms Pick's bodies. Because of these inclusions, neurons die, which provokes cognitive impairment. The process affects the frontal and temporal lobes, and this affects the course of the disease.
Make an appointment
Causes of the disease
The destruction of the cerebral cortex occurs due to deposits of tau protein, forming cytoplasmic inclusions called Pick bodies. They are formed as a result of a malfunction in its metabolism. This failure can occur under the influence of the following factors:
- genetic factor. In half of the cases, the disease is due to heredity. There are three genes whose mutations increase the risk of Pick's disease by 50%;
- toxic effect on brain cells as a result of the use of alcohol or drugs, taking certain drugs;
- traumatic effect, severe injuries as a result of infections affecting the brain tissue, or traumatic brain injury.
In some cases, Pick's disease is associated with oncological diseases, malnutrition, general disorders of metabolism, metabolism.
Do you have questions?
We will call you back within 30 seconds
Send
or call +7 (495) 373-20-18
By pressing the button "Send" , you automatically agree to the processing of your personal data and accept the terms of the User Agreement.
Features
Pick's disease has several typical symptoms:
- the disease appears at a relatively early age. If with Alzheimer's disease the average age of onset of dementia is 65 years, then with Pick's disease it is 55-56 years;
- the onset of the disease is gradual;
- specific onset of the disorder: the disease affects the frontal and temporal lobes of the brain. Because of this, personal changes appear first, while the functions of the intellect (memorization, recall, attention, orientation) are violated later. Because of this, the disease is often confused with age-related changes in character;
- motor activity decreases slightly, persists until the last stages of the disease.
Movement becomes monotonous. The course of Pick's disease does not affect the coordination of movements, fine motor skills, the ability to walk, and control physical actions.
Symptoms of Pick's disease:
Passivity. Gradually a person becomes less active, he does not show initiative, tries to avoid communication, reluctantly performs any work. The circle of his interests narrows. Apathy becomes almost permanent. Against this background, patients cease to take care of themselves, neglect personal hygiene.
Absence of criticism. Already at the initial stages of the disease, the patient ceases to adequately evaluate his actions, behavior, and the consequences of his actions. This looks like a sharp deterioration in character: a person behaves loosely, vulgarly, indecently, he can joke rudely, insult others, be rude to them. His own desires come to the fore for him, and because of this, he can consume too much alcohol, sweet, fatty, and show inappropriate sexual activity.
Planning problems. It becomes difficult to take deliberate, purposeful actions. As dementia develops, the patient loses the ability to plan his activities, to control it. There are problems with analysis and logic, generalization, formation of judgments. A person cannot set goals and achieve them. Even simple household chores become too difficult for him.
Speech disorders. In Pick's disease, the patient's speech is disturbed during the first two years of the disease: it becomes monosyllabic, simple, devoid of emotions. It is difficult for him to maintain a conversation, conduct a dialogue, follow the conversation, formulate and express thoughts. He prefers to express himself as simply as possible or shy away from communication. The less a person talks, participates in conversations, the more he limits his communication, the faster speech disorders progress.
The disease develops in three stages:
- initial stage.
Behavior changes, it becomes rude, selfish. There are problems with planning, which may look like disorganization or irresponsibility. Patients are often withdrawn, apathetic. If a diagnosis is made by a psychiatrist, thinking disorders are detected. At the same time, a person retains motor activity, he does not have ailments or specific symptoms;
- second stage. Self-control continues to decline, behavior becomes immoral, a person ceases to control his sexual and eating behavior. The patient ceases to recognize the emotions of others and respond to them. Speech becomes simple, rough, monosyllabic. Echolalia appears - the repetition of sent words, remarks, sounds. Thinking is simplified, problems with planning, regulation of activities become more pronounced;
- third stage: apathetic behavior, complete lack of activity, the person tries not to do anything at all. Speech is monosyllabic, the vocabulary is minimal, violations progress up to mutism (the patient stops responding to questions and appeals).
At this stage, there are violations of memory, orientation in time and space, movement disorders are formed (symptoms are similar to Parkinson's disease). The ability to self-care is lost.
Treatment options for Pick's disease
There is no specific treatment for Pick's disease, but patients receive pharmacotherapy to maintain functioning. Special rehabilitation techniques help slow down the development of the disease. Doctors of the medical center "Panacea" note that the treatment is most effective with early diagnosis of the disease. It must be comprehensive. As part of it, medication and physiotherapy, exercises and techniques, psychotherapeutic techniques aimed at correcting behavior and maintaining cognitive functions, and preventing memory loss can be used. The psychiatrist can additionally prescribe medications that correct behavior and emotional state.
Book a gerontologist visit
Experienced doctors. Treatment in a hospital or at home. Round-the-clock departure across Moscow and area. Professional, anonymous, secure.
- Online Dementia Consultation
- Factors that trigger dementia
- Factors that trigger alcoholism in the elderly
- Dementia with Lewy bodies
- Psychosis in the elderly
- Treatment of depression in the elderly 9015 Age-related changes in personality 016
- Early diagnosis of mental disorders in the elderly
- Senile aggression: why does it occur, what to do about it?
- Alcohol dementia
- Alcoholism in old age
- Mental disorders in the old age
- PICA disease
- Risk of dementia development
- Differential diagnostics in Alzheimer's disease
- behavioral and mental disorders ,
- Depression in older people
- Myths about treating depression
- Anxiety disorder
- Types of eating disorders
- Sleep disorders
- How to recognize depression?
- Neurotic disorders
- Risk factors and causes of depression
- Treatment of depression in hospital and at home
16
+7 (495) 373-20-18
I accept the user agreement and confirm that I have read and agree to the site's privacy policy. More.
Only until the end of this week!
The doctor will examine you and make a diagnosis. You will receive a treatment plan with terms and cost. If satisfied, you can immediately begin treatment.
30-40 minutes
free
Or call +7 (495) 373-20-18
We will contact you, find a convenient time for you and a highly qualified doctor.
By pressing the button "Send" , you automatically agree to the processing of your personal data and accept the terms User agreement.
Or call +7 (495) 373-20-18
We will contact you, find a convenient time for you and a highly qualified doctor.
Pressing button "Send" , you automatically agree to the processing of your personal data and accept the terms User agreement.